Abstract
A 38-year-old female underwent bilateral implantable collamer lens (ICL) implantation for hyperopic astigmatism. While performing intraoperative peripheral iridectomy (PI), iris and anterior lens capsule was drawn to anterior vitrectomy cutter which result in large PI and injury to anterior lens capsule. Anterior lens capsule injury closed by fibrosis and the patient has 20/20 vision and static traumatic lens changes without any undesirable sequelae at the last follow up. Performing PI preoperatively by laser or alternatively by scissor intraoperatively is advisable to avoid above mentioned complication and a close observation is recommended when lens injury encountered.
Keywords: Implantable collamer lens, Cataract, Peripheral iridectomy
Introduction
The Visian implantable collamer lens (ICL) (STAAR Surgical, monrovia, California) is a posterior chamber phakic intraocular lens which is accepted as an alternative treatment for ametropia correction among various refractive ranges1 with clinical and visual outcomes coparable to laser procedure.2 Trauma to crystalline lens has been described in literature.3 We present, to our knowledge the first case of anterior lens capsule injury by anterior vitrectomy cutter while creating surgical peripheral iridectomy (PI) with no significant impact on vision.
Case report
A 38-year-old female underwent bilateral ICL implantation for hyperopic astigmatism. Preoperatively, the corrected visual acuity was 20/20 for the right eye and 20/30 to the left eye. The intraocular pressure was 19 bilaterally. Slit lamp examination was unremarkable for both eyes. The preoperative Refraction was +4.25 −1.00 ×175° for the right eye and +6.00 −1.75 ×170° for the left eye. White-to-white measurement was 12 mm for both eyes. Anterior chamber depth from the endothelium was 3.3 mm in the right eye and 3.16 mm the left eye. The patient scheduled an appointment for laser neodymium-doped yttrium aluminum garnet (Nd:YAG) PI before surgery but failed to present. Hence, during ICL implantation, the surgeon elected to perform a surgical PI with anterior vitrectomy cutter (Inc., Fort Worth, TX, USA). The vitrectomy sitting was: vacuum 250 mmHg and cutting rate1. The anterior lens capsule was inadvertently cut by the anterior vitrectomy cutter together with iris tissue. Examination of the patient 2 hours post operatively indicated almost no distance between ICL and crystalline lens (zero vault). The intraocular pressure was 18 mmHg. Trauma to anterior lens capsule was visible through the large superior PI. Two weeks later, uncorrected distance visual acuity was 20/20 for the right eye. Slit lamp examination showed large superior PI with limited traumatic lens changes and a low ICL vault (Fig. 1). We elected to observe the patient and the probability of lens extraction and multifocal IOL implantation was discussed with the patient if the lens opacity progressed in the future. Two weeks later, uncorrected distance visual acuity of the right eye was 20/20 which was stable over two years and the traumatic lens changes was stable with closed anterior lens capsule opening by fibrosis. The vault was 348 micrometers as measured by anterior segment optical coherence tomography (OCT) (Fig. 2). Two months after right eye surgery, uneventful ICL implantation was done for the left eye after two YAG PI was performed preoperatively which result in 20/20 uncorrected visual acuity with 420 micrometer vaults by OCT.
Fig. 1.
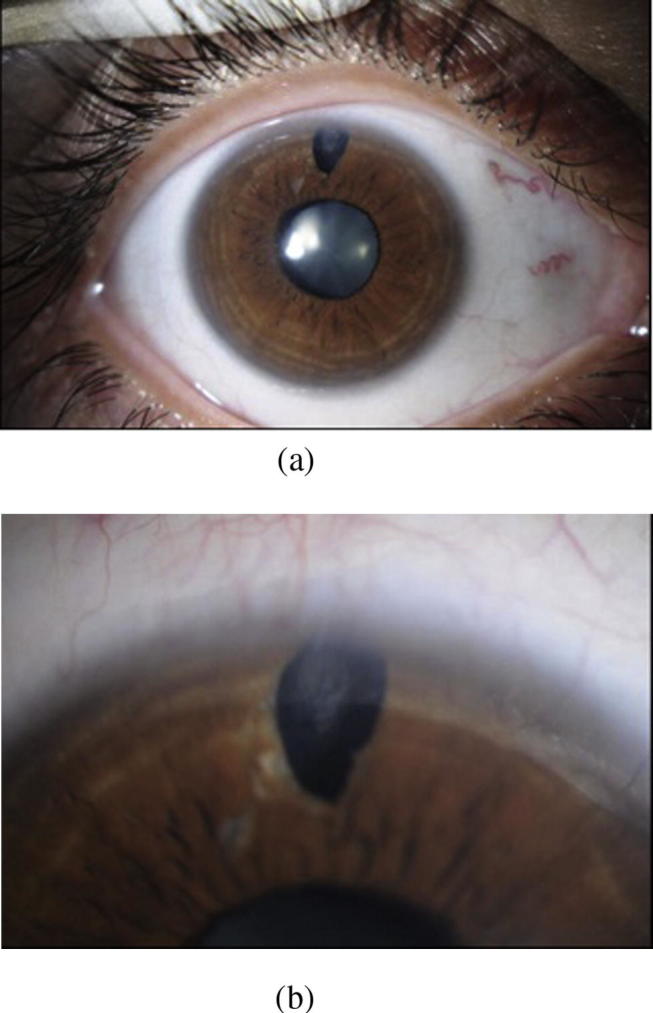
(A) Large superior PI with limited traumatic lens changes. (B) close-up view.
Fig. 2.
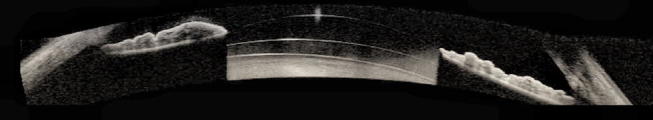
Ocular coherence tomography demonstrate good vault.
Discussion
ICL implantation is an emerging procedure in refractive surgery. The advantages of ICL implantation include. Faster visual recovery, stability of visual quality, preservation of accommodation, and reversibility.4 However, the safety of ICL implantation has been questioned due to potential complications, such as cataract formation5, trauma to the crystalline lens3 glaucoma, corneal endothelial decompensation6 and retinal detachment.7
Although the surgical technique for ICL implantation is identical in myopic eyes and hyperopic eyes, the shallower anterior chambers in hyperopic eyes makes the insertion of the ICL more technically challenging in order to minimize contact with the corneal endothelium.8 The myopic ICL (model V4c) has central hole which eliminates the need for PI. However, there is no corresponding hole in hyperopic ICL (model V3, VTICH) necessitating preoperative or intra-operative iridectomy to prevent pupillary block and high intraocular pressure and possible endothelial cell loss.
Pesando et al.6 found that endothelial cell loss was higher in eyes with a history of pupillary block than in the other hyperopic eyes over a 10-year follow-up. There are several techniques for performing PI. Although preoperative laser peripheral iridectomy (PI) is recommended by the manufacturers of ICL9 and preferred by most of surgeons, intraoperative PI has been used with good results.6 Intraoperative PI can be performed manually with scissors or with an anterior vitrectomy cutter. Selection of the PI technique depends on patient characteristics, available equipments, and surgeon’s preference in minimizing complications and achieving good level of patient satisfaction.9 In current case, surgery was performed under topical anesthesia with intracameral lidocaine which was insufficient to control the pain when the vacuum was activated for the anterior vitrectomy cutter to pull the iris. Intraoperatively while we were trying to reassure the patient, excess iris tissue and anterior lens capsule was drawn into the cutter which causing a large PI and loss of a segment of anterior lens capsule when cutting was initiated. Although PI was large but it was totally covered with upper eyelid and the patient was asymptomatic with 20/20 vision and no complain which necessitate PI suturing. To our knowledge, this is the first case that describes lens injury due to an anterior vitrectomy cutter while creating PI with no significant impact on the patient. To avoid this complication, we advise a preoperative YAG PI. If intraoperative PI is warranted, we advise adequate anesthesia, a short vacuum time if anterior vitrectomy cutter is to be used and to use a smaller gauge cutter which has smaller port that will minimize the amount of tissue drawn inside the smaller inner diameter cannula. Alternatively, surgical PI can be done by scissor. This report highlights the importance of observation of small peripheral lens injury which can close by fibrosis and save the patient from undergoing unnecessary lens aspiration with accommodation loss in such young group of patients.
Conflicting interest
The authors declared that there is no conflict of interest.
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
References
- 1.Maeng H., Chung T., Lee D., Chung E. Risk factor evaluation for cataract development in patients with low vaulting after phakic intraocular lens implantation. J Cataract Refract Surg. 2011;37(5):881–885. doi: 10.1016/j.jcrs.2010.11.037. [DOI] [PubMed] [Google Scholar]
- 2.Sanders D., Vukich J.A. Comparison of implantable collamer lens (ICL) and laser-assisted in situ keratomileusis (LASIK) for low myopia. Cornea. 2006;25(10):1139–1146. doi: 10.1097/ICO.0b013e31802cbf3c. [DOI] [PubMed] [Google Scholar]
- 3.Sanchez-Galeana C.A., Smith R.J., Sanders D.R. Lens opacities after posterior chamber phakic intraocular lens implantation. Ophthalmology. 2003;110(4):781–785. doi: 10.1016/s0161-6420(02)01973-5. [DOI] [PubMed] [Google Scholar]
- 4.Fernandes P.R., González-Méijome J.M., Madrid-Costa D., Ferrer-Blasco T., Jorge J., Montés-Micó R. Implantable collamer posterior chamber intraocular lenses: a review of potential complications. J Refract Surg. 2011;27(10):765–776. doi: 10.3928/1081597X-20110617-01. [DOI] [PubMed] [Google Scholar]
- 5.Menezo J.L., Peris-Martınez C., Cisneros-Lanuza A.L., Martínez-Costa R. Rate of cataract formation in 343 highly myopic eyes after implantation of three types of phakic intraocular lenses. J Refract Surg. 2004;20:317–324. doi: 10.3928/1081-597X-20040701-03. [DOI] [PubMed] [Google Scholar]
- 6.Pesando P.M., Ghiringhello M.P., Tagliavacche P. Posterior chamber collamer phakic intraocular lens for myopia and hyperopia. J Refract Surg. 1999;15:415423. doi: 10.3928/1081-597X-19990701-05. [DOI] [PubMed] [Google Scholar]
- 7.Bamashmus M.A., Al-Salahim S.A., Tarish N.A. Posterior vitreous detachment and retinal detachment after implantation of the visian phakic implantable collamer lens. Middle East Afr J Ophthalmol. 2013;20(4):327. doi: 10.4103/0974-9233.120019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alfonso J.F., Baamonde B., Belda-Salmerón L., Montés-Micó R., Fernández-Vega L. Collagen copolymer posterior chamber phakic intraocular lens for hyperopia correction: three-year follow-up. J Cataract Refract Surg. 2013;39(10):1519–1527. doi: 10.1016/j.jcrs.2013.04.035. [DOI] [PubMed] [Google Scholar]
- 9.Wu Y., Han F., Quan Y., Jiang W., Zhang H., Luo T. Comparison of peripheral iridectomy methods for posterior chamber phakic intraocular lens implantation in patients with brown irides. BMC Ophthalmol. 2016;16 doi: 10.1186/s12886-016-0229-x. [DOI] [PMC free article] [PubMed] [Google Scholar]


