Abstract
Background
Dental caries is a major public health problem in most industrialised countries, affecting 60% to 90% of school children. Community water fluoridation was initiated in the USA in 1945 and is currently practised in about 25 countries around the world; health authorities consider it to be a key strategy for preventing dental caries. Given the continued interest in this topic from health professionals, policy makers and the public, it is important to update and maintain a systematic review that reflects contemporary evidence.
Objectives
To evaluate the effects of water fluoridation (artificial or natural) on the prevention of dental caries.
To evaluate the effects of water fluoridation (artificial or natural) on dental fluorosis.
Search methods
We searched the following electronic databases: The Cochrane Oral Health Group's Trials Register (to 19 February 2015); The Cochrane Central Register of Controlled Trials (CENTRAL; Issue 1, 2015); MEDLINE via OVID (1946 to 19 February 2015); EMBASE via OVID (1980 to 19 February 2015); Proquest (to 19 February 2015); Web of Science Conference Proceedings (1990 to 19 February 2015); ZETOC Conference Proceedings (1993 to 19 February 2015). We searched the US National Institutes of Health Trials Registry (ClinicalTrials.gov) and the World Health Organization's WHO International Clinical Trials Registry Platform for ongoing trials. There were no restrictions on language of publication or publication status in the searches of the electronic databases.
Selection criteria
For caries data, we included only prospective studies with a concurrent control that compared at least two populations ‐ one receiving fluoridated water and the other non‐fluoridated water ‐ with outcome(s) evaluated at at least two points in time. For the assessment of fluorosis, we included any type of study design, with concurrent control, that compared populations exposed to different water fluoride concentrations. We included populations of all ages that received fluoridated water (naturally or artificially fluoridated) or non‐fluoridated water.
Data collection and analysis
We used an adaptation of the Cochrane 'Risk of bias' tool to assess risk of bias in the included studies.
We included the following caries indices in the analyses: decayed, missing and filled teeth (dmft (deciduous dentition) and DMFT (permanent dentition)), and proportion caries free in both dentitions. For dmft and DMFT analyses we calculated the difference in mean change scores between the fluoridated and control groups. For the proportion caries free we calculated the difference in the proportion caries free between the fluoridated and control groups.
For fluorosis data we calculated the log odds and presented them as probabilities for interpretation.
Main results
A total of 155 studies met the inclusion criteria; 107 studies provided sufficient data for quantitative synthesis.
The results from the caries severity data indicate that the initiation of water fluoridation results in reductions in dmft of 1.81 (95% CI 1.31 to 2.31; 9 studies at high risk of bias, 44,268 participants) and in DMFT of 1.16 (95% CI 0.72 to 1.61; 10 studies at high risk of bias, 78,764 participants). This translates to a 35% reduction in dmft and a 26% reduction in DMFT compared to the median control group mean values. There were also increases in the percentage of caries free children of 15% (95% CI 11% to 19%; 10 studies, 39,966 participants) in deciduous dentition and 14% (95% CI 5% to 23%; 8 studies, 53,538 participants) in permanent dentition. The majority of studies (71%) were conducted prior to 1975 and the widespread introduction of the use of fluoride toothpaste.
There is insufficient information to determine whether initiation of a water fluoridation programme results in a change in disparities in caries across socioeconomic status (SES) levels.
There is insufficient information to determine the effect of stopping water fluoridation programmes on caries levels.
No studies that aimed to determine the effectiveness of water fluoridation for preventing caries in adults met the review's inclusion criteria.
With regard to dental fluorosis, we estimated that for a fluoride level of 0.7 ppm the percentage of participants with fluorosis of aesthetic concern was approximately 12% (95% CI 8% to 17%; 40 studies, 59,630 participants). This increases to 40% (95% CI 35% to 44%) when considering fluorosis of any level (detected under highly controlled, clinical conditions; 90 studies, 180,530 participants). Over 97% of the studies were at high risk of bias and there was substantial between‐study variation.
Authors' conclusions
There is very little contemporary evidence, meeting the review's inclusion criteria, that has evaluated the effectiveness of water fluoridation for the prevention of caries.
The available data come predominantly from studies conducted prior to 1975, and indicate that water fluoridation is effective at reducing caries levels in both deciduous and permanent dentition in children. Our confidence in the size of the effect estimates is limited by the observational nature of the study designs, the high risk of bias within the studies and, importantly, the applicability of the evidence to current lifestyles. The decision to implement a water fluoridation programme relies upon an understanding of the population's oral health behaviour (e.g. use of fluoride toothpaste), the availability and uptake of other caries prevention strategies, their diet and consumption of tap water and the movement/migration of the population. There is insufficient evidence to determine whether water fluoridation results in a change in disparities in caries levels across SES. We did not identify any evidence, meeting the review's inclusion criteria, to determine the effectiveness of water fluoridation for preventing caries in adults.
There is insufficient information to determine the effect on caries levels of stopping water fluoridation programmes.
There is a significant association between dental fluorosis (of aesthetic concern or all levels of dental fluorosis) and fluoride level. The evidence is limited due to high risk of bias within the studies and substantial between‐study variation.
Keywords: Adolescent; Child; Child, Preschool; Humans; DMF Index; Dental Caries; Dental Caries/prevention & control; Fluoridation; Fluoridation/adverse effects; Fluoridation/methods; Fluorosis, Dental; Fluorosis, Dental/epidemiology; Fluorosis, Dental/etiology; Observational Studies as Topic; Prospective Studies; Selection Bias
Plain language summary
Water fluoridation to prevent tooth decay
Background
Tooth decay is a worldwide problem affecting most adults and children. Untreated decay may cause pain and lead to teeth having to be removed. In many parts of the world, tooth decay is decreasing. Children from poorer backgrounds still tend to have greater levels of decay. Fluoride is a mineral that prevents tooth decay. It occurs naturally in water at varying levels. Fluoride can also be added to the water with the aim of preventing tooth decay. Fluoride is present in most toothpastes and available in mouthrinses, varnishes and gels. If young children swallow too much fluoride while their permanent teeth are forming, there is a risk of marks developing on those teeth. This is called ‘dental fluorosis’. Most fluorosis is very mild, with faint white lines or streaks visible only to dentists under good lighting in the clinic. More noticeable fluorosis, which is less common, may cause people concern about how their teeth look.
Review question
We carried out this review to evaluate the effects of fluoride in water (added fluoride or naturally occurring) on the prevention of tooth decay and markings on teeth (dental fluorosis).
Study characteristics
We reviewed 20 studies on the effects of fluoridated water on tooth decay and 135 studies on dental fluorosis. The evidence is up to date at 19 February 2015.
Nineteen studies assessed the effects of starting a water fluoridation scheme. They compared tooth decay in two communities around the time fluoridation started in one of them. After several years, a second survey was done to see what difference it made. Around 70% of these studies were conducted before 1975. Other, more recent studies comparing fluoridated and non‐fluoridated communities have been conducted. We excluded them from our review because they did not carry out initial surveys of tooth decay levels around the time fluoridation started so were unable to evaluate changes in those levels since then. We reviewed one study that compared tooth decay in two fluoridated areas before fluoridation was stopped in one area. Again, after several years, a second survey was done to see what difference it made.
Around 73% of dental fluorosis studies were conducted in places with naturally occurring – not added – fluoride in their water. Some had levels of up to 5 parts per million (ppm).
Key results
Our review found that water fluoridation is effective at reducing levels of tooth decay among children. The introduction of water fluoridation resulted in children having 35% fewer decayed, missing and filled baby teeth and 26% fewer decayed, missing and filled permanent teeth. We also found that fluoridation led to a 15% increase in children with no decay in their baby teeth and a 14% increase in children with no decay in their permanent teeth. These results are based predominantly on old studies and may not be applicable today.
Within the ‘before and after’ studies we were looking for, we did not find any on the benefits of fluoridated water for adults.
We found insufficient information about the effects of stopping water fluoridation.
We found insufficient information to determine whether fluoridation reduces differences in tooth decay levels between children from poorer and more affluent backgrounds.
Overall, the results of the studies reviewed suggest that, where the fluoride level in water is 0.7 ppm, there is a chance of around 12% of people having dental fluorosis that may cause concern about how their teeth look.
Quality of the evidence
We assessed each study for the quality of the methods used and how thoroughly the results were reported. We had concerns about the methods used, or the reporting of the results, in the vast majority (97%) of the studies. For example, many did not take full account of all the factors that could affect children’s risk of tooth decay or dental fluorosis. There was also substantial variation between the results of the studies, many of which took place before the introduction of fluoride toothpaste. This makes it difficult to be confident of the size of the effects of water fluoridation on tooth decay or the numbers of people likely to have dental fluorosis at different levels of fluoride in the water.
Summary of findings
for the main comparison.
| Initiation of water fluoridation compared with low/non‐fluoridated water for the prevention of dental caries | ||||||
|
Patient or population: people of all ages Settings: community setting Intervention: initiation of water fluoridation Comparison: low/non‐fluoridated water | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk in area with low/non‐fluoridated water | Risk in area with initiation of water fluoridation | |||||
| Caries in deciduous teeth (dmft)1 Scale from: 0 to 20 (lower = better) Follow‐up: range from 3‐12 years |
The mean dmft at follow‐up in the low/non‐fluoridated areas ranged from 1.21 to 7.8 (median 5.1) | The mean dmft in the areas with water fluoridation was 1.81 lower (1.31 lower to 2.31 lower) | 44,2682 (9 observational studies) |
⊕⊕⊝⊝3,4,5,6 | This indicates a reduction in dmft of 35% in the water fluoridation groups over and above that for the control groups We have limited confidence in the size of this effect due to the high risk of bias within the studies and the lack of contemporary evidence |
|
| Caries score in permanent teeth (DMFT)7 Scale from: 0 to 32 (lower better) Follow‐up: range from 8‐11 years |
The mean DMFT at follow‐up in the low/non‐fluoridated areas ranged from 0.7 to 5.5 (median 4.4) | The mean DMFT in the areas with water fluoridation was 1.16 lower (0.72 lower to 1.61 lower) | 78,7642 (10 observational studies) |
⊕⊕⊝⊝3,4,5,6 | This indicates a reduction in DMFT of 26% in the water fluoridation groups over and above that for the control groups We have limited confidence in the size of this effect due to the high risk of bias within the studies and the lack of contemporary evidence |
|
| Change in proportion of caries‐free children (deciduous teeth) Scale: 0 to 1 Follow‐up: range 3‐12 years |
The proportion of caries‐free children at follow‐up in the low/non‐fluoridated areas ranged from 0.06 to 0.67 (median 0.22) | The proportion of caries‐free children increased in the areas with water fluoridation 0.15 (0.11 to 0.19) | 39,9662 (10 observational studies) |
⊕⊕⊝⊝3,4,5,6 | We have limited confidence in the size of this effect due to the high risk of bias within the studies and the lack of contemporary evidence | |
| Change in proportion of caries‐free children (permanent teeth) Scale: 0 to 1 Follow‐up: range 8‐12 years |
The proportion of caries‐free children at follow‐up in the low/non‐fluoridated areas ranged from 0.01 to 0.67 (median 0.14) | The proportion of caries‐free children increased in the areas with water fluoridation 0.14 (0.05 to 0.23) | 53,5382 (8 observational studies) |
⊕⊕⊝⊝3,4,5,6 | We have limited confidence in the size of this effect due to the high risk of bias within the studies and the lack of contemporary evidence. | |
| Disparities in caries by socioeconomic status (SES)8 | > 35,3999 (3 observational studies) |
⊕⊕⊝⊝3 | There is insufficient information to determine whether initiation of a water fluoridation programme results in a change in disparities in caries levels across SES | |||
| Adverse effects Dental fluorosis of aesthetic concern10 (measured by Dean's Index, TFI, TSIF)11 |
For a fluoride level of 0.7 ppm the percentage of participants with dental fluorosis of aesthetic concern was estimated to be 12% (95% CI 8% to 17%). Controlling for study effects, we would expect the odds of dental fluorosis to increase by a factor of 2.90 (95% CI 2.05 to 4.10) for each one unit increase in fluoride level (1 ppm F). |
59,630 (40 observational studies) |
⊕⊕⊝⊝3,12 | The estimate for any level of dental fluorosis at 0.7ppm was 40% (95% CI 35% to 44%; 90 studies). This includes dental fluorosis that can only be detected under clinical conditions and other enamel defects We have limited confidence in the size of this effect due to the high risk of bias and substantial between‐study variation. |
||
| ⊕⊕⊕⊕: We are very confident that the true effect lies close to that of the estimate of the effect. Further research is very unlikely to change the estimate of effect. ⊕⊕⊕⊝: We are moderately confident in the effect estimate. Further research may change the estimate. ⊕⊕⊝⊝: Our confidence in the effect estimate is limited. Further research is likely to change the estimate. ⊕⊝⊝⊝: We are very uncertain about the estimate. | ||||||
- dmft ‐ decayed, missing and filled deciduous teeth
- Total number of participants measured. Analysis undertaken on average number of participants measured at baseline and follow‐up for each study
- Studies at high risk of bias; quality of the evidence downgraded
- Substantial heterogeneity present, however, given that the direction of effect was the same in all but on of the studies/outcomes we did not downgrade due to heterogeneity
- Indirectness of evidence due to lack of contemporary evidence; quality of the evidence downgraded. 71% of the studies conducted prior 1975; the use of fluoridated toothpaste, the availability of other caries prevention strategies, diet and tap water consumption are all likely to have changed in the populations in which the studies were conducted. No studies on the effect of water fluoridation in adults met the inclusion criteria
- Very large effect size; quality of the evidence upgraded twice
- DMFT ‐ decayed, missing and filled permanent teeth
- SES ‐ socioeconomic status
- Number of participants not stated in one study
- Data come from studies of both naturally occurring and artificially fluoridated areas (i.e. not just areas where water fluoridation has been initiated). Dental fluorosis of aesthetic concern only with levels of reported fluoride exposure of 5 ppm or less
- TFI ‐ Thylstrup‐Fejerskov Index: TSIF ‐ Tooth Surface Index of Fluorosis
- Substantial heterogeneity; quality of the evidence downgraded
2.
| Cessation of water fluoridation compared with fluoridated water for the prevention of dental caries | |||
|
Patient or population: people of all ages Settings: community setting Intervention: cessation of water fluoridation Comparison: fluoridated water | |||
| Outcomes | No of participants (studies) | Quality of the evidence (GRADE) | Comments |
| Caries in permanent teeth (DMFS)1 Follow‐up: 3 years |
92492 (1 observational study) |
⊕⊝⊝⊝ 3 |
Insufficient evidence to determine the effect of the cessation of water fluoridation on caries |
| Caries in deciduous teeth (dmft/dmfs)4 | No evidence to determine the effect of the cessation of water fluoridation on caries | ||
| Change in proportion of caries‐free children (deciduous or permanent teeth) |
No evidence to determine the effect of the cessation of water fluoridation on caries | ||
| Disparities in caries by socioeconomic status (SES)5 | No evidence to determine the effect of the cessation of water fluoridation on disparities | ||
| Adverse effects | No evidence to determine whether cessation of a water fluoridation programme is associated with any harms | ||
| ⊕⊕⊕⊕: We are very confident that the true effect lies close to that of the estimate of the effect. Further research is very unlikely to change the estimate of effect. ⊕⊕⊕⊝: We are moderately confident in the effect estimate. Further research may change the estimate. ⊕⊕⊝⊝: Our confidence in the effect estimate is limited. Further research is likely to change the estimate. ⊕⊝⊝⊝: We are very uncertain about the estimate. | |||
- DMFS ‐ decayed missing and filled surfaces in permanent teeth
- Total number of participants measured
- Study at high risk of bias; quality of evidence downgraded
- dmft/dmfs ‐ decayed, missing and filled deciduous teeth/surfaces
- SES ‐ socioeconomic status
Background
Description of the condition
Dental caries is a chronic and progressive disease of the mineralised and soft tissues of the teeth. Its aetiology is multifactorial and is related to the interactions over time between tooth substance and certain micro‐organisms and dietary carbohydrates, producing plaque acids. Demineralisation of the tooth enamel (non‐cavitated dental caries) follows and in the absence of successful treatment, can extend into the dentine and the dental pulp, impairing its function (Ten Cate 1991). Despite reductions in the prevalence and severity of dental caries over time (CDC 2005), social inequalities in dental health persist (OECD 2011), with significant numbers of individuals and communities having a clinically significant burden of preventable dental disease. Dental caries is associated with pain, infection, tooth loss and reduced quality of life (Sheiham 2005). In children, the burden of dental disease also includes lost school time and restricted activity days, as well as problems in eating, speaking and learning. This especially affects those from lower income families owing to their higher prevalence of caries (Feitosa 2005). Given the progressive nature of the condition and widespread prevalence in adulthood, most children are at risk of dental caries.
Dental caries is a major public health problem in most industrialised countries, affecting 60% to 90% of school children (Petersen 2003). It has been estimated that in the USA 42% of children aged between two to 11 years have caries experience in their primary teeth and 59% of those aged 12 to 19 years have caries experience in their permanent teeth (Dye 2007). Prevalence studies in South America, Asia and Europe have indicated that caries may affect between 20% and 100% of the population (Bagramian 2009). Increasing levels of dental caries are observed in some developing countries, especially those where community‐based preventive oral care programmes are not established (Petersen 2004). Studies also suggest that the growing retention of teeth has also been accompanied by a rise in dental caries among ageing adults in different parts of the world (Selwitz 2007). This has major implications especially in high‐income countries experiencing an increase in life expectancy.
The link between fluoride and the prevention of dental caries dates back to the 1930s. There are many ways in which fluoride can be provided, including toothpastes, gels, varnishes, milk and water. An adverse effect associated with the use of fluoride is the development of dental fluorosis due to the ingestion of excessive fluoride by young children with developing teeth. Dental fluorosis occurs due to the hypomineralisation of the dental enamel caused by the chronic ingestion of sufficiently high concentrations of fluoride while the dentition is still forming (Pendrys 2001). Clinically, the appearance of teeth with fluorosis depends on the severity of the condition. In its mildest form, there are faint white lines or streaks visible only to trained examiners under controlled examination conditions. In more involved cases, fluorosis manifests as mottling of the teeth in which noticeable white lines or streaks often have coalesced into larger opaque areas. In the more severe forms, brown staining or pitting of the tooth enamel may be present and actual breakdown of the enamel may occur (Rozier 1994).
Description of the intervention
Water can be artificially fluoridated (also known as community water fluoridation) through the controlled addition of a fluoride compound to a public water supply (Department of Health and Human Services 2000). Water that is artificially fluoridated is set at the 'optimum level', considered to be around 1 ppm (Dean 1941; WHO 2011). The European Union water quality directive specifies 1.5 ppm as the maximum level for human consumption (European Union 1998). Community water fluoridation was initiated in the USA in 1945 and is currently practiced in about 25 countries around the world (The British Fluoridation Society 2012). Health authorities consider it to be a key strategy for preventing dental caries. In Western Europe around 3% of the population receive water with added fluoride (Cheng 2007), mainly in England, Ireland, and Spain. In the USA, over 70% of the population on public water systems receive fluoridated water (CDC 2008), as do a similar proportion of Australians (NHMRC 2007). The rationale behind the role of community water fluoridation is that it benefits both children and adults by effectively preventing caries, regardless of socioeconomic status or access to care. It is believed to have played an important role in the reductions in tooth decay (40% to 70% in children) and of tooth loss in adults (40% to 60%) in the USA (Burt 1999). Fluoridation is an intervention that occurs at the environmental level, meaning that individual compliance is not relied upon. Interventions at this level can have greater impact upon populations than those at the individual and clinical levels (Frieden 2010), although concerns have been raised around the ethics of 'mass intervention' (Cheng 2007).
Fluoride is also naturally present in the soil, in water and the atmosphere at varying levels depending on geographic location. In areas of Africa, Asia, the Middle East, Southern Europe and the Southern USA, ground waters have been found to contain particularly high concentrations of fluoride, well above the 'optimum level' of 1 ppm. However, while ground waters in some areas can contain high concentrations of fluoride, fluoride content in drinking water in many locations is too low to prevent and control tooth decay.
How the intervention might work
Fluoride impedes the demineralisation of the enamel and also enhances its remineralisation, if it is present in high enough concentrations in the saliva (Ten Cate 1991). This function is very important in caries prevention as the progression of cavities depends on the balance of the demineralisation and remineralisation processes (Selwitz 2007). The presence of fluoride in drinking water therefore confers the advantage of providing a constant exposure to fluoride ions in the oral cavity. The effectiveness of fluoridated water (McDonagh 2000; Truman 2002), and other fluoride sources, such as toothpastes and varnishes, have previously been documented (Marinho 2013; Walsh 2010). Some adverse effects of fluoridated water that have been explored are widely perceived to be dependent on dose, duration and/or time of exposure (Browne 2005). Within community water fluoridation programmes, maximum fluoride concentrations are set to prevent other harms related to very high fluoride concentrations. Supra‐optimal levels of fluoride (occurring naturally) have been linked to severe dental fluorosis and skeletal fluorosis. There is a lack of evidence for other postulated harms such as cancer and bone fractures; no evidence of a strong association with water fluoridation has been shown for these conditions (McDonagh 2000).
Why it is important to do this review
Water fluoridation was identified as a priority topic in the Cochrane Oral Health Group's international priority setting exercise, incorporating views from clinicians, guideline developers and members of the public.
The use of water fluoridation as a means of improving dental health has been endorsed by many national and international health institutions, including the World Health Organization (MRC 2002). It has been hailed by the US Surgeon General as "one of the most effective choices communities can make to prevent health problems while actually improving the oral health of their citizens" (ADA 2013). Opponents have raised concerns about ethical issues and its potential harms (Cheng 2007), as a result of which the practice has remained controversial. A comprehensive systematic review of water fluoridation has previously been published (McDonagh 2000). The review showed a benefit in terms of a reduction in caries as well as an increased risk of dental fluorosis. However, there was insufficient evidence to draw conclusions regarding other potential harms or health disparities. The review findings have often been misinterpreted and have been used to support arguments on both sides of the water fluoridation debate (Cheng 2007). In addition, little comment has been made on the applicability of the evidence to today's society. Many of the caries studies presented in the McDonagh 2000 review were conducted prior to the widespread use of fluoride toothpastes in the late 1970s, and the introduction and uptake of other preventative strategies, such as fluoride varnish. The McDonagh 2000 review was conducted 15 years ago. Given the continued interest in this topic, from both health professionals, policy makers and the public, it is important to update and maintain a systematic review that reflects any emerging, contemporary evidence.
This review updates the McDonagh 2000 review. It aims to contextualise the evidence to inform current national and international guidelines.
It should be noted, the original systematic review had a broader remit and aimed to evaluate the differential effects of natural and artificial fluoridation as well as adverse effects other than dental fluorosis (McDonagh 2000). The inclusion criteria for the objectives covered in this review follow those stated in McDonagh 2000.
Objectives
To evaluate the effects of water fluoridation (artificial or natural) on the prevention of dental caries.
To evaluate the effects of water fluoridation (artificial or natural) on dental fluorosis.
Methods
Criteria for considering studies for this review
Types of studies
Water fluoridation for the prevention of dental caries
For caries data, we included only prospective studies with a concurrent control, comparing at least two populations, one receiving fluoridated water and the other non‐fluoridated water, with at least two points in time evaluated. Groups had to be comparable in terms of fluoridated water at baseline. For studies assessing the initiation of water fluoridation the groups had to be from non‐fluoridated areas at baseline, with one group subsequently having fluoride added to the water. For studies assessing the cessation of water fluoridation, groups had to be from fluoridated areas at baseline, with one group subsequently having fluoride removed from the water.
For the purposes of this review, water with a fluoride concentration of 0.4 parts per million (ppm) or less (arbitrary cut‐off defined a priori) was classified as non‐fluoridated.
Water fluoridation and dental fluorosis
For the assessment of dental fluorosis, we included any study design, with concurrent control, comparing populations exposed to different water fluoride concentrations.
It should be noted that, due to the nature of the research question, randomised controlled trials are unfeasible.
Types of participants
Populations of all ages receiving fluoridated water (naturally or artificially) and populations receiving non‐fluoridated water.
Types of interventions
Water fluoridation for the prevention of dental caries
Caries data: a change in the level of fluoride in the water supply of at least one of the study areas within three years of the baseline survey. Exposure to fluoridated water or non‐fluoridated water (less than 0.4 ppm) could be in conjunction with other sources of fluoride (e.g. fluoridated toothpaste), provided the other sources were similar across groups. Where specific information on the use of other sources of fluoride was not supplied, we assumed that populations in studies conducted after 1975 in industrialised countries had been exposed to fluoridated toothpaste.
Water fluoridation and dental fluorosis
Fluoride at any concentration present in drinking water.
Types of outcome measures
Primary outcomes
Any measure of dental caries including the following.
Change in the number of decayed, missing and filled deciduous, and permanent teeth, (dmft and DMFT, respectively).
Change in the number of decayed, missing and filled deciduous, and permanent, tooth surfaces (dmfs and DMFS, respectively).
Incidence of dental caries.
Percentage of caries‐free children.
We also recorded data on disparities in dental caries across different groups of people, as reported in the included studies.
An a priori set of rules regarding the prioritisation of caries measures has been developed previously (Marinho 2013). We would have adopted these, if the data had required.
Secondary outcomes
Dental fluorosis, as measured by the following.
Percentage of children with fluorosis (any level of fluorosis, or fluorosis of aesthetic concern).
Dean's Fluorosis Index.
Tooth Surface Index of Fluorosis (TSIF).
Thylstrup and Fejerskov index (TFI).
Modified Developmental Defects of Enamel (DDE).
We aimed to record the prevalence of dental fluorosis for each dentition if reported in the studies. In measuring the percentage prevalence of dental fluorosis, we classified children with dental fluorosis according to the index used in the individual studies. As measured by the common epidemiologic indices for dental fluorosis (Rozier 1994), we classified children with a DDE, TSIF, TFI score greater than zero or Dean's classification of 'questionable' or higher as having dental fluorosis. If other indices had been used, we would have considered and adopted the percentage prevalence of dental fluorosis as reported by the original investigators using other methods (e.g. photographic method or other index). Any dental fluorosis scoring ≥ 3 (TFI), ≥ 2 (TSIF) and 'mild' or worse (Dean's) were considered to be of aesthetic concern. We restricted analysis on dental fluorosis of aesthetic concern to TFI, TSIF and Dean's indices as it is not easily determined from the modified DDE index.
Within the context of this review dental fluorosis is referred to as an 'adverse effect'. However, it should be acknowledged that moderate fluorosis may be considered an 'unwanted effect' rather than an adverse effect. In addition, mild fluorosis may not even be considered an unwanted effect.
We also recorded data on any other adverse effects (e.g. skeletal fluorosis, hip fractures, cancer, congenital malformations, mortality) reported in the included studies. However, this review did not aim to provide a comprehensive systematic review of adverse effects other than dental fluorosis.
Search methods for identification of studies
The original review involved searching a wide range of databases from their starting date to June/October 1999 (Appendix 1). Full details of all the strategies initially used have been published previously (McDonagh 2000).
For the identification of studies included or considered for this updated review, we developed detailed search strategies combining controlled vocabulary and free text terms for each database searched. These were based on the search strategy developed for MEDLINE (Appendix 4) but revised appropriately for each database to take account of differences in controlled vocabulary and syntax rules.
Electronic searches
We searched the following electronic databases (from inception):
The Cochrane Oral Health Group's Trials Register (to 19 February 2015; see Appendix 2);
The Cochrane Central Register of Controlled Trials (CENTRAL; The Cochrane Library 2015, Issue 1; see Appendix 3);
MEDLINE via OVID (1946 to 19 February 2015; see Appendix 4);
EMBASE via OVID (1980 to 19 February 2015; see Appendix 5);
Proquest (all databases; to 19 February 2015; Appendix 6);
Web of Science Conference Proceedings (1990 to 19 February 2015; see Appendix 7);
ZETOC Conference Proceedings (1993 to 19 February 2015; see Appendix 8).
There were no restrictions on language of publication and non‐English studies were translated, unless a translator could not be found through Cochrane.
Searching other resources
We searched the following databases for ongoing trials (see Appendix 9):
US National Institutes of Health Trials Register (clinicaltrials.gov to 19 February 2015);
The WHO Clinical Trials Registry Platform (apps.who.int/trialsearch/default.aspx to 19 February 2015).
Only handsearching conducted as part of the Cochrane Worldwide Handsearching Programme and uploaded to CENTRAL was included (see the Cochrane Masterlist for the details of journals searched to date). We reviewed the reference lists of identified trials and review articles for additional appropriate studies.
Data collection and analysis
Selection of studies
Two review authors independently and in duplicate screened the titles and abstracts (when available) of all reports identified through the electronic search update. We obtained the full report for all studies that appeared to meet the inclusion criteria, or for which there were insufficient data in the title and abstract to make a clear decision. Two review authors independently assessed the full reports obtained from the electronic and other methods of searching to establish whether or not the studies met the inclusion criteria. Disagreements were resolved by discussion. Where resolution was not possible, a third review author was consulted. Studies rejected at this or subsequent stages were recorded in the 'Characteristics of excluded studies' table, and reasons for their exclusion recorded.
Data extraction and management
Two review authors extracted data independently using specially designed data extraction forms (produced in Excel). We piloted the data extraction forms on several papers and modified them as required before use. Any disagreements were discussed and a third review author consulted where necessary.
For each study we aimed to record the following data.
Year of publication, country of origin and source of study funding.
Details of the participants including demographic characteristics (socioeconomic status (SES), ethnicity), age, deciduous/permanent dentition and criteria for inclusion and exclusion.
Details of the type of intervention, comparator and co‐interventions.
Details of the outcomes reported, including method of assessment, and time intervals.
Details of confounding factors considered (potential confounders of relevance to this review include sugar consumption/dietary habits, SES, ethnicity and the use of other fluoride sources).
Details on comparability of groups with regard to confounding factors.
Details on methods used to control for confounding.
Details regarding both unadjusted and adjusted effect estimates.
Assessment of risk of bias in included studies
McDonagh 2000 used specially designed validity assessment checklists that provided a 'validity score' and assigned a 'level of evidence' for each study. In this update, we aimed to assess all included studies (including those from the previous review by McDonagh 2000) for risk of bias using the Cochrane 'Risk of bias' assessment tool adapted for non‐randomised controlled studies (Higgins 2011). The domains assessed for each included study included: sampling, confounding, blinding of outcome assessment, completeness of outcome data, risk of selective outcome reporting and risk of other potential sources of bias. We did not include random sequence generation or allocation concealment, as these were not relevant for the study designs included and are covered by the domain for confounding. We had identified the following factors as important confounders for the primary and secondary outcomes: sugar consumption/dietary habits, SES, ethnicity and the use of other fluoride sources.
We tabulated a description of the 'Risk of bias' domains for each included trial, along with a judgement of low, high or unclear risk of bias.
We undertook a summary assessment of the risk of bias for the primary outcome (across domains) across studies (Higgins 2011). Within a study, we gave a summary assessment of low risk of bias when there was a low risk of bias for all key domains, unclear risk of bias when there was an unclear risk of bias for one or more key domains, and high risk of bias when there was a high risk of bias for one or more key domains.
Measures of treatment effect
We included the following caries indices in the analyses: dmft, DMFT, and proportion caries free in both dentitions. For dmft and DMFT analyses we calculated the difference in mean change scores between fluoridated and control groups. For the proportion caries free, we calculated the difference in the proportion caries free between the fluoridated and control groups.
For dental fluorosis data we calculated the log odds and presented them as probabilities for interpretation.
We have presented data on other adverse effects, reported in the included studies, as a narrative.
We intended to present data on both adjusted and unadjusted results, but the data allowed only for unadjusted values.
Dealing with missing data
Where outcome data were missing from the published report, or could not be calculated from the information presented in the report of a trial, we attempted to contact the authors to obtain the data and clarify any uncertainty. The analyses generally included only the available data (ignoring missing data). When the number of participants evaluated was not reported, we did not include outcome data in the analyses. Where standard deviations were missing for DMFT and dmft data we used the equation: log(SD) = 0.17 + 0.56 x log(mean) to estimate the standard deviations for both the before and after mean caries values. This equation was estimated from available data where the standard deviations were given (R² = 0.91; Appendix 10). We undertook no other imputations.
We undertook sensitivity analyses to determine the effect of the imputed standard deviations.
Assessment of heterogeneity
We planned to explore differences in fluoridation technique, fluoride concentration, outcome measurement index and technique as possible sources of heterogeneity. Initial consideration of heterogeneity would be via the DerSimonian‐Laird model (commonly referred to as a random‐effects meta‐analysis). When between study variance was deemed to be both robustly estimated and substantial (judged as the estimate being larger than twice its standard error), we favoured the random‐effects model over a fixed‐effect approach. We would have investigated any heterogeneity further via Baujat and normal quantile‐quantile (Q‐Q) plots, alongside influence diagnostics (for example difference in fitted values (DFFITS), Cook's distance, hat values and leave‐one‐out methods) as appropriate. However, due to the limited data and lack of clarity in reporting we were unable to undertake any of these analyses for the caries data. Fluoride concentration was explored as part of the fluorosis analysis.
Assessment of reporting biases
If more than 10 trials had been identified for any meta‐analysis of the primary outcome caries, we would have assessed publication bias according to the recommendations described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Had asymmetry been identified in the contour‐enhanced funnel plots, we would have investigated possible causes. The number of studies presented in each caries meta‐analyses precluded this.
Data synthesis
The primary analyses was based on all included studies, irrespective of risk of bias.
Caries
For the analyses of mean dmft and DMFT severity data, we used Review Manager (RevMan 2014; not shown) to calculate weighted (for age) mean change score for water fluoridation and control group separately, and the summary effect estimates across all age groups for each study (we only analysed data for dmft for children eight years and younger). The resulting effect estimates for the water fluoridation and control groups were then entered into RevMan for each study to calculate the mean difference in change scores for the review (see Analysis 1.1; Analysis 1.2). We decided to display this data using the average n for the before and after data for each study to give an indication of the size of the studies. The raw data and summary statistics are shown in Table 3; Table 4.
1.1. Analysis.
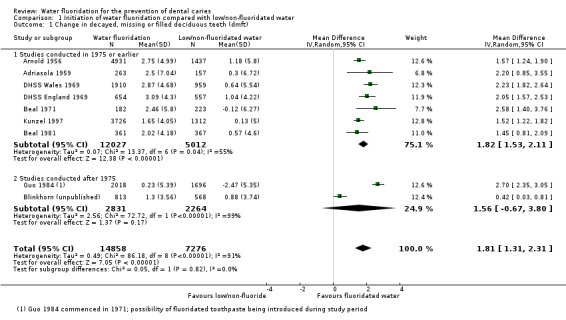
Comparison 1 Initiation of water fluoridation compared with low/non‐fluoridated water, Outcome 1 Change in decayed, missing or filled deciduous teeth (dmft).
1.2. Analysis.
Comparison 1 Initiation of water fluoridation compared with low/non‐fluoridated water, Outcome 2 Change in decayed, missing or filled permanent teeth (DMFT).
1. dmft data and underlying calculations.
| Study ID | Age | Fluoridated area | Non/low fluoridated area | |||||||||||
|
Baseline (before/at initiation) |
Follow‐up | Baseline | Follow‐up | |||||||||||
| MEAN | SD | N | MEAN | SD | N | MEAN | SD | N | MEAN | SD | N | |||
| ADRIASOLA 1959 | 5 | 8.9 | 5.03 | 186 | 6.4 | 4.18 | 340 | 8.1 | 4.77 | 174 | 7.8 | 4.67 | 140 | |
| 5 | Mean (SD) change in dmft: 2.5 (7.04) | Mean (SD) change in dmft: 0.3 (6.72) | ||||||||||||
| ARNOLD 1956a | 4 | 4.19 | 3.30 | 323 | 2.13 | 2.26 | 168 | 5.05 | 3.66 | 20 | 4.46 | 3.42 | 63 | |
| 5 | 5.37 | 3.79 | 1633 | 2.27 | 2.34 | 853 | 6.82 | 4.33 | 402 | 5.25 | 3.74 | 351 | ||
| 6 | 6.43 | 4.19 | 1789 | 2.98 | 2.73 | 750 | 7.17 | 4.46 | 462 | 5.67 | 3.91 | 294 | ||
| 7 | 6.29 | 4.14 | 1806 | 4.03 | 3.23 | 423 | 6.66 | 4.28 | 408 | 5.77 | 3.95 | 223 | ||
| 8 | 5.78 | 3.95 | 1647 | 4.12 | 3.27 | 470 | 6.06 | 4.06 | 376 | 5.32 | 3.77 | 275 | ||
| 4‐8 | Mean (SD) change in dmft: 2.75 (4.99) | Mean (SD) change in dmft: 1.18 (5.8) | ||||||||||||
| BEAL 1971 | 5 | 4.91 | 4.86 | 182 | 2.45 | 3.24 | 182 | 4.97 | 4.12 | 217 | 5.09 | 4.84 | 229 | |
| 5 | Mean (SD) change in dmft: 2.46 (5.8) | Mean (SD) change in dmft: ‐0.12 (6.27) | ||||||||||||
| BEAL 1981 | 5 | 4.29 | 3.50 | 196 | 1.8 | 2.48 | 170 | 4.28 | 3.58 | 205 | 3.49 | 3.62 | 180 | |
| 8 | 5 | 2.89 | 189 | 3.42 | 2.84 | 167 | 5.36 | 3.06 | 163 | 4.97 | 3.00 | 186 | ||
| 5/8 | Mean (SD) change in dmft: 2.02 (4.18) | Mean (SD) change in dmft: 0.57 (4.6) | ||||||||||||
| BLINKHORN 2015 | 5‐7 | 2.02 | 3.13 | 781 | 0.72 | 1.63 | 844 | 2.09 | 2.91 | 523 | 1.21 | 2.27 | 612 | |
| 5‐7 | Mean (SD) change in dmft: 1.3 (3.56) | Mean (SD) change in dmft: 0.88 (3.74) | ||||||||||||
| DHSS 1969 (Eng)a | 3 | 2.7 | 2.58 | 43 | 0.6 | 1.11 | 133 | 1.4 | 1.79 | 44 | 1.2 | 1.64 | 144 | |
| 4 | 3.6 | 3.03 | 66 | 1.3 | 1.71 | 131 | 2.6 | 2.53 | 47 | 1.8 | 2.06 | 162 | ||
| 5 | 5.4 | 3.80 | 148 | 1.6 | 1.92 | 111 | 5 | 3.64 | 110 | 2.8 | 2.63 | 119 | ||
| 6 | 5.7 | 3.92 | 182 | 2.5 | 2.47 | 130 | 5.4 | 3.80 | 127 | 4.1 | 3.26 | 107 | ||
| 7 | 6.4 | 4.18 | 192 | 2.7 | 2.58 | 172 | 6 | 4.03 | 121 | 4.3 | 3.35 | 133 | ||
| 3‐7 | Mean (SD) change in dmft: 3.09 (4.3) | Mean (SD) change in dmft: 1.04 (4.22) | ||||||||||||
| DHSS 1969 (Wales)a,b | 3 | 3.9 | 3.17 | 310 | 1.4 | 1.79 | 171 | 4 | 3.21 | 146 | 3.3 | 2.89 | 105 | |
| 4 | 5.54 | 3.86 | 413 | 2.6 | 2.53 | 267 | 5.8 | 3.96 | 210 | 4.8 | 3.56 | 122 | ||
| 5 | 5.5 | 3.84 | 556 | 2.9 | 2.69 | 284 | 5.5 | 3.84 | 256 | 4.8 | 3.56 | 138 | ||
| 6 | 6.3 | 4.15 | 603 | 3.1 | 2.79 | 310 | 6.2 | 4.11 | 331 | 5.9 | 4.00 | 133 | ||
| 7 | 6.85 | 4.35 | 640 | 3.65 | 3.05 | 266 | 7.3 | 4.50 | 346 | 6.8 | 4.33 | 130 | ||
| 3‐7 | Mean (SD) change in dmft: 2.87 (4.68) | Mean (SD) change in dmft: 0.64 (5.54) | ||||||||||||
| GUO 1984 | 3 | 3 | 3.4 | 202 | 2.6 | 3.3 | 79 | 1.3 | 3.2 | 205 | 3.7 | 3.9 | 128 | |
| 4 | 4.6 | 4 | 354 | 4.5 | 4.7 | 164 | 5.6 | 4.6 | 246 | 7.1 | 4.6 | 164 | ||
| 5 | 6.5 | 4.4 | 589 | 5.5 | 4.3 | 345 | 6.4 | 4.2 | 218 | 8.5 | 4.6 | 387 | ||
| 6 | 6.7 | 4.4 | 695 | 6.2 | 4.8 | 297 | 5.8 | 4.2 | 309 | 9 | 4.3 | 354 | ||
| 7 | 5.5 | 3.7 | 399 | 5.6 | 3.7 | 240 | 5.4 | 3.7 | 335 | 7.9 | 3.6 | 352 | ||
| 8 | 4.2 | 3 | 392 | 4.4 | 2.9 | 279 | 3.5 | 2.7 | 343 | 6 | 3.1 | 350 | ||
| 3‐8 | Mean (SD) change in dmft: 0.23 (5.39) | Mean (SD) change in dmft: ‐2.47 (5.35) | ||||||||||||
| KUNZEL 1992a | 5 | 2.4 | 2.415006452 | 688 | 1.4 | 1.7857954 | 1306 | 3.3 | 2.886475039 | 172 | 2.9 | 2.684991275 | 597 | |
| 8 | 4.9 | 3.601718817 | 2438 | 2.8 | 2.632743187 | 3020 | 4.9 | 3.601718817 | 777 | 4.9 | 3.601718817 | 1078 | ||
| 5‐8 | Mean (SD) change in dmft: 2.1 (5.01) | Mean (SD) change in dmft: 0.13 (5.0) | ||||||||||||
Note: Only data up to the age of 8 years included for the deciduous dentition
a. Imputed standard deviation
b. 2 fluoridated areas combined
2. DMFT data and underlying calculations.
| Study ID | Age | FLuoridated area | Non/low fluoridated area | |||||||||||
|
B aseline (before/at initiation) |
Follow‐up | Baseline | Follow‐up | |||||||||||
| MEAN | SD | N | MEAN | SD | N | MEAN | SD | N | MEAN | SD | N | |||
| ARNOLD 1956a | 6 | 0.78 | 1.29 | 1789 | 0.26 | 0.70 | 750 | 0.81 | 1.31 | 462 | 0.8 | 1.31 | 294 | |
| 7 | 1.89 | 2.11 | 1806 | 0.84 | 1.34 | 423 | 1.99 | 2.17 | 408 | 1.88 | 2.11 | 223 | ||
| 8 | 2.95 | 2.71 | 1647 | 1.58 | 1.91 | 470 | 2.81 | 2.64 | 376 | 2.63 | 2.54 | 275 | ||
| 9 | 3.9 | 3.17 | 1639 | 2.04 | 2.21 | 582 | 3.81 | 3.13 | 357 | 3.52 | 2.99 | 277 | ||
| 10 | 4.92 | 3.61 | 1626 | 2.93 | 2.70 | 141 | 4.91 | 3.61 | 359 | 4.32 | 3.36 | 62 | ||
| 11 | 6.41 | 4.19 | 1556 | 3.67 | 3.06 | 151 | 6.32 | 4.15 | 293 | 5.34 | 3.78 | 139 | ||
| 12 | 8.07 | 4.76 | 1685 | 5.89 | 3.99 | 176 | 8.66 | 4.95 | 328 | 7.71 | 4.64 | 48 | ||
| 13 | 9.73 | 5.29 | 1668 | 6.6 | 4.26 | 497 | 9.98 | 5.36 | 377 | 9.36 | 5.18 | 225 | ||
| 14 | 10.95 | 5.65 | 1690 | 8.21 | 4.81 | 128 | 12 | 5.95 | 369 | 11.36 | 5.77 | 59 | ||
| 15 | 12.48 | 6.08 | 1511 | 8.91 | 5.03 | 53 | 12.86 | 6.18 | 292 | 12.38 | 6.05 | 21 | ||
| 16 | 13.5 | 6.35 | 1107 | 11.06 | 5.68 | 198 | 14.07 | 6.50 | 248 | 13.16 | 6.26 | 155 | ||
| 6‐16 | Mean (SD) change in DMFT: 0.90 (3.20) | Mean (SD) change in DMFT: 0.15 (3.51) | ||||||||||||
| BEAL 1981 | 8 | 1.48 | 1.51 | 189 | 0.65 | 1.16 | 167 | 1.55 | 1.40 | 163 | 1.34 | 1.50 | 186 | |
| 12 | 3.53 | 3.32 | 192 | 2.74 | 2.33 | 189 | 4.28 | 2.47 | 188 | 4.11 | 2.95 | 197 | ||
| 8/12 | Mean (SD) change in DMFT: 0.82 (2.50) | Mean (SD) change in DMFT: 0.20 (2.64) | ||||||||||||
| BLINKHORN 2015a | 0.59 | 1.10 | 777 | 0.45 | 0.95 | 642 | 0.99 | 1.47 | 436 | 0.72 | 1.23 | 455 | ||
| Mean (SD) change in DMFT: 0.14 (1.44) | Mean (SD) change in DMFT: 0.28 (1.92) | |||||||||||||
| BROWN 1960 | 9‐11 | 4.07 | 2.20 | 595 | 1.52 | 1.80 | 502 | 4.21 | 2.63 | 571 | 3.68 | 2.35 | 521 | |
| 12‐14 | 7.68 | 3.90 | 593 | 3.23 | 2.92 | 503 | 7.94 | 4.41 | 486 | 7.46 | 4.40 | 485 | ||
| 9‐14 | Mean (SD) change in DMFT: 3.03 (3.31) | Mean (SD) change in DMFT: 0.52 (4.18) | ||||||||||||
| DHSS 1969 (Eng)a | 8 | 2.4 | 2.42 | 199 | 1.08 | 1.54 | 95 | 2.4 | 2.42 | 148 | 1.85 | 2.09 | 79 | |
| 9 | 3.1 | 2.79 | 227 | 1.5 | 1.86 | 135 | 2.9 | 2.68 | 166 | 2.4 | 2.42 | 95 | ||
| 10 | 3.6 | 3.03 | 134 | 2 | 2.18 | 115 | 3.8 | 3.12 | 160 | 3.1 | 2.79 | 80 | ||
| 11 | 4.6 | 3.48 | 145 | 3 | 2.74 | 200 | 4.7 | 3.52 | 126 | 3.9 | 3.17 | 122 | ||
| 12 | 5.6 | 3.88 | 111 | 3.52 | 2.99 | 134 | 6.1 | 4.07 | 51 | 4.99 | 3.64 | 99 | ||
| 13 | 7.1 | 4.43 | 91 | 4.9 | 3.60 | 132 | 6.6 | 4.26 | 52 | 6.1 | 4.07 | 127 | ||
| 14 | 8.4 | 4.87 | 70 | 5.77 | 3.95 | 90 | 7.9 | 4.71 | 36 | 6.74 | 4.31 | 108 | ||
| 8‐14 | Mean (SD) change in DMFT: 1.62 (3.92) | Mean (SD) change in DMFT: 0.65 (4.39) | ||||||||||||
| DHSS 1969 (Wales)a,b | 8 | 2.00 | 2.18 | 607 | 1.31 | 1.72 | 283 | 1.95 | 2.15 | 351 | 2.16 | 2.28 | 125 | |
| 9 | 2.65 | 2.55 | 553 | 1.98 | 2.17 | 260 | 2.6 | 2.53 | 325 | 2.9 | 2.68 | 134 | ||
| 10 | 3.35 | 2.91 | 502 | 2.59 | 2.52 | 241 | 3.2 | 2.84 | 308 | 3.6 | 3.03 | 133 | ||
| 11 | 3.83 | 3.14 | 278 | 2.99 | 2.73 | 126 | 3.3 | 2.89 | 270 | 4.1 | 3.26 | 42 | ||
| 12 | 4.65 | 3.50 | 186 | 4.38 | 3.38 | 108 | 3.95 | 3.19 | 265 | 6.16 | 4.09 | 108 | ||
| 13 | 6 | 4.03 | 178 | 5.9 | 4.00 | 93 | 5.2 | 3.72 | 274 | 7.6 | 4.61 | 105 | ||
| 14 | 6.95 | 4.38 | 158 | 6.73 | 4.30 | 93 | 5.6 | 3.88 | 243 | 7.64 | 4.62 | 96 | ||
| 8‐14 | Mean (SD) change in DMFT: 0.66 (3.72) | Mean (SD) change in DMFT: ‐0.73 (4.95) | ||||||||||||
| GUO 1984 | 6 | 0.2 | 0.6 | 695 | 0.2 | 0.5 | 297 | 0.1 | 0.4 | 309 | 0.5 | 0.9 | 354 | |
| 7 | 0.4 | 0.8 | 399 | 0.4 | 0.9 | 240 | 0.3 | 0.7 | 335 | 1.2 | 1.4 | 352 | ||
| 8 | 0.5 | 1 | 392 | 0.5 | 1 | 279 | 0.4 | 0.8 | 343 | 1.6 | 1.5 | 350 | ||
| 9 | 0.7 | 1.1 | 388 | 0.8 | 1.4 | 275 | 0.7 | 1.1 | 310 | 2.2 | 2 | 352 | ||
| 10 | 0.7 | 1.3 | 346 | 1.1 | 1.5 | 310 | 0.8 | 1.5 | 323 | 2.4 | 2 | 436 | ||
| 11 | 0.8 | 1.5 | 330 | 1.6 | 1.9 | 307 | 0.9 | 1.4 | 451 | 3 | 2.7 | 365 | ||
| 12 | 1.1 | 1.7 | 468 | 1.7 | 2.4 | 208 | 0.9 | 1.5 | 841 | 3.4 | 3 | 493 | ||
| 13 | 1.4 | 2 | 469 | 2.1 | 2.9 | 232 | 1.2 | 1.6 | 801 | 3.8 | 3.3 | 504 | ||
| 14 | 1.2 | 1.8 | 322 | 2.6 | 2.9 | 221 | 1 | 1.5 | 795 | 4.4 | 3.8 | 490 | ||
| 15 | 1.7 | 2.5 | 164 | 2.2 | 2.3 | 38 | 1.2 | 1.7 | 121 | 4.2 | 4 | 63 | ||
| 6‐15 | Mean (SD) change in DMFT: ‐0.11 (1.69) | Mean (SD) change in DMFT: ‐1.14 (2.59) | ||||||||||||
| HARDWICK 1982 | 12 | Mean (SD) increment in DMFT: ‐3.76 (2.86) | Mean (SD) increment in DMFT: ‐4.85 (3.39) | |||||||||||
| KUNZEL 1997c,d | 6 | 0.3 | 0.7 | 0.2 | 0.5 | 0.8 | 0.4 | 0.89 | ||||||
| 7 | 0.7 | 1.1 | 0.3 | 0.9 | 1.2 | 1 | 1.48 | |||||||
| 8 | 1.3 | 1.4 | 2419 | 0.5 | 1.00 | 3016 | 1.3 | 1.4 | 777 | 1.8 | 2.06 | 1076 | ||
| 9 | 1.9 | 1.5 | 0.9 | 1.8 | 1.6 | 2.4 | 2.42 | |||||||
| 10 | 2.4 | 1.8 | 1.2 | 2.4 | 1.8 | 3.2 | 2.84 | |||||||
| 11 | 3 | 2 | 1.6 | 2.8 | 1.8 | 3.9 | 3.17 | |||||||
| 12 | 3.7 | 2.3 | 1626 | 2 | 2.18 | 2426 | 3.5 | 2.1 | 563 | 4.8 | 3.56 | 925 | ||
| 13 | 4.3 | 2.7 | 2.6 | 4.1 | 2.6 | 5.5 | 3.84 | |||||||
| 14 | 5.3 | 3.1 | 3.4 | 4.7 | 2.5 | 6.5 | 4.22 | |||||||
| 15 | 5.8 | 3.5 | 1995 | 4 | 3.22 | 1897 | 5.2 | 3.1 | 744 | 7.4 | 4.54 | 756 | ||
| 8/12/15 | Mean (SD) change in DMFT: 1.02 (2.94) | Mean (SD) change in DMFT: ‐0.85 (3.26) | ||||||||||||
| LOH 1996 | 1.6 | 1.8 | 2 | 1.9 | 3.1 | |||||||||
| 4.4 | 2.1 | 3.7 | 4.5 | |||||||||||
| Insufficient data to include in further analysis | ||||||||||||||
| TESSIER 1987a | 6‐7 | 8.28 | 56 | 3.16 | 96 | 8.23 | 85 | 5.4 | 93 | |||||
| 6‐7 | Mean (SD) change in DMFT: 5.12 (6.16) | Mean (SD) change in DMFT: 2.83 (6.18) | ||||||||||||
a. Imputed standard deviation
b. 2 fluoridated areas combined
c. Imputed standard deviation for follow‐up data only
d. N values only available for ages 8, 12 and 15 years
Where standard deviations (SDs) are missing for the dmft, DMFT data we used the equation: log(SD) = 0.17 + 0.56 x log(mean) to estimate the SDs for both before and after mean caries values. We undertook a sensitivity analysis omitting all the data for studies/age groups where the standard deviation was imputed.
For the caries free data for both dentitions, we calculated the risk differences in RevMan (not shown) for water fluoridation and control groups separately, for each study, undertaking a meta‐analyses across age groups. These summary effect estimates and standard deviations were then combined in a meta‐analysis in RevMan (not shown) as continuous data to provide summary estimates of the change in the proportion caries free for both groups. For each dentition (rather than age group), we then combined the resulting data as a meta‐analysis in the review. Once again we decided to display this data using the average n for the before and after data for each study to give an indication of the size of the studies. Table 5 and Table 6 provide the raw data and summary estimates of the risk differences for each water fluoridation and control group separately, for each study, across age groups.
3. Number of caries‐free children: deciduous teeth.
| Study ID | Age | Fluoridated area | Non/low fluoridated area | ||||||
| Baseline (before/at initiation) | Follow‐up | Baseline | Follow‐up | ||||||
| n | N | n | N | n | N | n | N | ||
| Adriasola 1959a | 3 | 26 | 151 | 82 | 216 | 9 | 77 | 26 | 135 |
| 4 | 12 | 156 | 55 | 216 | 11 | 76 | 11 | 110 | |
| 5 | 4 | 186 | 45 | 340 | 7 | 174 | 14 | 140 | |
| 8 | 21 | 493 | 11 | 458 | 17 | 223 | 2 | 226 | |
| Ast 1951 | 5 | 63 | 274 | 108 | 217 | 73 | 259 | 107 | 324 |
| Beal 1971b | 5 | 62 | 297 | 138 | 314 | 35 | 217 | 55 | 229 |
| Beal 1981 | 5 | 41 | 196 | 78 | 170 | 43 | 205 | 54 | 180 |
| 8 | 18 | 189 | 31 | 167 | 12 | 163 | 18 | 186 | |
| Blinkhorn 2015 | 5‐7 | 397 | 781 | 632 | 844 | 254 | 523 | 412 | 612 |
| DHSS 1969 (Eng) | 3 | 16 | 43 | 96 | 133 | 27 | 44 | 97 | 144 |
| 4 | 23 | 66 | 84 | 131 | 16 | 47 | 89 | 162 | |
| 5 | 12 | 148 | 51 | 111 | 15 | 110 | 42 | 119 | |
| 6 | 16 | 182 | 47 | 130 | 13 | 127 | 18 | 107 | |
| 7 | 13 | 192 | 55 | 172 | 7 | 121 | 24 | 133 | |
| DHSS 1969 (Wales) | 3 | 89 | 310 | 100 | 171 | 39 | 146 | 21 | 105 |
| 4 | 78 | 413 | 114 | 267 | 32 | 210 | 27 | 122 | |
| 5 | 56 | 556 | 90 | 284 | 18 | 256 | 19 | 138 | |
| 6 | 29 | 603 | 78 | 310 | 20 | 331 | 15 | 133 | |
| 7 | 17 | 640 | 53 | 266 | 14 | 346 | 5 | 130 | |
| Gray 2001b | 5 | 1465 | 2462 | 1903 | 2524 | 345 | 466 | 273 | 419 |
| Guo 1984 | 3 | 67 | 202 | 31 | 79 | 54 | 205 | 39 | 128 |
| 4 | 74 | 354 | 39 | 164 | 32 | 246 | 14 | 164 | |
| 5 | 61 | 589 | 47 | 345 | 18 | 218 | 19 | 387 | |
| 6 | 53 | 695 | 56 | 397 | 27 | 309 | 12 | 354 | |
| 7 | 41 | 399 | 21 | 240 | 29 | 335 | 11 | 352 | |
| 8 | 53 | 392 | 24 | 279 | 50 | 343 | 16 | 350 | |
| 8 | 278 | 392 | 204 | 279 | 273 | 343 | 104 | 350 | |
| Kunzel 1997 | 5 | 231 | 688 | 682 | 1306 | 39 | 172 | 192 | 597 |
| 8 | 117 | 2438 | 746 | 3020 | 40 | 777 | 61 | 1078 | |
Note: Only data up to the age of 8 years included for the deciduous dentition
a. Baseline data not available for ages 6 and 7 years
b. Data from all fluoridated areas combined
4. Number of caries‐free children: permanent teeth.
| Study ID | Age | Fluoridated area | Non/low fluoridated area | ||||||
|
B aseline (before/at initiation) |
Follow‐up | Baseline | Follow‐up | ||||||
| n | N | n | N | n | N | n | N | ||
| ADRIASOLA 1959a | 8 | 21 | 493 | 11 | 458 | 17 | 223 | 2 | 226 |
| 12 | 7 | 292 | 8 | 419 | 3 | 197 | 9 | 211 | |
| BEAL 1981 | 8 | 77 | 189 | 115 | 167 | 56 | 163 | 82 | 186 |
| 12 | 51 | 192 | 41 | 189 | 13 | 188 | 14 | 197 | |
| BLINKHORN 2015 | 10 to 12 | 525 | 777 | 486 | 642 | 272 | 436 | 307 | 455 |
| BROWN 1960b | 9 to 11 | 34 | 595 | 220 | 502 | 35 | 571 | 42 | 521 |
| 12 to 14 | 7 | 593 | 94 | 503 | 3 | 486 | 11 | 485 | |
| DHSS 1969 (Eng) | 8 | 40 | 199 | 50 | 95 | 33 | 148 | 29 | 79 |
| 9 | 25 | 227 | 57 | 135 | 20 | 166 | 20 | 95 | |
| 10 | 13 | 134 | 36 | 115 | 14 | 160 | 10 | 80 | |
| 11 | 12 | 145 | 12 | 200 | 3 | 126 | 12 | 122 | |
| 12 | 3 | 111 | 20 | 134 | 0 | 51 | 4 | 99 | |
| 13 | 3 | 91 | 9 | 132 | 2 | 52 | 8 | 127 | |
| 14 | 0 | 70 | 4 | 90 | 2 | 36 | 9 | 180 | |
| DHSS 1969 (Wales) | 8 | 143 | 607 | 112 | 283 | 88 | 351 | 26 | 125 |
| 9 | 73 | 553 | 78 | 260 | 49 | 325 | 15 | 134 | |
| 10 | 63 | 502 | 44 | 241 | 25 | 308 | 8 | 133 | |
| 11 | 30 | 278 | 15 | 126 | 35 | 270 | 0 | 42 | |
| 12 | 15 | 186 | 10 | 108 | 27 | 265 | 2 | 108 | |
| 13 | 7 | 178 | 0 | 93 | 14 | 274 | 1 | 105 | |
| 14 | 8 | 158 | 3 | 93 | 15 | 243 | 1 | 96 | |
| Guo 1984 | 5 | 575 | 589 | 338 | 345 | 214 | 218 | 358 | 387 |
| 6 | 616 | 695 | 266 | 297 | 284 | 309 | 249 | 354 | |
| 7 | 305 | 399 | 189 | 240 | 272 | 335 | 162 | 352 | |
| 8 | 278 | 392 | 204 | 279 | 273 | 343 | 104 | 350 | |
| 9 | 242 | 388 | 167 | 275 | 195 | 310 | 98 | 352 | |
| 10 | 215 | 346 | 161 | 310 | 199 | 323 | 84 | 436 | |
| 11 | 213 | 330 | 133 | 307 | 245 | 451 | 65 | 365 | |
| 12 | 240 | 468 | 90 | 208 | 475 | 841 | 91 | 493 | |
| 13 | 227 | 469 | 88 | 232 | 434 | 801 | 77 | 504 | |
| 14 | 161 | 322 | 69 | 221 | 455 | 795 | 73 | 490 | |
| 15 | 78 | 164 | 11 | 38 | 66 | 121 | 11 | 63 | |
| Kunzel 1997 | 8 | 1021 | 2419 | 2147 | 3016 | 334 | 777 | 333 | 1076 |
| 12 | 120 | 1626 | 801 | 2426 | 42 | 563 | 50 | 925 | |
| 15 | 118 | 1995 | 249 | 1897 | 27 | 744 | 18 | 756 | |
a. Baseline data not available for ages 11 and 15 years
b. Data for 16‐17‐year olds presented but no N
Fluorosis
In line with the previous systematic review (McDonagh 2000), the primary analysis was carried out on data where fluoride exposure was 5 ppm or less, for reasons of applicability and robustness of evidence (the concentration of most naturally occurring fluoride will be below than this threshold, and the paucity of information from higher exposures leads to less precise estimates). We analysed two aspects of fluorosis: aesthetic concerns of fluorosis (as defined in Types of outcome measures), and any level of fluorosis. We used random‐effects models with random intercept and random slope to model the log odds of fluorosis as a function of fluoride exposure. In this model we allowed the intercept and slope to vary from study to study. The slope of the linear relationship between fluoride level (the predictor) and the log odds of fluorosis is the value of the coefficient for fluoride level plus the study specific random effect for that specific study. Fluoride exposure was centred upon the grand mean, and results presented as probabilities to aid interpretation.
Subgroup analysis and investigation of heterogeneity
We undertook subgroup analyses according to whether data were collected prior to the widespread use of fluoride toothpaste, or after: we used a cut‐off of 1975 for this purpose. We made the decision to undertake subgroup analyses by date of study conduct post hoc, following peer review comments.
We had planned to use meta‐regression to investigate and explain sources of heterogeneity among studies where possible (potential confounders of relevance to this review include sugar consumption/dietary habits, SES, ethnicity and the use of other fluoride sources). Dental caries results were to be analysed using meta‐regression in order to assess the impact of potential sources of heterogeneity and estimate the underlying effect of water fluoridation. We also planned to conduct subgroup analyses by study design. However, due to the small number of studies and lack of clarity in the reporting within the caries studies, we did not undertake these sub‐group analyses
Sensitivity analysis
We would have undertaken sensitivity analyses based on risk of bias if sufficient trials had been included. We had planned to undertake further sensitivity analyses to determine if the results of the meta‐analysis were influenced by the timing of baseline measurement, as appropriate. We did undertake sensitivity analyses to determine the effect of the imputed standard deviations.
Presentation of main results
We assessed the quality of the evidence for the primary and secondary outcomes for this review using GRADE methods (gdt.guidelinedevelopment.org). Due to the observational nature of the studies included in the review, GRADE stipulates that the quality of the body of evidence starts at 'low'. We considered susbequent downgrading of the quality of the body of evidence with reference to the overall risk of bias of the included studies, the directness of the evidence, the inconsistency of the results and the precision of the estimates. We considered upgrading the quality of the evidence on the basis of an assessment of the risk of publication bias, the magnitude of the effect and whether or not there was evidence of a dose response.
We presented the results and quality of evidence for each outcome in a 'Summary of findings' table. We made a post hoc decision not to use the GRADE terminology of high, moderate, low and very low to describe the quality of the evidence (see Quality of the evidence).
Results
Description of studies
Results of the search
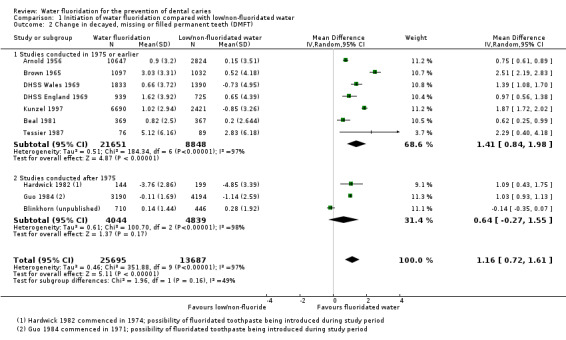
The search for literature produced a total of 4677 records after de‐duplication. Two reviewers in duplicate screened these records independently. Any disagreements were resolved by a third reviewer. After this initial screening, we obtained 158 articles, combined with 120 articles from additional sources (including McDonagh 2000; NHMRC 2007 and an unpublished paper, Blinkhorn (unpublished)) and read them in detail. We assessed 277 of these 278 articles for eligibility; 155 studies (162 publications) met the inclusion criteria for the review. However, only 107 studies (15 caries studies; 92 studies reporting data on either all fluorosis severities or fluorosis of aesthetic concern) presented sufficient data for inclusion in the quantitative syntheses. One study awaits classification. The search, screening results and selection of included studies are illustrated in the PRISMA flow diagram (Figure 1).
1.
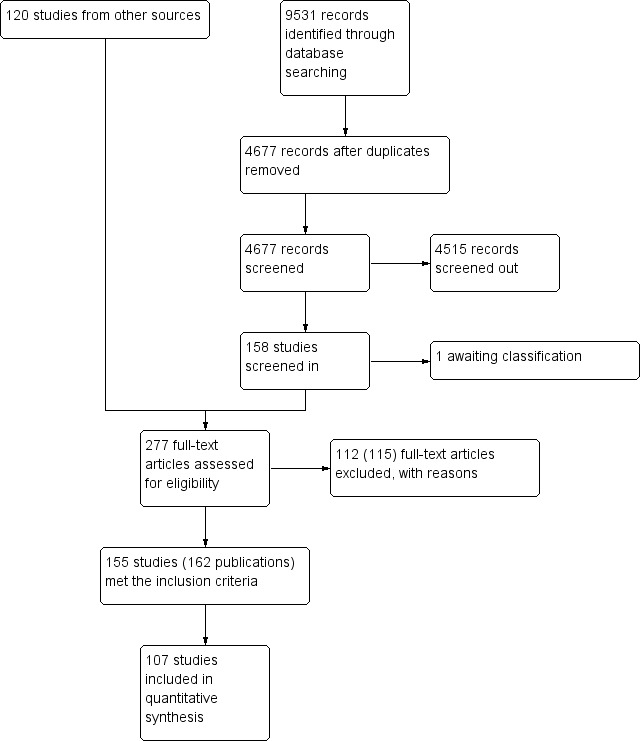
Figure 1. Study flow diagram.
Included studies
A total of 20 prospective observational studies provided data on caries or disparities in caries, or both (Adriasola 1959; Arnold 1956; Ast 1951; Backer‐Dirks 1961; Beal 1971; Beal 1981; Blinkhorn (unpublished); Brown 1965; DHSS England 1969; DHSS Scotland 1969; DHSS Wales 1969; Gray 2001; Guo 1984; Hardwick 1982; Holdcroft 1999; Kunzel 1997; Loh 1996; Maupome 2001; Pot 1974; Tessier 1987).
Caries
Nineteen prospective observational studies (22 publications) published between 1951 and 2015 met the inclusion criteria for the caries outcome. Eighteen of these studies looked at the effect of the initiation of water fluoridation programme on dental caries (Adriasola 1959; Arnold 1956; Ast 1951; Backer‐Dirks 1961; Beal 1971; Beal 1981; Blinkhorn (unpublished); Brown 1965; DHSS England 1969; DHSS Scotland 1969; DHSS Wales 1969; Gray 2001; Guo 1984; Hardwick 1982; Kunzel 1997; Loh 1996; Pot 1974; Tessier 1987), and one study focused on the effect of cessation of fluoridation on caries (Maupome 2001). Only one study followed the same participants over time (Hardwick 1982), evaluating 12‐year old children in a fluoridated and a non‐fluoridated area and following them for four years. All other studies evaluated specific age groups within three years of a change in fluoridation status and undertook a follow‐up evaluation of the same age groups (different children) at at least one other time point. A low/non‐fluoridated area was used as a control. These have been analysed as controlled before‐and‐after studies.
The studies were conducted in multiple centres in Europe (Backer‐Dirks 1961; Beal 1971; Beal 1981; DHSS England 1969; DHSS Scotland 1969; DHSS Wales 1969; Gray 2001; Hardwick 1982; Kunzel 1997; Pot 1974), North America (Arnold 1956; Ast 1951; Brown 1965; Maupome 2001; Tessier 1987), South America (Adriasola 1959), Australia (Blinkhorn (unpublished)) and Asia (Guo 1984; Loh 1996). Five studies were funded by research grants from research organisations, health authorities and government organisations (Beal 1971; Blinkhorn (unpublished); Booth 1991; Kunzel 1997; Maupome 2001), one study was funded in collaboration with members of the committee pro‐fluoridation (Adriasola 1959), while the other studies did not state their funding sources.
Participants, aged from three to 16 years, were mostly recruited from schools; the period of time between baseline and final measurement ranged from two to 12 years.
The intervention groups in all 'fluoride initiation' studies were exposed to naturally low fluoride at baseline and artificially fluoridated water at follow‐up, while the control groups were exposed to naturally low fluoride at both time points. In studies where it was not stated clearly, fluoride concentration was reported as 'high' or 'fluoridated' for the intervention group and 'low' or 'non‐fluoridated' for the control group. For the 'fluoride cessation' study that met our inclusion criteria, the intervention group was exposed to artificially fluoridated water at baseline and naturally low fluoride at follow‐up, while the control group remained artificially fluoridated at both time points.
Measures of dental caries reported were dmft (decayed missing and filled deciduous teeth), DMFT (decayed missing and filled permanent teeth), DMFS (decayed missing and filled surfaces in permanent teeth), and proportion of caries‐free children (deciduous and permanent dentition).
Disparities in caries
Three prospective observational studies (four publications) met the inclusion criteria for disparities in caries but did not provide data suitable for analysis (Beal 1971; Gray 2001; Holdcroft 1999). They all assessed the effect of the initiation of water fluoridation on caries in different SES groups receiving fluoridated and non‐fluoridated water. All three studies evaluated specific age groups within three years of a change in fluoridation status and undertook a follow‐up evaluation of the same age groups (different children) at a least one other time point. A low/non‐fluoridated area was used as a control. All these studies were conducted in the UK. Caries measures reported were decayed, extracted and filled deciduous teeth (deft; Beal 1971), dmft (Gray 2001; Holdcroft 1999), and percentage of caries‐free children (Beal 1971; Gray 2001).
Dental fluorosis
For dental fluorosis, 135 studies were included. These were published between 1941 and 2014. Of these studies, 28% were conducted in Europe, 23% in Asia, 19% in North America, 13% in South America, 10% in Africa, 5% in Australia and 2% in multiple centres in Europe and Asia. Forty‐four studies were supported by research grants from government organisations and health authorities, non‐governmental organisations, research organisations, universities or a combination of these sources (Adair 1999; Alarcon‐Herrera 2001; AlDosari 2010; Angelillo 1999; Awadia 2000; Azcurra 1995; Bao 2007; Butler 1985; Chen 1989; Clark 1993; Correia Sampaio 1999; de Crousaz 1982; Garcia‐Perez 2013; Hernandez‐Montoya 2003; Ibrahim 1995; Indermitte 2007; Indermitte 2009; Kanagaratnam 2009; Kumar 1999; Kumar 2007; Mackay 2005; Mandinic 2010; Milsom 1990; Nanda 1974; Narwaria 2013; Nunn 1992; Pontigo‐Loyola 2008; Ray 1982; Riordan 2002; Ruan 2005; Rwenyonyi 1999; Skinner 2013; Stephen 2002; Szpunar 1988; Tsutsui 2000; Vilasrao 2014; Villa 1998; Vuhahula 2009; Wang 1999; Wang 2012; Warren 2001; Whelton 2004; Whelton 2006; Wondwossen 2004); six studies were funded by: a sugar association (McInnes 1982), a water company (Firempong 2013; Warnakulasuriya 1992), the dental industry (Machiulskiene 2009; Wenzel 1982), or associated with a dental industry through authorship (McGrady 2012). Sources of support were not explicitly stated in 86 studies. One study explicitly stated that no funding had been obtained (Shanthi 2014).
Out of the 135 studies that met the inclusion criteria for fluorosis we aimed to extract cross‐sectional data. Ninety studies reported sufficient data for inclusion in the analysis for all severities of dental fluorosis (Appendix 11). Forty studies were included in the analysis for fluorosis of aesthetic concern (Appendix 11). The remaining studies did not report sufficient data for inclusion in the analysis, typically due to failure to indicate water fluoride concentration of the study areas or reporting inappropriate measure of fluorosis (e.g. mean value or Community Fluorosis Index (CFI)). Where studies reported fluorosis outcomes as CFI only, we could not use the data. The CFI is a composite score calculated by summing the scores of Dean's Index and dividing the total by the sample size. This gives an indication of the experience and severity of fluorosis at a population level, but individual level data cannot be derived from it alone.
Dean's index, TFI, TSIF, DDE were reported in 41%, 19%, 10%, 6% of the included studies, respectively, while 23% of the studies either reported on other indices, specific enamel defects, or did not state the index used at all.
Other adverse effects
Five studies that reported on the dental fluorosis outcome also presented data on other adverse effects associated with water fluoridation (Table 7). The outcomes reported were skeletal fluorosis (Chen 1993; Jolly 1971; Wang 2012), bone fracture (Alarcon‐Herrera 2001), and skeletal maturity (Wenzel 1982). Outcomes were assessed in participants using radiographs (Chen 1993; Jolly 1971; Wenzel 1982), the diagnostic criteria of endemic skeletal fluorosis (WS 192‐2008; Wang 2012), or methods that were not clearly stated (Alarcon‐Herrera 2001).
5. Harms: other.
| Study ID | Outcome | Age | Fluoride level | Assigned F level | Number of subjects | Proportion with outcome |
| Chen 1993 | Skeletal fluorosis | 16 to 65 | 5.5 | 5.5 | 28 | 82.1 |
| 3.1 | 3.1 | 114 | 71.1 | |||
| 0.4 | 0.4 | 50 | 46 | |||
| 3.1 | 3.1 | 50 | 86 | |||
| Wang 2012a | Skeletal fluorosis | ≥16 | 2.2 | 2.2 | 406,298 | 10.8 |
| 0.5 | 0.5 | 188,400 | 4.8 | |||
| Wenzel 1982b | Skeletal maturity | 12 to 14 | 2.4 | 2.4 | 122 | 0.59 (0.1)c |
| < 0.2 | 0.1 | 113 | 0.59 (0.09)c | |||
| Alarcon‐Herrera | Bone fracture | 6 to 12 | < 1.5 | 0.75 | 97 | 5.2 |
| 1.51‐4.99 | 3.25 | 112 | 8.9 | |||
| 5‐8.49 | 6.75 | 38 | 2.6 | |||
| 8.5‐11.99 | 10.25 | 27 | 11.1 | |||
| 12‐16 | 14 | 59 | 8.5 | |||
| 13 to 60 | < 1.5 | 0.75 | 192 | 3.1 | ||
| 1.51‐4.99 | 3.25 | 330 | 7.9 | |||
| 5‐8.49 | 6.75 | 146 | 8.9 | |||
| 8.5‐11.99 | 10.25 | 138 | 7.2 | |||
| 12‐16 | 14 | 96 | 6.3 | |||
| Jolly 1971b | Skeletal fluorosis | Not stated | 0.7 | 0.7 | Not stated | 3.6 |
| 1.4 | 1.4 | Not stated | 2.4 | |||
| 2.4 | 2.4 | Not stated | 17 | |||
| 2.4 | 2.4 | Not stated | 23 | |||
| 2.5 | 2.5 | Not stated | 33 | |||
| 3 | 3 | Not stated | 19.6 | |||
| 3 | 3 | Not stated | 42.2 | |||
| 3.3 | 3.3 | Not stated | 10 | |||
| 3.3 | 3.3 | Not stated | 45 | |||
| 3.6 | 3.6 | Not stated | 33.1 | |||
| 4.3 | 4.3 | Not stated | 19.4 | |||
| 5 | 5 | Not stated | 60 | |||
| 5.1 | 5.1 | Not stated | 44.5 | |||
| 5.5 | 5.5 | Not stated | 31.3 | |||
| 7 | 7 | Not stated | 47.4 | |||
| 8.5 | 8.5 | Not stated | 58.9 | |||
| 9.4 | 9.4 | Not stated | 70.1 |
a. Participants were diagnosed on the basis of diagnostic criteria for endemic skeletal fluorosis (WS 192‐2008)
b. Participants were examined radiologically
c. Reported outcome was mean (standard error) skeletal maturity
Excluded studies
Of the 277 studies that were assessed for eligibility, we excluded 112 studies (115 publications; see Characteristics of excluded studies). The reasons for exclusion were most frequently due to inappropriate study design, including:
absence of data from two time points for one or both study groups (Agarwal 2014; Ajayi 2008; Aldosari 2004; Antunes 2004; Archila 2003; ARCPOH 2008; Armfield 2004; Armfield 2005; Arora 2010; Bailie 2009; Baldani 2002; Baldani 2004; Binbin 2005; Blagojevic 2004; Bradnock 1984; Carmichael 1980; Carmichael 1984; Carmichael 1989; Evans 1995; Gillcrist 2001; Gushi 2005; Han 2011; Jones 1997; Jones 2000a; Jones 2000b; Kirkeskov 2010; Kumar 2001; Lee 2004; Peres 2006; Provart 1995; Rihs 2008; Riley 1999; Rugg‐Gun 1977; Sagheri 2007; Sales‐Peres 2002; Saliba 2008; Sampaio 2000; Slade 2013; Tagliaferro 2004; Tiano 2009; Tickle 2003; Zimmermann 2002);
unsuitable control group (Attwood 1988; Hobbs 1994; Kalsbeek 1993; Seppa 1998; Wragg 1999; Murray 1984; Murray 1991);
absence of concurrent control group (Buscariolo 2006; Kunzel 2000a; Wong 2006).
Risk of bias in included studies
The review authors' judgements about each risk of bias item for each included study is summarised in Figure 2.
2.
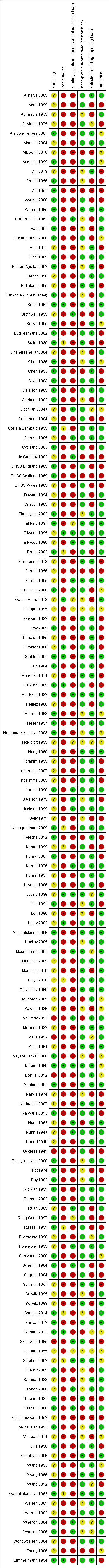
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Caries outcome
We judged that all the 20 studies included for the caries outcome (including disparities in caries) were at high risk of bias overall. The bias may occur in either direction.
Sampling
We judged 13 of the studies as being at low risk of bias in terms of sampling (Arnold 1956; Ast 1951; Backer‐Dirks 1961; Beal 1981; Blinkhorn (unpublished); Brown 1965; DHSS England 1969; DHSS Scotland 1969; Gray 2001; Guo 1984; Hardwick 1982; Pot 1974; Tessier 1987). For these studies, sampling was achieved either randomly or by including the entire eligible population of the study area. We judged seven studies to be at unclear risk of bias for sampling (Adriasola 1959; Beal 1971; DHSS Wales 1969; Holdcroft 1999; Kunzel 1997; Loh 1996; Maupome 2001). This judgement was based on insufficient or unavailable information in most cases, however in the study by Kunzel 1997, there was an unexplained exclusion of disabled children. In the DHSS Scotland 1969 study, different age criteria were used for each group resulting in an imbalance between the groups; the reason for this was not explained. No studies were found to be at high risk for selection bias for this outcome.
Confounding
We found all studies to be at high risk of bias for confounding. We considered confoundng factors for this outcome to be sugar consumption/dietary habits, SES, ethnicity and the use of other fluoride sources. We would have judged studies to be at low risk of confounding bias only if they had successfully controlled for all factors. Six of the studies attempted to control for none of these factors (Adriasola 1959; Ast 1951; Brown 1965; Guo 1984; Loh 1996; Pot 1974). Eight controlled for SES, but not for other sources of fluoride or for dietary habits (Arnold 1956; Backer‐Dirks 1961; Beal 1971; Beal 1981; DHSS England 1969; DHSS Scotland 1969; DHSS Wales 1969; Gray 2001). Hardwick 1982 matched for SES and reported the use of fluoride from other sources to be broadly similar across groups, but did not report on dietary habits. Maupome 2001 reported on dietary habits and the use of fluoride from other sources; this study showed that dietary habits did not confound the relationship between water fluoridation and caries.
Detection bias
The majority of the studies did not blind outcome assessors. This is perhaps unsurprising when considering the efforts that may be required to blind assessors for this type of study. We judged only two studies to be at low risk of bias for this domain (Backer‐Dirks 1961; Hardwick 1982). Backer‐Dirks 1961 utilised radiographs in order to blind assessors, and in the Hardwick 1982 study children were brought to a central examination centre for assessment.
Incomplete outcome data
Eight studies were judged as being at low risk of bias (Beal 1971; Beal 1981; Brown 1965; Gray 2001; Guo 1984; Hardwick 1982; Kunzel 1997; Maupome 2001), or unclear risk of bias for the domain of incomplete outcome data (Adriasola 1959; Arnold 1956; Backer‐Dirks 1961; Beal 1971; Blinkhorn (unpublished); Holdcroft 1999; Loh 1996; Pot 1974). We found four studies to be at high risk. In two studies (Ast 1951; Maupome 2001), the outcome data for participants was substantially lower than at baseline. The Brown 1965 study, which ran from 1948 to 1959, sampled and examined children aged six to eight years up until 1957, but ceased this activity after 1957 as no significant differences were found to exist in that age group. The DHSS Scotland 1969 study did not present data for all children examined.
Selective reporting
We found 11 of the studies to be at high risk of bias for selective reporting. Four studies recorded data on dental fluorosis, but this was not reported (Arnold 1956; DHSS England 1969; DHSS Scotland 1969; DHSS Wales 1969). Six studies did not report standard deviations (Arnold 1956; Blinkhorn (unpublished); DHSS England 1969; DHSS Wales 1969; Kunzel 1997; Tessier 1987), and Adriasola 1959 did not report complete baseline data for the proportion of caries‐free children aged six, seven, 11 and 15 years. Eight studies were found to be at low risk of bias for this domain with all expected data having been reported (Beal 1971; Beal 1981; Brown 1965; Gray 2001; Guo 1984; Hardwick 1982; Kunzel 1997; Maupome 2001). For one study the risk of bias remains unclear (Holdcroft 1999).
Other bias
We found 12 studies to be at high risk of other bias; for ten of these studies this was due to an apparent lack of reliability or consistency of the outcome assessments in terms of either calibration of examiners or tests for inter‐ and intra‐rater reliability (Arnold 1956; Ast 1951; Beal 1971; DHSS England 1969; DHSS Scotland 1969; DHSS Wales 1969; Gray 2001; Guo 1984; Pot 1974; Tessier 1987). In the Gray 2001 study the baseline fluoridation status of the children was determined by the location of the school they attended, which may not have taken into account any children attending schools in fluoridated areas who residede outside those areas. We assessed four studies as being at unclear risk of bias (Beal 1981; Brown 1965; Holdcroft 1999; Maupome 2001). The remaining six studies were not assessed as having any other apparent risk of bias.
Dental fluorosis outcome
Of the 135 studies included for this outcome, we found 131 to be at high risk of bias and four to be at unclear risk overall (Ellwood 1995; Levine 1989; Milsom 1990; Stephen 2002). We judged no studies as being at low risk.
We assessed five studies as being at high risk for sampling bias, 60 as being at low risk of bias and the remainder as 'unclear'. We found the majority of studies (114) to be at high risk for confounding; we assessed 11 as being at low risk of bias for this domain. For detection bias, we assessed 103 as being at high risk of detection bias, and 15 at low risk of bias. Overall, we found studies to be at low risk of bias for incomplete outcome data (92), with only 12 assessed as being at high risk of bias. For selective reporting, we assessed 42 as being at high risk of bias, with 82 at low risk of bias. With regard to other bias, we assessed 48 studies as being at high risk, 66 at low risk and all others at unclear risk. In most cases the reason for studies having high risk of other bias was that they did not report on the reliability or consistency of the outcome assessments.
Effects of interventions
Caries
Nineteen studies met the inclusion criteria (18 fluoride initiation studies and one fluoride cessation studies), with 15 providing sufficient data for analysis of caries levels following a change in fluoridation status. Only one of these studies examined the effect of water fluoridation on adults (Pot 1974); the reported outcome for this study was the percentage of participants with dentures. There are no data to determine the effect of water fluoridation on caries levels in adults.
Four studies provided insufficient data for analysis (Backer‐Dirks 1961; DHSS Scotland 1969; Loh 1996; Pot 1974).
Initiation of water fluoridation
The caries studies are presented in forest plots, sub‐grouped according to when they were conducted (those conducted in 1975 or before, and those conducted after 1975; Figure 3; Figure 4; Figure 5; Figure 6). Given the limited data post‐1975 and this being a post‐hoc analysis, the results presented below are for the overall body of evidence for each outcome.
3.

Initiation of water fluoridation compared with low/non‐fluoridated water: change in dmft
4.
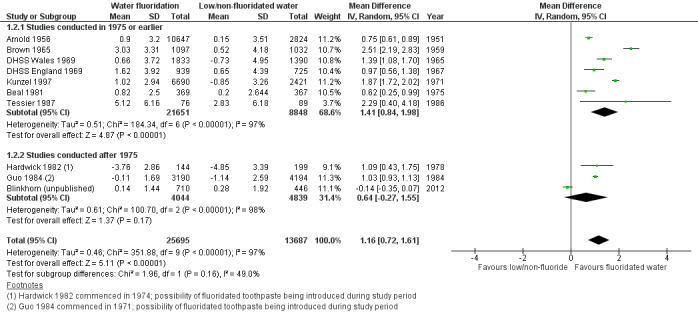
Initiation of water fluoridation compared with low/non‐fluoridated water: change in DMFT
5.
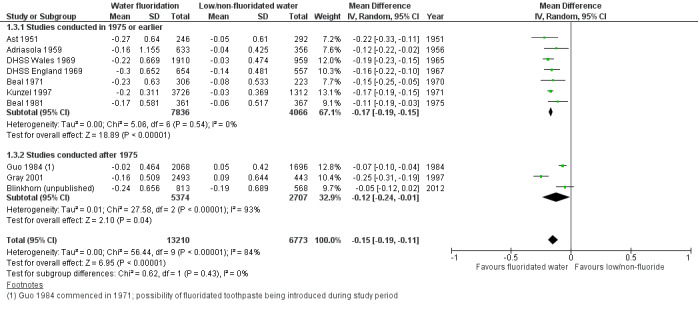
Initiation of water fluoridation compared with low/non‐fluoridated water: change in proportion of caries‐free children (deciduous teeth)
6.
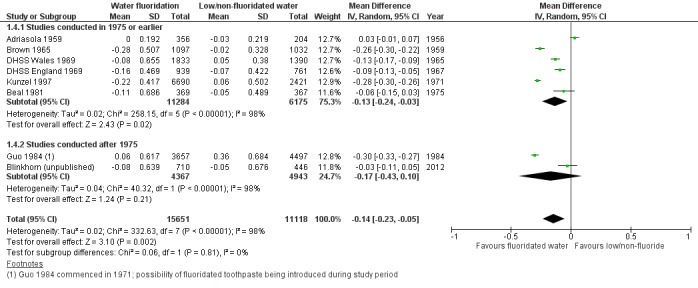
Initiation of water fluoridation compared with low/non‐fluoridated water: change in proportion of caries‐free children (permanent teeth)
Change in dmft/dmfs
Nine studies, with data from 44,268 participants, provided data for dmft (Adriasola 1959; Arnold 1956; Beal 1971; Beal 1981; Blinkhorn (unpublished); DHSS England 1969; DHSS Wales 1969; Guo 1984; Kunzel 1997). We judged all studies to be at high risk of bias and only two (22%) studies were conducted post‐1975. Data collection following initiation of water fluoridation ranged from two to 12 years. Data did not allow for an evaluation of effect by duration of exposure to fluoridated water.
The mean difference in change in dmft was 1.81 (95% CI 1.31 to 2.31; P value < 0.00001; Figure 3). At final assessment, the dmft means for the control groups ranged from 1.21 to 7.8, with a median of 5.1. A mean reduction of 1.81 indicates a 35% reduction in dmft in the water fluoridation groups over and above that for the control groups. Although there was considerable heterogeneity (P value < 0.00001; I² = 91%), we decided to pool the data as all the mean difference estimates were in the same direction. Some of the heterogeneity is expected due to the large size of the studies ensuring narrow confidence intervals.
Sensitivity analysis, excluding studies with imputed standard deviations gave rise to a similar effect estimate, mean difference in change score 1.83 (95% CI 0.68 to 2.98; 5 studies).
There were no data for dmfs.
Change in DMFT/DMFS
Ten studies, with data from 78,764 participants, provided data for DMFT (Arnold 1956; Beal 1981; Blinkhorn (unpublished); Brown 1965; DHSS England 1969; DHSS Wales 1969; Guo 1984; Hardwick 1982; Kunzel 1997; Tessier 1987). We judged all the studies to be at high risk of bias and only three studies (30%) were conducted post‐1975. Data collection following initiation of water fluoridation ranged from two to 11 years. Data did not allow for an evaluation of effect by duration of exposure to fluoridated water.
The mean difference in change in DMFT was 1.16 (95% CI 0.72 to 1.61; P value < 0.00001;Figure 4). At final assessment, the DMFT means for the control groups ranged from 0.71 to 5.5, with a median of 4.4. A mean reduction of 1.16 indicates a 26% reduction in DMFT in the water fluoridation groups over and above that for the control groups. It should be noted that in Guo 1984 the before mean DMFT values for both the control and water fluoridation groups were low at 0.8, and this increased in both groups, however the increase was greater for the control group. This explains why the changes are both negative. The data for Hardwick 1982 are mean DMFT increment data for both groups from the paper, following the same children over time. A lower increment was observed for the water fluoridation group and, as they are caries increments, they have been entered as negative values.
Although there was considerable heterogeneity (P value < 0.00001; I² = 97%), once again we decided to pool the data as all but one of the mean difference estimates were in the same direction (ranging from ‐0.14 to 2.51). Some of the heterogeneity is expected due to the large numbers in the studies ensuring narrow confidence intervals.
Sensitivity analysis in which we excluded studies with imputed standard deviations gave rise to a slightly larger effect estimate; mean difference in change score 1.32 (95% CI 0.53 to 2.11; 4 studies).
Only one study, with data from 343 participants, presented data on DMFS (Hardwick 1982). The study presented increment data for both groups, with a lower increment being observed for the water fluoridation group; mean difference 2.46 (95% CI 1.11 to 3.81).
Change in proportion of children caries free: deciduous dentition
Ten studies, with data from 39,966 children, provided data for the proportion of caries‐free children for deciduous dentition (Adriasola 1959; Ast 1951; Beal 1971; Beal 1981; Blinkhorn (unpublished); DHSS England 1969; DHSS Wales 1969; Gray 2001; Guo 1984; Kunzel 1997). We judged all studies to be at high risk of bias. Three studies (30%) were published post‐1975. For all studies combined, there was a 0.15 absolute increase in the proportion of caries‐free children in fluoridated areas with mean difference 0.15 (95% CI 0.11 to 0.19; Figure 5). At final assessment, the proportion of caries‐free children in the low/non‐fluoridated areas ranged from 0.06 to 0.67, with a median of 0.22; an increase of 0.15 in the proportion of caries‐free children could be considered substantial. There was considerable heterogeneity (P value < 0.00001; I² = 84%), but the value of Tau² from the random‐effects analysis was low (< 0.001; mean differences ranged from 0.05 to 0.25). Therefore we decided to pool the data.
Change in proportion of children caries free: permanent dentition
Eight studies, with data from 53,538 participants, provided data for the proportion of caries‐free children for permanent dentition (Adriasola 1959; Beal 1981; Blinkhorn (unpublished); Brown 1965; DHSS England 1969; DHSS Wales 1969; Guo 1984; Kunzel 1997). We judged all studies to be at high risk of bias and only two (25%) were conducted post‐1975. There was a 0.14 absolute increase in the proportion of caries‐free children in fluoridated areas with mean difference 0.14 (95% CI 0.05 to 0.23; Figure 6). At final assessment, the proportion of caries‐free children in the low/non‐fluoridated areas ranged from 0.01 to 0.67, with a median of 0.14; the increase of 0.14 doubles this. There was considerable heterogeneity (P value < 0.00001; I² = 98%), but the value of Tau from the random‐effects analysis was low at 0.02 (mean differences ranged from ‐0.03 to 0.30). Therefore we decided to pool the data.
Other caries measures
We did not include four studies that met the inclusion criteria in the quantitative analysis (Backer‐Dirks 1961; DHSS Scotland 1969; Loh 1996; Pot 1974). We judged all studies to be at high risk of bias and excluded them from the analysis due to insufficient data (e.g. no data on number of participants evaluated) or different measures of caries, or both. The Backer‐Dirks 1961 study reported dentinal approximal lesions as the caries measure, while Pot 1974 reported the percentage with false teeth. The other two studies did not report on the number of participants (DHSS Scotland 1969; Loh 1996). Three of the studies assessing children between the ages of four and 15 years showed a reduction in caries following the initiation of water fluoridation (Backer‐Dirks 1961; DHSS Scotland 1969; Loh 1996). Pot 1974 assessed participants between five and 55 years of age and showed an increase in percentage with dentures following fluoridation.
Cessation of water fluoridation
Change in DMFT/DMFS
Only one study, at high risk of bias, presented data on DMFS: the Maupome 2001 fluoride cessation study was conducted over three years. The study was conducted in a population with "generally low caries experience, living in an affluent setting with widely accessible dental services". The results did not demonstrate an increase in caries in the children in the fluoride‐ended group compared with the still‐fluoridated group, in fact there was a statistically significant decrease in caries severity (including incipient and cavitated lesions) for the fluoride‐ended group, which was not found in the still‐fluoridated group, for both of the age groups examined. A complex pattern of disease was found when different caries indices were examined.
No studies that met the inclusion criteria reported on change in dmft or proportion of caries‐free children (deciduous/permanent dentition) following the cessation of water fluoridation.
Disparities across social class
Three included studies' reported on the effect of water fluoridation on disparities in caries across social class (Beal 1971; Gray 2001; Holdcroft 1999; Table 8). The number of participants was reported in only two of the studies (Beal 1971; Gray 2001). The total number of participants measured for caries in these studies was 35,399. The studies focused on the initiation of water fluoridation in study areas that were reasonably comparable. Measures of caries reported in the studies were dmft, deft and percentage caries‐free subjects. All three studies were judged to be at high risk of bias.
6. Disparities in caries across social class.
| Study ID | Age | Group | Measure | Social class | Baseline | Final | ||||||
| F level | N | % caries free | dmft (SD) | F level | N | % caries free | dmft (SD) | |||||
| Beal 1971a | 5 | Balsall Heath | Descriptive | Poor area | Low | 115 | 9 | 5.16 (0.44) | 1 | 132 | 48 | 1.94 (0.22) |
| Northfield | Industrial area | Low | 182 | 29 | 4.91 (0.36) | 1 | 182 | 41 | 2.45 (0.24) | |||
| Dudley | Industrial area | < 0.1 | 217 | 16 | 4.97 (0.28) | < 0.1 | 229 | 24 | 5.09 (0.32) | |||
| Gray 2000b | 5 | South east Staffordshire | Jarman score | ‐23.09 | Low | 3435 | 66 | 1.21 (0.59) | 1 | 3120 | 75 | 0.64 (1.46) |
| Sandwell | 18.1 | Low | 3950 | 51 | 1.93 (2.88) | 1 | 3598 | 69 | 0.83 (1.68) | |||
| Walsall | 1.67 | Low | 3120 | 54 | 1.85 (2.31) | 1 | 363 | 67 | 0.94 (1.77) | |||
| Dudley | ‐13.68 | Low | 3657 | 58 | 1.6 (2.54) | 1 | 3474 | 73 | 0.78 (1.75) | |||
| North Birmingham | 21.57 | Low | 1965 | 72 | 0.88 (1.97) | 1 | 1904 | 74 | 0.71 (1.65) | |||
| North Staffordshire | ‐3.59 | Low | 464 | 47 | 2.24 (3.04) | Low | 1947 | 59 | 1.49 (2.46) | |||
| Herefordshire | ‐13.01 | Low | 406 | 57 | 1.61 (2.55) | Low | 305 | 50 | 1.79 (2.68) | |||
| Shropshire | ‐12.34 | Low | 366 | 61 | 1.29 (2.22) | Low | 311 | 60 | 1.33 (2.33) | |||
| Kidderminster | ‐13.13 | Low | 904 | 58 | 1.74 (2.81) | Low | 1053 | 61 | 1.4 (2.52) | |||
| Holdcroft 1999b | Not stated | North Birmingham | Jarman score | ‐7.85 | Not stated | Not stated | 2.18 | High | Not stated | 0.68 | ||
| Sandwell | 15.03 | Not stated | Not stated | 2.55 | High | Not stated | 1.13 | |||||
| North Staffordshire | ‐4.07 | Not stated | Not stated | 2.24 | Not stated | Not stated | 1.48 | |||||
| Shropshire | ‐11.73 | Not stated | Not stated | 1.76 | Not stated | Not stated | 1.29 | |||||
| Herefordshire | ‐11.97 | Not stated | Not stated | 2.56 | Not stated | Not stated | 1.53 | |||||
a. Caries data reported as deft (SE)
b. Caries data reported as dmft (SD)
Beal 1971 studied three areas, in two of which water fluoridation was initiated (one classed as 'poor' and the other 'industrial'). The control group was classed as 'industrial'. Given the lack of a validated measure of deprivation, and without knowing the composition of the groups under comparison, it is not possible to draw conclusions from this study.
Holdcroft 1999 and Gray 2001 both used the Jarman score (an index to measure socioeconomic variation across small geographical areas, originally developed as a measure of General Practice workload; a positive score equates to deprivation). The Holdcroft 1999 study contained insufficient information about fluoride levels at baseline or follow‐up and the number of participants measured at each time point was unclear. In both studies the Jarman scores at baseline for the control (non‐fluoridated areas) were all less than zero. The Jarman scores at baseline in the fluoridated areas ranged from ‐7.85 to 15.03 in the Holdcroft 1999 study, and from ‐23.09 to 21.57 in the Gray 2001 study.
Given the reasons above we are unable to draw robust conclusions about the initiation of water fluoridation and its effect on disparities in caries across social class.
Dental fluorosis
Aesthetic concern
Fluoride levels of 5 ppm or less
We included 40 studies, at high risk of bias, that reported data from 59,630 participants in the analysis of dental fluorosis of aesthetic concern. The reported fluoride exposure ranged from 0 to 4.9 ppm with a mean of 0.80 ppm (SD 0.90).
In order to assess the assumption of linearity we plotted the log odds of the prevalence of dental fluorosis with fluoride level and with log of fluoride level (not shown). A positive linear relationship could be assumed in both cases, indicating that as fluoride levels increase so does the prevalence of dental fluorosis. The reported fluoride level was used as a predictor rather than the log of reported fluoride exposure. This was then centred by taking away the grand mean (0.80) from the reported fluoride level.
Caterpillar plots (not shown) of the residuals for slope and intercept indicated that many of the studies differed significantly from the average (random effects at zero) at the 0.05 level of significance. The effect of fluoride exposure was positive and statistically significant; a higher prevalence of dental fluorosis is associated with increased fluoride exposure (OR 2.90, 95% CI 2.05 to 4.10). When controlling for study effects, we would expect the odds of dental fluorosis to increase by a factor of 2.90 for each one unit increase in fluoride exposure.
The random intercept and random slope model indicated that the effect of fluoride exposure differed across studies. The statistically significant negative covariance of ‐0.82 implies that studies with a higher than average probability of dental fluorosis tend to have a more shallow slope.
The results presented so far have been based on study‐specific values. This is indicated in the following graphic, where the random effects of intercept and slope are set to zero, in effect the plotted prevalence of dental fluorosis in an 'average' study. An alternative approach is to calculate the prevalence of dental fluorosis in all studies combined, to obtain the marginal probability of dental fluorosis. The study‐specific values indicate the probability of dental fluorosis in terms of 'any given participant' whereas the marginal probabilities indicate the probability of dental fluorosis 'among the participants' (Figure 7).
7.
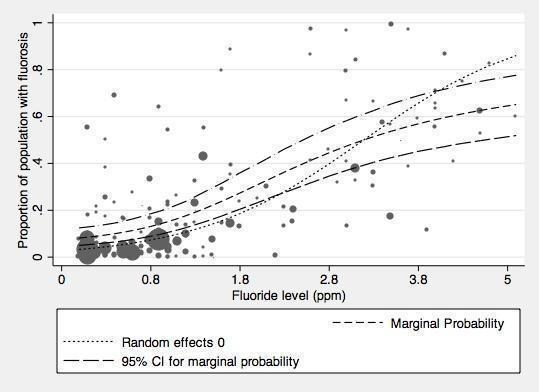
Proportion of the population with dental fluorosis of aesthetic concern by water fluoride level together with 95% confidence limits for the proportion (studies reporting up to and including 5ppm).
The marginal probabilities of dental fluorosis of aesthetic concern at different fluoride levels are given below.
| Fluoride exposure (ppm) | Probability of dental fluorosis of aesthetic concern (95% CI) |
| 0.1 | 0.08 (0.05 to 0.12) |
| 0.2 | 0.09 (0.06 to 0.13) |
| 0.4 | 0.10 (0.06 to 0.15) |
| 0.7 | 0.12 (0.08 to 0.17) |
| 1 | 0.15 (0.11 to 0.21) |
| 1.2 | 0.18 (0.13 to 0.24) |
| 2 | 0.31 (0.23 to 0.40) |
| 4 | 0.59 (0.46 to 0.71) |
All fluoride levels
The analysis of dental fluorosis of aesthetic concern at all reported fluoride exposure was based on 60,030 observations from 40 studies. The reported fluoride levels ranged from 0 to 7.6 ppm with a mean of 0.85 ppm (SD 1.03).There was very little difference in the results from the analysis restricted to 5 ppm or less. The effect of fluoride exposure is positive and statistically significant; a higher prevalence of dental fluorosis is associated with increased fluoride exposure (OR 2.84, 95% CI 2.00 to 4.03). When controlling for study effects, we would expect the odds of dental fluorosis to increase by a factor of 2.84 for each one unit increase in fluoride level (1 ppm F).
Any dental fluorosis
Fluoride levels of 5 ppm or less
We included 90 studies, at high risk of bias, that reported data from 180,530 participants in this analysis. The reported fluoride levels in the studies ranged from 0 to 5 ppm, with a mean of 1.22 ppm (SD 0.92). When restricted to studies reporting fluoride exposure of 5 ppm or less, there is a clearer positive relationship between the proportion of children with dental fluorosis and fluoride level.
The relationship between the log odds of dental fluorosis and fluoride level and log fluoride level were both approximately linear. Consequently the reported fluoride exposure was used as a predictor rather than the log of reported fluoride exposure. This was then centred by taking away the grand mean (1.22) from the reported fluoride exposure level.
The effect of fluoride exposure is positive and statistically significant; a higher prevalence of dental fluorosis is associated with increased fluoride exposure (OR 3.60, 95% CI 2.86 to 4.53). Controlling for study effects, we would expect the odds of dental fluorosis to increase by a factor of 3.60 for each one unit increase in fluoride exposure (1 ppm F).
The random intercept and random slope model indicated that the effect of fluoride exposure differed across studies. The statistically significant negative covariance of ‐1.05 implies that studies with a higher than average probability of dental fluorosis tend to have a more shallow slope.
The results presented so far have been based on study‐specific values. This is indicated in the following graph, where the random effects of intercept and slope are set to zero, in effect the plotted prevalence of dental fluorosis in an 'average' study
(Figure 8).
8.
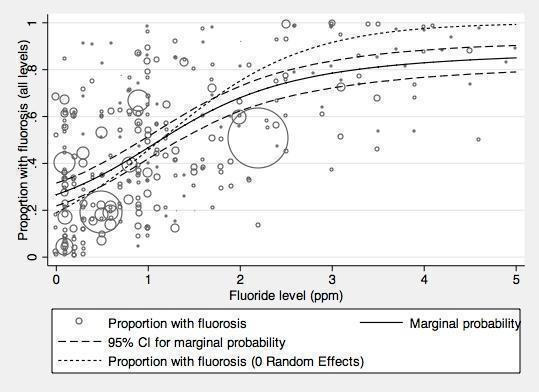
Proportion of the population with dental fluorosis of any level by water fluoride level together with 95% confidence limits for the proportion (studies reporting up to and including 5ppm F)
The marginal probabilities of any dental fluorosis are presented in the table below.
| Fluoride exposure (ppm) | Probability of any dental fluorosis (95% CI) |
| 0.1 | 0.28 (0.23 to 0.33) |
| 0.2 | 0.30 (0.25 to 0.34) |
| 0.4 | 0.33 (0.28 to 0.38) |
| 0.7 | 0.40 (0.35 to 0.44) |
| 1 | 0.47 (0.42 to 0.52) |
| 1.2 | 0.52 (0.47 to 0.56) |
| 2 | 0.68 (0.62 to 0.73) |
| 4 | 0.83 (0.77 to 0.88) |
All fluoride levels
We included 90 studies that reported data from 182,233 participants in this analysis. The reported fluoride levels ranged from 0 to 14 ppm with a mean fluoride level of 1.28 ppm (SD 1.11). There was little change in the pooled estimates when all fluoride levels were included in the analysis. The effect of fluoride exposure is positive and statistically significant; a higher prevalence of dental fluorosis is associated with increased fluoride exposure (OR 3.13, 95% CI 2.55 to 3.85). When controlling for study effects, we would expect the odds of dental fluorosis to increase by a factor of 3.13 for each one unit increase in fluoride exposure (1 ppm F).
The statistically significant negative covariance of ‐0.87 implies that studies with a higher than average probability of dental fluorosis tend to have a shallower slope. The between study variance increases as fluoride level increases.
Post hoc analysis
We used a multivariate analysis to investigate possible sources of heterogeneity in the model. We explored the effects of source of fluoride and its interaction with fluoride concentration by including them as fixed covariates in the models above. Source of fluoride was classed as natural or artificial. We excluded studies that reported mixed sources of fluoridation, or where the source of fluoridation was not reported, from the analysis. This analysis was carried out separately for the outcomes of fluorosis and fluorosis of aesthetic concern, and for studies reporting fluoride concentrations at any level and restricted to 5 ppm or less. The results from the models with the additional covariates and the ones containing fluoride concentration only as a covariate are not directly comparable, as the additional covariate analyses included fewer studies due to missing data (source of fluoride). For fluorosis of aesthetic concern at all concentrations, fluoride concentration and source of fluoride explain a proportion of the variation between estimates, whereas the interaction between these estimates does not (the OR for fluorosis due to fluoridation becomes 3.16 (95% CI 2.12 to 4.71) when controlling for source of fluoride (OR 0.25, 95% CI 0.09 to 0.70) and interaction (OR 1.89, 95% CI 0.74 to 4.82). The conclusions are the same for fluorosis of aesthetic concern at fluoride concentrations of 5 ppm or less (the OR for fluorosis due to fluoridation becomes 3.22 (95% CI 2.16 to 4.79) when controlling for source of fluoride (OR 0.25, 95% CI 0.10 to 0.70) and interaction (OR 1.82, 95% CI 0.71 to 4.62)). For the outcome of fluorosis at all levels, the additional covariates do not contribute significantly to the model.
Other dental fluorosis studies
Approximately one third of the dental fluorosis studies that met the review's inclusion criteria did not report data in a way that allowed for further analysis (Appendix 11).
Other adverse effects reported in the included studies
Five studies that reported on dental fluorosis also presented data on the association of water fluoridation with skeletal fluorosis (Chen 1993; Jolly 1971; Wang 2012), bone fracture (Alarcon‐Herrera 2001), and skeletal maturity (Wenzel 1982), in participants between the ages of six and over 66 years. Four of the studies included a total of 596,410 participants (Alarcon‐Herrera 2001; Chen 1993; Wang 2012; Wenzel 1982), and fluoride concentration in all four studies ranged from less than 0.2 ppm to 14 ppm. The studies were all at high risk of bias and we did not analyse their results further (Table 7).
Discussion
Summary of main results
Of the 155 studies that met the inclusion criteria, 107 studies provided sufficient data for quantitative synthesis. Fourteen studies provided adequate data for the assessment of the effect of the initiation of a water fluoridation programme on dental caries, one study focused on the effect of the cessation of water fluoridation. Although three studies evaluated disparities in dental caries across social class, no data were suitable for further analysis. Ninety studies provided sufficient data for inclusion in the analysis of dental fluorosis of any level (40 in the analysis of dental fluorosis of aesthetic concern).
Our confidence in the size of the effect estimates obtained for the prevention of caries is limited (see Quality of the evidence and Table 1; Table 2 ).
The results from the caries severity data indicate that the initiation of water fluoridation results in reductions in the order of 1.8 dmft and 1.2 DMFT for deciduous and permanent dentitions. This translates to reductions of 35% and 26% compared to the median control group mean values. In addition, there was an increase in the percentage of children who were caries free (15% increase when evaluating deciduous dentition and 14% in the permanent dentition).
There is insufficient information to determine whether initiation of a water fluoridation programme results in a change in disparities in caries levels across SES.
There is insufficient information to determine the effect of stopping water fluoridation programmes on caries levels.
There were no studies that met the review's inclusion criteria that investigated the effectiveness of water fluoridation for preventing caries in adults.
With regard to dental fluorosis, the percentage of participants with dental fluorosis of aesthetic concern was estimated to be approximately 12% for a fluoride level of 0.7 ppm. This increases to 40% when considering dental fluorosis of any level, however, this includes fluorosis that can only be detected under very controlled, clinical conditions and other enamel defects.
Adverse effects, other than dental fluorosis, were rarely reported in the included studies.
Overall completeness and applicability of evidence
The applicability of the evidence on water fluoridation to today’s societies is unclear and highly likely to vary according to setting.
The evidence included in the review pertains to caries in children only. Only one study, that met the review's inclusion criteria, examined the effect of water fluoridation on adults (Pot 1974); the reported outcome for this study was the percentage of participants with dentures. There are no data to determine the effect of water fluoridation on caries levels in adults. Research, utilising data from 26 countries, indicates that dental caries levels in permanent dentition in adults are significantly higher than in children (Bernabe 2014). It has been suggested that greater attention needs to be directed at preventing caries at all stages of life, not just childhood.
Approximately 71% of the included caries studies that evaluated the initiation of water fluoridation were conducted prior to 1975.
In developed countries, the widespread use of fluoride toothpastes from the mid to late 1970s, along with increased access to other caries‐preventive strategies of proven effectiveness, such as fluoride varnishes (Marinho 2013), and dental sealants (Ahovuo‐Saloranta 2013), may mean that the benefit of water fluoridation is reduced in such populations. However, the Marinho 2003a review evaluated the effect of topical fluorides for preventing dental caries in children and adolescents, and found no evidence that the effect of topical fluoride was dependent on background exposure to other fluoride sources. The reviewers did find evidence that the relative effect of topical fluoride may be greater in those who have higher baseline levels of caries.
Globally, caries levels have been reducing. In 1980 the global DMFT for 12 year olds was estimated to be 2.43 (Leclercq 1987). In 2011, this global estimate had reduced to 1.67 DMFT (although there is variation by World Health Organisation region; Table 9). Within the studies included in the review, the mean values for DMFT at follow‐up in the non‐fluoridated areas were higher, ranging from 0.7 to 5.5.
7. WHO region‐specific weighted DMFT among 12‐year olds.
| WHO regions | DMFT |
| 2011 | |
| Africa | 1.19 |
| Americas | 2.35 |
| Eastern Mediteranean | 1.63 |
| Europe | 1.95 |
| South East Asia | 1.87 |
| Western Pacific | 1.39 |
| GLOBAL | 1.67 |
http://www.mah.se/CAPP/Country‐Oral‐Health‐Profiles/According‐to‐Alphabetical/Global‐DMFT‐for‐12‐year‐olds‐2011/
Figure 9 shows global dental caries levels (DMFT) among 12 year olds. Out of the 189 countries that provided data, 148 (78%) have a DMFT of 3 or less. Areas where a large percentage of the population (more than 60%) receive fluoridated water (either natural or artificial fluoridation) include: North America, Australasia, parts of South America (namely Brazil, Columbia and Chile), the Republic of Ireland, and Malaysia. Whilst these areas tend to have low to very low DMFT (Figure 9), there are many other parts of the world where fluoridated water is not widespread that also have low caries levels. Equally, there are areas with relatively high distribution of water fluoridation and moderate caries levels (e.g. Brazil).
9.
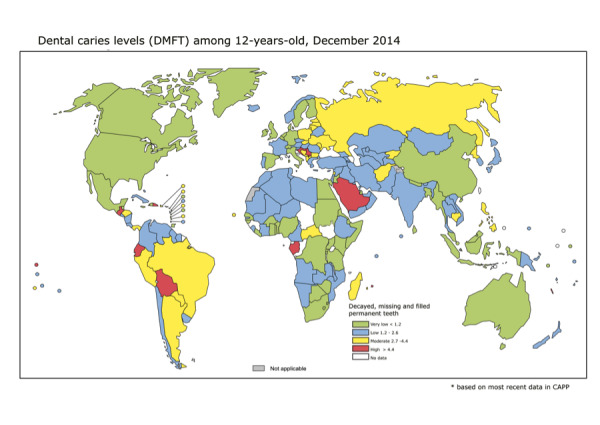
Source:CAPP database, 2015
The applicability of the evidence around water fluoridation has to be considered in the context of reductions in caries levels over time, the uptake of other strategies proven to prevent caries, and global changes in patterns of food consumption (Kearney 2010). Annual sugar consumption, specifically, has risen dramatically since the start of the 20th century when it was approximately 5.1 kg per capita. The consumption of sugar continues to rise with the average sugar consumption now estimated at 23 kg per capita; the greatest rates of growth are currently seen in Asia, the Middle East and Africa (SucDen 2015). In addition, in many parts of the world more industrially processed foods are consumed, with less food being prepared and cooked in the home using locally sourced water (Slimani 2009). Variation in fluoride concentrations in water across regions and countries, and the increase in processed foods and beverages and their transportation, make it difficult to assess dietary fluoride intake. Such changes may mean that, although the tap water is fluoridated in a particular area, some members of the population do not consume a sufficient volume, either through beverages or foods prepared with tap water, to provide a benefit to their oral health.
Ten of the 14 studies used in the analysis of water fluoridation initiation schemes included lifetime residents only. Whilst this is a valid approach it evaluates the absolute effect rather than the benefit to the whole population. The effect size shown in the review may, therefore, be larger than that found in the population, depending on population movement/migration.
There was limited reporting of adverse effects, other than dental fluorosis, in the included studies. The broader literature speculates about harms associated with higher levels of fluoride in water (e.g. cancer, lowered intelligence, endocrine dysfunction), however, there has been insufficient evidence to draw conclusions (MRC 2002).
Quality of the evidence
The GRADE approach was used to assess the quality of the evidence within the review. GRADE has developed over recent years as an internationally recognised framework for systematically evaluating the quality of evidence within both systematic reviews and guidelines. It aims to overcome the confusion that arises from having multiple systems for grading evidence and recommendations, and, because of this key aim, the GRADE working group discourages the use of modified GRADE approaches. However, there has been much debate around the appropriateness of GRADE when applied to public health interventions, particularly for research questions where evidence from randomised controlled trials is never going to be available due to the unfeasibility of conducting such trials. Community water fluoridation is one such area.
When applying GRADE to non‐randomised studies, the quality of the evidence automatically starts at 'low', as opposed to 'high' for RCTs. There has been some criticism of GRADE with regard to its inability to discriminate between stronger and weaker observational designs (Rehfuess 2013). It has been proposed that certain designs, such as quasi‐experimental designs and interrupted‐time‐series studies should begin at 'moderate' quality. Indeed, WHO have previously employed such a modified approach (Bruce 2014). Others suggest that starting non‐randomised studies at 'low' simply acknowledges our reduced certainty that observed effects are actually due to the intervention itself. With regard to the current review, using a modified approach to differentiate between stronger and weaker study designs would have no impact on the overall quality assessment as the study designs would still not merit commencing at 'moderate'.
Another concern about applying GRADE is the limited possibilities for 'upgrading' the quality of evidence from observational studies. Modified approaches to GRADE have incorporated the option to upgrade for consistency in findings (Bruce 2014). Within the current review, it was not felt appropriate to upgrade for consistency as there was statistically significant heterogeneity present in all four caries analyses. However, given that the direction of effect was the same for all but one of the outcomes in one of the studies, we have not downgraded with regard to inconsistency.
In our review protocol we stated that we would produce a 'Summary of findings' table, applying the GRADE criteria. We have attempted to be transparent in our decisions regarding the downgrading/upgrading of the quality of the evidence, and feel our decisions are justified. The quality of the evidence, when GRADE criteria are applied, is judged to be low. However, we accept that the terminology of 'low quality’ for evidence may appear too judgmental. We acknowledge that studies on water fluoridation, as for many public health interventions, are complex to undertake and that researchers are often constrained in their study design by practical considerations. For many public health interventions, the GRADE framework will always result in a rating of low or very low quality. Decision makers need to recognise that for some areas of research, the quality of the evidence will never be 'high' and that, as for any intervention, the recommendation for its use depends not just upon the quality of the evidence but also on factors such as acceptability and cost‐effectiveness (Burford 2012). In order to overcome some of the concerns around the use of GRADE within this review, a decision was made to omit the GRADE terminology of 'low quality' and discuss the findings in terms of our confidence in the results.
With regard to the caries outcomes, all included studies were observational and our confidence in the effect estimate is limited. We downgraded the quality of the evidence due to an overall high risk of bias in the included studies (excluding domains associated with randomisation, allocation concealment, blinding of participants). The main areas of concern were confounding and lack of blind outcome assessment. The evidence was additionally downgraded for indirectness due to the fact that about 71% of the caries studies that evaluated the initiation of water fluoridation were conducted prior to 1975 (Overall completeness and applicability of evidence). Present day reductions in caries may be of a smaller magnitude in developed countries. Also, there were no included studies evaluating caries levels in adults. There was statistically significant heterogeneity present in all four caries analyses (Analysis 1.1; Analysis 1.2; Analysis 1.3; Analysis 1.4), with I² statistics of 84% or more. However, given that the direction of effect was the same for all but one of the outcomes in one of the studies, we have not downgraded with regard to inconsistency. The study showing an effect in the opposite direction was the most recently conducted study, with low baseline caries levels, and, as yet, the shortest duration of follow‐up (Blinkhorn (unpublished)); both these factors could influence the effect estimate. It is also possible, given the widespread coverage of fluoridated water in Australia, that the low baseline caries reflects diffusion of fluoride from other areas through commercial foods and beverages.
1.3. Analysis.
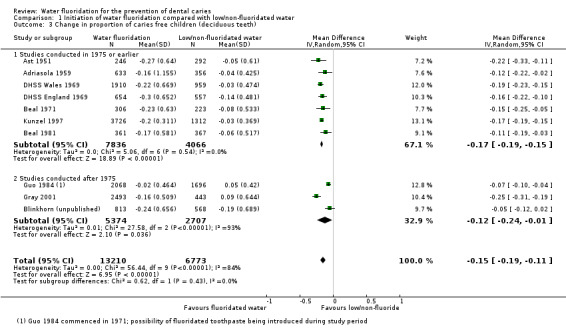
Comparison 1 Initiation of water fluoridation compared with low/non‐fluoridated water, Outcome 3 Change in proportion of caries free children (deciduous teeth).
1.4. Analysis.
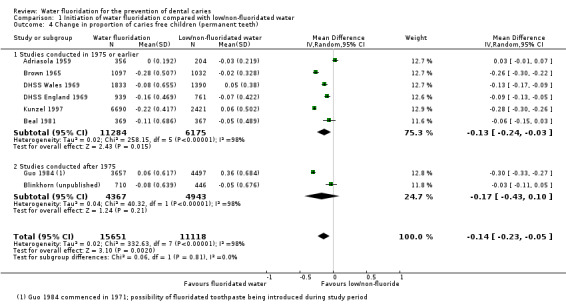
Comparison 1 Initiation of water fluoridation compared with low/non‐fluoridated water, Outcome 4 Change in proportion of caries free children (permanent teeth).
With regard to dental fluorosis, again, all studies were observational and we downgraded the quality of the evidence due to an overall high risk of bias and inconsistency due to substantial between‐study variation. Our confidence in the effect estimate is limited.
Potential biases in the review process
Within the review, water with a fluoride concentration of 0.4 ppm or less was classified as non‐fluoridated. This cut‐off was arbitrary, based on a priori clinical judgement. It is acknowledged that that this cut‐off might be high for equivalence of non‐fluoridation in hot climates. In practice, only one of the 15 studies that provided sufficient data for analysis of caries levels following a change in fluoridation status had a fluoride concentration greater than 0.2 ppm in the non‐fluoridated area.
We imputed the standard deviation for four studies included in the analysis of water fluoridation for preventing caries (dmft and DMFT). This was not prespecified in the protocol. The equation for imputing the standard deviations was estimated from available data where the standard deviations were given (Appendix 10). Sensitivity analysis, excluding those studies for which the standard deviation had been imputed gave similar results.
An arbitrary cut‐off date of 1975 was used as an indication of when fluoridated toothpaste use became widespread in industrialised countries. There is no indication in the included studies of the extent to which this is true.
We only reported on dmft in children eight years old and younger. This decision was based on clinical judgement, but was not prespecified in the protocol. The cut‐off is unlikely to alter the review's findings as very little data was excluded due to this cut‐off.
When analysing the dental fluorosis data, our primary analysis focused on fluoride concentrations of 5 ppm or less. Again, this was an arbitrary cut‐off; there was little difference in the results obtained when all fluoride concentrations were examined.
Agreements and disagreements with other studies or reviews
The most widely recognised systematic review of water fluoridation was published in 2000 (McDonagh 2000). Our review aimed to update this review, but has adopted different methods in certain areas. Importantly, these included changes to the evaluation of the cessation of water fluoridation programmes and the evaluation of disparities in caries levels.
The McDonagh 2000 review included 26 studies that looked at the effect of water fluoridation on oral health. No pooling of data was undertaken. The mean difference in change in dmft/DMFT and increase in proportion of caries‐free children were presented for selected ages/age groups. The range of mean reduction in dmft/DMFT score was from 0.5 to 4.4, with a median of 2.25 dmft/DMFT. In our review, we did undertake statistical pooling, imputing standard deviations where necessary. Rather than selecting specific ages from the data provided in the included studies, we undertook the analyses by dentition, utilising all data for deciduous teeth for children aged eight years and younger, and all available data for permanent teeth. The analyses showed mean reductions of 1.81 in dmft and 1.16 in DMFT, due to water fluoridation.
In terms of the proportion of caries‐free children following water fluoridation, the McDonagh 2000 review reported a range of mean differences from ‐0.05 to an increase of 0.64, with a median of 0.15. The pooled estimate obtained in our review demonstrates an increase in proportion of caries‐free children in the areas with water fluoridation of 0.15 for deciduous teeth and 0.14 for permanent teeth.
With regard to the cessation of water fluoridation programmes, the McDonagh 2000 review included eight studies, whereas our review included only one (Maupome 2001). This difference is due to the inappropriate choice of control group in the cessation studies. In a controlled before‐and‐after study, the groups should be comparable at baseline. Therefore, in the water fluoridation cessation studies, the two groups should both be fluoridated areas, one of which (the 'intervention' group) subsequently has the fluoride removed from the water. The area that remains fluoridated acts as the control. In the majority of the cessation studies, a non‐fluoridated area was used as the control at baseline. The intervention and control groups, therefore, were not comparable at the start of the study. Whilst the McDonagh 2000 review suggested that caries prevalence increases following the withdrawal of water fluoridation, this result was not confirmed in the study included in our review.
Neither the McDonagh 2000 review nor our review included studies that evaluated the effectiveness of water fluoridation for preventing caries in adults. However, Griffin 2007 undertook a comprehensive systematic review evaluating the effectiveness of fluoride in preventing caries in adults, including nine studies that examined the effectiveness of water fluoridation. The studies included fell outside the scope of both the McDonagh 2000 review and our review. One of the nine studies they included was a prospective cohort trial, and the remaining eight were cross‐sectional studies, with single time‐point data. In our review, we only included studies that reported caries data if they had a concurrent control, with at least two points in time evaluated. In the analyses, Griffin 2007 demonstrated a prevented fraction of 34.6% (95% CI 12.6% to 51.0%), when pooling data from seven studies of lifelong residents of control or fluoridated‐water communities (5409 participants). When the analysis was limited to studies published after 1979 the prevented fraction was 27.2% (95% CI 19.4% to 34.3%; 5 studies; 2530 participants). The most recent of these post‐1979 papers was published in 1992. The fluoride concentration evaluated in these more recent studies was not reported in two studies and was above what is considered the 'optimal level' in a further two studies. Griffin and colleagues acknowledge that the paucity of studies and the quality of the included studies limits their review.
A more recent evaluation of the effects of fluoridated drinking water on dental caries in adults has been conducted in Australia (Slade 2013). A comparison in caries levels was made between a cohort of adults born before the widespread implementation of fluoridation (before 1960; n = 2270) and a cohort born after widespread implementation (n = 1509). Greater lifetime exposure to water fluoridation was associated with lower levels of caries experience in both cohorts. In the study, 31% of participants were excluded from the complete‐case analysis due to missing data. The authors report that imputation to account for missing data "did not markedly alter estimated associations between fluoride exposure and caries experience" (Slade 2013).
When addressing the issue of whether water fluoridation results in a reduction in disparities in caries levels across different groups of people, the McDonagh 2000 review included 15 studies, all except two of which were cross‐sectional surveys. The authors concluded that, based on a small number of low quality, heterogeneous studies, there was "some evidence that water fluoridation reduces the inequalities in dental health across social classes in five and 12 year‐olds, using the dmft/DMFT measure. This effect was not seen in the proportion of caries‐free children among five year‐olds. The data for the effects in children of other ages did not show an effect." They suggested caution in interpreting these results due to the small number of studies and their low quality rating (McDonagh 2000). There were no data for disparities in caries levels amongst adults.
The cross‐sectional studies, whilst able to provide information on whether water fluoridation is associated with a reduction in disparities, are not able to address the question of whether water fluoridation results in a reduction in disparities in caries levels. There were insufficient data to determine whether initiation of a water fluoridation programme results in a change in disparities in caries levels across different groups of people.
In the past 20 years, the majority of research evaluating the effectiveness of water fluoridation for the prevention of dental caries has been undertaken using cross‐sectional studies with concurrent control, with improved statistical handling of confounding factors (Rugg‐Gunn 2012). We acknowledge that there may be concerns regarding the exclusion of these studies from the current review. A previous review of these cross‐sectional studies has shown a smaller measured effect in studies post‐1990 than was seen in earlier studies, although the effect remains significant. It is suggested that this reduction in size of effect may be due to the diffusion effect (Rugg‐Gunn 2012); this is likely to only occur in areas where a high proportion of the population already receive fluoridated water. The authors of the review conclude that "There is need for further thought to strengthen study design" (Rugg‐Gunn 2012).
The results from our review of the dental fluorosis data are fairly comparable with those of the McDonagh 2000 review. The McDonagh 2000 review fluorosis analysis excluded areas with natural fluoride levels above 5 ppm. It was acknowledged that this is significantly above the level recommended for artificial fluoridation, however the range of concentration of 0 ppm to 5 ppm allowed exploration of a dose‐response relationship. In the current review, we also conducted analyses of studies of fluoride concentrations of 5 ppm or lower, in addition to an analyses of all studies irrespective of fluoride concentrations. In the McDonagh 2000 review, the estimated percentage of the population with dental fluorosis of aesthetic concern at a fluoride concentration of 0.7 ppm was 9% (95% CI 4% to 17%; based on studies with fluoride concentration of 5 ppm or lower); in our review this was slightly higher at 12% (95% CI 8% to 17%). There was little change in the pooled estimates when all fluoride levels were included in the analysis.
The broader literature speculates about harms associated with higher levels of fluoride in water (e.g. cancer, lowered intelligence, endocrine dysfunction). These harms have not been systematically evaluated in this review, however, previous reviews suggest there is insufficient evidence to draw conclusions about them (MRC 2002; NHMRC 2007).
Authors' conclusions
Implications for practice.
There is very little contemporary evidence, meeting the review's inclusion criteria, evaluating the effectiveness of water fluoridation for the prevention of caries.
The data come predominantly from studies conducted prior to 1975, and indicate that water fluoridation is effective at reducing caries levels in both the deciduous and permanent dentition in children. Our confidence in the size of the effect estimates is limited by the observational nature of the study designs, the high risk of bias within the studies, and, importantly, the applicability of the evidence to current lifestyles. The decision to implement a water fluoridation programme relies upon an understanding of the population's oral health behaviours (e.g. use of fluoride toothpaste), the availability and uptake of other caries‐prevention strategies, diet and consumption of tap water, and the movement/migration of the population. There is insufficient evidence to determine whether water fluoridation results in a change in disparities in caries levels across socioeconomic status. There are no studies that met the review's inclusion criteria, from which to determine the effectiveness of water fluoridation for preventing caries in adults.
There is insufficient information to determine the effect of stopping water fluoridation programmes on caries levels.
There is a significant association between dental fluorosis (of aesthetic concern or all levels of dental fluorosis) and fluoride level. The evidence is limited due to high risk of bias within the studies and substantial between‐study variation.
The studies that have examined dental fluorosis as an outcome are generally more recent than those that have examined caries and, consequently, may be influenced by other sources of fluoride. These additional sources are seldom reported.
Implications for research.
More contemporary studies, evaluating the effectiveness of water fluoridation for the prevention of caries, are needed. These studies should include a concurrent control with comparable caries levels at baseline. Caries data should therefore be measured at at least two time points (i.e baseline and follow‐up).
Since all the included studies examined the effectiveness of water fluoridation in children, research on effectiveness among adults is needed.
Standardised diagnostic criteria and reporting techniques for caries and dental fluorosis would improve comparability of results across studies.
More research is also needed to understand the contribution of fluoride from sources other than water; the consumption of tap water within a population; the effect of water fluoridation over and above other caries preventive measures, namely dental sealants and fluoride varnishes; the impact of water fluoridation on disparities in oral health; and adverse effects associated with fluoridated water (particularly in areas with naturally high levels of fluoride).
What's new
| Date | Event | Description |
|---|---|---|
| 7 September 2015 | Amended | Plain Language Summary amended for simplification. |
History
Protocol first published: Issue 12, 2013 Review first published: Issue 6, 2015
| Date | Event | Description |
|---|---|---|
| 19 June 2015 | Amended | Minor edit to Plain Language Summary for clarification. Missing referee name added to Acknowledgements. |
| 2 February 2015 | Amended | Background updated to justify the need for the review. Change to risk of bias domains, incorporating an item on 'sampling' Change to the handling of missing data; imputation of missing standard deviations for DMFT and dmft data |
Acknowledgements
We wish to thank the staff of the Cochrane Oral Health Group for managing the literature searches and the editorial process. We would also like to thank the editors for comments and all those providing written referee comments: James D Bader, Laurie Barker, Anthony Blinkhorn, Davina Ghersi, Barbara Gooch, Susan Griffin, Colwyn Jones, Evangelos Kontopantelis, John Langford, Hardy Limeback, Stan Litras, John Morris, Denis O'Mullane, Derek Richards, Olive Russell, Aubrey Sheiham, Elizabeth Treasure, Helen Whelton and Sandra White. We acknowledge that the review does not reflect the views of all referees.
We would like to thank Fang Hua, Chengge Hua, Chunjie Li, Ignacio Araya, Monica Ballesteros, Paul Tramini and Zhao Shaofeng for translation support and Ashwini Sreekanta for her work on an earlier version of the protocol.
Appendices
Appendix 1. Databases searched in the original systematic review (McDonagh 2000)
• MEDLINE • EMBASE • NTIS (National Technical Information Service) • Biosis • Current Contents Search (Science Citation Index and Social Science Citation Index) • Healthstar (Health Service Technology, Administration and Research) • HSRProj • TOXLINE • Chemical Abstracts • OldMEDLINE • CAB Health • FSTA (Food Science and Technology Abstracts) • JICST‐ E Plus (Japanese Science and Technology) • Pascal • EI Compendex (Engineering Index) • Enviroline • PAIS (Public Affairs Information Services) • SIGLE (System for Information on Grey Literature in Europe) • Conference Papers Index • Water Resources Abstracts • Agricola (Agricultural Online Access) • Waternet • AMED (Allied and Complementary Medicine Database) • Psyclit • LILACS (Latin American and Caribbean Health Sciences Literature)
Appendix 2. The Cochrane Oral Health Group Trials Register search strategy
#1 ((fluorid* or flurid* or fluorin* or flurin*)) #2 water* #3 (#1 and #2)
Appendix 3. The Cochrane Central Register of Controlled Trials (CENTRAL) search strategy
#1 MeSH descriptor Fluoridation this term only #2 MeSH descriptor Fluorides explode all trees #3 MeSH descriptor Fluorine this term only #4 (fluorid* in All Text or fluorin* in All Text or flurin* in All Text or flurid* in All Text) #5 (#1 or #2 or #3 or #4) #6 MeSH descriptor Dietary supplements this term only #7 MeSH descriptor Water supply this term only #8 water* in All Text #9 (#6 or #7 or #8) #10 MeSH descriptor Tooth demineralization explode all trees #11 (caries in All Text or carious in All Text) #12 (teeth in All Text and (cavit* in All Text or caries in All Text or carious in All Text or decay* in All Text or lesion* in All Text or deminerali* in All Text or reminerali* in All Text)) #13 (tooth in All Text and (cavit* in All Text or caries in All Text or carious in All Text or decay* in All Text or lesion* in All Text or deminerali* in All Text or reminerali* in All Text)) #14 (dental in All Text and (cavit* in All Text or caries in All Text or carious in All Text or decay* in All Text or lesion* in All Text or deminerali* in All Text or reminerali* in All Text)) #15 (enamel in All Text and (cavit* in All Text or caries in All Text or carious in All Text or decay* in All Text or lesion* in All Text or deminerali* in All Text or reminerali* in All Text)) #16 (dentin in All Text and (cavit* in All Text or caries in All Text or carious in All Text or decay* in All Text or lesion* in All Text or deminerali* in All Text or reminerali* in All Text)) #17 (root* in All Text and (cavit* in All Text or caries in All Text or carious in All Text or decay* in All Text or lesion* in All Text or deminerali* in All Text or reminerali* in All Text)) #18 MeSH descriptor Dental plaque this term only #19 ((teeth in All Text or tooth in All Text or dental in All Text or enamel in All Text or dentin in All Text) and plaque in All Text) #20 MeSH descriptor Dental health surveys explode all trees #21 ("DMF Index" in All Text or "Dental Plaque Index" in All Text) #22 (#10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #21) #23 (#5 and #9 and #22)
Appendix 4. MEDLINE (OVID) search strategy
Fluoridation/
exp Fluorides/
Fluorine/
(fluorid$ or fluorin$ or flurin$ or flurid$).mp.
or/1‐4
Dietary supplements/
Water supply/
water$.mp.
or/6‐8
exp TOOTH DEMINERALIZATION/
(caries or carious).mp.
(teeth adj5 (cavit$ or caries$ or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp.
(tooth adj5 (cavit$ or caries$ or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp.
(dental adj5 (cavit$ or caries$ or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp.
(enamel adj5 (cavit$ or caries$ or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp.
(dentin$ adj5 (cavit$ or caries$ or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp.
(root$ adj5 (cavit$ or caries$ or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp.
Dental plaque/
((teeth or tooth or dental or enamel or dentin) and plaque).mp.
exp DENTAL HEALTH SURVEYS/
("DMF Index" or "Dental Plaque Index").mp.
or/10‐21
case reports.pt.
Comment/
Letter/
Editorial/
or/23‐26
exp animals/ not humans.sh.
5 and 9 and 22
29 not (28 or 27)
Appendix 5. EMBASE (OVID) search strategy
1. Fluoridation/ 2. exp Fluoride/ 3. Fluorine/ 4. (fluorid$ or fluorin$ or flurin$ or flurid$).ti,ab. 5. or/1‐4 6. Diet supplementation/ 7. Water supply/ 8. water$.ti,ab. 9. or/6‐8 10. exp Dental caries/ 11. (caries or carious).ti,ab. 12. (teeth adj5 (cavit$ or caries$ or carious or decay$ or lesion$ or deminerali$ or reminerali$)).ti,ab. 13. (tooth adj5 (cavit$ or caries$ or carious or decay$ or lesion$ or deminerali$ or reminerali$)).ti,ab. 14. (dental adj5 (cavit$ or caries$ or carious or decay$ or lesion$ or deminerali$ or reminerali$)).ti,ab. 15. (enamel adj5 (cavit$ or caries$ or carious or decay$ or lesion$ or deminerali$ or reminerali$)).ti,ab. 16. (dentin$ adj5 (cavit$ or caries$ or carious or decay$ or lesion$ or deminerali$ or reminerali$)).ti,ab. 17. (root$ adj5 (cavit$ or caries$ or carious or decay$ or lesion$ or deminerali$ or reminerali$)).ti,ab 18. Tooth plaque/ 19. ((teeth or tooth or dental or enamel or dentin) and plaque).ti,ab. 20. ("DMF Index" or "Dental Plaque Index" or "dental health survey*").ti,ab. 21. or/10‐20 22. 9 and 21 23. (exp animal/ or animal.hw. or nonhuman/) not (exp human/ or human cell/ or (human or humans).ti.) 24. 22 not 23
Appendix 6. Proquest search strategy
ab(fluorid*) AND ab(water*) AND ab(caries OR carious OR dental OR tooth OR teeth OR plaque)
Appendix 7. Web of Science Conference Proceedings search strategy
#1 TS=(fluorid* or fluorin* or flurin* or flurid*) #2 TS=water* #3 TS=(caries or carious) #4 TS=(teeth and (cavit* or caries* or carious or decay* or lesion* or deminerali* or reminerali*)) #5 TS=(tooth and (cavit* or caries* or carious or decay* or lesion* or deminerali* or reminerali*)) #6 TS=(dental and (cavit* or caries* or carious or decay* or lesion* or deminerali* or reminerali*)) #7 TS=(enamel and (cavit* or caries* or carious or decay* or lesion* or deminerali* or reminerali*)) #8 TS=(dentin* and (cavit* or caries* or carious or decay* or lesion* or deminerali* or reminerali*)) #9 TS=(root* and (cavit* or caries* or carious or decay* or lesion* or deminerali* or reminerali*)) #10 TS=((teeth or tooth or dental or enamel or dentin) and plaque) #11 TS=("DMF Index" or "Dental Plaque Index") #12 #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 #13 #1 and #2 and #12
Appendix 8. ZETOC Conference Proceedings search strategy
fluoride AND water AND caries fluoridation AND water AND caries fluoride AND water AND carious fluoridation AND water AND carious fluoride AND water AND dental fluoridation AND water AND dental fluoride AND water AND tooth fluoridation AND water AND tooth fluoride AND water AND teeth fluoridation AND water AND teeth
Appendix 9. US National Institutes of Health Trials Registry and WHO International Clinical Trials Registry Platform search strategy
fluoride and water and caries
Appendix 10. Imputation of standard deviations for caries data
Where standard deviations are missing for the DMFT, dmft data we used the equation: log(SD) = 0.17 + 0.56 x log(mean) to estimate the standard deviations for both before and after mean caries values. A sensitivity analysis was undertaken omitting all the data for studies/age groups where the standard deviation was imputed.
The equation we used was obtained from the data we had available to us from the other included studies in the review (102 mean and standard deviation data points). The equation had a similar regression coefficient to those developed by van Rijkom 1996 and Marinho 2003b shown below, although the intercept was smaller. This is probably because both these models had been developed on caries increments whereas the data we have used is cross‐sectional caries severity data.
Equation from:
van Rijkom 1996 log(SD) = 0.54 + 0.58 x log(mean), (R² = 0.83)
Marinho 2003b log(SD) = 0.64 + 0.55 x log(mean), (R² = 0.77)
This review log(SD) = 0.17 + 0.55 x log(mean), (R² = 0.90)
Appendix 11. Fluorosis studies
Studies included in the analysis of all level of fluorosis:
Acharya 2005; Adair 1999; Al‐Alousi 1975; Alarcon‐Herrera 2001; Albrecht 2004; AlDosari 2010; Angelillo 1999; Arif 2013; Azcurra 1995; Beltran‐Aguilar 2002; Booth 1991; Brothwell 1999; Chandrashekar 2004; Chen 1989; Chen 1993; Clark 1993; Clarkson 1989; Cochran 2004a; Correia Sampaio 1999; Cutress 1985; Driscoll 1983; Ekanayake 2002; Eklund 1987; Ellwood 1995; Ellwood 1996; Firempong 2013; Forrest 1965; Garcia‐Perez 2013; Gaspar 1995; Grimaldo 1995; Grobler 1986; Grobler 2001; Haavikko 1974; Heintze 1998; Heller 1997; Hernandez‐Montoya 2003; Hong 1990; Ibrahim 1995; Indermitte 2007; Indermitte 2009; Ismail 1990; Jackson 1975; Jackson 1999; Kanagaratnam 2009; Kotecha 2012; Kumar 2007; Kunzel 1976; Leverett 1986; Levine 1989; Lin 1991; Louw 2002; Machiulskiene 2009; Mackay 2005; Macpherson 2007; Mandinic 2009; Marya 2010; Masztalerz 1990; McGrady 2012; McInnes 1982; Mella 1992; Mella 1994; Milsom 1990; Montero 2007; Nanda 1974; Narbutaite 2007; Narwaria 2013; Nunn 1994a; Ockerse 1941; Pontigo‐Loyola 2008; Ray 1982; Riordan 1991; Riordan 2002; Rwenyonyi 1998; Rwenyonyi 1999; Saravanan 2008; Sellman 1957; Shekar 2012; Stephen 2002; Szpunar 1988; Tabari 2000; Tsutsui 2000; Wang 1993; Wang 1999; Wang 2012; Warnakulasuriya 1992; Warren 2001; Wenzel 1982; Wondwossen 2004; Zheng 1986; Zimmermann 1954
Studies included in the analysis of fluorosis of aesthetic concern:
Acharya 2005; Alarcon‐Herrera 2001; AlDosari 2010; Angelillo 1999; Arif 2013; Beltran‐Aguilar 2002; Chen 1989; Clark 1993; Correia Sampaio 1999; Driscoll 1983; Eklund 1987; Forrest 1965; Gaspar 1995; Grimaldo 1995; Grobler 1986; Grobler 2001; Haavikko 1974; Heller 1997; Hernandez‐Montoya 2003; Hong 1990; Ibrahim 1995; Jackson 1999; Kunzel 1976; Leverett 1986; Louw 2002; Macpherson 2007; McGrady 2012; Mella 1992; Mella 1994; Montero 2007; Nanda 1974; Pontigo‐Loyola 2008; Ray 1982; Riordan 1991; Riordan 2002; Ruan 2005; Russell 1951; Sellman 1957; Stephen 2002; Tabari 2000; Zheng 1986; Zimmermann 1954
Studies that could not be included in analysis:
Awadia 2000; Bao 2007; Baskaradoss 2008; Birkeland 2005; Butler 1985; Chen 1993; Clarkson 1992; Colquhoun 1984; Cypriano 2003; de Crousaz 1982; Downer 1994; Driscoll 1983; Ermis 2003; Forrest 1956; Franzolin 2008; Harding 2005; Heifetz 1988; Jolly 1971; Kumar 1999; Mandinic 2010; Mazzotti 1939; Rugg‐Gunn 1997; Scheinin 1964; Segreto 1984; Selwitz 1995; Selwitz 1998; Shanthi 2014; Skinner 2013; Skotowski 1995; Spadaro 1955; Sudhir 2009; Venkateswarlu 1952; Vilasrao 2014; Villa 1998; Vignarajah 1993; Vuhahula 2009; Whelton 2004; Whelton 2006
Data and analyses
Comparison 1. Initiation of water fluoridation compared with low/non‐fluoridated water.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in decayed, missing or filled deciduous teeth (dmft) | 9 | 22134 | Mean Difference (IV, Random, 95% CI) | 1.81 [1.31, 2.31] |
| 1.1 Studies conducted in 1975 or earlier | 7 | 17039 | Mean Difference (IV, Random, 95% CI) | 1.82 [1.53, 2.11] |
| 1.2 Studies conducted after 1975 | 2 | 5095 | Mean Difference (IV, Random, 95% CI) | 1.56 [‐0.67, 3.80] |
| 2 Change in decayed, missing or filled permanent teeth (DMFT) | 10 | 39382 | Mean Difference (IV, Random, 95% CI) | 1.16 [0.72, 1.61] |
| 2.1 Studies conducted in 1975 or earlier | 7 | 30499 | Mean Difference (IV, Random, 95% CI) | 1.41 [0.84, 1.98] |
| 2.2 Studies conducted after 1975 | 3 | 8883 | Mean Difference (IV, Random, 95% CI) | 0.64 [‐0.27, 1.55] |
| 3 Change in proportion of caries free children (deciduous teeth) | 10 | 19983 | Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.19, ‐0.11] |
| 3.1 Studies conducted in 1975 or earlier | 7 | 11902 | Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.19, ‐0.15] |
| 3.2 Studies conducted after 1975 | 3 | 8081 | Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.24, ‐0.01] |
| 4 Change in proportion of caries free children (permanent teeth) | 8 | 26769 | Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.23, ‐0.05] |
| 4.1 Studies conducted in 1975 or earlier | 6 | 17459 | Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.24, ‐0.03] |
| 4.2 Studies conducted after 1975 | 2 | 9310 | Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.43, 0.10] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Acharya 2005.
| Methods | FLUOROSIS STUDY Country of study: India Geographic location: Davangere‐Nallur, Naganur, Doddabathi, Kundawada and Holesirigere Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional | |
| Participants | Inclusion criteria: school children aged 12‐15 years; lifetime residency Exclusion criteria: absence on the day of the survey Other sources of fluoride: not stated Social class: socioeconomic position was similar in all villages Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 0.43 ppm Group 2: 0.72 ppm Group 3: 1.1 ppm Group 4: 1.22 ppm Group 5: 3.41 ppm |
|
| Outcomes | Dental fluorosis (Dean's Index) Age at assessment: 12‐15 years | |
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | 5 villages were selected out of a possible 90. There was insufficient detail reported to determine how selection took place |
| Confounding | High risk | Did not account for use of other fluoride sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | Low risk | No other apparent bias |
Adair 1999.
| Methods | FLUOROSIS STUDY Country of study: USA Geographic location: Warren County, Georgia Year of study: not stated Year of change in fluoridation status: not stated Study design: cross‐sectional | |
| Participants | Inclusion criteria: children attending sole elementary and middle schools in study area Exclusion criteria: children whose homes were served with well‐water. Other sources of fluoride: parents completed questionnaire regarding dentifrice use, home water source and current use of systemic fluoride supplements; all subjects received school water fluoridated at 0.5 ppm Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: not considered Other confounding factors: not stated |
|
| Interventions | Group 1: 0.5‐1.2 ppm (both natural and artifical fluoridation) Group 2: < 0.1 ppm (natural fluoridation) | |
| Outcomes | Dental fluorosis (Dean's Index); caries data collected but not presented in this review due to study design Age at assessment: 8‐10 and 11‐13 years | |
| Funding | NIDR Grant DE‐06113 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Participants were children attending the sole elementary and middle/high schools in Warren county. There was insufficient detail reported to determine how selection took place |
| Confounding | High risk | SES was not accounted for |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data for over 80% of participants were reported |
| Selective reporting (reporting bias) | High risk | Outcome of interest reported. However, data were not presented clearly enough to be considered reliable |
| Other bias | High risk | Exposure to fluoride water could not be controlled for. Some children had fluoride water at school across groups. Some had non‐fluoridated well‐water at home |
Adriasola 1959.
| Methods | CARIES STUDY Country of study: Chile Geographic location: Curico (F); San Fernando (non‐F) Year study started: 1953 Year study ended: 1956 Year of change in fluoridation status: 1953 Study design: CBA | |
| Participants | Inclusion criteria: children aged 3‐15; children from 2 primary schools in the study areas Exclusion criteria: none stated Other sources of fluoride: not stated Social class: based on knowledge of their demographics, culture and social economy, it was assumed that the study areas were comparable Ethnicity: not stated Residential history: not stated Other confounding factors: none stated |
|
| Interventions | Initiation of water fluoridation Group 1: low fluoride content (ppm not reported; natural fluoridation) Group 2: low fluoride content (ppm not reported; natural fluoridation) | |
| Outcomes | % caries‐free participants Age at baseline measure: 3‐8 years and 11, 12 and 15 years (unclear if deciduous or permanent dentition) Age at final measure: 3‐8 years and 11, 12 and 15 years (unclear if deciduous or permanent dentition) | |
| Funding | In collaboration with members of the committee Pro‐Fluoridation | |
| Notes | Data extracted from Adriasola 1959 differs from that presented in CRD review (additional data extracted) Paper translated from Spanish |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Following on from the 1953 survey, the authors re‐established contact with local authorities, teachers and health educators in 1956 and in a period of 2 months examined children in Curicco and San Fernando attending private and public technical schools, kindergartens, primary and secondary schools. There was insufficient detail reported to determine how selection took place |
| Confounding | High risk | Study groups assumed comparable for SES. No details were reported on the use of fluoride from other sources or on the dietary habits of the children |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Different children examined at before and after time points. Unclear if all eligible children examined at each time point |
| Selective reporting (reporting bias) | High risk | Baseline data for proportion of children caries free incomplete for ages 6, 7, 11 and 15 years |
| Other bias | Low risk | No other apparent bias |
Al‐Alousi 1975.
| Methods | FLUOROSIS STUDY Country of study: England Geographic location: Anglesey (F); Leeds (non‐F) Year of study: 1973 Year of change in fluoridation status: 1955 Study design: cross‐sectional | |
| Participants | Inclusion criteria: lifetime residents of study areas; children aged 12‐16 years Exclusion criteria: missing, fractured or crowned teeth; refusal to participate (1 school in Leeds) Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | Group 1: 0.9 ppm (artificial fluoridation) Group 2: < 0.01 ppm (natural fluoridation) | |
| Outcomes | Dental fluorosis Age at assessment: 12‐16 years |
|
| Funding | Not stated | |
| Notes | Data extracted from Al‐Alousi 1975 differs from that presented in CRD review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Children were selected from schools in Leeds in a quasi‐random way whereby every nth child (n = total children in school/20) from the register was selected. Eligible children in Anglesea were selected from schools randomly |
| Confounding | High risk | Did not account for use of other fluoride sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | A clinical investigation and double‐blinded photographic examination were conducted. However, the results reported are those of the unblinded clinical investigation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Unclear risk | Outcome of interest reported |
| Other bias | High risk | Diagnoses had to be "agreed" on by the two examiners and there was no mention of any sort of calibration of the examiners. This may have resulted in measurement bias |
Alarcon‐Herrera 2001.
| Methods | FLUOROSIS STUDY Country of study: Mexico Geographic location: Durango Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional | |
| Participants | Inclusion criteria: children aged 6‐12 years who had established permanent residence in the area Exclusion criteria: not stated Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: permanent residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: non‐detectable‐1.5 ppm Group 2: 1.51‐4.99 ppm Group 3: 5.0‐8.49 ppm Group 4: 8.5‐11.9 ppm Group 5: > 12 ppm | |
| Outcomes | Dental fluorosis (Dean's Index) Age at assessment: 6‐12 years | |
| Funding | Project grant from the Mexican National Council of Science and Technology Conacyt‐Sivilla, Project 9502160 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Through a polystage conglomerate random sampling, 380 families were selected and prorated into 77‐80 families per concentration area zone. The division yielded a total of 1437 individuals from the five different areas |
| Confounding | High risk | Did not account for use of other fluoride sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | Unclear risk | No information examiner calibration with regard to detection of the outcome variable |
Albrecht 2004.
| Methods | FLUOROSIS STUDY Country of study: Hungary Geographic location: Bár and Dunaszekcső Year of study: 2004 Year of change in fluoridation status: NA Study design: cross‐sectional | |
| Participants | Inclusion criteria: healthy schoolchildren, aged 6‐18 years; lifelong residents in the communities Bár or Dunaszekcső; only permanent teeth were investigated Exclusion criteria: any systemic disease Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 1.7 ppm Group 2: 2 ppm |
|
| Outcomes | Dental fluorosis (Dean's Index and TSIF) Age at assessment: 6‐18 years | |
| Funding | Not stated | |
| Notes | Paper translated from Hungarian | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | There was insufficient detail reported to determine how selection took place |
| Confounding | High risk | Did not account for use of other fluoride sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | Low risk | No other apparent bias |
AlDosari 2010.
| Methods | FLUOROSIS STUDY Country of study: Saudi Arabia Geographic location: Riyadh Year of study: 2010 Year of change in fluoridation status: NA Study design: cross‐sectional | |
| Participants | Inclusion criteria:Saudi nationality; lifetime residence in the area Exclusion criteria: non‐Saudi nationality; absence from school on the day of dental examination Other sources of fluoride: not stated Social class: both schools from urban and rural areas were included in the sample frame Ethnicity: Saudi nationals, no further details Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation
Group 1: 0‐0.3 ppm
Group 2: 0.31‐0.6 ppm Group 3: 0.61‐1 ppm Group 4: 1.01‐1.5 ppm Group 5: 1.51‐2 ppm Group 6: 2.01‐2.5 ppm Group 7: ≥ 2.51 ppm |
|
| Outcomes | Dental fluorosis (TF Index) Age at assessment: 6‐18 years | |
| Funding | Supported by a grant from King Abdulaziz City for Science and Technology, Riyadh, Saudi Arabia | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | A list of zones was considered as the sampling frame for the schools, and municipalities were randomly chosen from each zone to represent the urban area. Additionally, rural areas in the municipality with at least one school were surveyed. However there was insufficient detail reported to determine how selection of schools and children within those schools took place |
| Confounding | High risk | Did not account for use of other fluoride sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Over 95% of the subjects sampled were examined. However, it is not clear why fluorosis was not scored in permanent teeth of the 6‐ to 7‐year olds |
| Selective reporting (reporting bias) | High risk | The authors did not report or justify not presenting fluorosis data for the age group 15‐18 years |
| Other bias | Unclear risk | Clinical examination was carried out by 2 dentists, but no information on whether the examiners were calibrated with regard to detection of the outcome variable was given |
Angelillo 1999.
| Methods | FLUOROSIS STUDY Country of study: Italy Geographic location: areas around Naples (F); Catanzaro (non‐F) Year of study: 1997 Year of change in fluoridation status: NA Study design: cross sectional | |
| Participants | Inclusion criteria: lifetime residents of study areas (children only); children aged 12 years; used community water supply as main sources of drinking water Exclusion criteria: partially erupted teeth; orthodontic banding Other sources of fluoride: tooth brushing habits (frequency of tooth brushing); fluoride tablets; fluoride dentifrices Social class: parents' employment status Ethnicity: not stated Residential history: lifetime residents Other confounding factors: sweet consumption; climate |
|
| Interventions | All natural fluoridation Group 1: ≥ 2.5 ppm Group 2: ≤ 0.3 ppm | |
| Outcomes | Dental fluorosis; caries data evaluated in study but not included in review due to study design Age at assessment: 12 years |
|
| Funding | Partially supported by a grant of Acquedotto Vesu‐ viano S.p.A. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Schools were selected at random, as were classes with the schools. All eligible children within the selected class were recruited to the study |
| Confounding | High risk | There was a reported imbalance between groups in the use of fluoride supplements, toothbrushing behaviour and in SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data for the majority of participants presented |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | Unclear risk | The 2 examiners involved had previously been trained and calibrated, but details not presented |
Arif 2013.
| Methods |
FLUOROSIS STUDY Country of study: India Geographic location: Nagaur district Year of study: 2013 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: only villages where the mean fluoride concentration was > 1.0 mg/L were selected for the dental fluorosis survey. No other information provided for participants Exclusion criteria: not stated Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: not stated Other confounding factors: not stated |
|
| Interventions | 54 villages receiving water with different natural fluoride concentrations ranging from 0.9 5.8 ppm | |
| Outcomes | Dental fluorosis (Dean's Index) Age at assessment: not stated |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Only villages where the mean fluoride concentration was > 1.0 ppm were selected. There was insufficient detail reported to determine how selection took place |
| Confounding | High risk | Did not account for use of other fluoride sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to determine whether data presented for all participants as study details were poorly reported |
| Selective reporting (reporting bias) | Low risk | Outcome of interest not reported in paper, but made available by authors via email |
| Other bias | High risk | Fluoride concentration for the different villages overlapped making the data impossible to interpret |
Arnold 1956.
| Methods |
CARIES STUDY Country of study: USA Geographic location: Grand Rapids (F); Muskegon (non‐F) Year study started: 1944 Year study ended: 1951 (after which time the control group became fluoridated; evaluated until 1954) Year of change in fluoridation status: 1945 Study design: CBA |
|
| Participants | Inclusion criteria: children aged 4‐16 years; used city water supplies since birth Exclusion criteria: children who lived outside study areas for more than 3 months of any 1 year Other sources of fluoride: author stated that there were no concerted efforts to commence special caries control programmes e.g. topical fluoride programmes, in either of the cities since the study began Social class: not stated Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | Initiation of water fluoridation Group 1: 1 ppm (artificial fluoridation) Group 2: < 0.2 ppm (natural fluoridation) | |
| Outcomes | DMFT; deft Age at baseline measure: 5‐13 years (deciduous dentition); 6‐16 years (permanent dentition) Age at final measure: 5‐13 years (deciduous dentition); 6‐16 years (permanent dentition) |
|
| Funding | Not stated | |
| Notes | Data extracted from Arnold 1956 differed from that presented in CRD review (additional data extracted) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Children were selected through schools. Almost all eligible children in the areas of study were examined |
| Confounding | High risk | No efforts were made to stop topical fluoride application in either control or test group. However it is not known if the areas differed in terms of the programmes/services on offer. No details on the dietary habits of the children were reported |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding of assessors |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "samples consist of all available children in certain grades (or in sections of the grades)" Number of children examined each year presented, however, numbers varied across each age group and each year (not a continuous study sample) |
| Selective reporting (reporting bias) | High risk | It is noted in the results that fluorosis observations had been made, but no details were given for the methods and data (just % increase). Also, standard deviation not reported |
| Other bias | High risk | Calibration of examiners not mentioned |
Ast 1951.
| Methods |
CARIES STUDY Country of study: USA Geographic location: Newburgh (F); Kingston (non‐F) Year study started: 1945 Year study ended: 1952 Year of change in fluoridation status: 1945 Study design: CBA |
|
| Participants | Inclusion criteria: all 5‐ to 12‐year‐old children present at school on days of examination; lifetime residents of study areas Exclusion criteria: none stated Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions |
Initiation of water fluoridation Group 1 baseline: < 0.1 ppm (natural fluoridation) Group 1 post intervention: 1‐1.2 ppm (artificial fluoridation) Group 2: < 0.1 ppm (natural fluoridation) |
|
| Outcomes | DMFT rate per 100 erupted permanent teeth; % caries‐free children (deciduous dentition) Age at baseline measure: 5 years (deciduous dentition); 6‐12 years (permanent dentition) Age at final measure: 5 years (deciduous dentition); 6‐12 years (permanent dentition) |
|
| Funding | Not stated | |
| Notes | Data extracted from Ast 1951 differs from that presented in CRD review (additional data extracted) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | All 5‐ to 12‐year‐old school children present in the schools within the study areas on the days of examination were included in the study |
| Confounding | High risk | Did not account for SES, the use of other fluoride sources, or the dietary habits of the children |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The number of participants for whom outcome data was reported (F = 3054; non‐F = 2812) varied from the number of participants reported to have been included in the study (F = 3200; non‐F = 3100) |
| Selective reporting (reporting bias) | High risk | Baseline dates of children in the intervention (1944‐45) and control (1945‐46) groups varied, which would result in incomparability of data from both study groups |
| Other bias | High risk | There was no mention of examiner calibration |
Awadia 2000.
| Methods |
FLUOROSIS STUDY Country of study: Tanzania Geographic location: Arusha and Moshi Year of study: 1996 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: age 9‐14 years; lifelong residence in respective towns or villages Exclusion criteria: not stated Other fluoride sources: toothpaste use: Arusha = 94%; Arusha Meru = 100%; Moshi = 97.1% and Kibosho = 40%Magadi use: Arusha = 31(47%); Arusha Meru = 1(2.9%); Moshi = 41 (58.6%); Kibosho = 83(97.6%) Social class: peasant mothers: Arusha = 1 (1.5%); Arusah Meru = NR; Moshi = 7 (10%); Kibosho = 33 (38.8%); other: Arusha = 65 (98.5%); Arusha Meru = 35 (100%); Moshi = 63 (90%); Kibosho = 52 (61.2%) Ethnicity: Arusha area (Arusha and Arusha Meru) – mainly ethnic Asians; Kilimanjaro region (Moshi and Kibosho) ‐ Africans Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 0.2 ppm Group 2: 0.3 ppm Group 3: 3.6 ppm | |
| Outcomes | Dental fluorosis (TF Index) Age at assessment: 9‐14 years |
|
| Funding | Supported by the Norwegian State Educational Loan fund, NUFU project 61/96, and the committee for Research and Postgraduate Training, Faculty of Dentistry, University of Bergen, Norway | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Schools in all villages (except in Arusha Meru) as well as participants were randomly selected. For schools where participants were not randomly selected, including the school in Arusha Meru, all the registered school children were chosen to participate |
| Confounding | High risk | There was a reported imbalance between groups in terms of SES and use of fluoride from other sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | High risk | Outcome of interest not fully reported, rather presented as a median score |
| Other bias | High risk | Only one examiner was involved; no testing for intra‐rater reliability with regard to detection of the outcome variable. |
Azcurra 1995.
| Methods |
FLUOROSIS STUDY Country of study: Argentina Geographic location: Sampacho (F); Porteña (non‐F) in the Cordoba province Year of study: 1993 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: children aged 6‐7 years (1st grade) and 12‐13 years (7th grade) at primary school Exclusion criteria: none stated Other sources of fluoride: frequency of tooth brushing. Group 1 (aged 6‐7): 56% brushed at least once a day (28/50) Group 1 (aged 12‐13): 74% brushed at least once a day (37/50) Group 2 (aged 6‐7): 46% brushed at least once a day (23/50) Group 2 (aged 12‐13): 50% brushed at least once a day (25/50) Social class: determined by occupation and highest attained level of schooling attained by main breadwinner in familyClassified as high, medium, and low social class Group 1 (aged 6‐7): 80% low SES (40/50) Group 1 (aged 12‐13): 82% low SES (41/50) Control (aged 6‐7): 74% low SES (37/50) Control (aged 12‐13) 80% low SES (40/50) Residential history: not stated Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 9.05 ppm Group 2: 0.19 ppm | |
| Outcomes | Dental fluorosis (Dean’s Index); caries data evaluated in study but not included in review due to study design Age at assessment: 6‐7 years and 12‐13 years |
|
| Funding | Part of this work was subsidised by the Ministry of Science and Technology ( SeCyT ) of the National University of Córdoba , Córdoba, Argentina | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Stratified random selection was used. Following stratification by age, gender and SES,100 school children were randomly selected from each village |
| Confounding | High risk | Although SES was considered during sampling, it was not controlled for within the analysis. No details were reported on the use of fluoride from other sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding not stated, however the two calibrated operators, as authors of the study, were likely to have knowledge of the study areas |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest was fully reported on and balanced across both groups |
| Other bias | Low risk | No other apparent biases |
Backer‐Dirks 1961.
| Methods | CARIES STUDY Country of study: Holland Geographic location: Tiel (F); Culemborg (non‐F) Year study started: 1952 Year study ended: 1959 Year of change in fluoridation status: 1953 Study design: CBA | |
| Participants | Inclusion criteria: children aged 11‐15; lifelong residents of the study areas; used the piped water supply; 100 children of each age examined Exclusion criteria: not stated Other fluoride sources: not stated Social class: areas similar in social class structure and proportional numbers of subjects selected from each school type Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | Initiation of water fluoridation Group 1: 1.1 ppm (artificial fluoridation) Group 2: 0.1 ppm (natural fluoridation) | |
| Outcomes | Average number of all approximal lesions; average number of approximal dental lesions Age at baseline measure: 11‐15 years (permanent dentition) Age at final measure: 11‐15 years (permanent dentition) | |
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | A proportion of children were chosen at random from different types of schools (public school, Roman Catholic, Protestant) |
| Confounding | High risk | No details were reported on the use of fluoride from other sources or on the dietary habits of the children |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The radiographs made in Tiel and Culemborg were put into unlabelled envelopes, and examined at random". Each examiner evaluated the same number of radiographs without knowledge of the origin of the films |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It is not clear whether the outcome data were reported for all participants |
| Selective reporting (reporting bias) | High risk | Outcome of interest reported, however, data not in useable format |
| Other bias | Low risk | No other bias apparent |
Bao 2007.
| Methods |
FLUOROSIS STUDY Country of study: China Geographic location: 3 cities (Harbin, Mudanjiang, Zhaodong) and 3 rural areas (Zhaoyuan, Shuangcheng, Linkou) in the Heilongjiang province Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: 12‐year‐old children in Heilongjiang Exclusion criteria: not reported. Other sources of fluoride: not reported Social class: 396 (198 male; 198 female) from cities; 396 (198 male; 198 female) from rural areas Ethnicity: Chinese Residential history: not reported Other confounding factors: not reported |
|
| Interventions | All natural fluoridation Group 1 (Linkou): 0.29 ppm Group 2 (Mudanjiang): 0.40 ppm Group 3 (Shuangcheng): 0.68 ppm Group 4 (Harbin): 0.77 ppm Group 5 (Zhaoyuan): 0.80 ppm Group 6 (Zhaodong): 1.14 ppm |
|
| Outcomes | Dental fluorosis (CFI); caries data evaluated in study, but excluded from review due to study design Age at assessment: 12 years |
|
| Funding | Research Fund of Bureau of Health of Heilongjiang Province (grant no.2005[122]) | |
| Notes | Translation from Chinese | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Quote: "Representative samples were selected by multi‐stage, stratified and random sampling" "For each site, 66 12‐year‐old boys and 66 12‐year‐old girls were randomly chosen". |
| Confounding | High risk | 3 groups were from cities and 3 groups were from rural areas. The authors did not record/report or adjust for other confounding factors (e.g. other fluoride sources, diet, residential history) |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The authors did not report any information on loss of follow‐up or exclusion of participants. Judging by the number of people they chose randomly (792), and the number of people (792) with results of caries examination, there was no loss of follow‐up or exclusion of participants |
| Selective reporting (reporting bias) | High risk | Data not presented in a format that allowed for further evaluation Quote: "Dean’s Index was used to classify fluorosis." The authors did not report the number of affected people for each Dean's Index category. They did not report the prevalence fluorosis (number of affected people/number of people examined) |
| Other bias | Low risk | No other apparent bias |
Baskaradoss 2008.
| Methods | FLUOROSIS STUDY Country of study: India Geographic location: 9 villages (Munchirai, Thovalai, Melpuram, Rajakkamangalam, Kurunthencode, Thiruvattar, Agasteeswaram, Thuckalay, Killiyoor) in Kanyakumari district Year of study: 2006 Year of change in fluoridation status: NA Study design: cross‐sectional | |
| Participants | Inclusion criteria: not stated Exclusion criteria: not stated Other sources of fluoride: brushing patter (toothbrush) = 84.6%; toothpaste (Colgate) = 92.2%; frequency (once daily) = 80.7%; age of starting to brush (< 2 years) = 69.2% Social class: low SES (46.1%); urban residence (44.2%) Ethnicity: not stated Residential history: not stated Other confounding factors: Information was collected on diet, seafood intake and tea |
|
| Interventions | All natural fluoridation Groups 1–9: specific ppm not presented. Groups listed according to number of Panchayats in the various Blocks of Kanyakumari district with water fluoride level more than 1.5 and 1.7 ppm |
|
| Outcomes | Dental fluorosis (Dean's Index ) Age at assessment: 10‐15 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | A stratified cluster sampling method was used to select the samples. 2 schools from each block were selected at random from a list of higher secondary schools. After examining an entire class, only the first 20 were taken until sample size was achieved |
| Confounding | High risk | Participants had different oral hygiene habits and there was no mention of duration of residency |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data for all participants reported |
| Selective reporting (reporting bias) | High risk | Data not in suitable format for analysis |
| Other bias | Unclear risk | No mention of calibration |
Beal 1971.
| Methods | CARIES STUDY Country of study: England Geographic location: Balsall Heath and Northfield, Birmingham (F); Dudley (non‐F) Year study started: 1967 Year study ended: 1970 Year of change in fluoridation status: 1964 Study design: CBA | |
| Participants | Inclusion criteria: children aged 5 attending schools that participated in each year of the study Exclusion criteria: none stated Other sources of fluoride: not stated Social class: Quote: "The socio‐economic composition of the districts has been described previously ...". Balsall Heath is a poor area of the city with high proportion of immigrants; Northfield and Dudley are both industrial areas with comparable populations, but there were more immigrants in Dudley Ethnicity: all areas have some proportion of immigrants Residential history: no attempt was made to select continuously resident children from the samples Other confounding factors: not stated |
|
| Interventions | Initiation of water fluoridation Group 1 and Group 2: 1 ppm (artificial fluoridation) Group 3: < 0.1 ppm (natural fluoridation) | |
| Outcomes | dmft; % caries‐free children Age at baseline measure: 5 years (deciduous dentition) Age at final measure: 5 years (deciduous dentition) | |
| Funding | MRC grant funded trial | |
| Notes | Quote: "The children, who were 5 years old in 1967, were aged about 3 years when the fluoride in their drinking water reached the recommended level; they had erupted all their deciduous, and these would be expected to have derived only slight benefit at this time. These children do not represent a true baseline; any dental advantage that this group had received, compared with the true but unexamined baseline before fluoride was added would have the effect of decreasing the observed reduction, if any, over subsequent years." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | There was insufficient detail reported to determine how selection took place |
| Confounding | High risk | No details were reported on the use of fluoride from other sources or on the dietary habits of the children |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Different children examined at before and after time points. Unclear if all eligible children examined at each time point |
| Selective reporting (reporting bias) | Low risk | Reporting of outcome of interest balanced across groups |
| Other bias | High risk | No detail of who performed examinations, their training/consistency |
Beal 1981.
| Methods |
CARIES STUDY Country of study: England Geographic location: Scunthorpe (F); Corby (non‐F) Year study started: 1969 Year study ended: 1975 Year of change in fluoridation status: 1968 Study design: CBA |
|
| Participants | Inclusion criteria: lifetime residents in study areas; children aged 5, 8 and 12 Exclusion criteria: teeth extracted for orthodontic purposes Other sources of fluoride: not stated Social class: both areas had iron/steel as main industry‐socioeconomic; composition of the 2 areas was similar Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | Fluoride initiation Group 1: 0.9 ppm (artificial fluoridation) Group 2: 0.35 ppm (natural fluoridation) | |
| Outcomes | dmft; DMFT; % caries‐free subjects (deciduous teeth); % caries‐free subjects (permanent teeth) Age at baseline measure: 5, 8 and 12 years Age at final measure: 5, 8 and 12 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Schools were chosen by random selection and every child of eligible age in these schools was examined |
| Confounding | High risk | No details were reported on the use of fluoride from other sources or on the dietary habits of the children |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data for all participants appears to be presented |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | Low risk | The authors reported that was no difference in level of reproducibility of the examiners |
Beltran‐Aguilar 2002.
| Methods |
FLUOROSIS STUDY Country of study: USA Geographic location: not stated Year of study: 1986 Year study ended: 1987 Year of change in fluoridation status: not stated Study design: cross‐sectional |
|
| Participants | Inclusion criteria: aged 12‐14 years; availability of data on type of water system and fluorosis; having residences served by the same type of public water system with respect to fluoride status; determinable date of public water system fluoridation initiation and residence at area before initiation of water fluoridation; availability of continuous residence history if more than 1 residence; fewer than 5 residences; ascertainable exposure to fluoride drops or tables; served by public water systems with ascertainable fluoride status in residences Other fluoride sources: tablets = 623 (14.9%); drops = 627 (14.5%); tablets and drops = 317 (8.4%). Suboptimal fluoride: drops only = 507 (23.0); tablets only = 512 (22.5); tablets and drops = 279 (13.2). Optimal fluoride:drops only = 103 (6.8); tablets only = 98 (6.0); tablets and drops = 32 (2.2) Natural fluoride: drops only = 13 (5.5); tablets only = 17 (7.5);tablets and drops = 6 (2.5) Exclusion criteria: any criterion in discord with the inclusion criteria Social class: not stated Ethnicity: not stated Residential history: all the children were continuous residents of areas with the reported water systems Other confounding factors: not stated |
|
| Interventions | Group 1: < 0.7 ppm (natural fluoridation) Group 2: 0.7‐1.2 ppm (artificial fluoridation) Group 3: 0.7‐4 ppm (natural fluoridation) | |
| Outcomes | Dental fluorosis (Dean's Index) Age at assessment: 12‐14 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | The sampling frame was specified and the sample represented 41 percent of all 12‐ to 14‐year olds and more than 4 million schools children, there is no evidence that any eligible children were excluded |
| Confounding | High risk | The use of other fluoride sources was similar in those that consumed water with optimal and natural fluoride, but very different from those in the suboptimal fluoride group. Did not account for SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Children with missing outcome data were excluded. It is not clear whether there was an imbalance across groups in excluded children |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | High risk | There is an overlap in fluoride concentration between the exposure groups (0.7‐1.2 ppm and 0.7‐4.0 ppm) which is likely to dilute the observable effect of exposure to intervention across groups. It is unclear whether the examiners were calibrated as the paper provides insufficient information and we were unable to access associated reports which may have contained examination protocols |
Berndt 2010.
| Methods |
FLUOROSIS STUDY Country of study: Namibia Geographic location: Ombili, Ondera, Vryheid, Kakuse Year of study: October 2004 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: aged 8‐21 years Other fluoride sources: 47 (39.3%) reported oral hygiene practice with fluoridated toothpaste (1400 ppm); 8 (6.7%) used traditional 'natural' toothbrush. Different ethnic groups differed markedly in their oral hygiene behaviour (P value 0.02) Exclusion criteria: not stated Social class: not stated Ethnicity: !Kung (45%); Heikum (35%); Damara (13%); Bantu (7%) Residential history: residents of Ombili had been resident since 1991 and the residents of the other farms were lifetime residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 0.28 ppm Group 2: 0.38 ppm Group 3: 1.06 ppm Group 4: 1.43 ppm |
|
| Outcomes | Dental fluorosis (Dean's Index; CFI) Age at assessment: 8‐21 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Children selected from Ombill Primary School and divided into groups according into place of birth and ethnicity |
| Confounding | High risk | Imbalance in oral health behaviour and duration of residency between ethnic groups |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for in analysis |
| Selective reporting (reporting bias) | Low risk | Outcome data fully reported |
| Other bias | Low risk | No other apparent bias |
Birkeland 2005.
| Methods |
FLUOROSIS STUDY Country of study: Sudan Geographic location: Triet el Biga, Abu Delaig and Abu Groon Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: residence in the village from the age of 1 year Exclusion criteria: not stated Other fluoride sources: not stated Social class: similar socioeconomic conditions Ethnicity: similar ethnicity Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 0.3‐1.4 ppm Group 2: 0.8‐2.2 ppm Group 3: 2‐4.2 ppm | |
| Outcomes | Dental fluorosis (TF Index) Age at assessment: 11‐13 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | The schools were selected from an unspecified sampling frame and insufficient detail was reported to determine how selection of schools took place. However children were selected at random from the schools |
| Confounding | High risk | No details were reported on the use of fluoride from other sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | High risk | There is inconsistency in the number of water samples tested (Triet el Biga = 6, Abu Delaig = 11, Abu Groon = 8) and an overlap in range of fluoride concentrations between the 3 study areas. Also examinations were done by a dental assistant and it is not clear whether reliability testing was carried out |
Blinkhorn (unpublished).
| Methods |
CARIES STUDY Country of study: Australia Geographic location: Gosford city (newly‐F); Wyong Shire (F); Ballina and Byron (non‐F) Year study started: 2008 Year study ended: 2012 Year of change in fluoridation status: 2008 Study design: ITS |
|
| Participants | Inclusion criteria: children aged 5‐7 years (data for 10‐ to 12‐year olds also provided) Exclusion criteria: not stated Other fluoride sources: information on toothbrushing habit was collected, but not reported in details Social class: Shires of Ballina and Byron were more rural and less industrialised than Wyong Shire and Gosford CityInformation on parent's educational attainment and cardholder status was recorded, but not reported in details Ethnicity: aboriginal status was recorded, but not reported in details Residential history: not stated Other confounding factors: information on sugary drink was collected, but not reported in details |
|
| Interventions | Group 1: fluoridated (data not included in review) Group 2: newly fluoridated Group 3: non‐fluoridated |
|
| Outcomes | dmft; DMFT; % caries free (deciduous dentition); % caries free (permanent dentition) Age at baseline measure: 5‐7 years Age at final measure: 5‐7 years |
|
| Funding | Centre for Oral Health Strategy, New South Wales Health, the Australian Dental Association (New South Wales Branch) and Northern Sydney and Central Coast Local Health Service | |
| Notes | All data unpublished | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Children were drawn from Catholic and state schools in the 3 areas and schools were randomly selected from a master list until the individual school rolls for primary school children aged 5‐7 years added up to around 900 |
| Confounding | High risk | Multivariate analysis of dmft was done taking educational attainment of parents, toothbrushing behaviour and sugary drink consumption into account, however this was done by year, not by study area, and there was insufficient information to determine whether these confounding factors were balanced across study groups |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Though response rate was unbalanced across groups, data were presented for all examined participants |
| Selective reporting (reporting bias) | High risk | Standard deviation not reported |
| Other bias | Low risk | No other apparent bias |
Booth 1991.
| Methods |
FLUOROSIS STUDY Country of study: England Geographic location: Huddersfield (F); Dewsbury (non‐F) Year of study: 1989 Year of change in fluoridation status: 1989 Study design: cross‐sectional |
|
| Participants | Inclusion criteria: all 3‐year‐old white children; lifetime residents of study areas; positive informed consent Exclusion criteria: children who had moved out of the area; children who were ill; children taking fluoride tablets Other sources of fluoride: children taking fluoride tablets excluded from study Social class: areas matched using socioeconomic data from the 1981 census and recent unemployment data; parents asked about occupation of head of household during interview Ethnicity: white children only Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | Group 1: 1 ppm (artificial fluoridation) Group 2: < 0.3 ppm (natural fluoridation) | |
| Outcomes | Dental fluorosis (modified developmental defects of enamel index), caries data evaluated in study but excluded from review due to study design Age at assessment: 3 years |
|
| Funding | North Western Regional Health Authority | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Eligible children were identified from a list of all children in the health district and were randomly sampled from each population. The numbers required were based on a pilot study (no reference provided). No further details reported |
| Confounding | Low risk | Fluoride from other sources was controlled for using inclusion/exclusion criteria and there was no significant difference in SES between the groups |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data were presented for the majority of those recruited (attending appointments) |
| Selective reporting (reporting bias) | Low risk | All expected data reported |
| Other bias | Low risk | No other apparent bias |
Brothwell 1999.
| Methods | FLUOROSIS STUDY Country of study: Canada Geographic location: Wellington and Dufferin (neighbouring counties), South‐Western Ontario Year of study: 1996‐1997 (academic year) Year of change in fluoridation status: NA Study design: cross‐sectional | |
| Participants | Inclusion criteria: children resident in Wellington‐Dufferin‐Guelph Health Unit area; parental consent; children aged 7‐8 years Exclusion criteria: children with non‐erupted or insufficiently erupted central incisors; children absent on day of examination Other sources of fluoride: amount of toothpaste usually used ("48.9% use > pea sized amount, 365/747"); fluoride supplements ("14.5% take supplements, 107/740"); age started brushing; use of mouthwash ("4% routinely use fluoridated mouthwash, 30/752"); breast/bottle fed; whether toothpaste used when brushing Social class: household income; highest level of education received. "It is likely that respondents under‐represented the disadvantaged segment of the population. How the low response rate in this subgroup affects the estimates of prevalence is unknown; however, it is unlikely to be a major source of bias." Ethnicity: not stated Residential history: "The questionnaire assessed … years at current residence", 39% lifelong residents (293/752); 64.8% (487/752 resided at tested source from before the age of 3 (fluorosis‐sensitive period – multivariate analysis restricted to these 487 participants) Other confounding factors: breast‐feeding duration |
|
| Interventions | Group 1: ≥ 0.7 ppm (natural fluoridation) Group 2: < 0.7 ppm (natural fluoridation) | |
| Outcomes | Dental fluorosis (TSIF score > 1) Age at assessment: 7‐8 years | |
| Funding | Not stated | |
| Notes | Data extracted from Brothwell 1999 differs from that presented in CRD review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Children were selected via schools, however insufficient detail was reported regarding sampling |
| Confounding | High risk | Bivariate analysis showed that fluoridated mouthwash use and professional fluoride treatments were significantly associated with fluorosis prevalence, however, the data were not reported/presented in a manner which demonstrated adjustment for imbalance at baseline occurred, or was measured well and controlled for |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Testing of water samples for fluoridation level was conducted after screening examination (at the University of Toronto); examinations conducted by a single dental hygienist (in school clinics). It does not appear that, despite the lack of any attempt to blind being reported, that blinding would have had any effect on reducing bias |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Significant missing data (e.g. 34 participants from the water sample) |
| Selective reporting (reporting bias) | High risk | Comment: there is much that is either not reported in a sufficient manner to be able to glean the necessary information from (i.e. TSIF scores against fluoridation levels of water samples), or has significant missing data (e.g. 34 participants from the water sample) and so is difficult to draw the conclusions required for this review. No evidence of protocol in advance of obtaining data/undertaking analysis |
| Other bias | Low risk | Reporting dental fluorosis as TSIF score > 1 rather than ≥ 1 puts the results at risk of misclassification bias |
Brown 1965.
| Methods | CARIES STUDY Country of study: Canada Geographic location: Brantford (F); Stratford (natural F); Sarnia (non‐F), Ontario Year study started: 1948 Year study ended: 1959 Year of change in fluoridation status: 1945 Study design: CBA | |
| Participants | Inclusion criteria: children aged 9‐14 years; lifetime residents (absence of < 6 weeks since birth); all primary and secondary schools in study areas Exclusion criteria: none stated Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions |
Initiation of water fluoridation Group 1: artifical fluoridation ‐ ppm not stated Group 2: natural fluoridation ‐ ppm not stated Group 3: 'negligible' ‐ ppm not stated (natural fluoridation) |
|
| Outcomes | DMFT, % caries‐free subjects (permanent teeth) Age at baseline measure: 9‐11 years and 12‐14 years Age at final measure: 9‐11 years and 12‐14 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | The study sample was selected by random sampling (by school and grade) described in "A Suggested Methodology for Fluoridation Surveys in Canada" (Department of National Health and Welfare 1952) |
| Confounding | High risk | Did not account for use of other fluoride sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Children 6‐8 years were sampled and initially examined up until 1957, but were no longer included after 1957 as no significant differences were found to exist in that age group |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | Unclear risk | Inorder to maintain a uniform scale of observation, all examinations were done by the same examiner and intra‐examiner, reproducibility not reported |
Budipramana 2002.
| Methods | FLUOROSIS STUDY Country of study: Indonesia Geographic location: 10 villages in Asembagus subdistrict Year of study: 1999 Year of change in fluoridation status: NA Study design: cross‐sectional | |
| Participants | Inclusion criteria: school children aged 6‐12 years who were lifetime residents Exclusion criteria: not stated Other sources of fluoride: not stated Social class: the villages all had identical SES Ethnicity: the villages all had identical ethnic profiles Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 0.51 ppm Group 2: 0.81 ppm Group 3: 2.25 ppm Group 4: 3.16 ppm |
|
| Outcomes | Dental fluorosis (Dean's Index); caries data evaluated in study, but excluded from review due to study design Age at assessment: 6‐12 years | |
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | The authors reported that participants were chosen randomly from 1 selected primary school in each of the 10 villages. However, it is not clear why only 1 school was selected in each village and if the resulting sample was representative |
| Confounding | High risk | The use of other fluoride sources was not considered |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data for all participants was reported |
| Selective reporting (reporting bias) | Low risk | All expected outcome were reported |
| Other bias | High risk | No mention of examiner calibration |
Butler 1985.
| Methods |
FLUOROSIS STUDY
Country of study: USA
Geographic location: 16 Texas communities (selected to reflect a wide range of fluoride levels in drinking water)
Year of study: 1980
Year study ended: 1981 Year of change in fluoridation status: unclear if natural or artifical fluoridation Study design: cross‐sectional |
|
| Participants | Inclusion criteria: lifetime residents of study areas; enrolled in grades 2‐6 (aged 7‐13 years) and 9‐12 (aged 14‐19 years) in public schools Exclusion criteria: none stated Other sources of fluoride: fluoride toothpaste, fluoride drops, number of fluoride treatments Social class: mother's education Ethnicity: white/Spanish/black (ethnicity judged by surname?) Residential history: lifetime residents Other confounding factors: home air‐conditioning; air temperature; number of months breastfed; children in the family; mother's age at child's birth; total dissolved solids in drinking water and zinc in drinking water; age |
|
| Interventions | Unclear as to whether the fluoridation was natural in all areas Group 1: 0.2 ppm Group 2: 0.2 ppm Group 3: 0.3 ppm Group 4: 0.7 ppm Group 5: 1.0 ppm Group 6: 1.0 ppm Group 7: 1.1 ppm Group 8: 1.8 ppm Group 9: 1.9 ppm Group 10: 1.9 ppm Group 11: 2.1 ppm Group 12: 2.1 ppm Group 13: 2.3 ppm Group 14: 2.3 ppm Group 15: 2.4 ppm Group 16: 3.3 ppm | |
| Outcomes | Dental fluorosis (CFI score; prevalence of observed mottling (moderate)) Age at assessment: 7‐19 years | |
| Funding | Supported by grants from the US Environmental Protection Agency | |
| Notes | Data extracted from Butler 1985 differs from that presented in CRD review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | All eligible children were invited to participate |
| Confounding | Unclear risk | While some confounders were measured well and some controlled for in the analysis, it is not clear whether the necessary adjustment was done to the data relevant to this review |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | High risk | Comment: reporting balanced across all groups; however not all data presented in a form that can be interrogated. Despite collecting data on the CFI’s 6 categories of severity of mottling, only data for moderate mottling was presented independently of the overall CFI score for each group. Furthermore, identified confounders were not presented for each group, but for the portion of the study sample as a whole (despite being possible from authors having collected the data) |
| Other bias | High risk | Each child received a dental examination performed by one of the authors, however, calibration was not mentioned |
Chandrashekar 2004.
| Methods |
FLUOROSIS STUDY Country of study: India Geographic location: Davangere district Year of study: 2002 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: lifetime residency; age 12‐15 years Exclusion criteria: not stated Other fluoride sources: not stated Social class: similar socioeconomic conditions Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 0.22 ppm Group 2: 0.43 ppm Group 3: 0.74 ppm Group 4 0.93 ppm Group 5: 1.1 ppm Group 6: 1.22 ppm Group 7: 1.63 ppm Group 8: 2.08 ppm Group 9: 2.33 ppm Group 10: 2.64 ppm Group 11: 2.91 ppm group 12: 3.41 ppm | |
| Outcomes | Dental fluorosis (TF Index) Age at assessment: 12‐15 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Villages satisfying eligibility criteria were selected randomly and children were accessed via schools. It is not clear, however, how the children within the schools were selected |
| Confounding | High risk | No details were reported on the use of fluoride from other sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The number of participants analysed was not reported |
| Selective reporting (reporting bias) | High risk | Dean's fluorosis index was measured but not reported |
| Other bias | Low risk | No other apparent bias |
Chen 1989.
| Methods |
FLUOROSIS STUDY Country of study: Taiwan Geographic location: Shenkang Hsiang, Changwa Year of study: 1987‐1988 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: children aged 6‐16 years; lifetime residents of study areas; always used water wells as primary source of drinking water Exclusion criteria: not stated Other fluoride sources: not stated Social class: not stated Ethnicity: not stated Residential history: lifetime residents Other confounding factors: author states that project communities had approximately the same location, climate, diet, food habits and customs, mean average daily temp = 25 oC, range = 13 oC‐37 oC |
|
| Interventions | All natural fluoridation Group 1: 4.2‐4.9 ppm Group 2: 2.1‐2.8 ppm Group 3: 1.4‐2.1 ppm Group 4: 0.7‐1.4 ppm Group 5: 0.4‐0.7 ppm Group 6: < 0.4 ppm | |
| Outcomes | Dental fluorosis prevalence (Dean's Index); caries data evaluated in study but not included in review due to study design Age at assessment: 6‐16 years |
|
| Funding | National Science Council, Taiwan, ROC (NSC‐77‐0412‐B‐039‐05) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | All eligible participants in the were included in the study |
| Confounding | High risk | Did not account for use of other fluoride sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 5172 children recruited and examined, however, data presented for 5072 participants. Unclear if missing data balanced across groups |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | Unclear risk | Examiners were calibrated before actual assessments of caries and fluorosis were initiated, however, kappa values were not reported |
Chen 1993.
| Methods |
FLUOROSIS STUDY Country of study: China Geographic location: Anquan village (low F); Hubei village (high F), Fenshun county, Guangdong Province Year of study: 1984 Year study ended: 1991 Year of change in fluoridation status: 1984 Hubei, 1986 Anquan Study design: before‐and‐after |
|
| Participants | Inclusion criteria: native born children aged 8‐12 years for dental fluorosis Exclusion criteria: not stated Other sources of fluoride: not stated Social class: author stated that economic and living habits were similar in all study areas Ethnicity: not stated. Residential history: only native born children were assessed. Other confounding factors: not stated |
|
| Interventions | Water source from wells changed to river water Group 1: Hubei 4.1 mg/l (1984 pre‐intervention – natural from wells); 0.8 mg/l (1984 at point of intervention – natural from river); 3.1 mg/l*(1991, 7 years post‐intervention – natural from river) * Increase due to damaged walls of well at bottom of river bed allowing hot spring water with high fluoride content to amalgamate. No regular monitoring took place after changing water supply and therefore unclear when water fluoride content increased in Hubei Group 2: Anquan 12.5 mg/l (1984 pre‐intervention – natural from wells); 0.3 mg/l (1986 at point of intervention – natural from river); 0.4 mg/l (1991, 5 years post‐intervention – natural from river) |
|
| Outcomes | Dental fluorosis (Dean's Index); skeletal fluorosis Age at baseline measure: 8‐12 years (dental fluorosis) and 16‐65 years (skeletal fluorosis) Age at final measure: 8‐12 years (dental fluorosis) and 16‐65 years (skeletal fluorosis) |
|
| Funding | Not stated | |
| Notes | Data extracted from Chen 1993 differs from that presented in CRD review Discrepancies between text and table with regard to fluoride concentration |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | All eligible children were included in the study examined for dental fluorosis and for skeletal fluorosis, adults aged 16‐65 years were randomly sampled to have roentgenograms taken in pelvis |
| Confounding | High risk | Did not account for use of other fluoride sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | For both study areas, n = 800 (Anquan) and n = 1331 (Hubei), however, data not reported for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | High risk | No mention of examiner calibration. Also, quote: "by investigation, it was found that the walls of the well for storing water at the bottom of river bed and water pipe were damaged, the hot spring water with high fluoride content gushed into the well and pipe. Because there was no regular monitoring on the water fluoride after changing water sources, it was unclear when the water fluoride content increased in Hubei". |
Clark 1993.
| Methods |
FLUOROSIS STUDY Country of study: Canada Geographic location: Kelowna (F); Vernon (non‐F), British Columbia Year of study: not stated Year of change in fluoridation status: 1954 Study design: cross‐sectional |
|
| Participants | Inclusion criteria: children in selected schools Exclusion criteria: children with fixed orthodontic appliances; missing anterior teeth Other sources of fluoride: not stated Social class: 2 communities selected because of regional and socioeconomic similarities Ethnicity: not stated Residential history: information recorded in questionnaire and verified by telephone, but doesn't appear to have been prohibitive for inclusion in study Other confounding factors: 274 participants had been exposed to fluoride supplements |
|
| Interventions | Group 1: 1.2 ppm (artificial fluoridation) Group 2: < 0.1 ppm (natural fluoridation) | |
| Outcomes | Dental fluorosis (TSIF) Age at assessment: school age | |
| Funding | Supported by the British Columbia Health Research Foundation | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Primary schools were stratified into low, medium and high SES categories from a specified sampling frame. Schools were then randomly selected and all eligible children within the selected schools were included in the studies |
| Confounding | High risk | Did not account for use of other fluoride sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | High risk | Kappa value of 0.44 suggests a moderate degree of inter‐examiner agreement |
Clarkson 1989.
| Methods |
FLUOROSIS STUDY Country of study: Ireland and England Geographic location: Cork (low and high F; 2 separate areas) and Manchester (low F) Year of study: not stated Year of change in fluoridation status: not stated Study design: cross‐sectional |
|
| Participants | Inclusion criteria: children aged 8 and 15 years Exclusion criteria: not stated Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: not stated Other confounding factors: not stated |
|
| Interventions | Group 1: 'optimal' level ‐ ppm not stated (artificial fluoridation) Group 2: 'low' level ‐ ppm not stated (natural fluoridation) Gruop 3: 'low' level ‐ ppm not stated (natural fluoridation) | |
| Outcomes | Enamel defects (DDE) Age at assessment: 8 and 15 years |
|
| Funding | Not stated | |
| Notes | Data extracted from Clarkson 1989 differs from that presented in CRD review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Sampling was by stratified random selection of eligible children in the study areas. Stratification based on school size and gender |
| Confounding | High risk | Did not account for the use of other fluoride sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | To assess reproducibility, 46 children were examined twice without the examiner's knowledge, however, there is no indication of the examiner being blind to fluoridation status of participants |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest was fully reported and balanced across groups |
| Other bias | Low risk | No other apparent bias |
Clarkson 1992.
| Methods |
FLUOROSIS STUDY
Country of study: Ireland Geographic location: Ireland Year of study: 1984 Year of change in fluoridation status: 1964 Study design: cross‐sectional |
|
| Participants | Inclusion criteria: children aged 8 and 15 years Exclusion criteria: none stated Other sources of fluoride: increase in use of fluoride‐containing toothpaste and infant formula made with fluoridated water Social class: not stated Ethnicity: not stated Residential history: not stated Other confounding factors: problems of consistent levels in the fluoridated supply during the 1960s and early 1970s |
|
| Interventions | Group 1: 'optimal' level ‐ ppm not stated (artificial fluoridation) Group 2: 'low' level ‐ ppm not stated (natural fluoridation) | |
| Outcomes | Dental fluorosis (Deans Index); enamel defects (DDE) Age at assessment: 8 and 15 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | A stratified proportional random sampling procedure was used with size of school with fluoridation status and sex as stratifying factors |
| Confounding | High risk | Did not account for the use of other fluoride sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The number of participants recruited was not reported and there was a variation in the number of children examined for enamel defects and children interviewed on perception of defects. It is not clear whether data were presented for all recruited participants |
| Selective reporting (reporting bias) | High risk | Data not in suitable format for analysis |
| Other bias | Low risk | No other apparent bias |
Cochran 2004a.
| Methods |
FLUOROSIS STUDY Country of study: Ireland, England, Greece, Netherlands, Finland, Iceland, and Portugal Geographic location: Cork, Haalem, Athens, Reykjavik, Oulu, Knowsley, Almada/Setubal Year of study: 1997‐1998 Year of change in fluoridation status: varies Study design: cross‐sectional |
|
| Participants | Inclusion criteria: not stated Exclusion criteria: not stated Other sources of fluoride: information about use of fluoride supplements, age at which toothpaste was first used and the amount and type of toothpaste used were collected but not reported Social class: the sampling ensured a wide socioeconomic spread of participants Ethnicity: not stated Residential history: parents were given questionnaires to supply information on history of living a fluoridated area. No further details reported Other confounding factors: not stated |
|
| Interventions | Group 1: < 0.01 ppm (natural fluoridation) Group 2: 0.05 ppm (natural fluoridation) Group 3: 0.08 ppm (natural fluoridation) Group 4: < 0.1 ppm (natural fluoridation) Group 5: 0.13 ppm (natural fluoridation) Group 6: 1 ppm (artificial fluoridation) | |
| Outcomes | Dental fluorosis (TF Index); enamel defects (DDE) Age at assessment: 8 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | The sampling frame was specified, but the eligibility criteria were not stated. It is not clear whether the number of children photographed as a percentage of the total population of children in the age group (12‐23%) is representative |
| Confounding | High risk | Data were collected on the use of fluoride from other sources but not reported on |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Fluorosis was assessed using photographs and was done without reference to the area from which they were collected |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "A total of 5250 transparencies was taken, of which 114 (2.2%) were not suitable for analysis" Unlikely to influence results |
| Selective reporting (reporting bias) | Unclear risk | Outcome of interest fully reported, however data relating to confounding variables was collected but not reported |
| Other bias | Unclear risk | Reliability testing was carried out. The Kappa statistic from all the study sites showed substantial to excellent agreement with the 'gold standard', except for one study site that showed moderate agreement (0.49; Cochran 2004b). It is not clear what effect this moderate agreement would have on the results given that agreement at the other study sites was substantial to excellent |
Colquhoun 1984.
| Methods |
FLUOROSIS STUDY Country of study: New Zealand Geographic location: Auckland Year of study: 1983 Year of change in fluoridation status: 1953 Study design: cross‐sectional |
|
| Participants | Inclusion criteria: school children aged 7‐12 years Exclusion criteria: children with mottling who were known to have grown up in areas with different fluoridation status from the place in which they were examined Other sources of fluoride: fluoride toothpaste use accounted for 76% of toothpaste sales in New Zealand in 1980. Though there had been a marked increase in fluoride toothpaste use since 1970, there was no trend toward a greater severity of dental fluorosis among younger children Social class: results stratified on social class ‐ incidence of advanced dental fluorosis inversely related to social class but prevalence of dental fluorosis slightly higher in lower social class Ethnicity: ethnic composition of study areas was similar except for higher proportion of Maori and Pacific Island people in the lower socioeconomic areas Residential history: proportion of children at each clinic who were not life‐long residents of the suburb was not ascertained, but there was no reason to suppose that proportions differed between areas Other confounding factors: not stated |
|
| Interventions | Group 1: 1 ppm (artificial fluoridation) Group 2: 'low' level ‐ ppm not stated (natural fluoridation) | |
| Outcomes | Dental fluorosis (diffuse opacities) Age at baseline measure: 7‐12 years |
|
| Funding | Not stated | |
| Notes | Data extracted from Colquhoun 1984 differs from that presented in CRD review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | A population of 458 school children in the fluoridated area had initially been investigated, so the author made further observations on school children of the same age in 6 additional dental clinics chosen at random. An additional 342 children of same age were examined from the non‐fluoridated area, but how they were selected was not reported |
| Confounding | High risk | Some children had used fluoride tablets, but were not excluded from the analysis. The fluoridated area had participants that were of low, middle and high SES while the non‐fluoridated area had only participants of low SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | High risk | Data not in suitable format for analysis |
| Other bias | High risk | Intra‐ and inter‐examiner reliability not mentioned |
Correia Sampaio 1999.
| Methods |
FLUOROSIS STUDY Country of study: Brazil Geographic location: rural areas of Paraiba Year of study: 1997 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: lifetime residents of study areas; children attending public schools (aged 6‐11 years) Exclusion criteria: children who refused to be examined; those without permanent teeth; undetermined place of birth Other sources of fluoride: no topical or systemic fluoride programme implemented in schools; children interviewed about oral health habits and use of toothpaste Social class: all study areas were of low socioeconomic status Ethnicity: not stated Residential history: lifetime residents Other confounding factors: nutritional status |
|
| Interventions | Group 1: > 1.0 ppm (natural fluoridation) Group 2: 0.7‐1.0 ppm (natural fluoridation) Control: < 0.7 ppm (natural fluoridation) | |
| Outcomes | Dental fluorosis (TF Index) Age at assessment: 6‐11 years |
|
| Funding | Brazilian Ministry of Education CAPES (1666/95‐4) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | All eligible children attending schools in the study area were included |
| Confounding | Unclear risk | It was reported that the areas of study were generally low SES. Data were collected on the use of fluoride toothpaste and brushing habits, but showed that those brushing their teeth less frequently had higher levels of fluorosis. It was also reported that the levels of fluorosis in the area had not changed since the introduction of fluoride toothpastes |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest was fully reported and balanced across groups |
| Other bias | Low risk | No other apparent biases |
Cutress 1985.
| Methods |
FLUOROSIS STUDY Country of study: New Zealand Geographic location: Auckland, Frankton and Rodney Year of study: not stated Year of change in fluoridation: 1953 Study design: cross‐sectional |
|
| Participants | Inclusion criteria: children returning parental consent forms and completed questionnaires; lifetime residents of study areas; children aged 9 Exclusion criteria: none stated Other sources of fluoride: ingestion of fluoride tablets Social class: not stated Ethnicity: European (80% F; 84% non F); Polynesian (16%F; 11% non‐F); Asian (2% F; 1% Non‐F); Mixed (2% F; 4% non‐F). Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | Group 1: 1.0 ppm (artificial fluoridation) Group 2: < 0.3 ppm (natural fluoridation) | |
| Outcomes | Any enamel defect Age at assessment: 9 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Schools in the fluoridated area were randomly selected. All schools in the control area were selected. No details were reported about how the children were selected for the study |
| Confounding | High risk | There was an imbalance in lifetime residents using fluoride tables in the fluoridated area compared to the non‐fluoridated area. SES was not accounted for |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Children were taken to the examination centre by bus to prevent the examiner from identifying residence or fluoridation status |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest was fully reported on and balanced across groups |
| Other bias | Low risk | No other apparent bias |
Cypriano 2003.
| Methods |
FLUOROSIS STUDY Country of study: Brazil Geographic location: Porto Feliz, Ipero, Itaoca and Barra do Chapeu (F); Bom Sucesso do Itarare and Itapirapua Paulista (non‐F) Year of study: 2003 Year of change in fluoridation status: 1981 Study design: cross‐sectional |
|
| Participants | Inclusion criteria: pre‐school children aged 5‐6 years and students aged 7‐12 years Exclusion criteria: individuals outside the 5‐12 years age bracket Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: not stated Other confounding factors: not stated |
|
| Interventions | Group 1: 'optimal' level ‐ ppm not stated (artificial fluoridation) Group 2: 'low' level ‐ ppm not stated (natural fluoridation) | |
| Outcomes | Dental fluorosis (Community Fluorosis Index) Age at assessment: 5‐12 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | 7 out of 48 counties were randomly selected by raffle, based on size and the presence or absence of fluoridated water. Children were then randomly selected from schools |
| Confounding | High risk | Did not account for the use of other fluoride sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data for all participants appears to be presented |
| Selective reporting (reporting bias) | High risk | Fluorosis data were not reported for children between 5 and 6 years and no explanations were provided. |
| Other bias | Low risk | No other apparent bias |
de Crousaz 1982.
| Methods |
FLUOROSIS STUDY Country of study: Switzerland Geographic location: Bale‐Ville (F); Friburg and Neuchatel (non‐F) Year of study: 1979 Year of change in fluoridation status: 1961 Study design: cross‐sectional |
|
| Participants | Inclusion criteria: not stated for control areas, for fluoride area only Exclusion criteria: children born outside Switzerland Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | Group 1: 1 ppm (artificial fluoridation) Group 2: 'low' level ‐ ppm not stated (natural fluoridation) | |
| Outcomes | Dental fluorosis (TFI) Age at assessment: 6‐13 years |
|
| Funding | Subsidy from SSO research funds | |
| Notes | Data extracted from de Crousaz 1982 differs from that presented in CRD review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | The children were accessed via schools, however the sampling frame was unspecified |
| Confounding | High risk | Did not account for the use of other fluoride sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Examiners worked independently without knowledge of the origin of the children |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Data were not presented for all participants and missing outcome data varied greatly across study groups |
| Selective reporting (reporting bias) | High risk | Data not in suitable format for analysis |
| Other bias | High risk | Examiners were calibrated and trained but kappa values for reliability not reported. The authors assume that a combination of clinical and photographic examination are sufficient for the verification of intra‐and inter‐examiner reproducibility, so kappa values may not have been calculated |
DHSS England 1969.
| Methods |
FLUOROSIS STUDY Country of study: England Geographic location: Watford (F); Sutton (non‐F) Year of study: 1956 Year study ended: 1967 Year of change in fluoridation status: 1956 Study design: CBA |
|
| Participants | Inclusion criteria: lifetime residents of study areas; consumed piped water at home and at school Exclusion criteria: children that were not continuous residents Other sources of fluoride: none stated Social class: none stated, however, study areas and associated control area had be situated near to each other and be of the same character (e.g. industrial, semi‐industrial, rural or residential) Ethnicity: none stated Residential history: lifetime residents Other confounding factors: information on oral hygiene was recorded |
|
| Interventions |
Initiation of water fluoridation Group 1 at baseline: 'low' level ‐ ppm not stated (natural fluoridation) Group 1 post intervention: 0.89‐0.99 ppm (artificial fluoridation) Group 2: 'low level' ‐ ppm not stated (natural fluoridation) |
|
| Outcomes | dmft, DMFT, % caries‐free subjects (deciduous teeth), % caries‐free subjects (permanent teeth) Age at baseline measure: 3‐14 years Age at final measure: 3‐14 years | |
| Funding | Not stated | |
| Notes | Data extracted from DHSS England 1969 differs from that presented in CRD review (additional data extracted) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Representative groups of children of all ages included in the study were examined in each area and as far as possible the same standards of examination were maintained in the pairs of areas for which the dental findings were to be compared (HMSO 1962) |
| Confounding | High risk | No details were reported on the use of fluoride from other sources or on the dietary habits of the children |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data for all participants appears to have been presented |
| Selective reporting (reporting bias) | High risk | Enamel defects, white or stained, which might be confused with fluoride mottling were also noted but not presented in the report; standard deviation not reported |
| Other bias | High risk | No mention of calibration and reliability testing of the examiners |
DHSS Scotland 1969.
| Methods | CARIES STUDY Country of study: Scotland Geographic location: Kilmarnock (F); Ayr (non‐F) Year study started: 1961 Year study ended: 1968 Year of change in fluoridation status: 1956 Study design: cBA | |
| Participants | Inclusion criteria: lifetime residents of study areas; consumed piped water at home and at school Exclusion criteria: not stated Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: continuous residents Other confounding factors: not stated |
|
| Interventions |
Initiation of fluoridation Group 1: 1 ppm (artificial fluoridation) Group 2: 'low' level ‐ ppm not reported (natural fluoridation) |
|
| Outcomes | dmft, % caries‐free subjects (primary teeth) Age at baseline measure: 5 years Age at final measure: 5 years | |
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Representative groups of children of all ages included in the study were examined in each area and as far as possible the same standards of examination were maintained in the pairs of areas for which the dental findings were to be compared (HMSO 1962) |
| Confounding | High risk | The effect of sugary diet consumption and use of fluoride from other sources were not taken into account |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blind outcome assessment not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | A cross‐section of children were examined each year, together with some children in nurseries and nursery schools, but findings for the later were not presented |
| Selective reporting (reporting bias) | High risk | Enamel defects, white or stained, which might be confused with fluoride mottling were also noted but not presented in the report; standard deviation not reported |
| Other bias | High risk | No mention of calibration of examiners and reliability testing |
DHSS Wales 1969.
| Methods | CARIES STUDY Country of study: Wales Geographic location: Gwalchmai zone (F); Holyhead (mainly F ‐ gets most of water from Gwalchmai, but occasionally also receives water from Bodafon); and Bodafon zone (non‐F) Year study started: 1956 Year study ended: 1965 Year of change in fluoridation status: 1955 Study design: CBA | |
| Participants | Inclusion criteria: continuous residents of study areas; consumed piped water both at home and school; up to 15 years (Gwalchmai and Bodafon); up to 11 years (Holyhead) Exclusion criteria: not stated Other sources of fluoride: not stated Social class: none stated, however, study areas and associated control area had be situated near to each other and be of the same character (e.g. industrial, semi‐industrial, rural or residential) Ethnicity: not stated Residential history: continuous residents Other confounding factors: information on oral hygiene was recorded |
|
| Interventions |
Initiation of water fluoridation Group 1 baseline: 'low' level ‐ ppm not stated (natural fluoridation) Group 1 post intervention: 0.8‐0.9 ppm (artificial fluoridation) Group 2 baseline: 'low' level ‐ ppm not stated (natural fluoridation) Group 2 post intervention: 0.8‐0.9 ppm (artificial fluoridation) Group 3: 'low' level ‐ ppm not stated (natural fluoridation) |
|
| Outcomes | dmft, DMFT, % caries‐free subjects (deciduous teeth), % caries‐free subjects (permanent teeth) Age at baseline measure: 3‐14 years Age at final measure: 3‐14 years | |
| Funding | Not stated | |
| Notes | Data extracted from DHSS Wales 1969 differs from that presented in CRD review (additional data extracted) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Pre‐school children examined were a reasonably good cross‐section of Anglesey children of that age, however, different age criteria were used for school children in different study areas (up to 15 years in Gwalchmai and Bodafon; up to 11 years in Holyhead). The reason for this was not reported. (HMSO 1962) |
| Confounding | High risk | No details were reported on the use of fluoride from other sources or on the dietary habits of the children |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data for all participants appears to be presented |
| Selective reporting (reporting bias) | High risk | Enamel defects, white or stained, which might be confused with fluoride mottling were also noted but not presented in the report |
| Other bias | High risk | No mention of calibration and reliability testing of examiners |
Downer 1994.
| Methods |
FLUOROSIS STUDY Country of study: England, Scotland and Ireland Geographic location: Dublin (F); north London, Edinburgh and Glasgow (non‐F) Year of study: not stated Year of change in fluoridation status: 1965 Study design: cross‐sectional |
|
| Participants | Inclusion criteria: children aged 12 years; lifetime residents of study areas Exclusion criteria: not stated Other sources of fluoride: not stated Social class: not stated, however, sampling in the fluoridated areas was done to achieve a mix of participants from different SES Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | Group 1: 0.9 ppm (artificial fluoridation) Group 2: 'low' level ‐ ppm not stated (natural fluoridation) Group 3: 'low' level ‐ ppm not stated (natural fluoridation) Group 4: 'low' level ‐ ppm not stated (natural fluoridation) | |
| Outcomes | Enamel defects (DDE); caries data also evaluated within the study but excluded from review due to study design Age at assessment: 12 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | 25% of the secondary schools in Glasgow and Dublinwere randomly selected to participate, and participants were selected at random. Sampling in London was aimed at examining all 12‐year‐old children in secondary schools in 3 districts and 14 out of 19 schools. The reason for non‐participation of 5 out of the 19 eligible schools in the non‐fluoridated area was logistical and the authors state that this was (Quote:) “unlikely to have caused sampling bias”. In Edinburgh a random selection of 20% of children in 20 out of 50 eligible schools, drawn at random, formed the sample |
| Confounding | High risk | No details were reported on the use of fluoride from other sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | High risk | Data not in suitable format for analysis |
| Other bias | Low risk | No other apparent bias |
Driscoll 1983.
| Methods |
FLUOROSIS STUDY Country of study: USA Geographic location: 7 rural Illinois communities within 75 miles of each other Year of study: 1980 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: children in grades 3‐10 (age 8‐16 years); lifetime residents of study areas; consumed public water Parental consent Exclusion criteria: not stated Other sources of fluoride: not stated Social class: relatively small, rural communities chosen because they shared several similar characteristics Ethnicity: < 5% non white Residential history: lifetime residents Other confounding factors: same climatic zone |
|
| Interventions | Group 1: 3.84‐4.07 ppm (natural fluoridation) Group 2: 2.84‐3.77 ppm (natural fluoridation) Group 3: 2.08 ppm (natural fluoridation) Group 4: 1.06 ppm (natural fluoridation) | |
| Outcomes | Dental fluorosis (Dean's Index; CFI; TSIF was also used but reported in a later paper); caries data were measured but excluded from this review due to study design Age at assessment: 8‐16 years |
|
| Funding | Not stated | |
| Notes | None of the communities had made any change in its water source that was likely to alter the fluoride concentration during the period relevant to the study | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | There was insufficient detail reported to determine how selection took place |
| Confounding | High risk | Did not account for the use of other fluoride sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Different examiners carried out measurements in order to avoid bias, however, this may not have been sufficient to avoid detection bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All findings were based only on those children assessed for both fluorosis and majority of the children fall under this category. Also, the higher‐than‐optimal study area had considerably fewer children compared to the other areas due to small size of the communities and other similar communities in same geographic area were not available. This was not considered sufficient to introduce bias |
| Selective reporting (reporting bias) | High risk | Data not in suitable format for analysis |
| Other bias | Low risk | No other apparent bias |
Ekanayake 2002.
| Methods |
FLUOROSIS STUDY Country of study: Sri Lanka Geographic location: Uda Walawe Year of study: 2001 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: completion of the 14th but not the 15th birthday; availability in school on the day of the examination Exclusion criteria: not stated Other sources of fluoride: not stated Social class: almost all belonged to the low socioeconomic group Ethnicity: not stated Residential history: resident at present address since birth Other confounding factors: no details reported; nearly 75% of the subjects had used fluoride toothpaste from the age of about 9‐12 months (discussion section) |
|
| Interventions | All natural fluoridation Group 1: ≤ 0.3 ppm Group 2: 0.31‐0.49 ppm Group 3: 0.5‐0.7 ppm Group 4: > 0.7 ppm | |
| Outcomes | Enamel defect (DDE) Age at assessment: 14 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | 6 schools were selected on the basis of being sufficiently large for study. All eligible children present on day of study were examined |
| Confounding | High risk | While it is stated in the paper that "Less than 75% of the participants started teeth brushing with fluoride toothpaste from 9‐12 months of age", the use of other fluoride sources was not controlled for, neither was it reported by fluoridation status |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 6.25% of the children examined were not included in the analysis. The authors did not report their fluoride exposure, and it is not clear whether their exclusion may have introduced bias |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | Low risk | No other apparent bias |
Eklund 1987.
| Methods |
FLUOROSIS STUDY Country of study: USA Geographic location: Lordsburg (high‐F); Deming (lower‐F), New Mexico Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: resident in study areas for the first 6 years of life; subjects aged approximately 30‐60 years old; consumed city water supplies Exclusion criteria: not stated Other sources of fluoride: not stated Social class: areas similar for education and income level; number of years of education similar between areas Ethnicity: Lordsburg: 89.6% = Hispanic; Deming: 74.2% = Hispanic Residential history: residence for the first 6 years of life Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 3.5 ppm Group 2: 0.7 ppm | |
| Outcomes | Dental fluorosis (Dean's Index); caries data also evaluated within the study but excluded from review due to study design Age at assessment: 27‐65 years |
|
| Funding | Not stated | |
| Notes | Data extracted from Eklund 1987 differs from that presented in CRD review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Efforts were made to recruit all eligible adults in all the communities and 80%‐90% of eligible people consented and participated |
| Confounding | High risk | No details were reported on the use of fluoride from other sources |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest was fully reported on and balanced across groups |
| Other bias | Low risk | No other apparent bias |
Ellwood 1995.
| Methods |
FLUOROSIS STUDY Country of study: Ireland and Wales Geographic location: Chester (non‐F); Bala (non‐F); Anglesey (F); Cork (F) Year of study: 1991 Year study ended: not reported Year of change in fluoridation status: NA Study design: cross‐sectional study |
|
| Participants | Inclusion criteria: lifetime residents of study areas (children only); agreement to participate Exclusion criteria: fixed orthodontic appliances Other sources of fluoride: tooth brushing behaviour ‐ age started brushing; weekly tooth brushing frequency Social class: children from all 3 groups were from schools with a similar social profile Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | Group 1: 0.7 ppm (artificial fluoridation) Group 2: 0.9 ppm (artificial fluoridation) Group 3: < 0.1 ppm (natural fluoridation) | |
| Outcomes | Enamel defect (DDE) Age at assessment: 14 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | There was insufficient detail reported to determine how selection took place |
| Confounding | Low risk | SES and reported tooth brushing frequency were similar across groups |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Photographs were taken, identified randomly and examined without reference to subject details |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest was fully reported on and balanced across groups |
| Other bias | Low risk | No other apparent bias |
Ellwood 1996.
| Methods |
FLUOROSIS STUDY Country of study: England and Wales Geographic location: Anglesey (F); Chester and Bala (non‐F) Year of study: 1991 Year of change in fluoridation status: 1955 Study design: cross sectional |
|
| Participants | Inclusion criteria: children in their 3rd year of secondary education; lifelong residents of study areas Exclusion criteria: children with fixed orthodontic appliances; absence at the time of examination Other sources of fluoride: not stated Social class: not stated, however, the schools in the non‐fluoridated areas had similar catchment areas to those from the fluoridated area. No further details reported Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | Group 1: 0.7 (artificial fluoridation) Control: < 0.1 (natural fluoridation) | |
| Outcomes | Dental fluorosis (TF Index); caries data also evaluated within the study but excluded from review due to study design Age at assessment: 14 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | 3 schools from Anglesey were selected and for the control group, schools with catchment areas as similar as possible to those from Anglesey were chosen from Chester and Bala using national census statistics.There was no random selection of schools in Anglesey, and it is not clear whether the selected schools were a representative sample |
| Confounding | High risk | Did not account for the use of other fluoride sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Photographs were taken, randomly mixed and scored without reference to subject details |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest was fully reported on and balanced across groups |
| Other bias | Low risk | No other apparent bias |
Ermis 2003.
| Methods |
FLUOROSIS STUDY Country of study: Turkey Geographic location: Izmir and Isparta Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: lifelong residence; use of the public water supply continuously as source of drinking water; absence of nutrition deficiency Exclusion criteria: not stated Other sources of fluoride: not stated Social class: the selected schools were public secondary schools Ethnicity: not stated Residential history: lifetime residents Other confounding factors: toothbrushing frequency: did not brush = 22 (7.9%); irregularly = 49 (17.6%); once a day = 115 (41.4%); more than once = 92 (33.1%) |
|
| Interventions | All natural fluoridation Group 1: 0.3‐0.4 ppm Group 2: 1.42‐1.54 ppm Group 3: 1.55‐1.66 ppm | |
| Outcomes | Dental fluorosis prevalence (TSIF); caries data also evaluated within the study but excluded from review due to study design due to study design Age at assessment: 12‐14 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | 4 schools were selected using a random sampling technique from a list of all public secondary schools. Within these schools eligible children were selected randomly |
| Confounding | Unclear risk | Toothbrushing habits differed between participants, however it is not clear whether they varied across study groups |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | High risk | Fluorosis prevalence was measured, but only reported for the high fluoride areas and not for the low fluoride area |
| Other bias | Low risk | No other apparent bias |
Firempong 2013.
| Methods |
FLUOROSIS STUDY Country of study: Ghana Geographic location: Bongo district (Zone A: Atampiisi, Soeboko and Aliba; Zone B: Nayire, Boyrigo, Anabisa, Amagre and Tigre; Zone C: Soe, Kuyeligo, and Kunduo; Zone D: Yakanzanway, Gurigo, Ababorobiisi, Zaasi, and Anafobiisi) Year of study: 2008‐2009 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: lived in the area for the first 7 years of childhood; using water from a constant source that could still be traced Exclusion criteria: medically confirmed dental problem different from dental fluorosis; history of tobacco or kola use Other sources of fluoride: information on frequency of toothbrushing (P value 0.101) and type of oral health product (P value 0.179) were collected and there was no difference between the 4 zones Social class: the children had similar educational backgrounds Ethnicity: not stated Residential history: lifetime residents for first 7 years of childhood Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 0.95 ppm Group 2: 1 ppm Group 3: 1.86 ppm Group 4: 2.36 ppm | |
| Outcomes | Dental fluorosis (Dean's Index) Age at assessment: 7‐18 years |
|
| Funding | Supported by the Regional Laboratory of the Ghana Water Company/Aqua Viten Rands Limited in Tamale, Ghana | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Stated that eligible children were randomly selected, but insufficient detail provided to make a clear judgement |
| Confounding | High risk | While there appears to be little difference in the use of oral hygiene habits across groups, did not account for SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | High risk | Quote: "A professional examiner was engaged to carry out all the testing measurements ..." Comment: intra‐examiner reliability test not reported and may not have been conducted |
Forrest 1956.
| Methods |
FLUOROSIS STUDY Country of study: England Geographic location: West Mersey (5.8 ppm); Burnham‐on‐Crouch (3.5 ppm); Harwich (2/1.6 ppm); Slough (0.9 ppm) Saffron Walden and District (non‐F); Stoneleigh and Malden West (non‐F) Year of study: 1954 Year of change in fluoridation status: NA Study design: cross sectional |
|
| Participants | Inclusion criteria: lifetime residents of study areas; children aged 12‐14 years Exclusion criteria: not stated Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 5.8 ppm Group 2: 3.5 ppm Group 3: 2.0 ppm Group 4: 0.9 ppm Group 5: 0.1‐0.2 ppm Group 6: 0.1 ppm | |
| Outcomes | Dental fluorosis (Dean’s Index); caries data also evaluated within the study but excluded from review due to study design due to study design Age at assessment: 12‐14 years |
|
| Funding | Not stated | |
| Notes | Data extracted from Forrest 1956 differs from that presented in CRD review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Areas were selected opportunistically. Entire populations of children in some areas were selected for study but insufficient detail is given on how they were accessed |
| Confounding | High risk | SES and the use of other fluoride sources was not sufficiently reported and controlled for |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Results are presented for the majority of participants. However, while the results are presented in full for 4 of the 5 areas the area of highest F ppm appears to have 10% of participants missing from results |
| Selective reporting (reporting bias) | High risk | Data not in suitable format for analysis |
| Other bias | High risk | There is risk of measurement bias as examiner calibration was not mentioned |
Forrest 1965.
| Methods |
FLUOROSIS STUDY Country of study: Wales Geographic location: Gwalchmai (F); Bodafon (non‐F), Anglesey Year of study: 1963 Year of change in fluoridation status: 1955 Study design: cross‐sectional |
|
| Participants | Inclusion criteria: children aged 8 years from a selection of schools Exclusion criteria: schools in Holyhead; schools in Llangefni and Beaumaris, as changed supply from fluoridated to non‐fluoridated in 1961 Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: not clearly stated, however, the participants were chosen for being the only ones who had had fluoride for most of their lives Other confounding factors: not stated |
|
| Interventions | Group 1: 1 ppm (artificial fluoridation) Group 2: ≤ 0.2 ppm (natural fluoridation) | |
| Outcomes | Outcome: enamel defects Age at assessment: 8 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Schools were selected for study and then children within these schools, however it is not clear how the children were examined |
| Confounding | High risk | SES and the use of fluoride from other sources were not reported on |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The examiners were unaware of the children’s fluoridation status since they all resided in the same county. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest was fully reported on and balanced across groups |
| Other bias | Low risk | No other apparent bias |
Franzolin 2008.
| Methods |
FLUOROSIS STUDY Country of study: Brazil Geographic location: Sao Paulo Year of study: not stated Year of change in fluoridation status: 1975 Study design: cross‐sectional |
|
| Participants | Inclusion criteria: residence in the same geographical area as the school since birth Exclusion criteria: not stated Social class: homogenous population comprising entirely of public school students Ethnicity: white = 243 (67.5%); black = 41 (11.4%); admixture = 73 (20.3%); Asian = 3 (0.8%) Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | Group 1: 'optimal' level ‐ ppm not stated (artificial fluoridation via water treatment station) Group 2: 'optimal' level ‐ ppm not stated (artificial fluoridation via direct fluoridation in well) Group 3: 'low' level ‐ ppm not stated (natural fluoridation) | |
| Outcomes | Dental fluorosis (TF Index); caries data collected, however, excluded from the review due to study design Age at assessment: 12 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Multi‐stage random sampling was used whereby schools were selected randomly and the children within them |
| Confounding | High risk | Did not account for the use of other fluoride sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The examiner and recorder were reported to have been blinded to the type of water supply of the schools |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | High risk | Data not in suitable format for analysis |
| Other bias | Unclear risk | Examinations carried out by a single, previously calibrated examiner, however, kappa score not reported |
Garcia‐Perez 2013.
| Methods |
FLUOROSIS STUDY Country of study: Mexico Geographic location: Morelos Year of study: 2013 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: children who had been born in the community, lived in the community from 1 year of age onwards, or had not moved in or out of the community for more than 6 months Exclusion criteria: systemic diseases requiring premedication; absence on the days of the oral examination; children who had brackets Other sources of fluoride: bottled water often containing 0.3‐0.6 ppm fluoride levels; dentifrice use; number of times brushing teeth per day Social class: both communities had a low socioeconomic level Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 0.56‐0.76 ppm Group 2: 1.45‐1.61 ppm | |
| Outcomes | Dental fluorosis (TF Index); caries data also evaluated within the study but excluded from review due to study design Age at assessment: 12 years |
|
| Funding | Partially funded by the Metropolitan Autonomous University, Xochimilco (Universidad Autonoma Metropolitana, UAM‐X) and the National Council of Science and Technology (Consejo Nacional de Ciencia y Tecnologia, CONACYT) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | There was insufficient detail reported to determine how selection took place |
| Confounding | Low risk | Both villages were of low SES, participants were lifetime residents and there was no difference in toothbrushing frequency or bottled water consumption |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Data presented as percentages making it difficult to determine if all participants are accounted for |
| Selective reporting (reporting bias) | High risk | Fluorosis prevalence was not reported for all severities of dental fluorosis |
| Other bias | Low risk | No other apparent bias |
Gaspar 1995.
| Methods |
FLUOROSIS STUDY Country of study: Brazil Geographic location: Piracicaba (F); Iracemapolis (non‐F) Year of study: not stated Year of change in fluoridation status: 1974 Study design: cross‐sectional |
|
| Participants | Inclusion criteria: children aged 10‐14; lifetime residents of study areas Exclusion criteria: not stated Other sources of fluoride: not stated Ethnicity: not stated Social class: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | Group 1: < 0.2 ppm (natural fluoridation) Group 2: 0.7 ppm (artificial fluoridation) | |
| Outcomes | Dental fluorosis prevalence (TF Index) Age at assessment: 10‐14 years |
|
| Funding | Not stated | |
| Notes | Data from CRD review (unverified data) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Unable to make a judgement as study was unavailable |
| Confounding | High risk | Did not appear to account for the use of other fluoride sources or SES in analysis |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unable to make a judgement as study was unavailable |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unable to make a judgement as study was unavailable |
| Selective reporting (reporting bias) | Unclear risk | Unable to make a judgement as study was unavailable |
| Other bias | Unclear risk | Unable to make a judgement as study was unavailable |
Goward 1982.
| Methods |
FLUOROSIS STUDY Country of study: England Geographic location: 2 adjacent districts of Leeds with different fluoride levels Year of study: 1979 Year of change in fluoridation status: 1968 Study design: cross sectional |
|
| Participants | Inclusion criteria: lifetime residents of study areas (children only); children aged 5 Exclusion criteria: not clear, though children using systemic or topical fluoride supplements were excluded from the study Other sources of fluoride: children using systemic or topical fluoride supplements excluded from the study Social class: not stated Ethnicity: not stated Residential history: lifetime residents Other confounding factors: difference in breast fed vs bottle fed children |
|
| Interventions | Group 1: 0.9 ppm (artificial fluoridation) Group 2: < 0.1 ppm (natural fluoridation) | |
| Outcomes | Dental fluorosis (defined by Al‐Alousi) Age at time of measurement: 5 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | There was insufficient detail reported to determine how selection took place |
| Confounding | High risk | Did not account for SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | High risk | No information on calibration of examiners |
Gray 2001.
| Methods |
CARIES STUDY Country of study: England Geographic location: Dudley (F), Sedgeley and Cosely (F), Halesowen (F), Brierly Hill and Kingswinford (F); Stourbridge (non‐F) Year study started: 1988 Year study ended: 1997 Year of change in fluoridation status: 1987 Study design: CBA |
|
| Participants | Inclusion criteria: children living in study area since 1988 Exclusion criteria: not stated Other sources of fluoride: not stated Social class: participants were all from state‐funded primary schools and might have been socioeconomically similar Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions |
Initiation of water fluoridation Group 1: 1 ppm (artificial fluoridation) Group 2: 1 ppm (artificial fluoridation) Group 3: 1 ppm (artificial fluoridation) Group 4: 1 ppm (artificial fluoridation) Group 5: 0.3 ppm (natural fluoridation) |
|
| Outcomes | % caries free (deciduous teeth) Age at baseline measure: 5 years Age at final measure: 5 years |
|
| Funding | Not stated | |
| Notes | Data extracted from Gray 2001 differs from that from Gray 2000 (unpublished) which was originally presented in CRD review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | According to Pitts 1997, representative samples were drawn from a whole population of Dudley health authority |
| Confounding | High risk | No details were reported on the use of fluoride from other sources or on the dietary habits of the children |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "...blinding was not possible" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome was reported |
| Other bias | High risk | At baseline the fluoridation status of the children was determined by the location of their school |
Grimaldo 1995.
| Methods |
FLUOROSIS STUDY Country of study: Mexico Geographic location: San Luis Potasi Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: lifetime residents at same address; children aged 11‐13 years in selected schools; parental consent Exclusion criteria: not stated Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: lifetime residents Other confounding factors: local diet rich in calcium, reduces fluoride absorption |
|
| Interventions | All natural fluoridation Group 1: > 2.0 ppm Group 2: 1.2‐2.0 ppm Group 3: 0.7‐1.2 ppm Group 4: < 0.7 ppm | |
| Outcomes | Dental fluorosis (Dean's Index) Age at assessment: 11‐13 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | The authors reported that schools and participants from the study areas were selected at random. No further details reported |
| Confounding | High risk | Did not account for the use of other fluoride sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | There was a variation in the numbers of children reported to have been examined for dental fluorosis compared to the number of children initially reported to be receiving different water fluoride levels |
| Selective reporting (reporting bias) | Low risk | Outcome of interest was fully reported on and balanced across groups |
| Other bias | High risk | No indication that the examiners were calibrated |
Grobler 1986.
| Methods |
FLUOROSIS STUDY Country of study: South Africa Geographic location: Nourivier (low F); Tweeriviere (high F) in North Western Cape province Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: lifetime residents of study areas; children aged 12‐13 years Exclusion criteria: not stated Other sources of fluoride: both communities had virtually no dental care or fluoride therapy Social class: similar socioeconomic status in both study areas (reported by authors) Ethnicity: similar ethnicity in both study areas (reported by authors) Residential history: lifetime residents Other confounding factors: areas similar in nutrition and dietary habits (reported by authors); temperature 27 °C‐32 °C |
|
| Interventions | All natural fluoridation Group 1: 3.7 ppm Grpup 2: 0.62 ppm | |
| Outcomes | Outcome: fluorosis prevalence (Deans Index); caries data collected but not presented in this review due to study design Age at assessment: 12‐13 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | All available subjects were included in the study population. Insufficent information was reported on the sampling frame |
| Confounding | Low risk | SES was similar across groups and there was virtually no dental care or fluoride therapy in the population at the time |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information. Examinations were made at the children's schools but no mention of blind assessment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | High risk | Examinations were done by a single examiner but no mention of intra‐examiner calibration |
Grobler 2001.
| Methods |
FLUOROSIS STUDY Country of study: South Africa Geographic location: Leeu Gamka, Kuboes and Sanddrif Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: continuous residence since birth; having virtually no dental care or fluoride therapy including the use of fluoride‐containing toothpaste; absence of any obvious under‐nutrition and no dietary habits that could significantly contribute to the ingestion of fluorine Exclusion criteria: not stated Other sources of fluoride: participants had virtually no dental care or fluoride therapy, including the use of fluoride‐containing toothpaste Social class: similarly low socioeconomic status across groups reflected in the fact that they all lived in sub‐economic housing units Ethnicity: mixed ethnic origin from Khoi, Caucasian and Negroid roots which over hundreds of years have developed into a homogenous ethnic group Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 0.19 ppm Group 2: 0.48 ppm Group 3: 3 ppm | |
| Outcomes | Outcome: fluorosis prevalence (Deans Index); caries data also evaluated within the study but excluded from review due to study design Age at assessment: 10‐15 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | All available children in the specified study areas were examined |
| Confounding | Low risk | SES was similar across groups and there was virtually no exposure to fluoride from other sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | Low risk | No other apparent bias |
Guo 1984.
| Methods |
CARIES STUDY Country of study: Taiwan Geographic location: Chung‐Hsing New Village (F); Tsao‐Tun (non‐F) Year of study: 1971 Year study ended: 1984 Year of change in fluoridation status: 1971 Study design: CBA |
|
| Participants | Inclusion criteria: lifetime residents of study areas Exclusion criteria: children who migrated from other areas during study period Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: lifetime residents Other confounding factors: similar climate with mean daily air temperature of 24 °C |
|
| Interventions |
Initiation of water fluoridation Group 1 baseline: 0.07 ppm (natural fluoridation) Group 1 post intervention: 0.6 ppm (artificial fluoridation) Group 2: 0.08 ppm (natural fluoridation) |
|
| Outcomes | dmft, DMFT, % caries free (deciduous), % caries free (permanent) Age at baseline measure: 5, 8, 12 and 15 years Age at final measure: 5, 8, 12 and 15 years |
|
| Funding | Not stated | |
| Notes | Data extracted from Guo 1984 differs from that presented in CRD review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | All eligible children in the study areas were included in the study |
| Confounding | High risk | Did not account for the use of other fluoride sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | High risk | Examinations were carried out by the dentists from the University hospital and recorded on the same type of record forms but there is no mention of examiner calibration |
Haavikko 1974.
| Methods |
FLUOROSIS STUDY Country of study: Finland Geographic location: Espoo (low F); Elimaki (high F); Hanko (optimal F); Lohja (low F) Year of study: 1969 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: children who had been resident in study areas for the first 6 years of life; children aged 10‐11 years Exclusion criteria: none stated Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: continuous residence for the first 6 years Other confounding factors: food sources of fluoride |
|
| Interventions | All natural fluoridation Group 1: 1.08 ppm Group 2: 0.41 ppm Group 3: 0.11 ppm Group 4: 0.05 ppm | |
| Outcomes | Dental fluorosis (Dean's Index) Age at assessment: 10‐11 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Eligible children were selected at random from the health records. No further details regarding the sampling frame were reported |
| Confounding | High risk | SES and the use of fluoride from other sources were not reported on |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest was fully reported on and balanced across groups |
| Other bias | High risk | Both dentists carried out the diagnosis of enamel defects but there was no mention of examiner calibration |
Harding 2005.
| Methods |
FLUOROSIS STUDY Country of study: Ireland Geographic location: Cork city (F); Cork county (non‐F) Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: age 5 years; location of the school attended and fluoridation status of water supply Exclusion criteria: absence on the day of examination; too apprehensive to participate or < 5 years; incorrectly received a form; incomplete form; existing medical condition Other sources of fluoride: fluoride prevalence of children with different nutritional and brushing habits were reported: breast‐fed = 30 (28%) vs not breast‐fed = 38 (21%); brushing before 12 months: F = 47 (22.6%) vs non‐F = 19 (22.1%); started brushing with toothpaste between 12 and 18 months: F = 79 (38%) vs non‐F = 25 (29.1%); started brushing with toothpaste between 19 and 24 months: F = 37 (17.8%) vs non‐F = 21 (24.4%); started brushing with toothpaste after 24 months: F = 41 (19.7%) vs non‐F = 18 (20.9%) Social class: schools were chosen to provide a socioeconomic spread; 7 urban and 10 rural schools Ethnicity: not stated Residential history: lifetime residents Other confounding factors: food sources of fluoride |
|
| Interventions | Group 1: 0.8‐1 ppm (artificial fluoridation) Group 2: 'low' level ‐ ppm not stated (natural fluoridation) | |
| Outcomes | Dental fluorosis (TSIF) Age at assessment: 5 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | A stratified sample for 5‐year olds was drawn from study areas on the basis of age, location, school attended and fluoridation status. Schools were chosen to provide a socioeconomic spread |
| Confounding | Low risk | SES range (by school) was sampled. There were similar levels of toothpaste use across the groups |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Of the 311 participants examined, outcome data were not presented for 17 participants due to partial fluoride history; unlikely to influence the results |
| Selective reporting (reporting bias) | High risk | Data not in suitable format for analysis |
| Other bias | High risk | Clinical examination was carried out by one examiner trained extensively by a gold standard but no report of calibration nor intra‐examiner reliability tests |
Hardwick 1982.
| Methods |
CARIES STUDY Country of study: England Geographic location: Alsager, Middlewich, Nantwich (F), Northwich (non‐F) Year study started: 1974 Year study ended: 1978 Year of change in fluoridation status: 1975 Study design: prospective cohort |
|
| Participants | Inclusion criteria: 12‐year‐old children living in study area. Consent from relevant country authorities and teachers at schools included in the study Exclusion criteria: none stated Other sources of fluoride: Fluoride group (n = 152): 142 (94%) used only fluoride dentifrices; 125 (83%) used at least once a day Control group (n = 194): 185 (95%) used only fluoride dentifrices; 147 (76%) used at least once a day 2 children in fluoride group and 4 children in control had used fluoride tablets Social class: control and experimental groups matched on urban and rural characteristics Ethnicity: not stated Residential history: not stated Other confounding factors: not stated |
|
| Interventions |
Initiation of water fluoridation Group 1 baseline: < 0.1 ppm (natural fluoridation) Group 1 post intervention: 1.0 ppm (artificial fluoridation) Group 2: < 0.1 ppm (natural fluoridation) |
|
| Outcomes | DMFT, DMSF Age at baseline measure: 12 years Age at final measure: 16 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | All eligible children were invited to participate |
| Confounding | High risk | Use of fluoride from other sources was broadly equal between the groups. The groups were matched on SES however, no information was reported on the dietary habits of the children |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The children were transported to a central examination centre in small numbers and were then randomly mixed with children from the other group. Furthermore, the children were requested not to wear school uniform and, in case they forgot, donned a large operating gown to hide their clothes" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | Low risk | No other apparent bias |
Heifetz 1988.
| Methods |
FLUOROSIS STUDY Country of study: USA Geographic location: 7 rural towns within 75 miles of each other in Illinois Year of study: 1980‐1985 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: children aged 8‐10 and 13‐15 years; continuous residence in study community Exclusion criteria: not stated Other sources of fluoride: food and drinks produced in fluoride areas Social class: study areas shared similar socioeconomic characteristics Ethnicity: not stated Residential history: continuous residence Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 3.8‐4.1 ppm Group 2: 2.8‐3.8 ppm Group 3: 2.1 ppm Group 4: 1.1 ppm | |
| Outcomes | Dental fluorosis (TSIF); caries data also evaluated within the study but excluded from review due to study design Age at assessment: 13‐15 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | There was insufficient detail reported to determine how selection took place |
| Confounding | High risk | Participants consumed food and drinks produced in fluoride areas, however, it is not clear whether there was a difference in consumption among different areas. Insufficient detail is provided regarding use of fluoride from other sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | High risk | Data not in suitable format for analysis |
| Other bias | Low risk | No other apparent bias |
Heintze 1998.
| Methods |
FLUOROSIS STUDY Country of study: Brazil Geographic location: Garca (F); Itrapolis (non‐F), Sao Paulo state Year of study: 1995 Year of change in fluoridation status: 1973 and 1975 Study design: cross‐sectional |
|
| Participants | Inclusion criteria: subjects aged 5‐24 years; from all social strata; used tap water; took urine samples from all 3 daytime periods Exclusion criteria: usbjects that used tap water, otherwise not stated Other sources of fluoride: subjects asked about use of toothpaste or mouth rinses containing fluoride. 98% used toothpaste containing fluoride and 16.5% used a fluoride mouth rinse daily or weekly Social class: cities similar in socioeconomic and sociodemographic conditions, subjects from all social strata included Ethnicity: not stated Residential history: not stated Other confounding factors: Garca altitude = 526 m, mean temp = 22 °C, population = 41,351; Itapolis: altitude = 491 m, mean temp = 23 °C, population = 30, 111 |
|
| Interventions | Group 1: 0.9 ppm (artificial fluoridation) Group 2: 0.02 ppm (natural fluoridation) | |
| Outcomes | Dental fluorosis (TF Index) Age at assessment: 5‐24 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Participants were accessed via health centres, schools and factories and all eligible participants were included in the study |
| Confounding | High risk | Study areas were matched for SES. Information was collected on the use of fluoride paste and mouth rinse, however this was not reported according to exposure of water fluoridation |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Data presented as percentages making it difficult to determine if all participants are accounted for |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | Unclear risk | Dental fluorosis was recorded by a trained and calibrated examiner, however, details of intra‐examiner reliability not provided |
Heller 1997.
| Methods |
FLUOROSIS STUDY Country of study: USA Geographic location: national survey of oral health of US school children Year of study: 1986 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: lifetime residents of study areas; aged 7‐17 years; ompletion of survey by parents Exclusion criteria: none stated Other sources of fluoride: written questionnaire included question regarding child's use of fluoride drops, fluoride tablets, professional topical fluoride treatments and school fluoride rinses Social class: not stated Ethnicity: not stated Residential history: continuous residency Other confounding factors: results standardised to age and sex distribution of US schoolchildren who participated in survey |
|
| Interventions | Group 1: > 1.2 ppm (natural fluoridation) Group 2: 0.7‐1.2 ppm (artificial fluoridation) Group 3: 0.3‐0.7 ppm (natural fluoridation) Group 4: < 0.3 ppm (natural fluoridation) | |
| Outcomes | Dental fluorosis (Dean's Index); caries data also evaluated within the study but excluded from review due to study design Age at assessment: 7‐17 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Stratified sampling was carried out and oral examination was conducted for 78% of all sampled students |
| Confounding | High risk | Results were not adjusted for SES and the use of fluoride from other sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest was fully reported on and balanced across groups |
| Other bias | Low risk | No other apparent bias |
Hernandez‐Montoya 2003.
| Methods |
FLUOROSIS STUDY Country of study: Mexico Geographic location: not stated Year of study started: 2001 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: having at least 1 year residence in the study area Exclusion criteria: not stated Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: ≥ 1 year residence in study area Other confounding factors: in all study areas, parents reported the use of fluoride toothpaste |
|
| Interventions | All natural fluoridation Group 1: 0.74 ppm Group 2: 1.3 ppm Group 3: 3.56 ppm Group 4: 4.07 ppm Group 5: 5.19 ppm Group 6: 5.57 ppm Group 7: 7.59 ppm | |
| Outcomes | Dental fluorosis (Dean's Index); caries data also evaluated within the study but excluded from review due to study design Age at assessment: 9‐11 years |
|
| Funding | Financial and logistical support from the Health Institute of the State of Aguascalientes, Institute Tecnologico de Aguascalientes and COSNET | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Random sampling was performed and considered the total population exposed to fluoridated water at each study area |
| Confounding | High risk | Did not account for SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Some participants were excluded from the analysis but no reason was provided |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | Unclear risk | Outcome was assessed by a working group previously trained and calibrated. Insufficient information on reliability testing |
Holdcroft 1999.
| Methods |
CARIES STUDY Country of study: England Geographic location: north Birmingham and Sandwell (F), North Staffordshire, Herefordshire and Shropshire (non‐F) Year study started: 1985/6 Year of change in fluoridation status: 1986 Study design: CBA |
|
| Participants | Inclusion criteria: not stated Exclusion criteria: not stated Other sources of fluoride: not Stated Social class: measured using Jarman scores Ethnicity: not stated Residential history: not stated Other confounding factors: not stated |
|
| Interventions | Initiation of water fluoridation Group 1: not stated Group 2: not stated | |
| Outcomes | dmft Age at baseline measure: not stated Age at final measure: not stated |
|
| Funding | Not stated | |
| Notes | Data from original CRD review (unverified data) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Unable to make a judgement as study was unavailable |
| Confounding | High risk | Data does not appear to have been controlled for SES and use of fluoride from other sources |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unable to make a judgement as study was unavailable |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unable to make a judgement as study was unavailable |
| Selective reporting (reporting bias) | Unclear risk | Unable to make a judgement as study was unavailable |
| Other bias | Unclear risk | Unable to make a judgement as study was unavailable |
Hong 1990.
| Methods |
FLUOROSIS STUDY Country of study: Taiwan Geographic location: Chung‐hsing New village (F) and Tsao‐tun (non‐F) Year of study: not stated Year of change in fluoridation status: 1978 Study design: cross sectional |
|
| Participants | Inclusion criteria: children aged 6‐15 years: resident in village since initiation of fluoridation Exclusion criteria: children who migrated from other areas during study period Other sources of fluoride: not stated Social class: 2 communities alike in social and living customs Ethnicity: not stated Residential history: resident since fluoride initiation Other confounding factors: 2 areas have virtually identical climates, only 3 km apart |
|
| Interventions | Group 1: 0.6 ppm (artificial fluoridation) Group 2: 0.08 ppm (natural fluoridation) | |
| Outcomes | Dental fluorosis (Dean's Index) Age at assessment: 6‐15 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | The participating sample consisted of children from 6‐15 years in the study areas. No other information was provided on sample selection |
| Confounding | High risk | Did not account for the use of other fluoride sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest was fully reported on and balanced across groups |
| Other bias | Low risk | No other apparent bias |
Ibrahim 1995.
| Methods |
FLUOROSIS STUDY Country of study: Sudan Geographic location: Abu Gronn (F); Treit El Biga (low F) Year of study: 1992 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: at least 1 erupted permanent maxillary incisor; lifetime residents of study areas; age 7‐16 years Exclusion criteria: not stated Other sources of fluoride: not stated Social class: author stated that areas had more or less the same socioeconomic background Ethnicity: author stated that areas had more or less the same ethnic background Residential history: lifetime residents Other confounding factors: altitude= 300m for both areas; mean temperature = 25‐35 °C. In low F area boys had significantly more fluorosis than girls |
|
| Interventions | All natural fluoridation Group 1: 2.56 ppm Group 2: 0.25 ppm | |
| Outcomes | Dental fluorosis (Community Fluorosis Index) Age at assessment: 7‐16 years |
|
| Funding | Norwegian Universities Committee for Development Research and Education | |
| Notes | Data extracted from Ibrahim 1995 differs from that presented in CRD review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Insufficient information was reported on sampling; the sampling frame was unspecified |
| Confounding | High risk | Did not account for the use of fluoride from other sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | High risk | No mention of calibration of examiners and reliability testing |
Indermitte 2007.
| Methods |
FLUOROSIS STUDY Country of study: Estonia Geographic location: Tartu city Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: 12‐year‐old children; continuous residence; only districts supplied by definite tube wells of known fluoride concentration were selected Exclusion criteria: not stated Social class: selected districts were of same eco‐environmental, ethnic as well as socioeconomic standards Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 0.2 ppm Group 2: 0.3 ppm Group 3: 1.2 ppm Group 4: 1.6 ppm Group 5: 2.4 ppm Group 6 3.9 ppm | |
| Outcomes | Dental fluorosis (index not reported) Age at assessment: 12 years |
|
| Funding | The study was supported by the Target Funding Projects no. 0180052s07 and no. 0182648s04 of the Ministry of Education and Science of Estonia and by Estonian Society of Stomatololgy | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Areas of study were sampled purposively and limited information was reported on the selection of individuals |
| Confounding | High risk | Did not account for the use of fluoride from other sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | High risk | Examination carried out by a trained examiner with an assistant, but no mention of calibration and reliability testing |
Indermitte 2009.
| Methods |
FLUOROSIS STUDY Country of study: Estonia Geographic location: not stated Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: not stated Exclusion criteria: not stated Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: < 1 ppm Group 2: 1‐1.5 ppm Group 3: 1.51‐2 ppm Group 4: 2.1‐3 ppm Group 5: 3.1‐4 ppm Group 6: > 4 ppm | |
| Outcomes | Dental fluorosis (Dean's Index) Age at assessment: 7‐15 years |
|
| Funding | The study was supported by the Estonian Society of Stomatology and Estonian Science Foundation grant number 7403 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Sampling was partly based on data from 2 previous studies which provide insufficient sampling information while the sub‐sample was selected from town of Tartu, where the fluoride content in drinking water varied significantly between regions |
| Confounding | High risk | Did not account for the use of fluoride from other sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | High risk | Clinical examination by a 'trained' dentist. Insufficient information on intra‐examiner reliability testing |
Ismail 1990.
| Methods |
FLUOROSIS STUDY Country of study: Canada Geographic location: public and private schools in Trois Rivieres (F) and Sherbrooke (non‐F), Quebec Year of study: 1987 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: children randomly selected from private and public schools separately; children aged 11‐17 years; resident in study areas for first 6 years Exclusion criteria: none stated Other sources of fluoride: fluoride tablet use around 13% in F areas and 67% in non‐F area Social class: stratified on school type: private or public (authors state private school likely to have been higher social class) Ethnicity: not stated Residential history: resident from 0‐6 years Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 1.0 ppm Group 2: < 0.1 ppm | |
| Outcomes | Dental fluorosis prevalence (TSIF); caries data collected, however, not presented in this review due to study design Age at assessment: 11‐17 years |
|
| Funding | National Health Research and Development Program, Health and Welfare (6605‐1316‐53) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | A 2‐stage stratified sample was selected from each city. In the first stage, private and public schools were randomly selected. In the second stage, students were randomly selected from the private and public schools separately |
| Confounding | High risk | There was an imbalance of the use of fluoride supplements between groups with more supplements being consumed by those living in the non‐fluoridated area |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Examiners were blind to the content of questionnaire" and by implication, fluoridation status of participants |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data appear to be presented for all participants |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | Low risk | No other apparent bias |
Jackson 1975.
| Methods |
FLUOROSIS STUDY Country of study: Wales Geographic location: Anglesey (F); Bangor and Caernarfon (non‐F) Year of study: 1974 Year of change in fluoridation status: 1955 Study design: unclear |
|
| Participants | Inclusion criteria: lifetime residents of study areas; continuous use of public water supply; school children aged 15 years; parental consent Exclusion criteria: children who had ever received fluoride tablets; left the study area; did not consume piped water supply for entire life; unavailable at time of sampling Other sources of fluoride: children who had received fluoride tablets excluded Social class: not stated Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | Group 1: 0.9 ppm (artificial fluoridation) Group 2: < 0.1 ppm (natural fluoridation) | |
| Outcomes | Mottling; caries data collected, however, not presented in this review due to study design Age at assessment: 15 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Stated that children were randomly sampled, however information on sampling was insufficient |
| Confounding | High risk | Children who had received fluoride tablets were excluded, however SES was not taken into account |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants were taken to a central examination centre by taxi and examiners were unaware of the area from which a child came |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Data presented for approximately 30% of participants sampled from each study area (Anglesey 28%; Bangor 32%) |
| Selective reporting (reporting bias) | Low risk | All expected outcomes were reported |
| Other bias | High risk | Even though the examiners carried out their investigations independently, no sort of calibration seemed to have been carried out |
Jackson 1999.
| Methods |
FLUOROSIS STUDY Country of study: USA Geographic location: Connersville (non‐F); Brownsburg (optimal‐F); Lowell (high‐F), Indiana Year of study: 1992 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: lifetime residents of study areas; consumed public water from birth or supply with comparable water level;cChildren aged 7‐14; parental and personal consent Exclusion criteria: factors in medical history that would contraindicate a dental examination; full mouth fixed orthodontic appliance Other sources of fluoride: use of fluoride supplements: non‐F areas = 58%; optimal‐F area = 20%; high‐F area = 9%. Also fluoride from mouth rinses, gels, other topical applications Social class: not stated Ethnicity: approximately 2% non‐white (stated for baseline survey) Residential history: lifetime residents Other confounding factors: areas all in same climatic zone |
|
| Interventions | All natural fluoridation Group 1: 4.0 ppm Group 2: 1.0 ppm Group 3: 0.2 ppm | |
| Outcomes | Dental fluorosis (TSIF) Age at assessment: 7‐10 years and 11‐14 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | There was insufficient detail reported to determine how selection took place |
| Confounding | High risk | Information on the use of other fluoride sources was collected, however, the results were not adjusted for this factor. Did not account for SES |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The examiner was unaware of the residency status of the participants |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | Low risk | No other apparent bias |
Jolly 1971.
| Methods |
FLUOROSIS STUDY Country of study: India Geographic location: the Punjab Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: school children Exclusion criteria: none stated Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: not stated Other confounding factors: not stated |
|
| Interventions | All naturally fluoridated Group 1: 0.7 ppm Group 2: 1.4 ppm Group 3: 2.4 ppm Group 4: 2.4 ppm Group 5: 2.5 ppm Group 6: 3.0 ppm Group 7: 3.0 ppm Group 8: 3.3 ppm Group 9: 3.3 ppm Group 10: 3.6 ppm Group 11: 4.3 ppm Group 12: 5.0 ppm Group 13: 5.09 ppm Group 14: 5.49 ppm Group 15: 7.02 ppm Group 16: 8.5 ppm Group 17: 9.5 ppm | |
| Outcomes | Mottled enamel Age at assessment: 5‐15 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | There was insufficient detail reported to determine how selection took place |
| Confounding | High risk | Did not account for the use of fluoride from other sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Number of participants examined was not reported and the outcome was reported as a proportion |
| Selective reporting (reporting bias) | High risk | The outcome of interest was reported as a proportion; and without absolute numbers or the number of participants examined (n) it is unclear what the proportion represents. Data not in suitable format for analysis |
| Other bias | High risk | No mention of examiner calibration |
Kanagaratnam 2009.
| Methods |
FLUOROSIS STUDY Country of study: New Zealand Geographic location: Auckland Year of study: not stated Year of change in fluoridation status: not stated Study design: cross‐sectional |
|
| Participants | Inclusion criteria: only children who returned signed consent form and questionnaire completed by parents Exclusion criteria: schools with fewer than 5 9‐year‐old children were excluded because of resource, time and efficiency constraints Other sources of fluoride: data presented on fluoride tablet supplementation, brushing with toothpaste frequency, amount of toothpaste used and toothpaste swallowed, however, the use of other sources of fluoride had no effect on the proportion of children with diffuse opacities Social class: high (deciles 8–10) = 40% (F), 19% (non‐F); middle (deciles 4–7) = 141% (F) , 44% (non‐F); low (deciles 1–3) = 19% (F), 37% (non‐F) (a schools decile indicates the extent to which it includes students from low socioeconomic communities) Ethnicity: more children of European descent and fewer children of Asian descent attended schools within non‐fluoridated areas compared with fluoridated areas Residential history: lifetime residents and intermittent residents, however, data on lifetime residents alone presented in this review due to confounding Other confounding factors: not stated |
|
| Interventions | Group 1: 0.1‐0.3 ppm (natural fluoridation) Group 2: 0.7‐1 ppm (artificial fluoridation) | |
| Outcomes | Dental fluorosis (Dean's Index); caries data collected, however, not presented in this review due to study design Age at assessment: 7‐15 years |
|
| Funding | Funded by AUT University, Counties Manukau District Health Board and New Zealand Dental Research Foundation | |
| Notes | Fluoride concentrations were not reported in the study but deduced from discussion section and anecdotal evidence | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | The number of schools and students from each school were probabilistically sampled to reflect the overall decile and school size distribution representative of Auckland schools yet produce a sample that was balanced between fluoridated and non‐fluoridated regions. |
| Confounding | Unclear risk | While the sample included participants from a range of SES, the numbers in these groups were not equal. There were significantly fewer children in high‐decile schools in non‐fluoridated areas and fewer children in low‐decile schools in fluoridated areas |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data appear to be presented for all participants |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported |
| Other bias | Low risk | No other apparent bias |
Kotecha 2012.
| Methods |
FLUOROSIS STUDY Country of study: India Geographic location: not stated Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: all age groups Exclusion criteria: those who could not be studied in the second visit Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: not stated Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: < 1.5 ppm Group 2: > 1.5 ppm | |
| Outcomes | Dental fluorosis (index not reported); caries data also evaluated within the study but excluded from review due to study design Age at assessment: all age groups |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | 11 out of 261 villages with high fluoride content in the drinking water and 11 out of 1490 villages with normal fluoride drinking water were randomly selected for water sampling |
| Confounding | High risk | Did not account for the use of fluoride from other sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Data for 75% of population of the study areas presented and attrition was not balanced across groups |
| Selective reporting (reporting bias) | Low risk | All expected outcomes were reported |
| Other bias | High risk | Measurement done by trained tutors and assistant professors, however, it is not clear whether the personnel measuring the outcome were calibrated |
Kumar 1999.
| Methods |
FLUOROSIS STUDY Country of study: USA Geographic location: Newburgh City (F); Newburgh Town (F 1984); New Windsor (non‐F); Kingston (non‐F) Year study started: 1986 Year study ended: 1995 Year of change in fluoridation status: 1984 Study design: CBA |
|
| Participants | Inclusion criteria: children aged 7‐14 years; lifetime residents of study areas Exclusion criteria: not stated Other sources of fluoride: fluoridation plus early brushing or tablet use, fluoride tablet plus early brushing, early brushing, and fluoride tablets all associated with an increased risk of fluorosis scored very mild to severe compared to children exposed to none of these additional sources Social class: not stated Ethnicity: no difference in odds of fluorosis in African‐Americans compared to white and other races Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | Group 1: 1 ppm (artificial fluoridation) Group 2: 1 ppm (artificial fluoridation) Group 3: 'low' level ‐ ppm not stated (natural fluoridation) Group 4: 'low' level ‐ ppm not stated (natural fluoridation) Group 5: 'low' level ‐ ppm not stated (natural fluoridation) |
|
| Outcomes | Dental fluorosis (Dean's Index); caries data also evaluated within the study but excluded from review due to study design Age at baseline measure: 7‐14 years Age at final measure: 7‐14 years |
|
| Funding | Supported by a grant from the National Institute of Dental Research (R01 DE 1088801) | |
| Notes | Group 1 (Newburgh City) had been fluoridated since 1945; Group 2 (Newburgh Town) was fluoridated in 1984. Data for 1995 only were available for Group 5 (Ulster) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Insufficient detail reported to determine how selection took place |
| Confounding | Unclear risk | While the authors reported that SES was considered, this information was not reported |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | High risk | Data not in suitable format for analysis |
| Other bias | High risk | There were great methodological differences between the before‐ and after‐study in questionnaire design and examiner and the examiners were not reported to have been calibrated |
Kumar 2007.
| Methods |
FLUOROSIS STUDY Country of study: India Geographic location: not stated Year study started: 1999‐2000 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: not stated Exclusion criteria: not stated Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: not stated Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 0.6 ppm Group 2: 1.1 ppm Group 3: 1.1 ppm Group 4: 1.1 ppm Group 5: 1.2 ppm Group 6: 1.3 ppm Group 7: 1.7 ppm Group 8: 1.7 ppm Group 9: 1.8 ppm Group 10: 1.9 ppm Group 11: 2.1 ppm Group 12: 2.9 ppm Group 13: 4.6 ppm | |
| Outcomes | Dental fluorosis (Smith's classification) Age at assessment: 5‐14 years |
|
| Funding | Indian Council of Medical Research | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | A stratified random sampling procedure was adopted for selection of water sources and villages |
| Confounding | High risk | Did not account for the use of fluoride from other sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interested reported |
| Other bias | High risk | Examiner calibration was not mentioned |
Kunzel 1976.
| Methods |
FLUOROSIS STUDY Country of study: Cuba Geographic location: La Salud (low F); Mir (medium F); San Augustin and Blanqizal (high F) Year of study: 1973 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: children resident in study areas. Exclusion criteria: not stated Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: not stated however, most of the children were born in the area Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 2.3‐3.6 ppm Group 2: 1.1‐1.6 ppm Group 3: 0.6‐0.8 ppm Group 4: 0.1 ppm | |
| Outcomes | Dental fluorosis (Dean's Index); caries data also evaluated within the study but excluded from review due to study design Age at assessment: 9‐10 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | There was insufficient detail reported to determine how selection took place |
| Confounding | High risk | Did not account for the use of fluoride from other sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The dental examinations were carried out while the fluoride content of the water consumed was unknown" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | All expected outcome reported |
| Other bias | Low risk | No other apparent biases |
Kunzel 1997.
| Methods |
CARIES STUDY Country of study: Germany Geographic location: Chemnitz (F); Plauen (non‐F) Year study started: 1959 Year study ended: 1971 Year of change in fluoridation status: 1959 Study design: CBA |
|
| Participants | Inclusion criteria: children born in study areas Exclusion criteria: children who had moved into the 2 study areas; disabled children Other sources of fluoride: number of topical applications of fluoride toothpastes; solutions and gel was low ‐ water fluoridation was the only preventive measure Social class: not stated Ethnicity: not stated Residential history: lifetime residents Other confounding factors: increasing annual sugar consumption in both areas |
|
| Interventions |
Initiation of water fluoridation Group 1 baseline: 0.2 ppm (natural fluoridation) Group 1 post intervention: 1 ppm (artificial fluoridation) Group 2: 0.2 ppm (natural fluoridation) |
|
| Outcomes | dmft, DMFT, % caries free (deciduous dentition), % caries free (permanent dentition) Age at baseline measure: 6‐15 years Age at final measure: 6‐15 years |
|
| Funding | Supported by the German Federal Ministry of Education, Science, Research and Technology, grant 01 ZZ 9502 | |
| Notes | Data extracted from Kunzel 1997 differs from that presented in CRD review (additional data extracted) Study presents data on both initiation and cessation of water fluoridation, but cessation data excluded from this review due to unsuitable control group |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Sampling details had previously been published (Kunzel 1980), however, the exclusion of disabled children as stated in this study, puts the representativeness of the sample in doubt |
| Confounding | High risk | Did not account for SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data appear to be presented for all participants |
| Selective reporting (reporting bias) | Low risk | Standard deviation was not reported |
| Other bias | Low risk | No other biases apparent |
Leverett 1986.
| Methods |
FLUOROSIS STUDY Country of study: USA Geographic location: Rochester, NY and several surrounding towns (F); 4 towns in western New York state (non‐F) Year of study: 1981 Year of change in fluoridation status: 1963 Study design: cross sectional |
|
| Participants | Inclusion criteria: children resident in study areas; children aged 7‐17 years Exclusion criteria: none stated Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: children in both non‐F and F areas were "not necessarily lifetime residents of their communities" Other confounding factors: none stated |
|
| Interventions | Group 1: 1.0 ppm (artificial fluoridation) Group 2: ≤0.3 ppm (natural fluoridation) | |
| Outcomes | Dental fluorosis (Dean’s Index) Age at assessment: 7‐17 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | There was insufficient detail reported to determine how selection of children within schools took place |
| Confounding | High risk | Did not account for the use of fluoride from other sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | High risk | The examiners do not seem to have been calibrated |
Levine 1989.
| Methods |
FLUOROSIS STUDY Country of study: England Geographic location: Birmingham (F); Leeds (non‐F) Year of study: 1987 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: lifetime residents of study areas (children only); schools with catchment areas inside study areas; children aged 9‐10 years Exclusion criteria: Asian and West Indian children; non‐continuous residents; teeth with fractures or restorations; children who had received fluoride supplements at any time Other sources of fluoride: children who had received fluoride supplements at any time excluded Social class: schools selected that served similar socioeconomic populations (social class groups 3,4,5) Ethnicity: Asian and West Indian children excluded Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | Group 1: 1 ppm (artificial fluoridation) Group 2: < 0.1 ppm (natural fluoridation) | |
| Outcomes | Enamel defect‐hypoplasia (TSIF) Age at assessment: 9‐10 years |
|
| Funding | Not stated | |
| Notes | Data extracted from Levine 1989 differs from that presented in CRD review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | There was insufficient detail reported to determine how selection took place |
| Confounding | Low risk | Children using fluoride supplements were excluded and sampling ensured that groups were comparable in terms of SES |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Photographic examination was blinded Quote: "The colour transparencies were coded and placed in a random sequence before being projected and viewed" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition was balanced across groups as results for 18 (2.9%) and 12 (2.4%) children from the non‐F and F area respectively were not available for photographic assessment |
| Selective reporting (reporting bias) | Unclear risk | There was selective reporting on the central incisor and the reason was not stated |
| Other bias | Low risk | No other apparent bias |
Lin 1991.
| Methods |
FLUOROSIS STUDY Country of study: China Geographic location: Xinyuan (F); Langan and Jiayi (non‐F) Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: school children aged 7‐14 years Exclusion criteria: not stated Other sources of fluoride: not stated Social class: low socioeconomic status, mean annual income of about 200 yuan Ethnicity: not stated Residential history: not reported Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 0.88 ppm Group 2: 0.34 ppm | |
| Outcomes | Dental fluorosis Age at assessment: 7‐14 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Used rRandom stratified sampling |
| Confounding | High risk | Did not account for the use of fluoride from other sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It is unclear whether data presented for all participants assessed for dental fluorosis |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | High risk | The examiners do not seem to have been calibrated |
Loh 1996.
| Methods |
CARIES STUDY Country of study: Singapore and Malacca (West Malaysia) Geographic location: Singapore (F); Malacca (non‐F) Year study started: 1957 Year study ended: 1966 Year of change in fluoridation status: 1958 Study design: CBA |
|
| Participants | Inclusion criteria: Chinese and Malay children aged 7‐9 years Exclusion criteria: not stated Other sources of fluoride: not stated Social class: not stated Ethnicity: Chinese and Malay children ‐ results presented separately Residential history: unclear Other confounding factors: not stated |
|
| Interventions | Initiation of water fluoridation Group 1: 0.7 ppm (artificial fluoridation) Group 2: 'low' level ‐ ppm not stated (natural fluoridation) | |
| Outcomes | DMFT Age at baseline measure: 7‐9 years Age at final measure: 7‐9 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Insufficient detail reported to determine how selection of schools and children within those schools took place |
| Confounding | High risk | No details were reported on the use of fluoride from other sources, SES or on the dietary habits of the children |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding was not undertaken |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Numbers of children examined at each time point are approximate |
| Selective reporting (reporting bias) | High risk | The outcomes of interest were not clearly stated a priori and while dental caries was reported (not fully), dental fluorosis appears to have been measured on a different age group, but not reported in useful format |
| Other bias | Low risk | No other bias detected |
Louw 2002.
| Methods |
FLUOROSIS STUDY Country of study: South Africa Geographic location: Sanddrif, Williston, Kuboes, Fraserburg, Brandvlei, Kenhardt, and Leeu Gamka Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: aged 11‐13 years, similar nutrition and dietary habits, similar ethnic and socioeconomic status Exclusion criteria: not stated Other sources of fluoride: no dental care or fluoride therapy, including the use of fluoride containing toothpaste Social class: similarly low SES reflected in living in subeconomic housing units Ethnicity: mixed with Khoi, Caucasian and Negroid roots that developed into a homogenous ethnic group Residential history: lifetime residents Other confounding factors: similar nutrition and dietary habits ‐ mostly bread and potatoes with sporadic intake of vegetables and meat, all located in arid rural sections of South Africa |
|
| Interventions | All natural fluoridation Group 1: 0.19 ppm Group 2: 0.36 ppm Group 3: 0.48 ppm Group 4: 1 ppm Group 5: 1.66 ppm Group 6: 2.64 ppm Group 7: 3 ppm | |
| Outcomes | Dental fluorosis prevalence (Dean's Index) Age at assessment: 11‐13 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Insufficient detail reported to determine how selection took place |
| Confounding | Low risk | SES was reported as comparable and the participants were not in receipt of dental care, fluoride supplements or toothpaste |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all (99%) participants |
| Selective reporting (reporting bias) | Low risk | Expected outcome reported |
| Other bias | Low risk | No other apparent bias |
Machiulskiene 2009.
| Methods |
FLUOROSIS STUDY Country of study: Lithuania Geographic location: Vilkaviskis and Jonuciai Year of study: 2004 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: never having taken part in any caries preventive programme; lifetime residency in the area; informed consent to participate Exclusion criteria: 1 school in Vilkaviskis was not eligible to participate in the study as a result of current caries prevention programmes, involving fluoride rinses and fissure sealants; tooth surfaces from which recordings could not be made because of the presence of fixed orthodontic appliances Other sources of fluoride: not stated Social class: children affected by parental unemployment: 1.1 ppm fluoride group = 39%; 0.3ppm fluoride group = 23%. More children in the 1.1 ppm fluoride group reported parental unemployment, however, the 2 towns were initially considered similar from a socioeconomic point of view Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 0.3 ppm Group 2: 1.1 ppm | |
| Outcomes | Dental fluorosis (TF Index); caries data also evaluated within the study but excluded from review due to study design Age at assessment: 13 years (mean) |
|
| Funding | Funded by Unrestricted grant from Colgate Palmolive (USA) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | All eligible secondary schools and students within them were invited to participate |
| Confounding | High risk | Did not account for the use of fluoride from other sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information. The measurement and recording of outcome were by different personnel, but they were not reported to have been blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | All expected outcome reported |
| Other bias | Low risk | No other apparent bias |
Mackay 2005.
| Methods |
FLUOROSIS STUDY Country of study: New Zealand Geographic location: not stated Year of study: 2002 Year of change in fluoridation status: not stated Study design: cross‐sectional |
|
| Participants | Inclusion criteria: not stated Exclusion criteria: not stated Other sources of fluoride: ingestion of toothpaste before the age of three = 40%; use of fluoride tablets up to (and including) age three = 49 (11.2%) Ethnicity: not stated Social class: high SES school (deciles 8‐10) = 192 (44%); medium SES school (deciles 4‐7) = 121 (27.8%); low SES school (deciles 1‐3) = 128 (28.2%) Residential history: the study included both continuous and intermittent residents, however, only data from continuous residents included in analysis Other confounding factors: not stated |
|
| Interventions | Group 1: 0.1‐0.3 ppm (natural fluoridation) Group 2: 0.8 ppm (artificial fluoridation) | |
| Outcomes | Enamel defects (DDE); caries data also evaluated within the study but excluded from review due to study design Age at assessment: 8.7‐11.1 years |
|
| Funding | New Zealand Dental Research Foundation | |
| Notes | Fluoride concentration deduced from discussion section and anecdotal evidence | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | A random sample of 600 Year 5 children enrolled with the Southland District Health Board’s school dental service was invited to participate in the study |
| Confounding | High risk | A statistical model used showed that hypoplastic defects were influenced by ingestion of toothpaste before age four but the results were not adjusted for this factor |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 436 (74.5%) of the 600 children invited to the study were examined |
| Selective reporting (reporting bias) | Low risk | All expected outcome reported |
| Other bias | Low risk | No other apparent bias |
Macpherson 2007.
| Methods |
FLUOROSIS STUDY Country of study: Sweden Geographic location: Kungsbacken (F); Halmsted (non‐F) Year of study: 2002‐2003 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: presence of 2 individual anterior labial‐view photographs of any upper anterior teeth present; similar date of birth (difference in age due to undertaking fieldwork in study areas a year apart) Exclusion criteria: not stated Other sources of fluoride: Age at which started brushing: 6‐12 months vs 12 months (P value 0.99) Frequency of brushing: ≤ 1/day vs ≥ 2/day (P value 0.42) Toothpaste F < 1000 ppm vs ≥ 1000 ppm (P value 0.49) Amount of toothpaste ≤ pea size vs > pea size (P value 0.09) Fluoride tablets previously: 'No' vs 'Yes' (P value 0.001) Fluoride tablets now: 'No' vs 'Yes' (P value 0.001) Ethnicity: not stated Social class: low education: F = 47, non‐F = 56; high education: F = 64, nonF = 73. Both groups were similar with respect to parents’ education attainment (P value 0.87) Residential history: children from Kungsbacka were generally exposed to fluoridated water in early childhood, while those from Halmstad were not exposed to fluoridated water during infancy (discussion section) Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 0.1 ppm Group 2: 1.3 ppm | |
| Outcomes | Dental fluorosis (TF Index; photographic assessment) Age at assessment: 7‐10 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Cluster random sample of parents of eligible children aged 7‐10 years from the same birth cohort |
| Confounding | High risk | Use of fluoride toothpaste and frequency of brushing was similar across groups, however, current use of fluoride supplements as well as past use was significantly higher in the control group. This information is used to provide adjusted odds ratios however, for the purposes of this review only the raw data has been used which remains subject to confounding factors |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessors were blind to the source area of each slide |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Unclear risk | Photographic assessment as well as TF Index of dental fluorosis were measured but only photographic assessment reported |
| Other bias | Low risk | No other apparent bias |
Mandinic 2009.
| Methods |
FLUOROSIS STUDY Country of study: Serbia Geographic location: Valjevo and Vranjska Banja Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: not stated Exclusion criteria: not stated Other sources of fluoride: used the fluoride concentration database and consumption database to determine fluoride exposure Ethnicity: not stated Social class: not stated Residential history: used the fluoride concentration database and consumption database to determine fluoride exposure Other confounding factors: dietary sources of fluoride – potato, beans |
|
| Interventions | All natural fluoridation Group 1: 0.1 ppm Group 2: 11 ppm | |
| Outcomes | Dental fluorosis (Dean's Index) Age at assessment: 12 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Insufficient detail reported to determine how selection took place ‐ sampling frame was unspecified |
| Confounding | High risk | Fluoride exposure and consumption were measured but not reported. Did not account for SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Expected outcome reported |
| Other bias | Low risk | No other apparent bias |
Mandinic 2010.
| Methods | FLUOROSIS STUDY Country of study: Serbia Geographic location: Valjevo, Veliko Gradiste, Kacarevo and Vranjska Banja Year of study: 2006 Year of change in fluoridation status: NA Study design: cross‐sectional | |
| Participants | Inclusion criteria: healthy 12‐year‐old school children, both genders, lifetime residents of the same municipality Exclusion criteria: not stated Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: lifetime residents Other confounding factors: there were no addition sources of exposure, i.e. industries that could pollute the environment by fluoride emission |
|
| Interventions | All natural fluoridation Wells Group 1: 0.79 ppm Group 2: 0.1 ppm Group 3: 0.15 ppm Group 4: 11 ppm Tap water Group 1: 0.17 ppm Group 2: 0.07 ppm Group 3: 0.1 ppm Group 4: 0.15 ppm |
|
| Outcomes | Dental fluorosis (Dean's Index) Age at assessment: 12 years |
|
| Funding | Ministry of Science and Technological Development of the Republic of Serbia | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Insufficient information on sampling |
| Confounding | High risk | The use of other fluoride sources and SES were not considered |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data for all participants was reported |
| Selective reporting (reporting bias) | High risk | Data not in suitable format for analysis |
| Other bias | Low risk | No other bias apparent |
Marya 2010.
| Methods |
FLUOROSIS STUDY Country of study: India Geographic location: 30 villages from district Gurgaon and district Hissar Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: only continuous residents; selected individuals had to have all their permanent teeth (except third molars) erupted Exclusion criteria: not stated Other sources of fluoride: not stated Ethnicity: not stated Social class: environmental factors such as eating habits, nutritional status, consumption of water, living conditions were almost uniform in all 7 groups studied Residential history: continuous residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 0.5 ppm Group 2: 0.87 ppm Group 3: 1.51 ppm Group 4: 2.45 ppm Group 5: 5.27 ppm Group 6: 8.5 ppm | |
| Outcomes | Dental fluorosis (Dean's Index) Age at assessment: 12‐16 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Insufficient detail reported to determine how selection took place |
| Confounding | Unclear risk | Environmental factors such as eating habits, nutritional status, consumption of water, and living conditions were almost uniform in all 7 groups studied, however, it was unclear whether this extended to exposure to fluoride from other sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Expected outcome reported |
| Other bias | Low risk | No other apparent bias |
Masztalerz 1990.
| Methods |
FLUOROSIS STUDY Country of study: Poland Geographic location: Neisse (high‐F), Breslau (F), Militsch and Gryfόw (non‐F) Year of study: not stated Year of change in fluoridation status: not stated Study design: cross sectional |
|
| Participants | Inclusion criteria: none stated Exclusion criteria: children who were not lifetime residents and had those who did not yet have permanent canine teeth Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: lifelong residents Other confounding factors: fluoride in the air was high in Greifenberg |
|
| Interventions | Appeared to be natural fluoridation, however this was not clear Group 1: 4‐7 ppm Group 2: 0.7‐0.9 ppm Group 3: < 0.2 ppm | |
| Outcomes | Dental fluorosis (index unclear) Age at time of measurement: 12 years |
|
| Funding | Not stated | |
| Notes | Paper translated from German | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | The authors report that all eligible children were to be studies however, the sampling frame was not specified |
| Confounding | High risk | Did not account for SES or the use of fluoride from other sources (except from air pollution though this is unclear) |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information. No details on blinding were reported, no standard index for measurement of fluorosis appears to have been used |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for 88% of participants |
| Selective reporting (reporting bias) | Low risk | Data appears present |
| Other bias | Low risk | No other bias detected |
Maupome 2001.
| Methods |
CARIES STUDY Country of study: Canada Geographic location: British Columbia Year study started: 1993‐1994 Year study ended: 1996‐1997 Year of change in fluoridation status: 1992 Study design: CBA |
|
| Participants | Inclusion criteria: not stated Exclusion criteria: not stated Other sources of fluoride: data on oral hygiene and exposure to diverse fluoride technologies were collected but not reported. However, the authors stated that British Columbia had relatively homogeneous exposure to fluorides, widespread use of fluoride toothpastes. good adherence to oral hygiene regimens and good access to oral health care Social class: participants showed similar SES at baseline Ethnicity: not stated Residential history: information about the regression analysis suggests that both lifetime and non‐lifetime residents might have been included Other confounding factors: not reported |
|
| Interventions |
Fluoride cessation Group 1: 'optimal' level ‐ ppm not stated (artificial fluoridation) to non‐fluoridated Group 2: 'optimal' level ‐ ppm not stated (artificial fluoridation) |
|
| Outcomes | DMFS Age at baseline: Grades 2, 3, 8 and 9 Age at final measurement: Grades 2, 3, 8 and 9 |
|
| Funding | NHRDP operating grant 6610‐2225‐002 supported this study | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Study was a multi‐site study and also both a repeated cross‐sectional prevalence survey and a longitudinal investigation. Children were examined in their schools but no other sampling details reported |
| Confounding | High risk | At baseline data for lifetime and non‐lifetime residents were reported; information on diet (snacks) and other fluoride sources were collected but the results were not adjusted for these factors |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Used different examiners for different study sites who where not blinded to fluoridation status |
| Incomplete outcome data (attrition bias) All outcomes | High risk | About 90% of all eligible children were examined at baseline; 64.2% at follow‐up with variation across groups |
| Selective reporting (reporting bias) | Low risk | Expected outcome was presented |
| Other bias | Unclear risk | Baseline data were collected 14‐19 months after cessation of fluoridation. This gap between the actual cessation of fluoridation and the beginning of data collection might be a source of bias, towards the null, since the exposure had been modified from fluoridated to non‐fluoridated water |
Mazzotti 1939.
| Methods |
FLUOROSIS STUDY Country of study: Mexico Geographic location: all areas in Mexico, 11 states, 107 cities Year of study: 1938 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: not stated Exclusion criteria: not stated Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: not stated Other confounding factors: not stated |
|
| Interventions | Groups: 0‐4 unclear ppm | |
| Outcomes | Dental fluorosis (index unclear) Age at assessment: not stated |
|
| Funding | Not stated | |
| Notes | Paper translated from Spanish | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | There was insufficient detail reported to determine how selection took place |
| Confounding | High risk | No details were reported on SES or fluoride from other sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to determine whether there was attrition |
| Selective reporting (reporting bias) | High risk | Data not in suitable format for analysis |
| Other bias | Unclear risk | Overall reporting on any information too poor to permit thorough assessment of any risk of bias |
McGrady 2012.
| Methods |
FLUOROSIS STUDY Country of study: Thailand Geographic location: Chiang Mai Year of study: 2007 Year study ended: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: life long residency; good general health with both maxillary incisors fully erupted; free from fixed orthodontic appliances Exclusion criteria: non‐lifetime residents; unsuitable dentition Other sources of fluoride:
Ethnicity: not stated Social class: not stated Residential history: continuous residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: < 0.2 ppm Group 2: 0.2‐0.59 ppm Group 3: 0.6 ‐0.89 ppm Group 4: ≥ 0.9 ppm | |
| Outcomes | Dental fluorosis (TF Index) Age at assessment: 8‐13 years |
|
| Funding | One author was funded by a Clinician Scientist Award from the National Institute for Health Research (UK). The Colgate Palmolive Dental Health Unit was funded by an unrestricted grant from Colgate Palmolive Possible conflicts of interest: RPE is an employee of a manufacturer of oral care products |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | High risk | The study was based on a convenience sample population with varying exposures to fluoride |
| Confounding | High risk | The data on fluoride from other sources was not presented in a usable format and outcome data were not adjusted for it. Did not account for SES |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The examiners were blinded to the probable fluoride exposure and the images were presented for examination in a randomised order |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Data for 148 (21%) examined participants not analysed |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | Low risk | No other bias apparent |
McInnes 1982.
| Methods |
FLUOROSIS STUDY Country of study: South Africa Geographic location: Kenhardt (F); Keimoes (non‐F); North‐western Cape Province Year of study: not stated Year of change in fluoridation status: NA Study design: cross sectional |
|
| Participants | Inclusion criteria: lifetime residents of study area; pre‐school children aged 1‐5 years Exclusion criteria: none stated Other sources of fluoride: majority of babies were breastfed so would not be exposed to fluoride from water used in preparation of infant formula Social class: reported as being the same across groups; experimental and control groups reported as being similar (parents were land or railway labourers) Ethnicity: all children same ethnic origin i.e. European‐African‐Malay origin Residential history: lifetime residents Other confounding factors: same climatic conditions in both areas |
|
| Interventions | All natural fluoridation Group 1: 2.2‐4.1 ppm Group 2: 0.2 ppm | |
| Outcomes | Dental fluorosis (Dean's Index) Age at time of measurement: 1‐5 years |
|
| Funding | Part funded by South African Sugar Association | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Insufficient detail reported to determine how selection took place |
| Confounding | High risk | Malnutrition and SES were reported to be similar across groups but no supporting data provided Did not report any details about other sources of fluoride |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Did not undertake blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data appear to be presented for all participants |
| Selective reporting (reporting bias) | Low risk | All expected data appeared to be present |
| Other bias | Low risk | No other apparent bias |
Mella 1992.
| Methods |
FLUOROSIS STUDY Country of study: Chile Geographic location: students attending 2 boarding institutions in Santiago, who lived in areas throughout Chile Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: students at boarding institution, exposure estimated from home fluoride level; lived for first 6 years in home town Exclusion criteria: students who could not remember the areas in which they spent the first 6 years of their life Other sources of fluoride: not stated Social class: distribution of subjects by high, moderate, low social class, but no significant differences between fluoride groups Ethnicity: not stated Residential history: first 6 years of life Other confounding factors: years lived in city of birth |
|
| Interventions | All natural fluoridation Group 1: > 0.3 ppm Group 2: ≤0.3 ppm | |
| Outcomes | Dental fluorosis (Dean's Index) Age at assessment: 19 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | High risk | All subjects were selected from 2 boarding schools. Insufficient detail reported to determine how sampling took place |
| Confounding | High risk | Did not account for the use of fluoride from other sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Unclear risk | Unclear why only very mild, mild and moderate severities of dental fluorosis reported for both groups |
| Other bias | Low risk | No other apparent bias |
Mella 1994.
| Methods |
FLUOROSIS STUDY Country of study: Chile Geographic location: Iquique (F); Santiago (non‐F); Valparaiso‐Vina (F); Temuco (low‐F) Year of study: 1983 Year of change in fluoridation status: not stated Study design: cross‐sectional |
|
| Participants | Inclusion criteria: 4 schools in study areas Exclusion criteria: not stated Other sources of fluoride: not stated Social class: 2 schools in each area, 1 from low social class, 1 from medium/high social class, results presented separately by social class Ethnicity: not stated Residential history: not stated Other confounding factors: not stated |
|
| Interventions | Group 1: 2.2 ppm (natural fluoridation) Group 2: 0.0 ppm (natural fluoridation) Group 3: 1.0 ppm (artificial fluoridation) Group 4: 0.3 ppm (natural fluoridation) | |
| Outcomes | Dental fluorosis (Dean's Index) Age at assessment: 7 and 12 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Insufficient detail reported to determine how selection took place. 4 schools from a list of schools benefiting from school feeding programs were selected from each city, however it was not reported how these were chosen or how the children within the schools were chosen |
| Confounding | High risk | Did not account for the use of fluoride from other sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | Low risk | No other apparent bias |
Meyer‐Lueckel 2006.
| Methods | FLUOROSIS STUDY Country of study: Iran Geographic location: Youssefabad, Seman, Dibaj Year of study: 2003 Year of change in fluoridation status: NA Study design: cross‐sectional | |
| Participants | Inclusion criteria: school children aged 6‐9 years who were lifetime residents Exclusion criteria: not stated Other sources of fluoride: not stated Social class: Youssefabad, Semnan were of upper middle and lower middle class, social class of the third community was not mentioned Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 0.2 ppm Group 2: 0.3 ppm Group 3: 1.3 ppm |
|
| Outcomes | Dental fluorosis (TSIF); caries data evaluated in study but excluded from review due to study design Age at assessment: 6‐9 years | |
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | 2 schools (one boys' and one girls') were randomly selected from 2 of the 3 study areas, and in the third study area the only school (coeducation) was selected and all participants were then examined |
| Confounding | High risk | 2 study areas varied in social class, while there was no information on SES for the third study area; in addition the use of other fluoride sources was not considered |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Fluorosis outcome data were reported in bar charts making it difficult to assess whether there were incomplete outcome data or not. |
| Selective reporting (reporting bias) | High risk | Though outcome of interest was reported, fluorosis outcome was not reported for the Youssefabad area |
| Other bias | Unclear risk | The single examiner involved in the study was calibrated, and though the reliability of caries recording was assessed, it was not done for fluorosis outcome |
Milsom 1990.
| Methods |
FLUOROSIS STUDY Country of study: England Geographic location: Nantwich (F); Northwich (non‐F) Year of study: 1988 Year of change in fluoridation status: 1975 Study design: cross‐sectional |
|
| Participants | Inclusion criteria: children aged 8 years attending state‐maintained schools; lifetime residents of study areas; parental consent Exclusion criteria: parishes not bounded on all sides by parishes with optimally fluoridated water for fluoride areas; exposure to fluoride supplements Other sources of fluoride: age at which tooth brushing first began Social class: measured by parental occupation; social class makeup of study areas almost identical (data presented in paper) Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | Group 1: 1 ppm (artificial fluoridation) Group 2: < 0.3 ppm (natural fluoridation) | |
| Outcomes | Enamel defect (DDE) Age at assessment: 8 years |
|
| Funding | Financial support from the North Western Regional Health Authority | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | The study included all eligible children who lived in the non‐fluoridated area and those in the fluoridated area were selected by a two‐stage random sampling technique |
| Confounding | Low risk | There was no difference in SES across groups and children with exposure to fluoride supplements were excluded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants were taken to the examination centre by bus, examiner was unaware of the schools in attendance and fluoridation status |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data appear to be presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest appears present |
| Other bias | Unclear risk | Data were collected on age of commencement of tooth brushing but not reported |
Mondal 2012.
| Methods | FLUOROSIS STUDY Country of study: India Geographic location: Nalhati I (Nasipur, Vabanandapur, Deshnabagram) and Rampurhat II (Chalk Atla, Nowapara, Junitpur and Kamdebpur) Year of study: 2003 Year of change in fluoridation status: NA Study design: cross‐sectional | |
| Participants | Inclusion criteria: not stated Exclusion criteria: not stated Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 3.15 ppm Group 2: 3.83 ppm |
|
| Outcomes | Dental fluorosis (Dean's Index ) Age at assessment: < 10 years to > 50 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | High risk | "The recruitment of respondents was performed at seven primary schools in the study area with pupils in the age range of 4–10 years and the rest of the age group samples were collected from the respective villages". There was no indication that random sampling was carried out |
| Confounding | High risk | Participants were lifetime residents, however, SES and the use of other fluoride sources were not considered |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data for all participants reported |
| Selective reporting (reporting bias) | Low risk | Outcome of interest fully reported |
| Other bias | Unclear risk | Examination was done by a 'competent dentist', however, there was no mention of calibration |
Montero 2007.
| Methods |
FLUOROSIS STUDY Country of study: Venezuela Geographic location: Maria May, Roscio and Madre Emilia Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: not stated Exclusion criteria: not stated Other sources of fluoride: not stated Ethnicity: not stated Social class: not stated Residential history: not stated Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 0.13 ppm Group 2: 0.31 ppm Group 3: 1.58 ppm | |
| Outcomes | Dental fluorosis (Dean's Index); caries data also evaluated in study but excluded from review due to study design Age at assessment: 8‐12 years |
|
| Funding | Not stated | |
| Notes | Paper translated from Spanish | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Random sampling was used |
| Confounding | High risk | Did not account for the use of fluoride from other sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data appear to be presented for all participants |
| Selective reporting (reporting bias) | Low risk | All expected outcome presented |
| Other bias | Low risk | No other apparent bias |
Nanda 1974.
| Methods |
FLUOROSIS STUDY Country of study: India Geographic location: 23 villages in Lucknow (North Central India) Year of study: not stated Year of change in fluoridation status: NA Study design: cross sectional |
|
| Participants | Inclusion criteria: lifetime residents of study areas; children from 103 urban and 66 rural schools; all permanent teeth (excluding third molars) present Exclusion criteria: none stated Other sources of fluoride: dietary fluoride intake Social class: not stated Ethnicity: not stated Residential history: lifelong residents Other confounding factors: climate |
|
| Interventions | All natural fluoridation Group 1: > 1.21 ppm Group 2: 0.81‐1.2 ppm Group 3: 0.41‐0.8 ppm Group 4: 0‐0.4 ppm | |
| Outcomes | Dental fluorosis (Dean’s Index) Age at time of measurement: 6‐17 years |
|
| Funding | Supported by PL‐480 grants from the Bureau of Health Manpower Education, Division of Dental Health Public Health Service under the aegis of the Indian Council of Medical Research, New Delhi | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Insufficient detail reported to determine how selection took place |
| Confounding | High risk | Did not account for SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding was not undertaken |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear due to poor reporting of participant numbers and data |
| Selective reporting (reporting bias) | High risk | Poor reporting of outcome data |
| Other bias | High risk | No other bias detected |
Narbutaite 2007.
| Methods |
FLUOROSIS STUDY Country of study: Lithuania Geographic location: Klaipeda and Kaunas Year of study: 1997 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: not stated Exclusion criteria: not stated Other sources of fluoride: not stated Ethnicity: not stated Social class: Klaipeda and Kaunas said to be the 2 largest cities in Lithuania and to be of a similar size and socioeconomic structure Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 0.22 ppm Group 2: 1.7‐2.2 ppm | |
| Outcomes | Dental fluorosis (TF Index); caries data also evaluated within the study but excluded from review due to study design Age at assessment: 12 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | 8 out of 23 ordinary secondary schools in Klaipeda (the high‐F area) and 8 out of 30 in Kaunas (the low‐F area), were selected to cover the regions. However, it is not clear how these schools were selected |
| Confounding | High risk | No details were reported on the use of fluoride from other sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | All expected outcomes were reported |
| Other bias | High risk | All examinations were carried out by 1 examiner who was a specialist with additional training in dental fluorosis diagnosis but no mention of reliability testing; water was taken from 3 sampling sites in the high‐F area and 1 in the low‐F area, no explanation was provided for the inconsistency |
Narwaria 2013.
| Methods |
FLUOROSIS STUDY Country of study: India Geographic location: Dumduma, Bangama, Hazinager, Sillarpur, Sirsod, Nichroli, Toda Karera, Toda Rampur, Kali Pahadi and Zuzai in Karera Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: primary school children; mostly 5‐12 years Exclusion criteria: not stated Other sources of fluoride: not stated Ethnicity: not stated Social class: not stated. Residential history: not stated Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 1.65 ppm Group 2: 1.84 ppm Group 3: 1.84 ppm Group 4: 1.88 ppm Group 5: 1.91 ppm Group 6: 2.15 ppm Group 7: 2.22 ppm Group 8: 2.53 ppm Group 9: 3.91 ppm | |
| Outcomes | Dental fluorosis (Dean's Index) Age at assessment: 5‐12 years |
|
| Funding | Funding for travelling and laboratory facilities provided by Special Assistance Program (SAP)‐I UGC, New Delhi | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | 10 villages were selected for study using the eligibility criteria. Within these villages, all government schools were included and children were randomly selected from each class |
| Confounding | High risk | Did not account for the use of fluoride from other sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interested reported |
| Other bias | High risk | Examination was performed by 2 trained dentists. No mention of calibration or of reliability testing |
Nunn 1992.
| Methods |
FLUOROSIS STUDY Country of study: England Geographic location: Hartlepool, Newcastle and Middlesborough Year of study: 1989 Year of change in fluoridation status: NA Study design: cross‐sectional study |
|
| Participants | Inclusion criteria: lifetime residents of study areas; children in selected schools aged 15‐16 years Exclusion criteria: children with fractured incisor teeth, orthodontic bracket or surface otherwise obscured Other sources of fluoride: not stated Social class: occupation of head of household recorded; participants of low and high SES were recruited when possible Ethnicity: ethnicity recorded but no expansion on variable Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | Group 1: 1‐1.3 ppm Group 2: 1 ppm Group 3: 0.2 ppm | |
| Outcomes | Enamel defect Age at assessment: 12 years |
|
| Funding | Financial assistance from the British Council | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | There was insufficient detail reported to determine how selection took place |
| Confounding | High risk | Did not account for the use of fluoride from other sources. Balance of SES between groups was unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Photographs of the maxillary central incisors of participants were cut out from the print and identified with a code which would prevent identification by the examiners |
| Incomplete outcome data (attrition bias) All outcomes | High risk | In England, data for 68% of examined participants were reported due to camera failure in a school of SES |
| Selective reporting (reporting bias) | Low risk | Expected outcome appeared to be present |
| Other bias | Low risk | No other apparent bias |
Nunn 1994a.
| Methods |
FLUOROSIS STUDY Country of study: England Geographic location: north‐east England Year of study: 1990‐1991 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: lifetime residents of study areas (England only); children aged 12 years; parental consent (England only) Exclusion criteria: none stated Other sources of fluoride: not stated, but expected higher use of toothpaste in higher SES groups Social class: children divided into high and low social class Ethnicity: not stated Residential history: UK participants were lifetime residents. Other confounding factors: not stated |
|
| Interventions | Group 1: 0.1 ppm Group 2: 0.5 ppm Group 3: 1.0 ppm |
|
| Outcomes | Enamel defect (DDE) Age at assessment: 12 years |
|
| Funding | Not stated | |
| Notes | Two study centres: England Sri Lanka. Different methodology used in England and Sri Lankan study centres, therefore reported under different study ID's (England ‐ Nunn 1994a and Sri Lankan ‐ Nunn 1994b) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Schools were selected by the district dental officer in order to achieve a target of about 150 eligible 12 year old children in each sub‐group. Insufficient information provided regarding how the children were selected within the schools |
| Confounding | High risk | Higher reported use of toothpaste in the higher SES groups |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The examiner was largely unaware of fluoride and socioeconomic status of the children |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Participants sampled were < 80% in the study areas and not balanced across groups, however, data presented for all recruited participants |
| Selective reporting (reporting bias) | Low risk | Expected outcome was presented |
| Other bias | Low risk | No other apparent bias |
Nunn 1994b.
| Methods |
FLUOROSIS STUDY Country of study: Sri‐Lanka Geographic location: Sri Lanka Year of study: 1990‐1991 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: children aged 12. Exclusion criteria: none stated Other sources of fluoride: not stated, but expected higher use of toothpaste in higher SE groups Social class: children divided into high and low social class Ethnicity: not stated Residential history: Sri Lankan populations were non‐mobile and confirmed continuous residence when asked at the time of examination Other confounding factors: not stated |
|
| Interventions | Group 1: 0.1 ppm Group 2: 0.5 ppm Group 3: 1.0 ppm |
|
| Outcomes | Enamel defect (DDE) Age at assessment: 12 years |
|
| Funding | Not stated | |
| Notes | Two study centres: England Sri Lanka. Different methodology used in England and Sri Lankan study centres, therefore reported under different study ID's (England ‐ Nunn 1994a and Sri Lankan ‐ Nunn 1994b) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Schools were selected by the district dental officer in order to achieve a target of about 150 eligible 12‐year‐old children in each sub‐group. Insufficient information provided regarding how the children within the schools were selected |
| Confounding | High risk | Imbalance of SES between groups. Two of the three study areas recruited only children of low SES and one area recruited both low and high SES children |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | The examiner was aware of the fluoride and socioeconomic status of the children |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Participants sampled were < 80% in the study areas and not balanced across groups, however, data presented for all recruited participants |
| Selective reporting (reporting bias) | Low risk | Expected outcome was presented |
| Other bias | Low risk | No other apparent bias |
Ockerse 1941.
| Methods |
FLUOROSIS STUDY Country of study: South Africa Geographic location: Upington, Kenhardt and Pofadder Year of study: 1939 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: children attending schools in study areas; children aged 6‐17 years Exclusion criteria: none stated Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: participants were born and lived up to the age of 8 in the study areas Other confounding factors: sStudy areas at same altitude, same climate, similar countryside and vegetation, differences in drinking water composition discussed |
|
| Interventions | All natural fluoridation Group 1: 2.46 ppm (average) Group 2: 6.8 ppm Group 3: 0.38 ppm | |
| Outcomes | Mottled enamel; caries data also evaluated within the study but excluded from review due to study design Age at assessment: 6‐17 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | High risk | Areas thought to be most affected by caries and mottling were selected and visited. Selection of 'at risk' population is likely to have introduced bias |
| Confounding | High risk | Did not account for the use of fluoride from other sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | High risk | Caries data reporting may have been a post‐hoc decision |
| Other bias | High risk | Data were collected on age of commencement of tooth brushing but not reported. There was no mention of examiner training or calibration |
Pontigo‐Loyola 2008.
| Methods |
FLUOROSIS STUDY Country of study: Mexico Geographic location: urban ‐ Tula Centro and San Marcos; rural – El Llano Year of study: 1999 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: not stated Exclusion criteria: having fixed orthodontic appliances; metal crowns; refusal to be examined; unavailable for oral examination Other sources of fluoride: not stated Ethnicity: not stated Social class: not stated. Residential history: birth to ≥ 6 years Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 1.38 ppm Group 2: 1.42 ppm Group 3: 3.07 ppm | |
| Outcomes | Dental fluorosis (modified Dean's Index) Age at assessment: 12 and 15 years |
|
| Funding | Data collection by the Universidad Autonoma del Estado de Hidalgo and data analysis was partially supported by a grant from the National Council of Science and Technology of Mexico | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | All eligible participants were included in the study |
| Confounding | High risk | Did not account for the use of fluoride from other sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Only 66.6% of the included participants were in the final study population. The reason for withdrawal was not reported |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | Low risk | No other apparent bias |
Pot 1974.
| Methods |
CARIES STUDY Country of study: Holland Geographic location: Tiel (F); Culemborg (non‐F) Year study started: 1950 Year study ended: 1970 Year of change in fluoridation status: 1953 Study design: CBA |
|
| Participants | Inclusion criteria: residents of study areas born between 1896 and 1945; lifelong residents of study areas Exclusion criteria: subjects who left the study areas for more than 3 months after fluoridation was introduced Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: lifetime residents Other confounding factors: age: results for final survey presented in 5‐year age groups and showed that higher proportion of younger subjects had prosthetic teeth in Culemborg than in Tiel |
|
| Interventions | Group 1: 1.1 ppm (artificial fluoridation) Group 2: 0.1 ppm (natural fluoridation) |
|
| Outcomes | Outcome: % with false teeth Age at baseline measure: 5‐55 Age at final measure: 25‐75 |
|
| Funding | Not stated | |
| Notes | Paper translated from Dutch | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Participants were selected by random sampling from the city population registers |
| Confounding | High risk | Did not report on SES or the use of other fluoride sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Data presented for all participants |
| Selective reporting (reporting bias) | High risk | Study reports on % false teeth; no caries data |
| Other bias | High risk | There was no mention of examiner calibration or of reliability testing |
Ray 1982.
| Methods |
FLUOROSIS STUDY Country of study: India Geographic location: Rustampur and Ledhupur, 2 adjacent village in Varanasi District Year of study: not stated Year of change in fluoridation status: NA Study design: cross sectional |
|
| Participants | Inclusion criteria: none stated Exclusion criteria: none stated Other sources of fluoride: not stated Social class: study areas similar with respect to demographic and socioeconomic characteristics Ethnicity: not stated Residential history: not stated Other confounding factors: villages similar with respect to geoclimatic characteristics |
|
| Interventions | All natural fluoridation Group 1: > 2 ppm Group 2: 1‐2 ppm Group 3: < 1 ppm | |
| Outcomes | Dental fluorosis (index not stated) Age at assessment: not stated |
|
| Funding | Funded by the Indian Council of Medical Research | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | All eligible participants were included in the study |
| Confounding | High risk | Did not report on the use of fluoride from other sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Number of participants recruited not stated |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | High risk | No mention of how examination was conducted or whether the examiner was calibrated |
Riordan 1991.
| Methods |
FLUOROSIS STUDY Country of study: Australia Geographic location: Perth (F); Bunbury (non‐F), Western Australia Year of study: 1989 Year of change in fluoridation status: 1968 Study design: cross‐sectional |
|
| Participants | Inclusion criteria: children born in 1978; children attending government schools in study areas; parental consent Exclusion criteria: subjects with amelogenesis imperfecta or orthodontic banding Other sources of fluoride: questionnaire investigated periods and duration of use of fluoride supplements, use of fluoride toothpaste, included age at which use of toothpaste commenced, whether child swallowed toothpaste Social class: schools assigned socioeconomic score ‐ no significant difference in scores between study areas Ethnicity: not stated Residential history: not stated Other confounding factors: not stated |
|
| Interventions | Group 1: 0.8 ppm (artificial fluoridation) Group 2: < 0.2 ppm (natural fluoridation) | |
| Outcomes | Dental fluorosis (TF Index) Age at assessment: 12 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Random selection of 14 Dental Therapy Centres; selection of 1 class/centre of children born in 1978 |
| Confounding | High risk | Insufficient information to determine whether use of other fluoride sources was balanced across groups |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blind outcome assessment (with regard to residency) was not undertaken |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 7/376 and 3/338 not available for evaluation; unlikely to influence results |
| Selective reporting (reporting bias) | Low risk | All relevant outcome data reported |
| Other bias | Low risk | No other apparent bias |
Riordan 2002.
| Methods | FLUOROSIS STUDY Country of study: Australia Geographic location: Western Australia Year of study: 2000 Year of change in fluoridation status: NA Study design: Cross‐sectional | |
| Participants | Inclusion criteria: Children born around 1990 (10 yrs old) who had lived in Australia/New Zealand for most of their lives (so as to ensure life time exposure to water fluoridation) Exclusion criteria: Migrants from outside Australia and New Zealand, refusal to consent, not present at school at the time of exam Other sources of fluoride: Information was collected on use of infant formula, age at which toothpaste was introduced and the use of fluoride supplements. Fluoride supplement use was almost exclusive to residents of the non‐fluoridated areas Social class: Not specified Ethnicity: Not specified Residential history: Participants were categorised as having been exposed to water fluoridation if they had spent more than half their life between the ages of 0‐5 in a water fluoridated area Other confounding factors: Not specified | |
| Interventions | Group 1: 0.8ppm (artificial fluoridation) Group 2: 0.2‐0.3 ppm (naturally fluoridated) | |
| Outcomes | Dental fluorosis (TF index) Age at assessment: 10 years | |
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | The sampling frame was made up of children registered with the School dental service and children were accessed via schools. All eligible children were invited to take part in the study |
| Confounding | High risk | Information on other sources of fluoride was collected and more children in the non‐fluoridated area took fluoride supplements. SES was not stated. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | Low risk | No other apparent bias |
Ruan 2005.
| Methods |
FLUOROSIS STUDY Country of study: China Geographic location: urban ‐ Bao Ji and Jing Bian Year of study: 2002 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: not stated Exclusion criteria: absent or unavailable; non‐permanent residents Other sources of fluoride: no fluoride supply was provided by dental service and no fluoride supplement program was implemented in any of the communities Ethnicity: not stated Social class: the selected schools served rural communities where socioeconomic standards were comparable Residential history: permanent residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 0.4ppm Group 2: 1.0 ppm Group 3: 1.8 ppm Group 4: 3.5 ppm Group 5: 5.6 ppm | |
| Outcomes | Dental fluorosis (TF Index); caries data also evaluated within the study but excluded from review due to study design Age at assessment: 12 and 13 years |
|
| Funding | The study was supported by the Norwegian State Educational Loan Fund | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | 13 schools were contacted and all children were invited to participate. The sampling frame for schools was not specified |
| Confounding | High risk | Even though fluoride supplement and fluoride supply by dental service were taken into account, the use of fluoride toothpaste (a common source) was not mentioned. It is not clear why it was not acknowledged or investigated |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The fluoride concentration of the local drinking‐water supplies was unknown to the examiner at the time of the clinical examinations, which took place with the students seated on ordinary chairs outside the school building |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | High risk | Partial reporting of outcome ‐ only reported prevalence of fluorosis with TF score ≥ 3 (fluorosis of aesthetic concern) |
| Other bias | Low risk | No other apparent bias |
Rugg‐Gunn 1997.
| Methods |
FLUOROSIS STUDY Country of study: Saudi Arabia Geographic location: Jeddah (low F); Riyadh (moderate F); and Quassim (high F) Year of study: 1992 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: lifetime residents of study areas; boys aged 14 years; parental consent Exclusion criteria: photographs that failed to show whole buccal surface; out of focus photographs Other sources of fluoride: not stated Social class: schools grouped according to the socioeconomic status of residential areas in the urban community; family income and parental education measured using questionnaire Ethnicity: not stated Residential history: lifetime residents Other confounding factors: nutritional status |
|
| Interventions | All natural fluoridation Group 1: 2.7 ppm Group 2: 0.8 ppm Group 3: < 0.3 ppm | |
| Outcomes | Dental fluorosis (index unclear) Age at assessment: 14 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Quote: "All school were grouped according to SES of the residential area in the urban community only and schools sampled randomly" |
| Confounding | High risk | Schools were grouped according to the SES of residential areas however it is not clear whether the study areas were balanced in this regard. No detail was reported on the use of fluoride from other sources |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data appears to have been presented for all participants |
| Selective reporting (reporting bias) | High risk | Data not in suitable format for analysis |
| Other bias | High risk | No other apparent bias |
Russell 1951.
| Methods |
FLUOROSIS STUDY Country of study: USA Geographic location: Colorado Springs (F); Boulder (non‐F), Colorado Year of study: 1950 Year of change in fluoridation status: NA Study design: cross sectional |
|
| Participants | Inclusion criteria: white native residents listed in school census record for 1920, 1930 or 1940 and as resident in current city directory; mothers living in study area at time of birth; age 20‐44 years; residence and usage of local water unbroken except for periods not exceeding 60 days during calcification and eruption of permanent teeth Exclusion criteria: none stated Other sources of fluoride: not stated Social class: workers in 2 communities followed similar occupations and had similar average salaries Ethnicity: native born white = 98% of Boulder population, and 96% of Colorado Springs population. This study only reports upon white participants (not clear if this was coincidence or purpose) Residential history: lifetime residents Other confounding factors: Colorado Springs 3 times size of Bolder, similar altitude and climate, neither population ageing nor young, both were highly literate, water systems similar |
|
| Interventions | All natural fluoridation Group 1: 2.5 ppm Group 2: < 0.1 ppm | |
| Outcomes | Dental fluorosis (Dean’s Index); caries data also evaluated within the study but excluded from review due to study design Age at time of measurement: 20‐44 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Samples came from official registries in the areas (school, electoral, marriage etc). Authors estimate 5/6ths of eligible people participated |
| Confounding | Unclear risk | Considering the age of the study, other sources of fluoride are unlikely to affect the results. Although no measure of SES was provided, populations are reported as homogenous. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding was not undertaken |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data for all participants appeared to be present. |
| Selective reporting (reporting bias) | High risk | Only data on fluorosis of aesthetic concern reported as opposed to all severities |
| Other bias | High risk | All examinations were made by the senior author, however, there was no mention of examiner calibration |
Rwenyonyi 1998.
| Methods |
FLUOROSIS STUDY Country of study: Uganda Geographic location: 4 areas of Uganda located at different altitudes Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: lifetime residents of study areas Exclusion criteria: none stated Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: lifetime residents Other confounding factors: mothers interviewed about water intake and food habits of child during early childhood; altitude |
|
| Interventions | All natural fluoridation Group 1: 2.5 ppm (low altitude) Group 2: 2.5 ppm (high altitude) Group 3: 0.5 ppm (low altitude) Control: 0.5 ppm (high altitude) | |
| Outcomes | Dental fluorosis (index not stated) Age at assessment: 10‐14 years |
|
| Funding | The Norwegian Universities' Committee for Development Research and Education and the Committee for Research and Postgraduate Training, University of Bergen | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Children were selected from schools for study in a quasi‐random way |
| Confounding | High risk | While SES and use of fluoride toothpaste were reported as being similar across groups, there appeared to be a higher intake of tea (and therefore fluoride from water) among the participants in Kasese (0.5 ppm) than Kisoro (2.5 ppm) |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data appear to have been presented for all participants |
| Selective reporting (reporting bias) | Unclear risk | Outcome of interest was reported mainly in graphic form and was unclear |
| Other bias | Low risk | Examinations were carried out by a single examiner. Intra‐rater reliability was tested (kappa > 0.8) |
Rwenyonyi 1999.
| Methods |
FLUOROSIS STUDY Country of study: Uganda Geographic location: Kasese (low F); Kisoro (high F) Year of study: 1996‐1997 Year of change in fluoridation status: NA Study design: cross sectional |
|
| Participants | Inclusion criteria: children aged 10‐14 years (born between 1982 and 1987); lifetime residents of study areas; consumed drinking water from same source for first 6 years of life; parental consent Exclusion criteria: absence from the village for more than 1 month per year Other sources of fluoride: fluoride exposure from liquid estimated by daily liquid intake ‐ subjects from high fluoride area had higher intake of water, consumed more boiled water and consumed less tea than subjects from control area, higher consumption of fluoride from Trona in control group Social class: most families were small scale farmers and all appeared to be of similar social class Ethnicity: all children were ethnic Bantu Africans from the Bafumbria and Bakonjo tribes Residential history: lifelong residents Other confounding factors: vegetarianism (associated with fluorosis); altitude (results presented separately for different altitudes) ‐ no association found between altitude and fluorosis |
|
| Interventions | All natural fluoridation Group 1: 2.5 (altitude = 2800 m) Group 2: 2.5 (altitude = 1750 m) Group 3: 0.5 (altitude = 2200 m) Group 4: 0.5 (altitude = 900 m) | |
| Outcomes | Dental fluorosis (TF Index) Age at time of measurement: mean age 12.2 years (SD 1.3) |
|
| Funding | Norwegian Universities Committee for Development Research and Education and the Committee for Research and Postgraduate Trianing, University of Bergen | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Quasi‐random stratified sample of all eligible children |
| Confounding | High risk | SES was broadly similar, however, multivariate analysis revealed that factors that were not accounted for were associated with fluorosis. These included: daily intake of water (amount), altitude, water storage, vegetarianism and infant formula use |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Examiners were blind to fluoride concentrations at the start of the study and tests were carried out on the water after the children’s teeth were examined |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data appear to be presented for all participants |
| Selective reporting (reporting bias) | Low risk | All data appears to have been reported |
| Other bias | Low risk | No other bias was detected |
Saravanan 2008.
| Methods |
FLUOROSIS STUDY Country of study: India Geographic location: Tamil Nadu Year of study: not stated Year of change of fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: the coverage of children was confined only to primary schools as each village had a primary school and 99% of the children of primary school age group in the study area were attending schools Exclusion criteria: high school children were not included as only 85% of the children of high school age group (11‐16 years) in the study area were attending schools Other sources of fluoride: not stated Ethnicity: not stated Social class: the majority of people in the study setting were of lower socioeconomic class Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: < 0.1 ppm Group 2: < 0.1 ppm Group 3: 0.25 ppm Group 4: 0.56 ppm Group 5: 0.66 ppm Group 6: 0.67 ppm | |
| Outcomes | Dental fluorosis (Dean's Index) Age at assessment: 5‐10 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | All eligible children were invited to participate |
| Confounding | High risk | No details were reported on the use of fluoride from other sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Around 1.1% of the school children were eventually excluded because of absenteeism. It is not clear which fluoride areas they belonged to, however, these participants are unlikely to have been systematically different from those that completed the study |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | Unclear risk | High school children were not included as only 85% of the children of high school age group (11‐16 years) in the study area were attending schools; examiners were calibrated and intra‐and inter‐examiner reliability assessed, however, Kappa scores not reported |
Scheinin 1964.
| Methods |
FLUOROSIS STUDY Country of study: Finland Geographic location: Artjarvi, Askola, Elimaki, Litti, Myrskyla, Parikkala, Taipalsaari, Valkeala, Vehkalahti Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: children aged 11 Exclusion criteria: children resident in area for < 6 years; fluoride concentration of drinking water unknown Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: residence for < 6 years Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 0‐0.1 ppm Group 2: 0.11‐0.39 ppm Group 3: 0.40‐0.99 ppm Group 4: 1.0‐1.59 ppm Group 5: 1.6‐ppm |
|
| Outcomes | Dental fluorosis (community fluorosis index); caries data also evaluated within the study but excluded from review due to study design Age at assessment: 11 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | All eligible children were invited to participate |
| Confounding | High risk | Did not account for the use of fluoride from other sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The dental examinations were carried out as a blind study, the examiners having no information of the preliminary fluoride determinations" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | High risk | Data not in suitable format for analysis |
| Other bias | High risk | No mention of examiner calibration |
Segreto 1984.
| Methods |
FLUOROSIS STUDY Country of study: USA Geographic location: 16 Texas communities Year of study: 1978‐1981 Year of change in fluoridation status: Unclear Study design: cross‐sectional |
|
| Participants | Inclusion criteria: lifetime residents who may have resided at several different addresses in the same community; absence from community for no more than 3 months during any calendar year; grades 2‐6, aged 7‐12 years and grades 9‐12, aged 14‐18 years; city water supply as principal source of drinking water throughout lifetime; non‐usage of water treatment systems that result in defluoridation of water Exclusion criteria: subjects with staining attributable to medication such as tetracycline Other sources of fluoride: not stated Social class: not stated Ethnicity: subjects were primarily those with Spanish surnames or white Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | Unclear if natural or artificial fluoridation Group 1: 0.3 ppm Group 2: 0.3 ppm Group 3: 0.4 ppm Group 4: 1.0 ppm Group 5: 1.3 ppm Group 6: 1.3 ppm Group 7: 1.4 ppm Group 8: 2.3 ppm Group 9: 2.3 ppm Group 10: 2.5 ppm Group 11: 2.7 ppm Group 12: 2.7 ppm Group 13: 2.7 ppm Group 14: 2.9 ppm Group 15: 3.1 ppm Group 16: 4.3 ppm |
|
| Outcomes | Mottled enamel (Dean's Index) Age at assessment: 7‐12 years and 14‐18 years |
|
| Funding | Not stated | |
| Notes | Data extracted from Segreto 1984 differs from that presented in CRD review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | 16 study sites that had a central well as main water supply and sufficient school population were selected |
| Confounding | High risk | Did not account for the use of fluoride from other sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | High risk | Data not in suitable format for analysis |
| Other bias | High risk | No mention of examiner calibration |
Sellman 1957.
| Methods |
FLUOROSIS STUDY Country of study: Sweden Geographic location: Malmo (low F); Simirshamn, Astorp and Nyvang (High F) Year of study: 1953 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: children aged 11‐14 years Exclusion criteria: children missed due to illness; children under 11½ and over 14½ Other sources of fluoride: all children received yearly systematic treatment by the School Dental Service Social class: socioeconomic distribution of lifetime residents was similar in all study areas, however distribution was different for non‐continuous residents compared to continuous residents Ethnicity: not stated Residential history: only results of lifetime residents were presented Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 1.0 ppm Group 2: 1.0‐1.3 ppm Group 3: 1.3 ppm Control: 0.3‐0.5 ppm |
|
| Outcomes | Outcome: dental fluorosis (Dean's Index) Age at assessment: 12‐14 years |
|
| Funding | Not stated | |
| Notes | Data extracted from Sellman 1957 differs from that presented in CRD review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | There was insufficient detail reported to determine how selection took place |
| Confounding | High risk | All children received yearly systematic treatment by the School Dental Service, however, it is not clear whether the use of other fluoride sources was balanced across groups |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data appear to be presented for all participants |
| Selective reporting (reporting bias) | Low risk | All expected outcome reported |
| Other bias | High risk | No mention of examiner calibration and reliability testing |
Selwitz 1995.
| Methods |
FLUOROSIS STUDY Country of study: USA Geographic location: Kewanee (optimal), Monmouth (2 x optimal), Abingdon, Elmwood (3 x optimal), Bushneell, Ipava, Table Grove (4 x optimal), Illinois Year of study: 1980 Year study ended: 1990 Year of change in fluoridation status: unclear Study design: repeated cross‐sectional |
|
| Participants | Inclusion criteria: children aged 8‐10 years and 14‐16 years; written parental consent; lifetime residents of study areas; continuous use of community water supply Exclusion criteria: none stated Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | Unclear whether all was natural fluoridation, parts of the optimally fluoridated area may have been artificially adjusted Group 1: 4 ppm Group 2: 3 ppm Group 3: 2 ppm Group 4: 1 ppm |
|
| Outcomes | Dental fluorosis (% fluorosed surfaces (TSIF); caries data also evaluated within the study but excluded from review due to study design Age at assessment: 8‐10 years and 13‐15 years |
|
| Funding | Not stated | |
| Notes | Data extracted from Selwitz 1995 differs from that presented in CRD review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | There was insufficient detail reported to determine how selection took place. Reference was made to a previous study (Leverett 1986) for further information on sampling, however this study also reported insufficient information on sampling |
| Confounding | High risk | Did not account for the use of fluoride from other sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Data presented for all participants |
| Selective reporting (reporting bias) | High risk | Data not in suitable format for analysis |
| Other bias | Low risk | No other apparent bias |
Selwitz 1998.
| Methods |
FLUOROSIS STUDY Country of study: USA Geographic location: Kewanee (F); Holdrege and Broken Bow (non‐F) Year of study: 1990‐1998 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: lifetime residents of study areas; parental consent Exclusion criteria: none stated Other sources of fluoride: type of toothpaste currently used and used before age 6; use of dietary fluoride supplements; receipt of professionally applied fluoride treatments Social class: not stated Ethnicity: not stated Residential history: lifetime residents Other confounding factors: use of private well‐water |
|
| Interventions | All natural fluoridation Group 1: 1 ppm Group 2: < 0.3 ppm | |
| Outcomes | Dental fluorosis (TSIF); caries data also evaluated within the study but excluded from review due to study design Age at assessment: 8‐10 years and 13‐16 years |
|
| Funding | Not stated | |
| Notes | Data extracted from Selwitz 1998 differs from that presented in CRD review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | There was insufficient detail reported to determine how selection took place |
| Confounding | High risk | Did not account for SES, and there was a difference between groups in the use of fluoride supplements |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | High risk | Data not in suitable format for analysis |
| Other bias | Low risk | No other apparent bias |
Shanthi 2014.
| Methods |
FLUOROSIS STUDY Country of study: India Geographic location: 3 strata (according to fluoride concentration) Khammam district, Andhra Pradesh Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: school children, aged 9‐12 years irrespective of sex, race, and socioeconomic status, who were residents of that particular region and using the same source of drinking water; more than 50% of the crown erupted and no fillings on the facial surface of anterior teeth; co‐operative parental consent Exclusion criteria: children who obtained their drinking water from more than one source; those with orthodontic brackets; children with severe extrinsic stains on their teeth; children with any communicable or systemic diseases and fractured anterior teeth Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: lifetime residents Other confounding factors: the consumption of sugar in the study population was about 61.3% in boys and 38.7% in girls (not specified by group) |
|
| Interventions | All natural fluoridation
Group 1: < 0.7 ppm
Group 2: 0.7‐1.2 ppm Group 3: 1.3‐3.5 ppm |
|
| Outcomes | Dental fluorosis (Dean's Index); caries data also evaluated within the study but excluded from review due to study design Age at assessment: 9‐12 years |
|
| Funding | Stated no funding | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Quote: "A stratified random sampling technique was used" |
| Confounding | Unclear risk | Insufficient information on characteristics of the groups compared |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding not specified |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Number of children in each strata not specified; unclear whether all those sampled were evaluated |
| Selective reporting (reporting bias) | High risk | Fluorosis data not presented by strata |
| Other bias | Low risk | No other apparent bias |
Shekar 2012.
| Methods |
FLUOROSIS STUDY Country of study: India Geographic location: Nalgonda district Year of study: 2008 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: continuous residency; availability on the day of examination. Exclusion criteria: not stated Other sources of fluoride: information on oral hygiene practices, dietary habits, source of drinking water, and amount of liquid consumed in a day, use of fluoridated tooth paste was collected but not reported Ethnicity: not stated Social class: the majority of people in the study setting were from lower socioeconomic class Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: < 0.7 ppm Group 2: 0.7‐1.2 ppm Group 3: 1.2‐2 ppm Group 4: 2.1‐4 ppm Group 5: > 4 ppm | |
| Outcomes | Dental fluorosis (Dean's Index) Age at assessment: 12 and 15 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Schools were selected for study using simple random sampling. All children within those schools were invited to participate |
| Confounding | High risk | SES was broadly similar across groups as was the use of fluoride toothpaste, however, no details were reported regarding use of fluoride supplements |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | Low risk | No other apparent bias |
Skinner 2013.
| Methods |
FLUOROSIS STUDY Country of study: Australia Geographic location: New South Wales Year of study: 2010 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: school students aged 14‐15 years under the jurisdiction of the NSW Department of Education and Training, the Catholic Education Commission and Independent Schools Exclusion criteria: not stated Other sources of fluoride: not stated Ethnicity: aboriginal status was coded from parental responses (not reported by fluoridation status) Social class: self‐reported family income data were provided by parents or guardians and was used as a measure of SES (not reported by fluoridation status) Residential history: not stated Other confounding factors: not stated |
|
| Interventions | Group 1: fluoridated (artificial; ppm not specified) Group 2: non‐fluoridated |
|
| Outcomes | Dental fluorosis (TF); caries data also evaluated within the study but excluded from review due to study design Age at assessment: 14 and 15 years |
|
| Funding | The Centre for Oral Health Strategy NSW | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Quote: "random sample" |
| Confounding | Low risk | Quote: "initial weights were adjusted to ensure the distribution of the sample reflected the regional population distribution of 14‐15‐year‐olds in NSW" |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Particpation rate low (23%). Did not account for all participants in analysis |
| Selective reporting (reporting bias) | Unclear risk | Observed enamel fluorosis/defects were recorded for both the central incisors; not all data reported |
| Other bias | Unclear risk | No other apparent bias |
Skotowski 1995.
| Methods |
FLUOROSIS STUDY Country of study: USA Geographic location: Iowa Year of study: 1991 Year of change in fluoridation status: NA Study design: case‐control study |
|
| Participants | Inclusion criteria: children aged 8‐17 years; patients attending Iowa College of Dentistry's Paediatric clinic; all permanent incisors and first molars present and erupted; parent who could provide consent and details of fluoride exposure accompanied child Exclusion criteria: children with fixed orthodontic appliances; all permanent incisors and first molars present and erupted Other sources of fluoride: dietary fluoride supplement use; age began brushing with toothpaste; toothpaste usage in 8 years; mouth rinse usage; professional fluoride treatments Social class: not stated Ethnicity: not stated Residential history: not stated Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 3.1 ppm Group 2: 5.6 ppm |
|
| Outcomes | Dental fluorosis (TSIF) Age at assessment: 8‐17 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | High risk | The study population was a convenience sample of children receiving treatment at the clinic |
| Confounding | High risk | Did not account for SES. When analysed for effect of duration of residence and use of other fluoride sources, the results were found to have been influenced by duration of exposure and toothpaste usage in 8 years, however the results were not adjusted for these factors |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The examiner had no previous knowledge of subjects’ dental fluorosis status or fluoride exposures" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | High risk | Fluorosis prevalence was not reported according to fluoridation status or fluoride concentration |
| Other bias | High risk | The examiner was not calibrated. Quote: "Because of the burden that replicated examination would cause for the children and their parents, formal reliability assessments were not conducted" |
Spadaro 1955.
| Methods |
FLUOROSIS STUDY Country of study: Italy Geographic location: Barcelona, Pozzo di Gotto, Sicily Year of study: 1954 Year of change in fluoridation status: unclear Study design: cross‐sectional |
|
| Participants | Inclusion criteria: children attending schools in study areas Exclusion criteria: none stated Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: not stated Other confounding factors: not stated |
|
| Interventions | Unclear if natural or artificial fluoridation Group 1: 0.4 ppm Group 2: 1.9 ppm |
|
| Outcomes | Dental fluorosis (index not stated); caries data also evaluated within the study but excluded from review due to study design Age at assessment: 6‐11 years |
|
| Funding | Not stated | |
| Notes | Data from original CRD review (data unverified) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Unable to make a judgement as study was unavailable |
| Confounding | High risk | Did not account for the use of fluoride from other sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unable to make a judgement as study was unavailable |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unable to make a judgement as study was unavailable |
| Selective reporting (reporting bias) | Unclear risk | Unable to make a judgement as study was unavailable |
| Other bias | Unclear risk | Unable to make a judgement as study was unavailable |
Stephen 2002.
| Methods |
FLUOROSIS STUDY Country of study: Scotland Geographic location: Burghead, Kinloss and Findhorn Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: not stated Exclusion criteria: not stated Other sources of fluoride: information on the use of fluoridated tooth paste was collected but not reported Ethnicity: not stated Social class: the socioeconomic analyses showed that 17% of F subjects were in the ‘high’ SES groups I or II, 75% in 'non‐manual' group III, and 8% in 'manual' groups IV or V. For non‐F children, the corresponding percentages were 23%, 60% and 17%, thus revealing a higher percentage of non‐F subjects at either end of the SES scale Residential history: the participants were either lifetime or school‐lifetime (i.e. permanently present therein since commencing full‐time schooling at approximately 5 years of age) residents Other confounding factors: information about oral hygiene practices, dietary habits, source of drinking water, and amount of liquid consumed in a day |
|
| Interventions | All natural fluoridation Group 1: 1‐2.4 ppm Group 2: 0.03 ppm | |
| Outcomes | Dental fluorosis (TF Index); caries data also evaluated within the study but excluded from review due to study design Age at assessment: 5‐6 years (caries only) and 8‐12 years (caries and fluorosis) |
|
| Funding | Supported by a Scottish Office Department of Health grant | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | There was insufficient detail reported to determine how selection took place, however it was reported that about one‐fifth (21.9%) of the eligible participants were not examined because of non‐consent (9.4%) and unavailability for examination (12.6%) |
| Confounding | Unclear risk | Matched by SES, details on the use of fluoride sources show that fluorosis prevalence was not influenced by the use of other fluoride sources. Similar use of fluoride supplements across groups. The age at which brushing with fluoridated paste began did not appear to affect the prevalence of fluorosis, however information on brushing history was only available for the parents who were able to recall |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants were examined without knowledge of their fluoridation status. Slides were viewed blind and scored randomly under standardised projection conditions by the assessors with a 10% random reviewing for inter and intra‐observer agreement calculations |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Only lifetime residents between 8 and 12 years were assessed for fluorosis and data for all of them presented |
| Other bias | Unclear risk | The study involved children between the age of 5‐6 years and 8‐12 years, but the investigators only conducted fluorosis assessments on 8‐ to 12‐year olds so data have been extracted for only children for whom fluorosis assessment was conducted |
Sudhir 2009.
| Methods |
FLUOROSIS STUDY Country of study: India Geographic location: Andhra Pradesh Year of study: 2006‐2007 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: school children aged 13‐15 years; lifelong residence of the region; use of the same source of drinking water from birth to 10 years of age; having permanent teeth with at least > 50% of the crown erupted and no fillings on facial surface Exclusion criteria: migration from some other place; change of source of drinking water; drinking water from more than 1 source; having orthodontic brackets; having teeth with severe extrinsic stains Other sources of fluoride: information was collected on aids used for oral hygiene maintenance (fluoridated or non‐fluoridated); no data on aids used for oral hygiene maintenance reported Ethnicity: not stated Social class: not stated Residential history: lifetime residents Other confounding factors: the questionnaire consisted of information in 2 parts: the first part consisted of information on demographic data, permanent residential address, source of drinking water, duration of use of present source of drinking water, staple food, liquids routinely consumed |
|
| Interventions | All natural fluoridation Group 1: < 0.7 ppm Group 2: 0.7‐1.2 ppm Group 3: 1.3‐4 ppm Group 4: > 4 ppm | |
| Outcomes | Outcome: fluorosis prevalence (TF Index); Age at assessment: 13‐15 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Used a stratified random sampling technique. The entire geographical area of Nalgonda district was divided into 4 strata based on different levels of naturally occurring fluoride in drinking water supply. So in each stratum, or for each level, several villages were involved. Sample size was divided equally among all the 4 strata, and representation from both the sexes was included in the sampling |
| Confounding | High risk | Data were collected on aids used for oral hygiene maintenance (fluoridated or non‐fluoridated) but not reported |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Data presented for all participants |
| Selective reporting (reporting bias) | High risk | Data not in suitable format for analysis |
| Other bias | Low risk | No other apparent bias |
Szpunar 1988.
| Methods |
FLUOROSIS STUDY Country of study: USA Geographic location: Hudson, Redford, Richmond (F); Cadillac (non‐F), Michigan Year of study: not stated Year of change in fluoridation status: not stated Study design: cross‐sectional |
|
| Participants | Inclusion criteria: lifetime residents of study areas; children aged 6‐12 years Exclusion criteria: none stated Other sources of fluoride: use of fluoride supplements; dental attendance; time interval since last dental visit; age began brushing (parent & child); age at start of F rinsing; feeding method in 1st year of life. Social class: not stated Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | Group 1: 1.2 ppm (artificial fluoridation) Group 2: 1.0 ppm (artificial fluoridation) Group 3: 0.8 ppm (artificial fluoridation) Group 4: 0.0 ppm (natural fluoridation) | |
| Outcomes | Dental fluorosis (TSIF); caries data also evaluated in the study but not included in the review due to study design Age at assessment: 6‐12 years |
|
| Funding | NIH National Research Service Award | |
| Notes | Data extracted from Szpunar 1988 differs from that presented in CRD review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Classroom teachers distributed and collected permission slips |
| Confounding | High risk | Did not appear to account for the use of fluoride from other sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Data collected for 1103 participants but only lifetime resident data (n = 556) presented |
| Selective reporting (reporting bias) | Low risk | Relevant fluorosis outcome data |
| Other bias | Low risk | No other apparent risk of bias |
Tabari 2000.
| Methods |
FLUOROSIS STUDY Country of study: UK Geographic location: Northumberland and Newcastle upon Tyne Year of study: 1998 Year of change in fluoridation status: 1969 Study design: cross‐sectional |
|
| Participants | Inclusion criteria: parental consent; lifetime residency Exclusion criteria: not stated Ethnicity: not stated Other sources of fluoride: data on the use of fluoride drops and tablets collected but not presented. Data on toothbrushing habit/frequency presented in detail and appeared to be similar in F and non‐F areas Social class: the subjects from Newcastle tended to reside in more underprivileged areas than those in Northumberland. The mean Jarman UPA8 score was 16.3 (SD = 19.1) for subjects in Newcastle and 7.3 (SD = 15.0) for Northumberland (P value < 0.001). However, the authors were reported to have chosen schools to provide children from a spectrum of SES backgrounds Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | Group 1: 1 ppm (artificial fluoridation) Group 2: 0.1 ppm (natural fluoridation) | |
| Outcomes | Dental fluorosis (TF Index); Age at assessment: 8‐9 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | In Newcastle and Northumberland, 14 and 15 schools respectively were chosen. However, there was insufficient information on how the selection was done |
| Confounding | High risk | There was a significant difference in measure of deprivation between the 2 study areas |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessment was by the use of photographs in order to allow examination of teeth of children without the examiner being aware of which area the child was from |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | In the 2 groups, 78% and 79% of the eligible children had complete data. It was not clear whether those whose photographs were unacceptable (examined but not analysed) were systematically different from those who remained in the study |
| Selective reporting (reporting bias) | Low risk | Outcome of interested reported |
| Other bias | Low risk | No other apparent bias |
Tessier 1987.
| Methods |
CARIES STUDY Country of study: Canada (province of Québec) Geographic location: Windsor (F) and Richmond (non‐F) Year study started: 1977 Year study ended: 1986 Year of change in fluoridation status: 1978 Study design: CBA |
|
| Participants | Inclusion criteria: All 6‐ and 7‐year‐old schoolchildren Exclusion criteria: children living too far from the fluoridated water supply; or drinking fluoridated water 3 years or less Other sources of fluoride: mouthwash and toothpaste; participants underwent similar fluoride rinse programmes Social class: comparable study areas with similar socioeconomic status and lifestyles Ethnicity: not stated Residential history: not stated Other confounding factors: similar access to dental care, oral hygiene and levels of dental plaque |
|
| Interventions | Group 1: 'optimal' level ‐ ppm not stated (artificial fluoridation) Control: 'low' level ‐ ppm not stated (natural fluoridation) |
|
| Outcomes | DMFT; % caries prevalence Age at baseline measure: 6 and 7 years Age at final measure: 6 and 7 years |
|
| Funding | Not stated | |
| Notes | Translated from French | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | All children aged 6 and 7 years in both study areas were selected |
| Confounding | High risk | Participants might have had varied exposures to fluoridated water. No details were reported on the dietary habits of the children |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | High risk | Standard deviation not reported |
| Other bias | High risk | No mention of examiner calibration and reliability testing |
Tsutsui 2000.
| Methods |
FLUOROSIS STUDY Country of study: Japan Geographic location: not stated Year of study: 1987 Year of change in fluoridation status: naturally occurring fluoride Study design: cross‐sectional |
|
| Participants | Inclusion criteria: use of municipal water supply and lifelong residency of study area; difference of ≤ 0.2 ppm where home and school were located in different water supply areas Exclusion criteria: failure to meet any of the inclusion criteria; other reasons for exclusion were incomplete questionnaire and periodic application of topical fluoride Other sources of fluoride: children that had received periodic applications of topical fluoride were excluded; no children had used fluoride mouth rinses; use of fluoride‐containing toothpaste was not determined as the market share was only 12% and thus not commonly used by children at the time Ethnicity: not stated Social class: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 0‐0.2 ppm Group 2: 0.2‐0.4 ppm Group 3: 0.4‐0.6 ppm Group 4: 0.6‐0.8 ppm Group 5: 0.8‐1 ppm Group 6: 1‐1.4 ppm |
|
| Outcomes | Dental fluorosis (Dean's Index); caries data also evaluated within the study but excluded from review due to study design Age at assessment: 10‐12 years |
|
| Funding | Niigata University | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | All eligible children were invited to participate |
| Confounding | High risk | Did not account for SES |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The examiners had no knowledge of the concentration of fluoride in the drinking water where they carried out the examinations |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Out of the 1967 children that were examined, data for 907 (46.1%) were not presented |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | Low risk | No other apparent bias |
Venkateswarlu 1952.
| Methods |
FLUOROSIS STUDY Country of study: India and Switzerland Geographic location: villages in the Visakhapatnam area (India), and 3 villages in Switzerland Year of study: not stated Year of change in fluoridation study: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: children aged 3‐14 years; areas with ≤ 2 ppm F in water supplies Exclusion criteria: none stated Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: not stated Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 0.3 ppm Group 2: 0.5 ppm Group 3: 0.5 ppm Group 4: 0.9 ppm Group 5: 0.9 ppm Group 6: 0.9 ppm Group 7: 0.9 ppm Group 8: 1 ppm Group 9: 1.3 ppm Group 10: 1.4 ppm Group 11: 0.5‐0.8 ppm Group 12: 0.4‐1.6 ppm |
|
| Outcomes | Dental fluorosis (Dean's Index); caries data also evaluated within the study but excluded from review due to study design Age at assessment: 3‐14 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Children aged 3‐14 years belonging to the study areas were examined; as far as possible, at least 100 children per village. It was not clear how exactly these children were selected |
| Confounding | High risk | Did not account for the use of fluoride from other sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 12 Indian villages were involved in the study; data from 1 village (Malkapuram) with 102 participants not presented |
| Selective reporting (reporting bias) | High risk | Data not in suitable format for analysis |
| Other bias | High risk | Calibration of examiners not mentioned |
Vignarajah 1993.
| Methods |
FLUOROSIS STUDY Country of study: Antigua Geographic location: urban and rural areas in Antigua Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: children aged 12‐14 years; lifetime residents of study areas Exclusion criteria: restored or fractured tooth surfaces Other sources of fluoride: toothpaste swallowing when younger; consumption of mixed sources of water; fluoride mouth rinses Social class: not stated Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 0.6‐1 ppm Group 2: 0.1‐0.3 ppm |
|
| Outcomes | Dental fluorosis (TSIF) Age at assessment: 12‐14 years |
|
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | A stratified random technique using random number tables was used to select schools and children. Quote: "All the schools were first listed and then divided into two groups, urban and rural…" |
| Confounding | High risk | Did not account for SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Number of participants recruited not stated |
| Selective reporting (reporting bias) | Low risk | Outcome of interest presented |
| Other bias | Low risk | No other apparent bias |
Vilasrao 2014.
| Methods |
FLUOROSIS STUDY Country of study: India Geographic location: 7 districts of the Chhattisgarh State Year of study: 2013‐2014 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: none stated Exclusion criteria: none stated Other sources of fluoride: not stated Ethnicity: not stated Social class: not stated Residential history: not stated Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 3.8 ppm Group 2: 2.5 ppm Group 3: 2.0 ppm Group 4: 3.0 ppm Group 5: 2.2 ppm Group 6: 2.8 ppm Group 7: 3.3 ppm |
|
| Outcomes | Dental fluorosis (assessed using: mottled enamel, chalk white, yellowish brown or brownish black, horizontal streaks over teeth); bowing of legs/spine also evaluated | |
| Funding | Ministry of Health and Family Welfare | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Quote: "door‐to‐door survey .... randomly selected" |
| Confounding | High risk | Did not acount for potential confounding factors |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insuffieicnt information |
| Selective reporting (reporting bias) | High risk | Number of participants by district not reported |
| Other bias | Unclear risk | No other apparent bias |
Villa 1998.
| Methods |
FLUOROSIS STUDY Country of study: Chile Geographic location: Rancagua (non‐F), Santiago (low‐F), La Serena (medium‐F), San Felipe and Iquique (high‐F) Year of study: 1996 Year of change in fluoridation status: fluoride was naturally occurring Study design: cross‐sectional study |
|
| Participants | Inclusion criteria: lifetime residents of study areas; children aged 7,12 and 15 years in selected schools in study areas Exclusion criteria: none stated Other sources of fluoride: not stated Social class: children selected from schools graded according to socioeconomic status to give similar socioeconomic distribution in each study area Ethnicity: not stated Residential history: lifetime residents Other confounding factors: temperature |
|
| Interventions | All natural fluoridation Group 1: 0.07 ppm Group 2: 0.21 ppm Group 3: 0.55 ppm Group 4: 0.93 ppm Group 5: 1.10 ppm |
|
| Outcomes | Dental fluorosis (Deans Index); caries data also evaluated within the study but excluded from review due to study design Age at assessment: 15 years |
|
| Funding | Study was supported by the Chilean Council for Scientific and Technological Research (FONDECYT) through grant no. 1960993 | |
| Notes | Data extracted Villa 1998 differs from that presented in CRD review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Selection of schools for each community was made at random from the complete list of private schools and publicly supported elementary schools. All eligible children were invited to participate |
| Confounding | High risk | Did not account for the use of fluoride from other sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Data not in suitable format for analysis |
| Other bias | High risk | There may have been misclassification bias as fluorosis prevalence was reported without taking 'questionable' fluorosis prevalence into account |
Vuhahula 2009.
| Methods |
FLUOROSIS STUDY Country of study: Tanzania Geographic location: Arusha, Shinyanga, Manyara, Dodoma, Singida and Tabora Year of study: not stated Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: aged 12‐18 years; lifelong residence Exclusion criteria: in order to avoid over‐scoring, teeth that were tempered with by grinding or other forms of mutilations were excluded Other sources of fluoride: not stated Ethnicity: not stated Social class: not stated Residential history: mostly lifelong residents Other confounding factors: information on 'magadi' consumption was collected, however, participants seemed to be accessing 'magadi' from different sources making the correlation of fluoride in 'magadi' versus dental fluorosis complicated |
|
| Interventions | All natural fluoridation Group 1: 2.2 ppm Group 2: 2.4 ppm Group 3: 2.5 ppm Group 4: 4.2 ppm Group 5: 4.7 ppm Group 6: 5.6 ppm |
|
| Outcomes | Dental fluorosis (Dean's Index) Age at assessment: 12‐18 years |
|
| Funding | Funded by the Japanese International Cooperation Agency (JICA) of Tanzania | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Regions were randomly chosen and then schools within them. Children were quota sampled from these schools |
| Confounding | High risk | Did not account for the use of fluoride from other sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | High risk | Data not in suitable format for analysis |
| Other bias | Low risk | No other apparent bias |
Wang 1993.
| Methods |
FLUOROSIS STUDY Country of study: China Geographic location: Hotan, Kaxgar and Aksu, in south Xinjiang Year of study: 1991 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: children aged from 8‐15 years living around the water source Exclusion criteria: not stated Other sources of fluoride: not stated Social class: farmers and herdsmen in south Xinjiang Ethnicity: Minority, mainly Uygur ethnic group Residential history: living in study area for a long time ("since many years ago") Other confounding factors: the combined effects of iodine deficiency and high fluorine; the habit of tea drinking |
|
| Interventions | All natural fluoridation Group 1: 1.58 ppm Group 2: 1.85‐2.00 ppm Group 3: 0.48 ppm Group 4: 2.55 ppm Group 5: 0.43 ppm Group 6: 0.46 ppm Group 7: 0.43 ppm |
|
| Outcomes | Dental fluorosis (index not stated) Age at assessment: 15 years |
|
| Funding | Not stated in translation | |
| Notes | Paper translated from Chinese | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Children aged 8‐15 living in the vicinity of the water sources were included. Insufficient sampling information |
| Confounding | High risk | Did not account for the use of fluoride from other sources, residential history not clearly stated |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data for all participants reported |
| Selective reporting (reporting bias) | Low risk | Outcome of interest presented |
| Other bias | Unclear risk | Unable to identify information pertaining to the training/reliability of outcome assessors |
Wang 1999.
| Methods |
FLUOROSIS STUDY Country of study: China Geographic location: Xindiliang Village (high F), Shiligetu Village (lower F) Year of study: 1999 Year of change in fluoridation status: NA Study design: cross sectional study |
|
| Participants | Inclusion criteria: not stated Exclusion criteria: not stated Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: not stated Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 1.3 ppm Group 2: 2‐4 ppm |
|
| Outcomes | Dental fluorosis and skeletal fluorosis (3 grade classification for both) Age at assessment: all ages |
|
| Funding | Japan International Cooperation Agency | |
| Notes | Removal of fluoride from the water in these areas was attempted in the 1980s but failed to be applied continuously | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Households in the villages of study were arbitrarily chosen so that 25% were included in the study |
| Confounding | High risk | Did not account for the use of fluoride from other sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest presented |
| Other bias | High risk | There was no mention of examiner calibration |
Wang 2012.
| Methods |
FLUOROSIS STUDY Country of study: China Geographic location: not stated Year of study: 2008‐2009 Year of change in fluoridation status: NA Study design: cross sectional |
|
| Participants | Inclusion criteria: not stated Exclusion criteria: not stated Other sources of fluoride: not stated Social class: not stated Ethnicity: not stated Residential history: in the mild, moderate and severe endemic areas, the authors made reference to native‐born residents, but it is not clear what proportion of them constituted the entire population Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 1.3 ppm Group 2: 2‐4 ppm |
|
| Outcomes | Dental fluorosis (Dean's Index); skeletal fluorosis Age at assessment: 8‐12 years for dental fluorosis and > 16 years for skeletal fluorosis |
|
| Funding | Supported by the Chinese government for Endemic Disease Control in 2008‐2009 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | Villages were selected at random, and in the selected villages, all eligible children were invited to participate |
| Confounding | High risk | Did not account for the use of fluoride from other sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Unclear risk | Outcome of interest reported |
| Other bias | High risk | No mention of examiner calibration |
Warnakulasuriya 1992.
| Methods |
FLUOROSIS STUDY Country of study: Sri Lanka Geographic location: 4 geographic areas at same altitude and temperature from 4 districts in Sri Lanka (Galewala, Wariyapola, Kekirawa and Rambukkana) Year of study: 1986 Year of change in fluoridation status: NA Study design: cross‐sectional |
|
| Participants | Inclusion criteria: lifetime residents of study areas; children aged 14 years Exclusion criteria: children who lived more than 15 miles from school; children absent on day of examination Other sources of fluoride: fluoride containing toothpaste or other fluoride therapies had not been used by or on these children during time of development of primary dentition; tea consumption high Social class: wide ranges of socioeconomic differences not expected Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: <0.39 ppm Group 2: 0.4‐0.59 ppm Group 3: 0.6‐0.79 ppm Group 4: 0.8‐0.99 ppm Group 5: >1.0 ppm |
|
| Outcomes | Fluorosis (Dean's Index); caries data evaluated in study but not included in review due to study design Age at assessment: 14 years |
|
| Funding | National Water Supply, Sri Lanka | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | All eligible children in each school were invited to participate |
| Confounding | Unclear risk | The study authors considered that fluoride supplements or paste were not widely used among the study population and that SES was broadly similar across groups, however no supporting information was provided |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data presented for all participants |
| Selective reporting (reporting bias) | Low risk | Outcome of interest presented |
| Other bias | Low risk | No other apparent bias |
Warren 2001.
| Methods |
FLUOROSIS STUDY Country of study: USA Geographic location: Iowa Year of study: 1997‐2000 Year of change in fluoridation status: unclear Study design: cross‐sectional data from within cohort study |
|
| Participants | Inclusion criteria: not stated Exclusion criteria: not stated. Other sources of fluoride: fluoride dentifrice use = 159/637 (25%); dietary fluoride supplement use = 131/637 (20.6%). There was no difference in fluorosis prevalence between those who used other sources of fluoride and those who did not Ethnicity: not stated Social class: not stated Residential history: mostly lifelong residents Other confounding factors: not stated |
|
| Interventions | Group 1: < 0.7 ppm (natural fluoridation) Group 2: 0.7‐1.2 ppm (artificial fluoridation) Group 3: > 1.2 ppm (natural fluoridation) |
|
| Outcomes | Fluorosis prevalence (TSIF) Age at assessment: 4.5‐5 years |
|
| Funding | Supported by NIH grants 2ROl‐DE09551, 2P30‐10126, and CRC‐RROOO5 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Children included in the present study were part of the Iowa Fluoride Study cohort, which had been followed prospectively since birth. Full details were not reported |
| Confounding | High risk | Did not account for SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Outcome data available for 559 out of the 637 (87.8%) participants due to lack of information on water fluoride concentration |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | Low risk | No other apparent bias |
Wenzel 1982.
| Methods |
FLUOROSIS STUDY Country of study: Denmark Geographic location: Naestved (F); Greve (F); Ry (non‐F) Year of study: not stated Year of change in fluoridation status: not stated Study design: cross‐sectional |
|
| Participants | Inclusion criteria: lifetime residents of study areas; girls aged 12‐15 years Exclusion criteria: children with orthodontic appliances; history of additional fluoride use Other sources of fluoride: only children without fluoride use were included; no attempt was made to distinguish between users and non‐users of fluoridated dentifrice Social class: not stated Ethnicity: not stated Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | Group 1: < 0.2 ppm Group 2: 1.0 ppm Group 3: 2.4 ppm |
|
| Outcomes | Fluorosis (TF Index); skeletal maturity Age at assessment: 12‐14 years |
|
| Funding | Sponsored by Colgate Palmolive, Denmark | |
| Notes | Data extracted Wenzel 1982 differs from that presented in CRD review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Insufficient detail reported to determine how selection took place |
| Confounding | High risk | Did not account for SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data for all participants presented |
| Selective reporting (reporting bias) | Low risk | Outcome of interest presented |
| Other bias | High risk | No information on examiner calibration |
Whelton 2004.
| Methods | FLUOROSIS STUDY Country of study: Republic of Ireland (RoI) Geographic location: not stated Year of study: 2001/2002 Year of change in fluoridation status: 1964 Study design: cross‐sectional | |
| Participants | Inclusion criteria: children in Junior Infants, Second Class, Sixth Class, and Junior Certificate Exclusion criteria: not stated. Other sources of fluoride: participants in the fluoridated group may have had additional exposure to fluoride tablets and fluoride mouth rinses Ethnicity: not stated Social class: possesion of a medical card was used in this study as a surrogate for disadvantage; RoI medical card vs no medical card = 24% vs 75% (full F = 25.2% vs 74.4%; non‐F = 20.3% vs 79.4%); figures do not add up to 100%, however, authors reported that figures included children for whom medical card details were missing Residential history: fluoridated group subjects' home water supply had to have been fluoridated continuously since birth, and the non‐fluoridated group subjects' home water supply had never to have been fluoridated. No further details reported Other confounding factors: not stated |
|
| Interventions | Group 1: 0.8‐1 ppm (artificial fluoridation) Group 2: 'non‐fluoridated' |
|
| Outcomes | Fluorosis prevalence (Dean's Index); caries data (dmft/DMFT) evaluated in study but not included in review due to study design Age at assessment: 5, 8, 12 and 15 years | |
| Funding | Funded by the Department of Health and Children and the Health Boards in Ireland | |
| Notes | The authors carried out and reported power calculation for the primary outcome (DMFT) but not for the fluorosis outcome | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | National survey using a cluster sampling technique with schools as the clustering unit and children in Junior Infants, Second Class, Sixth Class and Junior Certificate were selected |
| Confounding | High risk | SES accounted for in caries analysis; did not account for the use of fluoride from other sources or the dietary habits of the children |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Fluoride codes ascribed after examinations; unlikely to be systematic bias |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Outcome data presented as a percentage; unclear if accounted for all participants |
| Selective reporting (reporting bias) | Unclear risk | Fluorosis outcomes presented as percentages; unclear if accounted for all participants |
| Other bias | Low risk | No other apparent bias |
Whelton 2006.
| Methods | FLUOROSIS STUDY Country of study: Republic of Ireland (RoI) and Northern Ireland (NI) Geographic location: not stated Year of study: 2001/2002 Year of change in fluoridation status:1964 Study design: cross‐sectional | |
| Participants | Inclusion criteria: Junior Infants, Second Class, Sixth Class and Junior Certificate in RoI and Primary 1, Primary 4, Year 1 and Year 4 in NI Exclusion criteria: not stated Other sources of fluoride: participants in the fluoridated group may have had additional exposure to fluoride tablets and fluoride mouth rinses Ethnicity: not stated Social class: possession of a medical card (MC) was used in this study as a surrogate for disadvantage in RoI, whilst receipt of low‐income benefits (LIB) was used as a surrogate for disadvantage in NI. RoI full‐F: MC vs no MC = 25.2% vs 74.4%; NI non‐F LIB vs no LIB = 37.3% vs 61.3%; figures do not add up to 100%, however, authors reported that figures included children for whom MC/LIB details were missing Residential history: fluoridated group subjects' home water supply had to have been fluoridated continuously since birth and the non‐fluoridation group subjects' home water supply had never to have been fluoridated. No further details reported Other confounding factors: not stated |
|
| Interventions | Group 1 (RoI): 0.8‐1 ppm (artificial fluoridation) Group 2 (NI): 'non‐fluoridated' ‐ ppm not reported |
|
| Outcomes | Fluorosis prevalence (Dean's Index); caries data (dmft/DMFT) evaluated in study but not included in review due to study design Age at assessment: 5, 8, 12 and 15 years | |
| Funding | Funded by the Department of Health and Children and the Health Boards in Ireland | |
| Notes | The authors carried out and reported power calculation for the primary outcome (DMFT), but not for the fluorosis outcome | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | National survey using a cluster sampling technique with schools as the clustering unit and children in Junior Infants, Second Class, Sixth Class and Junior Certificate in RoI and Primary 1, Primary 4, Year 1 and Year 4 in NI |
| Confounding | High risk | SES accounted for in caries analysis; did not account for the use of fluoride from other sources or the dietary habits of the children; used different measures for assessing SES |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Fluoride codes ascribed after examinations; unlikely to be systematic bias |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Outcome data presented as a percentage; unclear if accounted for all participants |
| Selective reporting (reporting bias) | Unclear risk | Fluorosis outcomes presented as percentages; unclear if accounted for all participants |
| Other bias | Low risk | No other apparent bias |
Wondwossen 2004.
| Methods | FLUOROSIS STUDY Country of study: Ethiopia Geographic location: not stated Year of study: 1997 Year of change in fluoridation status: NA Study design: cross‐sectional | |
| Participants | Inclusion criteria: not stated Exclusion criteria: not stated Other sources of fluoride: not stated Ethnicity: not stated Social class: the villages were of approximately the same size and socioeconomic standards and were selected purposively for the study. Residential history: fluoridated group subjects' home water supply had to have been fluoridated continuously since birth and the non‐fluoridation group subjects' home water supply had to have never been fluoridated. No further details reported Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 0.3‐2.2 ppm Group 2: 10‐14 ppm |
|
| Outcomes | Fluorosis prevalence (TF Index); caries data evaluated in study but not included in review due to study design Age at assessment: 12‐15 years | |
| Funding | Supported by the Norwegian State Educational Loan Fund, NUFU Project 61/96 and the Committee for Research and Postgraduate Training, Faculty of Dentistry, University of Bergen, Norway and the Faculty of Medicine (Fluoride Project), University of Addis Ababa, Ethiopia | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Participants were chosen from a census, however, insufficient detail was reported on individual selection |
| Confounding | High risk | Did not account for the use of fluoride from other sources |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "Intra‐oral examination was conducted at the health centers of the areas by two examiners" Blinding not undertaken |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data for all participants presented |
| Selective reporting (reporting bias) | Low risk | Outcome of interest reported |
| Other bias | Low risk | No other apparent bias |
Zheng 1986.
| Methods | FLUOROSIS STUDY Country of study: China Geographic location: Guangzhou and Fangcun (F); Fushan and Zhaoqing (non‐F) Year of study: not stated Year of change in fluoridation status: not stated Study design: cross‐sectional | |
| Participants | Inclusion criteria: students who were 7‐, 9‐, 12‐, 15‐, and 17‐years old Exclusion criteria: not stated Other sources of fluoride: not stated, but time point of 1975 in Guangdong province of China would be mean that exposure to fluoridated toothpaste could be assumed Social class: not stated Ethnicity: chinese Residential history: lifetime residents Other confounding factors: not stated |
|
| Interventions | Group 1: 0.6‐1.2 ppm (artificial fluoridation) Group 2: 0.4‐1.2 ppm (artificial fluoridation) Group 3: 0.2 ppm (natural fluoridation) Group 4: 0.2 ppm (natural fluoridation) |
|
| Outcomes | Outcome: fluorosis prevalence (Dean's Index) Age at assessment: 12‐17 years |
|
| Funding | Not stated | |
| Notes | Data extracted from Zheng 1986 differs from that presented in CRD review Translated from Chinese |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Unclear risk | Insufficent information to make a judgement |
| Confounding | High risk | Did not appear to account for SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Fluorosis data for all participants reported |
| Selective reporting (reporting bias) | High risk | The authors seem to have collected caries data at baseline, but reported only the follow‐up data |
| Other bias | Unclear risk | Unable to identify information pertaining to the training/reliability of outcome assessors |
Zimmermann 1954.
| Methods | FLUOROSIS STUDY Country of study: USA Geographic location: Aurora, Illinois (F); Montgomery and Prince Georges counties, Maryland (non‐F) Year of study: 1953 Year of change in fluoridation status: NA Study design: cross‐sectional | |
| Participants | Inclusion criteria: lifetime residents of study areas; white children aged 12‐14 years Exclusion criteria: children who had left study areas for periods of time other than for holidays Other sources of fluoride: not stated Social class: not stated Ethnicity: white children only Residential history: continuous residents Other confounding factors: not stated |
|
| Interventions | All natural fluoridation Group 1: 0.2 ppm Group 2: 1.2 ppm |
|
| Outcomes | Fluorosis (Deans Index); caries data evaluated in study but not included in review due to study design Age at assessment: 12‐14 years | |
| Funding | Not stated | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Sampling | Low risk | All eligible children were invited to participate |
| Confounding | Low risk | Did not account for the use of fluoride from other sources or SES |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Insufficient information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data for all participants presented |
| Selective reporting (reporting bias) | Low risk | Outcome of interest presented |
| Other bias | High risk | There was no mention of examiner calibration |
Abbreviations
CBA: controlled before‐and‐after study CFI: Community Fluorosis Index CRD: Centre for Reviews and Dissemination DDE: developmental defects of tooth enamel dmft: decayed, missing and filled deciduous teeth DMFT: decayed, missing and filled permanent teeth F: fluoride/fluoridated ITS: interrupted time series study LIB: low‐income benefits NA: not applicable NI: Northern Ireland non‐F: non‐fluoridated NUFU: Norwegian Programme for Development, Research and Education RoI: Republic of Ireland SD: standard deviation SE: standard error SES: socioeconomic status TF Index: Thylstrup‐Fejerskov Index TSIF: Tooth Surface Index of Fluorosis UPA8: under privileged area 8
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Acharya 2003 | Evaluated caries in a single time point cross‐sectional study |
| Agarwal 2014 | Evaluated fluorosis levels in single area |
| Ajayi 2008 | Evaluated caries in a single time point cross‐sectional study |
| Akosu 2008 | No direct comparison of different fluoride concentrations |
| Aldosari 2004 | Evaluated caries in a single time point cross‐sectional study |
| Aleksejuniene 2004 | Naturally high fluoride area was compared to a low fluoride area, however, there was no change in concentration at the 2 time points reported |
| Alimskii 2000 | Unable to locate study |
| Antunes 2004 | Evaluated caries in a single time point cross‐sectional study |
| Anuradha 2002 | Evaluation of periodontal disease in relation to fluoride concentration |
| Archila 2003 | Evaluated caries in a single time point cross‐sectional study |
| ARCPOH 2008 | Evaluated caries in a single time point cross‐sectional study |
| Armfield 2004 | Evaluated caries in a single time point cross‐sectional study |
| Armfield 2005 | Evaluated caries in a single time point cross‐sectional study |
| Armfield 2007 | Evaluated caries in a single time point cross‐sectional study |
| Armfield 2010 | Evaluated caries in a single time point cross‐sectional study |
| Arora 2010 | Evaluated caries in a single time point cross‐sectional study |
| Attwood 1988 | Inappropriate design for studying cessation of water fluoridation |
| Bailie 2009 | Evaluated caries in a single time point cross‐sectional study |
| Baldani 2002 | Evaluated caries in a single time point cross‐sectional study |
| Baldani 2004 | Evaluated caries in a single time point cross‐sectional study |
| Bihari 2008 | No fluorosis data |
| Binbin 2005 | Evaluated caries in a single time point cross‐sectional study |
| Blagojevic 2004 | Evaluated caries in a single time point cross‐sectional study |
| Blayney 1960 | Data measured at different time points for fluoridated and non‐fluoridated areas |
| Bo 2003 | Evaluation of skeletal/dental fluorosis |
| Bottenberg 2004 | No distinct comparison between areas |
| Bradnock 1984 | Evaluated caries in a single time point cross‐sectional study |
| Buchel 2011 | Comparison of water fluoridation and salt fluoridation |
| Burt 2000 | Assesses effect of break in water fluoridation in single area |
| Buscariolo 2006 | Evaluated fluorosis levels in single area |
| Buzalaf 2004 | Assessed effect of break in water fluoridation in single area |
| Campain 2010 | Evaluated cost savings from community water fluoridation in Australia |
| Carmichael 1980 | Evaluated caries in a single time point cross‐sectional study |
| Carmichael 1984 | Evaluated caries in a single time point cross‐sectional study |
| Carmichael 1989 | Evaluated caries in a single time point cross‐sectional study |
| Carvalho 2007 | Assessed fluorosis prior to commencing water fluoridation |
| Catani 2007 | Compared areas with ‘one with homogenous fluoride concentration and oscillating concentration’ |
| Chen 2009 | No direct comparison of different fluoride concentrations |
| Chen 2012 | No distinct comparison between areas |
| Cheng 2000 | Compared different ethnic populations receiving similar water fluoride levels |
| Ciketic 2010 | Cost‐effectiveness study |
| Clark 2006 | Assessed fluorosis after cessation of water fluoridation |
| de Lourdes Azpeitia‐Valadez 2009 | Compared areas but no mention of differing fluoride concentrations |
| Dini 2000 | Comparison of areas with different duration of water fluoridation |
| Do 2007 | Evaluated risk‐benefit balance of several fluoride exposures |
| Dobaradaran 2008 | No concurrent control |
| Evans 1995 | Evaluated caries in a single time point cross‐sectional study |
| Evans 2009 | Evaluated the effect of a water fluoridation programme in the single area |
| Faye 2008 | Evaluated fluorosis in single city following change in water supply |
| Gillcrist 2001 | Evaluated caries in a single time point cross‐sectional study |
| Gushi 2005 | Evaluated caries in a single time point cross‐sectional study |
| Han 2011 | Evaluated caries in a single time point cross‐sectional study |
| Hobbs 1994 | Inappropriate design for studying cessation of water fluoridation |
| Hoffmann 2004 | Evaluated dental caries between children attending public and private schools in fluoridated city |
| Hopcraft 2003 | Cross‐sectional study evaluating caries experience; no comparison of fluoride concentrations and no fluorosis data |
| Hussain 2013 | Focused on evaluation of groundwater concentrations |
| Ito 2007 | Thesis ‐ unable to access |
| Jones 1997 | Evaluated caries in a single time point cross‐sectional study |
| Jones 2000a | Evaluated caries in a single time point cross‐sectional study |
| Jones 2000b | Evaluated caries in a single time point cross‐sectional study |
| Kalsbeek 1993 | Inappropriate design for studying cessation of water fluoridation |
| Khan 2004 | Evaluated dose‐response relationship between the prevalence of dental caries; did not compare fluorosis levels by fluoride concentration |
| Kirkeskov 2010 | Evaluated caries in a single time point cross‐sectional study |
| Kozlowski 2002 | Abstract only |
| Kukleva 2007 | Evaluated fluorosis levels in single area (with high use of bottled water) |
| Kumar 2001 | Evaluated caries in a single time point cross‐sectional study |
| Kunzel 2000 | Data measured at different time points for fluoridated and non‐fluoridated areas |
| Kunzel 2000a | No concurrent control group |
| Lee 2004 | Evaluated caries in a single time point cross‐sectional study |
| Liu 2006 | Evaluated fluorosis with regard to improvement in water supply |
| Liu 2009 | Evaluated fluorosis with regard to improvement in water supply |
| Murray 1984 | Evaluated caries in a single time point cross‐sectional study |
| Murray 1991 | Evaluated caries in a single time point cross‐sectional study |
| Nayak 2009 | No comparison made |
| Ncube 2005 | Evaluated fluorosis with regard to improvement in water supply |
| Nirgude 2010 | Evaluated fluorosis levels in single area |
| Niu 2012 | Evaluated fluorosis with regard to improvement in water supply |
| Pandey 2002 | Evaluated fluorosis with regard to improvement in water supply |
| Pandey 2005 | Evaluated fluorosis with regard to improvement in water supply |
| Pandey 2010 | Evaluated fluorosis with regard to improvement in water supply |
| Peres 2006 | Evaluated caries in a single time point cross‐sectional study |
| Provart 1995 | Evaluated caries in a single time point cross‐sectional study |
| Rihs 2008 | Evaluated caries in a single time point cross‐sectional study |
| Riley 1999 | Evaluated caries in a single time point cross‐sectional study |
| Ruan 2004 | Evaluated fluorosis with regard to improvement in water supply |
| Rugg‐Gun 1977 | Evaluated caries in a single time point cross‐sectional study |
| Sagheri 2007 | Evaluated caries in a single time point cross‐sectional study |
| Sales‐Peres 2002 | Evaluated caries in a single time point cross‐sectional study |
| Saliba 2008 | Evaluated caries in a single time point cross‐sectional study |
| Sampaio 2000 | Evaluated caries in a single time point cross‐sectional study |
| Seppa 1998 | Inappropriate design for studying cessation of water fluoridation |
| Shitumbanuma 2007 | Evaluated fluorosis levels associated with drinking water from hot springs |
| Slade 2013 | Evaluated caries in a cross‐sectional study; no fluorosis data |
| Sohu 2007 | No clear comparison of fluorosis across different fluoride concentrations |
| Spencer 2008 | Mixed fluoridation status of study areas |
| Sun 2007 | Evaluated fluorosis with regard to improvement in water supply |
| Tagliaferro 2004 | Evaluated caries in a single time point cross‐sectional study |
| Tiano 2009 | Evaluated caries in a single time point cross‐sectional study |
| Tickle 2003 | Evaluated caries in a single time point cross‐sectional study |
| Vuhahula 2008 | Evaluated fluorosis with regard to improvement in water supply |
| Wang 2005 | Evaluated fluorosis with regard to improvement in water supply |
| Wang 2008 | Evaluated fluorosis with regard to improvement in water supply |
| Wei 2010 | Evaluated fluorosis with regard to improvement in water supply |
| Wong 2006 | No concurrent control |
| Wong 2014 | Evaluated fluorosis but no concurrent comparison groups |
| Wongdem 2001 | Focus on measurement of fluoride concentration |
| Wragg 1999 | Inappropriate design for studying cessation of water fluoridation |
| Wu 2006 | Evaluated fluorosis with regard to improvement in water supply |
| Wu 2008 | Evaluated fluorosis with regard to improvement in water supply |
| Zhu 2009 | Evaluated fluorosis with regard to improvement in water supply |
| Zietsman 2003 | Thesis – unable to access |
| Zimmermann 2002 | Evaluated caries in a single time point cross‐sectional study |
Characteristics of studies awaiting assessment [ordered by study ID]
Wang 2014.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | We are in the process of attempting to access this study report |
Characteristics of ongoing studies [ordered by study ID]
Pretty (ongoing).
| Trial name or title | An evaluation of a water fluoridation scheme in Cumbria |
| Methods | Cohort The study design aims to assess the topical effects of water fluoridation by recruiting groups of children and following them over 6 years |
| Participants | All children in their first school year in 2013 |
| Interventions | Re‐introduction of fluoridated water compared with non‐fluoridated area |
| Outcomes | Caries Age at assessment: 5, 7 and 11 years |
| Starting date | 2013 |
| Contact information | michaela.goodwin@manchester.ac.uk |
| Notes |
Differences between protocol and review
Types of studies: additional clarification on difference between initiation and cessation studies added; the fact that randomised controlled trials are unfeasible is highlighted.
Types of outcome measures: added sentence regarding disparities in dental caries across different groups of people. Changed 'fluorosis' to 'dental fluorosis'. Defined what is meant by adverse effects. Highlighted the fact that this review did not aim to provide a comprehensive systematic review of adverse effects other than dental fluorosis.
Search methods for identification of studies: additional sources added,
Assessment of risk of bias in included studies: 'sampling' was assessed while 'sequence generation' and 'allocation concealment' were not assessed.
Measures of treatment effect: dmft and DMFT analyses calculated the difference in mean change scores between fluoridated and control groups. For the proportion caries free we calculated the difference in the proportion caries free between the fluoridated and control groups. For dental fluorosis data we calculated the log odds and presented as probabilities for interpretation.
Protocol stated that adjusted and unadjusted results were to be presented for non‐randomised studies and the unadjusted value used for analysis. Adjusted values were not available,
Unit of analysis section deleted.
Addition to Dealing with missing data: where standard deviations were missing for DMFT and dmft data we used the equation:
log(SD) = 0.17 + 0.56 x log(mean) to estimate the standard deviations for both the before and after mean caries values. This equation was estimated from available data where the standard deviations were given (R² = 0.91). We undertook no other imputations. We undertook sensitivity analyses to determine the effect of the imputed standard deviations.
Data synthesis: the following text has been deleted (to reflect changes in effect estimate): "Risk ratios will be combined for dichotomous data and mean differences combined for continuous data. Meta‐analytic fixed‐effect and random‐effects models (with or without moderators) will be obtained via the linear (mixed‐effects) model. In the case of random‐effects, the DerSimonian‐Laird estimator for the amount of (residual) heterogeneity will be utilised. Appropriate adjustments to the test statistics and confidence intervals due to the uncertainty in the estimate of the (residual) heterogeneity will be undertaken by application of the method by Knapp and Hartung (Knapp 2003).Tables indicating the general effect of fluoridation found in each study will be created for each outcome, and where possible, the point estimate and a measure of statistical significance (using the 95% confidence interval or P value) of the finding will also be included."
Analysed dmft data only for children 8 years and younger.
Approach to dental fluorosis data amended (although cut‐offs regarding definition of dental fluorosis of aesthetic concern and decision to use data on 5 ppm or lower as primary analysis remain).
Subgroup analysis and investigation of heterogeneity: we deleted the following text: "The heterogeneity among fluorosis studies will be explored by including variables that may account for the observed heterogeneity in the regression model. Since fluoride concentrations of control (non‐fluoridated) groups across studies has been highlighted as a potential source of heterogeneity, a subgroup analysis of studies where the control group has fluoride concentration of 0.2 ppm or less will be undertaken".
Contributions of authors
All authors contributed equally to the writing of the protocol in the published format. Authors contributed at different stages of the review process:
Co‐ordinating the review (ZIE, AMG)
Data collection for the review (RA, ZIE, AMG, LO'M, TW, HW)
Data management for the review (ZIE, AMG, LO'M, TW, HW)
Analysis of data (AMG, HW, TW)
Interpretation of data (JC, ZIE, AMG, LO'M, TW, HW)
Writing the review (JC, ZIE, AMG, TW, HW)
Providing general advice on the review (PT, VW)
Performing previous work that was the foundation of the current review (RA, ZIE, AMG, RM, LO'M, PT, TW, HW, VW)
Sources of support
Internal sources
The University of Manchester, UK.
-
MAHSC, UK.
The Cochrane Oral Health Group is supported by the Manchester Academic Health Sciences Centre (MAHSC) and the NIHR Manchester Biomedical Research Centre.
External sources
-
National Institute for Health Research (NIHR), UK.
CRG funding acknowledgement: The NIHR is the largest single funder of the Cochrane Oral Health Group.
Disclaimer: The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR, NHS or the Department of Health.
-
Cochrane Oral Health Group Global Alliance, UK.
All reviews in the Cochrane Oral Health Group are supported by Global Alliance member organisations (British Association of Oral Surgeons, UK; British Orthodontic Society, UK; British Society of Paediatric Dentistry, UK; British Society of Periodontology, UK; Canadian Dental Hygienists Association, Canada; National Center for Dental Hygiene Research & Practice, USA; Mayo Clinic, USA; New York University College of Dentistry, USA; and Royal College of Surgeons of Edinburgh, UK) providing funding for the editorial process (http://ohg.cochrane.org/).
Declarations of interest
Authors on this review have also been involved in the evaluation of the evidence using different methodology for the CDC Task Force Recommendation on Water Fluoridation
Edited (no change to conclusions)
References
References to studies included in this review
Acharya 2005 {published data only}
- Acharya S. Dental caries, its surface susceptibility and dental fluorosis in South India. International Dental Journal 2005;55(6):359‐64. [DOI] [PubMed] [Google Scholar]
Adair 1999 {published data only}
- Adair S, Hanes C, Russell C, Whitford G. Dental caries and fluorosis among children in a rural Georgia area. Pediatric Dentistry 1999;21(2):81‐5. [PubMed] [Google Scholar]
Adriasola 1959 {published data only}
- Adriasola G. First evaluation of the program of fluoridation of drinking water in Curico‐San Fernando, Chile, 1956. Boletin de la Oficina Sanitaria Panamericana 1959;47:412‐20. [PubMed] [Google Scholar]
- Alvarez‐Ubilla A. [Primera evaluación del programa de fluoacion del agua potable Curico‐San Fernando]. Odontologica Chilena 1959;41:1277‐83. [Google Scholar]
Al‐Alousi 1975 {published data only}
- Al‐Alousi W, Jackson D, Crompton G, Jenkins O. Enamel mottling in a fluoridated and a nonfluoridated community. British Dental Journal 1975;138:9‐15. [DOI] [PubMed] [Google Scholar]
Alarcon‐Herrera 2001 {published data only}
- Alarcon‐Herrera M, Martin‐Dominguez I, Trejo‐Vazquez R, Rodriguez‐Dozal S. Well water fluoride, dental fluorosis, and bone fractures in the Guadiana Valley of Mexico. Fluoride 2001;34(2):139‐49. [Google Scholar]
Albrecht 2004 {published data only}
- Albrecht M, Maros E. [Dental fluorosis in children in Bár and Dunaszekcsó in the 6‐18 age group]. Orvosi Hetilap 2004;145(5):229‐32. [PubMed] [Google Scholar]
AlDosari 2010 {published data only}
- AlDosari A, Akpata E, Khan N. Associations among dental caries experience, fluorosis, and fluoride exposure from drinking water sources in Saudi Arabia. Journal of Public Health Dentistry 2010;70(3):220‐6. [DOI] [PubMed] [Google Scholar]
Angelillo 1999 {published data only}
- Angelillo I, Torre I, Nobile C, Villari P. Caries and fluorosis prevalence in communities with different concentrations of fluoride in the water. Caries Research 1999;33(2):114‐22. [DOI] [PubMed] [Google Scholar]
Arif 2013 {published data only}
- Arif M, Hussain J, Kumar S. Assessment of fluoride level in groundwater and prevalence of dental fluorosis in Didwana block of Nagaur district, central Rajasthan, India. International Journal of Occupational and Environmental Medicine 2013;4(4):178‐84. [PubMed] [Google Scholar]
Arnold 1956 {published data only}
- Arnold F, Dean H, Jay P, Knutson J. Effect of fluoridated public water supply on dental caries prevalence. Public Health Reports 1956;71:652‐8. [PMC free article] [PubMed] [Google Scholar]
Ast 1951 {published data only}
- Ast DB, Finn SB, Chase HC. Newburgh‐Kingston caries fluorine study. III. Further analysis of dental findings including the permanent and deciduous dentitions after four years of water fluoridation. Journal of the American Dental Association (1939) 1951;42:188‐95. [DOI] [PubMed] [Google Scholar]
Awadia 2000 {published data only}
- Awadia A, Birkeland J, Haugejorden O, Bjorvatn K. An attempt to explain why Tanzanian children drinking water containing 0.2 or 3.6 mg fluoride per liter exhibit a similar level of dental fluorosis. Clinical Oral Investigations 2000;4(4):238‐44. [DOI] [PubMed] [Google Scholar]
- Awadia A, Birkeland J, Haugejorden O, Bjorvatn K. Caries experience and caries predictors‐‐a study of Tanzanian children consuming drinking water with different fluoride concentrations. Clinical Oral Investigations 2002;6(2):98‐103. [DOI] [PubMed] [Google Scholar]
Azcurra 1995 {published data only}
- Azcurra A, Battellino L, Calamari S, Cattoni S, Kremer M, Lamberghini F. [Dental health status of students living in places supplied with drinking water of very high and very low levels of fluorides]. Revista de Saude Publica 1995;29(5):367‐75. [DOI] [PubMed] [Google Scholar]
Backer‐Dirks 1961 {published data only}
- Backer‐Dirks O, Houwink B, Kwant G. The results of 6½ years of artificial fluoridation of drinking water in the Netherlands. The Tiel‐Culemborg experiment. Archives of Oral Biology 1961;5:284‐300. [DOI] [PubMed] [Google Scholar]
Bao 2007 {published data only}
- Bao LL, Li YY, Zhang YY. [Dental caries and fluorosis among 12‐year‐old children with different fluoride exposure in Heilongjiang province]. Shanghai kou qiang yi xue = Shanghai Journal of Stomatology 2007;16(6):574‐7. [PubMed] [Google Scholar]
Baskaradoss 2008 {published data only}
- Baskaradoss JK, Clement RB, Narayanan A. Prevalence of dental fluorosis and associated risk factors in 11‐15 year old school children of Kanyakumari District, Tamilnadu, India: a cross sectional survey. Indian Journal of Dental Research 2008;19(4):297‐303. [DOI] [PubMed] [Google Scholar]
Beal 1971 {published data only}
- Beal J, James P. Dental caries prevalence in 5 year old children following five and a half years of water fluoridation in Birmingham. British Dental Journal 1971;130(7):284‐8. [DOI] [PubMed] [Google Scholar]
Beal 1981 {published data only}
- Beal J, Clayton M. Fluoridation a clinical survey in Corby and Scunthorpe England UK. Public Health 1981;95(3):152‐60. [DOI] [PubMed] [Google Scholar]
Beltran‐Aguilar 2002 {published data only}
- Beltran‐Aguilar E, Griffin S, Lockwood S. Prevalence and trends in enamel fluorosis in the United States from the 1930s to the 1980s. Journal of the American Dental Association 2002;133(2):157‐65. [DOI] [PubMed] [Google Scholar]
Berndt 2010 {published data only}
- Berndt Ch, Meller Ch, Poppe D, Splieth ChH. Fluorosis, caries and oral hygiene in schoolchildren on the Ombili Foundation in Namibia. Oral Health & Preventive Dentistry 2010;8:269‐75. [PubMed] [Google Scholar]
Birkeland 2005 {published data only}
- Birkeland J, Ibrahim Y, Ghandour I, Haugejorden O. Severity of dental caries among 12‐year‐old Sudanese children with different fluoride exposure. Clinical Oral Investigations 2005;9(1):46‐51. [DOI] [PubMed] [Google Scholar]
Blinkhorn (unpublished) {unpublished data only}
- Blinkhorn A, Byun R, Metha P, Kay M. A four year assessment of a new water fluoridation scheme in New South Wales, Australia. (Unpublished). [DOI] [PMC free article] [PubMed]
Booth 1991 {published data only}
- Booth I, Mitropoulos C, Worthington H. A comparison between the dental health of 3‐year old children living in fluoridated Huddersfield and non‐fluoridated Dewsbury in 1989. Community Dental Health 1991;9:151‐7. [PubMed] [Google Scholar]
Brothwell 1999 {published data only}
- Brothwell DJ, Limeback H. Fluorosis risk in grade 2 students residing in a rural area with widely varying natural fluoride. Community Dentistry and Oral Epidemiology 1999;27(2):130‐6. [DOI] [PubMed] [Google Scholar]
Brown 1965 {published data only}
- Brown H, McLaren H, Poplove M. The Brantford‐Sarnia‐Stratford Fluoridation Caries Study ‐ 1959 Report. Journal of the Canadian Dental Association 1960;26(3):131‐42. [PubMed] [Google Scholar]
- Brown H, Poplove M. The Brantford‐Sarnia‐Stratford Fluoridation Caries Study: Final Survey 1963. Canadian Journal of Public Health. Revue Canadienne de Sante Publique 1965;56(8):319‐24. [PubMed] [Google Scholar]
Budipramana 2002 {published data only}
- Budipramana ES, Hapsoro A, Irmawati ES, Kuntari S. Dental fluorosis and caries prevalence in the fluorosis endemic area of Asembagus, Indonesia. International Journal of Paediatric Dentistry 2002;12(6):415‐22. [DOI] [PubMed] [Google Scholar]
Butler 1985 {published data only}
- Butler WJ, Segreto V, Collins E. Prevalence of dental mottling in school‐aged lifetime residents of 16 Texas communities. American Journal of Public Health 1985;75(12):1408‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chandrashekar 2004 {published data only}
- Chandrashekar J, Anuradha K. Prevalence of dental fluorosis in rural areas of Davangere, India. International Dental Journal 2004;54(5):235‐9. [DOI] [PubMed] [Google Scholar]
Chen 1989 {published data only}
- Chen B. An epidemiological study on dental fluorosis and dental caries prevalence in communities with negligible, optimal and above‐optimal fluoride concentrations in drinking water supplies. Chinese Journal of Dental Research 1989;8:117‐27. [PubMed] [Google Scholar]
Chen 1993 {published data only}
- Chen W, Xu R, Chen G, Zao J, Chen J. Institution: Health and Epidemic Prevention Station of Guangdong Province. Changes in the prevalence of endemic fluorosis after changing water sources in two villages in Guangdong, China. Bulletin of Environmental Contamination and Toxicology 1993;51(4):479‐82. [DOI] [PubMed] [Google Scholar]
Clark 1993 {published data only}
- Clark D, Hann H, Williamson M, Berkowitz J. Aesthetic concerns of children and parents in relation to different classifications of the tooth surface iIndex of fluorosis. Community Dentistry and Oral Epidemiology 1993;21(6):360‐4. [DOI] [PubMed] [Google Scholar]
Clarkson 1989 {published data only}
- Clarkson J, O'Mullane D. A modified DDE index for use in epidemiological studies of enamel defects. Journal of Dental Research 1989;68(3):445‐50. [DOI] [PubMed] [Google Scholar]
Clarkson 1992 {published data only}
- Clarkson J, O'Mullane D. Prevalence of enamel defects‐fluorosis in fluoridated and non‐fluoridated areas in Ireland. Community Dentistry and Oral Epidemiology 1992;20(4):196‐9. [DOI] [PubMed] [Google Scholar]
Cochran 2004a {published data only}
- Cochran J, Ketley C, Arnadóttir I, Fernandes B, Koletsi‐Kounari H, Oila A‐M, et al. A comparison of the prevalence of fluorosis in 8‐year‐old children from seven European study sites using a standardized methodology. Community Dentistry and Oral Epidemiology 2004;32 Suppl 1:28‐33. [DOI] [PubMed] [Google Scholar]
Colquhoun 1984 {published data only}
- Colquhoun J. Disfiguring dental fluorosis in Aukland, New Zealand. Fluoride 1984;17:234‐42. [Google Scholar]
Correia Sampaio 1999 {published data only}
- Correia Sampaio F, Ramm von der Fehr F, Arneberg P, Petrucci Gigante D, Hatloy A. Dental fluorosis and nutritional status of 6‐ to 11‐year‐old children living in rural areas of Paraiba, Brazil. Caries Research 1999;33(1):66‐73. [DOI] [PubMed] [Google Scholar]
Cutress 1985 {published data only}
- Cutress T, Suckling G, Pearce E. Defects in tooth enamel in children in fluoridated and non‐fluoridated water areas of the Auckland Region. New Zealand Dental Journal 1985;81:12‐9. [PubMed] [Google Scholar]
Cypriano 2003 {published data only}
- Cypriano S, Pecharki GD, Sousa Mda L, Wada RS. [Oral health of schoolchildren residing in areas with or without water fluoridation in Sorocaba, Sao Paulo State, Brazil] [Portuguese]. Cadernos de Saude Publica 2003;19(4):1063‐71. [DOI] [PubMed] [Google Scholar]
de Crousaz 1982 {published data only}
- Crousaz P. Observations on enamel opacities in Switzerland in relation to water or salt fluoridation. SSO Schweiz Monatsschr Zahnheilkd 1982;92(4):332‐44. [PubMed] [Google Scholar]
DHSS England 1969 {published data only}
- Department of Health and Social Security, Scottish Office, Welsh Office. The fluoridation studies in the United Kingdom and results achieved after 11 years. A report of the Committee on Research into Fluoridation. London: Her Majesty's Stationary Office. Reports on Public Health Medical Subjects 1969; Vol. No. 122.
- Ministry of Health, Scottish Office and Ministry of Housing and Local Government. The Conduct of the Fluoridation Studies and the Results Achieved after Five Years. Reports on Public Health and Medical Subjects 1962; Vol. 105, issue London, HMSO.
DHSS Scotland 1969 {published data only}
- Department of Health and Social Security, Scottish Office, Welsh Office. The fluoridation studies in the United Kingdom and results achieved after 11 years. A report of the Committee on Research into Fluoridation. London: Her Majesty's Stationary Office. Reports on Public Health Medical Subjects 1969; Vol. No. 122.
- Ministry of Health, Scottish Office and Ministry of Housing and Local Government. The Conduct of the Fluoridation Studies and the Results Achieved after Five Years. Reports on Public Health and Medical Subjects 1962; Vol. 105, issue London, HMSO.
DHSS Wales 1969 {published data only}
- Department of Health and Social Security, Scottish Office, Welsh Office. The fluoridation studies in the United Kingdom and results achieved after 11 years. A report of the Committee on Research into Fluoridation. London: Her Majesty's Stationary Office. Reports on Public Health Medical Subjects 1969; Vol. No. 122.
- Ministry of Health, Scottish Office and Ministry of Housing and Local Government. The Conduct of the Fluoridation Studies and the Results Achieved after Five Years. Reports on Public Health and Medical Subjects 1962; Vol. 105, issue London, HMSO.
Downer 1994 {published data only}
- Blinkhorn A, Attwood D, Gavin G, O'Hickey S. Joint epidemiological survey on dental health of 12‐year‐old school children in Dublin and Glasgow. Community Dentistry and Oral Epidemiology 1992 Oct;20(5):307‐8. [DOI] [PubMed] [Google Scholar]
- Downer M, Blinkhorn A, Holt R, Wight C, Attwood D. Dental caries experience and defects of dental enamel among 12‐year‐old children in north London, Edinburgh, Glasgow and Dublin. Community Dentistry and Oral Epidemiology 1994;22(Pt1):283‐5. [DOI] [PubMed] [Google Scholar]
Driscoll 1983 {published data only}
- Driscoll W, Horowitz H, Meyers R, Heifetz S, Kingman A, Zimmerman E. Prevalence of dental caries and dental fluorosis in areas with optimal and above‐optimal water fluoride concentrations. Journal of the American Dental Association (1939) 1983;107(1):42‐7. [DOI] [PubMed] [Google Scholar]
Ekanayake 2002 {published data only}
- Ekanayake L, Hoek W. Dental caries and developmental defects of enamel in relation to fluoride levels in drinking water in an arid area of Sri Lanka. Caries Research 2002;36(6):398‐404. [DOI] [PubMed] [Google Scholar]
Eklund 1987 {published data only}
- Eklund S, Ismail A, Burt B, Calderon J. High‐fluoridated drinking water, fluorosis and dental caries in adults [Journal of the American Dental Association (1939)]. 1987 114;March(324‐8). [DOI] [PubMed] [Google Scholar]
Ellwood 1995 {published data only}
- Ellwood R, O'Mullane D. Dental enamel opacities in three groups with varying levels of fluoride in their drinking water. Caries Research 1995;29(2):137‐42. [DOI] [PubMed] [Google Scholar]
Ellwood 1996 {published data only}
- Ellwood R, O'mullane D. The association between developmental enamel defects and caries in populations with and without fluoride in their drinking water. Journal of Public Health Dentistry 1996;56(2):76‐80. [DOI] [PubMed] [Google Scholar]
Ermis 2003 {published data only}
- Ermis R, Koray F, Akdeniz B. Dental caries and fluorosis in low‐ and high‐fluoride areas in Turkey. Quintessence International 2003;34(5):354‐60. [PubMed] [Google Scholar]
Firempong 2013 {published data only}
- Firempong C, Nsiah K, Awunyo‐Vitor D, Dongsogo J. Soluble fluoride levels in drinking water ‐ a major risk factor of dental fluorosis among children in Bongo community of Ghana. Ghana Medical Journal 2013;47(1):16‐23. [PMC free article] [PubMed] [Google Scholar]
Forrest 1956 {published data only}
- Forrest J. Caries incidence and enamel defects in areas with different levels of fluoride in drinking water. British Dental Journal 1956;100:195‐200. [Google Scholar]
Forrest 1965 {published data only}
- Forrest J, James P. A blind study of enamel opacities and dental caries prevalence after eight years of fluoridation of water. British Dental Journal 1965;119(7):319‐22. [PubMed] [Google Scholar]
Franzolin 2008 {published data only}
- Franzolin Sde O, Goncalves A, Padovani C, Francischone L, Marta S. Epidemiology of fluorosis and dental caries according to different types of water supplies. Ciencia & Saude Coletiva 2008;15(Suppl 1):1841‐7. [DOI] [PubMed] [Google Scholar]
Garcia‐Perez 2013 {published data only}
- Garcia‐Perez A, Borges‐Yanez A. Fluorosis and dental caries in Mexican schoolchildren residing in areas with different water fluoride concentrations and receiving fluoridated salt. Caries Research 2013;47(4):299‐308. [DOI] [PubMed] [Google Scholar]
Gaspar 1995 {published data only}
- Gaspar M, Pereira A, Moreira B. Non‐fluorosis and dental fluorosis opacities in areas with lower (0.2 ppm F) and optimum (0.7 ppm F) fluoride concentration in drinking water [Opacidades de esmalte de origem não fluorótica e fluorose dentária em áreas com baixa (0,2 ppm F) e ótima (0,7 ppm F) concentrações de flúor nas águas de abastecimento público]. Revista Brasileira de Odontologia 1995;52(2):13‐8. [Google Scholar]
Goward 1982 {published data only}
- Goward P. Mottling on deciduous incisor teeth. A study of 5‐year‐old Yorkshire children from districts with and without fluoridation. British Dental Journal 1982;153(10):367‐9. [DOI] [PubMed] [Google Scholar]
Gray 2001 {published data only}
- Gray M, Davies‐Slowik J. Changes in the percentage of 5‐year‐old children with no experience of decay in Dudley towns since the implementation of fluoridation schemes in 1987. British Dental Journal 2001;190(1):30‐2. [DOI] [PubMed] [Google Scholar]
- Gray M, Langford K. Notes on the results of the studies of 5 year old children conducted in the West Midlands since 1985. Unpublished report 2000. [Google Scholar]
Grimaldo 1995 {published data only}
- Grimaldo M, Borja Aburto VH, Ramirez AL, Ponce M, Rosas M, Diaz Barriga F. Endemic fluorosis in San Luis Potosi, Mexico. I. Identification of risk factors associated with human exposure to fluoride. Environmental Research 1965;68(1):25‐30. [DOI] [PubMed] [Google Scholar]
Grobler 1986 {published data only}
- Grobler S, Vanwyk C, Kotze D. Relationship between enamel fluoride levels, degree of fluorosis and caries experience in communities with a nearly optimal and a high fluoride level in the drinking water. Caries Research 1986;20(3):284‐8. [DOI] [PubMed] [Google Scholar]
Grobler 2001 {published data only}
- Grobler S, Louw A, Kotze T. Dental fluorosis and caries experience in relation to three different drinking water fluoride levels in South Africa. International Journal of Paediatric Dentistry 2001;11(5):372‐9. [DOI] [PubMed] [Google Scholar]
Guo 1984 {published data only}
- Guo M, Hsieh C, Hong Y, Chen R. Effect of water fluoridation on prevalence of dental caries in Chung‐Hsing New Village Taiwan after 9 years. Journal of the Formosan Medical Association 1984;83(10):1035‐43. [PubMed] [Google Scholar]
Haavikko 1974 {published data only}
- Haavikko K, Helle A. The prevalence and distribution of enamel defects in with different fluoride contents in the drinking water. Proceedings of the Finnish Dental Society 1974;70(5):178‐85. [PubMed] [Google Scholar]
Harding 2005 {published data only}
- Harding M, Whelton H, O'Mullane D, Cronin M, Warren J. Primary tooth fluorosis in 5‐year‐old school children in Ireland. European Journal of Paediatric Dentistry 2005;6(3):155‐61. [PubMed] [Google Scholar]
Hardwick 1982 {published data only}
- Hardwick J, Teasdale J, Bloodworth G. Caries increments over 4 years in children aged 12 at the start of water fluoridation. British Dental Journal 1982;153(6):217‐22. [DOI] [PubMed] [Google Scholar]
Heifetz 1988 {published data only}
- Heifetz S, Driscoll W, Horowitz H, Kingman A. Prevalence of dental caries and dental fluorosis in areas with optimal and above‐optimal water‐fluoride concentrations: a 5‐year follow‐up survey. Journal of the American Dental Association (1939) 1988;116(4):490‐5. [DOI] [PubMed] [Google Scholar]
Heintze 1998 {published data only}
- Heintze s, Bastos J, Bastos R. Urinary fluoride levels and prevalence of dental fluorosis in three Brazilian cities with different fluoride concentrations in the drinking water. Community Dentistry and Oral Epidemiology 1998;26:316‐23. [DOI] [PubMed] [Google Scholar]
Heller 1997 {published data only}
- Heller K, Eklund S, Burt B. Dental caries and dental fluorosis at varying water fluoride concentrations. Journal of Public Health Dentistry 1997;57(3):136‐43. [DOI] [PubMed] [Google Scholar]
Hernandez‐Montoya 2003 {published data only}
- Hernandez‐Montoya V, Bueno‐Lopez JI, Sanchez‐Ruelas AM, Garcia‐Servin J, Trejo‐Vazquez R, Bonilla‐Petriciolet A, et al. [Fluorosis and dental decay in children aged 9 to 11 years in the State of Aguascalientes, Mexico]. Revista Internacional de Contaminacion Ambiental 2003;19(4):197‐204. [Google Scholar]
Holdcroft 1999 {published data only}
- Holdcroft C. Five year old dental health in England, 1993‐94. Unpublished report 1999.
Hong 1990 {published data only}
- Hong C, Hong Y, Guo M, Hsieh C, Chen R. Prevalence of mottled enamel after 12 years of water fluoridation in Chung‐Hsing New Village (Taiwan). Journal of the Formosan Medical Association 1990;89(3):225‐30. [PubMed] [Google Scholar]
Ibrahim 1995 {published data only}
- Ibrahim Y, Affan A, Bjorvatn K. Prevalence of dental fluorosis in Sudanese children from two villages with 0.25 and 2.56 ppm fluoride in the drinking water. International Journal of Paediatric Dentistry 1995;5(4):223‐9. [DOI] [PubMed] [Google Scholar]
Indermitte 2007 {published data only}
- Indermitte E, Saava A, Russak S, Kull A. The contribution of drinking water fluoride to the risk of dental fluorosis in Estonia. Environmental Health Risk IV. Vol. 11, 2007:161‐70. [DOI: 10.2495/EHR070171] [DOI] [Google Scholar]
Indermitte 2009 {published data only}
- Indermitte EE, Saava AA, Karro EE. Exposure to high fluoride drinking water and risk of dental fluorosis in Estonia. International Journal of Environmental Research and Public Health 2009;6(2):710‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ismail 1990 {published data only}
- Ismail A, Brodeur J‐M, Kavanagh M, Boisclair G, Tessier C, Picotte L. Prevalence of dental caries and dental fluorosis in students, 11‐17 years of age, in fluoridated and non‐fluoridated cities in Quebec (Canada). Caries Research 1990;24(2):290‐7. [DOI] [PubMed] [Google Scholar]
Jackson 1975 {published data only}
- Jackson D, James PM, Wolfe WB. Fluoridation in Anglesey. A clinical study. British Dental Journal 1975;138(5):165‐71. [DOI] [PubMed] [Google Scholar]
Jackson 1999 {published data only}
- Jackson R. Dental fluorosis in children residing in communities with different water fluoride levels: 33‐month follow‐up. Pediatric Dentistry 1999;21(4):248‐54. [PubMed] [Google Scholar]
Jolly 1971 {published data only}
- Jolly S, Prasad S, Sharma R, Rai B. [Human fluoride intoxication in Punjab]. Flouride 1971;4(2):64‐79. [Google Scholar]
Kanagaratnam 2009 {published data only}
- Kanagaratnam S, Schluter P, Durward C, Mahood R, Mackay T. Enamel defects and dental caries in 9‐year‐old children living in fluoridated and nonfluoridated areas of Auckland, New Zealand. Community Dentistry & Oral Epidemiology 2009;37(3):250‐9. [DOI] [PubMed] [Google Scholar]
Kotecha 2012 {published data only}
- Kotecha P, Patel S, Bhalani K, Shah D, Shah V, Mehta K. Prevalence of dental fluorosis & dental caries in association with high levels of drinking water fluoride content in a district of Gujarat, India. The Indian Journal of Medical Research 2012;135(6):873‐7. [PMC free article] [PubMed] [Google Scholar]
Kumar 1999 {published data only}
- Kumar J, Swango P. Fluoride exposure and dental fluorosis in Newburgh and Kingston, New York: policy implications. Community Dentistry and Oral Epidemiology 1999;27(3):171‐80. [DOI] [PubMed] [Google Scholar]
Kumar 2007 {published data only}
- Kumar R, Khandare A, Brahmam G, Venkiah K, Reddy C, Sivakumar B. Assessment of current status of fluorosis in north‐western districts of Tamil Nadu using community index for dental fluorosis. Journal of Human Ecology 2007;21(1):27‐32. [Google Scholar]
Kunzel 1976 {published data only}
- Kunzel W, Padron F. Caries and dental fluorosis in Cuban children. Caries Research 1976;10(2):104‐12. [DOI] [PubMed] [Google Scholar]
Kunzel 1997 {published data only}
- Kunzel W, Fischer T. Rise and fall of caries prevalence in German towns with different F concentrations in drinking water. Caries Research 1997;31(3):166‐73. [DOI] [PubMed] [Google Scholar]
Leverett 1986 {published data only}
- Leverett D. Prevalence of dental fluorosis in fluoridated and nonfluoridated communities‐‐a preliminary investigation. Journal of Public Health Dentistry 1986;46(4):184‐7. [DOI] [PubMed] [Google Scholar]
Levine 1989 {published data only}
- Levine R, Beal J, Flemming C. A photographically recorded assessment of enamel hypoplasia in fluoridated and non fluoridated areas. British Dental Journal 1989;166:249‐52. [DOI] [PubMed] [Google Scholar]
Lin 1991 {published data only}
- Lin F‐F, Zhao H‐X, Lin J, Jian J‐Y. The relationship of a low‐iodine an high‐fluoride environment to subclinical cretinism in Xinjiang. 1991 Xinjiang Institute for Endemic Disease Control and Research,Office of Leading Group for Endemic Disease Control of Hetian Prefectural Committee of theCommunist Party of China and County Health and Endemic Prevention Station, Yutian, Xinjiang. Unpublished report submitted through NHS CRD web site 1991.
Loh 1996 {published data only}
- Loh T. Thirty‐eight years of water fluoridation – the Singapore scenario. Community Dental Health 1996;13(2):47‐50. [PubMed] [Google Scholar]
Louw 2002 {published data only}
- Louw AJ, Grobler SR, van WKTJ. Degree of fluorosis in areas of South Africa with differing levels of fluoride in drinking water. General Dentistry 2002;50(4):352‐6. [PubMed] [Google Scholar]
Machiulskiene 2009 {published data only}
- Machiulskiene V, Baelum V, Fejerskov O, Nyvad B. Prevalence and extent of dental caries, dental fluorosis, and developmental enamel defects in Lithuanian teenage populations with different fluoride exposures. European Journal of Oral Sciences 2009;117(2):154‐60. [DOI] [PubMed] [Google Scholar]
Mackay 2005 {published data only}
- Mackay T, Thomson W. Enamel defects and dental caries among Southland children. New Zealand Dental Journal 2005;101(2):35‐43. [PubMed] [Google Scholar]
Macpherson 2007 {published data only}
- Macpherson L, Conway D, Gilmour W, Petersson L, Stephen K. Photographic assessment of fluorosis in children from naturally fluoridated Kungsbacka and non‐fluoridated Halmstad, Sweden. Acta Odontologica Scandinavica 2007;65(3):149‐55. [DOI] [PubMed] [Google Scholar]
Mandinic 2009 {published data only}
- Mandinic Z, Curcic M, Antonijevic B, Lekic C, Carevic M. Relationship between fluoride intake in Serbian children living in two areas with different natural levels of fluorides and occurrence of dental fluorosis. Food and chemical toxicology: an international journal published for the British Industrial Biological Research Association 2009;47(6):1080‐4. [DOI] [PubMed] [Google Scholar]
Mandinic 2010 {published data only}
- Mandinic Z, Curcic M, Antonijevic B, Carevic M, Mandic J, Djukic‐Cosic D, et al. Fluoride in drinking water and dental fluorosis. Science of the Total Environment 2010;408(17):3507‐12. [DOI] [PubMed] [Google Scholar]
Marya 2010 {published data only}
- Marya C, Ashokkumar B, Dhingra S, Dahiya V, Gupta A. Exposure to high‐fluoride drinking water and risk of dental caries and dental fluorosis in Haryana, India. Asia‐Pacific Journal of Public Health/Asia‐Pacific Academic Consortium for Public Health 2014;26(3):295‐303. [DOI] [PubMed] [Google Scholar]
- Marya C, Dahiya V, Gupta A. Prevalence and severity of dental fluorosis in endemic fluoride areas of Haryana, India: an epidemiologic study [Croatian, English]. Acta Stomatologica Croatica 2010;44(3):152‐8. [Google Scholar]
Masztalerz 1990 {published data only}
- Masztalerz A, Masztalerzowa Z, Szymanska M, Tomelka J. Fluoride and dentition. Epidemiologische Untersuchung 1990;51(4):234‐7. [DOI] [PubMed] [Google Scholar]
Maupome 2001 {published data only}
- Maupome G, Clark D, Levy S, Berkowitz J. Patterns of dental caries following the cessation of water fluoridation. Community Dentistry & Oral Epidemiology 2001;29(1):37‐47. [PubMed] [Google Scholar]
Mazzotti 1939 {published data only}
- Mazzotti L, Gonzalez Rivera M. Dental fluorosis in Mexico. Revista del Instituto de Salubridad y Enfermedades Tropicales 1939;1:105‐21. [Google Scholar]
McGrady 2012 {published data only}
- McGrady M, Ellwood R, Srisilapanan P, Korwanich N, Worthington H, Pretty I. Dental fluorosis in populations from Chiang Mai, Thailand with different fluoride exposures ‐ Paper 1: assessing fluorosis risk, predictors of fluorosis and the potential role of food preparation. BMC Oral Health 2012 Jun;21(12):16. [DOI: 10.1186/1472-6831-12-16] [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGrady MG, Ellwood RP, Srisilapanan P, Korwanich N, Taylor A, Goodwin M, et al. Dental fluorosis in populations from Chiang Mai, Thailand with different fluoride exposures ‐ Paper 2: The ability of fluorescence imaging to detect differences in fluorosis prevalence and severity for different fluoride intakes from water. BMC Oral Health 2012;12:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
McInnes 1982 {published data only}
- McInnes P, Richarson B, Cleaton‐Jones P. Comparison of dental fluorosis and caries in primary teeth of preschool‐children living in arid high and low fluoride villages. Community Dentistry and Oral Epidemiology 1982;10:182‐6. [DOI] [PubMed] [Google Scholar]
Mella 1992 {published data only}
- Mella S, Atalah E, Aranda W, Montagna R. Prevalence of dental fluorosis in Chile ‐ a pilot‐study. Revista Medica De Chile 1992;120(8):866‐71. [PubMed] [Google Scholar]
Mella 1994 {published data only}
- Mella S, Molina X, Atalah E. Prevalence of dental fluorosis and its relation with fluoride content of communal drinking‐water [Prevalencia de fluorosis dental end‚mica en relacion alcontenido de fluoruros en las aguas de abasto publico]. Revista Medica De Chile 1994;122(11):1263‐70. [PubMed] [Google Scholar]
Meyer‐Lueckel 2006 {published data only}
- Meyer‐Lueckel H, Paris S, Shirkhani B, Hopfenmuller W, Kielbassa AM. Caries and fluorosis in 6‐ and 9‐year‐old children residing in three communities in Iran. Community Dentistry and Oral Epidemiology 2006;34(1):63‐70. [DOI] [PubMed] [Google Scholar]
Milsom 1990 {published data only}
- Milsom K, Mitropoulos C. Enamel defects in 8 year old children in fluoridated and non‐fluoridated parts of Cheshire. Caries Research 1990;1990(24):286‐9. [DOI] [PubMed] [Google Scholar]
Mondal 2012 {published data only}
- Mondal NK, Pal KC, Kabi S. Prevalence and severity of dental fluorosis in relation to fluoride in ground water in the villages of Birbhum district, West Bengal, India. Environmentalist 2012;32(1):70‐84. [Google Scholar]
Montero 2007 {published data only}
- Montero M, Rojas‐Sanchez F, Socorro M, Torres J, Acevedo AM. Dental caries and fluorosis in children consuming water with different fluoride concentrations in Maiquetia, Vargas State, Venezuela [Spanish]. Investigacion Clinica 2007;48(1):5‐19. [PubMed] [Google Scholar]
Nanda 1974 {published data only}
- Nanda R, Zipkin I, Doyle J, Horowitz H. Factors affecting the prevalence of dental fluorosis in Lucknow, India. Archives of Oral Biology 1974;19:781‐92. [DOI] [PubMed] [Google Scholar]
Narbutaite 2007 {published data only}
- Narbutaite J, Vehkalahti M, Milciuviene S. Dental fluorosis and dental caries among 12‐yr‐old children from high‐ and low‐fluoride areas in Lithuania. European Journal of Oral Sciences 2007;115(2):137‐42. [DOI] [PubMed] [Google Scholar]
Narwaria 2013 {published data only}
- Narwaria Y, Saksena D. Incidence of dental fluorosis in domestic animals of Shivpuri, Madhya Pradesh, India. Journal of Environmental Research and Development July‐September 2012;7(1A):426‐30. [Google Scholar]
- Narwaria Y, Saksena D. Prevalence of dental fluorosis among primary school children in rural areas of Karera Block, Madhya Pradesh. Indian Journal of Pediatrics 2013;80(9):718‐20. [DOI] [PubMed] [Google Scholar]
Nunn 1992 {published data only}
- Nunn J, Murray J, Reynolds P, Tabari D, Breckon J. The prevalence of developmental defects of enamel in 15‐16‐year‐old children residing in three districts (natural fluoride, adjusted fluoride, low fluoride) in the north east of England. Community Dental Health 1992;9(3):235‐47. [PubMed] [Google Scholar]
Nunn 1994a {published data only}
- Nunn J, Rugg‐Gunn A, Ekanayake L, Saparamandu K. Prevalence of developmental defects of enamel with different fluoride and socio‐economic groups. International Dental Journal 1994;44:165‐73. [PubMed] [Google Scholar]
Nunn 1994b {published data only}
- Nunn J, Murray J, Reynolds P, Tabari D, Breckon J. The prevalence of developmental defects of enamel in 15‐16‐year‐old children residing in three districts (natural fluoride, adjusted fluoride, low fluoride) in the north east of England. Community Dental Health 1992;9(3):235‐47. [PubMed] [Google Scholar]
Ockerse 1941 {published data only}
- Ockerse T. Fluorosis in Kenhardt and Gordonia districts Cape Province, South Africa. Journal of the American Dental Association (1939) 1941;28:936‐41. [Google Scholar]
Pontigo‐Loyola 2008 {published data only}
- Pontigo‐Loyola A, Islas‐Marquez A, Loyola‐Rodriguez J, Maupome G, Marquez‐Corona M, Medina‐Solis C. Dental fluorosis in 12‐ and 15‐year‐olds at high altitudes in above‐optimal fluoridated communities in Mexico. Journal of Public Health Dentistry 2008;68(3):163‐6. [DOI] [PubMed] [Google Scholar]
Pot 1974 {published data only}
- Pot T, Purdell‐Lewis D, Groeneveld A. The influence of 17 years of water fluoridation upon the dentition of adults [De invloed van 17 jaren drinkwater‐fluoirdering op het gebit van volwassenen]. Nederlands Tijdschrift voor Tandheelkunde 1974;81(1):5‐12. [Google Scholar]
Ray 1982 {published data only}
- Ray S, Ghosh S, Tiwari I, Nagchaudhuri J, Kaur P, Reddy D. Prevalence of dental fluorosis in relation to fluoride in drinking water in two villages of Varanasi (U.P.). Indian Journal of Public Health 1982;26(3):173‐8. [PubMed] [Google Scholar]
Riordan 1991 {published data only}
- Riordan P, Banks J. Dental fluorosis and fluoride exposure in Western Australia. Journal of Dental Research 1991;70(7):1022‐8. [DOI] [PubMed] [Google Scholar]
Riordan 2002 {published data only}
- Riordan P. Dental fluorosis decline after changes to supplement and toothpaste regimens. Community Dentistry and Oral Epidemiology 2002;30(3):233‐40. [DOI] [PubMed] [Google Scholar]
Ruan 2005 {published data only}
- Ruan J, Yang Z, Wang Z, Astrom A, Bardsen A, Bjorvatn K. Dental fluorosis and dental caries in permanent teeth: rural schoolchildren in high‐fluoride areas in the Shaanxi province, China. Acta Odontologica Scandinavica 2005;63(5):258‐65. [DOI] [PubMed] [Google Scholar]
Rugg‐Gunn 1997 {published data only}
- Rugg‐Gunn A, Al Mohammadi S, Butler T. Effects of fluoride level in drinking water, nutritional status, and socio‐economic status on the prevalence of developmental defects of dental enamel in permanent teeth in Saudi 14‐year‐old boys. Caries Research 1997;31(4):259‐67. [DOI] [PubMed] [Google Scholar]
Russell 1951 {published data only}
- Russell A, Elvove E. Domestic Water and Dental Caries. A study of the fluoride‐dental caries relationship in an adult population. Public Health Reports 1951;66(43):1389‐401. [PubMed] [Google Scholar]
Rwenyonyi 1998 {published data only}
- Rwenyonyi M, Birkeland J, Bjorvatn K, Haugejorden O. Dental fluorosis in Ugandans related to fluoride in drinking water and altitude. Journal of Dental Research 1998;77:1299. [Google Scholar]
Rwenyonyi 1999 {published data only}
- Rwenyoyi C, Bjorvatn K, Birkeland J, Haugejorden O. Altitude as a risk Indicator of dental fluorosis in children residing in areas with 0.5 and 2.5 mg fluoride per litre in drinking water. Caries Research 1999;33:267‐74. [DOI] [PubMed] [Google Scholar]
Saravanan 2008 {published data only}
- Saravanan S, Kalyani C, Vijayarani M, Jayakodi P, Felix A, Nagarajan S, et al. Prevalence of dental fluorosis among primary school children in rural areas of Chidambaram Taluk, Cuddalore district, Tamil Nadu, India. Indian Journal of Community Medicine: official publication of Indian Association of Preventive & Social Medicine 2008;33(3):146‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Scheinin 1964 {published data only}
- Scheinin A, Kalijaervi E, Harjola O, Heikkinen K. Prevalence of dental caries and dental health in relation to variable concentration of fluorides in drinking water; a clinical study on Finnish school‐children. Acta Odontologica Scandinavica 1964;22:229‐54. [DOI] [PubMed] [Google Scholar]
Segreto 1984 {published data only}
- Segreto V, Collins E, Camann D, Smith C. A current study of mottled enamel in Texas. Journal of the American Dental Association (1939) 1984;108(1):56‐9. [DOI] [PubMed] [Google Scholar]
Sellman 1957 {published data only}
- Sellman S, Syrrist A, Gustafson G. Fluorine and dental health in southern Sweden. Odontologisk Tidskrift 1957;65:61‐93. [Google Scholar]
Selwitz 1995 {published data only}
- Selwitz R, Nowjack Raymer R, Kingman A, Driscoll W. Prevalence of dental caries and dental fluorosis in areas with optimal and above‐optimal water fluoride concentrations: a 10‐year follow‐up survey. Journal of Public Health Dentistry 1995;55(2):85‐93. [DOI] [PubMed] [Google Scholar]
Selwitz 1998 {published data only}
- Selwitz R, Nowjack Raymer R, Kingman A, Driscoll W. Dental caries and dental fluorosis among schoolchildren who were lifelong residents of communities having either low or optimal levels of fluoride in drinking water. Journal of Public Health Dentistry 1998;58(1):28‐35. [DOI] [PubMed] [Google Scholar]
Shanthi 2014 {published data only}
- Shanthi M, Reddy B, Venkataramana V, Gowrisankar S, Reddy B, Chennupati S. Relationship between drinking water fluoride levels, dental fluorosis, dental caries and associated risk factors in 9‐12 years old school children of Nelakondapally Mandal of Khammam district, Andhra Pradesh, India: a cross‐sectional survey. Journal of International Oral Health 2014;6(3):106‐10. [PMC free article] [PubMed] [Google Scholar]
Shekar 2012 {published data only}
- Shekar C, Cheluvaiah M, Namile D. Prevalence of dental caries and dental fluorosis among 12 and 15 years old school children in relation to fluoride concentration in drinking water in an endemic fluoride belt of Andhra Pradesh. Indian Journal of Public Health 2012;56(2):122‐8. [DOI] [PubMed] [Google Scholar]
- Sukhabogi J, Parthasarathi P, Anjum S, Shekar B, Padma C, Rani A. Dental fluorosis and dental caries prevalence among 12 and 15‐year‐old school children in Nalgonda district, Andhra Pradesh, India. Anals of Medical and Health Sciences Research Sep‐Oct 2014;4(3):245‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Skinner 2013 {published data only}
- Skinner J, Johnson G, Phelan C, Blinkhorn A. Dental caries in 14‐ and 15‐year‐olds in New South Wales, Australia. BMC Public Health 2013;13:1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
Skotowski 1995 {published data only}
- Skotowski M, Hunt R, Levy S. Risk‐factors for dental fluorosis in pediatric dental patients. Journal of Public Health Dentistry 1995;55(3):154‐9. [DOI] [PubMed] [Google Scholar]
Spadaro 1955 {published data only}
- Spadaro O, Pagano V. Fluorosis and dental caries in the community of Barcellona Pozzo di Gotto. Igiene e Sanita Pubblica 1955;11(7‐8):403‐10. [Google Scholar]
Stephen 2002 {published data only}
- Stephen K, Macpherson L, Gilmour W, Stuart R, Merrett M. A blind caries and fluorosis prevalence study of school‐children in naturally fluoridated and nonfluoridated townships of Morayshire, Scotland. Community Dentistry and Oral Epidemiology 2002;30(1):70‐9. [DOI] [PubMed] [Google Scholar]
Sudhir 2009 {published data only}
- Sudhir K, Prashant G, Subba Reddy V, Mohandas U, Chandu G. Prevalence and severity of dental fluorosis among 13‐ to 15‐year‐old school children of an area known for endemic fluorosis: Nalgonda district of Andhra Pradesh. Journal of the Indian Society of Pedodontics and Preventive Dentistry 2009;27(4):190‐6. [DOI] [PubMed] [Google Scholar]
Szpunar 1988 {published data only}
- Szpunar S, Burt B. Dental caries, fluorosis and fluoride exposure in Michigan schoolchildren. Journal of Dental Research 1988;67(5):802‐6. [DOI] [PubMed] [Google Scholar]
Tabari 2000 {published data only}
- Tabari E, Ellwood R, Rugg‐Gunn A, Evans D, Davies R. Dental fluorosis in permanent incisor teeth in relation to water fluoridation, social deprivation and toothpaste use in infancy. British Dental Journal 2000;189(4):216‐20. [DOI] [PubMed] [Google Scholar]
Tessier 1987 {published data only}
- Tessier C. [Effets de la fluoruration de l'eau a Windsor, Que. depuis 7 ans sur les enfants de 6 a 7 ans]. Journal Dentaire Du Quebec Janvier 1987;XXIV:17‐23. [PubMed] [Google Scholar]
Tsutsui 2000 {published data only}
- Tsutsui A, Yagi M, Horowitz AM. The prevalence of dental caries and fluorosis in Japanese communities with up to 1.4 ppm of naturally occurring fluoride. Journal of Public Health Dentistry 2000;60(3):147‐53. [DOI] [PubMed] [Google Scholar]
Venkateswarlu 1952 {published data only}
- Venkateswarlu P, Narayanu Rao D, Ranganatha Rao K. Endemic fluorosis: Visakhaptnam and suburban areas; fluorine, mottled enamel and dental caries. The Indian journal of Medical Research 1952;40(October):535‐48. [PubMed] [Google Scholar]
Vignarajah 1993 {published data only}
- Vignarajah S. Dental caries experience and enamel opacities in children residing in urban and rural areas of Antigua with different levels of natural fluoride in drinking water. Community Dental Health 1993;10(2):159‐66. [PubMed] [Google Scholar]
Vilasrao 2014 {published data only}
- Vilasrao G, Kamble K, Sabat R. Child fluorosis in Chhattisgarh, India: a community‐based survey. Indian Pediatrics November 15, 2014;51:903‐5. [DOI] [PubMed] [Google Scholar]
Villa 1998 {published data only}
- Villa A, Guerrero S, Villalobos J. Estimation of optimal concentration of fluoride in drinking water under conditions prevailing in Chile. Community Dentistry and Oral Epidemiology 1998;26(4):249‐55. [DOI] [PubMed] [Google Scholar]
Vuhahula 2009 {published data only}
- Vuhahula E, Masalu J, Mabelya L, Wandwi W. Dental fluorosis in Tanzania Great Rift Valley in relation to fluoride levels in water and in 'Magadi' (Trona). Desalination 2009;248(1‐3):610‐5. [Google Scholar]
Wang 1993 {published data only}
- Wang. An investigation on the fluoride level in drinking water sources and the condition of fluorosis in some part of South Xinjiang. Endemic Diseases Bulletin 1993;8(3):57‐60. [Google Scholar]
Wang 1999 {published data only}
- Wang X, Kawahara K, Guo X. Fluoride contamination of groundwater and its impacts on human health in Inner Mongolia area. Journal of Water Services Research and Technology‐Aqua 1999;48(4):146‐53. [Google Scholar]
Wang 2012 {published data only}
- Wang C, Gao Y, Wang W, Zhao L, Zhang W, Han H, et al. A national cross‐sectional study on effects of fluoride‐safe water supply on the prevalence of fluorosis in China. BMJ Open 2012;2(5):e001564. [DOI] [PMC free article] [PubMed] [Google Scholar]
Warnakulasuriya 1992 {published data only}
- Warnakulasuriya K, Balasuriya S, Perera P, Peiris L. Determining optimal levels of fluoride in drinking‐water for hot, dry climates ‐ a case‐study in Sri‐Lanka. Community Dentistry and Oral Epidemiology 1992;20(6):364‐7. [DOI] [PubMed] [Google Scholar]
Warren 2001 {published data only}
- Warren J, Levy S, Kanellis M. Prevalence of dental fluorosis in the primary dentition. Journal of Public Health Dentistry 2001;61(2):87‐91. [DOI] [PubMed] [Google Scholar]
Wenzel 1982 {published data only}
- Wenzel A, Thylstrup A, Melsen B. Skeletal development and dental fluorosis in 12‐ ‐14‐year‐old Danish girls from a fluoride and a non‐fluoride community. Scandinavian Journal of Dental Research 1982;90(2):83‐8. [DOI] [PubMed] [Google Scholar]
Whelton 2004 {published data only}
- Whelton H, Crowley E, O'Mullane D, Donaldson M, Kelleher V, Cronin M. [Dental caries and enamel fluorosis among the fluoridated and non‐fluoridated populations in the Republic of Ireland in 2002]. Community Dental Health 2004;21(1):37‐44. [PubMed] [Google Scholar]
Whelton 2006 {published data only}
- Whelton H, Crowley E, O'Mullane D, Donaldson M, Cronin M, Kelleher V. Dental caries and enamel fluorosis among the fluoridated population in the Republic of Ireland and non fluoridated population in Northern Ireland in 2002. Community Dental Health 2006;23(1):37‐43. [PubMed] [Google Scholar]
Wondwossen 2004 {published data only}
- Wondwossen F, Astrom A, Bjorvatn K, Bardsen A. The relationship between dental caries and dental fluorosis in areas with moderate‐ and high‐fluoride drinking water in Ethiopia. Community Dentistry and Oral Epidemiology 2004;32(5):337‐44. [DOI] [PubMed] [Google Scholar]
Zheng 1986 {published data only}
- Zheng CL. A Survey of Dental Caries in Guangzhou China After 18 Years of Community Water Fluoridation.. Chinese Journal of Preventive Medicine 1986;20(2):79‐82. [PubMed] [Google Scholar]
Zimmermann 1954 {published data only}
- Zimmermann. Fluoride and nonfluoride enamel opacities involving fluorosis. Public Health Reports 1954;69:1115‐20. [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Acharya 2003 {published data only}
- Acharya S, Anuradha KP. Correlation between water fluoride levels and dental caries in Davangere District, India. Indian Journal of Dental Research 2003;14(3):146‐51. [PubMed] [Google Scholar]
Agarwal 2014 {published data only}
- Agrawal M, Agrawal S, Adyanthaya B, Gupta H, Bhargava N, Rastogi R. Prevalence and severity of dental fluorosis among patients visiting a dental college in Jaipur, Rajasthan. Indian Journal of Research in Pharmacy and Biotechnology 2014;2(4):1339‐44. [Google Scholar]
Ajayi 2008 {published data only}
- Ajayi DM, Denloye OO, Dosumu OO. The fluoride content of drinking water and caries experience in 15‐19 year old school children in Ibadan, Nigeria. African Journal of Medicine & Medical Sciences 2008;37(1):15‐9. [PubMed] [Google Scholar]
Akosu 2008 {published data only}
- Akosu TJ, Zoakah AI. Risk factors associated with dental fluorosis in Central Plateau State, Nigeria. Community Dentistry and Oral Epidemiology 2008;36(2):144‐8. [DOI] [PubMed] [Google Scholar]
Aldosari 2004 {published data only}
- Al Dosari A, Wyne A, Akpata E, Khan N. Caries prevalence and its relation to water fluoride levels among schoolchildren in Central Province of Saudi Arabia. International Dental Journal 2004;54(6):424‐8. [DOI] [PubMed] [Google Scholar]
Aleksejuniene 2004 {published data only}
- Aleksejuniene J, Holst D, Balciuniene I. Factors influencing the caries decline in Lithuanian adolescents‐‐trends in the period 1993‐2001. European Journal of Oral Sciences 2004;112(1):3‐7. [DOI] [PubMed] [Google Scholar]
Alimskii 2000 {published data only}
- Alimskii AV, Alieva RK. The indices of caries and dental fluorosis prevalence in schoolchildren born and permanently living in regions of Azerbaijan differing by the level of the drinking water fluorine content [Russian]. Stomatologiia 2000;79(2):40‐2. [PubMed] [Google Scholar]
Antunes 2004 {published data only}
- Antunes JL, Narvai PC, Nugent ZJ. Measuring inequalities in the distribution of dental caries. Community Dentistry and Oral Epidemiology 2004;32(1):41‐8. [DOI] [PubMed] [Google Scholar]
Anuradha 2002 {published data only}
- Anuradha KP, Chadrashekar J, Ramesh N. Prevalence of periodontal disease in endemically flourosed areas of Davangere Taluk, India. Indian Journal of Dental Research 2002;13(1):15‐9. [PubMed] [Google Scholar]
Archila 2003 {published data only}
- Archila L, Bartizek RD, Gerlach RW, Jacobs SA, Biesbrock AR. Dental caries in school‐age children residing in five Guatemalan communities. Journal of Clinical Dentistry 2003;14(3):53‐8. [PubMed] [Google Scholar]
ARCPOH 2008 {published data only}
- Australian Research Centre for Population Oral Health TUoASA. The benefits of water fluoridation across areas of differing socio‐economic status. Australian Dental Journal 2008;53(2):180‐3. [DOI] [PubMed] [Google Scholar]
Armfield 2004 {published data only}
- Armfield JM, Spencer AJ. Consumption of nonpublic water: implications for children's caries experience. Community Dentistry and Oral Epidemiology 2004;32(4):283‐96. [DOI] [PubMed] [Google Scholar]
Armfield 2005 {published data only}
- Armfield JM. Public water fluoridation and dental health in New South Wales. Australian and New Zealand Journal of Public Health 2005;29(5):477‐83. [DOI] [PubMed] [Google Scholar]
Armfield 2007 {published data only}
- Armfield JM, Spencer AJ. Community effectiveness of fissure sealants and the effect of fluoridated water consumption. Community Dental Health 2007;24(1):4‐11. [PubMed] [Google Scholar]
Armfield 2010 {published data only}
- Armfield JM. Community effectiveness of public water fluoridation in reducing children's dental disease. Public Health Reports 2010;125(5):655‐64. [DOI] [PMC free article] [PubMed] [Google Scholar]
Arora 2010 {published data only}
- Arora A, Evans RW. Dental caries in children: a comparison of one non‐fluoridated and two fluoridated communities in NSW. New South Wales Public Health Bulletin 2010;21(11‐12):257‐62. [DOI] [PubMed] [Google Scholar]
Attwood 1988 {published data only}
- Attwood D, Blinkhorn A. Trends in dental health of ten‐year‐old schoolchildren in South‐West Scotland UK after cessation of water fluoridation. Lancet 1988;2 (8605):266‐7. [DOI] [PubMed] [Google Scholar]
- Blinkhorn A, Brown M, Attwood D, Downer M. The effect of fluoridation on the dental health of urban Scottish schoolchildren. Journal of Epidemiology and Community Health 1981;35:98‐101. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bailie 2009 {published data only}
- Bailie RS, Stevens M, Armfield JM, Ehsani JP, Beneforti M, Spencer J. Association of natural fluoride in community water supplies with dental health of children in remote indigenous communities ‐ implications for policy. Australian and New Zealand Journal of Public Health 2009;33(3):205‐11. [DOI] [PubMed] [Google Scholar]
Baldani 2002 {published data only}
- Baldani MH, Narvai PC, Antunes JLF. Dental caries and socioeconomic conditions in the State of Paraná, Brazil,1996. Cadernos de saude publica/Ministerio da Saude, Fundacao Oswaldo Cruz, Escola Nacional de Saude Publica 2002;18(3):755‐63. [DOI] [PubMed] [Google Scholar]
Baldani 2004 {published data only}
- Baldani MH, Vasconcelos AG, Antunes JL. [Association of the DMFT index with socioeconomic and dental services indicators in the state of Paraná, Brazil]. Cadernos de saude publica / Ministerio da Saude, Fundacao Oswaldo Cruz, Escola Nacional de Saude Publica 2004;20(1):143‐52. [DOI] [PubMed] [Google Scholar]
Bihari 2008 {published data only}
- Bihari S, Singh KK, Kumar A, Kumar N. Prevalence of fluorosis in Kachhariadih and Muslimtola villages of Nawadah district Bihar: a case study to mitigate sufferings. Fluoride 2008;41(3):248. [Google Scholar]
Binbin 2005 {published data only}
- Binbin W, Baoshan Z, Hongying W, Yakun P, Yuehua T. Dental caries in fluorine exposure areas in China. Environmental Geochemistry and Health 2005;27(4):285‐8. [DOI] [PubMed] [Google Scholar]
Blagojevic 2004 {published data only}
- Blagojevic D, Stojsin I. Effects of fluoride in drinking water on health of deciduous teeth [Serbian]. Medicinski Pregled 2004;57(7‐8):323‐6. [DOI] [PubMed] [Google Scholar]
Blayney 1960 {published data only}
- Blayney J. A report on thirteen years of water fluoridation in Evanston, III. Journal of the American Dental Association (1939) 1960;61:76‐9. [DOI] [PubMed] [Google Scholar]
Bo 2003 {published data only}
- Bo Z, Mei H, Yongsheng Z, Xueyu L, Xuelin Z, Jun D. Distribution and risk assessment of fluoride in drinking water in the west plain region of Jilin province, China. Environmental Geochemistry and Health 2003;25(4):421‐31. [DOI] [PubMed] [Google Scholar]
Bottenberg 2004 {published data only}
- Bottenberg P, Declerck D, Ghidey W, Bogaerts K, Vanobbergen J, Martens L. Prevalence and determinants of enamel fluorosis in Flemish schoolchildren. Caries Research 2004;38(1):20‐8. [DOI] [PubMed] [Google Scholar]
Bradnock 1984 {published data only}
- Bradnock G, Marchment M, Anderson R. Social background fluoridation and caries experience in 5 year old population. British Dental Journal 1984;156:127‐31. [DOI] [PubMed] [Google Scholar]
Buchel 2011 {published data only}
- Buchel K, Gerwig P, Weber C, Minning P, Wiehl P, Schild S, et al. Prevalence of enamel fluorosis in 12‐year‐olds in two Swiss cantons. Schweiz Monatsschr Zahnmed 2011;121(7‐8):647‐56. [PubMed] [Google Scholar]
Burt 2000 {published data only}
- Burt BA, Keels MA, Heller KE. The effects of a break in water fluoridation on the development of dental caries and fluorosis. Journal of Dental Research 2000;79(2):761‐9. [DOI] [PubMed] [Google Scholar]
Buscariolo 2006 {published data only}
- Buscariolo IA, Penha SS, Rocha RG. Chronic fluorine intoxication. Prevalence of dental fluorosis in schoolchildren. Revista de Ciencias Farmaceuticas Basica e Aplicada 2006;27(1):83‐7. [Google Scholar]
Buzalaf 2004 {published data only}
- Buzalaf MAR, Almeida BS, Olympio KPK, Cardoso VED, Peres S. Enamel fluorosis prevalence after a 7‐year interruption in water fluoridation in Jau, Sao Paulo, Brazil. Journal of Public Health Dentistry 2004;64(4):205‐8. [DOI] [PubMed] [Google Scholar]
Campain 2010 {published data only}
- Campain A, Marino R, Wright F, Harrison D, Bailey D, Morgan M. The impact of changing dental needs on cost savings from fluoridation. Australian Dental Journal Mar 2010;55(1):37‐44. [DOI] [PubMed] [Google Scholar]
Carmichael 1980 {published data only}
- Carmichael C, Rugg‐Gunn A, French A, Cranage J. The effect of fluoridation upon the relationship between caries experience and social class in 5‐year‐oldchildren in Newcastle and Northumberland. British Dental Journal 1980;149(6):163‐7. [DOI] [PubMed] [Google Scholar]
Carmichael 1984 {published data only}
- Carmichael C, Rugg‐Gunn A, French A, Cranage J. Carmichael CL, French AD, Rugg‐Gunn AJ, Furness JA. The relationship between social class and caries experience in five‐year‐old children in Newcastle andNorthumberland after twelve years' fluoridation. Community Dent Health 1984;1(1):47‐54. [PubMed] [Google Scholar]
- French A, Carmichael C, Rugg‐Gunn A, Furness J. Fluoridation and dental caries experience in 5‐year‐old children in Newcastle and Northumberland in 1981. British Dental Journal 1984;156(2):54‐7. [DOI] [PubMed] [Google Scholar]
Carmichael 1989 {published data only}
- Carmichael C, Rugg‐Gunn A, Ferrell R. The relationship between fluoridation, social class and caries experience in 5 year old children in Newcastle and Northumberland in 1987. British Dental Journal 1989;167:57‐61. [DOI] [PubMed] [Google Scholar]
Carvalho 2007 {published data only}
- Carvalho TS, Kehrle HM, Sampaio FC. Prevalence and severity of dental fluorosis among students from Joao Pessoa, PB, Brazil. Pesquisa Odontologica Brasileira = Brazilian Oral Research 2007;21(3):198‐203. [DOI] [PubMed] [Google Scholar]
Catani 2007 {published data only}
- Catani DB, Hugo FN, Cypriano S, Sousa MR, Cury JA. [Relationship between fluoride levels in the public water supply and dental fluorosis]. Revista de Saude Publica 2007;41(5):732‐9. [DOI] [PubMed] [Google Scholar]
Chen 2009 {published data only}
- Chen PZ, Yun ZJ, Bian JC, Li HX, Ma AH, Gao HX, et al. Analysis on surveillance outcome of endemic fluorosis in Shandong Province from 1992 to 2006. Chinese Journal of Endemiology 2009;28(5):537‐40. [Google Scholar]
Chen 2012 {published data only}
- Chen H, Yan M, Yang X, Chen Z, Wang G, Schmidt‐Vogt D, et al. Spatial distribution and temporal variation of high fluoride contents in groundwater and prevalence of fluorosis in humans in Yuanmou County, Southwest China. Journal of Hazardous Materials 2012;235‐236:201‐9. [DOI] [PubMed] [Google Scholar]
Cheng 2000 {published data only}
- Cheng H, Liang AX, Elly A, Ling ZQ, Li CR. Epidemiologic survey of dental fluorosis and caries in school students in Wensu county in Xinjiang. Shanghai kou qiang yi xue = Shanghai journal of stomatology 2000;9(4):232‐4. [PubMed] [Google Scholar]
Ciketic 2010 {published data only}
- Ciketic S, Hayatbakhsh M, Doran C. Drinking water fluoridation in South East Queensland: a cost‐effectiveness evaluation. Health Promotion Journal of Australia 2010;21(1):51‐6. [DOI] [PubMed] [Google Scholar]
Clark 2006 {published data only}
- Clark DC, Shulman JD, Maupomé G, Levy SM. Changes in dental fluorosis following the cessation of water fluoridation. Community Dentistry and Oral Epidemiology 2006;34(3):197‐204. [DOI] [PubMed] [Google Scholar]
de Lourdes Azpeitia‐Valadez 2009 {published data only}
- Lourdes Azpeitia‐Valadez M, Sanchez‐Hernandez MA, Rodriguez‐Frausto M. Risk factors for dental fluorosis in children between 6 and 15 years old [Spanish]. Revista Medica del Instituto Mexicano del Seguro Social 2009;47(3):265‐70. [PubMed] [Google Scholar]
Dini 2000 {published data only}
- Dini EL, Holt RD, Bedi R. Prevalence of caries and developmental defects of enamel in 9‐10 year old children living in areas in Brazil with differing water fluoride histories. British Dental Journal 2000;188(3):146‐9. [DOI] [PubMed] [Google Scholar]
Do 2007 {published data only}
- Do LG, Spencer AJ. Risk‐benefit balance in the use of fluoride among young children. Journal of Dental Research 2007;86(8):723‐8. [DOI] [PubMed] [Google Scholar]
Dobaradaran 2008 {published data only}
- Dobaradaran S, Mahvi AH, Dehdashti S, Abadi DRV. Drinking water fluoride and child dental caries in Dashtestan, Iran. Fluoride 2008;41(3):220‐6. [Google Scholar]
Evans 1995 {published data only}
- Evans D, Rugg‐Gunn A, Tabari E. The effect of 25 years of water fluoridation in Newcastle assessed in four surveys of 5‐year‐old children over an 18‐year period. British Dental Journal 1995;178(2):60‐4. [DOI] [PubMed] [Google Scholar]
Evans 2009 {published data only}
- Evans RW, Hsiau AC, Dennison PJ, Patterson A, Jalaludin B. Water fluoridation in the Blue Mountains reduces risk of tooth decay. Australian Dental Journal 2009;54(4):368‐73. [DOI] [PubMed] [Google Scholar]
Faye 2008 {published data only}
- Faye M, Diawara CK, Ndiaye KR, Yam AA. Dental fluorosis and dental caries prevalence in Senegalese children living in a high‐fluoride area and consuming a poor fluoridated drinking water [French]. Dakar Medical 2008;53(3):162‐9. [PubMed] [Google Scholar]
Gillcrist 2001 {published data only}
- Gillcrist JA, Brumley DE, Blackford JU. Community fluoridation status and caries experience in children. Journal of Public Health Dentistry 2001;61(3):168‐71. [DOI] [PubMed] [Google Scholar]
Gushi 2005 {published data only}
- Gushi LL, Soares Mda C, Forni TI, Vieira V, Wada RS, Sousa Mda L. Dental caries in 15‐to‐19‐year‐old adolescents in Sao Paulo State, Brazil, 2002 [Portuguese]. Cadernos de Saude Publica 2005;21(5):1383‐91. [DOI] [PubMed] [Google Scholar]
Han 2011 {published data only}
- Han DH, Kim JB, Bae KH. A comparison of dental caries status in cities with or without water fluoridation. Epidemiology 2011;22(1):S240. [Google Scholar]
Hobbs 1994 {published data only}
- Hobbs D. Annual report of the Director of Dental Public Health to Powys Health Authority. Powys 1994.
Hoffmann 2004 {published data only}
- Hoffmann RH, Cypriano S, Sousa Mda L, Wada RS. Dental caries experience in children at public and private schools from a city with fluoridated water [Portuguese]. Cadernos de Saude Publica 2004;20(2):522‐8. [DOI] [PubMed] [Google Scholar]
Hopcraft 2003 {published data only}
- Hopcraft M, Morgan M. Dental caries experience in a young adult military population. Australian Dental Journal 2003;48(2):125‐9. [DOI] [PubMed] [Google Scholar]
Hussain 2013 {published data only}
- Hussain I, Arif M, Hussain J. Fluoride contamination in drinking water in rural habitations of Central Rajasthan, India. Environmental Monitoring and Assessment 2012;184:5151‐8. [DOI] [PubMed] [Google Scholar]
Ito 2007 {published data only}
- Ito D. A cross‐sectional study to compare caries and fluorosis in 7‐year‐old schoolchildren from a fluoridated area with those in a neighbouring non‐fluoridated area in Ontario [MR27307][MSc thesis]. Canada: University of Toronto, 2007. [Google Scholar]
Jones 1997 {published data only}
- Jones C, Taylor G, Woods K, Whittle G, Evans D, Young P. Jarman underprivileged area scores,tooth decay and the effect of water fluoridation. Community Dental Health 1997;14(3):156‐60. [PubMed] [Google Scholar]
Jones 2000a {published data only}
Jones 2000b {published data only}
- Jones CM. The effect of water fluoridation and social deprivation on tooth decay. International Journal of Health Promotion and Education 2000;38(4):146‐50. [Google Scholar]
Kalsbeek 1993 {published data only}
- Kalsbeek H, Kwant G, Groeneveld A, Dirks O, Vaneck A, Theuns H. Caries experience of 15‐year‐old children in the Netherlands after discontinuation of water fluoridation. Caries Research 1933;27(3):201‐5. [DOI] [PubMed] [Google Scholar]
Khan 2004 {published data only}
- Khan AA, Whelton H, O'Mullane D. Is the fluoride level in drinking water a gold standard for the control of dental caries?. International Dental Journal 2004;54(5):256‐60. [DOI] [PubMed] [Google Scholar]
Kirkeskov 2010 {published data only}
- Kirkeskov L, Kristiansen E, Boeggild H, Platen‐Hallermund F, Sckerl H, Carlsen A, et al. The association between fluoride in drinking water and dental caries in Danish children. Linking data from health registers, environmental registers and administrative registers. Community Dentistry and Oral Epidemiology 2010;38(3):206‐12. [DOI] [PubMed] [Google Scholar]
Kozlowski 2002 {published data only}
- Kozlowski FC, Meneghim MC, Pereira AC, Ambrosano GMB. Dental caries and dental fluorosis prevalence after the water fluoridation. Journal of Dental Research 2002;81:B160. [Google Scholar]
Kukleva 2007 {published data only}
- Kukleva MP, Isheva AV, Kondeva VK, Dimitrova MM, Petrova SG. Prevalence of dental fluorosis among 4‐ to 14‐year‐old children from the town of Dimitrovgrad (Bulgaria). Folia Medica 2007;49(1‐2):25‐31. [PubMed] [Google Scholar]
Kumar 2001 {published data only}
- Kumar JV, Green EL, Coluccio C, Davenport R. Oral health status of second grade school children in upstate New York. New York State Dental Journal 2001;67(2):26‐31. [PubMed] [Google Scholar]
Kunzel 2000 {published data only}
- Kunzel W, Fischer T, Lorenz R, Bruhmann S. Decline of caries prevalence after the cessation of water fluoridation in the former East Germany. Community Dentistry and Oral Epidemiology 2000;28(5):382‐9. [DOI] [PubMed] [Google Scholar]
Kunzel 2000a {published data only}
- Kunzel W, Fischer T. Caries prevalence after cessation of water fluoridation in La Salud, Cuba. Caries Research 2000;34(1):20‐5. [DOI] [PubMed] [Google Scholar]
Lee 2004 {published data only}
- Lee M, Dennison PJ. Water fluoridation and dental caries in 5‐ and 12‐year‐old children from Canterbury and Wellington. New Zealand Dental Journal 2004;100(1):10‐5. [PubMed] [Google Scholar]
Liu 2006 {published data only}
- Liu SR, Li YX, Wu FP. Effect assessment of water supply improvement in the fluorosis prevalent regions in Meizhou, China. Journal of Environment and Health 2006;23(1):55‐7. [Google Scholar]
Liu 2009 {published data only}
- Liu X‐L, Ll X‐Q. Drinking water type fluorosis control and prevention in Shaanxi Province. Journal of Environment and Health 2009;26(11):994‐5. [Google Scholar]
Murray 1984 {published data only}
- Murray J, Gordon P, Carmichael C, French A, Furness J. Dental caries and enamel opacities in 10‐year old children in Newcastle. British Dental Journal 1984;156:255‐8. [DOI] [PubMed] [Google Scholar]
Murray 1991 {published data only}
- Murray J, Breckon J, Reynolds P, Tabari E, Nunn J. The effect of residence and social class on dental caries experience in 15‐16 year old children living in three towns (natural fluoride, adjusted fluoride and low fluoride) in the north east of England. British Dental Journal 1991;171(10):319‐22. [DOI] [PubMed] [Google Scholar]
Nayak 2009 {published data only}
- Nayak B, Roy MM, Das B, Pal A, Sengupta MK, De SP, et al. Fluoride contamination of groundwater: health effects of groundwater fluoride. Fluoride 2009;42(3):245‐6. [DOI] [PubMed] [Google Scholar]
Ncube 2005 {published data only}
- Ncube EJ, Schutte CF. The occurrence of fluoride in South African groundwater: a water quality and health problem. Water SA 2005;31(1):35‐40. [Google Scholar]
Nirgude 2010 {published data only}
- Nirgude AS, Saiprasad GS, Naik PR, Mohanty S. An epidemiological study on fluorosis in an urban slum area of Nalgonda, Andhra Pradesh, India. Indian Journal of Public Health 2010;54(4):194‐6. [DOI] [PubMed] [Google Scholar]
Niu 2012 {published data only}
- Niu ZH, Zhao JL. Analysis of monitoring data of drinking‐water borne endemic fluorosis in Xinzhou of Shanxi province in 2010. Chinese Journal of Endemiology 2012;31(3):321‐4. [Google Scholar]
Pandey 2002 {published data only}
- Pandey J, Nagda G. Prevalence of fluorosis in ten villages of Udaipur district of Rajasthan. Indian Journal of Environmental Sciences 2002;6(2):109‐112. [Google Scholar]
Pandey 2005 {published data only}
- Pandey J. Fluoride distribution and fluorosis in some rural areas of Udaipur, Rajashtan. Journal International Medical Sciences Academy 2005;18(3):133‐5. [Google Scholar]
Pandey 2010 {published data only}
- Pandey A. Prevalence of fluorosis in an endemic village in central India. Tropical Doctor 2010;40(4):217‐9. [DOI] [PubMed] [Google Scholar]
Peres 2006 {published data only}
- Peres M, Antunes J, Peres K. Is water fluoridation effective in reducing inequalities in dental caries distribution in developing countries? Recent findings from Brazil. Sozial‐und Praventivmedizin 2006;51(5):302‐10. [DOI] [PubMed] [Google Scholar]
Provart 1995 {published data only}
- Provart S, Carmichael C. The relationship between caries, fluoridation and material deprivation in five year‐old children in Country Durham. Community Dental Health 1995;12:200‐3. [PubMed] [Google Scholar]
Rihs 2008 {published data only}
- Rihs LB, Sousa Mda L, Wada RS. Root caries in areas with and without fluoridated water at the Southeast region of São Paulo State, Brazil. Journal of applied oral science: revista FOB 2008;16(1):70‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Riley 1999 {published data only}
- Riley J, Lennon M, Ellwood R. The effect of water fluoridation and social inequalities on dental caries in 5‐year‐old children. International Journal of Epidemiology 1999;28:300‐5. [DOI] [PubMed] [Google Scholar]
Ruan 2004 {published data only}
- Ruan JP, Liu ZQ, Song JL, Bjorvatn K, Ruan MS. [Effect of drinking water change upon the dental fluorosis]. Zhonghua kou qiang yi xue za zhi = Zhonghua kouqiang yixue zazhi = Chinese journal of stomatology 2004;39(2):139‐41. [PubMed] [Google Scholar]
Rugg‐Gun 1977 {published data only}
- Rugg‐Gunn A, Carmichael C, French A, Furness J. Fluoridation in Newcastle and Northumberland: a clinical study of five year old children. British Dental Journal 1977;142:395‐402. [DOI] [PubMed] [Google Scholar]
Sagheri 2007 {published data only}
- Sagheri D, McLoughlin J, Clarkson JJ. A comparison of dental caries levels in two communities with different oral health prevention strategies stratified in different social classes. Journal of Public Health Dentistry 2007;67(1):1‐7. [DOI] [PubMed] [Google Scholar]
Sales‐Peres 2002 {published data only}
- Sales‐Peres SH, Bastos JR. An epidemiological profile of dental caries in 12‐year‐old children residing in cities with and without fluoridated water supply in the central western area of the State of Sao Paulo, Brazil [Portuguese]. Cadernos de Saude Publica 2002;18(5):1281‐8. [DOI] [PubMed] [Google Scholar]
Saliba 2008 {published data only}
- Saliba NA, Moimaz SA, Casotti CA, Pagliari AV. Dental caries of lifetime residents in Baixo Guandu, Brazil, fluoridated since 1953‐‐a brief communication. Journal of Public Health Dentistry 2008;68(2):119‐21. [DOI] [PubMed] [Google Scholar]
Sampaio 2000 {published data only}
- Sampaio FC, Hossain AN, Fehr FR, Arneberg P. Dental caries and sugar intake of children from rural areas with different water fluoride levels in Paraíba, Brazil. Community Dentistry and Oral Epidemiology 2000;28(4):307‐13. [DOI] [PubMed] [Google Scholar]
Seppa 1998 {published data only}
- Seppa L, Karkkainen S, Hausen H. Caries in the primary dentition, after discontinuation of water fluoridation, among children receiving comprehensive dental care. Community Dentistry and Oral Epidemiology 2000;28(4):281‐8. [DOI] [PubMed] [Google Scholar]
- Seppa L, Larkkainen S, Hausen H. Caries frequency in permanent teeth before and after discontinuation of water fluoridation. Community Dentistry and Oral Epidemiology 1998;26:256‐62. [DOI] [PubMed] [Google Scholar]
Shitumbanuma 2007 {published data only}
- Shitumbanuma V, Tembo F, Tembo JM, Chilala S, Ranst E. Dental fluorosis associated with drinking water from hot springs in Choma district in southern province, Zambia. Environmental Geochemistry and Health 2007;29(1):51‐8. [DOI] [PubMed] [Google Scholar]
Slade 2013 {published data only}
- Slade G, Sanders A, Do L, Roberts‐Thomson K, Spencer A. Effects of fluoridated drinking water on dental caries in Australian adults. Journal of Dental Research 2013;92:376. [DOI] [PubMed] [Google Scholar]
Sohu 2007 {published data only}
- Sohu D, Sharma JD, Jain P. Groundwater quality of villages of Sanganer Tehsil: focus on fluoride and fluorosis. Journal of Ecotoxicology & Environmental Monitoring 2007;17(3):227‐33. [Google Scholar]
Spencer 2008 {published data only}
- Spencer AJ, Do LG. Changing risk factors for fluorosis among South Australian children. Community Dentistry and Oral Epidemiology 2008;36(3):210‐8. [DOI] [PubMed] [Google Scholar]
Sun 2007 {published data only}
- Sun DJ. Surveillance on endemic fluorosis of drinking water type in China: a two‐year report of 2003 and 2004. Chinese Journal of Epidemiology 2007;26(2):161‐4. [Google Scholar]
Tagliaferro 2004 {published data only}
- Tagliaferro EP, Cypriano S, Sousa Mda L, Wada RS. Caries experience among schoolchildren in relation to community fluoridation status and town size. Acta Odontologica Scandinavica 2004;62(3):124‐8. [DOI] [PubMed] [Google Scholar]
Tiano 2009 {published data only}
- Tiano AV, Moimaz SA, Saliba O, Saliba NA. Dental caries prevalence in children up to 36 months of age attending daycare centers in municipalities with different water fluoride content. Journal of Applied Oral Science 2009;17(1):39‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tickle 2003 {published data only}
- Tickle M, Milsom KM, Jenner TM, Blinkhorn AS. The geodemographic distribution of caries experience in neighboring fluoridated and nonfluoridated populations. Journal of Public Health Dentistry 2003;63(2):92‐8. [DOI] [PubMed] [Google Scholar]
Vuhahula 2008 {published data only}
- Vuhahula EAM, Masalu JRP, Mabelya L, Wandwi WBC. Dental fluorosis in Tanzania Great Rift Valley in relation to fluoride levels in water and in `Magadi' (Trona). Water and sanitation in international development and disaster relief (WSIDDR);. Edinburgh: Elsevier, 2008.
Wang 2005 {published data only}
- Wang BB, Zheng BS, Wang HY, Ping YK, Tao YH. Relationship between fluorine concentration in drinking water and dental health of residents in fluorine exposure areas in Bazhou city. Chinese Journal of Endemiology 2005;24(1):70‐2. [Google Scholar]
Wang 2008 {published data only}
- Wang JH, Zheng ZX, Liu W, Liu Y, Gao R, Li ZR, et al. Endemic fluorosis: prevalence and prevention in Liaoning Province. Chinese Journal of Epidemiology 2008;27(6):663‐7. [Google Scholar]
Wei 2010 {published data only}
- Wei SY, Lu Q, Ding P, Ding SR, Pu GL, Chen P, et al. Outcome analysis on drinking‐water type endemic fluorosis in Qinghai in 2008. Chinese Journal of Endemiology 2010;29(1):77‐9. [Google Scholar]
Wong 2006 {published data only}
- Wong HM, McGrath C, Lo ECM, King NM. Association between developmental defects of enamel and different concentrations of fluoride in the public water supply. Caries Research 2006;40(6):481‐6. [DOI] [PubMed] [Google Scholar]
Wong 2014 {published data only}
- Wong H, McGrath C, King N. Diffuse opacities in 12‐year‐old Hong Kong children‐‐four cross‐sectional surveys. Community Dentistry and Oral Epidemiology 2014;42(1):61‐9. [DOI] [PubMed] [Google Scholar]
Wongdem 2001 {published data only}
- Wongdem JG, Aderinokun GA, Ubom GA, Sridhar MK, Selkur S. Dental fluorosis and fluoride mapping in Langtang town, Nigeria. African Journal of Medicine and Medical Sciences 2001;30(1‐2):31‐4. [PubMed] [Google Scholar]
Wragg 1999 {published data only}
- Wragg K. Dental caries experience of 5 year olds in South Derbyshire. Unpublished 1992.
Wu 2006 {published data only}
- Wu JQ, Peng JW, Li TL, Wu HY, Li BL, Miao LJ. Investigating the current water‐related endemic fluorosis in Shaoguan City of Guangdong Province. Chinese Journal of Epidemiology 2006;25(5):535‐6. [Google Scholar]
Wu 2008 {published data only}
- Wu JQ, Dai CF, Wu HY, Feng GH, Du GX. Results of the national surveillance on endemic fluorosis in Fengshun County of Guangdong Province in 2005‐2006. Chinese Journal of Epidemiology 2008;27(6):673‐4. [Google Scholar]
Zhu 2009 {published data only}
- Zhu CS, Chen YF. Investigation of drinking water fluoride and fluorosis in Shaanxi Province from 2005 to 2007. Journal of Chinese Integrative Medicine 2009;7(5):181‐3. [Google Scholar]
Zietsman 2003 {published data only}
- Zietsman S. The relation between the fluoride content of drinking water and the occurrence of dental fluorosis in selected areas in South Africa: a medical geographical study [0807245]. South Africa: University of South Africa (South Africa) 2003. [Google Scholar]
Zimmermann 2002 {published data only}
- Zimmermann E, Salas A, Maino A, Gaitieri M, Novarese I, Cachia A, et al. Caries experience in children living in areas supplied with artificially fluoridated drinking water (Rosario, Santa Fe). 35th Annual Meeting of the International Association for Dental Research. Buenos Aires, 2002.
References to studies awaiting assessment
Wang 2014 {published data only}
- Wang Y, Wang C‐S, Xia Y‐T, Wang P‐H. Investigation on drinking water‐borne endemic fluorosis in Jiangsu, 2013. Journal of Environment and Health 2014;31(6):516‐8. [Google Scholar]
References to ongoing studies
Pretty (ongoing) {unpublished data only}
- An evaluation of a water fluoridation scheme in Cumbria. Ongoing study 2013.
Additional references
ADA 2013
- American Dental Association. Surgeon General Endorses Fluoridation. www.ada.org/news/8532.aspx (accessed August 2013).
Ahovuo‐Saloranta 2013
- Ahovuo‐Saloranta A, Forss H, Walsh T, Hiiri A, Nordblad A, Mäkelä M, et al. Sealants for preventing dental decay in the permanent teeth. Cochrane Database of Systematic Reviews 2013, Issue 3. [DOI: 10.1002/14651858.CD001830.pub4] [DOI] [PubMed] [Google Scholar]
Bagramian 2009
- Bagramian RA, Garcia‐Godoy F, Volpe AR. The global increase in dental caries. A pending public health crisis. American Journal of Dentistry 2009;22(1):3‐8. [PubMed] [Google Scholar]
Bernabe 2014
- Bernabe E, Sheiham A. Extent of differences in dental caries in permanent teeth between childhood and adulthood in 26 countries. International Dental Journal 2014;64(5):241‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Browne 2005
- Browne D, Whelton H, O'Mullane D. Fluoride metabolism and fluorosis. Journal of Dentistry 2005;33(3):177‐86. [DOI] [PubMed] [Google Scholar]
Bruce 2014
- Bruce N, Pruss‐Ustun A, Pope D, Adair‐ Rohani H, Rehfuess E. WHO Indoor Air Quality Guidelines: household fuel combustion. Methods used for evidence assessment. http://www.who.int/indoorair/guidelines/hhfc/Evidence_review_methods.pdf (accessed April 2015) 2014.
Burford 2012
- Burford BJ, Rehfuess E, Schünemann HJ, Akl EA, Waters E, Armstrong R, et al. Assessing evidence in public health: the added value of GRADE. Journal of Public Health (Oxford, England) 2012;34(4):631‐5. [DOI] [PubMed] [Google Scholar]
Burt 1999
- Burt BA, Eklund SA. Dentistry, Dental Practice and the Community. Philadelphia, Pennsylvania: WB Saunders Company, 1999. [Google Scholar]
CAPP database, 2015
- Global caries map for 12 year olds (2013‐2014). http://www.mah.se/CAPP/Country‐Oral‐Health‐Profiles/According‐to‐Alphabetical/Global‐caries‐map‐2013‐‐2014/ Accessed 9 February 2015.
CDC 2005
- Centers for Disease Control and Prevention (CDC). Surveillance for dental caries, dental sealants, tooth retention, edentulism and enamel fluorosis ‐ United States, 1988‐1994 and 1999‐2002. MMWR Surveillance Summaries 2005;54(3):1‐44. [PubMed] [Google Scholar]
CDC 2008
- Centers for Disease Control and Prevention (CDC). 2008 Water Fluoridation Statistics. www.cdc.gov/fluoridation/statistics/2008stats.htm (accessed March 2012).
Cheng 2007
- Cheng KK, Chalmers I, Sheldon TA. Adding fluoride to water supplies. BMJ 2007;335(7622):699‐702. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cochran 2004b
- Cochran J, Ketley C, Sanches L, Mamai‐Homata E, Oila A‐M, Arnadottir I, et al. A standardized photographic method for evaluating enamel opacities including fluorosis. Community Dentistry and Oral Epidemiology 2004;32(Suppl 1):19‐27. [DOI] [PubMed] [Google Scholar]
Dean 1941
- Dean T, Jay P, Arnold F, Elvove E. Domestic water and dental caries. II. A study of 2832 white children, aged 12‐14 years, of 8 suburban communities, including Lactobacillus acidophilus studies of 1761 children. Public Health Reports 1941;56(15):761‐92. [Google Scholar]
Department of Health and Human Services 2000
- Department of Health and Human Services (US), Office of the Surgeon General. Rockville: National Institutes of Health, National Institute of Dental and Craniofacial Research, 2000. [Google Scholar]
Department of National Health and Welfare 1952
- Dental Health Division and Research and Statistics Division. Department of National Health and Welfare, Ottawa: A suggested Methodology for Fluoridation Surveys in Canada. 1952.
Dye 2007
- Dye BA, Tan S, Smith V, Lewis BG, Barker LK, Thornton‐Evans G, et al. Trends in Oral Health Status: United States, 1988‐1994 and 1999‐2004. Vital and Health Statistics Series. Series 11, No 248. National Center for Health Statistics 2007:1‐92. [PubMed]
European Union 1998
- European Union 1998 Council Directive 98/83/EC. On the Quality of Water Intended for Human Consumption. Official Journal of the European Communities 1998; Vol. L330/42.
Feitosa 2005
- Feitosa S, Colares V, Pinkham J. The psychosocial effects of severe caries in 4‐year‐old children in Recife, Pernambuco, Brazil. Cadernos de Saúde Pública 2005;21(5):1550‐6. [DOI] [PubMed] [Google Scholar]
Frieden 2010
- Frieden TR. A framework for public health action: the health impact pyramid. American Journal of Public Health 2010;100(4):590‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Griffin 2007
- Griffin SO, Regnier E, Griffin PM, Huntley V. Effectiveness of fluoride in preventing caries in adults. Journal of Dental Research 2007;86(5):410‐5. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Kearney 2010
- Kearney J. Food consumption trends and drivers. Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences 2010;365:2793–807. [DOI] [PMC free article] [PubMed] [Google Scholar]
Knapp 2003
- Knapp G, Hartung J. Improved tests for a random effects meta‐regression with a single covariate. Statististics in Medicine 2003;22(17):2693‐710. [DOI] [PubMed] [Google Scholar]
Landis 1977
- Landis JR, Koch GG. An application of hierarchical kappa‐type statistics in the assessment of majority agreement among multiple observers. Biometrics 1977;33(2):363‐74. [PubMed] [Google Scholar]
Leclercq 1987
- Leclercq M, Barmes D, Sardo‐Infirri J. Oral health: global trends and projections. World Health Statistics Quarterly 1987;40:116‐28. [PubMed] [Google Scholar]
Leverett 1986
- Leverett D. Prevalence of dental fluorosis in fluoridated and nonfluoridated communities‐‐a preliminary investigation. J Public Health Dent 1986;46(4):184‐7. [DOI] [PubMed] [Google Scholar]
Loke 2007
- Loke YK, Price D, Herxheimer A, Cochrane Adverse Effects Methods Group. Systematic reviews of adverse effects: framework for a structured approach. BMC Medical Research Methodology 2007;7:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Marinho 2003a
- Marinho V, Higgins J, Logan S, Sheiham A. Topical fluoride (toothpastes, mouthrinses, gels or varnishes) for preventing dental caries in children and adolescents. Cochrane Database of Systematic Reviews 2003, Issue Issue 4. [DOI: 10.1002/14651858.CD002782] [DOI] [PMC free article] [PubMed] [Google Scholar]
Marinho 2003b
- Marinho VCC, Higgins JPT, Loga S, Sheiham A. Fluoride toothpastes for preventing dental caries in children and adolescents. Cochrane Database of Systematic Reviews 2003, Issue Issue 1. [DOI: 10.1002/14651858.CD002278] [DOI] [PMC free article] [PubMed] [Google Scholar]
Marinho 2013
- Marinho VCC, Worthington HV, Walsh T, Clarkson JE. Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database of Systematic Reviews 2013, Issue 7. [DOI: 10.1002/14651858.CD002279.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
McDonagh 2000
- McDonagh M, Whiting P, Bradley M, Cooper J, Sutton A, Chestnutt I, et al. A Systematic Review of Community Water Fluoridation. NHS Centre for Reviews and Dissemination, University of York 2000.
MRC 2002
- Medical Research Council (MRC). Working Group Report: Water Fluoridation and Health. www.mrc.ac.uk/pdf‐publications‐water_fluoridation_report.pdf (accessed February 2015).
NHMRC 2007
- National Health and Medical Research Council (NHMRC), Australian Government. A Systematic Review of the Efficacy and Safety of Water Fluoridation. Canberra: National and Medical Research Council 2007.
OECD 2011
- Organisation for Economic Co‐operation and Development (OECD). Health at a Glance 2011: OECD Indicators. OECD Publishing 2011.
Pendrys 2001
- Pendrys DG. Fluoride ingestion and oral health. Nutrition 2001;17(11‐12):979‐80. [DOI] [PubMed] [Google Scholar]
Petersen 2003
- Petersen PE. The World Oral Health Report 2003: continuous improvement of oral health in the 21st century‐‐the approach of the WHO Global Oral Health Programme. Community Dentistry and Oral Epidemiology 2003;31 Suppl 1:3‐23. [DOI] [PubMed] [Google Scholar]
Petersen 2004
- Petersen PE, Peng B, Tai B, Bian Z, Fan M. Effect of a school‐based oral health education programme in Wuhan City, Peoples Republic of China. International Dental Journal 2004;54(1):33‐41. [DOI] [PubMed] [Google Scholar]
Rehfuess 2013
- Rehfuess EA, Akl EA. Current experience with applying the GRADE approach to public health interventions: an empirical study. BMC Public Health 2013;13(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rozier 1994
- Rozier RG. Epidemiologic indices for measuring the clinical manifestations of dental fluorosis: overview and critique. Advances in Dental Research 1994;8(1):39‐55. [DOI] [PubMed] [Google Scholar]
Rugg‐Gunn 2012
- Rugg‐Gunn A, Do L. Effectiveness of water fluoridation in caries prevention. Community Dentistry and Oral Epidemiology 2012;40(Suppl 2):55‐64. [DOI] [PubMed] [Google Scholar]
Selwitz 2007
- Selwitz RH, Ismail AI, Pitts NB. Dental caries. Lancet 2007;369(9555):51‐9. [DOI] [PubMed] [Google Scholar]
Sheiham 2005
- Sheiham A. Oral health, general health and quality of life. Bulletin of the World Health Organization 2005;83(9):644. [PMC free article] [PubMed] [Google Scholar]
Slade 2013
- Slade GD, Sanders AE, Do L, Roberts‐Thomson K, Spencer AJ. Effects of fluoridated drinking water on dental caries in Australian adults. Journal of Dental Research 2013;92(4):376‐82. [DOI] [PubMed] [Google Scholar]
Slimani 2009
- Slimani N, Deharveng G, Southgate DAT, Biessy C, Chajes V, Bakkel MME, et al. Contribution of highly industrially processed foods to the nutrient intakes and patterns of middle‐aged populations in the European Prospective Investigation into Cancer and Nutrition study. European Journal of Clinical Nutrition 2009;63:S206–25. [DOI] [PubMed] [Google Scholar]
SucDen 2015
- SucDen. World Sugar Consumption. http://www.sucden.com/statistics/4_world‐sugar‐consumption (accessed February 2015).
Ten Cate 1991
- Cate JM, Featherstone JD. Mechanistic aspects of the interactions between fluoride and dental enamel. Critical Reviews in Oral Biology and Medicine 1991;2(3):283‐96. [DOI] [PubMed] [Google Scholar]
The British Fluoridation Society 2012
- The British Fluoridation Society. One in a million: the facts about water fluoridation 2012; Vol. 3rd Edition.
Truman 2002
- Truman BI, Gooch BF, Sulemana I, Gift HC, Horowitz AM, Evans CA, et al. Reviews of evidence on interventions to prevent dental caries, oral and pharyngeal cancers, and sports‐related craniofacial injuries. American Journal of Preventive Medicine 2002;23(1 Suppl):21‐54. [DOI] [PubMed] [Google Scholar]
van Rijkom 1996
- Rijkom HM, Truin GJ, van't Hof MA. A meta‐analysis of clinical studies on the caries‐inhibiting effect of chlorhexidine treatment. Journal of Dental Research 1996;75:790‐5. [DOI] [PubMed] [Google Scholar]
Walsh 2010
- Walsh T, Worthington HV, Glenny A‐M, Appelbe P, Marinho VCC, Shi X. Fluoride toothpastes of different concentrations for preventing dental caries in children and adolescents. Cochrane Database of Systematic Reviews 2010, Issue 1. [DOI: 10.1002/14651858.CD007868.pub2] [DOI] [PubMed] [Google Scholar]
WHO 2006
- World Health Organization (WHO). Fluoride in Drinking Water. Geneva: World Health Organization 2006.
WHO 2011
- World Health Organization (WHO). Guidelines for Drinking‐Water Quality, 4th edition. Geneva: World Health Organization 2011.


