Abstract
Background
Recent evidence has shown that many patients suffer from persistent pain and impaired function after primary or revision total knee arthroplasty (TKA). Post-surgical complications may in addition decrease physical performances and lead to more pain and impacted quality of life.
The purpose of the study was to assess the changes in pain intensity and functional capacity among patients with post-surgical complications after TKA three weeks of intensive, personalized multimodal rehabilitation.
Methods
A retrospective cohort study consisting of 217 patient of which 166 had primary TKA and 51 had revision TKA was conducted. On average, primary TKA patients and revision TKA patients were 3.7 and 2.7 months post-surgical, respectively. All patients have had post-surgical complications and were referred to an inpatient rehabilitation department, where they received a personalized three-week intensive, multimodal rehabilitation protocol. The rehabilitation consisted of sessions targeting neuromuscular function, postural control, and flexibility, sessions focusing on improving muscle strength and cardiovascular function and sessions with focus on gait retraining. The frequency of training was 2–4 sessions/day. The primary outcome was the Knee injury and Osteoarthritis Outcome Score (KOOS) and secondary outcomes were pain intensities measured using numerical rating scale, 6 min. walking test, stair-climbing test and range of motion for knee flexion and extension. Outcome measures were assessed at baseline upon referral and at follow-up before discharge.
Results
All outcomes, except pain at rest in the revision group, improved significantly. KOOS subscales, improved 8.5 to 14.2 in the primary TKA group (p < 0.001) and 6.9 to 10.8 in the revision group (p < 0.001). For the TKA group, effect sizes were medium-to-large for all KOOS subscales, 6 min. walking test, stair-climbing test, and pain intensity during activity. For the revision group, effect sizes were medium-to-large for KOOS subscales symptoms and activity of daily living, 6 min. walking test, stair-climbing test, and knee flexion.
Conclusion
Patients with post-surgical complications after primary or revision TKA experienced clinical relevant improvement in self-reported outcomes, pain relief, and improved physical performances after three weeks of personalized multimodal rehabilitation. The results suggest that an intensive, multimodal approach might be useful to obtain clinically relevant improvements.
Keywords: Total knee replacement, Revision, Pain, Intensive multimodal rehabilitation, Physical therapy
Background
Osteoarthritis (OA) is considered the most frequent cause of disability and pain in the elderly population, and the knee joint is one of the joints most commonly affected [1, 2]. End-stage knee OA is often treated with knee replacement and primary total knee arthroplasty (TKA) is considered an effective treatment for pain relief, improved function and hence quality of life [3, 4]. However, it is well documented that persistent pain and functional disability occur in a large proportion of the patient after an otherwise technically successful TKA [5, 6]. Studies have reported chronic pain rates after primary TKA at 12 months post-operative in 13–17% of the patients and chronic pain rates at 2–7 years post-operative varying between 8 and 27%. Furthermore, 20% of patients 6 months post-operative stated that their primary TKA was not successful in allowing them to resume their regular physical activities [6]. As for patients undergoing revision TKA, a study by Petersen et al. found that 47% of the patients reported severe or unbearable pain 3 years after their latest surgery and regarding functional ability, 37% of the patients were unable to walk a distance > 0.5 km. In general, the patients undergoing revision surgery were less satisfied with their surgery than the patients undergoing primary TKA and revision TKA based solely on the presence of pain cannot be recommended [7, 8].
Pain and surgery lead to a temporary loss of motor function and muscle strength, which often seems to improve in the post-operative phase, especially following a rehabilitation regimen [9–14]. When patients exhibit pain or other post-surgical complications, their rehabilitation may be compromised and result in impaired function, loss of muscle strength and poor postural control. Which rehabilitation strategy is the most optimal has yet to be resolved [15]. It has been proposed that some patients, who does not respond adequately to standard rehabilitation, require a more intensive rehabilitation approach to recover [15–17]. Furthermore, it has also been suggested that rehabilitation should be comprehensive in terms of muscle groups targeted and include progressive exercises [18]. A case study examined patients with post-surgical complications after TKA and found that quadriceps muscle weakness, knee flexion contracture or flexion deficit, muscle tightness and impaired gait were frequently observed in these patients [19]. With an intensive, multimodal treatment approach, the study reduced symptoms and improved function, but the authors did not specify the intervention or used any validated outcome measures, making the validity of the results questionably and treatment recommendations difficult.
Based on the lack of knowledge about management of patients with post-surgical complications after TKA, it is necessary to study the outcomes of intensive multimodal rehabilitation. Hence, there is a need for clinical studies using “best practice” as treatment and including validated outcomes measures to allow for interpretation of the benefits from the treatment. This may elucidate whether intensive rehabilitation can be an effective approach in patients with complications after primary or revision TKA. Therefore, the purpose of this retrospective pragmatic cohort study in real-life settings was to investigate the short-term effect of 3-weeks of intensive, multimodal rehabilitation in patients with complications after primary or revision TKA . The hypothesis was that self-reported outcomes and objective physical performance would improve and pain levels would decrease. Although this observational cohort study did not include a control group, it could provide important information of effect sizes and thereby, be used for designing future randomized controlled trials.
Methods
Patient selection
The study was a retrospective register-based study based on data collected from consecutive patients in the period from February 2017 to June 2018. All patients had been hospitalized at Montebello – Department of Rehabilitation, North Zealand Hospital, Denmark. All patients with primary or revision TKA were referred to the rehabilitation department by their surgeon or family physician, due to post-surgical complications. The main reasons for referral was persistent pain and impaired physical function due to lack of effect from initial rehabilitation, infection, loosening of implants and/or revision surgery. Inclusion criteria was 1) patients with primary TKA or revision TKA, 2) 40–80 years old, 3) body mass index (BMI) within 19–40 kg/m2 and 4) post-surgical complications based on surgeon or family physician examination. Exclusion criteria were lack of complete follow-up and lack of ability to adhere to the treatment. Overall, 166 patients with primary TKA and 51 patients with revision TKA were included in the analysis (Fig. 1). Since all patients were referred to rehabilitation and therefore, must receive the treatment, it was not possible to sample a control group. The study was conducted in accordance with STROBE guidelines and followed the TIDieR guidelines for reporting interventions (Additional file 1) [20, 21]. Due to the retrospective and the quality control nature of the study, no approval from the local ethics committee of the North Denmark Region was required. The study was approved by the Danish Data Protection Agency.
Fig. 1.
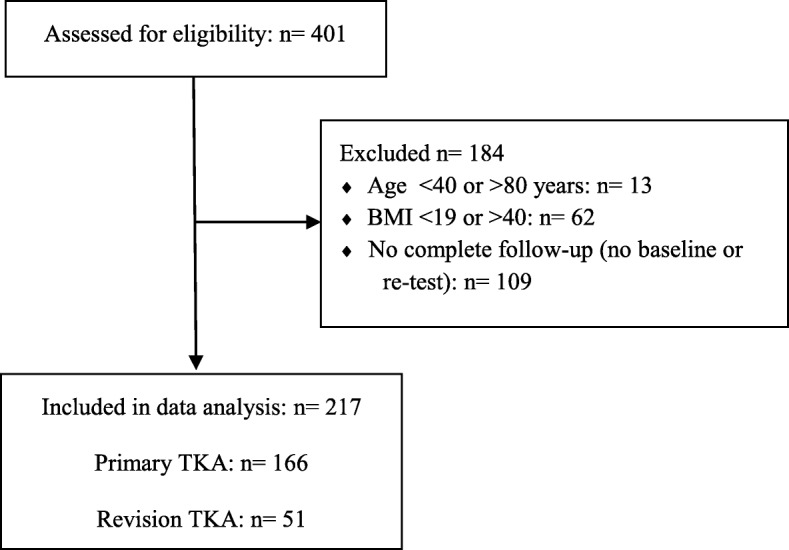
Flow chart. BMI: Body Mass Index. TKA: Total knee arthroplasty
Intervention
All patients referred to Montebello – Department of Rehabilitation undergo a standardized, personalized multimodal treatment protocol. The protocol is a 3-week stay in a rehabilitation hospital during which patients receive intensive, multimodal rehabilitation supervised by physiotherapists. The rehabilitation consisted of sessions targeting neuromuscular function, postural control, and flexibility, sessions focusing on improving muscle strength and cardiovascular function and sessions with focus on gait retraining. Rehabilitation was based on evidence-based exercise programs [22, 23] and included exercises such as pelvic lifts, sit-ups, sliding exercises, lunges, rubber band exercises, and functional movements like chair stands and stair climbing. The frequency of training was two to four sessions per day, lasting from 30 to 50 min. pr. session (for further information on the rehabilitation protocol - see Additional file 2). Exercises were personalized, i.e., adjusted to individual level during the group-based rehabilitation based on physical ability, fatigue and pain level. The total magnitude of exercises was also adjusted on individual basis in order to avoid a “one size fits all” approach since patients have different physical capacity and report different pain intensities. Educational sessions with focus on pain management, information on their prosthesis, relevance of exercise as treatment and how to continue exercising on their own after discharge were provided including teaching self-mobilization techniques to improve knee range of motion (ROM). Patients were gathered in groups of 11 with the same area of problems (i.e. knee) and the same physiotherapist supervised the group for the entire intervention period.
Assessment
All patients referred to the hospital undergoes a test battery at baseline after admission and at re-test before discharge, measuring self-reported outcomes, pain intensity, physical performance during activities of daily living (ADL) and active knee ROM, which are areas that has previously been highlighted as important quality indicators for rehabilitation in clinical practice after TKA [24, 25]. In the present study, the Knee injury and Osteoarthritis Outcome Score (KOOS) was used as the primary outcome. KOOS is a subjective questionnaire covering five subscales of pain, symptoms, activities of daily living (ADL), sports/recreation and quality of life (QOL). Each KOOS subscale consists of multiple items, scored on a 5-point Likert scale; The KOOS ranges from 0 (worst) to 100 (best) [26]. KOOS is a patient self-reported outcome measure reported to be valid and reliable during short-term and long-term follow-up in patients with TKA [27]. An 8–10 point improvement is commonly used as a minimal clinically important difference (MCID) [28]. In the present study, the mean change from baseline to 3-weeks follow-up of 4 subscales evaluating pain, symptoms, activities of daily living and quality of life was used as primary outcomes. The subscale sport/recreation was not included since it measures strenuous activities, which this patient cohort is not expected to participate in and often is contraindicated by the surgeon. This approach was in accordance a previous study within the field of osteoarthritis [29].
Secondary outcomes consists of pain intensity ratings and physical performance measurements. For the index knee, the pain intensity during rest and during activity (i.e. walking, stair climbing) was assessed. A numerical rating scale (NRS) was used, where “0” represents “no pain” and “10” represents “maximal pain”.
The included physical performance measures are part the recommended core set of outcome measures from the OsteoArthritis Research Society International (OARSI) [30]. The 6 min. walk test evaluates the ability to walk a longer distance and the aerobic capacity. The participants were asked to walk as quickly and as safely as possible, without running, along a 21 m. walkway and then turn around a cone, return, and then repeat to cover as much ground as possible on 6 min. Regular walking aid was allowed and as well as resting periods, if necessary. If safety was of concern, the tester followed slightly behind and off to one side of the participant, but not as to pace or impede the participant. The amount of meters covered in 6 min. was the outcome score [30]. The stair climb test consisted of ascending and descending stair activity and thereby was a test of lower body strength and balance. A staircase with 22 stairs was climbed up and down once and participants were asked to ascend and descend stairs as quickly and as safely as possible. Use of a handrail and walking aid were permitted if needed. The amount of time it took to complete the ascending and descending of the stairs was the outcome score [30]. Active knee ROM was assessed in the affected knee. For knee extension, the patient was lying supine and the knee was resting on the examination couch. The axis of the goniometer was aligned on the lateral aspect of the knee joint with one arm of the goniometer in line with the femur and the other in line with the tibia. Keeping the goniometer in place, the knee was actively extended as fully as possible while recording the angle in degrees. The largest angle of the three measurements was noted. For knee flexion, the patient was lying supine and the knee resting on the examination couch. The axis of the goniometer was aligned on the lateral aspect of the knee joint with one arm of the goniometer in line with the femur and the other in line with the tibia. Keeping the goniometer in place and the clinician supporting the weight of the limb, the knee was actively flexed fully with recording of the angles in degrees. The highest of three measurements was recorded [31]. Furthermore, demographic variables such as sex, age, BMI, index leg side, time-since-surgery and reasons for revision surgery were collected.
Data analysis
Data was checked for normality by assessing data frequency in histograms, QQ-plots, and Shapiro-Wilk tests.
For normal distributed outcomes, paired samples t-tests for all continuous outcomes were applied. Data is presented as mean (SD) unless otherwise stated. For the non-normal distributed outcomes, Wilcoxon signed rank test were used and data is presented with median and min-max.
Effect sizes were calculated as Cohen’s d = (MeanAfter - MeanBefore)/SDpooled. Effect sizes were interpreted as 0.2 = “small” effect size, 0.5 = “medium” effect size and 0.8 = “large” effect size, as suggested by Cohen [32].
The significance level was set to 0.05 and results are displayed with 95% confidence intervals. All analysis were performed with the use of the statistical software SPSS, Version 25.0 (SPSS Inc., Chicago, IL, USA).
Results
Demographics
A total of 217 patients (primary TKA: 166, Revision TKA: 51) were included in the analysis. The mean age in each group was 62 and 64 years, respectively. The mean time-since-surgery was 3.7 and 2.7 months in each group (Table 1). All patients with primary TKA had surgery due to end-stage knee OA. Patients with revision TKA had surgery because of infection (14%), implant loosening or instability (51%), pain (20%) or other reasons (15%). A proportion of patients (27%) were excluded from the analysis due to lack of complete data at both baseline or re-test. The major reasons behind the missing data were patient illnesses or early discharges as well as no data available from the KOOS questionnaire, due to a change in outcome measures in the study period. Baseline characteristics of excluded patients can be seen in Table 1. There no significant differences between the characteristics of the included and excluded patients. All included patients concluded three weeks of intensive, multimodal rehabilitation and no side effects were observed.
Table 1.
Patient characteristics for patients included and for those excluded. Values are mean (SD) unless otherwise stated
| Included patients | Excluded patients | |||
|---|---|---|---|---|
| Primary TKA (n: 166) |
Revision TKA (n: 51) |
Primary TKA (n: 68) |
Revision TKA (n: 23) |
|
| Age (years) | 64.0 (8.6) | 62.2 (8.8) | 64.2 (8.7) | 61.7 (9.8) |
| BMI (kg/m2) | 28.9 (4.3) | 28.3 (5.0) | 28.7 (4.5) | 29.4 (5.2) |
| Sex (females, %) | 114 (69%) | 30 (59%) | 48 (71%) | 14 (61%) |
| Index leg (right, %) | 87 (52%) | 30 (59%) | 29 (43%) | 12 (52%) |
| Time-since-surgery (months)a | 3.7 (5.9) | 2.7 (2.4) | 2.9 (3.0) | 2.0 (1.2) |
TKA Total Knee Arthroplasty. BMI Body Mass Index. a Time-since-surgery is the period from the date of surgery (TKA or revision TKA) to the date of starting the rehabilitation
Primary outcome - KOOS
Both the primary TKA and the revision TKA group had significant improvement of all 4 subscales in KOOS. For the primary TKA group there was a mean improvement in the subscales, ranging from 8.5 to 14.2. For the revision TKA group, there was a mean improvement in the subscales, ranging from 6.9 to 10.8. Both groups had the largest improvement in the ADL subscale (Table 2). Effect sizes were 0.57 for KOOS Pain, 0.58 for KOOS Symptoms, 0.88 for KOOS ADL and 0.51 for KOOS QOL for the primary TKA group. For the revision TKA group, effect sizes were 0.38 for KOOS Pain, 0.54 for KOOS Symptoms, 0.70 for KOOS ADL and 0.46 for KOOS QOL.
Table 2.
The Knee injury and Osteoarthritis Outcome Score subscale. Values are mean (SD)
| Primary TKA (n: 166) |
Revision TKA (n: 51) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Before | After | Change | 95% CI | Before | After | Change | 95% CI | |
| KOOS Pain | 54.1 (17.4) | 63.9 (17.8) | 9.8* (14.2) | 7.6; 12.0 | 52.3 (17.2) | 59.3 (19.3) | 6.9* (17.0) | 2.2; 11.7 |
| KOOS Symptoms | 52.8 (16.3) | 62.1 (15.3) | 9.4* (13.7) | 7.3; 11.5 | 52.4 (15.5) | 60.6 (15.0) | 8.2* (14.9) | 4.0; 12.4 |
| KOOS ADL | 58.0 (15.8) | 72.2 (15.5) | 14.2* (13.2) | 12.2; 16.2 | 58.4 (15.6) | 69.1 (15.1) | 10.8* (14.0) | 6.8; 14.7 |
| KOOS QOL | 39.2 (18.0) | 47.7 (17.4) | 8.5* (15.6) | 6.1; 10.9 | 36.5 (18.1) | 45.1 (18.9) | 8.6* (18.3) | 3.5; 13.8 |
ADL Activities of daily living, QOL Quality of life, *: P-value < 0.05.
Secondary outcomes – pain, physical performances and active knee ROM
For the primary TKA group, significant decreases in NRS pain intensity at rest and during activity were reported and a mean decrease on NRS of 1.7 were observed during activity. For the revision TKA group, a significant pain reduction on NRS of 0.8 was reported during activity. At rest, there was a tendency to lower pain intensity on NRS, although non-significant (Table 3). Effect sizes were 0.38 for NRS at rest and 0.62 for NRS at activity for the primary TKA group and 0.11 for NRS at rest and 0.28 for NRS at activity for the revision TKA group.
Table 3.
Pain, physical performances during activity of daily living and active knee range of motion. Values are mean (SD) unless otherwise stated
| Primary TKA (n: 166) |
Revision TKA (n: 51) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Before | After | Change | 95% CI | Before | After | Change | 95% CI | |
| NRS at rest (median, min-max) | 0.0 (0–8) | 0.0 (0–4) | NA * | NA | 0.0 (0–7) | 0.0 (0–7) | NA | NA |
| NRS during activity | 5.4 (2.9) | 3.7 (2.6) | 1.7* (2.6) | [1.3; 2.1] | 5.4 (2.9) | 4.6 (2.8) | 0.8* (1.9) | [0.2; 1.3] |
| 6 min. walking test (m) | 421.9 (91.6) | 513.1 (97.9) | 91.1* (56.6) | [82.4; 100.0] | 407.7 (108.9) | 496.6 (111.8) | 88.8* (60.0) | [72.0; 105.7] |
| Stair climbing test (sec) | 34.8 (18.6) | 23.2 (10.3) | 11.6* (11.9) | [9.7; 13.4] | 38.6 (24.7) | 23.1 (9.8) | 15.5* (17.4) | [10.6; 20.4] |
| Active knee extension (o)§ | 3.3 (5.0) | 2.2 (3.9) | 1.1* (3.0) | [0.6; 1.6] | 2.0 (2.9) | 1.1 (2.2) | 0.9* (2.0) | [0.3; 1.4] |
| Active knee flexion (o) | 106.6 (15.7) | 113.5 (14.9) | 6.9* (5.7) | [6.1; 7.8] | 105.4 (15.3) | 112.4 (14.0) | 7.0* (5.6) | [5.4; 8.5] |
NRS Numerical Rating Scale. Paired samples t-test were used for all outcomes except for NRS at rest, where Wilcoxon Signed Rank test was applied. *: P-value < 0.05. NA: Not applicable. §: Full knee extension = 0o
The primary TKA group had significant improvement in the physical performance tests. The mean improvement in the 6 min. walking test was 91 m and the time spent in the stairclimbing test decreased by 11.6 s. The revision TKA group demonstrated similar, significant improvements with an increase in walking distance of 89 m and a decrease in time spent stairclimbing of 15.5 s (Table 3). Effect sizes were 0.96 for the 6 min. walking test and 0.77 for the stairclimbing test for the primary TKA group and 0.81 for the walking test and 0.82 for the stairclimbing test in the revision TKA group.
Both the primary and the revision TKA groups showed similar, significant improvements in knee ROM. For knee extension, a mean increase in ROM of 1.1 and 0.9o were observed. For the knee flexion, a mean increase in ROM of 6.9 and 7.0o in the primary and revision TKA groups, respectively, were observed (Table 3). Effect sizes were 0.40 for knee extension and 0.45 for knee flexion in the primary TKA group and 0.35 for knee extension and 0.64 for knee flexion in the revision TKA group.
Discussion
This retrospective cohort study analyzed data from consecutive patients with post-surgical complications after primary or revision TKA that received three weeks of intensive, personalized multimodal rehabilitation. In line with the hypothesis, we found that both groups showed significant improvements in self-reported outcomes, pain intensities, and physical performances. Therefore, these results provide initial knowledge regarding exercise types and frequency in patients with post-surgical complications after primary or revision TKA in real-life settings.
The results indicate that patients with postoperative complications can benefit from intensive, multimodal rehabilitation. Both the primary and revision TKA groups had significant improvement in all outcome measures, except pain at rest for the revision TKA group. Effect sizes were interpreted as “small” in NRS at rest for both groups, NRS at activity for revision TKA group, knee extension for both groups, knee flexion in the TKA group, and KOOS Pain and QOL for the revision TKA group, as “medium” in NRS at activity and KOOS Pain, Symptoms and QOL for the primary TKA group, KOOS Symptoms and ADL for the revision TKA group, stair-climbing test in the TKA group and knee flexion in the revision TKA group and as “large” for the KOOS ADL in the TKA group, the 6 min. walking test for both groups and the stair-climbing test in the revision TKA group. When reviewing the results, a tendency towards better improvement from the multimodal rehabilitation program in the primary TKA group compared with the revision TKA group was observed. This tendency could indicate that patients undergoing revision TKA may require a longer period of rehabilitation and maybe different treatment protocols than standard care. Generally, patients with revision TKA are more complicated as they have had the pain longer with a stronger impact on the nervous system (e.g. central sensitization) [33]. This assumption is supported by the literature considering the reported lower level of satisfaction and markedly impaired function after revision TKA [7].
Regarding the primary outcome on the KOOS subscales, both the primary and the revision TKA groups experienced improvement ranging from 9–14 and 7–11 points, respectively. Thus, the improvement in KOOS can be considered clinically relevant [28]. However, threshold values for clinical relevance are still a matter of discussion [34]. Moreover, the timing of follow-up assessment might have an impact on the measured improvements in e.g., KOOS. Concerning the NRS scores, decreases in pain intensities were observed at both rest and during activity. A study by Salaffi et al. proposed that a decrease of 1 point in NRS could be interpreted as “slightly better” and a decrease of 2 points on NRS could be interpreted as “much better” and, therefore, proposed a MCID of 1–2 points on NRS [35]. Applied to the current study’s result, it would mean that the decrease in pain during activity for the primary TKA should be considered clinically relevant and the observed pain decreases during activity for the revision TKA group and at rest for both groups lies below what is considered clinically relevant.
The results of the current study indicates that some patients needs a more intensive and comprehensive approach regarding rehabilitation, than the often used 2–3 exercise sessions pr. week [29, 36, 37] underlining the importance of personalized intervention programs. Clinical significant improvements can be observed after an intensive three-week rehabilitation protocol. Due to the multimodal nature of the rehabilitation program, it is not possible to recommend specific elements of the rehabilitation protocol. Consequently, it is unknown if some exercises were more effective or if the combination of exercises were the most important component of the rehabilitation. Patients undergoing primary or revision TKA often exhibit multiple deficits, such as pains, impaired muscle strength and physical ability, poor balance, lack of ability to coordinate movement and recruit specific muscles and poor alignment during walking [6, 9]. This highlights the need for a thorough rehabilitation protocol when addressing deficits in patients after primary and revision TKA, aiming at treating the multi-factorial mechanisms behind the deficits. Seasonal variation in exercises occurred because of the real-life settings, which means that some patients received aquatic exercises while others did not. A secondary analysis (Additional file 3) revealed no clinical or significant differences in the outcomes between these groups. Since overall magnitude of the exercises was kept constant for all patients, this indicates that time spent exercising seems to be more important than inclusion of aquatic exercises or not.
Limitations
There are obvious limitations in a retrospective cohort study. Due to exclusion of patients because of no data available from the KOOS questionnaire, a secondary analysis between those patients with and without KOOS scores were performed. This analysis revealed no clinical or significant differences regarding pain intensities and functional performance (Additional file 4) reducing the potential role of selection bias. Due to discharge after three weeks, no long-term follow-up data exists. Therefore, it is unknown if the benefits gained from the intensive rehabilitation persists over time. A review has underlined that it is necessary to keep exercising to maintain the benefits [38]. As a part of the educational sessions, patients are taught the need of further exercising and a specific, personalized exercises program is being draw up by the physiotherapist. Due to the observational nature and clinical approach of the study, there was no control group and therefore, the effect of time cannot be taken into consideration. Thus, compared with a control group, the effect sizes might have differed. However, the study reflects the clinical settings the rehabilitation protocol must comply with and allows for overall advices for patients with post-surgical complications after primary and revision TKA.
Conclusion
The present retrospective study showed that, patients with post-surgical complications, undergoing three weeks of intensive, personalized multimodal rehabilitation after primary or revision TKA resulted in clinical relevant improvement in self-reported outcomes, significant pain relief, and improved physical performances. The results indicated that a tailored multimodal approach might be useful to obtain improvements in a cohort of patients with post-surgical complications after primary and revision TKA. Further randomized control trials assessing the effects of multimodal rehabilitation after primary or revision TKA are warranted.
Supplementary information
Additional file 2. Rehabilitation protocol.
Additional file 3. Table S4 illustrating a secondary analysis.
Additional file 4. Table S5 illustrating a secondary analysis.
Acknowledgements
We thank the staff at Montebello - Department of Rehabilitation, North Zealand Hospital, Denmark for their ongoing work and we thank the patients for their contributions to the study.
Abbreviations
- ADL
Activities of daily living
- BMI
Body mass index
- KOOS
Knee injury and osteoarthritis outcome score
- MCID
Minimal clinically important difference
- NRS
Numerical rating scale
- OA
Osteoarthritis
- QOL
Quality of life
- ROM
Range of motion
- SD
Standard deviation
- TKA
Total knee arthroplasty
Authors’ contributions
JBL was responsible for conception and designing the study, data analysis and interpretation of data and in drafting the manuscript. LM made substantial contributions to conception of the study and reviewed the manuscript critically for intellectual content. PM made substantial contributions to data analysis and interpretation of data and reviewed the manuscript critically for intellectual content. LAN made substantial contributions to data analysis and interpretation of data and reviewed the manuscript critically for intellectual content. All authors had full access to data in the study and made substantial contributions in preparing the final version of the paper. All authors approved the final manuscript, and agreed to be accountable for all aspects of this research.
Funding
Innovationsfonden (Individualized Osteoarthritis Interventions) was acknowledged for their individual and independent funding. The study sponsor had no involvement in executing the study, interpretation of data or publishing of the results.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Ethical approval is not required due to the register-based nature of the study. This is based on the Act on Research Ethics Review of Health Research Projects, section 14, [2] “Notification of questionnaire surveys and medical database research projects to the system of research ethics committee system is only required if the project involves human biological material” (http://en.nvk.dk/rules-and-guidelines/act-on-research-ethics-review-of-health-research-projects). The study was approved by the Danish Data Protection Agency.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jesper Bie Larsen, Email: jbl@hst.aau.dk.
Lisbeth Mogensen, Email: lisbeth.mogensen@montebello.es.
Lars Arendt-Nielsen, Email: LAN@hst.aau.dk.
Pascal Madeleine, Email: pm@hst.aau.dk.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s13102-020-0157-1.
References
- 1.Peat G, McCarney R, Croft P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann Rheum Dis. 2001;60(2):91–97. doi: 10.1136/ard.60.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dieppe PA, Lohmander LS. Pathogenesis and management of pain in osteoarthritis. Lancet. 2005;365(9463):965–973. doi: 10.1016/S0140-6736(05)71086-2. [DOI] [PubMed] [Google Scholar]
- 3.Price AJ, Alvand A, Troelsen A, Katz JN, Hooper G, Gray A, et al. Knee replacement. Lancet. 2018;392(10158):1672–1682. doi: 10.1016/S0140-6736(18)32344-4. [DOI] [PubMed] [Google Scholar]
- 4.Carr AJ, Robertsson O, Graves S, Price AJ, Arden NK, Judge A, et al. Knee replacement. Lancet. 2012;379(9823):1331–1340. doi: 10.1016/S0140-6736(11)60752-6. [DOI] [PubMed] [Google Scholar]
- 5.Beswick AD, Wylde V, Gooberman-Hill R, Blom A, Dieppe P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open. 2012;2(1):e000435. doi: 10.1136/bmjopen-2011-000435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wylde V, Dieppe P, Hewlett S, Learmonth ID. Total knee replacement: is it really an effective procedure for all? Knee. 2007;14(6):417–423. doi: 10.1016/j.knee.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 7.Petersen KK, Simonsen O, Laursen MB, Nielsen TA, Rasmussen S, Arendt-Nielsen L. Chronic postoperative pain after primary and revision total knee arthroplasty. Clin J Pain. 2015;31(1):1–6. doi: 10.1097/AJP.0000000000000146. [DOI] [PubMed] [Google Scholar]
- 8.Arendt-Nielsen L. Joint pain: more to it than just structural damage? Pain. 2017;158(Suppl 1):S66–S73. doi: 10.1097/j.pain.0000000000000812. [DOI] [PubMed] [Google Scholar]
- 9.Schache MB, McClelland JA, Webster KE. Lower limb strength following total knee arthroplasty: a systematic review. Knee. 2014;21(1):12–20. doi: 10.1016/j.knee.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 10.Danish Health Authority. Knee osteoarthritis – national clinical guidelines. Copenhagen: Danish Health Authority; 2012. www.sst.dk.
- 11.Artz N, Elvers KT, Lowe CM, Sackley C, Jepson P, Beswick AD. Effectiveness of physiotherapy exercise following total knee replacement: systematic review and meta-analysis. BMC Musculoskelet Disord. 2015;16:15. doi: 10.1186/s12891-015-0469-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Minns Lowe CJ, Barker KL, Dewey M, Sackley CM. Effectiveness of physiotherapy exercise after knee arthroplasty for osteoarthritis: systematic review and meta-analysis of randomised controlled trials. BMJ. 2007;335(7624):812. doi: 10.1136/bmj.39311.460093.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moutzouri M, Gleeson N, Coutts F, Tsepis E, John G. Early self-managed focal sensorimotor rehabilitative training enhances functional mobility and sensorimotor function in patients following total knee replacement: a controlled clinical trial. Clin Rehabil. 2018;1:269215518757291. doi: 10.1177/0269215518757291. [DOI] [PubMed] [Google Scholar]
- 14.Kauppila AM, Kyllonen E, Ohtonen P, Hamalainen M, Mikkonen P, Laine V, et al. Multidisciplinary rehabilitation after primary total knee arthroplasty: a randomized controlled study of its effects on functional capacity and quality of life. Clin Rehabil. 2010;24(5):398–411. doi: 10.1177/0269215509346089. [DOI] [PubMed] [Google Scholar]
- 15.Davila Castrodad IM, Recai TM, Abraham MM, Etcheson JI, Mohamed NS, Edalatpour A, et al. Rehabilitation protocols following total knee arthroplasty: a review of study designs and outcome measures. Ann Transl Med. 2019;7(Suppl 7):S255. doi: 10.21037/atm.2019.08.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bade MJ, Kohrt WM, Stevens-Lapsley JE. Outcomes before and after total knee arthroplasty compared to healthy adults. J Orthop Sports Phys Ther. 2010;40(9):559–567. doi: 10.2519/jospt.2010.3317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Oktas B, Vergili O. The effect of intensive exercise program and kinesiotaping following total knee arthroplasty on functional recovery of patients. J Orthop Surg Res. 2018;13(1):233. doi: 10.1186/s13018-018-0924-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bade MJ, Stevens-Lapsley JE. Restoration of physical function in patients following total knee arthroplasty: an update on rehabilitation practices. Curr Opin Rheumatol. 2012;24(2):208–214. doi: 10.1097/BOR.0b013e32834ff26d. [DOI] [PubMed] [Google Scholar]
- 19.Bhave A, Mont M, Tennis S, Nickey M, Starr R, Etienne G. Functional problems and treatment solutions after total hip and knee joint arthroplasty. J Bone Joint Surg Am. 2005;87(Suppl 2):9–21. doi: 10.2106/JBJS.E.00628. [DOI] [PubMed] [Google Scholar]
- 20.Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687. doi: 10.1136/bmj.g1687. [DOI] [PubMed] [Google Scholar]
- 21.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–1499. doi: 10.1016/j.ijsu.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 22.Ageberg E, Link A, Roos EM. Feasibility of neuromuscular training in patients with severe hip or knee OA: the individualized goal-based NEMEX-TJR training program. BMC Musculoskelet Disord. 2010;11:126. doi: 10.1186/1471-2474-11-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bade MJ, Struessel T, Dayton M, Foran J, Kim RH, Miner T, et al. Early high-intensity versus low-intensity rehabilitation after Total knee Arthroplasty: a randomized controlled trial. Arthritis Care Res (Hoboken) 2017;69(9):1360–1368. doi: 10.1002/acr.23139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Westby MD, Marshall DA, Jones CA. Development of quality indicators for hip and knee arthroplasty rehabilitation. Osteoarthr Cartil. 2018;26(3):370–382. doi: 10.1016/j.joca.2017.10.020. [DOI] [PubMed] [Google Scholar]
- 25.Howe TE, Dawson LJ, Syme G, Duncan L, Reid J. Evaluation of outcome measures for use in clinical practice for adults with musculoskeletal conditions of the knee: a systematic review. Man Ther. 2012;17(2):100–118. doi: 10.1016/j.math.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 26.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee injury and osteoarthritis outcome score (KOOS)--development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- 27.Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS) Arthritis Care Res (Hoboken) 2011;63(Suppl 11):S208–S228. doi: 10.1002/acr.20632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1:64. doi: 10.1186/1477-7525-1-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Skou ST, Roos EM, Laursen MB, Rathleff MS, Arendt-Nielsen L, Simonsen O, et al. A randomized, controlled trial of Total knee replacement. N Engl J Med. 2015;373(17):1597–1606. doi: 10.1056/NEJMoa1505467. [DOI] [PubMed] [Google Scholar]
- 30.Dobson F, Hinman RS, Roos EM, Abbott JH, Stratford P, Davis AM, et al. OARSI recommended performance-based tests to assess physical function in people diagnosed with hip or knee osteoarthritis. Osteoarthr Cartil. 2013;21(8):1042–1052. doi: 10.1016/j.joca.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 31.Jakobsen TL, Christensen M, Christensen SS, Olsen M, Bandholm T. Reliability of knee joint range of motion and circumference measurements after total knee arthroplasty: does tester experience matter? Physiother Res Int. 2010;15(3):126–134. doi: 10.1002/pri.450. [DOI] [PubMed] [Google Scholar]
- 32.Cohen J. The effect size. Statistical power analysis for the behavioral sciences. 2nd ed. United States of America: Lawrence Erlbaum Associates; 1988. p. 77.
- 33.Arendt-Nielsen L, Simonsen O, Laursen MB, Roos EM, Rathleff MS, Rasmussen S, et al. Pain and sensitization after total knee replacement or nonsurgical treatment in patients with knee osteoarthritis: identifying potential predictors of outcome at 12 months. Eur J Pain. 2018;22(6):1088–1102. doi: 10.1002/ejp.1193. [DOI] [PubMed] [Google Scholar]
- 34.Lyman S, Lee YY, McLawhorn AS, Islam W, MacLean CH. What are the minimal and substantial improvements in the HOOS and KOOS and JR versions after Total joint replacement? Clin Orthop Relat Res. 2018;476(12):2432–2441. doi: 10.1097/CORR.0000000000000456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Salaffi F, Stancati A, Silvestri CA, Ciapetti A, Grassi W. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur J Pain. 2004;8(4):283–291. doi: 10.1016/j.ejpain.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 36.Piva SR, Almeida GJ, Gil AB, DiGioia AM, Helsel DL, Sowa GA. Effect of comprehensive behavioral and exercise intervention on physical function and activity participation after Total knee replacement: a pilot randomized study. Arthritis Care Res (Hoboken) 2017;69(12):1855–1862. doi: 10.1002/acr.23227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fransen M, Nairn L, Bridgett L, Crosbie J, March L, Parker D, et al. Post-acute rehabilitation after Total knee replacement: a multicenter randomized clinical trial comparing long-term outcomes. Arthritis Care Res (Hoboken) 2017;69(2):192–200. doi: 10.1002/acr.23117. [DOI] [PubMed] [Google Scholar]
- 38.Kroll HR. Exercise therapy for chronic pain. Phys Med Rehabil Clin N Am. 2015;26(2):263–281. doi: 10.1016/j.pmr.2014.12.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 2. Rehabilitation protocol.
Additional file 3. Table S4 illustrating a secondary analysis.
Additional file 4. Table S5 illustrating a secondary analysis.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.


