Abstract
Objective
To elucidate the perceived health benefits of an urban home gardening and nutritional education program in a population at high cardiometabolic risk.
Design
Qualitative data collected via in-depth, semi-structured interviews in Spanish or English.
Setting
Community-based program offering supported urban home gardening together with nutrition education in Santa Clara County, California.
Participants
32 purposively-sampled low-income participants in an urban home gardening program. Participants were primarily female (n=24) and Latino/a (n=22).
Phenomenon of Interest
Perceptions of the nutrition and health benefits of education-enhanced urban home gardening.
Analysis
Bilingual researchers coded transcripts using a hybrid inductive/deductive approach. Two coders double-coded at intervals, independently reviewed coding reports, organized content into key themes, and selected exemplary quotes.
Results
The most salient perceived impacts were greater food access, increased consumption of fresh produce, a shift towards home cooking, and decreased fast food consumption. Participants attributed these changes to greater affordability, freshness, flavor and convenience of their garden produce, increased health motivation due to pride in their gardens, and improved nutritional knowledge. Participants also reported improved physical activity, mental health and stress management; some reported improved weight and adherence to diabetes-healthy diets.
Conclusions and Implications
Education-enhanced urban home gardening may facilitate multidimensional nutrition and health improvements in marginalized populations at high cardiometabolic risk.
Keywords: urban garden, nutrition, health, Latino, qualitative
INTRODUCTION
The persistence of social disparities in cardiometabolic health – including type 2 diabetes (T2DM) and cardiovascular disease – is a major public health challenge in the United States. Diabetes affects 12.2% of adults in the US and is a leading contributor to heart attacks, stroke, and kidney failure.1 One-third of U.S. adults have prediabetes. Compared to whites, Hispanic/Latinos in the US have 29% higher rates of overweight and obesity 2, a key cardiometabolic risk factor. In addition, Hispanic/Latinos have a 66% higher risk of developing T2DM3, 4, and among the highest prevalence of T2DM among all racial/ethnic groups in the US 4. Among Hispanic/Latinos, individuals of Mexican and Central American descent are among the most affected5. Disparities by socioeconomic status also exist: diabetes prevalence in California is 10.2% for individuals with family income under the federal poverty line (FPL), compared with 6.7% for individuals with family income >300% of the FPL6; and 13.1% for individuals with less than high school degree, compared with 7.5% for those with a college degree or higher. Strategies to reduce disparities in cardiometabolic risk are needed to improve health outcomes in vulnerable populations.
In line with the social-ecological model7, disparities in cardiometabolic risk may partially arise from inequities in the social and economic environment that reduce access to a healthy diet and physical activity as well as increased chronic stress associated with socioeconomic disadvantage.8–10 Food insecurity – defined as the limited or uncertain access to sufficient, safe, and nutritious food to maintain a healthy life – affects more than a third of low-income households, disproportionately affects Hispanic/Latinos, and is strongly associated with the development and poor control of diabetes11, 12. Food insecurity potentiates cardiometabolic risk when inadequate food budgets lead to coping strategies focused on purchasing cheap, calorie-dense foods, which can lead to weight gain and compromise blood sugar, blood pressure and lipid control13. Many experiencing urban food insecurity also may live in neighborhoods with limited access to affordable fresh fruits and vegetables relative to numerous cheap fast food outlets and convenience stores selling unhealthy foods14. In addition, studies indicate that low-income individuals engage in less leisure-time physical activity due in part to fewer resources for physical activity 15 and limitations in their physical environment (e.g. lack of safe, appealing recreational spaces such as parks) 16, 17.
Urban gardens may improve health for populations at high cardiometabolic risk by altering the community or household environment to provide a sustainable source of fresh fruit and vegetables, opportunities for physical activity, and stress reduction, in line with the social-ecological model of health behavior change.7 While several models of urban gardening exist, community gardens have received the most attention as a form of community development, environmental stewardship, and more recently, health promotion18, 19. Supported home-based urban gardening is another model that can complement community garden approaches, where the garden is grown at site of the household, but supported by education, gardening expertise and/or gardening resources by a community organization. This home-based model has the potential for more direct health impact by tying the garden more closely to the household. Qualitative research on home-based urban gardening programs is important to illuminate how participants perceive the health benefits and acceptability of such programs, which can inform future intervention development and the formation of hypotheses to be tested in quantitative research. Yet there is limited evidence using any research design, including qualitative designs, on the potential health benefits of urban home gardens among Hispanic/Latinos. To address this gap, a qualitative study was conducted with the objective to elucidate participant perceptions of the health benefits of an urban home gardening program among low-income, primarily Hispanic/Latino immigrant families.
METHODS
This qualitative study was a collaboration between researchers at the University of California San Francisco (UCSF) and Valley Verde, a community-based urban garden organization in Santa Clara County (SCC), California (CA). It was conducted in response to a growing interest in harnessing urban gardens to prevent chronic disease and improve chronic disease outcomes. Understanding participants’ perceptions of the health benefits and the acceptability of urban home gardening programs is a critical next step before undertaking large-scale trials of their effectiveness. The resulting hybrid study design was grounded in a phenomenological orientation to facilitate the study of the garden experience from the perspective of participants. This was blended with content analysis to allow some structure relevant to chronic disease prevention to inform data collection and analysis, which was appropriate given the goal of the study. In-depth interviews were employed as the data collection method (n=32) with participants in the Valley Verde gardening program to understand their perceptions of any health impacts (or lack thereof) and to inform future intervention development.
Study Setting
Valley Verde operates in the cities of San José and Gilroy in SCC. San José is a large city with over 1 million residents (33% Hispanic or Latino)20; Gilroy is a smaller, agricultural city of 52,000 people (58% Hispanic or Latino)21. SCC is the home of technological center Silicon Valley and is characterized by significant disparities in wealth, and one of the highest costs of living in the U.S (median income is $111,609)22. Latinos comprise the largest group living under the poverty line in Santa Clara County22, and have the highest rates of food insecurity, housing insecurity, and being uninsured of all racial/ethnic groups in SCC.23–25
Overview of the Valley Verde Garden Program
Valley Verde is a non-profit 501 c(3) organization which seeks to promote food security and health for low-income residents of SCC by providing the knowledge, skills, and tools for households to grow their own organic vegetable gardens. Valley Verde serves a predominantly low-income and immigrant population, with most participants of Mexican or Central American descent. The garden is implemented at the household level, (~5–6 people per household); one household member joins Valley Verde as the focal participant, and is referred to as the “gardener”. Gardeners are recruited to Valley Verde in groups of ~30 individuals and participate for one year (January-December).
The garden
Households receive all necessary supplies to start and maintain a household garden based in their homes (i.e. not within a community plot): 1–2 installed raised beds (4’×4’ or 4’×8’ depending on space), organic soil, compost, 1 fall and 2 spring cycles of organic seedlings, including those consistent with cultural preferences (e.g., bell peppers, spinach, tomatoes, cucumber, carrots, cilantro, jalapeño, cabbage, radish, cauliflower, onions, garlic), and a water-conserving drip irrigation system. The approximate cost to Valley Verde to provide the garden beds and irrigation system, built to last ~8 years, is $110 (for a 4×4 bed) to_$210 (for a 8×4 bed) per household. Seedlings cost Valley Verde an additional $20-$40 per household per year, and Valley Verde continues to provide seedlings to households past the program year for those who are interested in continuing to garden. Individualized monthly garden mentoring and home visits by Valley Verde staff during the gardening season provide an opportunity for personalized gardening support.
Nutrition education
Valley Verde staff provide 10 monthly workshops focused on nutritional education, in addition to organic gardening skills-building. The curriculum was adapted for cultural relevance from the University of California Cooperative Extension’s Expanded Food and Nutrition Education Program26. Topics include strategies to increase vegetable, fruit and whole grain intake, healthy shopping strategies, how to prepare and use harvested produce in ways aligned with personal and cultural preferences, culturally-preferred healthy recipes for common produce, and use of garden produce to meet heart- and diabetes-healthy dietary recommendations. In some sessions, participants prepare, share, and discuss a healthy dish using produce from their garden and the knowledge from the nutritional workshops. Children and all family members are welcome at all workshops.
Limited HIV program
Valley Verde also provided a limited program to residents of dedicated housing for people living with HIV, including a household garden bed and gardening support, but no formal education workshops.
Leadership opportunities
After the conclusion of the initial year-long programming, Valley Verde continues to engage gardeners to encourage sustainability. For instance, the previous cohort can participate in planting activities after the end of the program. Leadership opportunities are available through the Super Jardineros program, which trains past gardeners as Valley Verde peer leaders.
Study Population and Recruitment
Participants were recruited into the study until saturation of ideas (i.e. little to no emergence of new insights and experiences) in the in-depth interviews was reached27, 28. Based on prior experience and the literature it was anticipated to reach saturation within 25–30 interviews; in actuality, through continuous review of the data as it was collected for new ideas relevant to our research question, saturation was reached at 32 interviews. Participants were recruited via announcements at Valley Verde program events or directly by study staff (after Valley Verde reached out to individual gardeners to assess initial interest). Criteria for inclusion in the qualitative study were: being the focal Valley Verde program participant, age 18 years or older, Spanish- or English-speaking, and in the current or most recent program cycle. The study excluded individuals who no longer lived in San José, Gilroy, or surrounding communities. Purposive sampling was used to ensure gardeners across the two cities and program cycles were included in the study.
Data Collection
In-depth semi-structured interviews were conducted in 2014. The interview guide was created in English, professionally translated into Spanish and pilot tested. The guide covered a number of domains spanning the individual, household and community levels (consistent with the social-ecological model), including perceptions of food insecurity and dietary behaviors of the individual and the household, the local food environment, physical health and mental health. Questions to understand pre-program experiences in each domain were included, as well as questions to capture perceived changes in each domain over the course of garden participation (and reasons for these changes). Main questions in each domain were explored with follow-up questions and probes to draw out rich narratives centered on participant experience. See Table 1 for domains and example questions from the interview guide.
Table 1:
Interview Guide Domains and Example Questions
| Domains | Example question(s) |
|---|---|
| Living Situation | Now I’d like to hear a little about the area you live in. Can you describe your neighborhood to me? |
| Food Security, Diet and Nutrition | Please tell me more about your food situation. Can you talk to me about where you get the foods you eat, not including what you grow with Valley Verde? Can you describe your household’s food or nutrition situation since getting involved with Please tell me more about that. |
| Physical Health | I want to start by hearing about your health. I’d especially like to hear about your physical health before joining Valley Verde. Could you tell me about this? Now I’d like to hear more about your physical health since participating in Valley Verde. Can you describe your health, including any changes, since participating in Valley Verde? Please tell me more about that. |
| Mental Health | How were you feeling, mentally and emotionally, during the time right before starting Valley Verde? Now I’d like to hear more about your mental and emotional health since participating in Valley Verde. Can you describe how you’ve been doing mentally and emotionally, including any changes, since participating in Valley Verde? Please tell me more about that. |
| Program Improvement | Do you plan to continue with your garden after Valley Verde is over? Why or why not? What do you think could be improved about Valley Verde? |
Interviews were conducted in a private location of the participant’s choosing, in Spanish or English. Spanish-language interviews were conducted by native bilingual research team members (LLH, KH). Post-baccalaureate and Master’s-level interviewers were trained in qualitative interviewing by the doctoral-level study leads, who themselves had formal graduate-level training in qualitative research methods (KP, SW). Demographic information was collected prior to beginning each interview. Interviews were audio-recorded and lasted an average of 90 minutes. After the interview, participants received a $20 gift certificate to a garden supply store. UCSF’s institutional review board – the Human Research Protection Program – approved the study. Written consent to participate in the interview, in Spanish or English, was obtained from participants; verbal consent was requested for recording the interview.
Data Coding and Analysis
Interviews were transcribed, reviewed for accuracy, de-identified, and uploaded to Dedoose, a web-based qualitative data management platform (Dedoose [web-based computer program]. Version 8.0.35. Los Angeles, CA: SocioCultural Research Consultants, LLC; 2018). Using content coding methodology, a codebook of broad codes was created based on the main domains of the interview guide (See Table 1). In a hybrid deductive-inductive approach, inductive codes were identified by reviewing transcripts for emerging ideas. The transcripts were coded in their original language by fluent Spanish-English bilingual research staff (LLH, KH, KP), and double coded at regular intervals. The coders met weekly to resolve discrepancies in coding and come to consensus. The full bilingual research team reviewed and discussed coding reports to identify emerging themes and avenues for additional fine coding, in an iterative process. Analysis was conducted by (LLH, KH, KP) who independently reviewed coding reports, organized content into key themes, and selected exemplary quotes. Team coding and analysis meetings were used to resolve any potential challenges to working with data in both Spanish and English; however, the fully bilingual nature of the analytic team helped to minimize divergence in the data due to language. Person-by-theme matrices were used to identify salient themes. Spanish quotes were translated to English by bilingual team members (LLH, KH). The current analysis focuses primarily on perceived nutrition and health impacts, and the reasons for these impacts.
RESULTS
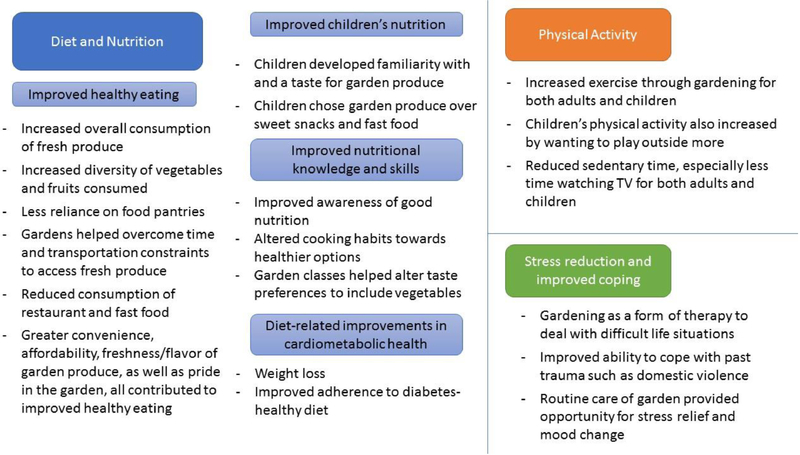
Of the 32 in-depth interviews conducted, the majority of participants (n=24) were women, born outside of the United States (n=24) and identified as Latino (n=22); of these, 20 reported being of Mexican descent (Table 2). Participants discussed a wide range of perceived health benefits of the gardening program. Major themes included perceptions of improved diet and nutrition, improved physical activity, and stress reduction. Within the diet and nutrition theme, there were additional sub-themes, including: Perceptions of improved healthy eating, perceptions of improved children’s nutrition, perceptions of improved nutritional knowledge and skills, and perceptions of diet-related improvements in cardiometabolic health (Figure). The range of participant experiences comprising each theme or sub-theme are described below, with illustrative quotes, and in the Figure.
Table 2:
Sociodemographic Characteristics of Study Participants (n=32)
| Gender identity, n (%) | |
| Man | 7 (22) |
| Woman | 24 (75) |
| Transgender/genderqueer | 1 (3) |
| Age, mean (range) | 46 (27, 67) |
| Race/ethnicity, n (%) | |
| Latino | 22 (69) |
| Black/African-American | 2 (6) |
| Asian | 2 (6) |
| White/Caucasian | 5 (16) |
| Other | 1 (3) |
| Born outside of the US, n | 24 (75) |
| Educational attainment, n | |
| Less than primary school | 5 (16) |
| Primary school | 7 (22) |
| High school or GED | 6 (19) |
| Some college | 5 (16) |
| College or above | 9 (28) |
| Child dependents, mean (range) | 1.8 (0, 5) |
| Location, n | |
| San José | 21 (66) |
| Gilroy | 11 (34) |
Figure: Perceived benefits of participation in an urban home garden program.
This figure outlines the salient themes and subthemes related to perceived nutrition and health impacts of the Valley Verde urban gardening program, described by program participants.
Perceived Impacts on Diet and Nutrition
Perceived impacts on nutrition were by far the most salient health-related impacts perceived by Valley Verde participants.
Perceptions of improved healthy eating
Almost all participants indicated that they ate more vegetables and fruits due to program participation. Participants gave a range of reasons for these changes, including increased affordability, accessibility, freshness, flavor, and convenience of the garden produce, as well as self-efficacy for improving their health through eating garden produce.
A 36-year old female participant described how the gardens addressed affordability to improve vegetable consumption:
“We have a little bit of everything now, of each vegetable, so now you eat more vegetables. Because before it was difficult for me to buy things – we only bought the most necessary, like potatoes, a cabbage, and a lettuce…But now it’s different, because we have carrots…and we don’t [have to] buy tomatoes anymore…. You go out there when you want a salad or something, and you have it. I think it’s changed our way of eating a lot.” (translated from Spanish)
Changes in diet were perhaps most pronounced among participants who described marked experiences of food insecurity, such as regularly running out of food at the end of the month. A 47-year old female participant described how the garden helped during times of the month when money ran low:
“We had some delicious meals with lots of peas because the winter peas were doing really well, and then we could just draw on that when you’re out of options. [Fruits and vegetables] are a more steady supply. Yeah it isn’t like, ‘Oh guess what? In this pay period we can actually afford some salad.’ Now we just go and just harvest it and just have it all the time.” (translated from Spanish)
Another participant, a 44-year-old female farmworker, described receiving food from a local food pantry during times when money was tight prior to the garden. After the garden, she no longer had to rely on the food pantry, commenting:
“…since we have the little gardens, well, we gather vegetables, cilantro, everything from there. If you wanted a little bit… well, now you don’t go to buy it, and you don’t go to get it for free.” (translated from Spanish)
Participants reported that the greater quality and convenience of the homegrown produce increased consumption and reduced affordability as a barrier. A 42-year old male participant noted that the convenience and freshness of the garden produce encouraged him to increase his vegetable consumption:
“I eat about 30% more [vegetables] now, because before I would have to go and buy them at the store, but now I just have them here, and they’re so fresh. If I’m cooking and I suddenly want to add something… I can just go and get some cucumbers or something… and it’s delicious.” (translated from Spanish)
One female participant with HIV described how having the produce right on hand increased her vegetable consumption:
“I mean I eat, I eat a ton of more vegetables than I used to….The other day I wanted to sauté some kales so I ran out to the garden… it doesn’t get any better than that.”
Convenience was a particularly salient driver of garden produce consumption for participants with limited access to transportation, or limited time to procure healthy food. For instance, one 33-year old female participant described,
“Sometimes, in the times when I work, I don’t have the chance to go walking to the store even though it’s more or less close by. I don’t drive, so I have to wait for my husband or someone to go, and now having them [the garden plants] here, well now it’s different. Because if I get to four, five in the evening or I want to make some broccoli or a salad, well now you just cut them and you wash them and you have it right there, instead of saying ‘oh, well, we’ll see what time I’ll go to the store and what time it’ll be here’…. Instead, already having them here [in the garden], well yeah, you eat them more.” (translated from Spanish)
In addition to increasing consumption of healthier foods, participants described reducing fast food or going out to eat at restaurants. For example, one 34-year old female participant commented that,
“[With the garden] you have more options of healthy things to eat, outside of buying meat, or eating street food, because honestly lots of people just think ‘Oh, let’s go to eat out.’ When you have food at home, why would you go out? Before [the garden] we would eat [out], and now we don’t.” (translated from Spanish)
Participants invested considerable time and energy into their gardens, prompting a sense of pride which led to healthy eating. For example, a 34-year old male participant expanded on how growing one’s own vegetables increases the motivation to consume them, hence, creating greater desire and pride to eat what is freshly grown, describing:
“I value more the things that I cook, and the things that I get from my garden, over the things I buy. There’s a big difference. So I have a greater desire to eat it. I feel good that I grew it and I am eating something that I grew. So for me, it’s priceless…. The fact of cooking something that I grew is something that’s important!”(translated from Spanish)
Perceptions of improved children’s nutrition
In addition to improvements in the participants’ own healthy eating, many participants described improvements in children’s eating behaviors. For example, one 47-year old female participant commented:
“I think [my kids] tolerate more greenery now – before, they were like a little standoffish. They would have rather had that burger… It’s funny because they were being city kids… They would go and pick something [from the garden] and then look at it as if it was an alien… what do I do with it?... So I had to get them, you know – you can pick that tomato and bite into it, it’s okay. But they’ve come around now. Now they go out, now they look for the strawberries.”
Another participant (35-year old female) also noted that fresh vegetables had replaced sweet snacks for her children in some cases:
“Like in the season when there are a lot of vegetables, if the cucumbers are there [in the garden], instead of eating something sweet [my kids] go and by themselves cut them and wash them and eat them. Or right there [in the garden] they put a little table and right there they eat them, and that is good because they stop going and eating something else that will do them harm, on the street or something else.” (translated from Spanish)
The garden also sometimes prompted a change in children’s preferences and habits away from fast food and towards healthier foods at home. A 34-year old female participant described such a change in her own children, which helped reinforce that the garden was worth the effort:
“The children know now… it’s not just going to get it at the store, but they know how to grow it, and how much of a process is involved in cultivating what they will eat… Before… they would say “Take me to McDonald’s” and now they don’t. They’ve been learning how to eat, how to substitute some foods with others. One of my children especially surprised me, that he would eat the green peas… he would go and cut them like he was eating peanuts… he would sit to eat them and eat them and watch TV, and I said, that’s more than worth the effort for me.” (translated from Spanish)
Perceptions of improved nutritional knowledge and skills
Participants talked at length about the way that the gardens and education classes together improved their knowledge and skills needed to eat healthfully. One participant with HIV described that gardening changed their general awareness of good nutrition:
“I feel as though [the program] made me more aware of what, how I eat now, where I wasn’t really in the past thinking about the nutritional value as much as I am now.”
A 43-year old male participant described how the classes, combined with access to fresh garden produce, changed his approach to cooking:
“Every day [the program] helps us learn more and different things to cook. Before I cooked with plenty of oil. Now we cook differently. Almost all of it is without oil… trying to not use a lot of salt, a lot of sugar, and to eat healthy. Eat a [good] diet, and your salad, and we’ll go take a walk after.” (translated from Spanish)
Other participants described how the classes helped them develop new habits that they were able to put into practice with the gardens. For instance, one 33-year old female participant described new appreciation for vegetables:
“For us [the garden is] really great because I tell you before I didn’t eat [vegetables] but now that I have them here, well I have to take advantage… Like before this…I didn’t like spinach and now I eat spinach. When we go to the garden classes [with Valley Verde] they tell us… just start with a little taste, and from there you’ll start developing a taste for new things… And now I buy myself a little bag of spinach and I put some on my plate each meal.”
Perceptions of diet-related improvements in cardiometabolic health
Some participants experienced weight loss and improved adherence to a diabetes diet which they attributed to the gardens. For example, one 42-year old male participant commented,
“Within the last six months I’ve been eating a lot of lettuce and vegetables. I am not lying, I used to weigh 265 pounds, and now I weigh 240… I feel better….feel lighter, like, wow, I can breathe better.” (translated from Spanish)
Among all participants, seven mentioned having pre-diabetes or diabetes, and half of all participants reported having a family member with diabetes in the household. These individuals sometimes described the gardens supporting diabetes health. For instance, a 50-year old female participant with type 2 diabetes noted that the more affordable produce helped her adhere with a diabetes-healthy diet:
“I can plant artichokes, but you go to the store and it costs a dollar an artichoke. So, if I planted them, I could eat them, because they cost me $2.50 for the little bag of seeds. So I did like that, and that is going to help me with my diabetes.” (translated from Spanish)
Perceived Impacts on Physical Activity
In addition to nutritional improvements, participants frequently described increased exercise and reduced sedentary behavior of both adults and children. Tending the garden led to physical activity for many participants, due to the need to water, weed, harvest and plant at regular intervals. As one 42-year-old male participant described:
“When you’re tired and bored, you can go and see your flowers. Water them, weed them, and it’s exercise for you… you have to get up and down a lot. And then after 4 weeks go you out and all of a sudden you have fruit!” (translated from Spanish)
Other participants perceived the gardens to be more important for reducing sedentary behaviors. One 47-year old female participant described how the garden led her family to watch less TV and spend more time being active:
“Well we do more [exercise] because before we would just finish dinner and sit down and watch TV, and now we don’t. Now we go outside and cut the grass, clean up the garden, so when we come back in we’re already tired. We have to prepare the soil, pull weeds, dig… when we finish we’re sweating.” (translated from Spanish).
Participants reported that the gardens were particularly important to provide opportunities for their children to be active. As one female participant noted,
“I think that [the kids] get more exercise now because they go outside more now and look at the garden, run around outside, and all that. Yes, it’s much better.” (translated from Spanish)
In particular, the gardens helped provide an alternative to sedentary screen time. A 44-year old female participant described the garden’s impact on the time her children spent playing video games:
“You know kids play those games. Sometimes I tell mine, ‘Son, instead of playing that [videogame] go to the little plants, go and pick some…’ And he does. They turn [the videogames] off and they go outside.” (translated from Spanish)
Perceived Impacts on Stress and Coping
Almost all participants described reduced stress due to their gardens. Some participants perceived the act of gardening to be a form of “therapy” for coping with stressful life situations, as one participant with HIV (55-year old, female), described:
“Having the garden has gotten me through some pretty tough times. There were times that were very stressful for me and… it’s like therapy. I go out there and I just garden and I plant. I find it very therapeutic.”
Other participants experienced gardening as a source of distraction and an opportunity to empty the mind of distressing thoughts or memories. A 55-year old female participant, who had recently experienced domestic violence, said of her garden:
“If I am with the plants I get distracted. You are not thinking, remembering the past. You are watching what you’re doing, what you’re growing, thinking how beautifully they can grow. You see they have leaves and the next day they already have more and you get excited. It changes you. Even though you never forget the ugly past, it does help a lot.” (translated from Spanish)
A male participant with diabetes described how caring for the garden improved his mood by providing both structure as well as an opportunity to spend time outdoors:
“When I first got my little plot every day I’d go and I had to water it….when I’m outside and I hear the birds singing and I see things around me, it helps get me out of my apartment into a different environment, so that also helps with my pain and not dealing with the pain as much.”
DISCUSSION
Participants in a home-based urban gardening program reported a wide range of perceived health-related benefits. All participants reported that the gardens led to healthier eating for both adults and children, attributed to the greater affordability, accessibility, freshness, flavor and convenience of their garden produce, motivation for healthy eating fostered by pride in their gardens, and/or greater nutritional knowledge. Multigenerational improvements in physical activity and the ability to cope with stress and trauma through gardening reported by participants were also highly salient. In addition, some reported direct improvements in weight management and adherence to diabetes-healthy diets. These findings suggest that an urban gardening model that integrates home gardening with culturally-appropriate nutrition and gardening education has the potential to improve a range of health behaviors that are critical to preventing and managing chronic disease, especially among low-income, urban Hispanic/Latino households.
These findings are relevant to cardiometabolic health promotion in low-income Hispanic/Latino immigrant communities. Healthy lifestyle behaviors form the cornerstone of diabetes and cardiovascular disease prevention29, including eating a diet high in fresh fruits and vegetables and low in processed, fatty and sugary foods, as well as consistently engaging in physical activity30. There is increasing awareness and recognized need to address the social determinants and structural constraints to healthy diet and lifestyles31 – such as food insecurity, lack of access to healthy foods in their neighborhoods, and lack of access to safe spaces for physical activity – that the social-ecological model suggests may undermine the ability to make lifestyle modifications7. Participants in our study found both the information (i.e. nutrition education classes) and the structural/resource (i.e. garden) components valuable, with the gardens providing a material resource and behavioral support to complement and reinforce the nutrition education. Together, these components were perceived by participants to create a positive feedback loop whereby participants could learn about healthy eating and behaviors, and then could enact them via the gardens, which then engendered further healthy behaviors.
This study extends previous research on the health benefits of gardening by generating evidence on the perceived benefits of a multicomponent home gardening program in an urban setting and in a predominantly low-income, Hispanic/Latino population. Studies in resource-rich settings – primarily the US and Canada – have demonstrated that gardening in general has the potential to contribute to healthier diets including increased fruit and vegetable consumption19, 32–42, improved mental health and emotional well-being32, 34, 35, 43–46, improved overall physical health18, 32, 34, 35, 40, 41, 43, 44, 46 including weight management33, 37, 40, 47, and improved disease management32, 36, 40. Most commonly, these studies focus on community gardens in urban settings, or on informal domestic gardens (i.e. not supported by program infrastructure or tied in to training/education). Two previous studies focused on Hispanic/Latino populations – one of which explored home gardens in a rural setting35, and the other which focused on a community garden intervention among Latino youth in LA37. Another study found that a community garden model improved diabetes control among Marshallese immigrants36. Evidence from Santa Clara County (where this study was conducted ) indicates that community gardens, using individual plots, may be cost-saving 48.
Urban agriculture is an important community resource that may contribute not only to nutrition and health but to urban development and social connection. When urban agriculture is community-led and focuses on increasing the empowerment, choice and collaboration of historically disadvantaged populations, it also falls within the framework of trauma-informed social policy49. This framework calls for food systems to recognize food insecurity as a form of trauma, and to develop solutions that help to counteract the effects of this trauma (e.g. stress, isolation, lack of control)50. While community garden models of urban agriculture have predominated, some individuals may have difficulty accessing them due to knowledge, transportation or time constraints51. Home gardens may therefore further a more robust, trauma-informed food system by offering households more control, as well as more convenient access to gardening and its benefits for those who have sufficient space requirements. For those without suitable home garden space, or who prefer to garden in a collective space, community gardens remain vital neighborhood resources.
This study also had several limitations. First, study participation was limited to current or recent gardeners who expressed interest and agreed to participate in the study, and were reachable for the interview. It is possible that gardeners who were interested or reachable would be more likely to report positive impacts of the gardens than those who did not participate (i.e. selection bias)52, limiting generalizability. However, significant efforts were made to sample a range of participants, address concerns of potential participants, and to contact difficult-to-reach participants, in order to minimize this potential bias. Second, given the nature of the garden intervention that relied upon having adequate space in the home for a raised bed, the potential benefits of urban gardens for some types of low-income families (i.e. those living in some types of apartments) were not explored. Nonetheless, since this initial formative research, Valley Verde has changed their programming such that households unable to accommodate raised beds due to lack of space now receive up to 4 wine barrels ensuring that gardeners living in houses, trailer homes or apartments with varying access to outdoor space can participate. Third, although the interviews were conducted by independent research staff, it is possible that social desirability bias led participants to overemphasize positive impacts and underplay potential barriers53. To minimize this possibility, interviewers were trained to be neutral and to emphasize that all participant responses were confidential from Valley Verde staff throughout the interview. It is also possible that the researcher’s subjectivity influenced the study results, for example by preferencing certain responses, themes or quotes that aligned with preexisting beliefs53. To reduce this, training for interviewers and data coders/analysts included techniques to recognize and reduce undue subjectivity. Having multiple researchers independently review interview transcripts, coded data and thematic analysis and making any necessary course corrections also helped to reduce the risk of excessive subjectivity. Finally, understanding the perceived impacts on health outcomes was limited by including participants who were not recruited based on any specific health conditions. Future studies among individuals with obesity, pre-diabetes or diabetes would better elucidate perceived impacts on cardiometabolic health.
IMPLICATIONS FOR RESEARCH AND PRACTICE
This study suggests that supported home gardening integrated with nutrition education in a community-based, culturally-appropriate program setting is acceptable to participants, who perceive it to benefit their nutrition and health in a myriad of ways. Key program elements perceived to be beneficial by participants include the educational component provided in tandem with garden support, the culturally appropriate garden produce and curriculum, and the promotion of organic gardening. While promising, a formal program evaluation is needed to assess whether supported home-gardening is an effective vehicle for health improvement for low-income populations with high cardiometabolic risk in urban settings. If effective, urban home gardening programs should be understood as a complement to – rather than a replacement for – community gardens, which together may promote a more resilient, trauma-informed local food system. Integrated into public health approaches for cardiometabolic disease prevention, urban home garden programs may be an innovative strategy to help reach the Healthy People 202054 goals of reducing the burden of pre-diabetes and diabetes in vulnerable populations.
Acknowledgements
This work was supported by the Center for Collaborative Research for an Equitable California at the University of California. Further salary support (Palar) was provided by the National Institute of Diabetes and Digestive and Kidney Diseases K01DK107335. The authors thank the Valley Verde staff for their invaluable support during this study. We thank our Valley Verde study participants for sharing their time and experiences as part of this research.
Footnotes
Notes: This study was approved by the UCSF Institutional Review Board
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2017 (https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf). Accessed January 23, 2019: CDC; 2017. [Google Scholar]
- 2.Centers for Disease Control and Prevention. Differences in prevalence of obesity among black, white, and Hispanic adults-United States, 2006–2008. MMWR. Morbidity and Mortality Weekly Report. 2009;58:740. [PubMed] [Google Scholar]
- 3.Chow EA, Foster H, Gonzalez V, McIver L. The disparate impact of diabetes on racial/ethnic minority populations. Clinical Diabetes. 2012;30:130–133. [Google Scholar]
- 4.Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and Trends in Diabetes Among Adults in the United States, 1988–2012. JAMA. 2015;314:1021–1029. [DOI] [PubMed] [Google Scholar]
- 5.Schneiderman N, Llabre M, Cowie CC, et al. Prevalence of diabetes among Hispanics/Latinos from diverse backgrounds: the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Diabetes Care. 2014;37:2233–2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.California Diabetes Program. 2012 California Diabetes Program Fact Sheet (https://www.crihb.org/wp-content/uploads/2014/12/CDP_Fact_Sheet_2012-1.pdf). Accessed January 23, 2019 Sacramento, CA: California Department of Public Health; 2012. [Google Scholar]
- 7.Stokols D Translating social ecological theory into guidelines for community health promotion. American journal of health promotion. 1996;10:282–298. [DOI] [PubMed] [Google Scholar]
- 8.Laraia BA, Karter AJ, Warton EM, Schillinger D, Moffet HH, Adler N. Place matters: neighborhood deprivation and cardiometabolic risk factors in the Diabetes Study of Northern California (DISTANCE). Social Science & Medicine. 2012;74:1082–1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Non AL, Rewak M, Kawachi I, et al. Childhood social disadvantage, cardiometabolic risk, and chronic disease in adulthood. American Journal of Epidemiology. 2014;180:263–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Slopen N, Goodman E, Koenen KC, Kubzansky LD. Socioeconomic and other social stressors and biomarkers of cardiometabolic risk in youth: a systematic review of less studied risk factors. PLoS One. 2013;8:e64418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999–2002. Journal of General Internal Medicine. 2007;22:1018–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seligman HK, Davis TC, Schillinger D, Wolf MS. Food insecurity is associated with hypoglycemia and poor diabetes self-management in a low-income sample with diabetes. Journal of Health Care for the Poor and Underserved. 2010;21:1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seligman HK, Schillinger D. Hunger and socioeconomic disparities in chronic disease. New England Journal of Medicine. 2010;363:6–9. [DOI] [PubMed] [Google Scholar]
- 14.Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the US. American Journal of Preventive Medicine. 2009;36:74–81. e10. [DOI] [PubMed] [Google Scholar]
- 15.Cerin E, Leslie E. How socio-economic status contributes to participation in leisure-time physical activity. Social Science & Medicine. 2008;66:2596–2609. [DOI] [PubMed] [Google Scholar]
- 16.Cohen DA, Han B, Derose KP, et al. Neighborhood poverty, park use, and park-based physical activity in a Southern California city. Social Science & Medicine. 2012;75:2317–2325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lovasi GS, Hutson MA, Guerra M, Neckerman KM. Built environments and obesity in disadvantaged populations. Epidemiologic Reviews. 2009;31:7–20. [DOI] [PubMed] [Google Scholar]
- 18.Alaimo K, Beavers AW, Crawford C, Snyder EH, Litt JS. Amplifying health through community gardens: A framework for advancing multicomponent, behaviorally based neighborhood interventions. Current Environmental Health Reports. 2016;3:302–312. [DOI] [PubMed] [Google Scholar]
- 19.Garcia MT, Ribeiro SM, Germani ACCG, Bógus CM. The impact of urban gardens on adequate and healthy food: a systematic review. Public Health Nutr. 2018;21:416–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.City of San Jose. City of San Jose: History and Geography (https://www.sanjoseca.gov/DocumentCenter/View/780). Accessed January 23, 2019: City of San Jose; 2018. [Google Scholar]
- 21.U.S. Census Bureau. Quick Facts: City of Gilroy, California (https://www.census.gov/quickfacts/fact/table/gilroycitycalifornia/PST045217). January 23, 2019: U.S. Census Bureau; 2017. [Google Scholar]
- 22.DataUSA. DataUSA: Santa Clara County, CA (https://datausa.io/profile/geo/santa-clara-county-ca/). Accessed January 23, 2019 2018.
- 23.Santa Clara County Food System Alliance. Santa Clara County Food System Assessment (http://www.caff.org/wp-content/uploads/2015/03/Final_VersionASSESS_010814_sm.pdf). Accessed January 23, 2019: Ag Innovations Network; 2013. [Google Scholar]
- 24.Santa Clara County Public Health Department. Latino Health in Santa Clara County (https://www.sccgov.org/sites/phd/collab/BHW/Documents/latino-fact.pdf). Accessed January 23, 2019 San Jose, CA: SCCDPH; 2018. [Google Scholar]
- 25.Santa Clara County Public Health Department. 2014 Santa Clara County Community Health Assessment (https://www.sccgov.org/sites/phd/collab/chip/Documents/cha-chip/SCC_Community_Health_Assessment-2014.pdf). Accessed Janaury 23, 2019 San Jose, CA: SCCDPH; 2014. [Google Scholar]
- 26.University of California. Healthy Families and Communities. EFNEP; https://ucanr.edu/sites/tularenutrition/Adult_Nutrition_Education_Program/EFNEP/. Accessed April 11, 2019 [Google Scholar]
- 27.Bernard H Research methods in anthropology: qualitative and quantitative approaches. Oxford: Rowan Altamira; 2006. [Google Scholar]
- 28.Mason M Sample size and saturation in PhD studies using qualitative interviews. Forum qualitative Sozialforschung/Forum: qualitative social research. Vol 112010. [Google Scholar]
- 29.American Diabetes Association. Standards of medical care in diabetes—2014. Diabetes Care. 2014;37:S14–S80. [DOI] [PubMed] [Google Scholar]
- 30.American Diabetes Association. Eating Patterns and Meal Planning. Vol 20192018. [Google Scholar]
- 31.Dunn SM, Beeney LJ, Hoskins PL, Turtle JR. Knowledge and attitude change as predictors of metabolic improvement in diabetes education. Social Science & Medicine. 1990;31:1135–1141. [DOI] [PubMed] [Google Scholar]
- 32.Spees CK, Joseph A, Darragh A, Lyons F, Wolf KN. Health behaviors and perceptions of cancer survivors harvesting at an urban garden. American Journal of Health Behavior. 2015;39:257–266. [DOI] [PubMed] [Google Scholar]
- 33.Castro DC, Samuels M, Harman AE. Growing healthy kids: a community garden–based obesity prevention program. American Journal of Preventive Medicine. 2013;44:S193–S199. [DOI] [PubMed] [Google Scholar]
- 34.Wakefield S, Yeudall F, Taron C, Reynolds J, Skinner A. Growing urban health: community gardening in South-East Toronto. Health Promotion International. 2007;22:92–101. [DOI] [PubMed] [Google Scholar]
- 35.Carney PA, Hamada JL, Rdesinski R, et al. Impact of a community gardening project on vegetable intake, food security and family relationships: a community-based participatory research study. Journal of Community Health. 2012;37:874–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Weltin AM, Lavin RP. The effect of a community garden on HgA1c in diabetics of Marshallese descent. Journal of Community Health Nursing. 2012;29:12–24. [DOI] [PubMed] [Google Scholar]
- 37.Gatto NM, Ventura EE, Cook LT, Gyllenhammer LE, Davis JN. LA Sprouts: a garden-based nutrition intervention pilot program influences motivation and preferences for fruits and vegetables in Latino youth. Journal of the Academy of Nutrition and Dietetics. 2012;112:913–920. [DOI] [PubMed] [Google Scholar]
- 38.Scott TL, Masser BM, Pachana NA. Exploring the health and wellbeing benefits of gardening for older adults. Ageing & Society. 2015;35:2176–2200. [Google Scholar]
- 39.McMahan M, Richey EJ, Tagtow A. Cultivating food security: low-resource Iowans’ perspectives on food gardening. Journal of Hunger & Environmental Nutrition. 2014;9:299–317. [Google Scholar]
- 40.Blair CK, Madan-Swain A, Locher JL, et al. Harvest for health gardening intervention feasibility study in cancer survivors. Acta Oncologica. 2013;52:1110–1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Litt J, Schmiege S, Hale J, Buchenau M, Sancar F. Exploring ecological, emotional and social levers of self-rated health for urban gardeners and non-gardeners: A path analysis. Social Science & Medicine. 2015;144:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ornelas IJ, Osterbauer K, Woo L, et al. Gardening for Health: Patterns of Gardening and Fruit and Vegetable Consumption Among the Navajo. Journal of Community Health. 2018:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shacham E, Donovan MF, Connolly S, Mayrose A, Scheuermann M, Overton ET. Urban farming: a non-traditional intervention for HIV-related distress. AIDS and Behavior. 2012;16:1238–1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sommerfeld AJ, Waliczek TM, Zajicek JM. Growing minds: evaluating the effect of gardening on quality of life and physical activity level of older adults. HortTechnology. 2010;20:705–710. [Google Scholar]
- 45.Blair D, Giesecke CC, Sherman S. A dietary, social and economic evaluation of the Philadelphia urban gardening project. Journal of Nutrition Education. 1991;23:161–167. [Google Scholar]
- 46.Freeman C, Dickinson KJ, Porter S, van Heezik Y. “My garden is an expression of me”: Exploring householders’ relationships with their gardens. Journal of Environmental Psychology. 2012;32:135–143. [Google Scholar]
- 47.Zick CD, Smith KR, Kowaleski-Jones L, Uno C, Merrill BJ. Harvesting more than vegetables: the potential weight control benefits of community gardening. American Journal of Public Health. 2013;103:1110–1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Algert SJ, Baameur A, Renvall MJ. Vegetable output and cost savings of community gardens in San Jose, California. Journal of the Academy of Nutrition and Dietetics. 2014;114:1072–1076. [DOI] [PubMed] [Google Scholar]
- 49.Bowen EA, Murshid NS. Trauma-informed social policy: A conceptual framework for policy analysis and advocacy. American journal of public health. 2016;106:223–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hecht AA, Biehl E, Buzogany S, Neff RA. Using a trauma-informed policy approach to create a resilient urban food system. Public Health Nutr. 2018;21:1961–1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Loopstra R, Tarasuk V. Perspectives on community gardens, community kitchens and the Good Food Box program in a community-based sample of low-income families. Canadian Journal of Public Health. 2013;104:e55–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Robinson OC. Sampling in interview-based qualitative research: A theoretical and practical guide. Qualitative research in psychology. 2014;11:25–41. [Google Scholar]
- 53.Hewitt J Ethical components of researcher—researched relationships in qualitative interviewing. Qualitative health research. 2007;17:1149–1159. [DOI] [PubMed] [Google Scholar]
- 54.Department of Health and Human Services. Healthy People 2020. Washington, DC: US: Department of Health and Human Services, Office of Disease Prevention and Health Promotion; 2016. [Google Scholar]