Abstract
Today is an age of rapid digital integration, yet the capabilities of modern-day smartphones and smartwatches are underappreciated in daily clinical practice. Smartphones are ubiquitous, and smartwatches are very common and on the rise. This creates a wealth of information simply waiting to be accessed, studied and applied clinically, ranging from activity level to various heart rate metrics. This review considers commonly used devices, the validity and accuracy of the data they obtain and potential clinical application of the data.
Keywords: mHealth, Apple Watch, Fitbit, Garmin, iPhone, smartwatch, iOS, Health App, S Health, Samsung Health, Google Health, Android, Fitness Tracker, single-lead ECG, Kardia, AF
Today is an age of rapid digital integration. A decade ago, technological advancement was represented by a bulky desktop computer. With the constant evolution of microprocessors and sophistication of programming, the capacity of the mainframe has been surpassed and miniaturised, so that the pinnacle of technology and innovation is quite literally in the palm of our hands. This opens a world of possibilities, because technology is more advanced, affordable and accessible than ever before. Technological advancement has been applied to all categories of applications from games to health and wellness. This development now provides both an opportunity and challenge to healthcare providers to take advantage of this ever-growing volume of personal data collected on our patients. Technology development in the healthcare sector is extensive and expanding rapidly, and a review of emerging technologies would illustrate the amazing future potential to help practitioners manage patients remotely. This article focuses on what could happen during today’s clinic appointments for patients who currently have smartphones and wearable fitness trackers. We consider the prevalence of these devices, capabilities, accuracy and clinical applications so that clinicians can optimise patient management.
Demographics
Smartphones are ubiquitous, carried and used by nearly all adolescents and adults today. The two dominant smartphone operating systems are Android and iOS, so dominant, in fact, that collectively they account for approximately 98% market share. In Europe, the market share in 2018 was approximately 70% Android and 28% iOS, whereas in the US and UK the market share in 2018 was approximately 54% iOS and 45% Android. By device, the Apple iPhone has the largest market share in the US and UK (55%), whereas Samsung holds the greatest market share in Europe (33%), with the Apple iPhone close behind (28%).[1] These statistics serve to emphasise the importance of becoming familiar with the two dominant operating systems and the health-related features they offer.
Basic Smartphone Capabilities
Having established that nearly everyone carrying a phone has a smartphone translates to the fact that nearly every patient has additional untapped data on hand that could be used to assess health parameters, such as activity levels and heart rate (HR) and, if fully utilised by the patient, much more information, such as weight and blood pressure (BP) logs.
All Apple iPhones come with a pre-installed app called Health. Simply open the app and enter some basic demographics and it is ready to use. The Health app can also display historical data, including steps, distance and flights of stairs climbed, which are logged when the phone is carried by the user. Android devices have an analogous capability via user-installed apps, such as S Health (Samsung Health) or Google Fit. In the authors’ experience, most iPhone users are not even aware of the Health app.
Smartphones are equipped with a multitude of sensors, including accelerometers, barometers and global positioning systems (GPS), allowing for metrics such as distance travelled, elevation gain and estimated calorie expenditure to be assessed. Some apps even use the torch and camera to act as a photoplethysmograph to read HR and the regularity or irregularity of rhythm. However, this is not the intended use of the camera and torch, and the data obtained have been shown to be highly variable.[2]
The various apps generally have the same user interface on either Android or Apple iOS, and many are free. With a little instruction and a tap of the screen, patients can record a walk and review distance travelled, elevation gain, pace and estimated calorie expenditure. This can be motivating to patients and help them track and make progress.[1]
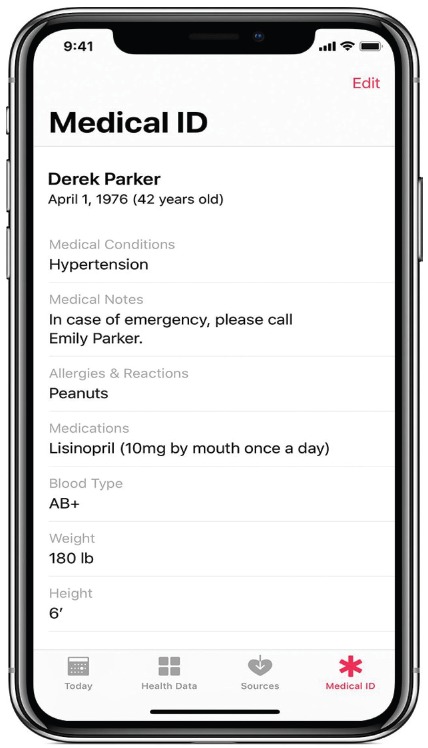
An under-appreciated feature with great potential is the electronic medical ID. The iOS Health app has this functionality built in, allowing users to input their key information, including medical conditions, medications, allergies and emergency contacts (Figure 3). US patients can even sign up on the Health app for organ donation with Donate Life America. Android apps have a similar functionality. In case of an emergency presentation, such as a cardiac arrest, physicians can easily access this information on a patient’s phone and directly call a patient’s emergency contact to notify them of the patient’s condition and obtain more history. A medical ID takes only a minute or two to set up, yet this feature is underutilised by both patients and clinicians. How far do we go with information on a smartphone-based medical ID? Is this a legal document? What if a patient’s medical ID states ‘do not resuscitate’? These are questions that need to be addressed today because these scenarios exist. We must not only consider these dilemmas, but also those that have not yet presented themselves.
Figure 3: Medical ID on iOS/iPhone.
Patients are also able to enter their own biometric information (e.g. weight and BP) for storage and easy review (Figures 1 and 2). Many scales and BP cuffs can automatically upload information to smartphones. Home BP monitoring is recommended for patients with hypertension, including the use of a BP journal to assist with ongoing management.[3] We have all had patients come into the clinic carrying a few scraps of paper with their BP readings on them. Now, for most patients, we can instruct them how to log these in their phones, solving the problem of patients who leave their paper-based BP log at home while rushing to make their appointment, because they rarely forget to bring their phone. In addition, such logging allows providers to see BP displayed as a graph over time, including ranges (Figure 1), and allows for better identification of temporal trends in BP for safer and more effective titration of BP medication. It also more actively engages patients in their own healthcare and has the potential to help increase adherence.
Figure 1: Blood Pressure Log in iOS Health App.
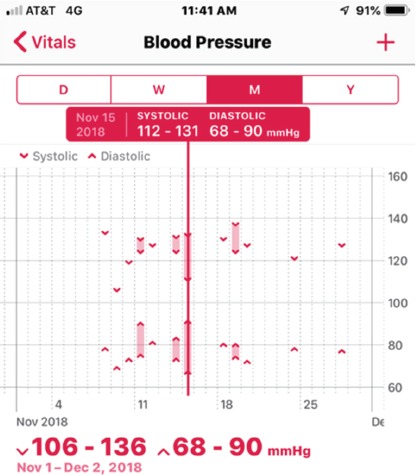
Views can be customised for different time periods and time scales. List view is also available.
Figure 2: Weight Log in iOS Health App, Plotted Over a 1-year Period.

Each data point represents the average weight for that month, and the time scale can be zoomed to a daily view, allowing for multiple weights to be logged in each day, if desired.
Addition of Sensors to Smartphones
In addition to smartphones being able to acquire primary data, they serve as a hub allowing for additional sensors to be used. AliveCor offers a small hand-held device (Kardia), which allows for on-demand, single-lead ECG recording. The device is small enough to be attached to a smartphone or can easily be kept in a pocket or purse. Patients can record a 30-second Lead 1 ECG tracing simply by placing their fingers on the contacts. This tracing is then reviewed by an algorithm to distinguish AF or other heart rhythms from sinus rhythm. Combining physician review with the algorithm increases accuracy, especially in the case of AF.[4] To date, over 30 million ECGs have been recorded using the AliveCor device. Recently, AliveCor has released the Kardia 6L, which can record 6 leads in a simple-to-use device using just the hands and a thigh.
These devices could replace traditional ambulatory ECG monitoring in some patients with palpitations. Because the device is owned by the patient, they can keep it with them indefinitely, allowing for longer-term monitoring without using intermittent monitors for a patient trying to capture a rare episode of palpitations. In some instances, this may potentially save patients from having a loop recorder implanted. It can even be used in guest mode on a friend or bystander who may be having symptoms.
Smartwatches
Currently, smartwatches are perhaps the best additional sensors to be added to a smartphone. Smartwatches have grown immensely in popularity, and Apple quickly dominated the entire watch industry, not just the smartwatch industry. In fact, Apple shipped more watches in the last quarter of 2016 than the entire Swiss watch industry combined, including Rolex and Swatch. Apple Watch quickly became the leading device, with 49% market share in 2016.[5] Over 18 million Apple Watches were sold in 2017. Fitbit, Garmin, Xiaomi and Samsung are also popular devices.
There is much similarity and overlap in the capabilities of the devices, except for a few leading technologies present in the Apple Watch Series 4 and 5, which are reviewed below. Competition and advancing technology push this market forward with better devices at lower prices, making them increasingly accessible to consumers. In 2016, Men’s Health journal estimated that one in five Americans wears a fitness tracker.[6] These data confirm the large size of this sector in technology, and the eagerness to use such devices by the general public. This is where it becomes our responsibility as clinicians to help guide patients in using the devices effectively and to their fullest.
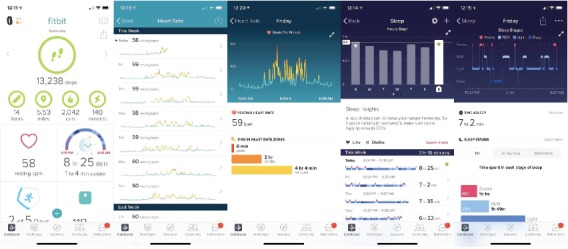
The addition of a smartwatch adds significant information without the need to carry a phone. A user with an Apple Watch, for example, will readily have metrics available, including steps, flights of stairs climbed, distance walked, stand hours, estimated energy expenditure (EE) and HR. These metrics are also available via Fitbit, Samsung and Garmin devices (Figure 4).
Figure 4: Fitbit Display.
Accuracy and Validity of Smartwatch Data
Prior to discussing the use of smartwatch data in daily practice, a review of accuracy is warranted, especially as it pertains to HR and EE. Several studies have shown that in sinus rhythm there was strong agreement between ECG HR and that recorded by the Apple Watch and Fitbit.[7,8] The Apple Watch demonstrated the strongest agreement with ECG across a variety of activities, including sitting, walking, running and cycling, within 5–10% of the ECG. In the setting of faster HRs and atrial arrhythmias, there was some underestimation of HR with smartwatches compared with ECG. Predictors of increased error in HR measurement include darker skin tone, larger wrist circumference and higher BMI. Several other studies have validated the accuracy of wrist-worn devices for HR assessment.[9–11]
The data tell a different story regarding EE. Compared against a reference standard of indirect calorimetry by expired gas analysis, all wrist-worn devices tested had a large margin of error of approximately 27%, typically overestimating expenditure.[8] Dooley et al. studied HR and EE assessment with Apple Watch, Fitbit and Garmin, and their findings are consistent with other studies showing reliability and accuracy of the devices for HR assessment, but overestimation of EE with wide error margins.[12] Attention to this fact is important in counselling patients who may make dietary decisions based on the calorie expenditure reported by their devices.
The inaccuracy of EE does not render this information useless. A study with over 2,000 participants using Fitbits over 6 months showed that a higher number of steps per day and highly active minutes per week were predictors of increased weight loss.[13] For example, patients walking <5,000 steps a day lost an average of 3.7% body weight, whereas those who walked >10,000 steps a day lost an average of 9% body weight. These metrics are easily measured by any modern activity tracker, and it appears that there may be benefit in having patients track this information. Furthermore, we as healthcare providers may review this information quickly and easily, allowing us to help patients play an active role in their health while holding them accountable to reach achievable goals. The study by Painter et al. also demonstrated that a high frequency of weigh-ins (three per week) was associated with increased weight loss at 6 months.[13] Such information is easily obtained by a scale at home and can be entered into health apps for easy tracking of progress, which is shown to correlate with achieving weight loss goals.[13]
Smartwatches also use gentle cues to nudge the wearer to live a more active life. They provide stand reminders every hour to help reduce sedentary behaviour; they also keep an easily accessible historic log of activity levels, which opens the door to many clinical applications. The use of step count has been studied as a potential marker of clinical improvement in treating patients with angina.[14] Another novel use of these data may include incorporating step count and activity level obtained by a smartwatch into a frailty model used to risk stratify patients prior to a procedure.
Heart Rate Monitoring
Perhaps the most underutilised information readily available by smartwatches is HR monitoring. Apple Watch, Fitbit, Garmin and many other smartwatches record HR data. Fitbit and Garmin watches monitor HR continuously, whereas the Apple Watch monitors HR continuously during exercise and periodically otherwise, at 3- to 10-minute intervals based on activity level.
Smartwatches use photoplethysmography (PPG)-based sensors able to distinguish pulsatile changes in blood volume under the skin, allowing for HR detection. This technology is generally capable of recognising HRs between 30 and 210 BPM. Combining HR with accelerometer data allows discrimination of resting and walking HR (Figure 5).
Figure 5: iOS Health App Heart Rate Display.

HR data may be used clinically ‘on the fly’ in many ways. Resting HR can be used as a measure of general fitness and to set a clear baseline for people with bradycardia. In patients with baseline sinus bradycardia, these devices can answer the question of chronotropic response, or guide decisions in titration of dose to achieve goal resting HR in patients on rate-lowering therapy.
In patients with known AF, HR data can be used to determine adequate rate control. In patients with paroxysmal AF, significant changes in resting HR could be indicative of the onset of AF and help determine the duration of episodes, although this is an extrapolation of data and not necessarily the intended use; however, the beauty of mHealth is integration of such information in novel ways.
In patients with palpitations, smartwatches can help determine the presence of tachyarrhythmias or bradyarrhythmias, including frequency and duration. This information can help determine whether a short- or long-term ECG monitor may be appropriate to capture an episode and identify the arrhythmia. The smartwatch data may be reviewed at each appointment as an additional tool to determine the recurrence of a supraventricular tachycardia. These uses would be extrapolations based on HR data, which can be obtained from most smartwatch fitness trackers today. However, the Apple Watch has distinguished itself with unmatched capabilities, having important implications for both patients and healthcare providers. The latest models of Apple Watch, the Series 4 and 5, are capable of screening for falls, AF, bradycardia, tachycardia and even single-lead ECG recording.
The Apple Watch Series 4 and 5 can detect AF in the background by combining accelerometer and PPG-derived HR and HR variability. PPG-based detection of AF has been validated with high accuracy.[15] A user can be notified that they may be in AF, and those with a Series 4 or 5 Apple Watch can immediately obtain a single-lead ECG right on the watch, for more accurate determination of the rhythm. “My Apple Watch says I may have AF,” has become a chief complaint from patients arriving at the emergency department or general practice or cardiology appointments. There are presumed benefits to early detection, such as more effective stroke risk reduction and prevention, given that one in five patients presenting with ischaemic stroke is newly diagnosed with AF.[16]
The recent Apple Watch Study demonstrated that the technology was rapidly mobilised to enrol over 419,000 participants in 8 months to determine whether the irregular pulse watch notification was able to identify AF on the watch and an ECG patch.[17,18] The notification occurred in 0.52% of participants, and AF was identified in 34% of the 450 who used the patch, resulting in a positive predictive value of 71%.
Although promising, there is concern about the potential for false-positive heart rhythms, and increased testing and anxiety for patients, but this was prior to the release of the Series 4 and 5 devices and their built-in ECG confirmation of rhythm, which will improve positive predictive value. This technology is not intended to monitor the burden of AF. Knowing these limitations should not deter use, but rather encourage it in an appropriate manner.
Novel Applications
The use of smartwatches is most common in the young to middle-aged population, but the advanced features of the Apple Watch Series 4 and 5 make it very appealing for use in the elderly, who are at increased risk for both falls and AF. When a fall is detected, the watch will display an alert that can be used to contact emergency services with a tap or may be dismissed if the fall was detected in error or assistance is not needed. The watch can also contact emergency services automatically if a fall is detected and there is no movement for about a minute. This feature can offer some piece of mind to families caring for members who may be alone and are at risk for falling, but the availability of this feature is probably not known to most family caregivers.
Limitations for Use
Limitations do exist, of course. The use of this technology is intimidating to some patients and physicians who may not consider themselves tech savvy and may not be comfortable reviewing these novel data sources. Patients need to be capable of understanding how to use the devices and apps and, unfortunately, the less likely users are often the same patients who may benefit the most from such monitoring, such as those who are less educated or some of the elderly population. As in every area of medicine, patient selection is key, and it comes as no surprise that frequent monitoring and availability of biometric data may be anxiety provoking for some.[19] These challenges should not be used as reasons to avoid utilisation. As our population ages, we will continue to see more patients who are more tech savvy, and the proportion of patients uncomfortable with this technology should decline.
An additional limitation relates to the amount of data. There is, of course, the potential for artefact and false-positive abnormalities. Furthermore, how do we deal with a potentially overwhelming number of patient requests to review biometric data? Data overload and patient misunderstandings in what this information means are certainly issues that will become more common, and as physicians we should be proactive in educating patients and setting achievable expectations.
In one study, 58% of smartphone users surveyed had downloaded a health app onto their device, with fitness and nutrition being the most common types of apps.[20] Not surprisingly, younger age, higher income and higher education level predicted higher-level use of such apps. Obesity was also a predictor of the use of these apps, suggesting that this subgroup of users is interested in health improvement. Some concerns among users included cost, burden of data entry and security of health information.[20]
Patient Recommendations
Because almost all patients carry a smartphone, as providers we can educate patients and encourage higher-level use of the devices they already have. A simple use may include showing a patient with poorly controlled hypertension how to enter home BP values into the iOS Health app for easy review at follow-up visits. Patients seeking to improve their fitness level may use smart devices to track activity and progress with real-time feedback. A HR monitoring smartwatch may be helpful for patients who have AF, especially with rapid HR or palpitations, because it would allow for simple, continuous HR monitoring. A Fitbit or Garmin account may be accessed from a computer or other smartphone, allowing for remote monitoring of HR and activity data. This may be particularly useful for family and caregivers to keep an eye on elderly loved ones. Smartphones and watches also have shortcuts to allow easy access to emergency services, as noted above. Of course, this is not an exhaustive list of uses, but rather the tip of the iceberg.
Although this is not intended to be a product review, it is important for clinicians to be familiar with common devices, their limitations and how to combine the cost and feature set of the watch to help patients select a device that will serve them well. In general, the entry point for a reliable wearable fitness tracker with HR monitoring is US$99–129 (Fitbit Inspire HR, Garmin vivosmart 4), with several additional models increasing in cost, screen size and functionality. This includes popular Fitbit and Garmin models with easy-to-navigate user interfaces via smartphone apps. These devices include long battery life with several days between charging. The Apple Watch Series 5 has recently replaced the Series 4 with the same entry point of US$399–429. The Series 5 adds an ‘always on display’ and a compass, but no new health-related features over the Series 4, which is available used or refurbished. Apple Watch requires daily charging but, in turn, offers a high-quality display and more advanced features, such as single-lead ECG recording and detection of falls and AF (Series 4 and later). Series 3 Apple Watches are still available at a lower price point (US$199), forgoing the advanced features of the later series. The Apple Watch does require an iPhone and cannot be used with Android devices, whereas Fitbit and Garmin smartwatches can be used with essentially all smartphones. On-demand ambulatory ECG monitoring may be added to any smartphone via the Kardia device, which is available for US$99 for single-lead ECG and US$149 for the 6-lead device..
Future Directions
mHealth is exciting not only for what it can do today, but for the seemingly endless possibilities of what it will be able to do tomorrow. Having a smartwatch capable of constant HR monitoring is becoming the norm, and the technology continues to evolve. There are prototypes of wrist-worn devices that can sense radial artery pulsation and use the data to estimate central aortic pressure (e.g. BPro Cardio Pulse-Wave Device). Further work is being done to extrapolate BP from PPG-based data and blood glucose via optical sensors of various wavelengths. It is quite plausible that, in the not-too-distant future, a smartwatch will be capable of reading HR, rhythm, BP and blood glucose, all non-invasively and in the background.
Conclusion
Only a few years ago it was hard to believe that a smartwatch no larger than a typical watch would be able to make phone calls, send and receive text messages, track sleep and activity, record HR in the background and record a single-lead ECG, but this technology is readily available and becoming increasingly affordable. In addition to their amazing capabilities today, these devices hold great potential for tomorrow as technology advances, allowing for more capabilities while we continue to study and learn how to use these metrics to improve patient care. This is the new era of medicine, and there is a plethora of untapped information waiting to be studied and applied. Limitations do exist, but they are recognisable and not prohibitive to use.
Perhaps ‘physical examination’ should now include looking for and asking whether patients are wearing a smartwatch and exploring and recording the data reported on these devices. Device interrogation now has a new meaning and is no longer limited to pacemakers, ICDs and loop recorders. This opportunity to pick such low-hanging fruit should not be missed. The information is there; we simply need to know how to review it. It is our responsibility as clinicians to understand the meaningfulness and limitations of smart devices and to be able to counsel our patients and use this information in daily practice. Not doing so leaves a wealth of unused information and potential on the table.
References
- 1.Kramer JN, Kunzler F, Mishra V et al. Investigating intervention components and exploring states of receptivity for a smartphone app to promote physical activity: protocol of a microrandomized trial. JMIR Res Protoc. 2019;8 doi: 10.2196/11540. e11540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coppetti T, Brauchlin A, Muggler S et al. Accuracy of smartphone apps for heart rate measurement. Eur J Prev Cardiol. 2017;24:1287–93. doi: 10.1177/2047487317702044. [DOI] [PubMed] [Google Scholar]
- 3.American Heart Association. Monitoring your blood pressure at home. 2017. www.heart.org/en/health-topics/high-blood-pressure/understanding-blood-pressure-readings/monitoring-your-blood-pressure-at-home Available at. (accessed 6 August 2019)
- 4.Bumgarner JM, Lambert CT, Hussein AA et al. Smartwatch algorithm for automated detection of atrial fibrillation. J Am Coll Cardiol. 2018;71:2381–8. doi: 10.1016/j.jacc.2018.03.003. [DOI] [PubMed] [Google Scholar]
- 5.Canalys. Media Alert: Apple Watch has its best quarter and takes nearly 80% of total smartwatch revenue in Q4; 2017. www.canalys.com/newsroom/media-alert-apple-watch-has-its-best-quarter-and-takes-nearly-80-total-smartwatch-revenue-q Available at. (accessed 30 August 2019) [Google Scholar]
- 6.Do Fitness Trackers Actually Help You Get Fit? What the Science Says. www.mensjournal.com/health-fitness/do-fitness-trackers-actually-help-you-get-fit-what-the-science-says-w445205 (accessed 30 August 2019)
- 7.Koshy AN, Sajeev JK, Nerlekar N et al. Smart watches for heart rate assessment in atrial arrhythmias. Int J Cardiol. 2018;266:124–7. doi: 10.1016/j.ijcard.2018.02.073. [DOI] [PubMed] [Google Scholar]
- 8.Shcherbina A, Mattsson CM, Waggott D et al. Accuracy in wrist-worn, sensor-based measurements of heart rate and energy expenditure in a diverse cohort. J Pers Med. 2017;7 doi: 10.3390/jpm7020003. pii: E3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bai Y, Hibbing P, Mantis C, Welk GJ. Comparative evaluation of heart rate-based monitors: Apple Watch vs Fitbit Charge HR. J Sports Sci. 2018;36:1734–41. doi: 10.1080/02640414.2017.1412235. [DOI] [PubMed] [Google Scholar]
- 10.Gillinov S, Etiwy M, Wang R et al. Variable accuracy of wearable heart rate monitors during aerobic exercise. Med Sci Sports Exerc. 2017;49:1697–703. doi: 10.1249/MSS.0000000000001284. [DOI] [PubMed] [Google Scholar]
- 11.Khushhal A, Nichols S, Evans W et al. Validity and reliability of the Apple Watch for measuring heart rate during exercise. Sports Med Int Open. 2017;1:E206–11. doi: 10.1055/s-0043-120195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dooley EE, Golaszewski NM, Bartholomew JB. Estimating accuracy at exercise intensities: a comparative study of self-monitoring heart rate and physical activity wearable devices. JMIR Mhealth Uhealth. 2017;5:e34. doi: 10.2196/mhealth.7043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Painter SL, Ahmed R, Hill JO et al. What matters in weight loss? An in-depth analysis of self-monitoring. J Med Internet Res. 2017;19:e160. doi: 10.2196/jmir.7457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Birkeland K, Khandwalla RM, Kedan I et al. Daily activity measured with wearable technology as a novel measurement of treatment effect in patients with coronary microvascular dysfunction: substudy of a randomized controlled crossover trial. JMIR Res Protoc. 2017;6:e255. doi: 10.2196/resprot.8057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krivoshei L, Weber S, Burkard T et al. Smart detection of atrial fibrillation. Europace. 2017;19:753–7. doi: 10.1093/europace/euw125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jaakkola J, Mustonen P, Kiviniemi T et al. Stroke as the first manifestation of atrial fibrillation. PLoS One. 2016;11 doi: 10.1371/journal.pone.0168010. e0168010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Apple Heart Study demonstrates ability of wearable technology to detect atrial fibrillation. http://med.stanford.edu/news/all-news/2019/03/apple-heart-study-demonstrates-ability-of-wearable-technology.html (accessed 30 August 2019)
- 18.Apple Heart Study Identifies AFib in Small Group of Apple Watch Wearers. www.acc.org/latest-in-cardiology/articles/2019/03/08/15/32/sat-9am-apple-heart-study-acc-2019 (accessed 30 August 2019)
- 19.Morrissey EC, Casey M, Glynn LG et al. Smartphone apps for improving medication adherence in hypertension: patients’ perspectives. Patient Prefer Adherence. 2018;12:813–22. doi: 10.2147/PPA.S145647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Krebs P, Duncan DT. Health app use among US mobile phone owners: a national survey. JMIR Mhealth Uhealth. 2015;3:e101. doi: 10.2196/mhealth.4924. [DOI] [PMC free article] [PubMed] [Google Scholar]


