Abstract
Background:
Calcaneal fractures are associated with substantial morbidity and socioeconomic impact, frequently leading to limited functional outcome and high economic costs. The Oxford foot model (OFM) has been reported as a valid addition to the biomechanical examination of the foot. The aim of our study was to analyze the gait of patients after operative repair of a calcaneal fracture in relation to functional outcome and radiographic findings.
Methods:
Thirteen patients with a calcaneal fracture underwent gait analysis with OFM at a minimum of six months after open surgery. Intersegmental range of motion was measured during gait. Results were compared with those of healthy subjects and those of patients who had undergone subtalar arthrodesis. Patient-reported questionnaires and radiographic images were also evaluated.
Results:
The range of motion between the hindfoot and the tibia in the push-off phase in the transverse plane was significantly correlated with the clinical outcome as reported by patients based on the Foot and Ankle Disability Index (FADI) (r2 = 0.51; p < 0.001) and the Short Form (SF)-36 physical component summary score (r2 = 0.52; p < 0.001). We found a significant correlation between the step-off in the subtalar joint as measured on postoperative computed tomography (CT) and range of motion (r2 = −0.74; p = 0.004). The step-off was also correlated with the patient-reported outcome questionnaire FADI (r2 = −0.76; p = 0.003) and the SF-36 physical component summary score (r2 = −0.78; p = 0.002).
Conclusions:
This study demonstrated that the subtalar joint range of motion of patients after a calcaneal fracture was related both to the quality of the reduction of the subtalar joint as evaluated on postoperative CT scans and patient-reported functional outcome.
Level of Evidence:
Therapeutic Level III. See Instructions for Authors for a complete description of levels of evidence.
Calcaneal fractures comprise 2% of all fractures and 4% of all foot and ankle fractures1,2. Three-quarters of calcaneal fractures are intra-articular, with the majority involving the major weight-bearing posterior facet3,4. Intra-articular calcaneal fractures can be disabling injuries with a high economic and social impact5,6. Functional outcomes after open reduction and internal fixation (ORIF) can be variable1,2. Outcome evaluations after the treatment of calcaneal fractures include the use of radiographic findings, physical examination, and questionnaires.
The computed tomography (CT) scan has been the most important diagnostic tool for the evaluation of calcaneal fractures, but the association between the restoration of joint congruency, calcaneal axes, and functional outcome parameters is inconsistent2. Less is known about the biomechanical changes after calcaneal fractures. Motion capture analysis of gait may provide a link between the evaluation of anatomic parameters and parameters reported by patients regarding functional outcome7,8. Kingwell et al. noted that the amount of subtalar joint motion after calcaneal fracture, measured on physical examination, is significantly related to patient satisfaction at two years, regardless of the method of treatment9. Direct, noninvasive measurement of motion in the subtalar axis is difficult to establish, although currently, gait analysis of the foot and ankle can be performed with reliable results using the Oxford foot model (OFM)10,11. This four-segment foot model can be used to measure intersegmental motions during gait that represent the motion in the subtalar joint12-15. Previous studies of gait analysis of patients after calcaneal fractures have shown mixed results; some studies have demonstrated abnormal gait compared with that of healthy subjects16,17, while a study by Hetsroni et al. found no abnormal gait in patients after treatment for calcaneal fractures18.
To our knowledge, no data linking radiographic results, functional outcome, and gait analysis previously have been presented. Therefore, the aim of the current prospective study was to analyze the gait of patients following a displaced intra-articular calcaneal fracture and to correlate this with patient-reported functional outcomes and imaging-based postoperative evaluation of congruency and axis of the subtalar joint. Our hypothesis was that a lower patient-reported functional outcome is influenced by an abnormal range of motion between the hindfoot and the tibia during gait and by the postoperative congruency and alignment of the subtalar joint. Because clinical studies involving the use of the OFM are limited, and range of motion in the subtalar joint cannot be directly measured, we compared results of the calcaneal fracture patient cohort with those of healthy subjects and patients after subtalar arthrodesis.
Materials and Methods
Study Population
Thirteen patients (thirteen feet) treated for a calcaneal fracture with ORIF, with an extended L-shaped lateral incision for plate-screw fixation, were recruited at a minimum of six months after surgery. Most postsurgical progress takes place between the first three and six months after surgery19,20. Exclusion criteria were concomitant surgery for fractures or pre-existent abnormalities of the lower extremities, neurotrauma, spinal or neurological injury, and pathologic fractures. Patients were between the ages of twenty-five and eighty-one years21,22.
Results were compared with those of seventeen healthy subjects (seven of whom were measured bilaterally to compensate for foot dominance, for a total of twenty-four feet) and eight patients (eight feet) who had undergone subtalar arthrodesis at a minimum of six months previously. Exclusion criteria for these patients were identical to those of the calcaneal fracture group. The subtalar arthrodesis group was included because the OFM is not able to measure the range of motion in the subtalar joint directly. The range of motion in the subtalar joint in patients with a subtalar arthrodesis should be 0°, so gait analysis results can give more insight into the motion in the adjacent joints and the error margin of the skin; this group can also be used as a control group.
For the calcaneal fracture and subtalar arthrodesis groups, the following were collected: baseline data from the case record form and radiographic findings directly postoperatively. In addition, patient-reported outcome questionnaires—including the American Orthopaedic Foot & Ankle Society (AOFAS) Ankle-Hindfoot Scale, the Foot and Ankle Disability Index (FADI), the Short Form (SF)-36 score, and the horizontal visual analog scale (VAS) for pain (ranging from 0 for no pain to 10 for very severe pain)—were administered and a physical examination was performed at the time of the OFM gait analysis.
All subjects provided signed informed consent. This study was approved by the medical ethics committee (METC number 10-3-072).
Equipment
Motion capture was conducted using the Vicon MX3 system (Vicon Motion Systems, Oxford, United Kingdom). The Vicon system comprises eight cameras (six MX3 and two T20, running at 200 Hz) connected to a computer for the detection of markers that were placed, using regular double-sided tape, on the skin of both lower extremities of the subjects at specific landmarks, according to the guidelines of the OFM (see Appendix). A subject walking with the markers at the movement laboratory is shown in Video 1 (online).
Video 1.
A subject walking with the markers at the movement laboratory.
Gait Analysis Protocol
Before gait analysis, the following characteristics were measured: height, weight, body mass index, knee and ankle width (measured as the distance between the lateral and medial condyles of the knee and the lateral and medial malleoli of the ankle), and leg length (measured as the distance between markers for the anterior iliac spine and the medial malleolus). All measurements were made by one trained researcher. At least one static trial was performed with all forty-two markers, with the subjects in an anatomically neutral position. After calibrating the markers and calculating the subject-specific joint axes in the static trial, six markers were removed, according to the OFM protocol. At least eight proper recordings were made during barefoot walking in normal and slow speed after some practice trials. The data of one whole step were divided as two intervals: the first interval, or loading phase, consisted of the first 50% of the stance phase (initial contact to midstance); the second interval, or push-off phase, consisted of the last 50% (midstance to toe-off). A force plate was used to determine these phases during walking. Corrections of insufficient ankle and knee axes were made.
Radiographic Evaluation
Preoperative and postoperative radiographs and CT scans were evaluated by two independent observers, who were blinded to the gait analysis and outcomes data. Differences between these two observers were resolved by consensus. The following parameters were evaluated on radiographs: the Böhler angle23, the Gissane angle24, and the talocalcaneal angle. On CT scans, the calcaneal width, posterior-facet height, the subtalar joint axis in the sagittal and transverse planes, and step-off and gap in the posterior facet were noted. Fractures were classified by the Sanders classification4. Complete consolidation of the subtalar arthrodesis was confirmed using radiographic evaluation.
Data Analysis
A power analysis was performed to determine the number of patients needed for inclusion. The power was calculated using a sample-size calculation tool with two averages (alpha = 5%, and 1 – beta = 90%). It was estimated to include seven patients taking into account the known subtalar joint range of motion in a healthy person (and standard deviation) of 10° ± 3.5° and an expected decrease in subtalar range of motion to 5° ± 3.0° in patients after surgery for a calcaneal fracture25,26. With an expected rate of missing data of 20%, the number of patients included in each group was nine. In the Vicon system, the speed and intersegmental range of motion were calculated between the hindfoot and the tibia and the tibia and the forefoot in the frontal, sagittal, and transverse planes (representing, respectively, abduction-adduction, flexion-extension, and inversion-eversion) (see Appendix)27,28. These data were converted with MATLAB software (MathWorks, Natick, Massachusetts) and minimally comprised six randomly chosen trials (steps). With use of SPSS software (version 20; IBM, Armonk, New York), the kinematic characteristics were analyzed using descriptive statistics and the independent sample t test for differences; a p value of <0.05 was considered significant. The Pearson correlation test was used to find correlations.
Source of Funding
No external funding was received for this study.
Results
Patient Characteristics
Table I presents the baseline characteristics of the calcaneal fracture group. The mean age was 50.6 ± 15.8 years (range, twenty-five to eighty-one years). Gait analysis was performed after surgery at a median of two years (mean, twenty-three months; range, six to thirty-six months). For all but two patients, the trauma mechanism was a fall from a height resulting in a joint depression-type fracture, with the majority having a Sanders type-2 or 3 fracture. No complications regarding infection or revision of the primary surgery were noted for these patients. Full weight-bearing was allowed and supported by physiotherapy after three months, and seven of the thirteen patients had returned to work at six months. During gait analysis, the median pain score was 4 (range, 0 to 9).
TABLE I.
Patient Characteristics
| Group |
|||
| Calcaneal Fracture | Subtalar Arthrodesis | Healthy Control | |
| No. of subjects (no. of feet) | 13 (13) | 8 (8) | 17 (24) |
| Age* (yr) | 50.6 ± 15.8 (25-81) | 55.8 ± 8.0 (46-66) | 30.3 ± 14.8 (20-59) |
| No. (% of subjects) male | 13 (100) | 5 (63) | 15 (88) |
| No. (% of feet) right side | 3 (23) | 3 (38) | 17 (71) |
| Sanders classification (no.) | |||
| 2A | 1 | ||
| 2B | 8 | ||
| 3AB | 1 | ||
| 3BC | 2 | ||
| 4 | 1 | ||
| Height* (m) | 1.74 ± 0.08 (1.60-1.87) | 1.70 ± 0.13 (1.55-1.86) | 1.79 ± 0.06 (1.69-1.88) |
| Weight* (kg) | 77.8 ± 12.2 (51.0-90.0) | 86.0 ± 16.9 (66.0-110.0) | 73.91 ± 10.5 (62.0-91.0) |
| Body mass index* (kg/m2) | 25.5 ± 3.4 (19.9-31.1) | 29.6 ± 4.9 (20.7-35.1) | 22.9 ± 2.8 (19.4-29.1) |
| Knee width* (mm) | 98.2 ± 7.6 (84.0-112.0) | 109.1 ± 9.1 (94.0-126.0) | 104.3 ± 6.8 (93.0-120.0) |
| Ankle width* (mm) | 68.6 ± 3.9 (59.0-75.0) | 69.3 ± 6.3 (58.0-80.0) | 71.5 ± 10.8 (61.0-110.0) |
| Leg length* (mm) | 921.2 ± 49.2 (835.0-1002.0) | 862.5 ± 58.7 (765.0-935.0) | 901.2 ± 58.6 (765.0-970.0) |
Values are presented as the mean and the standard deviation with the range in parentheses.
Table I also lists the characteristics of the other two groups. The mean age of the arthrodesis group was 55.8 ± 8.0 years (range, forty-six to sixty-six years), and the mean age of the healthy control group was 30.3 ± 14.8 years (range, twenty to fifty-nine years). For the arthrodesis group, the OFM analysis took place at a median of thirty-nine months after surgery (range, sixteen to sixty-one months).
The mean AOFAS score in the calcaneal fracture group was 72 ± 15 (range, 33 to 93), the mean FADI score was 72 ± 15 (range, 31 to 96), and the mean SF-36 physical function score was 64 ± 22 (range, 15 to 95). The mean step-off on postoperative CT scan in these patients was 0.74 ± 0.74 mm (range, 0 to 2.30 mm), while the mean intra-articular gap of the posterior facet was 1.17 ± 0.96 mm (range, 0 to 3.20 mm). The mean subtalar axis measured on postoperative CT scans in the sagittal view was 43.2° ± 7.3° (range, 23° to 50°). The mean Böhler angle preoperatively was 3.9° (range, −17° to 26°) and postoperatively, 33° (range, 16° to 42°); and the mean Gissane angle preoperatively was 113° (range, 89° to 132°) and postoperatively, 115° (range, 98° to 140°).
Gait Analysis
Table II shows the speed and intersegmental range of motion. We found a significant difference in speed among the three groups. The calcaneal fracture group and the arthrodesis group had a lower speed during walking compared with the healthy control group (p = 0.004 and p < 0.0001, respectively). Because walking speed substantially affects foot and ankle kinematics, the results of the calcaneal fracture arthrodesis groups were also compared with those of the healthy control group when corrected for the effect of walking speed29. At slow walking speed, there was no significant difference between the healthy control group and the calcaneal fracture group (p = 0.533) or between the healthy control group and the arthrodesis group (p = 0.052).
TABLE II.
Speed and Intersegmental Range of Motion
| Group |
P Value |
|||||
| Calcaneal Fracture | Subtalar Arthrodesis | Control | Calcaneal Vs. Control | Arthrodesis Vs. Control | Arthrodesis Vs. Calcaneal | |
| Speed (m/s) | ||||||
| Normal | 0.94 | 0.73 | 1.18 | 0.004 | <0.0001 | 0.086 |
| Slow | 0.89 | 0.533 | 0.052 | |||
| Hindfoot-tibia loading phase* (deg) | ||||||
| Flexion-extension | 7.45 ± 2.95 (4.12-16.00) | 8.47 ± 1.42 (5.91-9.99) | 10.22 ± 2.92 (3.86-15.98) | 0.009 | 0.155 | 0.374 |
| Abduction-adduction | 11.13 ± 4.25 (5.94-18.56) | 8.56 ± 4.32 (5.62-17.04) | 12.00 ± 2.95 (7.22-18.09) | 0.468 | 0.017 | 0.198 |
| Inversion-eversion | 4.97 ± 1.86 (3.28-9.71) | 3.94 ± 0.83 (2.99-5.54) | 5.89 ± 1.78 (2.39-9.25) | 0.150 | <0.0001 | 0.100 |
| Hindfoot-tibia push-off phase* (deg) | ||||||
| Flexion-extension | 7.32 ± 2.78 (3.67-11.64) | 7.98 ± 2.52 (4.55-12.44) | 11.27 ± 3.31 (5.32-18.35) | 0.001 | 0.016 | 0.587 |
| Abduction-adduction | 12.83 ± 4.06 (6.86-21.83) | 15.81 ± 3.63 (11.39-23.06) | 10.39 ± 2.92 (5.68-16.96) | 0.042 | <0.0001 | 0.106 |
| Inversion-eversion | 6.96 ± 3.58 (1.95-13.03) | 4.01 ± 2.06 (2.09-8.65) | 9.15 ± 3.04 (4.60-16.37) | 0.057 | <0.0001 | 0.048 |
| Forefoot-tibia loading phase* (deg) | ||||||
| Flexion-extension | 12.72 ± 2.33 (8.21-17.06) | 11.91 ± 3.16 (8.52-17.87) | 14.78 ± 2.31 (9.54-20.05) | 0.014 | 0.009 | 0.505 |
| Abduction-adduction | 11.02 ± 4.09 (5.94-18.75) | 8.68 ± 4.50 (4.39-17.31) | 12.21 ± 3.81 (5.43-19.31) | 0.384 | 0.038 | 0.235 |
| Inversion-eversion | 7.73 ± 2.82 (5.17-11.48) | 6.07 ± 1.70 (3.47-8.31) | 9.97 ± 2.78 (5.08-15.87) | 0.017 | 0.001 | 0.082 |
| Forefoot-tibia push-off phase* (deg) | ||||||
| Flexion-eversion | 21.31 ± 7.45 (4.98-30.38) | 18.52 ± 5.13 (12.42-29.48) | 26.30 ± 5.64 (16.11-36.07) | 0.028 | 0.002 | 0.365 |
| Abduction-adduction | 9.96 ± 4.19 (4.87-21.38) | 13.56 ± 4.22 (7.04-20.79) | 10.50 ± 3.88 (5.57-21.43) | 0.695 | 0.068 | 0.072 |
| Inversion-eversion | 11.05 ± 4.64 (5.93-18.92) | 8.08 ± 1.66 (5.89-11.69) | 15.58 ± 3.40 (10.60-24.20) | 0.006 | <0.0001 | 0.051 |
Values are presented as the mean and the standard deviation with the range in parentheses.
The arthrodesis group had significantly less range of motion between the hindfoot and the tibia in the transverse plane (inversion-eversion) during the loading phase and the push-off phase (p < 0.0001 for both) compared with the healthy control group. Range of motion between the hindfoot and the tibia in the transverse plane during the push-off phase also differed significantly between the calcaneal fracture group and the arthrodesis group (p = 0.048). Patients with a calcaneal fracture did not differ significantly from healthy subjects in hindfoot-tibia range of motion in either the loading phase (p = 0.150) or the push-off phase (p = 0.057).
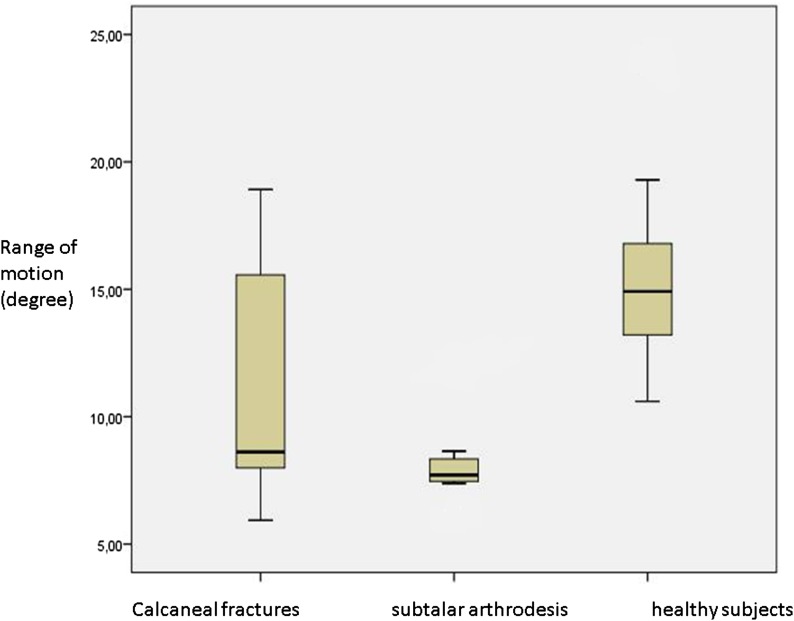
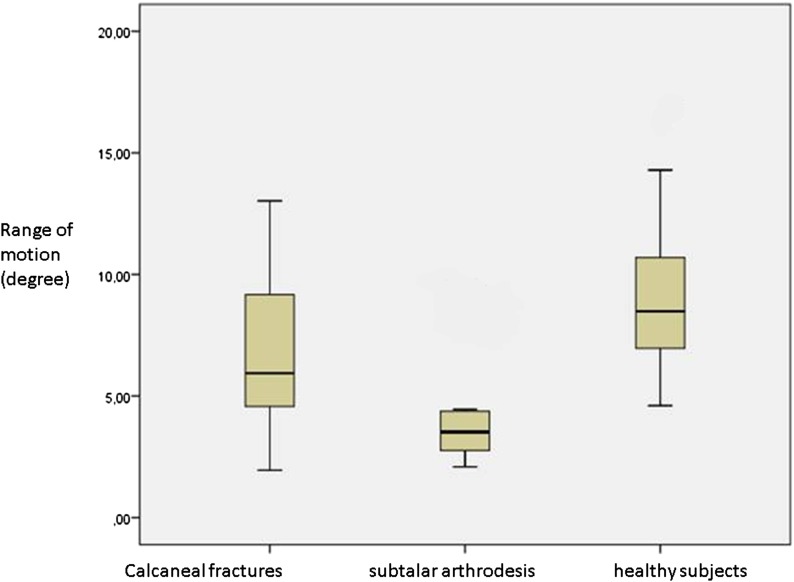
Regarding range of motion between the forefoot and the tibia in the transverse plane, the calcaneal fracture group had significantly less range of motion during both phases compared with the healthy control group (p = 0.017 for the loading phase, and p = 0.006 for the push-off phase). The arthrodesis group also had significantly less range of motion between the forefoot and the tibia in the transverse plane during both phases compared with the control group (p = 0.001 for the loading phase, and p < 0.0001 for the push-off phase). Interestingly, the variability in the inversion-eversion range of motion in the calcaneal fracture group was very high compared with that of the healthy control group and the arthrodesis group (Figs. 1 and 2).
Fig. 1.
Range of motion (inversion-eversion) between the forefoot and the tibia during the second phase of gait for the three groups (calcaneal fracture, subtalar arthrodesis, and healthy control), including mean and spread.
Fig. 2.
Range of motion (inversion-eversion) between the hindfoot and the tibia during the second phase of gait for the three groups (calcaneal fracture, subtalar arthrodesis, and healthy control), including mean and spread.
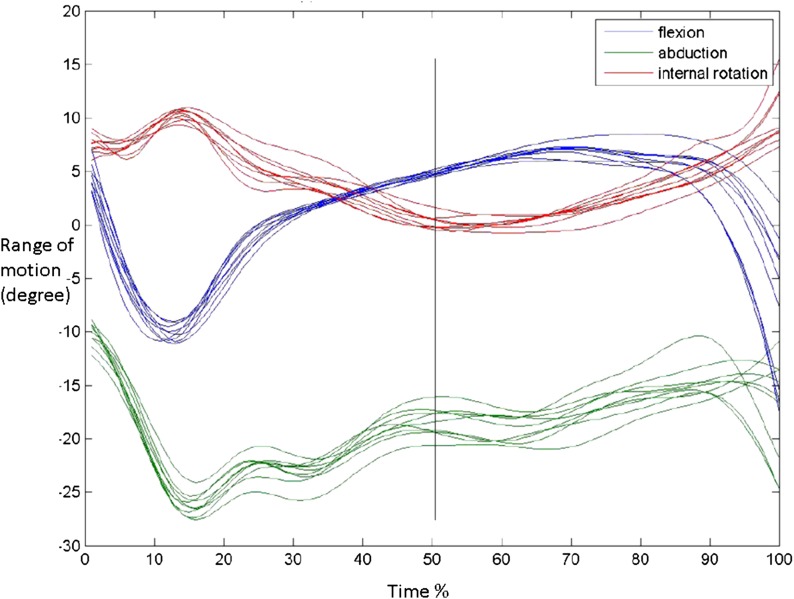
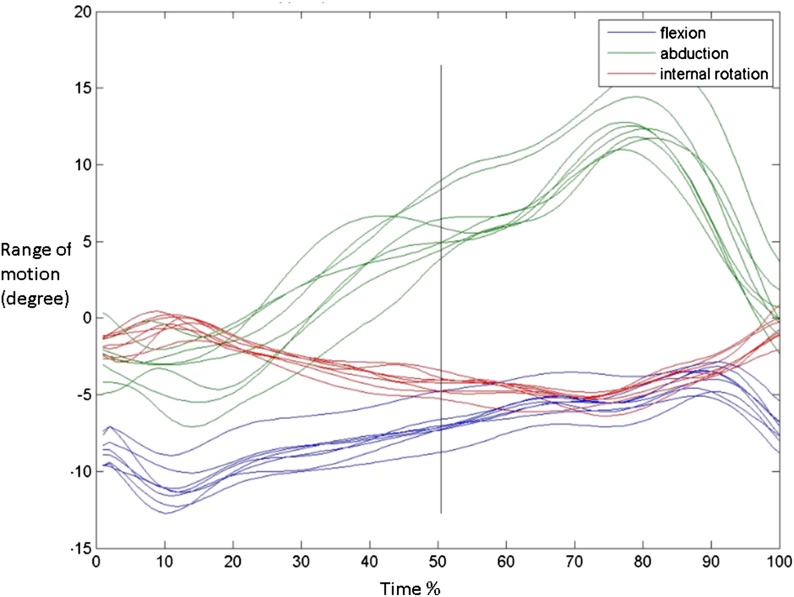
Both the calcaneal fracture group and the arthrodesis group had significantly less flexion-extension between the hindfoot and the tibia during the push-off phase compared with the healthy control group (p = 0.001 and p = 0.016, respectively). The calcaneal fracture group and the arthrodesis group also had significantly less flexion-extension between the forefoot and the tibia compared with the control group during the loading phase (p = 0.014 and p = 0.009, respectively) and the push-off phase (p = 0.028 and p = 0.002, respectively). In contrast, significantly greater abduction-adduction between the hindfoot and the tibia was found for the calcaneal fracture group and the arthrodesis group during the push-off phase compared with healthy subjects (p = 0.042 and p < 0.0001, respectively). In Figures 3, 4, and 5, the range of motion between the hindfoot and the tibia is plotted for a healthy subject, a patient after a calcaneal fracture, and a patient who underwent subtalar arthrodesis. Figure 6 presents an OFM animation model of a patient during gait.
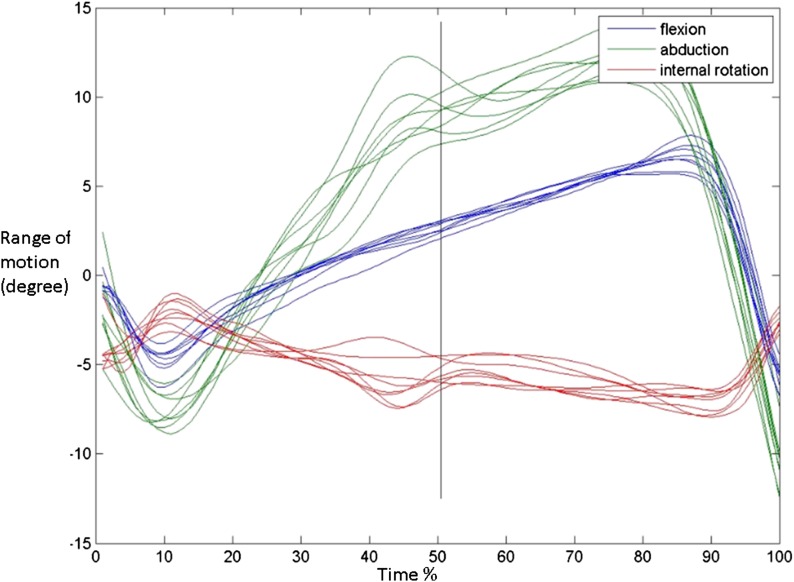
Fig. 3.
Range of motion between the hindfoot and the tibia during gait in a healthy subject. Blue = flexion-extension, green = abduction-adduction, and red = inversion-eversion.
Fig. 4.
Range of motion between the hindfoot and the tibia during gait in a patient after calcaneal fracture. Blue = flexion-extension, green = abduction-adduction, and red = inversion-eversion.
Fig. 5.
Range of motion between the hindfoot and the tibia in a patient after subtalar arthrodesis. Blue = flexion-extension, green = abduction-adduction, and red = inversion-eversion.
Fig. 6.
An OFM animation model of a patient during gait.
Functional and Radiographic Outcomes
The range of motion between the hindfoot and the tibia in the transverse plane during the push-off phase was significantly correlated with the patient-reported clinical outcome measures defined by the FADI (r2 = 0.51; p < 0.001) and the SF-36 physical component summary score (r2 = 0.52; p < 0.001) (Table III). The range of motion between the forefoot and the tibia in the transverse plane during the push-off phase was also significantly correlated with the FADI (r2 = 0.66; p < 0.001) and SF-36 physical component summary score (r2 = 0.64; p < 0.001). In addition, when analyzing the association between the hindfoot-tibia range of motion in the transverse plane during the push-off phase and postoperative CT findings, we found a significant correlation between the step-off in the subtalar joint and the range of motion (r2 = −0.74; p = 0.004). The step-off was also correlated with the patient-reported outcome questionnaires (FADI, r2 = −0.76; p = 0.003) and the SF-36 physical component summary score (r2 = −0.78; p = 0.002), while no correlation was found between the intra-articular gap of the posterior facet and the patient-reported functional outcome measures. There was a significant correlation between the postoperative sagittal subtalar joint axis measured on CT scans with the range of motion (inversion-eversion) between the forefoot and the tibia (r2 = 0.64; p = 0.018), but no correlation was found with the patient-reported outcome parameters. We found no significant correlations between the Böhler angle or the Gissane angle with patient-reported outcome measures or range of motion during gait.
TABLE III.
Correlations Between Subtalar Range of Motion, Functional Outcome, and Radiographic Findings in Patients After Calcaneal Fracture
| Push-off Phase Forefoot-Tibia Inversion-Eversion | Push-off Phase Hindfoot-Tibia Inversion-Eversion | FADI | Subtalar Axis (Sagittal, Postoperatively) | Step-off | Gap | AOFAS | SF-36 Physical | |
| Push-off phase forefoot-tibia inversion-eversion | 0.78† | 0.66† | 0.64† | −0.51 | −0.56 | 0.61† | 0.64† | |
| Push-off phase hindfoot-tibia inversion-eversion | 0.78† | 0.51† | 0.43 | −0.74† | −0.18 | 0.45† | 0.52† | |
| FADI | 0.66† | 0.51† | 0.10 | −0.76† | −0.08 | 0.95† | 0.95† | |
| Subtalar axis (sagittal, postoperatively) | 0.64* | 0.43 | 0.10 | 0.00 | −0.06 | 0.32 | 0.25 | |
| Step-off | −0.51 | −0.74† | −0.76† | 0.00 | −0.27 | −0.52 | −0.78† | |
| Gap | −0.56 | −0.18 | −0.08 | −0.06 | −0.27 | −0.05 | 0.16 | |
| Böhler angle | 0.23 | 0.10 | 0.47 | 0.22 | −0.38 | −0.26 | 0.39 | 0.26 |
| Gissane angle | 0.35 | 0.44 | 0.29 | 0.14 | −0.30 | −0.16 | 0.44 | 0.03 |
| AOFAS | 0.61† | 0.45† | 0.95† | 0.32 | −0.52 | −0.05 | 0.87† | |
| SF-36 physical | 0.64† | 0.52† | 0.95† | 0.25 | −0.78† | 0.16 | 0.87† |
Significance level = 0.05.
Significance level = 0.01.
Discussion
We evaluated the biomechanical gait properties after calcaneal fracture in relation to radiographic findings and patient-reported satisfaction. The primary focus was to compare the range of motion in the transverse plane (inversion-eversion), which is considered the main clinical function of the subtalar joint9. Our study demonstrated that the range of motion of the subtalar joint of patients after calcaneal fracture was significantly related both to the quality of reduction of the subtalar joint as evaluated on postoperative CT scan and the functional outcome as reported in questionnaires. This represents a notable finding, which may have important clinical implications by providing a link between postsurgical results and patient-reported outcome measures. Because patients completed the questionnaires before gait analysis was performed, and both researchers analyzed the images prior to gait analysis, detection bias was not present.
Previous studies using OFM with healthy subjects have revealed that the OFM is a reliable test for evaluating gait and differences in range of motion10,11,30. Studies investigating gait analysis in pathologic feet, especially after calcaneal fracture, are limited. Using physical examination, Kingwell et al. found a correlation between the range of motion in the subtalar joint and patient-reported outcome after treatment of calcaneal fractures. However, no data on postoperative CT-evaluated reconstruction of the calcaneus were presented9. In a study by Hetsroni et al., twenty patients with high-grade intra-articular fractures of the calcaneus underwent motion analysis of the leg and foot two years after operative treatment18. Data were compared with those of the contralateral leg and nine healthy subjects. A significant difference between walking speed and range of motion was found, as demonstrated in the present study. However, in their study, when correcting for the effect of speed, no differences in range of motion of the subtalar joint between healthy subjects and patients with calcaneal fractures were found, although the number of patients (n = 5) for this subanalysis was limited. In a study by Hirschmüller et al., sixty patients with unilateral intra-articular calcaneal fractures, treated operatively, were evaluated one year postoperatively for correlations between clinical, radiographic, and biomechanical differences in the measurement of plantar pressure distribution and gait velocity. They found a moderate correlation between muscle strength and patient satisfaction as reported on clinical questionnaires and a moderate correlation between standing duration and clinical questionnaires. The strongest correlation was between self-selected walking speed and clinical outcome as measured by the SF-36 physical component score31.
Two other studies evaluated gait after calcaneal fractures that were nonsurgically corrected. Analyzing the gait of twenty-one patients, Bozkurt et al. found a significantly lower range of motion in the ankle joint compared with that of healthy subjects16. These results were comparable with those of Kitaoka et al., who found gait abnormalities in the hindfoot and ankle in patients treated nonsurgically for intra-articular calcaneal fractures17.
Previous studies have identified the subtalar joint as the key factor in hindfoot function during gait9,32. The reduction in range of motion in this joint after calcaneal fracture is hypothesized to be related to reduced functional capacity of the foot. Following subtalar arthrodesis, inversion motion of the calcaneus is virtually 0° and is compensated with a higher range of motion in the transverse plane during push-off. In patients with a decreased patient-reported functional outcome after calcaneal fracture, this compensatory phenomenon was also identified.
A number of comments need to be made regarding the interpretation of our observations. The OFM does not allow for direct measurement of the motion in the subtalar joint because the talus and calcaneus are seen as one block. We therefore evaluated and compared the kinematic characteristics of calcaneal fracture patients with those of patients after subtalar arthrodesis and healthy subjects. This provided an estimation of the variability of the inversion-eversion movement in the subtalar joint. In patients after subtalar arthrodesis, the motion in the transverse plane was effectively eliminated, providing a positive control group, while the healthy subjects represent a negative control group with normal range of motion. In our study, some range of motion in the transverse plane (inversion-eversion) in the subtalar arthrodesis group was found. This measured motion is likely to have been caused in the adjacent joints, such as the ankle joint; skin motion also could have been detected. Our study did not provide data concerning the disease spectrum of different grades of malunion of the calcaneus but rather was limited to measuring the link between functional outcome and gait analysis in radiographically well-restored calcaneal fractures. The calcaneal fracture patient cohort represents a group ranging widely in age. In the literature, studies investigating the effect of age and speed on gait parameters are limited; however, no large differences in range of motion between young adults and older healthy subjects have been found, while speed has significantly influenced gait21,22,33 Nonetheless, the effect of age cannot be completely ruled out. Furthermore, the OFM has acceptable-to-good reproducibility, but small errors can occur by the placement of markers on skin, resulting in some variability, as seen in our results10,11.
Gait analysis of the patients in our study was performed at a minimum of six months postoperatively (a range of six months to three years and a median of two years). Although the literature reports on improvements in gait patterns during follow-up, it is not clear, because of the limited studies available, when these improvements in foot and ankle kinematics stop.
In conclusion, our study demonstrated that range of motion between the hindfoot and the tibia as measured using the OFM on the Vicon MX3 system in patients after a calcaneal fracture was both related to the quality of reduction of the subtalar joint as evaluated on postoperative CT scans and functional outcome as reported by the patients during follow-up.
Appendix
Details of the marker placement and motions analyzed are shown in Tables IV and V.
TABLE IV.
Marker Placement
| Marker Name* | Placement |
| RPSI, LPSI | Posterior iliac spine |
| RTHI, LTHI (thigh) | The midway point of a straight line between the major trochanter and the knee |
| RASI, LASI | Anterior iliac spine |
| RKNE, LKNE (knee) | Lateral joint space of the knee |
| RHFB, LHFB (head of the fibula) | Directly on the proximal head of the fibula |
| RTUB, LTUB (tuberosity) | Tuberosity of the tibia |
| RTIB, LTIB (tibia) | Laterally on a straight line between the marker for the knee and for the ankle |
| RSHN, LSHN (shin) | Anteriorly on the middle of the tibia |
| RPCA, LPCA | Posterior calcaneus |
| RANK, LANK (ankle) | Lateral malleolus |
| RMMA, LMMA (medial malleolus) | Medial aspect of the malleolus |
| RCPEG, LCPEG | Wand marker on the heel pointing in cranial direction |
| RHEE, LHEE (heel) | The most distal aspect of the heel |
| RSTAL, LSTAL | Sustentaculum tali |
| RLCA, LLCA | Lateral calcaneus |
| RP5M, LP5M (proximal 5th metatarsal) | Lateral aspect of the proximal 5th metatarsal |
| RD5M, LD5M (distal 5th metatarsal) | Lateral aspect of the distal 5th metatarsal |
| RTOE, LTOE (toe) | Dorsum of the foot between phalanges 2 and 3 |
| RHLX, LHLX (hallux) | Base of the hallux |
| RD1M, LD1M (distal 1st metatarsal) | Medial aspect of the distal 1st metatarsal |
| RP1M, RP1M (proximal 1st metatarsal) | Medial aspect of the proximal 1st metatarsal |
A total of forty-two markers, each measuring 15 mm in diameter. R = right and L = left in the marker name.
TABLE V.
Motions Analyzed
| Loading Phase | Push-off Phase | |
| Forefoot-hindfoot x | Dorsiflexion | Dorsiflexion |
| Forefoot-hindfoot y | Abduction | Abduction |
| Forefoot-hindfoot z | Inversion | Inversion |
| Forefoot-tibia x | Dorsiflexion | Dorsiflexion |
| Forefoot-tibia y | Abduction | Abduction |
| Forefoot-tibia z | Inversion | Inversion |
| Hindfoot-tibia x | Dorsiflexion | Dorsiflexion |
| Hindfoot-tibia y | Abduction | Abduction |
| Hindfoot-tibia z | Inversion | Inversion |
Footnotes
Investigation performed at Maastricht University Medical Center, Maastricht, the Netherlands
Disclosure: None of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of any aspect of this work. None of the authors, or their institution(s), have had any financial relationship, in the thirty-six months prior to submission of this work, with any entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. Also, no author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Bruce J, Sutherland A. Surgical versus conservative interventions for displaced intra-articular calcaneal fractures. Cochrane Database Syst Rev. 2013. January 31;1:CD008628. [DOI] [PubMed] [Google Scholar]
- 2.Guerado E, Bertrand ML, Cano JR. Management of calcaneal fractures: what have we learnt over the years? Injury. 2012. October;43(10):1640-50. Epub 2012 Jun 2. [DOI] [PubMed] [Google Scholar]
- 3.Ibrahim T, Rowsell M, Rennie W, Brown AR, Taylor GJS, Gregg PJ. Displaced intra-articular calcaneal fractures: 15-year follow-up of a randomised controlled trial of conservative versus operative treatment. Injury. 2007. July;38(7):848-55. Epub 2007 Apr 18. [DOI] [PubMed] [Google Scholar]
- 4.Sanders R. Displaced intra-articular fractures of the calcaneus. J Bone Joint Surg Am. 2000. February;82(2):225-50. [DOI] [PubMed] [Google Scholar]
- 5.Clarke M. Fractures of the calcaneus: trauma. In: Saunders R, editor. Trauma: core knowledge in orthopaedics. 1st ed Philadelphia: Elsevier Mosby; 2007. p 386-402. [Google Scholar]
- 6.Schepers T, van Lieshout EMM, van Ginhoven TM, Heetveld MJ, Patka P. Current concepts in the treatment of intra-articular calcaneal fractures: results of a nationwide survey. Int Orthop. 2008. October;32(5):711-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McPoil TG, Knecht HG. Biomechanics of the foot in walking: a function approach. J Orthop Sports Phys Ther. 1985;7(2):69-72. [DOI] [PubMed] [Google Scholar]
- 8.Piazza SJ. Mechanics of the subtalar joint and its function during walking. Foot Ankle Clin. 2005. September;10(3):425-42, v. [DOI] [PubMed] [Google Scholar]
- 9.Kingwell S, Buckley R, Willis N. The association between subtalar joint motion and outcome satisfaction in patients with displaced intraarticular calcaneal fractures. Foot Ankle Int. 2004. September;25(9):666-73. [DOI] [PubMed] [Google Scholar]
- 10.van Hoeve S, de Vos J., Weijers P.H.E, Verbruggen J.P.A.M, Willems P., Poeze M., Meijer K. Repeatability and reliability of the Oxford Foot Model for kinematic gait analysis of the foot and ankle. Unpublished data.
- 11.Wright CJ, Arnold BL, Coffey TG, Pidcoe PE. Repeatability of the modified Oxford foot model during gait in healthy adults. Gait Posture. 2011. January;33(1):108-12. [DOI] [PubMed] [Google Scholar]
- 12.Cappozzo A, Della Croce U, Leardini A, Chiari L. Human movement analysis using stereophotogrammetry. Part 1: theoretical background. Gait Posture. 2005. February;21(2):186-96. [DOI] [PubMed] [Google Scholar]
- 13.Chiari L, Della Croce U, Leardini A, Cappozzo A. Human movement analysis using stereophotogrammetry. Part 2: instrumental errors. Gait Posture. 2005. February;21(2):197-211. [DOI] [PubMed] [Google Scholar]
- 14.Leardini A, Chiari L, Della Croce U, Cappozzo A. Human movement analysis using stereophotogrammetry. Part 3. Soft tissue artifact assessment and compensation. Gait Posture. 2005. February;21(2):212-25. [DOI] [PubMed] [Google Scholar]
- 15.Della Croce U, Leardini A, Chiari L, Cappozzo A. Human movement analysis using stereophotogrammetry. Part 4: assessment of anatomical landmark misplacement and its effects on joint kinematics. Gait Posture. 2005. February;21(2):226-37. [DOI] [PubMed] [Google Scholar]
- 16.Bozkurt M, Kentel BB, Yavuzer G, Oçgüder A, Heycan C, Tonuk E. Functional evaluation of intraarticular severely comminuted fractures of the calcaneus with gait analysis. J Foot Ankle Surg. 2004. Nov-Dec;43(6):374-9. [DOI] [PubMed] [Google Scholar]
- 17.Kitaoka HB, Schaap EJ, Chao EYS, An KN. Displaced intra-articular fractures of the calcaneus treated non-operatively. Clinical results and analysis of motion and ground-reaction and temporal forces. J Bone Joint Surg Am. 1994. October;76(10):1531-40. [DOI] [PubMed] [Google Scholar]
- 18.Hetsroni I, Nyska M, Ben-Sira D, Arnson Y, Buksbaum C, Aliev E, Mann G, Massarwe S, Rozenfeld G, Ayalon M. Analysis of foot and ankle kinematics after operative reduction of high-grade intra-articular fractures of the calcaneus. J Trauma. 2011. May;70(5):1234-40. [DOI] [PubMed] [Google Scholar]
- 19.Agostini V, Ganio D, Facchin K, Cane L, Moreira Carneiro S, Knaflitz M. Gait parameters and muscle activation patterns at 3, 6 and 12 months after total hip arthroplasty. J Arthroplasty. 2014. June;29(6):1265-72. Epub 2013 Dec 18. [DOI] [PubMed] [Google Scholar]
- 20.Nantel J, Termoz N, Vendittoli PA, Lavigne M, Prince F. Gait patterns after total hip arthroplasty and surface replacement arthroplasty. Arch Phys Med Rehabil. 2009. March;90(3):463-9. [DOI] [PubMed] [Google Scholar]
- 21.Legault-Moore D, Chester VL, de Vries G. Multisegment foot kinematics during walking in younger and older adults. J Clin Med Res. 2012. August;4(4):259-66. Epub 2012 Jul 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arnold JBMS, Mackintosh S, Jones S, Thewlis D. Differences in foot kinematics between young and older adults during walking. Gait Posture. 2014. February;39(2):689-94. Epub 2013 Oct 10. [DOI] [PubMed] [Google Scholar]
- 23.Böhler L. Diagnosis, pathology, and treatment of fractures of the os calcis. J Bone Joint Surg Am. 1931. January;13(1):75-89. [Google Scholar]
- 24.Keener BJ, Sizensky JA. The anatomy of the calcaneus and surrounding structures. Foot Ankle Clin. 2005. September;10(3):413-24. [DOI] [PubMed] [Google Scholar]
- 25.DSS Research. Researcher’s Toolkit. 2015. http://www.dssresearch.com/toolkit/sscalc/size_a2.asp. Accessed 2015 Jun 18.
- 26.Lewis GS, Kirby KA, Piazza SJ. Determination of subtalar joint axis location by restriction of talocrural joint motion. Gait Posture. 2007. January;25(1):63-9. Epub 2006 Feb 7. [DOI] [PubMed] [Google Scholar]
- 27.Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng. 1983. May;105(2):136-44. [DOI] [PubMed] [Google Scholar]
- 28.Wu G, Siegler S, Allard P, Kirtley C, Leardini A, Rosenbaum D, Whittle M, D’Lima DD, Cristofolini L, Witte H, Schmid O, Stokes I; Standardization and Terminology Committee of the International Society of Biomechanics; International Society of Biomechanics. ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion—part I: ankle, hip, and spine. J Biomech. 2002. April;35(4):543-8. [DOI] [PubMed] [Google Scholar]
- 29.Dubbeldam R, Buurke JH, Simons C, Groothuis-Oudshoorn CG, Baan H, Nene AV, Hermens HJ. The effects of walking speed on forefoot, hindfoot and ankle joint motion. Clin Biomech (Bristol, Avon). 2010. October;25(8):796-801. [DOI] [PubMed] [Google Scholar]
- 30.Carson MC, Harrington ME, Thompson N, O’Connor JJ, Theologis TN. Kinematic analysis of a multi-segment foot model for research and clinical applications: a repeatability analysis. J Biomech. 2001. October;34(10):1299-307. [DOI] [PubMed] [Google Scholar]
- 31.Hirschmüller A, Konstantinidis L, Baur H, Müller S, Mehlhorn A, Kontermann J, Grosse U, Südkamp NP, Helwig P. Do changes in dynamic plantar pressure distribution, strength capacity and postural control after intra-articular calcaneal fracture correlate with clinical and radiological outcome? Injury. 2011. October;42(10):1135-43. Epub 2010 Nov 13. [DOI] [PubMed] [Google Scholar]
- 32.Lewis GS, Kirby KA, Piazza SJ. Determination of subtalar joint axis location by restriction of talocrural joint motion. Gait Posture. 2007. January;25(1):63-9. Epub 2006 Feb 7. [DOI] [PubMed] [Google Scholar]
- 33.van Hoeve S, Leenstra B, Verbruggen JPAM, Willems P, Poeze M, Meijer K. The effect of age and speed on a four-segmented foot model. Unpublished data.