Abstract
Purpose:
Social support is a key component in maintaining cancer caregiver well-being, and many resources exist to facilitate caregivers’ use of social support (e.g., cancer support groups). This study sought to determine how informal cancer caregivers use social resources over the course of caregiving.
Methods:
Data are from the Comprehensive Health Enhancement Support System (CHESS) study of informal caregivers (n=202) of recently-diagnosed lung cancer patients. Caregivers self-reported their sociodemographic and caregiving characteristics and social resource use over six months. Generalized additive models were used to assess social resource use over time and generalized estimating equations logistic regression models were used to assess the correlates of social resource use.
Results:
Nearly two-thirds of caregivers reported any social resource use. The most prevalent social resources were faith-based groups (38%) and social clubs (30%). Only one in four caregivers participated in a formal resource such as counseling (11%) or cancer support groups (6%). Social resource use was lowest immediately following diagnosis and increased over time. Formal resource use exhibited a non-linear association with time such that formal resource use peaked approximately 9–10 months after the cancer diagnosis. Caregivers were more likely to report social resource use if the patient also reported social engagement.
Conclusions:
This study found that many cancer caregivers do not use social resources, although social resource use increases over time following the cancer diagnosis. Given the association between social engagement and well-being, this information may inform future research and interventions to improve outcomes for cancer caregivers and their families.
Keywords: caregivers, cancer, psychosocial support systems, longitudinal studies, psycho-oncology
Precis:
Although many cancer caregivers did not engage in social activities, social resource use increased over the first year following a cancer diagnosis. Key correlates of social resource use include gender, health conditions, and the cancer patient’s resource use.
INTRODUCTION
Informal caregivers, such as family and friends, play a critical role in the care of cancer patients. Caregivers are part of the cancer care team,1 providing functional, emotional and even medical and nursing support.2 Lung cancer is one of the most common cancers affecting men and women, and is the leading cause of cancer deaths in the United States.3 At the time of diagnosis, most lung cancers have already advanced to regional or distant metastases, contributing to poor prognosis. These patients also have higher rates of physical and psychological burden than other cancers, including dyspnea, fatigue, anxiety, and depression. Likewise, their informal caregivers are at increased risk of poor physical and mental health status compared to non-caregivers.4,5 Evidence suggests that caregiver well-being is directly tied to patient outcomes.6
There is strong evidence that high quality social support is a vital component to cancer caregiver well-being and that caregivers receive different types of support from both formal and informal sources.7–10 Formal support includes the services provided by trained professionals, such as in-person or online cancer support groups and counseling. Informal support includes the support provided by an individual’s friends, family, or community, and can include social clubs or faith-based groups. Social engagement and the availability of social support has been linked to better outcomes in older adults,11 as well as cancer patients12 and their caregivers.13 As such, professional organizations and researchers recommend facilitating and enhancing caregivers’ engagement with social resources (e.g.,14,15).
Despite the benefits of social engagement, caregivers experience barriers to social resource utilization. For example, there is often low attendance and high attrition in support groups due to the time commitment and lack of affinity, even when conducted online.14,16 For those facing a poor prognosis, participants may have mixed reactions to witnessing the tragic nature of others’ stories.17 Furthermore, coping strategies aimed toward “maintaining normalcy” and avoiding cancer-related thoughts are in direct opposition to engagement in cancer-related peer support.17 In one study, only 14% of caregivers reported having attended a formal support group and of those only a third reported being satisfied with their experience.18 In another study, nearly a quarter of cancer caregivers reported receiving very little social support.19 There can also be a disconnect with the health care system: only 54% of cancer family caregivers report that providers asked about their needs to care for the patient, and only 29% say any provider asked about their needs to care for themselves.20
Finally, caregiving is a dynamic process and the need or availability of social support resources may change over time. Although there is a literature on social support needs in cancer patients and caregivers,21–23 few studies focus on change over time. A recent scoping review concluded that understanding how social consequences of caregiving evolve over time is a key gap in the existing literature.24 One small study indicated that caregivers’ social activities tended to remain steady over cancer treatment, and increased following the patient’s death.25 However, to our knowledge, no study has conducted an in-depth exploration of caregivers’ social engagement over the cancer trajectory. Further, the majority of studies focus on broad types of support needs (e.g. informational support), rather than the social resources used by caregivers to meet those needs (i.e. social clubs, support groups). This study sought to describe the proportion of caregivers participating in a variety of supportive social resources and identify how social resource use changed over time. We also identify demographic factors that predict social resource use. The findings of this work have important implications in identifying a general baseline of social resource usage for future interventions to increase access and acceptability of social resources to meet the support needs of cancer caregivers.
METHODS
Data Source
Data were from the National Cancer Institute-funded Comprehensive Health Enhancement Support System (CHESS) – Prolonging Life study. The CHESS “Coping with Lung Cancer” website was designed to provide lung cancer, caregiving, and bereavement information in a well-organized format, serve as a channel for communication among patient and caregiver peers, oncology clinicians, experts and the users’ own social support network, and act as a coach by gathering information from users and providing feedback based on algorithms (decision rules), all while being easy to use. Further details about CHESS development and content can be found in DuBenske et al.26
Study recruitment was conducted from December 2009 to September 2012 at eight cancer centers: three National Cancer Institute designated Comprehensive cancer centers (WI & TX), and five regional Cancer centers (WI, IL, CT). In total, 507 patients were approached for study participation. Patient inclusion criteria were: at least 18 years of age; diagnosed with non-small cell lung cancer (Stage IIIA non-surgical, IIIB or IV); within 12 months of their primary lung cancer diagnosis; metastatic or recurrent disease; an ECOG performance status rating of level 0, 1 or 2; any brain metastases were stable; under the care of a clinician who had consented to participate in the study; and able to complete informed consent written at a 6th grade level. There were ultimately 291 eligible subjects; 284 were randomized via a computer-generated list to either the internet control condition or the CHESS condition (seven eligible subjects died prior to randomization). Another 43% of subjects died post randomization during the study period. Seven percent of subjects withdrew from the study.
Patients were offered the option to have a primary support person (caregiver) participate with them. This was not a requirement of study participation. The present analysis included only those subjects for which dyadic patient-caregiver data were available (n=206). All subjects completed informed consent upon entry into the study. This study was approved by the Institutional Review Board.
Measures
Social resource use.
Participants reported whether they “regularly participate in any of the following” activities pertaining to social resource use: 1) individual or family counseling/psychotherapy; 2) cancer support groups; 3) non-cancer health-related group; 4) online (internet) support group; 5) social club/group (i.e., book club, recreation, parenting); 6) faith-based group; or 7) other. Items 1–4 were classified as “formal” resources; 5–7 were classified as “informal” resources. Participants who reported one or more of these activities were coded as having used social resources. Participants reported activities at baseline, 2, 4, and 6 months.
Caregiver characteristics.
Caregivers reported their gender (male vs. female), race/ethnicity (white non-Hispanic vs. other), education (high school or less, some college/technical degree/associates degree, or a bachelor’s degree or higher), employment status (employed full time vs. employed part time or unemployed/retired), income (≤$40,000; $40,001 to $80,000; $80,001 to $100,000; more than $100,000; or unreported), relationship with patient (spouse vs. other), coresidence (lives with the patient vs. doesn’t live with the patient), health conditions (none vs. one or more), the amount of caregiving help they receive (none, a little, a medium amount, or quite a bit/a lot), and how satisfied they are with that help (low-medium satisfaction, quite satisfied, or very satisfied). Age was calculated from date of birth and the date of the baseline survey. The 20-item Centers for Epidemiologic Studies Depression Scale (CES-D) was used to assess depressed mood; those with a score of ≥16 were coded as having clinically significant depressive symptoms.27 All characteristics were reported at baseline; coresidence, health conditions, amount of help, satisfaction with help, and depressed mood were reported at all time points.
Patient characteristics.
Patients reported their gender. Age was calculated from their date of birth and the date of the baseline survey. Patients reported their symptoms using the Edmonton Symptom Assessment Scale28 (range 0–100, higher score=worse symptoms). The Functional Assessment of Cancer Therapy (FACT-L)29 was used to assess patients’ physical and functional well-being in the past 7 days (range: 0–4; higher score=worse physical well-being and better functional well-being). Clinical cancer characteristics were also assessed including presence of brain metastasis, treatment types (chemotherapy, radiation, and/or surgery), and whether the cancer was a recurrence. Time since the cancer diagnosis was calculated in days based on the survey date at each time point and the date of diagnosis, and transformed into a continuous months variable for interpretability.
Analytic Approach
Visual inspection of the distribution of time since diagnosis was used to assess outliers. Three dyads with extreme values were dropped from the final analysis. One caregiver missing data on key time-invariant covariates (i.e., gender and employment) was dropped from the dataset, resulting in a final sample of 202 caregivers and a combined 584 observations.
Descriptive statistics (means/standard deviations and frequency distributions) were calculated on caregiver characteristics. Wilcoxon and chi-squared tests were used to compare baseline characteristics for those with and without any social resource use across time points. The proportions of caregivers using each social resource, and any social resource, were evaluated. To assess social resource use over time, we constructed generalized additive models with thin plate regression splines and a binomial outcome distribution.30 Time since diagnosis was included as the key independent variable and was tested for non-linearity. Bivariate generalized estimating equations (GEE) were used to assess whether time since diagnosis varied by any caregiver or cancer patient characteristics; as no statistically significant or borderline associations were found (p<0.10), no covariates were included in the generalized additive model. Results were graphed and to aid interpretability, odds ratios (OR) comparing likelihood of social resource use at 4 months versus 2 months post diagnosis were calculated and displayed using the oddsratio package in R.31
To assess correlates of social resource use GEE logistic regression models were constructed, first for any social resource use (Supplementary Table 1), and then for formal and informal social resource use. The models accounted for the repeated measures across subjects and employed empirical standard errors. To construct parsimonious models, characteristics that approached statistical significance (p<0.10) in models controlling only for CHESS randomization were selected for inclusion in the final model for each outcome. Randomization and time since diagnosis were controlled a priori. Sensitivity analyses limited the sample to subjects in the control condition, and tested controlling for covariates significantly associated with any of the outcomes in the bivariate analyses. Data management, descriptive statistics, and GEE analyses were conducted in SAS 9.4; generalized additive models were conducted in R 3.6.0.
RESULTS
Table 1 depicts selected caregiver and patient characteristics. On average, caregivers were 55 years of age and female (65%). Most were the patient’s spouse (71%). Compared to those who used one or more social resource at any time, those who did not use social resources were more likely to be male (44% vs. 30%, p=0.04) and employed full-time (54% vs. 35%, p=0.01), and their care recipients had worse functional well-being scores (2.21 vs. 2.45, p=0.04). See Supplementary Table 2 for complete characteristics.
Table 1.
Characteristics of informal caregivers of lung cancer survivors in the CHESS-Prolonging Life Study (2009–2012)
| Social Activities† | |||
|---|---|---|---|
| None | One or more | ||
| N | 68 | 134 | |
| % or Mean (SD) | % or Mean (SD) | p-value | |
| Caregiver Characteristics | |||
| Age (years) ‡ | 53.57 (11.40) | 55.40 (12.46) | 0.59 |
| Gender | 0.04 | ||
| Male | 44.1% | 29.9% | |
| Female | 55.9% | 70.1% | |
| Relationship to patient ‡ | 0.90 | ||
| Spouse | 70.6% | 71.4% | |
| Other | 29.4% | 28.6% | |
| Satisfaction with help (baseline) | 0.56 | ||
| Low-medium satisfaction | 35.3% | 28.4% | |
| Quite satisfied | 30.9% | 36.6% | |
| Very satisfied | 33.8% | 35.1% | |
| Patient Characteristics | |||
| Age (years) ‡ | 60.05 (9.10) | 59.71 (11.32) | 0.97 |
| Gender | 0.20 | ||
| Male | 42.6% | 52.2% | |
| Female | 57.4% | 47.8% | |
| Physical Well-being § | 1.36 (0.88) | 1.21 (0.90) | 0.10 |
| Functional Well-being § | 2.21 (0.90) | 2.45 (0.90) | 0.04 |
CHESS: Comprehensive Health Enhancement Support System; SD: Standard deviation
Summed across time points
N=201
Functional Assessment of Cancer Therapy Scale (FACT-L Version 4).
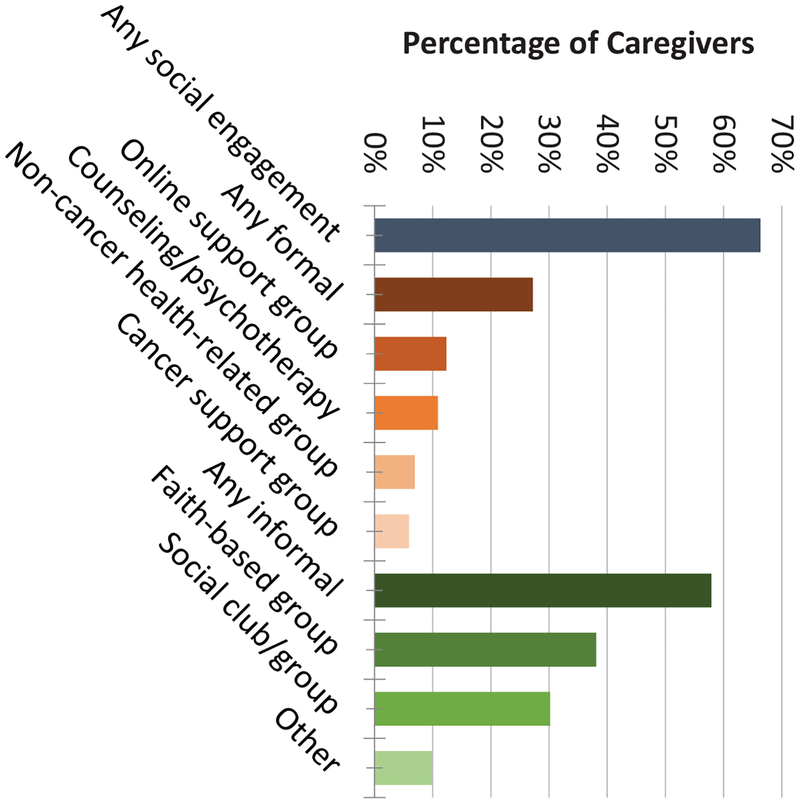
Nearly two-thirds of caregivers reported using one or more social resources at any time (66%, Figure 1). Informal resources were used more frequently than formal resources (58% and 27%, respectively). The most prevalent social resources were faith-based groups (38%) and social clubs (30%). Only a minority of caregivers participated in counseling (11%), other health-related groups (7%), or cancer support groups (6%). Online support group use was reported by 12% of caregivers.
Fig. 1.
Social Resource Use among Cancer Caregivers. Bars indicate the proportion of caregivers reporting use of the social resource at any time point over 6 months of follow-up. Data are from the Comprehensive Health Enhancement Support System (CHESS) – Prolonging Life study (2009–2012; n=202).
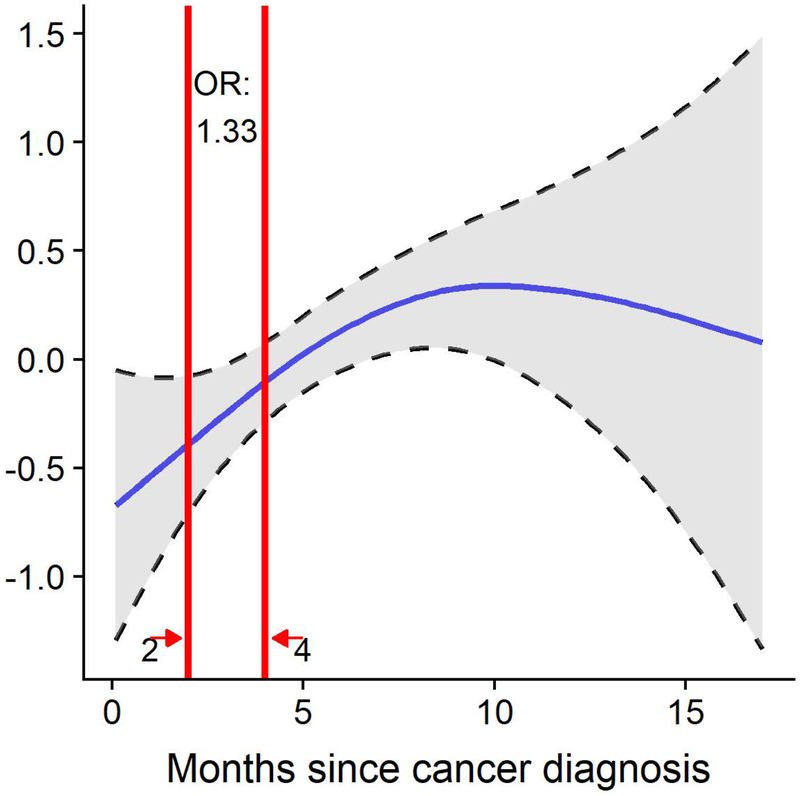
The generalized additive models showed that time since diagnosis was linearly associated with any and informal resource use and had a significant non-linear association with formal resource use (Figure 2). Formal social resource use increased early in the cancer trajectory such that a two month increase in time since diagnosis was associated with a 33% increase in likelihood of using formal resources (Odds ratio [OR]= 1.33, 95% confidence interval [CI]=1.18–1.50), leveling off at approximately ten-months post diagnosis.
Fig. 2.
Formal Social Resource Use over Time. The figure depicts the results of the generalized additive models regressing formal social resource use on time since diagnosis as a non-linear term. Unadjusted odds ratio comparing caregivers at 4 versus 2 months post cancer diagnosis is depicted. Data are from the Comprehensive Health Enhancement Support System (CHESS) – Prolonging Life study (2009–2012; n=202).
Table 2 depicts the correlates of formal social resource use. Caregivers with one or more health conditions were twice as likely to use formal resources compared to those with no health conditions (OR= 2.08, 95% CI=1.13–3.81). Conversely, patient comorbidities were associated with lower likelihood of caregivers’ formal resource use (OR=0.50, 95% CI=0.27–0.93), as was increased caregiver satisfaction with caregiving help (OR= 0.30, 95% CI=0.15–0.61). When the patient used social resources, caregivers were twice as likely to use formal resources themselves (OR=2.19, 95% CI=1.17–4.09).
Table 2.
Correlates of caregivers’ formal social resource use
| 95% CI | |||
|---|---|---|---|
| OR | Lower | Upper | |
| Coresidence | |||
| Caregiver does not live with patient | reference | ||
| Caregiver lives with patient | 0.72 | 0.43 | 1.21 |
| Income | |||
| ≤$40,000 | reference | ||
| $40,000-$80,000 | 0.96 | 0.40 | 2.32 |
| $80,000-$100,000 | 1.66 | 0.70 | 3.95 |
| $100,000 or more | 0.49 | 0.20 | 1.23 |
| Unreported | 0.19 | 0.02 | 1.86 |
| Caregiver comorbidities | |||
| None | reference | ||
| One or more | 2.12 | 1.16 | 3.90 |
| Satisfaction with caregiving help | |||
| Low-medium satisfaction | reference | ||
| Quite satisfied | 0.62 | 0.34 | 1.12 |
| Very satisfied | 0.30 | 0.15 | 0.59 |
| Patient comorbidities | |||
| None | reference | ||
| One or more | 0.51 | 0.28 | 0.96 |
| Recurrent cancer | |||
| No | reference | ||
| Yes | 2.00 | 0.75 | 5.37 |
| Patient social resource use | |||
| None | reference | ||
| One or more | 2.19 | 1.17 | 4.09 |
| Study condition | |||
| Control | reference | ||
| Intervention | 1.49 | 0.77 | 2.89 |
| Time since diagnosis | |||
| Months | 1.46 | 1.08 | 1.99 |
| Months squared | 0.98 | 0.96 | 1.00 |
OR: Odds Ratio; CI: Confidence Interval
Data are from the Comprehensive Health Enhancement Support System (CHESS) – Prolonging Life study (2009–2012)
Table 3 depicts the correlates of informal social resource use. Caregivers who were older and female were more likely to report using informal resources (OR =1.05, 95% CI=1.02–1.08 and OR=5.63, 95% CI= 2.36–13.44, respectively). Recurrent cancer was associated with decreased likelihood of the caregiver using informal social resources (OR=0.32, 95% CI=0.13–0.82). When the patient used social resources, caregivers were twice as likely to use informal resources themselves (OR= 2.03, 95% CI=1.35–3.05).
Table 3.
Correlates of caregivers’ informal social resource use
| 95% CI | |||
|---|---|---|---|
| OR | Lower | Upper | |
| Age (years) | 1.05 | 1.02 | 1.08 |
| Gender | |||
| Male | reference | ||
| Female | 5.63 | 2.36 | 13.44 |
| Employment | |||
| Employed full time | 0.72 | 0.42 | 1.24 |
| Employed part time or not employed | reference | ||
| Patient gender | |||
| Male | reference | ||
| Female | 1.54 | 0.75 | 3.13 |
| Surgery (yes vs no) | 0.58 | 0.23 | 1.45 |
| Recurrent cancer (yes vs no) | 0.32 | 0.13 | 0.82 |
| Patient social resource use | |||
| None | reference | ||
| One or more | 2.03 | 1.35 | 3.05 |
| Study condition | |||
| Control | reference | ||
| Intervention | 2.46 | 1.48 | 4.09 |
| Time since diagnosis (months) | 1.02 | 0.97 | 1.08 |
OR: Odds Ratio; CI: Confidence Interval
Data are from the Comprehensive Health Enhancement Support System (CHESS) – Prolonging Life study (2009–2012)
Sensitivity analyses.
When the sample was limited to caregivers assigned to the CHESS control condition (Supplementary Tables 3–5), many of the effects were amplified. For formal resources, the estimates for caregiver health conditions and recurrent cancer were further from the null (OR=2.78, 95% CI=1.01–7.67 and OR=4.05, 95% CI=1.49–11.04), while the estimates for patient comorbidities and satisfaction with caregiving help were similar but non-significant (OR= 0.59, 95% CI=0.22–1.61 and OR=0.41, 95% CI=0.13–1.30, respectively). For informal social resources, the estimate for age was similar (OR=1.06, 95% CI=1.02–1.10), and the estimates for gender, recurrent cancer, and the patient’s social resource use were further from the null (OR=11.10, 95% CI=3.31–37.16; OR=0.11, 95% CI=0.03–0.39; and OR=2.95, 95% CI=1.57–5.54, respectively). In the sensitivity analysis controlling for all covariates (Supplementary Tables 6–8), results were similar to the parsimonious models.
DISCUSSION
This study examined social resource use among informal caregivers of non-small cell lung cancer patients. Two-thirds of lung cancer caregivers reported engaging at least one social resource throughout the study and social resource use increased over time. The most common social resources were informal and were often not cancer-specific (i.e., social clubs/groups and faith-based activities). Only a quarter of caregivers reported using formal social resources (e.g., support groups) at any time, peaking at approximately 10-months post-diagnosis.
The levels of social engagement reported by the caregivers in this study were considerably lower than those noted in other populations. For example, among non-homebound older adults in the US, 80% attended a religious service and 69% attended a club, class or other organized activity in the past month.32 Caregivers in the present study were much less socially engaged: only 38% participated in religious groups and 30% participated in a social group or club over the 6 months of study follow-up. This finding echoes a broader body of evidence around social isolation and social activity constraints among family caregivers.24
Given the intensity and unpredictability of the cancer caregiving role, several nuanced phenomena likely underlie the patterns of social resource use across time. Increased social resource use may represent a return to caregivers’ usual patterns and routines as they adapt to the cancer diagnosis and the caregiving role, particularly with regard to informal social resources. This may also be motivated by coping strategies to maintain a “sense of normalcy.”17 As caregivers become increasingly comfortable with the role and label of caregiver, they may likewise be more likely to accept formal cancer-specific support. Early deterrents of “tragic stories” may become more accepted, and even validating, in face of their own reality of disease progression. As the cancer trajectory progresses, caregivers have more opportunities to hear about and use social resources available to them through interactions with social workers or other patients and families at clinics. Over time, caregiving may at turns become easier as caregivers learn the role, and harder as the patient’s disease progresses. The increasing need (e.g., because of stress, distress, or declining mental health) for social resources and different types of social support may be accompanied by decreasing capacity to engage these resources because of increasing patient needs and concomitant time and emotional constraints. The leveling out of formal social resource use after 10-months post-diagnosis, for example, could plausibly be driven by decreasing need, or alternatively, increasing intensity of the caregiving role as the patient’s cancer progresses.
In the present study, several predisposing and enabling/hindering factors emerged as key predictors of social resource use, including caregiver age and gender. In all analyses, the patients’ use of social resources was a strong independent predictor of caregivers’ social resource use. This association may indicate the interdependence and similarity between patients and caregivers’ experiences. Alternatively, patient social resource use may be a proxy for patient functional well-being or may directly influence the caregiver’s interest in or capacity for social engagement. Caregivers often feel guilty about needing a break,33 and the patient’s social engagement may provide tacit permission for the caregiver to engage in social activities as well. This finding points to the need for a more in-depth dyadic analysis of the interrelationships between caregiver and patient social resource use over time.
Myriad contextual factors likely play a role in caregivers’ choices around social activities, including time pressure and perceived strain,34,35 logistics (e.g., knowledge of available supports, transportation issues)36 and need/preference factors (e.g., feeling groups are “not for me”, trouble finding a group with “people like me”, perception of already having enough support).36 Given the heterogeneous needs, preferences, and constraints of cancer caregivers, better understanding these factors will improve our ability to understand which interventions are most likely to help individual caregivers. Such information will also inform better education, targeted needs assessments, and recommendations.
This study should be interpreted in light of several possible limitations. First, the list of social resources included in this study was not exhaustive. Furthermore, the question asked whether respondents “regularly participate” in these activities and did not specify a timeframe. Second, data were self-reported and are subject to possible reporting and recall bias. Third, though we sampled from sites across the country, our sample was largely receiving treatment at large urban cancer centers, possibly limiting generalizability to other populations. However, the patients and caregivers themselves represent urban, suburban and rural geographies. Fourth, the distribution of resource use limited our ability to examine each individual type of resource. Fifth, as a secondary analysis of data from an intervention study, the sample selection and participation in the intervention may impact the findings. We were unable assess pre-caregiving activity levels, caregivers’ need for social support, or support quality.
Nevertheless, this study offers the first assessment of social resource use over time for caregivers of lung cancer patients. While some features of the disease may be more unique or common to non-small cell lung cancer (e.g., dyspnea, smoking stigma, poor prognosis), much of the caregiver experience is shared across cancer disease sites (e.g., treatments, side effects, mortality salience) and is likewise applicable across cancer caregivers. Data were collected at multiple time points within the first year of the cancer trajectory. Although the findings here are primarily descriptive, the documented association between social engagement and well-being (e.g., higher positive and lower negative affect,37 lower levels of distress,13 and reductions in depressive symptoms11) suggests the potential importance of future research stemming from this work. Future research can build upon these findings to increase access to and acceptability of social resources in order to optimally meet the support needs of cancer caregivers. Such work will inform actionable recommendations and educational materials for caregivers and policy interventions to improve access to these important resources.
Supplementary Material
Acknowledgements:
Our thanks to Allison Woldt for her assistance with this project.
Funding: Funding for CHESS was provided by grants from the National Cancer Institute (1 P50 CA095817-01A1) and the National Institute of Nursing Research (R01 NR008260–01). Support for this project was also provided by the UW Carbone Cancer Center (P30 CA014520) and the UW Center for Demography of Health and Aging (P30 AG017266).
Footnotes
Conflicts of Interest: The authors do not have any conflicts to report.
REFERENCES
- 1.American Cancer Society. What is a Cancer Caregiver? https://www.cancer.org/treatment/caregivers/what-a-caregiver-does/who-and-what-are-caregivers.html. Published 2016. Accessed July 5, 2017.
- 2.Given BA, Given CW, Sherwood PR. Family and caregiver needs over the course of the cancer trajectory. J Support Oncol. 2012;10(2):57–64. [DOI] [PubMed] [Google Scholar]
- 3.American Cancer Society. Cancer Facts & Figures 2019. Atlanta: American Cancer Society;2019. [Google Scholar]
- 4.Stenberg U, Ruland CM, Miaskowski C. Review of the literature on the effects of caring for a patient with cancer. Psychooncology. 2010;19(10):1013–1025. [DOI] [PubMed] [Google Scholar]
- 5.Ji J, Zoller B, Sundquist K, Sundquist J. Increased risks of coronary heart disease and stroke among spousal caregivers of cancer patients. Circulation. 2012;125(14):1742–1747. [DOI] [PubMed] [Google Scholar]
- 6.Litzelman K, Yabroff KR. How are spousal depressed mood, distress, and quality of life associated with risk of depressed mood in cancer survivors? Longitudinal findings from a national sample. Cancer Epidemiol Biomarkers Prev. 2015;24(6):969–977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nijboer C, Tempelaar R, Triemstra M, van den Bos GA, Sanderman R. The role of social and psychologic resources in caregiving of cancer patients. Cancer. 2001;91(5):1029–1039. [PubMed] [Google Scholar]
- 8.Ownsworth T, Henderson L, Chambers SK. Social support buffers the impact of functional impairments on caregiver psychological well-being in the context of brain tumor and other cancers. Psychooncology. 2010;19(10):1116–1122. [DOI] [PubMed] [Google Scholar]
- 9.Wong AG, Ki P, Maharaj A, Brown E, Davis C, Apolinsky F. Social support sources, types, and generativity: a focus group study of cancer survivors and their caregivers. Soc Work Health Care. 2014;53(3):214–232. [DOI] [PubMed] [Google Scholar]
- 10.Longacre ML, Ridge JA, Burtness BA, Galloway TJ, Fang CY. Psychological functioning of caregivers for head and neck cancer patients. Oral Oncol. 2012;48(1):18–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Min J, Ailshire J, Crimmins EM. Social engagement and depressive symptoms: do baseline depression status and type of social activities make a difference? Age Ageing. 2016;45(6):838–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kroenke CH, Michael YL, Poole EM, et al. Postdiagnosis social networks and breast cancer mortality in the After Breast Cancer Pooling Project. Cancer. 2017;123(7):1228–1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Oshio T, Kan M. How do social activities mitigate informal caregivers’ psychological distress? Evidence from a nine-year panel survey in Japan. Health Qual Life Outcomes. 2016;14(1):117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Applebaum AJ, Breitbart W. Care for the cancer caregiver: a systematic review. Palliat Support Care. 2013;11(3):231–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.American College of Surgeons Commission on Cancer. Cancer Program Standards 2012: Ensuring Patient-Centered Care. Chicago, IL: American College of Surgeons;2012. [Google Scholar]
- 16.Kohle N, Drossaert CH, Oosterik S, et al. Needs and Preferences of Partners of Cancer Patients Regarding a Web-Based Psychological Intervention: A Qualitative Study. JMIR Cancer. 2015;1(2):e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mosher CE, Ott MA, Hanna N, Jalal SI, Champion VL. Coping with physical and psychological symptoms: a qualitative study of advanced lung cancer patients and their family caregivers. Support Care Cancer. 2015;23(7):2053–2060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morse KD, Gralla RJ, Petersen JA, Rosen LM. Preferences for cancer support group topics and group satisfaction among patients and caregivers. J Psychosoc Oncol. 2014;32(1):112–123. [DOI] [PubMed] [Google Scholar]
- 19.Van Ryn M, Sanders S, Kahn K, et al. Objective burden, resources, and other stressors among informal cancer caregivers: a hidden quality issue? Psycho‐Oncology. 2011;20(1):44–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Alliance for Caregiving. Caregiving in the US 2015. Washington DC: NAC and the AARP Public Institute;2015. [Google Scholar]
- 21.Korotkin BD, Hoerger M, Voorhees S, Allen CO, Robinson WR, Duberstein PR. Social support in cancer: How do patients want us to help? J Psychosoc Oncol. 2019:1–14. [DOI] [PubMed] [Google Scholar]
- 22.Sklenarova H, Krumpelmann A, Haun MW, et al. When do we need to care about the caregiver? Supportive care needs, anxiety, and depression among informal caregivers of patients with cancer and cancer survivors. Cancer. 2015;121(9):1513–1519. [DOI] [PubMed] [Google Scholar]
- 23.Williams GR, Pisu M, Rocque GB, et al. Unmet social support needs among older adults with cancer. Cancer. 2019;125(3):473–481. [DOI] [PubMed] [Google Scholar]
- 24.Keating N, Eales J. Social consequences of family care of adults: a scoping review. International Journal of Care and Caring. 2017;1(2):153–173. [Google Scholar]
- 25.Häggmark C, Theorell T, Ek B. Coping and social activity patterns among relatives of cancer patients. Soc Sci Med. 1987;25(9):1021–1025. [DOI] [PubMed] [Google Scholar]
- 26.DuBenske LL, Gustafson DH, Shaw BR, Cleary JF. Web-based cancer communication and decision making systems: connecting patients, caregivers, and clinicians for improved health outcomes. Med Decis Making. 2010;30(6):732–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 28.Bruera E, Kuehn N, Miller MJ, Selmser P, Macmillan K. The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patients. J Palliat Care. 1991;7(2):6–9. [PubMed] [Google Scholar]
- 29.Cella DF, Bonomi AE, Lloyd SR, Tulsky DS, Kaplan E, Bonomi P. Reliability and validity of the Functional Assessment of Cancer Therapy—Lung (FACT-L) quality of life instrument. Lung Cancer. 1995;12(3):199–220. [DOI] [PubMed] [Google Scholar]
- 30.Wood SN. Generalized additive models: an introduction with R. Chapman and Hall/CRC; 2017. [Google Scholar]
- 31.Schratz P. Odds Ratio Calculation for GAM(M)s & GLM(M)s (version 2.0.0). In: CRAN; 2019. [Google Scholar]
- 32.Szanton SL, Roberts L, Leff B, et al. Home but still engaged: participation in social activities among the homebound. Qual Life Res. 2016;25(8):1913–1920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dionne-Odom JN, Applebaum AJ, Ornstein KA, et al. Participation and interest in support services among family caregivers of older adults with cancer. Psychooncology. 2018;27(3):969–976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Miller B, Montgomery A. Family caregivers and limitations in social activities. Res Aging. 1990;12(1):72–93. [DOI] [PubMed] [Google Scholar]
- 35.Harding R, Higginson IJ, Leam C, et al. Evaluation of a short-term group intervention for informal carers of patients attending a home palliative care service. J Pain Symptom Manage. 2004;27(5):396–408. [DOI] [PubMed] [Google Scholar]
- 36.Ussher JM, Kirsten L, Butow P, Sandoval M. A qualitative analysis of reasons for leaving, or not attending, a cancer support group. Soc Work Health Care. 2008;47(1):14–29. [DOI] [PubMed] [Google Scholar]
- 37.Huxhold O, Miche M, Schüz B. Benefits of having friends in older ages: Differential effects of informal social activities on well-being in middle-aged and older adults. J Gerontol B Psychol Sci Soc Sci. 2013;69(3):366–375. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.