Abstract
Electronic cigarettes use is a growing trend in contemporary societies, with the propensity to compete with traditional tobacco smoking. Some preclinical studies demonstrated the toxic and detrimental effects of electronic cigarettes liquid components. Its impact on human health remains unknown and insufficiently studied. While some studies suggest that electronic cigarettes use might be associated with endothelial dysfunction, impaired platelet function and increased risk of adverse clinical events, other studies did not confirm these findings and epidemiological data mostly suggest that the use of electronic cigarettes appears to be safer than that of traditional tobacco cigarettes. This article provides an up-to-date overview of the current state of knowledge regarding electronic cigarettes and their impact on human health, with special emphasis on their effect on cardiovascular diseases.
Keywords: Electronic cigarettes, cardiovascular system, heart, health, risk, cerebrovascular, tobacco, mortality, smoking
The ancient rite of smoking dates back thousands of years, and tobacco smoking has been largely ingrained in our civilization since the arrival of Europeans to the Americas in the 16th century. For a long time, cigarette smoking was perceived as a symbol of wealth, glamour and sophistication, whereas nowadays it is largely recognised as the first preventable or modifiable cause of common diseases in developed societies.[1,2]
The prevalence of smoking worldwide is substantial and is associated with a high attributable disease burden. In particular, up to 11.5% of global deaths can be linked to smoking.[3] Being decisively fought by every medical association and government organisation, smoking addiction has dramatically evolved in recent times, thanks to the widespread distribution of electronic cigarettes. Consequently, classic cigarette smoking among US adults has declined from 20.9% in 2005 to 15.5% in 2016, as shown in the National Health Interview Survey, while the proportion of those who quit smoking increased by almost 10% from 2005 to 2016.[4] However, while a significant decline in cigarette smoking has been reported in the majority of developed societies, the upsurge in electronic cigarettes use is a worrying trend, particularly due to the lack of longitudinal data on their safety and health effects.[4]
Initially seen as a fancy object, electronic cigarettes have rapidly gained attention both as a tool aiding in tobacco smoking cessation and as a substitute for traditional tobacco addiction. Electronic nicotine delivery systems can emulate the gestures, sensations and pharmacological effects of cigarettes without a strictly defined combustion process. They do so by heating a solution of glycols or glycerol, flavourings and nicotine.
The first electronic cigarette device was patented in the 1930s. The first functioning prototypes were created in the 1960s, but their commercialisation failed. In the early 1980s, Phil Ray, a computer pioneer, along with his physician, Norman Jacobson, revisited and designed a more realistic functioning device, but this had a limited commercial impact. These first devices, merely relying on nicotine evaporation, were perceived as ineffective by conventional tobacco users. After a series of other, mostly unsuccessful, attempts at the dawn of the new millennium, the current version of the electronic cigarette was created in Beijing, China, in the early 2000s, by a smoker pharmacist who rediscovered the device after his father died of smoke-related lung cancer. After being patented in 2004, electronic cigarettes had a strong and steady increase in popularity worldwide.[5] They launched in Europe in 2006, and then in the US.[5,6] Subsequently, intense and controversial intellectual and legal battles began among supporters and opponents of this emerging smoking lifestyle.
Currently, there is no clear and unequivocal consensus about the health effects of ‘vaping’, as the act of smoking an electronic cigarette is commonly called. Is this a benign trend without detrimental health risks and consequences or is it a wolf in sheep’s clothing?[6] The principal goals of this article are to shed some light on the current state of medical and epidemiological knowledge on electronic cigarettes, and to provide succinct and up-to-date information regarding their potential association with cardiovascular risks.
Epidemiology of Electronic Cigarette Usage
In the US, there has been a constant rise in the number of electronic cigarette smokers. The latest data obtained from the National Health Interview Survey showed that 15.3% of adults had repeatedly used an electronic cigarette, while the incidence of active users (defined as at least one electronic cigarette smoked in the past 30 days) was 3.2%. Interestingly, the population that had the highest propensity for the new trend were current tobacco smokers, while former smokers constituted only a small fraction of new vapers; of note, the proportion of non-smokers who started using electronic smoking devices was rather low.[7]
Recent data from the Behavioural Risk Factor Surveillance System (BRFSS) suggest that the use of electronic cigarettes is increasing among never-smokers, to nearly 2 million US adults in 2016.[8] The mean prevalence of never-smokers who smoked electronic cigarettes at least once ranges from 0.1 to 3.8%.[7–9,10] Those electronic cigarette users who have never smoked conventional cigarettes are defined as ‘sole electronic cigarettearette’ users in the literature. Of note, electronic cigarettes are unlikely to be a trigger for smoking initiation or relapse among adults in the US.[11] A low prevalence of cessation among infrequent electronic cigarette users has been well-documented in a study of recent smokers in the US.[12] Similarly, individuals with a positive history of cardiovascular disease who recently quit smoking or reported a recent quit attempt were more likely to use electronic cigarettes compared with current smokers and those who did not report a quit attempt.[13]
In the EU, 20% of current smokers, 4.7% of former smokers and only 1.2% of never-smokers reported having used an electronic cigarette. Epidemiological data also suggest that electronic cigarette users appear to be younger, more educated, with higher income, and a slight and variable prevalence of men and white people.[14] Data from the BRFSS also showed that electronic cigarette use is a common habit, especially among younger adults, current cigarette smokers and people with comorbid conditions.[9,10]
There is an alarming uptrend in the use of electronic cigarettes among US high school students, with a prevalence ranging from 10 to 13% in 2016.[15] In the most recent annual National Youth Tobacco Survey, the Centers for Disease Control and Prevention found that the number of high school students using tobacco, including electronic cigarettes, increased by 38%, with most of the new smokers using electronic cigarettes. In this population, electronic cigarette use increased by almost 78%, with the total prevalence of active vapers reaching 21%, up from 12% in 2017. Importantly, 15% of this population combined vaping and smoking of traditional tobacco cigarettes. According to this report, the use of standard cigarettes and cigars did not increase during the observed period.[16] Furthermore, the introduction of JUUL, an innovative electronic cigarette that looks like a USB drive, has seen a rapid uptake among youth and young adults.[17] This design provides delivery of high nicotine concentrations, while the potential health hazards associated with this product are unknown.[18] The most recent report by Bold et al. revealed that electronic cigarette use among young people in public schools was associated with future cigarette use during the three-wave period (2013, 2014 and 2015), whereas cigarette use was not associated with future electronic cigarette use.[19] In contrast, according to large-scale surveys and cross-sectional analyses of randomised controlled trials, the majority of electronic cigarette users perceive these devices as a tool to quit regular tobacco smoking.[20,21]
How do Electronic Cigarettes Work?
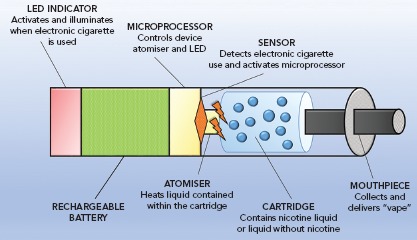
These devices try to mimic the experience of smoking by resembling the shape of a conventional cigarette. The most common type of electronic cigarette cartridge contains a propylene glycol or glycerol solution, with or without added nicotine, and generally with a flavour. Heating the compound creates a resistance within the cartridge, generating a vapour that is inhaled by the user. The basic functioning unit of electronic cigarettes is shown in Figure 1. Thousands of flavours are available, and health concerns exist about the potential role and effects of these chemicals. Almost more than 8,000 unique flavours and more than 450 brands of electronic cigarettes have been reported, with limited data suggesting that these substances are potentially detrimental to human health; many of these substances are known irritants or can increase susceptibility to viral infections.[22–24] As a consequence of the structure of the device itself, many different heavy metals, such as chromium, manganese and even arsenic, have been reported to be detected in electronic cigarette liquids and aerosols. Moreover, combustion is not part of the process, combustion-related compounds have been detected in electronic cigarette smoke, including nitrosamines, organic acids and phenolic compounds.[25,26]
Figure 1: Schematic Diagram of Electronic Cigarette System.
The average nicotine concentration per cartridge is usually <36 mg/ml, with the most common variants ranging from 6 to 18 mg/ml. Importantly, some biochemical analyses have shown that most of the devices actually provide an effective dose of nicotine that is higher than the concentration declared on the label, while some nicotine-free cartridges were found to deliver nicotine.[27,28] Furthermore, it has been documented that more experienced users, who exhibit longer and more frequent aspirations, have higher blood nicotine levels compared to classic tobacco smokers, whereas less experienced users have consistently lower levels of nicotine in their circulation.[29–31] Therefore it can be seen that these novel electronic cigarette systems allow users to regulate the amount of nicotine they inhale, thereby raising a valid concern regarding nicotine abuse and its addiction potential.[32] Furthermore, vaping low-nicotine versus high-nicotine e-liquid in electronic cigarettes is accompanied by an increase in wattage and larger quantities of potentially harmful e-liquid consumption.[33]
As the use of alternative nicotine delivery products is increasing worldwide and may surpass the use of conventional cigarettes in some parts of the world, it is a pertinent research question to elucidate the explicit role of nicotine in the development of cardiovascular and other systemic diseases. Recently, nicotine has been implicated in the impairment of vascular function, endothelial dysfunction and increased vascular calcification and stiffness.[34]
Potential Health Harms of Electronic Cigarettes Unrelated to Cardiovascular Risk
No long-term observational data exist about the health effects of these technologies on human health. However, it is an intuitive concept that electronic cigarettes should present fewer health risks than traditional cigarettes.[35] In support of this notion, a recent study by Goniewicz et al. demonstrated that substituting tobacco cigarettes with electronic cigarettes may result in significantly lower exposure to the wide array of toxins and carcinogens that are present in tobacco, thus suggesting a role of electronic cigarettes as a potential harm reduction device.[36] One study has shown that electronic cigarette smokers have fewer toxins and carcinogens in their urine compared with conventional cigarette smokers.[37,38] Nonetheless, the health-related effects of the vapour fumes are unknown, and the levels of carcinogenic compounds found may vary, largely due to the heterogeneity of the available commercial products.
It is known that at high temperatures, propylene glycol may form propylene oxide, a probable human carcinogen, while glycerol produces acrolein, which is a known human toxin.[39] Importantly, both of these substances constitute the major ingredients of most refill solutions, and can form formaldehyde and acetaldehyde, which are both established human carcinogens.[40–43] Electronic cigarettes also produce aerosols that include polycyclic aromatic hydrocarbons, nitrosamines and silicate particles, which are well-documented carcinogens.[44–47] Detrimental carbonyl content was significantly increased in exhaled breath during electronic cigarette use compared with non-vaping users.[46] The effects of artificial flavours are similarly uncertain. Some studies suggest a link between some chemical compounds used to emulate specific sweet tastes and respiratory irritation and cytotoxicity.[23,48]
Current data generally suggest a varying detrimental effect of electronic cigarettes on the inner mucosa of the craniofacial region and respiratory function when compared with standard tobacco, with an especially strong association with asthma.[49–51] This association was documented in two independent surveys carried out among teenage electronic cigarette users with a risk of bronchitis symptoms directly related to the frequency of electronic cigarette usage.[46–52,53]
Detrimental acute effects of electronic cigarettes inhalation were demonstrated in a study conducted by Antoniewicz et al. among 17 healthy individuals, which showed that inhaled electronic cigarette aerosol with nicotine caused a significant increase in heart rate and arterial stiffness, and a sharp increase in flow resistance in the conducting airways.[54] Similarly, acute vaping of propylene glycol/glycerol aerosol at high wattage with or without nicotine induced significant injury to airway epithelium and impaired pulmonary gas exchange.[55] Electronic cigarettes also induce an ion channel dysfunction in airway epithelial cells, and this was partially explained by the increased acrolein production, thus associating electronic cigarette use with chronic bronchitis onset and progression, as well as chronic obstructive pulmonary disease severity.[56]
Additionally, electronic cigarettes induced a greater efflux of inflammatory mediators from chronic obstructive pulmonary disease lung cells, implicating that the use of electronic cigarettes in chronic obstructive pulmonary disease might be associated with a worse clinical picture and exacerbations.[57] Oral gum disease has also been associated with electronic nicotine products, with electronic cigarette users having an increased odds of being diagnosed with gum disease and bone loss around teeth (OR 1.76, 95% CI [1.12–2.76] and OR 1.67, 95% CI [1.06–2.63], respectively), compared with non-smokers.[58] Among university students, vaping was associated with illicit drug use, mental health problems and impulsivity.[59] Finally, a preclinical study showed that electronic cigarette vapours impaired gonadal function in male rats, although this early finding is yet to be confirmed in human studies.[60]
Electronic Cigarettes as a Road to Quit Cigarette Addiction
The role of this technology in the difficult path to quitting smoking addiction has been postulated and investigated in small-sized studies. By looking and tasting like traditional tobacco and, moreover, by allowing the social rite of smoking as well as the physical hand-to-mouth gesture, electronic cigarettes could indeed be more effective than other smoking cessation strategies.
Preliminary evidence suggests that electronic cigarettes can reduce tobacco cravings and nicotine abstinence symptoms.[30,61] A survey study conducted in the US found that electronic cigarette smokers had a higher probability of succeeding in quitting (8.2% versus 4.8%), compared with smokers who did not use electronic cigarettes.[62] A small study conducted in Italy demonstrated a cessation rate of 12.5% among electronic cigarette smokers after 24 months.[63] This favourable trend is still debated, because other studies have failed to prove a higher rate of quitting. Recently a large meta-analysis found 28% (OR 0.72, 95% CI [0.57–0.91]) lower odds of quitting smoking in patients who used electronic cigarettes compared with those who did not use electronic cigarettes.[64–66]
In a very recent article by Hajek et al., a pragmatic randomised controlled trial with nearly 1,000 smokers motivated to quit smoking was reported. [67] Participants were randomised to either electronic cigarettes containing nicotine at 18 mg/ml or to a nicotine-replacement product, both accompanied with behavioural support. The results indicated that electronic cigarettes were more effective than standard replacement therapies considering the rate of abstinence at 1 year, although the overall success rate was poor in both examined groups (<1 in 5 for electronic cigarettes and <1 in 10 for nicotine replacement).[67] An interesting observation from this trial was that, among participants with sustained abstinence at one year, the cumulative incidence of continued electronic cigarette use was much higher among those that were randomised to electronic cigarettes compared with those that continued to use nicotine replacement in the nicotine-replacement group (80% versus 9%, respectively).[68]
This important finding further reinforces the need to ascertain potential health consequences of long-term electronic cigarette use. Furthermore, there is also a tangible concern about the role of electronic cigarettes as a bridge towards a classical tobacco addition. A systematic review and meta-analysis of epidemiological studies comprising thousands of US young adults, and a subsequent prospective study, showed that initiation of cigarette smoking is more common among previously electronic cigarette users compared with previous cigarette non-users.[69,70] A huge variety of available refill flavours certainly impose a potential to enhance the appeal to novice users, making the initial exposure more pleasurable and perhaps more likely to occur.
Electronic Cigarettes and Cardiovascular Risks
There is no consensus about the effects of electronic cigarettes on the cardiovascular system, with most of the available data coming from preclinical studies. The effects of electronic cigarettes on cardiovascular health are summarised in Table 1, while postulated effects on the heart and vasculature, mainly derived from preclinical studies, are shown in Figure 2.
Table 1: Clinical and Preclinical Studies that Examined the Effects of Electronic Cigarettes on Cardiovascular Health.
| Study | Type of Study | Observed Effect |
|---|---|---|
| Antoniewicz et al. 2019[54] | C | Acute inhalation of electronic cigarette aerosols with nicotine among healthy volunteers caused: ↑ heart rate, ↑ arterial stiffness, ↑ flow resistance in conducting airways |
| Chatterjee et al. 2019[79] | C | Acute electronic cigarette aerosol inhalation, without nicotine, led to the transient increase of circulating ↑ ICAM-1 and reactive oxygen species ↑ |
| Alzahrani et al. 2019[73] | C | Daily electronic cigarette use ↑ odds of having a myocardial infarction (OR 1.79, 95% CI 1.20–2.66, p=0.004) |
| Nocella et al. 2018[104] | C | ↑ Soluble CD-40 ligand, ↑ soluble P-selectin, ↑ platelet aggregation |
| Wang et al. 2018[105] | C | Electronic cigarette-only use, compared with no product use, was associated with ↑ general health scores, ↑ breathing difficulty scores, ↑ higher proportion of self-reported chest pain, palpitations, CAD, arrhythmia, COPD and asthma |
| Quasim et al. 2018[106] | P | In mice, short-term electronic cigarette exposure ↑ risk of thrombogenesis and ↑ platelet function |
| Chaumont et al. 2018[107] | C | Nicotine, but not electronic cigarette vehicles (propylene glycol and glycerol), ↑ acetylcholine-mediated vasodilation, ↑ indices of arterial stiffness, ↑ systolic and diastolic blood pressures and heart rate, ↑ plasma myeloperoxidase |
| Lee et al. 2018[108] | P | ↑ DNA damage, ↑ repair activity in mouse lung, heart and bladder |
| Franzen et al. 2018[75] | C | Electronic cigarette vaping led to ↑ peripheral and central arterial blood pressure, and ↑ pulse wave velocity |
| Moheimani et al. 2017[109] | C | Electronic cigarettes with nicotine caused ↑ sympathetic tone; ←→ no effect on oxidative stress (plasma paraoxonase) |
| Boas et al. 2017[96] | C | ↑ Activation of splenocardiac axis |
| Taylor et al. 2017[110] | P | No change ←→ in endothelial cell migration in vitro compared with scientific reference cigarette |
| Moheimani et al. 2017[80] | C | ↑ Cardiac sympathetic activity (habitual use), ↑ oxidative stress (habitual use) |
| Hom et al. 2016[76] | C | Platelets from healthy volunteers showed ↑ activation, ↑ adhesion, ↑ inflammation and ↑ aggregation potential upon exposure to electronic cigarette extracts of variable nicotine concentrations |
| Antoniewicz et al. 2016[111] | C | Ten puffs of electronic cigarette vapour ↑ endothelial progenitor cells in the blood of healthy volunteers |
| Anderson et al. 2016[80] | P | Electronic cigarette aerosol ↑ reactive oxygen species, induced DNA damage and cell death in EC |
| Vlachopoulos et al. 2016[78] | C | ↑ Aortic stiffness, ↑ blood pressure |
| Teasdale et al. 2016[86] | P | No change in ←→ stress response in human coronary artery endothelial cells in culture |
| Schweitzer et al. 2015[84] | P | Soluble components of electronic cigarettes, including nicotine, caused dose-dependent ↓ lung endothelial barrier function, ↑ oxidative stress, ↑ brisk inflammation |
| Palpant et al. 2015[112] | P | ↓ Decreased cardiac development in zebrafish and human embryonic stem cells |
| Farsalinos et al. 2014[77] | C | No immediate effects on myocardial relaxation |
| Szoltysek-Boldys et al. 2014[113] | C | No change ←→ in arterial stiffness |
| Farsalinos et al. 2013[48] | P | Some electronic cigarette samples had cytotoxic effect on cultured cardiomyoblasts |
C = clinical; CAD = coronary artery disease; COPD = chronic obstructive pulmonary disease; EC = endothelial cell; OR = odds ratio; P = preclinical.
Figure 2: The Physiological Effects of Electronic Cigarette Inhalation on the Heart and Vasculature.
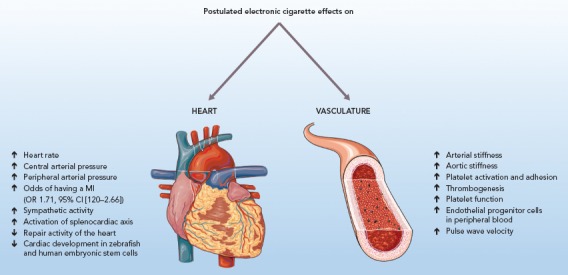
OR = odds ratio; Source: Central images kindly provided by Servier. Servier Medical Art is licensed under a Creative Commons Attribution 3.0 Unported License.
In a large cross-sectional analysis conducted among a US population, electronic cigarette use was associated with lower general health status, higher breathing difficulty scores and greater incidence of cardiac symptoms, such as chest pain, palpitations, arrhythmias or coronary artery disease.[71] Very recently, in a cross-sectional analysis of 400,000 adult respondents from the 2016 BRFSS survey, almost 70,000 people reported electronic cigarette use, and this was associated with a 71% increased risk of stroke, 59% higher risk of acute MI and a 40% higher risk of angina and coronary artery disease; moreover, they had twice the risk of switching to regular cigarettes.[72] Similarly, in a recent logistic regression analysis performed among the National Health Interview Surveys 2014–2016 population, daily electronic cigarette use, after adjusting for conventional tobacco exposure and other risk factors, was significantly associated with a 79% increase in the odds of suffering an acute MI.[73] In contrast, pooled data from the BRFSS 2016–2017 sample that included almost 450,000 participants failed to find a significant association between sole electronic cigarette use in never-smokers and cardiovascular disease, whereas dual use of electronic cigarettes and combustible cigarettes was associated with a 36% higher odds of cardiovascular disease compared with tobacco smoking alone.[74]
Limited data currently exist regarding the general cardiac effects of electronic cigarette smoking. After vaping one electronic cigarette, an acute and significant rise in peripheral arterial pressure was observed together with a steep increment in heart rate, and both changes lasted up to 45 minutes.[75] It has also been demonstrated that, among healthy electronic cigarette users, heart rate variability shifted towards a sympathetic predominance with the decreased vagal tone, which are both risk factors of cardiovascular mortality. Interestingly, these effects were unrelated to nicotine, as its plasma levels were virtually undetectable.[76]
A study used transthoracic echocardiography to evaluate LVF before and after smoking one tobacco cigarette or vaping an electronic cigarette for 7 minutes with a refill that had a medium-strength nicotine concentration. It was found that while baseline parameters were comparable in both groups, after regular tobacco cigarette use, participants had higher Myocardial Performance Index, prolonged isovolumic relaxation time, and decreased diastolic strain rate and mitral annular early diastolic velocity, thus indicating a relevant diastolic impairment. In contrast, electronic cigarette users had no significant changes in immediate haemodynamic parameters of both systolic and diastolic function.[77]
In a small prospective study, electronic cigarette smoking for >30 minutes (which is considered comparable to classic cigarette smoking for >5 minutes) induced an unfavourable acute effect on aortic stiffness and blood pressure, which are known predictors of cardiovascular risk and all-cause mortality.[78] In terms of acute effects of electronic cigarette aerosol inhalation in healthy subjects, one study revealed a transient increase in oxidative stress and inflammation parameters, thus suggesting that electronic cigarette exposure without nicotine might drive the onset of vascular pathologies through reactive oxygen species and immune cell adhesion pathways.[79] Similarly, a small clinical study by Antoniewicz et al. demonstrated that inhaled electronic cigarette aerosols with nicotine had an acute negative impact on vascular and pulmonary function.[54]
An in vitro study by Farsalinos et al. showed that the extract from electronic cigarettes (containing different flavours and nicotine quantity) applied to cultured myocardial cells at different dilution, both with or without nicotine, was cytotoxic at different concentrations irrespective of nicotine presence. The base solution consisting of glycerol and propylene glycol was not found to be cytotoxic at any concentration.[48] These results seem to suggest that the toxic effects of electronic cigarettes could be elicited by the added flavours.
In a similar experimental study, the application of aerosol extracts from electronic cigarettes on vascular endothelial cells for at least 4 hours induced a significant escalation in reactive oxygen species generation, causing DNA damage and reducing cell viability in a dose-dependent manner. Both apoptosis and programmed necrosis pathways were upregulated; moreover, treatment with alpha-tocopherol and n-acetylcysteine, which have recognised anti-oxidant properties, provided a partial rescue of these cells, thus suggesting the involvement of reactive oxygen species in this pathological cascade.[80]
The potential interference with thrombosis and inflammation mechanisms was suggested by another study showing that exposing platelets to electronic cigarette vapour extracts induced a significant upregulation of the pro-inflammatory complementary elements C1 and C3b, even higher than traditional tobacco smoke extracts, and was accompanied with a concomitant boost in platelet activation, aggregation and adhesion capacity. These effects were independent of nicotine concentration, as the presence of pure nicotine extract resulted in the inhibition of platelet functions, suggesting that maybe other constituents of electronic cigarettes can antagonise normal platelet function; nonetheless, the presence of nicotine could somehow perpetuate platelet functional changes in a dose-dependent manner, making its role in electronic cigarette-induced damage even more inconclusive.[81]
Another link to cellular dysfunction induced by vaping was provided by a study analysing the response of liver Kupffer cells both to classic and electronic cigarette extracts exposure. In both cases, a strong inflammatory response was elicited, paired with increased oxidative stress and systemic cytokine release, which likely affected platelet function and general circulatory homeostasis.[82]
Platelet function seems to be modified by electronic cigarette vapours. In a mouse model of electronic cigarette exposure, platelets that were exposed to electronic cigarettes were more hyperactive, with a greater propensity towards aggregation induced by dense alpha granules secretion, and activation of alphaIIb-beta3 receptors and protein kinase B-extracellular signal-regulated kinase pathways.[83] Moreover, these cells were also less sensitive to prostacyclin-induced inhibition when compared with clean air-exposed cells. These changes could theoretically increase the overall risk of thromboembolic events.
Other evidence of the possible irritant and inflammatory effect on cells comes from an in vitro study in which the exposure of tracheobronchial cells to electronic cigarette nicotine-free vapours was related to a concomitant increase in interleukin-6 and interleukin-8 cytokine production with a dose-dependent response and direct evidence of endothelial dysfunction.[84] The association with inflammation and endothelial dysfunction is most likely mediated via nitric oxide pathways; although to a lesser degree than standard cigarettes, electronic cigarettes lead to an important increase in soluble nicotinamide adenine dinucleotide phosphate oxidase 2-derived peptides and a concomitant decrease in nitric oxide bioavailability.[85] Nonetheless, in human coronary endothelial cells, tobacco smoke, but not electronic cigarette aerosols, was shown to induce nuclear factor erythroid 2-related factor 2 oxidative stress sensing factor transcription.[86]
In another study, exposure of umbilical endothelial vein cells to electronic cigarette compounds induced cytotoxic pathways, inhibited cell proliferation and altered cellular morphology when compared with regular tobacco.[87] An animal study suggested that electronic cigarettes could also hamper metabolic homeostasis. Experiments on 14-day-old mice showed that those exposed to electronic cigarettes had lower bodyweight compared with non-exposed mice, irrespective of nicotine concentration. Furthermore, these vapours could elicit persistent behavioural changes later in adulthood.[88]
A recent study focused on the new device subtype of the heat-not-burn tobacco cigarettes (IQOS in particular), also casting shadows on the potential toxic effect of these products. After 72 hours of exposure to the aerosols generated by heat-not-burn devices, both bronchial epithelial cells and smooth muscle cells suffered a loss of viability, and an increase in lactate dehydrogenase release, collagen I and fibronectin, with a detrimental effect on the mitochondrial respiration chain. Notably, many of these effects were achieved with lower concentrated aerosols than the aerosols produced by standard electronic cigarettes.[89]
Concerns about cardiac adverse events also directly involve nicotine, which is found at the same concentration in the blood of experienced electronic cigarette users as classic smokers. Nicotine has known pathological effects, mainly related to the excessive release of catecholamines, endothelial dysregulation and increased insulin resistance.[90] Nicotine in electronic cigarettes has been shown to increase heart rate after overnight abstinence.[91]
Regarding lipid metabolism, nicotine in electronic cigarettes has been shown to increase the amount of circulating saturated fatty acids, decreasing the content of unsaturated fatty acids and inducing insulin resistance. Nicotine can also promote endothelial dysfunction, inhibit cellular apoptosis and enhance angiogenesis, thereby raising concerns about its possible role in the pathophysiology of atherosclerosis and even cancer development.[92,93] Interestingly, in another experiment, rats exposed to electronic cigarette refill liquid had better metabolic profiles, with decreased total cholesterol, low-density lipoprotein cholesterol and low-density lipoprotein:high-density lipoprotein ratio. However, caution is required in interpreting these results, as this perceivable benefit was accompanied with a significant elevation in liver enzymes, thus establishing these apparently beneficial changes as a mere reflection of the toxic damage of electronic cigarette liquid on the liver.[94]
Recently, electronic cigarettes have been proposed as a possible interfering factor in the splenocardiac axis, a signalling network involving the brain, autonomic nervous system and hematopoietic tissues. Of note, after suffering acute stress, a sympathetic activity can cause efflux of leukocytes and progenitor cells from the bone marrow and spleen; these cells subsequently enter the arterial wall and promote atherosclerosis.[95] In young adults who chronically used electronic cigarettes, FDG-PET CT showed increased uptake in the spleen and aortic wall compared with non-users, which is consistent with the engagement of the splenocardiac axis by the substances released by these devices.[96]
The effect on physical properties of the cardiovascular system come from a study of mice exposed to electronic cigarette vapours for 8 months (4 hours a day for 5 days a week, emulating an equivalent of 20 years of exposure in humans). This resulted in a 2.5-fold increase in aortic stiffness, a 24% lower maximal aortic relaxation in response to methacholine and a trend towards a reduction in left ventricular ejection fraction.[97] Nonetheless, in humans, it seems that electronic cigarettes could be less harmful than standard cigarettes, as hypertensive patients who switched to electronic cigarettes benefited from a reduction in mean arterial blood pressure and improved pressure control.[98]
It should be emphasised that most of the data on the cardiovascular effects of electronic cigarettes are derived from preclinical, cross-sectional or small-sized clinical studies in which standard cigarettes were used as a comparison arm, thus providing limiting and conflicting results. A large majority of such studies were also not designed to infer causality. Furthermore, most of these studies focused on the acute effects of electronic cigarette exposure, whereas it is unknown how and if these effects would translate to chronic and longitudinal electronic cigarette use. Likewise, population-wide studies have been confounded by combustible cigarette use, thus making the effect of electronic cigarettes alone challenging for interpretation.
Another important issue is the varying pattern of electronic cigarette use among different groups; for example, dual users of electronic cigarettes and combustible cigarettes, former smokers, and never-smokers that use electronic cigarettes. Even within the electronic cigarette smoking population, the large heterogeneity of available electronic cigarette products, different nicotine concentrations and varying levels of daily exposure pose a real difficulty in ascertaining the true effect of electronic cigarettes on general and cardiovascular health.
It should also be noted that the National Academies of Sciences, Engineering, and Medicine in 2018 released a report summarising available evidence regarding the public health consequences of electronic cigarette use.[99] That report concluded that there is no available evidence as to whether or not electronic cigarette use is associated with clinical cardiovascular disease outcomes and subclinical atherosclerosis. Due to this, further investigation is warranted, as the long-term and longitudinal impacts of electronic cigarettes on cardiovascular health at the present moment remain unclear.
Regulatory Approval of Electronic Cigarettes
Regulatory approval of electronic cigarettes varies by country and is constantly evolving to preserve public health interests, as data build up. On a global scale, the WHO suggested stopping the promotion of electronic cigarettes to non-smokers and young people, and restricting the possibilities of advertising and indoor use.[100] Likewise, the American College of Preventive Medicine’s Prevention Practice Committee recently issued a consensus-based statement recommending that electronic nicotine delivery systems should be screened in the general population, with special emphasis on electronic nicotine delivery systems initiation prevention among youth, but also in smokers intending to quit.[101]
In 2016, the US Food and Drug Administration (FDA) firmly regulated cigarettes and smokeless tobacco, including electronic cigarettes, prohibiting their sale to teens and even distribution of free samples. However, it allowed commercialisation of flavours and did not impose restrictions on electronic cigarette advertisements. The current FDA regulations also bind manufacturers to submit an application to list the chemicals inside the devices and to prove that their products respect relevant safety standards. Besides FDA indications, many US states have banned the use of electronic cigarettes in areas where traditional smoking is already forbidden.
It is an interesting fact that in the largest coordinated enforcement effort in the FDA’s history, the agency issued more than 1,300 warning letters and fines to retailers that illegally sold JUUL and other electronic cigarettes brands to minors.[102] This phenomenon shows that there are substantial challenges involving the legal regulation and on-market monitoring of these products. The European Parliament approved a directive that limits the maximum amount of nicotine in electronic cigarettes; products containing >20 mg/ml of nicotine are regulated as medical devices.
Finally, as traditional smoking is forbidden in public places in most developed societies, resulting in a tangible reduction in smoking prevalence in the US, it has been postulated that electronic cigarettes could ‘renormalise’ the smoking habit, thus jeopardising the social perception of health risks imposed by tobacco products.[103]
Conclusion
To date, there is no conclusive and clear data on the effects of electronic cigarettes on cardiovascular and general health, especially from a longitudinal perspective. While waiting for more evidence, it seems reasonable to consider electronic cigarettes as a better option when compared with conventional tobacco products, but at the same time it should be fairly obvious that no smoke is better than electronic smoke.
References
- 1.Rippe JM. Lifestyle strategies for risk factor reduction, prevention, and treatment of cardiovascular disease. Am J Lifestyle Med. 2018;13:204–12. doi: 10.1177/1559827618812395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Castaldelli-Maia JM, Ventriglio A, Bhugra D. Tobacco smoking: From ‘glamour’ to ‘stigma’. A comprehensive review. Psychiatry Clin Neurosci. 2016;70:24–33. doi: 10.1111/pcn.12365. [DOI] [PubMed] [Google Scholar]
- 3.Reitsma MB, Fullman N, Ng M et al. Smoking prevalence and attributable disease burden in 195 countries and territories, 1990-2015: a systematic analysis from the Global Burden of Disease Study 2015. Lancet. 2017;389:1885–1906. doi: 10.1016/S0140-6736(17)30819-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang TW, Asman K, Gentzke AS et al. Tobacco product use among adults - United States, 2017. MMWR Morb Mortal Wkly Rep. 2018;67:1225–32. doi: 10.15585/mmwr.mm6744a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Franck C, Budlovsky T, Windle SB et al. Electronic cigarettes in North America: history, use, and implications for smoking cessation. Circulation. 2014;129:1945–52. doi: 10.1161/CIRCULATIONAHA.113.006416. [DOI] [PubMed] [Google Scholar]
- 6.Neuberger M. The electronic cigarette: a wolf in sheep’s clothing. Wien Klin Wochenschr. 2015;127:385–7. doi: 10.1007/s00508-015-0753-3. [DOI] [PubMed] [Google Scholar]
- 7.Bao W, Xu G, Lu J et al. Changes in electronic cigarette use among adults in the United States, 2014-2016. JAMA. 2018;319:2039–41. doi: 10.1001/jama.2018.4658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mirbolouk M, Charkhchi P, Orimoloye OA et al. E-cigarette use without a history of combustible cigarette smoking among U.S. adults: Behavioral Risk Factor Surveillance System, 2016. Ann Intern Med. 2019;170:76–9. doi: 10.7326/M18-1826. [DOI] [PubMed] [Google Scholar]
- 9.Mirbolouk M, Charkhchi P, Kianoush S et al. Prevalence and distribution of e-cigarette use among U.S. adults: Behavioral Risk Factor Surveillance System, 2016. Ann Intern Med. 2018;169:429–38. doi: 10.7326/M17-3440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hajek P, Etter JF, Benowitz N et al. Electronic cigarettes: review of use, content, safety, effects on smokers and potential for harm and benefit. Addiction. 2014;109:1801–10. doi: 10.1111/add.12659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Delnevo CD, Giovenco DP, Steinberg MB et al. Patterns of electronic cigarette use among adults in the United States. Nicotine Tob Res. 2016;18:715–9. doi: 10.1093/ntr/ntv237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Giovenco DP, Delnevo CD. Prevalence of population smoking cessation by electronic cigarette use status in a national sample of recent smokers. Addict Behav. 2018;76:129–34. doi: 10.1016/j.addbeh.2017.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stokes A, Collins JM, Berry KM et al. Electronic cigarette prevalence and patterns of use in adults with a history of cardiovascular disease in the United States. J Am Heart Assoc. 2018;7 doi: 10.1161/JAHA.117.007602. e007602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vardavas CI, Filippidis FT, Agaku IT. Determinants and prevalence of e-cigarette use throughout the European Union: a secondary analysis of 26 566 youth and adults from 27 countries. Tob Control. 2015;24:442–8. doi: 10.1136/tobaccocontrol-2013-051394. [DOI] [PubMed] [Google Scholar]
- 15.Jamal A, Gentzke A, Hu SS et al. Tobacco use among middle and high school students – United States, 2011-2016. MMWR Morb Mortal Wkly Rep. 2017;66:597–603. doi: 10.15585/mmwr.mm6623a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gentzke AS, Creamer M, Cullen K et al. Vital Signs: tobacco product use among middle and high school students – United States, 2011-2018. MMWR Morb Mortal Wkly Rep. 2019;68:157–64. doi: 10.15585/mmwr.mm6806e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hammond D, Wackowski OA Use of JUUL e-cigarettes among youth in the United States. Nicotine Tob Res. 2018. epub ahead of press. [DOI] [PMC free article] [PubMed]
- 18.Huang J, Duan Z, Kwok J et al. Vaping versus JUULing: how the extraordinary growth and marketing of JUUL transformed the US retail e-cigarette market. Tob Control. 2019;28:146–51. doi: 10.1136/tobaccocontrol-2018-054382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bold KW, Kong G, Camenga DR et al. Trajectories of e-cigarette and conventional cigarette use among youth. Pediatrics. 2018;141 doi: 10.1542/peds.2017-1832. e20171832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barbeau AM, Burda J, Siegel M. Perceived efficacy of e-cigarettes versus nicotine replacement therapy among successful e-cigarette users: a qualitative approach. Addict Sci Clin Pract. 2013;8:5. doi: 10.1186/1940-0640-8-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pokhrel P, Fagan P, Little MA et al. Smokers who try e-cigarettes to quit smoking: findings from a multiethnic study in Hawaii. Am J Public Health. 2013;103:e57–62. doi: 10.2105/AJPH.2013.301453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu Q, Jiang D, Minor M et al. Electronic cigarette liquid increases inflammation and virus infection in primary human airway epithelial cells. PLoS One. 2014;22:9–e108342. doi: 10.1371/journal.pone.0108342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Behar RZ, Davis B, Wang Y et al. Identification of toxicants in cinnamon-flavored electronic cigarette refill fluids. Toxicol In Vitro. 2014;28:198–208. doi: 10.1016/j.tiv.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 24.Zhu SH, Sun JY, Bonnevie E et al. Four hundred and sixty brands of e-cigarettes and counting: implications for product regulation. Tob Control. 2014;23((Suppl 3)):iii3–9. doi: 10.1136/tobaccocontrol-2014-051670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McAuley TR, Hopke PK et al. Comparison of the effects of e-cigarette vapor and cigarette smoke on indoor air quality. Inhal Toxicol. 2012;24:850–7. doi: 10.3109/08958378.2012.724728. [DOI] [PubMed] [Google Scholar]
- 26.Pisinger C, Dossing M. A systematic review of health effects of electronic cigarettes. Prev Med. 2014;69:248–60. doi: 10.1016/j.ypmed.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 27.Cheng T. Chemical evaluation of electronic cigarettes. Tob Control. 2014;23((Suppl 2)):ii11–7. doi: 10.1136/tobaccocontrol-2013-051482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cameron JM, Howell DN, White JR et al. Variable and potentially fatal amounts of nicotine in e-cigarette nicotine solutions. Tob Control. 2014;23:77–8. doi: 10.1136/tobaccocontrol-2012-050604. [DOI] [PubMed] [Google Scholar]
- 29.Shahab L, Goniewicz ML, Blount BC et al. Nicotine, carcinogen, and toxin exposure in long-term e-cigarette and nicotine replacement therapy users: a cross-sectional study. Ann Intern Med. 2017;166:390–400. doi: 10.7326/M16-1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bullen C, McRobbie H, Thornley S et al. Effect of an electronic nicotine delivery device (e cigarette) on desire to smoke and withdrawal, user preferences and nicotine delivery: randomised cross-over trial. Tob Control. 2010;19:98–103. doi: 10.1136/tc.2009.031567. [DOI] [PubMed] [Google Scholar]
- 31.Vansickel AR, Eissenberg T. Electronic cigarettes: effective nicotine delivery after acute administration. Nicotine Tob Res. 2013;15:267–70. doi: 10.1093/ntr/ntr316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Benowitz NL. Nicotine addiction. N Engl J Med. 2010;362:2295–303. doi: 10.1056/NEJMra0809890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Smets J, Baeyens F, Chaumont M et al. When less is more: vaping low-nicotine vs. high-nicotine e-liquid is compensated by increased wattage and higher liquid consumption. Int J Environ Res Public Health. 2019;16:723. doi: 10.3390/ijerph16050723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Babic M, Schuchardt M, Tolle M et al. In times of tobacco-free nicotine consumption: The influence of nicotine on vascular calcification. Eur J Clin Invest. 2019;49 doi: 10.1111/eci.13077. e13077. [DOI] [PubMed] [Google Scholar]
- 35.Rigotti NA. Balancing the benefits and harms of e-cigarettes: a National Academies of Science, Engineering, and Medicine report. Ann Intern Med. 2018;168:666–7. doi: 10.7326/M18-0251. [DOI] [PubMed] [Google Scholar]
- 36.Goniewicz ML, Gawron M, Smith DM et al. Exposure to nicotine and selected toxicants in cigarette smokers who switched to electronic cigarettes: a longitudinal within-subjects observational study. Nicotine Tob Res. 2017;19:160–7. doi: 10.1093/ntr/ntw160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Farsalinos KE, Gillman IG, Melvin MS et al. Nicotine levels and presence of selected tobacco-derived toxins in tobacco flavoured electronic cigarette refill liquids. Int J. Environ Res Public Health. 2015;12:3439–52. doi: 10.3390/ijerph120403439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hecht SS, Carmella SG, Kotandeniya D et al. Evaluation of toxicant and carcinogen metabolites in the urine of e-cigarette users versus cigarette smokers. Nicotine Tob Res. 2015;17:704–9. doi: 10.1093/ntr/ntu218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vreeke S, Peyton DH, Strongin RM. Triacetin enhances levels of acrolein, formaldehyde hemiacetals, and acetaldehyde in electronic cigarette aerosols. ACS Omega. 2018;3:7165–70. doi: 10.1021/acsomega.8b00842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jensen RP, Luo W, Pankow JF et al. Hidden formaldehyde in e-cigarette aerosols. N. Engl J Med. 2015;372:392–4. doi: 10.1056/NEJMc1413069. [DOI] [PubMed] [Google Scholar]
- 41.Kosmider L, Sobczak A, Fik M et al. Carbonyl compounds in electronic cigarette vapors: effects of nicotine solvent and battery output voltage. Nicotine Tob Res. 2014;16:1319–26. doi: 10.1093/ntr/ntu078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Laino T, Tuma C, Moor P et al. Mechanisms of propylene glycol and triacetin pyrolysis. J Phys Chem A. 2012;116:4602–9. doi: 10.1021/jp300997d. [DOI] [PubMed] [Google Scholar]
- 43.Han S, Chen H, Zhang X et al. Levels of selected groups of compounds in refill solutions for electronic cigarettes. Nicotine Tob Res. 2016;18:708–14. doi: 10.1093/ntr/ntv189. [DOI] [PubMed] [Google Scholar]
- 44.Farsalinos KE, Gillman G, Poulas K et al. Tobacco-Specific Nitrosamines in Electronic Cigarettes: Comparison between Liquid and Aerosol Levels. Int J Environ Res Public Health. 2015;12:9046–53. doi: 10.3390/ijerph120809046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Edwards SH, Rossiter LM, Taylor KM et al. Tobacco-specific nitrosamines in the tobacco and mainstream smoke of U.S. commercial cigarettes. Chem Res Toxicol. 2017;30:540–51. doi: 10.1021/acs.chemrestox.6b00268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Samburova V, Bhattarai C, Strickland M et al. Aldehydes in exhaled breath during e-cigarette vaping: pilot study results. Toxics. 2018;6 doi: 10.3390/toxics6030046. pii:E46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Thirion-Romero I, Perez-Padilla R, Zabert G, Barrientos-Gutierrez I. Respiratory impact of e-cigarettes and “low-risk” tobacco. Rev Invest Clin. 2019;71:17–27. doi: 10.24875/RIC.18002616. [DOI] [PubMed] [Google Scholar]
- 48.Farsalinos KE, Romagna G, Allifranchini E et al. Comparison of the cytotoxic potential of cigarette smoke and electronic cigarette vapour extract on cultured myocardial cells. Int J Environ Res Public Health. 2013;10:5146–62. doi: 10.3390/ijerph10105146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kar M, Emre IE, Bayar Muluk N et al. Effect of electronic cigarettes on the inner mucosa of the craniofacial region. J Craniofac Surg. 2019;30:e235–8. doi: 10.1097/SCS.0000000000005190. [DOI] [PubMed] [Google Scholar]
- 50.Schweitzer RJ, Wills TA, Tam E et al. E-cigarette use and asthma in a multiethnic sample of adolescents. Prev Med. 2017;105:226–31. doi: 10.1016/j.ypmed.2017.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Clapp PW, Jaspers I. Electronic cigarettes: their constituents and potential links to asthma. Curr Allergy Asthma Rep. 2017;17:79. doi: 10.1007/s11882-017-0747-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vardavas CI, Anagnostopoulos N, Kougias M et al. Short-term pulmonary effects of using an electronic cigarette: impact on respiratory flow resistance, impedance, and exhaled nitric oxide. Chest. 2012;141:1400–6. doi: 10.1378/chest.11-2443. [DOI] [PubMed] [Google Scholar]
- 53.McConnell R, Barrington-Trimis JL, Wang K et al. Electronic cigarette use and respiratory symptoms in adolescents. Am J Respir Crit Care Med. 2017;195:1043–9. doi: 10.1164/rccm.201604-0804OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Antoniewicz L, Brynedal A, Hedman L Acute effects of electronic cigarette inhalation on the vasculature and the conducting airways. Cardiovasc Toxicol. 2019. epub ahead of press. [DOI] [PMC free article] [PubMed]
- 55.Chaumont M, van de Borne P, Bernard A et al. Fourth generation e-cigarette vaping induces transient lung inflammation and gas exchange disturbances: results from two randomized clinical trials. Am J Physiol Lung Cell Mol Physiol. 2019;316:L705–19. doi: 10.1152/ajplung.00492.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lin VY, Fain MD, Jackson PL Vaporized e-cigarette liquids induce ion transport dysfunction in airway epithelia. Am J Respir Cell Mol Biol. 2018. epub ahead of press. [DOI] [PMC free article] [PubMed]
- 57.Bozier J, Rutting S, Xenaki D et al. Heightened response to e-cigarettes in COPD. ERJ Open Res. 2019;5:00192–2018. doi: 10.1183/23120541.00192-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Atuegwu NC, Perez MF, Oncken C et al. Association between regular electronic nicotine product use and self-reported periodontal disease status: Population Assessment of Tobacco and Health Survey. Int J Environ Res Public Health. 2019;16 doi: 10.3390/ijerph16071263. pii:E1263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Grant JE, Lust K, Fridberg DJ et al. E-cigarette use (vaping) is associated with illicit drug use, mental health problems, and impulsivity in university students. Ann Clin Psychiatry. 2019;31:27–35. [PMC free article] [PubMed] [Google Scholar]
- 60.Vivarelli F, Canistro D, Cirillo S et al. Impairment of testicular function in electronic cigarette (e-cig, e-cigs) exposed rats under low-voltage and nicotine-free conditions. Life Sci. 2019;228:53–65. doi: 10.1016/j.lfs.2019.04.059. [DOI] [PubMed] [Google Scholar]
- 61.Gualano MR, Passi S, Bert F et al. Electronic cigarettes: assessing the efficacy and the adverse effects through a systematic review of published studies. J Public Health (Oxf) 2015;37:488–97. doi: 10.1093/pubmed/fdu055. [DOI] [PubMed] [Google Scholar]
- 62.Zhu SH, Zhuang YL, Wong S et al. E-cigarette use and associated changes in population smoking cessation: evidence from US current population surveys. BMJ. 2017;358 doi: 10.1136/bmj.j3262. j3262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Polosa R, Caponnetto P, Morjaria JB et al. Effect of an electronic nicotine delivery device (e-cigarette) on smoking reduction and cessation: a prospective 6-month pilot study. BMC Public Health. 2011;11:786. doi: 10.1186/1471-2458-11-786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kalkhoran S, Glantz SA. E-cigarettes and smoking cessation in real-world and clinical settings: a systematic review and meta-analysis. Lancet Respir Med. 2016;4:116–28. doi: 10.1016/S2213-2600(15)00521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Grana RA, Popova L, Ling PM. A longitudinal analysis of electronic cigarette use and smoking cessation. JAMA Intern Med. 2014;174:812–3. doi: 10.1001/jamainternmed.2014.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Al-Delaimy WK, Myers MG, Leas EC et al. E-cigarette use in the past and quitting behavior in the future: a population-based study. Am J Public Health. 2015;105:1213–9. doi: 10.2105/AJPH.2014.302482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hajek P, Phillips-Waller A, Przulj D et al. A randomized trial of e-cigarettes versus nicotine-replacement therapy. N Engl J Med. 2019;380:629–37. doi: 10.1056/NEJMoa1808779. [DOI] [PubMed] [Google Scholar]
- 68.Borrelli B. O’Connor GT. E-cigarettes to assist with smoking cessation. N Engl J Med. 2019;380:678–9. doi: 10.1056/NEJMe1816406. [DOI] [PubMed] [Google Scholar]
- 69.Soneji S, Barrington-Trimis JL, Wills TA et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 2017;171:788–97. doi: 10.1001/jamapediatrics.2017.1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Leventhal AM, Strong DR, Kirkpatrick MG et al. Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. JAMA. 2015;314:700–7. doi: 10.1001/jama.2015.8950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wang JB, Olgin JE, Nah G et al. Cigarette and e-cigarette dual use and risk of cardiopulmonary symptoms in the Health eHeart Study. PLoS One. 2018;13 doi: 10.1371/journal.pone.0198681. e0198681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ndunda PM, Muutu TM. Abstract 9: Electronic cigarette use is associated with a higher risk of stroke. Stroke. 2019;50((Suppl 1)):A9. doi: 10.1161/str.50.suppl_1.9. [DOI] [Google Scholar]
- 73.Alzahrani T, Pena I, Temesgen N et al. Association between electronic cigarette use and myocardial infarction. Am J Prev Med. 2018;55:455–61. doi: 10.1016/j.amepre.2018.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Osei AD, Mirbolouk M, Orimoloye OA The association between e-cigarette use and cardiovascular disease among never and current combustible cigarette smokers. Am J Med. 2019. epub ahead of press. [DOI] [PubMed]
- 75.Franzen KF, Willig J, Cayo Talavera S et al. E-cigarettes and cigarettes worsen peripheral and central hemodynamics as well as arterial stiffness: A randomized, double-blinded pilot study. Vasc Med. 2018;23:419–25. doi: 10.1177/1358863X18779694. [DOI] [PubMed] [Google Scholar]
- 76.Moheimani RS, Bhetraratana M, Yin F et al. Increased cardiac sympathetic activity and oxidative stress in habitual electronic cigarette users: implications for cardiovascular risk. JAMA Cardiol. 2017;2:278–84. doi: 10.1001/jamacardio.2016.5303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Farsalinos KE, Tsiapras D, Kyrzopoulos S et al. Acute effects of using an electronic nicotine-delivery device (electronic cigarette) on myocardial function: comparison with the effects of regular cigarettes. BMC Cardiovasc Disord. 2014;14:78. doi: 10.1186/1471-2261-14-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Vlachopoulos C, Ioakeimidis N, Abdelrasoul M et al. Electronic cigarette smoking increases aortic stiffness and blood pressure in young smokers. J Am Coll Cardiol. 2016;67:2802–3. doi: 10.1016/j.jacc.2016.03.569. [DOI] [PubMed] [Google Scholar]
- 79.Chatterjee S, Tao JQ, Johncola A Acute exposure to e-cigarettes causes inflammation and endothelial oxidative stress in non-smoking healthy young subjects. Am J Physiol Lung Cell Mol Physiol. 2019. epub ahead of press. [DOI] [PMC free article] [PubMed]
- 80.Anderson C, Majeste A, Hanus J, Wang S. E-cigarette aerosol exposure induces reactive oxygen species, DNA damage, and cell death in vascular endothelial cells. Toxicol Sci. 2016;154:332–40. doi: 10.1093/toxsci/kfw166. [DOI] [PubMed] [Google Scholar]
- 81.Hom S, Chen L, Wang T et al. Platelet activation, adhesion, inflammation, and aggregation potential are altered in the presence of electronic cigarette extracts of variable nicotine concentrations. Platelets. 2016;27:694–702. doi: 10.3109/09537104.2016.1158403. [DOI] [PubMed] [Google Scholar]
- 82.Rubenstein DA, Hom S, Ghebrehiwet B et al. Tobacco and e-cigarette products initiate Kupffer cell inflammatory responses. Mol Immunol. 2015;67:652–60. doi: 10.1016/j.molimm.2015.05.020. [DOI] [PubMed] [Google Scholar]
- 83.Qasim H, Karim ZA, Silva-Espinoza JC et al. Short-term e-cigarette exposure increases the risk of thrombogenesis and enhances platelet function in mice. J Am Heart Assoc. 2018;7:pe009264. doi: 10.1161/JAHA.118.009264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Schweitzer KS, Chen SX, Law S et al. Endothelial disruptive proinflammatory effects of nicotine and e-cigarette vapor exposures. Am J Physiol Lung Cell Mol Physiol. 2015;309:L175–87. doi: 10.1152/ajplung.00411.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Athyros VG, Katsiki N, Doumas M et al. Effect of tobacco smoking and smoking cessation on plasma lipoproteins and associated major cardiovascular risk factors: a narrative review. Curr Med Res Opin. 2013;29:1263–74. doi: 10.1185/03007995.2013.827566. [DOI] [PubMed] [Google Scholar]
- 86.Teasdale JE, Newby AC, Timpson NJ et al. Cigarette smoke but not electronic cigarette aerosol activates a stress response in human coronary artery endothelial cells in culture. Drug Alcohol Depend. 2016;163:256–60. doi: 10.1016/j.drugalcdep.2016.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Putzhammer R, Doppler C, Jakschitz T et al. Vapours of US and EU market leader electronic cigarette brands and liquids are cytotoxic for human vascular endothelial cells. PLoS One. 2016;11 doi: 10.1371/journal.pone.0157337. e0157337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Smith D, Aherrera A, Lopez A et al. Adult behavior in male mice exposed to e-cigarette nicotine vapors during late prenatal and early postnatal life. PLoS One. 2015;10 doi: 10.1371/journal.pone.0137953. e0137953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Sohal SS, Eapen MS, Naidu VGM et al. IQOS exposure impairs human airway cell homeostasis: direct comparison with traditional cigarette and e-cigarette. ERJ Open Res. 2019;5:00159–2018. doi: 10.1183/23120541.00159-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.US Department of Health and Human Services. How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2010. [Google Scholar]
- 91.Vansickel AR, Weaver MF, Eissenberg T. Clinical laboratory assessment of the abuse liability of an electronic cigarette. Addiction. 2012;107:1493–500. doi: 10.1111/j.1360-0443.2012.03791.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Canistro D, Vivarelli F, Cirillo S et al. E-cigarettes induce toxicological effects that can raise the cancer risk. Scientific Reports. 2017;7:2028. doi: 10.1038/s41598-017-02317-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bhatnagar A, Whitsel LP, Ribisl KM et al. Electronic cigarettes: a policy statement from the American Heart Association. Circulation. 2014;130:1418–36. doi: 10.1161/CIR.0000000000000107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.McGrath-Morrow SA, Hayashi M, Aherrera A et al. The effects of electronic cigarette emissions on systemic cotinine levels, weight and postnatal lung growth in neonatal mice. PLoS One. 2015;10 doi: 10.1371/journal.pone.0118344. e0118344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Libby P, Nahrendorf M, Swirski FK. Leukocytes link local and systemic inflammation in ischemic cardiovascular disease: an expanded “cardiovascular continuum”. J Am Coll Cardiol. 2016;67:1091–103. doi: 10.1016/j.jacc.2015.12.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Boas Z, Gupta P, Moheimani RS et al. Activation of the “Splenocardiac Axis” by electronic and tobacco cigarettes in otherwise healthy young adults. Physiol Rep. 2017;5 doi: 10.14814/phy2.13393. e13393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Olfert IM, DeVallance E, Hoskinson H et al. Chronic exposure to electronic cigarettes results in impaired cardiovascular function in mice. J Appl Physiol (1985) 2018;124:573–82. doi: 10.1152/japplphysiol.00713.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Polosa R, Morjaria JB, Caponnetto P et al. Blood pressure control in smokers with arterial hypertension who switched to electronic cigarettes. Int J Environ Res Public Health. 2016;13 doi: 10.3390/ijerph13111123. E1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Eaton DL, Kwan LY, Stratton K . Washington, DC: National Academies Press; 2018. Public Health Consequences of E-Cigarettes. [DOI] [PubMed] [Google Scholar]
- 100.El Dib R, Suzumura EA, Akl EA et al. Electronic nicotine delivery systems and/or electronic non-nicotine delivery systems for tobacco smoking cessation or reduction: a systematic review and meta-analysis. BMJ Open. 2017;7 doi: 10.1136/bmjopen-2016-012680. e012680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Livingston CJ, Freeman RJ, Costales VC et al. Electronic nicotine delivery systems or e-cigarettes: American College of Preventive Medicine’s Practice Statement. Am J Prev Med. 2019;56:167–78. doi: 10.1016/j.amepre.2018.09.010. [DOI] [PubMed] [Google Scholar]
- 102.US Food and Drug Administration. Warning letters and civil money penalties issued to retailers for selling JUUL and other e-cigarettes to minors. 12 September. 2018. https://www.fda.gov/tobacco-products/ctp-newsroom/warning-letters-and-civil-money-penalties-issued-retailers-selling-juul-and-other-e-cigarettes Available at. (accessed 7 June 2019)
- 103.Fairchild AL, Bayer R, Colgrove J. The renormalization of smoking? E-cigarettes and the tobacco “endgame”. N Engl J Med. 2014;370:293–5. doi: 10.1056/NEJMp1313940. [DOI] [PubMed] [Google Scholar]
- 104.Nocella C, Biondi-Zoccai G, Sciarretta S et al. Impact of tobacco versus electronic cigarette smoking on platelet function. Am J Cardiol. 2018;122:1477–81. doi: 10.1016/j.amjcard.2018.07.029. [DOI] [PubMed] [Google Scholar]
- 105.Wang JB, Olgin JE, Nah G et al. Cigarette and e-cigarette dual use and risk of cardiopulmonary symptoms in the Health eHeart Study. PLoS One. 2018;13 doi: 10.1371/journal.pone.0198681. e0198681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Qasim H, Karim ZA, Silva-Espinoza JC et al. Short-term e-cigarette exposure increases the risk of thrombogenesis and enhances platelet function in mice. J Am Heart Assoc. 2018;7 doi: 10.1161/JAHA.118.009264. e009264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Chaumont M, de Becker B, Zaher W et al. differential effects of e-cigarette on microvascular endothelial function, arterial stiffness and oxidative stress: a randomized crossover trial. Sci Rep. 2018;8:10378. doi: 10.1038/s41598-018-28723-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Lee HW, Park SH, Weng MW et al. E-cigarette smoke damages DNA and reduces repair activity in mouse lung, heart, and bladder as well as in human lung and bladder cells. Proc Natl Acad Sci U S A. 2018;115 doi: 10.1073/pnas.1718185115. E1560–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Moheimani RS, Bhetraratana M, Peters KM et al. Sympathomimetic effects of acute e-cigarette use: role of nicotine and non-nicotine constituents. J Am Heart Assoc. 2017;6 doi: 10.1161/JAHA.117.006579. e006579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Taylor M, Jaunky T, Hewitt K et al. A comparative assessment of e-cigarette aerosols and cigarette smoke on in vitro endothelial cell migration. Toxicol Lett. 2017;277:123–8. doi: 10.1016/j.toxlet.2017.06.001. [DOI] [PubMed] [Google Scholar]
- 111.Antoniewicz L, Bosson JA, Kuhl J et al. Electronic cigarettes increase endothelial progenitor cells in the blood of healthy volunteers. Atherosclerosis. 2016;255:179–85. doi: 10.1016/j.atherosclerosis.2016.09.064. [DOI] [PubMed] [Google Scholar]
- 112.Palpant NJ, Hofsteen P. Pabon Let al. Cardiac development in zebrafish and human embryonic stem cells is inhibited by exposure to tobacco cigarettes and e-cigarettes. PLoS One. 2015. 10. e0126259. [DOI] [PMC free article] [PubMed]
- 113.Szoltysek-Boldys I, Sobczak A, Zielinska-Danch W et al. Influence of inhaled nicotine source on arterial stiffness. Przegl Lek. 2014;71:572–5. [PubMed] [Google Scholar]


