Abstract
Study objectives
Insomnia is the most common sleep disorder with significant psychiatric/physical comorbidities in the general population. The aim of this study is to investigate whether socioeconomic and demographic factors are associated with gender differences in insomnia and subtypes in Korean population.
Method
The present study used data from the nationwide, cross-sectional study on sleep among all Koreans aged 19 to 69 years. The Insomnia Severity Index (ISI) was used to classify insomnia symptoms and their subtypes (cutoff value: 9.5). The Pittsburgh Sleep Quality Index (PSQI), Goldberg Anxiety Scale (GAS) and Patient Health Questionnaire-9 (PHQ-9) were used to measure sleep quality, anxiety and depression.
Results
A total of 2695 participants completed the survey. The overall prevalence of insomnia symptoms was 10.7%, including difficulty in initiating sleep (DIS) (6.8%), difficulty in maintaining sleep (DMS) (6.5%) and early morning awakening (EMA) (6.5%), and these symptoms were more prevalent in women than in men. Multivariate analysis showed that female gender, shorter sleep time and psychiatric complications were found to be independent predictors for insomnia symptoms and subtypes. After adjusting for covariates among these factors, female gender remained a significant risk factor for insomnia symptoms and their subtypes. As for men, low income was related to insomnia.
Conclusion
Approximately one-tenth of the sample from the Korean general population had insomnia symptoms. The prevalence of insomnia symptom and the subtypes were more prevalent in women than men. Gender is an independent factor for insomnia symptoms.
Introduction
Insomnia is the most common sleep disorder in the general population. It is associated with impaired social performance, cultural difference and daytime functioning, along with other psychological/physical conditions [1–3]. Insomnia affects 6–18% of the general population [4–7]. Therefore, insomnia imposes a significant personal and social burden [8]. Insomnia prevalence varies according to the definition of insomnia or insomnia symptom [9].
Different insomnia symptoms have been defined as subtypes of insomnia. These subtypes include difficulty in initiating sleep (DIS), difficulty in maintaining sleep (DMS) and early morning awakening (EMA) [9]. There are differences in the prevalence, association with excessive daytime sleepiness and psychiatric comorbidities among these subtypes [10].
Gender, age, socioeconomic status and psychiatric comorbidities are known to be significant factors for insomnia prevalence [9]. The elderly population has an increased insomnia prevalence compared to the young or middle age population in almost all epidemiological studies [11–13]. Insomnia prevalence is stable from 15 to 44 years of age and increases over 45 years [9]. Insomnia prevalence is typically higher among individuals with lower incomes and lower education levels [14]. However, some studies have reported contradictory results [15, 16]. The association between insomnia and psychiatric disorders has been repeatedly demonstrated. Approximately 90% and 80% of individuals with anxiety and depression had insomnia symptoms in cross-sectional studies, respectively [17, 18]. Longitudinal studies confirmed the close association of anxiety and depression with insomnia [16, 19].
Short sleep time and poor sleep quality are significant factors for insomnia. A survey in six European countries showed that a significant proportion of individuals with insomnia had short sleep times either voluntarily or non-voluntarily [20]. The authors classified sleep deprivation as a subtype of insomnia. Poor sleep quality is also common among individuals with insomnia [21].
Female gender has been recognized as a significant factor for insomnia. Epidemiological studies have consistently shown a higher prevalence of insomnia symptoms among women compared to men [22–24]. The difference in insomnia prevalence between women and men increases with age [9]. In addition to insomnia or insomnia symptoms, women report more frequent dissatisfaction with sleep and the daytime consequences of insomnia [4, 22, 24].
Nevertheless, information regarding gender differences in insomnia subtypes is currently limited. In addition, gender differences in insomnia symptoms adjusting for significant covariates have rarely been reported. The purpose of this study is to investigate gender differences in insomnia symptoms and their subtypes regarding covariates using population data in South Korea.
Methods
Study population and survey process
The present study population was collected from cross-sectional surveys. In brief, it was a nationwide, cross-sectional study on sleep among Koreans aged 19 to 69 years. We used a two-stage clustered random sampling method proportional to the population and socioeconomic distribution for all Korean territories. The study protocol was approved by the institutional review board/ethics committee of Hallym University Sacred Heart Hospital in Korea(Approval No. 2011-I077), conducted according to the principles expressed in the Declaration of Helsinki.; Participants provided their written informed consent to participate in this study. Trained interviewers conducted structured interviews using a questionnaire to assess sleep time, sleepiness, anxiety and depression using a face-to-face interview. The interview included questions on sleep status. To minimize potential interest bias, we informed candidates that the topic of the survey was social health issues rather than sleep issues. All interviewers were employed by Gallup Korea and had previous social survey interviewing experience.
Assessment for sleep time
We asked all participants to report their usual sleep time in terms of hours and minutes, separately for workdays and free days, during the past month. The average sleep time was a weighted mean of the sleep time on workdays and free days, calculated as ([workday sleep time x 5] + [free day sleep time x 2))/7. Short sleep time was defined as an average sleep time of <6 h [25].
Assessment for insomnia symptom and poor sleep quality
The Insomnia Severity Index (ISI) was used to classify insomnia symptoms. The ISI is a self-reporting, brief screening measure of insomnia that contains questions corresponding in part to the diagnostic criteria of insomnia [26]. The ISI comprises seven items concerning the severity of sleep-onset difficulty, sleep-maintaining difficulty, early awakening and satisfaction with sleep patterns. Each item was rated on a 0–4 scale [27]. The ISI was previously validated with good sensitivity and specificity and showed a 9.5 cut-off score for discriminating patients with “insomnia symptoms” in the population-based sample [28]. Among those who satisfy this definition (ISI score ≥ 10), we further classified the subtypes of insomnia symptoms as difficulty in initiating sleep (DIS), difficulty in maintaining sleep (DMS) and early morning awakening (EMA) if a participant responded with ≥ 2 on the scale (intermediate or higher) for those items [20]. The Pittsburgh Sleep Quality Index (PSQI) was used to measure sleep quality. If a participant’s PSQI score was 6 or higher, she/he was classified as having poor sleep quality [29].
Anxiety and depression assessment
We used the Goldberg Anxiety Scale (GAS) to diagnose anxiety among participants. The GAS questionnaire was composed of nine items: four screening items and five supplementary items. Anxiety was diagnosed when there were positive answers to two or more screening items and five or more of all scale items [30]. The Korean version of the scale has a sensitivity of 82.0% and specificity of 94.4% for diagnosing anxiety [31].
The Patient Health Questionnaire-9 (PHQ-9) was used to diagnose depression [32]. It is composed of nine items each scored 0 to 3. Participants who scored 10 or higher on this measure were considered to have depression. The Korean PHQ-9 has a sensitivity of 81.8% and specificity of 89.9% [33].
Statistical analysis
The Kolmogorov–Smirnov test was used to confirm the normality of the distribution. The Student’s t-test was used to compare continuous variables after the normality of the sample was confirmed. Post hoc analyses were performed using Tukey’s method. Categorical variables were compared using the Chi-square test. The significance level was set at p < 0.05 for all analyses.
We calculated the odds ratios (ORs) with 95% confidence intervals (CIs) for the occurrence of insomnia symptoms and their subtypes through univariable and multivariable logistic regression analyses. In univariable analyses, we modelled the ORs for insomnia symptoms without adjusting for covariates. In multivariable analyses, we used four models. In Model 1, adjustment was conducted for sociodemographic variables (age, gender, size of residential area and educational level) and short sleep time. Model 2 incorporated anxiety (GAS score) with Model 1. Model 3 included depression (PHQ-9 score ≥ 10) with Model 1. The final model, Model 4, incorporated poor sleep quality (PSQI score ≥ 6), anxiety and depression with Model 1. Statistical analyses were performed using the Statistical Package for Social Sciences 23.0 (IBM, Armonk, NY, USA).
Results
Survey
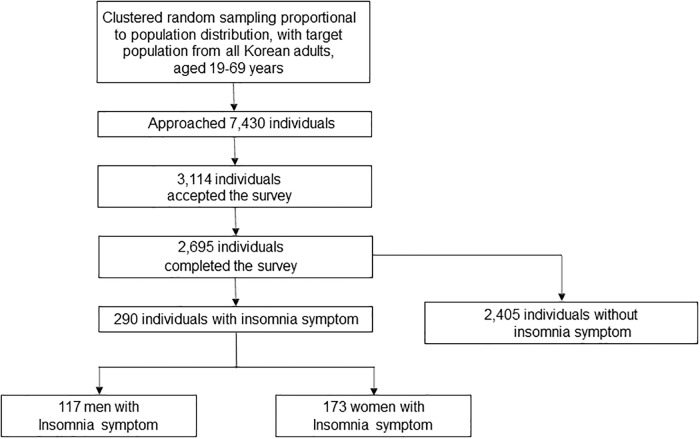
The interviewers approached 7,430 individuals and 3114 of them agreed to take the survey. After 352 individuals suspended the interview, 2695 participants completed the survey (cooperation rate of 36.2%; Fig 1). The distributions of age, gender, size of residential area and educational level were not significantly different from those of the general population of Korea. (Table 1).
Fig 1. Flow chart depicting the participation of subjects in the Korean headache-sleep study.
Table 1. Sociodemographic characteristics of survey participants; the total Korean population; and cases identified as having insomnia.
| Survey participants N (%) | Total population N (%) | P | Poor sleep quality N, % (95% CI) | p | Insomnia N, % (95% CI) | p | Short sleep time | p | Average sleep time (hours + SD) | P | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | |||||||||||
| Men | 1,345 (49.3) | 17,584,365 (50.6) | 0.854a | 334, 24.8 (22.5–27.1) | 0.046 | 117, 8.7 (7.2–10.2) | 0.001 | 141, 10.5 (8.8–12.1) | 0.727 | 7.3 + 1.2 | 0.109 |
| Women | 1,350 (50.7) | 17,198,350 (49.4) | 381, 28.2 (25.8–30.6) | 173, 12.8 (11.0–14.6) | 136, 10.1 (8.5–11.7) | 7.3 + 1.2 | |||||
| Age | |||||||||||
| 19–29 | 542 (20.5) | 7,717,947 (22.2) | 0.917a | 153, 28.3 (24.4–32.0) | 0.028 | 59, 10.9 (9.2–12.6) | 0.426 | 45, 8.3 (6.0–10.6) | 0.002 | 7.6 + 1.3 | <0.001 |
| 30–39 | 604 (21.9) | 8,349,487 (24.0) | 136, 22.5 (19.2–25.9) | 53, 8.8 (7.3–10.3) | 42, 7.0 (4.9–9.0) | 7.5 + 1.1 | |||||
| 40–49 | 611 (23.1) | 8,613,110 (24.8) | 167, 27.3 (23.8–30.1) | 66, 10.8 (9.1–12.5) | 73, 11.9 (9.4–14.5) | 7.1 + 1.2 | |||||
| 50–59 | 529 (18.9) | 6,167,505 (17.7) | 160, 30.2 (26.3–34.2) | 63, 11.9 (10.2–13.6) | 70, 13.2 (10.3–16.1) | 7.1 + 1.3 | |||||
| 60–69 | 409 (15.6) | 3,934,666 (11.3) | 99, 24.2 (20.0–28.4) | 49, 12.0 (10.2–13.7) | 47, 11.5 (8.4–14.6) | 7.1 + 1.2 | |||||
| Size of residential area | |||||||||||
| Large city | 1,248 (46.3) | 16,776,771 (48.2) | 0.921a | 338, 27.1 (24.6–30.0) | 0.541 | 136, 10.9 (9.2–12.6) | 0.945 | 131, 10.5 (8.8–12.2) | 0.670 | 7.3 + 1.2 | 0.471 |
| Medium-to-small city | 1186 (44.0) | 15,164,345 (43.6) | 303, 25.5 (23.1–28.0) | 125, 10.5 (8.9–12.2) | 116, 9.8 (8.1–11.5) | 7.3 + 1.2 | |||||
| Rural area | 261 (9.7) | 2,841,599 (8.2) | 74, 28.4 (22.8–33.9) | 29, 11.1 (9.4–12.8) | 30, 11.5 (7.6–15.4) | 7.3 + 1.3 | |||||
| Education | |||||||||||
| Middle school or Less | 393 (14.9) | 6,608,716 (19.0) | 0.752a | 110, 28.0 (23.5–32.4) | 0.917 | 62, 15.8 (13.8–17.7) | 0.006 | 47, 12.0 (8.7–15.2) | 0.514 | 7.2 + 1.4 | 0.012 |
| High school | 1,208 (44.5) | 15,234,829 (43.8) | 317, 26.2 (24.0–28.7) | 116, 9.6 (8.0–11.2) | 127, 10.5 (8.8–12.3) | 7.2 + 1.3 | |||||
| College or more | 1,068 (39.6) | 12,939,170 (37.2) | 281, 26.3 (23.7–29.0) | 109, 10.2 (8.6–11.8) | 100, 9.4 (7.6–11.1) | 7.4 + 1.3 | |||||
| Not responded | 26 (9.6) | 7, 26.9 (8.7–45.2) | 3, 1.0 (0.9–1.3) | 3, 11.5 (0.0–24.7) | 7.4 +1.2 | ||||||
| Total | 2695 (100.0) | 34,782,715 (100.0) | 715, 26.5 (24.8–28.2) | 290, 10.7 (9.1–12.4) | 277, 10.3 (9.1–11.4) | 7.4 + 1.3 |
aComparison of gender, age group, size of residential area, and educational level distributions between the sample in the present study and the total population of Korea
Abbreviations: CI = confidence interval
Prevalence of insomnia and poor sleep quality
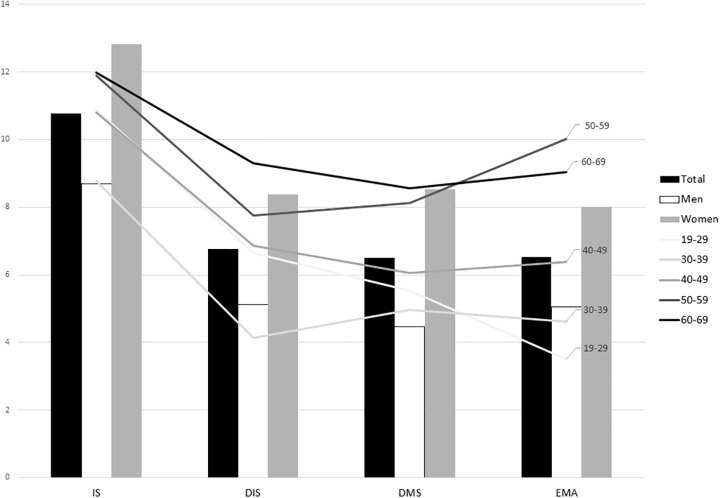
Of the 2695 participants, 290 (10.7%) were classified as having insomnia symptoms according to the ISI score. Seven-hundred and fifteen (26.5%) participants who reported PSQI scores higher than 5 were classified as having poor sleep quality. 182 (6.8% of all participants) were accompanied by DIS, 175 (6.5%) with DMS and 176 (6.5%) with EMA (Fig 2).
Fig 2. Prevalence of insomnia symptoms in men and women with different age groups.
p was calculated by χ2 test. Abbreviations: IS = Insomnia Symptoms, DIS = Difficulty in Initiating Sleep; DMS = Difficulty in Maintaining Sleep; EMA = Early Morning Awakening.
Demographic characteristics, psychiatric comorbidities and short sleep time according to the presence of insomnia symptom
The mean age of participants with insomnia symptoms did not significantly differ from participants without insomnia symptoms (43.8 ± 14.2 vs. 42.9 ± 13.7, p = 0.823). The proportion of women was higher among participants with insomnia symptoms than those without insomnia symptoms (59.6% vs. 49.1%, p < 0.001). The prevalence of anxiety and depression was significantly higher among participants with insomnia symptoms than in those without (40.3% vs. 6.3%, p < 0.001 for anxiety and 25.9% vs. 1.7%, p < 0.001 for depression). The average sleep time of all participants was 7.4 ± 1.3 h.
Two-hundred and seventy-seven (10.3%) participants were classified as having short sleep time. The average sleep time of participants with insomnia symptoms was significantly shorter than that of participants without insomnia symptoms (6.7 ± 1.5 h vs. 7.4 ± 1.2 h, p < 0.001). The prevalence of short sleep time (< 6 hours of average sleep time) was higher among participants with insomnia symptoms (35.5% vs. 15.2%, p < 0.001; Table 2).
Table 2. Distribution of demographic, social and lifestyle factors according to the presence of insomnia symptoms.
| Subjects with IS N = 290 | Subjects without IS N = 2405 | P-value | |
|---|---|---|---|
| Demographics | |||
| Mean age ± SD (years) | 43.76±14.20 | 42.88±13.70 | 0.366 |
| Women, N (%) | 173 (59.6) | 1182 (49.1) | 0.001 |
| Education level | |||
| Middle school or less | 62 | 331 | 0.006 |
| High school | 116 | 1092 | |
| College or more | 109 | 959 | |
| Not responded | 3 | 23 | |
| Residential area | |||
| Large city | 136 | 1112 | 0.943 |
| Medium-to-small city | 125 | 1061 | |
| Rural area | 29 | 232 | |
| Smoking, N (%) | 78 (26.9) | 666 (27.7) | 0.486 |
| Alcohol, N (%) | 185 (63.8) | 1597 (66.4) | 0.313 |
| ISI score, ± SD | 14.37±4.39 | 2.47±2.50 | |
| Anxiety, N (%) | 117 (40.3) | 151 (6.3) | <0.001 |
| Depression, N (%) | 75 (25.9) | 41 (1.7) | <0.001 |
| BMI, ± SD (kg/cm^2) | 23.09± 3.30 | 22.94± 2.97 | 0.031 |
| Average sleep duration, ± SD, N (short sleep duration) | 6.68± 1.54 (103) | 7.36± 1.17 (366) | <0.001 |
| Poor sleep quality, N (%) | 221 (76) | 494 (20.5) | <0.001 |
p was calculated by χ2 test or student’s t test.
Abbreviations: IS–Insomnia symptoms
Prevalence of insomnia symptoms in women and men
A higher percentage of women reported insomnia symptoms compared to men (12.8% vs. 8.7%, p = 0.001). The mean ISI score was significantly higher in women compared to men (4.2 ± 4.9 vs. 3.3 ± 4.2, p < 0.001). All subtypes of insomnia symptoms including DIS (8.3% vs. 5.1%, p < 0.001), DMS (8.5% vs. 4.4%, p < 0.001) and EMA (8.0% vs. 5.0%, p = 0.001) were more prevalent in women than men (Fig 2).
Insomnia severity of women and men among participants with insomnia
Among 290 participants with insomnia symptoms, the total ISI score was not significantly different between women and men (14.6 ± 4.4 vs. 14.0 ± 4.3, p = 0.199). The prevalence of DIS (37.6% vs. 33.3%, p = 0.460), DMS (40.5% vs. 32.5%, p = 0.168) and EMA (36.4% vs. 29.9%, p = 0.251) did not significantly differ between women and men.
Factors associated with insomnia symptoms in women and men
When comparing participants with insomnia symptoms to participants without insomnia symptoms, age, size of residential area and education level did not significantly affect the prevalence of insomnia. In contrast, female gender (OR = 1.3, 95% CI = 1.0–1.78), short sleep time (OR = 2.6, 95% CI = 1.9–3.5), anxiety (OR = 6.0, 95% CI = 4.3–8.3) and depression (OR = 9.6, 95% CI = 6.0–15.3) were found to be independent predictors of insomnia symptoms in multiple regression analysis (Table 3).
Table 3. Univariable and multivariable regression analysis for insomnia symptoms.
| Univariable ORs | Multivariable analysis ORs | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model4 | |||||||
| OR (95%Ci) | p-value | OR (95%Ci) | p-value | OR (95%Ci) | p-value | OR (95%Ci) | p-value | OR (95%Ci) | p-value | |
| Sex (Women) | 1.543 (1.204–1.977) | 0.001 | 1.513 (1.172–1.953) | 0.001 | 1.401 (1.068–1.839) | 0.015 | 1.388 (1.057–1.824) | 0.018 | 1.327 (1.000–1.760) | 0.05 |
| Age (40 years or older) | 1.199 (0.934–1.539) | 0.155 | 0.928 (0.702–1.226) | 0.599 | 0.938 (0.698–1.261) | 0.673 | 1.028 (0.762–1.387) | 0.856 | 0.999 (0.734–1.361) | 0.997 |
| Size of residential area (Large city) | 1.027 (0.804–1.311) | 0.831 | 1.037 (0.807–1.332) | 0.779 | 1.004 (0.768–1.312) | 0.977 | 1.010 (0.771–1.321) | 0.944 | 0.990 (0.749–1.308) | 0.943 |
| Education (Middle school or less) | 1.707 (1.260–2.314) | 0.001 | 1.552 (1.105–2.180) | 0.011 | 1.427 (0.993–2.051) | 0.055 | 1.556 (1.083–2.235) | 0.017 | 1.473 (1.009–2.150) | 0.045 |
| Sleep duration (6 hours or shorter) | 3.069 (2.354–4.000) | <0.001 | 3.081 (2.348–4.042) | <0.001 | 2.738 (2.039–3.675) | <0.001 | 2.780 (2.069–3.736) | <0.001 | 2.604 (1.913–3.544) | <0.001 |
| Anxiety | 10.095 (7.579–13.447) | <0.001 | 9.284 (6.910–12.473) | <0.001 | 6.014 (4.344–8.325) | <0.001 | ||||
| Depression | 20.113 (13.409–30.170) | <0.001 | 18.626 (12.243–28.336) | <0.001 | 9.588 (6.026–15.257) | <0.001 | ||||
In Model 1, adjustment was conducted for sociodemographic variables (age, sex, size of residential area and educational level) and short sleep time. Model 2 incorporated anxiety (GAS score) with Model 1. Model 3 included depression (PHQ-9 score ≥ 10) with Model 1. The final model, Model 4, incorporated poor sleep quality (PSQI score ≥ 6), anxiety and depression with Model 1. Subject with missing data was excluded from the analysis.
p was calculated by the univariable / multiple logistic regression analysis.
Abbreviations: OR = odds ratio, CI = confidence interval.
For DIS, female gender (OR = 1.4, 95% CI = 1.0–2.0), short sleep time (OR = 3.1, 95% CI = 2.1–4.4), anxiety (OR = 5.0, 95% CI = 3.4–7.3) and depression (OR = 9.6, 95% CI = 6.0–15.5) were found to be independent predictors (S1 Table).
In univariable analysis, age was a significant predictor of DIS (1.5, 95% CI = 1.1–2.1) and DMS (OR = 1.5, 95% CI = 1.1–2.0). However, age lost significance for DIS (p = 0.235) and DMS (p = 0.219) in multiple regression analysis. Female gender (OR = 1.8, 95% CI = 1.2–2.6), short sleep time (OR = 2.5, 95% CI = 1.7–3.7), anxiety (OR = 5.2, 95% CI = 3.6–7.7) and depression (OR = 8.6, 95% CI = 5.3–13.9) were significant predictors of DMS in multiple regression analysis (S2 Table).
In multiple regression analysis for EMA, female gender (OR = 1.4, 95% CI = 1.0–2.0), age (OR = 1.8, 95% CI = 1.2–2.6), educational level (OR = 1.6, 95% CI = 1.1–2.5), short sleep time (OR = 3.7, 95% CI = 2.6–5.3), anxiety (OR = 5.1, 95% CI = 3.4–7.6) and depression (OR = 5.7, 95% CI = 3.4–9.4) were independent predictors (S3 Table).
Women showed similar result aspects. In multiple regression analysis for insomnia symptoms, short sleep time (OR = 2.2, 95% CI = 1.4–3.3), anxiety (OR = 6.1, 95% CI = 4.0–9.3), and depression (OR = 6.9, 95% CI = 3.8–12.3) were significant predictors. Those factors also had significance for insomnia symptoms, DIS, DMS and EMA in multiple regression analysis for both genders. Additionally, relatively low monthly income was a significant risk factor for men in insomnia symptoms and their subtypes (Table 4), while no socio-economic risk factor was related to female insomnia. (S4 Table).
Table 4. Univariable and multivariable regression analysis for insomnia symptoms and insomnia subtypes in men.
| Multivariable analysis ORs | ||||||||
|---|---|---|---|---|---|---|---|---|
| IS | DIS | DMS | EMA | |||||
| OR (95%Ci) | p-value | OR (95%Ci) | p-value | OR (95%Ci) | p-value | OR (95%Ci) | p-value | |
| Age (40 years or older) | 0.772 (0.479–1.244) | 0.287 | 1.204 (0.653–2.222) | 0.552 | 1.220 (0.630–2.362) | 0.555 | 1.469 (0.767–2.816) | 0.246 |
| Size of residential area (Large city) | 1.433 (0.919–2.235) | 0.113 | 1.420 (0.809–2.493) | 0.222 | 1.104 (0.607–2.010) | 0.745 | 0.932 (0.523–1.659) | 0.810 |
| Education (Middle school or less) | 0.869 (0.411–1.836) | 0.713 | 0.598 (0.236–1.517) | 0.279 | 0.865 (0.362–2.071) | 0.745 | 0.810 (0.345–1.900) | 0.628 |
| Sleep duration (6 hours or shorter) | 3.489 (2.177–5.591) | <0.001 | 3.664 (2.055–6.533) | <0.001 | 3.247 (1.756–6.006) | <0.001 | 4.855 (2.724–8.654) | <0.001 |
| Anxiety | 6.031 (3.517–10.341) | <0.001 | 6.059 (3.215–11.419) | <0.001 | 9.307 (4.113–21.061) | <0.001 | 6.849 (3.630–12.922) | <0.001 |
| Depression | 18.158 (8.267–39.882) | <0.001 | 12.766 (5.677–28.711) | <0.001 | 5.578 (2.855–10.900) | <0.001 | 7.614 (3.306–17.536) | <0.001 |
| Monthly income (<,2000 dollar) | 2.030 (1.130–3.645) | 0.018 | 2.006 (0.988–4.074) | 0.054 | 2.776 (1.363–5.653) | 0.005 | 2.477 (1.231–4.984) | 0.011 |
| Occupation (unemployed) | 1.174 (0.644–2.141) | 0.600 | 1.487 (0.708–3.123) | 0.295 | 0.798 (0.338–1.881) | 0.606 | 0.834 (0.360–1.928) | 0.671 |
Subject with missing data was excluded from the analysis.
p was calculated by the univariable / multiple logistic regression analysis.
Abbreviations: OR = odds ratio, CI = confidence interval, IS = Insomnia Symptoms, DIS = Difficulty in Initiating Sleep, DMS = Difficulty in Maintaining Sleep, EMA = Early Morning Awakening
Discussion
The main findings of the present study were as follows: 1) The prevalence of insomnia symptoms in a Korean general population-based sample was 10.7% and 2) The prevalence of insomnia symptoms was significantly higher in women than men. Among the subtypes of insomnia symptoms, there was a higher prevalence of DIS, DMA and EMA in women than in men and 3) Female gender was a significant factor for insomnia symptoms even after adjusting for covariates including sociodemographic variables, short sleep time, anxiety and depression.
General insomnia prevalence was similar with that reported in previous study [34]. Gender differences in insomnia disorder or insomnia symptoms have also been demonstrated in epidemiological studies. A meta-analysis combining data from 29 studies reported that women were at a 41% greater risk for having insomnia than men in adult populations [22]. Our results are in agreement with the previous findings that women had more insomnia symptoms than men.
What are possible mechanisms for higher insomnia prevalence in women? One possible explanation is roles of sex steroids. The major gonadal sex steroids are estrogen and progesterone in women and testosterone in men [35]. Sleep complaints typically co-occur in women with the fluctuation of ovarian steroids such as puberty, pregnancy, the menstrual cycle and the menopausal period [36–38]. Estrogen replacement therapy improves sleep disturbances in menopausal women [37]. In men, androgen deprivation therapy worsens insomnia in prostate cancer patients [38, 39]. On the contrary, high-dose testosterone replacement was associated with a reduction of sleep efficacy and total sleep time [40]. In summary, low or fluctuating levels of estrogen was consistently associated with increase occurrence of sleep disturbances including insomnia in women. Nevertheless, role of testosterone level on sleep in men is currently uncertain owing to inconsistent results.
Another possible explanation is role of biological gender. Androgen and estrogen affect differently on sleep between women and men. Gonadectomized female and male rats showed no significant difference in NREM and REM sleep amount. However, estradiol replacement significantly reduces NREM and REM sleep time in dark phase in female rats. In contrast, NREM and REM sleep architecture did not change by estradiol treatment in male rats [41]. Therefore, gender difference may be owing to biological gender rather than sex steroids.
The higher prevalence of mood symptoms in women could be a reason for gender difference. Both anxiety and depression are closely associated with sleep disturbances, including insomnia. Epidemiological studies have consistently reported a close association of insomnia with anxiety and depression. A meta-analysis including 21 longitudinal epidemiological studies showed an odds ratio for insomnia to predict depression of 2.60 (confidence interval: 1.98–3.42) [42]. Women preponderance of anxiety and depression has been persistently noted [43, 44]. Therefore, a higher prevalence of anxiety and depression in women may account for the higher prevalence of insomnia in women than men. Nevertheless, insomnia prevalence was significantly higher in women than men even after adjusting for anxiety and depression in the present study (Table 3). Therefore, the higher prevalence of insomnia in women could not be solely explained by the higher prevalence of anxiety and depression in women.
Differences in pain and somatic perception can also explain gender differences in insomnia symptoms. Pain and somatic symptoms are generally more prevalent in women [22, 45]. In particular, pain, insomnia, and somatic symptoms showed significant differences in adults rather than in adolescents before puberty. [46] These differences might speculate the relationship between sex and insomnia symptoms.
The present study showed that all subtypes of insomnia symptoms including DIS, DMS and EMA were more common in women than men. The significant differences in prevalence between women and men persisted even after adjusting for covariates including sociodemographic variables, short sleep time, anxiety and depression. Gender differences in the subtypes of insomnia have been demonstrated in epidemiological studies. Janson et al. reported that female gender was positively related to DMS in a European study [47]. An interview-based study showed a clear correlation between female gender and insomnia symptoms as well as the DMS-IV inclusion criteria [23]. Another study showed that 11.9% (14.0% of women vs. 9.3% of men) of the Hong Kong Chinese adult population complained of insomnia in the preceding month. Insomnia symptoms including DIS, DMS and EMA, more prominently appeared in women than in men. Gender (as women) was a specific risk factor despite common risk factors for insomnia in both genders [24].
The prevalence of EMA only showed significance in older individuals after including anxiety and depression in the adjustment (S3 Table). Still, we found a tendency that prevalence of insomnia symptoms increased with age. In this study, inclusion criteria for participants maximally limited to 69 years, and the size of the sample was small. These are possible explanations for the absence of statistical significance. (Table 1). Gender differences in insomnia prevalence were apparent in the elderly in epidemiological studies. In elderly populations, the risk of insomnia in women was almost doubled compared to that of men. Elderly (>65 years) women had a 73% greater risk of insomnia compared to elderly men [22]. In contrast, the predisposition for insomnia in women did not appear before puberty. These findings suggest a possible role of hormonal changes in the differences in insomnia between women and men [48, 49]. Also, we failed to report lower education levels as independent risk factor for insomnia and all subtypes. The statistical significance of low monthly income in men alone offered weak explanatory power, due to disputes in recent studies [9].
Despite of the low response rate (36.3%), we can speculate the general status of the Korean population through our data: 1) there were no significant differences in the distribution of age, gender, size of residential area, and educational level between survey participants and the Korean general population. 2) The prevalence of insomnia symptoms, anxiety, depression, and short sleep duration in this sample were similar to that of previous studies [4].
The present study has some limitations. First, this study did not use any objective measurement of sleep or sleep disorders such as polysomnography or actigraphy. Nevertheless, we evaluated insomnia symptoms, sleep habits and sleep quality using validated questionnaires via face-to-face interviews. Second, we did not evaluate the use of antidepressants, anxiolytics, hypnotics or caffeine. Antidepressants, anxiolytics or hypnotics may have a positive effect on sleep time and caffeine may negatively affect sleep time. Also, we could not measure sleep-relevant-treatments such as sleep-education, relaxation training or cognitive behavioral therapy for insomnia (CBTI). Third, although the present study was a large population-based study, some subgroup analyses might not have statistical significance due to the limited sample size and low response rate. In other words, the lack of significant findings in subgroup analyses could be due to the small subgroup sample size.
The present study has several strengths. First, the present study included a large sample size across the Korean general population. The distribution of age, gender, size of residential area and educational level of our sample was similar to the Korean population. Second, the present study assessed potential covariates of insomnia symptoms such as sociodemographic variables, poor sleep quality, short sleep time, anxiety and depression, which are related to insomnia symptoms. Third, we investigated gender differences in the subtypes of insomnia symptoms including DIS, DMS and EMA in addition to overall insomnia symptoms. Further, we analyzed the factors affecting insomnia subtypes.
Conclusions
Approximately one-tenth of the Korean general population sample had insomnia symptoms. The prevalence of insomnia symptoms was higher in women than men. Among the subtypes of insomnia symptoms, DIS, DMS and EMA were more prevalent in women than in men. The predisposition of insomnia symptoms in women was prominent even after adjusting for covariates including anxiety and depression.
Supporting information
In Model 1, adjustment was conducted for sociodemographic variables (age, sex, size of residential area and educational level) and short sleep time. Model 2 incorporated anxiety (GAS score) with Model 1. Model 3 included depression (PHQ-9 score ≥ 10) with Model 1. The final model, Model 4, incorporated poor sleep quality (PSQI score ≥ 6), anxiety and depression with Model 1. Subject with missing data was excluded from the analysis. p was calculated by the univariable / multiple logistic regression analysis. Abbreviations: OR = odds ratio, CI = confidence interval.
(DOCX)
In Model 1, adjustment was conducted for sociodemographic variables (age, sex, size of residential area and educational level) and short sleep time. Model 2 incorporated anxiety (GAS score) with Model 1. Model 3 included depression (PHQ-9 score ≥ 10) with Model 1. The final model, Model 4, incorporated poor sleep quality (PSQI score ≥ 6), anxiety and depression with Model 1. Subject with missing data was excluded from the analysis. p was calculated by the univariable / multiple logistic regression analysis. Abbreviations: OR = odds ratio, CI = confidence interval.
(DOCX)
In Model 1, adjustment was conducted for sociodemographic variables (age, sex, size of residential area and educational level) and short sleep time. Model 2 incorporated anxiety (GAS score) with Model 1. Model 3 included depression (PHQ-9 score ≥ 10) with Model 1. The final model, Model 4, incorporated poor sleep quality (PSQI score ≥ 6), anxiety and depression with Model 1. Subject with missing data was excluded from the analysis. p was calculated by the univariable / multiple logistic regression analysis. Abbreviations: OR = odds ratio, CI = confidence interval.
(DOCX)
Subject with missing data was excluded from the analysis. p was calculated by the univariable / multiple logistic regression analysis. Abbreviations: OR = odds ratio, CI = confidence interval, IS = Insomnia Symptoms, DIS = Difficulty in Initiating Sleep, DMS = Difficulty in Maintaining Sleep, EMA = Early Morning Awakening.
(DOCX)
Acknowledgments
The authors would like to thank Gallup Korea for providing technical support.
Abbreviations
- CBTI
Cognitive Behavioral Therapy for Insomnia
- DIS
difficulty in initiating sleep
- DMS
difficulty in maintaining sleep
- EMA
early morning awakening
- GAS
Goldberg Anxiety Scale
- IS
insomnia symptoms
- ISI
The insomnia severity index
- PHQ-9
Patient Health Questionnaire-9
- PSQI
Pittsburgh Sleep Quality Index
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
This study was supported by a 2011 grant from Korean Academy of Medical Sciences and Korean Neurological Association (grant # KNA-10-MI-03). Funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Thase ME. Correlates and consequences of chronic insomnia. General hospital psychiatry 2005;27:100–12. 10.1016/j.genhosppsych.2004.09.006 [DOI] [PubMed] [Google Scholar]
- 2.Benca RM. Diagnosis and treatment of chronic insomnia: a review. Psychiatric services 2005;56:332–43. 10.1176/appi.ps.56.3.332 [DOI] [PubMed] [Google Scholar]
- 3.Léger D, Guilleminault C, Bader G, Lévy E, Paillard M. Medical and socio-professional impact of insomnia. Sleep 2002;25:621–5. [PubMed] [Google Scholar]
- 4.Cao X-L, Wang S-B, Zhong B-L, et al. The prevalence of insomnia in the general population in China: A meta-analysis. PloS one 2017;12:e0170772 10.1371/journal.pone.0170772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yeo B, Perera I, Kok L, Tsoi W. Insomnia in the community. Singapore Med J 1996;37:282–4. [PubMed] [Google Scholar]
- 6.Kim K, Uchiyama M, Okawa M, Liu X, Ogihara R. An epidemiological study of insomnia among the Japanese general population. Sleep 2000;23:41–7. [PubMed] [Google Scholar]
- 7.Ohayon MM, Hong S-C. Prevalence of insomnia and associated factors in South Korea. Journal of Psychosomatic Research 2002;53:593–600. 10.1016/s0022-3999(02)00449-x [DOI] [PubMed] [Google Scholar]
- 8.Daley M, Morin CM, LeBlanc M, Grégoire J-P, Savard J. The economic burden of insomnia: direct and indirect costs for individuals with insomnia syndrome, insomnia symptoms, and good sleepers. Sleep 2009;32:55–64. [PMC free article] [PubMed] [Google Scholar]
- 9.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep medicine reviews 2002;6:97–111. 10.1053/smrv.2002.0186 [DOI] [PubMed] [Google Scholar]
- 10.Hara C, Stewart R, Lima-Costa MF, et al. Insomnia subtypes and their relationship to excessive daytime sleepiness in Brazilian community-dwelling older adults. Sleep 2011;34:1111–7. 10.5665/SLEEP.1172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Henderson S, Jorm AF, Scott LR, Mackinnon AJ, Christensen H, Korten AE. Insomnia in the elderly: its prevalence and correlates in the general population. The Medical Journal of Australia 1995;162:22–4. [DOI] [PubMed] [Google Scholar]
- 12.Foley DJ, Monjan AA, Brown SL, Simonsick EM, Wallace RB, Blazer DG. Sleep complaints among elderly persons: an epidemiologic study of three communities. Sleep 1995;18:425–32. 10.1093/sleep/18.6.425 [DOI] [PubMed] [Google Scholar]
- 13.Chiu HF, Leung T, Lam LC, et al. Sleep problems in Chinese elderly in Hong Kong. Sleep 1999;22:717–26. 10.1093/sleep/22.6.717 [DOI] [PubMed] [Google Scholar]
- 14.Bixler EO, Kales A, Soldatos CR, Kales JD, Healey S. Prevalence of sleep disorders in the Los Angeles metropolitan area. The American Journal of Psychiatry 1979. [DOI] [PubMed] [Google Scholar]
- 15.Ancoli-Israel S, Roth T. Characteristics of insomnia in the United States: results of the 1991 National Sleep Foundation Survey. I. Sleep 1999;22:S347–53. [PubMed] [Google Scholar]
- 16.Breslau N, Roth T, Rosenthal L, Andreski P. Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biological psychiatry 1996;39:411–8. 10.1016/0006-3223(95)00188-3 [DOI] [PubMed] [Google Scholar]
- 17.Ohayon MM, Shapiro CM, Kennedy SH. Differentiating DSM-IV anxiety and depressive disorders in the general population: comorbidity and treatment consequences. The Canadian Journal of Psychiatry 2000;45:166–72. 10.1177/070674370004500207 [DOI] [PubMed] [Google Scholar]
- 18.Weissman MM, Bland RC, Canino GJ, et al. Cross-national epidemiology of major depression and bipolar disorder. Jama 1996;276:293–9. [PubMed] [Google Scholar]
- 19.Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders: an opportunity for prevention? Jama 1989;262:1479–84. 10.1001/jama.262.11.1479 [DOI] [PubMed] [Google Scholar]
- 20.Ohayon MM, Roth T. What are the contributing factors for insomnia in the general population? Journal of psychosomatic research 2001;51:745–55. 10.1016/s0022-3999(01)00285-9 [DOI] [PubMed] [Google Scholar]
- 21.Tsai P-S, Wang S-Y, Wang M-Y, et al. Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Quality of Life Research 2005;14:1943–52. 10.1007/s11136-005-4346-x [DOI] [PubMed] [Google Scholar]
- 22.Zhang B, Wing Y-K. Gender differences in insomnia: a meta-analysis. Sleep 2006;29:85–93. [DOI] [PubMed] [Google Scholar]
- 23.Pallesen S, Nordhus IH, Nielsen GH, et al. Prevalence of insomnia in the adult Norwegian population. Sleep 2001;24:771–9. [PubMed] [Google Scholar]
- 24.Li R, Wing Y, Ho S, Fong S. Gender differences in insomnia—a study in the Hong Kong Chinese population. Journal of psychosomatic research 2002;53:601–9. 10.1016/s0022-3999(02)00437-3 [DOI] [PubMed] [Google Scholar]
- 25.Itani O, Jike M, Watanabe N, Kaneita Y. Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep medicine 2017;32:246–56. 10.1016/j.sleep.2016.08.006 [DOI] [PubMed] [Google Scholar]
- 26.Association AP. Diagnostic and statistical manual of mental disorders (DSM-5®): American Psychiatric Pub, 2013. [DOI] [PubMed] [Google Scholar]
- 27.Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep medicine 2001;2:297–307. 10.1016/s1389-9457(00)00065-4 [DOI] [PubMed] [Google Scholar]
- 28.Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep 2011;34:601–8. 10.1093/sleep/34.5.601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry research 1989;28:193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 30.Goldberg D, Bridges K, Duncan-Jones P, Grayson D. Detecting anxiety and depression in general medical settings. Bmj 1988;297:897–9. 10.1136/bmj.297.6653.897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kim JS, Kim YS, Lee GY, et al. The standardization of Korean-translated Goldberg’s shart screening scale for Anxiety and Depression. Journal of the Korean Academy of Family Medicine 1997;18:1452–60. [Google Scholar]
- 32.Pignone MP, Gaynes BN, Rushton JL, et al. Screening for depression in adults: a summary of the evidence for the US Preventive Services Task Force. Annals of internal medicine 2002;136:765–76. 10.7326/0003-4819-136-10-200205210-00013 [DOI] [PubMed] [Google Scholar]
- 33.Choi HS, Choi JH, Park KH, et al. Standardization of the Korean version of Patient Health Questionnaire-9 as a screening instrument for major depressive disorder. Journal of the Korean Academy of Family Medicine 2007;28:114–9. [Google Scholar]
- 34.Nomura K, Yamaoka K, Nakao M, Yano E. Impact of insomnia on individual health dissatisfaction in Japan, South Korea, and Taiwan. Sleep 2005;28:1328–32. 10.1093/sleep/28.10.1328 [DOI] [PubMed] [Google Scholar]
- 35.Mong JA, Cusmano DM. Gender differences in sleep: impact of biological gender and gender steroids. Phil. Trans. R. Soc. B 2016;371:20150110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang J, Chan NY, Lam SP, et al. Emergence of gender differences in insomnia symptoms in adolescents: a large-scale school-based study. Sleep 2016;39:1563–70. 10.5665/sleep.6022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Polo-Kantola P, Erkkola R, Helenius H, Irjala K, Polo O. When does estrogen replacement therapy improve sleep quality? American Journal of Obstetrics & Gynecology 1998;178:1002–9. [DOI] [PubMed] [Google Scholar]
- 38.Moline ML, Broch L, Zak R. Sleep in women across the life cycle from adulthood through menopause. Medical Clinics of North America 2004;88:705–36. 10.1016/j.mcna.2004.01.009 [DOI] [PubMed] [Google Scholar]
- 39.Savard J, Hervouet S, Ivers H. Prostate cancer treatments and their side effects are associated with increased insomnia. Psycho‐Oncology 2013;22:1381–8. 10.1002/pon.3150 [DOI] [PubMed] [Google Scholar]
- 40.Liu PY, Yee B, Wishart SM, et al. The short-term effects of high-dose testosterone on sleep, breathing, and function in older men. The Journal of Clinical Endocrinology & Metabolism 2003;88:3605–13. [DOI] [PubMed] [Google Scholar]
- 41.Cusmano DM, Hadjimarkou MM, Mong JA. Gonadal steroid modulation of sleep and wakefulness in male and female rats is genderually differentiated and neonatally organized by steroid exposure. Endocrinology 2014;155:204–14. 10.1210/en.2013-1624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Baglioni C, Battagliese G, Feige B, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. Journal of affective disorders 2011;135:10–9. 10.1016/j.jad.2011.01.011 [DOI] [PubMed] [Google Scholar]
- 43.Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of general psychiatry 2003;60:929–37. 10.1001/archpsyc.60.9.929 [DOI] [PubMed] [Google Scholar]
- 44.Gallo EAG, Munhoz TN, de Mola CL, Murray J. Gender differences in the effects of childhood maltreatment on adult depression and anxiety: a systematic review and meta-analysis. Child abuse & neglect 2018;79:107–14. [DOI] [PubMed] [Google Scholar]
- 45.Gallo EAG, Munhoz TN, de Mola CL, Murray J. Gender differences in the effects of childhood maltreatment on adult depression and anxiety: a systematic review and meta-analysis. Child abuse & neglect 2018;79:107–14. [DOI] [PubMed] [Google Scholar]
- 46.Barsky AJ, Peekna HM, Borus JF. Somatic symptom reporting in women and men. Journal of general internal medicine 2001;16(4):266–275 10.1046/j.1525-1497.2001.00229.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhang J, Lam SP, Li SX, Tang NL. Insomnia, sleep quality, pain, and somatic symptoms: sex differences and shared genetic components. Pain 2012;153(3):666–673 10.1016/j.pain.2011.12.003 [DOI] [PubMed] [Google Scholar]
- 48.Johnson EO, Roth T, Schultz L, Breslau N. Epidemiology of DSM-IV insomnia in adolescence: lifetime prevalence, chronicity, and an emergent gender difference. Pediatrics 2006;117:e247–e56. 10.1542/peds.2004-2629 [DOI] [PubMed] [Google Scholar]
- 49.Calhoun SL, Fernandez-Mendoza J, Vgontzas AN, Liao D, Bixler EO. Prevalence of insomnia symptoms in a general population sample of young children and preadolescents: gender effects. Sleep medicine 2014;15:91–5. 10.1016/j.sleep.2013.08.787 [DOI] [PMC free article] [PubMed] [Google Scholar]