Abstract
Pityriasis versicolor is a common infection of the epidermis in adults, but only a few cases of this infection (especially the hypopigmented type) have been reported in infants aged under one year. Herein, we document a report of these cases and a review of the literature. Two patients with infantile pityriasis versicolor, who presented with hypopigmented macules on the neck, upper back, and chest are reported. A KOH examination was suggestive of pityriasis versicolor and our patients responded well to 1% clotrimazole lotion (twice a day) for four weeks. Pityriasis versicolor should be considered in the differential diagnosis of hypopigmented macules and patches in infants.
Keywords: Hypopigmented, infantile, pityriasis versicolor, tinea versicolor
Abstract
Pitiriyazis versikolor erişkinlerde epidermisin sık görülen bir enfeksiyonudur, ama bir yaşın altındaki bebeklerde sadece birkaç vaka bildirilmiştir (özellikle hipopigmente tip). Bu vakalarla ilgili bir bildirimi ve literatür incelemesini belgelendirdik. Boyun, sırtın üst bölümü ve göğüste hipopigmente maküllerle başvuran iki infantil pitiriyazis versikolor vakası bildirilmiştir. KOH testi pitiriyazis versikoloru düşündürmüştü ve hastalarımız dört hafta süre ile uygulanan %1 klotirmazol losyonuna (günde iki kere) iyi yanıt vermişlerdi. Bebeklerde, hipopigmente maküller ve lekelerin ayırıcı tanısında, pitiriyazis versikolor düşünülmelidir.
Introduction
Pityriasis versicolor (PV) is a common superficial fungal infection that usually involves the chest and back in early adulthood (1). However, it can also occur rarely in small children (2). Pityriasis versicolor can manifest as scaly macules or patches with various colors, red, pale yellow or brown (1).
To our knowledge, there are few reported cases of PV in infants aged under one year (especially the hypopigmented type). Herein, we report two cases of hypopigmented PV and review the associated literature.
Case
Case 1
An 8-month-old infant girl presented to our dermatology clinic with hypopigmented lesions. She was born by normal vaginal delivery at 38 weeks’ gestational age. She had a history of hypopigmented lesions from 3 months ago, without pruritus. Other family members had no similar cutaneous lesions. A physical examination showed numerous hypopigmented macules on the lateral face, neck, upper back and chest (Figure 1a, b).
Figure 1.
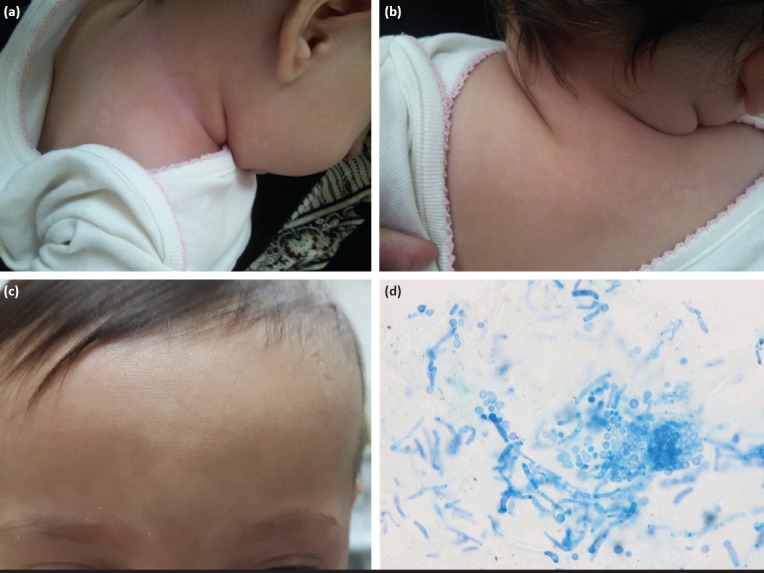
(a, b) Hypopigmented macules on the lateral face, neck, upper back; (c) Numerous confluent hypopigmented macules on the frontal area of the face; (d) Yeast and short hypha with appearance of ‘spaghetti and meatballs’ in KOH examination
Case 2
A 4-month-old infant girl in good health was examined for hypopigmented macules on the face that had been noted at the age of 2 months. On physical examination, numerous confluent hypopigmented macules with fine scales located on the frontal area of the face were noted (Figure 1c).
In both cases, examinations using a Wood’s lamp showed hypopigmented processes in the aforementioned areas and also yellowish fluorescence on some lesions. A potassium hydroxide (KOH) examination revealed yeast and short mycelial forms resembling ‘ziti and meatballs,’ which supported the diagnosis of PV (Figure 1d).
These patients were treated with 1% clotrimazole lotion (twice a day) for four weeks. After treatment, the lesions were still present but with less severity and KOH smears showed negative results for fungal elements. Written informed consent was given by the parents of the patients.
Discussion
Hypopigmented macules and patches in infants have a variety of etiologies such as pityriasis alba, nevus depigmentosus, nevus anemicus, ash-leaf spot in tuberous sclerosis, and uncommonly, PV (3). Malassezia species are commensal flora of the skin and its colonization is established at birth and increases with age (4). The genus Malassezia has been known to cause PV, and Malassezia furfur is the most common pathogen in this group (4). The prevalence of PV is higher in the third and fourth decades of life and it is uncommon in children (1, 4). We were able to find nine documented reports of infantile PV (Table 1).
Table 1.
Reported cases of infantile pityriasis versicolor (under one year of age) with clinical details
| Author/Year | Sex/Age | Region | Physical exam | Location | Family history | Past medical history | Delivery | Treatment | KOH after treatment | Follow up |
|---|---|---|---|---|---|---|---|---|---|---|
| Congly H 1984 | Male/ 3 m | Saskatchewan | Erythematous scaly macules and patches | Dorsal aspect of the upper arm, shoulders, upper back Cervical, scalp, face, | Negative | Negative | NA | Clotrimazole 1% solution | NA | 3 m |
| Di Silverio 1995 | Male/ 2 m | Italy | Hyper-hypo pigmented scaly macules | upper chest | Negative | Negative | NVD | Econazole 1% lotion | Negative | 3 wk. |
| Arti Nanda 1998 | Male/ 3 wk. | India | Several hypopigmented macules | Forehead | Negative | Negative | NVD | Clotrimazole 1% solution | Negative | 6 wk. |
| Male/ 4 m | India | Hypopigmented scaly lesion | Neck, upper trunk, arms, face | Positive (Mother) | Negative | NA | Clotrimazole 1% solution | Negative | 2 m | |
| Male/ 5 m | India | Light brown, scaly macules | Neck | Negative | Atopic dermatitis | NA | Clotrimazole 1% solution | NA | 1 m | |
| Male/ 4 wk. | India | Hypopigmented scaly macules | Forehead | Negative | NA | NVD | Tolnaftate solution | NA | NA | |
| Female/ 5 wk. | India | Hypopigmented scaly macules | Face, forehead | Negative | NA | NA | Tolnaftate solution | Negative | 2 m | |
| Elisabet J 2015 | Male /3 wk. | Spain | Hypopigmented macules and patches | Upper trunk, face, neck | Negative | Premature birth LBW | NA | Intravenous fluconazole | NA | 3 m |
| Hypopigmented macules with fine scale | TPN ICU admission Antibiotic therapy | |||||||||
| Z Ben Said/ 2010 | Male/ 3 m | Tunisia | Hypopigmented macules | Cervical, chest | Positive (mother) | Negative | NA | Topical antifungal | NA | 2 m |
| Present cases | Female/ 8 m | Iran | Lateral face, neck, upper back and chest | Negative | Negative | NVD | Topical antifungal | Negative | 2 m | |
| Female/ 4 m | Iran | Hypopigmented macules | On the frontal area of the face | Negative | Negative | NVD | Topical antifungal | Negative | 2 m |
m: Month; NA: Not available; NVD: Normal vaginal delivery; wk: Week
The site of involvement varies according to age; for example, lesions of the face and trunk in children and adolescents, respectively, are the most common sites to be affected (1, 4). Predisposing factors for PV include malnutrition, immunosuppression, diabetes mellitus, use of oils and oily creams, hyperhidrosis, and corticosteroid therapy (1, 5, 6). Genetic factors may play a role in the pathogenesis, and a positive family history was observed in approximately 20% of patients in some studies (7).
The clinical diagnosis of PV is comfortable, a gold-yellow fluorescence of the lesions in a Wood’s light examination is helpful. Direct observation of yeast and short hypha likened to ‘spaghetti and meatballs’ in KOH preparations of skin scrapings are characteristic (8). Treatment options include azole group, allylamines group, a hydroxy-pyridone group antifungals and also 6% salicylic acid, ciclopiroxolamine and selenium sulfide 2.5% (1, 5). Topical treatment in PV is sufficient and the initial therapy in most patients, as it was in our cases. The duration of topical treatments is 4-6 weeks (1, 9). Various systemic antifungals such as fluconazole are usually used for extensive and refractory infections (9).
Conclusion
Pityriasis versicolor is uncommon in infants, especially those aged under one year, and affected children mostly present with atypical features; therefore, this infection should be kept in dermatologists’ minds.
Footnotes
Informed Consent: Written informed consent was given by the parents of the patients.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - F.A.; Design - F.A.; Supervision - N.N.; Materials - N.N.; Data Collection and/or Processing - F.A., N.N.; Analysis and/or Interpretation - N.N.; Literature Review - N.N.; Writing - N.N.; Critical Review - M.N.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
Hasta Onamı: Hastanın ebeveynlerinden yazılı onam alındı.
Hakem Değerlendirmesi: Dış bağımsız.
Yazar Katkıları: Fikir - F.A.; Tasarım - F.A.; Denetleme - N.N.; Malzemeler - N.N.; Veri Toplanması ve/veya İşlemesi - F.A., N.N.; Analiz ve/veya Yorum - N.N.; Literatür Taraması - N.N.; Yazıyı Yazan - N.N.; Eleştirel İnceleme - M.N.
Çıkar Çatışması: Yazarlar çıkar çatışması bildirmemişlerdir.
Mali Destek: Yazarlar bu çalışma için mali destek almadıklarını beyan etmişlerdir.
References
- 1.Mayser PA, Preuss J. Pityriasis versicolor :new aspects of an old disease. Article in German] Hautarzt. 2012;63:859–67. doi: 10.1007/s00105-012-2380-5. [DOI] [PubMed] [Google Scholar]
- 2.Jena DK, Sengupta S, Dwari BC, Ram MK. Pityriasis versicolor in the pediatric age group. Indian J Dermatol Venereol Leprol. 2005;71:259–61. doi: 10.4103/0378-6323.16618. [DOI] [PubMed] [Google Scholar]
- 3.Hemady N, Noble C. An infant with a hypopigmented macule. Am Fam Physician. 2007;75:1053–4. [PubMed] [Google Scholar]
- 4.Di Silverio A, Zeccara C, Serra F, Ubezio S, Mosca M. Pityriasis versicolor in a newborn. Mycoses. 1995;38:227–8. doi: 10.1111/j.1439-0507.1995.tb00055.x. [DOI] [PubMed] [Google Scholar]
- 5.Congly H. Pityriasis versicolor in a 3-month-old boy. Can Med Assoc J. 1984;130:844–5. [PMC free article] [PubMed] [Google Scholar]
- 6.Nanda A, Kaur S, Bhakoo ON, Kaur I, Vaishnavi C. Pityriasis (tinea) versicolor in infancy. Pediatr Dermatol. 1988;5:260–2. doi: 10.1111/j.1525-1470.1988.tb00900.x. [DOI] [PubMed] [Google Scholar]
- 7.Gaitanis G, Magiatis P, Hantschke M, Bassukas ID, Velegraki A. The Malassezia genus in skin and systemic diseases. Clin Microbiol Rev. 2012;25:106–41. doi: 10.1128/CMR.00021-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thoma W, Krämer HJ, Mayser P. Pityriasis versicolor alba. J Eur Acad Dermatol Venereo. 2005;19:147–52. doi: 10.1111/j.1468-3083.2004.01085.x. [DOI] [PubMed] [Google Scholar]
- 9.Jubert E, Martin-Santiago A, Bernardino M, Bauzá A. Neonatal pityriasis versicolor. Pediatr Infect Dis J. 2015;34:329–30. doi: 10.1097/INF.0000000000000568. [DOI] [PubMed] [Google Scholar]


