Abstract
Background
Various methods of conscious sedation and analgesia (CSA) have been used during oocyte retrieval for assisted reproduction. The choice of agent has been influenced by the quality of sedation and analgesia and by concerns about possible detrimental effects on reproductive outcomes.
Objectives
To assess the effectiveness and safety of different methods of conscious sedation and analgesia for pain relief and pregnancy outcomes in women undergoing transvaginal oocyte retrieval.
Search methods
We searched; the Cochrane Gynaecology and Fertility specialised register, CENTRAL, MEDLINE, Embase, PsycINFO and CINAHL, and trials registers in November 2017. We also checked references, and contacted study authors for additional studies.
Selection criteria
We included randomised controlled trials (RCTs) comparing different methods and administrative protocols for conscious sedation and analgesia during oocyte retrieval.
Data collection and analysis
We used standard methodological procedures expected by Cochrane. Our primary outcomes were intraoperative and postoperative pain. Secondary outcomes included clinical pregnancy, patient satisfaction, analgesic side effects, and postoperative complications.
Main results
We included 24 RCTs (3160 women) in five comparisons. We report the main comparisons below. Evidence quality was generally low or very low, mainly owing to poor reporting and imprecision.
1. CSA versus other active interventions.
All evidence for this comparison was of very low quality.
CSA versus CSA plus acupuncture or electroacupuncture
Data show more effective intraoperative pain relief on a 0 to 10 visual analogue scale (VAS) with CSA plus acupuncture (mean difference (MD) 1.00, 95% confidence interval (CI) 0.18 to 1.82, 62 women) or electroacupuncture (MD 3.00, 95% CI 2.23 to 3.77, 62 women).
Data also show more effective postoperative pain relief (0 to 10 VAS) with CSA plus acupuncture (MD 0.60, 95% CI ‐0.10 to 1.30, 61 women) or electroacupuncture (MD 2.10, 95% CI 1.40 to 2.80, 61 women).
Evidence was insufficient to show whether clinical pregnancy rates were different between CSA and CSA plus acupuncture (odds ratio (OR) 0.61, 95% CI 0.20 to 1.86, 61 women). CSA alone may be associated with fewer pregnancies than CSA plus electroacupuncture (OR 0.22, 95% CI 0.07 to 0.66, 61 women).
Evidence was insufficient to show whether rates of vomiting were different between CSA and CSA plus acupuncture (OR 1.64, 95% CI 0.46 to 5.88, 62 women) or electroacupuncture (OR 1.09, 95% CI 0.33 to 3.58, 62 women).
Trialists provided no usable data for other outcomes of interest.
CSA versus general anaesthesia
Postoperative pain relief was greater in the CSA group (0 to 3 Likert: mean difference (MD) 1.9, 95% CI 2.24 to 1.56, one RCT, 50 women).
Evidence was insufficient to show whether groups differed in clinical pregnancy rates (OR 1.00, 95% CI 0.43 to 2.35, two RCTs, 108 women, I2 = 0%).
Evidence was insufficient to show whether groups differed in rates of vomiting (OR 0.46, 95% CI 0.08 to 2.75, one RCT, 50 women) or airway obstruction (OR 0.14, 95% CI 0.02 to 1.22, one RCT, 58 women). Fewer women needed mask ventilation in the CSA group (OR 0.05, 95% CI 0.01 to 0.20, one RCT, 58 women).
Evidence was also insufficient to show whether groups differed in satisfaction rates (OR 0.66, 95% CI 0.11 to 4.04, two RCTs, 108 women, I2 = 34%; very low‐quality evidence).
Trialists provided no usable data for outcomes of interest.
2. CSA + paracervical block (PCB) versus other interventions.
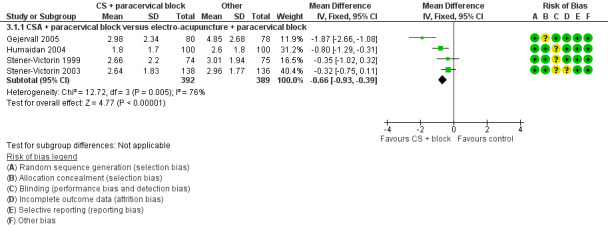
CSA + PCB versus electroacupuncture + PCB
Intraoperative pain scores were lower in the CSA + PCB group (0 to 10 VAS: MD ‐0.66, 95% CI ‐0.93 to ‐0.39, 781 women, I2 = 76%; low‐quality evidence).
Evidence was insufficient to show whether groups differed in clinical pregnancy rates (OR 0.96, 95% CI 0.72 to 1.29, 783 women, I2 = 9%; low‐quality evidence).
Trialists provided no usable data for other outcomes of interest.
CSA + PCB versus general anaesthesia
Evidence was insufficient to show whether groups differed in postoperative pain scores (0 to 10 VAS: MD 0.49, 95% CI ‐0.13 to 1.11, 50 women; very low‐quality evidence).
Evidence was insufficient to show whether groups differed in clinical pregnancy rates (OR 0.70, 95% CI 0.22 to 2.26, 51 women; very low‐quality evidence).
Trialists provided no usable data for other outcomes of interest.
CSA + PCB versus spinal anaesthesia
Postoperative pain scores were higher in the CSA + PCB group (0 to 10 VAS: MD 1.02, 95% CI 0.48 to 1.56, 36 women; very low‐quality evidence).
Evidence was insufficient to show whether groups differed in clinical pregnancy rates (OR 0.93, 95% CI 0.24 to 3.65, 38 women; very low‐quality evidence).
Trialists provided no usable data for other outcomes of interest.
CSA + PCB versus PCB
Evidence was insufficient to show whether groups differed in clinical pregnancy rates (OR 0.93, 95% CI 0.44 to 1.96, 150 women; low‐quality evidence) or satisfaction (OR 1.63, 95% CI 0.68 to 3.89, 150 women, low‐quality evidence).
Trialists provided no usable data for other outcomes of interest.
CSA + PCB versus CSA only
Evidence was insufficient to show whether groups differed in clinical pregnancy rates (OR 0.62, 95% CI 0.28 to 1.36, one RCT, 100 women; very low‐quality evidence). Rates of postoperative nausea and vomiting were lower in the CS + PCB group (OR 0.42, 95% CI 0.18 to 0.97, two RCTs, 140 women, I2 = 40%; very low‐quality evidence).
Trialists provided no usable data for other outcomes of interest.
Authors' conclusions
The evidence does not support one particular method or technique over another in providing effective conscious sedation and analgesia for pain relief during and after oocyte retrieval. Simultaneous use of sedation combined with analgesia such as the opiates, further enhanced by paracervical block or acupuncture techniques, resulted in better pain relief than occurred with one modality alone. Evidence was insufficient to show conclusively whether any of the interventions influenced pregnancy rates. All techniques reviewed were associated with a high degree of patient satisfaction. Women’s preferences and resource availability for choice of pain relief merit consideration in practice.
Plain language summary
Pain relief for women undergoing oocyte retrieval for assisted reproduction
Review question
Cochrane review authors investigated the effectiveness and safety of methods used for pain relief in women during transvaginal oocyte retrieval ‐ a technique used to collect eggs from the ovaries, to enable fertilisation outside the body.
Background
Conscious sedation comprises use of a drug or drugs to produce a state of relaxation enabling treatment to be carried out, during which verbal contact with the patient is maintained throughout the period of sedation. Conscious sedation and analgesia are methods used to relieve pain during surgery to retrieve eggs from the ovaries as part of in vitro (i.e. in an artificial environment such as a laboratory) fertilisation procedures. Concerns include that drugs used for sedation and pain relief may have an adverse effect on pregnancy rates.
Study characteristics
This review identified 24 randomised controlled trials, involving 3160 women, comparing the effects of five different methods of conscious sedation and pain relief including general anaesthesia. A randomised controlled trial uses research methods that aim to reduce bias when a new treatment is tested by allocating participants at random (i.e. by chance alone) to treatment or control treatment. The evidence is current to November 2017.
Key results
The evidence does not support one particular method or technique over another in providing effective conscious sedation and analgesia for pain relief during and after oocyte retrieval. Simultaneous use of sedation combined with analgesia such as the opiates, further enhanced by techniques of paracervical block or acupuncture, resulted in better pain relief than occurred with one method alone. Evidence was insufficient to show conclusively whether any of the interventions influenced pregnancy rates. All techniques reviewed were associated with a high degree of patient satisfaction. It would be appropriate to consider women’s preferences and choice of resources available for pain relief in practice.
Quality of the evidence
Evidence is generally of low or very low quality, mainly owing to poor reporting methods and small sample sizes with low event rates. As women vary in their experience of pain and awareness of coping strategies, the optimal method may be individualised.
Summary of findings
Background
Description of the condition
Transvaginal retrieval of oocytes from the ovary is a fundamental step of in vitro fertilisation (IVF) treatment. Although this approach is less invasive and of shorter duration than laparoscopic retrieval of oocytes, which is no longer common clinical practice, it remains a stressful and painful procedure, which requires analgesia and conscious sedation (Ng 2001).
Description of the intervention
Conscious sedation is defined by the American Society of Anaesthetists as “a drug‐induced depression of consciousness during which patients respond purposefully to verbal commands, either alone or accompanied by light tactile stimulation. No interventions are required to maintain a patent airway, and spontaneous ventilation is adequate. Cardiovascular function is usually maintained” (ASA 2015). Loss of consciousness should be unlikely due to the agents and techniques selected (Skelly 1996).
Analgesia is defined as “a state of reduced pain perception” (White 1987). An ideal analgesia is one that has the capability of offering pain relief without impairing consciousness.
Conscious sedation and analgesia may be combined for optimal effect. A variety of drugs and combinations thereof have been used to modify pain and anxiety during oocyte retrieval. Methods currently used to provide pain relief during transvaginal oocyte retrieval include conscious sedation, neuraxial anaesthesia (epidural or spinal), injection of local anaesthetic agents into the cervix (paracervical block), and alternative treatments such as acupuncture or electroacupuncture (Sharma 2015). General anaesthesia may be used for transvaginal oocyte retrieval; however, this approach has important resource requirements and many IVF units opt for conscious sedation and analgesia.
The primary goal of clinicians is to provide safe and effective sedation and analgesia that contribute to optimum surgical conditions and fast postoperative recovery. The aims of general and regional (epidural and spinal) anaesthesia are clear. The former renders the patient unconscious with no awareness of pain, and the latter achieves the endpoint of no sensation (of pain) while consciousness is maintained. Sedation, however, is much less clear or well defined than anaesthesia and has a smaller evidence base to guide practice. Giving too much or too little sedation can be hazardous, as too much sedation would be dangerous and too little would be ineffective. In addition, analgesics such as fentanyl and pethidine in high dosages can produce sedation, and intravenous anaesthetics such as propofol (sedative and analgesia) at subanaesthetic dosages can have sedative effects.
How the intervention might work
The pain experienced by patients during oocyte retrieval is caused by puncture of vaginal skin and the ovarian capsule by the aspirating needle and manipulation of the needle within the ovary during the procedure. It has been suggested that the pain associated with oocyte retrieval is intermittent rather than continuous (Zelcer 1992). Thus, an ideal strategy for pain relief is one that allows maximum flexibility to respond to the changing requirements of women undergoing oocyte retrieval. Patient‐controlled analgesia may facilitate an individualised approach by allowing women a degree of control over drug administration.
Acupuncture practices are based on the hypothesis that human physiological functions are controlled by Yin and Yang channels, which allow the flow of hypothetical “Qi” through the body (Han 2011). It is believed that blockage of these channels can lead to illness and pain. Insertion of acupuncture needles into specific acupuncture sites to resolve blockage and allow free flow of “Qi” is traditionally believed to relieve patient symptoms and is often used for pain relief (Han 2011).
Manual acupuncture involves insertion and manipulation of acupuncture needles within specific predetermined acupuncture sites. In electrical acupuncture, an additional current is administered through the acupuncture needles to stimulate acupoints (Zhao 2008).
Why it is important to do this review
Most oocyte retrievals are performed with the patient under conscious sedation: This approach is applied in 84% of IVF clinics in the UK (Elkington 2003), as well as 95% of IVF centres in the United States (Ditkoff 1997). However, 16% of UK clinics and about 50% of clinics in Germany have used general anaesthesia for IVF procedures (Rjosk 1993). Another survey showed that 48% of IVF clinics in the UK used conscious sedation; 29% general anaesthesia; 12% sedation combined with regional anaesthesia; and 2% regional anaesthesia; 9% offered a choice of anaesthesia for IVF procedures (Bokhari 1999). These reported variations in methods used for pain relief raise questions about the potential advantages and disadvantages of different methods and protocols for conscious sedation and analgesia. The efficacy of the various sedative‐analgesic combinations, including general anaesthesia, for women undergoing oocyte retrieval is of interest to practitioners. This systematic review aims to assess the effectiveness and safety of different methods of achieving conscious sedation and analgesia in women undergoing transvaginal oocyte retrieval, in terms of pain relief during and after the procedure, pregnancy outcomes, postoperative complications, and patient satisfaction.
Objectives
To assess the effectiveness and safety of different methods of conscious sedation and analgesia for pain relief and pregnancy outcomes in women undergoing transvaginal oocyte retrieval.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) only and excluded quasi‐randomised and cross‐over trials.
Types of participants
Women undergoing transvaginal oocyte retrieval during IVF treatment.
Types of interventions
Conscious sedation and analgesia versus no treatment or placebo
Conscious sedation and analgesia versus different methods such as general and spinal anaesthesia, including acupuncture and paracervical block
Different protocols of conscious sedation and analgesia such as patient‐controlled or physician‐controlled sedation
We excluded from this review trials involving the use of local anaesthesia such as vaginal lidocaine gel.
Types of outcome measures
Primary outcomes
Intraoperative pain score, defined as pain reported during or immediately after oocyte retrieval as measured on a visual analogue scale (VAS), a Likert scale, or another defined numerical or non‐numerical scale
Postoperative pain score, defined as pain reported at some time (minutes or hours) after oocyte retrieval as measured on a VAS, a Likert scale, or another defined numerical or non‐numerical scale
For the purposes of this review, we have defined postoperative pain as pain measured at some time after oocyte retrieval. In addition, none of the studies reporting pregnancy defined it, and in this review, we assumed that clinical pregnancy was reported, unless otherwise stated.
We converted to a 0 to 10 scale all VAS data related to pain.
Secondary outcomes
Live birth rate and ongoing pregnancy rate (beyond 20 weeks) per woman
Clinical pregnancy rate per woman (established by pregnancy test and confirmed by ultrasound)
Fertilisation rate per woman
Side effects of analgesia (nausea and vomiting)
Postoperative complications (airway, blood pressure, recovery time, spinal headache)
Patient satisfaction (women's reports of satisfaction with pain relief and anaesthetic care throughout the oocyte retrieval procedure)
Search methods for identification of studies
Electronic searches
We searched the Cochrane Gynaecology and Fertility Group (CGFG) Specialised Register (Procite platform), on 11 November 2017, to identify all RCTs that compared different methods of conscious sedation and analgesia for pain control during oocyte retrieval (refer to Appendix 1), without language restriction and in consultation with the CGFG Information Specialist.
We conducted electronic searches within the following electronic databases.
CENTRAL CRSO, web platform (Appendix 2) (searched 9 November 2017).
MEDLINE, Ovid platform, (Appendix 3) (searched from 1946 to 9 November 2017).
Embase, Ovid platform (Appendix 4) (searched from 1980 to 9 November 2017).
PsycINFO, Ovid platform (Appendix 5) (searched from 1806 to 9 November 2017).
CINAHL, Ebsco platform (Appendix 6) (searched from 1982 to 9 November 2017).
ClinicalTrials.gov search strategy; web platform (Appendix 7) (searched 10 January 2017).
WHO ICTRP search strategy, web platform (Appendix 8) (searched 10 December 2016).
Web of Science, web platform (Appendix 9) (searched 12 January 2017).
Portal Regional da BVS, web platform (Appendix 10) (searched 12 January 2017).
OpenGrey, web platform (Appendix 11) (searched 12 January 2017).
Searching other resources
We searched and checked the reference lists of the included studies. We translated one article from Turkish, one from Spanish, and four from Chinese.
Data collection and analysis
Selection of studies
Three review authors (IK, EP, RW) independently examined the titles and abstracts of articles retrieved by the search and retrieved full texts of all potentially eligible studies. Each review author independently applied the selection criteria to the trial reports, resolving disagreements by discussion and, if necessary, by consultation with one other review author (SB). IK contacted trial authors for clarification of details related to study eligibility such as allocation method.
Data extraction and management
We conducted data collection and analysis in accordance with the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Three review authors (IK, EP, RW) independently extracted data from eligible studies using a data extraction form designed and pilot‐tested by the review authors. Review authors were not blinded to trial authors or journal of publication when doing this. We compared results and resolved any differences by discussion. A fourth review author (SB) resolved any disagreement that arose between these three review authors. Where information provided in the published report was insufficient, IK contacted the study authors to request further information and clarification.
Assessment of risk of bias in included studies
Three review authors (IK, EP, RW) independently assessed each trial for risk of bias according to the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
We assessed random sequence generation, concealment of allocation, blinding, completeness of outcome data (including use of intention‐to‐treat analysis), and selective outcome reporting for each trial. We also assessed other potential sources of bias. We categorised each trial as having low, unclear, or high risk of bias for each domain by applying the standards described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). When the method used to conceal allocation was not reported clearly, IK contacted the study authors for clarification.
Measures of treatment effect
For dichotomous data, we used the numbers of events in control and intervention groups of each study to calculate Mantel‐Haenszel odds ratios (ORs). For continuous data, we calculated the mean difference (MD) between treatment groups. We have presented 95% confidence intervals (CIs) for all outcomes.
Unit of analysis issues
The primary analysis was per woman randomised. For reported data that did not allow valid analysis (e.g. 'per cycle' rather than 'per woman' when women contributed more than one cycle), we computed to obtain results ‘per woman’, if possible.
Dealing with missing data
We analysed data on an intention‐to‐treat basis as far as possible, and IK contacted the trial authors to request any missing data. When no additional information was forthcoming, we assumed any missing data were the result of failure to achieve the outcome.
Assessment of heterogeneity
For each meta‐analysis, we assessed statistical heterogeneity by using I2 and Chi2 statistics. We determined that substantial heterogeneity was present if I2 was greater than 50%, or if P < 0.10 in the Chi2 test for heterogeneity (Higgins 2011). For the remaining studies, we have presented a descriptive summary of study outcomes.
Assessment of reporting biases
We planned to present a funnel plot if publication bias was questionable because some trials had not been identified (Higgins 2011), but no analysis included sufficient studies to warrant this.
Data synthesis
When appropriate, we combined dichotomous data for meta‐analysis using RevMan software and the Mantel‐Haenszel method to estimate pooled ORs with 95% CIs based on a fixed‐effect model. For continuous data, we computed weighted MDs with 95% CIs, also using a fixed‐effect model in the meta‐analysis.
We classified and analysed interventions under broad categories or strategies of pain relief, for example, types of conscious sedation and analgesia methods and administration protocols. The interventions examined were so diverse that it was not possible to quantitatively combine the results of all 24 studies. However, we were able to combine the data from four trials that compared the effects of electro‐acupuncture versus conventional medical analgesia. We also attempted meta‐analysis of the four trials comparing patient‐controlled and physician‐controlled sedation and analgesia. For the remaining studies, we have presented a descriptive summary of the outcomes of each trial.
Subgroup analysis and investigation of heterogeneity
We did not perform subgroup analysis in this review. We assessed statistical heterogeneity using the Chi2 test (with P < 0.1 as evidence of significant heterogeneity) and the I2 statistic (Higgins 2011).
Sensitivity analysis
We performed sensitivity analysis for the primary outcomes to assess whether findings of the analysis were robust, or whether the conclusions would have differed if eligibility was restricted to studies without high risk of bias.
Overall quality of the body of evidence: "Summary of findings" table
We prepared "Summary of findings" tables using GRADEpro and Cochrane methods (Higgins 2011). These tables evaluate the overall quality of the body of evidence for review outcomes (intraoperative pain, postoperative pain, pregnancy outcomes, side effects of analgesia (nausea and vomiting), postoperative complications, and patient satisfaction) for the main review comparisons (conscious sedation and analgesia vs other active interventions; conscious sedation and analgesia plus paracervical block vs other active interventions). We assessed the quality of evidence using the following GRADEpro criteria: risk of bias, consistency of effect, imprecision, indirectness, and publication bias. Two review authors working independently made judgements about evidence quality (high, moderate, low, or very low) and resolved disagreements by discussion. Review authors justified, documented, and incorporated judgements into reporting of results for each outcome.
Results
Description of studies
See Characteristics of included studies.
Results of the search
In the original review, our search strategy yielded 390 reports, 27 of which were potentially eligible for inclusion in the review. After full‐text review, we excluded 16 reports because conscious sedation was not one of the comparators (see Characteristics of excluded studies). Twelve papers met our inclusion criteria (Ben‐Shlomo 1999; Bhattacharya 1997; Cook 1993; Humaidan 2004; Lok 2002; Ng 2001; Ocal 2002; Ramsewak 1990; Stener‐Victorin 1999; Stener‐Victorin 2003; Thompson 2000; Zelcer 1992). These trials involved 1350 women who underwent oocyte retrieval. For the 2012 review update, we identified nine additional studies involving 1624 women (Coskun 2011; Gejervall 2005; Guasch 2005; Gunaydin 2007; Ma 2008; Meng 2008; Meng 2009; Ozturk 2006; Sator‐Katzenschlager 2006). For the 2018 review update, we identified three new studies involving 186 women (Elnabtity 2017; Lier 2014; Matsota 2012).
The study flow is shown in Figure 1.
1.
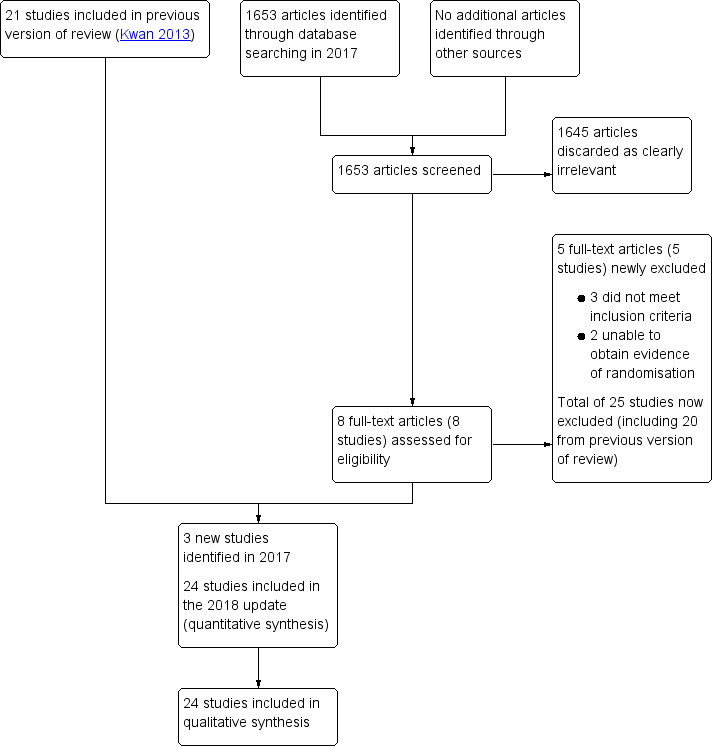
Study flow diagram.
Included studies
We included in this review a total of 24 studies involving 3160 women (see Characteristics of included studies).
Study design and setting
All 24 included studies were RCTs published between 1990 and 2017. They involved a total of 3160 women (range 30 to 700) and were conducted in Austria (N = 1), China (N = 5), Israel (N = 1), Spain (N = 1), Sweden (N = 4), the Netherlands (N = 1), Greece (N = 1), Turkey (N = 4), Eygpt (N = 1), UK (N = 4), and USA (N = 1). Two were multi‐centred trials, one involving three IVF centres (Stener‐Victorin 1999), and the other involving five IVF centres (Stener‐Victorin 2003). None of these trials reported specifically that participants included egg donors. We did not identify any quasi‐randomised or cross‐over trials.
Participants
The studies included 3160 women ‐ 1545 in control groups and 1615 in intervention groups. Two trials did not report participant age (Cook 1993; Ramsewak 1990). Overall age reported in the other studies was similar, and mean participant age was between 31 and 34 years (range 22 to 46 years). All participants were women with infertility problems due to tubal factors, endometriosis, polycystic ovary syndrome (PCOS), male factors, or unexplained infertility. Three trials reported the duration of infertility as about four to five years (Bhattacharya 1997; Elnabtity 2017; Meng 2009).
Interventions
Interventions varied substantially between studies, and review authors grouped them into five broad categories for comparison.
Conscious sedation and analgesia versus placebo (Ramsewak 1990).
Conscious sedation and analgesia versus other active interventions such as general and acupuncture anaesthesia (Ben‐Shlomo 1999; Matsota 2012; Meng 2008; Meng 2009; Sator‐Katzenschlager 2006).
Conscious sedation and analgesia plus paracervical block versus other active interventions such as general, spinal, and acupuncture anaesthesia (Gejervall 2005; Guasch 2005; Gunaydin 2007; Humaidan 2004; Ng 2001; Ozturk 2006; Stener‐Victorin 1999; Stener‐Victorin 2003).
Patient‐controlled conscious sedation and analgesia versus physician‐administered conscious sedation and analgesia (Bhattacharya 1997; Lier 2014; Lok 2002; Thompson 2000; Zelcer 1992).
Conscious sedation and analgesia with different agents or dosages (Cook 1993; Coskun 2011; Ma 2008; Ocal 2002).
Outcomes
Primary outcomes
A total of 22 studies reported intraoperative pain
In all, 11 studies reported postoperative pain (Ben‐Shlomo 1999; Elnabtity 2017; Gejervall 2005; Guasch 2005; Humaidan 2004; Lier 2014; Lok 2002; Meng 2008; Sator‐Katzenschlager 2006; Stener‐Victorin 1999; Stener‐Victorin 2003)
Two studies reported the primary outcomes of pain but did not specify whether pain was measured intraoperatively or postoperatively (Meng 2009; Thompson 2000)
Two studies did not report the primary outcomes of pain (Cook 1993; Matsota 2012)
Secondary outcomes
1/24 studies reported live birth per woman (Stener‐Victorin 1999)
2/24 studies reported ongoing pregnancy per woman (Lier 2014; Stener‐Victorin 2003)
14/24 studies reported clinical pregnancy rate per woman (Ben‐Shlomo 1999; Coskun 2011; Gejervall 2005; Guasch 2005; Humaidan 2004; Lier 2014; Lok 2002; Matsota 2012; Ng 2001; Ozturk 2006; Sator‐Katzenschlager 2006; Stener‐Victorin 1999; Stener‐Victorin 2003; Thompson 2000)
5/24 studies reported fertilisation rate per woman (Ben‐Shlomo 1999; Lok 2002; Matsota 2012; Ng 2001; Ozturk 2006)
13/24 studies reported side effects (nausea and vomiting) (Coskun 2011; Elnabtity 2017; Guasch 2005; Gunaydin 2007; Lier 2014; Ma 2008; Matsota 2012; Meng 2009; Ozturk 2006; Sator‐Katzenschlager 2006; Stener‐Victorin 1999; Stener‐Victorin 2003; Zelcer 1992)
5/24 studies reported complications (transient loss of consciousness; loss of airway) (Cook 1993; Coskun 2011; Guasch 2005; Matsota 2012; Thompson 2000)
15/24 studies reported patient satisfaction (Ben‐Shlomo 1999; Bhattacharya 1997; Cook 1993; Coskun 2011; Elnabtity 2017; Gejervall 2005; Guasch 2005; Gunaydin 2007; Lier 2014; Lok 2002; Matsota 2012; Ng 2001; Ozturk 2006; Sator‐Katzenschlager 2006; Thompson 2000)
No studies reported the incidence of abandoned procedures.
Excluded studies
See Characteristics of excluded studies.
After full‐text screening, we excluded 25 studies for the following reasons.
20/25 studies did not include conscious sedation and analgesia as a comparator.
1/25 studies did not provide clear inclusion criteria for the population and we received no response from trial authors when contacted.
1/25 studies compared conscious sedation and analgesia between different populations.
3/25 studies were abstracts, and we were unable to obtain evidence of randomisation.
Risk of bias in included studies
See Risk of bias in included studies, Figure 2, and Figure 3.
2.
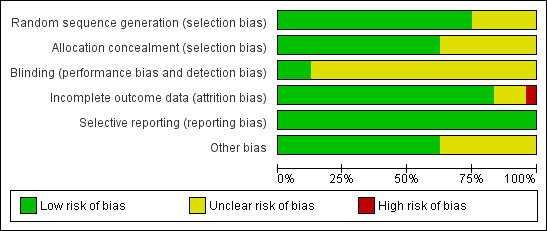
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
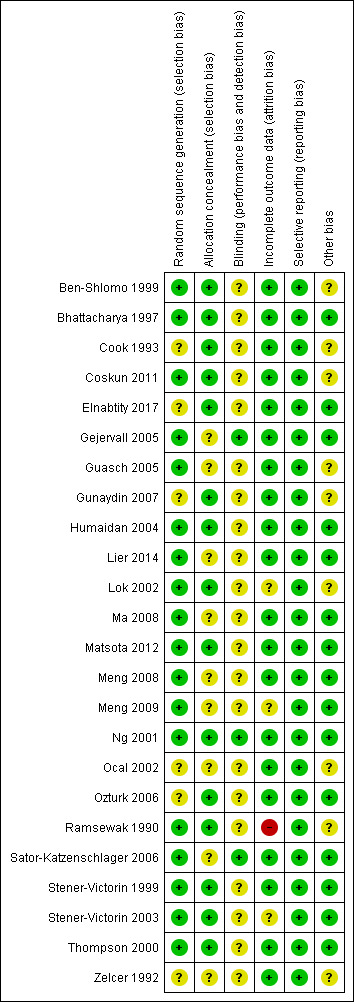
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Nineteen studies were at low risk of selection bias related to random sequence generation, as they used computer randomisation or a random numbers table. Six studies were at unclear risk of bias, as they did not describe the randomisation method used (Cook 1993; Elnabtity 2017; Gunaydin 2007; Ocal 2002; Ozturk 2006; Zelcer 1992). Eight studies did not describe allocation concealment and were at unclear risk of bias in this domain (Gejervall 2005; Guasch 2005; Lier 2014; Ma 2008; Meng 2009; Ocal 2002; Sator‐Katzenschlager 2006; Zelcer 1992).
Blinding
Blinding status could affect findings for the outcomes of pain, side effects, and women’s satisfaction. The subjective nature of pain has traditionally made it difficult to assess the efficacy of techniques for analgesia. We did not consider that blinding was likely to influence risk of performance bias for the outcomes of live birth and ongoing pregnancy. However, we noted the potential for bias for the outcomes of fertilisation and subsequent clinical pregnancy when operators were not blinded to allocation. Three studies reported adequate blinding of administrators of interventions to group allocation (Gejervall 2005; Ng 2001; Sator‐Katzenschlager 2006), and we consider these studies to be at low risk of bias. For 17 studies, blinding was not possible because of the nature of interventions such as general anaesthesia or techniques involving paracervical block (Ben‐Shlomo 1999; Bhattacharya 1997; Cook 1993; Gejervall 2005; Gunaydin 2007; Humaidan 2004; Lier 2014; Lok 2002; Matsota 2012; Meng 2008; Meng 2009; Ocal 2002; Ozturk 2006; Stener‐Victorin 1999; Stener‐Victorin 2003; Thompson 2000; Zelcer 1992), and we consider these studies to be at unclear risk of bias. Three studies described use of placebo identical to the intervention and were deemed to be at low risk of performance bias for both subjective and objective outcomes (Ng 2001; Ramsewak 1990; Sator‐Katzenschlager 2006).
Seven studies described blinding of outcome assessors for subjective outcomes of pain (Cook 1993; Gejervall 2005; Guasch 2005; Matsota 2012; Ng 2001; Sator‐Katzenschlager 2006; Zelcer 1992), and we consider these studies to be at low risk of performance bias for subjective outcomes. In one study (Coskun 2011), an independent blinded observer unaware of the women’s allocation status recorded postoperative side effects.
Incomplete outcome data
Eighteen studies analysed all or most (> 99%) randomised women, and we judged these studies to be at low risk of bias. For three studies, loss to follow‐up ranged from 4% to 20% (Lok 2002; Ramsewak 1990; Stener‐Victorin 2003). We judged these studies to be at unclear to high risk of attrition bias.
Selective reporting
All 24 studies reported outcomes prespecified in the methods section. Some outcomes such as plasma prolactin and follicular cortisol levels, sedation concentrations, recovery status, number of embryos transferred, oocyte retrieval rate, psychometric tests, and neuropeptide Y (NPY) level of follicular fluid were not of interest for this review (Cook 1993; Coskun 2011; Gejervall 2005; Guasch 2005; Gunaydin 2007; Ng 2001; Ozturk 2006); we neither extracted nor analysed these data.
Other potential sources of bias
We assessed publication bias by using a funnel plot for primary outcomes when appropriate. Ten studies did not compare causes of infertility in intervention and control groups (Ben‐Shlomo 1999; Cook 1993; Coskun 2011; Guasch 2005; Gunaydin 2007; Meng 2009; Ocal 2002; Ramsewak 1990; Thompson 2000; Zelcer 1992). Demographic details were absent from one study (Ramsewak 1990), and another study reported only women’s age (Ocal 2002). The risk of bias related to potential baseline differences between the two groups in these studies cannot be established, and we consider these studies to be at unclear risk of bias. In one study, women in the control group were younger than those in the intervention groups, although the cause of infertility was similar between groups (Lok 2002). We found no additional potential sources of other bias in the remaining studies.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5; Table 6; Table 7; Table 8
Summary of findings for the main comparison. Conscious sedation and analgesia (CSA) compared with CSA+acupuncture for women undergoing oocyte retrieval for assisted reproduction.
| Conscious sedation and analgesia (CSA) compared with CSA+acupuncture for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction Setting: assisted reproduction clinic Intervention: conscious sedation and analgesia (CSA) Comparison: CSA + acupuncture | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with CSA + acupuncture |
Risk with CSA only (95% CI) |
|||||
| Intraoperative pain | Mean intraoperative pain score in the comparison group was 4.9 points on a 0 to 10 VAS. | Mean score in the CSA‐only group was 1 point higher (0.18 higher to 1.82 higher) | ‐ | 62 (1 RCT) | ⊕⊝⊝⊝ VERY LOWa,b | |
| Postoperative pain | Mean postoperative pain score in the comparison group was 3.2 on a 0 to 10 VAS. | Mean score in the CSA‐only group was 0.6 points higher (0.1 lower to 1.3 higher) | ‐ | 61 (1 RCT) | ⊕⊝⊝⊝ VERY LOWa,b | |
| Pregnancy | 344 per 1000 | 242 per 1000 (95 to 493) |
OR 0.61 (0.20 to 1.86) |
61 (1 RCT) | ⊕⊝⊝⊝ VERY LOWa,b | |
| Patient satisfaction | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Side effects (postoperative vomiting and/or vomiting) | 156 per 1000 | 233 per 1000 (78 to 521) | OR 1.64 (0.46 to 5.88) | 62 (1 RCT) | ⊕⊝⊝⊝ VERY LOWa,b | |
| Postoperative complications | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; CSA: conscious sedation and analgesia; OR: odds ratio; VAS: visual analogue scale. | ||||||
| GRADE Working Group grades of evidence. High quality: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect. Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains.
bDowngraded two levels for very serious imprecision: very small sample size and low event rate and/or wide confidence intervals compatible with benefit in either group or no effect.
Summary of findings 2. Conscious sedation and analgesia (CSA) compared with CSA + electro‐acupuncture for women undergoing oocyte retrieval for assisted reproduction.
| Conscious sedation and analgesia (CSA) compared with CSA + electro‐acupuncture for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction Setting: assisted reproduction clinic Intervention: conscious sedation and analgesia (CSA) Comparison: CSA + electro‐acupuncture | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with CSA + electro‐acupuncture |
Risk with CSA only (95% CI) |
|||||
| Intraoperative pain | Mean intraoperative pain score in the comparison group was 2.9 points on a 0 to 10 VAS. | Mean score in the CSA‐only group was 3 points higher (2.23 higher to 3.77 higher). | ‐ | 62 (1 RCT) | ⊕⊝⊝⊝ VERY LOWa,b | |
| Postoperative pain | Mean postoperative pain score in the comparison group was 1.1 on a 0 to 10 VAS. | Mean score in the CSA‐only group was 2.1 points higher (1.4 higher to 2.8 higher). | ‐ | 61 (1 RCT) | ⊕⊝⊝⊝ VERY LOWa,b | |
| Pregnancy | 594 per 1000 | 243 per 1000 (95 to 491) |
OR 0.22 (0.07 to 0.66) |
61 (1 RCT) | ⊕⊝⊝⊝ VERY LOWa,b | |
| Patient satisfaction | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Side effects (postoperative vomiting and/or vomiting) | 218 per 1000 | 233 per 1000 (97 to 624) | OR 1.09 (0.33 to 3.58) | 62 (1 RCT) | ⊕⊝⊝⊝ VERY LOWa,b | |
| Postoperative complications | Airway obstruction: No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Need for mask ventilation: No studies reported this outcome. | Not estimable | ‐ | ‐ | |||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio; VAS: visual analogue scale. | ||||||
| GRADE Working Group grades of evidence. High quality: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect. Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains.
bDowngraded two levels for very serious imprecision: very small sample size and event rate.
Summary of findings 3. Conscious sedation and analgesia compared with general analgesia for women undergoing oocyte retrieval for assisted reproduction.
| Conscious sedation and analgesia (CSA) compared to general analgesia for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction Setting: assisted reproduction clinic Intervention: conscious sedation and analgesia Comparison: general analgesia (GA) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with GA |
Risk with CSA only (95% CI) |
|||||
| Intraoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Postoperative pain | Mean postoperative pain score in the comparison group was 2.1 points on a 0 to 3 Likert scale. | Mean score in the CSA‐only group was 1.9 points lower (2.24 lower to 1.56 lower). | ‐ | 50 (1 RCT) | ⊕⊝⊝⊝ VERY LOWa,b | |
| Pregnancy | 278 per 1000 | 278 per 1000 (142 to 475) |
OR 1.00 (0.43 to 2.35) |
108 (2 RCTs) | ⊕⊝⊝⊝ VERY LOWa,b | |
| Patient satisfaction (report of 'satisfactory') | 981 per 1000 | 972 per 1000 (854 to 995) |
OR 0.66 (0.11 to 4.04) |
108 (2 RCTs) | ⊕⊝⊝⊝ VERY LOWa,b | |
| Side effects (postoperative vomiting and/or vomiting) | 160 per 1000 | 81 per 1000 (15 to 344) | OR 0.46 (0.08 to 2.75) | 50 (1 RCT) | ⊕⊝⊝⊝ VERY LOWa,b | |
| Postoperative complications | Airway obstruction: 207 per 1000 | 35 per 1000 (5 to 241) | OR 0.14 (0.02 to 1.22) | 58 (1 RCT) | ⊕⊝⊝⊝ VERY LOWa,b | |
| Need for mask ventilation: 793 per 1000 | 161 per 1000 (37 to 434) | OR 0.05 (0.01 to 0.20) | 58 (1 RCT) | ⊕⊝⊝⊝ VERY LOWa,b | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio; RCT: randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence. High quality: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect. Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded two levels for very serious imprecision: very small sample size and event rate and/or wide confidence intervals compatible with benefit in either group or no effect.
bDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains.
Summary of findings 4. Conscious sedation and analgesia (CSA) + paracervical block (PCB) versus electro‐acupuncture + PCB.
| Conscious sedation and analgesia (CSA) plus PCB compared with electro‐acupuncture plus PCB for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction Setting: assisted reproduction clinic Intervention: CSA + PCB Comparison: electro‐acupuncture + PCB | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with electro‐acupuncture + PCB |
Risk with CSA + PCB (95% CI) |
|||||
| Intraoperative pain | Mean intraoperative pain score in the comparison group was 2.6 to 4.85 points on a 0 to 10 VAS. | Mean score in the CSA‐only group was 0.66 points lower (0.93 lower to 0.39 lower). | ‐ | 781 (4 RCTs) | ⊕⊕⊝⊝ LOWa,b | |
| Postoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Pregnancy | 367 per 1000 | 358 per 1000 (295 to 428) |
OR 0.96 (0.72 to 1.29) |
783 (4 RCTs) | ⊕⊕⊝⊝ LOWa,c | |
| Patient satisfaction | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Side effects (postoperative vomiting and/or vomiting) | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Postoperative complications | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio; RCT: randomised controlled trial; VAS: visual analogue scale. | ||||||
| GRADE Working Group grades of evidence. High quality: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect. Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains.
bDowngraded one level for serious inconsistency (I2 = 76%).
cDowngraded one level for serious imprecision: wide confidence intervals compatible with benefit in either group or no effect.
Summary of findings 5. Conscious sedation and analgesia (CSA) + paracervical block (PCB) versus general anaesthesia.
| Conscious sedation and analgesia (CSA) plus paracervical block (PCB) compared with general anaesthetic (GA) for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction Setting: assisted reproduction clinic Intervention: CSA + PCB Comparison: GA | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with GA |
Risk with CSA + PCB (95% CI) |
|||||
| Intraoperative pain | ||||||
| Postoperative pain | Mean postoperative pain score in the comparison group was 0.68 points on a 0 to 10 VAS. | Mean score in the CSA‐only group was 0.49 points higher (0.13 lower to 1.11 higher). | ‐ | 50 (1 RCT) | ⊕⊝⊝⊝ VERY LOWa,b | |
| Pregnancy | 375 per 1000 | 296 per 1000 (117 to 576) |
OR 0.70 (0.22 to 2.26) |
51 (1 RCT) | ⊕⊝⊝⊝ VERY LOWa,b | |
| Patient satisfaction | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Postoperative complications | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio; RCT: randomised controlled trial; VAS: visual analogue scale. | ||||||
| GRADE Working Group grades of evidence. High quality: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect. Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains.
bDowngraded two levels for very serious imprecision: small sample size and low event rate, wide confidence intervals compatible with benefit in either group or no effect.
Summary of findings 6. Conscious sedation and analgesia (CSA) + paracervical block (PCB) versus spinal anaesthesia.
| Conscious sedation and analgesia (CSA) plus paracervical block (PCB) compared with spinal anaesthesia for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction Setting: assisted reproduction clinic Intervention: CSA + PCB Comparison: spinal anaesthesia | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with spinal anaesthesia |
Risk with CSA + PCB (95% CI) |
|||||
| Intraoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Postoperative pain | Mean postoperative pain score in the comparison group was 0.15 on a 0 to 10 VAS, | Mean score in the CSA‐only group was 1.02 points higher (0.48 higher to lower to 1.56 higher). | ‐ | 36 (1 RCT) | ⊕⊝⊝⊝ VERY LOWa,b | |
| Pregnancy | 375 per 1000 | 358 per 1000 (126 to 687) |
OR 0.93 (0.24 to 3.65) |
38 (1 RCT) | ⊕⊝⊝⊝ VERY LOWa,b | |
| Patient satisfaction | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Side effects (postoperative vomiting and/or vomiting) | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Postoperative complications | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio; RCT: randomised controlled trial; VAS: visual analogue scale. | ||||||
| GRADE Working Group grades of evidence. High quality: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect. Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains.
bDowngraded two levels for very serious imprecision: very small sample size and low event rate, wide confidence intervals compatible with benefit in either group or no effect.
Summary of findings 7. Conscious sedation and analgesia (CSA) + paracervical block (PCB) versus PCB.
| Conscious sedation and analgesia (CSA) plus paracervical block (PCB) compared with PCB only for women undergoing oocyte retrieval for assisted reproduction | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction Setting: assisted reproduction clinic Intervention: CSA + PCB Comparison: PCB only | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with PCB only |
Risk with CSA + PCB (95% CI) |
|||||
| Intraoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ‐ | |
| Postoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ‐ | |
| Pregnancy | 253 per 1000 | 240 per 1000 (130 to 399) |
OR 0.93 (0.44 to 1.96) |
150 (1 RCT) | ⊕⊕⊝⊝ LOWa | |
| Patient satisfaction | 800 per 1000 | 867 per 1000 | OR 1.63 (0.68 to 3.89) |
150 (1 RCT) | ⊕⊕⊝⊝ LOWa | |
| Side effects (postoperative vomiting and/or vomiting) | No studies reported this outcome | Not estimable | ‐ | ‐ | ||
| Postoperative complications | No studies reported this outcome | Not estimable | ‐ | ‐ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio; RCT: randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence. High quality: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect. Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded two levels for very serious imprecision: low event rates and wide confidence intervals compatible with benefit in either group or no effect.
Summary of findings 8. Conscious sedation and analgesia (CSA) + paracervical block (PCB) versus CSA.
| Conscious sedation and analgesia (CSA) plus paracervical block (PCB) compared with CSA alone | ||||||
| Patient or population: women undergoing oocyte retrieval for assisted reproduction Setting: assisted reproduction clinic Intervention: CSA + PCB Comparison: CSA alone | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with CSA alone |
Risk with CSA + PCB (95% CI) |
|||||
| Intraoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Postoperative pain | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Pregnancy | 600 per 1000 | 482 per 1000 (296 to 671) |
OR 0.62 (0.28 to 1.36) |
100 (1 RCT) | ⊕⊝⊝⊝ VERY LOWa,b | |
| Patient satisfaction | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| Side effects (postoperative vomiting and/or vomiting) | 300 per 1000 | 153 per 1000 (72 to 294) | OR 0.42 (0.18 to 0.97) | 140 (2 RCTs) | ⊕⊝⊝⊝ VERY LOWa,b | |
| Postoperative complications | No studies reported this outcome. | Not estimable | ‐ | ‐ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio; RCT: randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence. High quality: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect. Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level for serious risk of bias: unclear risk of bias in one or two domains.
bDowngraded two levels for very serious imprecision: small sample size, very low event rates, and wide confidence intervals compatible with benefit in the CSA + PCB group or with no meaningful effect.
We have summarised the effects of interventions as follows.
Conscious sedation and analgesia versus placebo.
Conscious sedation and analgesia versus other active interventions.
Conscious sedation plus paracervical block versus other active interventions.
Conscious sedation and analgesia: patient‐controlled versus physician‐controlled.
Conscious sedation and analgesia via different agents or dosages.
1. Conscious sedation and analgesia versus placebo
Only one study made this comparison (Ramsewak 1990).
Primary outcome
1.1 Intraoperative pain
Conscious sedation and analgesia was associated with less pain than placebo during needle insertion (mean difference (MD) on 0 to 10 VAS ‐1.70, 94% CI ‐2.38 to ‐1.02; N = 24; Analysis 1.1) and with less pain during follicle aspiration (MD on 0 to 10 VAS ‐1.30, 95% CI ‐1.88 to ‐0.72; N = 24; Analysis 1.2).
1.1. Analysis.
Comparison 1 Conscious sedation + analgesia (CSA) versus placebo, Outcome 1 Pain during needle insertion (VAS 0 to 10).
1.2. Analysis.
Comparison 1 Conscious sedation + analgesia (CSA) versus placebo, Outcome 2 Pain during follicle aspiration (VAS 0 to 10).
Other outcomes were not reported.
2. Conscious sedation and analgesia (CSA) versus other active interventions
Five studies made the following comparisons.
CSA plus placebo acupuncture versus CSA plus electro‐acupuncture or acupuncture (Sator‐Katzenschlager 2006).
CSA versus CSA plus electro‐acupuncture (Meng 2008; Meng 2009).
CSA versus general anaesthesia (Ben‐Shlomo 1999; Matsota 2012).
Primary outcomes
2.1 Intraoperative pain
See Analysis 2.1.
2.1. Analysis.
Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 1 Intraoperative pain.
CSA plus placebo acupuncture versus CSA plus acupuncture or electro‐acupuncture
CSA plus placebo acupuncture (i.e. CSA without acupuncture) was associated with a higher pain score during oocyte retrieval than CSA plus acupuncture (MD on 0 to 10 VAS 1.00, 95% CI 0.18 to 1.82; N = 62; very low‐quality evidence) or CSA plus electro‐acupuncture (MD on 0 to 10 VAS 3.00, 95% CI 2.23 to 3.77; N = 62; very low‐quality evidence) (Sator‐Katzenschlager 2006).
This finding was supported by another study in which CSA only was associated with more pain during oocyte retrieval than conscious sedation plus electro‐acupuncture (MD on 1 to 12 numerical rating scale 1.7, 95% CI 1.07 to 2.33; N = 316). In this study, 99/170 (58%) versus 120/146 (82%) women rated pain as mild; 69/170 (41%) versus 23/146 (16%) rated pain as moderate; and 2/170 (1.2%) versus 3/146 (2%) rated pain as severe (P < 0.01) during oocyte retrieval (Meng 2008).
2.2 Postoperative pain
See Analysis 2.2.
CSA plus acupuncture versus CSA plus acupuncture or electro‐acupuncture
Postoperative pain was greater in the CSA plus placebo acupuncture (i.e. CSA without acupuncture) group than in the CSA plus acupuncture group (MD on 0‐10 VAS 0.60, 95% CI ‐0.10 to 1.30; N = 61; very low‐quality evidence) (Figure 4Sator‐Katzenschlager 2006).
4.
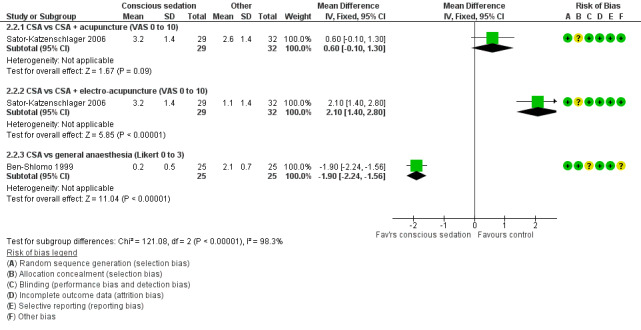
Forest plot of comparison: 2 Conscious sedation + analgesia (CSA) versus other active interventions, outcome: 2.2 Postoperative pain.
CSA plus placebo acupuncture was associated with a higher pain score after oocyte retrieval than conscious sedation plus electro‐acupuncture (MD on 0‐10 VAS 2.10, 95% CI 1.40 to 2.80; N = 61; very low‐quality evidence) (Sator‐Katzenschlager 2006).
This finding was supported by two other studies, which reported binary data, and in which conscious sedation only was associated with more pain at one hour postoperatively when compared with conscious sedation plus electro‐acupuncture (100/170 (59%) vs 47/146 (32%) reported pain), as well as at two to five hours postoperatively (70/170 (42%) vs 38/146 (26%) reported pain; P < 0.01; N = 316) (Meng 2008). Similarly, conscious sedation plus electro‐acupuncture was reported to be associated with lower cumulative pain scores than conscious sedation alone (insufficient data details; N = 694) (Meng 2009).
CSA versus general anaesthesia
CSA was associated with less pain (Likert scale 0 to 3) 30 minutes after completion of the procedure when compared with general anaesthesia (MD on 0 to 3 Likert scale ‐1.90, 95% CI ‐2.24 to ‐1.56; N = 50; very low‐quality evidence) (Ben‐Shlomo 1999).
Secondary outcomes
2.3 Live birth rate and ongoing pregnancy rate
These outcomes were not reported.
2.4 Clinical pregnancy rate
See Analysis 2.3.
Data show no clear evidence of a difference in pregnancy rate between CSA plus placebo and CSA plus acupuncture (OR 0.61, 95% CI 0.20 to 1.86; N = 61; P = 0.38; very low‐quality evidence) (Sator‐Katzenschlager 2006).
CSA plus placebo acupuncture was associated with a lower pregnancy rate per woman when compared with CSA plus electro‐acupuncture (OR 0.22, 95% CI 0.07 to 0.66; N = 61; very low‐quality evidence) (Sator‐Katzenschlager 2006).
Two studies reported that when researchers compared CSA with general anaesthetic, they found no evidence of a difference in the clinical pregnancy rate per woman (OR 1.00, 95% CI 0.43 to 2.35; two RCTs; N = 108; I2 = 0%; very low‐quality evidence; Analysis 2.3) (Ben‐Shlomo 1999; Matsota 2012).
2.5 Fertilisation rate
No study reported this outcome. One study reported oocyte fertilisation rate per oocytes retrieved (Matsota 2012).
2.6 Abandoned procedure of oocyte retrieval
This outcome was not reported.
2.7 Side effects of analgesia
See Analysis 2.4.
When investigators compared CSA plus placebo acupuncture versus CSA plus acupuncture, they provided insufficient evidence to show whether there was a difference in the number of women reporting nausea during oocyte retrieval (OR 1.64, 95% CI 0.46 to 5.88; N = 62; very low‐quality evidence). Similarly, when comparing CSA plus placebo acupuncture versus conscious sedation plus electro‐acupuncture, investigators found no clear evidence of differences between groups for this outcome (OR 1.09, 95% CI 0.33 to 3.58; N = 62; very low‐quality evidence). Two of 29 women (7%) in the CSA plus placebo group reported nausea and vomiting versus none in the other two groups one hour post treatment (Sator‐Katzenschlager 2006).
When investigators compared CSA plus placebo acupuncture versus conscious sedation plus electro‐acupuncture, they found no clear evidence of a difference in reported side effects for nausea and vomiting during oocyte retrieval (17/146 (12%) vs 28/170 (16%) and 3/146 (2%) vs 3/170 (1.8%), respectively; N = 80) nor at one hour postoperatively (13/146 (9%) vs 19/170 (11%) and 4/146 (2.7%) vs 2/170 (1.2%), respectively) nor at two to five hours postoperatively (15/146 (10%) vs 26/170 (15%) and 11/146 (7.5%) vs 15/170 (9%), respectively) (Meng 2008).
When comparing CSA with general anaesthetic, researchers found insufficient evidence to show whether there was a difference in postoperative vomiting (OR 0.46, 95% CI 0.08 to 2.75; N = 50) (Ben‐Shlomo 1999). In another study, researchers found no evidence of a difference in the number of women experiencing fewer than two episodes of vomiting (0/29 (0%) versus 2/29 (6.9%), and women experiencing more than two episodes of vomiting (0/29 (0%) versus 0/29 (0%), P = 0.15; respectively) (Matsota 2012).
2.8 Postoperative complications
See Analysis 2.6 and Analysis 2.7.
When comparing CSA versus general anaesthetic, investigators found no clear evidence of a difference in the rate of airway obstruction (OR 0.14, 95% CI 0.02 to 1.22; N = 58; very low‐quality evidence), but fewer women in the conscious sedation group needed mask ventilation (OR 0.05, 95% CI 0.01 to 0.20; N = 58; very low‐quality evidence) (Matsota 2012).
2.9 Patient satisfaction
When comparing CSA versus general anaesthesia, researchers found that women in both CSA and general anaesthesia groups were satisfied with the modality of pain relief and provided no evidence of a difference between groups, at 24/25 (96%) versus 25/25 (100%) (Ben‐Shlomo 1999). In another study, in which researchers did not assess pain as an outcome, women in both CSA and general anaesthesia groups were satisfied with treatment and were willing to repeat the procedure using the same anaesthesia protocols (27/29 (93%) vs 29/29 (100%)) (Matsota 2012). Combined data from these two studies show an OR of 0.66 (95% CI 0.11 to 4.04; two RCTs; N = 108; I2 = 34%; very low‐quality evidence; Analysis 2.5) (Ben‐Shlomo 1999; Matsota 2012).
2.5. Analysis.
Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 5 Satisfaction.
3. Conscious sedation plus paracervical block (PCB) versus other active interventions
Eight studies compared these interventions as follows.
CSA plus PCB versus general anaesthesia (Guasch 2005).
CSA plus PCB versus spinal anaesthesia (Guasch 2005).
CSA plus PCB versus placebo plus PCB (Ng 2001).
CSA plus PCB versus CSA alone (Gunaydin 2007; Ozturk 2006).
CSA plus PCB versus electro‐acupuncture plus PCB (Gejervall 2005; Humaidan 2004; Stener‐Victorin 1999; Stener‐Victorin 2003).
Primary outcomes
3.1 Intraoperative pain
See Analysis 3.1 and Figure 5.
3.1. Analysis.
Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 1 Intraoperative pain (VAS 0 to 10).
5.
Forest plot of comparison: 3 Conscious sedation + paracervical block versus other interventions, outcome: 3.1 Intraoperative pain (VAS).
Four trials reported data suitable for analysis (Gejervall 2005; Humaidan 2004; Stener‐Victorin 1999; Stener‐Victorin 2003), showing that CSA plus PCB was associated with less intraoperative pain during oocyte retrieval when compared with electro‐acupuncture plus PCB MD on a VAS 0 to 10 scale of ‐0.66 (95% CI ‐0.93 to ‐0.39; four RCTs; N = 781; I2 = 76%; low‐quality evidence). Heterogeneity was high, but the direction of effect was consistent.
Three trials reported data unsuitable for analysis (Gunaydin 2007; Ng 2001; Ozturk 2006).
Investigators in Ng 2001 found that CSA plus PCB was associated with less pain when compared with placebo plus PCB (median on 0 to 10 VAS scale 1.2 vs 3.0 during vaginal punctures, and 1.65 vs 4.30 for corresponding abdominal pain, respectively).
When comparing CSA plus PCB versus CSA only, researchers measured pain at five‐minute intervals during oocyte retrieval and found that CSA plus PCB was associated with less pain (mean VAS) when compared with CSA only (data presented graphically; N = 40) (Gunaydin 2007). Trialists considered a pain score higher than 3 on a simple numerical rating scale (SNRS) as significant. In a second study of the same comparison, CSA plus PCB was associated with less pain than CSA only at the first ovarian puncture (SNRS > 3: 0/50 (0%) vs 6/50 (12%); P < 0.05; N = 100) but SNRS scores at the second ovarian puncture were similar in the two groups (SNRS > 3: 3/50 (6%) vs 3/50 (6%); N = 100) (Ozturk 2006).
3.2 Postoperative pain
See Analysis 3.2.
3.2. Analysis.
Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 2 Postoperative pain.
CSA plus PCB was associated with a higher pain score at four hours postoperatively than was obtained with general anaesthesia (MD on 0 to 10 VAS scale of 0.49, 95% CI ‐0.13 to 1.11; N = 50; very low‐quality evidence). CSA plus PCB was associated with a higher pain score when compared with spinal anaesthesia (MD on 0 to 10 VAS scale 1.02, 95% CI 0.48 to 1.56; N = 36; very low‐quality evidence) (Guasch 2005).
Trials yielding data unsuitable for analysis have reported that when CSA plus PCB was compared with electro‐acupuncture plus PCB, data show no difference in pain between the two groups at 30 minutes (Humaidan 2004) nor at 60 minutes (Gejervall 2005) after oocyte retrieval. At two hours after retrieval, one trial found less pain in the electro‐acupuncture plus PCB group than in the CSA plus PCB group (median VAS 1.1, 95% CI 0 to 7 vs 1.6, 95% CI 0 to 9; P < 0.01; N = 274) (Stener‐Victorin 2003), but the other trial reported no meaningful differences between groups (mean VAS 2.29 (SD 2.34) vs 2.18 (SD 2.14); N = 149) (Stener‐Victorin 1999).
Secondary outcomes
3.3 Live birth rate and ongoing pregnancy rate
See Analysis 3.3.
3.3. Analysis.
Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 3 Live birth or ongoing pregnancy.
CSA plus PCB was associated with a higher live birth rate per woman than was electro‐acupuncture plus PCB (OR 2.35, 95% CI 1.09 to 5.05; N = 149) (Stener‐Victorin 1999). Researchers provided no clear evidence of a difference between the two groups in ongoing pregnancy rates per woman (OR 0.86, 95% CI 0.50 to 1.47; N = 274) (Stener‐Victorin 2003).
3.4 Clinical pregnancy rate
See Analysis 3.4.
3.4. Analysis.
Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 4 Pregnancy.
Evidence is insufficient to show whether there was a difference in pregnancy rates when researchers compared CSA versus general anaesthesia (OR 0.70, 95% CI 0.22 to 2.26; N = 51; very low‐quality evidence) or versus spinal anaesthesia (OR 0.93, 95% CI 0.24 to 3.65; N = 38; very low‐quality evidence) (Guasch 2005).
When CSA with PCB was compared with placebo plus PCB, evidence was insufficient to show whether there was a difference between the two groups in clinical pregnancy rate (OR 0.93, 95% CI 0.44 to 1.96; N = 150; Analysis 3.4) (Ng 2001).
Data show no evidence of a difference in pregnancy rates between electro‐acupuncture plus PCB and CSA plus PCB (OR 0.96, 95% CI 0.72 to 1.29; four RCTs; N = 783; I2 = 9%) and no significant heterogeneity (P = 0.78; Analysis 3.4) (Gejervall 2005; Humaidan 2004; Stener‐Victorin 1999; Stener‐Victorin 2003).
CSA plus PCB was associated with a lower pregnancy rate per woman when compared with CSA alone (OR 0.62, 95% CI 0.28 to 1.36; N = 100) (Ozturk 2006).
3.5 Fertilisation rate
Comparison of CSA with PCB versus placebo plus PCB yielded no evidence of a difference between the two groups in fertilisation rates (OR 0.83, 95% CI 0.42 to 1.66; N = 150; Analysis 3.5) (Ng 2001).
3.5. Analysis.
Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 5 Fertilisation rate per woman.
Comparison of CSA alone versus CSA with PCB yielded no evidence of a difference between groups in fertilisation rate per woman (35/50 (69.8%) vs 37/50 (73.3%); N = 100) (Ozturk 2006).
3.6 Abandoned procedure of oocyte retrieval
This outcome was not reported.
3.7 Side effects of analgesia
Two trials compared CSA and PCB versus CSA alone (Gunaydin 2007; Ozturk 2006). CSA with PCB was associated with a lower likelihood of nausea and vomiting when compared with CSA only (OR 0.42, 95% CI 0.18 to 0.97; two RCTs; N = 140; I2 = 40%; very low‐quality evidence). Data show no statistically significant heterogeneity (P = 0.26; Analysis 3.6).
3.6. Analysis.
Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 6 Postoperative nausea and/or vomiting.
Two trials reported data unsuitable for analysis (Guasch 2005; Ng 2001).
Trials comparing CSA plus PCB versus electro‐acupuncture plus PCB have provided no evidence of a difference in reports of nausea between the two groups at recovery (mean VAS 6.5 (13.0) vs 4.6 (8.8); N = 158) (Gejervall 2005) or at two hours after oocyte retrieval (mean VAS 4.1 (SD 8.0) vs 3.0 (SD 7.2); N = 149) (Stener‐Victorin 1999). Another study reported less nausea in the electro‐acupuncture and PCB group (2/136 (1.5%) vs 13/138 (9.4%) (VAS < 75; P < 0.01; N = 274) (Stener‐Victorin 2003).
3.8 Postoperative complications
This outcome was not reported.
3.9 Patient satisfaction
Comparisons of CSA plus PCB versus general or spinal anaesthesia show that all women reported a high degree of satisfaction (90% vs 88% vs 90%, respectively) (Guasch 2005).
Comparisons of CSA with PCB versus placebo plus PCB yielded no evidence of a difference in satisfaction rates, at 88% versus 80% who were very satisfied or satisfied (OR 1.63, 95% CI 0.68 to 3.89; N = 150; Analysis 3.7) (Ng 2001).
3.7. Analysis.
Comparison 3 Conscious sedation + analgesia (CSA) + paracervical block versus other interventions, Outcome 7 Patient satisfaction by Likert scale: report of 'excellent and satisfactory'.
Comparisons of CSA with PCB versus CSA alone yielded no evidence of a difference in satisfaction rates between groups in either trial (47/50 (94%) vs 48/50 (96%) and 20/20 (100%) vs 20/20 (100%) rated satisfaction as moderate and good, respectively) (Gunaydin 2007; Ozturk 2006).
Data show that when CSA plus PCB was compared with electro‐acupuncture plus PCB, electro‐acupuncture plus PCB was associated with a higher satisfaction score in relation to oocyte aspiration than CSA plus PCB (VAS 15.3 (SD 16.3) vs 9.8 (SD 12.6); P = 0.039; N = 158) (Gejervall 2005).
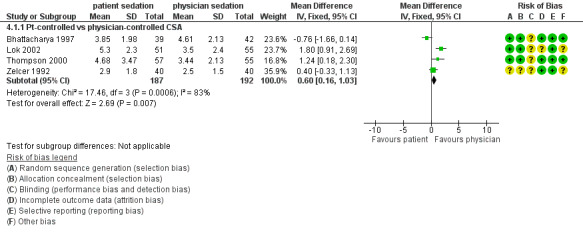
4. Patient‐controlled conscious sedation and analgesia (CSA) versus physician‐controlled CSA
Five studies compared these interventions (Bhattacharya 1997; Lier 2014; Lok 2002; Thompson 2000; Zelcer 1992). One of these studies reported that patient‐controlled CSA was administered with the use of inhalational isodesox (Thompson 2000).
Primary outcomes
4.1 Intraoperative pain
Two trials found that patient‐controlled CSA was associated with higher pain scores than were reported with physician‐controlled CSA (mean VAS 0 to 10 scale 5.3 vs 3.5; N = 106; and 4.68 vs 3.41; N = 112, respectively) (Lok 2002; Thompson 2000). Trialists in the other two studies found no evidence of a difference between groups (mean VAS 0 to 10 scale 3.85 vs 4.63; N = 81; and 2.9 vs 2.5; N = 80, respectively) (Bhattacharya 1997; Zelcer 1992). Combined data on intraoperative pain scores from these four trials show a mean difference in VAS of 0.60 (95% CI 0.16 to 1.03; four RCTs; N = 379; I2 = 83%; Analysis 4.1) (Figure 6) and significant heterogeneity (P = 0.006) favouring physician‐controlled CSA. Exclusion of the single trial in which patient‐controlled CSA was administered with the use of inhalational isodesox yielded a mean VAS score of 0.47 (95% CI ‐0.01 to 0.95; three RCTs; N = 271; I2 = 87%; Analysis 4.2) and significant statistical heterogeneity (P = 0.004) (Thompson 2000).
4.1. Analysis.
Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 1 Intraoperative pain score (VAS 0 to 10).
6.
Forest plot of comparison: 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), outcome: 4.1 Intraoperative pain score (VAS 0 to 10).
4.2. Analysis.
Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 2 Intraoperative pain score excluding inhalational sedation/analgesia (VAS 0 to 10).
In a study without data suitable for analysis, the numeric rating scale (NRS) pain score in the patient‐controlled CSA group was lower than in the physician‐administered CSA group but the difference did not reach statistical significance (median NRS 4 (3 to 7) vs 6 (4 to 8); P = 0.13; one RCT; N = 76) (Lier 2014).
4.2 Postoperative pain
Patient‐controlled CSA was associated with higher pain scores than physician‐controlled CSA two hours after oocyte retrieval (MD on a 0 to 10 VAS scale 1.20, 95% CI 0.26 to 2.14; N = 106; Analysis 4.3) (Lok 2002).
4.3. Analysis.
Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 3 Postoperative pain score (VAS 0 to 10).
In the study without data suitable for analysis, the pain score in the patient‐controlled CSA group 30 minutes after oocyte retrieval was higher than in the physician‐controlled CSA group (median NRS 2 (1 to 5) vs 1 (0 to 3); P = 0.016; N = 76), but this occurred at the cost of higher sedation in the physician‐controlled CSA group. Pain and discomfort five days post puncture were similar between the two groups (pain scores in NRS presented graphically) (Lier 2014).
Secondary outcomes
4.3 Ongoing pregnancy rate and clinical pregnancy rate
Data show no clear evidence of a difference in pregnancy rates per woman between patient‐controlled and physician‐administered CSA (OR 0.90, 95% CI 0.51 to 1.60; three RCTs; N = 294; I2 = 0%; P = 0.48; Analysis 4.4) (Lier 2014; Lok 2002; Thompson 2000).
4.4. Analysis.
Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 4 Pregnancy rate per woman.
4.4 Fertilisation rate
Comparisons of patient‐controlled CSA versus physician‐administered CSA yielded no evidence of a difference between the two groups in fertilisation rate per woman (OR 1.17, 95% CI 0.54 to 2.50; N = 106; Analysis 4.5) (Lok 2002).
4.5. Analysis.
Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 5 Fertilisation rate per woman.
4.5 Abandoned procedure of oocyte retrieval
One study reported that oocyte retrieval was completed in all trial participants (Lier 2014).
4.6 Side effects of analgesia
Comparisons of patient‐controlled CSA versus physician‐administered CSA yielded no evidence of a difference between the two groups in the degree of nausea noted during retrieval (nausea score 5.0 (SD 9.0) vs 9.0 (SD 18.0)) or two hours after oocyte retrieval (nausea score 7.0 (SD 1.0) vs 13.0 (18.0)) (Lok 2002) nor in the occurrence of postoperative nausea (8% vs 8%) (OR 1.00, 95% CI 0.19 to 5.28; N = 80; Analysis 4.6) and vomiting (3% vs 0%) (Zelcer 1992).
4.6. Analysis.
Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 6 Postoperative nausea: no. of patients.
Data show no evidence of a difference between the patient‐controlled CSA group and the physician‐controlled CSA group in reports of 'drowsiness or spinning sensations' and 'dry mouth' during the oocyte retrieval procedure (20/36 (56%) vs 15/40 (38%), and 4/36 (11%) vs 14/40 (35%)). At 30 minutes after completion of the procedure, 'drowsiness or spinning sensations' were reported less frequently in the patient‐controlled CSA group than in the physician‐controlled CSA group (4/36 (11.1%) vs 21/40 (52.5%); P < 0.001) (Lier 2014).
4.6 Postoperative complications
Trialists have reported that when patient‐controlled CSA was compared with physician‐administered CSA in 112 women, one individual in the group in which patient‐controlled CSA was administered via inhalational isodesox needed airway support perioperatively (Thompson 2000).
4.7 Patient satisfaction
Data show no evidence of a difference between the two groups in reported satisfaction with the procedure (OR 1.95, 95% CI 0.34 to 11.28; N = 81; Analysis 4.7) (Bhattacharya 1997), nor in patient satisfaction (MD on VAS 0 to 10 scale 0.20, 95% CI ‐0.64 to 1.04; N = 106; Analysis 4.8) (Lok 2002); satisfaction was high in both groups (95% vs 95%) (Thompson 2000).
4.7. Analysis.
Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 7 Patient satisfaction by LIkert scale: report of 'very and moderately satisfied'.
4.8. Analysis.
Comparison 4 Patient‐controlled versus physician‐controlled sedation + analgesia (CSA), Outcome 8 Patient satisfaction (VAS 0 to 10).
The patient‐controlled CSA group reported a higher satisfaction score than was reported by the physician‐controlled CSA group (median NRS 9 (8 to 10) vs 7 (4 to 9); P = 0.013) (Lier 2014).
5. Conscious sedation and analgesia (CSA) via different agents or dosages
Five studies compared different drug regimens for CSA.
CSA with pethidine versus pethidine plus piroxicam (Ocal 2002).
CSA with midazolam plus fentanyl versus CSA with propofol plus fentanyl (Ma 2008).
CSA with dexmedetomidine + paracervical block versus CSA with midazolam + paracervical block (Elnabtity 2017).
Patient‐controlled CSA with propofol versus patient‐controlled CSA with midazolam (Cook 1993).
Target‐controlled infusion of CSA plus propofol and remifentanil, with comparison of different infusion rates (Coskun 2011).
Primary outcomes
5.1 Intraoperative pain
Comparisons of CSA with pethidine versus CSA with pethidine plus piroxicam show that women in the pethidine group were more likely to report no pain and less likely to report intense pain than women given intramuscular pethidine plus oral piroxicam or oral piroxicam only (12% vs 0% vs 0%, and 0% vs 4% vs 31%, respectively; P = 0.035; N = 58) (Ocal 2002).
Comparisons of CSA with midazolam plus fentanyl versus CSA with propofol plus fentanyl yielded no evidence of a difference between groups in pain reported during oocyte retrieval (37/40 (93%) vs 36/40 (90%) reported no pain, 2/40 (5%) vs 2/40 (5%) reported mild pain, and 1/40 (2.5%) vs 2/40 (5%) reported severe pain; N = 316) (Ma 2008).
One study measured mean intraoperative pain at five‐minute intervals. CSA with dexmedetomidine plus PCB was associated with significantly less intraoperative pain when compared with CS with midazolam plus PCB at five minutes (MD on 0 to 10 VAS ‐0.74, 95% CI ‐1.48 to 0.00; N = 52; Analysis 5.1) and at 10 minutes (MD on 0 to 10 VAS ‐0.90, 95% CI ‐1.64 to ‐0.16; N = 52; Analysis 5.2), respectively. Data show no significant differences in mean pain scores between the two groups at 15, 20, and 25 minutes during oocyte retrieval (Elnabtity 2017).
5.1. Analysis.
Comparison 5 Conscious sedation (CSA) + analgesia via different agents or dosages, Outcome 1 Intraoperative pain score at 5 minutes (VAS 0 to 10).
5.2. Analysis.
Comparison 5 Conscious sedation (CSA) + analgesia via different agents or dosages, Outcome 2 Intraoperative pain score at 10 minutes (VAS 0 to 10).
Target‐controlled infusion (TCI) is a system that maintains a particular target plasma drug concentration via standard pharmacokinetic equations. Comparison of different doses of TCI yielded no evidence of a difference in pain between the three groups (TCI with remifentanil 1.5 ng/mL, 2 ng/mL, and 2.5 ng/mL, respectively) after the first puncture at five minutes (mean pain score on a 10‐point scale 0.7 (SD 0.3) vs 0.29 (SD 0.17) vs 0.35 (SD 0.19)) or at 10 minutes (1 (SD 1) vs 0.3 (SD 0.36) vs 0.28 (SD 0.28), respectively; N = 69) or at 15 and 20 minutes (mean pain score 0.57 (SD 0.57) vs 0 (SD 0) vs 0.11 (SD 0.11) and 2 (SD 0) vs 0 (SD 0) vs 0 (SD 0), respectively; N = 69). Data show no evidence of differences in pain between the three groups at completion of the procedure (mean pain score 0.13 (SD 0.1) vs 0.09 (SD 0.09) vs 0 (SD 0), respectively; N = 69) (Coskun 2011).
5.2 Postoperative pain
CSA with dexmedetomidine plus PCB was associated with less pain than CSA with midazolam plus PCB at 20 minutes postoperatively (MD on 0 to 10 VAS 0.42, 95% CI ‐0.04 to 0.88; N = 52; Analysis 5.3). Data show no significant difference in mean pain scores between the two groups at 40 and 60 minutes postoperatively (Elnabtity 2017).
5.3. Analysis.
Comparison 5 Conscious sedation (CSA) + analgesia via different agents or dosages, Outcome 3 Postoperative pain score at 20 minutes (VAS 0 to 10).
Secondary outcomes
5.3 Live birth rate and ongoing pregnancy rate
This outcome was not reported.
5.4 Clinical pregnancy rate
When researchers compared different doses of TCI (remifentanil 1.5 ng/mL, 2 ng/mL, and 2.5 ng/mL respectively), they found no evidence of a difference in pain between the three groups and no evidence of a difference in pregnancy rate between the three groups (10/23 (43%) vs 10/23 (43%) vs 12/23 (52%), respectively; N = 69) (Coskun 2011).
Pregnancy rates per embryo transfer were similar with CSA with dexmedetomidine plus PCB and CSA with midazolam plus PCB (10/26 (38.4%) vs 10/26 (38.4%)) (Elnabtity 2017).
5.5 Fertilisation rate
This outcome was not reported.
5.6 Abandoned procedure of oocyte retrieval
This outcome was not reported.
5.7 Side effects of analgesia
When investigators compared CSA with midazolam plus fentanyl versus CSA with propofol plus fentanyl, they found that midazolam plus fentanyl was associated with less nausea and vomiting (10/40 (25%) and 4/40 (10%) vs 13/40 (32.5%) and 11/40 (27.5%); P < 0.05, respectively; N = 316) (Ma 2008).
Comparisons of different doses of target‐controlled CSA infusion (remifentanil 1.5 ng/mL, 2 ng/mL, and 2.5 ng/mL respectively) yielded no evidence of differences in reports of postoperative nausea and vomiting between the three groups (0/23 (0%) vs 1/23 (4%) vs 2/23 (9%), respectively; N = 69) (Coskun 2011).
Postoperative side effects (nausea, vomiting, dizziness, restlessness, and headache) were similar between CSA with dexmedetomidine plus PCB and CSA with midazolam plus PCB groups (Elnabtity 2017).
5.8 Postoperative complications
Trialists comparing patient‐controlled CSA with propofol versus patient‐controlled CSA with midazolam found that one participant in the midazolam group became transiently unresponsive and two women in the propofol group reported syncope (Cook 1993).
Researchers comparing different doses of target‐controlled CSA infusion (remifentanil 1.5 ng/mL, 2 ng/mL, and 2.5 ng/mL respectively) reported that five women needed a jaw thrust followed by brief periods of assisted masked ventilation (Coskun 2011).
5.9 Patient satisfaction
Comparison of patient‐controlled CSA with propofol versus patient‐controlled CSA with midazolam revealed that both groups reported that they would like to be given the same drug again for a future procedure (20/22 (91%) in the midazolam group vs 24/25 (96%) in the propofol group) (OR 0.42, 95% CI 0.04 to 4.94; N = 47; Analysis 5.4) (Cook 1993).
5.4. Analysis.
Comparison 5 Conscious sedation (CSA) + analgesia via different agents or dosages, Outcome 4 Patient satisfaction rate.
Patient satisfaction scores were significantly higher in the group given CSA with dexmedetomidine plus PCB than in the group given CSA with midazolam plus PCB (OR 3.07, 95% CI 0.98 to 9.59; N = 52; Analysis 5.4) (Elnabtity 2017).
Comparisons of different doses of target‐controlled CSA infusion (remifentanil 1.5 ng/mL, 2 ng/mL, and 2.5 ng/mL respectively) revealed that 66 women (95%) who were free from postoperative nausea and vomiting were satisfied with their care (Coskun 2011).
Discussion
Summary of main results
This review included 24 trials examining five broad categories of pain relief methods of conscious sedation and analgesia that involved 3160 women undergoing oocyte retrieval. Women’s experience of pain showed conflicting results. No one particular modality of conscious sedation and analgesia was better than any other in providing effective pain relief. However, use of more than one method simultaneously, as when combined with acupuncture or paracervical block, resulted in better pain relief. Patient‐controlled sedation and analgesia was associated with greater intraoperative pain than was physician‐administered sedation and analgesia. Neither of these methods appeared to affect pregnancy rates. However, confidence intervals were wide in most comparisons; therefore these results should be interpreted with caution. Fifteen studies reported high levels of satisfaction in both intervention and comparison groups.
The procedure of oocyte retrieval is painful, as has been demonstrated by higher pain scores among women receiving placebo in Ramsewak 1990 and lower pain scores associated with the intervention. Regardless of the nature of the drug or the dose used, opiates such as fentanyl were effective in reducing the perception of pain. Addition to the opiate of a second drug or intervention, such as paracervical block (PCB), conferred further benefit. The principle of a balanced multi‐modal approach to analgesia has been shown to be effective for treating individuals with pain in other clinical settings such as cancer (World Health Organization (WHO) pain ladder; http://www.who.int/cancer/palliative/painladder/en/) (accessed 10 July 2017).
Paracervical block reduced abdominal pain during oocyte retrieval (Ng 1999); this was also demonstrated in a trial that reported higher pain scores in a placebo plus PCB group (Ng 2001). In trials evaluating PCB, women who were given additional intravenous fentanyl reported lower intraoperative pain scores. Meta‐analysis of the intraoperative pain scores associated with intravenous fentanyl plus PCB versus electro‐acupuncture plus PCB favoured intravenous fentanyl. However, in these two studies, the group given fentanyl also received premedication, whereas the group undergoing electro‐acupuncture received no premedication (Gejervall 2005; Humaidan 2004).
Two studies administered additional analgesia as needed during oocyte retrieval (Cook 1993; Gejervall 2005). One study investigated the dose‐effect relationship of target‐controlled infusion (TCI) of remifentanil and propofol. TCI is a system that maintains a particular target plasma drug concentration via standard pharmacokinetic equations. This study described the need to 'adjust' the dosage of the analgesic agent by increasing or decreasing the dosage (Coskun 2011). This is likely to have caused some women to change treatment groups, accounting for an important limitation in reporting of pain based on the allocated intervention.
Women who received conscious sedation and analgesia combined with electro‐acupuncture reported less pain than women who received conscious sedation and analgesia only (Meng 2008; Meng 2009; Sator‐Katzenschlager 2006). However, the overall result is inconclusive, as pooled data from four trials show that the pain score was higher among women who received auricular electro‐acupuncture and PCB than among women given conscious sedation and analgesia with PCB only (Gejervall 2005; Humaidan 2004; Stener‐Victorin 1999; Stener‐Victorin 2003).
Five trials evaluated the effect of conscious sedation plus acupuncture or electro‐acupuncture on pregnancy rate; the result was inconclusive. Evidence on live birth rate, based on the findings of one small trial, was also inconclusive (Stener‐Victorin 1999).
Several trials (15 out of 24) reported insufficient evidence upon comparison of rates of postoperative nausea and vomiting in the two groups. A trial that compared propofol and midazolam in the context of patient‐controlled sedation and analgesia reported that two women in the propofol group were unable to complete the assessment after completion of the procedure. One was emotionally upset by a difficult oocyte retrieval, and the other fainted upon sitting up. One woman in the midazolam group became transiently unresponsive intraoperatively when given rescue alfentanil by the anaesthetist (Cook 1993). One woman in the PCS via inhalational isodesox group needed perioperative airway support (Thompson 2000). Two women had perforation and one had vaginal bleeding after completion of the procedure (group not reported) (Guasch 2005). In another study, five women needed brief periods of assisted mask ventilation (Coskun 2011). The remaining reviewed trials documented no other serious adverse effects or cancellations of the oocyte retrieval procedure. It is unclear whether no adverse effects actually occurred, or whether these effects were simply unreported.
Patient satisfaction was high with all modalities of conscious sedation and analgesia that were reviewed. No one particular method or delivery system appeared to be clearly better than the other, although use of one method simultaneously with acupuncture or paracervical block resulted in better pain relief than was attained by use of one modality alone. In choosing conscious sedation and analgesia for oocyte retrieval, a balance may need to be struck between effectiveness, safety, and availability of resources. In this update, two studies measured women’s satisfaction as well as their well‐being (fear, stress, and anxiety), and this provided some indication of the quality of women's experiences (Gejervall 2005; Sator‐Katzenschlager 2006).
It is unclear whether global satisfaction can be regarded as a meaningful outcome in determining the effectiveness of the nature, dose, and delivery system of sedation and analgesia used for oocyte retrieval. It is possible that the overall success of the operative procedure (in terms of oocytes collected) and anxiety about side effects of drugs may override any distress caused by the pain. The effectiveness and adequacy of sedation and analgesia, important as they are, may not be the most important outcomes for women undergoing oocyte retrieval when compared with the satisfaction related to a good (or bad) experience of this painful but short and stressful procedure. When patient‐controlled analgesia was used, patients pressed the demand button only when the pain became intolerable (Chumbley 1998). It has also been reported that some patients were reluctant to eliminate pain completely, even when encouraged to do so (Hawkins 1993). The generally high satisfaction levels may reflect the fact that the overall success of the procedure had the potential to counteract the discomfort of the procedure.
In this review, most of the mean differences in pain on a visual analogue scale (VAS) (0 to 10) between different CSA methods were below 2.0, but a few exceeded 2.0, which we believe could represent a clinically important difference. However, tolerance and the experience of pain varied among individuals, making it difficult to interpret the findings of this outcome. General anaesthesia would eliminate pain altogether but is likely to have cost implications. For women who wish to avoid pharmacological analgesia and the side effects of opiates, general anaesthesia, or any agent, electro‐acupuncture may be an effective alternative, depending on the resources available. The ideal regimen of conscious sedation and analgesia would reduce pain to a tolerable level in all patients without risk of adverse respiratory or cardiovascular events. This review demonstrates the variety of approaches available to achieve this and underlines the difficulty of identifying the most superior method(s).
Overall completeness and applicability of evidence
We identified five main interventions comprising 14 dissimilar comparisons, with little consistency in the choice of outcomes. Intraoperative pain was reported in 22 studies, and 11 studies reported the outcome of only postoperative pain. Even when similar drugs were used, routes of administration and doses varied widely. Use of complex interventions in many trials impaired our ability to assess the effects of individual pain relief measures. When pain was the chosen outcome, data show marked differences in the timing of pain assessment and the measuring instruments used, which included the visual analogue scale (VAS), the Likert scale, and other numerical and non‐numerical rating scales. Although it is clear that intraoperative pain was measured during oocyte retrieval, the definition of postoperative pain ranged from pain immediately after oocyte retrieval (end of procedure) to time periods (minutes or hours) following oocyte retrieval. This ambiguity is likely to influence the applicability of the evidence on pain relief. Heterogeneity in the wide range of interventions, dosing regimens, and outcome measures limited our ability to aggregate data meaningfully and to generate conclusions. The subjective nature of pain and satisfaction and the different measures used to assess them limit our ability to interpret and aggregate these outcomes satisfactorily.
In many of the studies reviewed, it is not clear whether pain was measured retrospectively. It is also impossible to ascertain whether a low pain score was due to the increased efficacy of intravenous fentanyl, or whether the premedication altered pain perception or interfered with a person's ability to report the experience of pain. Co‐interventions such as premedication might distort the memory of pain. This must be taken into account in interpreting data from trials that measured pain retrospectively and highlights the difficulty of disentangling the individual anxiolytic, sedative, and analgesic effects of a sedative‐analgesic combination. For example, analgesics such as fentanyl and pethidine in high dosages can produce sedation, and intravenous anaesthetics such as propofol (sedative and analgesic) can have sedative effects at subanaesthetic dosages.
Measuring intraoperative pain would not be possible in two of the trials that used general anaesthesia as a comparator (Ben‐Shlomo 1999;Guasch 2005). Unlike the combination of midazolam and ketamine (Ben‐Shlomo 1999), short‐acting fentanyl may lack adequate residual analgesic effect to provide postoperative pain relief. The amnesic effect of midazolam may be an important confounder, as it can potentially obliterate the memory of pain. Pethidine was reported to be a more effective pain relief agent than piroxicam (Ocal 2002), a non‐steroidal anti‐inflammatory drug.
Comparison of the delivery system and the actual agents used in Bhattacharya 1997,Lier 2014,Lok 2002,Thompson 2000, and Zelcer 1992 shows that the validity of the comparison could be affected in trials of patient‐controlled sedation and analgesia (PCS). Although the theoretical advantage of PCS is that it allows women to administer as much pain relief as they need, this advantage may be limited by (1) the way the pump is set up to deliver a metered dose, and (2) a built‐in lockout time for reasons of safety. A physician may anticipate painful episodes and may give a dose larger than a PCS pump would permit. Meta‐analysis of the intraoperative pain score between patient‐controlled and physician‐administered sedation and analgesia shows that less pain was experienced by patients in the physician‐controlled group. However, this finding must be interpreted with caution in the light of different sedative and analgesic agents and dosages used in these trials.
Quality of the evidence
Using GRADE methods, review authors assessed evidence to be generally of low or very low quality, mainly owing to poor reporting and imprecision.
Risk of bias in the included trials varied. Six trials did not report the method of randomisation used. Methods of allocation concealment were unclear in nine studies, which were at unclear risk of bias. Attempts to contact trial authors by email and letter for clarification met with limited success. Seven trials did not carry out intention‐to‐treat analyses. Overall the sample size ranged from 30 to 700 women. To attain 80% power of detecting a difference of 7 mm on the VAS at the 5% significance level, a minimum of 70 women would be needed. Thirteen trials did not report sample size calculation. Although blinding of women was not feasible owing to the nature of the interventions (such as patient‐controlled sedation and analgesia vs physician‐administered sedation and analgesia), five trials reported blinding of participants and six reported blinding of outcome assessors, which is essential in principle to minimise measurement bias. Figure 1 and Figure 2 show the review authors’ judgements about risk of bias among the trials included in this review.
Potential biases in the review process
We did not exclude studies on the grounds of language. However, some bias in the review process may have arisen from inclusion of trials with insufficient information or outcome data and from lack of response of trial authors to our enquiries.
Agreements and disagreements with other studies or reviews
A systematic review of pain relief in oocyte retrieval restricted itself to trials comparing electro‐acupuncture versus other conscious sedation methods (Stener‐Victorin 2005). The findings of that review were similar to our findings in this population.
Authors' conclusions
Implications for practice.
Evidence does not support one particular method or technique over another for providing effective conscious sedation and analgesia for pain relief during and after oocyte retrieval. Simultaneous use of sedation combined with analgesia such as the opiates, further enhanced by paracervical block or acupuncture techniques, resulted in better pain relief than was attained by one modality alone. Evidence was insufficient to show conclusively whether any of the interventions provided influenced pregnancy rates. All reviewed techniques were associated with a high degree of patient satisfaction. Women’s preferences and resource availability for choice of pain relief merit consideration in practice.
Implications for research.
One of the limitations of previous research has been the diversity of methods available to provide conscious sedation and analgesia, as well as lack of standardisation of measures used to assess outcomes of pain and satisfaction. This limitation renders comparison across trials difficult and aggregation of data impossible. In planning future research, greater consensus is needed to determine both the tools to be used to evaluate pain and the timing of pain evaluation during and after the procedure. Postoperative pain should be monitored after discharge and until readmission for embryo transfer, so researchers can assess whether recovery from postoperative pain is sufficiently quick. Pain assessment based on both subjective and objective measures merits consideration. In addition, future trials should explore women’s views on how individualised analgesic support can best be provided during oocyte retrieval.
What's new
| Date | Event | Description |
|---|---|---|
| 5 February 2018 | New citation required but conclusions have not changed | The addition of 3 new studies has not led to any change in the conclusions of this review. |
| 5 February 2018 | New search has been performed | The review has been updated. |
History
Protocol first published: Issue 3, 2004 Review first published: Issue 3, 2005
| Date | Event | Description |
|---|---|---|
| 1 November 2012 | New search has been performed | Review title changed to "Pain relief for women undergoing oocyte retrieval for assisted reproduction" Following peer review, the primary outcomes have been changed to intra‐operative pain and post‐operative pain, and the secondary outcomes now include live birth rate. |
| 1 November 2012 | New citation required and conclusions have changed | New studies added with change to conclusions |
| 25 July 2012 | New search has been performed | New search performed. Nine new RCTs added to the review: Coskun 2011; Gejervall 2005; Guasch 2005; Gunaydin 2007; Ma 2008; Meng 2008; Meng 2009; Ozturk 2006; Sator‐Katzenschlager 2006 |
| 23 May 2005 | Feedback has been incorporated | Substantive amendment |
Acknowledgements
Authors of the 2018 update wish to thank Dr. Fiona Knox and Mr. Alex McNeil for their contributions to previous versions of this review.
We gratefully thank the trialists who responded to our queries. We also thank Michelle Proctor, Ruth Buist, Marian Showell, Jane Marjoribanks, and Helen Nagels of the Cochrane Gynaecology and Fertility Group for their help with this or previous versions of the review, along with Professor A. Metin Gulmezoglu for help in translation.
Appendices
Appendix 1. Cochrane Gynaecology and Fertility Group (CGFG) Specialised Register search strategy
Searched from inception to 9 November 2017
Procite platform
Keywords CONTAINS "oocyte" or "oocyte aspiration" or "oocyte collection" or "oocyte donors" or "oocyte pick‐up" or "oocyte pickup techniques" or "oocyte retrieval" or "follicular aspiration" or "follicle aspiration" or "donor egg cycles" or "donor oocytes" or "Aspirating ICSI" or "Aspiration" or Title CONTAINS "oocyte" or "oocyte aspiration" or "oocyte collection" or "oocyte donors" or "oocyte pick‐up" or "oocyte pickup techniques" or "oocyte retrieval" or "follicular aspiration" or "follicle aspiration" or "donor egg cycles" or "donor oocytes" or "Aspirating ICSI" or "Aspiration"
AND
Keywords CONTAINS "conscious sedation" or "sedation" or "sedatives" or "sedatives, nonbarbituate" or "alprazolam" or "diazepam" or "lorazepam" or "midazolam" or "midolazam" or "oxazepam" or "fentanyl" or "narcotics" or "opioid analgesia" or" opioids" or "bolus" or "antianxiety agents" or "anxiolytic" or "propofol" or "pain relief" or "*Analgesics, Opioid" or "analgesics" or "analgesia" or "anaesthetics" or "anaesthesia" or "acupuncture" or "electroacupuncture" or "pethidine" or Title CONTAINS "conscious sedation" or "sedation" or "sedatives" or "sedatives, nonbarbituate" or "alprazolam" or "diazepam" or "lorazepam" or "midazolam" or "midolazam" or "oxazepam" or "fentanyl" or "fentenyl" or "narcotics" or "opioid analgesia" or "opioids" or "bolus" or "antianxiety agents" or "anxiolytic" or "propofol" or "pain relief" or "*Analgesics, Opioid" or "analgesics" or "analgesia" or "anaesthetics" or "anaesthesia" or "acupuncture" or "electroacupuncture" or "pethidine"
(127 hits)
Appendix 2. Cochrane Register of Studies Online (CRSO) search strategy
Searched 9 November 2017
Web platform
#1 MESH DESCRIPTOR Fertilization in Vitro EXPLODE ALL TREES 1872
#2 MESH DESCRIPTOR Ovarian Follicle EXPLODE ALL TREES 517
#3 MESH DESCRIPTOR Oocytes EXPLODE ALL TREES 444
#4 MESH DESCRIPTOR Oocyte Retrieval EXPLODE ALL TREES 151
#5 MESH DESCRIPTOR Oocyte Donation EXPLODE ALL TREES 65
#6 MESH DESCRIPTOR Sperm Injections, Intracytoplasmic EXPLODE ALL TREES 487
#7 (oocyt* adj5 retriev*):TI,AB,KY 1229
#8 (oocyt* adj5 pickup*):TI,AB,KY 16
#9 (oocyt* adj5 pick up*):TI,AB,KY 54
#10 (egg* adj5 (retriev* or pick?up*)):TI,AB,KY 42
#11 (IVF or ICSI):TI,AB,KY 4062
#12 (vitro fertili*):TI,AB,KY 2170
#13 (intracytoplas* adj3 sperm*):TI,AB,KY 1354
#14 (egg* adj2 recover*):TI,AB,KY 8
#15 (oocyte* adj2 recover*):TI,AB,KY 119
#16 (follic* adj2 aspirat*):TI,AB,KY 116
#17 (ovum adj2 aspirat*):TI,AB,KY 1
#18 (oocyte* adj2 aspirat*):TI,AB,KY 51
#19 (egg* adj2 aspirat*):TI,AB,KY 1
#20 (egg* adj2 collect*):TI,AB,KY 46
#21 (oocyte* adj2 collect*):TI,AB,KY 147
#22 (ovum adj2 pick?up):TI,AB,KY 13
#23 (egg* adj2 dona*):TI,AB,KY 19
#24 (oocyte* adj2 dona*):TI,AB,KY 178
#25 ((egg* or oocyte*) adj2 donor*):TI,AB,KY 109
#26 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 5655
#27 MESH DESCRIPTOR Hypnotics and Sedatives EXPLODE ALL TREES 11857
#28 MESH DESCRIPTOR Conscious Sedation EXPLODE ALL TREES 1264
#29 MESH DESCRIPTOR Narcotics EXPLODE ALL TREES 13262
#30 MESH DESCRIPTOR Fentanyl EXPLODE ALL TREES 4309
#31 MESH DESCRIPTOR Tranquilizing Agents EXPLODE ALL TREES 16765
#32 MESH DESCRIPTOR Anti‐Anxiety Agents EXPLODE ALL TREES 9089
#33 (fentanyl or medazepam):TI,AB,KY 10433
#34 (diazepam or midazolam):TI,AB,KY 9829
#35 (propofol or ketamine or isoflurane):TI,AB,KY 13890
#36 MESH DESCRIPTOR Anesthesia and Analgesia EXPLODE ALL TREES 24147
#37 MESH DESCRIPTOR analgesia EXPLODE ALL TREES 6788
#38 MESH DESCRIPTOR acupuncture analgesia EXPLODE ALL TREES 266
#39 MESH DESCRIPTOR Electroacupuncture EXPLODE ALL TREES 632
#40 sedation:TI,AB,KY 11173
#41 (hypnotic* or sedative*):TI,AB,KY 7743
#42 (paracervical block):TI,AB,KY 181
#43 pethidine:TI,AB,KY 1773
#44 (analgesi* or pain relief):TI,AB,KY 41195
#45 (electro‐acupuncture or electroacupuncture):TI,AB,KY 1432
#46 (anaesthe* or anesthe*):TI,AB,KY 51765
#47 opioid*:TI,AB,KY 13697
#48 alfentanil:TI,AB,KY 1339
#49 (bolus adj2 injection*):TI,AB,KY 2196
#50 #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35 OR #36 OR #37 OR #38 OR #39 OR #40 OR #41 OR #42 OR #43 OR #44 OR #45 OR #46 OR #47 OR #48 OR #49 106316
#51 #26 AND #50 191
Appendix 3. MEDLINE search strategy
Searched from 1946 to 9 November 2017
OVID platform
1 Fertilization in Vitro/ or Ovarian Follicle/ or Oocytes/ (84069)
2 exp oocyte donation/ or exp oocyte retrieval/ (3956)
3 (oocyt$ adj5 retriev$).tw. (5466)
4 (oocyt$ adj5 picku$).tw. (103)
5 (egg$ adj5 (retriev$ or picku$)).tw. (350)
6 (IVF or ICSI).tw. (25664)
7 (in vitro adj fertili$).tw. (22958)
8 (intracytoplas$ adj5 sperm).tw. (6718)
9 (egg$ adj2 recover$).tw. (556)
10 (oocyte$ adj2 recover$).tw. (1616)
11 (egg$ adj5 (retriev$ or pick u$)).tw. (357)
12 (oocyt$ adj5 pick u$).tw. (311)
13 (follic$ adj2 aspirat$).tw. (1381)
14 (ovum adj2 aspirat$).tw. (21)
15 (oocyte$ adj aspirat$).tw. (349)
16 (egg$ adj aspirat$).tw. (10)
17 (egg$ adj2 collect$).tw. (1579)
18 (oocyte$ adj2 collect$).tw. (1786)
19 (ovum adj2 pickup).tw. (129)
20 (ovum adj2 pick up$).tw. (453)
21 (egg$ adj2 dona$).tw. (449)
22 ((egg or oocyte$) adj2 donor$).tw. (1491)
23 (oocyte$ adj donat$).tw. (1164)
24 or/1‐23 (101891)
25 exp "hypnotics and sedatives"/ or exp alprazolam/ or exp diazepam/ or exp lorazepam/ or medazepam/ or midazolam/ or nitrazepam/ or oxazepam/ (121622)
26 exp Conscious Sedation/ (8465)
27 (hypnotic$ or sedative$).tw. (28508)
28 exp narcotics/ or exp fentanyl/ or exp tranquilizing agents/ or exp anti‐anxiety agents/ (322760)
29 (fentanyl or medazepam).tw. (17520)
30 (diazepam or midazolam).tw. (31770)
31 (propofol or ketamine or isoflurane).tw. (44105)
32 exp analgesia/ or exp acupuncture analgesia/ or exp electroacupuncture/ (42138)
33 sedation.tw. (37059)
34 paracervical block.tw. (488)
35 pethidine.tw. (2442)
36 (analgesi$ or pain relief).tw. (132308)
37 (electro‐acupuncture or electroacupuncture).tw. (4261)
38 (anaesthe$ or anesthe$).tw. (360612)
39 opioid$.tw. (75881)
40 alfentanil.tw. (2272)
41 (bolus adj2 injection$).tw. (12499)
42 or/25‐41 (872293)
43 24 and 42 (1669)
44 randomised controlled trial.pt. (498672)
45 controlled clinical trial.pt. (99309)
46 randomized.ab. (435884)
47 placebo.tw. (208814)
48 clinical trials as topic.sh. (195915)
49 randomly.ab. (300285)
50 trial.ti. (196821)
51 (crossover or cross‐over or cross over).tw. (81138)
52 or/44‐51 (1244419)
53 exp animals/ not humans.sh. (4686392)
54 52 not 53 (1146893)
55 43 and 54 (153)
Appendix 4. Embase search strategy
Searched from 1980 to 9 November 2017
OVID platform
1 exp fertilization in vitro/ (59012)
2 exp ovary follicle/ (108174)
3 exp oocyte donation/ (3781)
4 exp oocyte retrieval/ (5572)
5 (oocyt$ adj5 retriev$).tw. (9089)
6 (oocyt$ adj5 picku$).tw. (160)
7 (egg$ adj5 (retriev$ or picku$)).tw. (739)
8 (IVF or ICSI).tw. (40905)
9 (in vitro adj fertili$).tw. (27451)
10 (intracytoplas$ adj5 sperm).tw. (8845)
11 (egg$ adj2 recover$).tw. (496)
12 (oocyte$ adj2 recover$).tw. (1748)
13 (egg$ adj5 (retriev$ or pick u$)).tw. (745)
14 (follic$ adj2 aspirat$).tw. (1579)
15 (ovum adj2 aspirat$).tw. (24)
16 (oocyte$ adj aspirat$).tw. (398)
17 (egg$ adj aspirat$).tw. (9)
18 (egg$ adj2 collect$).tw. (1881)
19 (oocyte$ adj2 collect$).tw. (2636)
20 (ovum adj2 pickup).tw. (166)
21 (ovum adj2 pick up$).tw. (611)
22 (egg$ adj2 dona$).tw. (907)
23 ((egg or oocyte$) adj2 donor$).tw. (2734)
24 (oocyte$ adj donat$).tw. (1953)
25 or/1‐24 (170724)
26 exp sedative agent/ or exp hypnotic sedative agent/ or exp hypnotic agent/ (315612)
27 exp conscious sedation/ (6222)
28 (hypnotic$ or sedati$).tw. (78460)
29 exp narcotic agent/ (233578)
30 exp FENTANYL/ (54085)
31 exp medazepam/ (876)
32 (diazepam or midazolam).tw. (37567)
33 (propofol or ketamine or isoflurane).tw. (57249)
34 exp tranquilizer/ (368348)
35 exp anxiolytic agent/ (169341)
36 (fentanyl or medazepam).tw. (23574)
37 exp PATIENT CONTROLLED ANALGESIA/ or exp ANALGESIA/ or exp ACUPUNCTURE ANALGESIA/ (139959)
38 sedati$.tw. (67849)
39 paracervical block.tw. (454)
40 pethidine.tw. (2632)
41 (analgesi$ or pain relief).tw. (170944)
42 (electro‐acupuncture or electroacupuncture).tw. (5161)
43 (anaesthe$ or anesthe$).tw. (413171)
44 opioid$.tw. (95217)
45 alfentanil.tw. (2598)
46 (bolus adj2 injection$).tw. (13434)
47 or/26‐46 (1248761)
48 25 and 47 (3169)
49 Clinical Trial/ (956884)
50 Randomized Controlled Trial/ (477722)
51 exp randomization/ (76318)
52 Single Blind Procedure/ (30101)
53 Double Blind Procedure/ (142031)
54 Crossover Procedure/ (53857)
55 Placebo/ (302896)
56 Randomi?ed controlled trial$.tw. (170823)
57 Rct.tw. (26275)
58 random allocation.tw. (1713)
59 randomly allocated.tw. (28714)
60 allocated randomly.tw. (2280)
61 (allocated adj2 random).tw. (788)
62 Single blind$.tw. (20075)
63 Double blind$.tw. (177147)
64 ((treble or triple) adj blind$).tw. (730)
65 placebo$.tw. (258758)
66 prospective study/ (414653)
67 or/49‐66 (1833790)
68 case study/ (50918)
69 case report.tw. (342376)
70 abstract report/ or letter/ (1016722)
71 or/68‐70 (1401761)
72 67 not 71 (1787292)
73 48 and 72 (336)
Appendix 5. PsycINFO search strategy
Searched from 1806 to 9 November 2017
OVID platform
1 exp Reproductive Technology/ (1656)
2 (oocyt$ adj5 retriev$).tw. (23)
3 (oocyt$ adj5 picku$).tw. (1)
4 (IVF or ICSI).tw. (535)
5 (egg$ adj5 (retriev$ or picku$)).tw. (20)
6 (in vitro adj fertili$).tw. (679)
7 (intracytoplas$ adj5 sperm).tw. (53)
8 (egg$ adj2 recover$).tw. (2)
9 (oocyte$ adj2 recover$).tw. (2)
10 (egg$ or pick u$).tw. (7096)
11 (oocyt$ adj5 pick u$).tw. (1)
12 (follic$ adj2 aspirat$).tw. (0)
13 (ovum adj2 aspirat$).tw. (0)
14 (oocyte$ adj aspirat$).tw. (0)
15 (egg$ adj aspirat$).tw. (0)
16 (egg$ adj2 collect$).tw. (44)
17 (oocyte$ adj2 collect$).tw. (0)
18 (ovum adj2 pickup).tw. (0)
19 (ovum adj2 pick up$).tw. (0)
20 (egg$ adj2 dona$).tw. (116)
21 ((egg or oocyte$) adj2 donor$).tw. (76)
22 (oocyte$ adj donat$).tw. (36)
23 or/1‐22 (8889)
24 exp Sedatives/ or exp Tranquilizing Drugs/ or exp Hypnotic Drugs/ (53370)
25 exp Alprazolam/ (690)
26 exp Midazolam/ (469)
27 exp Propofol/ (472)
28 exp Fentanyl/ (417)
29 exp Opiates/ or exp Analgesia/ or exp Narcotic Agonists/ (25591)
30 exp Anesthetic Drugs/ (19650)
31 (hypnotic$ and sedative$).tw. (1352)
32 paracervical block$.tw. (3)
33 pethidine.tw. (80)
34 sedati$.tw. (9203)
35 (analgesi$ or pain relief).tw. (15783)
36 (electro‐acupuncture or electroacupuncture).tw. (312)
37 (anaesthe$ or anesthe$).tw. (14967)
38 opioid$.tw. (19926)
39 alfentanil.tw. (89)
40 (bolus adj2 injection$).tw. (226)
41 or/24‐40 (120821)
42 23 and 41 (80)
Appendix 6. CINAHL search strategy
Searched from 1982 to 9 November 2017
Ebsco platform
| # | Query | Results |
| S33 | S8 AND S32 | 161 |
| S32 | S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 | 198,907 |
| S31 | TX bolus N2 injection* | 593 |
| S30 | TX opioid* | 24,706 |
| S29 | TX anaesthe* or anesthe* | 105,222 |
| S28 | TX pethidine | 340 |
| S27 | TX paracervical block* | 56 |
| S26 | TX electroacupuncture or TX acupuncture | 16,899 |
| S25 | (MM "Electroacupuncture") | 830 |
| S24 | (MM "Patient‐Controlled Analgesia") | 1,146 |
| S23 | (MM "Acupuncture Analgesia") OR (MM "Acupuncture Anesthesia") OR (MM "Anesthesia and Analgesia+") | 42,145 |
| S22 | TX medazepam or TX lorazepam | 981 |
| S21 | TX analgesi* | 43,331 |
| S20 | TX hypnotic* | 6,770 |
| S19 | (MM "Hypnotics and Sedatives+") | 8,371 |
| S18 | (MH "Analgesia") | 5,172 |
| S17 | TX (propofol or ketamine or isoflurane) | 9,783 |
| S16 | TX diazepam or TX midazolam | 4,403 |
| S15 | TX fentanyl | 4,682 |
| S14 | (MH "Alfentanil") OR TX "alfentanil" | 517 |
| S13 | TX"bolus injection*" | 516 |
| S12 | TX"pain relief" | 10,689 |
| S11 | (MM "Sedation") OR TX "sedation" | 11,628 |
| S10 | (MH "Narcotics+") OR TX"narcotics" OR (MH "Analgesics, Opioid+") | 35,974 |
| S9 | (MM "Conscious Sedation") OR TX"Conscious Sedation" | 2,912 |
| S8 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 | 4,291 |
| S7 | TX follicle aspiration* | 14 |
| S6 | (MH "Oocyte Donation") OR "oocyte donation" | 517 |
| S5 | TX oocyte collection* | 14 |
| S4 | TX egg pick up | 2 |
| S3 | TX oocyte retrieval* | 150 |
| S2 | TX ICSI | 429 |
| S1 | (MH "Fertilization in Vitro") OR "ivf" | 3,762 |
Appendix 7. ClinicalTrials.gov search strategy
Searched 10 January 2017
Web platform
“oocyte recovery AND pain”, “oocyte retrieval AND pain”, “oocyte aspiration AND pain”, “oocyte AND analgesia”, “oocyte AND analgesic”, “oocyte AND anaesthesia”, “oocyte AND anesthesia”, “oocyte AND sedation”, “oocyte AND acupuncture”, “oocyte AND block”, “oocyte AND remifentanil”, “oocyte AND fentanyl”, “oocyte AND propofol”, “oocyte AND pethidine”
(150 hits)
Appendix 8. WHO ICTRP search strategy
Searched 10 December 2016
Web platform
“oocyte recovery AND pain”, “oocyte retrieval AND pain”, “oocyte aspiration AND pain”, “oocyte AND analgesia”, “oocyte AND analgesic”, “oocyte AND anaesthesia”, “oocyte AND anesthesia”, “oocyte AND sedation”, “oocyte AND acupuncture”, “oocyte AND block”, “oocyte AND remifentanil”, “oocyte AND fentanyl”, “oocyte AND propofol”, “oocyte AND pethidine”
(48 hits)
Appendix 9. Web of Science search strategy
Searched 12 January 2017
Web platform
“oocyte recovery AND pain”, “oocyte retrieval AND pain”, “oocyte aspiration AND pain”, “oocyte AND analgesia”, “oocyte AND analgesic”, “oocyte AND anaesthesia”, “oocyte AND anesthesia”, “oocyte AND sedation”, “oocyte AND acupuncture”, “oocyte AND paracervical block”, “oocyte AND remifentanil”, “oocyte AND fentanyl”, “oocyte AND propofol”, “oocyte AND pethidine”
(329 hits)
Appendix 10. Portal Regional da BVS search strategy
Searched 12 January 2017
Web platform
“oocyte recovery AND pain”, “oocyte retrieval AND pain”, “oocyte aspiration AND pain”, “oocyte AND analgesia”, “oocyte AND analgesic”, “oocyte AND anaesthesia”, “oocyte AND anesthesia”, “oocyte AND sedation”, “oocyte AND acupuncture”, “oocyte AND paracervical block”, “oocyte AND remifentanil”, “oocyte AND fentanyl”, “oocyte AND propofol”, “oocyte AND pethidine”
(1007 hits)
Appendix 11. OpenGrey search strategy
Searched 12 January 2017
Web platform
“oocyte recovery AND pain”, “oocyte retrieval AND pain”, “oocyte aspiration AND pain”, “oocyte AND analgesia”, “oocyte AND analgesic”, “oocyte AND anaesthesia”, “oocyte AND anesthesia”, “oocyte AND sedation”, “oocyte AND acupuncture”, “oocyte AND block”, “oocyte AND remifentanil”, “oocyte AND fentanyl”, “oocyte AND propofol”, “oocyte AND pethidine”
(0 hits)
Data and analyses
Comparison 1. Conscious sedation + analgesia (CSA) versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain during needle insertion (VAS 0 to 10) | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | ‐1.70 [‐2.38, ‐1.02] |
| 2 Pain during follicle aspiration (VAS 0 to 10) | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | ‐1.30 [‐1.88, ‐0.72] |
Comparison 2. Conscious sedation + analgesia (CSA) versus other active interventions.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Intraoperative pain | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 CSA vs CSA + acupuncture (VAS 0 to 10) | 1 | 62 | Mean Difference (IV, Random, 95% CI) | 1.0 [0.18, 1.82] |
| 1.2 CSA vs CSA + electro‐acupuncture (VAS 0 to 10) | 1 | 62 | Mean Difference (IV, Random, 95% CI) | 3.00 [2.23, 3.77] |
| 1.3 CSA vs CSA + electro‐acupuncture (Pain scale 1 to 12) | 1 | 316 | Mean Difference (IV, Random, 95% CI) | 1.70 [1.07, 2.33] |
| 2 Postoperative pain | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 CSA vs CSA + acupuncture (VAS 0 to 10) | 1 | 61 | Mean Difference (IV, Fixed, 95% CI) | 0.60 [‐0.10, 1.30] |
| 2.2 CSA vs CSA + electro‐acupuncture (VAS 0 to 10) | 1 | 61 | Mean Difference (IV, Fixed, 95% CI) | 2.1 [1.40, 2.80] |
| 2.3 CSA vs general anaesthesia (Likert 0 to 3) | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | ‐1.90 [‐2.24, ‐1.56] |
| 3 Pregnancy | 3 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 CSA vs CSA + acupuncture | 1 | 61 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.20, 1.86] |
| 3.2 CSA vs CSA + electro‐acupuncture | 1 | 61 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.07, 0.66] |
| 3.3 CSA vs general anaesthesia | 2 | 108 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.43, 2.35] |
| 4 Postop vomiting and/or vomiting | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 CSA vs CSA + acupuncture | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 CSA vs general anaesthesia | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Satisfaction | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 CSA vs general anaesthesia | 2 | 108 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.11, 4.04] |
| 6 Postoperative complications (airway obstruction) | 1 | 58 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.02, 1.22] |
| 6.1 CSA vs general anaesthesia | 1 | 58 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.02, 1.22] |
| 7 Postoperative complications (mask ventilation) | 1 | 58 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.05 [0.01, 0.20] |
| 7.1 CSA vs general anaesthesia | 1 | 58 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.05 [0.01, 0.20] |
2.2. Analysis.
Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 2 Postoperative pain.
2.3. Analysis.
Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 3 Pregnancy.
2.4. Analysis.
Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 4 Postop vomiting and/or vomiting.
2.6. Analysis.
Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 6 Postoperative complications (airway obstruction).
2.7. Analysis.
Comparison 2 Conscious sedation + analgesia (CSA) versus other active interventions, Outcome 7 Postoperative complications (mask ventilation).
Comparison 3. Conscious sedation + analgesia (CSA) + paracervical block versus other interventions.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Intraoperative pain (VAS 0 to 10) | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 CSA + paracervical block versus electro‐acupuncture + paracervical block | 4 | 781 | Mean Difference (IV, Fixed, 95% CI) | ‐0.66 [‐0.93, ‐0.39] |
| 2 Postoperative pain | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 CSA + paracervical block vs general anaesthesia | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | 0.49 [‐0.13, 1.11] |
| 2.2 CSA + paracervical block vs spinal anaesthesia | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | 1.02 [0.48, 1.56] |
| 3 Live birth or ongoing pregnancy | 2 | 393 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.78, 1.86] |
| 3.1 CSA + paracervical block vs electro‐acupuncture + paracervical block | 1 | 149 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.35 [1.09, 5.05] |
| 3.2 CSA + paracervical block vs electro‐acupuncture + paracervical block | 1 | 244 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.50, 1.47] |
| 4 Pregnancy | 7 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 CSA + paracervical block vs general anaesthesia | 1 | 51 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.22, 2.26] |
| 4.2 CSA + paracervical block vs spinal anaesthesia | 1 | 38 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.24, 3.65] |
| 4.3 CSA + paracervical block vs paracervical block only | 1 | 150 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.44, 1.96] |
| 4.4 CSA + paracervical block vs electro‐acupuncture + paracervical block | 4 | 783 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.72, 1.29] |
| 4.5 CSA + paracervical block vs CSA alone | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.28, 1.36] |
| 5 Fertilisation rate per woman | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 CSA + paracervical block vs paracervical block only | 1 | 150 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.42, 1.66] |
| 6 Postoperative nausea and/or vomiting | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 CSA + paracervical block vs CS only | 2 | 140 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.18, 0.97] |
| 7 Patient satisfaction by Likert scale: report of 'excellent and satisfactory' | 1 | 150 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.63 [0.68, 3.89] |
| 7.1 CSA + paracervical block vs paracervical block only | 1 | 150 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.63 [0.68, 3.89] |
Comparison 4. Patient‐controlled versus physician‐controlled sedation + analgesia (CSA).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Intraoperative pain score (VAS 0 to 10) | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Pt‐controlled vs physician‐controlled CSA | 4 | 379 | Mean Difference (IV, Fixed, 95% CI) | 0.60 [0.16, 1.03] |
| 2 Intraoperative pain score excluding inhalational sedation/analgesia (VAS 0 to 10) | 3 | 267 | Mean Difference (IV, Fixed, 95% CI) | 0.47 [‐0.01, 0.95] |
| 2.1 Pt‐controlled vs physician‐controlled CSA | 3 | 267 | Mean Difference (IV, Fixed, 95% CI) | 0.47 [‐0.01, 0.95] |
| 3 Postoperative pain score (VAS 0 to 10) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Pt‐controlled vs physician‐controlled CSA | 1 | 106 | Mean Difference (IV, Fixed, 95% CI) | 1.2 [0.26, 2.14] |
| 4 Pregnancy rate per woman | 3 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 Pt‐controlled vs physician‐controlled CSA | 3 | 294 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.51, 1.60] |
| 5 Fertilisation rate per woman | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 Pt‐controlled vs physician‐controlled CSA | 1 | 106 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.54, 2.50] |
| 6 Postoperative nausea: no. of patients | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 Pt‐controlled vs physician‐controlled CSA | 1 | 80 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.19, 5.28] |
| 7 Patient satisfaction by LIkert scale: report of 'very and moderately satisfied' | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 Pt‐controlled vs physician‐controlled CSA | 1 | 81 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.95 [0.34, 11.28] |
| 8 Patient satisfaction (VAS 0 to 10) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Pt‐controlled vs physician‐controlled CSA | 1 | 106 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐0.64, 1.04] |
Comparison 5. Conscious sedation (CSA) + analgesia via different agents or dosages.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Intraoperative pain score at 5 minutes (VAS 0 to 10) | 1 | 52 | Mean Difference (IV, Fixed, 95% CI) | ‐0.74 [‐1.48, 0.00] |
| 2 Intraoperative pain score at 10 minutes (VAS 0 to 10) | 1 | 52 | Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐1.64, ‐0.16] |
| 3 Postoperative pain score at 20 minutes (VAS 0 to 10) | 1 | 52 | Mean Difference (IV, Fixed, 95% CI) | 0.42 [‐0.04, 0.88] |
| 4 Patient satisfaction rate | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 CSA with propofol vs CSA with midazolam | 1 | 47 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.04, 4.94] |
| 4.2 CSA with dexmedetomidine vs CSA with midazolam (very satisfied) | 1 | 52 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.07 [0.98, 9.59] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ben‐Shlomo 1999.
| Methods | Randomisation: random numbers Allocation concealment: sealed in consecutive envelopes Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 50 No. analysed: 50 Intention‐to‐treat analysis: yes Power and sample calculations not described Duration of trial: not stated |
|
| Participants | Women scheduled for oocyte retrieval Mean age: 34 years; cause of infertility not reported Similar baseline characteristics of age, height, and weight |
|
| Interventions |
No premedication in either group |
|
| Outcomes |
Other outcomes reported: no. of oocytes retrieved, cleavage rate, arousability, response to painful stimuli |
|
| Notes | Israel Single centre HaEmek Mecical Centre Funding: not stated Definition of pregnancy not documented |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers |
| Allocation concealment (selection bias) | Low risk | Adequate: sealed envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding not possible because of the nature of the interventions Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent dropout |
| Selective reporting (reporting bias) | Low risk | All pre‐stated outcomes reported |
| Other bias | Unclear risk | Comparable baseline characteristics of age, height, and weight but not cause of infertility |
Bhattacharya 1997.
| Methods | Randomisation: computer‐generated random numbers Allocation concealment: sealed in consecutively numbered envelopes Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 81 No. analysed: 81 Intention‐to‐treat analysis: yes Power and sample calculations described Duration of trial: not stated |
|
| Participants | Women undergoing vaginal oocyte recovery Mean age: 33 years Mean duration of infertility 5.5 years; 26% tubal disease Similar baseline demographic and infertility characteristics |
|
| Interventions |
All women received a preliminary IV loading dose of midazolam 4 mg. |
|
| Outcomes |
Other outcomes reported: perioperative blood pressure, pulse, oxygen, doses of fentanyl |
|
| Notes | Scotland Single centre Aberdeen University Funding: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation |
| Allocation concealment (selection bias) | Low risk | Adequate: sealed numbered envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding not possible because of the nature of the interventions Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
Cook 1993.
| Methods | Randomisation: method unclear Allocation concealment: sealed envelopes Blinding of participants/investigators: no Blinding of assessors: yes No. randomised: 47 No. analysed: 47 Intention‐to‐treat analysis: yes Power and sample calculations: not reported Duration of trial: not stated |
|
| Participants | Women presenting for transvaginal oocyte retrieval Mean age and weight similar in both groups (no data given) Cause of infertility: not reported Comparison of baseline characteristics: age/weight only |
|
| Interventions |
IV alfentanil administered at 3 points: before insertion of vaginal speculum, before needle entry into each ovary, on request |
|
| Outcomes | Secondary: patient satisfaction (VAS), adverse outcomes Other outcomes reported: sedation levels, psychometric tests |
|
| Notes | England Single centre London University Funding: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Methods unclear |
| Allocation concealment (selection bias) | Low risk | Adequate, sealed envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding not feasible because of the different appearance of drugs Assessors blind |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Unclear risk | Comparable baseline characteristics of age and weight but not cause of infertility |
Coskun 2011.
| Methods | Randomisation: computer‐generated Allocation concealment: quote "enclosed" numbers Blinding of participants/investigators: no Blinding of assessors: yes (for postop side effects) No. randomised: 69 No. analysed: 69 Intention‐to‐treat analysis: yes Power and sample calculations: described Duration of trial: not stated |
|
| Participants | Women scheduled for transvaginal oocyte retrieval Mean age: 33 to 35 years Cause of infertility: not reported Comparison of baseline characteristics: age, weight, and height only Similar demographic characteristics at baseline |
|
| Interventions |
TCI = A system that maintains a particular target plasma drug concentration via standard pharmacokinetic equations |
|
| Outcomes |
Other outcomes reported: sedation score, amount of sedation required, recovery score, blood pressure |
|
| Notes | Turkey Single centre Gazi University Funding: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation |
| Allocation concealment (selection bias) | Low risk | Quote "enclosed" numbers |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding not reported Blinding of assessors for postop side effects only |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Unclear risk | Comparable baseline characteristics of age, height, and weight but not cause of infertility |
Elnabtity 2017.
| Methods | Ransomisation: method unclear Allocation concealment: serially numbered, sealed opaque envelopes Blinding of participants/investigators: yes Blinding of assessors: not reported No. randomised: 52 No. analysed: 52 Intention‐to‐treat analysis: awaiting response from trial author Power and sample calculations described Duration of trial: from September 2014 to April 2015 |
|
| Participants | Women with ASA I/II undergoing ultrasound‐guided oocyte retrieval in an IVF programme Mean age: 25 to 38 years Cause of infertility: tubal disease, endometriosis, anovulation, male factor, unexplained Similar demographic (age, height, weight, BMI) and infertility characteristics at baseline Inclusion criteria: women in their first IVF cycle and showing bilateral ovarian follicular response Exclusion criteria: psychological abnormalities; cardiorespiratory, renal, or liver disease; requesting general anaesthesia; fewer than 3 dominant follicles present in either ovary; chronic alcohol/drug abusers; allergic to any of the medications used in the study |
|
| Interventions | 1. Intervention 1: IV fentanyl (1 µg/kg) plus paracervical block (100 mg lidocaine 1%) plus IV dexmedetomidine (1 µg/kg) (N = 26) 2. Intervention 2: IV fentanyl (1 µg/kg) plus paracervical block (100 mg lidocaine 1%) plus IV midazolam (0.06 mg/kg) (N = 26) |
|
| Outcomes |
Other outcomes reported: intraoperative vital signs, no. of oocytes obtained, embryos transferred per woman, amount of rescue propofol used |
|
| Notes | Egypt University Hospital No funding received |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method unclear |
| Allocation concealment (selection bias) | Low risk | Adequate: serially numbered and sealed opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Double‐blind (investigators and participants) Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
Gejervall 2005.
| Methods | Randomisation: computer‐generated list Allocation concealment: unclear Blinding of participants/investigators: yes Blinding of assessors: yes No. randomised: 160 No. analysed: 158 Intention‐to‐treat analysis: reported both as intention‐to‐treat and ‘as per protocol’ Power and sample calculations described Duration of trial: 19 months, from March 2002 to October 2003 |
|
| Participants | Women undergoing oocyte aspiration Mean age: 33 to 34 years (range 23 to 39 years) Cause of infertility: tubal factor, hormonal factor, endometriosis, male factor, unexplained Similar demographic and infertility characteristics at baseline |
|
| Interventions | In a 1:1 ratio,
Control group received premedication (oral flunitrazepam 0.5 mg and rectal paracetamol 1 g); EA group did not receive premedication. |
|
| Outcomes |
Other outcomes reported: well‐being, number of embryos transferred, pregnancy per cycle |
|
| Notes | Sweden Single centre University Hospital Goteborg Funding: Research & Development Council, Goteborg and Bohuslan, the Hjarmar Sevensson Foundation, the Organon Foundation, the Wilhelm & Marina Lundgren's Foundation Loss to follow‐up (N = 2) in intervention group due to ovulation before aspiration and missing VAS assessment Definition of pregnancy not documented |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer randomisation |
| Allocation concealment (selection bias) | Unclear risk | Methods unclear |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Blinding of participants not feasible owing to the nature of the intervention Person who assessed the VAS blinded to the groups to which participants belonged Other midwives not involved in administering EA assisted in the analgesia procedure during oocyte retrieval. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Two lost to follow‐up. Data available for intention‐to‐treat and ‘per protocol’ |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
Guasch 2005.
| Methods | Randomisation: computer generation Allocation concealment: method unclear Blinding of participants/investigators: no Blinding of assessors: yes No. randomised: 65 No. analysed: 65 (IVF outcomes); 45 (satisfaction) Intention‐to‐treat analysis: yes for IVF outcomes, no for satisfaction outcomes Power and sample calculations not reported Duration of trial: 18 months, from March 1999 to September 2002 |
|
| Participants | Women undergoing oocyte retrieval Age range 24 to 39 years Cause of infertility: not reported Similar baseline characteristics of age/height/weight |
|
| Interventions |
No premedication given to any groups |
|
| Outcomes |
Other outcomes reported: serum prolactin levels, follicular cortisol levels, oocyte recovery rate |
|
| Notes | Spain Single centre Hospital Universitario La Paz, Madrid Funding: not stated Definition of pregnancy not documented Fourth group (non‐randomised) receiving remifentanil: data not used for the review Paper in Spanish |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation |
| Allocation concealment (selection bias) | Unclear risk | Methods unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding not possible owing to the nature of the interventions Analysis conducted by an independent person not involved in the trial Oocyte and fertilisation data collected by a blinded investigator |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete for pain but incomplete for satisfaction |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Unclear risk | Comparable baseline characteristics of age, height, and weight but not cause of infertility |
Gunaydin 2007.
| Methods | Randomisation: methods unclear Allocation concealment: sealed envelopes Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 40 No. analysed: 40 Intention‐to‐treat analysis: yes Power and sample calculations briefly described Duration of trial: not stated |
|
| Participants | Women scheduled to undergo transvaginal oocyte retrieval Mean age: 32 to 33 years Cause of infertility: not reported Similar baseline characteristics of age, height, and weight |
|
| Interventions |
|
|
| Outcomes |
Other outcomes reported: plasma remifentanil levels, pulmonary function |
|
| Notes | Turkey Single centre Gazi University Funding: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Methods unclear |
| Allocation concealment (selection bias) | Low risk | Closed envelope allocation |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Unclear risk | Comparable baseline characteristics of age, height, and weight but not cause of infertility |
Humaidan 2004.
| Methods | Randomisation: computer‐generated Allocation concealment: sealed unlabelled envelopes Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 200 No. analysed: 200 Intention‐to‐treat analysis: yes Power and sample calculations described Duration of trial: 9 months, from April to December 2002 |
|
| Participants | Women in IVF programme undergoing transvaginal oocyte retrieval Mean age: 31 to 32 years (range 22 to 39) Cause of infertility: male, tubal disease, endometriosis, anovulation, unexplained Similar demographic and infertility characteristics at baseline |
|
| Interventions |
Conscious sedation and analgesia group received premedication (oral benzodiazepine 10 mg); EA group did not |
|
| Outcomes |
Other outcomes reported: no. of cycles, no. of embryos transferred, implantation rate |
|
| Notes | Denmark Single centre Skiive Hospital Funding: not stated Definition of pregnancy not documented |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | Adequate: sealed unlabelled envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding not possible owing to the nature of the interventions Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
Lier 2014.
| Methods | Randomisation: computer‐generated list Allocation concealment: not reported Blinding of participants/investigators: open‐label design, study not blind to participants nor to physicians and investigators Blinding of assessors: open‐label design, study not blind to participants nor to physicians and investigators No. randomised: 76 No. analysed: 76 Intention‐to‐treat analysis: yes Power and sample calculations described Duration of trial: 5 days after oocyte retrieval; duration of treatment: from 8 to 8.4 minutes |
|
| Participants | Women who had an indication for IVF/intracytoplasmic sperm injection (ICSI) Mean age: 35 ± 5 years Mean BMI: 24 ± 4 Causes of infertility (primary, secondary, endometriosis): similar in both groups IVF or ICSI: similar in both groups No. of previous cycles: similar in both groups |
|
| Interventions | 1. Control: patient‐controlled analgesia with IV remifentanil (0.5 µg/kg per bolus) via a pump; diclofenac suppository 50 mg given 30 minutes before remifentanil (N = 36) 2. Intervention: anaesthetist‐administered standard pethidine therapy with IM pethidine (2 mg/kg body weight) and midazolam (5 mg per os), given 30 minutes before oocyte retrieval; no diclofenac suppository given (N = 40) Both groups received atropine 0.5 mg IM 30 minutes before oocyte retrieval. |
|
| Outcomes | 1. Primary: intraoperative and postoperative pain via NRS (numeric rating scale) 2. Secondary: ongoing pregnancy rate, side effects of analgesia, postoperative complications, patient satisfaction |
|
| Notes | The Netherlands University Medical Centre Funding: VU University Medical Center (registered at the Netherlands Trial Registration (NTR 2431)) Pregnancy defined by positive foetal cardiac activity at 12 weeks' gestation on ultrasound |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Open‐label design, not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
Lok 2002.
| Methods | Randomisation: computer‐generated Allocation concealment: sealed opaque envelopes Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 110 No. analysed: 106 Intention‐to‐treat analysis: no Power and sample calculations described Duration of trial: not stated |
|
| Participants | Women undergoing transvaginal oocyte retrieval Mean age: 33 to 35 years Cause of infertility: tubal disease, male factor, endometriosis, anovulation, unexplained Women in control group 2 years younger than women in intervention group (P = 0.01); other baseline characteristics similar |
|
| Interventions |
No premedication in either group |
|
| Outcomes |
|
|
| Notes | China Single centre Chinese University of Hong Kong Funding: not stated Loss to follow‐up (N = 4) in intervention group due to pump failure (n = 1) and personal reasons (n = 3) Definition of pregnancy not documented |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | Adequate: sealed envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding not possible owing to the nature of the interventions Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Four lost to follow‐up (3%) |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Unclear risk | Significant differences in age between the 2 groups Comparable infertility characteristics at baseline |
Ma 2008.
| Methods | Randomisation: random numbers table Allocation concealment: methods unclear Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 80 No. analysed: 80 Intention‐to‐treat analysis: yes Power and sample calculations not described Duration of trial: 8 months from February to September 2006 |
|
| Participants | Women undergoing oocyte retrieval Mean age: 31 to 33 years Cause of infertility: tubal disease, PCOS, endometriosis, male factor, unexplained Similar demographic and infertility characteristics at baseline |
|
| Interventions |
|
|
| Outcomes |
Other outcomes reported: changes in blood pressure |
|
| Notes | China Single centre Zhejiang University, Hangzhou, China Funding: not stated Paper in Chinese |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation table |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
Matsota 2012.
| Methods | Randomisation: group allocation envelopes randomly selected by co‐investigators (additional information from trial author) Allocation concealment: group allocations in sealed envelopes kept in locked office (additional information from trial author) Blinding of participants/investigators: no, owing to the nature of the intervention Blinding of assessors: yes, assessors blind to group allocation (additional information from trial author) No. randomised: 58 No. analysed: 58 Intention‐to‐treat analysis: yes Power and sample calculations not described Duration of trial: not stated |
|
| Participants | Women scheduled for ultrasound transvaginal oocyte retrieval Mean age 34 to 35.5 years Mean body weight: 62 kg Cause of infertility: 51 cases of primary infertility, 7 cases of secondary infertility Similar demographic and infertility characteristics at baseline |
|
| Interventions | 1. Control: conscious sedation/analgesia with remifentanil (a bolus dose 1 μg.kg ‐1 of remifentanil administered slowly during 1 minute following by a continuous IV infusion at a rate of 0.15 to 0.4 μg.kg ‐1.min ‐1) (N = 29) 2. Intervention: general anaesthesia with IV propofol 2 mg.kg‐1 and alfentanil 15 μg.kg ‐1, maintained with propofol continuous infusion at a rate of 2 to 4 mg.kg ‐1.h ‐1 (N = 29). All participants unpremedicated and received midazolam 2 mg IV just before start of the procedure |
|
| Outcomes | Secondary: clinical pregnancy rate, fertilisation rate, side effects, postoperative complications, patient satisfaction Other outcomes reported: implantation and cleavage rates |
|
| Notes | Greece Single centre University Hospital Funding: not stated Definition of pregnancy: over 16 weeks of gestation |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Group allocation envelopes randomly selected by co‐investigators |
| Allocation concealment (selection bias) | Low risk | Group allocations in sealed envelopes kept in locked office (additional information from trial author) |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding not possible owing to the nature of the interventions Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
Meng 2008.
| Methods | Randomisation: random numbers table Allocation concealment: method unclear Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 316 No. analysed: 316 Intention‐to‐treat analysis: yes Power and sample calculations not reported Duration of trial: 5 months, from March to July 2007 |
|
| Participants | Women undergoing transvaginal oocyte retrieval Mean age: 31 years (23 to 46 years) Cause of infertility: tubal disease, PCOS, endometriosis, male factor, unexplained Similar demographic and infertility characteristics at baseline |
|
| Interventions |
|
|
| Outcomes |
Other outcomes reported: changes in pulse and blood pressure |
|
| Notes | China Single centre Nanjing university of TCM Funding: not stated Paper in Chinese |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation table |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding not possible owing to the nature of the interventions Assessors blinded to group allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
Meng 2009.
| Methods | Randomisation: random number table Allocation concealment: methods unclear Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 700 No. analysed: 694 Intention‐to‐treat analysis: no Power and sample calculations not reported Duration of trial: 8 months, from June 2007 to January 2008 |
|
| Participants | Women undergoing transvaginal oocyte retrieval Mean age: 30 to 31 years Cause of infertility: not reported, duration of infertility < 5 years Similar demographic and infertility characteristics at baseline |
|
| Interventions |
|
|
| Outcomes | Primary: pain (unclear whether intraoperative or postoperative) according to pain thresholds | |
| Notes | China Single centre Nanjing University of TCM Funding: not stated No reason given for dropout (N = 6) Paper in Chinese |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation table |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding not possible owing to the nature of the interventions Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Six lost to follow‐up (2 in control group; 4 in intervention group), no reason given |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
Ng 2001.
| Methods | Randomisation: computer‐generated Allocation concealment: sealed envelopes Blinding of participants/investigators: yes Blinding of assessors: yes No. randomised: 150 No. analysed: 150 Intention‐to‐treat analysis: yes Power and sample calculations described Duration of trial: not stated |
|
| Participants | Women undergoing egg collection Mean age: 35 years (range 27 to 43 years) Cause of infertility: tuboperitoneal, male factor, endometriosis, unexplained Similar demographic and infertility characteristics at baseline |
|
| Interventions |
Both groups received premedication (IM pethidine 50 mg and promethazine 25 mg) |
|
| Outcomes |
Other outcomes reported: no. of embryos transferred, implantation rate, multiple pregnancy rate |
|
| Notes | China Single centre University of Hong Kong Funding: not stated Definition of pregnancy not documented |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | Adequate: sealed envelopes |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Both participant and doctor carrying out the procedure were blind to the sedation given Nurses not involved in the Unit asked participants about pain levels |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
Ocal 2002.
| Methods | Randomisation: method unclear Allocation concealment: method unclear Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 58 No. analysed: 58 Intention‐to‐treat analysis: yes Power and sample calculations not reported Duration of study: not stated |
|
| Participants | Women admitted for vaginal oocyte retrieval Mean age: 31 to 33 years (range 25 to 41 years) Cause of infertility: not reported Similar baseline characteristics of age |
|
| Interventions |
|
|
| Outcomes | Primary: intraoperative pain score (Likert scale) | |
| Notes | Turkey Single centre Istanbul University Funding: not stated Paper in Turkish |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method unclear |
| Allocation concealment (selection bias) | Unclear risk | Method unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding not possible owing to the nature of the interventions Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Unclear risk | Comparable age but not cause of infertility |
Ozturk 2006.
| Methods | Randomisation: method unclear Allocation concealment: sealed envelopes Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 100 No. analysed: 100 Intention‐to‐treat analysis: yes Power and sample calculations not reported Duration of study: not stated |
|
| Participants | Women scheduled to undergo transvaginal oocyte retrieval Mean age: 33 to 35 years Cause of infertility: tuboperitoneal, male factor, anovulation, unexplained Similar demographic and infertility characteristics at baseline |
|
| Interventions |
All women not premedicated |
|
| Outcomes |
Other outcomes reported: remifentanil consumption, duration of anaesthesia, duration of procedure, no. of oocytes retrieved, retrieval rate |
|
| Notes | Turkey Single centre Gazi University, Ankara Funding: not stated Definition of pregnancy not documented |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method unclear |
| Allocation concealment (selection bias) | Low risk | Closed envelope |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding not possible owing to the nature of the interventions Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
Ramsewak 1990.
| Methods | Randomisation: by pharmacy Allocation concealment: sealed envelopes kept in medicine cupboard Blinding of participants/investigators: yes Blinding of assessors: no No. randomised: 30 No. analysed: 24 Intention‐to‐treat analysis: no Power and sample calculations not reported Duration of trial: 1 month, July 1989 |
|
| Participants | Women undergoing follicular aspiration Mean age: not reported Cause of infertility: not reported Baseline characteristics comparison not reported |
|
| Interventions |
|
|
| Outcomes | Primary: intraoperative pain (VAS) | |
| Notes | England Single centre Sheffield Univerity Funding: not stated 6 women (20%) excluded after randomisation 2 – transvaginal aspiration inaccessible 2 ‐ spontaneous rupture of follicle before needle insertion 1 ‐ failure to complete VAS score sheet 1 ‐ ampoule accidentally broken |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation by pharmacy |
| Allocation concealment (selection bias) | Low risk | Adequate: sealed envelope |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Neither medical and nursing personnel nor the patient knew which ampoule was used Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 6 women (20%) lost to follow‐up, reasons given |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Unclear risk | Baseline demographic and infertility characteristics comparison not reported |
Sator‐Katzenschlager 2006.
| Methods | Randomisation: computer‐generated Allocation concealment: method unclear Blinding of participants/investigators: yes Blinding of assessors: yes No. randomised: 94 No. analysed: 93 Intention‐to‐treat analysis: no Power and sample calculations described Duration of trial: 7 months, from April to December 2004 |
|
| Participants | Women undergoing oocyte aspiration Mean age: 33 to 34 years Cause of infertility: male factor, tubal disease, endometriosis, PCOS, unexplained Similar demographic and infertility characteristics at baseline |
|
| Interventions | Randomised in proportions of 1:1:1 to control and 2 interventions
All participants received IV metamizole 1 g 15 minutes before procedure. |
|
| Outcomes | Primary: intraoperative and postoperative pain scores (VAS 0 to 100) Secondary: pregnancy rate, side effects, patient satisfaction (good, moderate, reject) | |
| Notes | Austria Single centre Medical University of Vienna Funding: not stated Definition of pregnancy not documented |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | Methods unclear |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants and investigators blinded to the randomisation A second gynaecologist performed oocyte retrieval, and another doctor asked for outcome parameters to ensure blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | One participant in control group excluded owing to impaired compliance |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
Stener‐Victorin 1999.
| Methods | Randomisation: random number table Allocation concealment: sealed envelopes Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 150 No. analysed: 149 Intention‐to‐treat analysis: no Power and sample calculations not reported Duration of trial: 8 months, from September 1996 to May 1997 |
|
| Participants | Women undergoing oocyte aspiration Mean age: 33 to 34 years (range 35 to 46 years) Cause of infertility: male factor, tubal disease, endometriosis, unexplained Similar demographic and infertility characteristics at baseline |
|
| Interventions |
No premedication in either group |
|
| Outcomes |
|
|
| Notes | Sweden Multi‐centre (3 IVF centres) Goteburg University Funding: Foundation for Acupuncture and Alternative Biological Treatment Methods, and the Swedish Research Council PCB (10 mL lidocaine): given at 5 mg/mL at one IVF centre and at 10 mg/mL at the other 2 IVF centres One participant in the control group (0.7%) was excluded after randomisation because of protocol violation (received premedication) Definition of pregnancy not documented |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Each centre used its own randomisation. Method: random numbers table |
| Allocation concealment (selection bias) | Low risk | Adequate: sealed envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding not possible owing to the nature of the interventions Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | One participant lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
Stener‐Victorin 2003.
| Methods | Randomisation: in blocks of 20 to each group, random numbers table Allocation concealment: sealed unlabelled envelopes Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 286 No. analysed: 274 Intention‐to‐treat analysis: no Power and sample calculations described Duration of trial: from 1999 to 2001 |
|
| Participants | Women undergoing oocyte aspiration Mean age: 33 years (range 22 to 38 years) Cause of infertility: male factor, tubal disease, endometriosis, PCOS, unexplained Similar demographic and infertility characteristics at baseline |
|
| Interventions |
No premedication in either group |
|
| Outcomes |
|
|
| Notes | Sweden Multi‐centre (5 IVF centres) Goteburg University Funding: Hjalmar Svensson's Foundation, the Wilhelm and Martina Lundgren's Foundation Twelve women (4%) dropped out (7 in control group, 5 in intervention group): 4 ‐ administration failure 1 ‐ fall in blood pressure 1 ‐ nausea 6 ‐ withdrew voluntarily Definition of pregnancy not documented |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Each centre used its own randomisation Method: random numbers table |
| Allocation concealment (selection bias) | Low risk | Adequate: sealed envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding not possible owing to the nature of the interventions Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 12 participants lost to follow‐up (4%) |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
Thompson 2000.
| Methods | Randomisation: computer‐generated Allocation concealment: sealed opaque envelopes Blinding of participants/investigators: no Blinding of assessors: no No. randomised: 112 No. analysed: 112 Intention‐to‐treat analysis: yes Power and sample calculations described Duration of trial: not stated |
|
| Participants | Women undergoing outpatient oocyte recovery Mean age: 32 to 34 years Cause of infertility: not reported Similar baseline characteristics of age, height and weight, and history of previous oocyte recovery |
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes | Scotland Single centre Aberdeen University Funding: not stated Definition of pregnancy not documented |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Low risk | Adequate: sealed envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding not possible owing to the nature of the interventions Blinding of assessors not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Low risk | Comparable demographic and infertility characteristics at baseline |
Zelcer 1992.
| Methods | Randomisation: method unclear Allocation concealment: method unclear Blinding of participants/investigators: no Blinding of assessors: yes No. randomised: 80 No. analysed: 80 Intention‐to‐treat analysis: yes Power and sample calculations not reported Duration of trial: not stated |
|
| Participants | Women presenting for outpatient oocyte retrieval Mean age: 32 to 34 years Cause of infertility: not reported Similar baseline characteristics of age, height, and weight |
|
| Interventions |
All participants premedicated with midazolam 0.02 mg/kg |
|
| Outcomes |
|
|
| Notes | USA Single centre University of Texas Funding: Janssen‐Cilag |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method unclear |
| Allocation concealment (selection bias) | Unclear risk | Method unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding not possible owing to the nature of the interventions Postoperative side effects recorded by staff unaware of treatment groups |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Unclear risk | Comparable baseline characteristics of age, height, and weight but not cause of infertility |
Types of analgesic
Diazepam ‐ sedative and anxiolytic
Diclofenac suppository ‐ analgesic
Dolantin ‐ analgesic, same as pethidine
Electro‐acupuncture ‐ pain‐relieving method that activates endogenous pain‐inhibiting systems such as the spinal/segmental gate mechanism and the endogenous opoid systems. Any acupuncture effect rests on physiological and/or psychological mechanisms
Fentanyl/alfentanil/remifentanil ‐ analgesia
Isodesox ‐analgesic and sedative inhalational agent
Midazolam ‐ sedative and anxiolytic
Pethidine ‐ analgesic
Pirosikam ‐ analgesic (non‐steroidal anti‐inflammatory drug ‐ NSAID)
Propofol ‐ sedative and anxiolytic
Abbreviations
ASA = American Society of Anesthesiologists
BMI = body mass index
EA = electro‐acupuncture
IM = intramuscular
IV = intravenous
IVF = in vitro fertilisation
µg = microgram
mg = milligram
mg/kg = milligrams per kilogram
min = minute
mL = millilitre
no. = number
PCB = paracervical block. This involves injecting local anaesthetic adjacent to the cervix. Epidural analgesia involves injecting local anaesthetic into the epidural space close to the spinal cord to numb the lower part of the body
PCS = patient‐controlled sedation and analgesia
PAS = physician‐administered sedation and analgesia
PCOS = polycystic ovary syndrome
TCI = system that maintains a particular target plasma drug concentration via standard pharmacokinetic equations
VAS = visual analogue scale, usually a 100‐mm linear analogue scale
yr = year
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Atashkhoii 2006 | Unable to obtain evidence of randomisation |
| Bovenschen 2002 | Conscious sedation and analgesia not one of the comparators |
| Bumen 2010 | Conscious sedation and analgesia not one of the comparators |
| Casati 1999 | Conscious sedation and analgesia not one of the comparators |
| Corson 1994 | Conscious sedation and analgesia not one of the comparators |
| Godoy 1993 | Conscious sedation and analgesia not one of the comparators |
| Gotz 2014 | Unable to obtain evidence of randomisation |
| Hadimioglu 2002 | General anaesthesia. Conscious sedation not one of the comparators |
| Hong 2005 | Conscious sedation and analgesia among low‐ and high‐anxiety patients. No comparison with another technique |
| Manica 1993 | Spinal anaesthesia dose finding. Conscious sedation and analgesia not one of the comparators |
| Martin 1999 | Spinal anaesthesia. Conscious sedation and analgesia not one of the comparators |
| Muir 1995 | Subperitoneal xylocaine. Spinal anaesthesia dose finding. Conscious sedation and analgesia not one of the comparators |
| Ng 1999 | Paracervical block with lignocaine vs normal saline vs no paracervical block. Conscious sedation and analgesia not one of the comparators |
| Ng 2000 | Paracervical block dose finding. Conscious sedation and analgesia not one of the comparators |
| Ng 2002 | Premedication versus no premedication. Conscious sedation and analgesia not one of the comparators |
| Ng 2003 | Paracervical block dose finding. Conscious sedation and analgesia not one of the comparators |
| Oliveira 2016 | Conscious sedation and analgesia not one of the comparators |
| Ongun 2002 | Conscious sedation and analgesia not one of the comparators |
| Ramzy 2001 | Conscious sedation and analgesia not one of the comparators |
| Saleh 2012 | Conscious sedation and analgesia not one of the comparators |
| Sarikaya 2011 | Population not clarified. No response from trial author when contacted |
| Singh 2014 | Unable to obtain evidence of randomisation |
| Tsen 2001 | Spinal anaesthesia. Conscious sedation not one of the comparators |
| Zaccabri 2001 | Paracervical block vs vaginal anaesthetic cream. Conscious sedation and analgesia not one of the comparators |
| Zhang 2013 | Conscious sedation and analgesia not one of the comparators |
Characteristics of studies awaiting assessment [ordered by study ID]
Chen 2012.
| Methods | Randomisation: random numbers table used to divide into 2 groups Allocation concealment: not reported Blinding of participants/investigators: not reported Blinding of assessors: not reported No. randomised: 134 No. analysed: 134 Intention‐to‐treat analysis: yes Power and sample calculations: not described Duration of trial: not stated |
| Participants | Patients undergoing IVF‐E |
| Interventions | 1. Control: intramuscular (IM) Dolantin 50 milligrams (mg) 30 minutes before oocyte retrieval (N = 67) 2. Intervention: IM Dolantin 50 mg 30 minutes before electro‐acupuncture (N = 67) |
| Outcomes | 1. Primary: intraoperative pain (World Health Organization pain scale: Grade I (scores 1 to 3, minimal pain), Grade II (scores 4 to 6, mild pain), Grade III (scores 7 to 9, moderate pain), Grade IV (scores 10 to 12, severe pain)): postoperative (1 hour (h), 2 hours postoperatively) abdominal pain 2. Secondary: side effects of analgesia |
| Notes | China Reproductive Medicine Centre Funding: Gansu Province Paper in Chinese NB. Data unclear, awaiting response from trial authors |
IM = intramuscular
Characteristics of ongoing studies [ordered by study ID]
Kassira 2015.
| Trial name or title | A randomised controlled trial of oral acetaminophen for analgesic control after transvaginal oocyte retrieval |
| Methods | Double‐blind randomised controlled trial |
| Participants | Women undergoing IVF |
| Interventions | Transvaginal oocyte retrieval |
| Outcomes | Post‐procedure pain |
| Starting date | Not clear |
| Contact information | Email of co‐author: mpowell77@sky.com |
| Notes | Conference abstract published 2015. Trial authors/co‐authors contacted, no response |
Differences between protocol and review
For the 2012 update, as a result of peer review, review authors amended the objectives of the review to provide a clearer focus. We reorganised the list of outcomes, with intraoperative and postoperative pain as the primary outcomes, and clinical pregnancy rate as one of the secondary outcomes. We changed the review title to "Pain relief for women undergoing oocyte retrieval for assisted reproduction."
Contributions of authors
IK developed the protocol, screened citations, extracted data, assessed trial quality and contacted authors, entered data into RevMan, and wrote the review.
SB helped to develop the protocol and helped to write and finalise the review. SB was a consultant on clinical issues.
EP and RW screened citations, extracted data, assessed trial quality, and commented on the review.
Sources of support
Internal sources
None, Other.
External sources
None, Other.
Declarations of interest
IK, RW and EP have no conflicts to report.
SB has received support for travel and accommodation as invited speaker on topics unrelated to the current work.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Ben‐Shlomo 1999 {published data only}
- Ben‐Shlomo I, Moskovich R, Katz Y, Shalev E. Midazolam/ketamine sedative combination compared with fentanyl/propofol/isoflurane anaesthesia for oocyte retrieval. Human Reproduction 1999;14(7):1757‐9. [DOI] [PubMed] [Google Scholar]
Bhattacharya 1997 {published data only}
- Bhattacharya S, MacLennan F, Hamilton MP, Templeton A. How effective is patient‐controlled analgesia? A randomized comparison of two protocols for pain relief during oocyte recovery. Human Reproduction 1997;12(7):1440‐2. [DOI] [PubMed] [Google Scholar]
Cook 1993 {published data only}
- Cook LB, Lockwood GG, Moore CM, Whitwam JG. True patient‐controlled sedation. Anaesthesia 1993;48(12):1039‐44. [DOI] [PubMed] [Google Scholar]
Coskun 2011 {published data only}
- Coskun D, Gunaydin B, Tas A, et al. A comparison of three different target‐controlled remifentanil infusion rates during target‐controlled propofol infusion for oocyte retrieval. Clinics 2011;66(5):811‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elnabtity 2017 {published data only}
- Elnabtity AM, Selim MF. A prospective randomized trial comparing dexmedetomidine and midazolam for conscious sedation during oocyte retrieval in an in vitro fertilization program. Anesthesia Essays and Researches 2017;11:34‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gejervall 2005 {published data only}
- Gejervall AL, Stener‐Victorin E, Moller A, Janson PO, Werner C, Bergh C. Electro‐acupuncture versus conventional analgesia: a comparison of pain levels during oocyte aspiration and patients' experiences of well‐being after surgery. Human Reproduction 2005;20:728‐35. [DOI] [PubMed] [Google Scholar]
Guasch 2005 {published data only}
- Guasch E, Ardoy M, Cuadrado C, Gonzalez Gancedo P, Gonzalez A, Gilsanz F. [Comparison of 4 anesthetic techniques for in vitro fertilization]. [Spanish]. Revista Espanola de Anestesiologia y Reanimacion 2005;52:9‐18. [PubMed] [Google Scholar]
Gunaydin 2007 {published data only}
- Gunaydin B, Ozulgen IK, Ozturk E, Tekgul ZT, Kaya K. Remifentanil versus remifentanil with paracervical block on plasma remifentanil concentrations and pulmonary function tests for transvaginal ultrasound‐guided oocyte retrieval. Journal of Opioid Management 2007;3:267‐72. [DOI] [PubMed] [Google Scholar]
Humaidan 2004 {published data only}
- Humaidan P, Stener‐Victorin E. Pain relief during oocyte retrieval with a new short duration electro‐acupuncture technique ‐ an alternative to conventional analgesic methods. Human Reproduction 2004;19(6):1367‐72. [DOI] [PubMed] [Google Scholar]
Lier 2014 {published data only}
- Lier M, Douwenga W, Yilmaz F, Schats R, Hompes P, Boer C, et al. Patient‐controlled remifentanil analgesia as alternative for pethidine with midazolam during oocyte retrieval in IVF/ICSI procedures: a randomized controlled trial. Pain Practice 2015;15(5):487‐95. [DOI] [PubMed] [Google Scholar]
Lok 2002 {published data only}
- Lok IH, Chan MTV, Chan DLW, Cheung LP, Haines CJ, Yuen PM. A prospective randomized trial comparing patient‐controlled sedation using propofol and alfentanil and physician‐administered sedation using diazepam and pethidine during transvaginal ultrasound‐guided oocyte retrieval. Human Reproduction 2002;17(8):2101‐6. [DOI] [PubMed] [Google Scholar]
Ma 2008 {published data only}
- Ma YY, Shen Y, Zhang LS, Qian YL, Chen XZ. [Comparison of midazolam and propofol as conscious sedation in oocyte retrieval of IVE‐ET]. [Chinese]. Journal of Zhejiang University (Medical Sciences) 2008;37:304‐7. [DOI] [PubMed] [Google Scholar]
Matsota 2012 {published data only}
- Matsota P, Sidiropoulou T, Batistaki C, Giannaris D, Pandazi A, Krepi H, et al. Analgesia with remifentanil versus anesthesia with propofol‐alfentanil for transvaginal oocyte retrieval: a randomized trial on their impact on in vitro fertilization outcome. Middle East Journal of Anaesthesiology 2012;21(5):685‐92. [PubMed] [Google Scholar]
Meng 2008 {published data only}
- Meng P, Wang LL, Xu B, Sun HX. [Application of acupuncture compound anesthesia in transvaginal ultrasound‐guided oocyte retrieval]. [Chinese]. Chinese Acupuncture and Moxibustion 2008;28(6):451‐5. [PubMed] [Google Scholar]
Meng 2009 {published data only}
- Meng P, Wang LL. [Analgesic effect of acupuncture compound anesthesia for patients of different pain thresholds]. [Chinese]. Chinese Acupuncture and Moxibustion 2009;29(1):29‐31. [PubMed] [Google Scholar]
Ng 2001 {published data only}
- Ng EH, Chui DK, Tang OS, Ho PC. Paracervical block with and without conscious sedation: a comparison of the pain levels during egg collection and the postoperative side effects. Fertility and Sterility 2001;75(4):711‐7. [DOI] [PubMed] [Google Scholar]
Ocal 2002 {published data only}
- Ocal P, Cepni I, Idil M, Akbas F, Aksu M. Analgesic effect of pethidine and piroksikam during oocyte aspiration: a comparative study. Jinekoloji ve Obstetrik Dergisi 2002;88(3)16:230‐3. [Google Scholar]
Ozturk 2006 {published data only}
- Ozturk E, Gunaydin B, Karabacak O, Tuncer B, Erdem M, Erdem A, et al. Remifentanil infusion and paracervical block combination versus remifentanil infusion alone during in vitro fertilisation (IVF). Turkish Journal of Medical Sciences 2006;36:105‐11. [Google Scholar]
Ramsewak 1990 {published data only}
- Ramsewak SS, Kumar A, Welsby R, Mowforth A, Lenton EA, Cooke ID. Is analgesia required for transvaginal single‐follicle aspiration in in vitro fertilization? A double‐blind study. Journal of In Vitro Fertilization and Embryo Transfer 1990;7(2):103‐6. [DOI] [PubMed] [Google Scholar]
Sator‐Katzenschlager 2006 {published data only}
- Sator‐Katzenschlager SM, Wolfler MM, Kozek‐Langenecker SA, Sator K, Sator PG, Li B, et al. Auricular electro‐acupuncture as an additional perioperative analgesic method during oocyte aspiration in IVF treatment. Human Reproduction 2006;21:2114‐20. [DOI] [PubMed] [Google Scholar]
Stener‐Victorin 1999 {published data only}
- Stener‐Victorin E, Waldenstrom U, Nilsson L, Wikland M, Janson PO. A prospective randomized study of electro‐acupuncture versus alfentanil as anaesthesia during oocyte aspiration in in‐vitro fertilization. Human Reproduction 1999;14(10):2480‐4. [DOI] [PubMed] [Google Scholar]
Stener‐Victorin 2003 {published data only}
- Stener‐Victorin E, Waldenstrom U, Wikland M, Nilsson L, Hagglund L, Lundeberg T. Electro‐acupuncture as a perioperative analgesic method and its effects on implantation rate and neuropeptide Y concentrations in follicular fluid. Human Reproduction 2003;18(7):1454‐60. [DOI] [PubMed] [Google Scholar]
Thompson 2000 {published data only}
- Thompson N, Murray S, MacLennan F, Ross JA, Tunstall ME, Hamilton MP, et al. A randomised controlled trial of intravenous versus inhalational analgesia during outpatient oocyte recovery. Anaesthesia 2000;55(8):770‐3. [DOI] [PubMed] [Google Scholar]
Zelcer 1992 {published data only}
- Zelcer J, White PF, Chester S, Paull JD, Molnar R. Intraoperative patient‐controlled analgesia: an alternative to physician administration during outpatient monitored anesthesia care. Anesthesia & Analgesia 1992;75:41‐4. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Atashkhoii 2006 {published data only}
- Atashkhoii S, Abdollahi S, Farzadi L, Ghasemzadeh A. Conscious sedation with and without paracervical block for transvaginal ultrasonically guided egg collection. Human Reproduction 2006;21 Suppl:i135. [Google Scholar]
Bovenschen 2002 {published data only}
- Bovenschen JL, Lawrence KA, Abuzeid M, Jones ML, Achwal ML, Verril H, et al. Remifentanyl and fentanyl concentrations in follicular fluid during transvaginal oocyte retrieval. Middle East Fertility Society Journal 2002;7(1):18‐23. [Google Scholar]
Bumen 2010 {published data only}
- Bumen S, Gunusen I, Firat V, Karaman S, Akdogan A, Tavmergen Goker EN. A comparison of intravenous general anesthesia and paracervical block for in vitro fertilization: effects on oocytes using the transvaginal technique. Turkish Journal of Medical Sciences 2011;41(5):801‐8. [Google Scholar]
Casati 1999 {published data only}
- Casati A, Valentini G, Zangrillo A, Senatore R, Mello A, Airaghi B, et al. Anaesthesia for ultrasound guided oocyte retrieval: midazolam/remifentanil versus propofol/fentanyl regimens. European Journal of Anaesthesiology 1999;16(11):773‐8. [DOI] [PubMed] [Google Scholar]
Corson 1994 {published data only}
- Corson SL, Batzer FR, Gocial B, Kelly M, Gutmann JN, Go KJ, et al. Is paracervical block anesthesia for oocyte retrieval effective?. Fertility and Sterility 1994;62(1):133‐6. [DOI] [PubMed] [Google Scholar]
Godoy 1993 {published data only}
- Godoy H, Erard P, Munck L, Camus M, Gepts E, Steirteghem AC, et al. Comparison of two local anaesthetics in transvaginal ultrasound‐guided oocyte retrieval. Human Reproduction 1993;8(7):1093‐7. [DOI] [PubMed] [Google Scholar]
Gotz 2014 {published data only}
- Gotz T, Kiddop DA, Motan T. Optimizing patient analgesic experience during in vitro fertilisation (Conference: 70th Annual Meeting of the American Society for Reproductive Medicine, ASRM 2014 Honolulu, HI United States).. American Society for Reproductive Medicine. 2014; Vol. 102, issue 3:e132.
Hadimioglu 2002 {published data only}
- Hadimioglu N. Comparison of various sedation regimens for transvaginal oocyte retrieval. Fertility and Sterility 2002;78:648‐9. [DOI] [PubMed] [Google Scholar]
Hong 2005 {published data only}
- Hong JY, Jee YS, Luthardt FW. Comparison of conscious sedation for oocyte retrieval between low‐anxiety and high‐anxiety patients. Journal of Clinical Anesthesia 2005;17:549‐53. [DOI] [PubMed] [Google Scholar]
Manica 1993 {published data only}
- Manica VS, Bader AM, Fragneto R, Gilbertson L, Datta S. Anesthesia for in vitro fertilization: a comparison of 1.5% and 5% spinal lidocaine for ultrasonically guided oocyte retrieval. Anesthesia & Analgesia 1993;77(3):453‐6. [DOI] [PubMed] [Google Scholar]
Martin 1999 {published data only}
- Martin R, Tsen LC, Tzeng G, Hornstein MD, Datta S. Anesthesia for in vitro fertilization: the addition of fentanyl to 1.5% lidocaine. Anesthesia & Analgesia 1999;88(3):523‐6. [DOI] [PubMed] [Google Scholar]
Muir 1995 {published data only}
- Muir SE, Bowman MC, Mortimer D, Jansen RPS. Local xylocaine for transvaginal oocyte pick‐up: a randomised, double‐blind, placebo‐controlled trial. Fertility Society of Australia/Australian Gynaecological Endoscopy Society. 1995:78.
Ng 1999 {published data only}
- Ng EH, Tang OS, Chui DK, Ho PC. A prospective, randomized, double‐blind and placebo‐controlled study to assess the efficacy of paracervical block in the pain relief during egg collection in IVF. Human Reproduction 1999;14(11):2783‐7. [DOI] [PubMed] [Google Scholar]
Ng 2000 {published data only}
- Ng EH, Tang OS, Chui DK, Ho PC. Comparison of two different doses of lignocaine used in paracervical block during oocyte collection in an IVF programme. Human Reproduction 2000;15(10):2148‐51. [DOI] [PubMed] [Google Scholar]
Ng 2002 {published data only}
- Ng EH, Miao B, Ho PC. Anxiolytic premedication reduces preoperative anxiety and pain during oocyte retrieval. A randomized double‐blinded placebo‐controlled trial. Human Reproduction 2002;17(5):1233‐8. [DOI] [PubMed] [Google Scholar]
Ng 2003 {published data only}
- Ng EH, Miao B, Ho PC. A randomized double‐blind study to compare the effectiveness of three different doses of lignocaine used in paracervical block during oocyte retrieval. Journal of Assisted Reproduction and Genetics 2003;20(1):8‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Oliveira 2016 {published data only}
- Oliveira G, Serralheiro FC, Fonseca F, Ribeiro O, Adami F, Christofolini D, et al. Randomized double‐blind clinical trial comparing two anesthetic techniques for ultrasound‐guided transvaginal follicular puncture. Einstein 2016;14(3):305‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ongun 2002 {published data only}
- Ongun B, Ozornek MH, Ergin E, Karatekeli E. Prospective analysis of propofol versus midazolam for anaesthesia in oocyte retrieval (P‐346). Abstract of 18th Annual Meeting of ESHRE, Vienna, Austria. 2002:120.
Ramzy 2001 {published data only}
- Ramzy AM I, Hefzy OA, Rhodes CA, Sattar MM, Al‐Wasseef MM, Serour G, et al. Ovarian sub‐capsular and vaginal needle site infiltration of local anaesthetic: evaluation of a novel method of pain relief after oocyte retrieval. Middle East Fertility Society Journal 2001;6(2):169‐74. [Google Scholar]
Saleh 2012 {published data only}
- Saleh S, Elshmaa N, Ismail M. A comparison of two different regimens of total intravenous anesthesia for transvaginal ultrasound‐guided oocyte retrieval. Middle East Fertility Society Journal 2012;17:256‐61. [Google Scholar]
Sarikaya 2011 {published data only}
- Sarikaya HB, Iyilikci L, Gulekli B, Posaci C, Erbil Dogan O, et al. Comparison of the effects of 2 different doses of remifentanil infusion for sedation during in‐vitro fertilization procedure. Saudi Medical Journal 2011;32(7):689‐94. [PubMed] [Google Scholar]
Singh 2014 {published data only}
- Singh S, Dhaliwal LK, Jain K, Gainder S. Dexmedetomidine‐fentanyl versus pethidine‐promethazine for conscious sedation and analgesia during oocyte retrieval for in vitro fertilisation (33rd Annual European Society of Regional Anaesthesia and Pain Therapy, ESRA Congress 2014 Seville Spain). Regional Anesthesia and Pain Medicine. ESRA, 2014; Vol. 39, No 5, Suppl 1:E191.
Tsen 2001 {published data only}
- Tsen LC, Schultz R, Martin R, Datta S, Bader AM. Intrathecal low‐dose bupivacaine versus lidocaine for in vitro fertilization procedures. Regional Anesthesia and Pain Medicine 2001;26(1):52‐6. [DOI] [PubMed] [Google Scholar]
Zaccabri 2001 {published data only}
- Zaccabri A, Fresson J, Denis E, Guillet‐May F, Barbarino P, Routiot T. Ponction ovarienne en fecondation in vitro: quelle analgesie?. Gynecologie Obstetrique & Fertilite 2001;29:594‐8. [DOI] [PubMed] [Google Scholar]
Zhang 2013 {published data only}
- Zhang J, Wang X, Lu R. Analgesic effect of acupuncture at hegu (LI 4) on transvaginal oocyte retrieval with ultrasonography. Journal of Traditional Chinese Medicine 2013;33(3):294‐7. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Chen 2012 {published data only}
- Chen Q, Wei Q, Zhang X. Effects of electroacupuncture on supplementary analgesia and improvement of adverse reactions induced by dolantin in oocyte retrieval. [Chinese]. [Chinese] Zhongguo Zhenjiu 2012;32(12):1113‐6. [PubMed] [Google Scholar]
References to ongoing studies
Kassira 2015 {published and unpublished data}
- Kassira S, Bates G, Powell M, Bouknight JM, McLean M. A randomized controlled trial of oral acetaminophen for analgesic control after transvaginal oocyte retrieval. (Conference: 71st Annual Meeting of the American Society for Reproductive Medicine, ASRM 2015 Baltimore, MD, United States). Fertility and Sterility 2015; Vol. 104, issue 3:e181.
Additional references
ASA 2015
- American Society of Anesthesiologists (ASA). Continuum of Depth of Sedation: Definition of General Anesthesia and Levels of Sedation/Analgesia. 2015. [ebook]. http://www.asahq.org/quality‐and‐practice‐management/standards‐and‐guidelines (accessed 13 June 2017).
Bokhari 1999
- Bokhari A, Pollard BJ. Anaesthesia for assisted conception: a survey of UK practice. European Journal of Anaesthesiology 1999;16:225‐30. [DOI] [PubMed] [Google Scholar]
Chumbley 1998
- Chumbley GM, Hall GM, Salmon P. Patient‐controlled analgesia: an assessment by 200 patients. Anaesthesia 1998;53(3):216‐21. [DOI] [PubMed] [Google Scholar]
Ditkoff 1997
- Ditkoff EC, Plumb J, Selick A, Sauer MV. Anesthesia practices in the United States common to in vitro fertilisation (IVF) centers. Journal of Assisted Reproduction and Genetics 1997;14(3):145‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elkington 2003
- Elkington NM, Kehoe J, Acharya U. Intravenous sedation in assisted conception unit: a UK survey. Human Fertility 2003;6:74‐6. [DOI] [PubMed] [Google Scholar]
Han 2011
- Han J. Acupuncture analgesia: areas of consensus and controversy. Pain 2011;152 (Suppl):S41‐S48. [DOI] [PubMed] [Google Scholar]
Hawkins 1993
- Hawkins R, Price K. The effects of an education video on patients' requests for postoperative pain relief. Australian Journal of Advanced Nursing 1993;10(4):32‐40. [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editors. Cochrane Handbook of Systematic Reviews of Interventions. Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane–handbook.org. [Google Scholar]
Rjosk 1993
- Rjosk HK, Haeske‐Seeberg H, Seeberg B, Kreuzer E. IVF and GIFT‐ Ergebnisse in Deuchland 1993. Fertilitaet 1995;11:48‐54. [Google Scholar]
Sharma 2015
- Sharma A, Borle A, Trikha A. Anesthesia for in vitro fertilisation. Journal of Obstetric Anaesthesia and Critical Care 2015;5(2):62‐72. [Google Scholar]
Skelly 1996
- Skelly AM. Analgesia and sedation. In: Watkinson A, Adams A editor(s). Interventional Radiology. Oxford: Radcliffe Medical Press, 1996:3‐11. [Google Scholar]
Stener‐Victorin 2005
- Stener‐Victorin E. The pain‐relieving effect of electro‐acupuncture and conventional medical analgesic methods during oocyte retrieval: a systematic review of randomized controlled trials. Human Reproduction 2005;20(2):339‐49. [DOI] [PubMed] [Google Scholar]
White 1987
- White DC. Anaesthesia: a privation of the senses. An historical introduction and some definitions. In: Rosen M, Lunn JN, editor(s). Conscious Awareness and Pain in General Anaesthesia. London: Butterworth & Co., 1987:1‐9. [Google Scholar]
Zhao 2008
- Zhao, Z. Neural mechanism underlying acupuncture analgesia. Progress in Neurobiology 2008;85(4):355‐75. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Kwan 2004
- Kwan I, Bhattacharya S, Knox F, McNeil A. Conscious sedation for oocyte retrieval during in vitro fertilisation procedures. Cochrane Database of Systematic Reviews 2004, Issue 3. [DOI: 10.1002/14651858.CD004829] [DOI] [PubMed] [Google Scholar]
Kwan 2005
- Kwan I, Bhattacharya S, Knox F, McNeil A. Conscious sedation and analgesia for oocyte retrieval during in vitro fertilisation procedures. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD004829.pub2] [DOI] [PubMed] [Google Scholar]
Kwan 2013
- Kwan I, Bhattacharya S, Knox F, McNeil A. Pain relief for women undergoing oocyte retrieval for assisted reproduction. Cochrane Database of Systematic Reviews 2013, Issue 1. [DOI: 10.1002/14651858.CD004829.pub3] [DOI] [PubMed] [Google Scholar]


