Abstract
Purpose:
To assess and compare the endothelial cell changes after manual small incision cataract surgery (SICS) in diabetic patients versus age group matched non-diabetic patients.
Methods:
This comparative prospective observational follow-up study included 54 diabetic patients and 52 control patients without diabetes who underwent manual SICS. Preoperative, one day, one week, one month and three months post-surgery assessments of corneal endothelial cell changes were done using specular microscopy. Data analysis was performed using SPSS software (version 20.0, SPSS, Inc.). Mann–Whitney U test was used to compare the data between the test group and control group.
Results:
There was drop in the endothelial density in both the groups postoperatively, with the mean percentage of endothelial loss at three months post- surgery being 27.5% in diabetics and 18.3% in controls. There was also a significant increase in central corneal thickness and coefficient of variance in diabetics as compared to controls at every follow up one day, one week, one month and three months. The percentage of hexagonality was statistically significant at post-operative three months.
Conclusion:
The diabetic endothelium was found to be under greater metabolic stress and had less functional reserve after manual SICS than the normal corneal endothelium.
Keywords: Diabetes mellitus, Small incision Cataract surgery, Endothelial cell loss
An estimated 45 million people around the world are blind. Most of them have lost their sight to diseases that are treatable or preventable.[1] In the final push toward the elimination of avoidable blindness, cataract occupies a position of eminence for the success of the Right to Sight initiative (Vision 2020)[2] and diabetes mellitus is one of the major causes of early cataract.[3]
Today's cataract surgery focuses on rapid visual rehabilitation and minimum surgically induced astigmatism. Manual small incision cataract surgery is an alternative technique to phacoemulsification which gives comparable results and is cost-effective.[4]
The monolayer of cells called the corneal endothelium that lines the posterior corneal surface is derived from the neural crest during embryologic development.[5] Corneal endothelial numerical density is highest at birth (3000 cells/mm2) and declines slowly but steadily thereafter. A minimal numerical density of 400-500 cells/mm2 is required to sustain the pumping activity of the endothelium.[6]
The corneal endothelium is essential for maintenance of normal corneal hydration, thickness, and transparency.[4] The dehydrated state of cornea can be monitored by measurement of endothelial cell counts.[7] Loss or damage of endothelial cells leads to an increase in corneal thickness (edema) which may ultimately induce corneal decompensation and loss of vision.[6]
In order to evaluate the degree of surgical trauma, endothelial status and morphological criteria are more precise. This is because the functional capacity of the endothelium is substantial and corneal cell depletion is not reflected in corneal thickness measurements, until there is a substantial loss of corneal endothelial cell count.[8]
Worldwide more than 285 million people are affected by diabetes mellitus. This number is expected to increase to 439 million by 2030 according to the International Diabetes Federation.[3] Diabetes mellitus is perhaps the most important noninfective epidemic to hit the globe in the present millennium.[9] Hyperglycemia in diabetic patients causes metabolic stress which can lead to lower endothelial cell density and greater pleomorphism and polymegathism.[4]
Specular microscopy can provide a noninvasive morphological analysis of the corneal endothelial cell layer from subjects enrolled in clinical trials.[10] The response and effect of stress and trauma of cataract surgery on endothelial cell could not have been so well documented if it was not for the advent of specular microscopy.[11]
In most conditions that produce corneal edema, it is the endothelial layer that is malfunctioning and needs proper evaluation.
Hence, this study was undertaken to assess the stability and vulnerability of the corneal endothelium to avoid postoperative damage to corneal and reduce corneal edema to retain normal corneal function.
Methods
Objective
The primary objective of the study was to assess and compare the endothelial cell changes after small incision cataract surgery in diabetic patients versus age-matched nondiabetic patients. The secondary objective was to evaluate the corneal endothelial cell loss with respect to duration of diabetes; and in relation to glycosylated hemoglobin (HbA1c) after small incision cataract surgery.
Study design
A 1-year prospective observational follow-up (longitudinal) study was conducted in ophthalmology outpatient department of our institution.
Study subjects
Total of 106 patients (54 diabetics and 52 nondiabetics) with senile uncomplicated cataract (age range between 50 years and 80 years, divided in different age categories) who were assigned to undergo small incision cataract surgery at our tertiary center during November 2017 to November 2018. Unwillingness, an known/diagnosed case of glaucoma, history of uveitis/trauma, history of previous ocular surgery, history of any other systemic illness, corneal opacity, contact lens wearers, age-related macular degeneration, and traumatic cataract (penetrating injury-induced cataract) were excluded from this study. Written informed consent was obtained from all patients before surgery and examinations, and the study was conducted in tenets of the Declaration of Helsinki. Ethical approval was obtained from the Institutional Review Board of the hospital. Approval of ethics committee from institution obtained and dated October 2017.
Methodology
The included patients had a casual blood glucose test performed to disclose undetected diabetes. The patients with diabetes had a serum glycosylated hemoglobin (HbA1c) test performed to reveal the glycemic control. Preoperative, 1 day, 1 week, 1 month, and 3 months postsurgery assessments of corneal endothelial cell changes were done using noncontact specular microscopy (Tomey EM-4000). A specular microscopy photography of a case versus controls has been represented in Photograph 1.
Photograph 1.
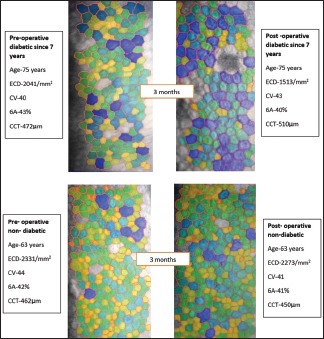
Specular microscopy image preoperative and postoperative in case versus controls
Surgical technique
All the eyes were dilated preoperatively with tropicamide 1% and phenylephrine 5% eye drops. Pupil dilatation was estimated using Rosenbaum chart. All surgeries will be performed by a single surgeon under peribulbar anesthesia using of 5 ml of lignocaine with 150 units of hyaluronidase. All surgeries were done by a single experienced surgeon. Surgery was done through 6.5 mm scleral incision. Nucleus was prolapsed in anterior chamber after performing capsulorrhexis and delivered with irrigating wire vectis. Single piece polymethylmethacrylate intraocular lens was implanted in the bag in all patients after cortical aspiration. All surgeries were performed by a single surgeon.
Statistical analysis
Data analysis was performed using SPSS software (version 20.0, SPSS, Inc.). Mann–Whitney U test was used to compare the data between the test group and control group. Microsoft office- Excel 2010 was used to construct the tables and graphs. The result was significant at P < 0.05.
Results
In this study, we compared the endothelial cell loss and other corneal endothelial cell morphology in 54 eyes of diabetic patients with 52 eyes of nondiabetic patients undergoing standard uncomplicated small incision cataract surgery. Age and gender distribution of diabetic and nondiabetic patients, grades of cataract, pupil dilatation, and duration of diabetes in diabetic patients are given in Table 1. The percentage of patients with poorly dilating pupil (i.e., ≤6 mm) in the diabetic group was 20.3% and in nondiabetic group was 5.7%.
Table 1.
Patient demographics
| Non-Diabetic | Diabetic | |||||
|---|---|---|---|---|---|---|
| Male | Female | Total | Male | Female | Total | |
| Sample Size | 25 | 27 | 52 | 31 | 23 | 54 |
| Age Group | ||||||
| 50-54 | 2 | 8 | 10 | 6 | 5 | 11 |
| 55-59 | 4 | 6 | 10 | 10 | 3 | 13 |
| 60-64 | 4 | 9 | 13 | 3 | 6 | 9 |
| 65-69 | 7 | 0 | 7 | 3 | 6 | 9 |
| 70-74 | 4 | 3 | 7 | 4 | 2 | 6 |
| 75-80 | 4 | 1 | 5 | 5 | 1 | 6 |
| Cataract grade | ||||||
| 1 | 4 | 0 | 4 | 6 | 3 | 9 |
| 2 | 8 | 21 | 29 | 11 | 6 | 17 |
| 3 | 4 | 4 | 8 | 8 | 6 | 14 |
| 4 | 1 | 2 | 3 | 1 | 0 | 1 |
| Mature | 8 | 0 | 8 | 2 | 8 | 10 |
| Hypermature | 0 | 0 | 0 | 3 | 0 | 3 |
| Duration of Diabetes | ||||||
| 0-5 years | 17 | 16 | 33 | |||
| 5-10 years | 4 | 3 | 7 | |||
| 10-15years | 4 | 2 | 6 | |||
| 15-20 years | 4 | 2 | 6 | |||
| above 20 years | 2 | 0 | 2 | |||
| HbAlc | 5.67±1.68 | 5.84±1.58 | 5.76±1.61 | 7.18±2.68 | 8.09±3.32 | 7.56±2.94 |
| Pupil Dilatation | ||||||
| 4 | 0 | 0 | 0 | 2 | 0 | 2 |
| 5 | 0 | 1 | 1 | 3 | 0 | 3 |
| 6 | 1 | 1 | 2 | 4 | 2 | 6 |
| 7 | 4 | 7 | 11 | 7 | 3 | 10 |
| 8 | 6 | 8 | 14 | 8 | 8 | 16 |
| 9 | 5 | 6 | 11 | 4 | 7 | 11 |
| 10 | 9 | 4 | 13 | 3 | 3 | 6 |
Corneal endothelial cell count
The mean preoperative endothelial count in the test and control group was not significant (P = 0.1141). On comparing postoperative endothelial loss in control group to diabetic group, the diabetic group had significantly higher endothelial loss 1 and 3 months postoperatively [Fig. 1].
Figure 1.
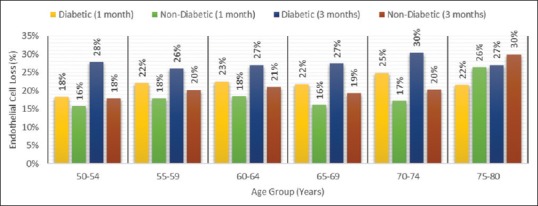
Endothelial cell loss percentage postoperative 1 and 3 months
Central Corneal Thickness (CCT)
The central cornea was thicker in diabetic group compared to control group (P = 0.0012). On comparing intergroup change there was significant increase in central corneal thickness post 1 month and thereby gradually decreased to nearly preoperative state post 3 months in diabetics as well as nondiabetics [Table 2].
Table 2.
Summary of corneal endothelial cell parameters postoperatively 1 and 3 months postoperatively
| Corneal Parameters | Diabetic | Non Diabetic | ||||
|---|---|---|---|---|---|---|
| Preop | 1 month | 3 months postop | Preop | 1 month | 3 months postop | |
| CCT | ||||||
| Mean±SD | 509.89±30.32 | 527.96±24.68 | 512.96±24.91 | 492.25±19.41 | 501.56±18.31 | 484.06±19.14 |
| Max | 586.00 | 599.00 | 585.00 | 529.00 | 536.00 | 525.00 |
| Min | 446.00 | 476.00 | 458.00 | 435.00 | 457.00 | 439.00 |
| ECD | ||||||
| Mean±SD | 2246.20±195.32 | 1764.09±233.49 | 1632.28±231.32 | 2356.19±218.32 | 1764.09±221.10 | 1869.25±225.98 |
| Max | 2669.00 | 2333.00 | 2240.00 | 3065.00 | 2597.00 | 2523.00 |
| Min | 1852.00 | 1111.00 | 1003.00 | 2008.00 | 1527.00 | 1457.00 |
| CV | ||||||
| Mean±SD | 34.83±4.04 | 38.96±4.80 | 42.83±4.76 | 32.69±4.59 | 38.96±5.19 | 38.00±5.26 |
| Max | 44.00 | 49.00 | 54.00 | 45.00 | 51.00 | 56.00 |
| Min | 29.00 | 30.00 | 32.00 | 23.00 | 27.00 | 30.00 |
| Hexagonal Cells | ||||||
| Mean±SD | 34.83±4.04 | 40.19±5.46 | 42.83±4.76 | 32.69±4.59 | 40.19±4.97 | 38.00±5.26 |
| Max | 63.00 | 49.00 | 46.00 | 61.00 | 51.00 | 50.00 |
| Min | 33.00 | 26.00 | 23.00 | 33.00 | 31.00 | 30.00 |
Coefficient of Variance (CV)
The preoperative coefficient of variance for control group was significantly lower to that of diabetic group (P < 0.001). The postoperative change in coefficient of variance increased in diabetic group significantly [Table 2].
Percentage of Hexagonal Cells (6A)
The change in percentage hexagonal cells in diabetic group and control group was not significant preoperatively (P = 0.8493). The postoperative change in percentage of hexagonal cells within both the groups changed and was significant 3 months postsurgery [Table 2]. All the corneal endothelial cell parameter results have been summarized in Table 2.
Corneal cell loss according to duration of diabetes
The intergroup changes in duration of diabetes were not significant [Table 3].
Table 3.
Endothelial cell loss with relation to duration of diabetes
| Duration of Diabetes (Years) | Count (n) | Pre-operative cell count | Post-operative cell count | ||||
|---|---|---|---|---|---|---|---|
| Endothelial cell loss % | 1 month | Endothelial cell loss % | 3 months | Endothelial cell loss % | |||
| 0-10 | 40 | 2228.50±216.61 | 17% | 1728.65±258.00 | 22% | 1597.98±0.00 | 28% |
| 11-20 | 12 | 2288.92±105.17 | 16% | 1862.75±87.52 | 19% | 1627.37±0.00 | 25% |
ECD loss in relation to HbA1c
The subgroup comparison between age-matched diabetic patients with HbA1c lower than 7% versus greater than 7% did not yield significant differences in terms of percentage of endothelial cell loss [Fig. 2].
Figure 2.
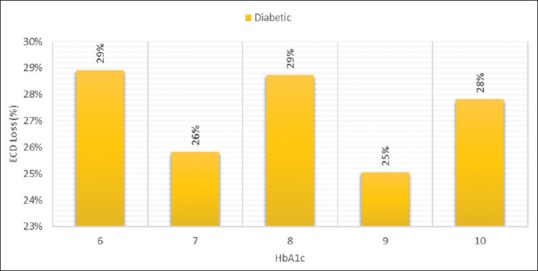
Endothelial cell loss % post 3 months in relation to HbA1c
Discussion
Endothelial cell density
In our study, we found that the preoperative corneal endothelial cell measured in the diabetic group and the healthy age-group matched control group was not significant contrary to study by Dhasmana et al.[4]
Like our study, studies conducted by Lee et al.,[12] Parekh et al.,[9] and Dhasmana et al.[4] and many other studies reported that both the groups showed significant corneal endothelial loss in the postoperative period. The endothelial count showed progressive decrease in postoperative period, up to 1 month in both groups. However, this endothelial loss was more pronounced in the diabetic group as compared to the control group. A recent study conducted in southern India with a large study sample showed that the mean endothelial cell density was significantly lower across all age groups in patients with type 2 diabetes mellitus compared with controls.[13] Despite the decrease in endothelial count in the diabetic group none of the patients developed corneal decompensation.
Central corneal thickness
According to our results, diabetic patients showed significant differences compared with normal persons in terms of the central corneal thickness. These findings were similar to studies by Busted et al.[14] and Lee et al.[12] Diabetes has reduced activity of Na+ - K+ ATPase of the corneal endothelium and this causes the morphological and functional changes of diabetic corneas.[14] It is thought that in diabetic's aldose reductase causes intracellular accumulation of polyol, which acts as an osmotic agent leads to swelling of the endothelial cells.[15] The recovery of cornea in diabetics takes longer compared to normal controls.
CV and % of hexagonal cells
In our study, diabetic cornea had lower percentage of hexagonal cells than in the normal cornea which was not significant and there was a significant increase in coefficient of variance. Intergroup difference noted at day 1, 1 week, 1 month, and 3 months postsurgery showed there was steady increase in coefficient of variance in both the groups which was statistically significant similar to studies by Sahu et al.,[16] Sudhir et al.[13] Study conducted by El-Agamy and Alsubaie[15] showed that the change in percentage of hexagonal cells and coefficient of variance in diabetic group was higher than in control group. On the contrary studies by Dhasmana et al.,[4] Hugod et al.[17] said that there was a significant decrease in percentage of hexagonal cells. It is thought that diabetes reduces the activity of Na+–K+ ATPase of the corneal endothelium, and this causes the morphological changes and permeability changes in the corneas.[18] However, decrease in percentage of hexagonal cells was not statistically significant which was similar to study by Lee et al. Both these parameters reflect the endothelial cellular repair of cornea.
Duration of diabetes
Duration of diabetes was further correlated with the mean postoperative endothelial loss. There was no statistical significance to the percentage endothelial cell loss to the duration of diabetes like study byBriggs et al. which compared Diabetic subjects of >10 years duration or less.[19] Hugod et al. showed that type 2 diabetes has no impact on corneal cell density in subjects with good glycemic status.[17] Since our patients had all good glycemic control to avoid postoperative complications, we noted that there was no significant preoperative difference between diabetics and controls.
Conclusion
On the basis of our study's results, diabetics have morphological abnormalities in contrast to normal persons such as
Significant steady decrease in corneal endothelial cell density
Greater baseline corneal thickness with increased thickness over a month which was statistically significant. The central corneal thickness was near preoperative value post 3 months
Decreased percentage of hexagonality which statistically significant at 3 months
Significant increase in coefficient of variation in cell size
The morphological changes in cornea of diabetics are associated with low functional reserve
Preoperative evaluation of corneal endothelium in diabetic patients is therefore recommended before intraocular surgeries. Due precautions should be taken to minimize insult to corneal endothelium during surgery.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Pizzarello L, Abiose A, Ffytche T, Duerksen R, Thulasiraj R, Taylor H, et al. VISION 2020: The right to sight. Arch Ophthalmol. 2004;122:615. doi: 10.1001/archopht.122.4.615. [DOI] [PubMed] [Google Scholar]
- 2.Murthy G, Shamanna B, John N, Pant H. Elimination of avoidable blindness due to cataract: Where do we prioritize and how should we monitor this decade? Indian J Ophthalmol. 2012;60:438. doi: 10.4103/0301-4738.100545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khan A, Kose S, Jharwal M, Meena A, Sharma A. Comparison of corneal endothelial cell count in patients of DM (Type 2) and Non Diabetics after Phacoemulsification and Intraocular Lens Implantation. Int Multispecialty J Health (IMJH) 2016;6:14–22. [Google Scholar]
- 4.Dhasmana R, Singh I, Nagpal R. Corneal changes in diabetic patients after manual small opthalmology section incision cataract surgery. J Clin Diagn Res. 2014;8:VC03–6. doi: 10.7860/JCDR/2014/7955.4288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bourne W. Biology of the corneal endothelium in health and disease. Eye. 2003;17:912–8. doi: 10.1038/sj.eye.6700559. [DOI] [PubMed] [Google Scholar]
- 6.Ventura A, Walti R, Bohnke M. Corneal thickness and endothelial density before and after cataract surgery. Br J Ophthalmol. 2001;85:18–20. doi: 10.1136/bjo.85.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Acar B, Utine C, Acar S, Ciftci F. Endothelial cell loss after phacoemulsification in eyes with previous penetrating keratoplasty, previous deep anterior lamellar keratoplasty, or no previous surgery. J Cataract Refract Surg. 2011;37:2013–7. doi: 10.1016/j.jcrs.2011.05.033. [DOI] [PubMed] [Google Scholar]
- 8.Sallet G. Viscoless microincision cataract surgery. Clin Ophthalmol. 2008;2:717–21. doi: 10.2147/opth.s1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parekh R, Ranganath K, Suresh K, Dharmalingam M. Corneal endothelium count and thickness in diabetes mellitus. Int J Diabetes Developing Countries. 2006;26:24. [Google Scholar]
- 10.Mc. Carey B, Edelhauser H, Lynn M. Review of corneal endothelial specular microscopy for FDA clinical trials of refractive procedures, surgical devices, and new intraocular drugs and solutions. Cornea. 2008;27:1–16. doi: 10.1097/ICO.0b013e31815892da. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jagani S, Lune A, Magdum R, Shah A, Singh M, Datta D. Comparison of endothelial cell loss by specular microscopy between phacoemulsification and manual small-incision cataract surgery. Niger J Ophthalmol. 2015;23:54. [Google Scholar]
- 12.Lee J, Oum B, Choi H, Lee J, Cho B. Differences in corneal thickness and corneal endothelium related to duration in Diabetes. Eye. 2005;20:315–8. doi: 10.1038/sj.eye.6701868. [DOI] [PubMed] [Google Scholar]
- 13.Sudhir R, Raman R, Sharma T. Changes in the corneal endothelial cell density and morphology in patients with type 2 diabetes mellitus. Cornea. 2012;31:1119–22. doi: 10.1097/ICO.0b013e31823f8e00. [DOI] [PubMed] [Google Scholar]
- 14.Busted N, Olsen T, Schmitz O. Clinical observations on the corneal thickness and the corneal endothelium in diabetes mellitus. Br J Ophthalmol. 1981;65:687–90. doi: 10.1136/bjo.65.10.687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.El-Agamy A, Alsubaie S. Corneal endothelium and central corneal thickness changes in type 2 diabetes mellitus. Clin Ophthalmol. 2017;11:481–6. doi: 10.2147/OPTH.S126217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sahu P, Das G, Agrawal S, Kumar S, Kumar N. Comparative evaluation of corneal endothelium in patients with diabetes undergoing phacoemulsification. Middle East Afr J Ophthalmol. 2017;24:74. doi: 10.4103/meajo.MEAJO_242_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hugod M, Storr-Paulsen A, Norregaard JC, Nicolini J, Larsen AB, Thulesen J. Corneal endothelial cell changes associated with cataract surgery in patients with type 2 diabetes mellitus. Cornea. 2011;30:749–53. doi: 10.1097/ICO.0b013e31820142d9. [DOI] [PubMed] [Google Scholar]
- 18.Tang Y, Chen X, Zhang X, Tang Q, Liu S, Yao K. Clinical evaluation of corneal changes after phacoemulsification in diabetic and non-diabetic cataract patients, a systematic review and meta-analysis. Sci Rep. 2017;7:14128. doi: 10.1038/s41598-017-14656-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Briggs S, Osuagwu U, AlHarthi E. Manifestations of type 2 diabetes in corneal endothelial cell density, corneal thickness and intraocular pressure. J Biomed Res. 2016;30:46–51. doi: 10.7555/JBR.29.20140075. [DOI] [PubMed] [Google Scholar]


