Abstract
Background:
Older adults are particularly vulnerable to complications from proton pump inhibitor (PPI) drugs. We sought to characterize the prevalence of potentially low-value PPI prescriptions among older adults in order to inform a quality improvement (QI) intervention.
Methods:
We created a cohort of patients ≥65 years old receiving primary care at a large academic health system in 2018. We identified patients currently prescribed any PPI using the electronic health record (EHR) medication list (current defined as September 1st, 2018). A geriatrician, gastroenterologist, QI expert, and two primary care physicians (PCPs) created multidisciplinary PPI appropriateness criteria based on evidenced-based guidelines. Supervised by a gastroenterologist and PCP, two internal medicine residents conducted manual chart reviews in a random sample of 399 patients prescribed PPIs. We considered prescriptions potentially low-value if they lacked a guideline-based (1) short-term indication (GERD/peptic ulcer disease/H. Pylori gastritis/dyspepsia) or (2) long-term (>8 weeks) indication (severe/refractory GERD/erosive esophagitis/Barrett’s esophagus/esophageal adenocarcinoma/esophageal stricture/high gastrointestinal bleeding risk/Zollinger-Ellison Syndrome). We used the Wilson score method to calculate 95% confidence intervals on low-value PPI prescription prevalence.
Results:
Among 69,352 older adults, 8,729 (12.6%) were prescribed a PPI. In the sample of 399 patients prescribed PPIs, 63.9% were female; mean age was 76.2 years, and they were seen by 169 PCPs. Of the 399 prescriptions, 143 (35.8% [95% CI 31.3–40.7%]) were potentially low-value—of which 82% began appropriately (e.g., GERD) but then continued long-term without a guideline-based indication. Among 169 PCPs, 32 (18.9%) contributed to 59.2% of potentially low-value prescriptions.
Conclusion:
One in eight older adults were prescribed a PPI, and over one-third of prescriptions were potentially low-value. Most often, appropriate short-term prescriptions became potentially low-value because they lacked long-term indications. With most potentially low-value prescribing concentrated among a small subset of PCPs, interventions targeting them and/or applying EHR-based automatic stopping rules may protect older adults from harm.
INTRODUCTION
Proton pump inhibitor (PPI) drugs are associated with complications such as C. difficile infections or kidney toxicity, and older adults are particularly vulnerable to such adverse events.1–6 Moreover, PPIs contribute to polypharmacy, prescription drug costs, and aging-related complications (e.g., osteoporotic fractures).7,8
Despite these harms, many PPI prescriptions are potentially low-value, meaning they lack an evidenced-based indication.9,10 Promisingly, six randomized PPI de-intensification trials in a meta-analysis found that deprescribing can reduce PPI use and pill burden.11 Other well-designed quality improvement studies attempting to reduce potentially low-value PPI prescriptions have found mixed results12,13 and importantly none of the six randomized trials were conducted among older Americans.
We sought to characterize the prevalence of potentially low-value PPI prescriptions among older adults at the University of California Los Angeles (UCLA) Health, a large academic health system, in order to inform a randomized quality improvement (QI) intervention.
METHODS
Study Design and Cohort Selection
We performed a chart review on a subset of older adults prescribed PPIs at UCLA Health in 2018 (Supplementary Figure S1). First, we identified the total cohort of patients ≥65 years old meeting any of the following criteria: (1) ≥2 UCLA primary care physician (PCP) visits in the past 3 years; (2) ≥1 UCLA preventive care PCP visit in the past year; (3) current membership in UCLA’s medical group insurance plan. We identified patients currently prescribed any PPI using the electronic health record (EHR) medication list (Supplementary Table S1), with “current” defined as September 1st, 2018. We excluded PPIs included historically on the medication list that were prescribed by non-UCLA clinicians or bought over the counter (n=3,317) because our proposed intervention to reduce PPI use will focus on UCLA clinician prescribing.
Because our expected low-value prescription rate was 30% (based on literature9,10 and an exploratory chart review, data not shown), we determined that a chart review sample size of 357 would ensure an estimate precision of 5% (i.e., half width of 95% confidence interval ≤5%).
Supervised by a board-certified gastroenterologist and general internist, two internal medicine residents performed standardized chart review on a small training set to assess inter-rater agreement for appropriateness (>90% agreement on the cases is considered excellent agreement).14 Next, the residents performed the standardized chart review on a random sample of 399 patients from the larger cohort to obtain demographic, clinical, and physician practice data. We also collected information on medication adherence (see the Supplemental Appendix for these results).
Appropriateness Measurement
A multidisciplinary committee (geriatrician, gastroenterologist, QI expert, two general internists) created guideline-based appropriateness criteria based on the American Geriatrics Society Beers Criteria, American Gastroenterological Association, and American College of Gastroenterology Practice Guidelines.15–17 The committee reviewed each recommendation and strength of evidence; all recommendations were accepted based on group discussion and consensus. We determined appropriateness by reviewing charts for problem lists, diagnoses, medications, visit notes, and endoscopy reports based on two categories of appropriateness: short-term and long-term PPI prescriptions from January 1, 2013—March 21, 2019 (Supplementary Table S2). Regarding evidenced-based indications for short-term (≤8 weeks) PPI prescriptions, we looked for GERD, peptic ulcer disease, H. Pylori gastritis, and dyspepsia diagnoses. Regarding evidenced-based indications for long-term (>8 weeks) PPI prescriptions, we reviewed the chart for erosive esophagitis, refractory/severe GERD, high risk for GI bleeding (e.g., on chronic non-steroidal anti-inflammatory drugs), Barrett’s esophagus, esophageal stricture, esophageal adenocarcinoma or Zollinger-Ellison Syndrome diagnoses. Reviewers deemed prescriptions lacking evidence-based indications as potentially low-value.
Analysis
We performed an exploratory analysis to assess whether any demographic characteristics are associated with potentially low-value prescriptions using Chi square tests and student t-tests. We also used the Wilson score method to calculate 95% confidence intervals on low-value PPI prescription prevalence. We created histograms of potentially low-value PPI prescription rates among all PPI prescriptions ranked by the patients’ primary care practice and the patients’ PCP. All analyses were completed using SAS, version 9.4 (SAS Institute Inc). The UCLA Health Institutional Review Board approved this retrospective quality improvement study.
RESULTS
Among 69,352 older adults, 8,729 (12.6%) were prescribed a PPI. In the chart review sub-sample (n=399), 63.9% of patients were female; mean age was 76.2 years; patients were seen by 169 PCPs (Table 1). After reviewing the guideline-based criteria, the two blinded reviewers independently agreed 100% of the time on whether the PPI prescription was low-value in the training set (n=9), indicating excellent inter-rater agreement.
Table 1.
Characteristics of Patients in Subsample Prescribed PPIs Stratified by Appropriateness (n=399)
| Potentially Low- Value (n=143) |
Appropriate (n=254) |
Total (N=399) | |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Age (Mean ± SD) | 76.0 ± 8.7 | 76.2 ± 8.3 | 76.2 ± 8.5 |
| Gender | |||
| Male | 46 (32.2) | 97 (38.2) | 144 (36.1) |
| Female | 97 (67.8) | 157 (61.8) | 255 (63.9) |
| Race | |||
| White | 93 (65.0) | 176 (69.3) | 271 (67.9) |
| Black | 5 (3.5) | 17 (6.7) | 22 (5.5) |
| Asian | 18 (12.6) | 23 (9.1) | 41 (10.3) |
| AI/AN | 2 (1.4) | 0 (0.0) | 2 (0.5) |
| Other | 21 (14.7) | 31 (12.2) | 52 (13.0) |
| Unknown | 4 (2.8) | 7 (2.8) | 11 (2.8) |
| Ethnicity | |||
| Hispanic | 27 (18.9) | 41 (16.1) | 69 (17.3) |
| Not Hispanic | 113 (79.0) | 205 (80.7) | 319 (79.9) |
| Unknown | 3 (2.1) | 8 (3.1) | 11 (2.8) |
| Median household income | |||
| Mean | $83,910 | $89,665 | $87,524 |
| Median | $79,242 | $84,937 | $82,630 |
| <$50,000 | 14 (9.8) | 23 (9.1) | 37 (9.3) |
| [$50,000, $75,000) | 35 (24.5) | 58 (22.8) | 94 (23.6) |
| [$75,000, $100,000) | 50 (35.0) | 93 (36.6) | 144 (36.1) |
| >=$100,000 | 42 (29.4) | 74 (29.1) | 116 (29.1) |
| Unknown | 2 (1.4) | 6 (2.4) | 8 (2.0) |
Analyses with chi square tests and t-tests found no stastically significant differences between patients with potentially low-value vs appropriate PPI use by age, gender, race, ethnicity, and zip code derived household income.
PPI = Proton Pump Inhibitor; SD = Standard Deviation; AI/AN = American Indian/Alaska Native
Of the 399 prescriptions, 143 (35.8% [95% CI 31.3–40.7%]) were potentially low-value—of which 82% began appropriately (e.g., GERD) but then continued long-term without a guideline-based indication (Table 2).
Table 2.
Categories of Initial PPI Indication and Long-Term Indication Stratified by Appropriateness
| Potentially Low- Value (n=143) n (%) |
Appropriate (n=254) n (%) |
Total (N=399) n (%) |
|
|---|---|---|---|
| Categories of Initial Indication for PPI (%) | |||
| GERD | 95 (66.4) | 163 (64.2) | 258 (65.0) |
| Peptic ulcer disease | 5 (3.5) | 15 (5.9) | 20 (5.0) |
| Chronic cough | 5 (3.5) | 4 (1.6) | 9 (2.3) |
| Atypical GERD symptoms | 4 (2.8) | 7 (2.8) | 11 (2.8) |
| Dyspepsia | 4 (2.8) | 7 (2.8) | 11 (2.8) |
| Laryngopharyngeal reflux | 3 (2.1) | 3 (1.2) | 6 (1.5) |
| Suspected Upper GI bleed | 3 (2.1) | 2 (0.8) | 5 (1.3) |
| Ulcer bleeding prophylaxis | 3 (2.1) | 5 (2.0) | 8 (2.0) |
| H. pylori eradication | 1 (0.7) | 1 (0.4) | 2 (0.5) |
| Unable to determine | 14 (9.8) | 14 (5.5) | 28 (7.1) |
| Anticoagulation | 0 (0.0) | 1 (0.4) | 1 (0.3) |
| Other | 6 (4.2) | 32 (12.6) | 38 (9.6) |
| Categories of Potentially Low-Value PPI (%) | |||
| Use extended long-term for a short-term indication | 116 (81.1) | NA | 116 (81.1) |
| No identifiable indication for use | 18 (12.6) | NA | 18 (12.6) |
| Use for indication not recommended by guidelines | 6 (4.2) | NA | 6 (4.2) |
| Started inpatient and continued to outpatient without indication | 1 (4.2) | NA | 1 (4.2) |
| Other | 1 (0.7) | NA | 1 (0.7) |
| Unknown | 1 (0.7) | NA | 1 (0.7) |
PPI = Proton Pump Inhibitor; GI = Gastrointestinal; GERD = Gastroesophageal Reflux Disease
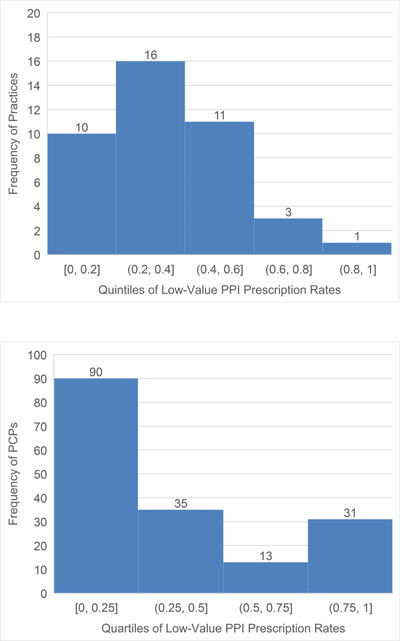
Among the 41 primary care practices, 16 (39.0%) contributed to 72.4% of the potentially low-value prescriptions (Figure 1). Among 169 PCPs, 32 (18.9%) contributed to 59.2% of potentially low-value prescriptions.
Figure 1.
Rates of Potentially Low-Value PPI Prescriptions Among All PPI Prescriptions Ranked by Primary Care Practice and Primary Care Physician (PCP)
Figure 1A. Quintiles of Low-Value Prescribing Rates Ranked by Primary Care Practices (n=41)
Figure 1B. Quartiles of Low-Value Prescribing Rates Ranked by PCP Prescribers (n=169 PCPs)
DISCUSSION
One in eight older adults were prescribed a PPI, and over one-third of prescriptions were potentially low-value. Most often, appropriate short-term prescriptions became potentially low-value because they lacked long-term indications. With most potentially low-value prescribing concentrated among a small subset of PCPs, interventions targeting them18 and/or applying EHR-based automatic stopping rules may protect older adults from harm.
Our results are concordant with prior studies assessing the rate of potentially low-value PPI prescriptions among older adults (ranging from 20–40%).9,10 Previous research highlights inpatient prescriptions as a major source of potentially low-value PPI prescriptions,19 suggesting that this is a major problem for post-acute and primary care providers who are trying to determine if and when the PPI can be discontinued, and is a major reason for ongoing low-value use. This work also suggests that requiring indications on post-acute care transfer forms could curb potentially low-value PPI prescriptions.
Our study adds to the literature by focusing on clinician-level performance data as a means for targeted QI as well as highlighting the dynamic nature of low-value care. For example, because most potentially low-value prescriptions began appropriately but then continue without an indication, an EHR choice architecture automatically defaulting prescriptions to the lowest dose, 8 weeks’ duration, and no refills could reduce needless long-term PPIs with minimal clinical workflow disruption.20 However, these defaults may inadvertently stop necessary PPIs if they lack clinical nuance.21,22 Therefore, the EHR defaults must be targeted precisely for low-value prescriptions to avoid unintended consequences such as GI bleeding that might have been prevented by PPIs.22,23
This study has important limitations. First, findings from this single institution study may not generalize to other health systems. Second, the lack of a documented indication does not exclude the possibility that there was an undocumented evidenced-based indication. Prompting clinicians to document an indication for long-term prescriptions can mitigate this clinical uncertainty while simultaneously improving documentation and the quality of care.12,24
Conclusions
Older adults are receiving PPI prescriptions at an alarmingly high rate, often against guidelines. This study suggests that potentially minor changes in EHR-based stopping rules and/or targeted physician profiling could have a substantial impact on reducing low-value prescribing. These findings will directly inform a system-level QI intervention to curb potentially low-value long-term PPI prescriptions among older adults.
Supplementary Material
ACKNOWLEDGEMENTS
Funding: This work was supported by the Kaiser Permanente Taking Action on Overuse Robert Wood Johnson Foundation Sub-award and a National Institutes of Health/National (NIH/NCATS) Center for Advanced Translational Science Institute (CTSI) KL2TR001882 award.
Role of the Sponsor: Dr. Mafi was supported by the Kaiser Permanente Taking Action on Overuse Robert Wood Johnson Foundation Sub-award and a National Institutes of Health/National (NIH/NCATS) Center for Advanced Translational Science Institute (CTSI) KL2TR001882 award. Dr. Sarkisian was supported by a National Institute on Aging 1K24AG047899-01 award and the UCLA CTSI NIH/NCATS Grant # UL1TR001881.
Dr. Damberg was supported by the RAND Center of Excellence on Health System Performance funded by grant 1U19HS024067-01 from the Agency for Healthcare Research and Quality.
The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Scientific Abstract Presentations: Society of General Internal Medicine 2019 Annual Meeting, UCLA 2019 Conference on Aging, Digestive Disease Week 2019 Meeting
Footnotes
Conflict of Interest: The authors report no relevant conflicts of interest to this work.
REFERENCES
- 1.Schoenfeld AJ, Grady D. Adverse Effects Associated With Proton Pump Inhibitors. JAMA Intern Med. 2016;176(2):172–174. [DOI] [PubMed] [Google Scholar]
- 2.Herzig SJ, Howell MD, Ngo LH, Marcantonio ER. Acid-suppressive medication use and the risk for hospital-acquired pneumonia. JAMA 2009;301(20):2120–2128. [DOI] [PubMed] [Google Scholar]
- 3.Lambert AA, Lam JO, Paik JJ, Ugarte-Gil C, Drummond MB, Crowell TA. Risk of Community-Acquired Pneumonia with Outpatient Proton-Pump Inhibitor Therapy: A Systematic Review and Meta-Analysis. PLoS ONE. 2015;10(6):e0128004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eom CS, Jeon CY, Lim JW, Cho EG, Park SM, Lee KS. Use of acid-suppressive drugs and risk of pneumonia: a systematic review and meta-analysis. CMAJ. 2011;183(3):310–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sultan N, Nazareno J, Gregor J. Association between proton pump inhibitors and respiratory infections: a systematic review and meta-analysis of clinical trials. Can J Gastroenterol. 2008;22(9):761–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maes ML, Fixen DR, Linnebur SA. Adverse effects of proton-pump inhibitor use in older adults: a review of the evidence. Ther Adv Drug Saf. 2017;8(9):273–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Steinman MA. Polypharmacy: time to get beyond numbers. JAMA Intern Med. 2016;176(4):482–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Charlesworth CJ, Smit E, Lee DSH, Alramadhan F, Odden MC. Polypharmacy Among Adults Aged 65 Years and Older in the United States: 1988–2010. J Gerontol A Biol Sci Med Sci. 2015;70(8):989–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gawron AJ, Pandolfino JE, Miskevics S, Lavela SL. Proton pump inhibitor prescriptions and subsequent use in US veterans diagnosed with gastroesophageal reflux disease. J Gen Intern Med. 2013;28(7):930–937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.George CJ, Korc B, Ross JS. Appropriate proton pump inhibitor use among older adults: a retrospective chart review. Am J Geriatr Pharmacother. 2008;6(5):249–254. [DOI] [PubMed] [Google Scholar]
- 11.Boghossian TA, Rashid FJ, Thompson W, et al. Deprescribing versus continuation of chronic proton pump inhibitor use in adults. Cochrane Database Syst Rev. 2017;3:Cd011969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Herzig SJ, Guess JR, Feinbloom DB, et al. Improving appropriateness of acid-suppressive medication use via computerized clinical decision support. J Hosp Med. 2015;10(1):41–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buckley MS, Park AS, Anderson CS, et al. Impact of a clinical pharmacist stress ulcer prophylaxis management program on inappropriate use in hospitalized patients. Am J Med. 2015;128(8):905–913. [DOI] [PubMed] [Google Scholar]
- 14.Hays RD, Brodsky M, Johnston MF, Spritzer KL, Hui KK. Evaluating the statistical significance of health-related quality-of-life change in individual patients. Eval Health Prof. 2005;28(2):160–171. [DOI] [PubMed] [Google Scholar]
- 15.American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. 2015;63(11):2227–2246. [DOI] [PubMed] [Google Scholar]
- 16.Freedberg DE, Kim LS, Yang YX. The Risks and Benefits of Long-term Use of Proton Pump Inhibitors: Expert Review and Best Practice Advice From the American Gastroenterological Association. Gastroenterology. 2017;152(4):706–715. [DOI] [PubMed] [Google Scholar]
- 17.Gyawali CP, Fass R. Management of Gastroesophageal Reflux Disease. Gastroenterology. 2018;154(2):302–318. [DOI] [PubMed] [Google Scholar]
- 18.Mafi JN, Godoy-Travieso P, Wei E, et al. Evaluation of an Intervention to Reduce Low-Value Preoperative Care for Patients Undergoing Cataract Surgery at a Safety-Net Health System. JAMA Intern Med. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Durand C, Willett KC, Desilets AR. Proton Pump Inhibitor use in Hospitalized Patients: Is Overutilization Becoming a Problem? Clin Med Insights Gastroenterol. 2012;5:65–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patel MS, Day SC, Halpern SD, et al. Generic Medication Prescription Rates After Health System-Wide Redesign of Default Options Within the Electronic Health Record. JAMA Intern Med. 2016;176(6):847–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mafi JN, Russell K, Bortz BA, Dachary M, Hazel WA Jr., Fendrick AM Low-Cost, High-Volume Health Services Contribute The Most To Unnecessary Health Spending. Health Aff (Millwood). 2017;36(10):1701–1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mafi JN, Parchman M. Low-value care: an intractable global problem with no quick fix. BMJ Qual Saf. 2018;27(5):333–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Platt KD, Saini SD, Kurlander JE. Selecting the Appropriate Patients for Proton Pump Inhibitor Discontinuation: A Teachable Moment. JAMA Intern Med. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schiff G, Mirica MM, Dhavle AA, Galanter WL, Lambert B, Wright A. A Prescription For Enhancing Electronic Prescribing Safety. Health Aff (Millwood). 2018;37(11):1877–1883. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.