Abstract
Background
The gag reflex is an involuntary defence mechanism to protect the pharynx and throat from foreign objects. Gagging is a common problem encountered during dental treatment, making therapeutic procedures distressing and often difficult or even impossible to perform. Various interventions can be used to control the gag reflex: anti‐nausea medicines, sedatives, local and general anaesthetics, herbal remedies, behavioural therapies, acupressure, acupuncture, laser, and prosthetic devices. This is an update of the Cochrane Review first published in 2015.
Objectives
To assess the effects of pharmacological and non‐pharmacological interventions for the management of gagging in people undergoing dental treatment.
Search methods
Cochrane Oral Health's Information Specialist searched the Cochrane Oral Health's Trials Register (to 18 March 2019), the Cochrane Central Register of Controlled Trials (CENTRAL; 2019, Issue 2) in the Cochrane Library (searched 18 March 2019), MEDLINE Ovid (1946 to 18 March 2019), Embase Ovid (1980 to 18 March 2019), CINAHL EBSCO (1937 to 18 March 2019), AMED Ovid (1985 to 18 March 2019), and the proceedings of the International Association for Dental Research (IADR) online (2001 to 18 March 2019). The US National Institutes of Health Ongoing Trials Register (ClinicalTrials.gov) and the World Health Organization International Clinical Trials Registry Platform were searched for ongoing trials. We also conducted forwards citation searching on the included studies via Google Scholar. No restrictions were placed on the language or date of publication when searching the electronic databases.
Selection criteria
We included randomised controlled trials (RCTs), involving people who were given a pharmacological or non‐pharmacological intervention to manage gagging that interfered with dental treatment. We excluded quasi‐RCTs. We excluded trials with participants who had central or peripheral nervous system disorders, who had oral lesions or were on systemic medications that might affect the gag sensation, or had undergone surgery which might alter anatomy permanently.
Data collection and analysis
We independently selected trials, extracted data, and assessed risk of bias. We followed Cochrane's statistical guidelines. We assessed the overall certainty of the evidence using GRADE.
Main results
We included four trials at unclear risk of bias with 328 participants (263 adults and 65 children who were four years or older), in which one trial compared acupuncture and acupressure (with thumb, device and sea band) at P6 (point located three‐finger breadths below the wrist on the inner forearm in between the two tendons) to sham acupuncture and acupressure with and without sedation. One trial compared acupuncture at P6 point to sham acupuncture. These trials reported both completion of dental procedure and reduction in gagging (assessor and patient reported) as their outcomes. One cross‐over and one split‐mouth trial studied the effect of laser at P6 point compared to control. One trial reported reduction in gagging and another reported presence or absence of gagging during dental procedure.
Acupuncture at P6 showed uncertain evidence regarding the successful completion of dental procedure (RR 1.78, 95% CI 1.05 to 3.01; two trials, 59 participants; very low‐certainty evidence) and uncertain evidence regarding the reduction in gagging (RR 2.57, 95% CI 1.12 to 5.89; one trial, 26 participants; very low‐certainty evidence) in comparison to sham acupuncture. Acupuncture at P6 with sedation did not show any difference when compared to sham acupuncture with sedation (RR 1.08, 95% CI 0.91 to 1.28; one trial, 34 participants; very low‐certainty evidence).
Acupressure using thumb pressure with or without sedation showed no clear difference in completing dental procedure (RR 0.96, 95% CI 0.84 to 1.10; one trial, 39 participants; very low‐certainty evidence; and RR 0.85, 95% CI 0.50 to 1.46; one trial, 30 participants; very low‐certainty evidence; respectively), or reduction in gagging (RR 1.06, 95% CI 0.92 to 1.23; one trial, 39 participants; very low‐certainty evidence; and RR 0.92, 95% CI 0.60 to 1.41; one trial, 30 participants; very low‐certainty evidence; respectively) when compared to sham acupressure with or without sedation.
Acupressure at P6 with device showed uncertain evidence regarding the successful completion of dental procedure (RR 2.63, 95% CI 1.33 to 5.18; one trial, 34 participants; very low‐certainty evidence) and uncertain evidence regarding the reduction in gagging (RR 3.94, 95% CI 1.63 to 9.53; one trial, 34 participants; very low‐certainty evidence) when compared to sham acupressure. However, device combined with sedation showed no difference for either outcome (RR 1.16, 95% CI 0.90 to 1.48; one trial, 27 participants; very low‐certainty evidence; and RR 1.26, 95% CI 0.93 to 1.69; one trial, 27 participants; very low‐certainty evidence; respectively).
Acupressure using a sea band with or without sedation showed no clear difference in completing dental procedure (RR 0.88, 95% CI 0.67 to 1.17; one trial, 21 participants; very low‐certainty evidence; and RR 1.80, 95% CI 0.63 to 5.16; one trial, 19 participants; very low‐certainty evidence; respectively), or reduction in gagging (RR 0.88, 95% CI 0.67 to 1.17; one trial, 21 participants; very low‐certainty evidence; and RR 2.70, 95% CI 0.72 to 10.14; one trial, 19 participants; very low‐certainty evidence; respectively) when compared to sham acupressure with or without sedation.
Laser at P6 showed a difference in absence of gagging (odds ratio (OR) 86.33, 95% CI 29.41 to 253.45; one trial, 40 participants; very low‐certainty evidence) and reduction in gagging (MD 1.80, 95% CI 1.53 to 2.07; one trial, 25 participants; very low‐certainty evidence) during dental procedure when compared to dummy laser application.
No noteworthy adverse effects were reported. For acupuncture at P6, the trial authors were unsure whether the reported adverse effects were due to participant anxiety or due to the intervention. None of the trials on acupressure or laser reported on this outcome.
We did not find trials evaluating any other interventions used to manage gagging in people undergoing dental treatment.
Authors' conclusions
We found very low‐certainty evidence from four trials that was insufficient to conclude if there is any benefit of acupuncture, acupressure or laser at P6 point in reducing gagging and allowing successful completion of dental procedures. We did not find any evidence on any other interventions for managing the gag reflex during dental treatment. More well‐designed and well‐reported trials evaluating different interventions are needed.
Plain language summary
Management of gagging in dental patients
Review question
With this Cochrane Review we tried to find out the best way to manage gagging in people having dental treatment.
Background
The gag reflex is a normal process to protect the throat and airway from foreign objects and prevent choking. Many people have an exaggerated gag reflex that causes distress during dental treatment. This can make it difficult or even impossible to perform the treatment. The interventions used to manage gagging include anti‐nausea medicines, sedatives, local and general anaesthetics, herbal remedies, behaviour therapy and cognitive behaviour therapy, acupressure, acupuncture, laser, and prosthetic devices.
We wanted to know how effective and safe these interventions are in helping people complete their dental treatment with less gagging. We compared them to no intervention or a placebo or to other interventions.
Study characteristics
This review is up‐to‐date as of 18 March 2019. We included four trials with 328 people (263 adults and 65 children who were 4 years or older). These people had nausea before when having dental treatment that caused the treatment to be stopped or not carried out properly.
Key results
Acupuncture at P6 point (a point located in the inside of the wrist) showed uncertain evidence regarding the successful completion of dental treatment and reduction in gagging when compared to sham (fake) acupuncture. The same intervention with sedation did not show a difference.
Acupressure (with thumb or sea band (bands that fit around the wrist just like a sweat band with a pressure stud sewn inside)) at P6 point with or without sedation did not show any difference when compared to sham acupressure. Acupressure at P6 point with device showed a difference in completing dental treatment and reduction in gagging. It did not show a difference when combined with sedation.
Laser at P6 point showed a difference in absence of gagging and reduction in gagging during dental treatment when compared to sham laser application.
The included studies did not report any important harmful effects of the treatment.
Certainty of the evidence
The level of belief we have in these findings is very low. This was due to unclear risk of bias and the small number of people studied in the four included trials.
Conclusion
We do not have enough evidence to say which intervention works better to manage gagging in people having dental treatment. We suggest that more well‐conducted studies should be done in this area.
Summary of findings
Summary of findings 1. Acupuncture with or without sedation for gagging in patients undergoing dental treatment.
| Acupuncture with or without sedation for gagging in patients undergoing dental treatment | ||||||
| Patient or population: patients undergoing dental treatment Setting: university hospital Intervention: acupuncture at P6 point with or without sedation Comparison: sham acupuncture with or without sedation | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with sham acupuncture | Risk with acupuncture | |||||
| Acupuncture without sedation | ||||||
| Completion of dental procedure | Study population | RR 1.78 (1.05 to 3.01) |
59 (2 RCTs)a,b | ⊕⊝⊝⊝ VERY LOWc,d,e | ||
| 357 per 1000 | 636 per 1000 (375 to 1000) | |||||
| Reduction in gagging (patient‐reported, dichotomous data) |
Study population | RR 2.57 (1.12 to 5.89) |
26 (1 RCT)a | ⊕⊝⊝⊝ VERY LOWc,f,h | No clear difference found when outcome was assessor‐reported or patient‐reported (VAS) (1 RCTb, 33 participants) | |
| 333 per 1000 | 857 per 1000 (373 to 1000) | |||||
| Presence or absence of gagging | None of the trials reported this outcome | |||||
| Adverse effects | ‐ | ‐ | 33 (1 RCT)b | ⊕⊝⊝⊝ VERY LOWc,f,g |
The trial authors were unsure whether the reported adverse events were due to participant anxiety or due to intervention | |
| Acupuncture with sedation | ||||||
| Completion of dental procedure | Study population | RR 1.08 (0.91 to 1.28) |
34 (1 RCT)a |
⊕⊝⊝⊝ VERY LOWc,f,i |
||
| 933 per 1000 | 1000 per 1000 (849 to 1000) |
|||||
| Reduction in gagging (patient‐reported, dichotomous data) |
Study population | RR 1.09 (0.87 to 1.37) |
34 (1 RCT)a |
⊕⊝⊝⊝ VERY LOWc,f,i |
||
| 867 per 1000 | 945 per 1000 (754 to 1000) |
|||||
| Presence or absence of gagging | None of the trials reported this outcome | |||||
| Adverse effects | None of the trials reported this outcome | |||||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) CI: confidence interval; P6: point located 3‐finger breadths below the wrist on the inner forearm in between the 2 tendons; RR: risk ratio; RCT: randomised controlled trial; VAS: visual analogue scale | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect | ||||||
aLu 2000. bZotelli 2014. cDowngraded 1 level for unclear risk of bias. dDowngraded 1 level for indirectness: only 2 studies and done only in adults. eDowngraded 1 level, imprecision apparent from width of confidence interval (due to small sample size even after combining 2 studies (n = 59)). fDowngraded 1 level for indirectness: single study including adults only. gDowngraded 1 level, imprecision apparent from width of confidence interval (due to small sample size (n = 33)). hDowngraded 1 level, imprecision apparent from width of confidence interval (due to small sample size (n = 26)). iDowngraded 1 level, imprecision apparent from width of confidence interval (due to small sample size (n = 34)).
Summary of findings 2. Acupressure with thumb, device or sea band compared to sham acupressure with or without sedation for gagging in patients undergoing dental treatment.
| Acupressure with thumb, device or sea band compared to sham acupressure with or without sedation for gagging in patients undergoing dental treatment | ||||||
| Patient or population: patients undergoing dental treatment Setting: university hospital Intervention: acupressure at P6 point with thumb, device or sea band with or without sedation Comparison: sham acupressure with or without sedation | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with sham acupressure | Risk with acupressure | |||||
| Presence or absence of gagging | None of the trials comparing acupressure with thumb, device or sea band to sham acupressure with or without sedation reported this outcome | |||||
| Adverse effects | None of the trials comparing acupressure with thumb, device or sea band to sham acupressure with or without sedation reported adverse effects | |||||
| Acupressure with thumb | ||||||
| Completion of dental procedure | Study population | RR 0.85 (0.50 to 1.46) |
30 (1 RCT)a |
⊕⊝⊝⊝ VERY LOWb,c,d | ||
| 692 per 1000 | 588 per 1000 (346 to 1000) |
|||||
| Reduction in gagging (patient‐reported) |
Study population | RR 0.92 (0.60 to 1.41) |
30 (1 RCT)a |
⊕⊝⊝⊝ VERY LOWb,c,d | ||
| 769 per 1000 | 708 per 1000 (462 to 1000) |
|||||
| Acupressure with device | ||||||
| Completion of dental procedure | Study population | RR 2.63 (1.33 to 5.18) | 34 (1 RCT)a | ⊕⊝⊝⊝ VERY LOWb,c,d | ||
| 333 per 1000 | 877 per 1000 (443 to 1000) | |||||
| Reduction in gagging (patient‐reported) |
Study population | RR 3.94 (1.63 to 9.53) | 34 (1 RCT)a | ⊕⊝⊝⊝ VERY LOWb,c,d | ||
| 222 per 1000 | 876 per 1000 (362 to 1000) | |||||
| Acupressure with sea band | ||||||
| Completion of dental procedure | Study population | RR 1.80 (0.63 to 5.16) | 19 (1 RCT)a |
⊕⊝⊝⊝ VERY LOWb,c,d | ||
| 333 per 1000 | 600 per 1000 (210 to 1000) |
|||||
| Reduction in gagging (patient‐reported) |
Study population | RR 2.70 (0.72 to 10.14) | 19 (1 RCT)a |
⊕⊝⊝⊝ VERY LOWb,c,d | ||
| 222 per 1000 | 600 per 1000 (160 to 1000) |
|||||
| Acupressure with thumb with sedation | ||||||
| Completion of dental procedure | Study population | RR 0.96 (0.84 to 1.10) | 39 (1 RCT)a |
⊕⊝⊝⊝ VERY LOWb,c,d | ||
| 1000 per 1000 | 960 per 1000 (840 to 1000) |
|||||
| Reduction in gagging (patient‐reported) |
Study population | RR 1.06 (0.92 to 1.23) | 39 (1 RCT)a |
⊕⊝⊝⊝ VERY LOWb,c,d | ||
| 944 per 1000 | 1000 per 1000 (869 to 1000) |
|||||
| Acupressure with device with sedation | ||||||
| Completion of dental procedure | Study population | RR 1.16 (0.90 to 1.48) | 27 (1 RCT)a |
⊕⊝⊝⊝ VERY LOWb,c,d | ||
| 857 per 1000 | 994 per 1000 (771 to 1000) |
|||||
| Reduction in gagging (patient‐reported) |
Study population | RR 1.26 (0.93 to 1.69) | 27 (1 RCT)a |
⊕⊝⊝⊝ VERY LOWb,c,d | ||
| 786 per 1000 | 990 per 1000 (731 to 1000) |
|||||
| Acupressure with sea band with sedation | ||||||
| Completion of dental procedure | Study population | RR 0.88 (0.67 to 1.17) | 21 (1 RCT)a |
⊕⊝⊝⊝ VERY LOWb,c,d | ||
| 1000 per 1000 | 880 per 1000 (670 to 1000) |
|||||
| Reduction in gagging (patient‐reported) |
Study population | RR 0.88 (0.67 to 1.17) | 21 (1 RCT)a |
⊕⊝⊝⊝ VERY LOWb,c,d | ||
| 1000 per 1000 | 880 per 1000 (670 to 1000) |
|||||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) CI: confidence interval; P6: point located 3‐finger breadths below the wrist on the inner forearm in between the 2 tendons; RR: risk ratio; RCT: randomised controlled trial | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect | ||||||
aLu 2000. bDowngraded 1 level for unclear risk of bias. cDowngraded 1 level for indirectness: single trial done only in adults. dDowngraded 1 level, imprecision apparent from width of confidence interval (due to small sample size).
Summary of findings 3. Laser for gagging in patients undergoing dental treatment.
| Laser for gagging in patients undergoing dental treatment | ||||||
| Patient or population: patients undergoing dental treatment Setting: university hospital Intervention: laser Comparison: control | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with control | Risk with laser | |||||
| Completion of dental treatment | None of the trials reported this outcome | |||||
| Reduction in gagging (assessor‐reported) |
The mean reduction in gagging was 0 | MD 1.80 higher (1.53 higher to 2.07 higher) |
‐ | 25 (1 RCT)a | ⊕⊝⊝⊝ VERY LOWc,d,f |
Low‐level laser at P6 point for 14 seconds |
| Presence or absence of gagging | Study population | OR 86.33 (29.41 to 253.45) | 40 (1 RCT)b | ⊕⊝⊝⊝ VERY LOWc,d,e | Low‐level laser at P6 point for 1 minute showed difference in absence of gagging | |
| 125 per 1000 | 925 per 1000 (808 to 973) | |||||
| Adverse effects | None of the trials reported adverse effects | |||||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) CI: confidence interval; MD: mean difference; OR: odds ratio; P6: point located 3‐finger breadths below the wrist on the inner forearm in between the 2 tendons; RCT: randomised controlled trial | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect | ||||||
aElbay 2016. bGoel 2017. cDowngraded 1 level for unclear risk of bias. dDowngraded 1 level for indirectness: single trial done only in children. eDowngraded 1 level, imprecision apparent from width of confidence interval (due to small sample size (n = 40)). fDowngraded 1 level, imprecision apparent from width of confidence interval (due to small sample size (n = 25)).
Background
Description of the condition
Gagging is described as a somatic natural response in which the body attempts to eliminate agents or foreign objects from the oral cavity by muscle contraction at the base of the tongue and the pharyngeal wall (Bassi 2004). Gagging, also known as retching or dental nausea, is a subjective sensation originating at the cortical level.
Although gagging is a natural phenomenon, exaggerated gag reflex is a known hindrance to dental treatment (Kumar 2011). Many dental procedures, such as obtaining maxillary and mandibular impressions, mapping the posterior vibrating line for complete dentures, tooth preparation for various restorative procedures and endodontic treatment in posterior teeth, extraction of third molars, and taking intraoral radiographs especially for the posterior teeth, may cause exaggerated gag reflex (Murthy 2011). A self‐reported gagging study reported 8.2% prevalence among dental patients (Van Houtem 2015). During denture try‐in sessions, the incidence of gagging was reported to be 44% compared to other situations (Bassi 2004; Conny 1983). Saita 2013 reported that gagging‐related problems account for 20% of dental avoidance.
Two main categories of gagging patients have been identified: namely the somatogenic group, where local and systemic disorders, anatomic factors and iatrogenic causes are believed to operate; and the psychogenic group, where psychological factors based on classical and operant conditioning are believed to be causal (Bartlett 1971; Bassi 2004; Conny 1983; Saunders 1997; Wright 1979).
Five regions in the oral cavity have been identified as the major trigger zones for initiating the gag reflex. They are the base of the tongue, fauces, palate, uvula, and posterior pharyngeal wall (Meeker 1986). The trigger zones become more posterior, usually located at the tonsillar pillars after the appearance of the first dentition. When stimulation occurs intraorally, afferent fibres from the trigeminal, glossopharyngeal and vagus nerves pass to the medulla oblongata (Conny 1983; Wright 1979). From here, efferent impulses give rise to spasmodic and unco‐ordinated muscle movements characteristic of gagging. The centre in the medulla oblongata is close to the vomiting, salivary and cardiac centres, which may be stimulated during gagging (Bassi 2004). This explains why gagging may be accompanied by excessive salivation, lacrimation, sweating, fainting or even a panic attack in a minority of patients. Furthermore, neural pathways from the gagging centre to the cerebral cortex allow the reflex to be modified by higher centres (Bassi 2004), thus making it possible to initiate gagging just by imagining a disagreeable experience or conversely by controlling the reflex to some extent by distractive action (Barenboim 2009).
Locally, the gag reflex depends mainly on five types of stimuli.
Acoustic stimuli, which are due to the noise of rotary instruments.
Olfactory/taste stimuli, which may be attributed to the odour or taste of dental materials.
Visual stimuli in which the mere sight of instruments, materials or dental set‐up triggers gag reflex.
Mechanical stimuli, which occur due to dental instruments and materials directly stimulating the trigger zones.
Psychic stimuli, which are initiated by fear and anxiety of the patient either due to a previous unpleasant experience or due to psychological reasons.
Different levels in severity of gagging have been noted. The severity of gagging is assessed by the Gagging Problem Assessment Questionnaire (GPA‐pa SF) (Akarslan 2012; Saita 2013; Van Linden van den Heuvell 2008), Gagging Severity Index (GSI) and the Gagging Prevention Index (GPI) (Dickinson 2005a; Dickinson 2005b; Rosted 2006) (Additional Table 4; Additional Table 5), classification of gagging problem index (CGP) (Elbay 2016) or using a visual analogue scale (VAS) (Bilello 2014), or the depth of swab insertion into the soft palate (Barenboim 2009).
1. Gagging Severity Index (GSI).
| Severity grading | Description |
| Grade I Normal gagging reflex |
Very occasional gagging occurs during high‐risk dental procedures such as maxillary impression taking or restoration to the distal, palatal or lingual surfaces of molar teeth. This is basically a 'normal' gag reflex under difficult treatment circumstances. Generally controlled by the patient |
| Grade II Mild gagging |
Gagging occurs occasionally during routine dental procedures such as fillings, scaling and impressions. Control can usually be regained by the patient, although they may need assistance and reassurance from members of the dental team, and treatment continued. No special measures are generally needed to facilitate routine treatment but may be required for more difficult procedures |
| Grade III Moderate gagging |
Gagging occurs routinely during normal dental procedures. This may include simple physical examination of high‐risk areas such as the lingual aspect of lower molars. Once instigated, control is difficult to regain without cessation of the procedure. Re‐commencement may be difficult. Gagging prevention measures are usually required. The gag may influence treatment planning and may limit treatment options |
| Grade IV Severe gagging |
Gagging occurs with all forms of dental treatment including simple visual examination. Routine treatment is impossible without some form of special measure to attempt to control the gag reflex. Treatment options may be limited and the gagging problem will be a major factor in treatment planning |
| Grade V Very severe gagging |
Gagging occurs easily and may not necessarily require physical intervention to trigger the reflex. The patient's behaviour and dental attendance may be governed by the gagging problem and it will be one of the prime factors when planning treatment. Treatment options may be severely limited. Dental treatment will be impossible to carry out without specific, special treatment for control of the gagging problem |
Quoted from Rosted 2006.
2. Gagging Prevention Index (GPI).
| Prevention grading | Description |
| Grade I Gagging reflex obtunded |
Very occasional gagging occurred during high‐risk dental procedures such as maxillary impression taking or restoration to the distal, palatal or lingual surfaces of molar teeth. This is basically a 'normal' gag reflex under difficult treatment circumstances. Generally controlled by the patient |
| Grade II Partial control |
Partial control of the gag reflex. The proposed treatment was possible but occasional gagging occurred |
| Grade III Partial control |
Partial control of the gag reflex. The proposed treatment was part completed or alternative treatment was carried out. This involved simpler procedures at lower risk of producing gagging. Gagging occurred frequently |
| Grade IV Inadequate control |
Inadequate control of the gag reflex. The proposed treatment was not possible. Some treatment was carried out but only very simple procedures. Gagging occurred regularly |
| Grade V No control |
Failure to control the gag reflex. Gag reflex was so severe that even simple treatment was not possible. No treatment was provided or possible using these gagging control methods |
Quoted from Rosted 2006.
Description of the intervention
The management strategies to prevent gagging include pharmacological and non‐pharmacological techniques.
Pharmacological interventions
Pharmacological agents used to manage gagging act peripherally or centrally. Peripherally‐acting agents are topical and local anaesthetics. Centrally‐acting agents are categorised as antihistamines, sedatives, tranquillisers, parasympatholytics, and central nervous system depressants (Murthy 2011).
Non‐pharmacological interventions
Non‐pharmacological interventions include behavioural modification and other interventions including acupressure, acupuncture, transcutaneous electric nerve stimulation (TENS), using salt on the tip of the tongue, prosthetic devices, laser stimulation, and ear plug technique (Bassi 2004; Lu 2000; Ramsay 1987). Some combination therapies like hypnopuncture were also tried (Eitner 2005).
How the intervention might work
Pharmacological interventions
Pharmacological interventions include peripherally‐acting and centrally‐acting agents.
Peripherally‐acting agents
These include.
Local anaesthetic sprays, gels, lozenges, mouthrinses, or injection.
Herbal preparations with local anaesthetic properties, such as Elaeagnus angustifolia lozenges or films.
Glossopharyngeal nerve block.
Some study authors have criticised the use of topical or local anaesthesia for gagging but proponents suggest that if the mucosal surfaces particularly of the soft palate are desensitised, the patient is less likely to gag (Kramer 1977).
It has been demonstrated that tannin in herbal drugs has an anaesthetic function on the mucosa of the oral cavity. A study reported that Elaeagnus angustifolia reduced gagging because of high tannin content which has a local anaesthetic action (Bhat 2006). It also has a muscle‐relaxant effect similar to that of 1 mg/kg diazepam (Hosseinzadeh 2003).
Several study authors have tried glossopharyngeal nerve block to reduce the gagging sensation (Murthy 2011).
Centrally‐acting agents
These include.
Trimethobenzamide.
5‐HT3 antagonists: palonosetron, dolasetron, granisetron, and tropisetron.
Conscious sedation using nitrous oxide sedation (Kaufman 1988), benzodiazapine (Yamashiro 1995), propofol (Yoshida 2007; Yoshida 2009) or intravenous propofol‐remifentanil (Shin 2017).
General anaesthesia: a minority of patients do not respond to any form of sedation or behavioural therapy, and dental treatment under general anaesthesia may be appropriate as a last resort (Bassi 2004).
The mechanism of action of trimethobenzamide is obscure, but may involve the chemoreceptor trigger zone (CTZ), an area in the medulla oblongata through which emetic impulses are conveyed to the vomiting centre (Grace 1963).
5‐HT3 antagonists are given enterally or parenterally and influence the peripheral and central nervous system for prevention of emesis (vomiting). Their primary use is in preventing nausea and emesis during antineoplastic treatment or post‐surgery, yet some are experimented for their anti‐gagging property so that they can be used for dental patients (Barenboim 2009).
The use of conscious sedation using inhalation anaesthetics, such as nitrous oxide, is an attractive alternative for relatively mild gagging as it does not cause venous injury in the forearm. It has low frequency of other adverse effects, such as respiratory distress and airway blockage, and is accompanied by vomiting and nausea in no more than 6% of cases (Allen 2006; Bassi 2004; Kaufman 1988). Other agents used for conscious sedation include benzodiazepines (Yamashiro 1995) and propofol (Yoshida 2007).
General anaesthesia is beneficial for severely retching patients who cannot tolerate dental care under conscious sedation (Bassi 2004).
Non‐pharmacological interventions
Behavioural modification
These are the most commonly used non‐pharmacological interventions in a clinical scenario. Exaggerated gagging or an extended period of gagging in the absence of a normal stimulus is usually considered as a learned response and therefore amenable to behavioural modification (Ramsay 1987). Generally, the ultimate goal is to make routine dental care possible by reducing anxiety and helping people who gag during dental treatment 'unlearn' the behaviour that leads to gagging (Ramsay 1987; Wilks 1983). Therefore, the management strategies have focused on behaviour modification techniques, namely.
Relaxation techniques: help by reducing the anxiety state and enabling the patient to override unhelpful thought processes (Bassi 2004).
Distraction techniques: temporarily divert the patient's attention and allow to perform minor dental procedures while the mind is dissociated from a potentially distressing situation (Hoad‐Reddick 1986; Kovats 1971; Krol 1963).
Suggestion and hypnosis: help to relax the patient and temporarily remove or ameliorate the gag reflex to allow dental treatment to be performed (Barsby 1994; Neumann 2001; Noble 2002; Ramazani 2016; Robb 1996; Zach 1989).
Systemic desensitisation: aims at re‐educating the patients by asking them to place an object in the mouth for a period of time. Toothbrush, radiograph, impression tray, marbles, acrylic discs, buttons, dentures, and training devices have been used to help patients overcome the gagging problem by desensitisation prior to dental procedure (Singer 1973).
Errorless learning: is based on the principles of systematic desensitisation to help patients use 'successive approximations' to increasingly tolerate graduated insertions of dental prostheses into the mouth (Foster 1985).
Cognitive behavioural therapy: aims to address cognitive distortions in patient fears of dental procedures that increase their sensitivity to gag (Barsby 1997).
Other non‐pharmacological interventions
Salt: some advocate the use of salt on the tip of the tongue. Salt stimulates the taste buds located in the anterior part of tongue subsequently activating the chorda tympani nerve and finally leading to inactivation of the gag reflex (Chidiac 2001).
Transcutaneous electric nerve stimulation (TENS): it utilises a preventive approach in which sensory stimulation of the cranial nerves of the superior laryngeal nerve branch (cranial nerve IX, pharyngeal branch of X, cranial nerve V, and cranial nerve X) block the physiological response of retching (Morrish 1997).
Acupressure: stimulation using acupressure at the sixth point on the Chinese pericardial meridian (Pericardium 6, PC6, or P6 point, also called Neiguan or Neikuan; English translation ‐ Inner gate), a point located three‐finger breadths below the wrist on the inner forearm in between the two tendons (Figure 1) has been reported to be effective in preventing nausea and vomiting (Ezzo 2006; Lu 2000). This point is situated on the palmar aspect of the forearm, 2 cm above the transverse crease of the wrist, on the line connecting PC3 and PC7, between the tendons of musculus palmaris longus and musculus flexor carpi radialis (Cyber 2015). Acupressure at the Conception Vessel 24 point (CV24; also called the Chengjiang or REN‐24 point) on the labio‐mental fold on the chin, has also been shown to decrease gag reflex during maxillary impression procedures (Rosted 2006; Vachiramon 2002).
Acupuncture: P6 stimulation particularly using electroacupuncture has been found to be effective for antiemesis (Rosted 2006; Vickers 1996).
Laser stimulation: red light soft magnetic field laser stimulation of the soft palate has been used to reduce the sensitivity of the soft palate (Sari 2010). Low‐level laser therapy on P6 acupoint was also used to control gag reflex in children to make it painless and for better patient compliance (Goel 2017).
Prosthetic management of gagging: by using palateless dentures (Farmer 1984; Jain 2013), reducing the extension of dentures (Hotta 2012), palateless custom bar overdentures (Singh 2012), prosthetic training devices (Yadav 2011), or use of correct impression trays and correct consistency of impression material (Farrier 2011).
Ear plug technique: in this technique the ear plug acts as an external auditory canal stimulator to suppress the profound gag reflex (Cakmak 2014).
Temple tap: is a digital stimulation of the tempoparietal suture that is given along with suggestion to control swallowing reflex (Boitel 1984).
1.
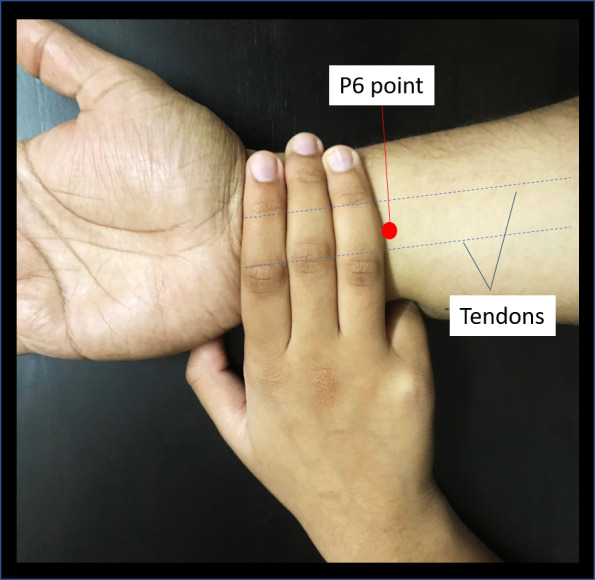
Pericardium 6 or P6 point.
Combination interventions
Hypnopuncture: a combination therapy of hypnosis and acupuncture has also been tried to reduce distinctive gag reflex. Acupuncture was done at Chengjiang REN‐24 point and anti‐gag point located on the upper part of the ear between concha and triangular fossa. Acupuncture addresses a short‐term depression of the gag reflex and hypnosis aims at long‐term therapeutic effect (Eitner 2005).
Why it is important to do this review
The previously published version of this Cochrane Review (Prashanti 2015) found very low‐quality evidence from a single trial that was insufficient to conclude if there was any benefit of acupuncture in reducing gagging and allowing successful completion of dental procedures. Considering the different complex interventions available to treat gagging in dental patients, it is important to identify the best intervention strategies. This will help clinicians to treat patients with gagging efficiently and improve patient comfort during treatment. This review update will allow us to identify the current evidence regarding management strategies for gagging during dental procedures and also impact the implementation of different approaches and trigger the development of new interventions. A review update on this topic is needed since interventions of questionable effectiveness and unclear consequences might be in use.
Objectives
To assess the effects of pharmacological and non‐pharmacological interventions for the management of gagging in people undergoing dental treatment.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) with either a pharmacological or non‐pharmacological intervention in this Cochrane Review. We excluded quasi‐RCTs.
Types of participants
People above the age of four years who were classified as having gagging of any degree of severity (and assessed by any means) that interfered with dental treatment.
We excluded trials including the following participants.
People who have undergone an intervention that can change the anatomy permanently (e.g. surgery).
People using any systemic medications that might interfere with the interventional drug or reduce the gag reflex.
People with any type of central or peripheral nervous system disorders.
People with oral lesions that might reduce/enhance the gag sensation (e.g. oral submucous fibrosis, tumour).
Types of interventions
Any pharmacological or non‐pharmacological intervention compared to placebo, or to no intervention, or to another intervention, given alone or in combination.
Types of outcome measures
Primary outcomes
Successful and comfortable completion of the dental treatment without any gagging problem.
Secondary outcomes
Reduction in gagging measured by any scale/method and assessed by either operator, patient or both.
Presence or absence of gagging measured by any scale/method and assessed by either operator, patient or both.
Adverse effects: adverse effects related to the intervention, e.g. adverse drug reactions or adverse reactions to acupuncture.
Search methods for identification of studies
Electronic searches
Cochrane Oral Health's Information Specialist conducted systematic searches in the following databases for randomised controlled trials and controlled clinical trials. There were no language, publication year or publication status restrictions.
Cochrane Oral Health's Trials Register (searched 18 March 2019) (Appendix 1);
Cochrane Central Register of Controlled Trials (CENTRAL; 2019, Issue 2) in the Cochrane Library (searched 18 March 2019) (Appendix 2);
MEDLINE Ovid (1946 to 18 March 2019) (Appendix 3);
Embase Ovid (1980 to 18 March 2019) (Appendix 4);
CINAHL EBSCO (Cumulative Index to Nursing and Allied Health Literature; 1937 to 18 March 2019) (Appendix 5);
AMED Ovid (Allied and Complementary Medicine; from 1985 to 18 March 2019) (Appendix 6).
Subject strategies were modelled on the search strategy designed for MEDLINE Ovid. Where appropriate, they were combined with subject strategy adaptations of the highly sensitive search strategy designed by Cochrane for identifying randomised controlled trials and controlled clinical trials as described in the Cochrane Handbook for Systematic Reviews of Interventions Chapter 6 (Lefebvre 2011).
Searching other resources
Cochrane Oral Health's Information Specialist searched the International Association for Dental Research\American Association for Dental Research Conference Proceedings (Appendix 7) on 18 March 2019.
The following databases were searched for ongoing trials:
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (clinicaltrials.gov; searched 18 March 2019) (Appendix 8);
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch; searched 18 March 2019) (Appendix 9).
We checked the reference lists of included studies to identify any further additional studies. Authors of the included studies were contacted for relevant unpublished material.
We searched Google Scholar with forward citation searching using the author names in the Included studies, Excluded studies, Ongoing studies, and Studies awaiting classification.
We checked that none of the included studies in this review were retracted due to error or fraud.
We did not perform a separate search for adverse effects of interventions used, we considered adverse effects described in included studies only.
For a previous version of this review, we searched the metaRegister of Controlled Trials (mRCT) (Appendix 10) and the International Federation of Pharmaceutical Manufacturers & Associations (IFPMA) Clinical Trials Portal (Appendix 11). These resources are no longer available.
Data collection and analysis
Selection of studies
Two review authors (Sumanth Kumbargere Nagraj (SKN) and Renjith George (RG)) independently screened the titles and abstracts from the electronic searches to identify potentially eligible studies. The search was designed to be sensitive and include controlled clinical trials, these were filtered out early in the selection process if they were not randomised. We obtained full‐text copies of all eligible and potentially eligible studies and these two review authors further evaluated the studies for inclusion. We recorded any reasons why studies did not meet the inclusion criteria in the Characteristics of excluded studies table. We resolved any disagreements by discussion. When resolution was not possible, we consulted the arbiter (Prashanti Eachempati (PE)). Articles in languages other than English were assessed by their abstracts where possible and if they appeared to be potentially eligible, we obtained and translated the full‐text article.
Data extraction and management
Two review authors (RG and Salian Kiran Kumar Krishanappa (SKKK)) extracted the data independently, using a data extraction form specifically designed for this Cochrane Review. We resolved any disagreements by discussion. Two review authors (SKKK and PE) independently checked data extraction forms obtained from translators and cross checked any doubtful aspects using Google translator. We entered all the study details in the Characteristics of included studies table in Review Manager 2014.
We recorded the following details for each included trial.
Publication details (e.g. year of publication and language).
Demographic details of the report.
Inclusion and exclusion criteria.
Sample size, method of randomisation, allocation concealment, blinding, type of trial, method of assessing the outcome, and dropouts if any.
Type of intervention.
Details of the outcome reported.
Duration of follow‐up.
Results of the intervention.
Funding details.
Details about trials registration.
For obtaining additional data and clarifications, we contacted the authors of the included and excluded trials via email.
Assessment of risk of bias in included studies
We independently assessed the risk of bias in the included trials for seven domains: sequence generation, allocation concealment, performance bias and detection bias, incomplete outcome data, selective outcome reporting, and other biases. For each of these components, we assigned a judgement regarding the risk of bias as either 'high', 'low' or 'unclear', based on guidance in Higgins 2011. We contacted the trial authors if details were missing in the publications or were unclear. We resolved disagreements through consensus. We recorded our judgements and justifications in 'Risk of bias' tables for each included study and generated a 'Risk of bias' summary figure. We used these judgements while grading of the overall certainty of the evidence for outcomes in the 'Summary of findings' tables for each comparison.
We summarised the risk of bias according to Higgins 2011 as follows.
| Risk of bias | Interpretation | In outcome | In included studies |
| Low | Plausible bias unlikely to seriously alter the results | Low risk of bias for all key domains | Most information is from studies at low risk of bias |
| Unclear | Plausible bias that raises some doubt about the results | Unclear risk of bias for one or more key domains | Most information is from studies at low or unclear risk of bias |
| High | Plausible bias that seriously weakens confidence in the results | High risk of bias for one or more key domains | The proportion of information from studies at high risk of bias is sufficient to affect the interpretation of results |
Measures of treatment effect
For dichotomous data in parallel‐group studies, we used risk ratios (RRs), and for continuous data, we assessed the mean difference (MD). For split‐mouth and cross‐over studies, we calculated odds ratios (ORs) for the dichotomous data using the Becker‐Balagtas method (BB OR) outlined in Curtin 2002 by R software version 3.3.1 (R ‐ 3.3.1 for Windows). We chose this method because we intended to pool data from cross‐over or split‐mouth and parallel‐group studies in the same meta‐analyses, and this method facilitated data synthesis (as outlined by Stedman 2011). If a split‐mouth study presented data only in marginals (as parallel‐group studies, not as 2 x 2 cross‐classification for paired data), we chose the conservative intraclass correlation coefficient (ICC) 0.5. Ordinal scale was converted into dichotomous data.
Unit of analysis issues
The participant was the unit of analysis in parallel‐group studies. One split‐mouth trial (Elbay 2016 ) and one cross‐over trial (Goel 2017) were included, and the two sides of the mouth, or two periods were used in the analysis as described above. We did not find any cluster‐RCTs. No other unit of analysis issues were present.
Dealing with missing data
We attempted to obtain missing data by contacting trial authors. One trial author responded to our queries. One of the included trials did not give standard deviation (SD) values. Based on the sample size and P value, we calculated the t values. Based on t values, we calculated the standard error. Based on standard error, we calculated the standard deviation (Higgins 2011, Section 7.7.3.3).
Assessment of heterogeneity
We assessed heterogeneity by examining the forest plots to check for overlapping confidence intervals (CIs), using the Chi2 test for heterogeneity with a 10% level of significance to detect inconsistency in study results that were not due to random error (chance), and the I2 statistic to denote the percentage of inconsistency in results due to inter‐trial variability that exceeded chance. We planned to interpret I2 values between 0% to 40% as possibly insignificant, 30% to 60% as possibly significant, 50% to 90% as possibly substantial, and 75% to 100% as possibly very substantial ('considerable'); depending on whether the inconsistency in results was due to differences in the direction of effect estimates between trials rather than due to differences in the magnitude of effect estimates favouring an intervention; as well as the strength of the evidence for heterogeneity from the P value for the Chi2 test for heterogeneity (Deeks 2011).
Assessment of reporting biases
We did not attempt to assess for funnel plot asymmetry as there was an insufficient number of trials included in any meta‐analysis.
Data synthesis
We used the fixed‐effect model using the Mantel‐Haenszel method to derive RRs or MDs. For the split‐mouth and cross‐over trials, the pairing of data was undertaken as described in the Measures of treatment effect section, and the generic inverse variance method was used.
Subgroup analysis and investigation of heterogeneity
We did not conduct any subgroup analysis as there were only single included trials for each comparison except for acupuncture at P6 versus sham acupuncture where two trials were analysed for a single outcome (completion of dental procedure).
Sensitivity analysis
We planned to undertake sensitivity analyses to exclude data from trials at high risk of bias and unclear risk of bias. However, there were insufficient studies.
Summarising findings and assessing the certainty of the evidence
We used the GRADE approach to interpret findings. We used GRADE 2015 and imported data from Review Manager 2014 to create 'Summary of findings' tables for the comparisons included in this review. The table provides information concerning the overall certainty of the evidence from the trials, the magnitude of effect of the interventions examined and the sum of available data on the primary and secondary outcomes. The GRADE approach considers 'certainty' to be a judgement of the extent to which we can be confident that the estimates of effect are correct. Evidence from randomised controlled studies is initially graded as high and downgraded by one, two or three levels on each of five domains after full consideration of limitations in the design of the studies, the directness (or applicability) of the evidence, the consistency and precision of the results, and the possibility of publication bias. A GRADE certainty level of 'high' reflects confidence that the true effect lies close to that of the estimate of the effect for an outcome. A judgement of 'moderate' certainty indicates that the true effect is likely to be close to the estimate of the effect, but acknowledges the possibility that it could be substantially different. 'Low' and 'very low' certainty evidence limit our confidence in the effect estimate (Balshem 2011).
Results
Description of studies
See Characteristics of included studies, Characteristics of excluded studies and Characteristics of studies awaiting classification.
Results of the search
The electronic search strategies identified 390 records from English and other language databases. We had 263 records after de‐duplication. We discarded 232 records after screening the abstracts as they were irrelevant and requested full‐text copies of 31 studies. From the 31 studies, we excluded 18 as they were not randomised controlled trials (RCTs). We assessed the remaining 13 studies for eligibility. From these, we excluded four studies with reasons. Five studies await further classification. Four RCTs met the inclusion criteria of this review. See Figure 2 for the selection process.
2.
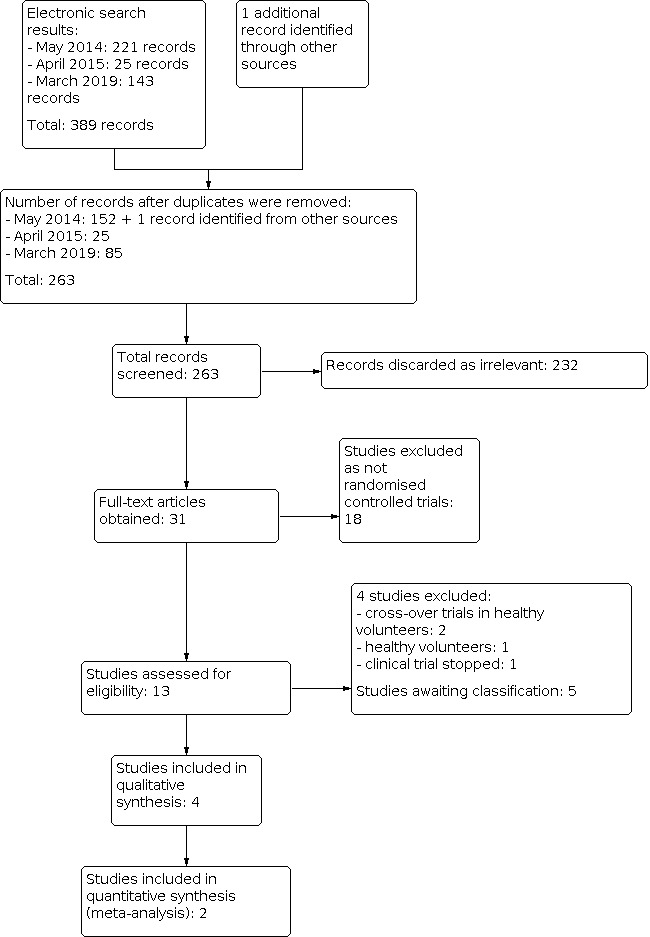
Study flow diagram.
Included studies
See the Characteristics of included studies table for further details.
Characteristics of trial settings
Trial design
All the four included trials were single‐centre trials. Two trials were of parallel‐group design (Lu 2000; Zotelli 2014). Elbay 2016 was a split‐mouth trial and Goel 2017 was a cross‐over trial. The trials were conducted in USA (Lu 2000), Brazil (Zotelli 2014), Turkey (Elbay 2016) and India (Goel 2017). None of the trials mentioned sources of funding.
Characteristics of participants
Consenting participants who reported previous unpleasant nausea during dental procedures that hindered or prevented the dental treatment from being carried out properly were recruited in all the trials. Lu 2000 and Zotelli 2014 included adults whereas Elbay 2016 and Goel 2017 included children.
Characteristics of the interventions
Lu 2000 included multiple interventions using acupuncture at P6 and acupressure with thumb pressure, device, sea band with and without sedation. For impressions, five‐minute stimulation and for other dental procedures, three‐minute stimulation were done during and prior to procedure. Zotelli 2014 also evaluated the effects of acupuncture at P6 point versus non‐penetrating sham acupuncture with a duration of 20 minutes. Elbay 2016 and Goel 2017 compared laser therapy at P6 point versus no laser with the former having a cross‐over design with a 30‐minute washout period.
Outcomes
Lu 2000 and Zotelli 2014 reported both successful completion of dental procedure and reduction in gagging. Lu 2000 reported data in an ordinal scale (excellent, good, fair, poor) which we converted into dichotomous data, whereas Zotelli 2014 reported the Gagging Severity Index (GSI), Gagging Prevention Index (GPI) and visual analogue scale (VAS). Elbay 2016 reported reduction in gagging (leading to completion of dental procedure) using the gagging severity score. Goel 2017 reported the presence or absence of gagging during maxillary impression‐making with dichotomous data.
Excluded studies
We excluded four studies for the reasons listed in the Characteristics of excluded studies section. Of these excluded trials, one trial randomised healthy volunteers (Ranjbaran 2011) and two had randomised healthy volunteers in their cross‐over trials (Barenboim 2009; NCT00502437). One clinical trial status shows that it has stopped (ISRCTN66117475).
Studies awaiting classification
Five trials currently await classification (see Characteristics of studies awaiting classification).
One clinical trial (NCT02938364) is from Saudi Arabia and compared ear plugs versus acupressure at P6 point. We could not find the published version of this trial.
One trial was conducted in Iran (Rahshenas 2015). The patients were divided into three groups: control (without palpation), case group 1 (with palpation of the palm pressure point), case group 2 (with palpation and pressing the palm pressure point). Only the abstract of this trial is available and the randomisation procedure is unclear.
Three studies from Iran (Hekmatian 2011a; Hekmatian 2011b; Hekmatian 2012) compared E angustifolia film, pomegranate peel extract, and E angustifolia lozenges with placebo, respectively. The nature of the participants and the randomisation procedure are unclear in these studies and we were unable to obtain additional information or clarifications from the trial authors despite our attempts to contact them.
Risk of bias in included studies
The overall risk of bias was unclear for all included studies (Figure 3).
3.

'Risk of bias' summary: review authors' judgements about each 'Risk of bias' item.
Allocation
Sequence generation
We judged two of the included trials, Elbay 2016 and Zotelli 2014, to be at low risk as the random allocation sequence was generated using a computer generated list and internet‐based program respectively. The other two trials, Goel 2017 and Lu 2000, were at unclear risk of bias as they did not report the method of randomisation.
Allocation concealment
All four trials did not describe the method of allocation concealment and hence we judged them as being at unclear risk of bias.
Blinding
Elbay 2016 and Zotelli 2014 were at low risk of performance and detection bias. Elbay 2016 simulated laser application using a non‐working laser for the control radiograph to ensure blinding. In Zotelli 2014, the acupuncture points were concealed from investigators by a disposable blue sheet and two researchers performed acupuncture and impression‐taking and nausea assessment independently. The participants were unaware of the group to which they belonged. The other two trials, Goel 2017 and Lu 2000, were at unclear risk of bias as they did not report the method of blinding.
Incomplete outcome data
Three trials Elbay 2016, Goel 2017 and Zotelli 2014 were at low risk of attrition bias as outcomes were reported for all randomised participants. Lu 2000 had unclear attrition bias as it did not report the exact number randomised.
Selective reporting
All four included trials were at low risk of reporting bias as all outcomes described were reported and conclusions were in accordance with the results.
Other potential sources of bias
No other potential biases which could influence the results were identified. We assessed Elbay 2016 and Goel 2017 as at unclear risk of other bias as we could not be certain regarding the carry‐over effect of the laser treatment.
Effects of interventions
See: Table 1; Table 2; Table 3
Acupuncture with or without sedation for gagging in patients undergoing dental treatment
Acupuncture at P6 point versus sham acupuncture
Successful completion of dental treatment
Acupuncture at P6 (point located three‐finger breadths below the wrist on the inner forearm in between the two tendons) showed successful completion of dental procedure in comparison to sham acupuncture (risk ratio (RR) 1.78, 95% confidence interval (CI) 1.05 to 3.01; two trials, 59 participants; Analysis 1.1; Figure 4) (Lu 2000; Zotelli 2014).
1.1. Analysis.

Comparison 1: Acupuncture at P6 point versus sham acupuncture, Outcome 1: Successful completion of dental procedure
4.

Forest plot of comparison: 1 Acupuncture at P6 point versus sham acupuncture, outcome: 1.1 Successful completion of dental procedure.
Reduction in gagging
Assessor‐reported outcome ‐ treatment effectiveness in controlling nausea
Acupuncture at P6 showed no clear difference in reducing the gagging sensation when compared to sham acupuncture in all three stages: stage 1 mean difference (MD) 0.40, 95% CI ‐0.12 to 0.93; stage 2 MD 0.49, 95% CI ‐0.26 to 1.24; and stage 3 MD 0.67, 95% CI ‐0.18 to 1.53 (one trial, 33 participants; Analysis 1.2) (Zotelli 2014).
1.2. Analysis.

Comparison 1: Acupuncture at P6 point versus sham acupuncture, Outcome 2: Reduction in gagging (reported by assessor ‐ treatment effectiveness)
Patient‐reported outcome (visual analogue scale (VAS))
Acupuncture at P6 showed no clear difference in reducing gagging when compared to sham acupuncture (MD 0.86, 95% CI ‐1.13 to 2.85; one trial, 33 participants; Analysis 1.3) (Zotelli 2014).
1.3. Analysis.

Comparison 1: Acupuncture at P6 point versus sham acupuncture, Outcome 3: Reduction in gagging (reported by patient ‐ VAS)
Patient‐reported outcome (ordinal scale converted to dichotomous)
Acupuncture at P6 showed clear difference in reducing gagging when compared to sham acupuncture (RR 2.57, 95% CI 1.12 to 5.89; one trial, 26 participants; Analysis 1.4) (Lu 2000).
1.4. Analysis.

Comparison 1: Acupuncture at P6 point versus sham acupuncture, Outcome 4: Reduction in gagging (reported by patient ‐ dichotomous data)
Presence or absence of gagging
None of the trials reported this outcome.
Adverse effects
Zotelli 2014 reported that one participant in the control group reported increased sweating; however, it was unclear if this was an adverse event or was due to fear of needles. Lu 2000 did not report any adverse events.
Acupuncture at P6 point with sedation versus sham acupuncture with sedation
Successful completion of dental treatment
Acupuncture at P6 with sedation showed no clear difference in completing dental procedure when compared to dummy acupuncture with sedation (RR 1.08, 95% CI 0.91 to 1.28; one trial, 34 participants; Analysis 2.1) (Lu 2000).
2.1. Analysis.

Comparison 2: Acupuncture + sedation versus sham acupuncture, Outcome 1: Completion of dental procedure
Reduction in gagging
Patient‐reported outcome (ordinal scale converted to dichotomous)
Acupuncture at P6 with sedation showed no clear difference in reducing gagging when compared to dummy acupuncture with sedation (RR 1.09, 95% CI 0.87 to 1.37; one trial, 34 participants; Analysis 2.2) (Lu 2000).
2.2. Analysis.

Comparison 2: Acupuncture + sedation versus sham acupuncture, Outcome 2: Reduction in gagging (reported by patient)
Presence or absence of gagging
None of the trials reported this outcome.
Adverse effects
Lu 2000 did not report any adverse events.
Acupressure with thumb, device, or sea band compared to sham acupressure with or without sedation for gagging in patients undergoing dental treatment
None of the trials reported on presence or absence of gagging or adverse effects.
Acupressure at P6 point with thumb versus sham acupressure
Successful completion of dental treatment
Acupressure at P6 with thumb showed no clear difference in completing dental procedure when compared to dummy acupressure (RR 0.85, 95% CI 0.50 to 1.46; one trial, 30 participants; Analysis 3.1) (Lu 2000).
3.1. Analysis.

Comparison 3: Acupressure with thumb versus sham acupressure, Outcome 1: Successful completion of dental procedure
Reduction in gagging
Patient‐reported outcome (ordinal scale converted to dichotomous)
Acupressure at P6 with thumb showed no clear difference in reducing gagging when compared to dummy acupressure (RR 0.92, 95% CI 0.60 to 1.41; one trial, 30 participants; Analysis 3.2) (Lu 2000).
3.2. Analysis.

Comparison 3: Acupressure with thumb versus sham acupressure, Outcome 2: Reduction in gagging (reported by patient)
Acupressure at P6 point with device versus sham acupressure
Successful completion of dental treatment
Acupressure at P6 with device showed a difference in completing dental procedure when compared to dummy acupressure (RR 2.63, 95% CI 1.33 to 5.18; one trial, 34 participants; Analysis 4.1; Figure 5) (Lu 2000).
4.1. Analysis.

Comparison 4: Acupressure with device versus sham acupressure, Outcome 1: Successful completion of dental procedure
5.

Forest plot of comparison: 4 Acupressure with device versus sham acupressure, outcome: 4.1 Successful completion of dental procedure.
Reduction in gagging
Patient‐reported outcome (ordinal scale converted to dichotomous)
Acupressure at P6 with device showed a difference in reducing gagging when compared to dummy acupressure (RR 3.94, 95% CI 1.63 to 9.53; one trial, 34 participants; Analysis 4.2) (Lu 2000).
4.2. Analysis.

Comparison 4: Acupressure with device versus sham acupressure, Outcome 2: Reduction in gagging (reported by patient)
Acupressure at P6 point with sea band versus sham acupressure
Successful completion of dental treatment
Acupressure at P6 with sea band showed no clear difference in completing dental procedure when compared to dummy acupressure (RR 1.80, 95% CI 0.63 to 5.16; one trial, 19 participants; Analysis 5.1) (Lu 2000).
5.1. Analysis.

Comparison 5: Acupressure with sea band versus sham acupressure, Outcome 1: Successful completion of dental procedure
Reduction in gagging
Patient‐reported outcome (ordinal scale converted to dichotomous)
Acupressure at P6 with sea band showed no clear difference in reducing gagging when compared to dummy acupressure (RR 2.70, 95% CI 0.72 to 10.14; one trial, 19 participants; Analysis 5.2) (Lu 2000).
5.2. Analysis.

Comparison 5: Acupressure with sea band versus sham acupressure, Outcome 2: Reduction in gagging (reported by patient)
Acupressure at P6 point with thumb with sedation versus sham acupressure with sedation
Successful completion of dental treatment
Acupressure at P6 with thumb plus sedation showed no clear difference in completing dental procedure when compared to dummy acupressure (RR 0.96, 95% CI 0.84 to 1.10; one trial, 39 participants; Analysis 6.1) (Lu 2000).
6.1. Analysis.

Comparison 6: Acupressure with thumb + sedation versus sham + sedation, Outcome 1: Successful completion of dental procedure
Reduction in gagging
Patient‐reported outcome (ordinal scale converted to dichotomous)
Acupressure at P6 with thumb plus sedation showed no clear difference in reducing gagging when compared to dummy acupressure (RR 1.06, 95% CI 0.92 to 1.23; one trial, 39 participants; Analysis 6.2) (Lu 2000).
6.2. Analysis.

Comparison 6: Acupressure with thumb + sedation versus sham + sedation, Outcome 2: Reduction in gagging
Acupressure at P6 point with device with sedation versus sham acupressure with sedation
Successful completion of dental treatment
Acupressure at P6 with device plus sedation showed no clear difference in completing dental procedure when compared to dummy acupressure (RR 1.16, 95% CI 0.90 to 1.48; one trial, 27 participants; Analysis 7.1) (Lu 2000).
7.1. Analysis.

Comparison 7: Acupressure with device + sedation versus sham + sedation, Outcome 1: Completion of dental procedure
Reduction in gagging
Patient‐reported outcome (ordinal scale converted to dichotomous)
Acupressure at P6 with device plus sedation showed no clear difference in reducing gagging when compared to dummy acupressure (RR 1.26, 95% CI 0.93 to 1.69; one trial, 27 participants; Analysis 7.2) (Lu 2000).
7.2. Analysis.

Comparison 7: Acupressure with device + sedation versus sham + sedation, Outcome 2: Reduction in gagging (reported by patient)
Acupressure at P6 point with sea band with sedation versus sham acupressure with sedation
Successful completion of dental treatment
Acupressure at P6 with sea band plus sedation showed no clear difference in completing dental procedure when compared to dummy acupressure (RR 0.88, 95% CI 0.67 to 1.17; one trial, 21 participants; Analysis 8.1) (Lu 2000).
8.1. Analysis.

Comparison 8: Acupressure with sea band + sedation versus sham + sedation, Outcome 1: Completion of dental procedure
Reduction in gagging
Patient‐reported outcome (ordinal scale converted to dichotomous)
Acupressure at P6 with sea band plus sedation showed no clear difference in reducing gagging when compared to dummy acupressure (RR 0.88, 95% CI 0.67 to 1.17; one trial, 21 participants; Analysis 8.2) (Lu 2000).
8.2. Analysis.

Comparison 8: Acupressure with sea band + sedation versus sham + sedation, Outcome 2: Reduction in gagging
Laser for gagging in patients undergoing dental treatment
None of the trials reported on completion of dental treatment or adverse effects.
Laser at P6 point versus control
Presence of absence of gagging
Laser at P6 showed a difference in absence of gagging during dental procedure when compared to dummy laser application for control group (odds ratio (OR) 86.33, 95% CI 29.41 to 253.45; one trial, 40 participants; Analysis 9.1; Figure 6) (Goel 2017).
9.1. Analysis.

Comparison 9: Laser versus control, Outcome 1: Presence or absence of gagging
6.

Forest plot of comparison: 9 Laser versus control, outcome: 9.1 Presence or absence of gagging.
Reduction in gagging
Assessor‐reported outcome
Low‐level laser at P6 showed a difference in reducing gagging when compared to dummy laser application for control group (MD 1.80, 95% CI 1.53 to 2.07; one trial, 25 participants; Analysis 9.2) (Elbay 2016).
9.2. Analysis.

Comparison 9: Laser versus control, Outcome 2: Reduction in gagging
Discussion
Summary of main results
Our main objective was to assess the effects of pharmacological and non‐pharmacological interventions for managing gagging in people undergoing dental treatment. We included four trials assessed as at unclear risk of bias. Lu 2000 compared acupuncture and acupressure (with thumb, device, or sea band) at P6 point (point located three‐finger breadths below the wrist on the inner forearm in between the two tendons) to sham acupuncture and acupressure (Lu 2000). This trial also studied the effects of adding sedation to both the intervention and control groups. Zotelli 2014 compared acupuncture at P6 point to sham acupuncture. Both trials reported on completion of dental treatment and reduction in gagging (assessor and patient reported) as their outcomes. Two other trials (Elbay 2016; Goel 2017) studied the effects of laser therapy at P6 point compared to control. Elbay 2016, a cross‐over trial, reported reduction in gagging as an outcome whereas Goel 2017, a split‐mouth study, reported presence or absence of gagging during dental procedure. Except Zotelli 2014, none of the trials reported adverse events. Even in Zotelli 2014 the authors were unsure whether the reported adverse event was due to anxiety of the participant or due to the intervention. Hence we did not consider this in our review. We assessed the certainty of the evidence as very low using GRADE 2015, which incorporates limitations in study design, the directness of the evidence, the consistency of results, the precision of estimates, and the risk of publication bias.
The main results of this Cochrane Review are.
Acupuncture at P6 point versus sham acupuncture with or without sedation
Acupuncture at P6 point showed successful completion of dental treatment and reduction in gagging when compared to sham acupuncture. The same intervention with sedation did not show a difference. We are uncertain whether acupuncture at P6 point is effective in managing gagging as the certainty of the evidence has been assessed as very low (Table 1).
Acupressure with thumb, device, or sea band compared to sham acupressure with or without sedation
Acupressure with thumb or sea band at P6 point with or without sedation did not show any difference when compared to sham acupressure. Acupressure at P6 point with device showed a difference in completing dental treatment and reduction in gagging. Acupressure at P6 point with device and sedation did not show a difference when compared to sham acupressure with sedation. We assessed the certainty of the evidence as very low (Table 2).
Laser at P6 point versus control
Laser at P6 point showed a difference in absence of gagging and a reduction in gagging during dental treatment when compared to sham laser application. However, we are uncertain whether laser at P6 point is effective as the certainty of the evidence has been assessed as very low (Table 3).
Overall completeness and applicability of evidence
Completeness
We systematically searched for trials according to the methodology written in the protocol. We did an independent Google scholar search for other systematic reviews on interventions for gagging and checked all cross references of included articles to be sure that we did not miss any article. Two pairs of review authors extracted data in duplicate. Trials, which were not included in the meta‐analysis were qualitatively explained. We included all interventions including interventions to manage gagging in patients undergoing dental treatment from the age of 4 to 76. All clinically relevant outcomes of interest were analysed. We did not find sufficient trials with adequate numbers of people from different age groups.
We did not exclude any trial due to missing data. When mean and standard error (SE) were given, we calculated the standard deviation (SD) according to guidance given in the Cochrane Handbook for Systematic Reviews of Interventions Section 7.7.3.3 (Higgins 2011). We used the generic inverse variance method for the dichotomous data of a cross‐over trial and the continuous data of a split‐mouth trial. We calculated SE for these trials using the conservative intraclass correlation coefficient (ICC) value of 0.5.
Behavioural modification techniques are often considered the most successful method for managing gagging in dental practice (Ramsay 1987). However, we did not identify any trials evaluating behavioural modification techniques to control gagging. We are unaware of any ongoing trials assessing any of the interventions proposed or commonly used to manage gagging, particularly behavioural approaches. The evidence base is thus incomplete and insufficient to draw robust conclusions on the most effective intervention for the management of gagging for people undergoing dental treatment.
Applicability
The results obtained from this Cochrane Review are insufficient to determine whether or not acupuncture or acupressure with and without sedation, or laser at P6 may be effective in reducing gagging and successfully completing dental procedures. In the included trials, acupuncture, acupressure and laser stimulation were provided by clinicians trained and skilled in the procedure. Even if their efficacy is confirmed in future trials, it is uncertain if interventions provided by the average dental practitioner without sufficient training or expertise in these procedures would yield comparable results. If the efficacy of the intervention is confirmed, the difficulty of a dentist being able to perform these procedures can be overcome by sufficient training programmes, so that people who are unable to benefit from dental treatment due to severe gagging can be better served.
Quality of the evidence
We included four randomised controlled trials with 328 participants of which 263 were adults (Lu 2000; Zotelli 2014) and 65 were children over the age of four years (Elbay 2016; Goel 2017). We assessed the certainty of the evidence for four outcomes, namely, successful completion of dental procedure, reduction in gagging, presence or absence of gagging, and adverse effects. We downgraded the certainty of the evidence by one level due to unclear risk of bias. We downgraded the certainty of evidence by one level each for serious imprecision and serious indirectness for all the trials. Hence the evidence available is of very low certainty. The results therefore do not allow us to draw a robust conclusion regarding the effects of acupuncture, acupressure and laser at P6 for any of the outcomes reported.
Potential biases in the review process
We have taken steps to minimise the bias in every step of the review. We conducted a thorough search of databases, conference proceedings, and trial registries as outlined in the Search methods for identification of studies section, to ensure we identified all the relevant reports. We tried to contact the study authors for missing data through emails. If the reports were very old, we tried to get the contact details of the study authors through peer contacts, Google search, and university/hospital websites where the study authors were previously affiliated. In spite of our comprehensive search strategies, we cannot rule out publication bias occurring due to non‐identification of unpublished trials.
We tried our best to follow the methodology described in our protocol. We used standard methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) and also ensured compliance with the Cochrane methodological standards for the conduct of new reviews of interventions (MECIR 2019).
Agreements and disagreements with other studies or reviews
We did not find any other systematic reviews on this topic.
Authors' conclusions
Implications for practice.
We have found very low‐certainty evidence from four trials that is insufficient to conclude whether or not acupuncture, acupressure (with or without sedation), and laser at P6 point are effective in the management of gagging in patients receiving dental treatment. We did not find any randomised controlled trials (RCTs) evaluating any other interventions for managing this problem.
Implications for research.
Further research should be done in the management of gagging in dental patients by conducting well‐planned RCTs with more clarity and uniformity in the variables. In designing such clinical trials, the following should be considered.
E (Evidence): the present evidence is insufficient to conclude that acupuncture, acupressure and laser at P6 will lead to successful completion of dental treatment or reduce the gag reflex. Trials should evaluate all the outcomes mentioned in this Cochrane Review. Furthermore, reports on clinical trials would be improved by following CONSORT guidelines (Schulz 2010).
P (Population): inclusion criteria for clinical trials should be well defined. The trials should include males and females in equal distribution. Outcome measures should be clearly defined for different age groups. The trial participants should be those people who have failed to undergo dental treatment due to gagging and not healthy volunteers. Participants should be classified according to standard scale, and mild, moderate and severe gaggers need to be stratified and randomised. Cross‐over trials testing non‐pharmacological interventions such as acupressure should report the washout period or compare the baseline data using a paired t‐test for both active and placebo treatment phases to ensure sufficient washout period.
I (Intervention): more interventional studies should be conducted on both pharmacological and non‐pharmacological interventions, with special emphasis on behavioural modification techniques.
C (Comparison): comparisons between two different interventions (pharmacological versus non‐pharmacological, or non‐pharmacological versus non‐pharmacological) can be considered in future trials instead of dummy/placebo groups.
O (Outcome): other than successful completion of treatment, reduction in gag reflex and presence or absence of gag reflex, further patient‐reported outcomes such as patient satisfaction and comfort of different types of dental procedure, and objective testing should be evaluated in the trials.
What's new
| Date | Event | Description |
|---|---|---|
| 19 August 2021 | Amended | Minor edit to plain language summary. |
History
Protocol first published: Issue 5, 2014 Review first published: Issue 10, 2015
| Date | Event | Description |
|---|---|---|
| 11 July 2019 | New citation required and conclusions have changed | Review update including 3 new studies (2 new trials on laser stimulation (Elbay 2016; Goel 2017) and 1 trial previously awaiting classification (Lu 2000)) bringing the total to 4 included studies. New review author. All sections and 'Summary of findings' tables updated. Wording of the secondary outcome 'reduction in gagging' changed. New secondary outcome 'presence or absence of gagging during dental procedure' added. |
| 18 March 2019 | New search has been performed | Searches updated to 18 March 2019. |
Acknowledgements
We are extremely thankful to Cochrane Oral Health, especially Ms Anne Littlewood, Information Specialist; Dr Philip Riley, Editor; Ms Luisa M Fernandez Mauleffinch, Managing Editor and Copy Editor; Ms Laura MacDonald, Managing Editor; and Professor Helen Worthington, Co‐ordinating Editor. We thank Professor Datuk Dr Abdul Razzak, Pro VC, Manipal Academy of Higher Education for his constant encouragement to take up Cochrane Reviews; Professor Dr Jaspal Singh Sahota, CE, Melaka‐Manipal Medical College, Melaka Campus for his support; Professor Adinegara Lutfi Abas, Dean, Faculty of Medicine, Melaka‐Manipal Medical College, and Professor Abdul Rashid Hj Ismail, Dean, Faculty of Dentistry, Melaka‐Manipal Medical College, for all the suggestions and help during the review preparation. We thank Professor Noorliza Mastura Ismail, Head of the Department of Community Dentistry, Faculty of Dentistry, Melaka‐Manipal Medical College for proofreading the review and helping us with language correction.
Our sincere gratitude and thanks to Dr Prathap Tharyan, Director of the South Asian Cochrane Centre, Christian Medical College, Vellore for being a source of inspiration, information, knowledge, and also playing a pivotal role in review completion. We also thank his team members Dr Richard Kirubakaran, Dr Rebecca Mathew, and Mr Jabez Paul Barnabas for their help. We thank Dr Himanshi Aggarwal, King George's Medical University, Lucknow for the help rendered during the review completion. We are also grateful to her for helping us in proofreading the review.
We are indebted to Ms Shazana MS, Chief Librarian, Melaka‐Manipal Medical College, and Ms Janet Lear, Cochrane Oral Health, for helping us procure full‐text articles. We thank Mr Farhad Shokraneh, University of Nottingham, Institute of Mental Health, Nottingham, and B‐lingo translations, Kuala Lumpur, for helping us with translations of foreign language articles. We express our gratitude to Vera Zotelli for the prompt reply to our queries.
We thank peer reviewers Walter YH Lam, Norvishie Arkutu and Srinivasan Narasimhan for their valuable feedback.
Appendices
Appendix 1. Cochrane Oral Health's Trials Register search strategy
Cochrane Oral Health's Trials Register is available via the Cochrane Register of Studies. For information on how the register is compiled, see oralhealth.cochrane.org/trials.
1 ((gag* or retch*):ti,ab) AND (INREGISTER) 2 ((pharyng* AND reflex*):ti,ab) AND (INREGISTER) 3 (#1 or #2) AND (INREGISTER)
Appendix 2. Cochrane Central Register of Controlled Trials (CENTRAL) search strategy
#1 [mh Dentistry] #2 (dental* or dentist* or "oral surg*" or orthodont* or pulpotom* or pulpect* or endodont* or "pulp cap*") #3 ((dental or tooth or teeth) and (fill* or restor* or extract* or remov* or "cavity prep*" or caries or carious or decay* or impress*)) #4 ("root canal") #5 ((tooth or teeth or dental) and (scal* or polish* or "oral prophylaxis")) #6 {or #1‐#5} #7 [mh ^Gagging] #8 (gag* or retch*) #9 (pharyng* and reflex*) #10 {or #7‐#9} #11 #6 and #10
Appendix 3. MEDLINE Ovid search strategy
1. exp Dentistry/ 2. (dental$ or dentist$ or "oral surg$" or orthodont$ or pulpotom$ or pulpect$ or endodont$ or "pulp cap$").mp. 3. ((dental or tooth or teeth) and (fill$ or restor$ or extract$ or remov$ or "cavity prep$" or caries or carious or decay$ or impress$)).mp. 4. "root canal$".mp. 5. ((tooth or teeth or dental) and (scal$ or polish$ or "oral prophylaxis")).mp. 6. or/1‐5 7. Gagging/ 8. (gag$ or retch$).mp. 9. (pharyng$ and reflex$).mp. 10. or/7‐9 11. 6 and 10
This subject search was linked to the Cochrane Highly Sensitive Search Strategy (CHSSS) for identifying randomised trials (RCTs) in MEDLINE: sensitivity‐maximising version (2008 revision) as referenced in Chapter 6.4.11.1 and detailed in box 6.4.c of the Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 (updated March 2011) (Lefebvre 2011).
1. randomised controlled trial.pt. 2. controlled clinical trial.pt. 3. randomised.ab. 4. placebo.ab. 5. drug therapy.fs. 6. randomly.ab. 7. trial.ab. 8. groups.ab. 9. or/1‐8 10. exp animals/ not humans.sh. 11. 9 not 10
Appendix 4. Embase Ovid search strategy
1. exp Dentistry/ 2. (dental$ or dentist$ or "oral surg$" or orthodont$ or pulpotom$ or pulpect$ or endodont$ or "pulp cap$").mp. 3. ((dental or tooth or teeth) and (fill$ or restor$ or extract$ or remov$ or "cavity prep$" or caries or carious or decay$ or impress$)).mp. 4. "root canal$".mp. 5. ((tooth or teeth or dental) and (scal$ or polish$ or "oral prophylaxis")).mp. 6. or/1‐5 7. Retching/ 8. (gag$ or retch$).mp. 9. (pharyng$ and reflex$).mp. 10. or/7‐9 11. 6 and 10
This subject search was linked to an adapted version of the Cochrane Centralised Search Project filter for identifying RCTs in Embase Ovid (see www.cochranelibrary.com/central/central-creation for information).
1. Randomized controlled trial/ 2. Controlled clinical study/ 3. Random$.ti,ab. 4. randomization/ 5. intermethod comparison/ 6. placebo.ti,ab. 7. (compare or compared or comparison).ti. 8. ((evaluated or evaluate or evaluating or assessed or assess) and (compare or compared or comparing or comparison)).ab. 9. (open adj label).ti,ab. 10. ((double or single or doubly or singly) adj (blind or blinded or blindly)).ti,ab. 11. double blind procedure/ 12. parallel group$1.ti,ab. 13. (crossover or cross over).ti,ab. 14. ((assign$ or match or matched or allocation) adj5 (alternate or group$1 or intervention$1 or patient$1 or subject$1 or participant$1)).ti,ab. 15. (assigned or allocated).ti,ab. 16. (controlled adj7 (study or design or trial)).ti,ab. 17. (volunteer or volunteers).ti,ab. 18. trial.ti. 19. or/1‐18 20. (exp animal/ or animal.hw. or nonhuman/) not (exp human/ or human cell/ or (human or humans).ti.) 21. 19 not 20
Appendix 5. CINAHL EBSCO (Cumulative Index to Nursing and Allied Health Literature) search strategy
S11 S6 AND S10 S10 S7 or S8 or S9 S9 (pharyng* and reflex*) S8 (gag* or retch*) S7 (MH Gagging) S6 S1 or S2 or S3 or S4 or S5 S5 ((tooth or teeth or dental) and (scal* or polish* or "oral prophylaxis")) S4 ("root canal") S3 ((dental or tooth or teeth) and (fill* or restor* or extract* or remov* or "cavity prep*" or caries or carious or decay* or impress*)) S2 (dental* or dentist* or "oral surg*" or orthodont* or pulpotom* or pulpect* or endodont* or "pulp cap*") S1 (MH Dentistry+)
This subject search was linked to Cochrane Oral Health's filter for CINAHL EBSCO.
S1 MH Random Assignment or MH Single‐blind Studies or MH Double‐blind Studies or MH Triple‐blind Studies or MH Crossover design or MH Factorial Design S2 TI ("multicentre study" or "multicenter study" or "multi‐centre study" or "multi‐ center study") or AB ("multicentre study" or "multicenter study" or "multi‐centre study" or "multi‐center study") or SU ("multicentre study" or "multicenter study" or "multi‐centre study" or "multi‐center study") S3 TI random* or AB random* S4 AB "latin square" or TI "latin square" S5 TI (crossover or cross‐over) or AB (crossover or cross‐over) or SU (crossover or cross‐over) S6 MH Placebos S7 AB (singl* or doubl* or trebl* or tripl*) or TI (singl* or doubl* or trebl* or tripl*) S8 TI blind* or AB mask* or AB blind* or TI mask* S9 S7 and S8 S10 TI Placebo* or AB Placebo* or SU Placebo* S11 MH Clinical Trials S12 TI (Clinical AND Trial) or AB (Clinical AND Trial) or SU (Clinical AND Trial) S13 S1 or S2 or S3 or S4 or S5 or S6 or S9 or S10 or S11 or S12
Appendix 6. AMED Ovid (Allied and Complementary Medicine) search strategy
1. exp Dentistry/ 2. (dental$ or dentist$ or "oral surg$" or orthodont$ or pulpotom$ or pulpect$ or endodont$ or "pulp cap$").mp. 3. ((dental or tooth or teeth) and (fill$ or restor$ or extract$ or remov$ or "cavity prep$" or caries or carious or decay$ or impress$)).mp. 4. "root canal$".mp. 5. ((tooth or teeth or dental) and (scal$ or polish$ or "oral prophylaxis")).mp. 6. or/1‐5 7. (gag$ or retch$).mp. 8. (pharyng$ and reflex$).mp. 9. 7 or 8 10. 6 and 9
Appendix 7. International Association for Dental Research Conference Proceedings search strategy
The conference proceedings can be found online at: www.iadr.org/IADR/About-Us/Proceedings
gag reflex
Appendix 8. US National Institutes of Health Ongoing Trials Register (ClinicalTrials.gov) search strategy
gag AND dental
gag AND dentistry
retch AND dental
retch AND dentistry
pharyngeal AND reflex AND dental
Appendix 9. World Health Organization International Clinical Trials Registry Platform search strategy
gag AND dental
gag AND dentistry
retch AND dental
retch AND dentistry
pharyngeal AND reflex AND dental
Appendix 10. metaRegister of Controlled Trials (mRCT) search strategy
gag AND dental
gag AND dentistry
retch AND dental
retch AND dentistry
pharyngeal AND reflex AND dental
Appendix 11. International Federation of Pharmaceutical Manufacturers & Associations (IFPMA) Clinical Trials Portal search strategy
gag AND dental
gag AND dentistry
retch AND dental
retch AND dentistry
pharyngeal AND reflex AND dental
Data and analyses
Comparison 1. Acupuncture at P6 point versus sham acupuncture.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Successful completion of dental procedure | 2 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.78 [1.05, 3.01] |
| 1.2 Reduction in gagging (reported by assessor ‐ treatment effectiveness) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.2.1 Stage 1 | 1 | 33 | Mean Difference (IV, Fixed, 95% CI) | 0.40 [‐0.12, 0.93] |
| 1.2.2 Stage 2 | 1 | 33 | Mean Difference (IV, Fixed, 95% CI) | 0.49 [‐0.26, 1.24] |
| 1.2.3 Stage 3 | 1 | 33 | Mean Difference (IV, Fixed, 95% CI) | 0.67 [‐0.18, 1.53] |
| 1.3 Reduction in gagging (reported by patient ‐ VAS) | 1 | 33 | Mean Difference (IV, Fixed, 95% CI) | 0.86 [‐1.13, 2.85] |
| 1.4 Reduction in gagging (reported by patient ‐ dichotomous data) | 1 | 26 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.57 [1.12, 5.89] |
Comparison 2. Acupuncture + sedation versus sham acupuncture.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Completion of dental procedure | 1 | 34 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.91, 1.28] |
| 2.2 Reduction in gagging (reported by patient) | 1 | 34 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.87, 1.37] |
Comparison 3. Acupressure with thumb versus sham acupressure.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Successful completion of dental procedure | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.50, 1.46] |
| 3.2 Reduction in gagging (reported by patient) | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.60, 1.41] |
Comparison 4. Acupressure with device versus sham acupressure.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Successful completion of dental procedure | 1 | 34 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.62 [1.33, 5.18] |
| 4.2 Reduction in gagging (reported by patient) | 1 | 34 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.94 [1.63, 9.53] |
Comparison 5. Acupressure with sea band versus sham acupressure.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Successful completion of dental procedure | 1 | 19 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.80 [0.63, 5.16] |
| 5.2 Reduction in gagging (reported by patient) | 1 | 19 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.70 [0.72, 10.14] |
Comparison 6. Acupressure with thumb + sedation versus sham + sedation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Successful completion of dental procedure | 1 | 39 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.84, 1.10] |
| 6.2 Reduction in gagging | 1 | 39 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.92, 1.23] |
Comparison 7. Acupressure with device + sedation versus sham + sedation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 Completion of dental procedure | 1 | 27 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.90, 1.48] |
| 7.2 Reduction in gagging (reported by patient) | 1 | 27 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.93, 1.69] |
Comparison 8. Acupressure with sea band + sedation versus sham + sedation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 8.1 Completion of dental procedure | 1 | 21 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.67, 1.17] |
| 8.2 Reduction in gagging | 1 | 21 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.67, 1.17] |
Comparison 9. Laser versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 9.1 Presence or absence of gagging | 1 | 80 | Odds Ratio (IV, Random, 95% CI) | 86.33 [29.41, 253.45] |
| 9.2 Reduction in gagging | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | 1.80 [1.53, 2.07] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Elbay 2016.
| Study characteristics | ||
| Methods | Study design: randomised, controlled, double‐blind, split‐mouth, clinical trial Location: Kocaeli University, Turkey Number of centres: 1 Recruitment period: not reported Funding source: not reported |
|
| Participants | Inclusion criteria: patients requiring bilateral periapical radiographs of the maxillary molar region; patients with moderate to very severe gagging according to the Classification of Gagging Problem (CGP) index Exclusion criteria: parents who were unwilling to implement the DAS for their children; children with unco‐operative attitudes, disabilities, or severe systemic diseases; children requiring emergency treatment Age: children 6 to 12 years old. Mean age group: 8.68 years Gender: male: 17; female: 8 Number randomised: 25 Number evaluated: 25 |
|
| Interventions | Intervention: low‐level laser therapy (LLLT) at P6 point (laser energy of 300 mW (energy density = 4 J/cm2) for 14 seconds on each P6 point) Control: without application of LLLT on P6 Duration of treatment: 14 seconds Duration of follow‐up: not reported |
|
| Outcomes | Reduction in gagging leading to completion of dental procedures ‐ as assessed by researcher/dentist using gagging severity score:
Assessed by participant: not reported Health‐related quality of life: not reported Adverse effects: none reported |
|
| Notes | Sample size calculation: minimum sample size of 22 was calculated using the G*Power software program (version 3.1.9.2; power 0.80, α = 0.05, β = 0.20). Therefore, considering possible dropouts, this study was conducted with 25 children Key conclusions of the study authors: "Both mean and median gagging scores were higher in the control group than in the experimental group. Patients who were unable to tolerate the intraoral control radiography were able to tolerate the procedure after LLLT. Differences between gagging scores of the control and experimental groups were statistically significant (P = .000). There was no significant correlation between gagging severity and anxiety score (P > .05). A negative correlation was found between age and gagging score in the control group (P.05). Within the limitations of this study, LLLT of the PC 6 acupuncture points appears to be a useful technique for controlling the gag reflex in children during maxillary radiography" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A computer generated list was used to randomly select the control and experimental sides" Comment: done |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quotes: "In order to blind patients to the LLLT, laser application was simulated using a non‐working laser for the control radiograph.." "All laser treatment was performed by a single operator who did not perform the radiography or gagging evaluation" Comment: done. Laser application was simulated using non‐working laser for control followed by actual laser for experimental. Both patients and operator wore protective eye wear regardless of laser activation |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All laser treatment was performed by a single operator who did not perform the radiography or gagging evaluation" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts. All subjects completed the study |
| Selective reporting (reporting bias) | Low risk | All outcomes described were reported. Conclusions are in accordance with the results |
| Other bias | Unclear risk | We are not sure regarding the carry‐over effect of the laser treatment |
Goel 2017.
| Study characteristics | ||
| Methods | Study design: randomised, cross‐over trial Location: Ghaziabad, India Number of centres: 1 Recruitment period: not reported Funding source: self‐funded |
|
| Participants | Inclusion criteria: patients requiring impression of the maxillary arch; patients with Gagging Severity Index scores of 3 to 5 Exclusion criteria: not reported Age: 4 to 14 years old Gender: male: 17; female: 23 Number randomised: 40 Number evaluated: 40 |
|
| Interventions | Intervention: diode laser with a penetration depth of few millimetres in a defocused continuous mode applied on P6 acupressure point (output 0.5 mW, wavelength 940 nm, energy 4J) Total number of intervention groups: 2 (cross‐over design):
Control: no laser Duration of treatment: 1 minute Duration of follow‐up: no follow‐up |
|
| Outcomes | Completion of dental procedure: not reported Reduction in gagging as assessed by researcher/dentist: dichotomous: presence or absence of gagging Assessed by participant: not reported Health‐related quality of life: not reported Adverse effects: not reported |
|
| Notes | Sample size calculation: reported. Data from pilot study was used, pooled variance S2 = 1.58 and mean difference d = 1.385 Key conclusions of the study authors: "LLLT on PC6 point was found to be effective in lowering anxiety levels as observed by faces modified anxiety rating scale. Further, it was authenticated as the pulse rates were significantly reduced and oxygen saturation levels were significantly increased. Also, gag reflex was significantly controlled when LASER stimulation was done at PC6" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not reported. Quote: "The patients were randomly assigned into two groups Group A and Group B" |
| Allocation concealment (selection bias) | Unclear risk | Method not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Method not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Method not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts. All subjects completed the study |
| Selective reporting (reporting bias) | Low risk | All outcomes described were reported. Conclusions are in accordance with the results |
| Other bias | Unclear risk | We are not sure regarding the carry‐over effect of the laser treatment |
Lu 2000.
| Study characteristics | ||
| Methods | Study design: randomised, parallel‐group (8 arms), controlled trial Location: University of Pennsylvania, Einstein College of Medicine, Bronx, New York (university hospital), USA Number of centres: 1 Recruitment period: not reported Funding source: not reported |
|
| Participants | Inclusion criteria: patients with severe gag reflex requiring any dental treatment (Impression, restoration, scaling/curettage to prophylaxis paste) Exclusion criteria: not reported Age: 17 to 76 years old Gender: not reported Number randomised: not reported Number evaluated: 230 |
|
| Interventions | Type of intervention:
Control: placebo Dosage: for sedation: any of the following:
Total number of intervention groups: 3 groups (with 3 subgroups for Group 2 and 4 for Group 3 respectively):
Duration of treatment:
Duration of follow‐up: no follow‐up |
|
| Outcomes | Completion of dental procedure: reported Completion of dental procedure as assessed by researcher/dentist*: reported as excellent, good, fair, poor:
* Completion of procedure: excellent, good and fair / Procedure incomplete: poor Reduction in gagging assessed by participant: reported as excellent, good, fair, poor*:
* Reduction in gagging: excellent, good and fair / No reduction: poor Health‐related quality of life: not reported Adverse effects: not reported |
|
| Notes | Sample size calculation: not reported Key conclusions of the study authors: "The P6 point has remarkable anti‐gagging effects if stimulation is applied correctly. Clinicians may apply thumb pressure at the P6 point to achieve some effect, although this is not as effective as acupuncture. Nevertheless, a substantial percentage of gagging patients would be able to go through dental procedures without gagging when the P6 point is stimulated" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not described. Quote: "The patients were randomised into three groups" |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Low risk | All outcomes described were reported. Conclusions are in accordance with the results |
| Other bias | Low risk | None |
Zotelli 2014.
| Study characteristics | ||
| Methods | Study design: parallel‐group, randomised trial Location: Piracicaba Dental School (FOP‐UNICAMP) in Piracicaba, Sau Paulo, Brazil Setting: dental hospital Number of centres: 1 Total study duration: 7 months (February 2013 to August 2013) Funding source: none declared |
|
| Participants | Inclusion criteria: previous history of unpleasant nausea during dental procedures that hindered or prevented the dental treatment from being carried out properly; either sex; age 18 to 85 Exclusion criteria: pregnant women and people who had been taking antiemetic drugs or medications that could produce nausea Age: 19 to 62 years old Gender: male: 11; female: 22 Ethnicity: 27 white; 4 non‐white Number randomised: random assignment of 33 participants (intervention = 17; sham = 16). Study details obtained by personal communication Number evaluated: 33 |
|
| Interventions | Intervention: acupuncture at P6 Control: sham acupuncture at P6 Details: for the intervention group, a disposable acupuncture needle was placed unilaterally in the right arm with perpendicular insertion angle. For the control group, a retractable needle with blunt tip that does not penetrate the skin was used, which gives the patient a pricking sensation. The needles were in place for 20 minutes and were removed before discharging the patient. The procedure was done by the same experienced and licensed acupuncturist for all participants |
|
| Outcomes | Completion of dental procedure: data obtained by personal communication Reduction in gagging Assessed by researcher: Gagging Severity Index (GSI) (evaluated severity of nausea) and Gagging Prevention Index (GPI) (evaluated the treatment effectiveness in controlling nausea) Time point: GSI was assessed prior to acupuncture and GPI was assessed after acupuncture. Both GSI and GPI were assessed in 3 stages of impression taking: when the empty impression tray was tried in the mouth, when the loaded tray was inserted into the mouth and the tolerance of the tray in the mouth until the alginate set Assessed by participant: VAS: it consisted of a horizontal line 10 inches long, with word anchors at both ends with words 'without nausea' at 0 and 'maximum nausea' at 10 Time point: VAS was recorded on 2 occasions, at the end of the first moulding without acupuncture and at the end of the second impression with acupuncture, in both groups Adverse effects: 1 participant reported increased sweating in control group; however, this participant had declared having a fear of needles, which explains the reported effect. In the test group, 11 people reported at least one of the possible sensations of Deqi |
|
| Notes | Sample size calculation: sample was defined based on scientific literature, other study authors used similar size of sample (from personal communication) Key conclusions of the study authors: "Acupuncture in PC6 was effective for controlling nausea during maxillary impression" Miscellaneous comments from study authors: "the volunteers' expectations had no influence on reducing nausea" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was done using the site http://www.randomizer.org. |
| Allocation concealment (selection bias) | Unclear risk | "This was a controlled, double‐blind clinical study, in which the researchers and the volunteer patients were not aware of the group to which the volunteers belonged". "...were informed that they would not be aware of the group to which would be assigned to". Comment: Details of allocation concealment not reported in the article and personal communication. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "This was a controlled, double‐blind clinical study, in which the researchers and the volunteer patients were not aware of the group to which the volunteers belonged". "So that neither the researchers nor the patients were able to differentiate between the real acupuncture and the sham acupuncture, we used the resin ring in both groups, and the patient was covered with a disposable blue sheet of 40 grammage thickness until the end of the procedure". "one (the volunteer researcher) inserted the acupuncture needles and the other (the main researcher) performed the impression‐taking procedures and nausea assessment". |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote from control group methodology: "this needle is retractable and has a blunt tip; therefore, it does not penetrate the skin. When it touches the skin, the patient feels a pricking sensation, simulating the puncturing of the skin". "So that neither the researchers nor the patients were able to differentiate between the real acupuncture and the sham acupuncture, we used the resin ring in both groups, and the patient was covered with a disposable blue sheet of 40 grammage thickness until the end of the procedure". "one (the volunteer researcher) inserted the acupuncture needles and the other (the main researcher) performed the impression‐taking procedures and nausea assessment". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All 33 participants were evaluated. |
| Selective reporting (reporting bias) | Low risk | All outcomes described were reported. Conclusions are in accordance with the results. |
| Other bias | Low risk | None |
IM = intramuscular; IV = intravenous; J = Joules; mW = milliwatts; nm = nanometres; P6 = a point located 3‐finger breadths below the wrist on the inner forearm in between the 2 tendons; TENS = transcutaneous electric nerve stimulation; VAS = visual analogue scale.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Barenboim 2009 | Cross‐over trial in healthy volunteers |
| ISRCTN66117475 | Clinical trial stopped |
| NCT00502437 | Cross‐over trial in healthy volunteers |
| Ranjbaran 2011 | Randomised controlled trial in healthy volunteers |
Characteristics of studies awaiting classification [ordered by study ID]
Hekmatian 2011a.
| Methods | Study design: unclear if randomised or non‐RCT Country: Iran Setting: radiology department of the School of Dentistry, Isfahan University of Medical Sciences, Isfahan, Iran Period of trial: not mentioned |
| Participants | Total number of participants (randomised?): 100 Age: not mentioned Gender: male = 31, female = 66 Inclusion criteria: patients admitted to the radiology department of the dentistry school; informed consent; no central or peripheral nervous system disorders or had any oral lesions; high co‐operation Exclusion criteria: people who suffered from any type of brain lesions; any oral lesions; learning disabilities |
| Interventions | Intervention: E angustifolia film (n = 50) Control: placebo film (n = 47) Intervention details: all patients were evaluated for gag reflex after 3 minutes of film in touch with the mucosa |
| Outcomes | Outcomes reported:
|
| Notes | Funding source: not mentioned Sample size calculation: simple non‐probability sampling Adverse effects: not mentioned Attrition: 3 Trials registration: not registered Notes: email sent for additional information regarding randomisation and nature of participants on 25 November 2014; no reply received |
Hekmatian 2011b.
| Methods | Study design: unclear if randomised or non‐RCT Country: Iran Setting: radiology department of the School of Dentistry, Isfahan University of Medical Sciences, Isfahan, Iran Period of trial: not mentioned |
| Participants | Total number of participants (randomised?): 84 Age: mean age 24.6 ± 0.8 years Gender: male = 42, female = 42 Inclusion criteria: patients admitted to the radiology department of the dentistry school; informed consent; no central or peripheral nervous system disorders or had any oral lesions; high co‐operation Exclusion criteria: patients who suffered from any type of central or peripheral nervous system disorders; any oral lesions |
| Interventions | Intervention: pomegranate peel extract lozenges (n = 42) Control: placebo lozenges (n = 42) Intervention details: "The patients sucked the lozenges in their mouth till it was completely dissolved. After five minutes, the patient felt senselessness in the soft palate and pharyngeal tonsil. The patient was then evaluated regarding the intensity and degree of gag reflex in the soft palate and pharyngeal tonsils" |
| Outcomes | Outcomes reported:
|
| Notes | Funding source: not mentioned Sample size calculation: simple non‐probability sampling Adverse effects: not mentioned Attrition: nil Trials registration: not registered Notes: email sent for additional information regarding randomisation and nature of participants on 12 June 2014; no reply received |
Hekmatian 2012.
| Methods | Study design: unclear if randomised or non‐RCT Country: Iran Setting: radiology department of the School of Dentistry, Isfahan University of Medical Sciences, Isfahan, Iran Period of trial: not mentioned |
| Participants | Total number of participants (randomised?): 84 Age: mean age was 24.6 ± 0.8 years Gender: not mentioned Inclusion criteria: patients admitted to the radiology department of the dentistry school; informed consent; no central or peripheral nervous system disorders or had any oral lesions; high co‐operation Exclusion criteria: patients who suffered from any type of central or peripheral nervous system disorders; any oral lesions |
| Interventions | Intervention: E angustifolia lozenges (n = 42) Control: placebo lozenges (n = 42) Intervention details: E angustifolia lozenges (the saturated sugar solution and the heated concentrated E angustifolia were mixed (80 mg fruit concentrate and 100 ml syrup) and were poured into the same mould to make 1 mg tablets) Placebo lozenges (placebo was made of water and sugar) Each patient sucked a lozenge in their mouth until it was completely dissolved. After 5 minutes, the patient felt senselessness in the soft palate and pharyngeal tonsil. The patient was then evaluated regarding the intensity and degree of gag reflex in the soft palate and pharyngeal tonsils. |
| Outcomes | Outcomes reported:
|
| Notes | Funding source: not mentioned Sample size calculation: simple non‐probability sampling Adverse effects: not mentioned Attrition: nil Trials registration: not registered Notes: email sent for additional information regarding randomisation and nature of participants on 12 June 2014; no reply received |
NCT02938364.
| Methods | Study design: randomised, single‐blinded, clinical trial Country: Saudi Arabia Setting: clinics of Riyadh Colleges of Dentistry and Pharmacy (RCsDP) in Riyadh, Saudi Arabia Period of trial: not mentioned |
| Participants | Total number of participants (randomised?): 30 Age: above 18 years old Gender: not mentioned Inclusion criteria: 18 years and older (adult, older adult); the individual is able to give informed consent; patients with gag reflex severity that are assigned to a Gagging Severity Index (GSI) III‐IV (for standardization of the baseline severity in between Groups) Exclusion criteria: pregnant women; patients with chronic heart diseases or cardiac pacemakers; patients with central or peripheral nervous system disorders; patients with oral lesions; patients with gastrointestinal disorders |
| Interventions | Intervention:
Control (n = 10): placebo bands: the participant will be asked to wear non‐pressure bands on both hand wrists for 10 minutes and then the impression will be made while they are still on |
| Outcomes | Outcomes reported:
|
| Notes | Funding source: not mentioned Sample size calculation: not mentioned Adverse effects: not mentioned Attrition: not clear Trials registration: NCT02938364 Notes: full text of the published report not available, email was sent to the author on 5 June 2019, awaiting response |
Rahshenas 2015.
| Methods | Study design: not clear Country: Iran Setting: dentistry department, Islamic Azad University, Dental Branch, Tehran, Iran |
| Participants | Total number of participants: 75 Age: not mentioned Gender: not specified Inclusion criteria: not mentioned Exclusion criteria: not mentioned |
| Interventions | Clinical trial was performed on patients with gag reflex during oral examinations with tongue blade The patients were divided to 3 groups:
|
| Outcomes | Outcomes reported:
|
| Notes | Study design is unclear and full text is not available Email was sent on 5 June 2019 to the author requesting the full text; awaiting response |
Differences between protocol and review
New author (Salian Kiran Kumar Krishanappa) is added.
There is a slight alteration in the contributions of the review authors, which is mentioned in the Contributions of authors section.
Cross‐over trials now included in review.
Wording of the secondary outcome 'reduction in gagging' changed.
New secondary outcome 'presence or absence of gagging during dental procedure' added.
Adverse effects now focused on adverse effects of the interventions.
We added laser stimulation to the list of non‐pharmacological interventions.
Contributions of authors
Prashanti Eachempati was the arbiter, updated review of literature, analysed data, and drafted the final review.
Sumanth Kumbargere Nagraj performed searches, obtained full‐text articles of trials, analysed data, and drafted the final review.
Salian Kiran Kumar Krishanappa performed searches, obtained full‐text articles of trials, helped with data extraction, data entry into Review Manager 2014, and drafted the final review.
Renjith P George selected trials, extracted data, and entered data into Review Manager 2014.
Htoo Htoo Kyaw Soe performed and interpreted analyses.
Laxminarayan Karanth interpreted analyses.
Sources of support
Internal sources
-
Faculty of Dentistry, Melaka‐Manipal Medical College, Manipal University, Melaka Campus, Malaysia
Internal grant of 3170 RM received, PO‐284/2014‐15 dated 3 November 2014.
External sources
-
National Institute for Health Research (NIHR), UK
This project was supported by the NIHR, via Cochrane Infrastructure funding to Cochrane Oral Health. The views and opinions expressed are those of the authors and not necessarily those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health and Social Care.
-
Cochrane Oral Health Global Alliance, Other
The production of Cochrane Oral Health reviews has been supported financially by our Global Alliance since 2011 (oralhealth.cochrane.org/partnerships-alliances). Contributors over the past year have been the American Association of Public Health Dentistry, USA; AS‐Akademie, Germany; the British Association for the Study of Community Dentistry, UK; the British Society of Paediatric Dentistry, UK; the Canadian Dental Hygienists Association, Canada; the Centre for Dental Education and Research at All India Institute of Medical Sciences, India; the National Center for Dental Hygiene Research & Practice, USA; New York University College of Dentistry, USA; NHS Education for Scotland, UK; and the Swiss Society for Endodontology, Switzerland.
-
Malaysian Cochrane Centre, Penang Medical College, Malaysia
Provided training for writing protocol.
-
South Asian Cochrane Centre, hosted by the Professor BV Moses Centre for Evidence‐Informed Health Care and Health Policy; Christian Medical College, Vellore, India
For training in review completion.
Division of Dentistry, The University of Manchester, UK
Declarations of interest
Prashanti Eachempati: none known. Sumanth Kumbargere Nagraj: none known. Salian Kiran Kumar Krishanappa: none known. Renjith P George: none known. Htoo Htoo Kyaw Soe: none known. Laxminarayan Karanth: none known.
Edited (no change to conclusions)
References
References to studies included in this review
Elbay 2016 {published data only}
- Elbay M, Tak O, Sermet Elbay U, Kaya C, Eryilmaz K. The use of low-level laser therapy for controlling the gag reflex in children during intraoral radiography. Lasers in Medical Science 2016;31(2):355-61. [PMID: ] [DOI] [PubMed] [Google Scholar]
Goel 2017 {published data only}
- Goel H, Mathur S, Sandhu M, Jhingan P, Sachdev V. Effect of low-level LASER therapy on P6 acupoint to control gag reflex in children: a clinical trial. Journal of Acupuncture and Meridian Studies 2017;10(5):317-23. [PMID: ] [DOI] [PubMed] [Google Scholar]
Lu 2000 {published data only}
- Lu DP, Lu GP, Reed JF 3rd. Acupuncture/acupressure to treat gagging dental patients: a clinical study of anti-gagging effects. General Dentistry 2000;48(4):446-52. [PMID: ] [PubMed] [Google Scholar]
Zotelli 2014 {published and unpublished data}
- Zotelli VL, Grillo CM, Sousa Mda L. Nausea control by needling at acupuncture point Neiguan (PC6) during an intraoral impression-taking procedure. Journal of Acupuncture and Meridian Studies 2014;7(6):318-23. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Barenboim 2009 {published data only}
- Barenboim SF, Dvoyris V, Kaufman E. Does granisetron eliminate the gag reflex? A crossover, double-blind, placebo-controlled pilot study. Anesthesia Progress 2009;56(1):3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
ISRCTN66117475 {unpublished data only}
- ISRCTN66117475. A pilot study using a single blind placebo controlled trial into the efficacy and specificity of the acupuncture point CV24 in controlling the gag reflex to permit dental treatment (impression taking). isrctn.com/ISRCTN66117475 (first received 28 September 2007).
NCT00502437 {unpublished data only}
- NCT00502437. The antigagging effect of Granisetron (Kytril), an antiemetic drug, in dental situations. clinicaltrials.gov/ct2/show/NCT00502437 (first received 17 July 2007).
Ranjbaran 2011 {unpublished data only}
- Ranjbaran FS. Evaluation of the efficacy of oral ondansetron on gag reflex in soft palate and palatine tonsil. Journal of Isfahan Dental School 2011;6(6):691-7. [Google Scholar]
References to studies awaiting assessment
Hekmatian 2011a {published data only}
- Hekmatian E, Asghari G, Najafi RB, Moosavi SH. Evaluation of the effect of Elaeagnus angustofolia drug film on gag reflex. Journal of Isfahan Dental School 2011;7(4):395-401. [Google Scholar]
Hekmatian 2011b {published data only}
- Hekmatian E, Shadmehr E, Asghari G. Effect of pomegranate peel extract lozenge on gag reflex in dental patients. Journal of Isfahan Dental School 2011;7(3):229-35. [Google Scholar]
Hekmatian 2012 {published data only}
- Hekmatian E, Shadmehr E, Asghari GH. Effect of Elaeagnus angustifolia lozenge on gag reflex in dental patients. Journal of Islamic Dental Association of Iran 2012;24(1):43-7. [Google Scholar]
NCT02938364 {published data only}
- NCT02938364. Ear plugs versus acupressure for management of severe gag reflex [Ear plugs versus acupressure for management of severe gag reflex: a randomized clinical trial]. clinicaltrials.gov/ct2/show/NCT02938364 (first received 19 October 2016). [NCT02938364]
Rahshenas 2015 {published data only}
- Rahshenas N, Mostofi Sh, Valaii N, Farajzad A. The effect of acupressure on the gag reflex. Journal of Research in Dental Sciences 2015;12(1):1. [Google Scholar]
Additional references
Akarslan 2012
- Akarslan ZZ, Biçer AZ. Utility of the gagging problem assessment questionnaire in assessing patient sensitivity to dental treatments. Journal of Oral Rehabilitation 2012;39(12):948-55. [PMID: ] [DOI] [PubMed] [Google Scholar]
Allen 2006
- Allen SC, Bernat JE, Perinpanayagam MK. Survey of sedation techniques used among pediatric dentists in New York State. New York State Dental Journal 2006;72(5):53-5. [PMID: ] [PubMed] [Google Scholar]
Balshem 2011
- Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. Journal of Clinical Epidemiology 2011;64(4):401-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Barsby 1994
- Barsby MJ. The use of hypnosis in the management of 'gagging' and intolerance to dentures. British Dental Journal 1994;176(3):97-102. [PMID: 7599007] [DOI] [PubMed] [Google Scholar]
Barsby 1997
- Barsby MJ. The control of hyperventilation in the management of 'gagging'. British Dental Journal 1997;182(3):109-11. [PMID: ] [DOI] [PubMed] [Google Scholar]
Bartlett 1971
- Bartlett KA. Gagging. A case report. American Journal of Clinical Hypnosis 1971;14(1):54-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Bassi 2004
- Bassi GS, Humphris GM, Longman P. The etiology and management of gagging: a review of the literature. Journal of Prosthetic Dentistry 2004;91(5):459-67. [PMID: 15153854 ] [DOI] [PubMed] [Google Scholar]
Bhat 2006
- Bhat MK. Fruit for ulcers. British Dental Journal 2006;201(6):323. [PMID: ] [DOI] [PubMed] [Google Scholar]
Bilello 2014
- Bilello G, Fregapane A. Gag reflex control through acupuncture: a case series. Acupuncture in Medicine 2014;32(1):24-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Boitel 1984
Cakmak 2014
- Cakmak YO, Ozdogmus O, Günay Y, Gürbüzer B, Tezulaş E, Kaspar EC, et al. An earplug technique to reduce the gag reflex during dental procedures. Forschende Komplementärmedizin 2014;21(2):94-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Chidiac 2001
- Chidiac JJ, Chamseddine L, Bellos G. Gagging prevention using nitrous oxide or table salt: a comparative pilot study. International Journal of Prosthodontics 2001;14(4):364-6. [PMID: ] [PubMed] [Google Scholar]
Conny 1983
- Conny DJ, Tedesco LA. The gagging problem in prosthodontic treatment. Part II: Patient management. Journal of Prosthetic Dentistry 1983;49(6):757-61. [PMID: ] [DOI] [PubMed] [Google Scholar]
Curtin 2002
- Curtin F, Elbourne D, Altman DG. Meta-analysis combining parallel and cross-over clinical trials. II: Binary outcomes. Statistics in Medicine 2002;21(15):2145-59. [DOI] [PubMed] [Google Scholar]
Cyber 2015
- Cyber Legend Ltd. Pericardium 6. www.acupuncture.com/education/points/pericardium/pc6.htm (accessed 12 May 2015).
Deeks 2011
- Deeks JJ, Higgins JP, Altman DG. Chapter 9: Analysing data and undertaking meta-analyses. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Dickinson 2005a
- Dickinson CM, Fiske J. A review of gagging problems in dentistry: 2. Clinical assessment and management. Dental Update 2005;32(2):74-6, 78-80. [PMID: ] [DOI] [PubMed] [Google Scholar]
Dickinson 2005b
- Dickinson CM, Fiske J. A review of gagging problems in dentistry: 1. Aetiology and classification. Dental Update 2005;32(1):26-8, 31-2. [PMID: ] [DOI] [PubMed] [Google Scholar]
Eitner 2005
- Eitner S, Wichmann M, Holst S. "Hypnopuncture"--a dental-emergency treatment concept for patients with a distinctive gag reflex. International Journal of Clinical and Experimental Hypnosis 2005;53(1):60-73. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ezzo 2006
- Ezzo J, Streitberger K, Schneider A. Cochrane systematic reviews examine P6 acupuncture-point stimulation for nausea and vomiting. Journal of Alternative and Complimentary Medicine 2006;12(5):489-95. [PMID: ] [DOI] [PubMed] [Google Scholar]
Farmer 1984
- Farmer JB, Connelly ME. Palateless dentures: help for the gagging patient. Journal of Prosthetic Dentistry 1984;52(5):691-4. [PMID: ] [DOI] [PubMed] [Google Scholar]
Farrier 2011
- Farrier S, Pretty IA, Lynch CD, Addy LD. Gagging during impression making: techniques for reduction. Dental Update 2011;38(3):171-2, 174-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Foster 1985
- Foster MA, Owens RG, Newton AV. Functional analysis of the gag reflex. British Dental Journal 1985;158(10):369-70. [PMID: ] [DOI] [PubMed] [Google Scholar]
Grace 1963
- Grace LE, Hackney RD, Dobbs EC. A clinical evaluation of trimethobenzamide (Tigan) as an antigagging drug. Oral Surgery, Oral Medicine, and Oral Pathology 1963;16:422-5. [PMID: 13949688] [DOI] [PubMed] [Google Scholar]
GRADE 2015 [Computer program]
- GRADEpro GDT. Version accessed 1 June 2019. Hamilton (ON): McMaster University (developed by Evidence Prime), 2015. Available at gradepro.org.
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Hoad‐Reddick 1986
- Hoad-Reddick G. Gagging: a chairside approach to control. British Dental Journal 1986;161(5):174-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hosseinzadeh 2003
- Hosseinzadeh H, Ramezani M, Namjo N. Muscle relaxant activity of Elaeagnus angustifolia L. fruit seeds in mice. Journal of Ethnopharmacology 2003;84(2-3):275-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hotta 2012
- Hotta H. Case report of difficult dental prosthesis insertion due to severe gag reflex. Bulletin of Tokyo Dental College 2012;53(3):133-9. [PMID: 23124303] [DOI] [PubMed] [Google Scholar]
Jain 2013
- Jain A, V V, Bharathi RM, Patil V, Alur J. Management of severe gag reflex by an unique approach: palateless dentures. Journal of Clinical and Diagnostic Research 2013;7(10):2394-5. [PMID: 24298541 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kaufman 1988
- Kaufman E, Weinstein P, Sommers EE, Soltero DJ. An experimental study of control of the gag reflex with nitrous oxide. Anesthesia Progress 1988;35(4):155-7. [PMID: ] [PMC free article] [PubMed] [Google Scholar]
Kovats 1971
- Kovats JJ. Clinical evaluation of the gagging denture patient. Journal of Prosthetic Dentistry 1971;25(6):613-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Kramer 1977
- Kramer RB, Braham RL. The management of the chronic or hysterical gagger. ASDC Journal of Dentistry for Children 1977;44(2):111-6. [PMID: ] [PubMed] [Google Scholar]
Krol 1963
- Krol AJ. A new approach to the gagging problem. Journal of Prosthetic Dentistry 1963;13(4):611-6. [Google Scholar]
Kumar 2011
- Kumar S, Satheesh P, Savadi RC. Gagging. New York State Dental Journal 2011;77(4):22-7. [PMID: ] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
MECIR 2019
- Higgins JPT, Lasserson T, Chandler J, Tovey D, Churchill R. Methodological Expectations of Cochrane Intervention Reviews. Cochrane: London, Version July 2019.
Meeker 1986
- Meeker HG, Magalee R. The conservative management of the gag reflex in full denture patients. New York State Dental Journal 1986;52(4):11-4. [PMID: 3457325] [PubMed] [Google Scholar]
Morrish 1997
- Morrish RB Jr. Suppression and prevention of the gag reflex with a TENS device during dental procedures. General Dentistry 1997;45(5):498-501. [PMID: ] [PubMed] [Google Scholar]
Murthy 2011
- Murthy V, Yuvraj V, Nair PP, Thomas S, Krishna A, Cyriac S. Management of exaggerated gagging in prosthodontic patients using glossopharyngeal nerve block. BMJ Case Reports 2011;pii:bcr0720114493. [PMID: ] [DOI] [PMC free article] [PubMed]
Neumann 2001
- Neumann JK, McCarty GA. Behavioral approaches to reduce hypersensitive gag response. Journal of Prosthetic Dentistry 2001;85(3):305. [PMID: ] [DOI] [PubMed] [Google Scholar]
Noble 2002
- Noble S. The management of blood phobia and a hypersensitive gag reflex by hypnotherapy: a case report. Dental Update 2002;29(2):70-4. [PMID: ] [DOI] [PubMed] [Google Scholar]
R ‐ 3.3.1 for Windows [Computer program]
- R. Version 3.3.1. Vienna, Austria: The R Foundation for Statistical Computing, 2013.
Ramazani 2016
- Ramazani M, Zarenejad N, Parirokh M, Zahedpasha S. How can hypnodontics manage severe gag reflex for root canal therapy? A case report. Iranian Endodontic Journal 2016;11(2):146-9. [PMID: ] [DOI] [PMC free article] [PubMed]
Ramsay 1987
- Ramsay DS, Weinstein P, Milgrom P, Getz T. Problematic gagging: principles of treatment. Journal of the American Dental Association 1987;114(2):178-83. [PMID: ] [DOI] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Robb 1996
- Robb ND, Crothers AJ. Sedation in dentistry. Part 2: management of the gagging patient. Dental Update 1996;23(5):182-6. [PMID: ] [PubMed] [Google Scholar]
Rosted 2006
- Rosted P, Bundgaard M, Fiske J, Pedersen AM. The use of acupuncture in controlling the gag reflex in patients requiring an upper alginate impression: an audit. British Dental Journal 2006;201(11):721-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
Saita 2013
- Saita N, Fukuda K, Koukita Y, Ichinohe T, Yamashita S. Relationship between gagging severity and its management in dentistry. Journal of Oral Rehabilitation 2013;40(2):106-11. [PMID: ] [DOI] [PubMed] [Google Scholar]
Sari 2010
- Sari E, Sari T. The role of acupuncture in the treatment of orthodontic patients with a gagging reflex: a pilot study. British Dental Journal 2010;208(10):E19. [PMID: 20489741] [DOI] [PubMed] [Google Scholar]
Saunders 1997
- Saunders RM, Cameron J. Psychogenic gagging: identification and treatment recommendations. Compendium of Continuing Dental Education in Dentistry 1997;18(5):430-3, 436, 438. [PMID: ] [PubMed] [Google Scholar]
Schulz 2010
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Annals of Internal Medicine 2010;152(11):726-32. [PMID: ] [DOI] [PubMed] [Google Scholar]
Shin 2017
- Shin S, Kim S. Dental treatment in patients with severe gag reflex using propofol-remifentanil intravenous sedation. Journal of Dental Anesthesia and Pain Medicine 2017;17(1):65-9. [PMID: ] [DOI] [PMC free article] [PubMed]
Singer 1973
- Singer IL. The marble technique: a method for treating the "hopeless gagger" for complete dentures. Journal of Prosthetic Dentistry 1973;29(21):146-50. [PMID: ] [DOI] [PubMed] [Google Scholar]
Singh 2012
- Singh K, Gupta N. Palateless custom bar supported overdenture: a treatment modality to treat patient with severe gag reflex. Indian Journal of Dental Research 2012;23(2):145-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Stedman 2011
- Stedman MR, Curtin F, Elbourne DR, Kesselheim AS, Brookhart MA. Meta-analyses involving cross-over trials: methodological issues. International Journal of Epidemiology 2011;40(6):1732-4. [DOI] [PubMed] [Google Scholar]
Vachiramon 2002
- Vachiramon A, Wang WC. Acupressure technique to control gag reflex during maxillary impression procedures. Journal of Prosthetic Dentistry 2002;88(2):236. [PMID: ] [DOI] [PubMed] [Google Scholar]
Van Houtem 2015
- Van Houtem CM, Van Wijk AJ, Boomsma DI, Ligthart L, Visscher CM, De Jongh A. Self-reported gagging in dentistry: prevalence, psycho-social correlates and oral health. Journal of Oral Rehabilitation 2015;42(7):487-94. [PMID: ] [DOI] [PubMed] [Google Scholar]
Van Linden van den Heuvell 2008
- Van Linden van den Heuvell GF, Ter Pelkwijk BJ, Stegenga B. Development of the Gagging Problem Assessment: a pilot study. Journal of Oral Rehabilitation 2008;35(3):196-202. [PMID: ] [DOI] [PubMed] [Google Scholar]
Vickers 1996
- Vickers AJ. Can acupuncture have specific effects on health? A systematic review of acupuncture antiemesis trials. Journal of the Royal Society of Medicine 1996;89(6):303-11. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wilks 1983
- Wilks CG, Marks IM. Reducing hypersensitive gagging. British Dental Journal 1983;155(8):263-5. [PMID: 6580017] [DOI] [PubMed] [Google Scholar]
Wright 1979
- Wright SM. An examination of factors associated with retching in dental patients. Journal of Dentistry 1979;7(3):194-207. [PMID: ] [DOI] [PubMed] [Google Scholar]
Yadav 2011
- Yadav S, Sheorain AK, Puneet, Shetty V. Use of training dentures in management of gagging. Indian Journal of Dental Research 2011;22(4):600-2. [PMID: ] [DOI] [PubMed] [Google Scholar]
Yamashiro 1995
- Yamashiro M. Effectiveness of conscious sedation with a single benzodiazepine compared with a combination of drugs. Anesthesia Progress 1995;42(3-4):103-6. [PMID: ] [PMC free article] [PubMed] [Google Scholar]
Yoshida 2007
- Yoshida H, Ayuse T, Ishizaka S, Ishitobi S, Nogami T, Oi K. Management of exaggerated gag reflex using intravenous sedation in prosthodontic treatment. Tohoku Journal of Experimental Medicine 2007;212(4):373-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Yoshida 2009
- Yoshida H, Nogami T, Hayashi Y, Oi K. Management of exaggerated gag reflex using conscious sedation techniques in endodontic therapy - a pilot study. Journal of Disability and Oral Health 2009;10(1):36-40. [Google Scholar]
Zach 1989
- Zach GA. Gag control. General Dentistry 1989;37(6):508-9. [PMID: ] [PubMed] [Google Scholar]
References to other published versions of this review
Eachempati 2014
- Eachempati P, Kumbargere Nagraj S, Renjith George P, Karanth L, Soe HHK. Management of gag reflex for patients undergoing dental treatment. Cochrane Database of Systematic Reviews 2014, Issue 5. Art. No: CD011116. [DOI: 10.1002/14651858.CD011116] [DOI] [PMC free article] [PubMed] [Google Scholar]
Prashanti 2015
- Prashanti E, Sumanth KN, Renjith George P, Karanth L, Soe HH. Management of gag reflex for patients undergoing dental treatment. Cochrane Database of Systematic Reviews 2015, Issue 10. Art. No: CD011116. [DOI: 10.1002/14651858.CD011116.pub2] [DOI] [PubMed] [Google Scholar]


