Abstract
We report a case of a right retroperitoneal hematoma compressing the inferior vena cava (IVC) in a patient with a left pelvic renal transplant. Noncontrast abdominal computed tomography scan diagnosed the cause of the hematoma, which was a ruptured nontraumatic renal cyst hemorrhage from the right native kidney. The patient had been anticoagulated for 5 days to treat pulmonary embolism upon clinical presentation. To minimize the risk of venous renal transplant thrombosis and to resume anticoagulation as fast as possible without the need of a long-term IVC filter, priority in management was to relieve the IVC compression and to stop the hemorrhage by selective embolization of the right native kidney. This case report will review the clinical presentation, the radiological findings and the management of retroperitoneal hematoma compressing the IVC in a patient with renal transplant.
Keywords: Retroperitoneal hematoma, Inferior vena cava obstruction, Kidney transplant
Introduction
Only a few cases in medical literature mention life-threatening retroperitoneal hematoma from a simple renal cyst [1,2]. Retroperitoneal hematoma from renal cause has been reported in patients with an underlying kidney tumor, as in Wunderlich's syndrome [1]. The relationship between spontaneous retroperitoneal hematoma and the use of anticoagulation and antiplatelet therapy is reported [1], [2], [3]. The clinical findings are variable and the pathology is infrequent which often lead to difficulty in making the diagnosis. However, a patient presenting with abdominal or lumbar pain with signs of hypovolemia is highly suspicious of a retroperitoneal hemorrhage, especially in the case of an anticoagulated patient [2,3]. Computed tomography [CT] scan is a quick and effective method to diagnose retroperitoneal hematoma [3], enabling to intervene in a timely manner [4,5]. Conservative therapy may allow resolution of renal bleeding, but some clinical presentations may be severe enough for surgical [6] or endovascular interventions [7]. We report our experience of a spontaneous retroperitoneal hematoma compressing the IVC in a patient with renal transplant.
Case presentation
Clinical presentation
A 71-year-old immunocompromised woman with history of end-stage renal disease with left pelvic renal transplant secondary to type 2 diabetes mellitus nephropathy was under an anticoagulation therapy for multifocal pulmonary embolisms. Other medical problems included controlled hypertension and class II obesity. The patient presented to the hospital for repeated orthostatic-related syncope with acute right flank pain and vomiting that had been present for a few hours. Physical examination revealed right flank pain tenderness upon palpation, without rigidity or rebound tenderness.
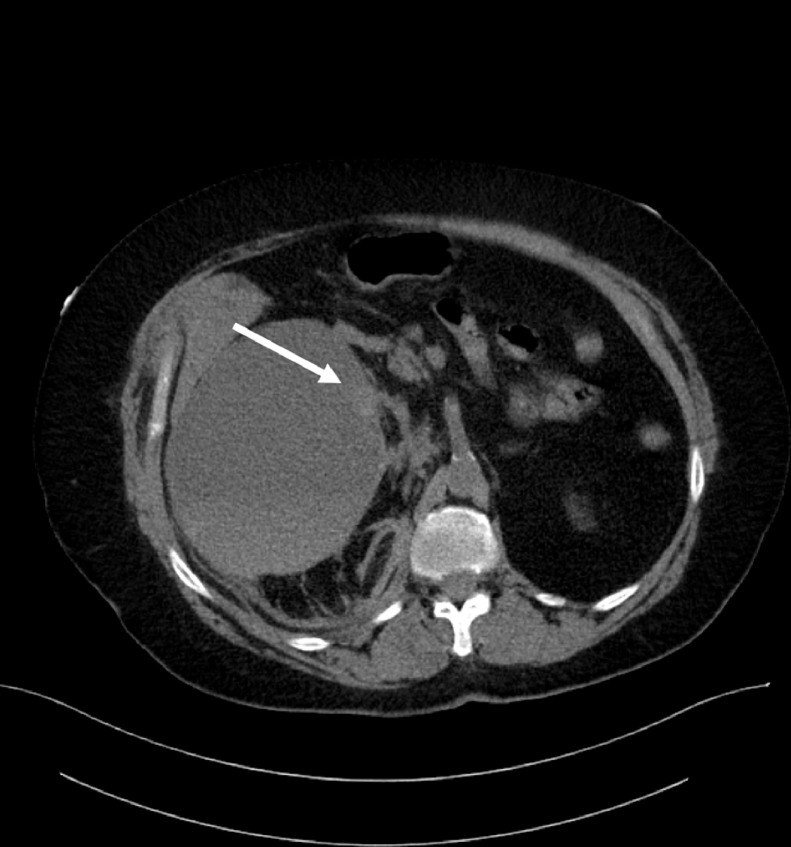
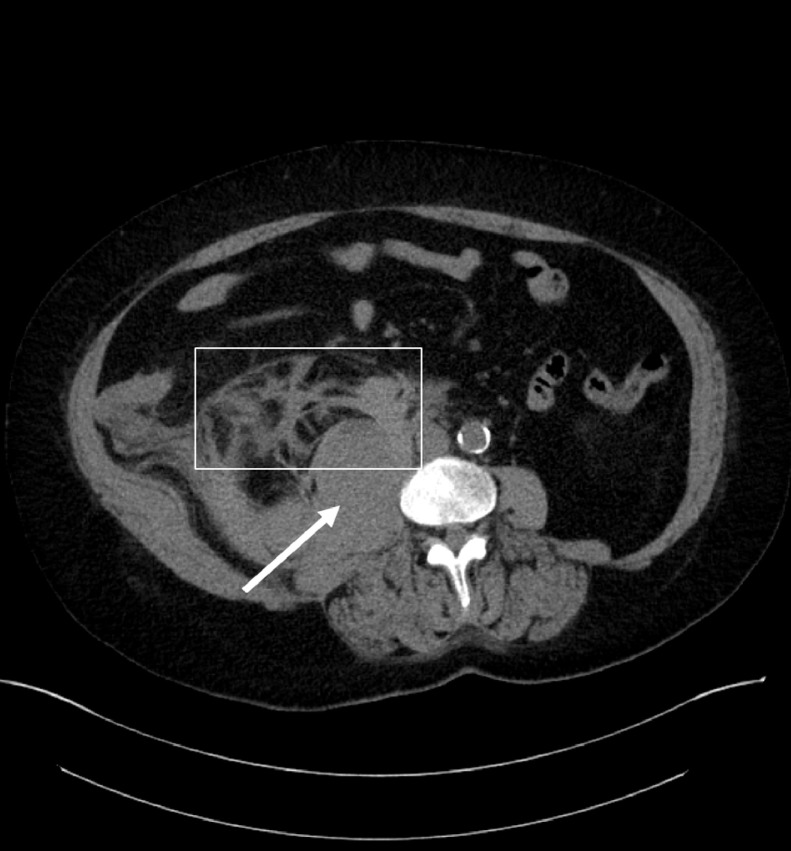
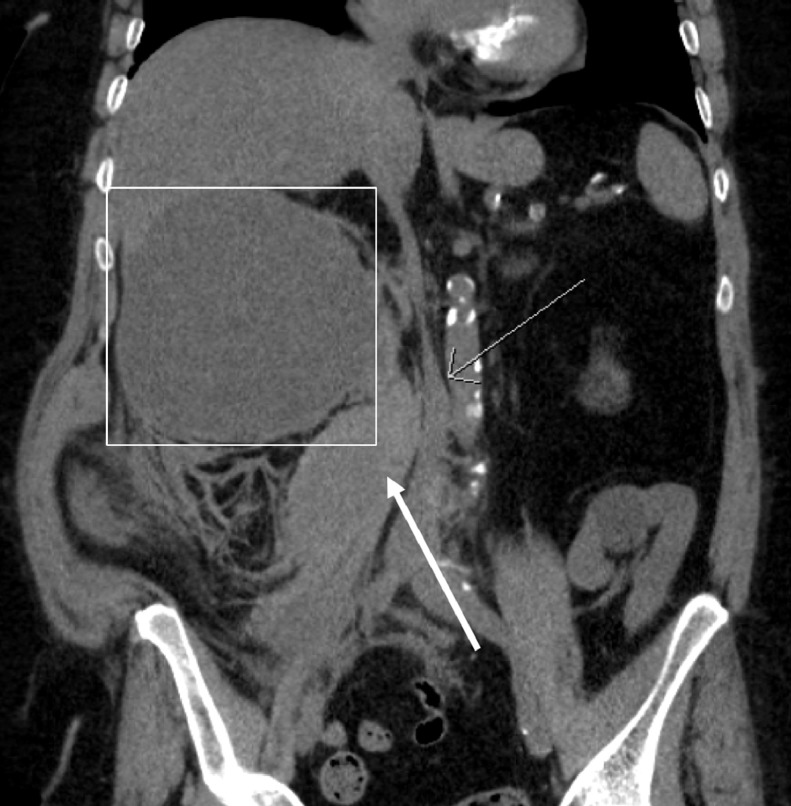
Noncontrast abdominal CT scan revealed an interval growth in size of a known cyst in the native right kidney. Maximal diameter increased from 9.7 to 13.9 cm from a prior CT scan performed 6 months earlier. The cyst presented a fluid-fluid level in keeping with hemorrhage (Fig. 1). A 1.8 cm dense nodule was noted on the medial surface of the cyst, representing a clot (Fig. 2). Ipsilateral psoas hematoma and fat stranding in the right paracolic gutter confirmed rupture of the hemorrhagic cyst from the right native kidney (Fig. 3). The retroperitoneal hematoma measured 13 × 4 mm diameter and severely compressed the inferior vena cava (IVC) (Fig. 4).
Fig. 1.
A fluid-fluid level (arrows) representing new cystic hemorrhage in the right native kidney, responsible for the retroperitoneal hematoma.
Fig. 2.
A dense nodule was noted on the medial surface of the cyst (arrow), considered the site of hemorrhage.
Fig. 3.
Ipsilateral psoas hematoma (arrow) with fat stranding (rectangle) in the right paracolic gutter was noted.
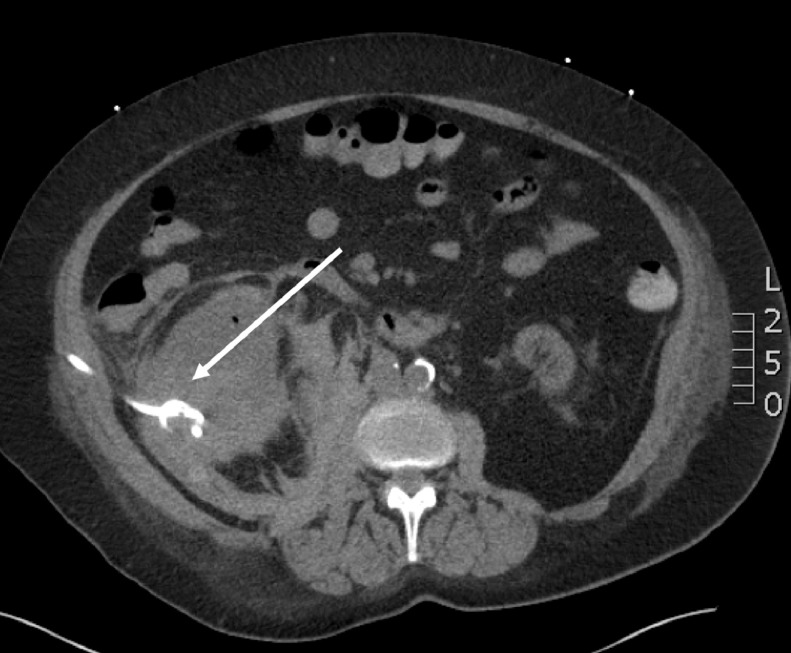
Fig. 4.
The hematoma (thick arrow) severely compressed the inferior vena cava (thin arrow). Hemorrhage from the cyst (rectangle) from the right native kidney was responsible.
Five hours after presentation, the patient's hemoglobin dropped from 113 g/L to 76 g/L with hematocrit level and vital signs stable despite medical management. The patient was admitted to the intensive care unit.
Management
The left pelvic renal transplant required special considerations regarding the best therapeutic approach. Conservative standard treatment would have been to withhold the anticoagulation therapy initially introduced 5 days earlier for pulmonary embolism. Placement of an IVC could have protected the patient from complications of additional pulmonary embolism while the retroperitoneal bleeding could resorb. However, the medical team was uncomfortable with this option. The presence of the retroperitoneal hematoma implied an increased risk for thrombosis of the IVC and iliac veins, with secondary loss of the renal transplant. Placement of an IVC increased furthermore the risk for thrombosis. The surgical option with partial or total nephrectomy with retroperitoneum decompression was considered, but ultimately the radiological intervention was simpler and less invasive. This plan consisted of draining the intracystic hemorrhagic fluid concomitant with complete embolization of the right renal artery. IVC filter would also be inserted for as little time as possible so the anticoagulation therapy could be withheld while the hemorrhage was being controlled.
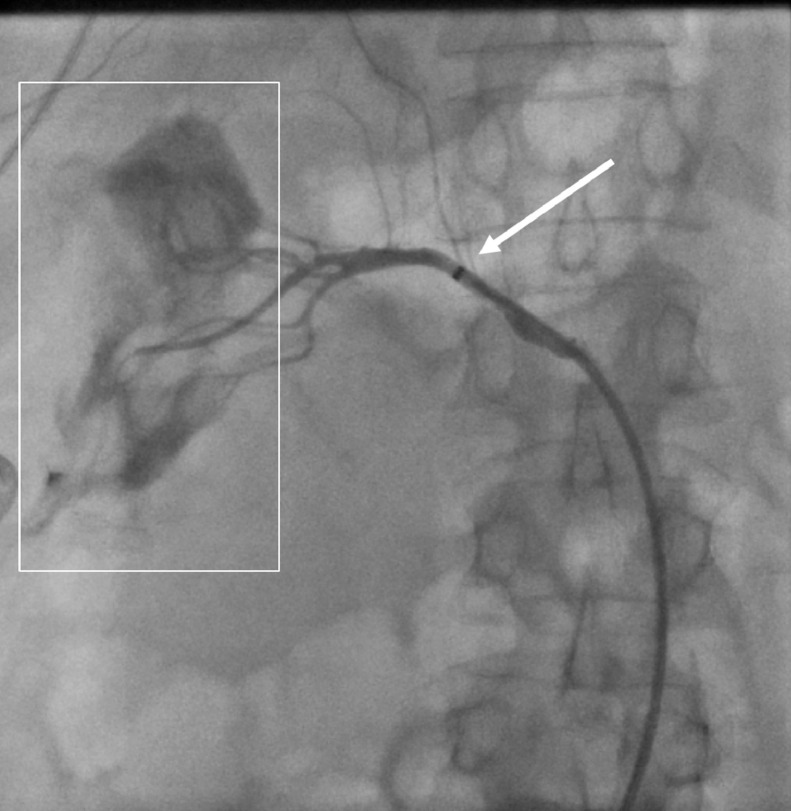
Ten hours after the initial syncope, the interventional radiologist drained 600 mL of intracystic hemorrhagic fluid with a 10 French pigtail drain to decompress the IVC. The percutaneous pigtail drain was left into the perirenal hemorrhagic collection to prevent infection and excreta were followed on ward to monitor the embolization. Selective angiography revealed active bleeding from the right kidney (Fig. 5). By femoral approach, embolization of the entire right renal artery using a 10 mm Amplatzer vascular plug was performed to prevent recurrence of bleeding once the anticoagulation therapy resumed (Fig. 6). Lastly, the interventional radiologist completed the intervention by inserting an IVC filter (Fig. 7). The intention was to leave it in place for the minimal time required to restart the anticoagulation therapy as quickly as possible.
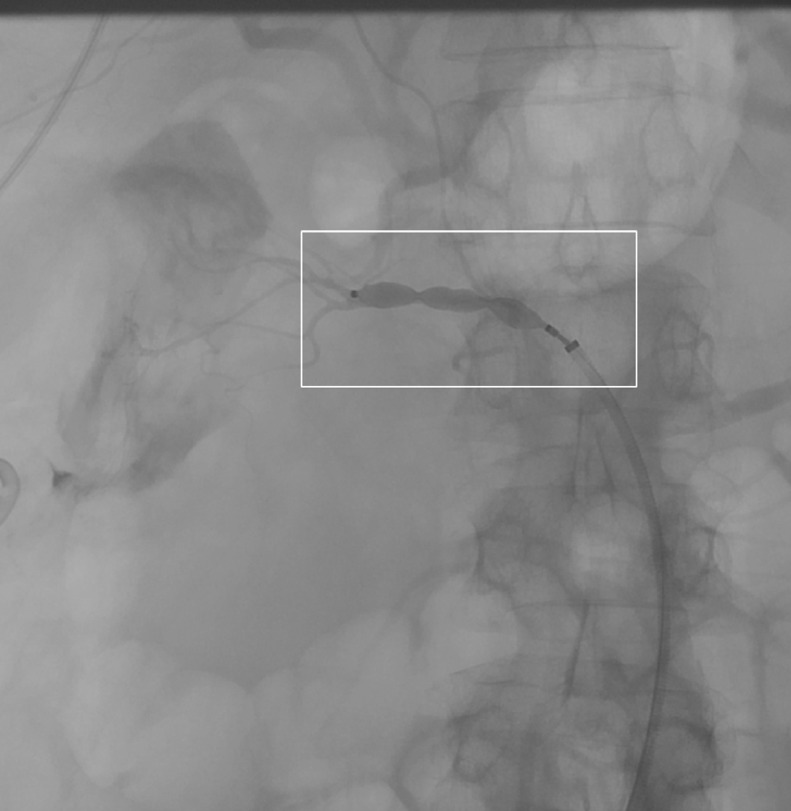
Fig. 5.
Selective angiography (thin arrow) of the origin of the right renal artery showed active extravasation (rectangle). The partially visualized percutaneous pigtail drain (thick arrow) was left into the perirenal hemorrhagic collection.
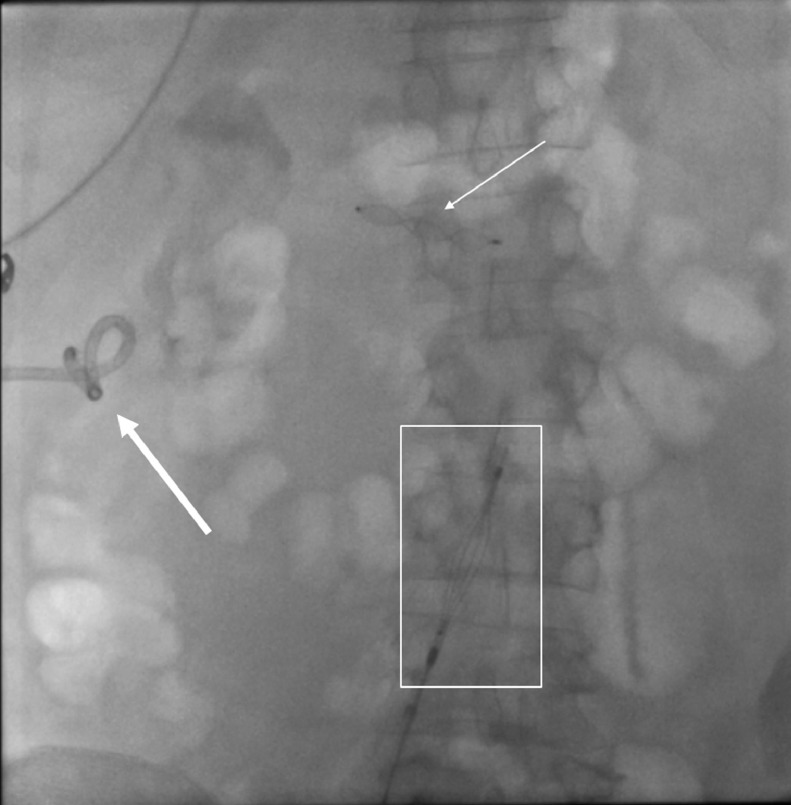
Fig. 6.
Selective embolization of the origin of the right renal artery using a 10 mm Amplatzer vascular plug (rectangle) by femoral approach was performed.
Fig. 7.
Inferior vena cava filter (rectangle) was also inserted to withhold the anticoagulation therapy while the hemorrhage was being controlled. Pigtail drain (thick arrow) in the retroperitoneal hematoma and an Amplatzer vascular plug (thin arrow) are also shown.
Four days after the radiologic intervention, the follow-up CT scan of the abdomen showed a regression of the drained cystic hemorrhagic lesion which allowed the removal of the 10 F percutaneous pigtail drain 4 days after the radiologic intervention (Fig. 8). The IVC filter was removed at the same time. The stabilized condition of the patient made it possible to resume the anticoagulation therapy at the same time. The patient improved without further intervention and was discharged.
Figure 8.
Pigtail drain in the hemorrhagic cyst from the right native kidney (thick arrow).
Discussion
When clinically suspected, CT scan is the most important step to obtain the diagnosis of a retroperitoneal hematoma. It can confirm the diagnosis and specify the origin and the severity of the hematoma [4,5]. It is an easy diagnosis by CT scan, with radiologic findings well described in the medical literature [2,3].
This case reinforces the need to rapidly diagnose renal bleeding extending to the retroperitoneum, because the pathology could have been fatal if it went undiagnosed. Once the diagnosis made, concerns were toward the compression of IVC by the hematoma in this patient with pelvic renal transplant. A personalized treatment plan was made in conjunction with the intensivist, the urologist, and the interventional radiologist to relieve the IVC, stop the hemorrhage and limit the potential complications of not being anticoagulated in a patient with known pulmonary embolism.
Nowadays, the advancement of vascular interventional radiology offers an alternate approach to surgical kidney exploration that often results in partial or complete nephrectomy [7]. Selective catheterization and embolization of the specific segmental bleeding arteries has become the standard of care for life-threatening renal hemorrhage because of its low morbidity and mortality rate, minimal parenchymal loss with maximal renal function preservation [7,8]. In addition, there is low complication rates and rapid recovery [4,5,[7], [8], [9]].
In conclusion, rapid diagnosis by imaging is important to accurately treat a patient presenting with retroperitoneal hematoma. When there is a retroperitoneal hematoma in a patient with pelvic renal transplant, we find it important to search and describe IVC compression. Interventional radiology can offer a personalized, efficient, and minimally invasive management.
Ethical standards
All procedures performed involving human were in accordance with the ethical standards of our institution as well as those of The Code of Ethic of the World Medical Association (Declaration of Helsinki of 1983) for experiments involving human.
Informed consent
Written patient's consent was obtained for the publication of this article and related radiology figures.
Footnotes
Declaration of Competing Interest: The authors have declared that no competing interests exist.
References
- 1.Kinnear N., Hennessey D.B., Douglass-Molloy H., Jack G. Life-threatening Wunderlich’s syndrome with concurrent clopidogrel use. Case Reports. 2016;2016 doi: 10.1136/bcr-2016-216171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chronopoulos P.N., Kaisidis G.N., Vaiopoulos C.K., Perits D.M., Varvarousis M.N., Malioris A.V. Spontaneous rupture of a giant renal angiomyolipoma-Wunderlich's syndrome: Report of a case. Int J Surg Case Rep. 2016;19:140–143. doi: 10.1016/j.ijscr.2015.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sunga K.L., Bellolio M.F., Gilmore R.M., Cabrera D. Spontaneous retroperitoneal hematoma: etiology, characteristics, management, and outcome. J Emerg Med. 2012;43(2):e157–e161. doi: 10.1016/j.jemermed.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 4.Loureiro J.L., Mendonca K.G., Pacheco Gde A., Soutinho M.F., Presidio G.A., Ferreira A.F. [Spontaneous perirenal hematoma in a lupic patient on haemodialysis treatment and with renal cysts] J Bras Nefrol. 2013;35(2):162–164. doi: 10.5935/0101-2800.20130025. [DOI] [PubMed] [Google Scholar]
- 5.Medda M., Picozzi S.C., Bozzini G., Carmignani L. Wunderlich's syndrome and hemorrhagic shock. J Emerg Trauma Shock. 2009;2(3):203–205. doi: 10.4103/0974-2700.55346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Syuto T., Hatori M., Masashi N., Sekine Y., Suzuki K. Chronic expanding hematoma in the retroperitoneal space: a case report. BMC Urol. 2013;13:60. doi: 10.1186/1471-2490-13-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pappas P., Leonardou P., Papadoukakis S., Zavos G., Michail S., Boletis J. Urgent superselective segmental renal artery embolization in the treatment of life-threatening renal hemorrhage. Urol Int. 2006;77(1):34–41. doi: 10.1159/000092932. [DOI] [PubMed] [Google Scholar]
- 8.Mabillard H., Srivastava S., Haslam P., Karasek M., Sayer J.A. Large retroperitoneal haemorrhage following cyst rupture in a patient with autosomal dominant polycystic kidney disease. Case Rep Nephrol. 2017;2017 doi: 10.1155/2017/4653267. 4653267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thulasidasan N., Sriskandakumar S., Ilyas S., Sabharwal T. Renal angiomyolipoma: mid- to long-term results following embolization with onyx. Cardiovasc Intervent Radiol. 2016;39(12):1759–1764. doi: 10.1007/s00270-016-1432-0. [DOI] [PubMed] [Google Scholar]