Abstract
Objectives:
To assess factors influencing treatment decision for maxillary third molars referred for cone beam CT (CBCT). Parameters influencing the decision to treat and to remove either the maxillary second molar or third molar were pursued.
Methods:
111 impacted maxillary third molars, clinically examined including a panoramic image, in 86 patients (mean age 26 years, range 15–55) were referred for CBCT on suspicion of pathology/root resorption in the second molar, based on information in the panoramic image. The following parameters were assessed from the patient’s file, including the radiographic images: (1) third molar angulation; (2) initial treatment plan based on clinical examination and the panoramic image; (3) diagnoses based on information from CBCT; (4) treatment decision after additional CBCT information was available; (5) pre-/post-operative complications; (6) treatment of the maxillary second molar.
Results:
70 cases (63.1%) underwent treatment, while 41 (36.9%) received no treatment. Change in treatment plan was registered in 65 cases (58.6%) after CBCT. In 12 cases (10.8%), treatment changed from removal of the third to removal of the second molar, while 25 (22.5%) were scheduled for removal in the initial treatment plan; but after CBCT, the decision was not to treat. If external root resorption involved the pulp of the second molar, there was an almost 17 times higher risk that this tooth was removed instead of the third molar (logistic regression analysis: odds ratio 16.8; p < 0.001).
Conclusions:
Findings in CBCT often changed the treatment plan. Severe external root resorption observed in CBCT was the main decisive factor for removing the second instead of the third molar.
Keywords: Radiography, CBCT, Panoramic imaging, Third molar, Maxilla
Introduction
Impaction of a maxillary third molar can be associated with disease, such as external root resorption (ERR) of the second molar, marginal bone loss on the distal surface of the second molar, and a cyst related to the third molar. Both ERR, marginal bone loss, and presence of a cyst may be treated by removal of the maxillary third molar since after removal, ERR in the second molar and marginal bone loss is expected to cease. ERR of the second molar may however be so severe that removal of the second molar may be considered instead of the third molar. No protocol guiding the clinician on when to remove the second instead of the third molar seems to exist though.
Panoramic imaging has been the first choice radiographic method when assessing impacted third molars and associated disease.1 Pathology such as ERR and marginal bone loss may, however, be difficult to observe due to overprojection of anatomical structures and neighbouring teeth, particularly in the maxillary third molar region. A previous study has shown that panoramic imaging was not able to predict ERR when compared to a three-dimensional radiographic method, cone beam CT (CBCT), while panoramic imaging was to some extent able to predict marginal bone loss.2 Nonetheless, CBCT exposes the patient to a higher radiation dose and involves higher costs for the patient and society than panoramic imaging,3,4 and for that reason it is important only to perform a CBCT examination on evidence-based indications. While many studies are available on the impact of CBCT in assessing mandibular third molars prior to removal,5–8 very few studies exist in the literature on maxillary third molars. One study investigated the occurrence of pathology in the area of the maxillary third molar as observed in panoramic images. The study included 5665 third molars (both maxillary and mandibular) in the adult Finish population. Based on their observations, resorption in the crown of the third molar was reported in 2% of cases (both maxillary and mandibular), but the paper did not include the percentage of ERR caused by the third molar.9 In a recent study of randomly selected CBCT examinations with large FOVs for different diagnostic purposes, 184 maxillary third molars were assessed. A frequency of 32.6% of maxillary second molars with ERR caused by the third molar was found.10 Mesioangulated and deeply impacted maxillary third molars in addition to age >25 years had an increased risk of causing resorption in the second molar.10 A previous study compared CBCT and panoramic imaging in the assessment of ERR including 91 maxillary third molars, and ERR in the maxillary second molar was seen in 14.3% using CBCT.11 A very recent study found an almost similar frequency of ERR in the second molar observed both in CBCT and in panoramic image of the same patients,2 but the cases scored with ERR with the two imaging methods were not congruent. Moreover, much more severe ERR in the second molar was detected with CBCT than in the panoramic image.2
No study has examined whether the additional use of CBCT changes the treatment plan based on the clinical examination and a panoramic image. Moreover, how often a maxillary second molar is removed instead of a third molar, when ERR is present in the distal surface of the second molar has not been established.
The aim of this study was to assess the treatment decision for maxillary third molars referred for CBCT on suspicion of pathology related to the third molar and/or ERR in the second molar. The treatment plan established on basis of the clinical examination and an initial panoramic image was compared to the treatment decision after additional CBCT examination was available, and changes were evaluated. Moreover, parameters influencing the decision to treat and the decision to remove either the maxillary second molar or third molar were assessed. Finally, occurrence of treatment complications was also estimated.
Methods and material
This retrospective study was based on 111 cases of impacted maxillary third molars in 86 patients (26 males and 60 females), thereby 25 patients with two third molars were included. Mean age was 26 years (ranging from 15 to 55 years). Patients were referred for assessment of the third molar—and optionally treatment—from either private practice, community dental healthcare clinics, or internally at the Department of Dentistry and Oral Health, Aarhus University, Denmark from the Section of Oral Surgery and Oral Pathology to the Section of Oral Radiology, between 2010 and 2017.
The patients were clinically examined, including a panoramic image for assessment of the third and second molar in question. The panoramic image was obtained either from the referring practice or recorded at the Section of Oral Radiology using a ProMax unit (Planmeca, Helsinki, Finland) with a CCD-based image receptor (66 kV, 8 mA, 16 s exposure time). To reduce radiation dose, the recording was sectioned to expose only the area of the third and second molar in question.
Based on the findings from clinical examination and the panoramic image, the patients had been referred for CBCT on suspicion of pathology in relation to the maxillary third molar and/or root resorption in the second molar as observed in the initial panoramic image. CBCT examination was performed with a Scanora 3D unit (Soredex, Helsinki, Finland) with a 6 × 6 cm field of view (FOV) and 0.13 mm voxel resolution (90 kV, 10 mA, 23 s exposure time, 451 base projections). The FOV was centered at the maxillary third molar region. Only patients, where CBCT was performed no more than 3 months after the panoramic image, were included in the study.
Patient records
All data from the clinical examination, the panoramic findings, the findings from the CBCT examination, the treatment, and complications after the treatment were described in a systematic manner in the surgical clinic and entered into the patient’s file. The radiographic reports in the patient’s file were made by one of two radiologists, who had worked together for several years and are well calibrated, as part of their daily clinical practice. The treatment plan, treatment, and assessment of complications were performed by the oral surgeons, who were present that day. The oral surgeons were almost equally experienced, each had more than 10 years of experience, and the eventual decision to remove a second molar was always performed in a consensus among at least two oral surgeons. For the final treatment decision, the surgeons had access to all data in the patients’ records, including the information from the CBCT examination.
Pre-operative complications—perforation of the maxillary sinus and fracture of the maxillary tuberosity—were reported during removal of the tooth and listed in the patient’s file. Post-operative complications—bleeding, ecchymosis, swelling, and infection—were reported in the patient’s file, when the patient returned to the clinic for removal of sutures, usually 1 or 2 weeks after tooth removal.
The data from the patients’ records including CBCT reports were then extracted by one observer. Prior to the evaluation of the records, the observer went through a training session on how to extract data from the records with an experienced oral radiologist. Parameters extracted from the patient’s clinical record and radiographic reports were: (1) tooth angulation of the maxillary third molar observed in CBCT (vertical/mesioangulated/distoangulated/horizontal/inverted/transversal); (2) initial treatment plan based on the clinical examination and the findings in the panoramic image (no decision made/removal of the maxillary third molar/removal of the maxillary second molar/removal of both teeth); (3) diagnoses based on findings in CBCT (no pathological findings/superficial ERR/ERR involving the dentin/ERR involving the pulp/cyst in relation to the third molar/marginal bone loss at the distal surface of the second molar); (4) treatment decision performed after additional CBCT findings (no treatment/removal of maxillary third molar/removal of maxillary second molar/removal of both teeth); (5) pre-/post-operative complications (no complications/perforation to the maxillary sinus/fracture of maxillary tuberosity/bleeding/ecchymosis/swelling/infection); and (6) treatment of the maxillary second molar, when not removed (no further treatment/endodontic and restorative treatment). The assessment of ERR was inspired by a previous grading of ERR in ectopic canines12 and has also been used in a previous report.2 Herein, this was modified according to the clinical relevance, since it is believed that a superficial ERR only involving the outer surface of the root may not be as severe as ERR into the dentin or involving the pulp and thereby not cause any treatment of the second molar. Furthermore, since guidelines on when to remove a second molar with ERR are non-existing, the assessment distinguished between ERR in dentin and involving the pulp.
Data treatment
Data from every patient record was entered in Microsoft Office Excel® 2010 (Microsoft Corp., Redmond, WA). Subsequently, data were imported into SPSS® (IBM Corp., New York, NY) for statistical analyses. A change in treatment was registered if the treatment plan, based on the initial clinical examination and the panoramic image and the treatment performed after CBCT was additionally available, was not the same. Number of removed teeth was recorded, either a maxillary third molar, second molar, or both teeth. Initial logistic regression analyses were performed for each parameter observed in CBCT as independent variable (angulation of the third molar/degree of ERR of the second molar/marginal bone loss at the distal surface of the second molar/other pathology) with treatment/no treatment as the dependent variable (treatment: removal of the maxillary second, third molar, or both). Only parameters with a significant impact in the initial logistic analyses (p < 0.05) were entered into a multivariate logistic regression analysis with treatment (yes/no) as the dependent (outcome) variable.
Initial logistic regression analyses were also performed for each parameter observed in CBCT as the independent variable in the group of patients, who eventually were treated removal of the maxillary second/third molar as dependent variable. Finally, parameters with a significant impact in the initial logistic analyses (p < 0.05) were entered into a multivariate logistic regression analysis with removal of the second/third molar as the dependent (outcome) variable.
Complications were counted for patients, who had the second molar extracted and those, who had the third molar removed, separately.
Results
Change in treatment (n=111)
70 cases (63.1%) in 60 patients underwent a surgical intervention comprising removal of either the second maxillary molar, the third molar, or both teeth. 41 cases (36.9%) received no treatment (Table 1). In total, 52 third molars and 21 second molars were eventually removed. Thus, in three cases, both the second and the third maxillary molar in the same side-were removed (Table 1).
Table 1. .
Change in treatment plan after CBCT examination was additionally available
| N (111) | CBCT examination additionally available | |||
|---|---|---|---|---|
| Clinical examination and panoramic image | No treatment | Removal of third molar | Removal of second molar | |
| No decision made | 16 | 18 | 7 | |
| Removal of third molar | 25 | 31 | 12 | |
| Removal of second molar | 0 | 3 | 2 | |
CBCT, cone beam CT.
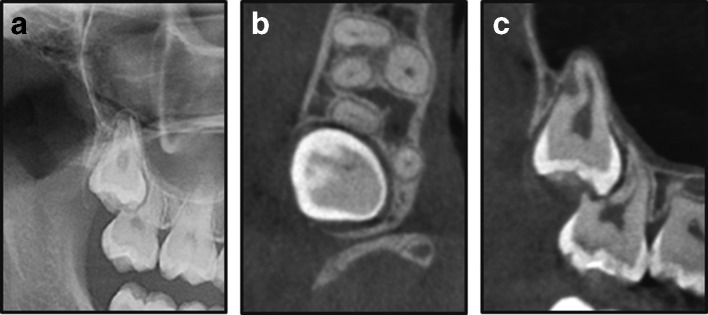
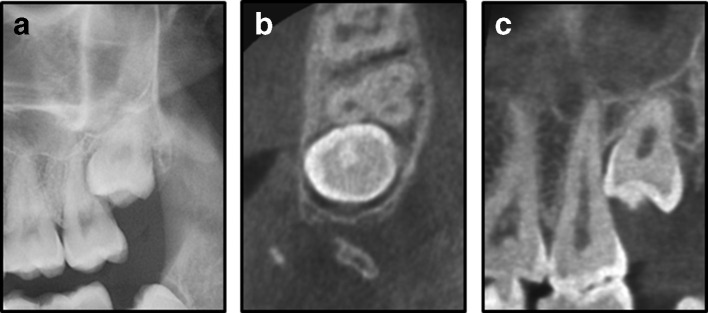
After additional information from CBCT was available, a change in treatment plan was registered in 65 cases (58.6%). Among these, 25 cases had not received any initial treatment plan; however, after CBCT, either a second (7 cases) or a third (18 cases) molar was removed (Table 1). Furthermore, for 12 cases treatment was changed from removal of a third molar in the initial plan to removal of a second molar. Inversely, 25 cases were scheduled to have a third molar removed in the initial plan; however, after CBCT was available, it was decided not to treat (Table 1). Figure 1 shows an example where removal was planned for the right maxillary third molar based on the initial clinical examination and the panoramic image, but in the CBCT severe ERR was observed, and the second molar was removed instead. Figure 2 shows an example of the opposite treatment decision, in which there was suspicion of severe ERR in the second molar in the initial panoramic image, but the CBCT showed no signs of ERR, and the third molar was removed.
Figure 1. .
An impacted right maxillary third molar shown in the panoramic image (a); CBCT image in the axial plane (b); and CBCT image in the sagittal plane (c). The CBCT shows severe ERR with ERR of the entire distobuccal root of the second molar. CBCT, cone beam CT; ERR, external root resorption.
Figure 2. .
An impacted left maxillary third molar shown in the panoramic image (a); CBCT image in the axial plane (b); and CBCT image in the sagittal plane (c). The CBCT shows close relation between the crown of the third molar and the root of the second molar, but no ERR. CBCT, cone beam CT; ERR, external root resorption.
Parameters influencing decision on removal vs no removal (n=111)
Based on the initial logistic regression analyses, angulation of the maxillary third molar and ERR in the second molar were the only two radiographic parameters with a statistically significant impact on the decision to intervene (Table 2). Mesioangulated third molars were removed nearly four times more often than vertically positioned molars, while no other angulation had significant impact on treatment decision compared with molars in the vertical position (odds ratio, OR 3.6; p < 0.027). Additionally, presence of ERR (no matter the severity) in the distal surface of the second molar was associated with nearly six times higher risk that removal of a tooth was decided (OR 5.6; p < 0.001), than if there was no ERR in the tooth.
Table 2. .
Multivariate logistic regression analysis for tooth-related parameters and gender and age which could influence decision to treat
| Parameter | Odds ratio | Receiving treatment vs no treatment (n = 111) p-value |
95% CI |
|---|---|---|---|
| ERR [no] | |||
| Yes | 5.6 | 0.001 | 2.012–15.720 |
| Angulation [vertical] | |||
| Mesioangulated | 3.7 | 0.027 | 1.158–11.613 |
| Horisontal | 2.4 | 0.559 | 0.123–48.458 |
| Distoangulated | 2.4 | 0.247 | 0.545–10.602 |
| Transverse/inverted | 0.999 | – | |
| Gender [male] | |||
| Female | 1.3 | 0.590 | 0.454–4.006 |
| Age [ascending] | 1.0 | 0.240 | 0.912–1.023 |
CI, confidence interval; ERR, external root resorptions.
Groupin [brackets] was the reference group.
Parameters influencing decision on removal of the second vs the third maxillary molar (n=67)
In 67 cases, either a third or a second molar was removed. ERR was the only statistically significant parameter in the initial logistic regression analyses (p < 0.001) that had a significant impact on removal of the second in stead of the third molar. Therefore, ERR was entered into the multivariate analysis together with gender and age (Table 3). The final analysis showed an almost 17 times (OR 16.8; p < 0.001) higher risk that the second maxillary molar was removed, if ERR involved the pulp of a root of that molar. Moreover, females had nearly nine times higher risk than males of having the maxillary second molar removed instead of the third molar (OR 8.7; p = 0.005). Age had no significant impact on which tooth was removed.
Table 3. .
Multivariate logistic regression analysis for ERR in the second molar and gender and age as independent variables with removal of the maxillary second vs third molar as dependent variable
| Parameter | Odds ratio | Removal of second molar vs third molar (n = 67) p-value |
95% CI |
|---|---|---|---|
| ERR [no] | |||
| Superficial ERR | 0.999 | - | |
| ERR involving the dentin | 4.5 | 0.118 | 0.682–30.205 |
| ERR involving the pulp | 16.8 | 0.001 | 2.976–95.302 |
| Gender [male] | |||
| Female | 8.7 | 0.005 | 1.941–38.670 |
| Age [ascending] | 1.0 | 0.583 | 0.937–1.122 |
CI, confidence interval; ERR, external root resorptions.
Group in square brackets was the reference group.
ERR of the second molar was present in 42 cases. 8 cases had superficial resorption, and ERR into the dentin of the second molar occurred in 12 cases, while 22 cases showed involvement of the pulp. Overall, 24 third molars (7 cases causing superficial ERR, 8 cases causing ERR into dentin, and 9 cases involving the pulp of the second molar) and 19 second molars were removed (5 cases with ERR into dentin and 14 cases involving the pulp) including 1 case in which both teeth were removed. In three cases, where the third molar was removed, endodontic and restorative treatment was performed of the second molar that had ERR involving the pulp.
Pre- and post-operative complications (n=67)
Pain followed by swelling were the most commonly reported complications after surgical intervention. There were no complaints about pain after removal of a second molar, whereas pain was recorded in nine cases after third molar removal, and only one patient reported that analgesics was unable to alleviate the pain. This patient also had a perforation to the maxillary sinus. Overall, five patients (7.1%; four after removal of a third molar and one after removal of a second molar) had a perforation to the maxillary sinus during the surgical intervention. Rehrmann-plastic was only needed in one case, which was performed by an oral surgeon on the same day that the perforation occurred. After 1–2 weeks, all perforations were closed, and none of the patients experienced further post-operative complications in relation to the perforations. Ecchymosis was reported in two patients at the 1-week control. One of the patients had a fracture of a small part of the maxillary tuberosity during the removal of a third molar, but no further surgical procedure was needed. No fracture of the entire maxillary tuberosity occurred. Likewise, neither excessive bleeding nor infection after removal was seen in any case.
Discussion
This study was retrospective in nature, a socalled “trohoc” study, which is the retrospective version of a cohort study. Though retrospective in nature, the data in our clinic were collected in a highly systematic manner, and the patients’ records were easily accessible. Many surgeons participated in the study, which we see as a strength compared with studies where only one person has taken the decision on treatment choice. Two calibrated radiologists made the radiographic reports, who have previously been shown to have a strong observer agreement.13
The study included a selected patient population, namely those referred for a CBCT examination on the suspicion of pathology related to the third molar/ERR in the second molar, and also selected based on the inclusion criterion that the patient had both a panoramic image and a CBCT examination of the third molar region within a short period of time. Therefore, the frequency of ERR in the second molar caused by the impacted third molar as well as frequency of tooth removal cannot be interpreted as prevalences that reflect a general population with impacted maxillary third molars. We believe, the study adds valuable information in the field of treatment of impacted third molars and may form a basis for establishing guidelines for the use of CBCT, where the literature currently is very sparse.
ERR in the distal surface of the maxillary second molar caused by an impacted third molar is considered irreversible pathology and according to The National Institute for Health and Care excellence, this indicates intervention.14 When ERR of the maxillary second molar is observed, intervention may traditionally be surgical removal of the impacted third molar causing the ERR. An alternative approach could be removal of the maxillary second molar, particularly when severe root destruction involving the pulp is observed. No studies so far have investigated when a maxillary second molar is removed instead of a third molar due to ERR, thus no guidelines exist on this topic. Furthermore, our study compared the treatment plan established on the basis of a panoramic image and subsequently with CBCT, to assess whether CBCT changed the final treatment decision. Therefore, the study can be seen as a Level 4 study in the Fryback and Thornbury hierarchical model for evidence-based guidelines regarding the use of a new radiographic method.15 No studies currently exist on level four or higher evidence levels.
Change in treatment
Based on the patient’s record and the CBCT report, 12 cases changed from removal of the third molar to removal of the second molar after CBCT was available. Furthermore, for 41 cases it was unclear after the initial panoramic image whether the patient should be offered any treatment. 25 of these cases received a treatment after CBCT was available, and 16 had no treatment. Another 25 cases changed from expected removal of a third molar based on the panoramic image to no removal after the CBCT. No previous studies have investigated the impact of CBCT for treatment decision regarding maxillary third molars. For mandibular third molars, however, similar studies have been conducted. A previous study investigated the influence of CBCT on the treatment plan before surgical intervention of mandibular third molars, the surgical intervention being either surgical removal or coronectomy of the mandibular third molar.5 A change in treatment was registered in 12% of the cases. In this study, all cases received an intervention. In comparison, if only cases where an intervention is considered in our study, overall 21% changed treatment either from removal of a third to removal of a second molar or vice versa. Deep ERR in a second molar due to an impacted third molar is also a finding for mandibular teeth,16 however, the panoramic image may be able to display this situation more validly than for maxillary second molars. There is more overlap of anatomic structures in the maxillary third molar region, and maxillary molars often have more roots, why it may be logical that CBCT when compared with panoramic imaging, may result in a diagnosis of more severe ERR of the second molar in the maxillary than in the mandibular regions.2
No guidelines exist on when a CBCT examination of maxillary third molars is indicated, nor when removal of the maxillary second molar should be considered, and therefore the decision to refer the patient for a CBCT and to remove the maxillary second molar instead of the third molar is based solely on “good clinical practice.” Removal of the second molar was not always the treatment choice, when ERR involving the pulp was seen in CBCT, since some surgeons (or patients) preferred to have root canal and restorative treatment performed of a second molar with deep ERR after removal of the third molar. The decision to remove a second molar was always performed in consensus among several surgeons in the department. All surgeons involved had many years of experience and had been working together also for many years. Treatment strategies in the clinic are thus calibrated among the surgeons. Nevertheless, when no international guidelines exist for when to perform a specific treatment, it may surely depend on the knowledge and the experience of the oral surgeons, which treatment they recommend. It cannot be guaranteed that the evaluation of the initial panoramic images, treatment planning, and final treatment decisions would be the same in another clinical environment. This will, however, always be a limitation in clinical studies. From our data, it was not possible to separate treatment choice as offered by the surgeons and the influence of the patient’s decision. Moreover, in the present study, we chose one way to classify ERR inspired by a classifaction system used in a previous study with CT scanning12 modified according to our clinical experience. One could speculate that “superficial resorption” may not be easily differentiated from ERR into dentin in radiographs especially small dentinal lesions or no resorption, and that this would influence our results. Other studies have suggested other classification systems based on periapical images, where minimal or slight resorption was defined as loss of tooth substance up to 2 mm.17,18 When comparing results from different studies, the classification of ERR as well as the imaging methods, on which the classification system is based, has to be considered since this could influence the decision-making.
Parameters influencing removal of a maxillary second instead of the third molar
Presence of a mesioangulated third molar seen in CBCT was a factor per se, associated with a significantly higher risk that the patient received an intervention. One study has suggested an association between mesioangulated third molars and presence of ERR in the distal surface of the maxillary third molar,10 whereas a recent study has shown no association between angulation and presence of ERR of the second molar.2 Presence of ERR was related to a very high risk of receiving an intervention in our study. This may not be surprising since it is in accordance with NICE guidelines on when to intervene on impacted third molars,14 but these guidelines do not state or differentiate between intervention options.
In case of severe ERR involving the pulp, our study showed an extremely high risk of having the second molar removed instead of the third molar. It may seem logical that in cases with severe ERR of the second molar, the prognosis of the tooth is poor, and particularly when the prognosis for eruption of the third molar is favourable, this would be a sensible treatment offer. Therefore, one could also speculate that younger age would have an impact when deciding on removal of a second molar, but this was not the case in the present study. Previous studies have concluded that older age is related to increased risk of ERR in the second molar caused by the third molar.10,19 This confirms our speculation that treatment decision should be performed at young age. Compared to other studies, the present study included patients with a relatively low mean age and small range in age. This may explain, why there was no significant relation between age and ERR/tooth removal in our study. On the other hand, the female gender was associated with higher risk of having a maxillary second molar removed. There seems to be no obvious explanation for this finding, other than more females than males were included in the study. Others did not find this association.10 Our study is the first to show a significant relationship between severe ERR and removal of the second molar. No studies seem to have performed follow ups on second molars with severely resorbed root(s) after removal of the third molar, and additionally, no follow-up study exists on the faith of the third molar in case of removal of the second molar. On one hand, the idea is that the third molar will erupt and to some extent establish function; on the other hand, there is also the risk that the third molar will stay impacted and eventually develop pathology. In this case, it would possibly be relevant to remove both teeth at the same time. Therefore at current, an evidence-based information on prognosis for the second or third molar, in cases of severe resorption in the second molar, cannot be given to the patient.
Pre- and post-operative complications
Pain and swelling were the postoperative complications that occurred most often, whereas perforation to the maxillary sinus, which is a more severe complication, occurred only in few cases. Several studies have investigated the occurrence of perforation to the maxillary sinus during removal of maxillary third molars.20,21 One study found a frequency of 24% for completely bony-impacted third molars and 10% for partially impacted third molars.20 In our study, the frequency was 7%, primarily after removal of a third molar, but it was also present in one case after removal of a second molar. Pain on the other hand only occurred in cases where a third molar was removed. This may not be surprising since this treatment most often is a simple tooth extraction and not an intervention that usually demands removal of bone. The risk of complications, together with the state of the third and second molar (caries, restorations, endodontic therapy) and need for treatment if preserved, should eventually be considered as a part of the treatment decision and information to the patient.
Prospective clinical studies with larger sample sizes and with clinical and radiographic protocols should be conducted in the future to establish prevalence for ERR in second molars and other pathoses related to an impacted third molar, in addition to accuracy studies with a clinical gold-standard, to define the true extent of ERR in the second molar.
Conclusions
In conclusion, it seems that a CBCT examination of the maxillary third molar region is indicated when ERR of the second molar is suspected from the panoramic image, since findings in CBCT often changed the final treatment decision. Removal of second molars was more often decided after CBCT was available, and severe ERR seen in CBCT was the main factor influencing removal of the maxillary second instead of the third molar.
Contributor Information
Louise Hermann, Email: louise_hermann@hotmail.com.
Ann Wenzel, Email: AWENZEL@dent.au.dk.
Lars Schropp, Email: lars.schropp@dent.au.dk.
Louise Hauge Matzen, Email: louise.hauge.matzen@dent.au.dk.
REFERENCES
- 1.Radiation Protection European guidelines on radiation protection in dental radiology: the safe use of radiographs in dental practice. European Commision. 2004; 136. [Google Scholar]
- 2.Hermann L, Wenzel A, Schropp L, Matzen LH. Marginal bone loss and resorption of second molars related to maxillary third molars in panoramic images compared with CBCT. Dentomaxillofac Radiol 2019; 48: 20180313. doi: 10.1259/dmfr.20180313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Petersen LB, Olsen KR, Christensen J, Wenzel A. Image and surgery-related costs comparing cone beam CT and panoramic imaging before removal of impacted mandibular third molars. Dentomaxillofac Radiol 2014; 43: 20140001.. doi: 10.1259/dmfr.20140001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Petersen LB, Olsen KR, Matzen LH, Vaeth M, Wenzel A. Economic and health implications of routine CBCT examination before surgical removal of the mandibular third molar in the Danish population. Dentomaxillofac Radiol 2015; 44: 20140406. doi: 10.1259/dmfr.20140406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matzen LH, Christensen J, Hintze H, Schou S, Wenzel A. Influence of cone beam CT on treatment plan before surgical intervention of mandibular third molars and impact of radiographic factors on deciding on coronectomy vs surgical removal. Dentomaxillofac Radiol 2013; 42: 98870341. doi: 10.1259/dmfr/98870341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Matzen LH, Wenzel A. Efficacy of CBCT for assessment of impacted mandibular third molars: a review - based on a hierarchical model of evidence. Dentomaxillofac Radiol 2015; 44: 20140189. doi: 10.1259/dmfr.20140189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Matzen LH, Berkhout E. Cone beam CT imaging of the mandibular third molar: a position paper prepared by the European Academy of DentoMaxilloFacial radiology (EADMFR. Dentomaxillofac Radiol 2019; 48: 20190039.. doi: 10.1259/dmfr.20190039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clé-Ovejero A, Sánchez-Torres A, Camps-Font O, Gay-Escoda C, Figueiredo R, Valmaseda-Castellón E. Does 3-dimensional imaging of the third molar reduce the risk of experiencing inferior alveolar nerve injury owing to extraction?: A meta-analysis. J Am Dent Assoc 2017; 148: 575–83. doi: 10.1016/j.adaj.2017.04.001 [DOI] [PubMed] [Google Scholar]
- 9.Ventä I, Vehkalahti MM, Huumonen S, Suominen AL. Signs of disease occur in the majority of third molars in an adult population. Int J Oral Maxillofac Surg 2017; 46: 1635–40. doi: 10.1016/j.ijom.2017.06.023 [DOI] [PubMed] [Google Scholar]
- 10.Li D, Tao Y, Cui M, Zhang W, Zhang X, Hu X. External root resorption in maxillary and mandibular second molars associated with impacted third molars: a cone-beam computed tomographic study. Clin Oral Investig 2019; 8. doi: 10.1007/s00784-019-02859-3 [DOI] [PubMed] [Google Scholar]
- 11.Oenning ACC, Neves FS, Alencar PNB, Prado RF, Groppo FC, Haiter-Neto F. External root resorption of the second molar associated with third molar impaction: comparison of panoramic radiography and cone beam computed tomography. J Oral Maxillofac Surg 2014; 72: 1444–55. doi: 10.1016/j.joms.2014.03.023 [DOI] [PubMed] [Google Scholar]
- 12.Ericson S, Kurol PJ. Resorption of incisors after ectopic eruption of maxillary canines: a CT study. Angle Orthod 2000; 70: 415–23. doi: [DOI] [PubMed] [Google Scholar]
- 13.Matzen LH, Hintze H, Spin-Neto R, Wenzel A. Reproducibility of mandibular third molar assessment comparing two cone beam CT units in a matched pairs design. Dentomaxillofac Radiol 2013; 42: 20130228. doi: 10.1259/dmfr.20130228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. National Institute of Clinical Excellence Guidance on the Extraction of Wisdom Teeth. London, UK: NICE; 2000. [Google Scholar]
- 15.Fryback DG, Thornbury JR. The efficacy of diagnostic imaging. Med Decis Making 1991; 11: 88–94. doi: 10.1177/0272989X9101100203 [DOI] [PubMed] [Google Scholar]
- 16.Matzen LH, Schropp L, Spin-Neto R, Wenzel A. Radiographic signs of pathology determining removal of an impacted mandibular third molar assessed in a panoramic image or CBCT. Dentomaxillofac Radiol 2017; 46: 20160330. doi: 10.1259/dmfr.20160330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nemcovsky CE, Libfeld H, Zubery Y. Effect of non-erupted 3rd molars on distal roots and supporting structures of approximal teeth. A radiographic survey of 202 cases. J Clin Periodontol 1996; 23: 810–5. doi: 10.1111/j.1600-051X.1996.tb00616.x [DOI] [PubMed] [Google Scholar]
- 18.Nitzan D, Keren T, Marmary Y. Does an impacted tooth cause root resorption of the adjacent one? Oral Surgery, Oral Medicine, Oral Pathology 1981; 51: 221–4. doi: 10.1016/0030-4220(81)90047-5 [DOI] [PubMed] [Google Scholar]
- 19.Wang D, He X, Wang Y, Li Z, Zhu Y, Sun C, et al. External root resorption of the second molar associated with mesially and horizontally impacted mandibular third molar: evidence from cone beam computed tomography. Clin Oral Investig 2017; 21: 1335–42. doi: 10.1007/s00784-016-1888-y [DOI] [PubMed] [Google Scholar]
- 20.Rothamel D, Wahl G, d'Hoedt B, Nentwig G-H, Schwarz F, Becker J. Incidence and predictive factors for perforation of the maxillary antrum in operations to remove upper wisdom teeth: prospective multicentre study. Br J Oral Maxillofac Surg 2007; 45: 387–91. doi: 10.1016/j.bjoms.2006.10.013 [DOI] [PubMed] [Google Scholar]
- 21.Pourmand PP, Sigron GR, Mache B, Stadlinger B, Locher MC. The most common complications after wisdom-tooth removal: Part 2: a retrospective study of 1,562 cases in the maxilla. Swiss Dent J 2014; 124: 1057–61. [DOI] [PubMed] [Google Scholar]