Abstract
Background
The prevalence of musculoskeletal symptoms among sedentary workers is high. Interventions that promote occupational standing or walking have been found to reduce occupational sedentary time, but it is unclear whether these interventions ameliorate musculoskeletal symptoms in sedentary workers.
Objectives
To investigate the effectiveness of workplace interventions to increase standing or walking for decreasing musculoskeletal symptoms in sedentary workers.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, Embase, OSH UPDATE, PEDro, ClinicalTrials.gov, and the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) search portal up to January 2019. We also screened reference lists of primary studies and contacted experts to identify additional studies.
Selection criteria
We included randomised controlled trials (RCTs), cluster‐randomised controlled trials (cluster‐RCTs), quasi RCTs, and controlled before‐and‐after (CBA) studies of interventions to reduce or break up workplace sitting by encouraging standing or walking in the workplace among workers with musculoskeletal symptoms. The primary outcome was self‐reported intensity or presence of musculoskeletal symptoms by body region and the impact of musculoskeletal symptoms such as pain‐related disability. We considered work performance and productivity, sickness absenteeism, and adverse events such as venous disorders or perinatal complications as secondary outcomes.
Data collection and analysis
Two review authors independently screened titles, abstracts, and full‐text articles for study eligibility. These review authors independently extracted data and assessed risk of bias. We contacted study authors to request additional data when required. We used GRADE considerations to assess the quality of evidence provided by studies that contributed to the meta‐analyses.
Main results
We found ten studies including three RCTs, five cluster RCTs, and two CBA studies with a total of 955 participants, all from high‐income countries. Interventions targeted changes to the physical work environment such as provision of sit‐stand or treadmill workstations (four studies), an activity tracker (two studies) for use in individual approaches, and multi‐component interventions (five studies). We did not find any studies that specifically targeted only the organisational level components. Two studies assessed pain‐related disability.
Physical work environment
There was no significant difference in the intensity of low back symptoms (standardised mean difference (SMD) ‐0.35, 95% confidence interval (CI) ‐0.80 to 0.10; 2 RCTs; low‐quality evidence) nor in the intensity of upper back symptoms (SMD ‐0.48, 95% CI ‐.96 to 0.00; 2 RCTs; low‐quality evidence) in the short term (less than six months) for interventions using sit‐stand workstations compared to no intervention. No studies examined discomfort outcomes at medium (six to less than 12 months) or long term (12 months and more). No significant reduction in pain‐related disability was noted when a sit‐stand workstation was used compared to when no intervention was provided in the medium term (mean difference (MD) ‐0.4, 95% CI ‐2.70 to 1.90; 1 RCT; low‐quality evidence).
Individual approach
There was no significant difference in the intensity or presence of low back symptoms (SMD ‐0.05, 95% CI ‐0.87 to 0.77; 2 RCTs; low‐quality evidence), upper back symptoms (SMD ‐0.04, 95% CI ‐0.92 to 0.84; 2 RCTs; low‐quality evidence), neck symptoms (SMD ‐0.05, 95% CI ‐0.68 to 0.78; 2 RCTs; low‐quality evidence), shoulder symptoms (SMD ‐0.14, 95% CI ‐0.63 to 0.90; 2 RCTs; low‐quality evidence), or elbow/wrist and hand symptoms (SMD ‐0.30, 95% CI ‐0.63 to 0.90; 2 RCTs; low‐quality evidence) for interventions involving an activity tracker compared to an alternative intervention or no intervention in the short term. No studies provided outcomes at medium term, and only one study examined outcomes at long term.
Organisational level
No studies evaluated the effects of interventions solely targeted at the organisational level.
Multi‐component approach
There was no significant difference in the proportion of participants reporting low back symptoms (risk ratio (RR) 0.93, 95% CI 0.69 to 1.27; 3 RCTs; low‐quality evidence), neck symptoms (RR 1.00, 95% CI 0.76 to 1.32; 3 RCTs; low‐quality evidence), shoulder symptoms (RR 0.83, 95% CI 0.12 to 5.80; 2 RCTs; very low‐quality evidence), and upper back symptoms (RR 0.88, 95% CI 0.76 to 1.32; 3 RCTs; low‐quality evidence) for interventions using a multi‐component approach compared to no intervention in the short term. Only one RCT examined outcomes at medium term and found no significant difference in low back symptoms (MD ‐0.40, 95% CI ‐1.95 to 1.15; 1 RCT; low‐quality evidence), upper back symptoms (MD ‐0.70, 95% CI ‐2.12 to 0.72; low‐quality evidence), and leg symptoms (MD ‐0.80, 95% CI ‐2.49 to 0.89; low‐quality evidence). There was no significant difference in the proportion of participants reporting low back symptoms (RR 0.89, 95% CI 0.57 to 1.40; 2 RCTs; low‐quality evidence), neck symptoms (RR 0.67, 95% CI 0.41 to 1.08; two RCTs; low‐quality evidence), and upper back symptoms (RR 0.52, 95% CI 0.08 to 3.29; 2 RCTs; low‐quality evidence) for interventions using a multi‐component approach compared to no intervention in the long term. There was a statistically significant reduction in pain‐related disability following a multi‐component intervention compared to no intervention in the medium term (MD ‐8.80, 95% CI ‐17.46 to ‐0.14; 1 RCT; low‐quality evidence).
Authors' conclusions
Currently available limited evidence does not show that interventions to increase standing or walking in the workplace reduced musculoskeletal symptoms among sedentary workers at short‐, medium‐, or long‐term follow up. The quality of evidence is low or very low, largely due to study design and small sample sizes. Although the results of this review are not statistically significant, some interventions targeting the physical work environment are suggestive of an intervention effect. Therefore, in the future, larger cluster‐RCTs recruiting participants with baseline musculoskeletal symptoms and long‐term outcomes are needed to determine whether interventions to increase standing or walking can reduce musculoskeletal symptoms among sedentary workers and can be sustained over time.
Plain language summary
Workplace interventions for increasing standing or walking for decreasing musculoskeletal symptoms in sedentary workers
Why is it important to increase standing or walking at work?
The number of people working in sedentary jobs has increased in recent decades. Many of these people complain of musculoskeletal symptoms. Walking or standing interventions at work have been effective in reducing sitting time at work. However, it is still unclear if these interventions are effective in reducing the intensity or presence of musculoskeletal symptoms among office workers.
The purpose of this review We wanted to find out the effects of interventions aimed at increasing standing or walking for decreasing musculoskeletal symptoms in sedentary workers. We searched the literature in various databases up to January 2019.
What trials did review authors find? We found 10 studies conducted with a total of 955 employees with musculoskeletal complaints from high‐income countries. Four studies evaluated changes to the physical work environment through provision of sit‐stand or treadmill workstations, two studies evaluated individual approaches involving use of an activity tracker, and five studies used multi‐component interventions and counselling interventions. However, no studies solely targeted interventions at the organisation level.
Effects of changes to the physical work environment
The available evidence is insufficient to show the effectiveness of sit‐stand desk or treadmill workstations in reducing the intensity of low back and upper back symptoms.
Effects of interventions targeted at the individual
The effectiveness of an activity tracker compared to an alternative intervention or no intervention in reducing the intensity or presence of low back, upper back, neck, shoulder, and elbow/wrist and hand symptoms cannot be determined based on available evidence at short‐term follow‐up (less than six months).
Effects of interventions targeted at the organisation
No available studies have examined the effectiveness of interventions targeted solely at the organisational level.
Effects of combining multiple interventions
Available evidence is insufficient to show the effectiveness of combining multiple interventions in reducing the proportions of people with low back or upper back pain at short‐term follow‐up (less than six months), medium‐term follow‐up (between six and 12 months), or long‐term follow‐up (12 months or longer).
Conclusions
The review did not find conclusively that interventions to increase standing or walking are effective in reducing the intensity or presence of musculoskeletal symptoms among sedentary workers in the short, medium, or long term. This may be due in part to the quality of the evidence, which is low or very low largely due to study design and small sample sizes. Some interventions that targeted changes to the work environment such as the use of sit‐stand desks are suggestive of an improvement in musculoskeletal symptoms. Therefore, additional studies of larger scale and longer duration that recruit people with baseline musculoskeletal symptoms are needed to determine whether interventions to increase standing or walking can reduce musculoskeletal symptoms among sedentary workers, and whether these changes can be maintained.
Summary of findings
Background
Description of the condition
Musculoskeletal symptoms (such as pain and discomfort in various body areas including back, neck, and lower and upper extremities) are a common problem, with approximately 40% of the general population reporting pain annually (Hoy 2012), and with transient pain at high risk for eventually leading to chronic symptoms (Kovacs 2005). Musculoskeletal symptoms are among the most prevalent occupational problems (Andersen 2007; Janwantanakul 2008), placing a large burden on the working population. Among the top ten causes of years lived with disability, low back pain and neck pain are ranked first and fourth, respectively (GBDSC 2015); they also impact medical costs, work productivity, work disability, and absenteeism (Bevan 2015; Buchbinder 2013; CDC 2013; Lambeek 2011).
In particular among sedentary workers, the prevalence of musculoskeletal symptoms is high (Cho 2012), and these symptoms are reported in more than 90% of office workers (Widanarko 2011). Occupational sedentary behaviour has been associated with musculoskeletal symptoms including pain in the low back and in the lower extremities (Al‐Eisa 2006; Messing 2008; Reid 2010). Spinal loading associated with sustained sitting (Pope 2002), increased activation of spinal muscles in specific sitting postures (Curran 2015; Waongenngarm 2015), and lack of variation in movement is among suggested mechanisms explaining the occurrence of musculoskeletal symptoms during sitting (Srinivasan 2012). Moreover, prolonged keyboard and mouse use, high mental workload, and stress are hypothesised to contribute to the occurrence of musculoskeletal symptoms among sedentary office workers (Chiu 2002; Cho 2012; Coenen 2019; Hannan 2005; Hush 2009; Huysmans 2012; Jensen 2003; Kiss 2012). Despite this, evidence of an association between sedentary behaviour and the occurrence of musculoskeletal symptoms remains inconsistent (Bakker 2009; Chen 2009; da Costa 2010; Lin 2011; Waersted 2010).
Innovations in technology have resulted in a shift of the workforce into more sedentary roles (Borodulin 2007; Brownson 2005; Juneau 2010), causing a substantial increase in sedentary occupations in developed countries over past decades (Church 2011; Kohl 2012). Recent studies of accelerometer determined sedentary time estimate that office workers spend 77% to 82% of their working time being sedentary (Parry 2013; Thorp 2012). This large amount of sedentary time at work combined with its musculoskeletal (and other) health risks underlines the importance of gaining a better understanding of the development of musculoskeletal symptoms in sedentary workers.
Description of the intervention
As sedentary workers can spend most working hours in sedentary activities (Parry 2013; Thorp 2012), the workplace is a convenient and practical venue for targeting interventions to modify these behaviours. Growing evidence suggests that these interventions might reduce or break up sedentary behaviour (Commissaris 2016; Shrestha 2018), thereby reducing cardiometabolic risk factors (Peddie 2013; Thorp 2014a). However, the impact of these interventions on reducing musculoskeletal symptoms is not well understood. Workplace interventions that will be examined in this review are interventions that specifically aim to reduce or break up sedentary behaviour by increasing standing or walking, which may fall into the following categories.
Interventions targeted at the physical work environment – including provision of an activity permissive workstation such as a treadmill or a sit‐stand workstation, or changes to the built environment.
Interventions targeted at the individual – including tailored walking programmes during work breaks or ‘incidental’ walking programmes, promoting the use of stairs during work hours, providing break‐reminding software, and providing individual counselling programmes.
Interventions targeted at the organisation – such as workplace policy modifications to encourage workplace activity, for example, standing meetings and ‘active/walking’ emails.
Workplace interventions may also be multi‐component, whereby a combination of intervention approaches is employed.
How the intervention might work
Alternatives to sitting, such as standing and walking, may result in improvement in musculoskeletal symptoms (intensity or presence of symptoms or pain‐related disability) by reducing or breaking up prolonged sitting, thereby modifying the sustained spinal load that occurs in prolonged sitting. Breaking up periods of prolonged sitting by standing or walking can increase muscle activity and can create movement and postural variation, reducing the risk of static muscle overload and increasing blood circulation (Srinivasan 2012; Tikkanen 2013). Interventions that promote the graded introduction of standing and walking may therefore improve the general musculoskeletal health of workers. This is supported by findings from recent systematic reviews of laboratory studies showing that interventions targeted at breaking up sitting, in particular those involving sit‐stand workstations, were effective in reducing musculoskeletal discomfort (Healy 2012; Karakolis 2014; Thorp 2014b).
However, alternatives to sitting (e.g. standing, walking) have also been associated with musculoskeletal symptoms. Occupational standing has been linked with musculoskeletal symptoms, including pain in the low back (Andersen 2007; Coenen 2017; Tissot 2009), as well as in the lower extremities (Messing 2008; Reid 2010). Associations between musculoskeletal pain and non‐neutral (e.g. sway, lordotic) lumbar postures during standing have been reported (O'Sullivan 2011), with the proposed mechanism of altered patterns of loading on the spine (Smith 2017; van Deursen 2005). Other study authors have reported increased patterns of trunk muscle activity linked to musculoskeletal symptoms in sustained standing (Gregory 2008; Nelson‐Wong 2010). Potential mechanisms include muscle fatigue (Balasubramanian 2009), along with swelling of the lower limbs due to blood pooling (Chester 2002). However, evidence conclusively supporting the above hypotheses is lacking. Associations between occupational walking and the occurrence of musculoskeletal symptoms (including leg pain) have been reported (Engels 1996), but evidence is inconclusive (Roffey 2010). However, recent evidence about thresholds for prolonged standing suggest that standing in excess of 40 minutes could be associated with adverse musculoskeletal effects (Coenen 2017).
Therefore, although reduced occupational sitting may result in improvement of some musculoskeletal symptoms, replacing it with standing or walking may cause alternate problems. For example, in a study among bank tellers who just sat, just stood, or alternated sitting and standing every 30 minutes, it was shown that workers had greater discomfort in the upper limbs while sitting, and greater discomfort in the lower limbs while standing (Roelofs 2002). This is highlighted in a review examining the effects of activity permissive workstations among office workers (i.e. sit‐stand workstations, but also under‐desk cycling and treadmill workstations), which reported both beneficial and detrimental effects on musculoskeletal outcomes (Neuhaus 2014b).
Given that there may be individual vulnerability to musculoskeletal discomfort in standing and sitting, the response to standing or walking interventions is likely to vary between workers (Gregory 2008). Personal factors, such as gender (Hooftman 2004), age (Viester 2013), and adiposity (Hooftman 2004; Moreira‐Silva 2013; Oha 2014), are known to play a role in the occurrence and recurrence of musculoskeletal symptoms among workers. Such factors may impact the effectiveness of these interventions.
Why it is important to do this review
Musculoskeletal disorders contribute significantly to the global burden of disease (GBDSC 2015), and they are associated with substantial economic and productivity costs within work settings (Bevan 2015; Buchbinder 2013). Sedentary workers report a high prevalence of musculoskeletal symptoms (Cho 2012; Harcombe 2009; Janwantanakul 2008), and they may be at increased risk of adverse cardiometabolic, cancer, and even mental health outcomes (Carson 2014; Chau 2014; Dunstan 2012; Parry 2013; Straker 2014; Vallance 2011). Because of these risks, there has been a rapid increase in workplace interventions provided to reduce sedentary behaviour, such as the introduction of activity permissive workstations. However, it is not clear whether such workplace changes aimed at reducing sedentary behaviour will have any impact on musculoskeletal symptoms.
Previous reviews have focused on workplace interventions to increase physical activity (Freak‐Poli 2013), or to reduce sitting (Shrestha 2018), but these reviews have not specifically explored the potential impact of changing workplace activity on musculoskeletal symptoms. Therefore, in relation to interventions that aim to reduce workplace sedentary behaviour by increasing standing or walking, it is important to examine not only changes to sedentary behaviour and cardiometabolic health outcomes, as considered in previous reviews, but also musculoskeletal health. The findings of this review will provide evidence to assist in the management of work‐related musculoskeletal symptoms.
This is a partner to another review on similar workplace interventions for preventing, rather than decreasing, musculoskeletal symptoms in sedentary workers (Parry 2017a).
Objectives
To investigate the effectiveness of workplace interventions to increase standing or walking for decreasing musculoskeletal symptoms in sedentary workers.
Methods
Criteria for considering studies for this review
Types of studies
We have included all eligible randomised controlled trials (RCTs), quasi‐RCTs (in which methods of allocating participants are not random, such as alternate allocation or allocation by date of birth or day of the week), and cluster‐RCTs (randomisation of a group of people such as a work group or workplace rather than randomisation of individual people). For some workplace interventions, the implementation of interventions is difficult to apply to an individual, so interventions operate on a group level (Ijaz 2014). In this situation, when the intervention takes place at a group level or within the one organisation where due to workplace or environmental restrictions, randomisation is not possible, we have also included controlled before‐and‐after studies (CBAs), which use a concurrent control group for the intervention. We have included studies reported as full text, those published as abstract only, and unpublished data.
Types of participants
We have included studies conducted with adult workers aged 18 or older, working in sedentary occupations (workers sedentary for more than 50% of the working day), such as seated office workers and laboratory technicians. We have excluded sedentary workers for whom it may not be possible to modify workplace posture, such as transport workers. Studies that did not report the proportion of sedentary time but described workers as ‘sedentary workers’ have been included. When studies included workers from different occupations, we included only results from participants identified as ‘sedentary workers’, or we reported sedentary time of more than 50%. We excluded studies that specifically focused on participants with the following comorbidities or characteristics.
Inflammatory systematic diseases such as rheumatoid arthritis.
Diseases of the central nervous system such as stroke and multiple sclerosis.
Sedentary workers who report the presence of musculoskeletal symptoms in at least one of the following regions ‐ cervical spine, mid‐back, lower back, upper limb, hip, or lower limb ‐ have been included as participants with symptoms.
In studies that include a mixture of participants reporting and not reporting musculoskeletal symptoms, only participants with symptoms at baseline have been included in the analyses.
We have included studies conducted with participants who report pain. ‘Participants with pain’ thresholds are defined as:
‘yes’ on a dichotomous symptom scale;
‘greater than 0’ on a visual analogue symptoms scale out of 10;
‘greater than 0’ on a numerical rating scale out of 10;
‘greater than 0’ on the McGill Pain Questionnaire;
‘greater than 0’ on the 18‐, 23‐, or 24‐point version of the Roland Morris Disability Questionnaire; or
‘greater than 0%' for overall score on the Oswestry Disability Index.
Types of interventions
We included trials that evaluated the effectiveness of interventions to reduce or break up workplace sitting by encouraging standing or walking at the workplace. Eligible interventions include the following.
-
Interventions targeted at the physical work environment.
Provision of an activity permissive workstation (sit/stand or treadmill).
Interventions that modify the built environment such as modifications to office layout that encourage standing or walking.
-
Interventions targeted at the individual.
Behavioural modification or counselling programmes that promote increased standing or walking.
Working style interventions that promote standing or walking, such as promotion of 'active' work breaks.
Workplace walking programmes including ‘pedometer challenges’.
Promoting the use of stairs during work hours.
Using break‐reminding software.
-
Interventions targeted at the organisation.
Workplace policy modifications such as standing meetings and ‘active/walking’ emails.
We included multi‐component trials that combine elements of the above interventions.
We included trials that compare the effectiveness of workplace interventions to increase standing or walking with usual care, with no intervention, or with another active intervention such as specific targeted musculoskeletal interventions.
We excluded interventions that focus on specific strengthening or stretching programmes that do not promote standing or walking. For example, an exercise programme that replaces sedentary time (with standing or walking) would be included as an intervention, whereas a seated exercise programme (seated stretching/strengthening programme) would not be included.
Types of outcome measures
Primary outcomes
We included trials that evaluated the effectiveness of interventions for self‐reported musculoskeletal symptoms by body region.
-
Musculoskeletal symptoms may be reported as pain on a scale (as listed below) or may be reported as 'discomfort' or 'trouble' on similar scales.
Presence of musculoskeletal symptoms may be reported on a dichotomous scale (yes/no) by outcome measures such as the Nordic Musculoskeletal Questionnaire (Kuorinka 1987).
Intensity of musculoskeletal symptoms may be reported on a visual analogue scale (or similar), a numerical rating scale, a Likert scale (Bond 1966; Harland 2015), or a McGill Pain Questionnaire (Melzack 1975).
Impact of pain such as pain‐related disability.
Disability may be assessed by outcome measures such as the Oswestry Disability Index, the Roland Morris Disability Questionnaire (Roland 2000), or the Neck Disability Index (Vernon 2008).
Secondary outcomes
The following secondary outcomes were reported.
-
Work performance and productivity.
Level of work function, change in work productivity, work time loss assessed by outcome measures such as the Work Ability Index (de Zwart 2002; van den Berg 2008).
Sickness absenteeism.
Adverse events such as venous disorders or perinatal complications.
Reporting one or more of the secondary outcomes listed here was not an inclusion criterion for this review. In addition, secondary outcomes were used only to support the conclusions of the primary outcomes and not to draw conclusions on the effectiveness of the interventions.
The primary measurement time points have been short term (less than six months). We have categorised additional follow‐up times as medium term (six months to less than 12 months) and long term (12 months or longer).
Search methods for identification of studies
Electronic searches
We conducted a systematic literature search to identify all published and unpublished trials that can be considered eligible for inclusion in this review. The literature search identified studies in all languages. We arranged for the translation of key sections of potentially eligible non‐English language papers, or we arranged that people who are proficient in the language of the publications fully assess them for potential inclusion in the review as necessary.
We searched the following electronic databases from inception to January 2019.
The Cochrane Central Register of Controlled Trials (CENTRAL), in the Wiley Online Library.
MEDLINE (PubMed).
Embase (embase.com).
National Institute for Occupational Safety and Health's (NIOSH) electronic, bibliographic database of literature in the field of occupational safety and health (NIOSHTIC) (Occupational Safety and Health (OSH)‐UPDATE).
NIOSHTIC‐2 (OSH‐UPDATE).
UK Health and Safety Executive Information Services (HSELINE) (OSH‐UPDATE).
Archived OSH Bibliographic Datbase (CISDOC) (OSH‐UPDATE).
Physiotherapy Evidence Database (PEDro).
We also conducted a search of unpublished trials at ClinicalTrials.gov (www.ClinicalTrials.gov) and at the World Health Organization (WHO) trials portal (www.who.int/ictrp/en/). We imposed no restrictions on language of publication.
Searching other resources
We checked the reference lists of all primary studies and review articles for additional references. We contacted experts in the field to identify additional unpublished materials.
Data collection and analysis
Selection of studies
We conducted the selection of eligible studies in two stages. First, two review authors (SP and PC) independently screened titles and abstracts of all potentially relevant studies identified through our systematic search to identify studies for inclusion. The same review authors coded them as 'include' (eligible or potentially eligible/unclear) or 'exclude'. At this stage, we excluded all references that clearly do not fulfil our inclusion criteria or that do fulfil our exclusion criteria. At the second stage, we retrieved the full‐text study reports/publications, and two review authors (SP and PC) independently assessed the full text and identified studies for inclusion. At this stage, we included all references that do fulfil our inclusion criteria. We recorded reasons for exclusion of ineligible studies assessed as full texts, so that we could report these in a Characteristics of excluded studies table. We resolved any disagreement through discussion, or, if required, we consulted a third review author (NS). We identified and excluded duplicates and collated multiple reports of the same study, so that each study rather than each report is the unit of interest in the review. We recorded the selection process in sufficient detail to complete a PRISMA study flow diagram.
When our systematic searches identified studies conducted by authors of this review, we avoided conflicts of interest by having all decisions concerning inclusion and exclusion made by review authors who were not involved with the study.
Data extraction and management
We used a data collection form for study characteristics and outcome data that had been piloted on at least one study in the review. Two review authors (SP and PC) extracted the following study characteristics from included studies.
Study authors and year of publication.
Methods: study design, total duration of study, study location, study setting, withdrawals, date of study.
Participants: N, mean age or age range, sex/gender, severity of condition, intensity of sedentary work (percentage of workday sedentary), type of sedentary work, diagnostic criteria if applicable, inclusion criteria, exclusion criteria.
Interventions: description of intervention, comparison, duration, intensity, content of both intervention and control conditions, co‐interventions.
Outcomes: description of primary and secondary outcomes specified and collected, time points reported.
Notes: funding for trial, notable conflicts of interest of trial authors.
Two review authors (SP and PC) independently extracted outcome data from included studies. We noted in the Characteristics of included studies table if outcome data were not reported in a usable way. We resolved disagreements by consensus or by involving a third review author (NS). One review author (NS) transferred data into the Review Manager file (RevMan 2014). We double‐checked that data were entered correctly by comparing the data presented in the systematic review with the study reports. A second review author (PC) spot‐checked study characteristics for accuracy against the trial report. When included studies published in one or more languages in which our author team is not proficient, we arranged for a native speaker or someone sufficiently qualified in each foreign language to fill in a data extraction form for us.
Assessment of risk of bias in included studies
Two review authors (SP and PC) independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved any disagreements by discussion or by consultation with another review author (NS). We assessed risk of bias according to the following domains.
Random sequence generation.
Allocation concealment.
Blinding of participants and personnel.
Blinding of outcome assessment.
Incomplete outcome data.
Selective outcome reporting.
Other bias such as baseline imbalance.
In addition, if cluster‐randomised trials were identified and included in the review, we considered the following additional biases.
Recruitment bias.
Baseline imbalance.
Loss of clusters.
Incorrect analysis.
Comparability with individually randomised trials.
We graded each potential 'Risk of bias' item as high, low, or unclear, and we provided a quote from the study report together with a justification for our judgement in the 'Risk of bias' table. We summarised 'Risk of bias' judgements across different studies for each of the domains listed. We considered blinding separately for different key outcomes when necessary (e.g. for unblinded outcome assessment, risk of bias for work productivity may be very different than for a patient‐reported pain scale). When information on risk of bias related to unpublished data or correspondence with a trialist, we noted this in the 'Risk of bias' table.
We consider allocation concealment, blinding of participants and outcome assessors, and incomplete outcome data to be key domains. We judged a study to have high risk of bias when one or more key domains had high risk of bias. Conversely, we judged a study to have low risk of bias when we judged that most of the key domains had low risk of bias.
For CBA studies, we used the instrument for appraising risk of bias of CBA studies validated by Downs (Downs 1998). The instrument has been shown to have good reliability and internal consistency and validity. The list consists of five different subscales: reporting, external validity, bias, confounding, and power. We used the combined score on the two internal validity subscales (bias and confounding) to judge risk of bias only for the included CBA studies. We used an arbitrary cut‐off score of 50% of the maximum attainable score of the internal validity scale to discern low from high risk of bias. We modified the criteria for risk of bias so that they fit the 'Risk of bias' tool as implemented in RevMan by changing them from 0 and 1 to high, low, and unclear (RevMan 2014).
We also checked for relevant and considerable baseline differences between control and intervention groups based on age and gender.
When considering treatment effects, we took into account the risk of bias for studies that contributed to that outcome.
Assessment of bias in conducting the systematic review
We conducted the review according to the published protocol and reported any deviations from it in the Differences between protocol and review section of the systematic review.
Measures of treatment effect
We entered the outcome data for each study into the data tables in RevMan to calculate treatment effects (RevMan 2014). We used odds ratio/risk ratio for dichotomous outcomes, and mean differences or standardised mean differences for continuous outcomes, or another type of data as reported by study authors. For outcomes reported as dichotomous data in some studies and as continuous data in other studies, we re‐expressed the odds ratio as the standardised mean difference. This method assumes logistic distribution and comparable variability for both intervention and control groups according to the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). If only effect estimates and their 95% confidence intervals or standard errors were reported in studies, we entered these data into RevMan using the generic inverse variance method. We ensured that higher scores for continuous outcomes have the same meaning for the particular outcome, explained the direction to the reader, and reported where the directions were reversed if this was necessary. When results could not be entered either way, we described them in the Characteristics of included studies table, or we entered the data into additional tables.
Unit of analysis issues
For studies that employ a cluster‐randomised design and that report sufficient data for inclusion in the meta‐analysis but do not make an allowance for the design effect, we calculated the design effect based on a fairly large assumed intracluster correlation of 0.10. We based this assumption of 0.10 being a realistic estimate by analogy on studies about implementation research (Campbell 2001). We followed the methods provided in the Cochrane Handbook for Systematic Reviews of Interventions when performing the calculations (Higgins 2011).
Dealing with missing data
We contacted investigators or study sponsors to verify key study characteristics and to obtain missing data when possible (e.g. when a study is identified as abstract only). When this was not possible, and missing data were thought to introduce serious bias, we explored the impact of including such studies in the overall assessment of results by performing a sensitivity analysis.
If data such as standard deviations or correlation coefficients were missing and they could not be obtained from the study authors, we calculated them from other available statistics such as P values according to the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Assessment of heterogeneity
We assessed the clinical homogeneity of the results of included studies based on similarity of population, intervention, outcome, and follow‐up. We considered populations as similar when sedentary work is being conducted for more than 50% of working hours, or when participants are described as 'sedentary workers'. Populations that report musculoskeletal symptoms in one or more body region, of any intensity, were considered as similar. We considered interventions as similar when they target workplace sedentary behaviour by promoting standing or walking according to the category of the intervention as defined under Types of interventions. We did not consider interventions that implement exercise or educational programmes to target specific muscle groups such as neck/shoulder or low back exercise as similar to sedentary behaviour modification programmes (as stated under Types of interventions). We considered all outcome measures of pain or discomfort including dichotomous measures, Likert scale, visual analogue scale, and standardised questionnaires such as the Nordic Musculoskeletal Questionnaire as similar. For measurement of work performance, pain‐related disability, and work productivity, we considered all self‐reported outcomes from standardised questionnaires (e.g. Work Performance Index, Neck Disability Index) as similar. We regarded follow‐up times of up to six months as short term, from six months to less than 12 months as medium term, and from 12 months onward as long‐term outcomes, and we treated these outcomes as different.
Assessment of reporting biases
We were not able to pool more than five trials in any single meta‐analysis; therefore we did not explore possible small‐study biases using a funnel plot.
Data synthesis
We pooled data from studies judged to be clinically homogeneous using Review Manager 5.3 software (RevMan 2014). If more than one study provided usable data in any single comparison, we performed a meta‐analysis. We calculated the standardised mean difference when data for the same outcome were presented in some studies as dichotomous data and in other studies as continuous data (Section 9.4.6, Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011)), or when studies measured the same outcome on different scales. We used a random‐effects model when I² was above 40%; otherwise we used a fixed‐effect model. When I² was higher than 75%, we did not pool study results in a meta‐analysis.
We narratively described skewed data reported as medians and interquartile ranges.
When multiple trial arms were reported in a single trial, we included only the relevant arms. When two comparisons (e.g. provision of sit‐stand desk vs standard desk and behavioural modification vs standard desk) were combined in the same meta‐analysis, we halved the control group to avoid double‐counting.
We considered minimally important differences for validated outcome measures when we discussed the magnitude of the effect size. We considered pooled effect sizes greater than the minimally important difference to be clinical significant.
'Summary of findings' table
We reported the presence or intensity of musculoskeletal symptoms for the following regions ‐ low back, upper back, neck, and shoulder ‐ and disability at short‐term follow‐up in the 'Summary of findings' table.
We used the five GRADE considerations (study limitations, consistency of effect, imprecision, indirectness, and publication bias) to assess the quality of a body of evidence as it relates to studies that contributed data to the meta‐analyses for pre‐specified outcomes. We used methods and recommendations as described in Section 8.5 and Chapter 12 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), using GRADEpro software. We justified all decisions to downgrade or upgrade the quality of evidence by using footnotes.
Subgroup analysis and investigation of heterogeneity
We planned to carry out the following subgroup analyses.
Intervention approach (workstation design, workplace built environment, workplace policy, interventions in non‐productive periods (work breaks)).
Intervention effects on different body regions (cervical spine, mid‐back, lower back, upper limb/shoulder, lower limb).
Participant characteristics (age, gender, body mass index).
Participant work group characteristics (specific occupations).
We planned to use the following outcomes in subgroup analyses.
Musculoskeletal symptoms (pain/discomfort).
Pain‐related disability.
As studies were insufficient, we were not able to conduct planned subgroup analyses.
Sensitivity analysis
We planned to perform sensitivity analyses to determine whether our findings are affected by high risk of bias and baseline pain of low intensity. To perform sensitivity analysis, we defined ‘high quality’ as studies with appropriate random allocation and concealment and attrition bias of less than 20%. We defined the low‐intensity pain threshold as 3 out of 10 on a pain intensity scale (Moore 2013). As studies were insufficient, we were not able to conduct the planned sensitivity analyses.
Reaching conclusions
We based our conclusions only on findings from the quantitative or narrative synthesis of included studies for this review. We avoided making recommendations for practice based on more than just the evidence, such as values and available resources. Our implications for research have suggested priorities for future research and have outlined remaining uncertainties in this area.
Results
Description of studies
See Figure 1, Characteristics of included studies, Characteristics of excluded studies, and Characteristics of ongoing studies.
1.
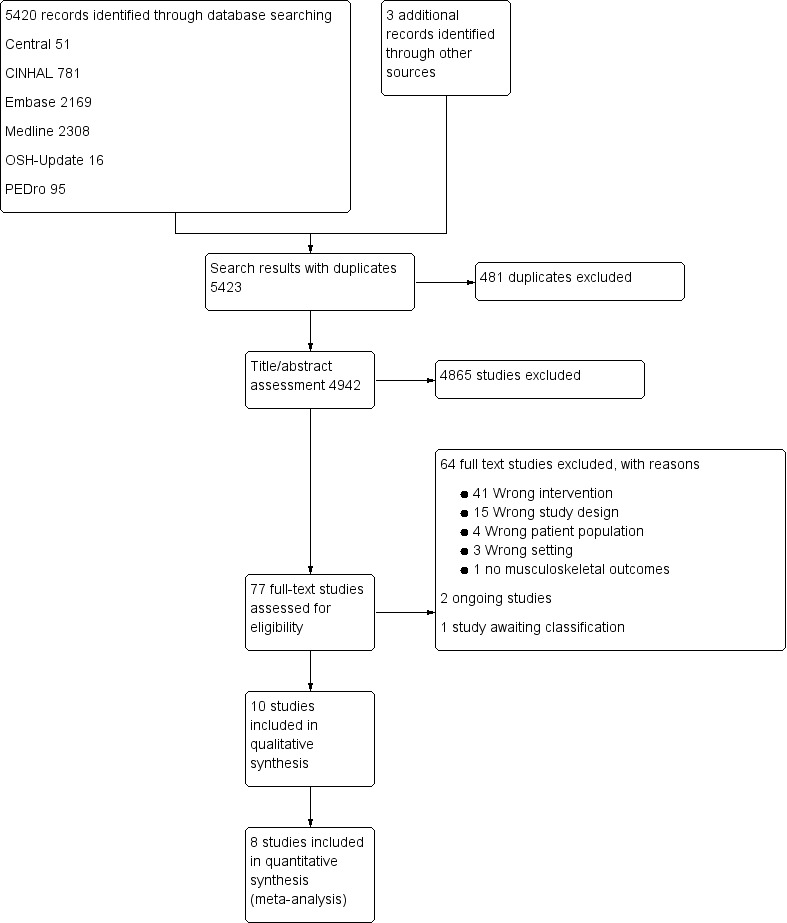
PRISMA study flow diagram.
Results of the search
We conducted systematic electronic database searches and handsearching of the literature. In total, we identified 5420 studies through electronic database searching and found four studies in other sources (January 2019): 51 from the Cochrane Central Register of Controlled Trials (CENTRAL; Appendix 1); 781 from the Cumulative Index to Nursing and Allied Health Literature (CINAHL; Appendix 2); 2169 from Embase (Appendix 3); 2308 from MEDLINE (Appendix 4); 16 from the Occupational Safety and Health (OSH) UPDATE (Appendix 5); 95 from the Physiotherapy Evidence Database (PEDro; Appendix 6); 2 from ClinicalTrials.gov (Appendix 7); and 0 from the World Health Organization (WHO) trials search portal (Appendix 8). We found three additional papers by reviewing the reference lists of the included papers and systematic reviews. After removal of duplicate studies, 4942 studies remained. After title and abstract screening, we retrieved 77 studies for full‐text screening. Of these studies, we excluded 64 studies (see Excluded studies), classified one study as awaiting classification (study authors could not be contacted), and found two ongoing studies that could not be included. Therefore, we included ten studies in this review.
Included studies
Study design
Eight studies that were included in the review were randomised controlled trials (RCTs). Of these, five were cluster‐RCTs (Brakenridge 2016; Danquah 2017; Edwardson 2018; Healy 2016; Parry 2015). For these studies, we used unadjusted data provided by the study authors. We adjusted their results for the design effect according to the calculation methods stated in Section 16.3 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). The two remaining studies that were included in this review were controlled before‐and‐after studies (CBAs) (Alkhajah 2012; Healy 2013). Although study authors described Alkhajah 2012 as a quasi‐RCT, we categorised this study as a CBA study because the risk of baseline differences for studies with only two clusters is very high. Details of each study can be found in the Characteristics of included studies section.
Participants
The total number of participants in the included studies was 955 employees, and sample sizes ranged from 15 in Alkhajah 2012 to 317 in Danquah 2017. However, not all of these participants had baseline musculoskeletal symptoms. With the exception of Gibbs 2018 and Ognibene 2016, which had an inclusion criterion of the presence of musculoskeletal symptoms, all other included studies provided outcomes only for those participants with baseline musculoskeletal symptoms when we contacted study authors. The number of participants with baseline musculoskeletal symptoms across the included studies ranged from one participant with baseline hip discomfort in Healy 2013 to 140 participants with baseline neck pain in Danquah 2017. Neck/shoulder and low back symptoms were most frequently reported in the included studies. Four studies predominantly included participants recruited from a university setting (Alkhajah 2012; Gibbs 2018; Graves 2015; Ognibene 2016), and the other six studies recruited participants from a combination of government and private organisations (Brakenridge 2016; Danquah 2017; Edwardson 2018; Healy 2013; Healy 2016; Parry 2015).
Gender
Eight of the included studies included participants who were predominantly female (66% to 94% female) (Alkhajah 2012; Danquah 2017; Edwardson 2018; Gibbs 2018; Healy 2013; Healy 2016; Ognibene 2016; Parry 2015). Female participation was 37% in Graves 2015) and 54% in Brakenridge 2016.
Country
The included studies were conducted in Australia, Denmark, Greenland, the United States of America, and the United Kingdom.
Interventions
Interventions targeted at the physical work environment
Four studies examined activity permissive workstations (treadmill workstation or sit‐stand workstation) to increase standing or walking and their effects on musculoskeletal symptoms (Alkhajah 2012; Graves 2015; Ognibene 2016; Parry 2015).
Sit‐stand workstation
Three studies examined the effectiveness of sit‐stand workstations (Alkhajah 2012; Graves 2015; Ognibene 2016). Graves 2015 incorporated personalised training and ergonomic information, whereas Alkhajah 2012 and Ognibene 2016 did not provide specific instructions or information on recommended time intervals or duration of use.
Treadmill workstation
One study assessed the effectiveness of a treadmill workstation in combination with promoting incidental office activity (Parry 2015). This study compared the effectiveness of (1) the treadmill workstation and promoting incidental office activity, (2) traditional physical activity promotion (pedometer challenge), and (3) ergonomic advice.
Interventions targeted at the individual
Two studies assessed the use of an activity tracker (Brakenridge 2016; Parry 2015). One study assessed the effectiveness of providing an activity tracker with organisational support for reducing musculoskeletal symptoms (Brakenridge 2016). The other study provided a pedometer to promote physical activity at work and during non‐work hours (Parry 2015).
Activity tracker
The effectiveness on an activity tracker was examined as part of a multi‐component trial that also provided organisational intervention strategies such as informational booklets, weekly emails, and workplace health promotion presentations. The activity tracker provided individual feedback with respect to standing, sitting, posture, and sleep (Brakenridge 2016). The other study provided a pedometer to monitor and promote workplace and non‐work daily steps as part of a 'pedometer challenge' (Parry 2015).
Interventions targeted at the organisation
No studies were found that specifically looked at modifying workplace policy to encourage workplace standing or walking.
Multi‐component interventions
Five studies incorporated multi‐component interventions (Danquah 2017; Edwardson 2018; Gibbs 2018; Healy 2013; Healy 2016). One study used a multi‐component approach to develop and tailor a programme to an organisation (Danquah 2017). Components of the intervention comprised both individual interventions and organisational interventions. Edwardson 2018 implemented "SMArt Work", a multi‐component intervention based on behavioural change theories, incorporating organisational strategies (management involvement), environmental strategies (provision of sit‐stand workstation with brief training), and individual and group strategies (educational seminar, feedback from baseline sit/stand/stepping measurements, provision of DARMA cushion that tracks sitting and prompts user to regularly break up sitting, provision of educational posters, individual coaching sessions). In Gibbs 2018, the multi‐component intervention incorporated personal behavioural counselling with follow‐up monthly phone calls, a sit‐stand desk attachment, and an activity prompter to reduce sedentary behaviour and enhance pain self‐management. Healy 2013 and Healy 2016 targeted the multi‐component interventions to "Stand Up, Sit Less, Move More". These interventions incorporated organisational strategies (workshops with managers, recruitment of team champions), environmental strategies (provision of sit‐stand workstations installed for 12 months), and individual strategies (individual coaching sessions for three months).
Control interventions
Waiting list control
Two studies had a waiting list control intervention (Graves 2015; Ognibene 2016). In both studies, participants in the control intervention maintained their normal duties and were then offered a sit‐stand workstation at the end of the intervention period.
No intervention
In six studies, the control group was not provided with any intervention and continued with usual work (Alkhajah 2012; Danquah 2017; Edwardson 2018; Gibbs 2018; Healy 2013; Healy 2016.) Gibbs 2018 provided no intervention to the control group but offered a 60‐minute educational session following the intervention period. Similarly, in Danquah 2017, the control group continued with the usual working practice. For this workplace, participants in the control group had previously been provided with a sit‐stand workstation. In two studies, participants were provided with feedback about physiological outcomes (Edwardson 2018; Healy 2016), and one study also provided feedback about physical activity at three months and 12 months (Healy 2016)
Written information
In Brakenridge 2016, written materials and emails developed from a multi‐component organisational intervention were provided as the control intervention. In another study, participants were provided with ergonomic advice in reviewing workstation set‐up (Parry 2015).
Outcomes
Musculoskeletal symptoms
Four studies assessed musculoskeletal symptom intensity on a numerical pain scale or a visual analog scale (0 to 10) (Brakenridge 2016; Gibbs 2018; Graves 2015; Ognibene 2016), and six studies used a dichotomous measure of the presence or absence of musculoskeletal symptoms (Alkhajah 2012; Danquah 2017; Edwardson 2018; Healy 2013; Healy 2016; Parry 2015). Two studies, upon assessing a sit‐stand workstation intervention, reported low back and upper back symptoms at short‐term follow‐up on different scales. Graves 2015 assessed intensity of pain using a Likert scale from 0 (no discomfort) to 10 (maximal discomfort); Ognibene 2016 used a modified pain inventory from 0 (better) to 10 (worse). Therefore the standardised mean difference for the pooled effect estimate was reported for these outcomes. We converted odds ratios from two studies for musculoskeletal outcomes at various sites to standardised mean differences, so that they could be pooled in a meta‐analysis.
We calculated the mean difference between intervention and control groups adjusted for baseline for two studies (Brakenridge 2016; Gibbs 2018), using pre‐post correlation data for musculoskeletal outcomes at various sites obtained from the Parry 2015 study.
Pain‐related disability
Gibbs 2018 and Ognibene 2016) assessed pain‐related disability. Gibbs 2018 used the Oswestry Disabilty Index, and Ognibene 2016 used the Roland Morris Disability Questionnaire.
Follow‐up times
In six studies, the longest follow‐up was six months or less (Alkhajah 2012; Danquah 2017; Graves 2015; Healy 2013; Ognibene 2016; Parry 2015), which we categorised as short‐term follow‐up. Gibbs 2018 followed participants between six and less than 12 months, which we categorised as medium‐term follow‐up. Brakenridge 2016,Edwardson 2018, and Healy 2016 provided follow‐up for 12 months, which we defined as long‐term follow‐up.
Excluded studies
Of the 77 papers that we assessed as full text, 67 did not meet our inclusion criteria, and we excluded them. Forty‐one studies provided the wrong intervention, and 15 studies used an inappropriate study design. Four studies were not conducted with employees with musculoskeletal symptoms, three studies were not conducted in the workplace setting, one study did not report musculoskeletal symptoms, two were ongoing studies, and one study is awaiting classification. See the Characteristics of excluded studies table for further details.
Risk of bias in included studies
Risk of bias for the eight included RCTs was assessed based on the seven criteria as outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). For the two CBA studies, we assessed risk of bias using the five Cochrane criteria (blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and baseline imbalance) and the two additional criteria (confounding and selection bias) modified from Downs (Downs 1998). We combined the risk of bias for all studies and illustrated this in Figure 2 and Figure 3. Risk of bias varied considerably across the studies (Figure 2).
2.
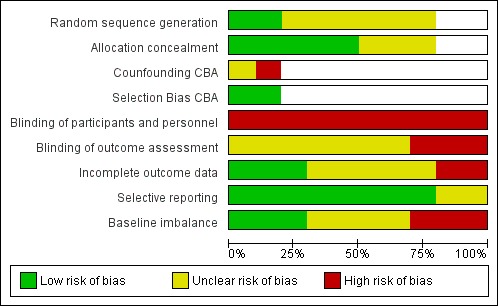
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
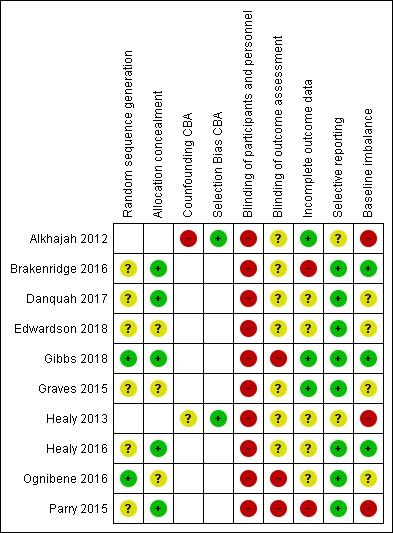
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
For the eight included RCTs, although all used randomisation procedures for either participants ‐ Gibbs 2018; Graves 2015; Ognibene 2016 ‐ or clusters ‐ Brakenridge 2016; Danquah 2017; Edwardson 2018; Healy 2016; Parry 2015 ‐ only two studies included participants who all had baseline musculoskeletal symptoms (Gibbs 2018; Ognibene 2016). For these studies, the randomisation sequence was sufficiently described and was rated at low risk of bias for this criterion. For the other six studies (Brakenridge 2016; Danquah 2017; Edwardson 2018; Healy 2016; Graves 2015; Parry 2015), as only data from participants with baseline musculoskeletal symptoms were included in the analyses, randomisation of participants from these studies was rated as unclear. Five of the studies reported concealment of allocation (Brakenridge 2016; Danquah 2017; Gibbs 2018; Healy 2016; Parry 2015), and we rated these studies at low risk of bias. For the other three studies (Edwardson 2018; Graves 2015; Ognibene 2016), allocation concealment was not described, and we judged the risk of bias as unclear for this criterion.
Blinding
Due to the nature of the interventions, it was not possible to blind participants to the interventions that they were receiving, so for all of the included studies, the risk of performance bias was high. Self‐reported musculoskeletal symptoms was the main outcome for this review, and as participants were not blinded to the intervention, even if studies reported blinding of the outcome assessor (Edwardson 2018; Danquah 2017), the risk of bias could be judged at best to be unclear, as not being blinded to the intervention may contribute to bias in the self‐reporting of musculoskeletal symptoms. Parry 2015 stated that the researcher responsible for data analysis was not blinded to participant allocation; for this study, we judged the risk of detection bias to be high. For two studies (Gibbs 2018; Ognibene 2016), self‐reported musculoskeletal symptoms was the primary outcome measure and participants were not blinded to the intervention, so we judged the risk of risk of bias to be high for these studies.
Incomplete outcome data
Two studies were judged to be at high risk of attrition bias due to incomplete outcome data (Brakenridge 2016; Parry 2015). Both of these studies used stratified data for participants with baseline musculoskeletal symptoms and loss to follow‐up was substantial ‐ in excess of 40% for most body regions. We judged five studies to have unclear risk of attrition (Danquah 2017; Edwardson 2018; Healy 2013; Healy 2016; Ognibene 2016). For Edwardson 2018, Healy 2013, and Healy 2016, attrition details for participants with baseline pain were not provided. In Ognibene 2016, attrition was 19%, and it was unclear whether the data were analysed by intention‐to‐treat. We judged Alkhajah 2012,Gibbs 2018, and Graves 2015 to have low risk of attrition bias due to use of intention‐to‐treat analyses in Graves 2015 and low attrition rate in Alkhajah 2012 and Gibbs 2018; sensitivity analysis comparing only completers with reported data showed similar results (Gibbs 2018).
Selective reporting
All of the included RCTs were judged to have low risk of reporting bias. All studies reported outcomes that were consistent with the published trial protocols. For the two CBA studies (Alkhajah 2012; Healy 2013), we judged the risk of reporting bias to be unclear, as there was no published trial protocol for each of these studies.
Other potential sources of bias
Another source of potential bias that was examined was imbalance of baseline characteristics such as gender, age, baseline musculoskeletal symptoms, and work‐related factors. We judged Brakenridge 2016,Gibbs 2018, and Healy 2016 to have low risk of bias for this criterion, as identified baseline differences were adjusted for in the analyses. We judged Danquah 2017,Edwardson 2018,Graves 2015, and Ognibene 2016 to have unclear risk of bias for baseline imbalance, as baseline data for only the full group (not for intervention and control groups separately) were provided. For Alkhajah 2012, Healy 2013, and Parry 2015, we judged risk of bias due to baseline imbalance as high due to large differences in musculoskeletal symptoms at baseline for some body regions.
Confounding bias CBA
We judged Alkhajah 2012 to have high risk of confounding bias, as it was not possible to adjust for all potential confounders due to the small sample. For Healy 2013, even though adjustments were made for baseline values, unmeasured confounders such as baseline activity levels or job tasks may have influenced the results, so we judged the risk of confounder bias to be unclear.
Selection bias CBA
For both CBAs (Alkhajah 2012; Healy 2013), we judged risk of selection bias to be low, as intervention and control participants were recruited from the same organisation over the same time period.
Overall risk of bias
Overall, we judged only one study to have low risk of bias (Gibbs 2018). None of the included studies were able to blind participants or personnel due to the nature of the interventions. In eight of the included studies (Alkhajah 2012; Brakenridge 2016; Danquah 2017; Edwardson 2018; Graves 2015; Healy 2013; Healy 2016; Parry 2015), only data for select participants with baseline musculoskeletal symptoms were included in the analyses. This has compromised the randomisation process of the study; therefore we judged these studies to have high risk of bias. For these studies, some of the risk of bias criteria were unclear, as musculoskeletal symptoms were secondary outcomes, so full details were not reported in the studies for this outcome. In addition, high risk of bias overall was due to blinding of outcome assessors (Gibbs 2018; Ognibene 2016; Parry 2015); incomplete outcome data (Brakenridge 2016; Parry 2015); and baseline imbalances (Alkhajah 2012; Healy 2013; Parry 2015). We have illustrated the summary of judgements for each item in the risk of bias for included studies in Figure 3.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
Summary of findings for the main comparison. Sit‐stand desk compared to no intervention for increasing standing or walking for decreasing musculoskeletal symptoms in sedentary workers.
| Sit‐stand desk compared to no intervention for increasing standing or walking for decreasing musculoskeletal symptoms in sedentary workers | ||||||
| Patient or population: sedentary workers with musculoskeletal symptoms Setting: office setting Intervention: sit‐stand desk Comparison: no intervention | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with no intervention | Risk with sit‐stand desk | |||||
| Mean difference in low back pain follow‐up short‐term | SMD 0.35 lower (0.8 lower to 0.1 higher) | ‐ | 79 (2 RCTs) | ⊕⊕⊝⊝ Lowa,b | ||
| Mean difference in upper back pain follow‐up short‐term | SMD 0.48 lower (0.96 lower to 0) | ‐ | 71 (2 RCTs) | ⊕⊕⊝⊝ Lowa,b | ||
| Mean difference in neck and shoulder pain/discomfort follow‐up short‐term | Mean difference in neck and shoulder pain/discomfort follow‐up short‐term: 2.2 score | MD 0.6 score lower (1.5 lower to 0.3 higher) | ‐ | 31 (1 RCT) | ⊕⊕⊝⊝ Lowb,c | |
| Mean difference in physical disability caused by LBP, RMDQ score follow‐up short‐term | Mean difference in physical disability caused by LBP, RMDQ score follow‐up short‐term: 5.67 score | MD 0.4 score lower (2.7 lower to 1.9 higher) | ‐ | 46 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; LBP: low back pain; MD: mean difference; RCT: randomised controlled trial; RMDQ: Roland Morris Disability Questionnaire; SMD: standardised mean difference. | ||||||
| GRADE Working Group grades of evidence. High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aConcerns about blinding of personnel and outcome assessors as well as allocation concealment. Unacceptable loss to follow‐up in Ognibene (2016); downgraded one level.
bLow number of participants, wide confidence intervals; downgraded one level.
cConcerns about blinding of personnel and outcome assessors as well as random sequence generation; downgraded one level.
Summary of findings 2. Treadmill workstation compared to no intervention for increasing standing or walking for decreasing musculoskeletal symptoms in sedentary workers.
| Treadmill workstation compared to no intervention for increasing standing or walking for decreasing musculoskeletal symptoms in sedentary workers | ||||||
| Patient or population: sedentary workers with musculoskeletal symptoms Setting: office setting Intervention: treadmill workstation Comparison: no intervention | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with no intervention | Risk with treadmill workstation | |||||
| Proportion of participants with low back pain/discomfort follow‐up short‐term | 714 per 1000 | 750 per 1000 (357 to 1000) | RR 1.05 (0.50 to 2.19) | 11 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | |
| Proportion of participants with neck pain/discomfort follow‐up short‐term | 571 per 1000 | 714 per 1000 (320 to 1000) | RR 1.25 (0.56 to 2.77) | 14 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | |
| Proportion of participants with shoulder pain/discomfort follow‐up short‐term | 667 per 1000 | 753 per 1000 (340 to 1000) | RR 1.13 (0.51 to 2.50) | 10 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence. High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aConcerns about blinding of participants and personnel, loss to follow‐up and baseline imbalance; downgraded one level.
bLow number of participants and wide confidence intervals; downgraded one level.
Summary of findings 3. Activity tracker compared to alternate intervention or no intervention for increasing standing or walking for decreasing musculoskeletal symptoms in sedentary workers.
| Activity tracker compared to alternate intervention or no intervention for increasing standing or walking for decreasing musculoskeletal symptoms in sedentary workers | ||||||
| Patient or population: sedentary workers with musculoskeletal symptoms Setting: office setting Intervention: activity tracker Comparison: alternate intervention or no intervention | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with alternate intervention or no intervention | Risk with activity tracker | |||||
| Mean difference in low back pain/discomfort follow‐up short‐term | SMD 0.05 lower (0.87 lower to 0.77 higher) | ‐ | 31 (2 RCTs) | ⊕⊕⊝⊝ Lowa,b | ||
| Mean difference in upper back pain/discomfort follow‐up short‐term | SMD 0.04 lower (0.92 lower to 0.84 higher) | ‐ | 23 (2 RCTs) | ⊕⊕⊝⊝ Lowa,b | ||
| Mean difference in neck pain/discomfort follow‐up short‐term | SMD 0.05 higher (0.68 lower to 0.78 higher) | ‐ | 33 (2 RCTs) | ⊕⊕⊝⊝ Lowa,b | ||
| Mean difference in shoulder pain/discomfort follow‐up short‐term | SMD 0.14 higher (0.63 lower to 0.9 higher) | ‐ | 31 (2 RCTs) | ⊕⊕⊝⊝ Lowa,b | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; SMD: standardised mean difference. | ||||||
| GRADE Working Group grades of evidence. High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aConcerns about personnel and outcome assessor blinding; downgraded one level.
bSmall sample size and wide confidence intervals; downgraded one level.
Summary of findings 4. Multi‐component intervention compared to no intervention for increasing standing or walking for decreasing musculoskeletal symptoms in sedentary workers.
| Multi‐component intervention compared to no intervention for increasing standing or walking for decreasing musculoskeletal symptoms in sedentary workers | ||||||
| Patient or population: sedentary workers with musculoskeletal symptoms Setting: office setting Intervention: multi‐component intervention Comparison: no intervention | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with no intervention | Risk with multi‐component intervention | |||||
| Proportion of participants with low back pain/discomfort follow‐up short‐term | 625 per 1000 | 581 per 1000 (431 to 794) | RR 0.93 (0.69 to 1.27) | 107 (3 RCTs) | ⊕⊕⊝⊝ Lowa,b | |
| Proportion of participants with upper back pain/discomfort follow‐up short‐term | 353 per 1000 | 311 per 1000 (141 to 692) | RR 0.88 (0.40 to 1.96) | 40 (2 RCTs) | ⊕⊕⊝⊝ Lowa,b | |
| Proportion of participants with neck pain/discomfort follow‐up short‐term | 623 per 1000 | 623 per 1000 (473 to 822) | RR 1.00 (0.76 to 1.32) | 115 (3 RCTs) | ⊕⊕⊝⊝ Lowa,b | |
| Proportion of participants with shoulder pain/discomfort follow‐up short‐term | 207 per 1000 | 172 per 1000 (25 to 1000) | RR 0.83 (0.12 to 5.80) | 66 (2 RCTs) | ⊕⊝⊝⊝ Very lowa,b,c | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence. High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aConcerns about personnel and outcome assessor blinding; downgraded one level.
bSmall sample size and wide confidence intervals; downgraded one level.
cHigh heterogeneity, I² = 69%; downgraded one level.
Studies were insufficient to perform the planned subgroup and sensitivity analysis. Because we could not pool more than two studies for any single outcome, we could not test for the effect of small studies using a funnel plot.
Interventions targeted at the physical work environment
Outcome: musculoskeletal symptoms
Musculoskeletal symptoms: follow‐up at short term
Sit‐stand workstation
Three studies compared the effects of using a sit‐stand desk compared to no intervention (Alkhajah 2012; Graves 2015; Ognibene 2016). Alkhajah 2012 was a CBA study with a small number of participants with baseline musculoskeletal symptoms. The Cochrane Handbook for Systematic Reviews of Interventions does not recommend pooling studies using different designs (two RCTs and one CBA) due to differences in risk of bias between the studies (Higgins 2011). Therefore data from Alkhajah 2012 were not pooled with data from the other RCTs (Analysis 1.5; Analysis 1.6; Analysis 1.7; Analysis 1.8; Analysis 1.9; Analysis 1.10).
1.5. Analysis.
Comparison 1 Sit‐stand desk versus no intervention, Outcome 5 Proportion of participants with low back pain follow‐up short‐term (CBA).
1.6. Analysis.
Comparison 1 Sit‐stand desk versus no intervention, Outcome 6 Proportion of participants with upper back pain follow‐up short‐term (CBA).
1.7. Analysis.
Comparison 1 Sit‐stand desk versus no intervention, Outcome 7 Proportion of participants with neck pain follow‐up short‐term (CBA).
1.8. Analysis.
Comparison 1 Sit‐stand desk versus no intervention, Outcome 8 Proportion of participants with shoulder pain follow‐up short‐term (CBA).
1.9. Analysis.
Comparison 1 Sit‐stand desk versus no intervention, Outcome 9 Proportion of participants with wrist/hand pain follow‐up short‐term (CBA).
1.10. Analysis.
Comparison 1 Sit‐stand desk versus no intervention, Outcome 10 Proportion of participants with hip pain follow‐up short‐term (CBA).
Pooled analysis of the other two studies ‐ Graves 2015 and Ognibene 2016 ‐ with 79 participants (43 in the intervention group) revealed no considerable effect of using a sit‐stand desk on low back symptom intensity (standardised mean difference (SMD) ‐0.35, 95% confidence interval (CI) ‐0.80 to 0.10; I² = 0%; Figure 4; Analysis 1.1).
4.
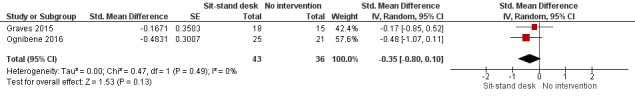
Forest plot of comparison: 1 Sit‐stand desk versus no intervention, outcome: 1.1 Mean difference in low back pain follow‐up short‐term.
1.1. Analysis.
Comparison 1 Sit‐stand desk versus no intervention, Outcome 1 Mean difference in low back pain follow‐up short‐term.
Similarly, pooled analysis of these two studies (71 participants, with 41 in the intervention group) showed no considerable effect of using a sit‐stand desk on upper back symptom intensity (SMD ‐0.48, 95% CI ‐0.96 to 0.00; I = 0%; Figure 5; Analysis 1.2).
5.
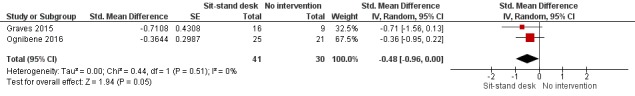
Forest plot of comparison: 1 Sit‐stand desk versus no intervention, outcome: 1.2 Mean difference in upper back pain follow‐up short‐term.
1.2. Analysis.
Comparison 1 Sit‐stand desk versus no intervention, Outcome 2 Mean difference in upper back pain follow‐up short‐term.
One study found no significant reduction in the intensity of symptoms in the neck/shoulder when a sit‐stand desk was used compared to no intervention (mean difference (MD) ‐0.60, 95% CI ‐1.50 to 0.30; Graves 2015; Analysis 1.3).
1.3. Analysis.
Comparison 1 Sit‐stand desk versus no intervention, Outcome 3 Mean difference in neck and shoulder pain/discomfort follow‐up short‐term.
Treadmill workstation
One study compared the effect of a treadmill workstation versus no intervention on the presence or absence of musculoskeletal symptoms (Parry 2015). However, as only participants with baseline symptoms were included in these analyses, participant numbers were very low for each body region (0 to 14). Analyses on such small participant numbers did not provide statistically meaningful results for low or upper back pain, nor for neck, shoulder, elbow, or knee pain (Analysis 2.1; Analysis 2.2; Analysis 2.3; Analysis 2.4; Analysis 2.5; Analysis 2.6).
2.1. Analysis.
Comparison 2 Treadmill workstation versus no intervention, Outcome 1 Proportion of participants with low back pain/discomfort follow‐up short‐term.
2.2. Analysis.
Comparison 2 Treadmill workstation versus no intervention, Outcome 2 Proportion of participants with upper back pain/discomfort follow‐up short‐term.
2.3. Analysis.
Comparison 2 Treadmill workstation versus no intervention, Outcome 3 Proportion of participants with neck pain/discomfort follow‐up short‐term.
2.4. Analysis.
Comparison 2 Treadmill workstation versus no intervention, Outcome 4 Proportion of participants with shoulder pain/discomfort follow‐up short‐term.
2.5. Analysis.
Comparison 2 Treadmill workstation versus no intervention, Outcome 5 Proportion of participants with elbow/wrist/hand pain/discomfort follow‐up short‐term.
2.6. Analysis.
Comparison 2 Treadmill workstation versus no intervention, Outcome 6 Proportion of participants with knee pain/discomfort follow‐up short‐term.
Musculoskeletal symptoms: follow‐up at medium and long term
No studies comparing the effects of interventions targeted at the physical work environment versus no intervention reported musculoskeletal symptoms at medium‐ and long‐term follow‐up.
Outcome: pain‐related disability
Pain‐related disability: follow‐up at short term
Sit‐stand workstation
One study examined the use of a sit‐stand desk compared to no intervention for pain‐related disability caused by low back symptoms using the Roland Morris Disability Questionnaire (Ognibene 2016). No significant reduction in pain‐related disability was found in this study with 46 participants (25 in the intervention group) (MD ‐0.4, 95% CI ‐2.70 to 1.90; Analysis 1.4).
1.4. Analysis.
Comparison 1 Sit‐stand desk versus no intervention, Outcome 4 Mean difference in physical disability caused by LBP, RMDQ score follow‐up short‐term.
Pain‐related disability: follow‐up at medium and long term
Disability was not reported in any studies comparing the effects of interventions targeted at the physical work environment versus no intervention.
Outcome: work performance and productivity
Work performance and productivity were not reported in any study comparing the effects of interventions targeted at the physical work environment versus no intervention.
Outcome: sickness absenteeism
No studies comparing the effects of interventions targeted at the physical work environment versus no intervention reported sickness absenteeism.
Outcome: adverse events
No studies comparing the effects of interventions targeted at the physical work environment versus no intervention reported adverse events such as venous disorders or perinatal complications.
Interventions targeted at the individual
Outcome: musculoskeletal symptoms
Musculoskeletal symptoms: follow‐up at short term
Activity tracker
Two studies examined the effects of using an activity tracker compared to an alternative intervention or no intervention in the short term on musculoskeletal symptoms (Brakenridge 2016; Parry 2015). Pooled analysis of these two studies (31 participants; 11 in the intervention group) found no considerable effect of the activity tracker on low back symptoms (pooled intensity and presence of symptoms) (SMD ‐0.05, 95% CI ‐0.87 to 0.77; Analysis 3.1). Similarly, no considerable effects were found for upper back symptoms (23 participants; 11 in the intervention group) (SMD ‐0.04, 95% CI ‐0.92 to 0.84; I² = 41%; Analysis 3.2); neck symptoms (33 participants; 14 in the intervention group) (SMD ‐0.05, 95% CI ‐0.68 to 0.78; I² = 0%; Analysis 3.3); shoulder symptoms (31 participants; 12 in the intervention group) (SMD ‐0.14, 95% CI ‐0.63 to 0.90; I² = 0%; Analysis 3.4); and elbow/wrist/hand symptoms (18 participants; 5 in the intervention group) (SMD ‐0.30, 95% CI ‐1.44 to 0.85; I² = 0%; Analysis 3.5). Musculoskeletal symptoms were assessed for the remaining body regions by both studies (Brakenridge 2016; Parry 2015); however, there were no participants with baseline musculoskeletal symptoms in the activity tracker intervention group in Parry 2015. Therefore, only data from Brakenridge 2016 are presented. No significant difference was found in the proportion of participants reporting hip/thigh/buttock symptoms (MD ‐1.42, 95% CI ‐3.63 to 0.79; Analysis 3.6); knee symptoms (MD ‐0.40, 95% CI ‐2.37 to 1.57; Analysis 3.7); or ankle/foot symptoms (MD ‐0.86, 95% CI ‐3.73 to 2.01; Analysis 3.8) following the intervention.
3.1. Analysis.
Comparison 3 Activity tracker versus alternate intervention or no intervention, Outcome 1 Mean difference in low back pain/discomfort follow‐up short‐term.
3.2. Analysis.
Comparison 3 Activity tracker versus alternate intervention or no intervention, Outcome 2 Mean difference in upper back pain/discomfort follow‐up short‐term.
3.3. Analysis.
Comparison 3 Activity tracker versus alternate intervention or no intervention, Outcome 3 Mean difference in neck pain/discomfort follow‐up short‐term.
3.4. Analysis.
Comparison 3 Activity tracker versus alternate intervention or no intervention, Outcome 4 Mean difference in shoulder pain/discomfort follow‐up short‐term.
3.5. Analysis.
Comparison 3 Activity tracker versus alternate intervention or no intervention, Outcome 5 Mean difference in elbow, wrist/hand pain/discomfort follow‐up short‐term.
3.6. Analysis.
Comparison 3 Activity tracker versus alternate intervention or no intervention, Outcome 6 Mean difference in hip/thigh/buttock pain/discomfort follow‐up short‐term.
3.7. Analysis.
Comparison 3 Activity tracker versus alternate intervention or no intervention, Outcome 7 Mean difference in knee pain/discomfort follow‐up short‐term.
3.8. Analysis.
Comparison 3 Activity tracker versus alternate intervention or no intervention, Outcome 8 Mean difference in ankle/feet pain/discomfort follow‐up short‐term.
Musculoskeletal symptoms: follow‐up at medium term
No studies comparing the effects of interventions targeted at the individual versus no intervention reported musculoskeletal symptoms at medium‐term follow‐up.
Musculoskeletal symptoms: follow‐up at long term
Activity tracker
One study examined the effects of using an activity tracker compared to an alternative intervention or no intervention on the intensity of musculoskeletal symptoms in the long term (Brakenridge 2016). Results were inconsistent between body regions, with MD ranging from ‐1.61 to 1.86 in various body regions (Analysis 3.9; Analysis 3.10; Analysis 3.11; Analysis 3.12; Analysis 3.13; Analysis 3.14; Analysis 3.15); as only participants with baseline pain were included in these analyses, participant numbers for each body region were very low, ranging from six to 13 participants.
3.9. Analysis.
Comparison 3 Activity tracker versus alternate intervention or no intervention, Outcome 9 Mean difference in low back pain/discomfort follow‐up long‐term.
3.10. Analysis.
Comparison 3 Activity tracker versus alternate intervention or no intervention, Outcome 10 Mean difference in upper back pain/discomfort follow‐up long‐term.
3.11. Analysis.
Comparison 3 Activity tracker versus alternate intervention or no intervention, Outcome 11 Mean difference in neck pain/discomfort follow‐up long‐term.
3.12. Analysis.
Comparison 3 Activity tracker versus alternate intervention or no intervention, Outcome 12 Mean difference in shoulder pain/discomfort follow‐up long‐term.
3.13. Analysis.
Comparison 3 Activity tracker versus alternate intervention or no intervention, Outcome 13 Mean difference in hip/thigh/buttock pain/discomfort follow‐up long‐term.
3.14. Analysis.
Comparison 3 Activity tracker versus alternate intervention or no intervention, Outcome 14 Mean difference in knee pain/discomfort follow‐up long‐term.
3.15. Analysis.
Comparison 3 Activity tracker versus alternate intervention or no intervention, Outcome 15 Mean difference in ankle/feet pain/discomfort follow‐up long‐term.
Outcome: pain‐related disability
Pain‐related disability was not reported in any studies comparing the effects of interventions targeted at the individual versus no intervention.
Outcome: work performance and productivity
Work performance and productivity were not reported in any studies comparing the effects of interventions targeted at the individual versus no intervention.
Outcome: sickness absenteeism
No studies comparing the effects of interventions targeted at the individual versus no intervention reported sickness absenteeism.
Outcome: adverse events
No studies comparing the effects of interventions targeted at the individual versus no intervention reported adverse events.
Interventions targeted at the organisation
No studies evaluated the effects of interventions targeted at the organisation on musculoskeletal symptoms, work performance and productivity, sickness absenteeism, or adverse events.
Multi‐component interventions
Outcome: musculoskeletal symptoms
Musculoskeletal symptoms: follow‐up at short term
Four studies examined the effects of a multi‐component intervention compared to no intervention in the short term on musculoskeletal symptoms (Danquah 2017; Edwardson 2018; Healy 2013; Healy 2016).
Healy 2013 was a CBA study with a small number of participants with baseline musculoskeletal symptoms. The Cochrane Handbook for Systematic Reviews of Interventions does not recommend pooling studies of different designs due to differences in risk of bias between studies (Higgins 2011). Therefore the data from Healy 2013 were not pooled with data from the other RCTs (Analysis 4.24; Analysis 4.25; Analysis 4.26; Analysis 4.27; Analysis 4.28; Analysis 4.29; Analysis 4.30; Analysis 4.31; Analysis 4.32). Pooled analysis of the other three studies ‐ Danquah 2017,Edwardson 2018, and Healy 2016 ‐ revealed no statistically significant reduction in the likelihood of reporting the presence of low back symptoms from a multi‐component intervention compared to no intervention (107 participants; 59 in the intervention group) (RR 0.93, 95% CI 0.69 to 1.270; I² = 0%; Analysis 4.1; Figure 6). Results showed no statistically significant reduction in the presence of neck symptoms between intervention and control groups (115 participants; 62 in the intervention group) (risk ratio (RR) 1.00, 95% CI 0.76 to 1.32; I² = 43%; Analysis 4.3).
4.24. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 24 Proportion of participants with low back pain follow‐up short‐term (CBA).
4.25. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 25 Proportion of participants with upper back pain follow‐up short‐term (CBA).
4.26. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 26 Proportion of participants with neck pain follow‐up short‐term (CBA).
4.27. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 27 Proportion of participants with shoulder pain follow‐up short‐term (CBA).
4.28. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 28 Proportion of participants with elbow pain follow‐up short‐term (CBA).
4.29. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 29 Proportion of participants with wrist/hand pain follow‐up short‐term (CBA).
4.30. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 30 Proportion of participants with legs/feet/ankles pain follow‐up short‐term (CBA).
4.31. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 31 Proportion of participants with hip pain follow‐up short‐term (CBA).
4.32. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 32 Proportion of participants with knee pain follow‐up short‐term (CBA).
4.1. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 1 Proportion of participants with low back pain/discomfort follow‐up short‐term.
6.
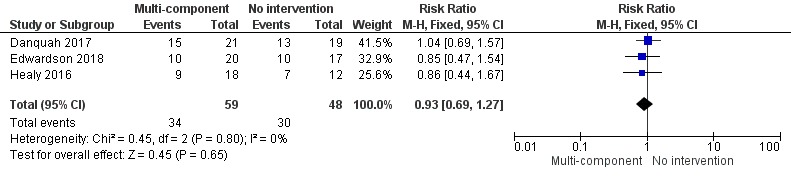
Forest plot of comparison: 4 Multi‐component intervention versus no intervention, outcome: 4.1 Proportion of participants with low back pain/discomfort follow‐up short‐term.
4.3. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 3 Proportion of participants with neck pain/discomfort follow‐up short‐term.
Two studies (40 participants; 23 in the intervention group) found no statistically significant reduction in the likelihood of reporting the presence of upper back symptoms from a multi‐component intervention compared to no intervention (RR 0.88, 95% CI 0.40 to 1.96; I² = 0%; Analysis 4.2) (Edwardson 2018; Healy 2016).
4.2. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 2 Proportion of participants with upper back pain/discomfort follow‐up short‐term.
Edwardson 2018 and Healy 2016 found no statistically significant reduction in the likelihood of reporting the presence of shoulder symptoms (66 participants; 37 in the intervention group) (RR 0.83, 95% CI 0.12 to 5.80; I² = 69%; Analysis 4.4).
4.4. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 4 Proportion of participants with shoulder pain/discomfort follow‐up short‐term.
Healy 2016 found no statistically significant reduction in the likelihood of reporting the presence of hand and wrist symptoms (18 participants; 13 in the intervention group) (RR 0.77, 95% CI 0.30 to 1.94; Analysis 4.5).
4.5. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 5 Proportion of participants with wrist/hand pain/discomfort follow‐up short‐term.
Edwardson 2018 and Healy 2016 found no statistically significant reduction in the likelihood of reporting the presence of elbow symptoms (20 participants; 13 in the intervention group) (RR 0.31, 95% CI 0.09 to 1.06; I² = 0%; Analysis 4.6); hip symptoms (34 participants; 18 in the intervention group) (RR 1.15, 95% CI 0.56 to 2.34; I² = 0%; Analysis 4.7); knee symptoms (43 participants; 22 in the intervention group) (RR 1.25, 95% CI 0.28 to 5.68; I² = 68%; Analysis 4.8); and foot and ankle symptoms (37 participants; 19 in the intervention group) (RR 0.62, 95% CI 0.34 to 1.15; I² = 0%; Analysis 4.9). Danquah 2017 found no statistically significant difference in the likelihood of reporting the presence of symptoms in the extremities (40 participants; 19 in the intervention group) (RR 1.02, 95% CI 0.63 to 1.65; Analysis 4.10).
4.6. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 6 Proportion of participants with elbow pain/discomfort follow‐up short‐term.
4.7. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 7 Proportion of participants with hip pain/discomfort follow‐up short‐term.
4.8. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 8 Proportion of participants with knee pain/discomfort follow‐up short‐term.
4.9. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 9 Proportion of participants with legs/feet/ankles pain/discomfort follow‐up short‐term.
4.10. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 10 Proportion of participants with extremity pain/discomfort follow‐up short‐term.
Musculoskeletal symptoms: follow‐up at medium term
One study examined the effects of a multi‐component intervention compared to no intervention in the medium term on the intensity of musculoskeletal symptoms (Gibbs 2018). Researchers found no statistically significant reduction in the intensity of low back symptoms (27 participants; 13 in the intervention group) (MD ‐0.40, 95% CI ‐1.95 to 1.15; Analysis 4.11); upper back symptoms (27 participants; 13 in the intervention group) (MD ‐0.70, 95% CI ‐2.12 to 0.72; Analysis 4.12); leg symptoms (27 participants; 13 in the intervention group) (MD ‐0.80, 95% CI ‐2.49 to 0.89; Analysis 4.13).
4.11. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 11 Mean difference in low back pain/discomfort follow‐up medium‐term.
4.12. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 12 Mean difference in upper back pain/discomfort follow‐up medium‐term.
4.13. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 13 Mean difference in leg pain/discomfort follow‐up medium‐term.
Musculoskeletal symptoms: follow‐up at long term
Two studies examined the effects of a multi‐component intervention compared to no intervention in the long term on musculoskeletal symptoms (Edwardson 2018; Healy 2016). Pooled analysis of these two studies found no statistically significant difference in the likelihood of reporting the presence of low back symptoms (67 participants; 38 in the intervention group) (RR 0.89, 95% CI 0.57 to 1.40; I² = 0%; Analysis 4.15); upper back symptoms (40 participants; 23 in the intervention group) (RR 0.52, 95% CI 0.08 to 3.29; I² = 68%; Analysis 4.16); neck symptoms (60 participants; 32 in the intervention group) (RR 0.67, 95% CI 0.41 to 1.08; I² = 19%; Analysis 4.17); shoulder symptoms (66 participants; 37 in the intervention group) (RR 0.93, 95% CI 0.57 to 1.54; I² = 0%; Analysis 4.18); leg, foot, or ankle symptoms (37 participants; 19 in the intervention group) (RR 1.48, 95% CI 0.74 to 2.96; I² = 0%; Analysis 4.20); hip symptoms (34 participants; 18 in the intervention group) (RR 0.92, 95% CI 0.36 to 2.37; I² = 57%; Analysis 4.21); knee symptoms (43 participants; 22 in the intervention group) (RR 0.91, 95% CI 0.46 to 1.79; I² = 0%; Analysis 4.22); and elbow symptoms (20 participants; 13 in the intervention group) (RR 0.35, 95% CI 0.08 to 1.52; I² = 23%; Analysis 4.23). Healy 2016 found no statistically significant effect on symptoms in the hand and wrist (18 participants; 13 in the intervention group) (RR 0.90, 95% CI 0.37, 2.15; Analysis 4.19) when comparing a multi‐component intervention versus no intervention.
4.15. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 15 Proportion of participants with low back pain/discomfort follow‐up long‐term.
4.16. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 16 Proportion of participants with upper back pain/discomfort follow‐up long‐term.
4.17. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 17 Proportion of participants with neck pain/discomfort follow‐up long‐term.
4.18. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 18 Proportion of participants with shoulder pain/discomfort follow‐up long‐term.
4.20. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 20 Proportion of participants with legs/feet/ankle pain/discomfort follow‐up long‐term.
4.21. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 21 Proportion of participants with hip pain/discomfort follow up long‐term.
4.22. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 22 Proportion of participants with knee pain/discomfort follow‐up long‐term.
4.23. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 23 Proportion of participants elbow pain/discomfort follow‐up long‐term.
4.19. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 19 Proportion of participants with wrist/hand pain/discomfort follow‐up long‐term.
Outcome: pain‐related disability
Pain‐related disability: follow‐up at short term
Pain related disability was not reported in any studies comparing the effects of multi‐component intervention versus no intervention.
Disability: follow‐up at medium and long term
Gibbs 2018 (27 participants; 13 in the intervention group) found a statistically significant difference in disability in the medium term following a multi‐component intervention compared to no intervention (MD ‐8.80, 95% CI ‐17.46 to ‐0.14; Analysis 4.14).
4.14. Analysis.
Comparison 4 Multi‐component intervention versus no intervention, Outcome 14 Mean difference in disability follow‐up medium‐term.
Disability: follow‐up at long term
Disability was not reported in any studies comparing the effects of a multi‐component intervention versus no intervention.
Outcome: work performance and productivity
Work performance and productivity were not reported in any study comparing the effects of a multi‐component intervention versus no intervention.
Outcome: sickness absenteeism
No studies comparing the effects of a multi‐component intervention versus no intervention reported sickness absenteeism.
Outcome: adverse events
No studies comparing the effects of a multi‐component intervention versus no intervention reported adverse events.
As only a small number of studies provided sufficient pooled data, we could not conduct subgroup or sensitivity analyses as planned.
Discussion
Summary of main results
Ten studies were included in this review, which examined workplace interventions that promoted standing or walking to decrease musculoskeletal symptoms in sedentary workers. Of these studies, only two ‐ Gibbs 2018 and Ognibene 2016 ‐ included participants who all had baseline musculoskeletal symptoms, and musculoskeletal symptoms was the primary outcome measure. These studies investigated changes to the physical work environment, interventions targeted at the individual, and multi‐component interventions to increase standing or walking in the workplace. No studies were found that evaluated the effects of interventions targeted solely at the organisational level.
Changes to the physical work environment
The provision of a sit‐stand workstation did not significantly reduce the intensity of low back or upper back symptoms compared to no intervention in the short term (standardised mean difference (SMD) ‐0.35, 95% confidence interval (CI) ‐0.80 to 0.10; 2 studies; low‐quality evidence) (Table 1). A single study found no significant reduction in the intensity of neck/shoulder symptoms when a sit‐stand desk was used compared to no intervention in the short term. A single study found no significant reduction in pain‐related disability between provision of a sit‐stand workstation and no intervention in the short term. No studies examined medium‐ or long‐term musculoskeletal symptoms or pain‐related disability outcomes, so it is not possible to assess the stability of these results over time. One study investigated the effects of a treadmill workstation on the presence or absence of musculoskeletal symptoms in various body regions, but as participant numbers were so small, none of the results were statistically significant (Table 2).
Interventions targeted at the individual
The pooled effect size from two studies, which evaluated the use of an activity tracker compared to an alternative intervention or no intervention, was irrelevant, with a non‐significant change in low back symptoms (pooled intensity and presence of symptoms) (SMD ‐0.05, 95% CI ‐0.87 to 0.77; low‐quality evidence); upper back symptoms (SMD ‐0.04, 95% CI ‐0.92 to 0.84; low‐quality evidence); neck symptoms (SMD ‐0.05, 95% CI ‐0.68 to 0.78; low‐quality evidence); shoulder symptoms (SMD ‐0.14, 95% CI ‐0.63 to 0.90; low‐quality evidence); and elbow/wrist/hand symptoms (SMD ‐0.30, 95% CI ‐1.44 to 0.85; low‐quality evidence) in the short term (Table 3). For the other body regions, no participants in the activity tracker intervention group had baseline musculoskeletal symptoms, so data could not be pooled. No studies examined medium‐term musculoskeletal outcomes. One study evaluated the use of an activity tracker compared to an alternative intervention or no intervention for intensity of musculoskeletal symptoms in the long term and found no significant reduction in the intensity of low back, upper back, neck, shoulder or lower limb symptoms.
Interventions incorporating multiple interventions
Multi‐component interventions incorporated individual and organisational interventions such as behavioural counselling, provision of a sit‐stand workstation attachment, use of an activity prompter, and pain self‐management. The pooled effect size from three studies that evaluated the effects of a multi‐component intervention compared to no intervention was a small, non‐significant reduction in the likelihood of reporting the presence of low back symptoms (risk ratio (RR) 0.93, 95% CI 0.69 to 1.27; low‐quality evidence) and neck symptoms (RR 1.00, 95% CI 0.76 to 1.32; low‐quality evidence) in the short term (Table 4). Similarly, two studies found a small, non‐significant reduction in the likelihood of reporting the presence of upper back symptoms (RR 0.88, 95% CI 0.40 to 1.96; low‐quality evidence) and shoulder symptoms (RR 0.83, 95% CI 0.12 to 5.80; very low‐quality evidence) following a multi‐component intervention compared to no intervention in the short term. Only one study examined the effect of a multi‐component intervention compared to no intervention in the medium term. The pooled effect from two studies that evaluated the effects of a multi‐component intervention compared to no intervention in the long term was a small non‐significant reduction in the likelihood of reporting the presence of low back symptoms (RR 0.89, 95% CI 0.57 to 1.40; low‐quality evidence). Similar results were found for upper back, neck, and upper and lower limb symptoms. One study found a statistically significant reduction in pain‐related disability following a multi‐component intervention compared to no intervention (mean difference (MD) ‐8.80, 95% CI ‐17.46 to ‐0.14) in the medium term. No studies examined long‐term disability outcomes, so it is not possible to assess the stability of these results over time.
Overall completeness and applicability of evidence
This review included ten studies that implemented interventions to increase workplace standing or walking for sedentary workers. For two studies, the primary outcome was the intensity of musculoskeletal symptoms and pain‐related disability, whereas for the other eight studies, musculoskeletal symptoms, measured by presence or intensity, were secondary outcomes or were reported as adverse events. A variety of workplace interventions were evaluated, with seven studies incorporating the use of a sit‐stand or treadmill workstation. Contemporary research related to the use of activity permissive workstations (treadmill or sit‐stand workstations) has mainly examined the effectiveness of these workstations in relation to changing sedentary behaviour in the workplace (Shrestha 2018), whereas only a few studies have evaluated the impact of activity permissive workstations on musculoskeletal symptoms.
All studies included in this review were reported from high‐income countries (Australia, Europe, USA, and UK). This is not surprising, as sedentary workers are more prevalent in high‐income countries (Brownson 2005), so it is likely that research in this field would be conducted in these countries. It is arguable that results from this review would be applicable only to people in high‐income countries; however, although high‐income countries rank back and neck as first and second in terms of years lived with disability, developing countries still rank back pain first and neck pain fourth in years lived with disability (GBDSC 2015). Therefore, in developing countries, where musculoskeletal symptoms are highly prevalent and there is a move toward increased urbanisation and a more sedentary lifestyle (Tan 2011), the findings of this review are likely to still be important. However additional research in this emerging group of sedentary workers is needed to identify potential differences in other populations.
Most outcomes were assessed only in the short term (up to six months), so it is not possible to assess the stability of intervention effects. The initial response to an intervention may be reflective of the novelty of the intervention, and health changes may or may not be sustained over time. The major barrier to workplace research that involves changes to the work environment is the cost related to providing new furniture such as sit‐stand workstations. Some studies have overcome this barrier by having a manufacturer provide the sit‐stand workstations. For example, in this review, participants in Graves 2015 were provided with a sit‐stand workstation from the manufacturer. At the conclusion of the eight‐week intervention period, participants in the control group were then offered a sit‐stand workstation. Sit‐stand workstations were also provided to participants by the manufacturer in Healy 2013, Healy 2016, and Ognibene 2016. However, there is a potential conflict of interest when research is funded in part by manufacturers providing equipment for research purposes. Positive research outcomes could provide financial benefit to the manufacturers. The potential conflict of interest in the included studies was mitigated by statements made by the researchers that manufacturers providing equipment were not involved in the research design or process. Future studies may consider incorporating longer intervention periods and follow‐up times.
All study participants were office‐based workers from universities and government or private organisations. This review included a small number of workers from a call centre ‐ Parry 2015 ‐ but did not include workers from other workplaces such as data processing centres, where workers predominantly sit and have little control over workflow. In four of the included studies, participants were recruited from a university setting, which may include a greater proportion of workers with a high educational level. Therefore, the results of this review would be applicable to populations that are primarily office‐based workers rather than predominantly call centre or data processing workers.
Although this review included studies with a variety of interventions, with the exception of a small number of participants in Parry 2015, no other study included interventions that evaluated a workplace walking intervention. Recent systematic reviews and laboratory studies have found that breaking up sitting by intermittent standing has led to reduced musculoskeletal symptoms (Healy 2012; Karakolis 2014; Thorp 2014b); however it is unclear whether occupational walking can reduce musculoskeletal symptoms. In a recent observational study, it was found that sedentary workers who walk more (measured with accelerometers) report lower‐intensity low back pain (Neilsen 2017). However, another recent study did not find an association between objectively measured occupational stepping and musculoskeletal symptoms in sedentary workers (Coenen 2018). As this review included only one study with a small number of participants given a treadmill/workstation intervention, no further conclusions can be drawn about the impact of occupational walking interventions based on this review. Future studies that implement intermittent walking such as walking meetings, 'active' email delivery, or short regular walking breaks are important to enhance our understanding of whether occupational walking can reduce musculoskeletal symptoms in sedentary workers.
Only two small studies (73 participants in total) specifically recruited participants with baseline musculoskeletal symptoms (low back pain) (Gibbs 2018; Ognibene 2016). Ognibene 2016 installed a sit‐stand workstation for three months and found a significant reduction in the intensity of low back symptoms compared to the waiting list control group (change from baseline 3.02, 95% CI 1.06 to 4.98; P = 0.03). Similarly, Gibbs 2018 found that a multi‐component intervention compared to no intervention resulted in a non‐significant reduction in low back pain intensity and a significant reduction in self‐reported disability (50% in the intervention group; 14% in the control group; P = 0.042). These two studies could not be combined for meta‐analysis due to heterogeneous interventions. Although interventions that increase standing or walking for people with baseline musculoskeletal symptoms, specifically low back symptoms, may be effective in relieving symptoms, more high‐quality studies targeting only participants with musculoskeletal symptoms are needed before strong conclusions can be drawn.
Quality of the evidence
Eight of the included studies were randomised controlled trials (RCTs) or cluster‐RCTs. Only Gibbs 2018 was judged to have low risk of bias, and the other seven RCTs and two controlled before‐and‐after (CBA) studies were rated as having high risk of bias, so that the overall quality of evidence presented in this review was found to be low to very low. Only two of the included studies reported that all participants had baseline musculoskeletal symptoms; for the other eight studies, only data from select participants with baseline musculoskeletal symptoms were included in the review. By including only select participants from RCTs, the original randomisation procedure was compromised, so for the remaining six RCTs, randomisation was rated as unclear; therefore for the included studies, randomisation may not have been effective in reducing the influence of confounding variables. In addition, as only select participants were included for eight studies, it remains unclear whether there was baseline imbalance among participant characteristics or work‐related factors, as studies provided baseline data only for the whole study cohort rather than for select participants with baseline musculoskeletal symptoms. As it is not possible to ascertain whether there was baseline imbalance for some studies, this additional source of bias contributed to the overall rating of low to very low evidence in this review.
For all included studies, it was not possible to blind participants or personnel due to the nature of the interventions. As this is consistent across all studies and would be likely in all workplace interventions, performance bias was not considered to influence the overall quality of the studies. Two studies reported blinding of the outcome assessor; however, as the main outcome for this review was self‐reported musculoskeletal symptoms, not being blinded to the intervention may have contributed to detection bias. Upon considering all criteria, review authors rated the overall quality of evidence as low to very low.
Potential biases in the review process
Studies were included in this review that did not have musculoskeletal symptoms as the main outcome, even though this was the main outcome of the review. For these studies, the primary outcomes were other outcomes such as changes in sedentary behaviour, physical activity, or metabolic health indicators such as body mass index (BMI). Therefore, these studies were not primarily designed to bring about a reduction in musculoskeletal symptoms and did not specifically target or recruit participants with musculoskeletal symptoms. In addition, although interventions to change workplace sedentary behaviour may secondarily have an impact on musculoskeletal symptoms, an intervention designed specifically to reduce musculoskeletal symptoms may focus more on posture variation (e.g. sit‐stand transitions) or on other pain‐modifying behaviours, which could influence the overall findings of this review. Studies were insufficient to test through sensitivity analysis whether studies designed to reduce musculoskeletal symptoms were different from studies that reported musculoskeletal symptoms as secondary outcomes.
In addition, as studies were insufficient, it was not possible to conduct planned sensitivity analyses. As only a small number of studies were pooled for any single outcome, it was not possible to test for the effects of small studies or publication bias by using funnel plots.
Agreements and disagreements with other studies or reviews
Several recent reviews have examined workplace interventions to reduce musculoskeletal symptoms or have included musculoskeletal outcomes as part of the review (Agarwal, 2018; Karol 2015; Neuhaus 2014 a; Shrestha 2018; Waongenngarm 2018). Agarwal, 2018, which included 12 articles, evaluated the effectiveness of sit‐stand workstations to reduce low back discomfort. This review included all study designs from laboratory and field studies. The population included in the review consisted of healthy working adults. Review authors found that sit‐stand workstations significantly reduced low back discomfort, with a pooled SMD of ‐0.23 (95% CI ‐0.437 to ‐0.023). In the current review, pooled results of two studies did not show a significant reduction in low back symptoms when sit‐stand workstations were provided. However, Agarwal, 2018 included only healthy participants and many study designs, whereas the current review included only participants from RCTs or CBA studies with baseline musculoskeletal symptoms. Although Agarwal, 2018 provides useful information on the impact of sit‐stand workstations by including a healthy population that would have consisted of participants with and without musculoskeletal symptoms, it is difficult to predict how this intervention modifies symptom behaviour among those with and without baseline symptoms. Waongenngarm 2018 found inconsistent results from two studies (one field study and one laboratory study) that examined the effects of active breaks on reducing low back symptoms. The two included studies included different populations, both with low back pain, but in one study, participants had acute pain, which may account for different responses to active breaks. The current review did not find any studies that specifically examined active breaks, so a direct comparison to the Waongenngarm 2018 review cannot be drawn. Three reviews examined workplace interventions and included musculoskeletal outcomes (Karol 2015; Neuhaus 2014 a; Shrestha 2018). Two reviews included all study designs and included a mixed population of those with and without baseline symptoms (Karol 2015; Neuhaus 2014 a); both of these reviews did not provide a meta‐analysis. Shrestha 2018 described musculoskeletal outcomes under adverse events in both the short term and the long term. Shrestha 2018 found inconsistent findings from four studies that implemented sit‐stand workstations, and found that these studies were too heterogeneous to be pooled in a meta‐analysis.
Authors' conclusions
Implications for practice.
The overall quality of the evidence is low. This review did not find a statistically significant reduction in musculoskeletal symptoms (intensity or presence of symptoms) from interventions that increased standing or walking for sedentary workers with baseline musculoskeletal symptoms. For participants with baseline musculoskeletal symptoms, the intensity of these symptoms was low. Most of the studies in this review included a mixed population of sedentary workers ‐ those with and without musculoskeletal symptoms ‐ and these studies were designed to measure other health outcomes (sedentary behaviour or cardiometabolic outcomes) rather than musculoskeletal outcomes. Therefore, the population of participants with baseline pain is a mixture of people specifically recruited because they have musculoskeletal symptoms and those who incidentally have musculoskeletal symptoms. Expectations and responses to the interventions are likely to be different if the primary goal of a study is to modify musculoskeletal symptoms rather than to change other health behaviours. Arguably, the intention of the study could account for different responses to an intervention, which could explain the overall finding of this review.
The effect of standing on musculoskeletal symptoms could also be mediated through a variety of mechanisms, depending on the nature of the symptoms and the body regions affected. For example, individuals with low and upper back symptoms may respond favourably or adversely to standing or walking, depending on the factors that underlie their musculoskeletal symptoms. For some people, loading the spinal region by standing or walking could exacerbate symptoms, whereas for others, this may bring symptom relief. Targeting interventions that promote standing or walking may be most suitable for people who indicate that standing or walking relieves symptoms, or for those who find that prolonged sitting increases musculoskeletal symptoms.
One of the findings from this review is that there was not a statistically significant increase in lower limb musculoskeletal symptoms when standing or walking interventions were provided to participants with baseline lower limb symptoms, and no other significant adverse events were reported. One of the potential barriers to implementing standing or walking interventions is the perceived potential to cause or exacerbate lower limb musculoskeletal symptoms. However, the number of participants with baseline lower limb musculoskeletal symptoms in this review was very low, and it is unclear whether participants with baseline pain in different body regions developed lower limb symptoms. Therefore, it is not clear whether standing or walking interventions contribute to lower limb musculoskeletal symptoms.
Implications for research.
Although some large RCTs have examined interventions targeted at the physical work environment and at the organisation by providing sit‐stand workstations and multi‐component interventions, these studies have included a general population of sedentary workers. No large‐scale, multi‐site trials have specifically recruited participants with baseline musculoskeletal symptoms nor have they assessed a range of clinical outcomes. It may be useful to also explore interventions to increase standing and walking for specific people who find that sitting provokes musculoskeletal symptoms.
One of the largest barriers to implementing interventions to increase standing or walking is the cost of providing interventions such as sit‐stand workstations. Some studies have bypassed this barrier by allowing manufacturers to provide workstations. Some new workplaces or re‐designed workplaces are opting to provide sit‐stand workstations for all workers. Monitoring of workers before and after an office move may be a useful way to examine the effects of sit‐stand workstations. Although it is not possible to randomise workers into a control workplace in this situation, a matched controlled work site could be recruited. Stratification of participants based on baseline musculoskeletal symptoms at the start of a controlled before‐and‐after trial would provide valuable information regarding the differential effects of standing interventions for people with and without baseline musculoskeletal symptoms. Opportunistic research of this nature, although not yielding evidence of highest quality, could provide important findings when research is cost‐prohibitive.
Alternatively, other lower‐cost interventions should be examined, such as interventions targeted at increasing incidental office walking and standing by encouraging standing or walking meetings. These interventions would have to be targeted at the organisational level, as organisational support is essential when work practices that may be perceived to reduce worker productivity are changed.
Most of the studies in this review were short term (less than six months), with only a few reporting medium‐ and long‐term outcomes. Musculoskeletal adaptations to variation in sitting and standing may not provide evidence in the short and medium term, so it is important to provide long‐term interventions while monitoring to assess whether changes in occupational standing or walking behaviour can be sustained over time, and if associated changes in musculoskeletal symptoms are evident.
What's new
| Date | Event | Description |
|---|---|---|
| 20 November 2019 | Amended | Corrected typo in the abstract from SMD ‐0.096 to ‐0.96 |
Notes
Parts of the methods section and Appendix 4 of this protocol are based on a standard template established by the Cochrane Work Review Group.
Acknowledgements
We thank Diana Blackwood, Faculty Librarian, Curtin University, for assistance in developing the search strategy for this protocol
We thank Jos Verbeek, Coordinating Editor, from the Cochrane Work Review Group, for help at all stages of preparation of the current review. We also thank Jani Ruotsalainen, Managing Editor, and Editor Leslie Stayner and external peer referees Don Krawcic, Jukka Salmi, Rosanne Freak‐Poli, and Virpi Kalakoski for their comments and Dolores Matthews for copyediting the text.
Appendices
Appendix 1. CENTRAL search strategy
#1 MeSH descriptor: Workplace
#2 MeSH descriptor: Sedentary Lifestyle
#3 office:ti,ab,kw
#4 office worker:ti,ab,kw
#5 MeSH descriptor: Occupational Exposure
#6 "sedentary":ti,ab,kw
#7 sedentary behaviour or sedentary behavior:ti,ab,kw
#8 "office worker*" or "sedentary worker*":ti,ab,kw
#9 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8
#10 MeSH descriptor: Musculoskeletal Pain
#11 MeSH descriptor: Back Pain
#12 MeSH descriptor: Neck Pain
#13 #10 or #11 or #12
#14 #9 and #13
#15 sit:ti,ab,kw
#16 "sitting":ti,ab,kw
#17 walk*:ti,ab,kw
#18 inactiv*:ti,ab,kw
#19 sit‐stand desk:ti,ab,kw
#20 sit stand desk:ti,ab,kw
#21 sit‐stand workstation:ti,ab,kw
#22 sit stand workstation:ti,ab,kw
#23 "workstation":ti,ab,kw
#24 "pedometer":ti,ab,kw
#25 wearable device:ti,ab,kw
#26 "worksite":ti,ab,kw
#27 #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26
#28 #14 and #27
#29 #28 and trials
Appendix 2. CINAHL search strategy
S5 S3 AND S4
S4 S1 AND S2
S3 TX sit OR TX sitting OR TX sitting posture OR TX walk* OR TX ( sit‐stand desk or sit‐stand workstation or sit stand desk or sit stand workstation or adjustable workstation or adjustable desk ) OR TX ( pedometer‐based intervention or pedometer intervention ) OR TX wearable devices OR TX worksite health promotion Limiters ‐ Exclude MEDLINE records; Human
S2 TX musculoskeletal OR TX musculoskeletal disorders OR TX low back pain OR TX lumbar pain OR TX ( lbp or low back pain or nonspecific low back pain ) OR TX ( neck pain or cervical pain ) OR TX ( musculoskeletal pain or dysfunction ) Limiters ‐ Exclude MEDLINE records; Human Limiters ‐ Exclude MEDLINE records; Human
S1 TX workplace OR TX job OR TX vocation OR TX office work* OR TX office workers OR TX sedentary lifestyle OR TX ( sedentary behaviour or sedentary behavior or sedentary time or sedentariness or sedentary lifestyle or physical inactivity or sitting ) OR TX sedentary workplace OR TX ( "sedntary worker" or "office worker" ) Limiters ‐ Exclude MEDLINE records; Human
Appendix 3. Embase search strategy
#1 office worker/ or worker.mp. or worker/ or white collar worker/
#2 occupation/ or vocation/
#3 job.mp.
#4 sedentary lifestyle/ or sedentary.mp.
#5 sedentary behavior.mp.
#6 sedentary behaviour.mp.
#7 1 or 2 or 3 or 4 or 5 or 6
#8 musculoskeletal pain.mp. or musculoskeletal pain/ or musculoskeletal disease/ or musculoskeletal.mp.
#9 back pain.mp. or backache/
#10 low back pain.mp. or low back pain/
#11 lumbar pain.mp.
#12 neck pain.mp. or neck pain/
#13 8 or 9 or 10 or 11 or 12
#14 7 and 13
#15 sit.mp.
#16 sitting.mp. or body posture/ or sitting/
#17 walking/ or walk*.mp.
#18 inactiv*.mp.
#19 sit‐stand desk*.mp.
#20 sit stand desk*.mp.
#21 sit‐stand workstation*.mp.
#22 sit stand workstation*.mp.
#23 workstation*.mp. or ergonomics/
#24 pedometer/ or pedometer*.mp.
#25 wearable device*.mp.
#26 worksite*.mp.
#27 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26
#28 14 and 27
#29 limit 28 to human
Appendix 4. MEDLINE search strategy
#1 Workplace/ or worker.mp.
#2 vocation.mp.
#3 job.mp.
#4 office.mp.
#5 Sedentary Lifestyle/ or sedentary.mp.
#6 occupational diseases.mp. or Occupational Diseases/
#7 Occupations/ or occupation*.mp.
#8 sedentary behaviour.mp.
#9 sedentary behavior.mp.
#10 ("office worker" or "sedentary worker").tw.
#11 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10
#12 Musculoskeletal Diseases/ or musculoskeletal pain.mp. or Musculoskeletal Pain/ or musculoskeletal.mp
#13 back pain.mp. or Back Pain/
#14 low back pain.mp. or Low Back Pain/
#15 lumbar pain.mp.
#16 neck pain.mp. or Neck Pain/
#17 12 or 13 or 14 or 15 or 16
#18 11 and 17
#19 sit.mp.
#20. Posture/ or sitting.mp.
#21 walk*.mp.
#22 inactiv*.mp.
#23 sit‐stand desk*.mp.
#24 sit stand desk*.mp.
#25 sit‐stand workstation*.mp.
#26 sit stand workstation*.mp.
#27 workstation*.mp.
#28 pedometer*.mp.
#29 wearable device*.mp.
#30 worksite*.mp.
#31 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30
#32 18 and 31
#33 limit 32 to humans
Appendix 5. OSH Update search strategy
#1 GW sedentary lifestyle
#2 GW sedentary
#3 GW office worker
#4 GW sedentary worker
#5 GW sedentary behaviour
#6 GW sedentary behavior
#7 #1 or #2 or #3 or # or 5 or #6
#8 GW musculoskeletal pain
#9 GW low back pain
#10 GW back pain
#11 GW lumbar pain
#12 GW neck pain
#13 #8 or #9 or #10 or #11 or #12
#14 #7 and #13
#15 GW sit*
#16 GW walk*
#17 GW sit‐stand desk*
#18 GW sit stand desk*
#19 GW sit‐stand workstation*
#20 GW sit stand workstation*
#21 GW pedometer*
#22 GW wearable device
#23 #15 or #16 or #17 or #18 or #18 or #19 or #20 or #21 or #22
#23 #14 and #23
Appendix 6. PEDro search strategy
Abstract & title: stand; Problem: pain AND Method: clinical trial
Appendix 7. ClinicalTrials.gov
Workplace AND Sedentary
Appendix 8. World Health Organization (WHO) International Trials Registry Platform (ICTRP) search portal
Workplace AND Sedentary
Data and analyses
Comparison 1. Sit‐stand desk versus no intervention.
Comparison 2. Treadmill workstation versus no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Proportion of participants with low back pain/discomfort follow‐up short‐term | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Proportion of participants with upper back pain/discomfort follow‐up short‐term | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Proportion of participants with neck pain/discomfort follow‐up short‐term | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Proportion of participants with shoulder pain/discomfort follow‐up short‐term | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5 Proportion of participants with elbow/wrist/hand pain/discomfort follow‐up short‐term | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6 Proportion of participants with knee pain/discomfort follow‐up short‐term | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 3. Activity tracker versus alternate intervention or no intervention.
Comparison 4. Multi‐component intervention versus no intervention.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Alkhajah 2012.
| Methods |
Study design: controlled before‐and‐after trial Study duration: 3 months Dropout: 6% of all participants (0 to 18 in intervention group and 2 to 15 in control group); no specific information provided about participants with baseline musculoskeletal symptoms Location: Australia Recruitment: 2 academic institutions in Brisbane; to reduce contamination, participants in the comparison group were separated from intervention participants by at least 1 building level |
|
| Participants |
Population: office workers Intervention group: 18 participants (total) with 0 to 7 participants with baseline pain Control group: 15 participants (total) with 0 to 4 participants with baseline pain Included criteria: between 20 and 65 years of age with a non‐adjustable workstation and a desktop computer Excluded criteria: non‐ambulatory, pregnant at baseline, working less than 0.5 full‐time equivalent, planned relocation to another work site within 3 months Baseline characteristics: imbalance in the proportion of participants in intervention and control groups that reported baseline musculoskeletal symptoms |
|
| Interventions |
Intervention
Control
|
|
| Outcomes |
Outcome name, measurement tool, body region
|
|
| Identification | ||
| Notes | Sponsorship source: nil relevant reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Counfounding CBA | High risk | Quote: "the sample is not widely representative of workplaces and workers, and some confounding is possible. Further, models adjusted for baseline levels but not for other potential confounders because of insuffıcient sample size" Judgement comment: due to the small sample size in this study, adjustment for potential confounders was not possible |
| Selection Bias CBA | Low risk | Judgement comment: intervention and control participants were recruited from the same organisation and over the same time period |
| Blinding of participants and personnel | High risk | Judgement comment: due to the nature of the intervention of a sit‐stand workstation provided, it would not have been possible to blind researchers or participants from the intervention |
| Blinding of outcome assessment | Unclear risk | Judgement comment: in this study, musculoskeletal outcomes were a secondary outcome, so it is unclear whether the fact that participants were not blinded to the intervention would contribute to bias in self‐reporting of musculoskeletal outcomes |
| Incomplete outcome data | Low risk | Judgement comment: only 1 participant in the control group was excluded from analyses due to monitor malfunction |
| Selective reporting | Unclear risk | Judgement comment: all outcomes were reported in the paper, but there was no published protocol for the study, so it is not possible to determine if additional outcomes were proposed that were not reported |
| Baseline imbalance | High risk | Judgement comment: there were considerable differences in baseline symptoms for some body regions (e.g. neck, shoulder) |
Brakenridge 2016.
| Methods |
Study design: cluster‐randomised controlled trial Study duration: 12 months Dropout: 55% (baseline pain participants) Location: Australia Recruitment: 1 large Australian organisation with offices around the country. Participants attended an information session and were invited to participate in the study |
|
| Participants |
Population: office workers from a private organisation with mean age of 23 to 58 years Intervention group: 66 participants (total) with 2 to 22 participants with baseline pain Control group: 87 participants (total) with 5 to 32 participants with baseline pain Included criteria: working at study locations or working nearby or visiting a location regularly; working 50% or more than full‐time equivalent, able to walk 10 m Excluded criteria: pregnant at baseline, allergies to adhesive tape, planned absence from work for longer than 2 weeks during the first 3‐month study period, having an activity permissive workstation at baseline assessment Baseline characteristics: at baseline, the control group had a higher proportion of males, senior leaders, and overweight participants. This group also had fewer managers and reported more lower extremity musculoskeletal problems when compared to the intervention group. Baseline activity levels between groups were comparable |
|
| Interventions |
Intervention
Control
|
|
| Outcomes |
Outcome name, measurement tool, body region
|
|
| Identification | ||
| Notes | Sponsorship source: the National Heart Foundation of Australia; the Office Ergonomics Research Committee (OERC); the National Health and Medical Research Council (NHMRC) of Australia; Australian Postgraduate Award; the Victorian Government’s Operational Infrastructure Support Program; Lendlease | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Unclear risk | Quote: "randomisation occurred after the final list of team managers for each location had been obtained and prior to the staff information session and baseline assessment. A university staff member not involved in the study randomised teams by strata (location B/small location A teams/large location A teams) to either Group ORG or Group ORG + Tracker, using a randomisation website" Judgement comment: randomisation (at cluster level) was performed by a researcher not involved in the study using a randomisation website. Although the overall randomisation procedure was low risk, as only a select group of participants with baseline pain were included in the review, the randomisation was compromised |
| Allocation concealment | Low risk | Judgement comment: randomisation occurred after the final list of team managers for each location had been obtained and before the staff information session and baseline assessment. A research team member informed the champion of the allocation. Randomisation was conducted by a staff member not involved in the study using a randomisation website (third party) to conceal allocation; then a research team member applied the randomisation schedule to the list of teams |
| Blinding of participants and personnel | High risk | Judgement comment: due to the nature of the intervention of workplace support with and without an activity tracker, it would not have been possible to blind researchers or participants from the intervention |
| Blinding of outcome assessment | Unclear risk | Judgement comment: in this study, musculoskeletal outcomes were a secondary outcome, so it is unclear whether the fact that participants were not blinded to the intervention would contribute to bias in self‐reporting of musculoskeletal outcomes |
| Incomplete outcome data | High risk | Judgement comment: loss to follow‐up was substantial (e.g. 13/30 in the control group and 18/26 in the intervention group for the neck pain outcome measure). Although missing data were imputed by chained equations, it is unclear whether musculoskeletal data were imputed, as the primary outcome in this review was only a secondary outcome in the study; it appears that no further analyses were conducted |
| Selective reporting | Low risk | Judgement comment: outcomes reported are consistent with the published protocol; (upon request) study authors provided results of all musculoskeletal outcomes measured |
| Baseline imbalance | Low risk | Judgement comment: although some baseline imbalances were reported, analyses were adjusted for potential confounders |
Danquah 2017.
| Methods |
Study design: cluster‐randomised controlled trial Study duration: 3 months Dropout: 11% of all participants, but no specific information provided about participants with baseline musculoskeletal symptoms Location: Denmark Recruitment: recruited through a press release and an open invitation in an electronic newsletter aimed at practitioners and health workers in municipalities and private workplaces all over Denmark |
|
| Participants |
Population: practitioners and health workers in municipalities and private workplaces all over Denmark
Intervention group: 173 (total) with 50 to 76 participants with baseline pain recruited from 10 offices
Control group: 144 (total) with 50 to 64 participants with baseline pain from 9 offices Included criteria: office‐based workplaces with employees who were sitting for most of the day. Each workplace was required to have at least 4 offices, divided by walls, floors, or locations (minimise contamination between groups) to act as clusters. To be included, workers from each workplace could not take part in collaborative activities. Management needed to agree to participate in the activities and to provide necessary resources for the study such as sit‐stand desks. Individuals who agreed to participate needed to be over 18 years of age, to understand Danish, and to work more than 4 days per week (> 30 hours) Excluded criteria: sickness or disability that prevented standing or walking, pregnancy Baseline characteristics: no major differences in participant characteristics or in sitting at baseline were reported between groups |
|
| Interventions |
Intervention
Control
|
|
| Outcomes |
Outcome name, measurement tool, body region
|
|
| Identification | ||
| Notes | Sponsorship source: supported by Tryg Fonden, Denmark. Sponsors had no role in study design, data collection or analysis, decision to publish, or preparation of the manuscript | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Unclear risk | Quote: "a senior researcher carried out the randomization blinded, using random number sequence in Stata (13.1)" Judgement comment: randomisation at each workplace was carried out by a senior researcher using a random sequence generator. Although the overall randomisation procedure was low risk, as only a select group of participants with baseline pain were included in the review, randomisation was compromised |
| Allocation concealment | Low risk | Judgement comment: randomisation took place before baseline measurements by a blinded researcher. Allocation was not disclosed to participants, researchers, or data collectors until after baseline measurements were complete |
| Blinding of participants and personnel | High risk | Judgement comment: participants and/or researchers were not blinded. Although attempts were made to physically separate clusters within the workplace, it is unlikely that participants would not be aware of their allocation. It would not be possible to blind research personnel due to the nature of the intervention |
| Blinding of outcome assessment | Unclear risk | Judgement comment: a blinded version of the data was used for data management and analysis. However, in this study, musculoskeletal outcomes were a secondary outcome, so it is unclear whether the fact that participants were not blinded to the intervention would contribute to bias in self‐reporting of musculoskeletal outcomes |
| Incomplete outcome data | Unclear risk | Judgement comment: at first follow‐up, 16/123 in the control group were lost to follow‐up and 14/156 in the intervention group. Attrition was balanced between groups, but it is unclear whether other factors may have contributed to attrition. Although missing data were imputed by multiple imputations using chained equations, it is unclear whether musculoskeletal data were imputed and to what extent |
| Selective reporting | Low risk | Judgement comment: all outcomes reported were reported at trial registration, and no outcomes in the trial registration were omitted |
| Baseline imbalance | Unclear risk | Judgement comment: details from full group baseline factors, not only pain; no baseline sitting behaviour reported |
Edwardson 2018.
| Methods |
Study design: cluster‐randomised controlled trial Study duration: 12 months Dropout: 25% at 12 months (all participants) Location: UK Recruitment: team managers and staff from 3 hospitals across Leiscester, as part of the University Hospitals of Leicester NHS Trust, were approached to participate in the study. Recruitment also took place through intranet online advertisements, e‐newsletters, and posters |
|
| Participants |
Population: office workers as self‐reported and later confirmed by site visit Intervention group: 19 clusters with 77 participants (whole group), 12 to 50 with baseline pain Control group: 18 clusters with 69 participants (whole group), 14 to 44 with baseline pain Included criteria: 18 to 70 years of age, office‐based, spent ≥ 75% of the workday sitting, worked 0.6 full‐time equivalent, worked at the same desk for at least 3 days/week, capable of standing Excluded criteria: not reported Baseline characteristics: for the whole group, baseline characteristics were similar between intervention and control groups, except for ethnicity. Physical activity, sitting, and standing were similar between groups. Baseline characteristics for participants with baseline pain not available |
|
| Interventions |
Intervention
Control
|
|
| Outcomes |
Outcome name, measurement tool, body region
|
|
| Identification | ||
| Notes | Sponsorship source: nil relevant | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Unclear risk | Quote: "using computer generated lists, a statistician randomised office groups (clusters) 1:1 to either intervention or control group stratified by cluster size (≤4 and >4 participants) with a block size of six. Randomisation was performed in batches after participant clusters had completed their baseline measures" Judgement comment: randomisation at the office group level was carried out by a statistician using computer‐generated lists. Although the overall randomisation procedure was low risk, as only a select group of participants with baseline pain were included in the review, randomisation was compromised |
| Allocation concealment | Unclear risk | Judgement comment: it is not stated whether allocation was concealed |
| Blinding of participants and personnel | High risk | Quote: "randomisation occurred at the office group level to reduce the risk of contamination" Quote: "the team leads could not be blinded as they were responsible for study coordination, including delivery of the desks and intervention components. Team leads had no involvement in data processing and analysis" Judgement comment: participants and/or researchers were not blinded. Although attempts were made to physically separate clusters within the workplace, it is unlikely that participants would not be aware of their allocation. It would not be possible to blind research personnel due to the nature of the intervention |
| Blinding of outcome assessment | Unclear risk | Quote: "team members who took measurements were blinded to group randomisation" Judgement comment: team leads were not not involved with data processing or analysis, and it is stated that team members who took measurements were blinded to group allocation but is not stated whether there was blinding of outcome assessors for all outcome measures. In addition, in this study, musculoskeletal outcomes were a secondary outcome, so it unclear whether the fact that participants were not blinded to the intervention would contribute to bias in self‐reporting of musculoskeletal outcomes |
| Incomplete outcome data | Unclear risk | Judgement comment: for the whole cohort ‐ at 3‐month follow‐up, 52/69 in the control group were lost to follow‐up and 69/77 in the intervention group; at 6‐month follow‐up, 50/69 in the control group were lost to follow‐up and 65/77 in the intervention group; and at 12‐month follow‐up, 46/69 in the control group were lost to follow‐up and 63/77 in the intervention group. Attrition was greater in the control group (33%) than in the intervention group (17%). Attrition details were not provided for participants with baseline pain |
| Selective reporting | Low risk | Judgement comment: all outcomes reported were reported at trial registration, and no outcomes in the trial registration were omitted |
| Baseline imbalance | Unclear risk | Judgement comment: some differences in baseline symptoms were noted for some body regions (e.g. neck, shoulder) |
Gibbs 2018.
| Methods |
Study design: randomised controlled trial Study duration: 6 months Dropout: 3% at 1 month Location: USA Recruitment: via fliers, University‐based electronic mailings and University of Pittsburgh research registries |
|
| Participants |
Population: office employees from the greater Pittsburgh area working at least 20 hours per week at a desk Intervention group: 13 participants, all with baseline pain Control group: 14 participants, all with baseline pain Included criteria: chronic LBP defined as persistent pain for at least 3 months resulting in pain on more than half the days over the last 6 months; LBP disability as defined by an Oswestry Diability Index > 10%; current desk work ≥ 20 hours/week; stable employment; approval from supervisor to participate and install a desk attachment, Internet access to complete questionnaires Excluded criteria: not providing informed consent; cardiovascular event in the last 6 months; comorbidity that limited ability to reduce sedentary behaviour; recent or planned back surgery; symptoms consistent with more serious spinal condition; currently using a height‐adjustable/standing workstation; currently planning to get pregnant; blood pressure ≥ 160/100 mmHg Baseline characteristics: intervention group participated in more occupational MVPA than control group, but overall MVPA was consistent between groups. Education level was higher in the control group, so group comparisons were adjusted for education |
|
| Interventions |
Intervention
Control
|
|
| Outcomes |
Outcome name, measurement tool, body region
|
|
| Identification | ||
| Notes | Sponsorship source: nil relevant | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Low risk | Judgement comment: randomisation was done using sealed envelopes in blocks of 4 participants |
| Allocation concealment | Low risk | Judgement comment: randomisation was done using sealed envelopes in blocks of 4 participants |
| Blinding of participants and personnel | High risk | Quote: "most participants worked in separate locations, with the exception of some university employees working on the same floor of a building (one cluster of 2; one cluster of 3); the investigators asked these participants not to discuss the study among each other to limit contamination" Judgement comment: attempts were made to avoid contamination between intervention and control participants, but blinding was not possible |
| Blinding of outcome assessment | High risk | Judgement comment: physical function measured by blinded researcher but for the other outcome assessment, blinding of outcome personnel not reported. In addition, as self‐reported musculoskeletal symptoms was the primary outcome measure and participants were not blinded to the intervention, risk of bias is high |
| Incomplete outcome data | Low risk | Judgement comment: 1 intervention participant withdrew after 1 month for personal reasons. One control participant withdrew at 2 months for personal reasons, and 1 control participant withdrew due to extended work leave for a medical procedure unrelated to LBP. Completion rate of monthly assessment questionnaires was 93%. Sensitivity analysis between completers only; reported data were similar |
| Selective reporting | Low risk | Judgement comment: all pain and disability data were reported according to the protocol in the trial registry |
| Baseline imbalance | Low risk | Judgement comment: there was baseline imbalance for education between intervention groups. Analyses were subsequently adjusted for education |
Graves 2015.
| Methods |
Study design: randomised controlled trial Study duration: 8 weeks Dropout: 4% Location: UK Recruitment: consent was sought from 11 departmental managers for employee recruitment. All employees in consenting departments received an overview of the study and a participant information sheet, and all were invited to a study information session via an email from the research team |
|
| Participants |
Population: office workers from 1 organisation (Liverpool John Moores University, Liverpool, UK). Employees within the approached departments were predominantly administrative staff
Intervention group: 26 participants (total) with 16 to 18 participants with baseline pain
Control group: 21 participants (total) with 9 to 15 participants with baseline pain Included criteria: office workers from 1 organisation (predominantly administrative staff from a university). Full‐time members of staff with access to a work telephone or a desktop computer were included Excluded criteria: cardiovascular or metabolic disease, taking medication, pregnant, planning absence > 1 week during the trial Baseline characteristics: baseline group differences were not statistically tested for. However, some differences were noted, such as more females and participants with a tertiary education in the intervention group compared to the control group |
|
| Interventions |
Intervention
Control
|
|
| Outcomes |
Outcome name, measurement tool, body region
|
|
| Identification | ||
| Notes | Sponsorship source: Ergotron Ltd (www.ergotron.com) provided sit‐stand workstations for the present study. Ergotron had no involvement or influence on the provenance, commissioning, conduct, or findings of the study. No other financial disclosures were reported by the authors of this paper | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Unclear risk | Judgement comment: following baseline assessments, participants were assigned by a member of the research team to a treatment arm using a randomised block design and a random numbers table. Departments served as blocks, and participants within departments were randomly assigned at the individual level. Assignment of individual participants within each department alternated between arms. Although the overall randomisation procedure was low risk, as only a select group of participants with baseline pain were included in the review, randomisation was compromised |
| Allocation concealment | Unclear risk | Judgement comment: although it states that 1 member of the research team performed the randomisation, it is not stated whether there was allocation concealment |
| Blinding of participants and personnel | High risk | Judgement comment: it appears that within each department, some participants were using the sit‐stand workstations and others were not, so blinding of participants and personnel was not possible |
| Blinding of outcome assessment | Unclear risk | Judgement comment: in this study, musculoskeletal outcomes were a secondary outcome, so it is unclear whether the fact that participants were not blinded to the intervention would contribute to bias in self‐reporting of musculoskeletal outcomes |
| Incomplete outcome data | Low risk | Judgement comment: 47 participants were randomised; 46 completed the intervention (25 intervention; 21 control), and all participants who provided data for musculoskeletal outcomes completed the study |
| Selective reporting | Low risk | Judgement comment: outcomes reported are consistent with clinical trial registration |
| Baseline imbalance | Unclear risk | Judgement comment: gender imbalance between groups was noted. No adjustments were made in the analyses |
Healy 2013.
| Methods | Study design: non‐random allocation by clusters (floor): CBA, unblinded Study duration: 3 months Dropout: 12% at 3 months (all participants) Location: Melbourne, Australia Recruitment: an invitation email was sent to all potential participants to attend one of two 30‐minute study information sessions delivered by research staff. Participants who subsequently expressed interest were screened via telephone for eligibility | |
| Participants |
Population: office workers from a single workplace (Comcare: the government agency responsible for workplace safety, rehabilitation, and compensation for Australian government workplaces) in metropolitan Melbourne, Australia
Intervention group: 19 participants (whole group), 2 to 9 with baseline pain
Control group: 19 participants (whole group), 1 to 13 with baseline pain Included criteria: required to work at least 0.6 full‐time equivalent; 18 to 65 years of age; ability to speak English; access to telephone, Internet, and dedicated desk at the workplace Excluded criteria: pregnant, non‐ambulatory, planned absence from work for longer than 1 week during the intervention period, no pre‐existing musculoskeletal disorder Baseline characteristics: imbalance in the proportion of participants in intervention and control groups who reported baseline musculoskeletal symptoms |
|
| Interventions |
Intervention
Control
|
|
| Outcomes |
Outcome name, measurement tool, body region
|
|
| Identification | ||
| Notes | This study was funded by an NHMRC project grant and the Victorian Health Promotion Foundation. Ergotron provided height‐adjustable desks (www.ergotron.com). No financial disclosures were reported by study authors, and they declared that there were no conflicts of interest | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Counfounding CBA | Unclear risk | Quote: "although we adjusted for baseline values and tested for confounding, unmeasured confounders may have affected the results" Judgement comment: there may have been influence from confounders that were not identified |
| Selection Bias CBA | Low risk | Judgement comment: intervention and control participants were recruited from the same organisation and over the same time period |
| Blinding of participants and personnel | High risk | Quote: "research staff, participants, and assessors were not blinded to group allocation" |
| Blinding of outcome assessment | Unclear risk | Quote: "research staff, participants, and assessors were not blind to group allocation" Judgement comment: in addition, for this study, musculoskeletal outcomes were a secondary outcome, so it is unclear whether the fact that participants were not blinded to the intervention would contribute to bias in self‐reporting of musculoskeletal outcomes |
| Incomplete outcome data | Unclear risk | Judgement comment: for the whole cohort ‐ at 4‐week follow‐up, 3/22 in the intervention group were lost to follow‐up and 2/21 in the control group. Attrition was greater in the intervention group (14%) than in the control group (10%). Attrition details for participants with baseline pain were not provided |
| Selective reporting | Unclear risk | Judgement comment: the study was not registered as a clinical trial, and there is protocol for comparison. However, all outcomes listed in the methods are reported in the paper |
| Baseline imbalance | High risk | Judgement comment: Differences in baseline symptoms were considerable for some body regions (e.g. neck, shoulder) |
Healy 2016.
| Methods |
Study design: cluster‐randomised controlled trial Study duration: 12 months Dropout: 18% at 12 months (all participants) Location: 1 government organisation at various work sites in metropolitan and regional Victoria, Australia Recruitment: sites were identified if they were geographically separate (≥ 1 km apart) from other sites in the same organisation. At each site, a team was formed that included a working group and a line manager; the team met on a regular basis |
|
| Participants |
Population: office workers working in the organisation Intervention group: 136 participants with 12 to 54 participants with baseline pain in 1 or more body regions Control group: 95 participants with 4 to 37 participants with baseline pain in 1 or more body regions Included criteria: required to work at least 0.6 full‐time equivalent; 18 to 65 years of age; ability to speak English; access to telephone, Internet, and dedicated desk at the workplace Excluded criteria: pregnant, non‐ambulatory, planned absence from work for longer than 2 weeks, planned relocation to another work site within the first 3 months of the intervention Baseline characteristics: approximately equal proportions of participants in intervention and control groups reported baseline musculoskeletal symptoms |
|
| Interventions |
Intervention
Control
|
|
| Outcomes |
Outcome name, measurement tool, body region
|
|
| Identification | ||
| Notes | Sponsorship source: Ergotron Ltd (www.ergotron.com) provided sit‐stand workstations for the present study. Ergotron had no influence on the conduct or findings of the study | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Unclear risk | Quote: "randomization to either the intervention or the control arms of the trial was at the level of the work site via simple cluster randomization. This was achieved by generating a randomization plan for up to 24 clusters in one block (www.randomization.com)" Judgement comment: although the overall randomisation procedure was low risk, as only a select group of participants with baseline pain were included in the review, randomisation was compromised |
| Allocation concealment | Low risk | Quote: "this was achieved by generating a randomization plan for up to 24 clusters in one block (www.randomization.com) by a research staff member not involved in recruitment or data collection" |
| Blinding of participants and personnel | High risk | Quote: "participants and study staff were unblinded to group allocation" |
| Blinding of outcome assessment | Unclear risk | Judgement comment: in addition, for this study, musculoskeletal outcomes were a secondary outcome, so it is unclear whether the fact that participants were not blinded to the intervention would contribute to bias in self‐reporting of musculoskeletal outcomes |
| Incomplete outcome data | Unclear risk | Judgement comment: for the whole cohort ‐ at 3‐month follow‐up, 7/136 in the intervention group were lost to follow‐up and 5/95 in the control group; at 12‐month follow‐up, 22/136 in the intervention group were lost to follow‐up and 20/95 in the intervention group. Attrition was greater in the control group (31%) than in the intervention group (16%). Attrition details for participants with baseline pain were not provided |
| Selective reporting | Low risk | Judgement comment: outcomes reported are consistent with the clinical trial registration. However, the full list of outcomes is reported elsewhere (Healy 2017) |
| Baseline imbalance | Low risk | Judgement comment: appears to be equal balance of participants with baseline pain in intervention and control groups |
Ognibene 2016.
| Methods |
Study design: cluster‐randomised controlled trial Study duration: 3 months Dropout: 19% Location: USA Recruitment: recruitment details were not specified |
|
| Participants |
Population: University employees Intervention group: 25 participants, all with baseline pain Control group: 21 participants, all with baseline pain Included criteria: University employees 18 years of age or older who spent at least 6 hours of an 8‐hour day sitting at a computer desk and reported at least a 4/10 level of back pain that had lasted a minimum of 3 months Excluded criteria: physically incapable of standing for at least 10 minutes, already using a sit‐stand workstation Baseline characteristics: appeared to be some minor baseline differences between intervention and control groups ‐ median length of time with low back pain and upper back pain was greater in the intervention group; baseline worst LBP score was greater in the intervention group; more people undergoing treatment(s) in the intervention group than in the control group |
|
| Interventions |
Intervention
Control
|
|
| Outcomes |
Outcome name, measurement tool, body region
|
|
| Identification | ||
| Notes | Sponsorship source: Ergotron provided sit‐stand computer workstations for study participants | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Low risk | Quote: "participants who met eligibility criteria were randomized using block methodology, specifically the ‘‘blockrand’’ package in R (R Version 3.0.0), 29 to either receive a SSW after 2 weeks of baseline surveys (intervention group) or at the conclusion of the 12‐week active period of the study (control group)" Judgement comment: suitable computer programme to provide block randomisation |
| Allocation concealment | Unclear risk | Judgement comment: it is not stated whether allocation was concealed or who conducted the randomisation |
| Blinding of participants and personnel | High risk | Judgement comment: participants were not blinded and the study did not state whether any attempts were made to isolate participants from intervention and control groups to mitigate contamination. It would not be possible to blind research personnel |
| Blinding of outcome assessment | High risk | Judgement comment: as self‐reported musculoskeletal symptoms were the primary outcome measure and participants were not blinded to the intervention, risk of bias is high |
| Incomplete outcome data | Unclear risk | Judgement comment: it is stated that 11 participants dropped out of the study (19%), but it is unclear whether participants left the study during the course of the study or before the start of the study. Further, no reasons are provided as to why participants withdrew from the study. Analysis appears to have included only those who completed the study |
| Selective reporting | Low risk | Judgement comment: all outcomes in the protocol described in the trial registry were reported. All measured outcomes appeared to be reported |
| Baseline imbalance | Unclear risk | Judgement comment: There appeared to be some baseline imbalance with respect to length of time with low back pain. Analyses did not adjust for baseline imbalances. Baseline pain scores were slightly higher in the intervention group |
Parry 2015.
| Methods |
Study design: cluster‐randomised controlled trial Study duration: 3 months Dropout: 50% in primary study; unclear how many with baseline pain dropped out Location: Australia Recruitment: recruitment meetings were held at suburban branches of 3 large government organisations |
|
| Participants |
Population: office workers (clerical, data entry, and call centre workers) from 3 government organisations in Perth, Western Australia Intervention group: 1 to 18 with baseline pain Control group: 1 to 11 with baseline pain Included criteria: office workers (clerical, call centre, and data processing) from 3 large government organisations Excluded criteria: inability to wear an accelerometer due to disability, wheelchair bound Baseline characteristics: information related to participants with baseline pain was not available |
|
| Interventions |
Intervention Active office
Traditional physical activity
Control
|
|
| Outcomes |
Outcome name, measurement tool, body region
|
|
| Identification | ||
| Notes |
Sponsorship source: 1 study author was supported by an Australian National Health and Medical Research Council Fellowship Comments: this is an analysis of secondary outcomes from a larger study examining workplace interventions to reduce sedentary time and promote light and moderate/vigorous physical activity. Full details of the study can be found at the following source: Parry S, Straker L, Gilson ND, Smith AJ (2013). Participatory workplace interventions can reduce sedentary time for office workers ‐ a randomised controlled trial. PLoS ONE 8(11), e78957 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation | Unclear risk | Quote: "self‐reported musculoskeletal symptoms. Methods: a randomised controlled trial was conducted with office workers (clerical, call centre and data processing; n = 63, aged 35–59 years) from three large government organisations in Perth, Australia. Three intervention groups were developed" Judgement comment: further description of the randomisation process was provided in the primary paper related to this smaller secondary analysis conference presentation. Randomisation is described as follows: "a parallel arms clustered randomised control" (Parry et al, 2013). Further, "simple randomisation with a 1:1:1 allocation ratio was used by drawing a sealed envelope containing allocation from a hat" (Parry et al, 2013). Although the overall randomisation procedure was low risk, as only a select group of participants with baseline pain were included in the review, randomisation was compromised |
| Allocation concealment | Low risk | Judgement comment: primary paper for this study states: "simple randomisation with a 1:1:1 allocation ratio was used by drawing a sealed envelope containing allocation from a hat" (Parry et al, 2013) |
| Blinding of participants and personnel | High risk | Judgement comment: no information on blinding is provided. It is likely though that participants and researchers were aware of the allocation |
| Blinding of outcome assessment | High risk | Judgement comment: primary paper states: "the researcher with primary responsibility for collection and analysis of accelerometer data (SP) had conducted the interventions and was not blinded to group allocation" (Parry et al, 2013). In addition, for this study, musculoskeletal outcomes were a secondary outcome, so it is unclear whether the fact that participants were not blinded to the intervention would contribute to bias in self‐reporting of musculoskeletal outcomes |
| Incomplete outcome data | High risk | Judgement comment: from the primary paper, 133 participants were randomised, but only 63 participants completed the study. Incompleteness of data for some outcomes was considerable (e.g. with only 5, 10, and 6 participants in the analysis of hip, knee, and ankle, respectively) |
| Selective reporting | Low risk | Judgement comment: this current study reported only 1 outcome from a larger registered trial. The pain outcome was listed as an outcome in the trial registry |
| Baseline imbalance | High risk | Judgement comment: differences in baseline symptoms for some body regions (e.g. neck) were considerable |
BMI: body mass index.
BREF: generic quality of life scale developed by WHO.
CBA: controlled before‐and‐after.
EMA: ecological momentary assessment.
LBP: low back pain.
MVPA: moderate to vigorous physical activity.
ODI: Oswestry Disability Index.
RMDQ: Roland Morris Low Back Pain and Disability Questionnaire.
VAS: visual analog scale.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aghilinejad 2014 | Wrong patient population |
| Andersen 2010 | Wrong intervention |
| Baker 2013 | Wrong study design |
| Bergman 2018 | Wrong population |
| Bernaards 2006 | Wrong intervention |
| Bernaards 2008 | Wrong intervention |
| Bernaards 2011 | Wrong intervention |
| Blangsted 2008 | Wrong intervention |
| Blasche 2013 | Wrong intervention |
| Brendbekken 2016 | Wrong intervention |
| Carr 2013 | Wrong intervention |
| Carr 2016 | Wrong intervention |
| Castagnoli 2015 | Wrong intervention |
| Chung 2009 | Wrong study design |
| Cristancho 2012 | Wrong study design |
| Curwin 2013 | Wrong study design |
| Dahl 2001 | Wrong patient population |
| delPozo Cruz 2012 | Wrong intervention |
| delPozo Cruz 2013 | Wrong intervention |
| Denis 2012 | Wrong intervention |
| Doda 2015 | Wrong intervention |
| Driessen 2011 | Wrong intervention |
| Dugan 2006 | Wrong study design |
| Ebara 2008 | Wrong study design |
| Engelen 2014 | Wrong study design |
| Esmaeilzadeh 2014 | Wrong intervention |
| Estabrooks 2011 | Wrong intervention |
| Fazioli 2004 | Wrong intervention |
| Fewster 2017 | Wrong study design |
| Gao 2016 | Wrong patient population ‐ mixture of participants with and without baseline pain |
| Gerr 2005 | Wrong intervention |
| Grunseit 2012 | Wrong study design |
| Hillsdon 2002 | Wrong intervention |
| Husemann 2009 | Wrong intervention |
| Irmak 2012 | Wrong intervention |
| Jay 2014 | Wrong study design |
| Jay 2015 | Wrong intervention |
| Jay 2016 | Wrong intervention |
| Kilpikoski 2009 | Wrong intervention |
| Kline 2017 | Wrong outcome |
| Levanon 2012 | Wrong intervention |
| Levanon 2012a | Wrong intervention |
| Loisel 1997 | Wrong intervention |
| Mackey 2011 | Wrong study design |
| McDonough 2011 | Wrong setting |
| Mills 2011 | Wrong setting |
| Pedersen 2009 | Wrong intervention |
| Phattharasupharerk 2018 | Wrong intervention |
| Pozo Cruz 2012 | Wrong intervention |
| Robertson 2008 | Wrong intervention |
| Robertson 2013 | Wrong intervention |
| Robertson 2017 | Wrong study design |
| Roemmich 2014 | Wrong intervention |
| Shnayderman 2013 | Wrong setting |
| Sihawong 2014 | Wrong intervention |
| Sjogaard 2012 | Wrong intervention |
| Spekle 2010 | Wrong intervention |
| Suni 2017 | Wrong intervention |
| Szeto 2015 | Wrong intervention |
| Thorp 2014 | Wrong intervention |
| Tronarp 2018 | Wrong study design |
| vanSluijs 2005 | Wrong patient population |
| Wang 2014 | Wrong study design |
| Wollesen 2017 | Wrong study design |
Characteristics of studies awaiting assessment [ordered by study ID]
Neuhaus 2014.
| Methods |
Study design: allocation by clusters, 2 groups randomly and 2 groups non‐randomly: CBA Study duration: 3 months Dropout: 10% at 3 months (all participants). Location: University of Queensland, Brisbane, Australia Recruitment: 3 sites on different campuses. A recruitment email was sent to all staff in the units |
| Participants |
Population: office workers located on the same office floor
Intervention group: 16 participants multi‐component (whole group); 14 participants workstation only (whole group)
Control group: 14 participants (whole group) Included criteria: 18 to 65 years of age, able to speak English, ambulatory and working at least 0.5 full‐time equivalent Excluded criteria: pregnancy, allergies to medical tape (used to attach the activity monitor), planned absence from work for longer than 1 week during intervention period, no pre‐existing musculoskeletal disorder Baseline characteristics: stratified data not available, so not able to assess whether there were any baseline imbalances in the proportion of participants reporting baseline musculoskeletal symptoms |
| Interventions |
Intervention ‐ multi‐component
Intervention ‐ workstation only
Control
|
| Outcomes |
Outcome name, measurement tool, body region
|
| Notes | Study authors could not be contacted for stratified data for participants with baseline pain |
CBA: controlled before‐and‐after.
Characteristics of ongoing studies [ordered by study ID]
NCT02376504.
| Trial name or title | Modifying the Workplace to Decrease Sedentary Behavior and Improve Health |
| Methods | Randomised controlled trial |
| Participants | Overweight full‐time sedentary workers |
| Interventions | Treadmill workstation; sit‐to‐stand workstation; control (three 10‐minute walking bouts/week) |
| Outcomes | Primary: change in weight Secondary: cardiovascular and metabolic health variables, musculoskeletal discomfort, psychological affect, job stress |
| Starting date | April 2014 |
| Contact information | Dinesh John, PhD |
| Notes | Study completed but no publication found |
NCT03556670.
| Trial name or title | Active Workplace Study |
| Methods | Randomised controlled trial |
| Participants | Call centre employees |
| Interventions | Total worker health: multi‐component organisational and individual level interventions |
| Outcomes | Primary: sedentary behaviour Secondary: multiple cardiovascular, work‐related, and other health outcomes including musculoskeletal discomfort |
| Starting date | June 2018 |
| Contact information | Brad Wipfli, PhDl wipflib@ohsu.edu |
| Notes | Recruitment phase |
Differences between protocol and review
We received stratified data for participants with baseline musculoskeletal pain from study authors of the eight included studies (Alkhajah 2012; Brakenridge 2016; Danquah 2017; Edwardson 2018; Graves 2015; Healy 2013; Healy 2016; Parry 2015). We used these stratified data for our analysis, thus compromising the study randomisation.
Initially, we planned to report risk ratio (RR) for dichotomous data and mean difference (MD) for continuous data, but later we found that the same outcome was presented in some studies as dichotomous data and in other studies as continuous data. So we calculated standardised mean differences for such outcomes and pooled them in a meta‐analysis.
Due to the large number of outcomes, it was not practical to incorporate a GRADE rating of the quality of evidence for every single result. Hence we reported the presence/intensity of musculoskeletal symptoms for the following regions: low back, upper back, neck, and shoulder, and disability for short‐term follow‐up, in the ’Summary of findings’ table.
Contributions of authors
Conceiving the protocol: SP.
Designing the protocol: SP, PC, LS, CM, PO.
Coordinating the protocol: SP.
Designing search strategies: SP, PC.
Writing the protocol: SP, PC.
Providing general advice on the protocol: LS, CM, PO, NS (peer reviewer for protocol).
Extracting data and conducting analysis: SP, PC, NS.
Completing GRADE Assessments: SP, NS.
Writing the review: SP, PC, NS.
Contributing to writing of the review and approving the final draft: LS, CM, PO.
Sources of support
Internal sources
There were no internal sources of support, Other.
External sources
There were no external sources of support, Other.
Declarations of interest
Sharon Parry: none known.
Pieter Coenen: none known..
Peter O'Sullivan: none known.
Chris Maher: member of Editorial Board of the Cochrane Back and Neck Group.
Leon Straker: none known.
Nipun Shrestha: none known.
Edited (no change to conclusions)
References
References to studies included in this review
Alkhajah 2012 {published and unpublished data}
- Alkhajah T, Reeves M, Eakin E, Winkler E, Owen N, Healy G. Sit‐stand workstations: a pilot intervention to reduce office sitting time. American Journal of Preventive Medicine 2012;43:298‐303. [DOI] [PubMed] [Google Scholar]
Brakenridge 2016 {published data only}
- ACTRN12614000252617. Comparison of organisational support vs. organisational plus technology support for reducing prolonged sitting in office workers. https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=365886 (accessed 7 August 2018).
- Brakenridge CL, Fjeldsoe BS, Young DC, Winkler EA, Dunstan DW, Straker LM. Organizational level strategies with or without an activity tracker to reduce office workers’ sitting time: rationale and study design of a pilot cluster randomized trial. JMIR Research Protocols 2016 2016;5(2):e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brakenridge CL, Fjeldsoe BS, Young DC, Winkler EAH, Dunstan DW, Straker LM, et al. Evaluating the effectiveness of organisational‐level strategies with or without an activity tracker to reduce office workers' sitting time: a cluster‐randomised trial. International Journal of Behavioral Nutrition & Physical Activity 2016;13:1‐15. [DOI: 10.1186/s12966-016-0441-3] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brakenridge Cl, Chong YY, Winkler EA, Hadgraft NT Fjeldsoe BS, Johnston V, et al. Evaluating short‐term musculoskeletal pain changes in desk‐based workers receiving a workplace sitting‐reduction intervention. International Journal of Environmental Research and Public Health 2018;15:1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
Danquah 2017 {published data only}
- Danquah IH, Kloster S, Holtermann A, Aadahl M, Tolstrup JS. Effects on musculoskeletal pain from "Take a Stand!" ‐ a cluster‐randomized controlled trial reducing sitting time among office workers. Scandinavian Journal of Work Environment & Health 2017;43(4):350‐7. [DOI: 10.5271/sjweh.3639] [DOI] [PubMed] [Google Scholar]
- NCT01996176. Take a Stand! ‐ an intervention to reduce occupational sitting time. https://clinicaltrials.gov/ct2/show/NCT01996176 (accessed 7 August 2018).
Edwardson 2018 {published data only}
- Edwardson C, Yates T, Biddle S, Davies M, Dunstan D, Esliger D, et al. Effectiveness of the Stand More AT (SMArT) Work intervention: cluster randomised controlled trial. British Medical Journal 2018;363:k3870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ISRCTN10967042. SMArT Work: Stand More AT Work. https://doi.org/10.1186/ISRCTN10967042 (accessed 19 February 2019).
Gibbs 2018 {published data only}
- Gibbs B, Hergenroeder AL, Perdomo SJ, Kowalsky R, Delitto A, Jakicic JM. Reducing sedentary behavior to decrease chronic low back pain: the Stand Back randomized trial. Occupational and Environmental Medicine 2018;75(5):321‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT02624687. Reducing sedentary behavior to decrease low back pain: Stand Back study (StandBack). https://clinicaltrials.gov/ct2/show/NCT02624687 (accessed 7 August 2018).
Graves 2015 {published data only}
- Graves LEF, Murphy RC, Shepherd SO, Cabot J, Hopkins ND. Evaluation of sit‐stand workstations in an office setting: a randomised controlled trial. BMC Public Health 2015;15(1):1145. [DOI: 10.1186/s12889-015-2469-8] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT02496507. A mixed‐methods evaluation of sit‐stand workstations in an office setting. https://clinicaltrials.gov/ct2/show/NCT02496507 (accessed 7 August 2018).
Healy 2013 {published and unpublished data}
- Healy GN, Eakin EG, Lamontagne AD, Owen N, Winkler EA, Wiesner G, et al. Reducing sitting time in office workers: short‐term efficacy of a multi component intervention. Preventive Medicine 2013;57:43‐8. [DOI] [PubMed] [Google Scholar]
Healy 2016 {published and unpublished data}
- ACTRN12611000742976. Stand Up Victoria: a trial to determine whether environmental modification and behavioural counselling can lead to reductions in workplace sitting time in office workers. https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12611000742976 (accessed 19 February 2019).
- Dunstan DW, Wiesner G, Eakin EG, Neuhaus M, Owen N, LaMontagne AD, et al. Reducing office workers’ sitting time: rationale and study design for the Stand Up Victoria cluster randomised trial. BMC Public Health 2013;13:105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healy G, Eakin E, Owen N, Lamontagne A, Moodie M, Winkler E, et al. A cluster randomized controlled trial to reduce office workers' sitting time: effect on activity outcomes. Medicine and Science in Sports and Exercise 2016;48(9):1787‐97. [DOI] [PubMed] [Google Scholar]
Ognibene 2016 {published data only}
- NCT02146482. Access to a sit‐stand computer workstation and back pain. https://clinicaltrials.gov/ct2/show/NCT02146482 (accessed 7 August 2018).
- Ognibene GT, Torres W, Eyben R, Horst KC. Impact of a sit‐stand workstation on chronic low back pain: results of a randomized trial. Journal of Occupational and Environmental Medicine 2016;58(3):287‐93. [DOI] [PubMed] [Google Scholar]
Parry 2015 {published data only}
- ACTRN12612000743864. Can a participatory workplace intervention improve sedentary behaviour and physical activity in office workers?. http://www.anzctr.org.au/ACTRN12612000743864.aspx (accessed 7 August 2018).
- Parry S, Straker L, Gilson N, Smith A. Can participatory workplace interventions that aim to reduce sedentary time modify musculoskeletal symptoms of office workers?. Physiotherapy (United Kingdom) 2015;101:eS1178‐9. [Google Scholar]
- Parry S, Straker L, Gilson ND, Smith AJ. Participatory workplace interventions can reduce sedentary time for office workers ‐ a randomised controlled trial. PLoS One 2013;8(11):e78957. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Aghilinejad 2014 {published data only}
- Aghilinejad M, Bahrami‐Ahmadi A, Kabir‐Mokamelkhah E, Sarebanha S, Hosseini HR, Sadeghi Z. The effect of three ergonomics training programs on the prevalence of low‐back pain among workers of an Iranian automobile factory: a randomized clinical trial. International Journal of Occupational and Environmental Medicine 2014;5(2):65‐71. [PMC free article] [PubMed] [Google Scholar]
Andersen 2010 {published data only}
- Andersen LL, Christensen KB, Holtermann A, Poulsen OM, Sjogaard G, Pedersen MT, et al. Effect of physical exercise interventions on musculoskeletal pain in all body regions among office workers: a one‐year randomized controlled trial. Manual Therapy 2010;15(1):100‐4. [DOI] [PubMed] [Google Scholar]
Baker 2013 {published data only}
- Baker NA, Moehling K. The relationship between musculoskeletal symptoms, postures and the fit between workers' anthropometrics and their computer workstation configuration. Work (Reading, Mass.) 2013;46(1):3‐10. [DOI] [PubMed] [Google Scholar]
Bergman 2018 {published data only}
- Bergman F, Wahlstrom V, Stomby A, Otten J, Lanthen E, Renklint R, et al. Treadmill workstations in office workers who are overweight or obese: a randomised controlled trial. Lancet Public Health 2018;3(11):e523‐35. [DOI] [PubMed] [Google Scholar]
Bernaards 2006 {published data only}
- Bernaards CM, Ariens GA, Hildebrandt VH. The (cost‐)effectiveness of a lifestyle physical activity intervention in addition to a work style intervention on the recovery from neck and upper limb symptoms in computer workers. BMC Musculoskeletal Disorders 2006;7:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bernaards 2008 {published data only}
- Bernaards CM, Ariens GA, Simons M, Knol DL, Hildebrandt VH. Improving work style behavior in computer workers with neck and upper limb symptoms. Journal of Occupational Rehabilitation 2008;18(1):87‐101. [DOI] [PubMed] [Google Scholar]
Bernaards 2011 {published data only}
- Bernaards CM, Bosmans JE, Hildebrandt VH, Tulder MW, Heymans MW. The cost‐effectiveness of a lifestyle physical activity intervention in addition to a work style intervention on recovery from neck and upper limb symptoms and pain reduction in computer workers [with consumer summary]. Occupational and Environmental Medicine 2011;68(4):265‐72. [DOI] [PubMed] [Google Scholar]
Blangsted 2008 {published data only}
- Blangsted AK, Søgaard K, Hansen EA, Hannerz H, Sjøgaard G. One‐year randomized controlled trial with different physical‐activity programs to reduce musculoskeletal symptoms in the neck and shoulders among office workers. Scandinavian Journal of Work, Environment & Health 2008;34(1):55‐65. [DOI] [PubMed] [Google Scholar]
Blasche 2013 {published data only}
- Blasche G, Pfeffer M, Thaler H, Gollner E. Work‐site health promotion of frequent computer users: comparing selected interventions. Work (Reading, Mass.) 2013;46(3):233‐41. [DOI] [PubMed] [Google Scholar]
Brendbekken 2016 {published data only}
- Brendbekken R, Harris A, Ursin H, Eriksen H, Tangen T. Multidisciplinary intervention in patients with musculoskeletal pain: a randomized clinical trial. International Journal of Behavioral Medicine 2016;23(1):1‐11. [DOI: 10.1007/s12529-015-9486-y] [DOI] [PMC free article] [PubMed] [Google Scholar]
Carr 2013 {published data only}
- Carr LJ, Dunsiger SI, Lewis B, Ciccolo JT, Hartman S, Bock B, et al. Randomized controlled trial testing an internet physical activity intervention for sedentary adults. Health Psychology 2013;32(3):328‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carr 2016 {published data only}
- Carr LJ, Leonhard C, Tucker S, Fethke N, Benzo R, Gerr F. Total worker health intervention increases activity of sedentary workers. American Journal of Preventive Medicine 2016;50(1):9‐17. [DOI] [PubMed] [Google Scholar]
Castagnoli 2015 {published data only}
- Castagnoli C, Cecchi F, Canto A, Paperini A, Boni R, Pasquini G, et al. Effects in short and long term of global postural reeducation (GPR) on chronic low back pain: a controlled study with one‐year follow‐up. Scientific World Journal 2015;2015 (no pagination)(271436):na. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chung 2009 {published data only}
- Chung M, Melnyk P, Blue D, Renaud D, Breton M. Worksite health promotion: the value of the Tune Up Your Heart program. Population Health Management 2009;12(6):297‐304. [DOI: 10.1089/pop.2008.0044] [DOI] [PubMed] [Google Scholar]
Cristancho 2012 {published data only}
- Cristancho MY. Participatory ergonomics among female cashiers from a department store. Work 2012;41(Suppl 1):2499‐505. [DOI] [PubMed] [Google Scholar]
Curwin 2013 {published data only}
- Curwin S, Allt J, Szpilfogel C, Makrides L. The Healthy LifeWorks project: the effect of a comprehensive workplace wellness program on the prevalence and severity of musculoskeletal disorders in a Canadian government department. Journal of Occupational & Environmental Medicine 2013;55(6):628‐33. [DOI] [PubMed] [Google Scholar]
Dahl 2001 {published data only}
- Dahl JC, Nilsson A. Evaluation of a randomized preventive behavioural medicine work site intervention for public health workers at risk for developing chronic pain. European Journal of Pain 2001;5(4):421‐32. [DOI] [PubMed] [Google Scholar]
delPozo Cruz 2012 {published data only}
- Pozo‐Cruz B, Parraca JA, Pozo‐Cruz J, Adsuar JC, Hill JC, Gusi N. An occupational, internet‐based intervention to prevent chronicity in subacute lower back pain: a randomised controlled trial. Journal of Rehabilitation Medicine 2012;44(7):581‐7. [DOI] [PubMed] [Google Scholar]
delPozo Cruz 2013 {published data only}
- Pozo‐Cruz B, Gusi N, Pozo‐Cruz J, Adsuar JC, Hernandez‐Mocholi M, Parraca JA. Clinical effects of a nine‐month web‐based intervention in subacute non‐specific low back pain patients: a randomized controlled trial. Clinical Rehabilitation 2013;27(1):28‐39. [DOI] [PubMed] [Google Scholar]
Denis 2012 {published data only}
- Denis A, Zelmar A, Pogam MA, Chaleat‐Valayer E, Bergeret A, Colin C. The PRESLO study: evaluation of a global secondary low back pain prevention program for health care personnel in a hospital setting. Multicenter, randomized intervention trial. BMC Musculoskeletal Disorders 2012;13(234):na. [DOI] [PMC free article] [PubMed] [Google Scholar]
Doda 2015 {published data only}
- Doda D, Rothmore P, Pisaniello D, Briggs N, Stewart S, Mahmood M, et al. Relative benefit of a Stage of Change approach for the prevention of musculoskeletal pain and discomfort: a cluster randomised trial. Occupational and Environmental Medicine 2015;72(11):784‐91. [DOI] [PubMed] [Google Scholar]
Driessen 2011 {published data only}
- Driessen MT, Proper KI, Anema JR, Knol DL, Bongers PM, Beek AJ. Participatory ergonomics to reduce exposure to psychosocial and physical risk factors for low back pain and neck pain: results of a cluster randomised controlled trial. Occupational and Environmental Medicine 2011;68(9):674‐81. [DOI] [PubMed] [Google Scholar]
Dugan 2006 {published data only}
- Dugan SA. The role of exercise in the prevention and management of acute low back pain. Clinics in Occupational and Environmental Medicine 2006;5(3):615‐32. [DOI] [PubMed] [Google Scholar]
Ebara 2008 {published data only}
- Ebara T, Kubo T, Inoue T, Murasaki GI, Takeyama H, Sato T, et al. Effects of adjustable sit‐stand VDT workstations on workers' musculoskeletal discomfort, alertness and performance. Industrial Health 2008;46(5):497‐505. [DOI] [PubMed] [Google Scholar]
Engelen 2014 {published data only}
- Engelen L, Chau J, Dhillon H, Hespe D, Bauman A. Does moving to a new health promoting building change behaviour and workplace perceptions? A pilot study. Journal of Science and Medicine in Sport 2014;18:e124. [Google Scholar]
Esmaeilzadeh 2014 {published data only}
- Esmaeilzadeh S, Ozcan E, Capan N. Effects of ergonomic intervention on work‐related upper extremity musculoskeletal disorders among computer workers: a randomized controlled trial. International Archives of Occupational and Environmental Health 2014;87(1):73‐83. [DOI] [PubMed] [Google Scholar]
Estabrooks 2011 {published data only}
- Estabrooks PA, Smith‐Ray RL, Almeida FA, Hill J, Gonzales M, Schreiner P, et al. Move More: translating an efficacious group dynamics physical activity intervention into effective clinical practice. International Journal of Sport and Exercise Psychology 2011;9(1):4‐18. [Google Scholar]
Fazioli 2004 {published data only}
- Fazioli R, Galli L, Antoniazzi E, Cirla AM. Value of ergomotricity in the prevention of musculoskeletal disorders in sedentary workers. [Italian]. Giornale Italiano di Medicina del Lavoro ed Ergonomia 2004;26(4 Suppl):225‐6. [Google Scholar]
Fewster 2017 {published data only}
- Fewster KM, Gallagher KM, Callaghan JP. The effect of standing interventions on acute low‐back postures and muscle activation patterns. Applied Ergonomics 2017;58:281‐6. [DOI] [PubMed] [Google Scholar]
Gao 2016 {published data only}
- Gao Y, Nevala N, Cronin NJ, Finni T. Effects of environmental intervention on sedentary time, musculoskeletal comfort and work ability in office workers. European Journal of Sport Science 2016;16(6):747‐54. [DOI] [PubMed] [Google Scholar]
Gerr 2005 {published data only}
- Gerr F, Marcus M, Monteilh C, Hannan L, Ortiz D, Kleinbaum D. A randomised controlled trial of postural interventions for prevention of musculoskeletal symptoms among computer users. Occupational & Environmental Medicine 2005;62(7):478‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
Grunseit 2012 {published data only}
- Grunseit A, Chau J, Ploeg H, Bauman A. Thinking on your feet: a qualitative evaluation of an installation of sit‐stand desks in a medium‐sized workplace. Journal of Science and Medicine in Sport 2012;15:S195‐6. [Google Scholar]
Hillsdon 2002 {published data only}
- Hillsdon M, Thorogood M, White I, Foster C. Advising people to take more exercise is ineffective: a randomized controlled trial of physical activity promotion in primary care [with consumer summary]. International Journal of Epidemiology 2002;31(4):808‐15. [DOI] [PubMed] [Google Scholar]
Husemann 2009 {published data only}
- Husemann B, Mach CY, Borsotto D, Zepf KI, Scharnbacher J. Comparisons of musculoskeletal complaints and data entry between a sitting and a sit‐stand workstation paradigm. Human Factors 2009;51(3):310‐20. [DOI] [PubMed] [Google Scholar]
Irmak 2012 {published data only}
- Irmak A, Bumin G, Irmak R. The effects of exercise reminder software program on office workers' perceived pain level, work performance and quality of life. Work 2012;41:5692‐5. [DOI] [PubMed] [Google Scholar]
Jay 2014 {published data only}
- Jay K, Brandt M, Sundstrup E, Schraefel M, Jakobsen MD, Sjogaard G, et al. Effect of individually tailored biopsychosocial workplace interventions on chronic musculoskeletal pain, stress and work ability among laboratory technicians: randomized controlled trial protocol. BMC Musculoskeletal Disorders 2014;15:444. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jay 2015 {published data only}
- Jay K, Brandt M, Hansen K, Sundstrup E, Jakobsen MD, Schraefel MC, et al. Effect of individually tailored biopsychosocial workplace interventions on chronic musculoskeletal pain and stress among laboratory technicians: randomized controlled trial. Pain Physician 2015;18(5):459‐71. [PubMed] [Google Scholar]
Jay 2016 {published data only}
- Jay K, Brandt M, Jakobsen MD, Sundstrup E, Berthelsen KG, Schraefel M, et al. Ten weeks of physical‐cognitive‐mindfulness training reduces fear‐avoidance beliefs about work‐related activity: randomized controlled trial. Medicine 2016;95(34):na. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kilpikoski 2009 {published data only}
- Kilpikoski S, Alen M, Paatelma M, Simonen R, Heinonen A, Videman T. Outcome comparison among working adults with centralizing low back pain: secondary analysis of a randomized controlled trial with 1‐year follow‐up. Advances in Physiotherapy 2009;11(4):210‐7. [Google Scholar]
Kline 2017 {published data only}
- Kline CE, Perdomo SJ, Hergenroeder AL, Barone Gibbs B. The effect of reducing sedentary behavior on sleep quality among adults with chronic low back pain: a randomized controlled pilot study. Sleep 2017;40:A387‐8. [Google Scholar]
Levanon 2012 {published data only}
- Levanon Y, Gefen A, Lerman Y, Givon U, Ratzon NZ. Multi dimensional system for evaluating preventive program for upper extremity disorders among computer operators. Work 2012;41(Suppl 1):669‐75. [DOI] [PubMed] [Google Scholar]
Levanon 2012a {published data only}
- Levanon Y, Gefen A, Lerman Y, Givon U, Ratzon NZ. Reducing musculoskeletal disorders among computer operators: comparison between ergonomics interventions at the workplace. Ergonomics 2012;55(12):1571‐85. [DOI] [PubMed] [Google Scholar]
Loisel 1997 {published data only}
- Loisel P, Abenhaim L, Durand P, Esdaile JM, Suissa S, Gosselin L, et al. A population‐based, randomized clinical trial on back pain management. Spine 1997;22(24):2911‐8. [DOI] [PubMed] [Google Scholar]
Mackey 2011 {published data only}
- Mackey M, Bohle P, Taylor P, Biase T, McLoughlin C, Purnell K. 'Walking to wellness' in an ageing sedentary university community ‐ a randomised controlled feasibility study. Physiotherapy (United Kingdom) 2011;97:eS733‐4. [Google Scholar]
McDonough 2011 {published data only}
- McDonough S, Tully MA, O'Connor S, Boyd A, Kerr D, O'Neill S, et al. A pedometer‐based walking programme for people with chronic low back pain: experience from the BACK 2 activity trial. Physiotherapy (United Kingdom) 2011;97:eS782. [Google Scholar]
Mills 2011 {published data only}
- Mills R, Tully MA, Daly L, Mechelen W, Boreham C, McDonough S, et al. Adherence with an eight week individualised walking programme for people with chronic low back pain: report from the Swift trial. Physiotherapy (United Kingdom) 2011;97:eS812. [Google Scholar]
Pedersen 2009 {published data only}
- Pedersen MT, Blangsted AK, Andersen LL, Jorgensen MB, Hansen EA, Sjogaard G. The effect of worksite physical activity intervention on physical capacity, health, and productivity: a 1‐year randomized controlled trial. Journal of Occupational & Environmental Medicine 2009;51(7):759‐70. [DOI] [PubMed] [Google Scholar]
Phattharasupharerk 2018 {published data only}
- Phattharasupharerk S, Purepong N, Eksakulkla S, Siriphorn A. Effects of Qigong practice in office workers with chronic non‐specific low back pain: a randomized control trial. Journal of Bodywork and Movement Therapies 2018;23(2):375‐381. [DOI] [PubMed] [Google Scholar]
Pozo Cruz 2012 {published data only}
- Pozo‐Cruz BD, Adsuar JC, Parraca J, Pozo‐Cruz JD, Moreno A, Gusi N. A web‐based intervention to improve and prevent low back pain among office workers: a randomized controlled trial. Journal of Orthopaedic and Sports Physical Therapy 2012;42(10):831‐41. [DOI] [PubMed] [Google Scholar]
Robertson 2008 {published data only}
- Robertson MM, Huang YH, O'Neill MJ, Schleifer LM. Flexible workspace design and ergonomics training: impacts on the psychosocial work environment, musculoskeletal health, and work effectiveness among knowledge workers. Applied Ergonomics 2008;39(4):482‐94. [DOI] [PubMed] [Google Scholar]
Robertson 2013 {published data only}
- Robertson MM, Ciriello VM, Garabet AM. Office ergonomics training and a sit‐stand workstation: effects on musculoskeletal and visual symptoms and performance of office workers. Applied Ergonomics 2013;44(1):73‐85. [DOI] [PubMed] [Google Scholar]
Robertson 2017 {published data only}
- Robertson MM, Huang YH, Lee J. Improvements in musculoskeletal health and computing behaviors: effects of a macroergonomics office workplace and training intervention. Applied Ergonomics 2017;62:182‐96. [DOI] [PubMed] [Google Scholar]
Roemmich 2014 {published data only}
- Roemmich J. Effect of height adjustable desks on standing time, discomfort, and productivity of office workers with sedentary occupations. FASEB Journal. Conference: Experimental Biology 2014;28(1):na. [Google Scholar]
Shnayderman 2013 {published data only}
- Shnayderman I, Katz‐Leurer M. An aerobic walking programme versus muscle strengthening programme for chronic low back pain: a randomized controlled trial. Clinical Rehabilitation 2013;27(3):207‐14. [DOI: 10.1177/0269215512453353] [DOI] [PubMed] [Google Scholar]
Sihawong 2014 {published data only}
- Sihawong R, Janwantanakul P, Jiamjarasrangsi W. A prospective, cluster‐randomized controlled trial of exercise program to prevent low back pain in office workers. European Spine Journal 2014;23(4):786‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sjogaard 2012 {published data only}
- Sjogaard G. Evidence of worksite physical exercise training to promote health in jobs ranging from low to high occupational physical demands. Journal of Science and Medicine in Sport 2012;15:S194‐5. [Google Scholar]
Spekle 2010 {published data only}
- Spekle EM, Hoozemans MJ, Blatter BM, Heinrich J, Beek AJ, Knol DL, et al. Effectiveness of a questionnaire based intervention programme on the prevalence of arm, shoulder and neck symptoms, risk factors and sick leave in computer workers: a cluster randomised controlled trial in an occupational setting. BMC Musculoskeletal Disorders 2010;11:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
Suni 2017 {published data only}
- Suni JH, Rinne M, Tokola K, Manttari A, Vasankari T. Effectiveness of a standardised exercise programme for recurrent neck and low back pain: a multicentre, randomised, two‐arm, parallel group trial across 34 fitness clubs in Finland [with consumer summary]. BMJ Open Sport & Exercise Medicine 2017;3(1):e000233. [DOI] [PMC free article] [PubMed] [Google Scholar]
Szeto 2015 {published data only}
- Szeto G, Hung LK, So B, Tsang S. Integrating ergonomics intervention and motor control training: an innovative approach in managing work‐related musculoskeletal disorders. Physiotherapy (United Kingdom) 2015;101:eS1465‐6. [Google Scholar]
Thorp 2014 {published data only}
- Thorp AA, Kingwell BA, Owen N, Dunstan DW. Breaking up workplace sitting time with intermittent standing bouts improves fatigue and musculoskeletal discomfort in overweight/obese office workers. Occupational and Environmental Medicine 2014;71(11):765‐71. [DOI: 10.1136/oemed-2014-102348] [DOI] [PubMed] [Google Scholar]
Tronarp 2018 {published data only}
- Tronarp R, Nyberg A, Hedlund M, Häger CK, McDonough S, Björklund M. Office‐cycling: a promising way to raise pain thresholds and increase metabolism with minimal compromising of work performance. BioMed Research International 2018;2018:1‐12. [DOI: 10.1155/2018/5427201] [DOI] [PMC free article] [PubMed] [Google Scholar]
vanSluijs 2005 {published data only}
- Sluijs EMF, Poppel MNM, Twisk JWR, Brug J, Mechelen W. The positive effect on determinants of physical activity of a tailored, general practice‐based physical activity intervention. Health Education Research 2005;20(3):345‐56. [DOI] [PubMed] [Google Scholar]
Wang 2014 {published data only}
- Wang S, Jiang C, Chern J. Promoting healthy computer use: timing‐informed computer health animations for prolonged sitting computer users. Behaviour & Information Technology 2014;33(3):294‐300. [DOI: 10.1080/0144929X.2012.695394] [DOI] [Google Scholar]
Wollesen 2017 {published data only}
- Wollesen B, Menzel J, Drogemuller R, Hartwig C, Mattes K. The effects of a workplace health promotion program in small and middle‐sized companies: a pre‐post analysis. Journal of Public Health (Germany) 2017;25(1):37‐47. [Google Scholar]
References to studies awaiting assessment
Neuhaus 2014 {published data only}
- ACTRN12612001246875. Reducing sitting time in office workers: comparison of a multifaceted workplace approach vs. installation of height‐adjustable desks only using a three‐armed controlled trial. http://www.anzctr.org.au/ACTRN12612001246875.aspx (accessed 7 August 2014) 2012.
- Neuhaus M, Healy GN, Dunstan DW, Owen N, Eakin EG. Workplace sitting and height‐adjustable workstations:a randomised controlled trial. American Journal of Preventive Medicine 2014;46(1):30‐40. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
NCT02376504 {published data only}
- NCT02376504. Modifying the workplace to decrease sedentary behavior and improve health. https://clinicaltrials.gov/ct2/show/NCT02376504 (accessed 7 August 2018).
NCT03556670 {published data only}
- NCT03556670. Active Workplace Study. https://clinicaltrials.gov/ct2/show/NCT03556670 (accessed 7 August 2018).
Additional references
Agarwal, 2018
- Agarwal, S, Steinmaus, C, Harris‐Adamson, C. Sit‐stand workstations and impact on low back discomfort: a systematic review and meta‐analysis. Ergonomics 2018;61(4):538‐52. [DOI] [PubMed] [Google Scholar]
Al‐Eisa 2006
- Al‐Eisa E, Egan D, Deluzio K, Wassersug R. Effects of pelvic asymmetry and low back pain on trunk kinematics during sitting: a comparison with standing. Spine 2006;31:135‐43. [DOI] [PubMed] [Google Scholar]
Andersen 2007
- Andersen JH, Haahr JP, Frost P. Risk factors for more severe regional musculoskeletal symptoms: a two‐year prospective study of a general working population. Arthritis & Rheumatism 2007;56:1355‐64. [DOI] [PubMed] [Google Scholar]
Bakker 2009
- Bakker EW, Verhagen AP, Trijffel E, Lucas C, Koes BW. Spinal mechanical load as a risk factor for low back pain: a systematic review of prospective cohort studies. Spine 2009;34:E281‐93. [DOI] [PubMed] [Google Scholar]
Balasubramanian 2009
- Balasubramanian V, Adalarasu K, Regulapati R. Comparing dynamic and stationary standing postures in an assembly task. International Journal of Industrial Ergonomics 2009;39:649‐54. [Google Scholar]
Bevan 2015
- Bevan S. Economic impact of musculoskeletal disorders (MSDs) on work in Europe. Best Practice & Research Clinical Rheumatology 2015;29(3):356‐73. [DOI] [PubMed] [Google Scholar]
Bond 1966
- Bond MR, Pilowsky I. Subjective assessment of pain and its relationship to the administration of analgesics in patients with advanced cancer. Journal of Psychosomatic Research 1966;10(2):203‐8. [DOI] [PubMed] [Google Scholar]
Borodulin 2007
- Borodulin K, Laatikainen T, Juolevi A, Jousilahti P. Thirty‐year trends of physical activity in relation to age, calendar time and birth cohort in Finnish adults. European Journal of Public Health 2007;18:339‐44. [DOI] [PubMed] [Google Scholar]
Brownson 2005
- Brownson RC, Boehmer TK, Luke DA. Declining rates of physical activity in the United States. Annual Review of Public Health 2005;26:421‐43. [DOI] [PubMed] [Google Scholar]
Buchbinder 2013
- Buchbinder R, Blyth F, March L, Brooks P, Woolf A, Hoy D. Placing the global burden of low back pain in context. Best Practice & Research Clinical Rheumatology 2013;27:575‐89. [DOI] [PubMed] [Google Scholar]
Campbell 2001
- Campbell MK, Mollison J, Grimshaw JM. Cluster trials in implementation research: estimation of intracluster correlation coefficients and sample size. Statistics in Medicine 2001;20(3):391‐9. [DOI] [PubMed] [Google Scholar]
Carson 2014
- Carson V, Wong SL, Winkler E, Healy GN, Colley RC, Tremblay MS. Patterns of sedentary time and cardiometabolic risk among Canadian adults. Preventive Medicine 2014;65C:23‐7. [DOI] [PubMed] [Google Scholar]
CDC 2013
- Centers for Disease Control and Prevention. Work‐Related Musculoskeletal Disorders (WMSDs) Interventions. www.cdc.gov/workplacehealthpromotion/health‐strategies/musculoskeletal‐disorders/interventions/index.html (accessed 16 September 2016).
Chau 2014
- Chau J, Grunseit A, Midthjell K, Holmen J, Holmen T, Bauman AE, et al. Cross‐sectional associations of total sitting and leisure screen time with cardiometabolic risk in adults. Results from the HUNT Study, Norway. Journal of Science and Medicine in Sport 2014;17(1):78‐84. [DOI] [PubMed] [Google Scholar]
Chen 2009
- Chen SM, Liu MF, Cook J, Bass S, Lo SK. Sedentary lifestyle as a risk factor for low back pain: a systematic review. International Archives of Occupational & Environmental Health 2009;82:797‐806. [DOI] [PubMed] [Google Scholar]
Chester 2002
- Chester MR, Rys MJ, Konz SA. Leg swelling, comfort and fatigue when sitting, standing, and sit/standing. International Journal of Industrial Ergonomics 2002;29:289‐96. [Google Scholar]
Chiu 2002
- Chiu T, Ku W, Lee M, Sum W, Wan M, Wong C, et al. A study on the prevalence of and risk factors for neck pain among University academic staff in Hong Kong. Journal of Occupational Rehabilitation 2002;12:77‐91. [DOI] [PubMed] [Google Scholar]
Cho 2012
- Cho C, Hwang Y, Cherng R. Musculoskeletal symptoms and associated risk factors among office workers with high workload computer use. Journal of Manipulative and Physiological Therapeutics 2012;35:534‐40. [DOI] [PubMed] [Google Scholar]
Church 2011
- Church T, Thomas D, Tudor‐Locke C, Katzmarzyk PT, Earnest CP, Rodarte R, et al. Trends over 5 decades in U.S. occupation‐related physical activity and their associations with obesity. PLoS ONE 2011;6(5):e19657. [DOI] [PMC free article] [PubMed] [Google Scholar]
Coenen 2017
- Coenen P, Parry S, Willenberg L, Shi JW, Romero L, Blackwood DM, et al. Associations of prolonged standing with musculoskeletal symptoms ‐ a systematic review of laboratory studies. Gait and Posture 2017;58:310‐8. [DOI] [PubMed] [Google Scholar]
Coenen 2018
- Coenen P, Healy G, Winkler E, Dunstan D, Owen N, Moodie M, et al. Associations of office workers’ objectively assessed occupational sitting, standing and stepping time with musculoskeletal symptoms. Ergonomics 2018;61(9):1187‐95. [DOI] [PubMed] [Google Scholar]
Coenen 2019
- Coenen P, Molen HF, Burdorf A, Huysmans MA, Straker L, Frings‐Dresen MH, et al. Associations of screen work with neck and upper extremity symptoms: a systematic review with meta‐analysis. Occupational and Environmental Medicine 2019;76(7):502‐509. [DOI] [PubMed] [Google Scholar]
Commissaris 2016
- Commissaris DA, Huysmans MA, Mathiassen SE, Srinivasan D, Koppes LLJ, Hendriksen IJ. Interventions to reduce sedentary behavior and increase physical activity during productive work: a systematic review. Scandinavian Journal of Work, Environment & Health 2016;42(3):181‐91. [DOI] [PubMed] [Google Scholar]
Curran 2015
- Curran M, O'Sullivan L, O'Sullivan P, Dankaerts W, O'Sullivan K. Does using a chair backrest or reducing seated hip flexion influence trunk muscle activity and discomfort? A systematic review. Human Factors 2015;57:1115‐48. [DOI] [PubMed] [Google Scholar]
da Costa 2010
- Costa BR, Vieira ER. Risk factors for work‐related musculoskeletal disorders: a systematic review of recent longitudinal studies. American Journal of Industrial Medicine 2010;53:285‐323. [DOI] [PubMed] [Google Scholar]
de Zwart 2002
- Zwart BCH, Frings‐Dresen MHW, Duivenbooden JC. Test–retest reliability of the Work Ability Index questionnaire. Occupational Medicine 2002;52(4):177‐81. [DOI] [PubMed] [Google Scholar]
Downs 1998
- Downs S, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non‐randomised studies of health care interventions. Journal of Epidemiology and Community Health 1998;52:377‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dunstan 2012
- Dunstan D, Howard B, Healy GN, Owen N. Too much sitting ‐ a health hazard. Diabetes Research and Clinical Practice 2012;97(3):368‐76. [DOI] [PubMed] [Google Scholar]
Engels 1996
- Engels JA, Gulden JW, Senden TF, Van't Hof B. Work related risk factors for musculoskeletal complaints in the nursing profession: results of a questionnaire survey. Occupational and Environmental Medicine 1996;53:636‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Freak‐Poli 2013
- Freak‐Poli RLA, Cumpston M, Peeters A, Clemes SA. Workplace pedometer interventions for increasing physical activity. Cochrane Database of Systematic Reviews 2013, Issue 4. [DOI: 10.1002/14651858.CD009209.pub2] [DOI] [PubMed] [Google Scholar]
GBDSC 2015
- Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386:743‐800. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gregory 2008
- Gregory DE, Callaghan JP. Prolonged standing as a precursor for the development of low back discomfort: an investigation of possible mechanisms. Gait & Posture 2008;28:86‐92. [DOI] [PubMed] [Google Scholar]
Hannan 2005
- Hannan L, Monteilh C, Gerr F, Kleinbaum D, Marcus M. Job strain and risk of musculoskeletal symptoms among a prospective cohort of occupational computer users. Scandinavian Journal of Work, Environment & Health 2005;31:375‐86. [DOI] [PubMed] [Google Scholar]
Harcombe 2009
- Harcombe H, McBride D. Prevalence and impact of musculoskeletal disorders in New Zealand nurses, postal workers and office workers. Australian and New Zealand Journal of Public Health 2009;33:437‐41. [DOI] [PubMed] [Google Scholar]
Harland 2015
- Harland NJ, Dawkin MJ, Martin D. Relative utility of a visual analogue scale vs. a six‐point Likert scale in the measurement of global subject outcome in patients with low back pain receiving physiotherapy. Physiotherapy 2015;101(1):50‐4. [DOI] [PubMed] [Google Scholar]
Healy 2012
- Healy GN, Lawler S, Thorp A, Neuhaus M, Robson E, Owen N, et al. Reducing Prolonged Sitting in the Workplace (An Evidence Review: Full Report). Melbourne, Australia: VIctorian Health Promotion Foundation, 2012.
Healy 2017
- Healy G, Winkler E, Eakin E, Owen N, Lamontagne A, Mooie M, et al. A cluster RCT to reduce workers' sitting time: impact on cardiometabolic biomarkers. Medice and Science in Sports and Exercise 2017;49(10):2032‐9. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Hooftman 2004
- Hooftman WE, Poppel MNM, Beek AJ, Bongers PM, Mechelen W. Gender differences in the relations between work‐related physical and psychosocial risk factors and musculoskeletal complaints. Scandinavian Journal of Work, Environment & Health 2004;30(4):261‐78. [DOI] [PubMed] [Google Scholar]
Hoy 2012
- Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, et al. A systematic review of the global prevalence of low back pain. Arthritis & Rheumatism 2012;64(6):2028‐37. [DOI] [PubMed] [Google Scholar]
Hush 2009
- Hush J, Michaleff Z, Maher C, Refshauge K. Individual, physical and psychological risk factors for neck pain in Australian office workers: a 1‐year longitudinal study. European Spine Journal 2009;18:1535‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Huysmans 2012
- Huysmans M, Ijmker S, Blatter BM, Knol DL, Mechelen W, Bongers PM, et al. The relative contribution of work exposure, leisure time exposure, and individual characteristics in the onset of arm‐wrist‐hand and neck‐shoulder symptoms among office workers. International Archives of Occupational and Environmental Health 2012;85(6):651‐66. [DOI] [PubMed] [Google Scholar]
Ijaz 2014
- Ijaz S, Verbeek JH, Mischke C, Ruotsalainen J. Inclusion of nonrandomized studies in Cochrane systematic reviews was found to be in need of improvement. Journal of Clinical Epidemiology 2014;67(6):645‐53. [DOI] [PubMed] [Google Scholar]
Janwantanakul 2008
- Janwantanakul P, Pensri P, Jiamjarasrangsri V, Sinsongsook T. Prevalence of self‐reported musculoskeletal symptoms among office workers. Occupational Medicine 2008;58:436‐8. [DOI] [PubMed] [Google Scholar]
Jensen 2003
- Jensen C. Development of neck and hand‐wrist symptoms in relation to duration of computer use at work. Scandinavian Journal of Work, Environment & Health 2003;29:197‐205. [DOI] [PubMed] [Google Scholar]
Juneau 2010
- Juneau C, Potvin L. Trends in leisure‐, transport‐, and work‐related physical activity in Canada 1994‐2005. Preventive Medicine 2010;51:384‐6. [DOI] [PubMed] [Google Scholar]
Karakolis 2014
- Karakolis T, Callaghan JP. The impact of sit‐stand office workstations on worker discomfort and productivity: a review. Applied Ergonomics 2014;45:799‐806. [DOI] [PubMed] [Google Scholar]
Karol 2015
- Karol, S, Robertson, M. Implications of sit‐stand and active workstations to counteract the adverse effects of sedentary work: a comprehensive review. Work 2015;52:255‐67. [DOI] [PubMed] [Google Scholar]
Kiss 2012
- Kiss P, Meester M, Kruse A, Chavee B, Braeckman L. Neck and shoulder complaints in computer workers and associated easy to assess occupational factors ‐ a large‐scale cross‐sectional multivariate study. International Archives of Occupational and Environmental Health 2012;85:197‐206. [DOI] [PubMed] [Google Scholar]
Kohl 2012
- Kohl HW 3rd, Craig CL, Lambert EV, Inoue S, Alkandari JR, Leetongin G, et al. The pandemic of physical inactivity: global action for public health. Lancet 2012;380(9838):294‐305. [DOI] [PubMed] [Google Scholar]
Kovacs 2005
- Kovacs FM, Abraira V, Zamora J, Fernandez C. The transition from acute to subacute and chronic low back pain: a study based on determinants of quality of life and prediction of chronic disability. Spine (Phila Pa 1976) 2005;30(15):1786‐92. [DOI] [PubMed] [Google Scholar]
Kuorinka 1987
- Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Biering‐Sorensen F, Andersson G, et al. Standardised Nordic Questionnaires for the analysis of musculoskeletal symptoms. Applied Ergonomics 1987;18(3):233‐7. [DOI] [PubMed] [Google Scholar]
Lambeek 2011
- Lambeek LC, Tulder MW, Swinkels IC, Koppes LL, Anema JR, Mechelen W. The trend in total cost of back pain in The Netherlands in the period 2002 to 2007. Spine (Phila Pa 1976) 2011;36(13):1050‐8. [DOI] [PubMed] [Google Scholar]
Lin 2011
- Lin C, McAuley J, Macedo L, Barnett D, Smeets R, Verbunt J. Relationship between physical activity and disability in low back pain: a systematic review and meta‐analysis. Pain 2011;152:607‐13. [DOI] [PubMed] [Google Scholar]
Melzack 1975
- Melzack R. The McGill Pain Questionnaire: major properties and scoring methods. Pain 1975;1(3):277‐99. [DOI] [PubMed] [Google Scholar]
Messing 2008
- Messing K, Tissot F, Stock S. Distal lower‐extremity pain and work postures in the Quebec population. American Journal of Public Health 2008;98:705‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moore 2013
- Moore RA, Straube S, Aldington D. Pain measures and cut‐offs – no worse than mild pain as a simple, universal outcome. Anaesthesia 2013;68(4):400‐12. [DOI] [PubMed] [Google Scholar]
Moreira‐Silva 2013
- Moreira‐Silva I, Santos R, Abreu S, Mota J. Associations between BMI and musculoskeletal pain and related symptoms in different body regions among workers. SAGE Open 2013;3(2):1‐6. [Google Scholar]
Neilsen 2017
- Neilsen MC, Gupta N, Knudsen LE, Holtermann A. Association of objectively measured occupational walking and standing still with low back pain: a cross‐sectional study. Ergonomics 2017;60(1):118‐26. [DOI] [PubMed] [Google Scholar]
Nelson‐Wong 2010
- Nelson‐Wong E, Callaghan JP. Is muscle co‐activation a predisposing factor for low back pain development during standing? A multifactorial approach for early identification of at‐risk individuals. Journal of Electromyography & Kinesiology 2010;20:256‐63. [DOI] [PubMed] [Google Scholar]
Neuhaus 2014 a
- Neuhaus M, Eakin E, Straker L, Owen N, Dunstan D, Reid N, et al. Reducing occupational sedentary time: a systematic review and meta‐analysis of evidence on activity‐permissive workstations. Obesity Reviews 2014;15:822‐38. [DOI] [PubMed] [Google Scholar]
Neuhaus 2014b
- Neuhaus M, Healy G, Fjeldsoe B, Lawler S, Owen N, Dunstan D, et al. Iterative development of Stand Up Australia: a multi‐component intervention to reduce workplace sitting. International Journal of Behavioral Nutrition and Physical Activity 2014;11:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
O'Sullivan 2011
- O'Sullivan PB, Smith AJ, Beales DJ, Straker LM. Association of biopsychosocial factors with degree of slump in sitting posture and self‐report of back pain in adolescents: a cross‐sectional study. Physical Therapy 2011;91:470‐83. [DOI] [PubMed] [Google Scholar]
Oha 2014
- Oha K, Animagi L, Paasuke M, Coggon D, Merisalu E. Individual and work‐related risk factors for musculoskeletal pain: a cross‐sectional study among Estonian computer users. BMC Musculoskeletal Disorders 2014;15:151. [DOI] [PMC free article] [PubMed] [Google Scholar]
Parry 2013
- Parry S, Straker L. Office work contributes significantly to sedentary behaviour associated risk. BMC Public Health 2013;13:296. [DOI] [PMC free article] [PubMed] [Google Scholar]
Parry 2017a
- Parry SP, Coenen P, O'Sullivan PB, Maher CG, Straker LM. Workplace interventions for increasing standing or walking for preventing musculoskeletal symptoms in sedentary workers. Cochrane Database of Systematic Reviews 2017, Issue na. [DOI: 10.1002/14651858.CD012486] [DOI] [PMC free article] [PubMed] [Google Scholar]
Peddie 2013
- Peddie MC, Bone JL, Rehrer NJ, Skeaff CM, Gray AR, Perry TL. Breaking prolonged sitting reduces postprandial glycemia in healthy, normal‐weight adults: a randomized crossover trial. American Journal of Clinical Nutrition 2013;98:358‐66. [DOI] [PubMed] [Google Scholar]
Pope 2002
- Pope MH, Goh KL, Magnusson ML. Spine ergonomics. Annual Review of Biomedical Engineering 2002;4:49‐68. [DOI] [PubMed] [Google Scholar]
Reid 2010
- Reid CR, Bush PM, Karwowski W, Durrani SK. Occupational postural activity and lower extremity discomfort: a review. International Journal of Industrial Ergonomics 2010;40:247‐56. [Google Scholar]
RevMan 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Roelofs 2002
- Roelofs A, Straker L. The experience of musculoskeletal discomfort amongst bank tellers who just sit, just stand or sit and stand at work. Ergonomics Journal of South Africa 2002;14(2):11‐29. [Google Scholar]
Roffey 2010
- Roffey D, Wai E, Bishop P, Kwon B, Dagenais S. Causal assessment of occupational sitting and low back pain: results of a systematic review. Spine Journal 2010;10(3):252‐61. [DOI] [PubMed] [Google Scholar]
Roland 2000
- Roland M, Fairbank J. The Roland‐Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine 2000;25(24):3115‐24. [DOI] [PubMed] [Google Scholar]
Shrestha 2018
- Shrestha N, Kukkonen‐Harjula KT, Verbeek JH, Ijaz S, Hermans V, Pedisic Z. Workplace interventions for reducing sitting at work. Cochrane Database of Systematic Reviews 2018, Issue 6. [DOI: 10.1002/14651858.CD010912.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2017
- Smith A, Beales D, O'Sullivan P, Bear N, Straker L. Low back pain with impact at 17 years of age is predicted by early adolescent risk factors from multiple domains: analysis of the Western Australian Pregnancy Cohort (Raine) Study. Journal of Orthopaedic and Sports Physical Therapy 2017;47(10):752‐62. [DOI] [PubMed] [Google Scholar]
Srinivasan 2012
- Srinivasan D, Mathiassen SE. Motor variability in occupational health and performance. Clinical Biomechanics 2012;27:979‐93. [DOI] [PubMed] [Google Scholar]
Straker 2014
- Straker L, Healy G, Dunstan D, Atherton R. Excessive occupational sitting is not a 'safe system of work'. Medical Journal of Australia 2014;201:138‐40. [DOI] [PubMed] [Google Scholar]
Tan 2011
- Tan DA. Changing disease trends in the Asia‐Pacific. Climacteric 2011;14(5):529‐34. [DOI] [PubMed] [Google Scholar]
Thorp 2012
- Thorp A, Healy GN, Winkler E, Clark B, Gardiner P, Owen N, et al. Prolonged sedentary time and physical activity in workplace and non‐work contexts: a cross‐sectional study of office, customer service and call centre employees. International Journal of Behavioral Nutrition and Physical Activity 2012;9:128. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thorp 2014a
- Thorp A, Kingwell B, Owen N, Dunstan D. Breaking up workplace sitting time with intermittent standing bouts improves fatigue and musculoskeletal discomfort in overweight/obese office workers. Occupational and Environmental Medicine 2014;71:765‐71. [DOI] [PubMed] [Google Scholar]
Thorp 2014b
- Thorp A, Kingwell B, Sethi P, Hammond L, Owen N, Dunstan D. Alternating bouts of sitting and standing attenuates postprandial glucose responses. Medicine and Science in Sports and Exercise 2014;46:2053‐61. [DOI] [PubMed] [Google Scholar]
Tikkanen 2013
- Tikkanen O, Haakana P, Pesola AJ, Hakkinen K, Rantalainen T, Havu M, et al. Muscle activity and inactivity periods during normal daily life. PLoS One 2013;8:e52228. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tissot 2009
- Tissot F, Messing K, Stock S. Studying the relationship between low back pain and working postures among those who stand and those who sit most of the working day. Ergonomics 2009;52:1402‐18. [DOI] [PubMed] [Google Scholar]
Vallance 2011
- Vallance J, Winkler EAH, Gardiner P, Healy GN, Lynch B, Owen N. Associations of objectively‐assessed physical activity and sedentary time with depression: NHANES (2005 ‐ 2006). Preventive Medicine 2011;53(4):284‐8. [DOI] [PubMed] [Google Scholar]
van den Berg 2008
- Berg T, Elders L, Zwart B, Burdorf A. The effects of work‐related and individual factors on the work ability index: a systematic review. Occupational and Environmental Medicine 2008;66:211‐20. [DOI] [PubMed] [Google Scholar]
van Deursen 2005
- Deursen LL, Deursen DL, Snijders CJ, Wilke HJ. Relationship between everyday activities and spinal shrinkage. Clinical Biomechanics 2005;20:547‐50. [DOI] [PubMed] [Google Scholar]
Vernon 2008
- Vernon H. The Neck Disability Index: state‐of‐the‐art, 1991‐2008. Journal of Manipulative & Physiological Therapeutics 2008;31(7):491‐502. [DOI] [PubMed] [Google Scholar]
Viester 2013
- Viester L, Verhagen EALM, Hengel KMO, Koppes LLJ, Beek AJ, Bongers PM. The relation between body mass index and musculoskeletal symptoms in the working population. BMC Musculoskeletal Disorders 2013;14(1):1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Waersted 2010
- Waersted M, Hanvold TN, Veiersted KB. Computer work and musculoskeletal disorders of the neck and upper extremity: a systematic review. BMC Musculoskeletal Disorders 2010;11:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
Waongenngarm 2015
- Waongenngarm P, Rajaratnam BS, Janwantanakul P. Perceived body discomfort and trunk muscle activity in three prolonged sitting postures. Journal of Physical Therapy Science 2015;27:2183‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Waongenngarm 2018
- Waongenngarm P, Areerak K, Janwantanakul P. The effects of breaks on low back pain, discomfort, and work productivity in office workers: a systematic review of randomized and non‐randomized controlled trials. Applied Ergonomics 2018;68:230‐9. [DOI] [PubMed] [Google Scholar]
Widanarko 2011
- Widanarko B, Legg S, Stevenson M, Devereux J, Eng A, Mannetje A, et al. Prevalence of musculoskeletal symptoms in relation to gender, age, and occupational/industrial group. International Journal of Industrial Ergonomics 2011;41:561‐72. [Google Scholar]
References to other published versions of this review
Parry 2017b
- Parry, SP, Coenen, P, O'Sullivan, P, Maher, CG, Straker, LM. Workplace interventions for increasing standing or walking for decreasing musculoskeletal symptoms in sedentary workers. Cochrane Database of Systematic Reviews 2017, Issue na. [DOI: 10.1002/14651858.CD012487] [DOI] [PMC free article] [PubMed] [Google Scholar]


