Abstract
Since 2005, coccidioidomycosis has increased among inmates at a California prison. Our initial investigation found an incidence of 3,323 cases/100,000 persons. Black race, age ≥41 years, and residence on Yard C were significantly associated with coccidioidomycosis (p < .05). Inmates at this prison have continued to be at risk for coccidioidomycosis.
Keywords: coccidioidomycosis, Coccidioides, prisons, California
Introduction
Coccidioidomycosis is acquired through inhalation of Coccidioides species, a fungus endemic in soil of the San Joaquin Valley of California. Although infections are often asymptomatic or mild, persons with diabetes or compromised immune systems and those of certain racial/ethnic backgrounds are at increased risk for severe or disseminated disease (Chiller, Galgiani, & Stevens, 2003; Rosenstein et al., 2001). During 1998 to 2011, reported coccidioidomycosis cases increased in California, although reasons for the increase are unknown (Centers for Disease Control and Prevention [CDC], 2013). Notably, coccidioidomycosis among state prison inmates in endemic Fresno and Kings Counties increased in 2005 and subsequent years (California Correctional Health Care Services [CCHCS], 2012; Pappagianis, 2007). In fall 2005, medical staff at Pleasant Valley State Prison (PVSP), an all men’s state prison in Fresno County less than 10 miles from the city of Coalinga, noted an increase in coccidioidomycosis among inmates. CCHCS invited the California Department of Public Health [CDPH] to investigate during December 2005 to January 2006. We describe this initial investigation.
Method
A prison case was defined as a PVSP inmate with symptom onset during 2005, clinically compatible disease, and serologic evidence of coccidioidomycosis (CDC, 1996). We estimated PVSP incidence in 2005 by using the number of 2005 cases and the PVSP population on June 30, 2005. We calculated coccidioidomycosis incidence in Coalinga and Fresno County by using the reported number of noninmate cases with clinical and serologic evidence of infection (CDC, 1996) and the 2005 California Department of Finance (2012) population estimates, excluding PVSP population. We received employee population estimates and illness information from the California Department of Corrections and Rehabilitation Office of Risk Management.
We abstracted case patients’ medical charts for demographic characteristics, medical conditions, symptoms, diagnostic testing, treatment, and outcome. Records were unavailable for those released or transferred to another prison. We used logistic regression to compare race–ethnicity among inmates with disseminated coccidioidomycosis to those with disease confined to the lungs.
To assess risk factors, we conducted a retrospective cohort study using the PVSP population on January 19, 2006. We collected age, self-reported race/ethnicity, housing yard, and custody level (from least to most supervised) from a prison administrative database and analyzed data for association with infection. We also reviewed data summarizing the percentage of inmates from each housing yard confined indoors on lockdown each week during 2005. PVSP has four main yards A–D, enclosed areas where inmates reside and engage in outdoor recreation. Yard C housed inmates with special medical needs including diabetes and chronic respiratory diseases. We used SAS® Version 9.0 (SAS Institute, Cary, NC) to identify variables significantly associated with coccidioidomycosis on χ2 bivariate analysis in a forward logistic regression model. Statistical significance was defined as p < .05.
Results
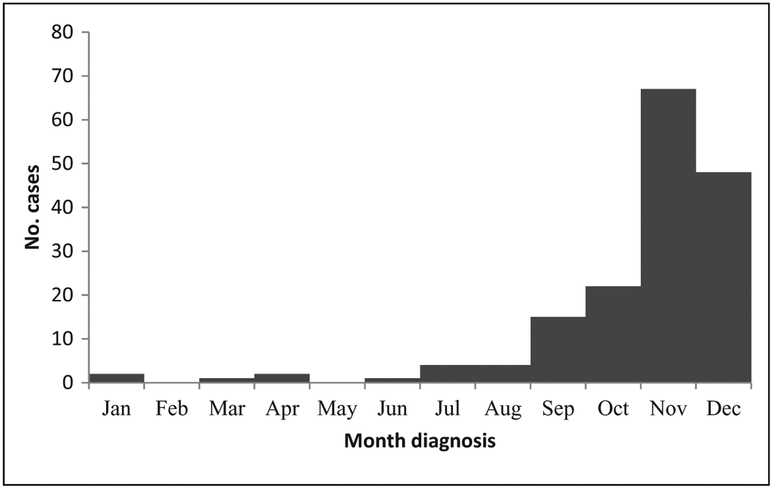
During 2005, 241 PVSP inmates experienced illness, 36 did not meet the case definition, and 39 had been transferred. Among 166 inmates who had medical records and met the case definition, 152 (92%) were diagnosed during September to December 2005 (see Figure 1). Coccidioidomycosis incidence at PVSP during 2005 was 3,323 cases/100,000 persons, 27 times higher than the incidence in Coalinga (121 cases/100,000 persons) and 415 times higher than the incidence in Fresno County (8 cases/100,000 persons). The 2005 incidence of coccidioidomycosis among the 1,200 PVSP staff was 3,083 cases/100,000 persons, or 25 times higher than the incidence in Coalinga.
Figure 1.
Epidemic curve by month of coccidioidomycosis diagnosis, Pleasant Valley State Prison, California, 2005 (N = 166).
As shown in Table 1, median age was 40 years (range 18 to 71 years); median age of the general PVSP inmate population was 36 years (range 18 to 86 years). Fifty-eight (35%) were Hispanic, 55 (33%) were Black, and 41 (25%) were White. Many resided on Yard C (76, 46%). Conditions included hepatitis C (39, 23%), asthma (26, 16%), and diabetes (18, 11%). Symptoms included cough, fever, and night sweats; median symptom duration was 10 days (range 1 to 270 days). Most (152, 92%) had a positive IgM latex agglutination test; the remainder had rising coccidioidal IgG titer by complement fixation. Of 108 patients with chest radiograph, 103 had an infiltrate consistent with coccidioidomycosis. One hundred forty-one (85%) patients received antifungal medication. Of 11 patients with disseminated disease, 7 were White, 2 were Hispanic, 1 was Black, and 1 was missing race/ethnicity data. Of these 11, 2 had coccidioidomycosis meningitis; none were immunocompromised, and none died. Inmates with disseminated cocci did not differ significantly by race/ethnicity from those with pulmonary disease.
Table 1.
Characteristics of Patients With Diagnosed Coccidioidomycosis at Pleasant Valley State Prison, California, 2005.
| Characteristic | N (%) |
|---|---|
| Median age, years (range) | 40 (18–71) |
| Race/ethnicity | |
| Hispanic | 58 (35) |
| Black | 55 (33) |
| White | 41 (25) |
| Other | 8 (5) |
| Unknown | 4 (2) |
| Residence yard | |
| A | 25 (15) |
| B | 18 (11) |
| C | 76 (46) |
| D | 39 (23) |
| Other/unknown | 8 (5) |
| Symptoms | |
| Cough | 119 (72) |
| Fever | 78 (47) |
| Night sweats | 77 (46) |
| Infiltrate on chest radiograph | 103 (62) |
| Disseminated infection | 11 (7) |
| Hospitalized | 29 (17) |
| Deaths | 4 (2) |
Note. N = 166.
Twenty-nine (17%) patients were hospitalized and 4 (2%) died. On bivariate analyses, patients with diabetes were significantly more likely to be hospitalized than patients without diabetes (50% vs. 14%, risk ratio [RR] 3.7, and confidence interval [CI] = [2.0, 6.9]). Patients with a chest radiograph infiltrate were more likely to be hospitalized than patients without an infiltrate (23% vs. 8%, RR 2.9, and CI [1.2, 7.3]).
The cohort study comprised 4,885 inmates; 160 inmates with coccidioidomycosis were included. Data were unavailable for 6 inmates with coccidioidomycosis who were not included. On bivariate analysis, Blacks were 2 times more likely to have coccidioidomycosis, compared with Whites (RR 2.0, CI [1.3, 2.9], and p < .001). Persons aged ≥41 years were 1.6 times more likely to be ill, compared with persons aged ≤40 (RR 1.6, CI [1.2, 2.1], and p < .01). Lastly, Yard C residents were 2.7 times more likely to have coccidioidomycosis, compared with residents on other yards (RR 2.7; CI [2.0, 3.7]; p < .0001; see Table 2).
Table 2.
Attack Rates and Relative Risks for Coccidioidomycosis, Pleasant Valley State Prison, California, 2005.
| Characteristic | Population at Risk | Number Ill | Attack Rate (Per 1,000) | RR [95% CI] | p |
|---|---|---|---|---|---|
| Total | 4,885 | 160 | |||
| Age (years) | |||||
| ≤40 | 3,036 | 82 | 27 | Reference | |
| ≥41a | 1,849 | 78 | 42 | 1.6 [1.2, 2.1] | .003 |
| Race/ethnicity | |||||
| White | 1,453 | 39 | 27 | Reference | |
| Hispanic | 2,039 | 58 | 28 | 1.1 [0.7, 1.6] | .8 |
| Blacka | 1,047 | 55 | 53 | 2.0 [1.3, 2.9] | .0009 |
| Other | 346 | 8 | 23 | 0.9 [0.4, 1.8] | .7 |
| Residence yardb | |||||
| A | 1,069 | 25 | 23 | 0.7 [0.4, 1.0] | .05 |
| B | 1,118 | 17 | 15 | 0.4 [0.2, 0.7] | .0002 |
| Ca | 1,115 | 71 | 64 | 2.7 [2.0, 3.7] | <.0001 |
| D | 1,126 | 39 | 35 | 1.1 [0.8, 1.5] | .7 |
Note. CI = confidence interval; RR = risk ratio.
Variables remained statistically significant in multivariate model.
Reference group for residence yard was residence on all other housing areas.
Inmates on Yards C and D were not on lockdown during September to December 2005; inmates on Yards A and B were on lockdown for 5 to 10 weeks during that time. In multivariate analysis, Black race/ethnicity, age ≥41 years, and residence on Yard C were significantly associated with coccidioidomycosis adjusted odds ratio (aOR 1.9, 1.5, and 2.6, respectively, p < .05 for all).
Conclusions
At the time of this investigation, the rate of coccidioidomycosis among PVSP inmates was substantially higher than the rates in Coalinga and Fresno County, but reasons for the higher rate are unknown. Substantial morbidity occurred: 62% had infiltrate suggestive of pneumonia, 17% were hospitalized, 7% had disseminated disease, and 2% died.
While our investigation did not find a higher risk for disseminated coccidioidomycosis for inmates who were Black as compared to those who were White or Hispanic, it did find a higher risk for primary pulmonary coccidioidomycosis among Blacks. The attack rate in Blacks was 53/1,000, substantially higher than the attack rate in Whites and Hispanics. Of reported cases in California since 2003 with complete race/ethnicity data, the highest rates have occurred among Blacks (CDPH, 2011). Although Black race is a known risk factor for disseminated coccidioidomycosis (Crum, Lederman, Stafford, Parrish, & Wallace, 2004; Rosenstein et al., 2001), whether Black race is also a risk factor for primary pulmonary disease is currently unknown. Analysis of 2011 coccidioidomycosis data from two California prisons similarly reported increased risk of primary pulmonary coccidioidomycosis in Blacks ages 40 years and older (Wheeler, Lucas, & Mohle-Boetani, 2015). More research might be needed to determine whether Blacks or other racial/ethnic groups are at increased risk for primary pulmonary coccidioidomycosis.
Lockdown data indicated inmates on Yards C and D had more opportunities than inmates on other yards to be outdoors exposed to dust during the months when most infections occurred. Further, Yard C housed inmates with special medical needs; therefore, they might have had increased risk for infection overall.
Several limitations existed. Data regarding comorbid conditions were available for infected inmates but not for others. We were unable to examine the hypothesis that older persons might be at increased risk for coccidioidomycosis due to comorbidities. We did not explore outdoor exposures that might increase risk for infection. Lastly, we were unable to examine the effect of turnover in the PVSP population. Inmates with longer stays may have had more opportunities to be exposed to coccidioidomycosis.
We describe an investigation among California inmates in 2005 to 2006. Since this investigation, CCHCS has educated staff and inmates about coccidioidomycosis, introduced dust control measures, and relocated inmates with medical conditions that predisposed them to complications (California Department of Corrections and Rehabilitation, 2007). However, coccidioidomycosis has continued to be a pertinent issue in California and among inmates in the endemic area. Rates have increased in California and peaked at 13.9 cases/100,000 in 2011 (CDPH, 2014). At PVSP, the rate of coccidioidomycosis also increased and averaged 7,011 cases/100,000 during 2006 to 2010 (CCHCS Public Health and Quality Management Units, 2012). Because of this continued burden, in 2013, CCHCS and CDPH invited CDC to investigate anew and evaluate additional strategies to reduce coccidioidomycosis-associated morbidity (Purfield, 2014). Based on recommendations from this recent CDC investigation, skin testing for coccidioidomycosis immune status was administered in January 2015 to identify nonimmune inmates who are medically restricted from living at PVSP and nearby Avenal State Prison (Thompson, 2015).
Acknowledgments
We thank the staff at the local health department and the warden and staff of the prison for their contributions to this investigation.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Declaration of Conflicting Interests
The authors disclosed no conflicts of interest with respect to the research, authorship, or publication of this article. For information about JCHC’s disclosure policy, please see the Self-Study Program.
References
- California Correctional Health Care Services Public Health and Quality Management Units. (2012). Coccidioidomycosis in California’s adult prisons 2006–2010. Retrieved from http://consumer-justice.org/wp-content/uploads/2013/10/12.10.12-CDCR-Cocci-Report.pdf
- California Department of Corrections and Rehabilitation. (2007). Exclusion of inmate-patients susceptible to coccidioidomycosis from highest risk (hyperendemic) area institutions. Retrieved from http://consumer-justice.org/wp-content/uploads/2013/10/CDC-Memo-11-20-2007.pdf
- California Department of Finance. (2012). E-4 Population estimates for cities, counties, and the state, 2001–2010, with 2000 & 2010 census counts. Retrieved from http://www.dof.ca.gov/Forecasting/Demographics/Estimates/E-4/2001-10/
- California Department of Public Health. (2011). Coccidioidomycosis yearly summary report, 2001–2010. Retrieved from https://www.cdph.ca.gov/data/statistics/Documents/YearlySummaryReportsofSelectedGeneralCommDiseasesinCA2001-2010.pdf
- California Department of Public Health. (2014). Epidemiologic summary of coccidioidomycosis in California, 2009–2012. Retrieved from http://www.cdph.ca.gov/programs/sss/Documents/CocciEpiSummary09-12.pdf
- Centers for Disease Control and Prevention. (1996). National Notifiable Diseases Surveillance System coccidioidomycosis case definition. Retrieved from http://wwwn.cdc.gov/NNDSS/script/casedef.aspx?CondYrID=641&DatePub=1/1/199612:00:00AM
- Centers for Disease Control and Prevention. (2013). Increase in reported coccidioidomycosis—United States, 1998–2011. Morbidity and Mortality Weekly Report, 2, 217–221. [PMC free article] [PubMed] [Google Scholar]
- Chiller TM, Galgiani JN, & Stevens DA (2003). Coccidioidomycosis. Infectious Disease Clinics of North America, 17, 41–57. [DOI] [PubMed] [Google Scholar]
- Crum NF, Lederman ER, Stafford CM, Parrish JS, & Wallace MR (2004). Coccidioidomycosis: A descriptive survey of a reemerging disease. Clinical characteristics and current controversies. Medicine, 83, 149–175. [DOI] [PubMed] [Google Scholar]
- Pappagianis D (2007). Coccidioidomycosis in California state correctional institutions. Annals of the New York Academy of Sciences, 1111, 103–111. [DOI] [PubMed] [Google Scholar]
- Purfield A (2014). Epi-Aid 2013-050 Trip Report: Coccidioidomycosis in Pleasant Valley State Prison and Avenal State Prison in the California Central Valley. Retrieved from http://www.prisonlaw.com/pdfs/2014CDCValleyFeverReport.pdf
- Rosenstein NE, Emery KW, Werner SB, Kao A, Johnson R, Rogers D, … Hajjeh RA (2001). Risk factors for severe pulmonary and disseminated coccidioidomycosis: Kern County, California, 1995–1996. Clinical Infectious Diseases, 32, 708–715. [DOI] [PubMed] [Google Scholar]
- Thompson D (2015, January 11). California spends $5 M to screen inmates for valley fever. Southern California Public Radio. Retrieved from http://www.scpr.org/news/2015/01/11/49218/california-spends-5m-to-screen-inmates-for-valley/ [Google Scholar]
- Wheeler C, Lucas KD, & Mohle-Boetani JC (2015). Rates and risk factors for coccidioidomycosis among prison inmates, California, USA, 2011. Emerging Infectious Diseases, 21, 70–75. [DOI] [PMC free article] [PubMed] [Google Scholar]