Abstract
We present findings of an international conference of diverse participants exploring the influence of electronic health records (EHRs) on the patient–practitioner relationship. Attendees united around a belief in the primacy of this relationship and the importance of undistracted attention. They explored administrative, regulatory, and financial requirements that have guided United States (US) EHR design and challenged patient-care documentation, usability, user satisfaction, interconnectivity, and data sharing. The United States experience was contrasted with those of other nations, many of which have prioritized patient-care documentation rather than billing requirements and experienced high user satisfaction. Conference participants examined educational methods to teach diverse learners effective patient-centered EHR use, including alternative models of care delivery and documentation, and explored novel ways to involve patients as healthcare partners like health-data uploading, chart co-creation, shared practitioner notes, applications, and telehealth. Future best practices must preserve human relationships, while building an effective patient–practitioner (or team)-EHR triad.
Keywords: patient–practitioner relationship, international experience with electronic health records, burnout, solutions to electronic health record challenges, design, patient–practitioner–computer triad
INTRODUCTION AND CONFERENCE DESIGN
The electronic health record (EHR) has profoundly influenced the practice of medicine and patient–practitioner interactions in clinical settings.1,2 Alongside benefits of consolidated patient records, improved communication, and ability to address population health have come unintended consequences, including challenges to the patient–practitioner relationship3–7 and, in the United States, a precipitous decline in clinician wellbeing and professional satisfaction.8–11 In March 2017, 160 patients, practitioners, educators, technology designers and vendors, government officials, patient advocates, and healthcare stakeholders from the United States and 6 industrialized nations (Canada, United Kingdom, Denmark, Portugal, Israel, and Australia) gathered at The Warren Alpert Medical School of Brown University to explore this pressing topic. Practitioners included physicians, nurses, nurse practitioners, and mental health professionals; medical students, and residents also participated. There were plenary sessions, TED-style talks, symposia, research papers, posters, and digital demonstrations. Conference leaders invited experts, distributed email requests for submissions, and advertised this open conference through mailings, LISTSERVs, social media, and word of mouth. Presenters comprised about half the attendees. International participants were invited because non-US practitioners have had longer and generally more positive EHR experiences than many in the United States. This article summarizes conference conclusions.12
THE VALUE OF THE PATIENT–PRACTITIONER RELATIONSHIP
Patients and practitioners expressed remarkably similar wishes for relationship-based care as technology advances, underscoring the central elements of constructive patient–practitioner interactions.13,14 Both groups want time and space to rekindle or establish trusting relationships, receive or offer eye contact and full attention,2,3,13–17 and be heard or engage in careful listening.1,2 Patients want to be known as individuals who have valuable firsthand knowledge of their health experiences. Practitioners want to be respected for medical expertise and technical skills but recognized as having human limitations, especially when grappling with healthcare system challenges. Both groups believe clinical encounters should be about patient care and not its documentation.
EHR BENEFITS TO PATIENTS AND PRACTITIONERS
Patients praised many EHR features, noting that records do not get lost, are accessible from anywhere, and allow patients to participate in their own care by using portals to schedule appointments, review test results, and communicate with practices. Patients imagine contributing further to their EHRs by uploading health materials, creating personalized biographies,18 reviewing practitioners’ notes,19 and even co-creating notes. Practitioners value EHRs for their legibility, accessibility, consolidated health information, embedded references, decision support, and potential to enhance patient education and understanding.
EHR CHALLENGES TO THE PATIENT–PRACTITIONER RELATIONSHIP
Many challenges have accompanied the rapid introduction of EHRs into clinical care. Managing the volume of information and juggling the complexities of patient needs and EHR systems, while recording care that justifies reimbursement has overwhelmed US practitioners.11,16,20,21 Longer workdays, work after work, more time spent documenting care and completing administrative tasks than face-to-face with patients, and fewer patients seen have left both patients and practitioners feeling that people often play second fiddle to computers.8–11,13,15,16,20–27 Both groups described a distressing decrease in human connections and meaningful interactions.2,20–24 They worry about patient privacy and confidentiality.4–6,13,28,29 These trends have contributed significantly to the EHR’s implication in US practitioner burnout.8–11,21,23,26,27,30
Roll-out challenges
Conference participants noted that the EHR was introduced into traditional ways of conducting care before rethinking roles, tasks, workflow, workloads, and redundancy. They observed that change is difficult. Implementing untested systems and integrating new tools before having confidence in them is stressful, particularly when patient health is at stake. Furthermore, new systems reveal hidden flaws, for example, poorly controlled patients lost to care. They also present unforeseen challenges like balancing improved access to patient records with maintaining confidentiality4–6,28,29 or leveraging tools such as templates and copy and paste while creating useful and ethical documentation.4,13,14
Design and vendor challenges
The US designers and vendors of small and large EHRs described challenges of designing effective EHRs and interconnected systems. The absence of national standards in areas like preventive measures and laboratory results present additional hurdles.4,31,32 Regulations imposed by institutions fearing data breaches and subsequent penalties further challenge interoperability and data access,32,33 as has the open market of the past decade, which led to the emergence of hundreds of companies creating a variety of propriety and open source products.31,34 The financial burden of designing software to meet changing guidelines such as meaningful use has hampered competition by smaller, innovative companies. Ultimately, however, fewer dominant EHRs may facilitate interoperability.
Government challenges
Government presenters described accountability to tax payers and legislators, and the herculean task of developing programs to move health information technology ahead in US regions with vastly different population densities, demographics, geographies, and technological maturity. They described listening to patients’ and practitioners’ needs when devising statewide initiatives such as Colorado’s telehealth bill and Vermont’s improved broadband access initiative, as well as current federal legislative mandates like accountable care, interconnectivity, and data accessibility.
OBSERVATIONS FROM OTHER NATIONS
International attendees recounted stories from their national and personal EHR experiences. While anecdotal, their reports offered valuable opportunities for sharing insights and collaborative reflection. An Australian participant described the pain of rolling out health information technology infrastructure and adopting EHRs in his nation, but noted that patients welcomed EHRs, believing it would be difficult to practice modern medicine without a computer. A Danish presenter elucidated his government’s well-regarded EHR used in all facilities of their single-payer health system, allowing clinicians easy access to patient records and clinical data to feed directly into national population and public health research and policy development.35 A participant from Portugal described that nation’s creation of a similar comprehensive infrastructure, but its progression to a more siloed and less streamlined system because of inconsistent internet access and the establishment of parallel infrastructures for e-prescribing, death records, and epidemiology.
In the United Kingdom, EHRs initially designed by family physicians for patient care have been deployed on a national scale and are well liked and trusted. Anecdotally, as US EHRs have been imported for inpatient use, UK hospitals face some of the same challenges to efficiency and overdocumentation as US users of the same products.
In Israel, EHRs also designed around patient care require many fewer clicks for prescribing, writing orders, and documenting than their US counterparts. Billing is separated from the EHR. Israel’s 12 major health systems, including the Israeli Defense Forces, have successfully interconnected their EHRs, with data based in each home institution but accessible within seconds from any other system.36 Thus far there have been no breaches.
A Canadian speaker described innovative efforts to help patients with complex medical problems set visit agendas directly into the EHR.37 A UK presenter described a pioneering program in Bangladesh connecting patients to primary and specialty care when signing up for banking.
Perhaps the most striking feature noted by international presenters was that their countries’ EHRs were designed to record patient care; interestingly, clinical notes are, on average, 4 times shorter than US notes.27
SUGGESTED SOLUTIONS
While identifying current challenges to the patient–practitioner relationship, conference attendees expressed the need to move toward a constructive triad of patient–practitioner–computer, or patient-healthcare team-computer in coming years.38,39 Diverse solutions were explored, encouraging all to imagine others.
Education
Education was cited as a critical component of all solutions. Complex EHR skills require time and effort to master and must be balanced with other medical and systems knowledge clinicians need to learn for their daily work. Institutions must commit time and resources to robust initial and ongoing education of all medical professionals, whether at the outset of training or employment or in mid-career, taking into consideration diverse backgrounds, technological skills, and trends toward inter-professional team care. While software subtleties may allow for more efficiency, users need training and practice in these areas, too, including effective use of embedded EHR feedback tools.40
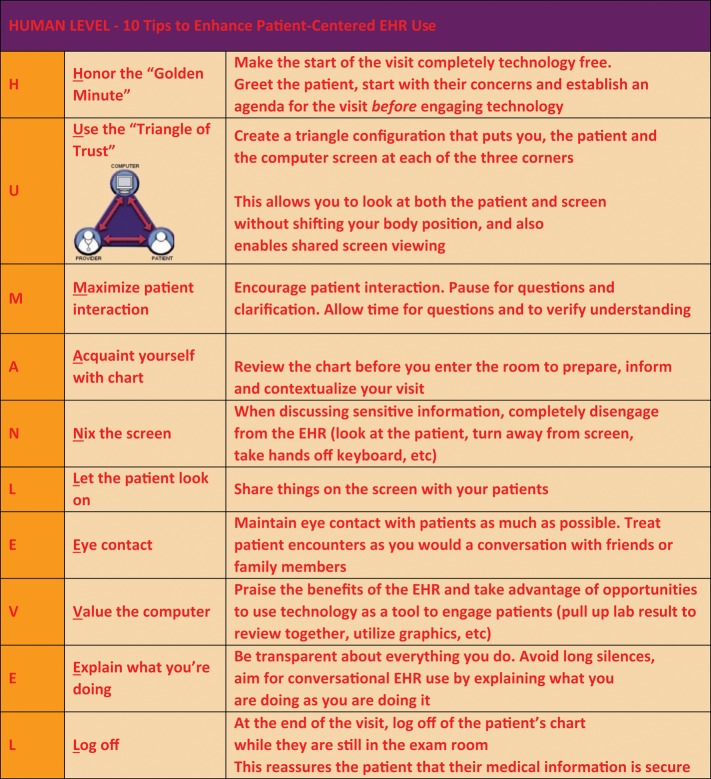
Most importantly, education should focus on effective EHR use during encounters to strengthen rather than detract from patient–practitioner communication.1,2 Tips to create patient-centered EHR best practices are shown in Figure 1.41,42 Optimal use requires personalization, observed evaluation, ongoing feedback, and organizational support. Curricula are being developed at a variety of institutions43 (Table 1). Learners need training to create EHR documentation that encourages and conveys their thinking, while selectively employing time-saving tools like voice-to-text, text-forward, and templates.13,53
Figure 1.
HUMAN LEVEL mnemonic for patient-centered electronic medical record use. Abbreviation: EHR: electronic health record. From Mann and Slaboch41 and Lee et al.42
Table 1.
Examples of EHR curricula
| Institution | Components | Materials and methods |
|---|---|---|
| Alpert Medical School of Brown University (Wald et al)44 |
|
|
| Hebrew University of Jerusalem (Reis) |
|
|
| Oregon Health & Science University (Hersh et al) |
|
|
| University of Chicago (Alkureishi and Lee) |
|
|
| University of Toronto (Shachak et al) |
|
|
Abbreviations: EHR: electronic health record; MS2: second year medical students; MS3: third year medical students; OSCE: objective structured clinical examination; PGY1: postgraduate Year 1 (interns); PGY2: postgraduate Year 2 residents; PGY3: postgraduate Year 3 residents; e-CEX: Electronic-clinical evaluation exercise; CME: Continuing Medical Education.
Rethinking documentation
It is time to reconsider the components of a well-crafted note as past information is accessible in the EHR. Conference attendees spoke about filtering information to meet clinician needs; tailoring the style of notes to fit their clinical purposes such as preventive, chronic care, consult, or community based care; and choosing the form that best conveys information. The imperative to separate billing from extent of documentation was noted throughout the meeting.53
Until ordering and documenting become more streamlined in US EHRs, it is not realistic—for patients who need full attention or clinicians who are more likely to make mistakes when multi-tasking3,20,53,54—to expect clinicians to document fully while attending to patients or for hours at night.8–11 Rather, trained scribes or team members co-managing the visit should be documenting.55,56 This may change when EHR charting becomes simpler and features like dictation, virtual assistants, and natural language processing improve.57
EHR design
Attendees stressed the need for clinicians and designers to share ongoing front-line experiences and communication.20 For example, streamlined software will allow nurses to enter data in real time rather than copying handwritten logs, and smaller devices can facilitate bedside nursing care while entering data.58,59
Rethinking job descriptions and workflow
The EHR affords us the opportunity to re-evaluate our work and who does it, improve efficiency, reduce redundancy, and commit to restoring and protecting human interactions between patients and practitioners and among medical professionals. All are integral to excellent patient care and professional satisfaction. Suggested EHR design improvements to support optimal patient care are shown in Table 2.
Table 2.
Design improvements in EHRs and clinical workflows
| Specific suggestions and examples | |
|---|---|
| EHR improvement | |
| Streamline EHR log-in |
|
| Improve usability |
|
| Tailor information presentation | |
| Match data entry modality with task | |
| Tailor note design to encounter type |
|
| Use virtual assistants | |
| Use EHR to educate |
|
| Protect patient confidentiality |
|
| Embrace patient contribution67 (eg, screening, visit agenda37, updated personal data and biographies18) |
|
| Facilitate meaningful documentation |
|
| Improve interoperability and data sharing | |
| Workflow improvement | |
| Previsit preparation | Staff oversees:
|
| Task reallocation (“Lean” concept)a |
|
| Additional staff | |
| Reduce administrative burden11,30 |
|
| Facilitate team communication61,62 |
|
| Decrease documentation time | |
| Maximize EHR placement and usefulness | |
Abbreviation: EHR: electronic health record.
aLean refers to a set of operating philosophies and methods that help create a maximum value for patients by reducing waste and waits.65
Lean principles of industrial engineering can help design workplaces to maximize teamwork,65 streamline patients’ movement through care, and utilize EHRs to support and educate.42–51 As shown in Table 2, the healthcare team works as a unit according to lean principles with tasks allocated at the level of training; all help document. Many clinical settings still rely on paper for reviewing past care, completing forms, and faxing information. When EHR functions, graphics, and information display become more user-friendly, this work can be done once using the computer.66
Reimagined care delivery includes teams of medical professionals maximizing their training and skills to support patients and one another.56,61,62
The patient as team member
Patients are indispensable team members who can serve as valuable data providers.67 This can be achieved by expanding portal functions to enable patients to initiate visit documentation from home or on devices at the point of care. Patients can update demographic, insurance, and biographical information,18 or review EHR data and set visit agendas.37,53 The OpenNotes project has pioneered promoting patient access to their clinical notes, including behavioral health notes68,69; remaining challenges include maintaining adolescent and parent confidentiality6,29, and practitioner perceptions that sharing notes impacts full discussions of clinical thinking, differential diagnoses, and psychosocial issues.68,70
Interestingly, patients and practitioners have expressed overall satisfaction with shared notes, finding them respectful and communicative, and patients are better able to adhere to recommendations when they review the thinking behind them.19,69 Patients also identify and correct errors in their records.19,69 Patients have begun sharing photos and videos with clinicians on their smart phones; these can be uploaded into their records—first steps toward having patients co-create documentation. One can imagine a future in which a personal health record belongs to the patient, who shares data with practitioners and institutions, generating care centered around shared decisions, clear communication, and consideration of the patient’s life outside the medical system.
New technologies
Many ideas were shared among participants across disciplines regarding new technologies. For example, SMS texting is a powerful tool to remind patients about appointments, support behavior modification,71 and communicate information. So too, applications (“Apps”) can help patients manage health issues like dietary change, asthma,72 diabetes,73 menstrual cycles, and anxiety. Some are employed by patients on their own, while others transmit data to practitioners for review. Patients and practitioners need guidance in sorting through the many available products to be confident that apps advance patient health and support clinical care with manageable data loads. Telehealth also holds great promise to connect patients, practitioners, and family members when geographical, medical, and psychological barriers prevent in-person visits.74
SUMMARY
Participants at this groundbreaking conference valued hearing the aspirations, challenges, and perspectives of a diverse group of attendees. They remained committed to protecting the patient–practitioner relationship as the foundation of excellent care and patient and practitioner satisfaction in this age of advancing health information technology. International colleagues demonstrated the value of EHRs with documentation centered around clinical care, seamless interoperability, and prompt data access for patient care and population health. The US attendees were challenged to find ways to decrease clicks, screen shifts, and excessive documentation and improve interconnectivity and data sharing. Conference attendees highlighted the importance of ongoing communication and advocacy by all to ensure a future medical system that preserves the healing power of human relationships, while harnessing the tremendous potential of health information technology to improve medical care and health.
Two commercial products are mentioned in the references.
The conference had no connection or commercial relationship with Imagining a Medical Record of the Future (Ref.57).
Gregory Makoul, PhD, Founder and CEO of PatientWisdom was a conference presenter and received support for travel and housing from The Physicians Foundation, a conference funder, but no additional remuneration (Ref.18).
The LEVEL mnemonic/behaviors in Figure 1. were originally published as Mann WR, Slaboch J. Computers in the exam room—friend or foe? Perm J. 2004; 8 (4): 49–51. Copyright 2004, The Permanente Federation, LLC and is used with permission.
The HUMAN LEVEL figure was originally published as Alkureishi M, Lee W, Farnan J, Arora V. Breaking away from the iPatient to care for the real patient: implementing a patient-centered EMR use curriculum. MedEdPORTAL 2014; 10: 995 and is used with permission from Maria Alkureishi, MD and Wei Wei Lee MD/MPH.
FUNDING
Funding for The Patient, the Practitioner, and the Computer: Holding on to the Core of Our Healing Professions in a Time of Technological Change (March 17–19, 2017) was received from: The Warren Alpert Medical School of Brown University (Office of the Associate Dean for Medical Education, Department of Family Medicine, Department of Pediatrics), American Medical Association, Arnold P. Gold Foundation, Josiah Macy Jr. Foundation, The Physicians Foundation, Rhode Island Foundation, Rhode Island Quality Institute, Rhode Island Medical Imaging, University Emergency Medicine Foundation (now Brown Emergency Medicine), University Medicine Foundation (now Brown Medicine), University Orthopedics, Andrew and Shelley Sigal, and an Anonymous Donor.
Conflict of interest statement. E.T.T. received salary support from the Rhode Island Foundation and salary support and housing costs from The Physicians Foundation. Both organizations were conference funders. She is a member of The Warren Alpert Medical School Departments of Pediatrics and Medicine, both conference funders. M.A.A. received travel and housing support from The Physicians Foundation and received grant support from the Arnold P. Gold Foundation, both conference funders. W.W.L. received travel and housing support from The Physicians Foundation and received grant support from the Arnold P. Gold Foundation, both conference funders. S.F.B. received travel and housing support from The Physicians Foundation, a conference funder. P.A.B. received travel and housing support from The Physicians Foundation, a conference funder. J.W.B. received travel and housing support from The Physicians Foundation, a conference funder. R.M.F. and S.S.W. have no conflict of interest to declare. A.A.L. received travel and housing support from The Physicians Foundation, a conference funder. H.S.W. received housing support from The Physicians Foundation, a conference funder. W.R.H. received travel and housing support from The Physicians Foundation, a conference funder.
Acknowledgements
We wish to thank our editor Mindy A. SMITH, MD/MS for her enormous and invaluable contribution to this project and to recognize the ideas, input, and encouragement of:
Jeffrey M. Borkan, MD/PhD
Raymond H. Curry, MD
Ross W. Hilliard, MD
James Morrow, MD
Christopher Pearce, PhD/MFM
Shmuel P. Reis, MD/MHPE
Christine A. Sinsky, MD
Dilermando Sobral, MD/MS
REFERENCES
- 1. Alkureishi MA, Lee WW, Lyons M, et al. Impact of electronic medical record use on the patient–doctor relationship and communication: a systematic review. J Gen Intern Med 2016; 315: 548–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Crampton HN, Reis S, Shachak A.. Computers in the clinical encounter: a scoping review and thematic analysis. J Am Med Inform Assoc 2016; 233: 654–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Frankel RF. When it comes to the physician-patient-computer relationship, the “eyes” have it In: Papadokos P, Bertman SE, eds. Distracted Doctoring: Returning to Patient-Centered Care in the Digital Age. New York, NY: Springer; 2017: 87–99. [Google Scholar]
- 4. Hripcsak G, Bloomrosen M, FlatelyBrennan P, et al. Health data use, stewardship, and governance: ongoing gaps and challenges: a report from AMIA’s 2012 Health Policy Meeting. J Am Med Inform Assoc 2014; 212: 204–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wallace I. Is patient confidentiality compromised with the electronic health record?: A position paper. Comput Inform Nurs 2015; 332: 58–62. [DOI] [PubMed] [Google Scholar]
- 6. Bayer R, Santelli J, Klitzman R.. New challenges for electronic health records: confidentiality and access to sensitive health information about parents and adolescents. JAMA 2015; 3131: 29–30. [DOI] [PubMed] [Google Scholar]
- 7. Gephart S, Carrington JM, Finley B.. A systematic review of nurses' experiences with unintended consequences when using the electronic health record. Nurs Adm Q 2015; 394: 345–56. [DOI] [PubMed] [Google Scholar]
- 8. Sinsky C, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med 2016; 16511: 753–60. [DOI] [PubMed] [Google Scholar]
- 9. Arndt BG, Beasley JW, Watkinson MD, et al. Tethered to the EHR: primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med 2017; 155: 419–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc 2016; 917: 836–48. [DOI] [PubMed] [Google Scholar]
- 11. Babbott S, Manwell LB, Brown R, et al. Electronic medical records and physician stress in primary care: results from the MEMO Study. J Am Med Inform Assoc 2014; 21 (e1): e100–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. For materials related to The Patient, the Practitioner, and the Computer: Holding on to the Core of Our Healing Professions in a Time of Technological Change. https://www.brown.edu/academics/medical/education/otherprograms/continuing-medical-education/live-conferences/PPC-Conference; https://www.youtube.com/playlist?list=PL5hLO22cWOrBGTteM8dUvb65v4soCy_cj. Accessed November 11, 2018.
- 13. Sulmasy LS, López AM, Horwitch CA; American College of Physicians Ethics, Professionalism and Human Rights Committee. Ethical implications of the electronic health record: in the service of the patient. J Gen Intern Med 2017; 328: 935–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Committee on Quality Health Care in America, Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001. [Google Scholar]
- 15. Montague E, Asan O.. Dynamic modeling of patient and physician eye gaze to understand the effects of electronic health records on doctor-patient communication and attention. Int J Med Inform 2014; 833: 225–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Toll E. A piece of my mind. The cost of technology. JAMA 2012; 30723: 2497–8. [DOI] [PubMed] [Google Scholar]
- 17. Ventres W, Kooienga S, Vuckovic N, Marlin R, Nygren P, Stewart V.. Physician, patient, and the electronic health record: an ethnographic analysis. Ann Fam Med 2006; 42: 124–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.PatientWisdom. https://patientwisdom.com/. Accessed November 11, 2018.
- 19.OpenNotes. https://www.opennotes.org/. Accessed November 11, 2018.
- 20. Misto K, Padula C, Bryand E, Nadeau K.. Nurses' perception of the impact of electronic documentation on the nurse-patient relationship. J Nurs Care Qual 2019; 342: 163–8. [DOI] [PubMed] [Google Scholar]
- 21. Halamka JD, Tripathi M.. The HITECH era in retrospect. N Engl J Med 2017; 37710: 907–9. [DOI] [PubMed] [Google Scholar]
- 22. Kossman SP, Scheidenhelm SL.. Nurses' perceptions of the impact of electronic health records on work and patient outcomes. Comput Inform Nurs 2008; 262: 69–77. [DOI] [PubMed] [Google Scholar]
- 23. New York Times. https://well.blogs.nytimes.com/2011/02/02/caring-for-the-chart-or-the-patient/. Accessed November 11, 2018.
- 24. Joshi KG. I am not a checklist. BMJ 2016; 355: i6023. [Google Scholar]
- 25. McMullen PC, Howie WO, Philipsen N, et al. Electronic medical records and electronic health records: overview for nurse practitioners. JNP 109: 660–665. [Google Scholar]
- 26. Verghese A. How tech is turning doctors into clerical workers. New York Times. May 18, 2018. https://www.ntimes.com/interactive/2018/05/16/magazine/health-issue-what-we-lose-with-data-driven-medicine.html. Accessed November 11, 2018. [Google Scholar]
- 27. Downing NL, Bates DW, Longhurst CA.. Physician burnout in the electronic health record era: are we ignoring the real cause? Ann Int Med 2018; 1691: 50–51. doi:10.7326/M18-0139v. [DOI] [PubMed] [Google Scholar]
- 28. Fernández-Alemán JL, Señor IC, Lozoya PÁ, et al. Security and privacy in electronic health records: a systematic literature review. J Biomed Inform 2013; 464: 541–62. [DOI] [PubMed] [Google Scholar]
- 29. Bourgeois FC, DesRoches CM, Bell SK.. Ethical challenges raise by OpenNotes for pediatric and adolescent patients. Pediatrics 2018; 1416: e20172745.. [DOI] [PubMed] [Google Scholar]
- 30. Erickson SM, Rockwern B, Koltov M, et al. Putting patients first by reducing administrative tasks in health care: a position paper of the American College of Physicians. Ann Intern Med 2017; 1669: 659–61. [DOI] [PubMed] [Google Scholar]
- 31. Reisman M. The challenge of making electronic data usable and interoperable. P T 2017; 429: 572–5. [PMC free article] [PubMed] [Google Scholar]
- 32. Adler-Milstein J, Pfeifer E.. Information blocking: is it occurring and what policy strategies can address it? Milbank Q 2017; 951: 117–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. American Medical Association. Debunking regulatory myths. https://www.ama-assn.org/practice-management/debunking-regulatory-myths. Accessed November 11, 2018.
- 34. Mandl KD, Kohane IS.. Escaping the EHR trap—the future of health IT. N Engl J Med 2012; 36624: 2240–2. [DOI] [PubMed] [Google Scholar]
- 35. Protti D, Johansen I.. Widespread adoption of information technology in primary care physician offices in Denmark: a case study. Issue Brief (Commonw Fund) 2010; 80: 1–14. [PubMed] [Google Scholar]
- 36.Allscripts. Israel: a case study in national connectivity for better health. https://www.allscripts.com/news-insights/blog/blog/2017/02/israel-a-case-study-in-national-connectivity-for-better-health. Accessed November 18, 2018.
- 37. Glaser E, Richard C, Lussier MT.. The impact of a patient web communication intervention on reaching treatment suggested guidelines for chronic diseases: a randomized controlled trial. Patient Educ Couns 2017; 10011: 2062–70. [DOI] [PubMed] [Google Scholar]
- 38. Scott D, Purves I.. Triadic relationship between doctor, computer and patient. Interacting Comput 1996; 84: 347–63. [Google Scholar]
- 39. Pearce C. Computers, patients, and doctors—theoretical and practical perspectives In: Shachak A, Borycki EM, Reis SP, eds. Health Professionals' Education in the Age of Clinical Information Systems, Mobile Computing and Social Networks. London: Elsevier, Academic Press; 2017: 5–22. [Google Scholar]
- 40. Stevens LA, DiAngi YT, Schremp JD, et al. Designing an individualized EHR learning plan for providers. Appl Clin Inform 2017; 83: 924–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Mann WR, Slaboch J.. Computers in the exam room—friend or foe? Perm J 2004; 84: 49–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lee W, Alkureishi M, Wroblewski K, Farnan J, Arora V.. Incorporating the human touch: piloting a curriculum for patient-centered electronic health record use. Med Educ Online 2017; 221: 1396171.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Levy S. Nurse education in the digital age—a perspective from the United Kingdom In: Shachak A, Borycki EM, Reis SP, eds. Health Professionals' Education in the Age of Clinical Information Systems, Mobile Computing and Social Networks. London: Elsevier, Academic Press; 2017: 289–97. [Google Scholar]
- 44. Wald H, George P, Reis SP, Taylor JS.. Electronic health record training in undergraduate medical education: bridging theory to practice curricula for empowering patient-and relationship-centered care in the computerized setting. Acad Med 2014; 893: 380–6. [DOI] [PubMed] [Google Scholar]
- 45. Makoul G. The SEGUE framework for teaching and assessing communication skills. Patient Educ Couns 2001; 451: 23–34. [DOI] [PubMed] [Google Scholar]
- 46. Assis-Hassid S, Reychav I, Heart T, Pliskin JS, Reis S.. Enhancing patient-doctor-computer communication in primary care: towards measurement construction. Isr J Health Policy Res 2015; 4: 4.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hersh WR, Gorman PN, Biagioli FE, et al. Beyond information retrieval and EHR use: competencies in clinical informatics for medical education. Adv Med Educ Pract 2014; 5: 205–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Hersh WR, Biagioli FE, et al. From competencies to competence: model, approach, and lessons learned from implementing a clinical informatics curriculum for medical students In: Shachak A, Borycki EM, Reis SP, eds. Health Professionals' Education in the Age of Clinical Information Systems, Mobile Computing and Social Networks. London: Elsevier, Academic Press; 2017: 269–87. [Google Scholar]
- 49. Alkureishi M, Lee W, Farnan J, et al. Breaking away from the iPatient to care for the real patient: implementing a patient-centered EMR use curriculum. MedEdPORTAL 2014; 10: 9953. [Google Scholar]
- 50. Alkureishi M, Lee W, Webb S, et al. Integrating patient-centered electronic health record communication training into resident onboarding: curriculum development and post-implementation survey among housestaff. JMIR Med Educ 2018; 41: e1.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Alkureishi M, Lee W, Lyons M, Wroblewski K, Farnan J, Arora V.. Electronic-clinical evaluation exercise (e-CEX): a new patient-centered EHR use tool. Patient Educ Couns 2018; 1013: 481–9. [DOI] [PubMed] [Google Scholar]
- 52. Sulmasy LS, Bledsoe TA; ACP Ethics, Professionalism and Human Rights Committee. American College of Physicians Ethics Manual: Seventh Edition. Ann Intern Med 2019; 170 (2_Supplement): S1–32. doi:10.7326/M18-2160. [DOI] [PubMed] [Google Scholar]
- 53. Toll ET. The other office. J Am Med Inform Assoc 2019; 261: 71–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ratanawongsa N, Matta GY, Bohsali FB, Chisolm MS.. Reducing misses and near misses related to multitasking on the electronic health record: observational study and qualitative analysis. JMIR Hum Factors 2018; 51: e4.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Martel ML, Imdieke BH, Holm KM, et al. Developing a medical scribe program at an academic hospital: the Hennepin County Medical Center Experience. Jt Comm J Qual Patient Saf 2018; 445: 238–49. [DOI] [PubMed] [Google Scholar]
- 56. American Medical Association. Implementing team-based care. https://www.stepsforward.org/modules/team-based-care. Accessed November 18, 2018.
- 57. Sato L., Augello TA. Better, Safer Care: Imagining a Medical Record of the Future. https://www.rmf.harvard.edu/Clinician-Resources/Podcast/2012/EMR-of-the-future. Accessed November 18, 2018.
- 58. McBride S, Tietze M, Robichaux C, et al. Identifying and addressing ethical issues with use of electronic health records. J Issues Nurs 2018; 23 http://ojin.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Vol-23-2018/No1-Jan-2018/Identifying-and-Addressing-Ethical-Issues-EHR.html. Accessed March 1, 2019. [Google Scholar]
- 59.Electronic Health Records and PAs: A White Paper. 2017. https://www.aapa.org/wp-content/uploads/2017/12/EHR_AAPA-White-Paper-Final-11-17.pdf. Accessed March 1, 2019.
- 60. Pozdnyakova A, Laiteerapong N, Volerman A, et al. Impact of medical scribes on physician and patient satisfaction in primary care. J Gen Intern Med 2018; 337: 1109–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Jerzak J. Radical redesign: the power of team-based care. Ann Fam Med 2017; 153: 281.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Sinsky CA. Moving our attention from keyboards to patients: a way forward for improving professional fulfillment and health care value. Jt Comm J Qual Patient Saf 2018; 44: 235–7. J Am Med Inform Assoc 2013; 21: e100–106. 10.1016/j.jcjq.2018.01.003. Epub 2018 April 26. Accessed June 6, 2019. [DOI] [PubMed] [Google Scholar]
- 63. Mundt MP, Gilchrist VJ, Fleming MF, Zakletskaia LI, Tuan WJ, Beasley JW.. Effects of primary care team social networks on quality of care and costs for patients with cardiovascular disease. Ann Fam Med 2015; 132: 139–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Ventres W, Kooienga S, Marlin R.. EHRs in the exam room: tips on patient-centered care. Fam Pract Manag 2006; 133: 45–7. [PubMed] [Google Scholar]
- 65. Lawal AK, Rotter T, Kinsman L, et al. Lean management in health care: definition, concepts, methodology and effects reported (systematic review protocol). Syst Rev 2014; 3: 103.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Payne TH, Corley S, Cullen TA, et al. Report of the AMIA EHR-2020 Task Force on the status and future direction of EHRs. J Am Med Inform Assoc 2015; 225: 1102–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Woods SS, Evans NC, Frisbee KL.. Integrating patient voices into health information for self-care and patient-clinician partnerships: Veterans Affairs design recommendations for patient-generated data applications. J Am Med Inform Assoc 2016; 233: 491–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Mafi JN, Gerard M, Chimowitz H, et al. Patients contributing to their doctors' notes: insights from expert interviews. Ann Intern Med 2018; 1684: 302–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Why you should share notes with patients. Posted by Tom Delbanco, MD, MACP, Co-Founder, OpenNotes 2018. https://blog.meditech.com/author/tom-delbanco-md-macp-co-founder-opennotes. Accessed March 1, 2019.
- 70. Yu MM, Weathers AL, Wu AD, Evans DA.. Sharing notes with patients: a review of current practice and considerations for neurologists. Neurol Clin Pract 2017; 72: 179–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Ranney ML, Choo EK, Cunningham RM, et al. Acceptability, language, and structure of text message-based behavioral interventions for high-risk adolescent females: a qualitative study. J Adolesc Health 2014; 551: 33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Hogan AH, Rastogi D, Rinke ML.. A quality improvement Intervention to improve inpatient pediatric asthma controller accuracy. Hosp Pediatr 2018; 83: 127–34. [DOI] [PubMed] [Google Scholar]
- 73. Veazie S, Winchell K, Gilbert J, et al. Rapid evidence of mobile applications for self-management of diabetes. J Gen Intern Med 2018; 337: 1167–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Kruse CS, Krowski N, Rodriguez B, et al. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open 2017; 78: e016242. [DOI] [PMC free article] [PubMed] [Google Scholar]