Abstract
Background:
Patellar resurfacing after routine arthroplasty remains controversial. Few studies have specifically examined the effect of patellar resurfacing on outcomes after resection of the distal part of the femur and reconstruction with a megaprosthesis. Our objective was to compare the outcomes of megaprosthesis reconstructions of the distal part of the femur with and without patellar resurfacing after resection of a distal femoral tumor.
Methods:
We retrospectively reviewed the clinical records of patients with a femoral tumor who underwent resection of the distal part of the femur and endoprosthetic reconstruction between 1993 and 2013. We excluded patients who had had extra-articular knee resection, patellectomy, revision, reconstruction with an expandable prosthesis, or a proximal tibial replacement associated with the distal femoral replacement. We compared demographic characteristics, surgical variables, anterior knee pain, range of motion, extensor lag, Insall-Salvati ratio, Insall-Salvati patellar tendon insertion ratio, impingement, patellar degenerative disease, additional patellar procedures, complications, and Musculoskeletal Tumor Society (MSTS) score between the patellar resurfacing and nonresurfacing groups.
Results:
One hundred and eight patients—sixty without patellar resurfacing and forty-eight with patellar resurfacing—were included in the study. The mean age was 33.9 years (range, twelve to seventy-five years). There were fifty-four men and fifty-four women. The mean duration of follow-up was 4.5 years (range, 0.7 to twenty years). There was no significant difference in anterior knee pain between the groups (p = 0.51). Anterior knee pain did not significantly affect the range of motion, extensor lag, or reoperation or complication rate. Patellar degenerative disease occurred in 48% of the nonresurfaced knees but was not associated with focal pain. Complication rates were similar in the two groups, although peripatellar calcifications were significantly more common in the resurfacing group (19% versus 2%; p = 0.005). There was no significant difference in the mean MSTS score between the nonresurfacing (81%) and resurfacing (71%) groups (p = 0.34).
Conclusions:
There were no differences in anterior knee pain, range of motion, extensor lag, or MSTS score between the patients with and those without patellar resurfacing. There were no cases of patellar component loosening or revision. In light of the similar outcomes in the two groups, the decision to resurface should be left up to the individual surgeon, who should take into account preoperative peripatellar pain and the status of the patella at the time of resection.
Level of Evidence:
Therapeutic Level III. See Instructions for Authors for a complete description of levels of evidence.
The efficacy of patellar resurfacing in improving knee function after knee replacement remains unclear1. Patellar resurfacing has been associated with extensor mechanism failure2, and while some authors have proposed that patellar resurfacing decreases anterior knee pain3 others have determined that the prevalence of anterior knee pain in resurfaced and nonresurfaced patellae is the same4. Furthermore, it has been shown that patients who do not undergo patellar resurfacing have more knee operations than patients who do undergo patellar resurfacing4.
Distal femoral resection and endoprosthetic reconstruction performed for malignant tumors of bone differ significantly from total knee arthroplasty performed to treat osteoarthritis. Patients undergoing arthroplasty following femoral tumor resection tend to be younger; more bone and soft tissue are removed; and the reconstruction is done with constrained rotating-hinge devices, which have a distinct mechanical behavior and limited function. Complications related to the extensor mechanism are frequent after distal femoral resections5, and restoration of the articular line is more difficult6. Patella baja can cause impingement, pain, and a decreased range of motion. Few studies have focused on the patellofemoral joint after distal femoral tumor resection5,7. Because patients with neoplastic disease are often young and young people generally have minimal degenerative changes in the patellar cartilage, the question arises: is routine patellar resurfacing needed or does it lead to additional procedures following the arthroplasty?
The purpose of this study was to determine the effects of patellar resurfacing on the clinical, radiographic, and functional outcomes of patients who underwent distal femoral resection for a femoral tumor and megaprosthesis reconstruction.
Materials and Methods
After institutional review board approval was obtained for this retrospective cohort study, we reviewed the medical records of patients who had undergone primary distal femoral resection and reconstruction with a megaprosthesis at our institution from 1993 to 2013. We excluded patients who underwent extra-articular knee resection, revision, patellectomy, reconstruction with an expandable prosthesis, or proximal tibial replacement associated with the distal femoral replacement. We also excluded patients when imaging and/or clinical data were incomplete. However, we included patients when only the body mass index was missing from the data.
One year was chosen as the minimum follow-up time because most patients have completed both their chemotherapy and rehabilitation by one year and their functional condition has stabilized. If the patient later underwent a revision of the prosthesis, isolated patellar resurfacing or revision, or amputation, the last follow-up visit was defined as the last one before that procedure. Patients who underwent isolated patellar resurfacing or revision after the primary procedure were included even if their follow-up time was less than one year.
The patients were analyzed according to their treatment group: patellar resurfacing or nonresurfacing. The primary functional outcomes that were compared between those groups were anterior knee pain, range of motion, and extensor lag, which were determined from the last clinical record available.
Anterior knee pain was graded according to the criteria of Waters and Bentley3, with Grade 0 indicating no pain, Grade I indicating mild pain (does not interfere with daily activities), Grade II indicating moderate pain (patient not considering additional surgery), and Grade III indicating severe pain (patient considering additional surgery).
We collected data on variables that could have a direct or indirect impact on anterior knee pain, range of motion, and anterior knee pain (Table I). These confounding variables were included in the multivariate linear regression model (Table I).
TABLE I.
Variables Included in the Study
| Primary outcome variables | Anterior knee pain*, range of motion*, extensor lag* |
| General and other variables | |
| Patient variables | Age*, sex, diagnosis, body mass index*, follow-up time* |
| Surgical variables | Patellar surface*, mean amount (%) of femoral resection*, type of prosthesis*, surgical approach* |
| Patellar height | Insall-Salvati ratio*, Insall-Salvati patellar tendon insertion ratio* |
| Complications | Instability feeling, patellar clunk, patellar subluxation/dislocation, patellar impingement*, articular patellar degeneration |
| Other patellar complications observed and not listed above* | Distal or proximal patellar calcification, arthrofibrosis, patellar fracture, patellar crepitus, chronic synovitis, heterotopic ossification, effusion |
| Complications of limb-sparing reconstruction according to ISOLS classification* | Soft-tissue failure, aseptic loosening, prosthesis structural failure, infection |
| Patellar procedures* | Resurfacing, patellar component revision, other procedures |
| Functional score | MSTS |
Included in multivariate linear regression model for anterior knee pain, range of motion, and extensor lag.
Patellar height was defined by the Insall-Salvati ratio and the Insall-Salvati patellar tendon insertion ratio (Figs. 1-A and 1-B). Both ratios were based on the last lateral radiographs made with the knee in flexion (20° to 70°)8,9. Patients presenting with patella baja (Insall-Salvati ratio of <0.8) were analyzed to determine whether patella baja was associated with the range of motion, anterior knee pain, or impingement.
Figs. 1-A and 1-B A case of patellar impingement and distal patellar calcification. LP = length of the patella, HI = height of the insertion, LT = length of the tendon, ISR = Insall-Salvati ratio, and PTR = patellar tendon insertion ratio.
Fig. 1-A.
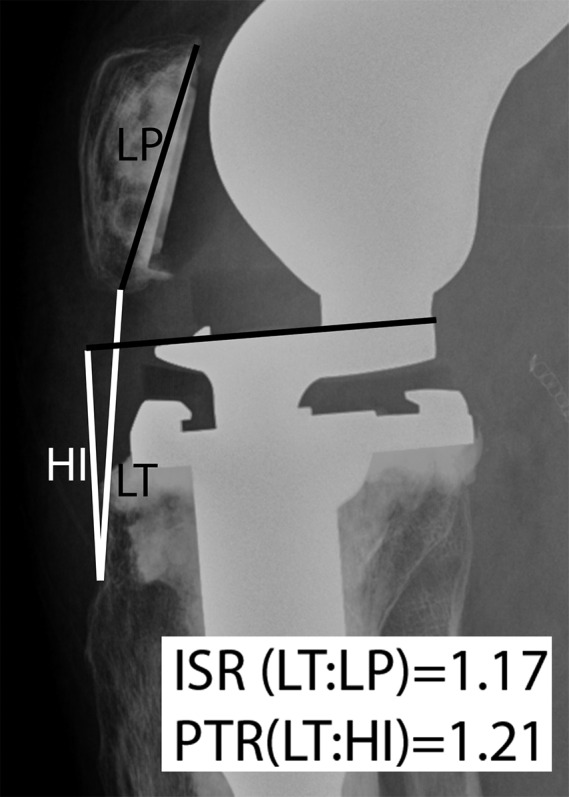
Lateral knee radiograph made two months after the femoral replacement.
Fig. 1-B.
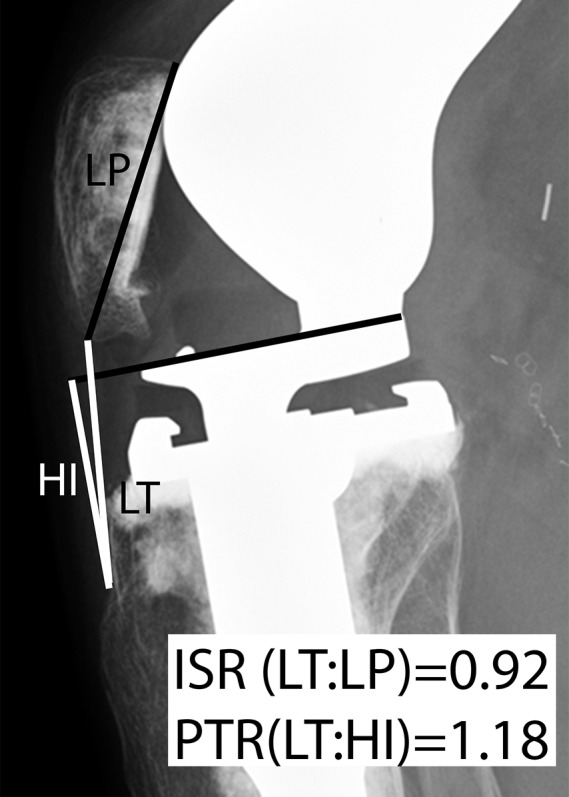
At three years postoperatively, the patient presented with a distal patellar spur with impingement on the tibial component. Despite the impingement, the range of motion was 0° to 120°, and anterior knee pain was mild (Grade I).
Patellar complications that were evaluated included a feeling of instability and a patellar clunk recorded in the medical record; patellar subluxation or dislocation observed on the last anteroposterior knee radiograph; patellar impingement, which was considered present if patellar notching was observed on the lateral knee radiograph; patellar degenerative changes observed on the lateral knee radiograph; and “other patellar complications” as listed in Table I.
We also identified any patellar procedures performed after the femoral replacement, complications of limb-sparing reconstructions as classified by the International Society of Limb Salvage (ISOLS)10, and the last functional (Musculoskeletal Tumor Society [MSTS]11) score available in our database.
We evaluated the associations between pairs of variables. Complications that occurred in small numbers were grouped to permit statistical analysis. The Fisher exact test or chi-square test was used to evaluate associations between pairs of categorical variables. The Wilcoxon rank sum test was performed to compare continuous variables between patient groups. Multivariate linear regression models were used to assess the relationships between covariates that could potentially influence anterior knee pain, range of motion, extensor lag, and complication rate. Logistic regression models were used for multivariate analysis to include important and significant covariates (Table I). The significance level was set at 0.05.
The statistical software program SAS 9.3 (SAS Institute) was used for all analyses.
Results
During the period from 1993 through 2013, 183 distal femoral endoprosthesis reconstructions were performed at our institution. After exclusions, the final cohort comprised 108 patients. Tables II and III summarize the cohort’s demographic, clinical, and surgical characteristics. Forty-eight patients underwent patellar resurfacing and sixty did not. The patients in the resurfacing group were significantly older (mean, 40.9 years) than those in the nonresurfacing group (mean, 28.3 years) (p = 0.0002). The two most common types of knee prostheses were the Finn prostheses (Biomet Manufacturing), used in fifty-three patients, and the Global Modular Replacement System (GMRS; Stryker), used in fifty-five patients. The mean duration of follow-up was 4.5 years (range, 0.7 to twenty years). One patient had an eight-month follow-up because she underwent isolated patellar resurfacing for anterior knee pain less than one year postoperatively.
TABLE II.
Demographic and Clinical Characteristics
| Characteristic | Nonresurfacing (N = 60; 56%) | Resurfacing (N = 48; 44%) | Total (N = 108) | P Value |
| Mean age (SD) (yr) | 28.3 (17.4) | 40.9 (18.8) | 33.9 (19.3) (range, 12-75) | 0.0002 |
| Sex (no.) | ||||
| Female | 30 (50%) | 24 (50%) | 54 (50%) | |
| Male | 30 (50%) | 24 (50%) | 54 (50%) | |
| Diagnosis (no.) | 0.85* | |||
| Benign | 5 (8%) | 6 (13%) | 11 (10%) | |
| Primary malignant | 47 (78%) | 34 (71%) | 81 (75%) | |
| Metastasis or myeloma | 8 (13%) | 7 (15%) | 15 (14%) | |
| Post-radiation fracture | 0 | 1 (2%) | 1 (1%) | |
| Body mass index† | 0.11 | |||
| Mean (kg/m2) | 26.4 | 27.9 | 27.0 | |
| <25 kg/m2 (no.) | 26 (46%) | 10 (29%) | 36 (40%) | |
| ≥25 kg/m2 (no.) | 30 (54%) | 24 (71%) | 54 (60%) | |
| Mean amount of femoral resection | 41% | 37% | 39% | 0.33 |
| Type of endoprosthesis (no.) | <0.0001 | |||
| GMRS | 44 (73%) | 11 (23%) | 55 (51%) | |
| Finn | 16 (27%) | 37 (77%) | 53 (49%) | |
| Surgical approach (no.) | <0.0001 | |||
| Medial | 39 (65%) | 8 (17%) | 47 (44%) | |
| Lateral | 21 (35%) | 40 (83%) | 61 (56%) | |
| Mean follow-up time (SD) (yr) | 3.8 (3.0) | 5.37 (4.8) | 4.5 (3.97) | 0.08 |
For the difference in the number of patients who presented with metastasis or myeloma versus another diagnosis (benign, malignant primary, or post-radiation fracture).
The body mass index is reported for ninety patients (fifty-six in the nonresurfacing group and thirty-four in the resurfacing group).
TABLE III.
Histological Diagnosis
| Nonresurfacing (N = 60; 56%) | Resurfacing (N = 48; 44%) | Total (N = 108) | |
| Benign tumor | 5 | 6 | 11 |
| Giant cell tumor | 4 | 6 | 10 |
| Enchondroma | 1 | 0 | 1 |
| Primary malignant tumor | 47 | 34 | 81 |
| Osteosarcoma | 43 | 24 | 67 |
| Undifferentiated pleomorphic sarcoma | 0 | 4 | 4 |
| Chondrosarcoma | 1 | 4 | 5 |
| Ewing sarcoma | 1 | 0 | 1 |
| Angiosarcoma | 0 | 1 | 1 |
| Unclassified sarcoma | 2 | 0 | 2 |
| Spindle cell sarcoma | 0 | 1 | 1 |
| Metastasis or myeloma | 8 | 7 | 15 |
| Renal cell carcinoma | 6 | 2 | 8 |
| Breast | 0 | 2 | 2 |
| Myeloma | 0 | 2 | 2 |
| Basal cell carcinoma | 1 | 0 | 1 |
| Rhabdomyosarcoma | 1 | 0 | 1 |
| Chondrosarcoma | 0 | 1 | 1 |
| Post-radiation fracture | 0 | 1 | 1 |
Complication Rates
Table IV summarizes the complications in both groups. The most common complication related to the patella in the nonresurfacing group was articular degenerative disease, which was observed in twenty-nine patients (48%). However, the presence of patellar degenerative disease was not associated with anterior knee pain (p = 0.35). Impingement occurred in 23% of the patients in the series as a whole, and patellar subluxation or dislocation occurred in 16%; the rates of these complications did not differ significantly between the resurfacing and nonresurfacing groups. The prevalence of peripatellar calcifications was significantly higher in the resurfacing group than in the nonresurfacing group (nine patients [19%] versus one patient [2%]; p = 0.005).
TABLE IV.
Additional Patellar Procedures and Complications Related to the Patella and Reconstruction
| Complication | Nonresurfacing (N = 60; 56%) | Resurfacing (N = 48; 44%) | Total (N = 108) | P Value |
| Instability feeling | 1 (2%) | 3 (6%) | 4 (4%) | 0.32 |
| Patellar clunk | 3 (5%) | 4 (8%) | 7 (7%) | 0.70 |
| Patellar subluxation/dislocation | 11 (18%) | 6 (13%) | 17 (16%) | 0.41 |
| Patellar impingement | 16 (27%) | 9 (19%) | 25 (23%) | 0.33 |
| Articular patellar degeneration | Not applicable | Not applicable | ||
| Yes | 29 (48%) | |||
| No | 31 (52%) | |||
| Other patellar complications | 11 (18%) | 13 (27%) | 24 (22%) | 0.27 |
| Distal or proximal patellar calcification | 1 (2%) | 9 (19%) | 10 (9%) | 0.005 |
| Arthrofibrosis | 5 (8%) | 1 (2%) | 6 (6%) | 0.22 |
| Patellar fracture | 1 (2%) | 2 (4%) | 3 (3%) | |
| Patellar crepitus | 1 (2%) | 0 | 1 (1%) | |
| Chronic synovitis | 1 (2%) | 0 | 1 (1%) | |
| Heterotopic ossification | 1 (2%) | 0 | 1 (1%) | |
| Effusion | 1 (2%) | 1 (2%) | 2 (2%) | |
| Complications of limb-sparing reconstruction (ISOLS classification) | 14 (23%) | 15 (31%) | 29 (27%) | 0.36 |
| Infection | 3 (5%) | 2 (4%) | 5 (5%) | 1.00 |
| Prosthesis structural failure | 5 (8%) | 5 (10%) | 10 (9%) | 0.75 |
| Patellar procedures | 6 (10%) | 3 (6%) | 9 (8%) | 0.72 |
| Resurfacing or patellar component revision | 3 (5%) | 0 | 3 (3%) | |
| Articular release | 0 | 2 (4%) | 2 (2%) | |
| Patellar realignment | 0 | 1 (2%) | 1 (1%) | |
| Closed manipulation of knee | 3 (5%) | 0 | 3 (3%) |
The prevalences of complications of limb-sparing reconstruction according to the ISOLS classifications were comparable between the two groups, with no significant difference in the rates of prosthesis structural failure or infection (Table IV).
Anterior Knee Pain, Range of Motion, and Extensor Lag (Table V)
TABLE V.
Anterior Knee Pain, Range of Motion, and Extensor Lag
| Outcome | Nonresurfacing (N = 60; 56%) | Resurfacing (N = 48; 44%) | Total (N = 108) | P Value |
| Anterior knee pain (no.) | ||||
| Present | 13 (22%) | 13 (27%) | 26 (24%) | 0.51 |
| Grade I | 7 (12%) | 6 (13%) | 13 (12%) | |
| Grade II | 2 (3%) | 5 (10%) | 7 (7%) | |
| Grade III | 4 (7%) | 2 (4%) | 6 (6%) | |
| Mean range of motion (SD) (deg) | 106 (21.1) | 105 (22.5) | 105 (21.6) | 0.87 |
| Mean extensor lag (SD) (deg) | 4 (12.8) | 2 (5.3) | 3 (10.2) | 0.43 |
| MSTS score (SD)* (%) | 81 (25.8) | 71 (33.7) | 76 | 0.34 |
| Mean follow-up time (range)* (yr) | 2.8 (1-10) | 4.5 (1-11) | 3.6 | 0.02 |
The mean MSTS score and follow-up time are for sixty-two patients (thirty-two in the nonresurfacing group and thirty in the resurfacing group).
Anterior knee pain was reported by twenty-six patients (24%), thirteen (27%) in the resurfacing group and thirteen (22%) in the nonresurfacing group (p = 0.51). There was no association between anterior knee pain and range of motion (p = 0.52) or extensor lag (p = 0.42).
The multivariate logistic regression model revealed a significant association between anterior knee pain and the “other patellar complications” listed in Tables I and IV. Patients with “other patellar complications” had nine times greater odds of having anterior knee pain compared with patients who did not have “other patellar complications” (p = 0.002; odds ratio = 9.643). However, no specific type of complication was associated with anterior knee pain.
There was no significant difference between the resurfacing and nonresurfacing groups with respect to range of motion (p = 0.87) or extensor lag (p = 0.43). However, multivariate analysis showed an extensor lag to be significantly associated with age (p = 0.0094); the older the patient, the more likely an extensor lag was to be observed. There was no statistical association between range of motion and any of the other fifteen variables included in the multivariate linear regression (Table I).
Patellar Height
The mean Insall-Salvati ratio was 0.95 and did not differ significantly between the resurfacing (0.95) and nonresurfacing (0.94) groups. Patella baja (an Insall-Salvati ratio of <0.8) was present in twenty-four patients (22%) and was not significantly associated with anterior knee pain or a limited range of motion (<90°). However, patella baja was significantly associated with impingement in the whole cohort (p < 0.0001) and in both the resurfacing (p = 0.003) and the nonresurfacing (p = 0.012) group.
The mean Insall-Salvati patellar tendon insertion ratio was 1.40 (standard deviation [SD] = 0.34) in the total cohort, 1.49 (SD = 0.36) in the nonresurfacing group, and 1.28 (SD = 0.28) in the resurfacing group (p = 0.0008 for the difference between groups). Multivariate analysis showed no association between the Insall-Salvati patellar tendon insertion ratio and anterior knee pain or the range of motion.
Patellar Procedures After Femoral Reconstruction
Nine patients (8%) had an additional patellar procedure (Table IV) after the femoral reconstruction, with no significant difference in the prevalence of such procedures between the resurfacing and nonresurfacing groups. In the nonresurfacing group, three patients underwent resurfacing or patellar component revision at eight, thirty-eight, and 130 months after the distal femoral reconstruction, and three patients underwent closed knee manipulation. In the resurfacing group, two patients underwent articular release and one patient underwent patellar realignment. No patient had patellar component loosening or patellar component revision.
MSTS Scores
MSTS scores (Table V) were available for sixty-two patients: thirty-two in the nonresurfacing group and thirty in the resurfacing group. Because there were only sixteen cases in which the date when the MSTS scores were obtained matched the date when the range of motion, extensor lag, and anterior knee pain were determined for final follow-up, we did not compare MSTS scores with the other variables. However, there was no significant difference between the mean MSTS scores of the nonresurfacing (81%; SD = 26%) and resurfacing (71%; SD = 34%) groups (p = 0.34) (Table V).
Discussion
Resurfacing of the patella after tumor resection and distal femoral reconstruction remains controversial. Patients with bone tumors, especially primary bone tumors, are generally younger than patients who undergo total knee arthroplasty for osteoarthritis. One school of thought is that resurfacing the patella may increase the chance that the patient will have additional surgery (for patellar component loosening) and hence increase the chance of infection and failure of the limb salvage. Another is that not resurfacing the patella may lead to anterior knee pain and/or extensor lag. This study of patients who underwent distal femoral resection and reconstruction revealed no differences in terms of anterior knee pain, range of motion, extensor lag, infection, or revision surgery between those who had the patella resurfaced and those who did not.
We observed a lower rate of anterior knee pain in our entire cohort (24%) than previously reported by Schwab et al. (32%)5. However, the patients in that study were specifically asked whether they were experiencing anterior knee pain, whereas we collected the data from clinical notes. It is possible that a patient’s report of very mild anterior knee was not recorded in the medical record. Nonetheless, even if our study underrepresented the prevalence of anterior knee pain, there was no significant difference between the resurfacing and nonresurfacing groups. Patients in the nonresurfacing group who had articular patellar degeneration did not experience significantly more anterior knee pain than those without patellar degenerative disease. The only variable associated with anterior knee pain in the multivariate logistic regression analysis was the presence of “other patellar complications” (Table IV) (p = 0.002). However, the rates of these complications did not significantly differ between the resurfacing and nonresurfacing groups.
The range of motion did not differ significantly between the resurfacing and nonresurfacing groups and was not associated with any other variables. The mean range of motion in the whole cohort was 105°. Schwab et al.5 also found no difference in the range of motion between resurfacing and nonresurfacing groups; however, the mean range of motion in their study was 94°. The difference between those values in the two studies may be explained by the fact that we collected range-of-motion data retrospectively whereas Schwab et al. gathered their data prospectively with the use of a goniometer as part of their protocol.
Our linear regression model showed that older age was associated with a greater extensor lag (p = 0.0094), which was not a surprise. Older patients probably have less muscle mass and therefore less extension power, which may explain the increased extensor lag.
The only complication rate that differed significantly between the resurfacing and nonresurfacing groups was that of peripatellar calcifications (p = 0.005) (Fig. 1-B): nine patients in the resurfacing group developed calcification (a spur at the patella), but only one patient in the nonresurfacing group did. However, there was no association between calcification and anterior knee pain or range of motion. The cause of calcification after resurfacing is not clear. Another complication was arthrofibrosis, which occurred in five patients (8%) in the nonresurfacing group and one (2%) in the resurfacing group (p = 0.22). The infection rate also was similar between the two groups. Thus, the additional time and surgical trauma required to perform a patellar resurfacing procedure did not increase the infection rate in our study.
Schwab el al.5 reported two patellar component revisions in fifteen patients who had undergone patellar resurfacing. None of the patients in our series underwent patellar component revision or had failure of the patellar component. Of our patients who did not originally undergo patellar resurfacing, only one underwent patellar resurfacing before one year, as a result of anterior knee pain and a restricted range of motion. This patient had mild improvement in the range of motion but still had low-grade anterior knee pain, suggesting that the anterior knee pain and limited range of motion were not entirely due to the patellar pain.
The Insall-Salvati patellar tendon insertion ratio was significantly lower in the resurfacing group than in the nonresurfacing group (p = 0.0008). However, this ratio was not associated with anterior knee pain or range of motion. It was less than the lower limit of normal of 1.61 in both groups. The difference in the ratio between the groups has questionable clinical relevance. In fact, in 1971, Insall and Salvati8 stated that this ratio should be disregarded for clinical evaluation. We also evaluated the classic ratio described by Insall and Salvati in 1971 (Figs. 1-A and 1-B)8, which we chose because it is a widely used ratio and could be measured even after distal femoral resection and patellar resurfacing had been performed. Patella baja (defined as an Insall-Salvati ratio of <0.8) was significantly associated with patellar impingement in both the resurfacing (p = 0.003) and the nonresurfacing (p = 0.012) group. However, patella baja was not associated with anterior knee pain or a range of motion of <90°. This finding is similar to that of Schwab et al., who did not report associations between patella baja and impingement, anterior knee pain, or range of motion5. However, Schwab et al. also did not find an association between patella baja and impingement, whereas we did.
The limitations of our study are related to its retrospective nature. We relied on the information in our database and a review of the medical records. Although there was no significant difference in MSTS scores between the resurfacing and nonresurfacing groups (p = 0.34), we had MSTS scores for only sixty-two patients; thus, the lack of significance could be related to a power issue. More to the point, our study was designed to evaluate the patellar joint, which is not specifically addressed in the MSTS system11. However, our method of evaluating extensor function on the basis of range of motion, extensor lag, and anterior knee pain seems to be appropriate.
We performed a comprehensive evaluation of knee extensor mechanism variables that could influence range of motion, extensor lag, and anterior knee pain. We could not avoid selection bias. Patients in the resurfacing group were older (mean, 40.9 years) than those in the nonresurfacing group (mean, 28.3 years) (p = 0.0002). This was the case even though the numbers of sarcomas and benign tumors as well as metastases and myelomas were similar in the two groups (p = 0.51). Surgeons tend to resurface the patellae of older patients, and older patients can have a worse functional result. However, our data showed that anterior knee pain and range of motion were not associated with age. Older patients had a higher prevalence of extensor lag, but surprisingly the extensor lag was not significantly increased in either group (Table V).
The surgical approach was more often lateral in the resurfacing group and more often medial in the nonresurfacing group (p < 0.0001). This is a reflection of surgeon predilection and tumor location. However, the surgical approach was included in the multivariate linear regression model and was not found to be associated with anterior knee pain, range of motion, or extensor lag. The same was true for the type of prosthesis.
The lack of symptoms associated with the nonresurfaced patellae in our study could be related to the megaprosthesis design and to the more limited function inherent to that type of reconstruction. Even patients with moderate degenerative changes of the patella and a nonresurfaced patella did not present with substantial patellofemoral symptoms. Thus, the decision to resurface should be based more on preoperative femoropatellar symptoms than on radiographic degenerative findings.
In summary, in our study of patients who underwent distal femoral resection for a tumor and reconstruction with a megaprosthesis, patellar resurfacing did not significantly affect anterior knee pain, range of motion, extensor lag, the rate of infection, or the rate of any other complication except patellar calcification. It may need to be anticipated that patients who undergo distal femoral replacement may develop patellar calcification when the operation included patellar resurfacing and arthrofibrosis when it did not include resurfacing, but the clinical impact of those conditions appears to be minimal. We concluded that because patellar resurfacing did not have a significant effect on the functional and long-term outcomes of distal femoral resection and reconstruction, the decision to resurface can be left to the clinical judgment of the surgeon.
Footnotes
Investigation performed at The University of Texas MD Anderson Cancer Center, Houston, Texas
A commentary by Raffi Stephen Avedian, MD, is linked to the online version of this article at jbjs.org.
Disclosure: M. Etchebehere received a scholarship grant from the São Paulo Research Foundation-FAPESP, Brazil. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author (or the author’s institution) had a relevant financial relationship in the biomedical arena outside the submitted work.
References
- 1.Sandiford NA, Alao U, Salamut W, Weitzel S, Skinner JA. Patella resurfacing during total knee arthroplasty: have we got the issue covered? Clin Orthop Surg. 2014. December;6(4):373-8. Epub 2014 Nov 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schiavone Panni A, Cerciello S, Del Regno C, Felici A, Vasso M. Patellar resurfacing complications in total knee arthroplasty. Int Orthop. 2014. February;38(2):313-7. Epub 2013 Dec 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Waters TS, Bentley G. Patellar resurfacing in total knee arthroplasty. A prospective, randomized study. J Bone Joint Surg Am. 2003. February;85(2):212-7. Epub 2003 Feb 7. [DOI] [PubMed] [Google Scholar]
- 4.Pilling RW, Moulder E, Allgar V, Messner J, Sun Z, Mohsen A. Patellar resurfacing in primary total knee replacement: a meta-analysis. J Bone Joint Surg Am. 2012. December 19;94(24):2270-8. Epub 2013 Jan 16. [DOI] [PubMed] [Google Scholar]
- 5.Schwab JH, Agarwal P, Boland PJ, Kennedy JG, Healey JH. Patellar complications following distal femoral replacement after bone tumor resection. J Bone Joint Surg Am. 2006. October;88(10):2225-30. Epub 2006 Oct 4. [DOI] [PubMed] [Google Scholar]
- 6.Springfield DS. Patellar complications following distal femoral replacement after bone tumor resection. J Bone Joint Surg Am. 2007. February;89(2):453-5; author reply 455. Epub 2007 Feb 3. [DOI] [PubMed] [Google Scholar]
- 7.Tsuboyama T, Windhager R, Campanacci D, Galletti S, Catani F, Capanna R, Campanacci M, Yamamuro T, Kotz R. Patellar resurfacing in tumor endoprosthesis: a study in regard to power transmission. Chir Organi Mov. 1994. Jul-Sep;79(3):243-50. Epub 1994 Jul 1. [PubMed] [Google Scholar]
- 8.Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971. October;101(1):101-4. Epub 1971 Oct 1. [DOI] [PubMed] [Google Scholar]
- 9.Bruderer J, Servien E, Neyret P. Patellar height: which index? In: Zaffagnini S, Dejour D, Arendt EA, editors. Patellofemoral pain, instability, and arthritis. Berlin: Springer; 2010. p 61-7. [Google Scholar]
- 10.Henderson ER, O’Connor MI, Ruggieri P, Windhager R, Funovics PT, Gibbons CL, Guo W, Hornicek FJ, Temple HT, Letson GD. Classification of failure of limb salvage after reconstructive surgery for bone tumours : a modified system including biological and expandable reconstructions. Bone Joint J. 2014. November;96-B(11):1436-40. Epub 2014 Nov 6. [DOI] [PubMed] [Google Scholar]
- 11.Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993. January;286:241-6. Epub 1993 Jan 1. [PubMed] [Google Scholar]


