Abstract
Introduction
The preferred venous access site for percutaneous management of deep venous thrombosis (DVT) is the popliteal vein, with the patient in the prone position. Owing to the need for additional venous access, including the jugular or femoral veins, popliteal access in the prone position requires supine repositioning of the patient. A technique for puncturing the popliteal vein in the supine position is proposed, which allows for additional venous access in the same position in patients with DVT.
Report
Ultrasound guided popliteal vein access was obtained in the supine position and then pharmacomechanical thrombectomy and iliocaval stent placement was performed for the management of DVT when indicated.
Discussion
Eight patients were included (four men, four women; mean ± standard deviation age of 44.2 ± 14.1 years). Popliteal access was performed successfully in the supine position in all patients. An inferior vena cava filter was inserted in five patients and stents were placed in four. Complete recanalisation of occluded vein segments was obtained successfully with popliteal access in supine position in all patients. None of the patients had early or late complications, including arterial puncture, bleeding, haematoma, or neurological disorder. Veins and stents were patent on duplex ultrasound in all seven patients reaching the six month follow up. One patient with patent veins and stents has not yet reached the six month follow up. The technique of popliteal vein access in the supine position for percutaneous endovenous interventions appears to provide a reliable alternative to access in the prone position.
Keywords: Deep venous thrombosis, Endovascular procedures, Popliteal vein, Supine position
Highlights
-
•
Popliteal access for percutaneous management of deep vein thrombosis may require the patient to be supine.
-
•
A technique of puncturing the popliteal vein in the supine position is proposed.
-
•
Popliteal access was performed successfully in eight patients.
-
•
Complete recanalisation of occluded vein segments was achieved successfully.
-
•
Veins and stents were patent on duplex ultrasound at the six month follow up.
Introduction
Percutaneous endovenous interventions such as catheter directed thrombolysis, pharmacomechanical thrombectomy (PMT), balloon angioplasty, and iliocaval venous stent placement are widely accepted methods in the management of select patients with deep vein thrombosis (DVT). The most commonly used access site for these procedures is the popliteal vein (PV) with the patient in the prone position. However, during the procedure, additional access using the femoral and tibial veins with the patient in the supine position may be needed.1 In a patient with DVT, these access sites may also be needed for the insertion of various devices for thrombus extraction, stent placement, and balloon angioplasty, as well as venography and intravascular ultrasound examination.2 For prevention of pulmonary embolism during the procedure, temporary inferior vena cava (IVC) filter placement via the internal jugular vein in the supine position is used selectively or routinely before thrombus management.3 However, prone positioning for popliteal access prevents additional access to the femoral, tibial, and jugular veins. Therefore, moving the patient to the supine position may be required when anterior access is needed. Thus, the endovenous management of DVT may require two venous access sites in two different positions: supine and prone. This approach increases the potential for haemorrhage and discomfort for the patient. Although the disadvantages of popliteal access in the prone position have not been well documented, it has been reported that some elderly patients and those who had undergone lumbar spine or joint operations found it difficult to change position.4 A new PV access technique in patients with DVT, allowing for multiple accesses in the supine position, is described.
Materials and methods
Consecutive patients treated with PMT using PV access in the supine position for symptomatic acute lower limb DVT were identified from a single institutional database. The records were reviewed retrospectively for demographic and clinical data, venous duplex ultrasound (DUS) examination, and computed tomographic venography, which was used to define the proximal extension of thrombi, as well as underlying lesions. Patients over 18 years of age with acute symptomatic DVT were included. Following assessment for PMT, as well as obtaining consent, patients were transferred to the angiography suite for the procedure. All procedures were performed under local anaesthesia.
Puncture technique
In this new technique, access to the PV is gained with an ultrasound guided vein puncture with the patient in the supine position. Both legs are prepped and draped, and the patient's feet are covered. The knee of the access site is flexed and rotated laterally, and the foot is supported posteriorly with a pad. The ultrasound guided approach is performed with the M-Turbo ultrasound system (SonoSite, Bothell, WA, USA) using a linear array vascular probe with a frequency of 6–13 MHz and width of 6 cm in non-obese patients. A lower frequency, or even an abdominal probe, will facilitate greater tissue penetration in patients with thicker or oedematous subcutaneous tissue. The operator stands on the right hand side of the patient and uses his/her left hand to hold the probe while the right hand is used for intervention, for a right handed operator.
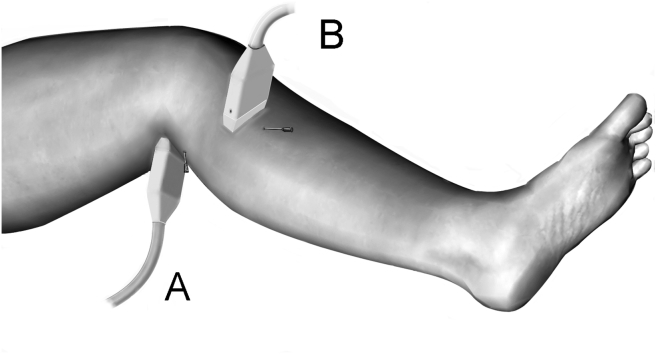
There are two ways to visualise the PV during the pre-operative ultrasound examination in the supine position (Fig. 1). The posterior approach is commonly used by clinicians. This technique is also used during the procedure; the probe is placed just below the popliteal skin crease, where the vein is placed most superficially. When the probe is placed in the popliteal fossa in the supine position, which is behind the leg, the image is upside down on the ultrasound screen. If the image on the screen is changed to be upside down using the controls on the device, the image and procedure become compatible with each other, as in procedures with a direct anterior approach, making manipulations much easier. The insertion point of the needle is approximately a few centimetres distal to the probe. The posterior approach is easier as the PV is superficial in this location and preferred for proximally located thrombi. Equivalent to the arterial terminology, by subdividing the popliteal artery into three segments (P1, P2, and P3) the puncture site of the PV can be defined as PV1, PV2, and PV3, respectively. The posterior approach allows access to the most cranial part of PV2 or caudal part of PV1. However, the anteromedial approach allows access to the more caudal part of the PV (PV3) or to the level of the tibioperoneal trunk, which is below and medial to the head of tibia. In this approach, the vein lies deeper and access may be more difficult than the posterior route. It is favourable in non-oedematous and non-obese patients with thrombi involving the PV distally.
Figure 1.
Location of ultrasound probes and needles for popliteal access. (A) posterior access and (B) medial access.
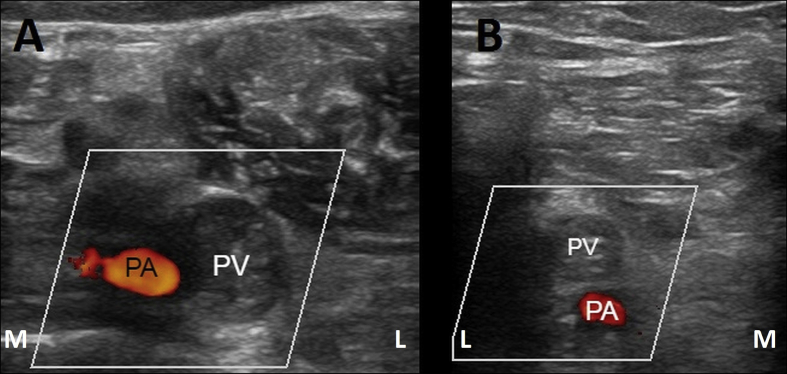
Avoiding arterial puncture is crucial because of the risk of haemorrhage during PMT, which is possible after gaining access. The vein usually lies more superficial than the artery in both types of access (Fig. 2). Both the transverse and longitudinal views are used for targeting the PV. However, vein puncture is performed in the transverse view. Following vein puncture using an 18 gauge needle by the Seldinger technique, a 0.035 wire and then a 7 F sheath is inserted.
Figure 2.
Ultrasound images obtained with different probe positions in a patient with popliteal venous thrombosis. (A) posterior access and (B) medial access. M = medial; L = lateral; PA = popliteal artery; PV = popliteal vein.
Thrombus removal
Following PV access, venography with manual injection was obtained. PMT was performed using a Cleaner thrombectomy device (Argon Medical Devices, Plano, TX, USA) as a single session technique, as described previously elsewhere.1 During the procedure, when balloon angioplasty and stent placement were needed, the popliteal sheath was replaced with 10 or 11 F sheaths. After a completion venogram, all catheters and sheaths were removed, and manual pressure applied to the access sites. Patients were given 5 000 units of unfractionated heparin during the procedure and were therapeutically anticoagulated with low molecular weight heparin (Enoxaparin, Clexane; Sanofi-Aventis, Paris, France [1 mg/kg subcutaneously q12h]) post-procedure.
Post-interventional observation and follow up
All patients were discharged on the second post-interventional day, after clinical and DUS examination for symptom relief, patency, and access site complications. They were discharged on enoxaparin, and warfarin was started at the same day to a target international normalised ratio (INR) of 2.0–3.0. Enoxaparin was discontinued when INR levels were within the therapeutic range. Anticoagulation was continued for a minimum of 12 months. Three follow up examinations, clinical and DUS, were done at the end of one, three, and six months. In the first month's follow up, INR, access site, neurological examination, and vein/stent patency were evaluated. At the second and third follow ups, INR and vein/stent patency were evaluated. However, the six month follow up results were evaluated as the result of the study with the main goal of revealing patency.
Results
Eight patients (four men; mean ± standard deviation age 44.2 ± 14.1 years) were included. Pre-interventional radiological evaluation revealed femoropopliteal vein thrombosis in three and iliofemoropopliteal vein thrombosis in five patients (Table 1). Popliteal access was performed successfully in the supine position in all patients. Contralateral femoral access was obtained in four patients: one for IVC filter insertion and three for better definition of the proximal extension of thrombus at the IVC confluence. An IVC filter was inserted in five patients using the contralateral femoral vein in one patient and the right internal jugular vein in four. Iliocaval venous stents were placed in four patients. Using PMT, complete thrombus resolution was obtained in all patients with popliteal access in the supine position. Additional catheter directed thrombolysis before or after PMT was not used. Follow up at six months was accomplished in seven of eight patients. None of the patients had early or late complications, including arterial puncture, bleeding, haematoma, and neurological disorder. Veins and stents were patent on DUS in all seven patients reaching their six month follow up. One patient with patent stent and treated veins has not yet reached this point.
Table 1.
Patient characteristics and results.
| Patient | Age – y | Sex | Body mass index | Deep vein thrombosis | Inferior vena cava filter | Contralateral femoral access | Stent | Thrombus removal | Patency at six mo |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 51 | Male | 23.9 | Iliofemoropopliteal | Yes | None | Yes | Complete | Patent |
| 2 | 26 | Female | 22.0 | Iliofemoropopliteal | Yes | Venography | Yes | Complete | Patent |
| 3 | 34 | Male | 31.8 | Femoropopliteal | No | None | No | Complete | Patent |
| 4 | 42 | Female | 25.5 | Iliofemoropopliteal | Yes | Venography | Yes | Complete | Patent |
| 5 | 44 | Male | 25.1 | Femoropopliteal | No | None | No | Complete | Patent |
| 6 | 66 | Female | 30.0 | Iliofemoropopliteal | Yes | For inferior vena cava filter | No | Complete | Patent |
| 7 | 51 | Male | 33.4 | Femoropopliteal | No | None | No | Complete | Patent |
| 8 | 24 | Female | 20.0 | Iliofemoropopliteal | Yes | Venography | Yes | Complete | Patenta |
Patient eight has not yet reached the six month follow up.
Discussion
Performing multiple procedures in the same position obviously has an impact on patient comfort, operative time, and cost. During endovascular procedures elimination of repositioning the patient is a common problem and several authors have proposed new access techniques in the supine position for different settings, such as retrograde popliteal arterial puncture in femoropopliteal recanalisation,5 and small saphenous vein ablation for venous insuffiency.6 Here, a technique of puncturing the PV in supine position is proposed, which allows for additional venous access in the same position. Although comparative data are not presented for this procedure, it is evident that a significant amount of time would be added while repositioning the patient.
The incidence of iatrogenic pulmonary embolism (PE) during percutaneous endovenous management of DVT has been reported to be as high as 33%–45%.7, 8 An eightfold increase in iatrogenic symptomatic PE in patients not receiving a filter was noted by Sharifi et al.9 Therefore, IVC filter insertion has been proposed as a strategy to prevent PE during percutaneous endovenous intervention of iliofemoral DVT.3, 10 Placement of an IVC filter is commonly accomplished using the femoral or internal jugular veins with the patient in the supine position. After placement of the IVC filter, patients are repositioned, prepped, and draped for PV access in the prone position. Therefore, IVC filter insertion and endovenous management of DVT may require two separate procedures performed either on different days or in the same session because of the need for venous access in different body positions. To avoid repositioning during the procedure, Kim et al. reported the successful use of popliteal access for both the placement of an IVC filter and percutaneous endovenous intervention for DVT in the prone position.11 However, filter placement through the ipsilateral PV carries the risk of iatrogenic PE because the filter delivery system has to pass through the sites of thrombi. Recently, several peri-interventional IVC filter devices have been introduced to overcome the limitations of conventional temporary filters, such as the inability to retrieve the filter and filter migration. These devices are inserted at the start of PMT and retrieved just after its completion. Although the clinical data are insufficient, one of the possible advantages of this proposed PV access technique is to allow peri-interventional IVC filter placement and retrieval concomitant with PMT in the supine position.
One potential advantage of supine position PV access is anaesthetic management of the patient. Sometimes iliocaval balloon angioplasty and stent placement may be painful and the patient may need additional anaesthetic support, ranging from conscious sedation to general anaesthesia, which is difficult if the procedure is started with the patient in the prone position. Therefore, anaesthetic management of a patient in the supine position is easier than in a patient in the prone position.
In conclusion, the described technique of PV access in the supine position for percutaneous endovenous interventions appears to provide a reliable alternative to access in the prone position, particularly when multiple access sites for IVC filter placement and percutaneous endovenous management of DVT are required.
Conflict of interest
None.
Funding
None.
References
- 1.Köksoy C., Yılmaz M.F., Başbuğ H.S., Calik E.S., Erkut B., Kaygın M.A. Pharmacomechanical thrombolysis of symptomatic acute and subacute deep vein thrombosis with a rotational thrombectomy device. J Vasc Interv Radiol. 2014;25:1895–1900. doi: 10.1016/j.jvir.2014.08.018. [DOI] [PubMed] [Google Scholar]
- 2.Semba C.P., Razavi M.K., Kee S.T., Sze D.Y., Dake M.D. Thrombolysis for lower extremity deep venous thrombosis. Tech Vasc Interv Radiol. 2004;7:68–78. doi: 10.1053/j.tvir.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 3.Yamagami T., Nishimura T. Prophylactic implantation of inferior vena cava filter during endovascular therapies for deep venous thrombosis of the lower extremities. Ann Vasc Dis. 2011;4:19–23. doi: 10.3400/avd.ra.10.01048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Duan P.F., Ni C.F. Randomized study of different approaches for catheter-directed thrombolysis for lower-extremity acute deep venous thrombosis. J Formos Med Assoc. 2016;115:652–657. doi: 10.1016/j.jfma.2015.07.001. [DOI] [PubMed] [Google Scholar]
- 5.Ewedaa A., Shemyb W.E., Sada M., Hamzaa M., Goudac A., Tawfi A. Retrograde transpopliteal access in the supine patient for recanalization of the superfi cial femoral artery after failed antegrade angioplasty. Egypt J Surg. 2015;34:141–145. [Google Scholar]
- 6.Monahan T.S., Belek K., Sarkar R. Results of radiofrequency ablation of the small saphenous vein in the supine position. Vasc Endovas Surg. 2012;46:40–44. doi: 10.1177/1538574411425108. [DOI] [PubMed] [Google Scholar]
- 7.Kolbel T., Alhadad A., Acosta S., Lindh M., Ivancev K., Gottsater A. Thrombus embolization into IVC filters during catheter-directed thrombolysis for proximal deep venous thrombosis. J Endovasc Ther. 2008;15:605–613. doi: 10.1583/08-2462.1. [DOI] [PubMed] [Google Scholar]
- 8.Théry C., Bauchart J.J., Lesenne M., Asseman P., Flajollet J.G., Legghe R. Predictive factors of effectiveness of streptokinase in deep venous thrombosis. Am J Cardiol. 1992;69:117–122. doi: 10.1016/0002-9149(92)90686-s. [DOI] [PubMed] [Google Scholar]
- 9.Sharifi M., Bay C., Skrocki L., Lawson D., Mazdeh S. Role of IVC filters in endovenous therapy for deep venous thrombosis: the FILTER-PEVI (filter implantation to lower thromboembolic risk in percutaneous endovenous intervention) trial. Cardiovasc Interv Radiol. 2012;35:1408–1413. doi: 10.1007/s00270-012-0342-z. [DOI] [PubMed] [Google Scholar]
- 10.Lee S.H., Kim H.K., Hwang J.K., Kim S.D., Park S.C., Kim J.I. Efficacy of retrievable inferior vena cava filter placement in the prevention of pulmonary embolism during catheter-directed thrombectomy for proximal lower-extremity deep vein thrombosis. Ann Vasc Surg. 2016;33:181–186. doi: 10.1016/j.avsg.2015.10.034. [DOI] [PubMed] [Google Scholar]
- 11.Kim H.O., Kim J.K., Park J.G., Yim N.Y., Kang Y.J., Jung H.D. Inferior vena cava filter insertion through the popliteal vein: enabling the percutaneous endovenous intervention of deep vein thrombosis with a single venous access approach in a single session. Diagn Interv Radiol. 2016;22:455–459. doi: 10.5152/dir.2016.15347. [DOI] [PMC free article] [PubMed] [Google Scholar]