Abstract
Background:
Lower mortality and improved physical function following major polytrauma have been associated with treatment at level-I trauma centers compared with that at hospitals without a trauma center (nontrauma centers). This study investigated the impact of trauma-center care on outcomes after pelvic and acetabular injuries.
Methods:
Mortality and quality-of-life-related scores were compared among patients treated in eighteen level-I trauma centers and fifty-one nontrauma centers in fourteen U.S. states. Complete data were obtained on 829 adult trauma patients (eighteen to eighty-four years old) who had at least one pelvic ring or acetabular injury (Orthopaedic Trauma Association [OTA] classification of 61 or 62). We used inverse probability of treatment weighting to adjust for observable confounding.
Results:
After adjusting for case mix, we found that, for patients with more severe acetabular injuries (OTA 62-B or 62-C), in-hospital mortality was significantly lower at trauma centers compared with nontrauma centers (relative risk [RR], 0.10; 95% confidence interval [CI], 0.02 to 0.47), as was death within ninety days (RR, 0.10; 95% CI, 0.02 to 0.47) and within one year (RR, 0.21; 95% CI, 0.06 to 0.76). Patients with combined pelvic ring and acetabular injuries treated at a trauma center had lower mortality at ninety days (RR, 0.34; 95% CI, 0.14 to 0.82) and at one year (RR, 0.30; 95% CI, 0.14 to 0.68). Care at trauma centers was also associated with mortality risk reduction for those with unstable pelvic ring injuries (OTA 61-B or 61-C) at one year (RR, 0.71; 95% CI, 0.24 to 0.91). Seventy-eight percent of included subjects discharged alive were available for interview at twelve months. For those with more severe acetabular injuries, average absolute differences in the Short Form-36 (SF-36) physical function component and the Musculoskeletal Function Assessment at one year were 11.4 (95% CI, 5.3 to 17.4) and 13.2 (1.7 to 24.7), respectively, indicating statistically and clinically significant improved outcomes following treatment at a trauma center for those patients.
Conclusions:
Mortality was reduced for patients with unstable pelvic and severe acetabular injuries when care was provided in a trauma center compared with a nontrauma center. Moreover, those with severe acetabular fractures experienced improved physical function at one year. Patients with these injuries represent a well-defined subset of trauma patients for whom our findings suggest preferential triage or transfer to a level-I trauma center.
Level of Evidence:
Therapeutic Level III. See Instructions for Authors for a complete description of levels of evidence.
Critically injured trauma patients benefit from an organized trauma service and integrated multidisciplinary care1. Efforts at regionalization of trauma care have been based on the premise that the concentration of resources for the delivery of this complex specialty care will result in improved outcomes2,3. However, the majority of studies supporting this notion have been retrospective studies of registry data4. The National Study on Costs and Outcomes of Trauma (NSCOT) is a prospective study that was initiated to examine variations in care across level-I trauma centers and hospitals without a trauma center (nontrauma centers), to identify predictors of outcomes, and to estimate cost-effectiveness of trauma care5. The study (by E.M., F.P.R, G.J.J., and colleagues), showed that the risk of death was significantly lower when care to critically injured patients was provided in a level-I trauma center than when provided in a nontrauma center6. Although this study also demonstrated modest benefits associated with treatment at a level-I trauma center in terms of the physical functioning of patients with a major lower-limb injury, a similar benefit in terms of mortality was not found among patients across the broad spectrum of orthopaedic injuries7.
Patients with pelvic and acetabular injuries compose a subset of trauma patients with particularly high morbidity and mortality8-10. These injuries typically result from high-energy trauma and are often accompanied by severe hemorrhage and other potential life-threatening injuries. Given the complexity and multimodal needs of trauma patients with pelvic and acetabular injuries compared with other extremity trauma, we hypothesized that such patients would show significant mortality and functional benefits from trauma-center care. We conducted a secondary analysis of the NSCOT data to assess both the effect on mortality and functional outcomes among patients who received trauma-center care, specifically those with pelvic and acetabular injuries.
Materials and Methods
The NSCOT was conducted in fifteen regions, defined by contiguous Metropolitan Statistical Areas in fourteen states, using sampling procedures that have been previously described5. The Metropolitan Statistical Areas were selected from among the twenty-five largest such areas in nineteen states; excluded were those in which large nontrauma centers collectively treated annually fewer than seventy-five patients with major traumatic injury (an Injury Severity Score of >15 derived by ICD-9-CM [International Classification of Diseases, Ninth Revision, Clinical Modification] diagnostic codes)4. Within each Metropolitan Statistical Area, all level-I trauma centers and large nontrauma centers were identified, as were large nontrauma centers that annually treated at least twenty-five patients with major traumatic injury. Of the trauma centers included, thirteen were designated as such by the state and ten were verified by the American College of Surgeons Committee on Trauma (ACSCOT); five were recognized by both the state and ACSCOT. Level-II and level-III centers were not included. Ultimately, eighteen trauma centers and fifty-one nontrauma centers agreed to participate and received institutional review board approval to do so.
Patients
Patients were included if they were between the ages eighteen and eighty-four years and were treated for a moderate-to-severe injury (defined by at least one injury with a score of ≥3 on the Abbreviated Injury Scale [AIS])11 between July 2001 and November 2002. Patients who presented with no vital signs and were pronounced dead within thirty minutes of arrival were excluded, as were patients who delayed seeking treatment for more than twenty-four hours, were sixty-five years of age or older and had a first-listed diagnosis of hip fracture, had major burns, did not speak English or Spanish, were not a U.S. resident, or were incarcerated or homeless at the time of injury.
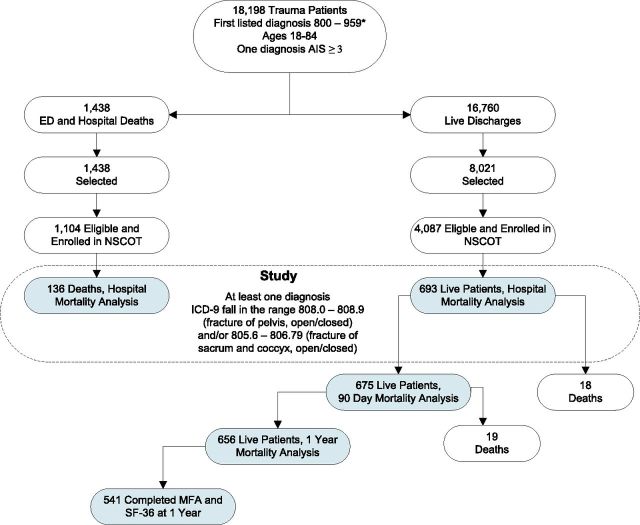
Patient selection and eligibility was determined in two stages, and for the present study, a third-stage query was used to identify and include only those subjects with pelvic and/or acetabular injuries (Fig. 1). In the first stage, administrative discharge records and emergency department logs were prospectively reviewed to identify patients with a principal ICD-9-CM diagnostic code of 800 to 959 (excluding those due to late effects, foreign bodies, complications, burns, and—among patients sixty-five years of age or older—hip fracture). A computer program was then used to map ICD-9-CM diagnoses to AIS scores to identify patients with at least one diagnosis involving an AIS score of ≥312. A total of 18,198 patients satisfied these initial eligibility criteria.
Fig. 1.
Flow of subject inclusion and follow-up. ED = emergency department, and MFA = Musculoskeletal Function Assessment.
In the second stage, all 1438 patients who died in the hospital and a sample of 8021 of the patients who were discharged alive were selected. A quota sampling strategy was used with the goal of enrolling approximately 3000 patients who were eighteen to sixty-four years of age and 1200 patients who were sixty-five to eighty-four years of age, evenly distributed across trauma centers and nontrauma centers and across categories of injury severity and principal region injured. Completed medical records were obtained for 1391 of the patients who died in the hospital. After exclusion of 287 who did not meet eligibility criteria, 1104 eligible deceased subjects were identified and their medical-record data were abstracted. Patients who were discharged alive and selected for the study were contacted at three months by mail and then by telephone, and informed consent was obtained to access their medical records and interview them at three and twelve months after injury. Of these 8021 patients who were selected for the study, 4866 were enrolled, and 4087 were ultimately found eligible; their complete medical-record data were abstracted.
For the purposes of this study, a third stage involved the inclusion only of patients with a traumatic pelvic ring and/or acetabular injury from among the emergency department and hospital deaths and the live discharges found eligible in stage 2. Patients with at least one ICD-9 diagnostic code in the range of 808.0 to 808.9 (fracture of pelvis, open/closed) and/or 805.6 to 806.79 (fracture of sacrum and coccyx, open/closed) and an Orthopaedic Trauma Association (OTA) fracture classification13 of 61 or 62 were selected for inclusion in the final cohort of this study. This resulted in the inclusion of 278 patients from nontrauma centers and 551 patients from level-I trauma centers.
It was necessary to weight data on these 829 participants with pelvic/acetabular injury and complete medical records to the population of eligible patients for two reasons: the sampling protocol selected all patients who died in the hospital but only a proportion of patients who were discharged alive, and not all patients selected for inclusion in the study were enrolled. The resulting “sampling” weights consist of the reciprocal product of two probabilities: the conditional probability of being selected and the probability of being enrolled and having data abstracted from the medical record given that the patient was selected. The target population for whom inferences were made in this secondary analysis of the NSCOT data consists of 2644 patients with a pelvic and/or acetabular injury who were projected to meet the inclusion criteria.
Outcomes
Outcomes of primary interest were death in the hospital and death within ninety days following injury. Deaths that occurred after discharge were identified either by interviewing a proxy or through a match with the National Death Index. Secondary outcomes were twelve-month follow-up functional assessments as measured with the Short Form-36 (SF-36)14 and the Musculoskeletal Function Assessment (MFA)15.
Statistical Analysis
All analyses were performed with use of data weighted to the population of eligible patients (n = 2644). To adjust for potential confounding bias by observable factors explaining differences in patients treated at trauma centers and those treated at nontrauma centers, the inverse probability of treatment weighting approach described by Robins et al.16 was used. Robust standard errors were computed to account for clustering within hospitals. We compared mortality risk both in-hospital and within ninety days; effects attributable to level of care were hypothesized to exist within this period of time from injury. Quality-of-life outcomes (SF-36 physical and mental component summary scores and MFA results) at one-year after injury were compared. We used SAS version 9.2 (SAS Institute, Cary, North Carolina) and R version 2.1.1 (R Foundation for Statistical Computing, Vienna, Austria) for all analyses.
Source of Funding
Funding for NSCOT came from a grant (R49/CCR316840) from the National Center for Injury Prevention and Control of the Centers for Disease Control and Prevention, and a grant (R01/AG20361) from the National Institute on Aging of the National Institutes for Health. No funding was received for the present investigation.
Results
On the basis of data weighted to the target population of 2644 eligible patients (1727 pelvic, 297 acetabular, and 620 combined injuries), 92% survived at least twelve months after injury. Compared with trauma-center patients, nontrauma-center patients were older, carried more comorbidities, and were more likely to be female and insured (Table I). Patients treated at a trauma center had a higher Injury Severity Score (ISS) and a lower motor score of the Glasgow Coma Scale (GCS) at the time of admission (Table I). Patients treated at a trauma center had higher AIS scores for nearly every anatomical region. After inverse probability of treatment-weighted adjustment of the population for reduction of confounding bias due to imbalances in covariates, the two groups were found to be similar (Table I). Only the sex of patients and AIS maximum scores for the abdominal, lower-extremity, and spine regions significantly differed between the two groups in the reweighted population, and these variables were subsequently adjusted for in the statistical analysis.
TABLE I.
Patient Characteristics*
| Before Adjustment |
After Adjustment |
||||||
| No. of Patients (Unweighted) | Nontrauma Center N = 278 (N = 638 Weighted) | Trauma Center N = 551 (N = 2006 Weighted) | P Value | Nontrauma Center N = 278 (N = 2331 Weighted) | Trauma Center N = 551 (N = 2520 Weighted) | P Value | |
| Age (yr) | |||||||
| Mean, SD | 58.3 ± 33.4 | 40.0 ± 31.1 | <0.0001 | 42.3 ± 63.3 | 42.2 ± 37.8 | 0.96 | |
| <55 | 494 | 35.6% | 81.9% | <0.0001 | 68.2% | 77.1% | 0.17 |
| 55-64 | 81 | 12.6% | 8.9% | 9.6% | 9.2% | ||
| 65-74 | 114 | 17.3% | 5.7% | 9.0% | 7.5% | ||
| 75-84 | 140 | 34.5% | 3.5% | 13.2% | 6.2% | ||
| Sex | <0.0001 | 0.003 | |||||
| Male | 451 | 33.5% | 63.7% | 41.8% | 62.4% | ||
| Female | 378 | 66.5% | 36.3% | 58.2% | 37.6% | ||
| Race | 0.09 | 0.87 | |||||
| Hispanic | 107 | 9.1% | 17.9% | 14.0% | 16.2% | ||
| Non-Hispanic, white | 594 | 81.9% | 61.8% | 70.5% | 64.9% | ||
| Non-Hispanic, non-white | 128 | 9.0% | 20.3% | 15.5% | 18.9% | ||
| Insurance | <0.0001 | 0.21 | |||||
| None | 162 | 10.7% | 30.6% | 18.4% | 27.5% | ||
| Medicare only | 183 | 38.2% | 6.9% | 16.3% | 10.5% | ||
| Medicare and private | 104 | 15.2% | 6.3% | 7.0% | 7.2% | ||
| Private | 295 | 26.4% | 46.3% | 41.5% | 45.4% | ||
| Medicaid | 52 | 4.7% | 5.3% | 10.0% | 4.8% | ||
| Other | 33 | 4.9% | 4.6% | 6.8% | 4.6% | ||
| Injury mechanism | 0.24 | 0.44 | |||||
| Penetrating | 35 | 3.1% | 5.5% | 7.4% | 4.8% | ||
| Blunt | 794 | 96.9% | 94.5% | 92.6% | 95.2% | ||
| First ED motor GCS | 0.0002 | 0.24 | |||||
| 6 | 636 | 93.3% | 75.5% | 73.3% | 78.5% | ||
| 4, 5 | 50 | 3.0% | 7.3% | 4.3% | 6.7% | ||
| 2, 3 | 13 | 0.4% | 1.8% | 1.6% | 1.6% | ||
| 1 (not paralyzed) | 49 | 0.8% | 4.2% | 1.5% | 3.9% | ||
| 1 (paralyzed) | 81 | 2.5% | 11.2% | 19.3% | 9.3% | ||
| Injury Severity Score | |||||||
| Mean, SD | 11.3 ±14.7 | 22.5 ± 22.3 | <0.0001 | 22.3 ± 44.8 | 21.0 ± 25.0 | 0.80 | |
| <16 | 348 | 77.4% | 34.6% | <0.0001 | 42.0% | 40.8% | 0.06 |
| 16-24 | 206 | 12.7% | 27.5% | 22.7% | 25.8% | ||
| 25-34 | 165 | 5.3% | 22.9% | 10.3% | 20.5% | ||
| >34 | 110 | 4.6% | 14.9% | 25.0% | 12.9% | ||
| Maximum AIS | <0.0001 | 0.44 | |||||
| ≤3 | 551 | 89.2% | 63.6% | 65.0% | 67.4% | ||
| 4 | 187 | 7.7% | 24.6% | 17.1% | 22.1% | ||
| 5, 6 | 91 | 3.1% | 11.8% | 17.9% | 10.5% | ||
| Maximum AIS ≥3 | |||||||
| Head region | 164 | 8.2% | 24.0% | <0.0001 | 28.0% | 21.7% | 0.54 |
| Face region | 23 | 1.0% | 3.3% | 0.05 | 3.0% | 3.0% | 0.98 |
| Thoracic region | 319 | 14.7% | 42.0% | <0.0001 | 40.9% | 37.9% | 0.75 |
| Abdominal region | 170 | 4.4% | 24.4% | <0.0001 | 11.8% | 21.3% | 0.02 |
| Upper-extremity region | 111 | 7.7% | 15.4% | 0.002 | 12.8% | 14.8% | 0.53 |
| Lower-extremity region | 487 | 39.5% | 70.5% | <0.0001 | 50.7% | 68.9% | 0.01 |
| Neck region | 2 | 0% | 0.7% | NA | 0.0% | 0.3% | NA |
| Spine region | 55 | 1.7% | 8.9% | 0.001 | 2.9% | 8.0% | 0.02 |
| External region | 3 | 0.4% | 0.4% | 0.90 | 0.7% | 0.3% | 0.58 |
| Charlson Comorbidity Index | <0.0001 | 0.07 | |||||
| 0 | 535 | 50.5% | 76.0% | 69.9% | 72.5% | ||
| 1 | 136 | 17.5% | 16.0% | 12.0% | 16.7% | ||
| 2 | 75 | 13.6% | 4.5% | 9.3% | 6.3% | ||
| ≥3 | 83 | 18.4% | 3.5% | 8.8% | 4.5% | ||
SD = standard deviation, ED = emergency department, GCS = Glasgow Coma Scale, AIS = Abbreviated Injury Scale, and NA = not applicable.
The unadjusted in-hospital mortality rate was higher for trauma centers (6.1% compared with 2.5%; p < 0.0001) but was lower within one year after injury (7.2% compared with 11.5%; p = 0.03) (see Appendix). These results were no longer significant after adjustment for case mix, although the relative risk (RR) reduction and 95% confidence interval (CI) suggested a trend toward lower overall one-year mortality with treatment at a trauma center (RR, 0.67; 95% CI, 0.44 to 1.01) (Table II). Stratification revealed that those with combined pelvic and acetabular injuries, unstable pelvic ring injuries (an OTA classification of 61-B or 61-C), or more severe acetabular fractures (OTA 62-B or 62-C) benefitted from trauma-center care.
TABLE II.
Adjusted Mortality Effect (Trauma Center vs. Nontrauma Center) by OTA Classification*
| Outcomes | Relative Risk (95% CI) |
| Hospital death | |
| All subjects | 1.39 (0.59-3.28) |
| Pelvis only | 1.89 (0.75-4.76) |
| Acetabulum only | 2.20 (0.26-18.63) |
| Combined injury | 0.51 (0.15-1.72) |
| Death within 90 days | |
| All subjects | 0.96 (0.64-1.46) |
| Pelvis only | 1.18 (0.60-2.31) |
| Acetabulum only | 4.04 (0.53-30.86) |
| Combined injury | 0.34 (0.14-0.82) |
| Death within 1 year | |
| All subjects | 0.67 (0.44-1.01) |
| Pelvis only | 0.71 (0.43-1.16) |
| Acetabulum only | 5.80 (0.80-42.01) |
| Combined injury | 0.30 (0.14-0.68) |
Among total cohort of patients with pelvic injuries (weighted number of patients = 1727), acetabular injuries (weighted number of patients = 297), or combined injuries (weighted number of patients = 620). Values calculated with use of a propensity score-based adjustment model including the following covariates: all demographic and injury characteristics listed in Table I as well as ED (emergency department) first shock, first ED assessment of pupils, midline shift, flail chest, open skull fracture, obesity, and paralysis along with relevant two-way interaction terms.
Patients with combined pelvic ring and acetabular injuries treated at a trauma center had lower mortality at ninety days (RR, 0.34; 95% CI, 0.14 to 0.82) and at one year (RR, 0.30; 95% CI, 0.14 to 0.68) (Table II). In-hospital mortality was significantly lower at trauma centers compared with nontrauma centers (RR, 0.10; 95% CI, 0.02 to 0.47), as was death within ninety days (RR, 0.10; 95% CI, 0.02 to 0.47) and one year (RR, 0.21; 95% CI, 0.06 to 0.76), for patients with more severe acetabular injuries (OTA 62-B or 62-C) (Table III).
TABLE III.
Adjusted Mortality Effect (Trauma Center vs. Nontrauma Center) by OTA Subclassification*
| Outcomes | Relative Risk (95% CI) |
| Hospital death | |
| Pelvic A-Type | 3.40 (1.23-9.39) |
| Pelvic B or C-Type | 0.90 (0.22-3.67) |
| Acetabular A-Type | 2.66 (0.32-22.15) |
| Acetabular B or C-Type | 0.10 (0.02-0.47) |
| Death within 90 days | |
| Pelvic A-Type | 1.08 (0.51-2.30) |
| Pelvic B or C-Type | 0.69 (0.23-2.06) |
| Acetabular A-Type | 5.17 (0.72-37.02) |
| Acetabular B or C-Type | 0.10 (0.02-0.47) |
| Death within 1 year | |
| Pelvic A-Type | 0.48 (0.26-0.91) |
| Pelvic B or C-Type | 0.71 (0.24-0.91) |
| Acetabular A-Type | 5.17 (0.72-37.02) |
| Acetabular B or C-Type | 0.21 (0.06-0.76) |
A-Type is stable with regard to pelvic ring disruption and involves a single column with regard to acetabular injury. B-Type is partially unstable with regard to pelvic ring disruption and includes a transverse component with regard to acetabular injury. C-Type is unstable with regard to pelvic ring disruption (complete disruption of the posterior arch) and involves complete articular injury of both columns with regard to the acetabulum. The weighted number of pelvic A-Type injuries was 1240; of pelvic B or C-Type, 941; of acetabular A-Type, 209; and of acetabular B or C-Type, 152. Thirty pelvic and eight acetabular injuries were not subclassified and were excluded from the stratified analysis.
The results for subjects with pelvic injuries or single-column acetabular fractures were mixed. Although patients with stable pelvic ring injuries (OTA 61-A) had a higher hospital mortality risk when treated at a trauma center compared with a nontrauma center, this association was reversed and favored trauma centers at one year (Table III). There was no association between trauma-center care and mortality among subjects with single-column (OTA 62-A) acetabular fractures. Patients with unstable pelvic ring injuries (OTA 61-B or 61-C) had RR reductions associated with trauma-center care that reached significance by one year (RR, 0.71; 95% CI, 0.24 to 0.91).
Seventy-eight percent of the patients who were discharged alive, eligible for inclusion in NSCOT, and included in the present study were successfully located and interviewed at twelve months (Fig. 1). For those with more severe acetabular injuries, mean differences in scores of the SF-36 physical component and the MFA at one year were 11.4 (95% CI, 5.3 to 17.4) and −13.2 (95% CI, −24.7 to −1.7), respectively, indicating statistically and clinically significant improved outcomes following treatment at a trauma center (Table IV).
TABLE IV.
Twelve-Month Adjusted Differences in Functional Outcomes (Trauma Center vs. Nontrauma Center)*
| SF-36 Physical Component† | SF-36 Mental Component† | MFA‡ | |
| Unstratified sample | 0.8 (−2.1 to 3.7) | 1.3 (−1.4 to 4.1) | 13.8 (−2.1 to 29.7) |
| Pelvic-only injury | 2.3 (−0.8 to 5.3) | 2.1 (−1.9 to 6.0) | 7.9 (−11.3 to 27.2) |
| Acetabular-only injury | −2.8 (−9.7 to 4.0) | −0.5 (−7.5 to 6.5) | 12.5 (−10.5 to 35.5) |
| Combined injury | 1.7 (−3.2 to 6.6) | 0.5 (−6.7 to 7.6) | 14.7 (−10.2 to 39.6) |
| OTA subclassification | |||
| Pelvic A-Type§ | 1.5 (−1.8 to 4.7) | 2.3 (−1.0 to 5.7) | 10.4 (−6.6 to 27.3) |
| Pelvic B or C-Type# | 2.9 (−7.1 to 12.9) | −0.7 (−8.5 to 7.1) | 16.3 (−10.3 to 42.8) |
| Acetabular A-Type§ | −2.8 (−10.5 to 4.8) | −4.1 (−11.2 to 3.1) | 9.4 (−13.3 to 32.1) |
| Acetabular B or C-Type# | 11.4 (5.3 to 17.4) | 3.8 (−1.7 to 9.3) | −13.2 (−24.7 to −1.7) |
Propensity score-based adjustment model including the following covariates: all demographic and injury characteristics listed in Table I as well as ED (emergency department) first shock, first ED assessment of pupils, midline shift, flail chest, open skull fracture, obesity, and paralysis along with relevant two-way interaction terms. Values are presented as the mean difference with the 95% confidence interval in parentheses.
A positive score implies improved quality of life.
Standardized Musculoskeletal Functional Assessment mobility subscale. A negative score implies less functional impairment.
A-Type is stable with regard to pelvic ring disruption and involves a single column with regard to acetabular injury.
B-Type is partially unstable with regard to pelvic ring disruption and includes a transverse component with regard to acetabular injury. C-Type is unstable with regard to pelvic ring disruption (complete disruption of the posterior arch) and involves complete articular injury of both columns with regard to the acetabulum.
Discussion
We studied the effects of trauma-center compared with nontrauma-center care on mortality and functional outcomes among patients in NSCOT who had experienced major traumatic injuries, including pelvic and/or acetabular injuries. It is important to note that the inferences drawn from the findings of the present study pertain only to the comparison of level-I compared with nontrauma centers. Conclusions about the relative performance of level-II and level-III centers cannot be drawn from these data. Despite treating more severely injured patients, trauma centers were associated with reduced risk of mortality for patients with combined pelvic and acetabular injuries and those with severe acetabular injuries. Moreover, the most critically injured patients experienced improved physical functioning at one year when care was provided in a trauma center.
These findings are consistent with a growing body of literature examining the effect of trauma-center care on mortality and functional outcome. One reason for the benefits of dedicated trauma-center care is the concentration of expertise cultivated by high volumes of severely injured patients17. Much work has focused on elucidating which subsets of severely injured trauma patients benefit most from trauma-center care given the ramifications that this knowledge would have on improving triage. An analysis of National Trauma Data Bank (NTDB) data including only those patients with severe cardiovascular, neurological, liver, or complex pelvic injuries demonstrated mortality and disablement benefits associated with level-I trauma-center care18. Patients with complex pelvic injuries had significantly better functional outcomes when treated at a level-I center. Similarly, a retrospective cohort analysis of data from 18,103 primary trauma admissions from the State of Ohio Trauma Registry demonstrated improved survival associated with level-I trauma-center care19. This survival advantage was present among those with an ISS of >15 as well as those with head and pelvic injuries.
Given that injuries to the pelvis and acetabulum represent among the most life-threatening of orthopaedic injuries, these injuries have been implicated as indicators of patients most likely to benefit from the expertise, experience, and multidisciplinary resources available at trauma centers. Injuries to the pelvis are associated with high rates of blood loss, morbidity, and mortality20-24, although relatively little has been written about these severe complications in the management of high-energy acetabular fracture. Magnussen et al. found that, when evaluating 289 high-energy isolated pelvic or acetabular injuries, similar rates of subjects required blood transfusion25. However, patients with combined pelvic and acetabular injuries among this cohort required transfusions at a significantly higher rate (57%) compared with that for either isolated pelvic (24%) or acetabular (35%) injuries. In the present study, we benefitted from the increased granularity of NSCOT data by which pelvic and acetabular injuries were classified according to the OTA classification scheme, enabling us to make more precise comparisons than would have been possible with use of NTDB and registry data. The large risk reductions for mortality associated with trauma-center care that we noted among those with combined pelvic and acetabular injuries, more severe acetabular fractures, and unstable pelvic ring injuries are consistent with the notion that patients with the most devastating pelvic injuries benefit from the resources and expertise available at a trauma center.
Fewer studies have been conducted on the benefit of trauma-center care with respect to functional outcomes or health-related quality of life. Demetriades et al. used NTDB data to show that patients with complex pelvic fractures (defined by ICD-9 codes 808.43 to 808.53) had significantly better functional outcomes (functional independence measure at discharge) when care was provided at a level-I trauma center compared with lower-level trauma center18. Unfortunately, measurement of function at the time of discharge is a problematic and inconsistent time point for analysis26. Gabbe and colleagues27 used twelve-month functional outcomes (Glasgow Outcome Scale-Extended) to show longer-term benefits of level-I trauma-center care among survivors of blunt major trauma (an ISS of >15). Although they reported inferior function associated with orthopaedic injuries, no subgroup analysis was conducted to assess whether patients with specific skeletal injuries benefitted more or less from trauma-center care. E.M. and colleagues analyzed functional outcomes among those with major lower-extremity trauma and found greater improvement in the physical component of the SF-36 and the MFA for those treated at a trauma center7. NSCOT patients with at least one injury to a lower limb (including the pelvis and acetabulum) with an AIS score of ≥3 points were included for analysis. In that substudy, as well as the parent NSCOT study6, there were trends toward relative trauma-center benefit for those with more severe trauma. However, the functional outcome of patients with specific pelvic and acetabular fractures was not explored separately. In the present study, we report improvement in prospectively obtained physical function measurements at one year associated with trauma-center care, specifically among those with the most severe acetabular injuries, a finding that is consistent with these prior studies.
Regarding subjects with less severe injuries, such as a stable pelvic ring injury (61-A) or a single-column acetabular injury (62-A), the findings were less consistent. For the latter, there was no significant trauma-center mortality effect at any time point, whereas for stable pelvic ring injuries, the association reversed from favoring nontrauma centers in-hospital to favoring trauma centers at one year. Adjustment for case mix was studied by Nathens et al. and—at least with respect to mortality outcomes—the consideration of ISS, age, systolic blood pressure at emergency department arrival, presence of a severe head injury or severe abdominal injury (as measured by AIS), mechanism of injury, and sex have been regarded as sufficient28. Still, one possible reason for the inconsistent effects over time for patients with stable pelvic injuries is incomplete confounding adjustment for the disproportionately more severe injuries at trauma centers and older subjects with more comorbidities at nontrauma centers (Table I). The findings presented here do not support recommendations to preferentially triage patients with stable A-Type pelvic or acetabular injuries to trauma-center care.
This study had several potential limitations. First, it was observational and, despite sophisticated sampling and confounding adjustment to enhance causal inferences, it is still prone to bias from unknown or unmeasured confounding. Second, multiple subgroup analyses were run, which could have inflated the possible false-positive rate for the hypothesis tests we conducted. Still, this study used high-quality, prospectively gathered data for what we believe is the largest study of its kind to assess the relationships between trauma-center versus nontrauma-center care and outcomes.
Appendix
A table showing unadjusted mortality rates is available with the online version of this article as a data supplement at jbjs.org.
Footnotes
Investigation performed at the Orthopaedic Trauma Institute, Departments of Orthopaedic Surgery and of Epidemiology and Biostatistics, San Francisco General Hospital and University of California, San Francisco, California, and University of Washington School of Medicine, Seattle, Washington
A commentary by James P. Stannard, MD, is linked to the online version of this article at jbjs.org.
Disclosure: None of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of any aspect of this work. None of the authors, or their institution(s), have had any financial relationship, in the thirty-six months prior to submission of this work, with any entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. Also, no author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Dalal SA, Burgess AR, Siegel JH, Young JW, Brumback RJ, Poka A, Dunham CM, Gens D, Bathon H. Pelvic fracture in multiple trauma: classification by mechanism is key to pattern of organ injury, resuscitative requirements, and outcome. J Trauma. 1989. July;29(7):981-1000; discussion 1000-2. [PubMed] [Google Scholar]
- 2.West JG, Trunkey DD, Lim RC. Systems of trauma care. A study of two counties. Arch Surg. 1979. April;114(4):455-60. [DOI] [PubMed] [Google Scholar]
- 3.West JG, Williams MJ, Trunkey DD, Wolferth CC., Jr Trauma systems. Current status—future challenges. JAMA. 1988. June 24;259(24):3597-600. [DOI] [PubMed] [Google Scholar]
- 4.Mann NC, Mullins RJ, MacKenzie EJ, Jurkovich GJ, Mock CN. Systematic review of published evidence regarding trauma system effectiveness. J Trauma. 1999. September;47(3)(Suppl):S25-33. [DOI] [PubMed] [Google Scholar]
- 5.Mackenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, Salkever DS, Weir S, Scharfstein DO. The National Study on Costs and Outcomes of Trauma. J Trauma. 2007. December;63(6)(Suppl):S54-67; discussion S81-6. [DOI] [PubMed] [Google Scholar]
- 6.MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, Salkever DS, Scharfstein DO. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006. January 26;354(4):366-78. [DOI] [PubMed] [Google Scholar]
- 7.Mackenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Egleston BL, Salkever DS, Frey KP, Scharfstein DO. The impact of trauma-center care on functional outcomes following major lower-limb trauma. J Bone Joint Surg Am. 2008. January;90(1):101-9. [DOI] [PubMed] [Google Scholar]
- 8.Grotz MR, Allami MK, Harwood P, Pape HC, Krettek C, Giannoudis PV. Open pelvic fractures: epidemiology, current concepts of management and outcome. Injury. 2005. January;36(1):1-13. [DOI] [PubMed] [Google Scholar]
- 9.Suzuki T, Smith WR, Hak DJ, Stahel PF, Baron AJ, Gillani SA, Morgan SJ. Combined injuries of the pelvis and acetabulum: nature of a devastating dyad. J Orthop Trauma. 2010. May;24(5):303-8. [DOI] [PubMed] [Google Scholar]
- 10.van Vugt AB, van Kampen A. An unstable pelvic ring. The killing fracture. J Bone Joint Surg Br. 2006. April;88(4):427-33. [DOI] [PubMed] [Google Scholar]
- 11.Committee on Injury Scaling. The abbreviated injury scale: 1998 revision (AIS-98). Des Plaines, IL: Association for the Advancement of Automotive Medicine; 1998. [Google Scholar]
- 12.MacKenzie EJ, Steinwachs DM, Shankar B. Classifying trauma severity based on hospital discharge diagnoses. Validation of an ICD-9CM to AIS-85 conversion table. Med Care. 1989. April;27(4):412-22. [DOI] [PubMed] [Google Scholar]
- 13.Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B, Audigé L. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007. Nov-Dec;21(10)(Suppl):S1-133. [DOI] [PubMed] [Google Scholar]
- 14.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992. June;30(6):473-83. [PubMed] [Google Scholar]
- 15.Engelberg R, Martin DP, Agel J, Obremsky W, Coronado G, Swiontkowski MF. Musculoskeletal Function Assessment instrument: criterion and construct validity. J Orthop Res. 1996. March;14(2):182-92. [DOI] [PubMed] [Google Scholar]
- 16.Robins JM, Hernán MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000. September;11(5):550-60. [DOI] [PubMed] [Google Scholar]
- 17.Nathens AB, Jurkovich GJ, Maier RV, Grossman DC, MacKenzie EJ, Moore M, Rivara FP. Relationship between trauma center volume and outcomes. JAMA. 2001. March 7;285(9):1164-71. [DOI] [PubMed] [Google Scholar]
- 18.Demetriades D, Martin M, Salim A, Rhee P, Brown C, Chan L. The effect of trauma center designation and trauma volume on outcome in specific severe injuries. Ann Surg. 2005. October;242(4):512-7; discussion 517-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cudnik MT, Newgard CD, Sayre MR, Steinberg SM. Level I versus Level II trauma centers: an outcomes-based assessment. J Trauma. 2009. May;66(5):1321-6. [DOI] [PubMed] [Google Scholar]
- 20.Demetriades D, Karaiskakis M, Toutouzas K, Alo K, Velmahos G, Chan L. Pelvic fractures: epidemiology and predictors of associated abdominal injuries and outcomes. J Am Coll Surg. 2002. July;195(1):1-10. [DOI] [PubMed] [Google Scholar]
- 21.Ben-Menachem Y, Coldwell DM, Young JW, Burgess AR. Hemorrhage associated with pelvic fractures: causes, diagnosis, and emergent management. AJR Am J Roentgenol. 1991. November;157(5):1005-14. [DOI] [PubMed] [Google Scholar]
- 22.Burgess AR, Eastridge BJ, Young JW, Ellison TS, Ellison PS, Jr, Poka A, Bathon GH, Brumback RJ. Pelvic ring disruptions: effective classification system and treatment protocols. J Trauma. 1990. July;30(7):848-56. [PubMed] [Google Scholar]
- 23.Letournel E, Judet R. Fractures of the acetabulum. 2nd ed. New York: Springer-Verlag; 1993. [Google Scholar]
- 24.Pennal GF, Tile M, Waddell JP, Garside H. Pelvic disruption: assessment and classification. Clin Orthop Relat Res. 1980. September;(151):12-21. [PubMed] [Google Scholar]
- 25.Magnussen RA, Tressler MA, Obremskey WT, Kregor PJ. Predicting blood loss in isolated pelvic and acetabular high-energy trauma. J Orthop Trauma. 2007. October;21(9):603-7. [DOI] [PubMed] [Google Scholar]
- 26.Gabbe BJ, Simpson PM, Sutherland AM, Williamson OD, Judson R, Kossmann T, Cameron PA. Functional measures at discharge: are they useful predictors of longer term outcomes for trauma registries? Ann Surg. 2008. May;247(5):854-9. [DOI] [PubMed] [Google Scholar]
- 27.Gabbe BJ, Simpson PM, Sutherland AM, Wolfe R, Fitzgerald MC, Judson R, Cameron PA. Improved functional outcomes for major trauma patients in a regionalized, inclusive trauma system. Ann Surg. 2012. June;255(6):1009-15. [DOI] [PubMed] [Google Scholar]
- 28.Nathens AB, Xiong W, Shafi S. Ranking of trauma center performance: the bare essentials. J Trauma. 2008. September;65(3):628-35. [DOI] [PubMed] [Google Scholar]