Abstract
Objective
This study evaluated the characteristics of new users of sodium glucose co-transporter 2 inhibitors (SGLT2i) in clinical practice to assess the applicability of the findings from clinical trials (Empagliflozin, Cardiovascular Outcomes and Mortality in Type 2 Diabetes (EMPA-REG OUTCOME) trial, Dapagliflozin Effect on Cardiovascular Events (DECLARE)-TIMI 58 trial, Canagliflozin Cardiovascular Assessment Study (CANVAS) program and the Evaluation of Ertugliflozin Efficacy and Safety Cardiovascular Outcomes (VERTIS-CV) trial) and multinational observational studies (CVD-REAL Nordic study and CVD-REAL 2 study).
Research design and methods
We conducted a retrospective cohort study using the largest electronic medical records database from seven hospitals in Taiwan. We included adult patients with type 2 diabetes initiating canagliflozin, dapagliflozin and empagliflozin between 1 January 2018 and 31 August 2019. We compared the patient characteristics with SGLT2i to examine the data representativeness of clinical trials and to evaluate channeling uses between canagliflozin, dapagliflozin and empagliflozin.
Results
We identified a cohort of 11 650 patients newly initiating SGLT2i, 49.9% of whom received empagliflozin. However, only 18.7%, 19.2%, 50.4% and 57.3% of real-world SGLT2i new users were included in the EMPA-REG OUTCOME trial, VERTIS-CV trial, DECLARE-TIMI 58 trial and CANVAS program, respectively. Reasons for exclusion were largely reduced cardiovascular disease risks in real-world patients, namely 72.8%, 73.6% and 34.2% for EMPA-REG OUTCOME trial, VERTIS-CV trial and DECLARE-TIMI 58 trial and CANVAS program, respectively. However, hemoglobin A1c out of range accounted for the most frequent reason (25.0%) for exclusion of real-world patients from the CANVAS program. We found channeling uses in different SGLT2i, for example, more patients receiving empagliflozin (15.3%) and canagliflozin (19.6%) had poorer renal functions (eg, estimated glomerular filtration rate <60 mL/min/1.73 m2), compared with dapagliflozin (9.3%).
Conclusions
The findings provide clear evidence that results from current studies may be less applicable to real-world patients. Further studies are required to support the concept of real-world cardiovascular event protection through SGLT2i.
Keywords: type 2 diabetes, sodium glucose cotransporter, health service research
Significance of this study.
What is already known about this subject?
Several studies found the risk of cardiovascular events reduced in patients with type 2 diabetes receiving sodium glucose co-transporter 2 inhibitors (SGLT2i).
The recent DISCOVER study found that cardiovascular outcome trials of SGLT2i were not equally generalizable to real-world patients; however, it did not focus on patients newly initiating SGLT2i.
What are the new findings?
Only 18.7%, 19.2%, 50.4% and 57.3% of real-world SGLT2i new users were included in the Empagliflozin, Cardiovascular Outcomes and Mortality in Type 2 Diabetes (EMPA-REG OUTCOME) trial, the Evaluation of Ertugliflozin Efficacy and Safety Cardiovascular Outcomes (VERTIS-CV) trial, Dapagliflozin Effect on Cardiovascular Events (DECLARE)-TIMI 58 trial and Canagliflozin Cardiovascular Assessment Study (CANVAS) program, respectively.
Lower cardiovascular disease risk in the real-world patients initiating SGLT2i was the major exclusion reason in the EMPA-REG OUTCOME trial, VERTIS-CV trial and DECLARE-TIMI 58 trial.
Potential confounding by indication, often also referred to as channeling use, of SGLT2i was identified; for example, a higher proportion of empagliflozin (15.3%) and canagliflozin (19.6%) new users had poorer renal functions (eg, estimated glomerular filtration rate <60 mL/min/1.73 m2), compared with dapagliflozin (9.3%).
Significance of this study.
How might these results change the focus of research or clinical practice?
Draw attention to the built-in heterogeneity within SGLT2i class for better understanding the cardiovascular benefits of individual SGLT2i.
Future studies should adjust for different characteristics of both patients and SGLT2i to confirm the real-world class effects in regard to cardiovascular event protection, especially in patients with type 2 diabetes with lower cardiovascular diseases risks.
Introduction
Sodium glucose co-transporter 2 inhibitor (SGLT2i) is a new drug class for type 2 diabetes management based on reducing renal glucose re-absorption and increasing elimination of excess glucose. It decreases blood glucose levels and provides additional benefits through the control of body weight and blood pressure.1 Meta-analyses from three large randomized clinical trials (RCT), Canagliflozin Cardiovascular Assessment Study (CANVAS) program, Dapagliflozin Effect on Cardiovascular Events (DECLARE)-TIMI 58 trial, Empagliflozin, Cardiovascular Outcomes and Mortality in Type 2 Diabetes (EMPA-REG OUTCOME) trial, found that SGLT2i reduced major adverse cardiovascular event risks in patients with established atherosclerotic cardiovascular disease.2–5 These trials established the fundamental evidence regarding the uses of SGLT2i for cardiovascular disease (CVD) prevention, and the findings from another trial, the evaluation of ertugliflozin efficacy and safety cardiovascular outcomes (VERTIS-CV) will be available after 2020.6
However, the situation and the effect of drugs differ between clinical trials and real-world practice.7 8 For example, the CVD-REAL Nordic and CVD-REAL 2 studies with multinational data found that the characteristics of patients receiving SGLT2i in a real-world situation differed from those in clinical trials; in particular, only 13%–25% of patients in the studies had a CVD history, while the CANVAS program and DECLARE-TIMI 58 trial included 65.6% and 40.6% of patients with CVD history, respectively.9–11 This prompts the question of applicability of evidence from clinical trials to real-world patients since the baseline risks of patients are different and the effects of drugs are unpredictable.
Observational studies using healthcare databases can provide population-based evidence from real-world situations. However, since patient allocation cannot be randomized while conducting studies, investigators should pay attention to validity issues resulting from selection biases and confounders. Potential confounding by indication, often also referred to as channeling use, of SGLT2i was acknowledged. For example, while the new class of diabetic medication (eg, SGLT2i) is broadly available, the claimed superior benefits (eg, lower CVD morbidity and mortality) of new drugs may channel to patients with higher risks (eg, patients with established CVD), which could result in an incorrect estimation of the true effect of the drugs, an effect we call confounding by indication or channeling bias. Furthermore, since key information regarding the severity of diabetes or renal functions is unavailable in the CVD-REAL Nordic and CVD-REAL 2 studies, adjustments for baseline risks when evaluating outcomes (eg, CVD) are not possible.12
Understanding the characteristics of real-world patients receiving SGLT2i is the first but crucial step in the adoption of current evidence from clinical trials and observational studies into routine practice. This study aimed to compare the characteristics of patients with type 2 diabetes initiating SGLT2i in the RCT cohort and those in the real-world population to evaluate the applicability of results from RCT. Furthermore, we used multi-institutional electronic health records that included examination data to address the issues of unmeasured confounders while conducting real-world studies related to SGLT2i. To assess the extent of channeling uses in SGLT2i, we compared patient characteristics between users of canagliflozin, dapagliflozin and empagliflozin.
Research design and methods
Data source
We conducted a retrospective cohort study using the Chang Gung Research Database (CGRD). Details of the CGRD have been described elsewhere.13 Briefly, CGRD is a standardized electronic medical records (EMR) database which includes seven hospitals with different levels (two medical centers, two regional hospitals and three district hospitals) located from northern to southern Taiwan and covering approximately 8.9% of outpatients with endocrine and metabolic diseases.13 The CGRD is updated every month to facilitate timely assessments, and the diagnosis codes in CGRD have been validated for diabetes, heart failure, ischemic stroke and varicose veins of the lower extremities.14–16
Study cohort assembly
Consistent with the American Diabetes Association (ADA) guidelines, Taiwan’s National Health Insurance reimbursement guideline suggests the use of SGLT2i as intensification therapy after failure of treatment with metformin. Because Taiwan has maintained a universal mandatory insurance programme covering almost all healthcare facilities, and all treatments are largely based on the guidelines, there should be no substantial difference in clinical practice between our study population and other Taiwanese patients. Dapagliflozin/empagliflozin and canagliflozin have been reimbursed under the Taiwan National Health Insurance programme since 1 May 2016 and 1 March 2018, respectively, and the medication reimbursement criteria are identical for all Taiwanese hospitals. We identified a cohort of adult outpatients newly initiating SGLT2i treatment for the management of type 2 diabetes between 1 January 2018 and 31 August 2019. We considered the first date of prescription for SGLT2i as the index date. We excluded patients without CGRD records at least 1 year prior to the index date to ensure all selected patients had sufficient data for baseline characteristics.
Eligibility of cardiovascular outcome trials
We used age, sex, International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes for the identification of comorbidity and laboratory data as the principal determinants in selecting patients from the CGRD who would meet the clinical trial inclusion/exclusion criteria. The major inclusion/exclusion criteria in the CANVAS program, DECLARE-TIMI 58 trial, EMPA-REG OUTCOME trial and VERTIS-CV trial were derived primarily from the trial design with clarification sought from supplementary appendices and primary clinical trial result publications where required.2–4 6 17 Of note, the EMPA-REG OUTCOME trial and VERTIS-CV trial required adult patients with type 2 diabetes to have existing CVD history, such as unstable angina, coronary artery disease (CAD), stroke and peripheral arterial disease (PAD). The DECLARE-TIMI 58 trial and CANVAS program recruited patients with type 2 diabetes at broad CVD risk according to two categories: 1) existing CVD history and 2) CVD risk factors, such as dyslipidemia, hypertension and duration of diabetes over 10 years. The major exclusion criteria based on the laboratory data in these cardiovascular outcome trials included hemoglobin A1c (HbA1c) (eg, CANVAS program: 7%–10.5%; DECLARE-TIMI 58 trial: 6.5%–12%; EMPA-REG OUTCOME trial/VERTIS-CV trial: 7%–10%) and estimated glomerular filtration rate (eGFR) values (eg, CANVAS program/EMPA-REG OUTCOME trial/VERTIS-CV trial: <30 mL/min/1.73 m2; DECLARE-TIMI 58 trial: <60 mL/min/1.73 m2) out of range.
Covariates
We described patients’ characteristics at baseline such as age and sex, and other covariates including comorbid chronic conditions related to diabetic concerns,18 such as macrovascular (eg, CAD, stroke and PAD) and microvascular diseases (eg, retinopathy, nephropathy and neuropathy), cancer and other characteristics and we have listed them in table 1. We also evaluated the characteristics of healthcare facilities prescribing SGLT2i (eg, medical specialties) and baseline antidiabetes drugs (ADD) before initiation of SGLT2i, including insulins, sulfonylureas, metformin, glinides, pioglitazone, dipeptidyl peptidase-4 inhibitors (DPP4i) and glucagon-like peptide-1 (GLP-1) receptor agonists. We present the details of baseline comorbidities and ADD in online supplementary appendix table 1 and 2, respectively.
Table 1.
Proportion of real-world SGLT2i new users excluded from cardiovascular outcome trials
| Real-world data in Taiwan | ||||
| All | Canagliflozin | Dapagliflozin | Empagliflozin | |
| N (%) | N | N (%) | N (%) | |
| All patients | 11 650 (100.0) | 1091 (9.4) | 4748 (40.8) | 5811 (49.9) |
| Comparison of CANVAS program | ||||
| Excluded for any of the following: | 4977 (42.7) | 443 (40.6) | ---- | ---- |
|
2811 (24.1) | 240 (22.0) | ---- | ---- |
| HbA1c >10.5% or HbA1c <7% | 2917 (25.0) | 263 (24.1) | ---- | ---- |
| eGFR <30 mL/min/1.73 m2 | 166 (1.4) | 27 (2.5) | ---- | ---- |
| Comparison of DECLARE-TIMI 58 trial | ||||
| Excluded for any of the following: | 5773 (49.6) | ---- | 2270 (47.8) | ---- |
|
3979 (34.2) | ---- | 1740 (36.6) | ---- |
| HbA1c >12% or HbA1c <6.5% | 704 (6.0) | ---- | 257 (5.4) | ---- |
| eGFR <60 mL/min/1.73 m2 | 1544 (13.3) | ---- | 441 (9.3) | ---- |
| Comparison of EMPA-REG OUTCOME trial | ||||
| Excluded for any of the following: | 9466 (81.3) | ---- | ---- | 4611 (79.3) |
| No CVD history (unstable angina, CAD, stroke, lower extremity amputation, MI and PAD) | 8480 (72.8) | ---- | ---- | 4006 (68.9) |
| HbA1c >10% or HbA1c <7% | 3402 (29.2) | ---- | ---- | 1837 (31.6) |
| eGFR <30 mL/min/1.73 m2 | 166 (1.4) | ---- | ---- | 88 (1.5) |
| Comparison of VERTIS-CV trial | ||||
| Excluded for any of the following: | 9411 (80.8) | ---- | ---- | ---- |
| Aged ≥40 years without CVD history (unstable angina, CAD, ischemic stroke, MI and PAD) | 8577 (73.6) | ---- | ---- | ---- |
| HbA1c >10.5% or HbA1c <7% | 2917 (25.0) | ---- | ---- | ---- |
| eGFR <30 mL/min/1.73 m2 | 166 (1.4) | ---- | ---- | ---- |
| BMI<18 kg/m2 | 125 (1.1) | ---- | ---- | ---- |
BMI, body mass index; CAD, cardiovascular artery disease; CVD, cardiovascular disease; eGFR, estimated glomerular filtration rate; HbA1c, hemoglobin A1c; MI, myocardial infarction; PAD, peripheral artery disease.
bmjdrc-2019-000742supp001.pdf (80KB, pdf)
Additionally, we have included baseline information from physical and laboratory examination dating to 1 year prior to the index date in the analyses, including HbA1c levels, renal function (eg, eGFR), body mass index (BMI), systolic blood pressure (SBP) and diastolic blood pressure (DBP). In general, clinicians would confirm patients’ condition before initiation of SGLT2i; hence the rates of missing values were low in our analysis (eg, only 3.6% for baseline HbA1c values). Nevertheless, to manage the missing values, we implemented multiple imputations using the Markov chain Monte Carlo method and combined 10 simulations.
Validation analyses
As with all studies using hospital-based EMR databases, the issues of incomplete medical or medication history are of concern. We reviewed all patients’ medical charts from one of the hospitals (n=1832) to confirm whether SGLT2i were prescribed for type 2 diabetes cases in this study and the accuracy of baseline ADD through CGRD. Our validation findings indicated that all the patients had been diagnosed with type 2 diabetes and 5.3% of patients had received other ADD from other healthcare facilities that could not be captured by CGRD.
Statistical analysis
We performed descriptive analysis for all characteristics using counts and proportions for categorical variables and means and standard deviation (SD) for continuous variables. We presented the proportion of patients initiating SGLT2i from the CGRD who would be eligible for the CANVAS program, DECLARE-TIMI 58 trial, EMPA-REG OUTCOME and VERTIS-CV trial. We also classified patients based on SGLT2i (canagliflozin, dapagliflozin and empagliflozin) to compare their characteristics with corresponding clinical trials, and the baseline differences of covariates between real-world practice and clinical trials were assessed using the absolute standardized mean difference method.19 All statistical analyses were performed using SAS Enterprise Guide V.5.1 (SAS Institute, Cary, North Carolina, USA).
Results
Patients eligible for four large cardiovascular outcome trials
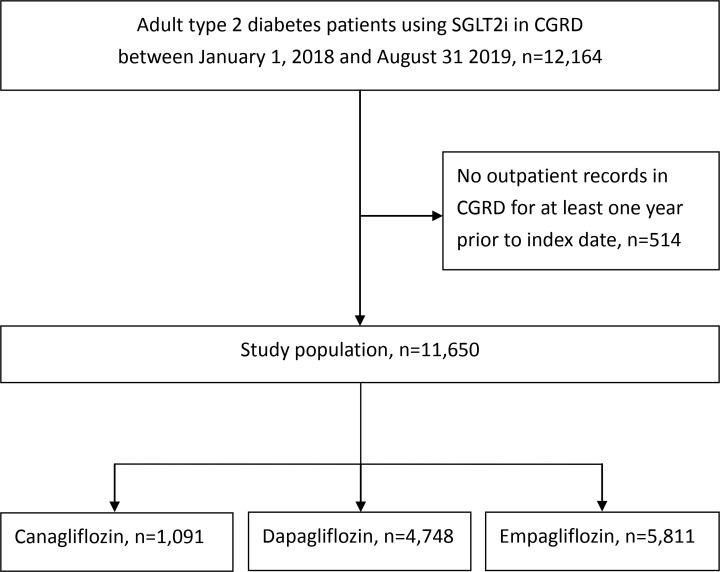
We identified a cohort of 12 164 adult patients with type 2 diabetes who initiated SGLT2i between 1 January 2018 and 31 August 2019. We excluded 514 patients who lacked baseline medical records in CGRD, and a total of 11 650 patients entered the analyses. We found 5811 (49.9%), 4748 (40.7%) and 1091 (9.4%) patients received empagliflozin, dapagliflozin and canagliflozin, respectively (figure 1). Based on the inclusion/exclusion criteria of EMPA-REG OUTCOME trial, VERTIS-CV trial, DECLARE-TIMI 58 trial and CANVAS program, only 18.7%, 19.2%, 50.4% and 57.3% of real-world SGLT2i new users in Taiwan were included in these trials, respectively (table 1). Within the inclusion/exclusion criteria, the greatest difference between clinical trials was seen with regard to CVD definitions, whereby 72.8%, 73.6% and 34.2% of the real-world patients initiating SGLT2i did not meet the criteria in the EMPA-REG OUTCOME trial, VERTIS-CV trial and DECLARE-TIMI 58 trial, respectively. However, we found that HbA1c out of range (7%–10.5%) meant excluding 25.0% of real-world SGLT2i new users from the CANVAS program (table 1).
Figure 1.
Study flow chart. CGRD, Chang Gung Research Database; SGLT2i, sodium glucose co-transporter 2 inhibitors.
Comparing patient characteristics between real-world settings and clinical trials
Compared with the CANVAS program, DECLARE-TIMI 58 trial and EMPA-REG OUTCOME trial (table 2), the real-world SGLT2i new users had poorer HbA1c controls (canagliflozin: 8.2%±0.9% vs 8.4%±1.6%; dapagliflozin: 8.3%±1.2% vs 8.5%±1.6%; empagliflozin: 8.1%±0.9% vs 8.5%±1.7%).
Table 2.
Patient characteristics between real-world practice in Taiwan and cardiovascular outcome trials
| CANVAS programme | Canagliflozin new uses | ASMD | DECLARE-TIMI 58 trial | Dapagliflozin new uses | ASMD | EMPA-REG OUTCOME trial | Empagliflozin new uses | ASMD | |
| Patient number | 5795 | 1091 | 8582 | 4748 | 4687 | 5811 | |||
| Patient characteristics | |||||||||
| Age, mean (SD) | 63.2 (8.3) | 60.9 (11.6) | 0.22 | 63.9 (6.8) | 59.5 (11.9) | 0.45 | 63.1 (8.6) | 61.0 (12.1) | 0.2 |
| Female, % | 35.1 | 39.3 | 0.08 | 36.9 | 38.1 | 0.02 | 28.8 | 38.1 | 0.19 |
| Race, % | |||||||||
| White | 77.8 | 0 | 2.64 | 79.7 | 0 | 2.8 | 72.6 | 0 | 2.3 |
| Asian | 13.4 | 100 | 3.59 | 13.4 | 100 | 3.59 | 21.5 | 100 | 2.7 |
| Others | 8.8 | 0 | 0.43 | 6.8 | 0 | 0.38 | 6 | 0 | 0.35 |
| HbA1c, mean mg/dL (SD) | 8.2 (0.9) | 8.4 (1.6) | 0.15 | 8.3 (1.2) | 8.5 (1.6) | 0.14 | 8.1 (0.9) | 8.5 (1.7) | 0.29 |
| eGFR, mean ml/min/1.73 m2(SD) | 76.7 (20.3) | 85.3 (27.5) | 0.35 | 85.4 (15.8) | 91.9 (26.2) | 0.3 | 74.2 (21.6) | 88.4 (28.8) | 0.55 |
| ≥90 mL/min/1.73 m2, % | NA | 42.3 | NA | NA | 49.6 | NA | 22.4 | 44.4 | 0.47 |
| 60–90 mL/min/1.73 m2, % | NA | 38.2 | NA | NA | 41.1 | NA | 51.7 | 40.3 | 0.23 |
| 30–60 mL/min/1.73 m2, % | NA | 17.1 | NA | NA | 8.2 | NA | 25.9 | 15.3 | 0.26 |
| <30 mL/min/1.73 m2, % | NA | 2.5 | NA | NA | 1.1 | NA | |||
| SBP, mean mm Hg (SD) | 136.4 (15.8) | 140.2 (18.5) | 0.22 | 135.1 (15.3) | 140.3 (18.5) | 0.3 | 135.3 (16.9) | 138.8 (19.6) | 0.19 |
| DBP, mean mm Hg (SD) | 77.6 (9.6) | 79.1 (12.1) | 0.13 | NA | 79.5 (12.3) | NA | 76.6 (9.7) | 78.5 (12.3) | 0.17 |
| BMI, mean kg/m2(SD) | 31.9 (5.9) | 28.3 (4.4) | 0.69 | 32.1 (6.0) | 28.2 (4.0) | 0.76 | 30.6 (5.3) | 28.0 (4.0) | 0.55 |
| Comorbidity | |||||||||
| Microvascular diseases, % | NA | 29.6 | NA | NA | 24.4 | NA | NA | 23.1 | NA |
| Retinopathy | 20.8 | 6.9 | 0.39 | NA | 9.1 | NA | NA | 7.3 | NA |
| Nephropathy | 17.2 | 24.9 | 0.19 | NA | 20.3 | NA | NA | 19.1 | NA |
| Neuropathy | 30.8 | 6.5 | 0.65 | NA | 6.6 | NA | NA | 7.1 | NA |
| Macrovascular diseases, % | 64.8 | 23.5 | 0.91 | 40.5 | 23.4 | 0.37 | 99.9 | 31.1 | 2.09 |
| Coronary artery disease | 55.8 | 20 | 0.79 | 32.9 | 19.7 | 0.3 | 75.6 | 27 | 1.11 |
| Myocardial infraction | NA | 2.9 | NA | NA | 2.6 | NA | 46.5 | 6.8 | 1 |
| Unstable angina | NA | 0.9 | NA | NA | 0.9 | NA | NA | 1.1 | NA |
| Stroke | 19.2 | 3 | 0.53 | 7.6 | 3.8 | 0.16 | 23.1 | 4.2 | 0.57 |
| Peripheral arterial disease | 20.3 | 1.4 | 0.63 | 6.1 | 1 | 0.27 | 21 | 1.3 | 0.65 |
| Hypertension | 89.5 | 66.8 | 0.57 | NA | 64.9 | NA | NA | 65.1 | NA |
| Dyslipidemia | NA | 71.8 | NA | NA | 70.9 | NA | NA | 64.6 | NA |
| Heart failure | 13.9 | 6.2 | 0.25 | 9.9 | 5.4 | 0.16 | 10.6 | 9.9 | 0.02 |
| Lower extremity amputation | 2.3 | 0 | 0.21 | NA | 0 | NA | NA | 0.1 | NA |
| Atrial fibrillation | NA | 3.8 | NA | NA | 3.1 | NA | NA | 4 | NA |
| Liver disease | NA | 15.5 | NA | NA | 17.1 | NA | NA | 15.6 | NA |
| Cancer | 0 | 5.7 | 0.34 | 0 | 5.5 | 0.34 | 0 | 5.2 | 0.33 |
| Healthcare facility characteristics | |||||||||
| Medical specialties | |||||||||
| Endocrine | NA | 62.8 | NA | NA | 56.6 | NA | NA | 45.1 | NA |
| Cardiology | NA | 28.6 | NA | NA | 27.8 | NA | NA | 34.4 | NA |
| Nephrology | NA | 6 | NA | NA | 2.9 | NA | NA | 5.5 | NA |
| Other | NA | 2.7 | NA | NA | 12.8 | NA | NA | 15 | NA |
| Drug characteristics | |||||||||
| No. antidiabetes drug, mean (SD) | NA | 2.3 (1.1) | NA | NA | 2.1 (1.2) | NA | NA | 2.0 (1.2) | NA |
| Antidiabetes drug regimen, % | |||||||||
| Treatment native | NA | 5.5 | NA | NA | 11.3 | NA | NA | 13.9 | NA |
| Monotherapy | NA | 16.4 | NA | NA | 16.4 | NA | 29.4 | 19.9 | 0.22 |
| Dual therapy | NA | 31.4 | NA | NA | 30.2 | NA | 48.2 | 28.1 | 0.42 |
| At least triple therapy | NA | 46.7 | NA | NA | 42.1 | NA | NA | 38.1 | NA |
| Antidiabetes drug class, % | |||||||||
| Metformin | 77.2 | 83.5 | 0.15 | 81.8 | 80.5 | 0.03 | 73.8 | 74.2 | 0.01 |
| Sulfonylurea | 43 | 48.9 | 0.11 | 42.1 | 44.3 | 0.04 | 43 | 38.9 | 0.08 |
| DPP4i | 12.4 | 61 | 1.16 | 16.5 | 55.7 | 0.89 | 11.3 | 54.5 | 1.03 |
| Glinide | NA | 2.1 | NA | NA | 1.8 | NA | NA | 1.9 | NA |
| Acarbose | NA | 3.6 | NA | NA | 4.7 | NA | NA | 4.9 | NA |
| Thiazolidinedione | NA | 19.2 | NA | NA | 14.4 | NA | 4.2 | 11.3 | 0.26 |
| GLP-1 receptor agonists | 4 | 1.7 | 0.13 | 4.6 | 1 | 0.21 | 2.7 | 1.1 | 0.22 |
| Insulin | 50.2 | 12.3 | 0.89 | 41.6 | 11.8 | 0.71 | 48 | 14.4 | 1.12 |
ASMD, absolute standardized mean difference; BMI, body mass index; DBP, diastolic blood pressure; DPP4i, dipeptidyl peptidase 4 inhibitor; eGFR, estimated glomerular filtration rate; GLP, glucagon-like peptide; HbA1c, hemoglobin A1c; NA, not available; SBP, systolic blood pressure.
Comparing patient characteristics between canagliflozin, dapagliflozin and empagliflozin
Compared with the CVD-Real Nordic and CVD-Real 2 studies, we provide more detailed patient-level information from EMR databases in real-world settings (table 2), for example, we present the prescribing patterns from the perspective of laboratory findings (eg, HbA1c, eGFR, BMI, SBP and DBP) in patients newly initiating SGLT2i. We found the mean values of HbA1c (8.4%±1.6%, 8.5%±1.6% and 8.5%±1.7%), BMI (28.3±4.4, 28.2±4.0 and 28.0±4.0 kg/m2), SBP (140.2±18.5, 140.3±18.5 and 138.8±19.6 mm Hg) and DBP (79.1±12.1, 79.5±12.3 and 78.5±12.3 mm Hg) at baseline were similar between canagliflozin, dapagliflozin and empagliflozin new users, but patients receiving canagliflozin (19.6%) and empagliflozin (15.3%) had worse renal functions (eg, eGFR <60 mL/min/1.73 m2) than those receiving dapagliflozin (9.3%). Empagliflozin new users had a higher proportion of major CVD (31.1%), compared with canagliflozin (23.5%) and dapagliflozin (23.4%) users. Channeling patterns in the receiving of medical care and number of baseline ADD in patients with different SGLT2i were also identified (table 2), for example, canagliflozin was prescribed more by endocrinologists (62.8%), compared with 56.6% for dapagliflozin and 45.1% empagliflozin. A higher proportion of canagliflozin new users received more than three kinds of ADD (46.7%) than dapagliflozin (42.1%) and empagliflozin (38.1%) users.
Discussion
Patients with diabetes have an up to 50% increased risk of CVD compared with individuals without diabetes, but the optimization of glycemic control can reduce the long-term incidence of CVD and mortality.20 Although the CANVAS program, DECLARE-TIMI 58 trial and EMPA-REG OUTCOME demonstrated beneficial cardiovascular effects of SGLT2i, the eligibility of patients with type 2 diabetes for cardiovascular outcome trials of SGLT2i was not equally generalizable into routine clinical settings according to the global DISCOVER (DISCOVERing Treatment Reality of Type 2 Diabetes in Real World Settings) study.21 However, the DISCOVER study only focused on patients with type 2 diabetes initiating a second-line glucose-lowering therapy instead of SGLT2i. Our study indicated that characteristics of SGLT2i new users differed between real-world practice and clinical trials, possibly reflecting the fact that the timing of SGLT2i use and baseline CVD risks were not comparable to those in clinical trials. The applicability of the findings from clinical trials remains questionable.
Existing CVD history provides strong associations with an increased risk of recurrent CVD events, for example, Hu et al indicated around two-fold increase in CVD mortality in patients with diabetes and previous myocardial infarction, compared with diabetes only.22 This may highlight the importance of separating the roles of medications for primary prevention for those without a CVD history, and secondary prevention of re-occurrence of CVD events. Similar to other studies,8 21 23 24 we considered the EMPA-REG OUTCOME trial and VERTIS-CV trial results only applicable to a small proportion of patients with type 2 diabetes with CVD history (26.4%–27.2%) before receiving SGLT2i in our cohort.
Although the CANVAS program and DECLARE-TIMI 58 trials enrolled patients with type 2 diabetes with varying CVD risks, such as prevalent CVD or non-prevalent CVD with at least one major risk factor (eg, dyslipidemia), only 75.9% of canagliflozin and 65.8% of dapagliflozin new users met their inclusion criteria of CVD risk for the corresponding clinical trials. In addition, adherence to SGLT2i might differ between clinical trials and real-world practice, which may contribute to contrasting results.25 For example, medication adherence can be confounded by selection bias, where patients with more severe diseases (eg, established CVD) tend to be more adherent to medication, perhaps due to a perception of greater need.26 Therefore, patients with established CVD may have better awareness of disease controls with optimal treatment outcomes.27 28 Based on our evaluations, we suggest that the findings from current CV outcome trials may not apply to real-world patients, especially in patients with lower CVD risk.
Patients with poor blood sugar controls at baseline were prone to not obtaining the CVD benefits after use of SGLT2i. For example, subgroup analysis from the EMPA-REG OUTCOME trial found attenuating effects of empagliflozin in composite major adverse cardiovascular event end points when patients had higher HbA1c at baseline (HR <8.5%: 0.76; 95% CI 0.64 to 0.90; ≥8.5%: 1.14; 95% CI 0.86 to 1.50; p value for interaction=0.01). The effects of sustained hyperglycemia were often irreversible and promoted atherosclerosis,29 which may negate the CVD benefits from SGLT2i. We indicated that mean HbA1c was higher in real-world patients (canagliflozin: 8.4%; dapagliflozin: 8.5%; empagliflozin: 8.5%) than in either the CANVAS program (8.2%), DECLARE-TIMI 58 trial (8.3%) or EMPA-REG OUTCOME trial (8.1%). Our findings show the importance of re-evaluating CVD outcomes in patients with higher baseline HbA1c levels due to the potentially lower effectiveness of CVD outcomes from SGLT2i.
The relationship between HbA1c and CVD risk was U-shaped, with greater risk at both higher and lower HbA1c levels. Nichols et al indicated an 18%, 68% and 98% increased risk of CVD hospitalization with mean HbA1c of 6.0%–6.4%, <6.0% and >9.0%, respectively.30 In our cohort of SGLT2i new users, 25.0% had been excluded from CANVAS program due to baseline HbA1c levels outside the range of 7%–10.5%. Although SGLT2i could reduce the cardiovascular event and death risks in patients with type 2 diabetes with established atherosclerotic CVD, we should fill in the evidence gap by defining whether similar CVD benefits are to be found in patients with bidirectional HbA1c levels when adding SGLT2i into their treatment.
The CVD-Real Nordic and CVD-Real 2 studies assessed real-world data from 22 830 and 235 064 patients with type 2 diabetes, respectively, across different countries, and over 70% had no history of CVD. These studies showed SGLT2i significantly associated with a reduction in overall mortality from CVD by 47% and from any causes by 49%, respectively, compared with other treatment approaches.9 10 However, bias by drug indication between SGLT2i and other ADD cannot be excluded in these real-world studies due to the lack of clinical chemistry data, such as blood sugar levels and renal function data.12 20 In our analyses, we found SGLT2i new users had higher HbA1c levels (8.5%±1.7%), compared with other patients with type 2 diabetes receiving other ADD in Taiwan (7.7%±1.5%).31
Patients’ renal functions were important predictors for future CVD events in patients with type 2 diabetes,32 but the failure to adjust for renal functions may threaten the result validity of the CVD-Real Nordic and CVD-Real 2 studies.32 We found only 4.3% of SGLT2i new users with eGFR <45 mL/min/1.73 m2, since severe renal impairment is a contraindication for SGLT2i.33 Given that other ADD (eg, sulfonylurea, DPP4i and thiazolidinediones) could be used in patients with type 2 diabetes with severe renal impairment by adjusting dose, we considered the baseline eGFR may be higher in patients newly initiating SGLT2i than in other second-line ADD because of selection bias. Due to potential imbalances such as between laboratory findings of SGLT2i and other ADD new users, we still need further real-world studies that adjust for these confounders to estimate the true CVD effects of SGLT2i.
Although the CVD benefits of SGLT2i were proven by the CVD-REAL Nordic and CVD-REAL 2 studies with dapagliflozin constituting the most exposure time, individual SGLT2i drugs may possess unique features which contribute to different effectiveness and safety profiles. For example, canagliflozin has been reported with a two-fold increase in risk for lower-leg amputation, but this is not well documented with the other SGLT2i.34 We first confirmed the channeling uses of different SGLT2i in real-world settings, whereby the clinical indication for selecting a specific SGLT2i also potentially affected the CVD outcome.
Greenfield et al found better quality of diabetes care provided by endocrinologists than other specialties, including measurements and outcomes of metabolic indicators.35 We found 62.8% of canagliflozin new users were prescribed by endocrinologists, compared with 56.6% for dapagliflozin and 45.1% for empagliflozin; hence, treatment benefits may be overestimated in canagliflozin due to better clinical care of type 2 diabetes. Although SGLT2i was not associated with additional risk of hypoglycemia during monotherapy or dual therapy with metformin, it was found to increase odds of hypoglycemia over placebo in clinical trials during triple therapy with the combination of metformin and sulfonylurea (OR 2.33; 95% CI 1.52 to 3.55).36 Severe hypoglycemia was strongly associated with a higher risk of CVD incidence (HR 1.64; 95% CI 1.15 to 2.34) and mortality (HR 1.64, 95% CI 1.15 to 2.34).37 Compared with dapagliflozin and empagliflozin, a higher proportion of real-world canagliflozin new users used at least three kinds of ADD in combination as background therapy (46.7%), especially in combination with sulfonylurea (48.9%). Those with lower eGFR were at high risk of developing CVD, independent of albuminuria and metabolic control, for example, So et al found a 5% and three-fold risk increase of CVD in Chinese patients with type 2 diabetes with eGFR of 30–59 and 15–29 mL/min/1.73 m2, respectively, compared with eGFR ≥90 mL/min/1.73 m2.38 In our cohort, clinical physicians preferred to prescribe canagliflozin (19.6%) or empagliflozin (15.3%) to patients with type 2 diabetes with worse renal functions (eg, eGFR <60 mL/min/1.73 m2), compared with dapagliflozin (9.3%), which may lead to an imbalance in CVD risk at baseline among SGLT2i.
To discover real-world CVD benefits and risks both in the individual SGLT2i and whole SGLT2i class, we need further studies that consider these confounders (eg, medical specialties, background ADD therapy and renal functions) in the analyses to address the built-in heterogeneity of the SGLT2i class that may provide more valid results to better inform real-world clinical decisions.
The major strength of this study is direct comparison of baseline characteristics among different SGLT2i new users from the largest multi-institutional cohort of outpatients with type 2 diabetes in Taiwan, which allowed us to explore the discrepancies between current evidence and real-world data. The limitation is the potentially missing data on inclusion/exclusion criteria from the EMPA-REG OUTCOME trial, VERTIS-CV trial, DECLARE-TIMI 58 trial and CANVAS program in our EMR records.39 A number of patients may have a condition of interest without documentation in our database, such as current tobacco use with at least five cigarettes/day. Second, we also lack the information on ‘initial onset’ of comorbidity because we only screened the 1-year baseline period prior to the first use of SGLT2i. However, most major inclusion/exclusion criteria have been included in our study, so this effect may be limited. Third, we did not directly compare patient characteristics associated with ertugliflozin between real-world practice in Taiwan and the VERTIS-CV trial, because ertugliflozin was not available in study hospitals during our study period. We conducted post hoc comparisons of patient characteristics with all SGLT2i new users in Taiwan versus participants in the VERTIS-CV trial, and found suboptimal data representativeness of the VERTIS-CV trial (online supplementary appendix table 3). Fourth, the study only included SGLT2i trials for cardiovascular outcomes. Other trials of SGLT2i such as the Ccanagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation were not evaluated in this study. Fifth, one notable difference between the data source used in this study and the patient populations of the RCT studied is that the RCT enrolled patients from a heterogeneous racial/ethnic background whereas this study was restricted to Taiwanese patients. Finally, we did not include clinical end point in the analysis so no inference can be made on the effect to clinical outcome in the study. Future study to ensure the impact on clinical outcome resulted from different baseline characteristics of patients could be considered.
Conclusion
There is emerging evidence about the CVD benefits of SGLT2i from clinical trials and observational studies, but we have indicated that the generalizability of current evidence to real-world patients is suboptimal. More studies are needed to delineate similar cardiovascular effects of SGLT2i in patients with type 2 diabetes with lower CVD risks but poor blood sugar controls at baseline. In addition, we should consider more factors related to patient characteristics between the SGLT2i and other ADD to generate more accurate comparative CVD benefits. Specifically, researchers should note the channeling uses within SGLT2i and adjust these confounders to confirm real-world class effects in regard to cardiovascular event protection.
Acknowledgments
The authors would like to thank Chang Gung Memorial Hospital for providing Chang Gung Research Database data.
Footnotes
Contributors: The proposal for the analysis was developed by S-CS and EC-CL and reviewed by all authors. The general content of the manuscript was agreed on by all authors. The statistical analysis was conducted by S-CS and K-CC. The first draft of the manuscript was developed by S-CS and critically reviewed by all authors. All authors approved the final version of the manuscript before its submission. S-CS and EC-CL are the guarantors of this work.
Funding: This study received a grant from Chang Gung Medical Foundation (ID: CMRPG3H1551) and Ministry of Science and Technology of Taiwan (107-2320-B-006-070-MY3), which had no role in design, analysis, interpretation, reporting of results or the decision to develop this manuscript.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: This study has been approved by the Institutional Review Board and the Ethics Committee of Chang Gung Medical Foundation (CGMF), Taoyuan, Taiwan (201700241B0).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1.Wu JHY, Foote C, Blomster J, et al. . Effects of sodium-glucose cotransporter-2 inhibitors on cardiovascular events, death, and major safety outcomes in adults with type 2 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 2016;4:411–9. 10.1016/S2213-8587(16)00052-8 [DOI] [PubMed] [Google Scholar]
- 2.Zinman B, Wanner C, Lachin JM, et al. . Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 2015;373:2117–28. 10.1056/NEJMoa1504720 [DOI] [PubMed] [Google Scholar]
- 3.Wiviott SD, Raz I, Bonaca MP, et al. . Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med 2019;380:347–57. 10.1056/NEJMoa1812389 [DOI] [PubMed] [Google Scholar]
- 4.Neal B, Perkovic V, Mahaffey KW, et al. . Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med 2017;377:644–57. 10.1056/NEJMoa1611925 [DOI] [PubMed] [Google Scholar]
- 5.Zelniker TA, Wiviott SD, Raz I, et al. . Sglt2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet 2019;393:31–9. 10.1016/S0140-6736(18)32590-X [DOI] [PubMed] [Google Scholar]
- 6.Cannon CP, McGuire DK, Pratley R, et al. . Design and baseline characteristics of the eValuation of ertugliflozin effIcacy and safety cardiovascular outcomes trial (VERTIS-CV). Am Heart J 2018;206:11–23. 10.1016/j.ahj.2018.08.016 [DOI] [PubMed] [Google Scholar]
- 7.Hemkens LG, Contopoulos-Ioannidis DG, Ioannidis JPA. Agreement of treatment effects for mortality from routinely collected data and subsequent randomized trials: meta-epidemiological survey. BMJ 2016;352 10.1136/bmj.i493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Birkeland KI, Bodegard J, Norhammar A, et al. . How representative of a general type 2 diabetes population are patients included in cardiovascular outcome trials with SGLT2 inhibitors? a large European observational study. Diabetes Obes Metab 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kosiborod M, CSP L, Kohsaka S, et al. . Lower Cardiovascular Risk Associated with SGLT-2i in >400,000 Patients: The CVD-REAL 2 Study. J Am Coll Cardiol 2018;71:2628–39. [DOI] [PubMed] [Google Scholar]
- 10.Birkeland KI, Jørgensen ME, Carstensen B, et al. . Cardiovascular mortality and morbidity in patients with type 2 diabetes following initiation of sodium-glucose co-transporter-2 inhibitors versus other glucose-lowering drugs (CVD-REAL Nordic): a multinational observational analysis. Lancet Diabetes Endocrinol 2017;5:709–17. 10.1016/S2213-8587(17)30258-9 [DOI] [PubMed] [Google Scholar]
- 11.Raz I, Mosenzon O, Bonaca MP, et al. . DECLARE-TIMI 58: participants' baseline characteristics. Diabetes Obes Metab 2018;20:1102–10. 10.1111/dom.13217 [DOI] [PubMed] [Google Scholar]
- 12.Fitchett D. Sglt2 inhibitors in the real world: too good to be true? Lancet Diabetes Endocrinol 2017;5:673–5. 10.1016/S2213-8587(17)30259-0 [DOI] [PubMed] [Google Scholar]
- 13.Shao SC, Chan YY, Kao YH, et al. . The Chang Gung Research Database - a Multi-Institutional Electronic Medical Records Database for Real-World Epidemiological Studies in Taiwan. Pharmacoepidemiol Drug Saf 2019:1–8. [DOI] [PubMed] [Google Scholar]
- 14.Chao HY, Liu PH, Lin SC, et al. . Association of in-hospital mortality and dysglycemia in septic patients. PLoS One 2017;12:e0170408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lin YS, Chen TH, Chi CC, et al. . Different implications of heart failure, ischemic stroke, and mortality between nonvalvular atrial fibrillation and atrial flutter-a view from a national cohort study. J Am Heart Assoc 2017;21:e006406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chang S-L, Huang Y-L, Lee M-C, et al. . Association of varicose veins with incident venous thromboembolism and peripheral artery disease. JAMA 2018;319:807–17. 10.1001/jama.2018.0246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wiviott SD, Raz I, Bonaca MP, et al. . The design and rationale for the Dapagliflozin Effect on Cardiovascular Events (DECLARE)-TIMI 58 Trial. Am Heart J 2018;200:83–9. [DOI] [PubMed] [Google Scholar]
- 18.Piette JD, Kerr EA. The impact of comorbid chronic conditions on diabetes care. Diabetes Care 2006;29:725–31. 10.2337/diacare.29.03.06.dc05-2078 [DOI] [PubMed] [Google Scholar]
- 19.Austin PC. The use of propensity score methods with survival or time-to-event outcomes: reporting measures of effect similar to those used in randomized experiments. Stat Med 2014;33:1242–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schnell O, Standl E, Catrinoiu D, et al. . Report from the 3rd Cardiovascular Outcome Trial (CVOT) Summit of the Diabetes & Cardiovascular Disease (D&CVD) EASD Study Group. Cardiovasc Diabetol 2018;17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pintat S, Fenici P, Hammar N, et al. . Eligibility of patients with type 2 diabetes for sodium-glucose cotransporter 2 inhibitor cardiovascular outcomes trials: a global perspective from the discover study. BMJ Open Diabetes Res Care 2019;7:e000627 10.1136/bmjdrc-2018-000627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hu G, Jousilahti P, Qiao Q, et al. . The gender-specific impact of diabetes and myocardial infarction at baseline and during follow-up on mortality from all causes and coronary heart disease. J Am Coll Cardiol 2005;45:1413–8. 10.1016/j.jacc.2005.01.039 [DOI] [PubMed] [Google Scholar]
- 23.Wittbrodt E, Chamberlain D, Arnold SV, et al. . Eligibility of patients with type 2 diabetes for sodium-glucose co-transporter-2 inhibitor cardiovascular outcomes trials: an assessment using the diabetes collaborative registry. Diabetes Obes Metab 2019;21:1985–9. 10.1111/dom.13738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wittbrodt ET, Eudicone JM, Bell KF, et al. . Eligibility varies among the 4 sodium-glucose cotransporter-2 inhibitor cardiovascular outcomes trials: implications for the general type 2 diabetes US population. Am J Manag Care 2018;24:S138–45. [PubMed] [Google Scholar]
- 25.Cohen AT, Goto S, Schreiber K, et al. . Why do we need observational studies of everyday patients in the real-life setting?: Table 1. Eur Heart J Suppl 2015;17:D2–8. 10.1093/eurheartj/suv035 [DOI] [Google Scholar]
- 26.Yu AP, Yu YF, Nichol MB, et al. . Estimating the effect of medication adherence on health outcomes among patients with type 2 diabetes--an application of marginal structural models. Value Health 2010;13:1038–45. 10.1111/j.1524-4733.2010.00787.x [DOI] [PubMed] [Google Scholar]
- 27.Simpson SH, Lin M, Eurich DT. Medication adherence affects risk of new diabetes complications: a cohort study. Ann Pharmacother 2016;50:741–6. 10.1177/1060028016653609 [DOI] [PubMed] [Google Scholar]
- 28.Pladevall M, Williams LK, Potts LA, et al. . Clinical outcomes and adherence to medications measured by claims data in patients with diabetes. Diabetes Care 2004;27:2800–5. 10.2337/diacare.27.12.2800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aronson D, Rayfield EJ. How hyperglycemia promotes atherosclerosis: molecular mechanisms. Cardiovasc Diabetol 2002;1:1 10.1186/1475-2840-1-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nichols GA, Joshua-Gotlib S, Parasuraman S. Glycemic control and risk of cardiovascular disease hospitalization and all-cause mortality. J Am Coll Cardiol 2013;62:121–7. 10.1016/j.jacc.2013.04.031 [DOI] [PubMed] [Google Scholar]
- 31.Yu N-C, Su H-Y, Chiou S-T, et al. . Trends of ABC control 2006-2011: a national survey of diabetes health promotion Institutes in Taiwan. Diabetes Res Clin Pract 2013;99:112–9. 10.1016/j.diabres.2012.11.018 [DOI] [PubMed] [Google Scholar]
- 32.Ragot S, Saulnier P-J, Velho G, et al. . Dynamic changes in renal function are associated with major cardiovascular events in patients with type 2 diabetes. Diabetes Care 2016;39:1259–66. 10.2337/dc15-2607 [DOI] [PubMed] [Google Scholar]
- 33.American Diabetes Association Pharmacologic approaches to glycemic treatment: standards of medical care in Diabetes-2019. Diabetes care 2018;42:S90–102. [DOI] [PubMed] [Google Scholar]
- 34.Cefalu WT, Kaul S, Gerstein HC, et al. . Cardiovascular Outcomes Trials in Type 2 Diabetes: Where Do We Go From Here? Reflections From a Diabetes Care Editors' Expert Forum. Diabetes Care 2018;41:14–31. 10.2337/dci17-0057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Greenfield S, Kaplan SH, Kahn R, et al. . Profiling care provided by different groups of physicians: effects of patient case-mix (bias) and physician-level clustering on quality assessment results. Ann Intern Med 2002;136:111–21. 10.7326/0003-4819-136-2-200201150-00008 [DOI] [PubMed] [Google Scholar]
- 36.Palmer SC, Mavridis D, Nicolucci A, et al. . Comparison of clinical outcomes and adverse events associated with glucose-lowering drugs in patients with type 2 diabetes: a meta-analysis. JAMA 2016;316:313–24. 10.1001/jama.2016.9400 [DOI] [PubMed] [Google Scholar]
- 37.Lee AK, Warren B, Lee CJ, et al. . The association of severe hypoglycemia with incident cardiovascular events and mortality in adults with type 2 diabetes. Diabetes Care 2018;41:104–11. 10.2337/dc17-1669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.So WY, Kong APS, Ma RCW, et al. . Glomerular filtration rate, cardiorenal end points, and all-cause mortality in type 2 diabetic patients. Diabetes Care 2006;29:2046–52. 10.2337/dc06-0248 [DOI] [PubMed] [Google Scholar]
- 39.McGovern A, Feher M, Munro N, et al. . Sodium-Glucose Co-Transporter-2 (SGLT2) inhibitors: comparing trial and real world use (study protocol). Diabetes Ther 2017;8:355–63. 10.1007/s13300-017-0229-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjdrc-2019-000742supp001.pdf (80KB, pdf)