Abstract
Immune-mediated reactions to dairy products may vary depending on the mammalian source. We present a case of anaphylaxis to goat/sheep's milk with tolerance to cow’s milk. A 4-year-old boy of Eastern European descent presented with gastrointestinal and respiratory symptoms within minutes after eating a goat/sheep’s milk-derived food product. The tryptase level measured 1 hour post initial symptoms and 1 month after the allergic reaction were 14.6 µg/L and 5.1 µg/L, respectively (norm: 0.0–13.5 µg/L), confirming the diagnosis of anaphylaxis. A skin prick test performed 1 month after the reaction was highly positive for goat/sheep’s milk, but negative for cow’s milk. Skin prick tests may establish a life-threatening goat/sheep’s milk allergy. Goat/sheep’s milk allergy should always be considered in cow’s milk-tolerant patients who present with an allergic reaction to dairy products, or when undergoing/have completed of oral immunotherapy for cow’s milk allergy.
Keywords: immunology; allergy, asthma
Background
Goat’s and sheep’s milk allergies are rare in patients who display tolerance to cow’s milk. Due to shared kappa-casein protein epitopes, 90% of cow’s milk protein allergic patients cross react to both goat’s and sheep’s milk protein.1 Despite this high cross-reactivity between the three dairy products, immunological response may vary depending on the mammalian source.
Caseins are suspected to be the major allergen causing these rare reactions rather than whey proteins.2 Patients with IgE antibodies that are unreactive to bovine β-casein are reported to be reactive to caprine (goat) β-casein (βcap), despite a sequence identity of 91% between the two proteins.3 Although the two casein types contain similar binding epitopes, selective IgE response to βcap can be due to non cross-reactive epitopes.3 Further, the generation of five amino acid substitutions on βcap has been described to decrease IgE reactivity in goat’s milk-allergic/cow’s milk-tolerant patients.3
While cow’s milk allergy can be IgE-mediated or non-IgE-mediated, reported cases of goat’s and sheep’s milk allergy with tolerance to cow’s milk have so far been described only as IgE-mediated allergic reactions.2 4–8 IgE-mediated reactions occur within 2 hours after ingestion of a particular allergen.9 Non-IgE-mediated reactions still involve the immune system, but are delayed up to 48 hours.9
We present a case of anaphylaxis to sheep/goat cheese in a 4-year-old boy who is tolerant to cow’s milk products, demonstrating a mammalian-specific dairy allergy.
Case presentation
A 4-year-old boy of Eastern European descent who is tolerant to cow’s milk presented with an allergic reaction after eating puff pastries made with feta cheese (consisting of a mixture of goat’s and sheep’s milk). He had known intermittent asthma and known eczema, but no previous history of food allergies. The patient had previously tolerated puff pastries made with cow’s milk on multiple occasions. This was his first exposure to the dessert made out of goat’s and sheep’s cheese.
Within minutes after eating the pastry, he experienced drowsiness and angioedema, as well as gastrointestinal symptoms (abdominal cramps, vomited multiple times) and respiratory symptoms (coughing, wheezing and congestion). Urticaria was not reported; however the patient experienced flushing of the neck.
The patient was brought to the emergency room within the first hour after symptoms developed, and treated there with intramuscular epinephrine (0.15 mg), diphenhydramine (15 mg orally) and dexamethasone (10 mg orally). However, 20 min later, given continuous wheezing, a second dose of intramuscular epinephrine was given (0.15 mg), along with salbutamol (0.5 mL) and ipratropium (1 mL). The patient was administered fluids intravenously during this time due to decreasing O2 saturation (87%) and increased work of breathing, which was followed by another dose of diphenhydramine (20 mg intravenous) and solumedrol (15 mg intravenous). The patient was admitted to the hospital ward and was discharged home 22 hours after arriving to the emergency room. He was prescribed an epinephrine autoinjector (0.15 mg x 2 injectors).
The tryptase level was measured 2 hours post initial symptoms and was 14.6 µg/L (norm: 0.0–13.5 µg/L).
Investigations
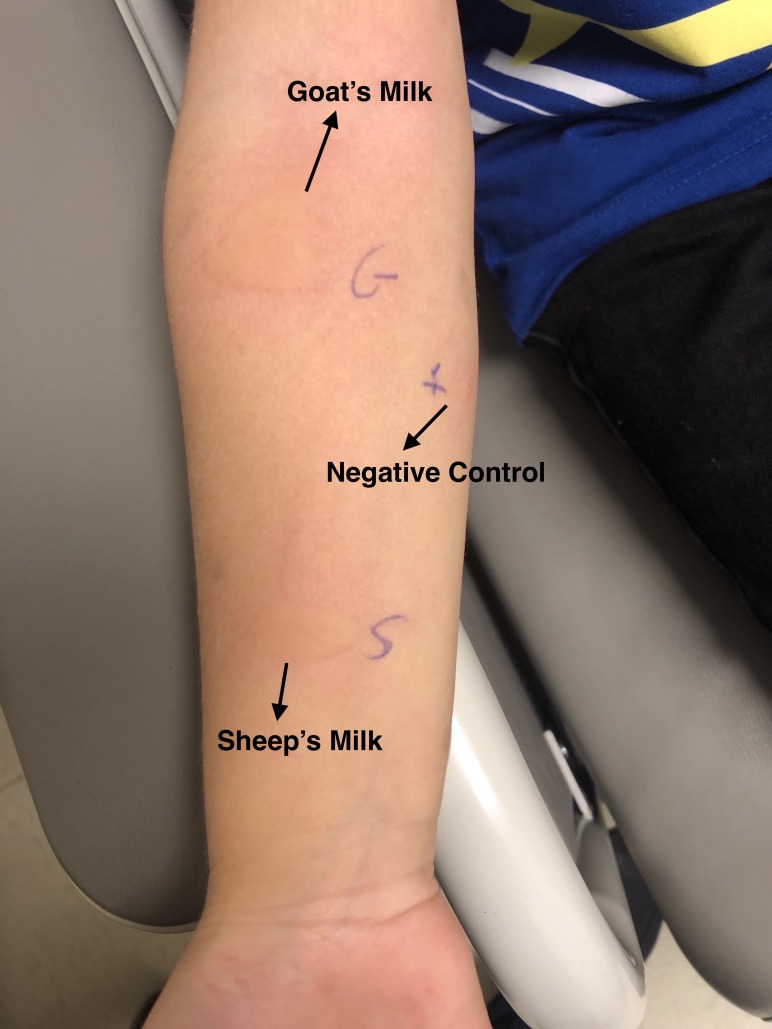
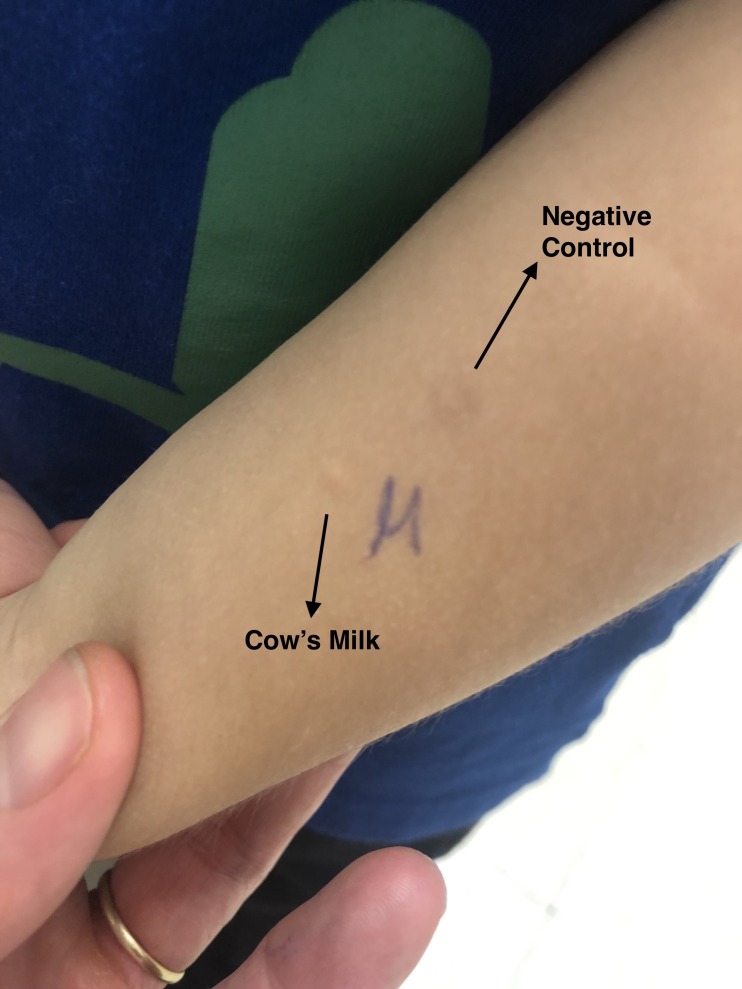
The patient was assessed in the allergy clinic at the Montreal Children’s Hospital 1 month after the reaction. Skin prick tests were performed to goat’s, sheep’s and cow’s milk. The skin prick test was highly positive for goat’s and sheep’s milk (17 mm and 16 mm weal diameter compared with the negative control done with saline solution 0.9%, respectively), and negative for cow’s milk (0 mm weal diameter compared with the negative control) (figures 1 and 2).
Figure 1.
Highly positive skin prick test to goat’s and sheep’s milk (17 mm and 16 mm weal diameter compared with the negative control, respectively).
Figure 2.
Negative skin prick test to cow’s milk (0 mm weal diameter compared with the negative control).
A repeated tryptase a month later was within normal limits (5.1 µg/L, norm: 0.0–13.5 µg/L), a difference of 9.5 µg/L compared with the level measured during reaction.
Differential diagnosis
Common clinical conditions which may present themselves in a similar fashion to anaphylaxis include vasovagal reactions (associated with cool and pale skin along with a low heart rate) and flushing syndromes (may either be wet such as sweating or dry such as with neuroendocrine tumours).10 Other rare conditions which may be present with clinical features suggesting anaphylaxes are respiratory or cardiovascular diseases, neuroendocrine tumours, poisoning, mast cell clonal disorders and psychogenic conditions.10
The patient presented with an acute episode consistent with an IgE-mediated reaction within minutes after food ingestion, resolved with epinephrine and antihistamine administration and did not have previous or subsequent recurrent episodes of flushing or other findings consistent with an underlying neuroendocrine tumour (eg, heart murmur or hypertension). The difference in tryptase levels was consistent with an anaphylaxis induced by goat/ship milk. Elevated tryptase levels (defined as a reaction level of at least 2 ng/mL+1.2 × (postreaction tryptase level)) are used as a marker for anaphylaxis.11
The three main triggers of anaphylaxis are food, insect stings and drugs.10 Foods are reported to be the primary allergen of these three (33.3%–56% of all cases of anaphylaxis), mainly peanut and tree nut.10 The patient was not exposed to any insects at the time of the reaction, nor was he taking any medication; therefore drugs or insect stings are an improbable allergen.
Non-immunologic cofactors of anaphylaxis include exercise, cold exposure, radiocontrast materials and opioids.10 However, in our case, the reaction occurred in the absence of the above-mentioned triggers. Finally, the highly positive skin prick test to goat’s and sheep’s milk and a negative skin prick test to cow’s milk establish that goat’s and sheep’s milk-induced anaphylaxis is the most likely diagnosis.
Treatment
Recommendations include strict avoidance of goat’s and sheep’s milk with continuation of ingestion of cow’s milk containing products. Adherence to such recommendations should not be challenging, as cow’s milk and its derivatives are the main source of dairy in a typical Western diet. The patient’s parents were educated on how and when to administer an epinephrine autoinjector, and were advised to carry the autoinjector at all times.
Outcome and follow-up
No challenges were performed, as the previous severe allergic reaction and positive skin prick tests were considered sufficient to confirm the presence of goat’s and sheep’s milk allergy with cow’s milk tolerance. In the following 6 months, the patient has not had any other accidental exposure to goat’s or sheep’s milk and continued to tolerate cow’s milk.
Discussion
Our case exemplifies the need for careful history taking and assessment for rare food allergens. This case also demonstrates the importance of considering other types of dairy allergies, despite a patient’s tolerance to cow’s milk. Milk allergy should be treated on a mammalian specific basis.
The history of reaction is consistent with previous cases on the clinical presentation of goat/sheep’s milk allergy with cow’s milk-tolerance. However, previously reported cases noted the presence of urticaria, which our patient did not have.4 5 7 12 Our case is also unique as it presented in a young child. In previous cases, the age ranged from 2 to 27 years old,4–8 12 and it was stated that goat’s and sheep’s milk allergy differs from cow’s milk allergy in that it generally affects older children and appears later in life.2
The majority of reported cases are from Europe (Spain,4 6 Italy,7 France2 and Portugal5). This can possibly be due to a Mediterranean diet, in which goats and sheep are the main source of animal fat, and are commonly used as sources of cheese and yoghurt.13 To our knowledge, this is the first case in Canada, and the third case in North America8 14 to report a patient who is unreactive to cow’s milk, but reactive towards goat’s and sheep’s milk.
More recently, oral immunotherapy has been reported to be effective and is increasingly used to desensitise children with severe food allergies including milk.15 16 Patients who successfully complete oral immunotherapy for cow’s milk allergy should be informed that their increased tolerance may be restricted to cow’s milk protein, and not to other mammals. A study consisting of 58 cow’s milk allergic patients who successfully underwent cow’s milk oral immunotherapy reported that 15 (26%) of the patients were allergic to goat’s or sheep’s milk, or both.17 Increased tolerance to goat’s and sheep’s milk after completion of cow’s milk oral immunotherapy can be easily assessed with skin prick tests in order to avoid life-threatening allergic reactions.
Our case supports the use of skin tests to confirm the diagnosis of goat/sheep’s milk allergy as well as the use of tryptase measurements to confirm the diagnosis of anaphylaxis. Specific skin prick tests may help establish a goat/sheep’s milk allergy, while allowing continuous consumption of cow’s milk.
This paper has some limitations. Specific IgE levels at the time of the reaction, which was not measured in our case, could have been used alongside skin prick tests to determine the allergen causing this reaction. However, the history is clearly compatible with the diagnosis of anaphylaxis to goat’s and sheep’s milk. In addition, the few reported cases describing this clinical presentation limit the amount of comparison that can be done with other cases, which can help further our understanding of the topic.
In conclusion, this case exemplifies a rare sensitisation to a particular mammalian milk, hypersensitivity to goat/sheep's milk with tolerance to cow’s milk. Caregivers and patients with cow’s milk tolerance should be aware of the risk of allergy to milk caseins found in different mammals. Goat/sheep’s milk allergy should always be considered in the context of a dairy allergy, or when undergoing/have completed of oral immunotherapy.
Learning points.
Caregivers and patients should be aware of the risk of goat/sheep’s milk allergy in cow’s milk tolerant individuals.
Skin prick tests may establish a goat/sheep’s milk allergy, allow continuous consumption of cow’s milk and ultimately avoid life-threatening allergic reactions such as anaphylaxis.
Oral immunotherapy is a mammalian-specific procedure. Therefore, patients who complete oral immunotherapy for cow’s milk should be informed that their increased tolerance may be restricted to cow’s milk protein, and not to other mammals. Protocols for oral immunotherapy for goat/sheep’s milk proteins are required.
Footnotes
Contributors: PM: conception and design, analysis and interpretation of data, drafting the article, final approval of the version published. SG, JU and AEM: conception and design, analysis and interpretation of data, revising the article critically for important intellectual content, final approval of the version published. MB-S: planning, conception and design, acquisition of data, analysis and interpretation of data, revising the article critically for important intellectual content, final approval of the version published.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Parental/guardian consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Levy M, Nachshon L, Goldberg M, et al. Cross-Desensitization to goat and sheep milk protein in cow's milk protein desensitized patients. Journal of Allergy and Clinical Immunology 2014;133:AB107 10.1016/j.jaci.2013.12.395 [DOI] [PubMed] [Google Scholar]
- 2. Ah-Leung S, Bernard H, Bidat E, et al. Allergy to goat and sheep milk without allergy to cow's milk. Allergy 2006;61:1358–65. 10.1111/j.1398-9995.2006.01193.x [DOI] [PubMed] [Google Scholar]
- 3. Hazebrouck S, Ah-Leung S, Bidat E, et al. Goat's milk allergy without cow's milk allergy: suppression of non-cross-reactive epitopes on caprine β-casein. Clin Exp Allergy 2014;44:602–10. 10.1111/cea.12261 [DOI] [PubMed] [Google Scholar]
- 4. Muñoz Martín T, de la Hoz Caballer B, Marañón Lizana F, et al. Selective allergy to sheep's and goat's milk proteins. Allergol Immunopathol 2004;32:39–42. 10.1016/s0301-0546(04)79222-8 [DOI] [PubMed] [Google Scholar]
- 5. Tavares B, Pereira C, Rodrigues F, et al. Goat's milk allergy. Allergol Immunopathol 2007;35:113–6. 10.1157/13106780 [DOI] [PubMed] [Google Scholar]
- 6. Cabanillas Platero M, Piñero Saavedra M, Goat PSM. Goat and sheep's milk allergy with cow's milk tolerance. A case report. J Allergy Clin Immunol 2011;127 10.1016/j.jaci.2010.12.747 [DOI] [Google Scholar]
- 7. Tripodi S, Comberiati P, Di Rienzo Businco A, et al. Severe anaphylaxis to sheep's milk cheese in a child desensitized to cow's milk through specific oral tolerance induction. Eur Ann Allergy Clin Immunol 2013;45:56–60. [PubMed] [Google Scholar]
- 8. Pazheri F, Melton AL, Poptic E, et al. Allergy to sheep milk with or without allergy to cow milk. J Allergy Clin Immunol 2014;133:AB199 10.1016/j.jaci.2013.12.714 [DOI] [Google Scholar]
- 9. Walsh J, Meyer R, Shah N, et al. Differentiating milk allergy (IgE and non-IgE mediated) from lactose intolerance: understanding the underlying mechanisms and presentations. Br J Gen Pract 2016;66:e609–11. 10.3399/bjgp16X686521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ben-Shoshan M, Clarke AE. Anaphylaxis: past, present and future. Allergy 2011;66:1–14. 10.1111/j.1398-9995.2010.02422.x [DOI] [PubMed] [Google Scholar]
- 11. De Schryver S, Halbrich M, Clarke A, et al. Tryptase levels in children presenting with anaphylaxis: temporal trends and associated factors. J Allergy Clin Immunol 2016;137:1138–42. 10.1016/j.jaci.2015.09.001 [DOI] [PubMed] [Google Scholar]
- 12. Wüthrich B, Johansson SG. Allergy to cheese produced from sheep's and goat's milk but not to cheese produced from cow's milk. J Allergy Clin Immunol 1995;96:270–3. 10.1016/S0091-6749(95)70021-8 [DOI] [PubMed] [Google Scholar]
- 13. Romagnolo DF, Selmin OI. Mediterranean diet and prevention of chronic diseases. Nutr Today 2017;52:208–22. 10.1097/NT.0000000000000228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Maskatia ZK, Davis CM. Perinatal environmental influences on goat's and sheep's milk allergy without cow's milk allergy. Ann Allergy Asthma Immunol 2013;111:574–5. 10.1016/j.anai.2013.09.022 [DOI] [PubMed] [Google Scholar]
- 15. Yeung JP, Kloda LA, McDevitt J, et al. Oral immunotherapy for milk allergy. Cochrane Database Syst Rev 2012;11:CD009542 10.1002/14651858.CD009542.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. De Schryver S, Mazer B, Clarke AE, et al. Adverse events in oral immunotherapy for the desensitization of cow's milk allergy in children: a randomized controlled trial. J Allergy Clin Immunol 2019;7:1912–9. 10.1016/j.jaip.2019.02.007 [DOI] [PubMed] [Google Scholar]
- 17. Rodríguez del Río P, Sánchez-García S, Escudero C, et al. Allergy to goat’s and sheep’s milk in a population of cow’s milk-allergic children treated with oral immunotherapy*. Pediatr Allergy Immunol 2012;23:128–32. 10.1111/j.1399-3038.2012.01284.x [DOI] [PubMed] [Google Scholar]