Abstract
It is well known that the most common sites for venous access are the superficial veins of the upper limb, particularly dorsal metacarpal veins and median cubital vein. Although dorsal metacarpal veins are the first choice for venous cannulation, there is scarce information about their anatomic variation. Hence, detailed anatomical information about these veins will improve the anatomic knowledge of the health care providers. Subsequently, this study was designed to study the dorsal metacarpal veins and to determine the most prominent dorsal metacarpal vein. A cross sectional study of 402 subjects (804 hands), was prepared to study the superficial veins on the dorsum of the hand among Jordanian students and staff of one of the major governmental medical colleges in Jordan, by using infrared illumination system. The obtained data was analyzed according to sex, sidedness, and handedness. Six locations of the most prominent dorsal metacarpal veins were identified. There was a significant relation between both females and males and the most prominent dorsal metacarpal vein (P=0.01). For the first time this study identified the most common location of the most prominent dorsal metacarpal vein in the fourth intermetacarpal space.
Keywords: Anatomic variation, Dorsal metacarpal veins, Hand, Veins, Venous access
Introduction
One of the most common procedures used by medical staff is setting up venous access. It is considered a major component of care for both inpatients and outpatients. It seems viewed as a simple technique, but it requires good anatomical knowledge about the targeted veins.
Veins are classified according to their location to the deep fascia into superficial and deep veins; they communicate by perforating veins. The location of the superficial veins within the superficial fascia provides an easy access for cannulation and blood drawing for clinical tests. In addition to venous access, the superficial veins are clinically used for right cardiac catheterization [1].
The superficial veins of the upper extremities are more desirable than the superficial veins of the lower extremities. The venous access of the lower extremities is less durable and accompanied with more complications like venous thromboembolism [2,3]. Moreover, venous access in the lower extremities limits patients mobility [4].
The superficial veins of the forearm, the hand and less often the foot have been commonly used for venous access [5]. Among the superficial veins; dorsal metacarpal veins (dorsal MCVs), cephalic vein (CV), and basilic vein (BV) are the most common sites for venous access [3]. The superficial veins of the hands are the digital, metacarpal and the begening of the BV on the ulnar side and the CV on the radial side on dorsum of the hand. The veins on the dorsum of the hand are easily palpated, readily visible and supported by metacarpal bones. The dorsal MCVs are the first choice for venous cannulation essentially in pediatric patients [6], while the distal part of the CV has been suggested for vein puncture [7]. It has been indicated that catheterization of the veins in the dorsum of the hand in obstetric patients is more successful than the veins in the lower forearm [8]. However, in urgent situations, the median cubital vein of the forearm is the first choice for cannulation [3].
The advantages to use dorsal MCVs are easeness of accessibility and distal location of the veins, which allow utilization of more proximal veins in the same upper limb when needed [8]. On the other hand, the disadvantages to use these veins are the small size of the veins and the tendency to be mobile [9].
In the elderly however, the veins in the dorsum of the hand are not the preferable site for venous access because the veins are more mobile and fragile and the needle may cause bruising and bleeding under the skin, furthermore, they are tortuous and could be thrombosed [2].
Vein viewer can be applied for many purposes as in plastic surgery procedure; microsurgical anastomoses and most commonly in phlebotomy and intravenous access [10]. Many studies were performed to determine the efficiency of the vein viewer in difficult vein access or vein find specifically in pediatric patients with excellent results, having successful venous access from the first attempt, as well in locating the vein [11,12].
Thus, it seems that the superficial veins on the dorsum of the hand are of a major clinical value. Numerous papers and books have provided detailed information about the normal anatomical variations of the antecubital veins [13,14]. While the superficial veins of the hand are variant and complicated, despite their clinical value, there is scarce information about their normal anatomical variations. Thus the goals of the present study were to identify the dorsal MCVs and to determine the most prominent dorsal MCV.
Materials and Methods
Subjects
Four hundred and two subjects were enrolled in the study; 217 males and 185 females. Subjects ranged from 18 to 35 years old; they were students and staff of the medical college. A total number of 804 hands were examined. Subjects who had hand injuries, scars, burns were excluded. Subjects were informed in details about the procedure and a written consent was signed. The study was approved by the Institution Review Board of the university (IRB No. P.0/222/1704841).
Instruments
The infrared (IR) vein illumination system (Sure vein ZD-JM-260-01) has been used to identify the dorsal MCVS. It utilizes 750–980 nm wavelength of infrared light, with effective distance of projection of 29–31 cm.
Study design
The procedure was conducted in a dark room with a temperature between 24℃ and 26℃. On the day of the experiment, subjects were instructed to sit and to grip the transmitter device while the forearm was in pronated position (Fig. 1). Before exposing the hand to the IR beam, the targeted area was carefully identified. The targeted area was bounded distally by the flexed second, third, fourth, and fifth metacarpophalangeal joints (MPJs) and proximally by the wrist joint. On the sides of the dorsum of the hand, an imaginary line from the medial side of the fifth MPJ considered the medial boundary of the target area, while an imaginary line from the lateral side of second MPJ considered the lateral boundary.
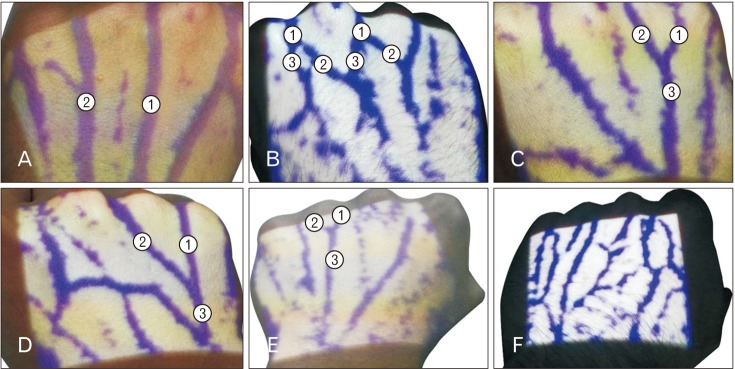
Fig. 1. (A) Left hand showing long dorsal metacarpal veins (1) and (2), which neither bifurcate nor unite and continue to pass on the dorsum of the hand between the metacarpophalangeal joints. (B) Right hand showing the dorsal metacarpal veins (1), which bifurcate into two veins (2) and (3). (C) Right hand showing short dorsal metacarpal veins (1) and (2), which unite near their origin to form one long dorsal metacarpal vein (3). (D) Right hand showing two adjacent dorsal metacarpal veins (1) and (2), which unite away from their origin to form one short dorsal metacarpal vein (3). (E) Left hand showing two short dorsal metacarpal veins (1) and (2), which unite near their origin and form one long dorsal metacarpal vein (3) passes parallel to the corresponding extensor tendon. (F) Left hand showing dorsal metacarpal veins running in different directions and forming network of veins on the dorsum of the hand with no prominent vein.
The most prominent dorsal MCV was identified as straighter, more vertical and with less communicating veins. The subject's hand was then exposed to the IR beam; the dorsal MCVs were photographed by a mobile phone camera. Images were carefully analyzed and grouped according to the course of the metacarpal veins.
Statistical analysis
Data analysis was performed using IBM SPSS Statistics version 22 software (IBM Corp., Armonk, NY, USA). A chi-square test was used to test the association between gender, sidedness and handedness, and common site of the most prominent dorsal MCV. Statistical comparisons were made by Student's unpaired t test. The association was considered statistically significant if P<0.05.
Results
The initial population of this study consisted of 402 subjects; 217 males and 185 females (Table 1). The total number of hands was 804 hands. The number of hands included in this study was 435 in males and 369 in females (Table 1). The number of right hands included in the study 401 was nearly equal to left hands 403 (Table 1). One hundred and eighteen hands were excluded (exclusion rate 15%) and 187 hands (23%) were with complex pattern of veins. The final number of hands included in the study was 503 hands.
Table 1. Demographic and experimental characteristics of the final population of the dorsal metacarpal veins study.
| Characteristic | No. of subjects (%) | No. of hands (%) |
|---|---|---|
| Sex | ||
| Male | 217 (54) | 435 (54) |
| Female | 185 (46) | 369 (46) |
| Hand | - | - |
| Right | - | 401 (49.9) |
| Left | - | 403 (50.1) |
| Symmetry | ||
| Yes | 212 (53) | - |
| No | 190 (47) | - |
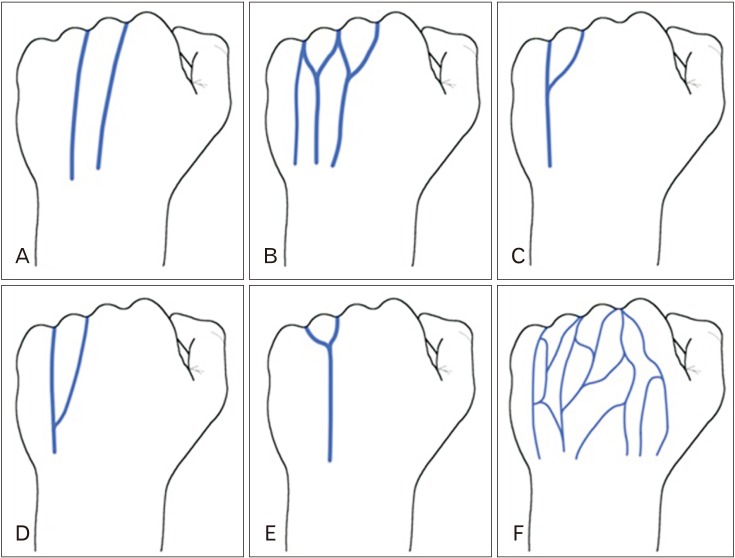
It was found during the examination of the dorsum of the hand, that the dorsal MCVs had different courses and communications. Some dorsal MCVs ran between the knuckles of the hand as long dorsal MCVs on the dorsum of the hand (Figs. 1A, 2A), while other dorsal MCVs bifurcated into two veins, where they united with the adjacent bifurcated vein to form short metacarpal veins (Figs. 1B, 2B). It has been also identified that some dorsal MCVs united with an adjacent vein near their origin and formed long metacarpal veins (Figs. 1C, 2C), or away from their origin and formed short metacarpal veins (Figs. 1D, 2D). In addition, some of the dorsal MCVs united with an adjacent vein near their origin and passed parallel to the corresponding extensor tendon (Figs. 1E, 2E). Finally, some of the examined dorsal MCVs were running in different directions and were forming a network of veins on the dorsum of the hand (Figs. 1F, 2F).
Fig. 2. Illustration of the different courses and communications of the dorsal metacarpal veins showing long dorsal metacarpal veins (A). (B) Short dorsal metacarpal veins which bifurcate into two veins. (C) Short dorsal metacarpal veins which unite near their origin to form one long dorsal metacarpal vein (D) Two adjacent dorsal metacarpal veins (1) which unite away from their origin to form one short dorsal metacarpal vein. (E) Two short dorsal metacarpal veins which unite near their origin and form one long dorsal metacarpal vein. (F) Dorsal metacarpal veins running in different directions and forming network of veins on the dorsum of the hand with no prominent vein.
The most prominent metacarpal vein was identified according to its origin relative to the MPJs (knuckles) of the hand which courses in intermetacarpal spaces. Veins were classified according to their origin as follows.
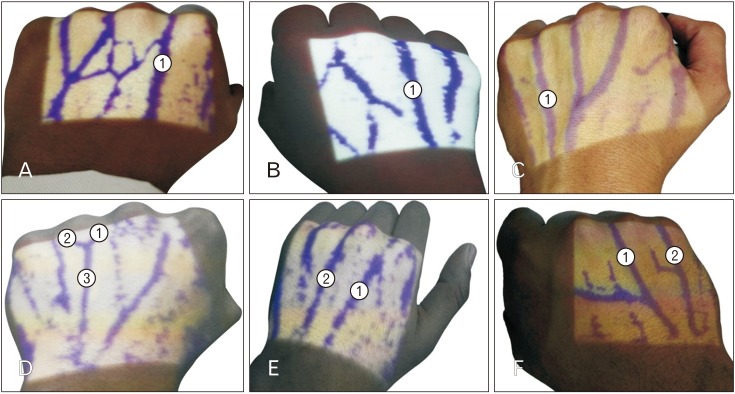
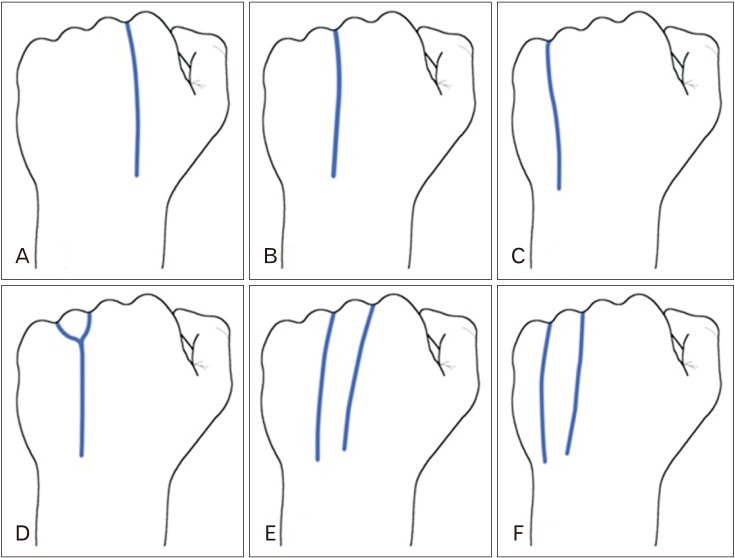
Type A1 was present in 53 (11%) of the examined hands, being one prominent vein in the second intermetacarpal space originated between second and third MPJs (Figs. 3, 4). Type A2 occurred in 128 (25%) of the examined hands, where there was one prominent vein in third intermetacarpal space originated between third and fourth MPJs (Figs. 3, 4). Type A3 was the most common being in 229 (46%) of the examined hands (one prominent vein in fourth intermetacarpal space originated between fourth and the fifth MPJs (Figs. 3, 4). Lastly in the A subtypes, A4, accounted for 6% (n=29) of the examined hands having one prominent vein parallel to extensor digitorum tendon of the fourth digit (ring finger) (Figs. 3, 4). There were two type Bs: type B1 (n=12, 2%) of the examined hands, where two prominent veins were found in second and third intermetacarpal spaces, they originated between second and third MPJs and between third and fourth MPJs, respectively (Figs. 3, 4), and type B2 (n=52, 10%) where two prominent veins were found in third and fourth intermetacarpal spaces, they originated between third and fourth MPJs and between fourth and fifth MPJs, respectively (Figs. 3, 4).
Fig. 3. (A) Left hand showing prominent dorsal metacarpal vein (1) in the second metacarpal space between the second and third metacarpophalangeal joints. (B) Right hand showing prominent dorsal metacarpal vein (1) in the third metacarpal space between the third and fourth metacarpophalangeal joints. (C) Left hand showing prominent dorsal metacarpal vein (1) in the fourth metacarpal space between fourth and fifth metacarpophalangeal joints. (D) Left hand showing two short dorsal metacarpal veins (1) and (2) unite to form one prominent dorsal metacarpal vein (3) parallel to the extensor digitorum tendon of the fourth digit (ring finger). (E) Left hand showing two prominent dorsal metacarpal veins, one vein (1) in the second metacarpal space, between the second and third metacarpophalangeal joints and another vein (2) in the third metacarpal space between the third and fourth metacarpophalangeal joints. (F) Left hand showing two prominent dorsal metacarpal veins, one vein (1) in the third metacarpal space between third and fourth metacarpophalangeal joints and another vein (2) in fourth metacarpal space between fourth and fifth metacarpophalangeal joints.
Fig. 4. Illustration of the classification of the most prominent dorsal metacarpal veins according to their origin.
The most common location of the most prominent dorsal MCV was in fourth intermetacarpal space (A3) at 46% (Table 2) and was the most common in both males 118 (45%) and females 101 (44%) (Table 3). In addition, it was equally distributed in both the right (n=112, 46%) and left hands (n=117, 45%) (Table 3) as well as both right handed 99 (42%) and left handed 12 (31%) participants (Table 3). Moreover, it was noted that the symmetry of location of the most prominent dorsal MCV between both hands in the same subject was 29% (n=117) (Table 4).
Table 2. Subtotal frequencies of the anatomic variants under study of the most prominent MCV on the dorsum of the hand.
| Most prominent dorsal MCV | Subtotal (% total) (n=503) |
|---|---|
| A1 | 53 (11) |
| A2 | 128 (25) |
| A3 | 229 (46) |
| A4 | 29 (6) |
| B1 | 12 (2) |
| B2 | 52 (10) |
MCV, metacarpal vein.
Table 3. Frequency and number of the most prominent MCVon the dorsum of the hand according to sidedness, sex, and handedness (laterality).
| Most prominent dorsal MCV | Sidedness (n=503) | Sex (n=493) | Handedness (n=276) | |||
|---|---|---|---|---|---|---|
| Right hand | Left hand | Male | Female | Right handed | Left handed | |
| A1 | 25 (10) | 28 (11) | 33 (13) | 20 (9) | 26 (11) | 5 (13) |
| A2 | 63 (26) | 65 (25) | 71 (27) | 57 (25) | 57 (24) | 7 (18) |
| A3 | 112 (46) | 117 (45) | 118 (45) | 101 (44) | 99 (42) | 12 (31) |
| A4 | 12 (5) | 17 (7) | 7 (3) | 22 (10) | 18 (8) | 5 (13) |
| B1 | 8 (3) | 4 (2) | 9 (3) | 3 (1) | 7 (3) | 1 (3) |
| B2 | 24 (10) | 28 (11) | 26 (10) | 26 (11) | 30 (13) | 9 (23) |
| Subtotal | 244 (48.5) | 259 (51.5) | 264 (53.5) | 229 (46.5) | 237 (86) | 39 (14) |
Values are presented as number (%). MCV, metacarpal vein.
Table 4. The possible symmetry of location of the most prominent dorsal MCV between both hands in the same subject.
| Most prominent dorsal MCV | Right and left hand frequency |
|---|---|
| A1 | 4 (1) |
| A2 | 22 (5) |
| A3 | 51 (13) |
| A4 | 5 (1) |
| B1 | 2 (0.5) |
| B2 | 8 (2) |
| No vein | 25 (6) |
| Total | 117/402 (29) |
Values are presented as number (%). MCV, metacarpal vein.
Statistical analysis using chi-square test, there was not a significant relation between both right and left hands, and site of the most prominent dorsal MCV (P=0.769). There was a significant relation between both females and males, and the site of the most prominent dorsal MCV (P=0.013). There was not a significant relation between right handed and left handed subjects, and the site of the most prominent dorsal MCV (P=0.376).
Discussion
The aim of the present study was to identify the most prominent vein on the dorsum of the hand. A recent study that examined the dorsal MCVs and for the first time they were recognized and classified into different anatomical patterns rather than considering them as a network of veins [15]. However, employing earlier mentioned patterns would not help in recognition of a prominent vein. Patterns were based on the shape of connections between different veins, while identifying a prominent vein should have focused on the individual course of the vein. Thus, the course of the individual dorsal metacarpal veins that were investigated in the present study found that veins on the dorsum of the hand have different courses and communications.
Findings in the present study clearly showed that whatever the course of dorsal MCVs, there were predominantly one or two veins that would run in a straight, vertical course and have less communicating veins connected to them. The only exception was, perhaps, when the dorsal metacarpal veins were forming a network of veins on the dorsum of the hand. Therefore, to identify the most prominent vein on the dorsum of the hand three major criteria were proposed based on the common criteria generally used in choosing an ideal vein for venous access. The criteria of an ideal vein were reported as straight, vertical and has less branches or anastomosis veins [16]. The present study adopted almost the same criteria and took the MPJs and intermetacarpal spaces as reference points to make the recognition of the veins easier.
Applying the above mentioned criteria, it was found that the most prominent vein was located in the fourth intermetacarpal space in 46% of the examined hands. Moreover, the prominent vein which often was located in the fourth intermetacarpal space in both hands as well as in both genders. To a lesser extent there was one prominent vein in the third intermetacarpal space between third and fourth MPJs in 25% and there was one prominent vein in the second intermetacarpal space between second and third MPJs. In addition, there was one prominent vein parallel to extensor digitorum tendon of the fourth digit.
The present study did not investigate why it was possible to have a prominent vein but it has been noted that the location of the prominent vein was more frequent on the medial side of the hand, with the veins of the dorsum of the hand ultimately grouped into radial veins on the lateral side of the dorsum of the hand to form the CV and ulnar group of veins on the medial side to form the BV [17]. Therefore, veins coming from the third intermetacarpal space may need to cross the dorsum of the hand in an oblique course or be connected to adjacent vein to reach the medial side of the hand to participate in the formation of the BV. However, the dorsal MCV in the fourth metacarpal space between the fourth and fifth MPJs is more medial and in line with the BV without any need to be connected to other veins. This may explain the fact that most prominent veins were found on the medial rather than on the lateral side. Moreover, when two prominent veins were identified they were also located in the third and fourth intermetacarpal spaces between third and fourth MPJs and fourth and fifth MPJs.
It is important to mention that the dorsal MCVs on the lateral side of the dorsum of the hand coming from the first and second metacarpal spaces were usually involved in the formation of the radial group of veins that form the CV. In addition, the dorsal MCV that usually runs in the first metacarpal space was not examined in the present study as it was outside of the designed experimental procedure. However, veins in this space are usually oblique and close to radial artery located in this area and to the superficial branch of the radial nerve, therefore, veins in this area are not preferable for venous access [18,19].
Footnotes
- Conceptualization: MAS.
- Data acquisition: MAS.
- Data analysis or interpretation: MAS, ATS.
- Drafting of the manuscript: MAS.
- Critical revision of the manuscript: ATS, DHB, MAAA, IMM, AMBH.
- Approval of the final version of the manuscript: all authors.
Conflicts of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Lee SH, Chun KJ, Lee DS, Lee SY, Hwang J, Chon MK, Hwang KW, Kim JS, Park YH, Kim JH. Right cardiac catheterization using the antecubital fossa vein in Korean patients. Korean Circ J. 2016;46:207–212. doi: 10.4070/kcj.2016.46.2.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scales K. Vascular access in the acute care setting. In: Dougherty L, Lamb J, editors. Intravenous Therapy in Nursing Practice. Oxford: Blackwell Publishing; 2008. pp. 261–299. [Google Scholar]
- 3.Ortega R, Sekhar P, Song M, Hansen CJ, Peterson L. Videos in clinical medicine. Peripheral intravenous cannulation. N Engl J Med. 2008;359:e26. doi: 10.1056/NEJMvcm0706789. [DOI] [PubMed] [Google Scholar]
- 4.Mbamalu D, Banerjee A. Methods of obtaining peripheral venous access in difficult situations. Postgrad Med J. 1999;75:459–462. doi: 10.1136/pgmj.75.886.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheung E, Baerlocher MO, Asch M, Myers A. Venous access: a practical review for 2009. Can Fam Physician. 2009;55:494–496. [PMC free article] [PubMed] [Google Scholar]
- 6.King C, Henretig FM. Textbook of pediatric emergency procedures. Philadelphia, PA: Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 7.Loukas M, Tubbs RS, Feldman J. Netter's introduction to clinical procedures. Philadelphia, PA: Elsevier Health Sciences; 2016. [Google Scholar]
- 8.Tan PC, Mackeen A, Khong SY, Omar SZ, Noor Azmi MA. Peripheral intravenous catheterisation in obstetric patients in the hand or forearm vein: a randomised trial. Sci Rep. 2016;6:23223. doi: 10.1038/srep23223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Malamed SF. Sedation: a guide to patient management. 6th ed. St. Louis, MO: Elsevier; 2017. [Google Scholar]
- 10.Varma NR, Sahane SD, Thankre SS. Infrared VeinViewer. Int J Eng Educ Technol. 2014;2:1–6. [Google Scholar]
- 11.Kim MJ, Park JM, Rhee N, Je SM, Hong SH, Lee YM, Chung SP, Kim SH. Efficacy of VeinViewer in pediatric peripheral intravenous access: a randomized controlled trial. Eur J Pediatr. 2012;171:1121–1125. doi: 10.1007/s00431-012-1713-9. [DOI] [PubMed] [Google Scholar]
- 12.Hess HA. A biomedical device to improve pediatric vascular access success. Pediatr Nurs. 2010;36:259–263. [PubMed] [Google Scholar]
- 13.Ukoha UU, Oranusi CK, Okafor JI, Ogugua PC, Obiaduo AO. Patterns of superficial venous arrangement in the cubital fossa of adult Nigerians. Niger J Clin Pract. 2013;16:104–109. doi: 10.4103/1119-3077.106777. [DOI] [PubMed] [Google Scholar]
- 14.Hamzah AA, Ramasamy S, Adnan AS, Khan AH. Pattern of superficial venous of the cubital fossa among volunteers in a tertiary hospital. Trop Med Surg. 2014;2:1000164 [Google Scholar]
- 15.Elmegarhi SS, Amarin JZ, Hadidi MT, Badran DH, Massad IM, Bani-Hani AM, Shatarat AT. Dorsal metacarpal veins: anatomic variation and potential clinical implications. Anat Sci Int. 2018;93:238–243. doi: 10.1007/s12565-017-0403-0. [DOI] [PubMed] [Google Scholar]
- 16.Dougherty L, Lamb J. Intravenous therapy in nursing practice. 2nd ed. Oxford: Blackwell Publishing; 2008. [Google Scholar]
- 17.Zhang SX, Schmidt HM. Clinical anatomy of the subcutaneous veins in the dorsum of the hand. Ann Anat. 1993;175:381–384. doi: 10.1016/s0940-9602(11)80048-8. [DOI] [PubMed] [Google Scholar]
- 18.Robson AJ, See MS, Ellis H. Applied anatomy of the superficial branch of the radial nerve. Clin Anat. 2008;21:38–45. doi: 10.1002/ca.20576. [DOI] [PubMed] [Google Scholar]
- 19.Samarakoon LB, Lakmal KC, Thillainathan S, Bataduwaarachchi VR, Anthony DJ, Jayasekara RW. Anatomical relations of the superficial sensory branches of the radial nerve: a cadaveric study with clinical implications. Patient Saf Surg. 2011;5:28. doi: 10.1186/1754-9493-5-28. [DOI] [PMC free article] [PubMed] [Google Scholar]