Abstract
Afferent loop syndrome is a rare complication after gastrectomy with Billroth II or Roux-en-Y reconstruction, caused by an obstruction in the proximal loop. The biliary stasis and bacterial overgrowth secondary to this obstruction can lead to repeated episodes of acute cholangitis. We present the case of a male patient who had previously undergone gastrectomy with Roux-en-Y reconstruction and later experienced multiple episodes of acute cholangitis secondary to choledocolithiasis. He underwent an open exploration of the bile ducts with choledocolitotomy, but the events of cholangitis persisted. Further investigation permitted to identify a dilation of the biliary loop of the Roux-en-Y anastomosis, suggesting enterobiliary reflux as the cause of recurrent acute cholangitis. Therefore, a bowel enterectomy and new jejunojejunostomy were undertaken, and normal biliary flow was re-established. The surgical treatment is mandatory in benign causes, leading to the resolution of the obstruction and subsequent normalisation of bile flow.
Keywords: pancreas and biliary tract, gastrointestinal surgery
Background
Afferent loop syndrome is a rare complication of partial gastrectomy with Billroth II gastrojejunostomy reconstruction.1 It is caused by a partial or total obstruction of the afferent loop of the anastomosis. It is typically a chronic complication that may occur several years after surgery and can be caused by adhesions, kinking and angulation of the small bowel, internal herniation or stenosis of the gastro-jejunal anastomosis.2 3 A similar effect can occur after a Roux-en-Y reconstruction by stenosis or obstruction of the biliopancreatic limb.2–5
Obstruction of the afferent loop causes biliary and pancreatic secretions to accumulate and cause distention of this bowel segment. In rare cases, the stasis of these secretions in the intestinal lumen can promote bacterial infection within the biliary tree, resulting in recurrent episodes of cholangitis.6
The authors present a challenging case of a patient with a personal background of a distal gastrectomy secondary to peptic ulcer disease. He developed multiple cholangitis episodes, which were initially attributed to choledocolithiasis, but ultimately were due to afferent loop syndrome and secondary choledocolithiasis.
Case presentation
A 49-year-old Caucasian male patient presented to the emergency department with epigastric pain, nausea and vomiting of 1 day duration. He had a previous subtotal gastrectomy with Roux-en-Y anastomosis 15 years ago, secondary to pyloric stenosis due to peptic ulcer disease. His medical history included type 2 diabetes and hypertension, and he took pantoprazole, bisoprolol and metformin.
On admission, the patient was apyrexial and haemodynamically stable, with epigastric and right upper quadrant tenderness on palpation.
Laboratory tests revealed elevation of aspartate aminotransferase (140 U/L), alanine aminotransferase (184 U/L), gamma-glutamyl transferase (GGT) (448 U/L) and total bilirubin (4.8 mg/dL; normal: <1.2 mg/dL); white cell count and C-reactive protein (CRP) were normal. The abdominal ultrasound showed a dilated common bile duct at 12 mm and gallbladder. The gallbladder was thin-walled and contained a single stone in the infundibulum. The patient was admitted to the surgical department with the diagnosis of biliary colic with likely choledocolithiasis. He was treated with fluids and analgesics. There was a clinical deterioration in the subsequent days, with respiratory failure and elevation of inflammatory parameters and worsening cholestasis. This deterioration precipitated intensive care admission and endotracheal intubation with mechanical ventilation. To gain acute biliary drainage, a percutaneous cholecystostomy was performed, and broad-spectrum antibiotics were administered with an associated clinical improvement. The patient was discharged on the 20th day of hospitalisation.
Investigations
One month after this episode, the patient came again to the emergency department with fever (38.2°C) and right upper quadrant pain. Analytically, the patient had leucocytosis (15.700×109/L), elevated serum bilirubin level (6.1 mg/dL), elevated CRP (13.7 mg/dL) and GGT (354 U/L). Abdominal ultrasound revealed dilation of the intrahepatic and common bile ducts and a collapsed gallbladder with the cholecystostomy drain inside it. He was admitted with a second episode of acute cholangitis (Escherichia coli identified in bile cultures) and completed therapy with piperacillin–tazobactam for 7 days with clinical improvement.
One month after, the patient underwent elective open cholecystectomy, complicated with deep infection of the suture by Methicillin-resistant Staphylococcus aureus (MRSA), having received vancomycin therapy for 10 days.
After 3 years, the patient came to the emergency department with hyperglycaemia for 2 weeks, polydipsia, polyuria, asthenia, vomiting, fever and abdominal pain for 2 days. Abdomen examination did not reveal signs of peritoneal irritation. Laboratory exams showed elevation of glucose levels (345 mg/dL), GGT (859 U/L), alkaline phosphatase (AP) (526 U/L), total bilirubin (5.5 mg/dL), white cell count (15.800×109/L) and CRP (5.44 mg/dL). Ultrasound revealed dilatation of both intrahepatic and extrahepatic bile ducts.
The patient was admitted with his third episode of acute cholangitis, with diabetic decompensation. He started on broad-spectrum antibiotics and adjustment of insulin therapy.
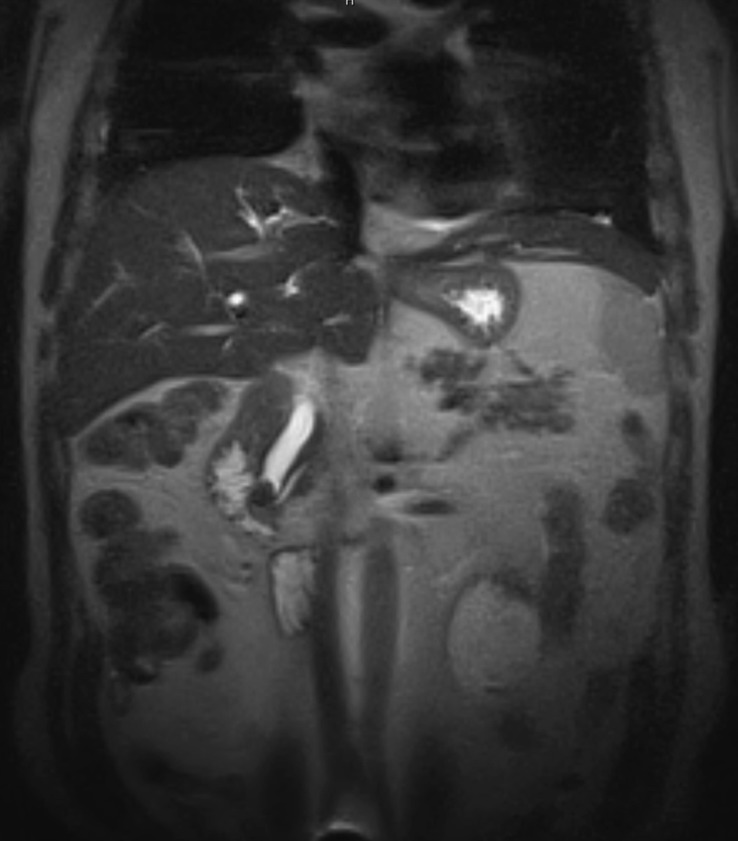
A magnetic resonance cholangiopancreatography (MRCP) was performed, showing intrahepatic and extrahepatic bile duct dilation (16 mm), with two obstructive stones at its distal end (figure 1).
Figure 1.
Magnetic resonance cholangiopancreatography showing obstructive stones in the distal common bile duct.
The patient was discharged after 12 days of imipenem, with clinical and laboratorial improvement.
Treatment
Two months after the last admission, the patient was submitted to an exploration of the bile ducts with choledocolitotomy and choledochoduodenostomy. He was discharged on the sixth postoperative day without complications.
Two weeks after the surgery, the patient came to the emergency department with fever and right upper quadrant pain. Laboratory tests showed leucocytosis (16.600×109/L), and elevated bilirubin level (4.9 mg/dL), GGT (198 U/L) and AP (405 U/L). He was hospitalised with a new episode of acute cholangitis and was discharged after intravenous antibiotic therapy.
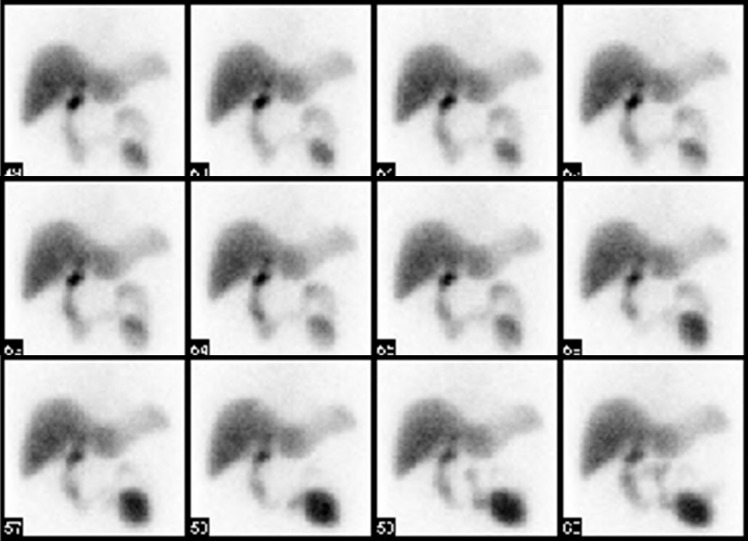
After 2 weeks, the patient presented with the same symptoms and with leucocytosis, elevated CRP and cholestasis in laboratory tests. He performed an abdominal CT, which showed pneumobilia and a dilated segment of small bowel in left quadrants; no abscesses or peritoneal effusion were identified (figure 2). After that, a hepatobiliary iminodiacetic acid (HIDA) scintigraphy was done, showing a delay in bile elimination through the small bowel, with good permeability of bile ducts (figure 3).
Figure 2.
Abdominal CT with dilated jejunojejunostomy of the Roux-en-Y anastomosis.
Figure 3.
Hepatobiliary iminodiacetic acid scintigraphy showing a delay in bile elimination and accumulation of contrast in the afferent small bowel loop.
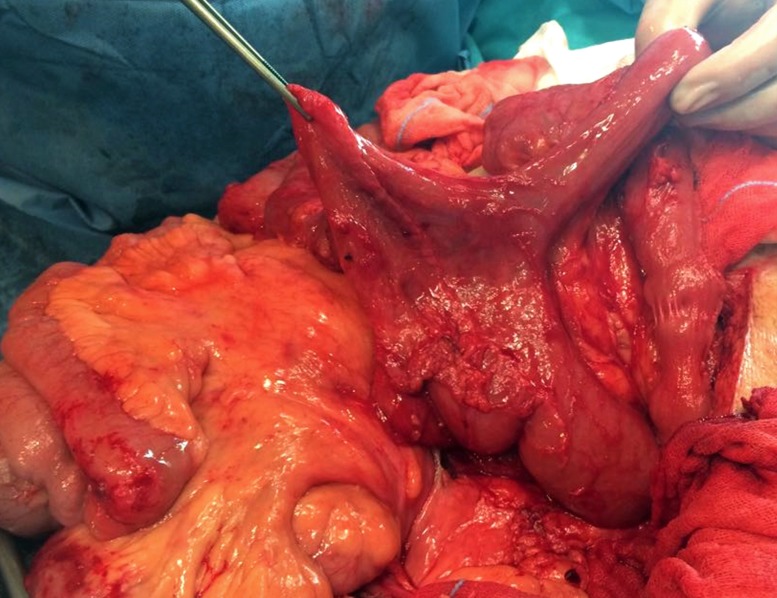
The diagnosis of afferent loop syndrome was considered, and the patient underwent a midline laparotomy, in which a massive dilation of afferent Roux-en-Y loop, secondary to multiple adhesions, was observed (figure 4). A bowel enterectomy was performed, and new jejunojejunostomy of the Roux-en-Y anastomosis was created. The patient was discharged on the eighth postoperative day without complications.
Figure 4.
Massive dilation of afferent Roux-en-Y loop.
Outcome and follow-up
HIDA scintigraphy 1 month after surgery revealed average bile clearance.
The patient is in follow-up in a surgical consult for 4 years, with no complaints and without new episodes of acute cholangitis.
Discussion
Afferent loop syndrome is a rare complication that occurs in 0.2%–1% in patients after gastrectomy with a Billroth II or Roux-en-Y anastomosis.2–4 This condition is generally caused by mechanical occlusion of the afferent or biliopancreatic loop, due to recurrence or metastasis of cancer in malignant settings, adhesions, internal hernia, torsion, kinking at the anastomosis or enterolithiasis. In contrast, non-obstructive afferent loop syndrome may be caused by biliary stasis due to jejunal motility failure, or biliary enteric reflux due to a short biliopancreatic Roux-en-Y limb, leading to acute cholangitis, liver abscess, acute pancreatitis and the formation of intrahepatic stones.3–7 In some patients, afferent loop syndrome can rapidly develop, and rarely causing bowel perforation or peritonitis.
In the present case, we have a patient who had five episodes of acute cholangitis, whose aetiology was due to two entities: gallbladder and extrahepatic biliary lithiasis and afferent loop syndrome, caused by multiple adhesions involving the jejunojejunostomy in the Roux-en-Y anastomosis.
The diagnosis of afferent loop syndrome is challenging because the symptoms are non-specific, and can be attributed to other conditions6–8 ; as we can see in this case, the patient continued to have repeating acute cholangitis, even after the bilioenteric diversion for the treatment of symptomatic choledocolithiasis.
Abdominal CT is essential to determine the cause of afferent loop syndrome. Hepatobiliary scintigraphy confirms not only the dilation of the intrahepatic and extrahepatic biliary ducts but also the biliary stasis due to jejunal motility failure or obstruction.6–8 HIDA scintigraphy is also useful in the evaluation of the therapeutic efficacy of surgical treatment.
Treatment of the afferent loop syndrome depends on the aetiology. In patients with benign aetiologies, as in this case, surgical management, including adhesiolysis, bypass or reconstruction of the anastomosis, can generally resolve the cause.4 6
Learning points.
Afferent loop syndrome can cause recurrent acute cholangitis due to biliary retention in the proximal loop.
The principal causes of afferent loop syndrome are adhesions, angulation of the loop, internal hernias, stenosis of the anastomosis or cancer recurrence.
Abdominal CT and hepatobiliary iminodiacetic acid scintigraphy are useful for the diagnosis of this condition.
Surgeons need to fashion an afferent or biliopancreatic loop with an appropriate length to prevent this complication.
Footnotes
Contributors: FA and CC collected the data and wrote the manuscript. JGT and HC supervised the study and reviewed the manuscript. All authors approved the final version.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Sanada Y, Yamada N, Taguchi M, et al. Recurrent cholangitis by biliary stasis due to non-obstructive afferent loop syndrome after pylorus-preserving pancreatoduodenectomy: report of a case. Int Surg 2014;99:426–31. 10.9738/INTSURG-D-13-00243.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Katagiri H, Tahara K, Yoshikawa K, et al. Afferent loop syndrome after Roux-en-Y total gastrectomy caused by volvulus of the Roux-Limb. Case Rep Surg 2016;2016:1–3. 10.1155/2016/4930354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lehnert T, Buhl K. Techniques of reconstruction after total gastrectomy for cancer. Br J Surg 2004;91:528–39. 10.1002/bjs.4512 [DOI] [PubMed] [Google Scholar]
- 4. Aoki M, Saka M, Morita S, et al. Afferent loop obstruction after distal gastrectomy with Roux-en-Y reconstruction. World J Surg 2010;34:2389–92. 10.1007/s00268-010-0602-5 [DOI] [PubMed] [Google Scholar]
- 5. Fleser PS, Villalba M. Afferent limb volvulus and perforation of the bypassed stomach as a complication of Roux-en-Y gastric bypass. Obes Surg 2003;13:453–6. 10.1381/096089203765887831 [DOI] [PubMed] [Google Scholar]
- 6. House MG, Cameron JL, Schulick RD, et al. Incidence and outcome of biliary strictures after pancreaticoduodenectomy. Ann Surg 2006;243:571–8. 10.1097/01.sla.0000216285.07069.fc [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tien Y-W, Lee P-H, Chang K-J. Enterolith: an unusual cause of afferent loop obstruction. Am J Gastroenterol 1999;94:1391–2. 10.1111/j.1572-0241.1999.01092.x [DOI] [PubMed] [Google Scholar]
- 8. Spiliotis J, Karnabatidis D, Vaxevanidou A, et al. Acute cholangitis due to afferent loop syndrome after a Whipple procedure: a case report. Cases J 2009;2:6339 10.4076/1757-1626-2-6339 [DOI] [PMC free article] [PubMed] [Google Scholar]