Abstract
Objective:
To evaluate whether implementation of a geographic model of assigning hospitalists is feasible and sustainable in a large hospitalist program and assess its impact on provider satisfaction, perceived efficiency and patient outcomes.
Methods:
Pre (3 months) – post (12 months) intervention study conducted from June 2014 through September 2015 at a tertiary care medical center with a large hospitalist program caring for patients scattered in 4 buildings and 16 floors. Hospitalists were assigned to a particular nursing unit (geographic assignment) with a goal of having over 80% of their assigned patients located on their assigned unit. Satisfaction and perceived efficiency were assessed through a survey administered before and after the intervention.
Results:
Geographic assignment percentage increased from an average of 60% in the pre-intervention period to 93% post-intervention. The number of hospitalists covering a 32 bed unit decreased from 8-10 pre to 2-3 post-intervention. A majority of physicians (87%) thought that geography had a positive impact on the overall quality of care. Respondents reported that they felt that geography increased time spent with patient/caregivers to discuss plan of care (p < 0.001); improved communication with nurses (p = 0.0009); and increased sense of teamwork with nurses/case managers (p < 0.001). Mean length of stay (4.54 vs 4.62 days), 30-day readmission rates (16.0% vs 16.6%) and patient satisfaction (79.9 vs 77.3) did not change significantly between the pre- and post-implementation period. The discharge before noon rate improved slightly (47.5% - 54.1%).
Conclusions:
Implementation of a unit-based model in a large hospitalist program is feasible and sustainable with appropriate planning and support. The geographical model of care increased provider satisfaction and perceived efficiency; it also facilitated the implementation of other key interventions such as interdisciplinary rounds.
Keywords: geographic assignment, unit based rounding, hospitalist deployment, provider satisfaction with rounding
1. Introduction:
Hospital-based care has become increasingly complex over the last decade with patients being older, sicker and having more chronic comorbidities. At the same time hospitals are under scrutiny and pressure to deliver more efficient, high-quality and high-value care. Currently there are more than 50,000 hospitalists in the United States and approximately 75% of all US hospitals have a hospitalist group.1 Hospitalist groups have generally focused on clinical pathways and standardization protocols to redesign work flow and improve interdisciplinary team collaboration with patient centered bedside-rounds or ‘whiteboards’ to enhance communication.2-6 Although each of these interventions has potential value, their implementation and sustainability remains challenging in hospitalist groups with large patient volume if providers have patients assigned on different medical units (also known as hospital floors, referred to as units or unit based in this paper). Hospitals have various methods in assigning patients to hospitalists, but most try to prioritize equal number and acuity of patients per provider, continuity of patient care and improved patient flow out of the emergency department. Several studies have examined the value of interdisciplinary rounds and found a positive impact on length of stay,5 efficiency of rounds7 and sense of collaboration and teamwork.8 When hospitalists have patients scattered to multiple locations in the hospital interdisciplinary rounds are almost impossible to schedule and assure constant participation of the hospitalist. Additionally, the general sense of teamwork with the nurses and case managers is less likely to be achieved. This system leads to time waste, multiple interruptions in work flow and limited time and availability to meet with families. Prior evidence showed hospitalists caring for patients on up to 5 different units spent 69% of their day in indirect care, 13% in paging or responding to pages and 3% traveling between patients.9-12 These findings suggest that limiting fragmentation of care, such as would occur with a unit based hospitalist service, could increase efficiency by cutting down on pages and travel time; this extra time could be used for other aspects of patient care to increase efficiency and quality.
Geographical or unit-based assignment (in this paper geographic assignment is defined as the deployment of a hospitalist on one medical unit) of hospitalists represents a promising alternative to the old model of hospitalists following patients distributed on multiple hospital units. Despite a high level of enthusiasm for this model of care, only few studies have described how to successfully implement such a geographic assignment.4,13-19 Singh et al, assessed the impact of patient localization from two medical teams to a single nursing unit and found that the new model of care led to higher productivity and better workflow.16In a qualitative follow-up study the authors found increased provider satisfaction and more frequent face-to-face communication however, there was no improvement in the shared understanding of the care plan by team members20. Other studies showed that geographically assigned hospitalists may lead to reduction in length of stay14 and costs17, increase in total proportion of bedside rounding and nursing presence during rounds15 and improved discharges by noon and patient satisfaction.13
Our institution has steadily expanded the hospitalist program which in 2014 was one of the largest in the country with more than 58 hospitalists and has continued to grow since then. Our patient assignment system was originally structured to have a constant and equitable number of patients for all providers. Historically there was little effort to assign patients to hospitalists in a fashion that would allow the hospitalist to stay on one unit most of the day. Occasionally a hospitalist could have patients in up to 16 different hospital units, which were located in 4 different buildings. This resulted in significant waste of time as it takes up to eight to ten minutes to walk from one end of the hospital to the other. Some possible scenarios could result in inefficiency: if a patient deteriorated, the hospitalist had to be on that unit and could not attend other patients; the hospitalist could come to round on the patient but the patient was at not in the room but had a test done and the physician had to come back later. Additionally, hospitalists would frequently be called back to patients they had already seen once families arrived at the bedside. Our attempt to institute interdisciplinary rounds was not successful as hospitalists had to be at these rounds on different units, often at the same time. Perceived inefficiencies in the hospitalists’ workflow, low patient satisfaction survey scores, and other concerns led to the decision of the hospital leadership to institute interdisciplinary rounds, which were piloted on one unit and thought to be effective in improving patient outcomes.5 .
“Geographic” assignment of the physicians was considered a critical foundation for a series of planned interventions to improve quality of care. The institution and hospital medicine program leadership felt strongly that having physicians unit -based, working with a limited number of nurses and case managers would improve workflow and teamwork and result in better patient care. In prior years there were several attempts to implement a geographic assignment but invariably after few days the hospitalists again cared for patients scattered on several units due to the fact that the patients would be frequently relocated and that patients admitted the night before who were still in the ED did not have a bed assignment, making it impossible to place them in a geographic rounding assignment. We recognized that the success of this performance improvement initiative was contingent on more systemic solutions and collaboration with several other departments including the emergency department, patient placement (also known as admitting in other hospitals) and case management. In the fall of 2014 after six months of planning, our hospitalist program transitioned to a geographic assignment of hospitalists as a new model of care delivery. We hypothesized that if this process were to be successful it would assist in improving provider, nurse and case manager satisfaction, communication and efficiency and in the end patient outcomes. In this article, we describe our institutional experience in developing, implementing and sustaining a geographically located hospitalist service and examine the impact on provider satisfaction, perceived efficiency and patient outcomes.
2. Methods
2.1. Setting and Participants
Baystate Medical Center is a 710-bed tertiary care academic medical center in Western Massachusetts. It serves a diverse urban and rural population of nearly one million people and frequently runs over 100% capacity. At the time the institution had an employed hospitalist group of more than 58 total providers, 24/7 coverage, a house staff-covered teaching service with 10 academic hospitalists and a non-teaching service. Residents did not cover any patients that were not under the direct supervision of an academic hospitalist. All residents experienced the pre-geography model of care. Additionally, the hospitalists at our institution were all employed by the hospital, there were no private groups. A few private attendings admitted their own patients; their combined census was usually five or fewer. On average, the hospitalist group cared daily for around 300 patients admitted to 16 different hospital floors in 4 attached buildings and discharged 1500 patients monthly. Our hospitalists do not round in the critical care units. Most of the time the hospital runs at over 100% occupancy rate, as was the case in this time period of 2014 – 2015. The average patient census for our program in 2014 was around 280 patients a day, and the following year was up to an average of 320 patients a day (post intervention).
2.2. Pre-intervention period:
Patients were admitted to the hospitalist service after the ED physician determined need for admission to the hospital. They would be seen by the hospitalist assigned to admissions that day and moved to any of the 16 hospital units based on bed availability and care needs. After admission, patients were allocated to rounding teams (usually the following day) with a general location (mostly by building) and a programmatic goal of insuring an equitable distribution of workload for physicians (number of patients and acuity). Patients would frequently be moved to different units depending on their needs (i.e. telemetry monitoring) and their assigned hospitalist would continue to care for them in their new location until they were discharged or the physician rotated off service.
2.3. Planning period:
In March 2014 the leadership of our hospital identified the reorganization of the hospital medicine service and deployment of the hospitalists in a geographic assignment model as a major organizational goal in order to achieve other priorities. A period of 6 months was agreed upon to prepare and complete the necessary tasks before implementation. A working group which included the primary stakeholders was convened. The hospital medicine division chief, two hospital medicine medical directors, leadership from the internal medicine residency program, nursing, case management and the emergency room department were included. Several barriers and challenges which had hampered prior attempts to implement geographic hospitalists units were first identified and multiple changes were implemented. Financial resources were made available as additional providers were needed. (Table 1) All involved departments (emergency, patient placement, hospital medicine, medicine residency program, case management) were acutely aware that this was a high level institutional goal with the backing of the chair of medicine.
Table 1:
Barriers and Solutions to the Geographic Model.
| BARRIERS | SOLUTIONS | DELIVERABLES | FACILITATORS |
|---|---|---|---|
| Hospital Medicine Program | |||
| Mismatch of staffing to patient volume | Staffing vacancies were filled. FTE's were increased to targeted census 16-18 patients/ 12 hour/ nonacademic shift, and 12-14/ 8 hour/academic shifts | NA | HMP leadership |
| Mechanism to redistribute patients when providers unexpectedly cant’ work their assigned shift | Implemented jeopardy system covering 365 days/year, intact geographic list covered by covering physician. | minimize geographic distribution interruptions | HMP leadership |
| Mismatch of unit size to MD rounding capacity | Mapped # of our patients per unit and turnover to understand staffing needs and assigned correct number of MD to each unit. Most units had more patients than 2 MD's could cover. A ‘Flex MD’ who covered 3-4 contiguous units cared for those patients. | NA | HMP leadership |
| Traditionally split list to be "even # of patients /provider Providers prioritized continuity over geography | Group agreed to slight uneven daily distribution in return for stability. Equitable work flow/productivity to be achieved over time as providers rotate to different units. Tracked # of rotations by providers to various units | Over time equitable workflow for hospitalists in terms of acuity and patient encounters | HMP leadership |
| Disruptions in patient care if patient moved to another unit | Verbal sign-out when patient is relocated to another | Improved communication | HMP leadership/hospitalists |
| Adherence to group rules and monitoring. Exceptions to geography clearly outlined |
Daily monitoring of all MD patient lists. Reporting geographic integrity daily. Nightly group pages before end of shift reminding nocturnists the need for maintaining geography. Continuity trumps geography if: CMO/hospice, high stakes family/doctor relationship, anticipated next day discharge. |
>75% geographic patient assignment integrity IE each provider would have >75% of their patients located on their assigned floors |
HMP leadership/hospitalists |
| Institutional barriers | |||
| Assignment of patients to unit based on next bed available | Change PPM (patient placement manager) work flow and 3 way call (ED, PPM, and hospitalist) to agree on unit prior to accepting patient. Monitored lists and received feedback from teams when patients not moved to correct floor. PPM supervisors drilled down to root cause of incorrect moves to improve accuracy of bed predictions | >95% reliability of prediction. | HMP leadership and administrative support |
| Frequent relocation of patients due to lack of telemetry or volume flux from other service lines | Increased telemetry capability. Institution of a telemetry protocol and adherence monitored to decrease inappropriate use. Agreement to relocate patients only for change in level of care and not for volume in other service lines (i.e. surgery). | Unit accountability to manage patient flow | Hospital leadership/hospital medicine leadership and ED |
| Academic medical center with large medicine residency program | Residency program leadership involved in selecting the medical units residents will be caring for to get exposed to the breadth and depth of disease processes. | Ensure that interns/residents admitted and kept their own patients to adhere to GME rules | Hospital administration HMP leadership/ |
| ED/bed management priority of moving patient out of ED | Buy in from ED that deciding factor for patients moving out is correct bed location not duration of waiting. This process provided equal outflow of ED, but unequal wait time by patients. | No Net increase in patient wait time in ED Decrease imminent bed changes on units |
Internal Medicine Program Hospital administration/Hospital leadership/ |
| IT Barriers | |||
| Lists in EMR | Created new lists in EMR to match new assigned locations | Correct names of teams to match units, and identify if it is a teaching or nonteaching team | HMP leadership |
| Paging to correct providers | Created workflows to nursing units to correctly identify first call (to interns residents or attendings depending on units). New names of teams matched old historical naming of teams with teaching services. (Ie A B C etc) | Pathway for nursing to page correct team pagers | HMP leadership |
| Admitting list "grid" | Edited web based tracking form for incoming admissions, to reflect which floor patient was being assigned. The triaging hospitalist provider would enter patient information including floor assignment after 3 way call with PPM and Ed provider | Mechanism to identify for teams to select pending admissions to their floor | Sound Physicians IT department |
FTE = Full Time Equivalent; HMP = Hospital Medicine Practice; PPM = Patient Placement Manager; this is a clerical position. The PPM had access to bed availability information and aids the admitting physician with geographic patient bed assignments; Flex MD = Providers who would see patients who were not assigned to geographic teams due to the fact that the geographic teams were capped (i.e had reached maximum acceptable patient census). Flex physicians are assigned to a building rather than a floor and by nature, were not expected to be geographic. CMO = comfort measures only ;Grid = an electronic table which lists all the patients being admitted, their diagnosis, clinical status, and the floor to which they are being assigned; EMR = electronic medical record
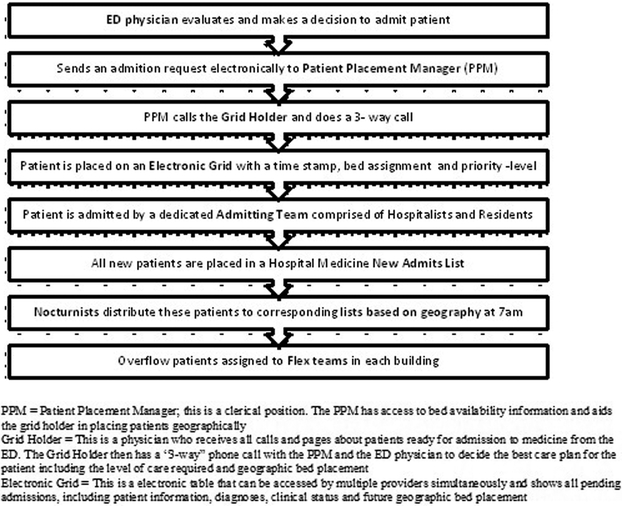
We began to look at changes from the point of entry, the Emergency Department (ED). One major change was in the way patient placement allocated patients to beds. Once the ED physician decided that the patient should be admitted instead of the “next bed available” patients were assigned to an actual room number; thus even if a patient was still in the ED he/she could be placed in the correct geographic assignment. (Figure 1). We committed to the ED there would be no net increase in ED wait time for inpatient beds. We then assessed our patient census on each of the 16 units which varied between 10 and 36. Based on the number of patients cared for by one provider we approximated the number of physicians needed for each unit. Using this information we successfully advocated for and received funding for five additional hospitalists. To be clear, these additional hospitalists were needed to achieve appropriate coverage for patient volume regardless of geographic assignment, but this planning exercise assisted us in assessing our staffing needs.
Figure 1:
Patient Assignment Process
Due to the fact that some units had a patient census that did not allow for complete geographic assignment (e.g. 36 patients and two hospitalists with a combined patient cap of 32 patients), we created two “flex” teams to absorb patients who remained unassigned. Flex physicians were assigned to buildings rather than floors, and cared for a similar census. All hospitalists rotate onto flex teams.
Several meetings were held with the hospitalists to get buy-in for the intervention. We discussed the rationale for the planned changes, recognized concerns and incorporated providers’ suggestions. One significant concern was that due to the differing census per geographic assignment (e.g. one unit had only 30 patients and one averaged around 10s), the number of patients cared for by providers will vary. However, since everyone would rotate through all the geographic assignments it was understood that eventually the numbers would even out. Another important point of contention pertained to patient transfers. The group agreed that patients would be transferred to the geographically appropriate provider unless the discharge was planned for the following day, acknowledging this would decrease provider continuity. We also met with the leadership of the Internal Medicine Residency as residents have patient assignment responsibilities to their teams.
An administrative assistant was tasked to focus on daily geographic assignment, track dropped patients, and facilitate patient swaps to preserve geographic assignment. At the start of each hospitalist seven-day block, patients were realigned to ensure that every physician was starting with geographic assignments. One of the two hospitalist medical directors was responsible for overseeing the new geographic model and had the authority to mobilize additional resources when appropriate. The hospital medicine administration and the chair of the department provided strong support for the intervention and facilitated the necessary financial and personnel resources.
2.4. Metrics/Outcomes
Because our main aim was to examine the implementation of the new geographical model of care, we first assessed if we achieved this goal. The geographical assignment was defined as the percentage of all patients cared for by the hospitalist in the units they were assigned. For each geographically assigned hospitalist we determined the percentage of patients matched to their assignment each morning. (The ‘flex teams’ are not included in this report as they were by virtue of design not expected to have a geographic assignment). We aimed to achieve ≥ 80% geography. For example, if a hospitalist had a total of 16 patients to care for and if 13 of those patients were residing in the geographic assignment of that provider, this was considered a success (81% geography).
Patient outcomes, including length of stay, 30-day readmission and patient satisfaction were closely monitored and are reported for the pre and post-implementation period. Additionally, the discharge before noon rate is also reported.
Survey administration
One week prior to implementation of the geography model and six months after implementation, we invited all the hospitalists and residents to answer an anonymous survey. (On line supplement) The questions asked about their perceptions about efficiency, teamwork, workload (e.g.: “on average, on how many floors were your patients during your last 2 weeks of service) and time spent communicating with patients, families and colleagues. The post-intervention survey also asked questions assessing satisfaction with the geographical model and the impact on work-flow (e.g.: “Do you think geography has decreased number of interruptions?”). Questions were piloted first with 4 hospitalists and modified to improve clarity. Survey questions had both negative and positive answers, and comment boxes were provided for additional input.
We also surveyed nurses and case managers regarding their perceived communication with the hospitalists before and after the intervention.
An email invitation was sent containing an informational cover letter and a link to the online survey. The survey was distributed on-line using Survey Monkey an online secure cloud- based software.
2.5. Analysis
We report the percentage of successful hospitalist geographic assignment monthly before and after the intervention. Rates of geographic assignment were analyzed by unit and period (pre- post-intervention) using Analysis of Variance. Survey results are presented descriptively using summary statistics (medians or proportions with 95% confidence intervals) appropriate to the scale of measurement. Change in perceptions of physicians and nurses pre- and post-intervention were assessed with the Wilcoxon signed rank test.
All analyses were performed in STATA (Stata, 2015).(StataCorp. STATA/MP. 14.0 for Windows ed. College Station, TX: StataCorp; 2015)
The study was approved by the Baystate Medical Center Institutional Review Board, with a waiver for written informed consent.
3. Results
3.1. Geography Results
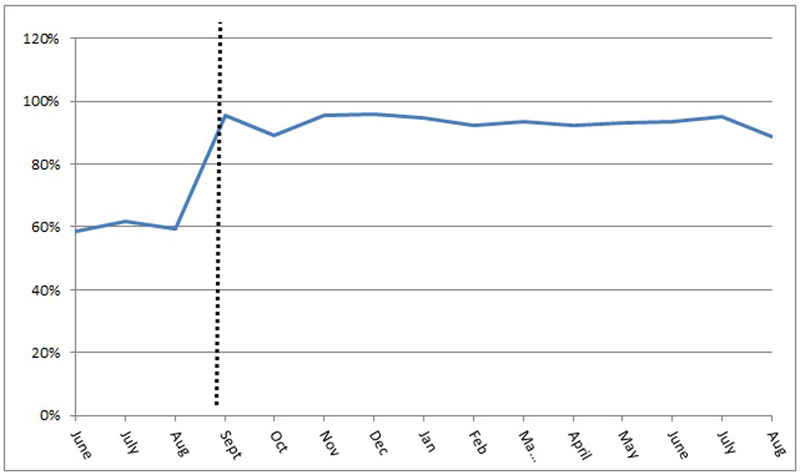
The average daily number of patients cared for by the hospitalists was 280 in the pre-implementation period and 320 in the post-implementation. The overall percentage of geographic assignment was 60% in the pre-intervention period (meaning that for every 10 patients a hospitalist cared for only 6 were in their geographic assignment) and 93% in the post-intervention period (meaning that 9 of 10 were in the geographic assignment) (p << 0.001). Additionally, the number of hospitalists assigned to any given unit dropped from up ten hospitalists to a total of two to three.
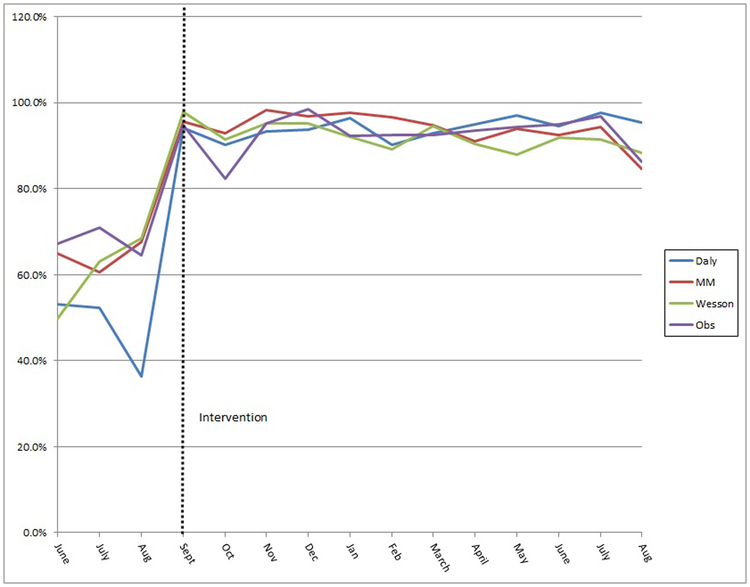
The proportion of successful geographic assignment increased sharply to 96% during the first month after implementation of the intervention and remained between 90% and 95% for the following 12 months. (Figure2) Differences in pre-post intervention geographic assignment varied by hospital unit (p <<0.0001). (Figure 3) Most of this difference was from variability in pre-intervention rates of geographic assignment among the units. Geography assignment was continuously monitored post intervention and continues to be above 80%
Figure 2:
Proportion of Patients Assigned Geographically
Figure 3:
Proportion of Patients Assigned Geographically in each medical unit
3.2. Patient outcomes:
Mean length of stay (4.54 vs 4.62 days), 30-day readmission rates (16.0% vs 16.6%) and patient satisfaction (79.9 vs 77.3% – as defined by HCAHPS score of rating doctors performance as excellent) did not change significantly between the pre- and post-implementation period. The discharge before noon rate improved slightly from 47.5% to 54.1%. (Table 2)
Table 2:
Patient outcomes before and after the intervention
| Pre-implementation | Post-implementation | |
|---|---|---|
| 30-day readmission rate % (median, IQR) | 16.0 (14.9-16.7) | 16.6 (15.7-17.2) |
| No of discharges (median) | 1372 | 1523 |
| Length of stay, days (median, IQR) | 4.54 (4.5-4.64) | 4.62 (4.55-4.77) |
| Patient satisfaction * (overall percentage of physicians rated as providing excellent care as per HCAHPS doctor questions) | 79.92 | 77.32 |
| Discharge before noon rate (percent of discharges before noon/total daily discharges) | 47.5% | 54.1% |
3.3. Survey Results
Of the 155 physicians (58 hospitalists and 90 internal medicine residents) invited to participate, 97 (62%) (41 hospitalists and 56 residents) and 57 (36%) (26 and 31 respectively) responded to the pre and post survey. The median number of years in practice of the hospitalists was 3 (range 0 to 19) and 39% had some prior experience with unit-based rounding.
The majority of physicians (hospitalists and residents) thought that geography decreased the number of pages and interruptions (76% and 70%) and had a positive impact on the overall quality of care (87%). There was a significant decrease in perceived number of floors of rounding after the intervention (p< 0.001) and an increase in perceived time spent with patient or caregivers to discuss plan of care for the day (p < 0.001) or to communicate with nurses (p = 0.0009). There was also an increased sense of teamwork with nurses (p < 0.001) and case managers (p < 0.001). Sixty-seven percent of respondents thought that geography allowed more time for teaching during bed-side rounds (95% CI 51% - 81%).
Ten case managers and 67 nurses responded to the pre survey and 7 and 39 to the post survey. Their rating of hospitalist communication regarding discharge plan of care significantly increased after the intervention (p < 0.0001).
Discussion
The assessment of the implementation of this quality improvement intervention demonstrated that transforming a large hospital medicine program from a “who’s up next” model to a geographic assignment model of patient care is possible and sustainable, though it requires substantial planning, institutional/leadership support and constant vigilance. Geographical assignment increased from 60% in the pre-implementation period to 93% in the 12 months after the intervention, with monthly rates between 90–95%. Almost 3 years post implementation we achieve more than 80% geographical assignments daily.
This intervention occurred in a tertiary care hospital with a large hospitalist group and high patient-volume and it is likely generalizable to comparable institutions and hospitalist groups. If other programs want to implement a geographical model, we believe that the main strategies which contributed to success included: a) team acceptance and buy-in through group discussions and transparency b) institutional leadership support which facilitated operational changes and c) periodic review of the data to maintain team engagement and make required changes.
Outcomes such as length of stay 30-day readmission and patient satisfaction were collected, reported and monitored monthly during and after the implementation of the geographical assignment. As reported in few other studies the geographical model implementation in our program was not associated with a decrease in length of stay or readmission rate.7,8
Three years into our transition to geographic rounding we continue to measure and report weekly geography and have consistently been able to maintain a rate above 80%. This achievement requires daily supervision at the medical director level with the ability to make decisions on staffing as well as clerical support. As evidenced by the results of the surveys health care provider satisfaction with this model was high, and providers believed that communication with patients, families and nurses improved. Additionally, having fewer interruptions during the day led providers to perceive increased work-flow and efficiency.
Geographic rounding was a first step in instituting a number of changes in patient care. First, it allowed for daily interdisciplinary plan of care rounds (IPOC) on every floor. These are bedside rounds, attended by the hospitalist, case manager and nurse. Families are told ahead of time to expect these rounds and often attend with questions. Most floors also do a “my plan” leaving behind written comments from the rounds about the next steps in the plan of care. These rounds are also used by the patient care team as an opportunity to check in on utilization and patient care needs, for example whether a patient still needs telemetry or intercare. Additionally, next day discharges are flagged and the group has successfully maintained a discharge before noon rate of 50%.
This intervention also allowed for geographical assignments of admissions. Hospitalists now get a call from the patient placement manager when a patient is in the emergency room and booked for inpatient admission to their floor. This allows for a direct conversation between the ED provider and accepting physician, and also improves patient continuity by having the geographically assigned hospitalist care for the patient from the beginning of their admission.
Another opportunity that arose from this intervention was the creation of a new leadership position for hospitalists, that of “Unit Medical Directors” for each unit primarily staffed by hospitalists. Together with the nurse manager these medical directors formed a leadership team, each with its own metrics and quality improvement projects. This intervention created a shared purpose and increased engagement amongst these hospitalists, as they better understood institutional goals. It also provided leadership opportunities and growth for career advancement and vitality.
The house staff also felt this model was a positive change. One resident reported “There is easier coordination of care with the nurse, case management and social work. Ease of workflow, drastically reduced pages since I am on site. It is easier to coordinate and set up family meetings during the day.” Hospitalist-educators indicated that they have more time for bedside rounds and for teaching, as they are not always moving from unit to unit. Nurses and case managers also felt that communication about plan of care and discharges improved. These results are similar with those reported by Singh et al in a study which qualitatively assessed the impact of co-locating hospitalists and nurses on the same unit. Using focus groups, nurses and hospitalists reported a positive impact on communication which further mediated key elements of patient care.20
Although overall the geographic model is more efficient than having providers’ patients scattered over multiple units, there are few negative aspects. First, when patients have to be relocated to a different unit for change in level-of care, they are assigned a new provider, decreasing continuity of care. We have tried to mitigate this with a formal sign out process. However, providers and patients alike express dissatisfaction when patients are moved to a new unit with a new provider. Second, there are instances when some teams are busier than others; however, given the fact that all physicians rotate their geographic assignments, over time there is an equitable share of patients and patient mix. Third, there is a lot of schedule administrative support required to ensure that hospitalists have variety in their assignments.
Our study has several strengths. It was conducted in a tertiary care hospital with high patient volume and a large hospitalist group. This model could be transferable to other hospitalist programs that struggle with implementing a geographic assignment of providers and we have provided detailed information for planning for success. The study also has several limitations. First, although we surveyed the providers about their perceived sense of communication following our intervention, we cannot definitively determine whether our survey results were mediated by simultaneous interventions such as interdisciplinary rounding. Second, the low response rate and mix of house staff and attendings is another limitation in interpreting the results of the surveys. Third, our hospitalists group has a large number of physicians and this model may not be as important to implement in a small hospitalist program, especially if there are only few nursing units.
Conclusion
Our study proves that implementing a geographic assignment system of rounding is feasible and sustainable but requires careful planning and the involvement of multiple departments. Localization of health care providers in a geographic assignment is an important step that allows implementation of other interventions, such as interdisciplinary care rounds. The geographical model has the potential of improving efficiency, communication and provider satisfaction.
Supplementary Material
Acknowledgements:
The authors would like to thank the following health care professionals for their contributions: Carmen Sanderson and Britt Arlin for their help with data collection; Michael Rosenblum, MD and Andy Artenstein, MD for their support for this performance improvement effort. We want to thank the entire hospitalist group for their commitment to the implementation of this intervention.
Funding
Dr. Stefan is supported by grant 1K01HL114631–01A1 from the National Heart, Lung, and Blood Institute of the National Institutes of Health.
Footnotes
Declaration of Interests
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Definitions:
“Unit” a particular area in a hospital where patients are boarded, also referred to as a “floor” or “ward”.
“Geographic Assignment” – number of patients on a provider’s list who are located in the assigned area in the hospital (i.e. on a particular hospital unit)
“Flex teams” extra provider team responsible for seeing patients who are on a floor that already has a provider, but that provider is at their patient limit. This flex provider usually ends up with 3–5 patients on 3 – 4 floors
“Hospitalist Group” – a blend of academic and non-academic providers who care for all medicine patients in the hospital except in the ICUs
“Unit Medical Director” hospitalist who has been assigned a leadership position and paired with a nurse manager for one medical unit in the hospital
References
- 1.Wachter RM, Goldman L. Zero to 50,000 - The 20th Anniversary of the Hospitalist. N Engl J Med. 2016;375(11):1009–1011. [DOI] [PubMed] [Google Scholar]
- 2.Wertheimer B, Jacobs RE, Bailey M, et al. Discharge before noon: an achievable hospital goal. J Hosp Med. 2014;9(4):210–214. [DOI] [PubMed] [Google Scholar]
- 3.Starmer AJ, Spector ND, Srivastava R, et al. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371(19):1803–1812. [DOI] [PubMed] [Google Scholar]
- 4.O’Leary KJ, Haviley C, Slade ME, Shah HM, Lee J, Williams MV. Improving teamwork: impact of structured interdisciplinary rounds on a hospitalist unit. J Hosp Med. 2011;6(2):88–93. [DOI] [PubMed] [Google Scholar]
- 5.Artenstein AW, Higgins TL, Seiler A, et al. Promoting high value inpatient care via a coaching model of structured, interdisciplinary team rounds. Br J Hosp Med (Lond). 2015;76(1):41–45. [DOI] [PubMed] [Google Scholar]
- 6.Herring R, Desai T, Caldwell G. Quality and safety at the point of care: how long should a ward round take? Clin Med (Lond). 2011;11(1):20–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dunn AS, Reyna M, Radbill B, et al. The Impact of Bedside Interdisciplinary Rounds on Length of Stay and Complications. J Hosp Med. 2017;12(3):137–142. [DOI] [PubMed] [Google Scholar]
- 8.O’Leary KJ, Wayne DB, Landler MP, et al. Impact of localizing physicians to hospital units on nurse-physician communication and agreement on the plan of care. J Gen Intern Med. 2009;24(11):1223–1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tipping MD, Forth VE, O’Leary KJ, et al. Where did the day go?--a time-motion study of hospitalists. J Hosp Med. 2010;5(6):323–328. [DOI] [PubMed] [Google Scholar]
- 10.O’Leary KJ, Liebovitz DM, Baker DW. How hospitalists spend their time: insights on efficiency and safety. J Hosp Med. 2006;1(2):88–93. [DOI] [PubMed] [Google Scholar]
- 11.Epstein K, Juarez E, Epstein A, Loya K, Singer A. The impact of fragmentation of hospitalist care on length of stay. J Hosp Med. 2010;5(6):335–338. [DOI] [PubMed] [Google Scholar]
- 12.Kim CS, King E, Stein J, Robinson E, Salameh M, O’Leary KJ. Unit-based interprofessional leadership models in six US hospitals. J Hosp Med. 2014;9(8):545–550. [DOI] [PubMed] [Google Scholar]
- 13.Boxer R VM, Gershanik E, Lewine H, Aylward P, Rossi P, Clemence E. 5Th Time’s a Charm: Creation of Unit-Based Care Teams in a High Occupancy Hospital Paper presented at: Society of Hospital Medicine Annual Meeting 2015; Washington, DC. [Google Scholar]
- 14.Cohen JBW CM Weber S Geographically Assigned Hospitalists with a Multi-Disciplinary Approach: Can Unit-Based Rounding Decrease Length of Stay in a Non-Academic Setting? Paper presented at: Society of Hospital Medicine Annual Meeting 2015; Washington, DC. [Google Scholar]
- 15.Huang KT, Minahan J, Brita-Rossi P, et al. All Together Now: Impact of a Regionalization and Bedside Rounding Initiative on the Efficiency and Inclusiveness of Clinical Rounds. J Hosp Med. 2017;12(3):150–156. [DOI] [PubMed] [Google Scholar]
- 16.Singh S, Tarima S, Rana V, et al. Impact of localizing general medical teams to a single nursing unit. J Hosp Med. 2012;7(7):551–556. [DOI] [PubMed] [Google Scholar]
- 17.Yu DJ. Unit-Based Rounding: A Holy Grail? . The hospitalist. 2012;2012 July;2012(7) [Google Scholar]
- 18.Mueller SK, Call SA, McDonald FS, Halvorsen AJ, Schnipper JL, Hicks LS. Impact of resident workload and handoff training on patient outcomes. Am J Med. 2012;125(1):104–110. [DOI] [PubMed] [Google Scholar]
- 19.Stein J, Payne C, Methvin A, et al. Reorganizing a hospital ward as an accountable care unit. J Hosp Med. 2015;10(1):36–40. [DOI] [PubMed] [Google Scholar]
- 20.Singh S, Fletcher KE. A qualitative evaluation of geographical localization of hospitalists: how unintended consequences may impact quality. J Gen Intern Med. 2014;29(7):1009–1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.