Dear Editor,
Goyal et al. describe the use of a condensing lenses with a smartphone attached to a portable, noncontact device to capture retinal images of eyes with retinopathy of prematurity (ROP)[1] Using the iPhone 5S (Apple, Cupertino, USA) and either 20D, 28D, or 40D lenses they were able to achieve 46°, 53°, or 90° of field of view, respectively. The lens and the phone were mounted on a device (MIIRetCam) which was invented for adult fundus imaging. These fields do not qualify as “wide-field” from the perspective of screening for ROP.
The images from the device in their manuscript have high glare artefacts reflecting from the surface of the condensing lens. This is due to the flash of the smart phone, which the authors acknowledge, “is much stronger and divergent than the light source of binocular indirect ophthalmoscope or professional wide-field imaging systems.” The authors must address phototoxicity testing which is imperative while imaging the infant retina. The 3Nethra Neo Camera (Forus Health, India)[2] and the RetCam Shuttle (Natus, USA), which the authors compare their device with, were extensively tested for light and electrical safety before the use on human subjects.
Obtaining oriented images is also a challenge when a noncontact imaging camera like the MIIRetCam is used on awake, preterm infants. Only two of the 16 images in their third figure, are correctly oriented, with the others obliquely slanted or with a quadrant – location mismatch. To a large extent, contact devices eliminate this limitation.
The authors allude to the KIDROP program and compare their process with it. Although they describe a single operator who captures all the study images, they agree that a “nurse assistant is needed to hold the head during examination.”[1] This is effectively the same as the KIDROP program, where only “one” trained technician is needed for capture per geographic area. KIDROP nonphysician imagers are trained not only to image, but also to grade and report simultaneously, as well as receive a validated review by the specialist within 15 min.[3] This obviates the need of the limited ROP specialists we face in the country. The MIIRetCam needs to be tested in the hands of nonophthalmologists before its consideration as a telemedicine tool in the outreach.
Finally, Goyal et al. mention that the “Optos ultrawide camera, RetCam Shuttle, and the 3Nethra Neo” are “unable to image out to the ora serrata.” Whereas the former two cameras are well known as wide-field retinal cameras and have a published track record of imaging the retinal periphery including the ora serrata, we present images from the Neo device which depicts the ora serrata in a mature retina [Fig. 1a] and Type 2 ROP [Fig. 1b] and during laser treatment [Fig. 2a and b]. The KIDROP program uses the depiction of the ora serrata (on both the RetCam shuttle and the Neo) in both eyes to demonstrate a “fully vascularized” or mature retina before the infant is discharged from the screening protocol.[4,5] The depiction of the ora serrata is also used for determining the adequacy of laser treatment [Fig. 2].
Figure 1.
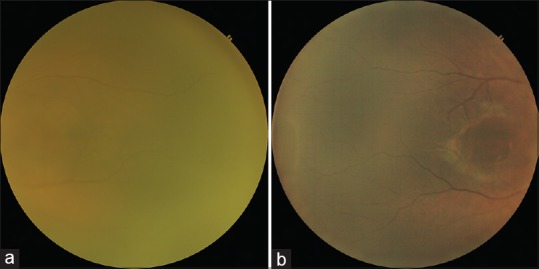
Ora serrata imaged during ROP screening on the Neo Camera (Forus Health, India). (a) Left eye showing a mature retina, with vascularization reaching the ora serrata. This allows the baby to be discharged from screening. (b) Right eye showing one clock hour of stage 1 ROP in zone 3 and the ora serrata anterior to it
Figure 2.
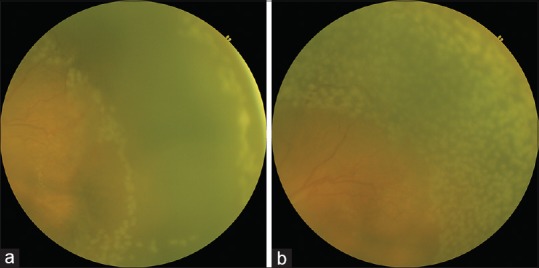
Ora serrata imaged during ROP laser treatment on the Neo Camera (Forus Health, India). (a) Left eye- temporal quadrant showing laser marks at the ora serrata (and part of the posterior border) at the initiation of the laser procedure to mark the anterior extent of the treatment. This method is often performed during training for laser. (b) The same quadrant at the completion of the laser which demonstrates adequacy of laser until the ora serrata
Devices like the MIIRetCam serve as a cost-effective tool for photodocumentation in the office setting. A tool for telemedicine especially in the outreach requires more than just a device.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Goyal A, Gopalakrishnan M, Anantharaman G, Chandrashekharan DP, Thachil T, Sharma A. Smartphone guided wide-field imaging for retinopathy of prematurity in neonatal intensive care unit - A Smart ROP (SROP) initiative. Indian J Ophthalmol. 2019;67:840–5. doi: 10.4103/ijo.IJO_1177_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vinekar A, Rao SV, Murthy S, Jayadev C, Dogra MR, Verma A, et al. A novel, low-cost, wide-field, infant retinal camera, “Neo”: Technical and safety report for the use on premature infants. Transl Vis Sci Technol. 2019;8:2. doi: 10.1167/tvst.8.2.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vinekar A, Jayadev C, Bauer N. Need for telemedicine in retinopathy of prematurity in middle-income countries: e-ROP vs KIDROP. JAMA Ophthalmol. 2015;133:360–1. doi: 10.1001/jamaophthalmol.2014.4913. [DOI] [PubMed] [Google Scholar]
- 4.Vinekar A, Gilbert C, Dogra M, Kurian M, Shainesh G, Shetty B, et al. The KIDROP model of combining strategies for providing retinopathy of prematurity screening in underserved areas in India using wide-field imaging, tele-medicine, non-physician graders and smart phone reporting. Indian J Ophthalmol. 2014;62:41–9. doi: 10.4103/0301-4738.126178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vinekar A, Jayadev C, Mangalesh S, Shetty B, Vidyasagar D. Role of tele-medicine in retinopathy of prematurity screening in rural outreach centers in India - A report of 20,214 imaging sessions in the KIDROP program. Semin Fetal Neonatal Med. 2015;20:335–45. doi: 10.1016/j.siny.2015.05.002. [DOI] [PubMed] [Google Scholar]


