Abstract
Nuclear factor-κB (NF-κB) is a transcription factor that regulates the expression of various genes involved in inflammation and the immune response. The activation of NF-κB occurs via two pathways: inflammatory cytokines, such as TNF-α and IL-1β, activate the “classical pathway”, and cytokines involved in lymph node formation, such as CD40L, activate the “alternative pathway”. NF-κB1 (p50) and NF-κB2 (p52) double-knockout mice exhibited severe osteopetrosis due to the total lack of osteoclasts, suggesting that NF-κB activation is required for osteoclast differentiation. These results indicate that NF-κB may be a therapeutic target for inflammatory bone diseases, such as rheumatoid arthritis and periodontal disease. On the other hand, mice that express the dominant negative form of IκB kinase (IKK)-β specifically in osteoblasts exhibited increased bone mass, but there was no change in osteoclast numbers. Therefore, inhibition of NF-κB is thought to promote bone formation. Taken together, the inhibition of NF-κB leads to “killing two birds with one stone”: it suppresses bone resorption and promotes bone formation. This review describes the role of NF-κB in physiological bone metabolism, pathologic bone destruction, and bone regeneration.
Keywords: NF-κB, inflammation, osteoclasts, osteoblasts
1. Introduction
As well as supporting and protecting the body, bones support movement in coordination with muscles, host hematopoiesis, and store minerals such as calcium [1,2]. Although bone appears to be a static tissue, it is, in fact, a dynamic tissue that is resorbed and formed constantly and repeatedly. This is called “bone remodeling” [1,2]. Osteoclasts that differentiate from hematopoietic stem cells are responsible for bone resorption, and osteoblasts that differentiate from mesenchymal cells are responsible for bone formation [1,2,3,4,5]. The differentiation and function of these cells are tightly regulated by hormones and local cytokines. In normal bone, the balance between bone resorption and bone formation is maintained, and the bone mass is kept constant; however, in inflammatory bone diseases, such as osteoporosis, rheumatoid arthritis (RA), and periodontitis, bone resorption exceeds bone formation, and then the balance is lost [1,2,3,4,5].
Excessive immune and inflammatory responses enhance bone resorption by osteoclasts and cause bone destruction by impairing osteoblastic bone formation [6]. RA, a typical inflammatory bone disease, is characterized by chronic polysynovitis accompanied with bone destruction by systemic autoimmunity [6]. During the RA activity period, the pannus, which is an abnormal layer of fibrovascular or granulation tissue, infiltrates into the destroyed joint by osteoclasts. At this time, the T-cell immune reaction in the RA synovium causes an excessive biological reaction, and the signal in the synovial cells is continually activated. As a result, synovial cells produce inflammatory cytokines, such as interleukin (IL)-1, IL-6, and tumor necrosis factor (TNF)-α, and matrix-degrading enzymes, such as matrix metalloproteases (MMPs) [7,8].
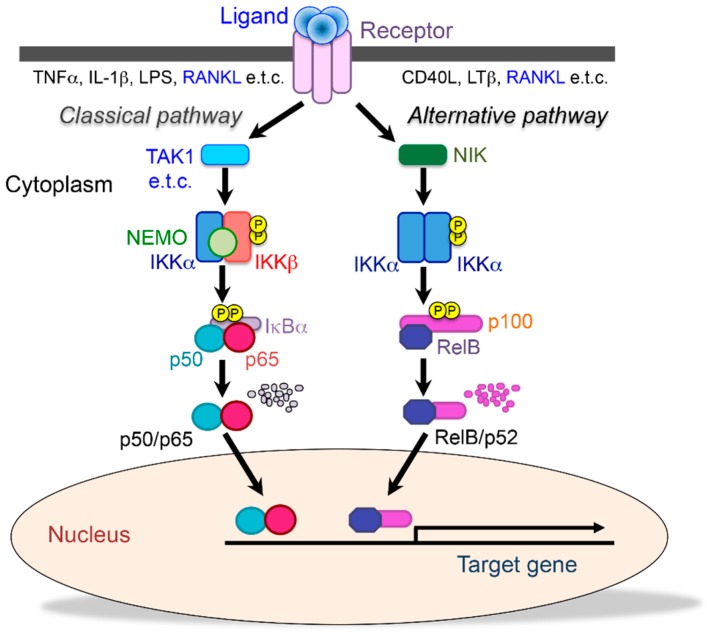
Nuclear factor-κB (NF-κB) is a collective term for five transcription factors: p50/p105, p52/p100, p65 (relA), c-Rel, and RelB, which together form homo- or heterodimers [9,10]. NF-κB binds to the inhibitory molecules IκBs, IκBα, IκBβ, IκBγ, and IκBε, and they remain as a complex sequestered in the cytoplasm. When cells are stimulated by inflammatory cytokines such as TNF-α and IL-1, IκB is phosphorylated by the IκB kinase complex (IKKα, IKKβ, NEMO: NF-κB essential modulator), ubiquitinated, and then degraded by the ubiquitin-proteasome system [9,10,11]. Then, free NF-κB translocates into the nucleus, recognizes specific DNA sequences, and binds to them to regulate the expression of target genes. This is called “the classical NF-κB pathway”. However, there is also an NF-κB activation mechanism that is independent of IκB degradation. In the unstimulated state, p100 remains in the cytoplasm by associating with RelB. When activated, the C-terminal end of p100, which has the same function as IκBs, is degraded, and then a heterodimer of RelB/p52 is formed and translocates into the nucleus. This activation pathway is referred to as “the alternative NF-κB pathway” (Figure 1) [9,10,11]. Since these two pathways play different roles, the p50/p65, p50/c-Rel, and p52/RelB heterodimers are expected to bind to their specific DNA sequences. However, the sequence to which the p52/RelB heterodimer specifically binds and its target genes have not been identified [11,12] (Figure 1).
Figure 1.
Two different NF-κB signaling pathways. The classical (canonical) pathway (left) is activated by a large number of agonists, such as TNF-α, IL-1, lipopolysaccharide, and T cell receptors. The activation of this pathway depends on the IκB kinase (IKK) complex (IKKEMO), which phosphorylates IκBα (Ser32, 36) to induce rapid degradation. This pathway is essential for immune responses, inflammation, tumorigenesis, and cell survival. The alternative (noncanonical) pathway (right) is activated by a limited number of agonists, which are involved in secondary lymphoid organogenesis, mature B cell function, and adaptive immunity. This pathway requires NIK and IKKα, which induce the slow processing of p100 to generate p52, resulting in the dimerization and activation of the p52/RelB heterodimer. Receptor activator of NF-κB ligand (RANKL) activates both classical and alternative pathways.
NF-κB is a transcription factor regulated by genes that control immune and inflammatory responses, but NF-κB1 (p50) and NF-κB2 (p52) double-knockout (dKO) mice exhibited severe osteopetrosis and lacked osteoclasts, suggesting that NF-κB also directly controls osteoclast differentiation [13,14]. Recent findings also showed that NF-κB controls osteoblast differentiation directly or indirectly [15,16]. In this review, we will mainly explain the physiological and pathological roles of NF-κB in bone development and disease, focusing on osteoclasts and osteoblasts.
2. The Role of NF-κB on Bone Metabolism
2.1. The Functions of NF-κB Signaling in Physiological Osteoclastic Bone Resorption
Osteoclasts differentiate from hematopoietic stem cells into osteoclasts via macrophage and monocyte pathways [3,4,5,17]. During differentiation, osteoclast progenitor cells proliferate and differentiate into mono- and binucleated osteoclasts that fuse to become multinucleated osteoclasts. Multinucleated osteoclasts recognize the bone matrix, form a sealing zone to separate the resorption surface from the outside, form a ruffled border, and secrete acid and proteolytic enzymes into the resorption lacunae [3,4,5,17].
Osteoclast differentiation is controlled by two cytokines: macrophage colony-stimulating factor (M-CSF) and receptor activator of NF-κB ligand (RANKL). M-CSF is essential for differentiation into osteoclast progenitors, and it induces the expression of the RANKL receptor RANK. Transcription factors PU.1 and MITF induce the expression of M-CSF receptor (c-fms), and individuals lacking these transcription factors have impaired osteoclast differentiation and present with marble bone disease. In addition, op/op mice and c-fms-deficient mice that cannot produce functional M-CSF exhibit marble bone disease and lack osteoclasts [3,4,5,17].
RANKL is produced by various cells, such as osteoblasts, osteocytes, T cells and B cells [3,4,5,17]. Mice that lack RANKL and its receptor RANK have severe osteopetrosis caused by a total lack of osteoclasts [18,19]. On the other hand, the number of osteoclasts increases in mice that lack the RANKL decoy receptor, osteoprotegerin (OPG), resulting in osteoporosis [20,21]. In human hereditary bone disease, mutations in RANKL, RANK, and OPG have been found, and these three molecules have been shown to be important for osteoclast formation, which maintains bone mass [22].
RANK belongs to the TNF receptor family, and various adapter molecules can interact with the intracellular domain of RANK [23]. Among TNF receptor-activating factor (TRAF) members, TRAF6-deficient mice exhibit an osteopetrosis phenotype that is similar to RANKL- or RANK-deficient mice [24]. Of the downstream molecules of TRAF6, c-Fos and c-Jun regulate the transcription factor AP-1. c-Fos-deficient mice also exhibited osteopetrosis [25]. Another downstream molecule, the transcription factor NF-κB, is composed of five family members. In mice with both NF-κB1 and NF-κB2 knocked out, there is also osteopetrosis due to the total lack of osteoclasts, but deletion of either NF-κB1 or NF-κB2 alone causes no detectable bone phenotype [13,14]. The molecular mechanism by which osteoclasts cannot form in NF-κB1 and NF-κB2 dKO mice is still unknown, but it is certain that NF-κB signaling is important for osteoclast formation.
Among the molecules involved in the signal transduction of NF-κB, p65 (RelA), IKKβ and NEMO could not be analyzed regarding a bone phenotype because these molecules are embryonic lethal [26,27,28,29,30,31]. Thus, to make IKKβ specifically deficient (IKKβcKO) in myeloid cells, IKKβflox/flox mice were crossed with Mx1 or CD11b-Cre transgenic mice to generate conditional knockout mice in which IKKβ is specifically deficient (IKKβcKO) in myeloid cells [32,33]. IKKβcKO mice showed an increase in the trabecular bone volume due to a decrease in the number of osteoclasts. Furthermore, the number of osteoclast precursor cells (F4/80 positive cells) was also significantly reduced. When IKKβcKO mice were crossed with tumor necrosis factor receptor 1(TNFR1)–/– mice to generate IKKβcKO/TNFR1KO dKO mice, osteoclast precursor cells were resistant to apoptosis; further, IκBα was not degraded by RANKL stimulation, and osteoclast differentiation was still suppressed. By contrast, in IKKα knock-in (IKKαA/A) mice in which the serine residue necessary for IKKα kinase activity was substituted with alanine, osteoclast formation by RANKL stimulation was suppressed in vitro but not in vivo. The trabecular bone volume in IKKαA/A mice was comparable to that of wild-type (WT) mice [30]. Furthermore, IKKβ-deficient osteoclasts resulted in RANKL-induced apoptosis by the activation of c-Jun N-terminal kinase (JNK), and the addition of JNK inhibitor restored RANKL-induced apoptosis derived from IKKβcKO mice in vitro [33]. Thus, IKKβ, but not IKKα, is important as a RANK downstream signal in osteoclast differentiation. Consistent with these results, treatment with specific inhibitors of IKKβ activity suppressed RANKL-induced osteoclastogenesis in vitro and in vivo [34,35,36,37].
Since p65-deficient (p65–/–) mice are also embryonic lethal, p65–/– fetal liver cells were studied; the cells were transplanted into irradiated mice to reconstitute bone marrow cells. Fewer osteoclasts were observed in p65–/– chimera mice. When p65–/– chimera mice were crossed with TNFR1–/– mice, p65–/– precursors were found to be sensitive to RANKL-induced apoptosis even on the TNFR1–/– background. ZVAD, a caspase inhibitor, restored RANKL-induced osteoclastogenesis in p65–/– precursors in vitro, suggesting that p65 induces proapoptotic gene expression in osteoclastogenesis [38].
Several lines of evidence have shown that the alternative NF-κB pathway also involves RANKL-induced osteoclastogenesis. When RANKL is administered to NIK-deficient (NIK–/–) mice, osteoclast formation is more inhibited than it is when RANKL is administered to wild-type mice. Osteoclast progenitor cells derived from NIK–/– mice did not induce processing of p100 to p52 by RANKL stimulation due to IκB-like function of the C-terminus of p100 [39,40]. In addition, mice lacking IKKα, which is a molecule that is downstream of NIK, contain osteoclasts but are small in size and have reduced bone resorbing activity. As with NIK–/– mice, processing of p100 to p52 by RANKL stimulation does not occur in IKKα-deficient mice [32,41]. The role of RelB in osteoclastic bone resorption is still unclear. Although the number of osteoclasts was normal, the bone mass was slightly increased. However, overexpression of RelB restored RANKL-induced osteoclastogenesis in NIK–/– mice [42]. Recently, NIK-deficient and RelB-deficient female mice, but not male mice, revealed a 2-fold increase in trabecular bone mass, suggesting that the alternative NF-κB pathway involves gender difference in bone metabolism [43]. Alymphoplasia (aly/aly) mice do not undergo p100 to p52 processing because NIK is inactive. Aly/aly mice showed mild osteopetrosis and had a greatly reduced osteoclast count [44,45]. RANKL-induced osteoclast formation from the bone marrow cells of aly/aly mice was also suppressed. RANKL still induced IκBα degradation and activated classical NF-κB, but p100 to p52 processing was abolished by the aly/aly mutations. Overexpression of NFATc1 and constitutive activation of IKKα or p52 restored RANKL-induced osteoclastogenesis in aly/aly cells. The overexpression of RelB in aly/aly cells restored RANKL-induced osteoclastogenesis by inducing cancer Osaka thyroid (Cot) expression, which induces the processing of p52 from p100 in place of NIK [46]. Taken together, the balance between p52 and p100 determines RANKL-induced osteoclastogenesis.
2.2. NF-κB Inhibition Suppresses Inflammatory Bone Diseases
2.2.1. Rheumatoid Arthritis (RA)
Rheumatoid arthritis (RA) is a chronic inflammatory disease with progressive joint destruction over time [6,7,8]. Biologics such as anti-TNF-α antibodies have been shown to be effective in cases where existing drugs have not been effective [47]. The characteristic feature of RA is the proliferation and infiltration of synovial cells and angiogenesis of the joint area [6,7,8]. In the joint area, the overproduction of inflammatory cytokines such as IL-1, TNF-α, IL-6, and IL-17, adhesion molecules, and MMPs and the induction of osteoclasts are involved in bone and cartilage destruction in RA [6,7,8]. Recently, biological products, such as anti-TNF-α neutralized antibody (etanercept, infliximab, and adalimumab, etc.,) and anti-IL-6 neutralized antibody (tocilizumab), which are drugs created by biotechnology, have been used for rheumatoid arthritis. Compared to conventional antirheumatic drugs, the cost is high, but it is known to be particularly effective in suppressing joint destruction. Treatment guidelines exist to prevent the destruction of joints by introducing biologics as soon as possible when treatments centered on rheumatox are not enough to control the disease. These guidelines are widely accepted internationally [47]. Anti-TNF-α neutralized antibodies directly inhibit the binding of TNF-α to its receptor and suppress excessive inflammation that induces RANKL expression in synovial cells. IL-6 is required for the differentiation of Th17 cells that promote osteoclast differentiation, and these neutralizing antibodies are thought to not only sink local inflammation but also suppress RANKL induction and osteoclast differentiation. However, these biologics cause serious side effects, such as triggering an autoimmune anti-antibody response or weakening the body’s immune defenses. Therefore, alternative small-molecule-based therapies for inhibition of these cytokines’ effects is a hot topic both in academia and industry [47,48].
Since NF-κB is a transcription factor that regulates the expression of inflammatory cytokines, including TNF-α and IL-6, and serves as mediator for RANK signaling, selective inhibition of the classical NF-κB pathway appears to be a target for RA bone destruction [9,10,11]. Thus, to suppress the classical NF-κB pathway, experiments have been conducted [34,35,49,50,51,52,53,54] on the treatment of arthritis models with NF-κB inhibitors, such as decoy oligonucleotides, NEMO-binding domain (NBD) peptide, TAT-IκBα-super repressor, the dominant negative form of IKKβ, or IKKβ inhibitors such as N-(6-chloro-7-methoxy-9H-beta-carbolin-8-yl)-2-methylnicotinamide (ML120B), 4(2′-aminoethyl)amino-1,8-dimethylimidazo(1,2-a)quinoxaline (BMS-345541), 2-methoxy-N-((6-(1-methyl-4-(methylamino)-1,6-dihydroimidazo[4,5-d]pyrrolo[2–b]pyridin-7-yl)pyridin-2-yl)methyl)acetamide (BMS-066), or (7-[2-(cyclopropyl-methoxy)-6-hydroxyphenyl]-5-[(3S)-3-piperidinyl]-1,4-dihydro-2H-pyrido[2–d][1,3]oxazin-2-one hydrochloride (CHPD). These inhibitors can suppress bone destruction by suppressing local inflammation and osteoclast formation (Figure 2).
Figure 2.
Schematic representation of a healthy joint and rheumatoid arthritis. Rheumatoid arthritis (RA) is a characterized by extensive synovitis, cartilage erosion, and bone destruction by excessive immune and inflammatory responses. Synovial cells and immune cells produce inflammatory cytokines, such as IL-1, IL-6, and TNFα, and matrix metalloproteases (MMPs). NF-κB inhibitors, such as decoy oligonucleotides, NBD peptide, TAT-IκBα-super repressor, or IKKβ inhibitor, suppress bone destruction by suppressing local inflammation.
Iguratimod (IGU), a methanesulfonanilide, is a novel disease-modifying antirheumatic drug (DMARD) that inhibits the production of immunoglobulins without affecting B cell proliferation, various inflammatory cytokines (IL-1, -6 and -8 and TNF-α), and osteoclastogenesis by inhibiting NF-κB [55]. IGU is orally bioavailable and easily absorbed from the gastrointestinal tract, and food does not affect its pharmacokinetics. Several clinical studies have shown that IGU has immediate and long-lasting effects on RA treatment [55,56]. Thus, IGU has been acceptable as an alternative where other DMARDs are less effective or conventional RA treatment does not work well. However, some side effects, including nausea, dizziness, headaches, and itching, have been reported [55]. A recent study identified that patients carrying the ABCG2 rs2231142 allele were highly responsive to IGU, while those carrying NAT rs1495742G had the lowest response. Furthermore, patients carrying CYP2C19*2 rs4244285 had a higher risk of IGU toxicity [57]. This report may useful to predict the patient’s response to IGU and to avoid the potential toxicity.
It has been reported that not only these inhibitors but also components contained in plant extracts, such as turmeric supplements, Trachelospermi caulis, Moutan cortex radicis, or Saposhnikovia divaricata, can suppress the activation of the classical NF-κB pathway, which mediates excessive immune responses and inflammation followed by cartilage destruction in arthritis [58,59,60,61,62,63,64,65,66]. The dietary ω-3 polyunsaturated fatty acids (PUFAs), eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), originating from fish oils, also reduce pain and inflammation in RA by suppressing IL-1 or TNF-α production via NF-κB activation. A recent clinical trial indicated that when fish oil was used as an adjunctive therapy in drug treatment for recent onset RA, rates of remission increased and drug use decreased [67]. Moreover, a daily diet of extra-virgin olive oil significantly reduced joint edema and cartilage destruction, preventing arthritis development in a mouse CIA model by suppressing inflammatory cytokines and MMP3 production induced by the Janus kinase signal transducer and activator of transcription (JAK/STAT), mitogen-activated protein kinases (MAPKs), and the NF-κB pathway [68]. These ingredients are safe because they can be taken into the body as foods and supplements, but they are less effective as therapeutic agents for rheumatism, and may be synergistic when used as an aid to therapeutic agents.
Recent findings showed the involvement of the alternative NF-κB pathway on the development of RA [69,70]. NIK is highly expressed in synovial endothelial cells of RA patients [69]. NIK promotes pathogenic angiogenesis and synovial inflammation via CXCL12 production from endothelial cells [70]. Furthermore, NIK–/– mice have been found to be resistant to antigen-induced arthritis resulting from T cell responses [40,71]. So far, there is no suggestion that the specific inhibitor of NIK suppresses bone destruction on an RA model. However, for the B cell activating factor belonging to the tumor necrosis factor family (BAFF), which activates the alternative NF-κB pathway [10], antagonists improved the arthritis score of collagen-induced arthritis [72]. Taken together, these findings show that the alternative pathway is involved in the development of RA.
2.2.2. Ankylosing Spondylitis (AS)
Ankylosing spondylitis (AS) is a chronic arthritis accompanied by inflammation of bone at the cartilage–bone interface [73,74]. AS develops with time via chronic inflammation mainly in the spine, and extra bone is formed in the spine, followed by the fusion of vertebrae. The disease’s most prominent onset starts from the ages of 20 to 30 and is most prominent in males; men and women are affected at a ratio of approximately 3:1. Although the etiology of AS is unknown, HLA-B27 belongs to the class-1 surface antigens present on the interface of “MHC” antigenic peptides of T-cells, and is mainly involved in the pathogenesis of AS. The functions of HLA-B27 regulate its ability to misfold, to induce an endoplasmic reticulum stress response, and to promote autophagy/unfolded protein responses (UPR). The expression of UPR genes induces inflammatory cytokine production, such as TNF-α and IL-17 from Th17 cells [73,74]. Since AS is an HLA-B27-linked inflammatory disease, AS has been treated with anti-inflammatory or immunosuppressive drugs [73]. Recent data suggested a role for TNF-α in the pathophysiology of AS and showed that TNF-α mRNA is upregulated in the sacroiliac joints of AS patients. Therefore, if a patient continues to suffer high AS disease symptoms and the conventional treatments are not effective, then anti-TNF-α or anti-TNF receptor antibodies (such as adalimumab, etanercept, certolizumab pegol, infliximab, and golimumab) can be an option [75]. Anti-TNF antibodies not only effectively treat AS but they also suppress inflammation and improve spine mobility with sustained effects. In general, suppressing TNF not only suppresses bone resorption but also enhances bone formation [76]. AS is a disease in which excessive bone formation occurs, but an improvement in symptoms is considered to be an anti-inflammatory effect that is stronger than the promotion of bone formation. However, it is necessary to select alternative DMARDs, including selective NF-κB inhibitor, for patients who do not respond well to TNF-α inhibition, or when considering the costs and side effects of anti-TNF-α treatments.
2.2.3. Periodontal Disease
Periodontal disease is a chronic inflammation caused by a bacterial infection [77,78]. Bacterial plaques induce host inflammation, and the ongoing inflammatory response induces periodontal tissue destruction. Periodontal disease is characterized by the formation of periodontal pockets, the resorption of alveolar bone, and the movement of the tip barrier of the epithelium, which destroys periodontal tissue. It is also well known that multiple risk factors accelerate periodontitis. Periodontal disease is mainly treated by the mechanical removal of causative substances such as bacteria and plaque; pharmacotherapy is not very effective. This difficulty in treatment may be because of the anatomical complexity of the periodontal tissue and its constant contact with the external environment [77,78]. Since NF-κB is involved in the onset and progression of various inflammatory diseases, pharmacotherapies targeting NF-κB have been attempted. Similarly, in periodontal disease, the administration of IMD-0354, a novel NF-κB inhibitor that suppresses IKKβ activity, has been used in ligation-induced periodontitis models, and it significantly suppresses RANKL, IL-1β, and TNF-α expression in gingival tissues. Furthermore, the number of osteoclasts also decreased following treatment, and bone resorption was suppressed [79]. The application of NF-κB inhibitors may represent new pharmacotherapy options for periodontal patients.
2.3. The Activation of NF-κB Suppresses Bone Formation
Bone is composed of hydroxyapatite crystals and various extracellular matrix proteins, including type I collagen, osteocalcin, osteopontin, bone sialoprotein, and proteoglycan. Most of these bone matrix proteins are secreted and deposited by mature osteoblasts that are aligned on the bone surface. The formation of hydroxyapatite crystals in osteoid is also regulated by osteoblasts. The expression of numerous bone-related extracellular matrix proteins and the activity of alkaline phosphatase (ALP) are key features of osteoblasts [1,2].
Osteoblasts differentiate from mesenchymal stem cells, and their differentiation stage is cooperatively and dynamically controlled by specific signal transduction pathways, directly or indirectly. Osteoblasts differentiate from mesenchymal stem cells through various intracellular signaling mechanisms by various cytokines and hormones, such as bone morphogenetic proteins (BMPs), transforming growth factor (TGF)-β, Wnt, hedgehog, fibroblast growth factor, and estrogen. This intracellular signal transduction is activated by phosphorylation, ubiquitination, protein–protein interactions and structural changes following the binding of ligands to receptors. Since mice with either Runx2 or Osterix transcription factors knocked out exhibited impaired bone formation, these two transcription factors have been reported to be important for osteoblast differentiation [1,2,80].
It is known that bone formation is suppressed in an inflammatory state, and, in particular, TNF-α is known to suppress osteoblast differentiation in various culture systems [76,81,82,83,84]. TNF-α activates various signals in the cell, but a specific IKK inhibitor, BAY11-7082, restores the suppression of osteoblast differentiation induced by TNF-α [85]. Recently, it has been reported that the inhibition of NF-κB by the dominant negative form of IKKβ enhances bone formation [13]. The administration of an inhibitor of IKK, S1627, promoted bone formation in ovariectomized (OVX) mice [14]. Mice expressing the dominant negative form of IKKβ in mature osteoblasts showed increased bone mass, bone mineral density, and osteoblast activity without exhibiting any changes to osteoclast activity. Furthermore, expressing the dominant negative form of IKKβ maintained the bone mass of OVX mice by increasing the expression of Fos-related antigen-1 (Fra1), which is an essential transcription factor involved in bone matrix formation [13]. There are also reports supporting these findings that show that estrogen receptors inhibit the activation of the classical NF-κB pathway by interacting with NF-κB [86]. As another possibility, TNF-α, IL-1β, IL-6, and IL-17 produced by T cells and other cells during osteoporosis have been reported to activate the classical NF-κB pathway [87].
Bone morphogenetic proteins (BMPs) belong to the TGF-β superfamily and were originally identified by their ability to induce ectopic bone formation when implanted into muscle tissue [88,89]. Since BMP signaling and the classical NF-κB pathway have opposing biological activities, crosstalk between the two is possible. A cell-permeable inhibitor of the classical NF-κB pathway restored the inhibitory effects of TNF-α on BMP2-induced Runx2 expression and osteoblast differentiation [90]. Zinc inhibits the classical NF-κB pathway by TNF-α and promotes BMP2-induced osteoblast differentiation [91]. Pyrrolidine dithiocarbamate (PDTC), which inhibits the classical NF-κB pathway, partially blocked the TNF-α-induced suppression of osteoblast differentiation. These results indicate that inhibition of the classical NF-κB pathway by BMP [92] reverses osteoblast differentiation in a mechanism dependent on TNF-α. Thus, the implantation of collagen sponges containing BAY11-7082, a selective inhibitor of the classical NF-κB pathway, with BMP2 under the fascia resulted in the formation of larger amounts of ectopic bone than what was seen following treatment with only BMP2 [93]. These results suggest that selective inhibitors of the classical NF-κB pathway have the effect of promoting bone formation by BMP. However, the side effects of its administration must be considered, since inhibition of the classical NF-κB pathway activity might induce cell death [26,27,28,29,30,31]. Therefore, to enhance the effect of BMP without impairing the function of the classical NF-κB pathway, the suppression mechanism of the BMP/Smad signal of the classical NF-κB pathway was examined. There are various stages of BMP/Smad signaling, but the classical NF-κB pathway does not affect the phosphorylation of Smad1/5 or the formation of the Smad1–Smad4 complex; however, the classical NF-κB pathway does interfere with the DNA binding complex. Furthermore, we found that the p65 subunit of the classical NF-κB pathway associates with Smad4 but not Smad1 [64]. Therefore, when the association sites of p65 and Smad4 were examined, the transactivation domain 2 (TA2) of p65 and the mad homology (MH) 1 region of Smad1 were directly associated. We further narrowed the association site to the amino acid level and found that the 16 amino acid sites on the N-terminal side of the TA domain of p65 were critical for binding to Smad4; we named the site the Smad binding domain (SBD) [94]. We synthesized the SBD peptide to compete with the interaction of p65 with Smad4. The SBD peptide promoted ALP activity and calcification induced by BMP2 in vitro. Furthermore, administration of SBD peptide together with BMP2 induced ectopic thick cortical bone formation in vivo. The SBD peptide did not affect the activation of the classical NF-κB pathway by TNF-α stimulation [94]. Based on these results, it is possible that peptides targeting the association site of NF-κB, p65 and Smad4 may be useful for promoting bone formation by BMP with few side effects (Figure 3).
Figure 3.
A peptide that blocks the interaction of NF-κB p65 subunit with Smad4 enhances BMP2-induced bone formation. Inhibitors of the classical NF-κB pathway have been reported to promote bone formation, but mice deficient in p65, the main subunit of NF-κB, are embryonic lethal and must be considered for possible side effects. Therefore, we investigated the molecular mechanism by which NF-κB suppresses BMP signaling and revealed that p65 and the BMP-signaling molecule Smad4 are associated. We suggested the possibility of enhancing the effect of BMP without impairing the function of NF-κB by using a peptide that specifically inhibits the association site.
Recently, a heterozygous de novo missense mutation (c.1534_1535delinsAG, p.Asp512Ser) in exon 11 of RELA encoding Rela/p65 was found in a neonate who had died suddenly and unexpectedly with high bone mass (HBM) that was judged radiographically and by skeletal histopathology [95]. Numerous morphologically normal osteoclasts in the neonate were observed in bone histology, suggesting that the missense change was associated with neonatal osteosclerosis from increased osteoblastic bone formation in utero rather than failed osteoclastic bone resorption. Moreover, LPS stimulation failed to activate the classical NF-κB pathway in fibroblasts derived from the neonate. This is the first report that demonstrates the importance of the Rela/p65 subunit within the classical NF-κB pathway for human skeletal homeostasis and represents a new genetic cause of HBM [95].
Bone histomorphometric data from aly/aly mice show an increase in trabecular bone volume caused by both the suppression of bone resorption and increased bone formation, suggesting that the alternative NF-κB pathway also regulates osteoblastic bone formation [96]. ALP activity and the expression of osteoblastic markers (including osteocalcin, Id1, Osterix, and Runx2) induced by either β-glycerophosphate and ascorbic acid or BMPs were increased in primary osteoblasts (POB) derived from aly/aly mice compared with WT mice. The ectopic bone formation in vivo induced by BMP2 was enhanced in aly/aly mice compared with WT mice, due to enhancement of BMP2 signaling [96]. Thus, the alternative NF-κB pathway via the processing of p52 from p100 negatively regulates osteoblastic differentiation and bone formation by modifying BMP activity. Mice that have RelB, a main subunit of the alternative NF-κB pathway, knocked out develop age-related increased trabecular bone mass associated with increased bone formation [97]. RelB–/– bone marrow stromal cells enhanced osteoblastic differentiation by increasing Runx2 expression. RelB directly bound to the Runx2 promoter to inhibit its activation. Moreover, RelB–/– bone-derived mesenchymal progenitor cells (MPCs) formed bone more rapidly than WT cells after they were injected into a murine bone defect model [97].
Notch is a family of evolutionarily conserved receptors that regulate cell fate, and its signaling plays various important roles in bone metabolism [98]. Notch signaling and the alternative NF-κB pathway were identified as signaling pathways responsible for the inhibitory effects of TNF-α on osteoblastic differentiation. This was done by RNA sequencing and pathway analysis of mesenchymal stem cells using WT and TNF-α transgenic (Tg) mice, a model of RA [99]. Notch inhibitors restored bone loss and osteoblast inhibition in TNF-α Tg mice. The transplantation of fibroblasts from TNF-α Tg mice treated with Notch inhibitors formed more new bone in recipient mice with bone defects. The activation of the alternative NF-κB pathway in a murine pluripotent stem cell line induced RPBjκ and HES1 in a Notch intracellular domain dependent manner (NICD-dependent). TNF-α enhanced the binding of p52/RelB heterodimer to NICD, which induced binding at the RBPjκ site within the Hes1 promoter. Elevated levels of HES1, p52, and RelB were observed in mesenchymal stem cells from RA patients [99]. These results indicate that the inhibition of the alternative NF-κB pathway could reduce age-related bone loss and enhance bone repair as well as inflammation-mediated bone loss.
3. Conclusions
The balance between bone resorption and bone formation is important in maintaining bone mass. Bone resorption is enhanced in a state of inflammation, and bone mass is reduced when bone formation is inhibited. Although the molecular mechanisms of osteoclast differentiation, osteoclast activation, osteoblast differentiation, and bone formation have been analyzed in detail, NF-κB is commonly associated with key terms such as “inflammation”, “bone resorption”, and “suppression of bone formation” [9,10,11]. The inhibitors of NF-κB have been reported to promote bone formation in addition to anti-inflammatory action and osteoclast formation inhibition. Iguratimod (IGU) is a low molecular weight compound that inhibits the classical NF-κB pathway. It is currently used as one of the therapeutic agents for RA and has been reported to be effective [56]. Thus, targeting NF-κB is effective at maintaining bone mass during inflammation [13,14,15,34,35,36,37,49,50,51,52,53,54,55,56,58,59,60,61,62,63,64,65,66,67,68,69,85,91,92,93,94], and there is a possibility for “killing two birds with one stone”. However, embryonic lethality has been reported in mice where molecules involved in the NF-κB signaling have been knocked out [26,27,28,29,30,31], and it is necessary to consider the possibility of causing serious side effects simply by inhibiting NF-κB. In fact, there are reports of RA patients who are less responsive to IGU and patients who experience adverse side effects. To find practical applications of other NF-κB inhibitors, translational research not only for animal experiments, but also for human applications, will become necessary. It is important to continue to work on basic and clinical research regarding the molecular mechanism of inflammatory bone disease to provide more options to patients.
Abbreviations
| NF-κB | Nuclear factor κB |
| IKK | IκB kinase |
| NIK | NF-κB-inducing kinase |
| RA | Rheumatoid arthritis |
| NEMO | NF-κB essential modulator |
| MMPs | Matrix metalloproteases |
Author Contributions
E.J. designed and wrote the manuscript including a figure by critical discussion with N.T., F.H., I.N., and S.H.-T. All authors contributed to the final manuscript.
Funding
This work was supported by the research grant for the OBT Research Center from Kyushu University (to EJ.) and by Grants-in-Aid from the Ministry of Education, Culture, Sports, Science and Technology of Japan (JP17K11706 to S.TH.).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Aubin J.E., Triffitt J.T. Mesenchymal stem cells and osteoblast differentiation. In: Bilezikian J.P., Raisz L.G., Rodan G.A., editors. Principles of Bone Biology. 2nd ed. Academic Press; San Diego, CA, USA: 2002. pp. 59–81. [Google Scholar]
- 2.De Paula F.J., Rosen C.J. Bone remodeling and energy metabolism: New perspectives. Bone Res. 2013;1:72–84. doi: 10.4248/BR201301005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Feng X., Teitelbaum S.L. Osteoclasts: New Insights. Bone Res. 2013;1:11–26. doi: 10.4248/BR201301003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kobayashi Y., Uehara S., Udagawa N., Takahashi N. Regulation of bone metabolism by Wnt signals. J. Biochem. 2016;159:387–392. doi: 10.1093/jb/mvv124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Okamoto K., Nakashima T., Shinohara M., Negishi-Koga T., Komatsu N., Terashima A., Sawa S., Nitta T., Takayanagi H. Osteoimmunology: The Conceptual framework unifying the immune and skeletal systems. Physiol. Rev. 2017;97:1295–1349. doi: 10.1152/physrev.00036.2016. [DOI] [PubMed] [Google Scholar]
- 6.Selmi C. Autoimmunity in 2018. Clin. Rev. Allergy Immunol. 2019;56:375–384. doi: 10.1007/s12016-019-08745-w. [DOI] [PubMed] [Google Scholar]
- 7.Favero M., Giusti A., Geusens P., Goldring S.R., Lems W., Schett G., Bianchi G. OsteoRheumatology: A new discipline? RMD Open. 2015;15:e000083. doi: 10.1136/rmdopen-2015-000083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ceccarelli F., Saccucci M., Di Carlo G., Lucchetti R., Pilloni A., Pranno N., Luzzi V., Valesini G., Polimeni A. Periodontitis and rheumatoid arthritis: The same inflammatory mediators? Mediat. Inflamm. 2019;2019:6034546. doi: 10.1155/2019/6034546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jimi E., Ghosh S. Role of nuclear factor-κB in the immune system and bone. Immunol. Rev. 2005;208:80–87. doi: 10.1111/j.0105-2896.2005.00329.x. [DOI] [PubMed] [Google Scholar]
- 10.Hayden M.S., Ghosh S. Regulation of NF-κB by TNF family cytokines. Semin. Immunol. 2014;26:253–266. doi: 10.1016/j.smim.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sun S.C. The non-canonical NF-κB pathway in immunity and inflammation. Nat. Rev. Immunol. 2017;17:545–558. doi: 10.1038/nri.2017.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Britanova L., Makeev V.J., Kuprash D.V. In vitro selection of optimal RelB/p52 DNA-binding motifs. Biochem. Biophys. Res. Commun. 2008;365:583–588. doi: 10.1016/j.bbrc.2007.10.200. [DOI] [PubMed] [Google Scholar]
- 13.Iotsova V., Caamaño J., Loy J., Yang Y., Lewin A., Bravo R. Osteopetrosis in mice lacking NF-κB1 and NF-κB2. Nat. Med. 1997;3:1285–1289. doi: 10.1038/nm1197-1285. [DOI] [PubMed] [Google Scholar]
- 14.Franzoso G., Carlson L., Xing L., Poljak L., Shores E.W., Brown K.D., Leonardi A., Tran T., Boyce B.F., Siebenlist U. Requirement for NF-κB in osteoclast and B-cell development. Genes Dev. 1997;11:3482–3496. doi: 10.1101/gad.11.24.3482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chang J., Wang Z., Tang E., Fan Z., McCauley L., Franceschi R., Guan K., Krebsbach P.H., Wang C.Y. Inhibition of osteoblastic boneformation by nuclear factor-κB. Nat. Med. 2009;15:682–689. doi: 10.1038/nm.1954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alles N., Soysa N.S., Hayashi J., Khan M., Shimoda A., Shimokawa H., Ritzeler O., Akiyoshi K., Aoki K., Ohya K. Suppression of NF-κB increases bone formation and ameliorates osteopenia in ovariectomized mice. Endocrinology. 2010;151:4626–4634. doi: 10.1210/en.2010-0399. [DOI] [PubMed] [Google Scholar]
- 17.Nakashima T., Hayashi M., Takayanagi H. New insights into osteoclastogenic signaling mechanisms. Trends Endocrinol. Metab. 2012;23:582–590. doi: 10.1016/j.tem.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 18.Kong Y.Y., Yoshida H., Sarosi I., Tan H.L., Timms E., Capparelli C., Morony S., Oliveira-dos-Santos A.J., Van G., Itie A., et al. OPGL is a key regulator of osteoclastogenesis, lymphocyte development and lymph-node organogenesis. Nature. 1999;397:315–323. doi: 10.1038/16852. [DOI] [PubMed] [Google Scholar]
- 19.Dougall W.C., Glaccum M., Charrier K., Rohrbach K., Brasel K., De Smedt T., Daro E., Smith J., Tometsko M.E., Maliszewski C.R., et al. RANK is essential for osteoclast and lymph node development. Genes Dev. 1999;13:2412–2424. doi: 10.1101/gad.13.18.2412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mizuno A., Amizuka N., Irie K., Murakami A., Fujise N., Kanno T., Sato Y., Nakagawa N., Yasuda H., Mochizuki S., et al. Severe osteoporosis in mice lacking osteoclastogenesis inhibitory factor/osteoprotegerin. Biochem. Biophys. Res. Commun. 1998;247:610–615. doi: 10.1006/bbrc.1998.8697. [DOI] [PubMed] [Google Scholar]
- 21.Min H., Morony S., Sarosi I., Dunstan C.R., Capparelli C., Scully S., Van G., Kaufman S., Kostenuik P.J., Lacey D.L., et al. Osteoprotegerin reverses osteoporosis by inhibiting endosteal osteoclasts and prevents vascular calcification by blocking a process resembling osteoclastogenesis. J. Exp. Med. 2000;192:463–474. doi: 10.1084/jem.192.4.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martin T.J., Sims N.A. RANKL/OPG; Critical role in bone physiology. Rev. Endocr. Metab. Disord. 2015;16:131–139. doi: 10.1007/s11154-014-9308-6. [DOI] [PubMed] [Google Scholar]
- 23.Darnay B.G., Haridas V., Ni J., Moore P.A., Aggarwal B.B. Characterization of the intracellular domain of receptor activator of NF-κB (RANK). Interaction with tumor necrosis factor receptor-associated factors and activation of NF-κB and c-Jun N-terminal kinase. J. Biol. Chem. 1998;273:20551–20555. doi: 10.1074/jbc.273.32.20551. [DOI] [PubMed] [Google Scholar]
- 24.Naito A., Azuma S., Tanaka S., Miyazaki T., Takaki S., Takatsu K., Nakao K., Nakamura K., Katsuki M., Yamamoto T., et al. Severe osteopetrosis, defective interleukin-1 signalling and lymph node organogenesis in TRAF6-deficient mice. Genes Cells. 1999;4:353–362. doi: 10.1046/j.1365-2443.1999.00265.x. [DOI] [PubMed] [Google Scholar]
- 25.Grigoriadis A.E., Wang Z.Q., Cecchini M.G., Hofstetter W., Felix R., Fleisch H.A., Wagner E.F. c-Fos: A key regulator of osteoclast-macrophage lineage determination and bone remodeling. Science. 1994;266:443–448. doi: 10.1126/science.7939685. [DOI] [PubMed] [Google Scholar]
- 26.Beg A.A., Sha W.C., Bronson R.T., Ghosh S., Baltimore D. Embryonic lethality and liver degeneration in mice lacking the RelA component of NF-κB. Nature. 1995;376:167–170. doi: 10.1038/376167a0. [DOI] [PubMed] [Google Scholar]
- 27.Li Q., Van Antwerp D., Mercurio F., Lee K.F., Verma I.M. Severe liver degeneration in mice lacking the IκB kinase 2 gene. Science. 1999;284:321–325. doi: 10.1126/science.284.5412.321. [DOI] [PubMed] [Google Scholar]
- 28.Tanaka M., Fuentes M.E., Yamaguchi K., Durnin M.H., Dalrymple S.A., Hardy K.L., Goeddel D.V. Embryonic lethality, liver degeneration, and impaired NF-κB activation in IKK-β-deficient mice. Immunity. 1999;10:421–429. doi: 10.1016/S1074-7613(00)80042-4. [DOI] [PubMed] [Google Scholar]
- 29.Li Z.W., Chu W., Hu Y., Delhase M., Deerinck T., Ellisman M., Johnson R., Karin M. The IKKβ subunit of IκB kinase (IKK) is essential for nuclear factor kB activation and prevention of apoptosis. J. Exp. Med. 1999;189:1839–1845. doi: 10.1084/jem.189.11.1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Makris C., Godfrey V.L., Krähn-Senftleben G., Takahashi T., Roberts J.L., Schwarz T., Feng L., Johnson R.S., Karin M. Female mice heterozygous for IKKγ/NEMO deficiencies develop a dermatopathy similar to the human X-linked disorder incontinentia pigmenti. Mol. Cell. 2000;5:969–979. doi: 10.1016/S1097-2765(00)80262-2. [DOI] [PubMed] [Google Scholar]
- 31.Schmidt-Supprian M., Bloch W., Courtois G., Addicks K., Israël A., Rajewsky K., Pasparakis M. NEMO/IKKγ-deficient mice model incontinentia pigmenti. Mol. Cell. 2000;5:981–992. doi: 10.1016/S1097-2765(00)80263-4. [DOI] [PubMed] [Google Scholar]
- 32.Ruocco M.G., Maeda S., Park J.M., Lawrence T., Hsu L.C., Cao Y., Schett G., Wagner E.F., Karin M. IkB kinase (IKK)β, but not IKKα, is a critical mediator of osteoclast survival and is required for inflammation-induced bone loss. J. Exp. Med. 2005;201:1677–1687. doi: 10.1084/jem.20042081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Otero J.E., Dai S., Foglia D., Alhawagri M., Vacher J., Pasparakis M., Abu-Amer Y. Defective osteoclastogenesis by IKKβ-null precursors is a result of receptor activator of NF-κB ligand (RANKL)-induced JNK-dependent apoptosis and impaired differentiation. J. Biol. Chem. 2008;283:24546–24553. doi: 10.1074/jbc.M800434200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jimi E., Aoki K., Saito H., D’Acquisto F., May M.J., Nakamura I., Sudo T., Kojima T., Okamoto F., Fukushima H., et al. Selective inhibition of NF-κB blocks osteoclastogenesis and prevents inflammatory bone destruction in vivo. Nat. Med. 2004;10:617–624. doi: 10.1038/nm1054. [DOI] [PubMed] [Google Scholar]
- 35.Dai S., Hirayama T., Abbas S., Abu-Amer Y. The IκB kinase (IKK) inhibitor, NEMO-binding domain peptide, blocks osteoclastogenesis and bone erosion in inflammatory arthritis. J. Biol. Chem. 2004;279:37219–37222. doi: 10.1074/jbc.C400258200. [DOI] [PubMed] [Google Scholar]
- 36.Shishodia S., Gutierrez A.M., Lotan R., Aggarwal B.B. N-(4-hydroxyphenyl) retinamide inhibits invasion, suppresses osteoclastogenesis, and potentiates apoptosis through down-regulation of IκBα kinase and nuclear factor-κB-regulated gene products. Cancer Res. 2005;65:9555–9565. doi: 10.1158/0008-5472.CAN-05-1585. [DOI] [PubMed] [Google Scholar]
- 37.Takatsuna H., Asagiri M., Kubota T., Oka K., Osada T., Sugiyama C., Saito H., Aoki K., Ohya K., Takayanagi H., et al. Inhibition of RANKL-induced osteoclastogenesis by (-)-DHMEQ, a novel NF-κB inhibitor, through downregulation of NFATc1. J. Bone Miner. Res. 2005;20:653–662. doi: 10.1359/JBMR.041213. [DOI] [PubMed] [Google Scholar]
- 38.Vaira S., Alhawagri M., Anwisye I., Kitaura H., Faccio R., Novack D.V. RelA/p65 promotes osteoclast differentiation by blocking a RANKL-induced apoptotic JNK pathway in mice. J. Clin. Investig. 2008;118:2088–2097. doi: 10.1172/JCI33392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Novack D.V., Yin L., Hagen-Stapleton A., Schreiber R.D., Goeddel D.V., Ross F.P., Teitelbaum S.L. The IκB function of NF-κB2 p100 controls stimulated osteoclastogenesis. J. Exp. Med. 2003;198:771–781. doi: 10.1084/jem.20030116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Aya K., Alhawagri M., Hagen-Stapleton A., Kitaura H., Kanagawa O., Novack D.V. NF-κB-inducing kinase controls lymphocyte and osteoclast activities in inflammatory arthritis. J. Clin. Investig. 2005;115:1848–1854. doi: 10.1172/JCI23763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chaisson M.L., Branstetter D.G., Derry J.M., Armstrong A.P., Tometsko M.E., Takeda K., Akira S., Dougall W.C. Osteoclast differentiation is impaired in the absence of inhibitor of κB kinase α. J. Biol. Chem. 2004;279:54841–54848. doi: 10.1074/jbc.M406392200. [DOI] [PubMed] [Google Scholar]
- 42.Vaira S., Johnson T., Hirbe A.C., Alhawagri M., Anwisye I., Sammut B., O’Neal J., Zou W., Weilbaecher K.N., Faccio R., et al. RelB is the NF-κB subunit downstream of NIK responsible for osteoclast differentiation. Proc. Natl. Acad. Sci. USA. 2008;105:3897–3902. doi: 10.1073/pnas.0708576105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zarei A., Yang C., Gibbs J., Davis J.L., Ballard A., Zeng R., Cox L., Veis D.J. Manipulation of the alternative NF-κB pathway in mice has sexually dimorphic effects on bone. JBMR Plus. 2018;3:14–22. doi: 10.1002/jbm4.10066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Soysa N.S., Alles N., Weih D., Lovas A., Mian A.H., Shimokawa H., Yasuda H., Weih F., Jimi E., Ohya K., et al. The pivotal role of the alternative NF-κB pathway in maintenance of basal bone homeostasis and osteoclastogenesis. J. Bone Miner. Res. 2010;25:809–818. doi: 10.1359/jbmr.091030. [DOI] [PubMed] [Google Scholar]
- 45.Maruyama T., Fukushima H., Nakao K., Shin M., Yasuda H., Weih F., Doi T., Aoki K., Alles N., Ohya K., et al. Processing of the NF-κB2 precursor p100 to p52 is critical for RANKL-induced osteoclast differentiation. J. Bone Miner. Res. 2010;25:1058–1067. doi: 10.1359/jbmr.091032. [DOI] [PubMed] [Google Scholar]
- 46.Taniguchi R., Fukushima H., Osawa K., Maruyama T., Yasuda H., Weih F., Doi T., Maki K., Jim E. RelB-induced expression of Cot, an MAP3K family member, rescues RANKL-induced osteoclastogenesis in alymphoplasia mice by promoting NF-κB2 processing by IKKα. J. Biol. Chem. 2014;289:7349–7361. doi: 10.1074/jbc.M113.538314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Abbasi M., Mousavi M.J., Jamalzehi S., Alimohammadi R., Bezvan M.H., Mohammadi H., Aslani S. Strategies toward rheumatoid arthritis therapy; the old and the new. J. Cell Physiol. 2019;234:10018–10031. doi: 10.1002/jcp.27860. [DOI] [PubMed] [Google Scholar]
- 48.Zaka M., Abbasi B.H., Durdagi S. Novel tumor necrosis factor-α (TNF-α) inhibitors from small molecule library screening for their therapeutic activity profiles against rheumatoid arthritis using target-driven approaches and binary QSAR models. Biomol. Struct. Dyn. 2019;37:2464–2476. doi: 10.1080/07391102.2018.1491423. [DOI] [PubMed] [Google Scholar]
- 49.Tomita T., Takeuchi E., Tomita N., Morishita R., Kaneko M., Yamamoto K., Nakase T., Seki H., Kato K., Kaneda Y., et al. Suppressed severity of collagen-induced arthritis by in vivo transfection of nuclear factor κB decoy oligodeoxynucleotides as a gene therapy. Arthritis Rheum. 1999;42:2532–2542. doi: 10.1002/1529-0131(199912)42:12<2532::AID-ANR5>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 50.Tak P.P., Gerlag D.M., Aupperle K.R., van de Geest D.A., Overbeek M., Bennett B.L., Boyle D.L., Manning A.M., Firestein G.S. Inhibitor of nuclear factor κB kinase β is a key regulator of synovial inflammation. Arthritis Rheum. 2001;44:1897–1907. doi: 10.1002/1529-0131(200108)44:8<1897::AID-ART328>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 51.Wen D., Nong Y., Morgan J.G., Gangurde P., Bielecki A., Dasilva J., Keaveney M., Cheng H., Fraser C., Schopf L., et al. A selective small molecule IκB kinase β inhibitor blocks nuclear factor κB-mediated inflammatory responses in human fibroblast-like synoviocytes, chondrocytes, and mast cells. J. Pharmacol. Exp. Ther. 2006;317:989–1001. doi: 10.1124/jpet.105.097584. [DOI] [PubMed] [Google Scholar]
- 52.Schopf L., Savinainen A., Anderson K., Kujawa J., DuPont M., Silva M., Siebert E., Chandra S., Morgan J., Gangurde P., et al. IKKβ inhibition protects against bone and cartilage destruction in a rat model of rheumatoid arthritis. Arthritis Rheum. 2006;54:3163–3173. doi: 10.1002/art.22081. [DOI] [PubMed] [Google Scholar]
- 53.Gillooly K.M., Pattoli M.A., Taylor T.L., Chen L., Cheng L., Gregor K.R., Whitney G.S., Susulic V., Watterson S.H., Kempson J., et al. Periodic, partial inhibition of IκB Kinase β-mediated signaling yields therapeutic benefit in preclinical models of rheumatoid arthritis. J. Pharmacol. Exp. Ther. 2009;331:349–360. doi: 10.1124/jpet.109.156018. [DOI] [PubMed] [Google Scholar]
- 54.Tsuchiya A., Imai K., Asamitsu K., Waguri-Nagaya Y., Otsuka T., Okamoto T. Inhibition of inflammatory cytokine production from rheumatoid synovial fibroblasts by a novel IκB kinase inhibitor. J. Pharmacol. Exp. Ther. 2010;333:236–243. doi: 10.1124/jpet.109.158899. [DOI] [PubMed] [Google Scholar]
- 55.Li J., Bao J., Zeng J., Yan A., Zhao C., Shu Q. Iguratimod: A valuable remedy from the Asia Pacific region for ameliorating autoimmune diseases and protecting bone physiology. Bone Res. 2019;7:27. doi: 10.1038/s41413-019-0067-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mimori T., Harigai M., Atsumi T., Fujii T., Kuwana M., Matsuno H., Momohara S., Takei S., Tamura N., Takasaki Y., et al. Safety and effectiveness of iguratimod in patients with rheumatoid arthritis: Final report of a 52-week, multicenter postmarketing surveillance study. Mod. Rheumatol. 2019;29:314–323. doi: 10.1080/14397595.2018.1460230. [DOI] [PubMed] [Google Scholar]
- 57.Xiao W., Guo J.P., Li C., Ye H., Wei W., Zou Y., Dai L., Li Z., Zhang M., Li X., et al. Genetic predictors of efficacy and toxicity of iguratimod in patients with rheumatoid arthritis. Pharmacogenomics. 2018;19:383–392. doi: 10.2217/pgs-2017-0162. [DOI] [PubMed] [Google Scholar]
- 58.Funk J.L., Frye J.B., Oyarzo J.N., Kuscuoglu N., Wilson J., McCaffrey G., Stafford G., Chen G., Lantz R.C., Jolad S.D., et al. Efficacy and mechanism of action of turmeric supplements in the treatment of experimental arthritis. Arthritis Rheum. 2006;54:3452–3464. doi: 10.1002/art.22180. [DOI] [PubMed] [Google Scholar]
- 59.Kim H.S., Kim A.R., Lee J.M., Kim S.N., Choi J.H., Kim D.K., Kim J.H., Kim B., Her E., Yang Y.M., et al. A mixture of Trachelospermi caulis and Moutan cortex radicis extracts suppresses collagen-induced arthritis in mice by inhibiting NF-κB and AP-1. J. Pharm. Pharmacol. 2012;64:420–429. doi: 10.1111/j.2042-7158.2011.01415.x. [DOI] [PubMed] [Google Scholar]
- 60.Kong X., Liu C., Zhang C., Zhao J., Wang J., Wan H., Zhu H., Zhang P., Chen W., Xiao Y., et al. The suppressive effects of Saposhnikovia divaricata (Fangfeng) chromone extract on rheumatoid arthritis via inhibition of nuclear factor-κB and mitogen activated proteinkinases activation on collagen-induced arthritis model. J. Ethnopharmacol. 2013;148:842–850. doi: 10.1016/j.jep.2013.05.023. [DOI] [PubMed] [Google Scholar]
- 61.Min H.K., Kim S.M., Baek S.Y., Woo J.W., Park J.S., Cho M.L., Lee J., Kwok S.K., Kim S.W., Park S.H. Anthocyanin Extracted from Black Soybean Seed Coats Prevents Autoimmune Arthritis by Suppressing the Development of Th17 Cells and Synthesis of Proinflammatory Cytokines by Such Cells, via Inhibition of NF-κB. PLoS ONE. 2015;10:e0138201. doi: 10.1371/journal.pone.0138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Xu W., Huang M., Zhang Y., Li H., Zheng H., Yu L., Chu K. Extracts of Bauhinia championii (Benth.) Benth. inhibit NF-κB-signaling in a rat model of collagen-induced arthritis and primary synovial cells. J. Ethnopharmacol. 2016;185:140–146. doi: 10.1016/j.jep.2016.03.035. [DOI] [PubMed] [Google Scholar]
- 63.Sun W.X., Liu Y., Zhou W., Li H.W., Yang J., Chen Z.B. Shikonin inhibits TNF-α production through suppressing PKC-NF-κB-dependent decrease of IL-10 in rheumatoid arthritis-like cell model. J. Nat. Med. 2017;71:349–356. doi: 10.1007/s11418-016-1064-3. [DOI] [PubMed] [Google Scholar]
- 64.Xia Z.B., Yuan Y.J., Zhang Q.H., Li H., Dai J.L., Min J.K. Salvianolic acid B suppresses inflammatory mediator levels by downregulating NF-κB in a rat modelof rheumatoid arthritis. Med. Sci. Monit. 2018;24:2524–2532. doi: 10.12659/MSM.907084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Uttra A.M., Shahzad M., Shabbir A., Jahan S. Ephedra gerardiana aqueous ethanolic extract and fractions attenuate freund complete adjuvant induced arthritis in Sprague Dawley rats by downregulating PGE2, COX2, IL-1β, IL-6, TNF-α, NF-κB and upregulating IL-4 and IL-10. J. Ethnopharmacol. 2018;224:482–496. doi: 10.1016/j.jep.2018.06.018. [DOI] [PubMed] [Google Scholar]
- 66.Morin C., Blier P.U., Fortin S. Eicosapentaenoic acid and docosapentaenoic acid monoglycerides are more potent than docosahexaenoic acid monoglyceride to resolve inflammation in a rheumatoid arthritis model. Arthritis Res. Ther. 2015;17:142. doi: 10.1186/s13075-015-0653-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Proudman S.M., Cleland L.G., Metcalf R.G., Sullivan T.R., Spargo L.D., James M.J. Plasma n-3 fatty acids and clinical outcomes in recent-onset rheumatoid arthritis. Br. J. Nutr. 2015;114:885–890. doi: 10.1017/S0007114515002718. [DOI] [PubMed] [Google Scholar]
- 68.Rosillo M.A., Sánchez-Hidalgo M., Sánchez-Fidalgo S., Aparicio-Soto M., Villegas I., Alarcón-de-la-Lastra C. Dietary extra-virgin olive oil prevents inflammatory response and cartilage matrix degradation in murine collagen-induced arthritis. Eur. J. Nutr. 2016;55:315–325. doi: 10.1007/s00394-015-0850-0. [DOI] [PubMed] [Google Scholar]
- 69.Maijer K.I., Noort A.R., de Hair M.J., van der Leij C., van Zoest K.P., Choi I.Y., Gerlag D.M., Maas M., Tak P.P., Tas S.W. Nuclear Factor-κB-inducing Kinase Is Expressed in Synovial Endothelial Cells in Patients with Early Arthritis and Correlates with Markers of Inflammation: A Prospective Cohort Study. J. Rheumatol. 2015;42:1573–1581. doi: 10.3899/jrheum.150245. [DOI] [PubMed] [Google Scholar]
- 70.Noort A.R., van Zoest K.P., Weijers E.M., Koolwijk P., Maracle C.X., Novack D.V., Siemerink M.J., Schlingemann R.O., Tak P.P., Tas S.W. NF-κB-inducing kinase is a key regulator of inflammation-induced and tumour-associated angiogenesis. J. Pathol. 2014;234:375–385. doi: 10.1002/path.4403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yang C., McCoy K., Davis J.L., Schmidt-Supprian M., Sasaki Y., Faccio R., Novack D.V. NIK stabilization in osteoclasts results in osteoporosis and enhanced inflammatory osteolysis. PLoS ONE. 2010;5:e15383. doi: 10.1371/journal.pone.0015383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wang H., Marsters S.A., Baker T., Chan B., Lee W.P., Fu L., Tumas D., Yan M., Dixit V.M., Ashkenazi A., et al. TACI-ligand interactions are required for T cell activation and collagen-induced arthritis in mice. Nat. Immunol. 2001;2:632–637. doi: 10.1038/89782. [DOI] [PubMed] [Google Scholar]
- 73.Xi Y., Jiang T., Chaurasiya B., Zhou Y., Yu J., Wen J., Shen Y., Ye X., Webster T.J. Advances in nanomedicine for the treatment of ankylosing spondylitis. Int. J. Nanomed. 2019;14:8521–8542. doi: 10.2147/IJN.S216199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pedersen S.J., Maksymowych W.P. The Pathogenesis of Ankylosing Spondylitis: An Update. Curr. Rheumatol. Rep. 2019;21:58. doi: 10.1007/s11926-019-0856-3. [DOI] [PubMed] [Google Scholar]
- 75.Callhoff J., Sieper J., Weiß A., Zink A., Listing J. Efficacy of TNFα blockers in patients with ankylosing spondylitis and non-radiographic axial spondyloarthritis: A meta-analysis. Ann. Rheum. Dis. 2015;74:1241–1248. doi: 10.1136/annrheumdis-2014-205322. [DOI] [PubMed] [Google Scholar]
- 76.Zhao B. TNF and Bone Remodeling. Curr. Osteoporos Rep. 2017;15:126–134. doi: 10.1007/s11914-017-0358-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Di Benedetto A., Gigante I., Colucci S., Grano M. Periodontal disease: Linking the primary inflammation to bone loss. Clin. Dev. Immunol. 2013;2013:503754. doi: 10.1155/2013/503754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Li C.H., Amar S. Morphometric, histomorphometric, and microcomputed tomographic analysis of periodontal inflammatory lesions in a murine model. J. Periodontol. 2007;78:1120–1128. doi: 10.1902/jop.2007.060320. [DOI] [PubMed] [Google Scholar]
- 79.Kure K., Sato H., Suzuki J.I., Itai A., Aoyama N., Izumi Y. A novel IκB kinase inhibitor attenuates ligature-induced periodontal disease in mice. J. Periodontal. Res. 2019;54:164–173. doi: 10.1111/jre.12615. [DOI] [PubMed] [Google Scholar]
- 80.Katagiri T., Takahashi N. Regulatory mechanisms of osteoblast and osteoclast differentiation. Oral Dis. 2002;8:147–159. doi: 10.1034/j.1601-0825.2002.01829.x. [DOI] [PubMed] [Google Scholar]
- 81.Canalis E. Effects of tumor necrosis factor on bone formation in vitro. Endocrinology. 1987;121:1596–1604. doi: 10.1210/endo-121-5-1596. [DOI] [PubMed] [Google Scholar]
- 82.Nakase T., Takaoka K., Masuhara K., Shimizu K., Yoshikawa H., Ochi T. Interleukin-1β enhances and tumor necrosis factor-α inhibits bone morphogenetic protein-2-induced alkaline phosphatase activity in MC3T3-E1 osteoblastic cells. Bone. 1997;21:17–21. doi: 10.1016/S8756-3282(97)00038-0. [DOI] [PubMed] [Google Scholar]
- 83.Gilbert L., He X., Farmer P., Boden S., Kozlowski M., Rubin J., Nanes M.S. Inhibition of osteoblast differentiation by tumor necrosis factor-α. Endocrinology. 2000;141:3956–3964. doi: 10.1210/endo.141.11.7739. [DOI] [PubMed] [Google Scholar]
- 84.Nanes M.S. Tumor necrosis factor-α: Molecular and cellular mechanisms in skeletal pathology. Gene. 2003;321:1–15. doi: 10.1016/S0378-1119(03)00841-2. [DOI] [PubMed] [Google Scholar]
- 85.Yamazaki M., Fukushima H., Shin M., Katagiri T., Doi T., Takahashi T., Jimi E. Tumor necrosis factor α represses bone morphogenetic protein (BMP) signaling by interfering with the DNA binding of Smads through the activation of NF-κB. J. Biol. Chem. 2009;284:35987–35995. doi: 10.1074/jbc.M109.070540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Raisz L.G. Pathogenesis of osteoporosis: Concepts, conflicts, and prospects. J. Clin. Investig. 2005;115:3318–3325. doi: 10.1172/JCI27071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tyagi A.M., Srivastava K., Mansoori M.N., Trivedi R., Chattopadhyay N., Singh D. Estrogen deficiency induces the differentiation of IL-17 secreting Th17 cells: A new candidate in the pathogenesis of osteoporosis. PLoS ONE. 2012;7:e44552. doi: 10.1371/journal.pone.0044552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Katagiri T., Watabe T. Bone Morphogenetic Proteins. Cold Spring Harb. Perspect. Biol. 2016;8:a021899. doi: 10.1101/cshperspect.a021899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Jimi E. The Role of BMP Signaling and NF-κB Signaling on osteoblastic differentiation, cancer development, and vascular diseases—Is the activation of NF-κB a friend or foe of BMP function? Vitam. Horm. 2015;99:145–170. doi: 10.1016/bs.vh.2015.05.002. [DOI] [PubMed] [Google Scholar]
- 90.Li Y., Li A., Strait K., Zhang H., Nanes M.S., Weitzmann M.N. Endogenous TNFα lowers maximum peak bone mass and inhibits osteoblastic Smad activation through NF-κB. J. Bone Miner. Res. 2007;22:646–655. doi: 10.1359/jbmr.070121. [DOI] [PubMed] [Google Scholar]
- 91.Yamaguchi M., Weitzmann M.N. Zinc stimulates osteoblastogenesis and suppresses osteoclastogenesis by antagonizing NF-κB activation. Mol. Cell Biochem. 2011;355:179–186. doi: 10.1007/s11010-011-0852-z. [DOI] [PubMed] [Google Scholar]
- 92.Tang Y., Xie H., Chen J., Geng L., Chen H., Li X., Hou Y., Lu L., Shi S., Zeng X., et al. Activated NF-κB in bone marrow mesenchymal stem cells from systemic lupus erythematosus patients inhibits osteogenic differentiation through downregulating Smad signaling. Stem. Cells Dev. 2013;22:668–678. doi: 10.1089/scd.2012.0226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hirata-Tsuchiya S., Fukushima H., Katagiri T., Ohte S., Shin M., Nagano K., Aoki K., Morotomi T., Sugiyama G., Nakatomi C., et al. Inhibition of BMP2-induced bone formation by the p65 subunit of NF-κB via an interaction with Smad4. Mol. Endocrinol. 2014;28:1460–1470. doi: 10.1210/me.2014-1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Urata M., Kokabu S., Matsubara T., Sugiyama G., Nakatomi C., Takeuchi H., Hirata-Tsuchiya S., Aoki K., Tamura Y., Moriyama Y., et al. A peptide that blocks the interaction of NF-κB p65 subunit with Smad4 enhances BMP2-induced osteogenesis. J. Cell Physiol. 2018;233:7356–7366. doi: 10.1002/jcp.26571. [DOI] [PubMed] [Google Scholar]
- 95.Frederiksen A.L., Larsen M.J., Brusgaard K., Novack D.V., Knudsen P.J., Schrøder H.D., Qiu W., Eckhardt C., McAlister W.H., Kassem M., et al. Neonatal high bone mass with first mutation of the NF-κB complex: Heterozygous de novo missense (p.Asp512Ser) RELA (Rela/p65) J. Bone Miner. Res. 2016;31:163–172. doi: 10.1002/jbmr.2590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Seo Y., Fukushima H., Maruyama T., Kuroishi K.N., Osawa K., Nagano K., Aoki K., Weih F., Doi T., Zhang M., et al. Accumulation of p100, a precursor of NF-κB2, enhances osteoblastic differentiation in vitro and bone formation in vivo in aly/aly mice. Mol. Endocrinol. 2012;26:414–422. doi: 10.1210/me.2011-1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Yao Z., Li Y., Yin X., Dong Y., Xing L., Boyce B.F. NF-κB RelB negatively regulates osteoblast differentiation and bone formation. J. Bone Miner. Res. 2014;29:866–877. doi: 10.1002/jbmr.2108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zanotti S., Canalis E. Notch and the skeleton. Mol. Cell Biol. 2010;30:886–896. doi: 10.1128/MCB.01285-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Zhang H., Hilton M.J., Anolik J.H., Welle S.L., Zhao C., Yao Z., Li X., Wang Z., Boyce B.F., Xing L. NOTCH inhibits osteoblast formation in inflammatory arthritis via noncanonical NF-κB. J. Clin. Investig. 2014;124:3200–3214. doi: 10.1172/JCI68901. [DOI] [PMC free article] [PubMed] [Google Scholar]