Abstract
The risk for major depression is both genetically and environmentally determined. It has been proposed that epigenetic mechanisms could mediate the lasting increases in depression risk following exposure to adverse life events and provide a mechanistic framework within which genetic and environmental factors can be integrated. Epigenetics refers to processes affecting gene expression and translation that do not involve changes in the DNA sequence and include DNA methylation (DNAm) and microRNAs (miRNAs) as well as histone modifications. Here we review evidence for a role of epigenetics in the pathogenesis of depression from studies investigating DNAm, miRNAs, and histone modifications using different tissues and various experimental designs. From these studies, a model emerges where underlying genetic and environmental risk factors, and interactions between the two, could drive aberrant epigenetic mechanisms targeting stress response pathways, neuronal plasticity, and other behaviorally relevant pathways that have been implicated in major depression.
Keywords: depression, genome-wide association study, DNA methylation, microRNA, histone acetylation, histone methylation
Abstract
El riesgo de presentar una depresión mayor está determinado genética y ambientalmente. Se ha planteado que los mecanismos epigenéticos podrían mediar los aumentos permanentes en el riesgo de depresión después de la exposición a acontecimientos adversos de la vida y proporcionar un marco mecanicista dentro del cual se puedan integrar los factores genéticos y ambientales. La epigenética abarca procesos que afectan la expresión y la traducción de genes que no implican cambios en la secuencia de ADN e incluyen metilación del ADN (DNAm), microARN (miARN), así como modificaciones de histonas. En este artículo se revisa la evidencia de la participación de la epigenética en la patogénesis de la depresión a partir de estudios que investigan las modificaciones de ADNm, miRNA e histonas mediante el empleo de diferentes tejidos y varios diseños experimentales. De estos estudios surge un modelo en el que los factores de riesgo genéticos y ambientales subyacentes, como las interacciones entre ambos, podrían conducir a mecanismos epigenéticos aberrantes con efectos en las vías de respuesta al estrés, en la plasticidad neuronal y en otras vías relevantes conductualmente que se han implicado en la depresión mayor.
Abstract
Le risque de dépression majeure est déterminé à la fois génétiquement et par l’environnement. Des mécanismes épigénétiques pourraient relayer les augmentations durables de risque de dépression après une exposition aux événements de vie difficiles et fournir un cadre mécanistique dans lequel facteurs environnementaux et génétiques pourraient s’intégrer. L’épigénétique fait référence aux processus en rapport avec la traduction et l’expression des gènes sans modification de la séquence d’ADN : méthylation de l’ADN (ADNm), microARN (ARNmi) et modifications de l’histone. Dans cet article nous analysons des données d’études, dans différents tissus et à l’aide de schémas expérimentaux variés, sur l’ADNm, les ARNm et les modifications de l’histone comme preuves d’un rôle de l’épigénétique dans la pathogenèse de la dépression. De ces études émerge un modèle dans lequel des facteurs de risque génétiques et environnementaux, et les interactions entre les deux, pourraient susciter des mécanismes épigénétiques aberrants ciblant les voies de réponse au stress, la plasticité neuronale et d’autres voies comportementales impliquées dans la dépression majeure.
Introduction
Major depressive disorder (MDD) is currently the primary cause of disability worldwide 1 and the World Health Organization predicts it will generate the greatest global burden by 2030. 2 Despite these significant social and economic costs, the molecular mechanisms underlying MDD remain poorly understood.
It is well established that the risk for MDD is partially mediated by genetic factors. A meta-analysis quantified the increased risk of MDD as an odds ratio (OR) of 2.84 (95% CI = 2.31-3.49) for first-degree relatives of individuals with MDD. 3 A large twin study in a Swedish population estimated the heritability of MDD to be approximately 37%, which is consistent with estimates made in previous studies. 4 In more recent years, technological advances made in high-throughput genotyping have enabled researchers to move beyond family-based heritability studies of MDD to identify disease-associated susceptibility loci using genome-wide association studies (GWAS). What has become clear from these studies is that MDD is a polygenic disorder, with multiple loci being identified, but each with a small effect. The latest GWAS of MDD meta-analyzed data from 807 553 individuals and identified 102 loci that were associated with the disorder at genome-wide significance. 5 Despite the strong evidence from both family-based heritability studies and GWAS indicating that genetic risk factors play an integral role in the pathogenesis of MDD, the heritability estimates (~40%) are less than those for other neuropsychiatric disorders, such as schizophrenia, bipolar disorder, and attention-deficit/hyperactivity disorder (all between 75% and 80%). 6 , 7 , 8 This suggests that other factors also play a role in mediating the risk for MDD. Indeed, it is well established that environmental factors, especially stress and exposure to adverse life events, contribute to the risk. 9 For example, a meta-analysis of 26 studies found that childhood trauma, especially neglect and emotional abuse, was strongly associated with depression in adulthood (OR 2.78 for neglect and 2.75 for emotional abuse). 10
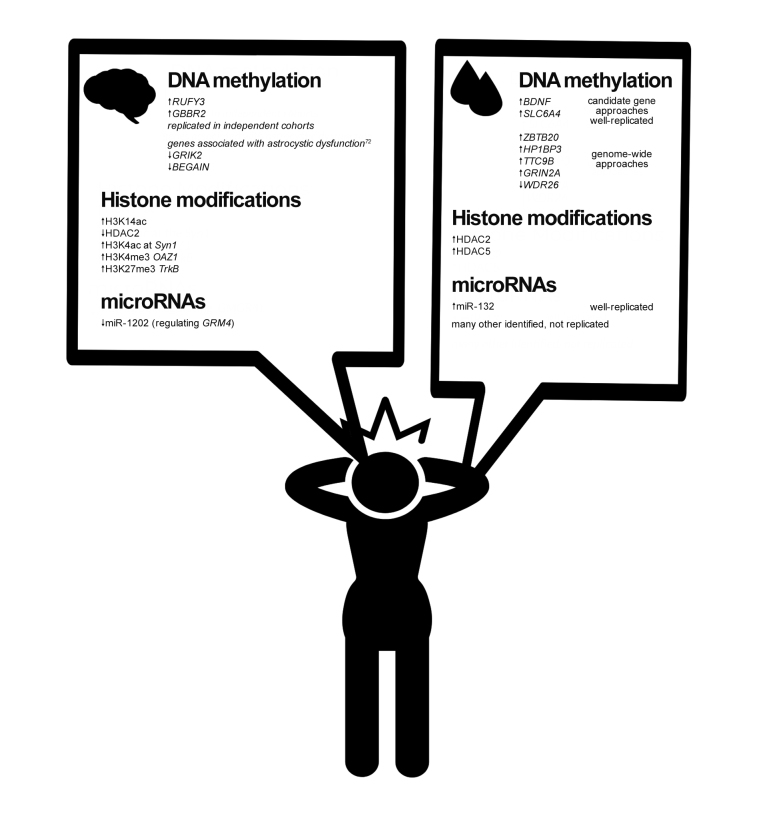
Recently, it was proposed that epigenetic mechanisms could mediate the lasting increases in depression risk following exposure to an adverse life event and provide a mechanistic framework within which genetic and environmental factors can be integrated. 11 Broadly, epigenetics refers to processes affecting gene expression and translation that do not involve changes in the DNA sequence. Epigenetic processes include DNA methylation (DNAm), small noncoding RNAs such as microRNAs (miRNAs), and histone modifications, among others. Epigenetic processes are integral in normal biological processes such as cellular differentiation, but have also been implicated in disease states. In the following, we will summarize evidence for the contribution of epigenetic processes in the pathogenesis of MDD. We include results from studies investigating DNAm, miRNAs, and histone modifications using different tissues and various experimental designs. This is summarized in Figure 1 .
Evidence for epigenetic processes playing a role in depression: case/control differences in epigenetic modifications
DNAm in peripheral tissue
A number of studies have focused on whether there are differences in epigenetic modifications in various tissues of individuals with MDD versus controls. This has largely been centered on differences in the levels of DNAm, a process in which methyl groups are added to the 5′ position of cytosines in cytosine-phosphate-guanine dinucleotides (CpGs), which is generally associated with transcriptional repression. 12 The majority of studies on DNAm in MDD have been performed in peripheral tissues. A recent systematic review of 67 publications, 13 61 of which were done in peripheral tissue, mainly blood cells, concluded there was evidence for DNAm differences between cases and controls at selected loci. Most consistently, candidate gene studies found that patients with MDD had hypermethylation in the loci encoding brain derived neurotrophic factor ( BDNF ), and SLC6A4 , the serotonin transporter gene. However, even these findings are not consistent across all studies, highlighting the importance of sufficient cohort sizes, longitudinal study design, and robust experimental and statistical workflows. 13 Genome-wide methylation approaches were also included, and although all studies found that DNAm was significantly associated with MDD at some loci, no consistent changes, either for direction or position, have been identified. 13 Overall, there is very limited evidence for altered DNAm in peripheral blood in patients with MDD.
Figure 1. Examples of aberrant epigenetic modifications observed in patients with depression compared with healthy controls in brain and peripheral tissue.72.
DNAm in brain tissue
Since DNAm is cell-type specific, 12 and MDD is a neuropsychiatric disorder, aberrant DNAm patterns in brain tissue may provide more valuable insight into the molecular pathology of the disease than peripheral tissues. Studies performed in brain tissue, even when limited to smaller sample sizes, reveal some case/control differences. A recent methylome-wide association study in blood of MDD patients vs controls (n=1132) and in post-mortem brain (n=61) of patients who died by suicide vs psychiatrically healthy controls, found a number of significant MDD-associated regions in both brain and blood tissue. 14 Interestingly, there was a significant overlap between the top MDD-associated differentially methylated regions (DMRs) in the blood with the top MDD-associated DMRs in Brodmann area (BA) 10 ( P =5.4×10 −3 ). BDNF , one of the most robust findings from studies in peripheral tissue, was significantly associated with MDD in both blood and BA10. However, there was no significant overlap between the top DMRs in blood and those in another cortical region (BA25). In fact, only three loci overlapped in blood, BA10, and BA25. These three loci were replicated in an independent cohort, suggesting that despite the cell-specificity of DNAm, some DMRs have cross-tissue relevance. One of these three loci ( GABBR2 ) encodes the metabotropic GABA B receptor subunit, important for inhibitory neural activity, while the other two were located in RUFY3 , encoding a protein involved in establishing neuronal polarity 15 and axon growth. 16 Both genes are important in normal brain development and function.
More studies have investigated MDD associated DNAm than the examples highlighted above, and they provide some evidence that case/control differences in DNAm exist in peripheral and brain tissues. However, the factors driving these differences in epigenetic modifications have not yet been explored. Likely, a combination of both genetic and environmental factors contributes to these epigenetic changes in patients with MDD. These potential mechanisms will be explored in depth later in this review.
Histone modifications
Histone modifications have also been studied in MDD, albeit to a lesser degree than DNAm. Though various modifications of histones are possible, most studies have focused on histone acetylation and methylation. Histone acetylation is generally associated with transcriptional activation as it leads to chromatin decondensation, thus allowing transcriptional machinery access. The process is controlled by histone acetyltransferases (HATs) and histone deacetyltransferases (HDACs), enzymes responsible for adding and removing acetyl groups from histone tails, respectively. Like with DNAm, case/control differences in depression have been observed. Global acetylation of the histone 3 at lysine 14 (H3K14ac), a modification shown to be dynamically regulated by social defeat in rodent models in various brain regions, 17 , 18 was increased in the nucleus accumbens (NAc) taken from postmortem tissue of patients with MDD vs psychiatrically healthy controls. 19 Accordingly, a downregulation of HDAC2 was observed in these patients. 19 Another study of histone modifications in postmortem prefrontal cortex (PFC) of MDD patients reported enrichment of trimethylated H3K4—a modification generally associated with transcriptional activity—at the SYN1 promoter. 20 SYN1 is a member of the synapsin vesicle family of neuronal phosphoproteins and plays a role in neurotransmitter release and synaptic plasticity. 21 Aberrant H3K4me3 or H3K27me3—a repressive histone mark—has also been described in the promoter regions of OAZ1 , TRKB , and BDNF in patients treated with antidepressants, in postmortem PFC. 22 , 23 , 24
In peripheral tissue, a limited number of studies have measured the expression of HDACs in peripheral blood cells from individuals with MDD compared with healthy controls. 25 , 26 One study found elevated HDAC2 and HDAC5 levels in patients experiencing an acute depressive episode. Interestingly, upon remission, the levels normalized to those of healthy controls, highlighting the potential of HDAC levels to be used as a biomarker for disease monitoring. 25 Overall, very few studies have described case/control differences in histone acetylation and methylation, and they have not been performed on a genome-wide scale. Whether and how histone modifications are altered in depression thus remains to be seen.
MicroRNAs
Although miRNAs were discovered in the late 20th century, 27 it has only been in recent years that they have been implicated in psychiatric disease. miRNAs are a type of short (typically 22 nt) noncoding RNA molecule that post-transcriptionally regulate gene expression for example via binding to mRNAs, causing their degradation and thus, translational repression. Not only do miRNAs play an important role in development and cellular differentiation by acting as a switch to silence appropriate gene groups, they also have a more nuanced role in dampening gene expression by decreasing, but not obliterating, mRNA transcripts of specific targets. 28 Therefore, miRNAs may have a role in disease, via dysregulation of genes involved in specific disease relevant processes. Indeed, studies show altered levels of specific miRNAs in patients with psychiatric disorders, including MDD. In a recent review of 23 studies assessing miRNAs in peripheral tissues of patients with MDD, 178 different miRNAs were altered in cases versus controls. 29 However, with the exception of miRNA-132 which was replicated in four independent studies, these miRNAs were not consistently altered across studies, highlighting the need for more robust studies with larger sample sizes, consistent methodologies, and more stringent diagnostic criteria. 29
There have also been studies focused on miRNAs in human brain tissue of patients with MDD. For example, miR-1202, a miRNA regulating a glutamate receptor ( GRM4 ) was found to be downregulated in PFC of MDD patients who died by suicide compared with psychiatrically healthy controls. This was further replicated in two independent cohorts. Correspondingly, mRNA levels of GRM4 increased in both cohorts. Additionally, upon antidepressant treatment, peripheral levels of miR-1202 increased after 8 weeks of treatment, 30 an example of how findings in human brain tissue could be applied for clinical use. Other studies of postmortem brain and peripheral tissues have identified altered levels of miRNAs in patients with MDD and after treatment with antidepressant medication (see ref 31 for a review). This highlights miRNAs’ potential as biomarkers for treatment response; however, further studies are needed.
Challenges and solutions for overcoming cell-type specificity in epigenetic research in depression
The above briefly described some of the evidence for altered epigenetic modifications in MDD both in brain and peripheral tissue. It is worth noting that in addition to the epigenetic modifications mentioned in this review, other epigenetic modifications have been observed in patients with MDD, such as RNA methylation; however, these are much less studied. 32 Modifications in peripheral tissue have clinical potential to be used as biomarkers for diagnosis, treatment selection, and treatment monitoring. Although marks found in brain tissue are not suitable for biomarkers, they provide valuable insight into the pathological mechanisms, which is needed to develop a mechanistic understanding of disease and novel treatments. The cross-tissue relevance of findings in one tissue to another remains unclear and is most likely modification- and region-specific. Indeed, a recent study performed genome-wide methylation assays on blood, brain, saliva, and buccal samples and found that cross-tissue correlation strength was highly region-specific, with the correlation coefficient varying widely for different CpGs. Overall, the saliva-brain correlations (r=0.9) were higher than blood-brain and buccal-brain correlations, suggesting some peripheral tissues may be more useful than others. However, at the individual CpG level, correlations for all peripheral tissues were only nominally significantly correlated with brain tissue. 33
Given the cell-type specificity of epigenetic marks, even studies done using specific regions from postmortem brain are limited by the fact that tissue homogenates were used; these contain both neuronal and non-neuronal cell-types. Recent developments in single-cell technologies are circumventing this issue and allowing epigenetic modifications to be assessed on a single-cell level. 34 However, to date, single-cell work in postmortem brain for MDD research is limited, and what exists is mainly limited to single-cell transcriptomics. A study published in 2018 analyzed single nuclei from the PFC of MDD patients and psychiatrically healthy controls. Twenty-six unique cellular clusters were identified, with the majority of the clusters showing case/control differences at the transcriptome level. 35 Whether epigenetic modifications were involved in driving these transcriptional changes within the cellular clusters was not examined, but may be an indication of possible epigenetic modifications specific to certain cell types.
An alternative method to assess cell-type specific modifications relies on flow cytometry to sort cells into subtypes by using established cell-type specific markers, to which downstream epigenetic analyses are applied. Though not depression-specific, a recent study 36 assessed various epigenetic modifications in postmortem brain sorted into excitatory glutamatergic neurons, medial ganglionic eminence-derived y-aminobutryric acid (GABA)-ergic inhibitory neurons, and oligodendrocytes. Downstream epigenetic analyses on specific cell types revealed patterns of epigenetic modifications exclusive to certain brain cell types. Most notably, there was an association between hydroxymethylation, an intermediate state in the reaction responsible for DNAm, and gene expression in the inhibitory neurons, but not in the other subtypes. The activity of these inhibitory neurons has previously been implicated in psychiatric disorders, 37 providing an example of how studying a specific cell population may reveal unique disease relevant mechanisms that may have otherwise not been identified. Further cell-type specific studies may reveal other cell-type specific mechanisms and identify more robust epigenetic mechanisms involved in depression.
The abovementioned studies in single-cell transcriptomics and cell-specific epigenetic modifications have provided valuable insight into new cell populations that may be relevant in the molecular pathology of MDD, but more depression-focused studies on cell-type specific epigenetic modifications are required.
Drivers of aberrant epigenetic processes— genetic mechanisms
As described above, some evidence for case/control differences in epigenetic marks exist. However, the modifications themselves are only end-point observations, and most studies provide little insight into the factors driving these differences. Given the strong genetic component of MDD, genetically driven epigenetic mechanisms are a suitable starting point for further mechanistic studies. Drawing on research from neurodevelopmental disorders provides insight into how genetic factors can cause aberrant epigenetic processes. For example, there are monogenetic brain disorders in which the phenotype is driven by mutations in genes encoding epigenetic modifiers, such as Rett Syndrome (see ref 38 for review). Even though depression is clearly not a monogenetic disorder, variants in genes coding for epigenetic modifiers may still drive the epigenetic changes observed in patients with MDD. Indeed, one of the first single-nucleotide polymorphisms (SNPs; rs12413112) identified genome-wide to be associated with MDD is located next to SIRT1 , 39 which encodes a type III HDAC, an epigenetic modifier. A second SNP (rs10997875) in SIRT1 was found to be associated with MDD in a Japanese population. 40 SIRT1 deacetylates histones and non-histone proteins involved in chromatin processes to modulate gene expression. 41 It has been shown to modulate mood-related behaviors in rodent models, 42 and to be necessary for normal neuronal excitability and synaptic functions. 43
A handful of studies have also identified depression risk variants in precursor miRNA encoding genes, 44 , 45 variants located in or near miRNA target genes 46 , 47 or variants located in genes involved in miRNA processing. 48 In a study of both European-Americans and African- Americans, a variant (rs41305272), located in a predicted target site of the microRNA miR-330-3p in MAP2K5 , was associated with MDD in the African-American population (OR=2.64, P =0.01; 427 cases), but not in the European- American population. 47
Another line of research on how genetic variants influence epigenetic modifications are methylation quantitative trait loci (mQTL) studies. An mQTL is a genetic variant that explains, or partly explains, variation of DNAm at a locus. A GWAS meta-analysis of MDD published in 2018 identified 44 depression-associated loci and integrated genetic and mQTL data from two large studies to identify nine risk variants controlling local DNAm in blood. 49 This overlap indicates that a subset of the risk variants for MDD could be responsible for the DMRs observed in patients with MDD. Interestingly, some of the nine mQTLs are located near genes encoding miRNAs; however, the function of these variants and DMRs must still be assessed.
Collectively, these studies indicate that the epigenetic differences observed in patients with MDD may have genetic correlates driving the aberrant epigenetic processes. However, these studies have not been followed up by directly measuring the epigenetic modifications themselves. Rather, they have identified genetic variants located in genes that encode epigenetic modifiers. As the power of GWAS continues to increase and more MDD risk variants are identified, more variants in genes encoding for epigenetic modifiers are likely to be discovered. To directly assess whether the genetic variants are driving the aberrant epigenetic modifications observed in case control studies of MDD, functional assays are required.
Drivers of aberrant epigenetic processes— environmental mechanisms
Since environmental factors mediate the risk for MDD, it is plausible that they too can drive the epigenetic differences observed in patients with MDD compared with healthy controls. Indeed, environmental factors have been shown to modulate epigenetic processes. Since stress and exposure to adverse life events are one of the most robust environmental risk factors for MDD, we will focus on them in this review. Studies from animal models demonstrate that stress, usually psychological stress via chronic social defeat paradigms, can induce changes in epigenetic marks. In a high-resolution genome-wide methylation study, O’Toole et al 50 identified striking changes in methylation patterns in the NAc of mice subjected to chronic social defeat stress compared with non-stressed controls. Hypermethylation at CpG sites was more prevalent than hypomethylation in the stressed versus control mice. Genes (such as Est1 , Cacna1c , and Dcc ) associated with stress sensitivity and psychiatric disorders, including MDD in humans, 51 were significantly differentially methylated. Network analysis of the DMRs showed involvement of β-catenin-related WNT/frizzled signalling, a pathway involved in neuroplasticity. 52 β-catenin, one of the hub genes identified in the network, has previously been shown to modulate social stress. NAc-selective β-catenin knockout mice showed increased vulnerability to chronic stress, whereas an overexpression in the NAc increased stress resilience. 53 Although transcriptomics were not performed in this particular study, other findings have identified widespread transcriptional changes in the NAc of chronically stressed mice. 54 Collectively, this suggests that aberrant DNAm, specifically in the NAc of chronically stressed mice, may be a mechanism driving these transcriptional changes.
In human models, there is also evidence of environmental factors inducing epigenetic changes. 55 In a model of stress using a human hippocampal progenitor cell line (HPCs), exposure to glucocorticoids (GCs) during differentiation and proliferation induced long-lasting DNAm changes. Subsequent post-differentiation exposure to GCs resulted in robust transcriptional changes in the HPCs that were initially treated during proliferation and differentiation, indicating that GC induced DNAm changes are long-lasting and prime the stress response for future exposure. Furthermore, the DMRs were enriched for the binding motif of the glucocorticoid receptor (GR), a key modulator of the hypothalamus-pituitary-adrenal (HPA) axis. The DMRs with GR binding motifs were more commonly demethylated than hypermethylated. Given that there is evidence that GRs can induce demethylation at glucocorticoid response elements (GREs), 56 the authors postulate that the molecular mechanisms underlying the observed methylation changes in this study are GR- mediated. Further evidence of GR-mediated methylation changes will be discussed later in the review.
The effect of stress and exposure to adverse life events has also been well studied in human populations. Studies of adults with a history of child abuse, which is a strong risk factor for depression, have investigated whether childhood adversity is associated with aberrant DNAm patterns in brain and peripheral tissues. A genome-wide study of hippocampal tissue from 41 adult males found 362 differentially methylated gene promoter regions in individuals (n=25) who had experienced child abuse and completed suicide, compared with the psychiatrically healthy controls (n=16). These DMRs were most pronounced in the neuronal fraction of the brain tissue, and consistent with the findings in animal studies mentioned above, were enriched in genes involved in neuroplasticity. 57 Other studies have also observed associations between childhood maltreatment and differences in DNAm in the brain, 58 blood, 59 , 60 and even gametes. 61 However, well-powered studies have also reported negative results. 62
As with the case/control studies described previously, to date most work investigating how stress and exposure to adverse life events induce epigenetic modifications has focused on methylation. Nonetheless, a few studies have shown environmentally driven changes of the epigenetic landscape in other ways, such as via histone modifications and long noncoding RNAs. This has almost exclusively been done in animal models, 63 , 64 , 65 , 66 with a few exceptions of studies in human cohorts. 67 Overall, DNAm remains the most characterized epigenetic process that changes in response to exposure to adverse life events.
Gene x environment mechanisms in depression
Both genetic and environmental factors can drive epigenetic processes. However, these factors are not independent, and they have been shown to interact. Gene by environment (GxE) interactions refer to the influence of environmental and genetic factors on a measured phenotype, in this case, epigenetic modifications. However, in GxE interactions, the magnitude of the environmental influence on the phenotype depends on the genotype of the individual. For example, in a recent study of over 2000 newborns, the influence of the prenatal environment on genome-wide DNAm was examined. The prenatal environment (E), genotypes in cis (G), their additive (G+E) or interaction (GxE) effects on DNAm at DMRs in neonatal blood were assessed. The GxE and G+E models outperformed the models with G or E only in predicting DNAm at the DMRs, indicating a synergistic interaction between genetic and environmental factors. Notably, both models (G+E and GxE) were enriched for DMRs associated with GWAS of psychiatric disease, including MDD. 68
In another mechanistic study of GxE interactions driving epigenetic modifications, Klengel et al 69 identified an interaction between a variant (rs1360780) located in an enhancer region in FK506 binding protein 5 gene ( FKBP5 ) and childhood trauma on DNA methylation of FKBP5 in peripheral blood cells. FKBP5 is an important regulator of the HPA axis and is involved in a negative feedback loop to terminate the stress response. The authors found that methylation of FKBP5 was associated with childhood trauma in carriers of the risk allele, but not those with childhood trauma with the major allele, an example of gene x childhood trauma interaction. Importantly, this study identified not only an interaction, but also the mechanism by which it induces changes to DNAm. Using a series of experiments, the authors propose the following model: the risk allele of rs1360780 causes differential interactions between the enhancer and transcription start site upon GR activation induced via child abuse, resulting in transcriptional activation of FKBP5 . Persistent overexpression of FKBP5 results in impaired termination of the stress response, including prolonged GR activation. The genotype dependent changes in chromatin structure, along with prolonged GR activity, cause DNA demethylation at CpGs located within and proximal of GREs that have been shown to increase FKBP5 mRNA levels. Highly dynamic GR-dependent changes in DNAm of CpGs in FKBP5 after acute GR activation have been shown to occur in adult peripheral blood cells, with de- and remethylation occurring within a period of 24 hours following GR activation. 56 However, as shown in a human hippocampal progenitor cell line, GR-induced demethylation can become stable when initiated during certain early developmental periods. 55 Such lasting changes in DNAm result in an altered set-point for transcriptional changes of FKBP5 upon subsequent GR activation. 55 , 69 , 72 The exact mechanisms contributing to such stable changes have not been investigated so far, but likely involve developmental stage-specific functions of DNA methyltransferase, enzymes involved in active DNA de-methylation such as the ten-eleven translocation protein family as well as methyl-CpG binding proteins. Differences in the levels and dynamics of these proteins will have an impact on DNAm levels.
In summary, in the FKBP5 model, the genotype, via differential chromatin interactions, and environmental risk, via enhanced GR activation, converge to establish the long-term transcriptional changes of FKBP5 by lasting changes in DNAm of enhancer regions. Further studies have associated this interaction between rs1360780 and childhood abuse with psychiatric conditions later in life, including MDD, 70 , 71 highlighting its clinical relevance.
Future directions
The risk for MDD is both genetically and environmentally determined. There is evidence from case/control studies that implicate epigenetic processes in MDD, and these epigenetic processes are likely driven by both genetic and environmental factors. Collectively, a model emerges where underlying genetic and environmental factors, and interactions between the two, drive aberrant epigenetic mechanisms targeting stress response pathways, neuronal plasticity, and other behaviorally relevant pathways that have been implicated in MDD.
Yet, many gaps remain in our understanding of epigenetic processes in MDD. Most studies describing epigenetic modifications in patients with MDD have focused on DNAm, with fewer studies focused on histone modifications and long noncoding RNAs. Most studies have been done using peripheral tissue, and those that have used postmortem brain tissue are generally limited to smaller cohort sizes and brain tissue homogenates. These factors have contributed to the difficulty in validating depression-associated epigenetic modifications across cohorts. Other factors currently inherent to psychiatric research, such as the polygenic architecture of depression, symptom-based diagnoses, and retrospective recall of environmental exposures, have only added to the difficulty. However, recent advances have been made, such as consortium-based cohorts for GWAS, decreasing costs of next-generation sequencing technologies, and developments in single-cell methods. These developments, among others, can help to identify robust aberrant epigenetic mechanisms occurring in MDD, to increase our understanding of the molecular mechanisms governing this disease, and to guide future treatment.
Acknowledgments
The authors declare no conflict of interest
Contributor Information
Signe Penner-Goeke, Dept of Translational Research in Psychiatry, Max Planck Institute of Psychiatry, Munich, Germany..
Elisabeth B. Binder, Dept of Translational Research in Psychiatry, Max Planck Institute of Psychiatry, Munich, Germany..
REFERENCES
- 1.Friedrich MJ. Depression is the leading cause of disability around the world. JAMA. 2017;317(15):1517. doi: 10.1001/jama.2017.3826. [DOI] [PubMed] [Google Scholar]
- 2.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):2011–2030. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sullivan PF, Neale MC, Kendler KS. Genetic epidemiology of major depression: Review and meta-analysis. Am J Psychiatry. 2000;157(10):1552–1562. doi: 10.1176/appi.ajp.157.10.1552. [DOI] [PubMed] [Google Scholar]
- 4.Kendler KS, Gatz M, Gardner CO, Pedersen NL. A Swedish national twin study of lifetime major depression. Am J Psychiatry. 2006;163(1):109–114. doi: 10.1176/appi.ajp.163.1.109. [DOI] [PubMed] [Google Scholar]
- 5.Howard DM, Adams MJ, Clarke TK, et al Genome-wide meta-analysis of depression identifies 102 independent variants and highlights the importance of the prefrontal brain regions. Nat Neurosci. 2019;22(3):343–352. doi: 10.1038/s41593-018-0326-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sullivan PF, Kendler KS, Neale MC. Schizophrenia as a complex trait: Evidence from a Meta-analysis of twin studies. Arch Gen Psychiatry. 2003;60(12):1187–1192. doi: 10.1001/archpsyc.60.12.1187. [DOI] [PubMed] [Google Scholar]
- 7.McGuffin P, Rijsdijk F, Andrew M, Sham P, Katz R, Cardno A. The heritability of bipolar affective disorder and the genetic relationship to unipolar depression. Arch Gen Psychiatry. 2003;60(5):497–502. doi: 10.1001/archpsyc.60.5.497. [DOI] [PubMed] [Google Scholar]
- 8.Chang Z, Lichtenstein P, Asherson PJ, Larsson H. Developmental twin study of attention problems: High heritabilities throughout development. JAMA Psychiatry. 2013;70(3):311–318. doi: 10.1001/jamapsychiatry.2013.287. [DOI] [PubMed] [Google Scholar]
- 9.Kendler KS, Karkowski LM, Prescott CA. Causal relationship between stressful life events and the onset of major depression. Am J Psychiatry. 1999;156(6):837–841. doi: 10.1176/ajp.156.6.837. [DOI] [PubMed] [Google Scholar]
- 10.Mandelli L, Petrelli C, Serretti A. The role of specific early trauma in adult depression: A meta-analysis of published literature. Childhood trauma and adult depression. Eur Psychiatry. 2015;30(6):665–680. doi: 10.1016/j.eurpsy.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 11.Klengel T, Binder EB. Epigenetics of stress-related psychiatric disorders and gene x environment interactions. Neuron. 2015;86(6):1343–1357. doi: 10.1016/j.neuron.2015.05.036. [DOI] [PubMed] [Google Scholar]
- 12.Khavari DA, Sen GL, Rinn JL. DNA methylation and epigenetic control of cellular differentiation. Cell Cycle. 2010;9(19):3880–3883. doi: 10.4161/cc.9.19.13385. [DOI] [PubMed] [Google Scholar]
- 13.Li M, D’Arcy C, Li X, Zhang T, Joober R, Meng X. What do DNA methylation studies tell us about depression? A systematic review. Transl Psychiatry. 2019;9(1):e68. doi: 10.1038/s41398-019-0412-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aberg KA, Dean B, Shabalin AA, et al Methylome-wide association findings for major depressive disorder overlap in blood and brain and replicate in independent brain samples. Mol Psychiatry. doi: 10.1038/s41380-018-0247-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Honda A, Ito Y, Takahashi-Niki K, et al Extracellular signals induce glycoprotein M6a clustering of lipid rafts and associated signaling molecules. J Neurosci. 2017;37(15):4046–4064. doi: 10.1523/JNEUROSCI.3319-16.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wei Z, Sun M, Liu X, Zhang J, Jin Y. Rufy3, a protein specifically expressed in neurons, interacts with actin-bundling protein Fascin to control the growth of axons. J Neurochem. 2014;130(5):678–692. doi: 10.1111/jnc.12740. [DOI] [PubMed] [Google Scholar]
- 17.Covington HE, Maze I, Vialou V, Nestler EJ. Antidepressant action of HDAC inhibition in the prefrontal cortex. Neuroscience. 2015;298:329–335. doi: 10.1016/j.neuroscience.2015.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Covington HE , Vialou VF, LaPlant Q, Ohnishi YN, Nestler EJ. Hippocampal-dependent antidepressant-like activity of histone deacetylase inhibition. Neurosci Lett. 2011;493(3):122–126. doi: 10.1016/j.neulet.2011.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Covington HE, Maze I, Laplant QC, et al Antidepressant Actions of HDAC Inhibitors. J Neurosci. 2009;29(37):11451–11460. doi: 10.1523/JNEUROSCI.1758-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cruceanu C, Nagy C, Freemantle E, Turecki G, Alda M, Rouleau GA. H3K4 tri-methylation in synapsin genes leads to different expression patterns in bipolar disorder and major depression. Int J Neuropsychopharmacol. 2013;16(2):289–299. doi: 10.1017/S1461145712000363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baldelli P, Fassio A, Valtorta F, Benfenati F. Lack of synapsin i reduces the readily releasable pool of synaptic vesicles at central inhibitory synapses. J Neurosci. 2007;27(49):13520–13531. doi: 10.1523/JNEUROSCI.3151-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fiori LM, Gross JA, Turecki G. Effects of histone modifications on increased expression of polyamine biosynthetic genes in suicide. Int J Neuropsychopharmacol. 2012;15(8):1161–1166. doi: 10.1017/S1461145711001520. [DOI] [PubMed] [Google Scholar]
- 23.Chen ES, Ernst C, Turecki G. The epigenetic effects of antidepressant treatment on human prefrontal cortex BDNF expression. Int J Neuropsychopharmacol. 2011;14(3):427–429. doi: 10.1017/S1461145710001422. [DOI] [PubMed] [Google Scholar]
- 24.Ernst C, Chen ES, Turecki G. Histone methylation and decreased expression of TrkB.T1 in orbital frontal cortex of suicide completers. Mol Psychiatry. 2009;14(9):830–832. doi: 10.1038/mp.2009.35. [DOI] [PubMed] [Google Scholar]
- 25.Hobara T, Uchida S, Otsuki K, et al Altered gene expression of histone deacetylases in mood disorder patients. J Psychiatr Res. 2010;44(5):263–270. doi: 10.1016/j.jpsychires.2009.08.015. [DOI] [PubMed] [Google Scholar]
- 26.Iga J, Ueno S, Yamauchi K, et al Altered HDAC5 and CREB mRNA expressions in the peripheral leukocytes of major depression. Prog Neuro-Psychopharmacology Biol Psychiatry. 2007;31(3):628–632. doi: 10.1016/j.pnpbp.2006.12.014. [DOI] [PubMed] [Google Scholar]
- 27.Lee RC, Feinbaum RL, Ambros V. The C. elegans heterochronic gene lin-4 encodes small RNAs with antisense complementarity to lin-14. Cell. 1993;75(5):843–854. doi: 10.1016/0092-8674(93)90529-y. [DOI] [PubMed] [Google Scholar]
- 28.Bartel DP. MicroRNAs: target recognition and regulatory functions. Cell. 2009;136(2):215–233. doi: 10.1016/j.cell.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yuan H, Mischoulon D, Fava M, Otto MW. Circulating microRNAs as biomarkers for depression: Many candidates, few finalists. J Affect Disord. 2018;233:68–78. doi: 10.1016/j.jad.2017.06.058. [DOI] [PubMed] [Google Scholar]
- 30.Lopez JP, Lim R, Cruceanu C, et al MiR-1202 is a primate-specific and brain-enriched microRNA involved in major depression and antidepressant treatment. Nat Med. 2014;20(7):764–768. doi: 10.1038/nm.3582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lopez JP, Kos A, Turecki G. Major depression and its treatment: MicroRNAs as peripheral biomarkers of diagnosis and treatment response. Curr Opin Psychiatry. 2018;31(1):7–16. doi: 10.1097/YCO.0000000000000379. [DOI] [PubMed] [Google Scholar]
- 32.Engel M, Eggert C, Kaplick PM, et al The Role of m(6)A/m-RNA Methylation in Stress Response Regulation. Neuron. 2018;99(2):389–403. doi: 10.1016/j.neuron.2018.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Braun PR, Han S, Hing B, et al Genome-wide DNA methylation comparison between live human brain and peripheral tissues within individuals. Transl Psychiatry. 2019;9(1):47. doi: 10.1038/s41398-019-0376-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Clark SJ, Lee HJ, Smallwood SA, Kelsey G, Reik W. Single-cell epigenomics: Powerful new methods for understanding gene regulation and cell identity. Genome Biol. 2016;17(1):72. doi: 10.1186/s13059-016-0944-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nagy C, Maitra M, Suderman M, et al Single-nucleus RNA sequencing shows convergent evidence from different cell types for altered synaptic plasticity in major depressive disorder. bioRxiv. 2019 doi: 10.1101/384479. [DOI] [Google Scholar]
- 36.Kozlenkov A, Li J, Apontes P, et al A unique role for DNA (hydroxy)methylation in epigenetic regulation of human inhibitory neurons. Sci Adv. 2018;4(9) doi: 10.1126/sciadv.aau6190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Le Magueresse C, Monyer H. GABAergic interneurons shape the functional maturation of the cortex. Neuron. 2013;77(3):388–405. doi: 10.1016/j.neuron.2013.01.011. [DOI] [PubMed] [Google Scholar]
- 38.Jakovcevski M, Akbarian S. Epigenetic mechanisms in neurological disease. Nat Med. 2012;18:1194–1204. doi: 10.1038/nm.2828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ledford H. First robust genetic links to depression emerge. Nature. 2015;523(7560):268–269. doi: 10.1038/523268a. [DOI] [PubMed] [Google Scholar]
- 40.Kishi T, Yoshimura R, Kitajima T, et al SIRT1 gene is associated with major depressive disorder in the Japanese population. J Affect Disord. 2010;126(1-2):167–173. doi: 10.1016/j.jad.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 41.Bosch-Presegué L, Vaquero A. Sirtuin-dependent epigenetic regulation in the maintenance of genome integrity. FEBS J. 2015;282(9):1745–1767. doi: 10.1111/febs.13053. [DOI] [PubMed] [Google Scholar]
- 42.Kim HD, Hesterman J, Call T, et al SIRT1 mediates depression-like behaviors in the nucleus accumbens. J Neurosci. 2016;36(32):8441–8452. doi: 10.1523/JNEUROSCI.0212-16.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lei Y, Wang J, Wang D, et al SIRT1 in forebrain excitatory neurons produces sexually dimorphic effects on depression-related behaviors and modulates neuronal excitability and synaptic transmission in the medial prefrontal cortex. Mol Psychiatry. 2019 doi: 10.1038/s41380-019-0352-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Saus E, Soria V, Escaramís G, et al Genetic variants and abnormal processing of pre-miR-182, a circadian clock modulator, in major depression patients with late insomnia. Hum Mol Genet. 2010;19(20):4017–4025. doi: 10.1093/hmg/ddq316. [DOI] [PubMed] [Google Scholar]
- 45.Xu Y, Liu H, Li F, et al A polymorphism in the microRNA-30e precursor associated with major depressive disorder risk and P300 waveform. J Affect Disord. 2010;127(1-3):332–336. doi: 10.1016/j.jad.2010.05.019. [DOI] [PubMed] [Google Scholar]
- 46.Rahman OA, Sasvari-Szekely M, Szekely A, Faludi G, Guttman A, Nemoda Z. Analysis of a polymorphic microRNA target site in the purinergic receptor P2RX7 gene. Electrophoresis. 2010;31(11):1790–1795. doi: 10.1002/elps.200900664. [DOI] [PubMed] [Google Scholar]
- 47.Jensen KP, Kranzler HR, Stein MB, Gelernter J. The effects of a MAP2K5 microRNA target site SNP on risk for anxiety and depressive disorders. Am J Med Genet Part B Neuropsychiatr Genet. 2014;165(2):175–183. doi: 10.1002/ajmg.b.32219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.He Y, Zhou Y, Xi Q, et al Genetic variations in microRNA processing genes are associated with susceptibility in depression. DNA Cell Biol. 2012;31(9):1499–1506. doi: 10.1089/dna.2012.1660. [DOI] [PubMed] [Google Scholar]
- 49.Wray NR, Ripke S, Mattheisen M, et al Genome-wide association analyses identify 44 risk variants and refine the genetic architecture of major depression. Nat Genet. 2018;50(5):668–681. doi: 10.1038/s41588-018-0090-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.O’Toole N, Zhang T-Y, Wen X, et al Epigenetic signatures of chronic social stress in stress-susceptible animals. bioRxiv. 2019 doi: 10.1101/690826. [DOI] [Google Scholar]
- 51.Torres-Berrío A, Lopez JP, Bagot RC, et al DCC confers susceptibility to depression-like behaviors in humans and mice and is regulated by miR-218. Biol Psychiatry. 2017;81(4):306–315. doi: 10.1016/j.biopsych.2016.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.MacDonald B, Tamai K, He X. Wnt/beta-catenin signaling: components, mechanisms, and diseases. Develpmental Cell. 2009;17(1):9–26. doi: 10.1016/j.devcel.2009.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dias C, Feng J, Sun H, et al β-catenin mediates behavioral resilience through Dicer1/ microRNA regulation. Nature. 2014;516(7529):51–55. doi: 10.1038/nature13976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bagot RCC, Cates HMM, Purushothaman I, et al Circuit-wide transcriptional profiling reveals brain region-specific gene networks regulating depression susceptibility. Neuron. 2016;90(5):969–983. doi: 10.1016/j.neuron.2016.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Provençal N, Arloth J, et al Glucocorticoid exposure during hippocampal neurogenesis primes future stress response by inducing changes in DNA methylation. Proc Natl Acad Sci U S A. 2019 doi: 10.1073/pnas.1820842116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wiechmann T, Röh S, Sauer S, et al Identification of dynamic glucocorticoid-induced methylation changes at the FKBP5 locus. Clin Epigenetics. 2019;11(1):83. doi: 10.1186/s13148-019-0682-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Labonté B, Suderman M, Maussion G, et al Genome-wide epigenetic regulation by early-life trauma. Arch Gen Psychiatry. 2012;69(7):722–731. doi: 10.1001/archgenpsychiatry.2011.2287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.McGowan PO, Sasaki A, D’Alessio AC, et al Epigenetic regulation of the glucocorticoid receptor in human brain associates with childhood abuse. Nat Neurosci. 2009;12(3):342–348. doi: 10.1038/nn.2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Suderman M, Borghol N, Pappas JJ, et al Childhood abuse is associated with methylation of multiple loci in adult DNA. BMC Med Genomics. 2014;7(13) doi: 10.1186/1755-8794-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mehta D, Klengel T, Conneely KN, et al Childhood maltreatment is associated with distinct genomic and epigenetic profiles in posttraumatic stress disorder. Proc Natl Acad Sci. 2013;110(20):8302–8307. doi: 10.1073/pnas.1217750110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Roberts AL, Gladish N, Gatev E, et al Exposure to childhood abuse is associated with human sperm DNA methylation. Transl Psychiatry. 2018;8:194. doi: 10.1038/s41398-018-0252-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Marzi SJ, Sugden K, Arseneault L, et al Analysis of DNA methylation in young people: Limited evidence for an association between victimization stress and epigenetic variation in blood. Am J Psychiatry. 2018;175(6):517–529. doi: 10.1176/appi.ajp.2017.17060693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gapp K, Jawaid A, Sarkies P, et al Implication of sperm RNAs in transgenerational inheritance of the effects of early trauma in mice. Nat Neurosci. 2014;17(5):667–669. doi: 10.1038/nn.3695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rodgers AB, Morgan CP, Leu NA, Bale TL. Transgenerational epigenetic programming via sperm microRNA recapitulates effects of paternal stress. Proc Natl Acad Sci U S A. 2015;112(44):13699–13704. doi: 10.1073/pnas.1508347112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Peña CJ, Neugut YD, Champagne FA. Developmental timing of the effects of maternal care on gene expression and epigenetic regulation of hormone receptor levels in female rats. Endocrinology. 2013;154(11):4340–4351. doi: 10.1210/en.2013-1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bagot RC, Zhang T-Y, Wen X, et al Variations in postnatal maternal care and the epigenetic regulation of metabotropic glutamate receptor 1 expression and hippocampal function in the rat. Proc Natl Acad Sci. 2012;109(2):17200–17207. doi: 10.1073/pnas.1204599109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Dickson DA, Paulus JK, Mensah V, et al Reduced levels of miRNAs 449 and 34 in sperm of mice and men exposed to early life stress. Transl Psychiatry. 2018;8:101. doi: 10.1038/s41398-018-0146-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Czamara D, Eraslan G, Page CM, et al Integrated analysis of environmental and genetic influences on cord blood DNA methylation in new-borns. Nat Commun. 2019;10(1):2548. doi: 10.1038/s41467-019-10461-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Klengel T, Mehta D, Anacker C, et al Allele-specific FKBP5 DNA demethylation mediates gene-childhood trauma interactions. Nat Neurosci. 2013;16(1):33–41. doi: 10.1038/nn.3275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Appel K, Schwahn C, Mahler J, et al Moderation of adult depression by a polymorphism in the FKBP5 gene and childhood physical abuse in the general population. Neuropsychopharmacology. 2011;36(10):1982–1991. doi: 10.1038/npp.2011.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zimmermann P, Brückl T, Nocon A, et al Interaction of FKBP5 gene variants and adverse life events in predicting depression onset: Results from a 10 -year prospective community study. Am J Psychiatry. 2011;68(10):1107–1116. doi: 10.1176/appi.ajp.2011.10111577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nagy C, Suderman M, Yang J, et al Astrocytic abnormalities and global DNA methylation patterns in depression and suicide. Mol Psychiatry. 2015;20(3):320–328. doi: 10.1038/mp.2014.21. [DOI] [PMC free article] [PubMed] [Google Scholar]