Abstract
Background
According to the International Study of Asthma and Allergies in Childhood (ISAAC) methodology, in 2003, the prevalence of asthma symptoms in children 6–7 years old and adolescents 13–14 years old was 11.6% and 13.7%, respectively. Since then, the number of asthma cases has increased worldwide. The study was conducted in several districts in northern Mexico City to evaluate the prevalence of asthma in these age groups and examine possible risk factors. The data were compared to the 2003 results from the same area.
Methods
This was a comparative cross-sectional study following the official Global Asthma Network (GAN) methodology. The parents or guardians of participants completed a questionnaire that explored demographics, asthma symptoms, diagnoses, and possible risk factors. Central tendency measurements were determined for statistical analysis and chi-squared distribution for possible risk factors.
Results
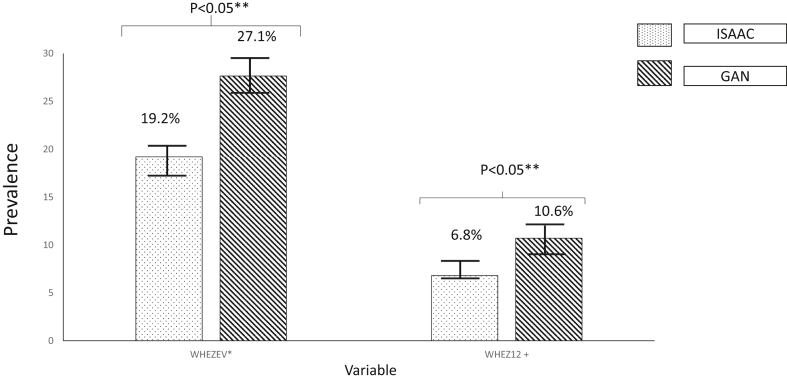
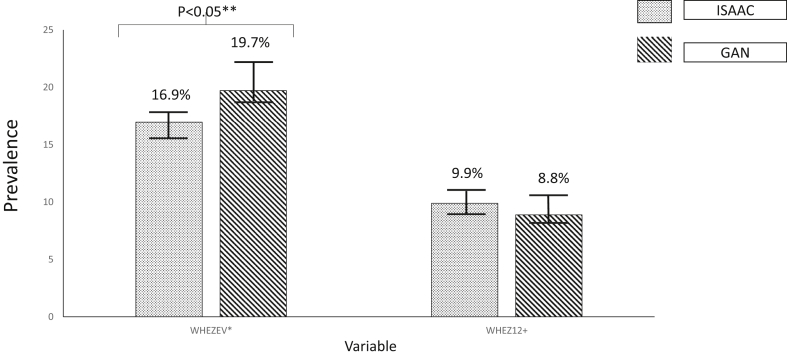
A total of 2515 children aged 6–7 years and 3375 adolescents aged 13–14 years participated in the study. Compared to the ISAAC results, we found a greater prevalence of wheezing in both children (at some time in life, 19.2% vs. 27.1%; over the last year, 6.8% vs. 10.6%) and adolescents (at some time in life, 16.9% vs. 19.7%), and for children with an asthma diagnosis (4.5% vs. 5.1%). For both groups, the most common risk factor associated with wheezing was the presence of rhinitis symptoms.
Conclusions
Asthma symptoms are highly prevalent in Mexico City, occurring in almost 20% of adolescents. Compared to a decade ago, there was a 7.9% increase in the prevalence of asthma symptoms in children. Almost half of the children and adolescents presenting with symptoms had experienced more than four episodes per year. However, less than 50% of children and adolescents with asthma symptoms had been diagnosed with this disorder, suggesting under-diagnosis.
Keywords: Asthma, Atopic allergic diseases, Wheezing, Rhinitis, Risk factors, ISAAC, GAN
Abbreviations: Isaac, International Study of Asthma and Allergies in Childhood; Gan, Global Asthma Network; Himfg, Hospital Infantil de México Federico Gómez
BACKGROUND
Asthma is now considered one of the main chronic illnesses worldwide,1 affecting more than 300 million people.2 According to several studies, the prevalence of asthma has increased in many countries over the past decade.3,4 Asthma is associated with other atopic allergic diseases, including allergic rhinitis and atopic dermatitis, the prevalence of which has also increased, though to a lesser extent, over the past 10 years.4
Despite the many insights into asthma over the past few decades, the reasons behind the greater prevalence are still not clear. Genetics are known to play an important role, as well as environmental factors. Diet and exposure to microorganisms, pollutants, and allergens also contribute to the development of this condition in genetically predisposed individuals.5 Some hypotheses have been formulated with regard to asthma. One suggests immunological mechanisms that manifest as an imbalance in the Th1–Th2 immune response6 and related to changes in the epithelial microbiome. Another hypothesis proposes the involvement of obesity and other nutritional factors during in utero formation and after birth.
The International Study of Asthma and Allergies in Childhood (ISAAC), which began in 1991, was the first multinational effort to research the prevalence of asthma and other allergic conditions in different countries around the world. It was carried out in three phases from 1992 to 2003. A validated, standardized questionnaire was applied to two age groups at distinct places around the world (translated into the appropriate language): children aged 6–7 years and adolescents aged 3–14 years.7 The study described the prevalence and severity of asthma, rhinitis, and eczema in various regions, examined risk factors, and evaluated temporary trends in the prevalence of these conditions.
The last phase of ISAAC included a total of 1,059,053 children from 236 centres in 98 countries.8 The prevalence of asthma symptoms was 13.7% in the older group and 11.6% in the younger group. Substantial variations were detected in the prevalence of the three illnesses, even among subjects with similar genetic backgrounds. Consideration was given to possible protective factors (vegetable consumption and immunization for DPT and measles) and aggravating factors (the presence of certain kinds of pollen, climactic factors, and outdoor pollution). The identified risk factors were the gross national income (GNI) of a country, climatic factors, the consumption of acidic trans fats, and the use of paracetamol and antibiotics. The prevalence of asthma symptoms increased at a similar or higher rate in developing and developed countries.9
Due to the success of the ISAAC program, the Global Asthma Network (GAN) was created in 2012 with the objective of approaching asthma as a significant, worldwide, non-contagious disease. Meanwhile, the existing multinational collaboration projects continued their research into the variations in asthma prevalence in children and adolescents, focusing on the same populations involved in the ISAAC study.
The current study was part of the GAN initiative and aimed to update the prevalence rates of asthma in Mexico City and examine the most relevant risk factors associated with this disease.
Materials and methods
A comparative cross-sectional study was carried out in school-aged populations of children 6–7 years old and adolescents 13–14 years old at the No. 515002 GAN Centre. This location corresponds to the northern region of Mexico City, including the districts of Azcapotzalco, Miguel Hidalgo, Gustavo A. Madero, and Venustiano Carranza. After providing informed consent, parents completed validated and standardized questionnaires given by GAN's global coordination for the younger group, and the older group completed the questionnaires by themselves.10
Following the official GAN protocol,10 the sample unit was the whole population of children aged 6–7 years or adolescents aged 13–14 years in a given school. The schools were within a certain geographical radius of the study centre and were chosen randomly based on the school register (organized in alphabetical order). A minimum of 10 schools were necessary to obtain a representative sample, with a projected sample size of 3000 (a minimum of 1000) subjects per age group. This sample size gave the study enough statistical power to detect significant epidemiological differences in the prevalence and severity of asthma symptoms11 and complied with the guidelines of the ISAAC methodology.
The questionnaires focused on three areas (Supplemental Tables S1 and S2). Demographic factors were explored, including the age, date of birth, education level, and gender of the children. Specific questions were asked about asthma, including the existence of wheezing at some time in life and over the past year and the diagnosis of asthma by a doctor. The risk factors examined were the presence of rhinitis or eczema, the use of paracetamol and/or antibiotics, consumption of basic foodstuffs, education level of the mother, diagnosis of pneumonia, and exposure to cigarette smoke.
A period of 3 days was allowed for returning the questionnaire. After this period, the anthropometric parameters of the participants were established. Weight was measured on an 804 Seca digital scale and height with a portable Frankfort 213 Seca stadiometer. Waist measurements were taken at the mid-point between the last rib and the iliac crest with an inelastic measuring tape (without applying pressure). The subjects were in a standing position, feet together, arms at their sides, and abdomen relaxed. They were asked to inhale deeply and the measurement taken upon exhalation.
Data entry for the electronic GAN database was done by the medical personnel at the study center, with random selection of 10% of the questionnaires on two occasions to ensure that the margin of error was less than 1%. To limit possible mistakes in the data entry process, the electronic data were cross-checked with the original physical questionnaires. The methodology for the ISAAC study in northern Mexico City, which was described previously12 was used. The present investigation was conducted by the same researchers involved in the previous study, allowing a comparison of both results to the original databases. The GAN and ISAAC databases were reviewed by the GAN and ISAAC committees, respectively, before performing statistical analyses.
Central tendency measurements (the average ± standard deviation [SD] and 95% confidence interval [CI]) were obtained for analysis of the accumulated and current prevalence of symptoms and diagnosis of asthma and asthma severity. For qualitative variables, the chi-squared test was used.
The variables WHEZ12 (current wheeze) and ASTHMAEV (a previous asthma diagnosis) were chosen to examine the risk factors for asthma. Subsequently, factors that were likely to increase or decrease the prevalence of these two variables were identified (p ≤ 0.10) with the chi-squared test and Fisher correction on 2 × 2 tables. These factors were analysed by conditional logistic regression to create models that better explain WHEZ12 and ASTHMAEV risk.
Microsoft Excel 2016 v16.0.6568.2036 (Microsoft Corporation) was used to organize data and IBM SPSS Statistics v20.0 (SPSS Inc., IBM Company) for statistical analysis. The present study was approved by the Ethics, Research, and Biosafety committees of the Hospital Infantil de México Federico Gómez (HIMFG, protocol #HIM/2015/059) in accordance with the guidelines of the institution.
Results
A total of 2900 children and 3600 adolescents from 67 schools were asked to participate in the study. The actual number of participants was 2515 children aged 6–7 years (44.9% male, 55.1% female) and 3375 adolescents aged 13–14 years (47.5% male, 52.5% female). The response rate to the questionnaire was 90%.
For the younger group, wheezing (ever or current wheeze) was more common in the present GAN data than in the ISAAC results for both male and female subjects (Fig. 1, Table 1). In the adolescent group, a similar significant increase was observed for the GAN versus the ISAAC study, but only in relation to the prevalence of wheezing at some point during life (WHEZEV). Females were affected more than males, especially with regard to asthma symptoms at some time in life (Fig. 2, Table 1). Interestingly, there was a much higher frequency of wheezing during both time periods than a previous asthma diagnosis with respect to both age groups and genders. Asthma symptoms assessed by WHEZEV were more frequent in male children than in female children. However, in adolescents, WHEZEV and WHEZ12 were more common in females (Table 1).
Fig. 1.
Prevalence of wheezing any time in the past and wheezing in the past 12 months in children (6–7 years) from northern Mexico City. ISAAC (2003) vs. GAN (2017). *WHEZEV: Wheezing or whistling in the chest at any time in the past. +WHEZ12: Wheezing or whistling in the chest in the past 12 months. ** Chi2 Fisher Test
Table 1.
Prevalence and severity of asthma symptoms in children and teenagers from the northern area of Mexico City, ISAAC vs. GAN.
| Variable | 6 and 7 years old |
13 and 14 years old |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| ISAAC |
GAN |
ISAAC |
GAN |
||||||
| N | Frequency, % (95% CI) | N | Frequency, % (95% CI) | N | Frequency, % (95% CI) | N | Frequency, % (95% CI) | ||
| WHEZEV | Men | 350/1626 | 21.5 (19.7–23.7) | 337/1130 | 29.8 (27.2–32.5) | 311/2036 | 15.3 (13.8–16.9) | 264/1602 | 16.5 (14.7–18.3) |
| Women | 266/1579 | 16.8 (15.1–18.8) | 345/1385 | 24.9 (22.6–27.2) | 348/1855 | 18.8 (17.0–20.6) | 400/1773 | 22.6 (20.7–24.6) | |
| Both | 616/3205 | 19.2 (17.9–20.6) | 682/2515 | 27.1 (25.4–28.9) | 659/3891 | 16.9 (15.8–18.1) | 664/3375 | 19.7 (18.4–21.1) | |
| WHEZ12 | Men | 116/1626 | 7.1 (6.0–8.5) | 137/1130 | 12.1 (10.2–14.0) | 168/2036 | 8.3 (7.1–9.5) | 104/1602 | 6.4 (5.4–7.8) |
| Women | 101/1579 | 6.4 (5.3–7.7) | 129/1385 | 9.3 (7.8–10.8) | 217/1855 | 11.7 (10.3–13.2) | 196/1773 | 11.0 (9.7–12.6) | |
| Both | 217/3205 | 6.8 (5.9–7.7) | 266/2515 | 10.6 (9.4–11.8) | 385/3891 | 9.9 (9.0–10.9) | 300/3375 | 8.8 (8.0–9.9) | |
| ASTHMAEV | Men | 90/1626 | 5.5 (4.5–6.8) | 66/1130 | 5.8 (4.5–7.2) | 150/2036 | 7.4 (6.3–8.6) | 121/1602 | 7.5 (6.3–8.9) |
| Women | 54/1579 | 3.4 (2.6–4.4) | 63/1385 | 4.7 (3.6–5.8) | 160/1855 | 8.6 (7.4–10.0) | 129/1773 | 7.3 (6.2–8.6) | |
| Both | 144/3205 | 4.5 (3.8–5.3) | 129/2515 | 5.1 (4.3–6.0) | 310/3891 | 8.0 (7.2–8.9) | 250/3377 | 7.4 (6.6–8.3) | |
| ASTHDOC | Men | NI | NI | 59/1130 | 5.2 (3.9–6.5) | NI | NI | 93/1602 | 5.8 (4.8–7.0) |
| Women | NI | NI | 51/1385 | 3.7 (2.7–4.7) | NI | NI | 93/1773 | 5.2 (4.3–6.4) | |
| Both | NI | NI | 110/2515 | 4.4 (3.6–5.2) | NI | NI | 186/3375 | 5.5 (4.8–6.3) | |
| SPEECH12 | Men | 26/1624 | 1.6 (1.0–2.2) | 53/1130 | 4.7 (3.5–5.9) | 64/2036 | 3.1 (2.4–3.9) | 40/1602 | 2.5 (1.8–3.4) |
| Women | 25/1578 | 1.6 (1.0–2.2) | 35/1385 | 2.5 (1.7–3.4) | 97/1855 | 5.2 (4.2–6.2) | 96/1773 | 5.4 (4.4–6.6) | |
| Both | 51/3202 | 1.6 (1.2–2.0) | 88/2515 | 3.5 (2.8–4.2) | 161/3891 | 4.1 (3.5–4.8) | 136/3375 | 4.0 (3.4–4.7) | |
| NWHEZ12 | 1–3 | 173/3202 | 5.4 (4.6–6.2) | 243/2515 | 9.7 (8.5–10.8) | 247/3888 | 6.4 (5.6–7.1) | 283/3375 | 8.4 (7.5–9.3) |
| 4–12 | 26/3202 | 0.8 (0.5–1.1) | 29/2515 | 1.2 (0.7–1.6) | 97/3888 | 2.5 (2.0–3.0) | 46/3375 | 1.4 (1.0–1.8) | |
| >12 | 2/3202 | 0.1 (0.0–0.1) | 4/2515 | 0.2 (0.0–0.3) | 17/3888 | 0.4 (0.2–0.6) | 8/3375 | 0.2 (0.1–0.4) | |
| AWAKE12 | <1 NIGHT/W |
107/3200 | 3.3 (2.7–4.0) | 131/2515 | 5.2 (4.3–6.1) | 72/3890 | 1.9 (1.4–2.3) | 136/3375 | 4.0 (3.4–4.7) |
| ≥1 NIGHT/W |
32/3200 | 1.0 (0.7–1.3) | 48/2515 | 1.9 (1.4–2.4) | 28/3890 | 0.7 (0.5–1.0) | 21/3375 | 0.6 (0.4–0.9) | |
WHEZEV- Has this child ever had wheezing or whistling in the chest at any time in the past? WHEZ12- Has this child had wheezing or whistling in the chest in the past 12 months? ASTHMAEV- Has this child ever had asthma? ASTHMADOC- Was this child's asthma confirmed by a doctor? SPEECH12- In the past 12 months, has wheezing ever been severe enough to limit this child's speech to only one or two words at a time between breaths? NWHEZ12- How many attacks of wheezing has this child had in the past 12 months? AWAKE12- In the past 12 months, how often, on average, has this child's sleep been disturbed due to wheezing? NI- No information, NIGHT/W - Night for a week
Fig. 2.
Prevalence of wheezing any time in the past and wheezing in the past 12 months in teenagers (13–14 years old) from northern Mexico City. ISAAC (2003) vs. GAN (2017). *WHEZEV: Wheezing or whistling in the chest at any time in the past. +WHEZ12: Wheezing or whistling in the chest in the past 12 months. **Chi2 Fisher Test
The variables linked to asthma severity were compared between the GAN (2017) and ISAAC (2003) data, utilizing the questions evaluating the intensity of NWHEZ12 (number of wheezing episodes in the last 12 months), AWAKE12 (number of times that the child/adolescent's sleep has been disturbed due to wheezing), and SPEECH12 (difficulties with speech caused by wheezing) (Table 1). Almost double the number of children of both sexes reported 1–3 wheezing episodes over the past year in the GAN data than the ISAAC data. In addition, more participants in this study reported sleep interrupted by wheezing (especially for males; data not shown) and difficulties with speech caused by wheezing (both sexes) than in the previous study. For adolescents, the number of female subjects with 1–3 wheezing episodes over the past year was increased in GAN vs. ISAAC.
In both genders, there were significant increases in children in the frequency of WHEZEV, SPEECH12, NWHEZE12 (1–3 times a week), and AWAKE12 (≥1 times per week), but not ASTHMAEV (Table 1), in GAN compared to ISAAC. In contrast, in the adolescents, the only significant increases between ISAAC and GAN were in WHEZEV and NWHEZE12 (1–3 times a week) (Table 1).
The presence of hay fever, eczema, early infections, tobacco use at home, and paracetamol use are possible risk factors for WHEZEV and WHEZ12 in both groups. In 2003, the analysis showed a higher risk of wheezing over the past year for participants diagnosed with allergic rhinitis (hay fever), those with symptoms of allergic rhinitis (e.g., sneezing, rhinorrhoea, or obstruction), and those diagnosed with atopic dermatitis (Table 2). Other risk factors include the use of antibiotics during the first year of life, having had a cat during the first year of life, and the administration of paracetamol for a fever over the past year.
Table 2.
Evaluation of risk factors for current and accumulated prevalence of asthma in the 6-7-year age group, ISAAC vs. GAN.
| Risk factor | ISAAC |
GAN |
|||
|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | ||
| Wheezing in the past 12 months | Hay fever symptoms in the last 12 months. | 2.99 (2.10–4.26) | 0.000 | 3.24 (2.34–4.48) | 0.000 |
| Diagnosis of hay fever ever | 3.00 (1.89–4.75) | 0.000 | NS | NS | |
| Diagnosis of eczema ever | 2.06 (1.44–2.97) | 0.000 | NS | NS | |
| Wheezing during their first year of life | NI | NI | 2.53 (1.79–3.57) | 0.000 | |
| Diagnosis of pneumonia or bronchopneumonia at least one time in their life | NI | NI | 2.05 (1.27–3.30) | 0.003 | |
| Use of antibiotics in the first 12 months of life | 1.85 (1.25–2.73) | 0.002 | NS | NS | |
| Use of paracetamol for fever in the last 12 months | 1.99 (1.49–2.67) | 0.000 | 1.11 (0.99–1.25) | 0.071 | |
| Cat at home in the first year of life | 1.67 (1.09–2.57) | 0.018 | NS | NS | |
| Mother with college, university, or another form of tertiary education concluded | 1.62 (1.16–2.25) | 0.004 | NI | NI | |
| Family background of changes at home to prevent symptoms of allergies, asthma, or breathing problems. | NI | NI | 0.30 (0.38–0.40) | 0.000 | |
| Weekly consumption of rice | NS | NS | 0.80 (0.62–1.03) | 0.096 | |
| Weekly consumption of soft drink | NI | NI | 1.11 (0.99–1.25) | 0.071 | |
| Age | NS | NS | 0.67 (0.48–0.94) | 0.020 | |
| Wheezing at any time in the past | Hay fever symptoms ever | 2.44 (1.56–3.81) | 0.000 | 3.11 (2.00–4.83) | 0.000 |
| Diagnosis of hay fever ever | 3.61 (2.12–6.15) | 0.000 | NS | NS | |
| Diagnosis of eczema ever | 2.06 (1.13–3.75) | 0.018 | NS | NS | |
| Diagnosis of pneumonia or bronchopneumonia ever | NI | NI | 2.63 (1.55–4.47) | 0.000 | |
| At least one chest infection in the first year of life | NI | NI | 1.21 (0.96–1.52) | 0.096 | |
| Child treated with inhaled and/or oral medicines for breathing problems during the first year of life | NI | NI | 1.80 (1.06–3.03) | 0.027 | |
| Use of paracetamol for fever in the first 12 months of life | 1.49 (0.98–2.26) | 0.061 | NS | NS | |
| Use of paracetamol for fever in the last 12 months | 1.46 (1.01–2.09) | 0.040 | NS | NS | |
| Use of antibiotics in the first 12 months of life | 1.74 (1.07–2.84) | 0.025 | NS | NS | |
| Mother with secondary school concluded | 2.60 (1.27–5.34) | 0.009 | NI | NI | |
| Mother with college, university, or another form of tertiary education concluded | 1.75 (1.18–2.60) | 0.005 | NI | NI | |
| Weekly consumption of pasta | 0.66 (0.51–0.86) | 0.002 | NS | NS | |
| Family background of changes at home to prevent symptoms of allergies, asthma, or breathing problems. | NI | NI | 0.26 (0.18–0.37) | 0.000 | |
NI: No information, NS: Not significant
The results from 2017 demonstrate the same trends for some of the risk factors, including the prevalence of rhinitis symptoms or wheezing over the past year. However, the results were different for the diagnosis of rhinitis or atopic dermatitis. Having been diagnosed with pneumonia at least once increased the risk of asthma symptoms over the past year (Table 2). Regarding an asthma diagnosis, the protective effect of changes made in the household to mitigate allergy or asthma symptoms was significant. This variable, which was not included in the 2003 ISAAC study, was added to the GAN questionnaire.
For adolescents in both the ISAAC and GAN studies, nasal symptoms (e.g., sneezing, rhinorrhoea, or nasal obstruction) increased the risk of wheezing episodes over the past year (Table 3). There was also a greater risk of a diagnosis of asthma in subjects previously diagnosed with rhinitis, which was not evaluated in the ISAAC study.
Table 3.
Evaluation of risk factors for current and accumulated prevalence of asthma in the 13-14-year age group, ISAAC vs. GAN.
| Risk factor | ISAAC |
GAN |
|||
|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | ||
| Wheezing in the past 12 months | Hay fever symptoms in the last 12 months | 2.39 (1.90–3.02) | 0.000 | 2.03 (1.33–3.08) | 0.001 |
| Diagnosis of hay fever confirmed by a doctor | NI | NI | 2.46 (1.62–3.75) | 0.000 | |
| Presence of itchy rash in the past 12 months | 1.89 (1.34–2.65) | 0.000 | NS | NS | |
| Diagnosis of eczema ever | NS | NS | 2.32 (1.63–3.31) | 0.000 | |
| Use of paracetamol for fever in the last 12 months | 1.22 (1.04–1.43) | 0.015 | 1.12 (1.01–1.25) | 0.022 | |
| Background of smoking tobacco on a daily basis or less than daily | NI | NI | 1.98 (1.43–2.75) | 0.000 | |
| The frequency of trucks passing by their street | 1.19 (1.07–1.32) | 0.001 | NS | NS | |
| Mother with college, university, or another form of tertiary education concluded | 0.63 (0.46–0.88) | 0.007 | NI | NI | |
| Hours a day watching television per week | 1.20 (1.02–1.41) | 0.006 | NS | NS | |
| Weekly consumption of meat | 1.34 (1.13–1.58) | 0.001 | NS | NS | |
| Weekly consumption of seafood | 0.73 (0.61–1.50) | 0.001 | NS | NS | |
| Weekly consumption of fruit | 1.26 (1.05–1.50) | 0.009 | NS | NS | |
| Weekly consumption of pulses | 0.86 (0.73–1.00) | 0.061 | NS | NS | |
| Weekly consumption of pasta | 1.18 (1.01–1.39) | 0.034 | 1.25 (1.02–1.53) | 0.026 | |
| Weekly consumption of rice | 1.42 (1.20–1.69) | 0.000 | NS | NS | |
| Weekly consumption of eggs | 1.20 (1.02–1.41) | 0.026 | NS | NS | |
| Sex | 1.28 (1.02–1.60) | 0.033 | 1.39 (1.05–1.84) | 0.019 | |
| Wheezing at any time in the past | Hay fever symptoms in the last 12 months. | 2.61 (2.04–3.33) | 0.000 | NS | NS |
| Diagnosis of hay fever ever | 2.23 (1.55–3.20) | 0.000 | 2.54 (1.34–4.81) | 0.004 | |
| Diagnosis of hay fever confirmed by a doctor | NI | NI | 2.49 (1.28–4.86) | 0.007 | |
| Diagnosis of eczema ever | NS | NS | 1.64 (1.02–2.62) | 0.038 | |
| Use of paracetamol for fever in the last 12 months | 1.23 (1.04–1.47) | 0.015 | NS | NS | |
| Mother with history of smoking cigarettes | 1.34 (1.03–1.75) | 0.026 | NI | NI | |
| Cat at home in the past 12 months | NS | NS | 1.39 (1.00–1.91) | 0.045 | |
| Hours a day watching television per week | NS | NS | 1.15 (1.00–1.32) | 0.046 | |
| Weekly consumption of seafood | 1.41 (1.23–1.63) | 0.000 | NS | NS | |
| Weekly consumption of fast food/burgers | NS | NS | 1.34 (1.08–1.65) | 0.006 | |
NI: No information, NS: Not significant
Discussion
Epidemiological studies conducted in the 1980s–1990s found important increases in asthma and asthma symptoms in the Western world and Asia, but after the 1990s, the trends in these symptoms were contradictory; in some countries, the prevalence of asthma was still increasing, whereas in others it seemed to be stable or even decreasing slightly.13 In the ISAAC phase three study, centers previously reporting a low prevalence demonstrated an increase in current asthma symptoms, whereas the centers with a higher baseline prevalence had decreases, particularly in English-speaking countries and Western Europe.7,14
Other surveys conducted after ISAAC phase three have also found the prevalence to be stabilizing and a decrease in asthma prevalence in Western countries and Asia. For example, using 2001–2016 National Health Interview Survey data for children aged 0–17 years, current asthma prevalence in the United States increased from 8.7% in 2001 to 9.4% in 2010, followed by a plateau until 2013, and then decreased to 8.3% by 2016.15,16
Repeated surveys in the southeast Netherlands conducted in 1989, 1993, 1997, 2001, 2005, and 2010 demonstrated a decreased prevalence of current asthma symptoms in children from 1989 (13.4%) to 2001 (7.4%), with no significant change up to 2010 (6.2%).17,18 Similarly, in South Korea, a 6-year nationwide survey found a decrease in the prevalence of current asthma symptoms from 2009 (20%) to 2014 (13.2%) in children aged <10 years.19
In the present study, there was a frank increase in asthma symptoms and asthma severity in children. In the adolescent group, the only significant increases were in WHEZEV and NWHEZ12. Therefore, northern Mexico City has a mixed pattern of asthma prevalence increase in children and a possible stabilization in adolescents. This study is among the first reports to compare the prevalence of asthma symptoms between ISAAC and GAN.
It has not been easy to identify the factors underlying the epidemiological changes. Some factors have been explored in ISAAC and GAN, such as changes in diet, time spent using screens (computers and video games), second-hand smoke, and the presence of pollutants.10,20
In the present study, possible risk factors identified for WHEZEV and WHEZ12 were the presence of other allergic diseases (hay fever and eczema), early infections, smoking at home, and paracetamol use. These patterns have been described previously; for example, the evolution of allergic sensitization followed by atopic dermatitis, allergic rhinitis, and asthma have been demonstrated in several epidemiological studies.21,22 A possible explanation for the association of atopic dermatitis, allergic rhinitis, and asthma could be the filaggrin loss-of-function mutations. Filaggrin is a skin epidermal protein that contributes to the natural skin barrier protecting against transcutaneous water loss, as well as preventing the entry of environmental allergens through the skin. Filaggrin loss-of-function mutations provoke epidermal barrier dysfunction, increasing the risk of eczema. These mutations are also associated with allergic sensitization and airway allergy, expressed as allergic rhinitis and asthma later in childhood.23
The relationship between passive tobacco smoke and asthma in children has been well-established by studying the levels of serum cotinine and the prevalence of asthma. High exposure to second-hand tobacco smoke is related to high risk of asthma, asthma exacerbations, and poorly controlled asthma in children.24,25
The use of paracetamol, perinatally and currently, has also been associated with allergic conditions, especially with asthma,26,27 but this association could be explained by confounding factors, such as fever and respiratory infections.27
How can we explain the differences in asthma symptom prevalence in different cities, regions, and countries? It is possible that all populations with Western life styles follow the same pattern of asthma evolution, but in different stages. In underdeveloped countries, the prevalence of asthma symptoms should increase, and then plateau and decrease over the subsequent years.
The ISAAC and GAN studies have tried to explore the possible causes of the heterogeneity in asthma prevalence. Yet, other factors should be considered in future studies, including exposure to pollutants of different kinds and sizes; changes in pollination patterns and type of flora; microbiome fluctuations; and the history, evolution, and aetiology of respiratory infections and parasitic diseases.
Conclusions
The prevalence of asthma in Mexico City is now higher than the prevalence in 2003. Almost 20% of adolescents present with symptoms of asthma at least once in their lifetime. Since the ISAAC study performed over a decade ago, there has been a 7.8% increase in the prevalence of asthma symptoms in children. Almost half of the children and adolescents presenting with asthma symptoms had experienced more than four episodes per year. However, less than 50% of children and adolescents with asthma symptoms were diagnosed with asthma, suggesting under-diagnosis.
Ethics approval and consent to participate
The authors declare that all procedures were carried out in accordance with the ethical standards of the institutional committee on human investigation, the World Medical Association, and the Helsinki Declaration.The authors obtained informed consent from the parents or guardians of participants in the study. The corresponding author accepts responsibility for this manuscript.The present study was approved by the Ethics, Research, and Biosafety committees of the Hospital Infantil de México Federico Gómez (HIMFG, protocol #HIM/2015/059) in accordance with the guidelines of the institution.
Consent for publication
Not applicable.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Funding
The financing to carry out this project came from the resources of the researchers, as well as a donation from AstraZeneca laboratory to cover the costs of printing the questionnaires and data entry.
Authors' contributions
DRNBE - Made substantial contributions to conception, design, and acquisition of data.
NREM - Made substantial contributions to design, acquisition of data and drafting the manuscript.
BA - Made substantial contributions to the analysis and interpretation of data.
RNN - Made substantial contributions to design and acquisition of data.
GMAL - Involved in revising it critically for important intellectual content.
GAR - Made substantial contributions to conception and design.
MPJV - Made substantial contributions to conception and design.
SROJ - Involved in revising it critically for important intellectual content.
DRCJM - Involved in revising it critically for important intellectual content.
SMJJL - Involved in revising it critically for important intellectual content.
Declaration of competing interest
The authors declare that they have no conflict of interest in relation to the methods or materials employed in this study.
Acknowledgments
The authors thank AstraZeneca for their support in carrying out this project, specifically for the financial aid to cover the costs of printing the questionnaires and data entry. The authors thank The Global Asthma Network Steering Group especially Philippa Ellwod and Innes Asher for their constant help with our research.
Footnotes
Full list of author information is available at the end of the article
Supplementary data to this article can be found online at https://doi.org/10.1016/j.waojou.2019.100092.
Contributor Information
Elsy Maureen Navarrete-Rodríguez, Email: draenavarrete@gmail.com.
Grupo GAN México, Grupo ISAAC México:
Roberto García-Almaraz, Juan Valente Mérida-Palacio, Omar Josué Saucedo-Ramirez, Jaime Mariano Del-Rio-Chivardi, and Juan Jose Luis Sienra-Monge
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Asher I., Pearce N. Global burden of asthma among children. Int J Tuberc Lung Dis. 2014;18(11):1269–1278. doi: 10.5588/ijtld.14.0170. [DOI] [PubMed] [Google Scholar]
- 2.Pawankar R., Canonica G.W., ST Holgate S.T., Lockey R.F., Blaiss M. 2013. The WAO White Book on Allergy. [Google Scholar]
- 3.Global Initiative for Asthma . 2017. Global Strategy for Asthma Management and Prevention.www.ginasthma.org Available from: [Google Scholar]
- 4.Downs S.H., Marks G.B., Sporik R., Belosouva E.G., Car N.G., Peat Jk. Continued increase in the prevalence of asthma and atopy. Arch Dis Child. 2001 Jan;84(1):20–23. doi: 10.1136/adc.84.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Braman S.S. The global burden of asthma. Chest. 2006 Jul;130(1 Suppl):4S–12S. doi: 10.1378/chest.130.1_suppl.4S. [DOI] [PubMed] [Google Scholar]
- 6.Toskala E., Kennedy D.W. Asthma risk factors. Int forum Allergy Rhinol. 2015 Sep;5(Suppl 1):S11–S16. doi: 10.1002/alr.21557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Asher M.I., Montefort S., Bjorksten B., ISAAC Phase Three Study Group Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet. 2006 Aug 26;368(9537):733–743. doi: 10.1016/S0140-6736(06)69283-0. [DOI] [PubMed] [Google Scholar]
- 8.Aït-Khaled N., Pearce N., Anderson H.R., Ellwood P., Montefort S., Shah J., the ISAAC Phase Three Study Group Global map of the prevalence of symptoms of rhinoconjunctivitis in children: the international study of asthma and Allergies in childhood(ISAAC) phase three. Allergy. 2009;64:123–148. doi: 10.1111/j.1398-9995.2008.01884.x. [DOI] [PubMed] [Google Scholar]
- 9.Mallol J., Crane J., von Mutius E., Odhiambo J., Keil U., Stewart A., ISAAC Phase Three Study Group The international study of asthma and Allergies in childhood (ISAAC) phase three: a global synthesis. Allergol Immunopathol. 2013 Mar-Apr;41(2):73–85. doi: 10.1016/j.aller.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 10.Ellwood P., Asher M.I., Billo N.E. The Global Asthma Network rationale and methods for Phase I global surveillance: prevalence, severity, management and risk factors. Eur Respir J. 2017 Jan 11;49(1) doi: 10.1183/13993003.01605-2016. 1601605. [DOI] [PubMed] [Google Scholar]
- 11.ISAAC Steering Committee . second ed. ISAAC Phase One Manual; Auckland/Münster: 1993. International Study of Asthma and Allergies in Childhood. [Google Scholar]
- 12.Del-Rio-Navarro B., Del Rio-Chivardi J.M., Berber A., Sienra-Monge J.J., Rosas-Vargas M.A., Baea-Bacab M. Asthma prevalence in children living in north Mexico City and a comparison with other Latin American cities and world regions. Allergy Asthma Proc. 2006 Jul-Aug;27(4):334–340. doi: 10.2500/aap.2006.27.2880. [DOI] [PubMed] [Google Scholar]
- 13.Eder W., Ege M.J., von Mutius E. The asthma epidemic. N Engl J Med. 2006;355(21):2226–2235. doi: 10.1056/NEJMra054308. [DOI] [PubMed] [Google Scholar]
- 14.Pearce N., Aït-Khaled N., Beasley R. Worldwide trends in the prevalence of asthma symptoms: phase III of the international study of asthma and allergies in childhood (ISAAC) Thorax. 2007;62(9):758–766. doi: 10.1136/thx.2006.070169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Akinbami L.J., Simon A.E., Rossen L.M. Changing trends in asthma prevalence among children. Pediatrics. 2016;137(1):1–7. doi: 10.1542/peds.2015-2354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zahran H.S., Bailey C.M., Damon S.A., Garbe P.L., Breysse P.N. Vital signs: asthma in children - United States, 2001-2016. MMWR Morb Mortal Wkly Rep. 2018;67(5):149–155. doi: 10.15585/mmwr.mm6705e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mommers M., Gielkens-Sijstermans C., Swaen G.M., van Schayck C.P. Trends in the prevalence of respiratory symptoms and treatment in Dutch children over a 12 year period: results of the fourth consecutive survey. Thorax. 2005;60(2):97–99. doi: 10.1136/thx.2004.024786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Korte-de Boer D., Mommers M., Gielkens-Sijstermans C.M. Stabilizing prevalence trends of eczema, asthma and rhinoconjunctivitis in Dutch schoolchildren (2001-2010) Allergy. 2015;70(12):1669–1673. doi: 10.1111/all.12728. [DOI] [PubMed] [Google Scholar]
- 19.Kim B.K., Kim J.Y., Kang M.K. Allergies are still on the rise? a 6-year nationwide population-based study in Korea. Allergol Int. 2015;65(2):186–191. doi: 10.1016/j.alit.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 20.Asher M.I., Keil U., Anderson H.R. International study of asthma and allergies in childhood (ISAAC): rationale and methods. Eur Respir J. 1995;8(3):483–491. doi: 10.1183/09031936.95.08030483. [DOI] [PubMed] [Google Scholar]
- 21.Tran M.M., Lefebvre D.L., Dharma C. Canadian healthy infant longitudinal development study investigators. Predicting the atopic march: results from the Canadian healthy infant longitudinal development study. J Allergy Clin Immunol. 2018;141(2):601–607. doi: 10.1016/j.jaci.2017.08.024. [DOI] [PubMed] [Google Scholar]
- 22.Lau S., Matricardi P.M., Wahn U., Lee Y.A., Keil T. Allergy and atopy from infancy to adulthood: messages from the German birth cohort MAS. Ann Allergy Asthma Immunol. 2018;(18):25–32. doi: 10.1016/j.anai.2018.05.012. pii: S1081-1206. [DOI] [PubMed] [Google Scholar]
- 23.Chan A., Terry W., Zhang H. Filaggrin mutations increase allergic airway disease in childhood and adolescence through interactions with eczema and aeroallergen sensitization. Clin Exp Allergy. 2018;48(2):147–155. doi: 10.1111/cea.13077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang X., Johnson N., Carrillo G., Xu X. Decreasing trend in passive tobacco smoke exposure and association with asthma in U.S. children. Environ Res. 2018;166:35–41. doi: 10.1016/j.envres.2018.05.022. [DOI] [PubMed] [Google Scholar]
- 25.Neophytou A.M., Oh S.S., White M.J. Secondhand smoke exposure and asthma outcomes among African-American and Latino children with asthma. Thorax. 2018 Nov;73(11):1041–1048. doi: 10.1136/thoraxjnl-2017-211383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Magnus M.C., Karlstad Ø., Håberg S.E., Nafstad P., Davey Smith G., Nystad W. Prenatal and infant paracetamol exposure and development of asthma: the Norwegian Mother and Child Cohort Study. Int J Epidemiol. 2016;45(2):512–522. doi: 10.1093/ije/dyv366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lourido-Cebreiro T., Salgado F.J., Valdes L., Gonzalez-Barcala F.J. The association between paracetamol and asthma is still under debate. J Asthma. 2017;2(1):32–38. doi: 10.1080/02770903.2016.1194431. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.