Abstract
A young female patient presented with features of ascites and cholecystitis. She was subsequently diagnosed with an acute Epstein-Barr virus infection. This is a rare presentation of a common infection. The patient was managed conservatively and the illness resolved within 6 weeks.
Keywords: infection (gastroenterology), hepatitis other, hepatitis and other GI infections
Background
Epstein-Barr virus (EBV) is a gammaherpesvirus in the family Herpesviridae and is one of the most common viral infections worldwide.1 It is transmitted via bodily fluids, especially saliva2 3 and causes infectious mononucleosis, which is usually self-limiting.4 Hepatosplenomegaly and derangement of liver function tests are common.4 5 However, acute acalculous cholecystitis with ascites as a complication of primary EBV infection is rare.4 6 We present the case of a patient with acute EBV infection complicated by acute acalculous cholecystitis and ascites.
Case presentation
A 20-year-old woman who was previously healthy, presented with 9-day history of malaise, fever of 39°C, rigours, sore throat, intermittent lower abdominal pain, vomiting and a mass on the left side of the neck. She had no significant medical history and no allergies. She had moved in the UK 3 months ago from Poland and lived with the same partner.
On examination, there was jaundice and tenderness of the epigastrium and right hypochondrium with mild abdominal distention. She had mildly swollen eyelids, inflamed and erythematous tonsils, palpable cervical lymph nodes measuring about 1.5 cm on the left side and palpable bilateral axillary lymph nodes measuring about 2 cm.
Investigations
Her liver function tests were deranged and cholestatic markers were significantly elevated. Bilirubin peaked at 118 umol/L, alanine aminotransferase (ALT) at 247 unit/L and alkaline phosphatase (ALP) at 840 unit/L. Inflammatory markers were mildly raised and peripheral blood lymphocytosis was noted. Atypical lymphocytes were also seen in blood film microscopy. Hepatitis A IgG and IgM, hepatitis E IgM and hepatitis C IgG antibodies were not detected. Hepatitis B surface antigen was not detected and hepatitis B surface antibody was 24 mIU/mL. HIV-1 and HIV-2 antibodies were negative. Cytomegalovirus IgM and IgG were positive. Anti-EBV IgM antibody against viral capsid antigen was detected, in the absence of IgG antibody, indicating an acute primary EBV infection. Infectious mononucleosis screening for heterophile antibodies came back positive.
CT of abdomen and pelvis was carried out to check for hepatosplenomegaly and demonstrated moderate hepatosplenomegaly, very oedematous gallbladder with marked peripheral oedema and moderate amount of fluid in the recto-uterine pouch, appearances suggesting acute hepatitis.
Ultrasound scan of the abdomen (figure 1) was done to look for gallstones and revealed enlarged liver measuring 17.2 cm, oedematous and thickened gallbladder throughout, measuring 12.2 cm. No gallstones were detected. The spleen was enlarged to 16.6 cm and splenic varices were noted. Free fluid in the hepatorenal space was also identified. These appearances were consistent with cholecystitis with oedema throughout the gallbladder wall and ascites.
Figure 1.
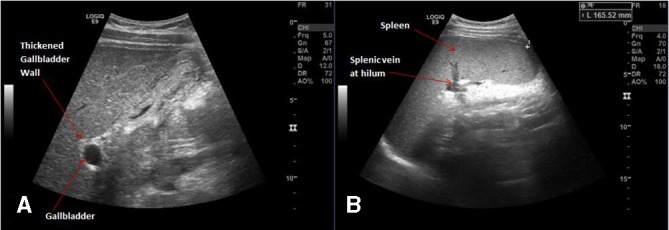
Abdominal ultrasonography demonstrating thickened and oedematous gallbladder, without gallstones (A) and enlarged spleen (B).
Treatment
This illness is generally self-resolving and patient required no further intervention, apart from supportive care. No antiviral medications have been shown to be beneficial in clinical trials.7 In this patient, this was a rare presentation of an acute EBV infection and an important diagnosis to make, in order to avoid unnecessary investigations and treatment as well as prolonged hospital stays. She was discharged home shortly after her EBV results were known. Advice was given to avoid contact sports for the next 6 weeks to prevent rupture of the enlarged spleen.8
Outcome and follow-up
The patient was seen in the infectious diseases clinic 6 weeks after discharge. The liver function tests were within normal range and bilirubin was found to be 15 umol/L, ALT was 25 unit/L and ALP was 107 unit/L. She was clinically well, without any residual lymph node enlargement or tenderness. The patient was therefore discharged from clinic.
Discussion
Gallstones are involved in more than 90% of cholecystitis cases. Acute acalculous cholecystitis refers to inflammation of the gallbladder without presence of gallstones. Various bacterial and viral infections have been shown to cause this type of cholecystitis.9 It is however rare during acute primary EBV infection. The overwhelming majority of these cases are in female patients,4–6 such as ours. Acute acalculous cholecystitis and ascites in the context of primary EBV infection is rare. Acute acalculous cholecystitis in primary EBV infection has been reported in patients most commonly in those in their 40s or 80s.9
The virus remains latent in memory B cells in the majority of cases. Asymptomatic viral shedding can lead to transmission to other individuals.10 After an incubation period of typically 2–7 weeks,10 patients initially develop non-specific symptoms, which may be followed by fever, pharyngitis, tonsillitis, lymphadenopathy, periorbital oedema, palatal petechiae, splenomegaly, hepatomegaly and rash. Blood testing usually reveals lymphocytosis, elevated liver enzymes and raised bilirubin levels.5 Acute acalculous cholecystitis is accompanied by fever, vomiting, right upper quadrant pain and high ALP.4
The pathogenesis of acute acalculous cholecystitis and ascites resulting from EBV infection has not been clearly defined, but it is believed that cholestasis, resulting from hepatitis, leads to inflammation of the gallbladder.3 In comparison to hepatitis A infection, EBV has not been shown to directly infect the gallbladder.5
Diagnosis is suspected based on clinical and laboratory findings and confirmed by an abdominal ultrasound scan or CT.4 In our case, blood tests demonstrated a cholestatic picture and abdominal CT and ultrasound revealed thickened and oedematous gallbladder and enlarged liver with ascites, appearances consistent with hepatitis and cholecystitis.
Most reported cases were managed conservatively and only one patient, who was treated with azathioprine for inflammatory bowel disease, required cholecystectomy.11 Treatment with antibiotics was of no benefit and in the majority of cases it was discontinued after EBV was detected. The infection was self-remitting and complete resolution was noted in all patients.4
Learning points.
Acute acalculous cholecystitis and ascites are rare complications of Epstein-Barr viral infection and mostly affect female patients.
Elevated cholestatic markers are noted in blood tests and abdominal ultrasound is the most useful for the diagnosis of acalculous cholecystitis.
Conservative management of this condition is sufficient to achieve full resolution and antibiotics are not indicated. Surgical intervention is very rarely required.
Footnotes
Contributors: KTL contributed to planning, reporting the work described, language editing and technical editing. NE contributed to technical editing, language editing and proofreading. EP was involved in patient care, consented the patient and reviewed the final version of the case report. ST was involved in patient care and contributed to language editing and proofreading. ST also critically reviewed the case report and provided general supervision.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Virgin HW, Wherry EJ, Ahmed R. Redefining chronic viral infection. Cell 2009;138:30–50. 10.1016/j.cell.2009.06.036 [DOI] [PubMed] [Google Scholar]
- 2. Pagano JS. Is Epstein-Barr virus transmitted sexually? J Infect Dis 2007;195:469–70. 10.1086/510861 [DOI] [PubMed] [Google Scholar]
- 3. Gagneux-Brunon A, Suy F, Pouvaret A, et al. Acute acalculous cholecystitis, a rare complication of Epstein-Barr virus primary infection: report of two cases and review. J Clin Virol 2014;61:173–5. 10.1016/j.jcv.2014.05.019 [DOI] [PubMed] [Google Scholar]
- 4. Yesilbag Z, Karadeniz A, Kaya FO. Acute acalculous cholecystitis: a rare presentation of primary Epstein-Barr virus infection in Adults—Case report and review of the literature. Case Rep Infect Dis 2017;2017:1–5. 10.1155/2017/5790102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Agergaard J, Larsen CS. Acute acalculous cholecystitis in a patient with primary Epstein-Barr virus infection: a case report and literature review. Int J Infect Dis 2015;35:67–72. 10.1016/j.ijid.2015.04.004 [DOI] [PubMed] [Google Scholar]
- 6. Beltrame V, Andres A, Tona F, et al. Epstein-Barr virus - associated acute acalculous cholecystitis in an adult. Am J Case Rep 2012;13:153–6. 10.12659/AJCR.883245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pagano J, Whitehurst C, Andrei G. Antiviral drugs for EBV. Cancers 2018;10:197 10.3390/cancers10060197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lennon P, Crotty M, Fenton JE. Infectious mononucleosis. BMJ 2015;350:h1825 10.1136/bmj.h1825 [DOI] [PubMed] [Google Scholar]
- 9. Barie PS, Eachempati SR. Acute acalculous cholecystitis. Curr Gastroenterol Rep 2003;5:302–9. 10.1007/s11894-003-0067-x [DOI] [PubMed] [Google Scholar]
- 10. Peter J, Ray CG. Infectious mononucleosis. Pediatr Rev 1998;19:276–9. 10.1542/pir.19-8-276 [DOI] [PubMed] [Google Scholar]
- 11. Hagel S, Bruns T, Kantowski M, et al. Cholestatic hepatitis, acute acalculous cholecystitis, and hemolytic anemia: primary Epstein–Barr virus infection under azathioprine. Inflamm Bowel Dis 2009;15:1613–6. 10.1002/ibd.20856 [DOI] [PubMed] [Google Scholar]


