Abstract
Purpose:
To report the outcomes of pars-plana approach for the management of brunescent cataract in eyes with severe microcornea and associated chorio-retinal coloboma.
Methods:
This was a retrospective, single center, interventional case series performed in a tertiary eyecare center in central Medical records of consecutive cases of microcornea with coloboma who underwent pars-plana vitrectomy with phacofragmentation (PF) between January 2015 and December 2017 were reviewed.
Results:
The study group comprised of 30 eyes of 30 patients, of which 18 (60%) were males and 12 (40%) were females. The mean age of the patients was 41.9 years (range of 17–70 years). The mean corneal diameter was 6.7 mm with a range of 4–8 mm and all the eyes had dense cataract with nuclear sclerosis of grade 4 or more. The mean preoperative visual acuity was 1.97 (+/-0.067) Log MAR and the mean postoperative vision at 1 month was 1.6 (+/-0.39) Log MAR. Postoperatively, 21 patients (70%) gained ambulatory vision. The visual gain in all the patients was maintained over a mean follow-up period of 15.5 months.
Conclusion:
Pars-plana vitrectomy with PF can be considered in eyes with severe microcornea and brunescent cataracts, where cataract surgery through the limbal (anterior) approach is not only difficult but at times impossible due to anatomical restraints.
Keywords: Brunescent cataract, cataract extraction, chorio-retinal coloboma, pars-plana approach, phacofragmentation, severe microcornea
The spectrum of microcornea and chorio-retinal (CR) coloboma is vast and varied. This is thought to arise due to the premature arrest of fusion of embryonic fissure at 5–8 weeks of gestation leading to microopthalmia and coloboma formation.[1] The incidence of nuclear sclerosis is much higher in the cases of microcornea with irido-fundal coloboma compared to the general population; in addition, the development and progression of cataract occurs at a much younger age in these eyes.[2,3,4,5]
Cataract surgery in eyes with microcornea and coloboma can be challenging and carries a higher risk of surgical complications, due to associated anatomical anomalies. The use of standard techniques like phacoemulsification (PE)/extra capsular cataract extraction (ECCE)/manual small incision cataract surgery (M-SICS), in these small eyes, is fraught with serious intraoperative and postoperative risks which include: damage to the corneal endothelium, descemet's membrane detachment, posterior capsular dehiscence, vitreous loss, and nucleus drop. The risk increases with the severity of microcornea and grade of nuclear sclerosis.
Literature pertaining to the surgical experience in coloboma is limited with respect to surgical options available, especially in scenarios where the irido-fundal coloboma is associated with extreme severity of microcornea, and any form of intervention in these cases is challenging and is often threatened by the risk of complication.
In the present study, we report our experience of using an alternate pars-plana approach in eyes with severe and very severe grade of microcornea with CR coloboma and hard cataract. These eyes were initially deemed inoperable through the anterior route due to the same but fared well after pars-plana fragmentation.
Methods
This is a retrospective, single center, interventional case series. Consecutive eyes with severe or very severe grade of microcornea with iris and CR coloboma and brunescent cataracts that underwent pars-plana vitrectomy with phacofragmentation (PF) were included in the study.
Case records of all patients were screened for demographic data, clinical presentation, preoperative and postoperative visual acuity, surgical details, and intra and postoperative surgical complications. A written informed consent was obtained from all patients before undergoing surgical intervention. The study adhered to the tenets of Declaration of Helsinki.
The eyes were categorized based on the maximum horizontal corneal diameter: severe microcornea when maximum horizontal corneal diameter was less than 8 mm and very severe microcornea when maximum corneal diameter was less than 6 mm. The corneal diameter was measured intraoperatively, just before the placement of the ports.
Corrected distance visual acuity (CDVA) was measured using Snellen vision chart, which was converted to Log MAR values and was further graded for severity of blindness using the visual standard report of International Council of Ophthalmology [Chart 1].[6]
Pre and postoperative vision was recorded using Snellen's distance vision chart. In the cases with vision less than 6/60, the patient was moved closer to the chart until vision could be recorded. In the cases with vision less than 3/60, the vision was recorded based on the ability to count fingers at 1 m, 2 m, and 3 m. The cases with vision less than 1/60 were evaluated for having the ability to perceive the examiner's hand movement.
It was indeed difficult to quantify the benefits of functional gain after having undergone catarct surgery. To better elucidate the visual gain, the log mar values obtained were superimposed on to a standardized international visual impairment scale by the international council of ophthalmology; this helped us in grading the functional impairment and highlighting the achieved change in terms of change in severity of the grade of blindness.
The specular count could not be obtained in the majority of these patients due to nystagmus and extremely small eyes making the specular examination impossible. Postoperatively the patients were examined at 1 week and 4 weeks; the best possible aphakic correction was given in the immediate postoperative period whenever possible.
Corneal edema grading was graded using the Oxford cataract treatment and evaluation team (OCTET) grading.[7,8] The OCTET grades corneal edema as transient corneal edema (+), transient corneal edema with descemet membrane folds of <10 (++), and transient corneal edema with descemet membrane folds of > 10 (+++).
Surgical technique
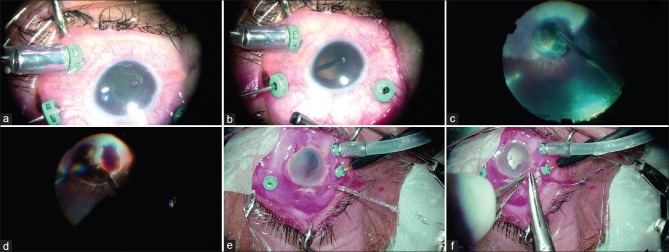
All the surgeries were performed under peribulbar anesthesia. The surgeries were done by four senior surgeons (AS, AM, SS, and SG), who followed uniform and standard surgical steps based on institution's protocols [Fig. 1a-f]. (Image-1) Standard 20/23 gauge sclerostomy ports were made at 3.0 mm from the limbus in the infero-temporal (ITQ), supero-nasal (SNQ), and supero-temporal (STQ) quadrants, respectively.
Figure 1.
(a) Sclerostomy ports are made at 3 mm from the limbus following which the cutter is used to engage the zonules and truncate it; this also in parallel creates dehiscence in the posterior capsule. The cutter is also used to mechanically dislocate the nucleus while cutting the zonules; this allows convenient visualization of the site of interest. (b) Once the zonulectomy is completed, the nucleus spontaneous dislodges into the vitreous cavity. Any capsular remnants can then be attended to. (c) Dislodged nucleus is maintained in the area of coloboma and this avoids undue manipulations over the healthy retina, thereby decreasing the possibility of iatrogenic breaks. (d) PF of the lens is done preferably over the colobomatous area after completing posterior vitreous detachment and performing adequate vitrectomy. Cracking of the hard nucleus if facilitated by using a phacofragmatome to burr-hole into the nuclear substance, hence, creating a fracture, which is subsequently enlarged bimanually using both the fragmatome and the light pipe; this further widens the rift between the fractured fragments. Bimanual technique using light pipe and cutter is adopted to ease the nuclear fracture under chandelier-assisted illumination, after which the smaller segments are conveniently emulsified and aspirated. (e) Sclerostomy utilized for fragmatome is checked for wound burns and closed. (f) Fragmentation is completed successfully without any scleral wound burns, after which the fragmatome is removed and the scleral wounds are securely closed using a running shoelace suture.
The infusion cannula was placed in the ITQ and visualized through the window provided by the iris coloboma and lens coloboma since dense cataract obscured any useful view of posterior segment. In the cases where visualization of the cannula was not possible, the surgeon used an anterior chamber maintainer, which was later removed once the infusion cannula was securely placed and confirmed in the vitreous cavity.
After securing the active and passive ports, anterior vitrectomy was initiated; the cutter was then used to engage and truncate the lens zonules and to open up the posterior capsule to facilitate dislocation of the nucleus into the vitreous cavity. Posterior vitreous detachment (PVD) was then induced using vitrectomy probe and active suction. A thorough vitrectomy was done to free the nucleus from all its vitreous adhesions and the PVD was extended beyond the equator.
PF of the nucleus was performed in the mid vitreous cavity using a 20-gauge phaco-fragmatome (Alcon constellation system©, ALCON, USA), inserted through a separate 20-gauge sclerostomy port, with pulsed ultrasound setting and power ranging from 40% to 80%, depending on the grade of cataract. Continuous port side irrigation during PF was done to prevent any thermal damage to the sclera. Before closure, the peripheral retina was thoroughly checked for iatrogenic break, if any were treated with endo-laser photocoagulation or cryopexy followed by internal tamponade using silicone oil (SO) when needed.
Statistical analysis
The data collected on continuous and ordinal scale was expressed as mean, median, and range. Paired t test has been used to compare preoperative and postoperative corrected distance visual acuity; P value of <0.05 was considered statistically significant.
Results
In the present study, 30 eyes of 30 patients underwent cataract extraction through pars-plana route. Mean age was 41.93 (+/-15.38) years; there were 18 males (60%) and 12 females (40%). All the eyes that underwent surgery had bilateral conjugate horizontal jerky nystagmus. Mean preoperative vision was 1.95 +/-0.067 log MAR while 21 out of 30 eyes had presenting vision of light perception. The majority of the patients (24 out of 30) were one eyed, having no light perception in the other eye. Table 1 shows the baseline characteristics of all the patients. The mean follow-up period was 15.5 months, ranging from 12 to 24 months.
Table 1a.
Patient demographics, clinical presentation and preoperative findings
| Demographic Details | Study cohort (n = 30) eyes |
|---|---|
| Age | 41.93years |
| Sex | 18 males (60%); 12 females (40%) |
| Laterality | 18 right eye (60%); 12 left eye (40%) |
| Preoperative assessment | |
| Preoperative BCVA (distance) | 1.95+/-0.067 |
| Corneal diameter | 6.7+/-0.64 mm (<= 6 mm: 20 eyes) (6-8 mm: 10 eyes) |
| Pupil<6 mm | 5 eyes |
| Nystagmus | 30 eyes |
| Lens grade (LOCS-3) | mature cataract: 5 eyes; NS grade 4: 25 eyes |
| Phacodonesis | 11 EYES |
| Dislocated nucleus | 2 eyes |
| Type of CR coloboma | Type 3 (28 eyes); no CR coloboma (2 eyes) |
| Intercalary membrane defect (ICMD) | no ICMD (16 eyes) ICMD present (14 eyes) |
| Blindness grade | grade 4 (30 eyes) |
| Other Eye Status | |
| Anophthalmia | 2 eyes |
| Phthisis Bulbi | 21 eyes |
| Micro Cornea With RD | 1 eye |
| Micro Cornea With IMSC | 3 eyes |
| Micro Cornea With Pciol | 1 eye |
| Emmetropic | 2 eyes |
Table1 b.
Intraoperative and postoperative details
| Study cohort (n=30) | |
|---|---|
| Intraoperative details | |
| Gauge of vitrectomy | 20 G (7 eyes); 23 G (23 eyes) |
| Fragmatome power | 65.66+/-13.14% |
| Phaco time | 5.16 +/-1.36 minute |
| PVD induction | 28 eyes |
| Intraoperative difficulty and complications | |
| Small pupil | 5 eyes |
| Use of iris hooks | 2 eyes |
| Retinal break and detachment | iatrogenic break (3 eyes) preexistent RD (1 eye) |
| Silicone oil injection | 4 eyes |
| Postoperative status | |
| Aphakia | 30 eyes |
| Corneal edema | 1 eye (3%) |
| BCVA 1 week | log MAR 1.69 (+/-0.37) |
| BCVA 1 month | log MAR 1.62 (+/-0.39) |
| Blindness grade | grade 1 (1 eye); grade 2 (5 eyes); grade 3 (5 eyes) |
| Retinal detachment | 1 eye |
The median corneal diameter of the eyes which underwent surgery was 6 mm with a mean value of 6.7 mm +/-0.64 mm. The mean axial length of the eyes operated was 22.98 mm +/-1.042 mm. Phacodonesis was present in 11 out of 30 eyes and 2 eyes already had a posteriorly dislocated nucleus. All 30 eyes had Ida-Mann type-1 CR coloboma.
A 20-gauge vitrectomy was performed in 7 eyes and 23-gauge was used in the remaining 23 eyes. Posterior dislocation of the lens by truncating the zonules was accomplished in all cases, except 2 eyes where the lens was already posteriorly dislocated. PVD was already present in 2 eyes and was induced during surgery in rest of the eyes.
In one eye, intraoperative pupilloplasty was performed and iris hooks were applied in the second eye for adequate visualization.
Iatrogenic breaks were noted during the procedure in 2 out of 30 eyes. In both eyes, the breaks occurred between the equator and ora above the horizontal meridian and were associated with localized retinal detachment (RD). Both the cases were treated with endo drainage followed by endo laser and SO tamponade. One eye developed RD on postoperative day 1; here, a break was localized in the ICM, however, no peripheral break could be detected. The case was treated with fluid air exchange through the ICM break and endo laser to the coloboma edge was done followed by SO tamponade. Intraoperative barrage laser to the coloboma edge was not done in any of the eyes.
On postoperative of day 1, the cornea was clear in 29 eyes. Only one eye showed a grade 1 epithelial edema. None of the eyes showed a spike in intraocular pressure (IOP) or significant anterior chamber cellular reaction [Figs. 2-4].
Figure 2.
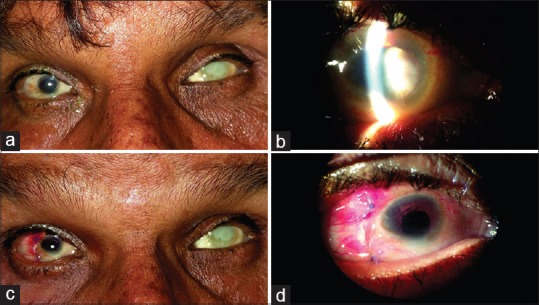
(a) Microcornea of 7 mm diameter measured on slit lamp with a hard brown cataract in the right eye (b), while the left eye is phthisical. Postoperative day one picture of the same patient with a clear cornea, well-formed anterior chamber and minimal congestion (c and d)
Figure 4.
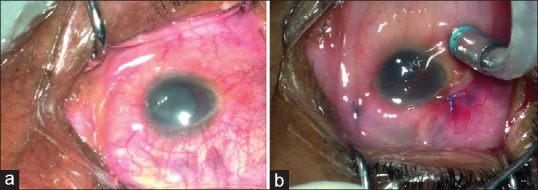
(a) Comparative pre and immediate postoperative images of a case with very severe grade of microcornea. (b) Corneal clarity is maintained at the end of the procedure
Figure 3.
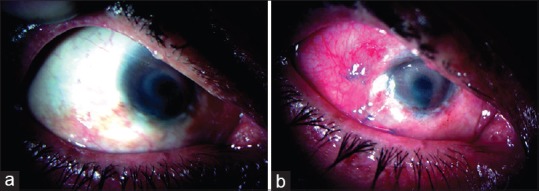
Preoperative slit lamp photo of an eye with very severe microcornea with nebular grade stromal opacity and hard brown cataract (a). Postoperative of day one, the cornea is clear with minimal intraocular inflammation and circumcorneal congestion. The wounds are secure with no corneal distortion (b)
Visual acuity improved in 21 eyes and remained unchanged in 9 eyes. The mean CDVA at the first postoperative month was 1.6 log MAR (+/-0.39) [Table 2]; 3 of the 9 eyes that did not show visual improvement at 1 month had features suggestive of a self-settled RD and the remaining 6 eyes had extensive CR coloboma with dysplastic optic disc.
Table 2.
Paired Samples Statistics
| Mean | n | Std. deviation | n | |
|---|---|---|---|---|
| Pair 1 | ||||
| Pre Op V/A | 1.959 | 29 | 0.0682 | |
| Post Op V/A 1 Day | 1.824 | 29 | 0.2668 | 0.003 |
| Pair 2 | ||||
| Pre Op V/A | 1.959 | 29 | 0.0682 | |
| Post Op V/A Day 7 | 1.690 | 29 | 0.3707 | 0.009 |
| Pair 3 | ||||
| Pre Op V/A | 1.959 | 29 | 0.0682 | |
| Post Op V/A 1 month | 1.624 | 29 | 0.3916 | 0.046 |
Paired correlation of vision in microcornea eyes with chorio-retinal coloboma pre and post operatively
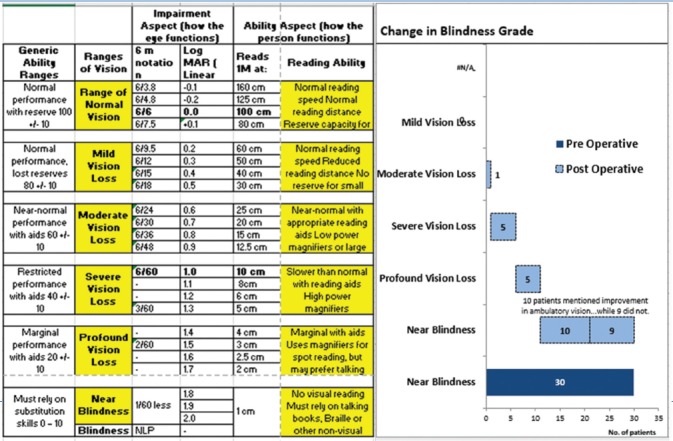
Notably, 21 of the 30 patients operated showed subjective improvement in ambulatory vision. However, since the majority of the study subjects had extensive CR coloboma involving the macula and optic disc, the final vision was too less for us to compute the quantitative significance of the gain achieved using log MAR values alone. Hence, we graded the vision at presentation and the final vision achieved by the patient as per the blindness grade provided by the ICD 9, 10, and 9-M classification system [Chart 1] and later compared it to quantitatively evaluate the change.[6] Accordingly 11 patients showed improvement in the grade of blindness taking the ICD criteria into account. Of these 11 patients, 5 showed alleviation of the near blindness grade to the level of profound visual impairment; 5 eyes stepped up to severe visual impairment grade and 1 eye improved to the level of moderate visual impairment. In 10 eyes, no objective visual improvement could be documented [Table 3].
Chart 1.
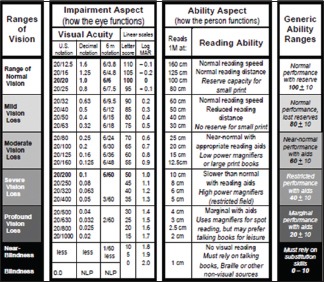
Aspects and ranges of vision and vision loss. Adapted from visual standard report[4]
Table 3.
This chart represents the different grades of blindness as per the ICD 9 classification and depicts the change in the blindness grade following surgery, among the study cohort
Discussion
The prevalence of congenital coloboma is estimated to be 4.89 per 100,000 newborns.[2] Most studies report significant cataract formation in eyes with CR coloboma; this is believed to occur at a relatively younger age compared to the age-related cataract. Many of these eyes are also associated with microcornea.[2,3,4,5]
Cataract surgery in these eyes remains challenging, often associated with the higher risk of intraoperative and postoperative complications. Among these, eyes with severe (corneal diameter <8 mm) and very severe grade of microcornea (corneal diameter <6 mm) with dense hard cataracts are probably the most difficult cases to operate. The limited anterior chamber space combined with hard bulky nucleus poses great challenge to the operating surgeon.
Several studies have reported the outcomes of cataract surgery in eyes with coloboma, but they are limited by the small sample size and heterogeneity of cases.[3,4,5]
Khokhar S et al. reported favorable outcomes with PE and foldable intra-ocular lens (IOL) implantation in a retrospective study of 22 eyes with coloboma and cataract.[4] In their study, the mean corneal diameter was 11.16 mm and only 6 eyes had severe microcornea. All the 3 eyes that were left aphakic in this study had a small white to white diameter. Postoperative corneal edema was noted in 18% of cases in this series. This suggests that smaller eyes are at a greater risk of complications and endothelial damage.
Similarly Chaurasia et al. reported outcomes of cataract surgery in 26 eyes with coloboma and cataract.[3] They noted more complications in patients undergoing M-SICS/ECCE/ICCE compared to the eyes in whom PE was performed. It is also interesting to note that 5 out of 8 eyes with hard cataract that were left aphakic had a complicated surgery with posterior capsule rent (PCR) and required anterior vitrectomy, possibly due to a harder grade of cataract. This further reflects that more complications are encountered in the management of hard cataracts in small eyes.
In a recently published series of 8 cases by Khokhar et al.,[6] a modified PE technique using sclero-corneal tunnel for microcornea with CR coloboma and hard cataracts was described; 3 eyes in their series with severe grade microcornea had PCR and were left aphakic. It is relevant to note that 4 of the 8 eyes in their study were reported to have persistent corneal edema in the early postoperative period.
All the above studies point towards the fact that cornea-related complications, intraoperative difficulties, and posterior capsular dehiscence need anterior vitrectomy, and the inability to implant an IOL appears to be higher in eyes with hard cataracts and small cornea when approached with the corneo-scleral route. The existent case series on the management of cataracts in eyes with microcornea and coloboma remain focused on the outcomes in the early postoperative period but with little information on the long-term outcome of cases which incurred complications and were left aphakic in their series.
Although the above studies have included the cases of microcornea with hard cataracts, they were not carried out exclusively in the extreme cases of microcornea and, therefore, the outcome and management in this special subset remain unanswered.
However, we consider corneal diameter to be an important finding, our retrospective series represent cases with severe grade (<8 mm) of microcornea only, as PE can safely be performed with IOL insertion in less severe grade of microcornea. We believe that corneal measurements can help in deciding a possibly safe approach for the represented subset of eyes.
In our study, we included only those cases which had very severe microcornea (mean horizontal diameter 6.7 mm) with hyper dense nucleus (brunescent cataract). The eyes having severe or very severe grade of microcornea usually have been observed to have flatter and thicker corneas with a very shallow anterior chamber and a bulky nucleus.[7] Phacoemulsification in these eyes could lead to severe damage to corneal endothelium and also frequent wound burns resulting from the use of excessive phaco-power in relatively shallow anterior chamber.[9] To perform SICS or ECCE in these eyes, a minimum incision of 7 to 9 mm should be made, which is not possible considering the anatomical restraints, i.e. the overall corneal diameter lesser than 7 mm. This led us to attempt an alternate method for removal of cataract using the pars-plana approach by the use of phaco-fragmatome. Since many of the patients in our series were one eyed, we were more desperate to intervene in these cases with a more pragmatic approach.
We considered posterior approach via pars plana in these cases, as we thought that the limbal approach would lead to irreversible damage to the cornea considering the intraoperative struggle. Hence, we refrained from undertaking an anterior limbal approach dreading complications in an already visually challenged individual.
Advantages of pars planar approach
The surgical procedure-related advantages of adopting a pars-plana approach in this special subset of patients include better intraoperative stability of the globe, minimal endothelial damage,[10,11,12] large room for intraoperative manipulation, minimal iris manipulation, and lower incidence of postoperative inflammation. (Image-4)
The trans-planar procedure also safeguards against early postoperative spikes in the IOP and toxic anterior segment syndrome (TASS), often associated with excessive use and inability to completely remove ocular visco-elastic devices (OVD) in these cases.[13]
All eyes in our series had clear cornea on the first day following surgery, with minimal anterior chamber reaction. Only one eye had mild corneal edema which resolved by the first postoperative week. None of the eyes had a raised IOP above 21 mmHg and none had severe postoperative inflammation.
The functional improvement in eyes with microcornea and CR coloboma depends mainly upon the extent of the coloboma and associated with optic nerve involvement. In the cases where the disc and macula lie within the colobomatous area, the functional outcomes remain mostly poor.
Out of the 30 eyes that were operated upon, 21 eyes showed subjective improvement in vision. Importantly, 11 of these 21 eyes showed an alleviation out of the near blindness grade, 5 eyes improved to the level of profound visual impairment, 5 eyes stepped up to the grade of severe visual impairment, and 1 eye improved to the level of moderate visual impairment [Table 3]. The visual improvement in our series was comparable to the existing studies.[3,4,5]
Having discussed the outcomes of anterior approach as provided by Chaurasiya et al. and kholkar et al., it becomes clear that the frequency of incurring anterior segment complication with the pars-plana route remains substantially less. However, in the absence of a comparative arm in our study and lack of long-term outcomes for the anterior approach in the existent literature, it becomes difficult to substantiate the same.
Although the pars-plana approach seems to offer several benefits, yet there are a few difficulties that a surgeon could face while performing this procedure. Smaller corneal diameter in these eyes often leads to closely placed sclerostomy ports, which in turn leads to crowding of instruments and frequently displaces the noncontact viewing system during manipulations, especially during vertical orientation of instruments when approaching the posterior pole.
The small pupil in these eyes frequently poses a challenge for adequately viewing the fundus periphery. In 9 eyes, we encountered axial myopia with associated posterior staphyloma. The combination of closely placed ports and obstruction by the non-contact viewing system in association with posterior staphyloma made it nearly impossible in some cases to access the posterior pole for induction of posterior vitreous detachment. This issue can be partly overcome by removal of cannula and direct introduction of the vitrector through sclerostomy port, thus providing an additional 1 mm to 1.5 mm length for effective manipulation and accessibility of posterior pole.
Laser to the coloboma margin intraoperatively was not done in all cases; considering that an estimated 23–42% of the eyes with coloboma have a risk of developing RD, that too being more prevalent in younger individuals.[14,15,16] Even though retrospective studies have conformed the beneficial effects of laser in decreasing the chances of RD, however, the benefits are most in the suspected high-risk group, as not all eyes develop RD.[14,15,16] There are no established guidelines or consensus for identifying high-risk individuals; hence, performing prophylactic laser barrage in all cases of coloboma might not be necessary.
In our series, we refrained from applying retinopexy to the coloboma margin considering the damage to the residual functional macula, in patients with extensive chorioretinal coloboma. We did thought about the benefits of retinopexy, but considering the absence of ICM defect (ICMD) in 14 eyes and inability to find any break at the coloboma margin in the remaining 16 eyes with ICMD, all of whom were above 50 years of age were deterrent of performing an additional retinopexy procedure, the associated risks of which cannot be overlooked. However, in the post-operative period, the patients did undergo a sequential OCT examination to rule out the possibility of dehiscence in the locus minoris Resistencia warranting laser barrage.
Retinal breaks and subsequent RD remain a pertinent intraoperative concern as for any other vitreoretinal procedure. In our series, retinal breaks with RD were detected in 2 cases and 1 case developed RD during the early postoperative period, all of which were independent on an associated ICM break. All the cases where managed successfully by doing a thorough vitrectomy and fluid air exchange, followed by laser photocoagulation to the breaks and instillation of SO tamponade. SO removal was done in all the eyes after 3 months and retina remained attached in all cases until the last follow-up visit.
The vision was represented as CDVA; comparison of vision gained to that of the expected potential acuity is not possible since all the patients had congenital chorioretinal coloboma of various grades with variable macular involvement.
The reason for suboptimal vision recovery in these cases has been attributed to the extensive chorioretinal coloboma. The few patients incurring intraoperative complications had visual gain comparable to the rest; however, these still remained limited due to their existing anatomical malformation. The median visual acuity in these four eyes who required additional procedure for RD was 1.7 log MAR, this was comparable to the rest of the eyes in the present study.
Being a new technique, our primary outcomes remains centered on the visual outcomes and time to visual rehabilitation. Since there is no comparative arm, it is not possible to compare the CDVA; this has been mentioned as the limitation of the study
Limitations
Our study is a retrospective, non-comparative case series, and the absence of a control arm in this study makes it difficult to provide conclusive evidence with regard to the superiority of this procedure over the sclero-corneal approach. However, since we took only cases that the anterior segment surgeons refused to operate, it was difficultly for us to have a control group.
As mentioned earlier, we could not obtain specular counts, but we assume that there would be less endothelial cell loss with our technique than PE or ECCE in these eyes as the PF was performed in the vitreous cavity, quite away from corneal endothelium.
Strenghts
To the best of our knowledge, this study is one of the largest interventional case series, carried out in the cases of very severe grade of microcornea with coloboma and dense cataracts. Till date, our study provides a long follow-up duration, ranging from 12 to 24 months and describes early as well as late procedural outcomes of an alternate, pars-plana approach for the management of hard cataracts in the eyes with extreme microcornea and CR coloboma.
Conclusion
Pars-plana approach with PF is an effective technique having encouraging outcomes when used in the management of hyperdense cataract with severe microcornea and coloboma, comparing this with the current available standard of care is needed.
Patient consent
The patients/patients' legal guardian consented for the interventions performed and authorized the use of their images.
Authorship
All authors attest that they meet the current ICMJE criteria for authorship.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Mann . Developmental Abnormalities of the Eye. 2nd ed. London: B.M.A; 1958. [Google Scholar]
- 2.Bermejo F, Martinez-Frias ML. Congenital eye malformations: Clinical–epidemiological analysis of 1, 124,654 consecutive births in Spain. Am J Med Genet. 1998;75:497–504. [PubMed] [Google Scholar]
- 3.Chaurasia S, Ramappa M, Sangwan VS. Cataract surgery in eyes with congenital iridolenticular choroidal coloboma. Br J Ophthalmol. 2012;96:138e140. doi: 10.1136/bjophthalmol-2011-300233. [DOI] [PubMed] [Google Scholar]
- 4.Khokhar S, Gupta S, Kusumesh R, Kumar G. Outcomes of phacoemulsification in eyes with congenital choroidal coloboma. Graefes Arch Clin Exp Ophthalmol. 2013;251:2489–90. doi: 10.1007/s00417-013-2397-1. [DOI] [PubMed] [Google Scholar]
- 5.Khokhar S, Gupta S, Tewari R, Agarwal R. Scleral tunnel phacoemulsification: Approach for eyes with severe microcornea. Indian J Ophthalmol. 2018;64:320–2. doi: 10.4103/0301-4738.182949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Colenbrander A. Visual Standards aspects and ranges of vision loss with emphasis on population surveys. 2002 [Google Scholar]
- 7.Long-Tern corneal endothelial cell loss after cataract surgery. Results of a randomized controlled trial. Oxford Cataract Treatment and Evaluation Team (OCTET) Arch Ophthalmol. 1986;104:1170–5. [PubMed] [Google Scholar]
- 8.Use of a grading system in the evaluation of complications in a randomised controlled trial on cataract surgery. Oxford Cataract Treatment and Evaluation Team (OCTET) Br J Ophthalmol. 1986;70:411–41. doi: 10.1136/bjo.70.6.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mohamed A, Chaurasia S, Ramappa M, Jalali S. Corneal thickness in uveal coloboma with microcornea. Eye. 2017;32:586–9. doi: 10.1038/eye.2017.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stănilă DM, Florea AM, Stănilă A, Panga AA. Endothelial cells loss to the hyperopic patients during phacoemulsification. Rom J Ophthalmol. 2017;61:256–60. [PMC free article] [PubMed] [Google Scholar]
- 11.Mittl RN, Koester CJ, Kates MR, Wilkes E. Endothelial cell counts following pars plana vitrectomy in pseudophakic and aphakic eyes. Ophthalmic Surg. 1989;20:13–6. [PubMed] [Google Scholar]
- 12.Wang H, Li L, Li X. The effect of extracting lens on damage of corneal endothelium in vitreous surgery. Zhonghua Yan Ke Za Zhi. 1999;35:110–2. [PubMed] [Google Scholar]
- 13.Althomali T. Viscoelastic substance in prefilled syringe as an etiology of toxic anterior segment syndrome. Cutan Ocul Toxicol. 2015;35:237–41. doi: 10.3109/15569527.2015.1082579. [DOI] [PubMed] [Google Scholar]
- 14.Gopal L, Khan B, Jain S, Prakash V. A Clinical and Optical Coherence Tomography Study of the Margins of Choroidal Colobomas. 2019 doi: 10.1016/j.ophtha.2006.06.048. [DOI] [PubMed] [Google Scholar]
- 15.Jesberg D, Schepens C. Retinal detachment associated with coloboma of the choroid. Arch Ophthalmol. 1961;65:163–73. doi: 10.1001/archopht.1961.01840020165003. [DOI] [PubMed] [Google Scholar]
- 16.Schepens CL. Retinal Detachment and Allied Diseases. Vol. 2. Philadelphia: WB Saunders; 1983. pp. 615–7. [Google Scholar]