Abstract
Purpose
Individual measures of health literacy are not feasible for administration on a large scale, yet estimates of community-level health literacy in the US recently became available. We sought to investigate whether community-level health literacy estimates are associated with the initiation of oral antihyperglycemic agents (OHA) and the use of standard preventive care services among older adults with newly diagnosed diabetes.
Patients and methods
We conducted a retrospective cohort study of 169,758 patients, ≥65 years old with hypertension and newly diagnosed type 2 diabetes using 2007–2011 data from the Center for Medicare and Medicaid Services Chronic Conditions Warehouse. We examined the relationship between community-level health literacy estimates and initiation of OHA, receipt of flu shots, eye exams, Hemoglobin A1c tests, and lipid tests within 12 months post diabetes diagnosis.
Results
Patients living in communities with above basic health literacy (vs. basic/below basic) were 15% more likely to initiate OHA (Hazard Ratio=1.15; 95% CI 1.12 to 1.18). After classifying the health literacy distribution as quintiles, the analysis revealed a dose–response relationship with OHA initiation that plateaued at the third and fourth quintiles and declined at the fifth quintile. Individuals residing in communities with higher health literacy were more likely to participate in preventive care services (relative risk ranged from 1.09 for lipid test [95% CI 1.07–1.11] to 1.43 for flu shot [95% CI 1.41–1.46]).
Conclusion
Community-level health literacy estimates were associated with the initiation of OHA and uptake of standard preventive care services in older adults. Community-level health literacy may help to inform targeted diabetes education and support efforts.
Keywords: health literacy, diabetes mellitus, adherence, preventive care
Introduction
Diabetes has become a global epidemic affecting 366 million people, including almost 29 million in the US, or 9% of the US population.1,2 The elderly are disproportionally affected by diabetes: in the US, more than a quarter (11.2 million) of persons 65 years of age and older have diabetes.2 Approximately 71% of US adults with diabetes also have hypertension, a common comorbid condition.2 Patients with both hypertension and diabetes are at considerably increased risk for mortality and morbidities, especially cardiovascular diseases. Timely use of antihyperglycemic agents and standard preventive care is important among these high-risk patients to prevent diabetes complications and comorbidities.3 Clinical guidelines stress the importance of assessing medical, functional, mental, and social determinants of health to improve diabetes management in older adults.4
Health literacy, defined as one’s ability to obtain, process and understand the information needed to make health decisions, has been shown to influence patient health behaviors, chronic disease self-management, and communication with clinicians.5,6 Yet challenges related to health literacy measurement have limited investigation of the complex relationship between health literacy, health behaviors and health outcomes. Commonly used individual-level health literacy assessments can be time- and resource-intensive; in most cases, they are not be feasible for administration on a broad scale. As a result, most health literacy studies have had small sample sizes and have been underpowered to assess the association between health literacy and treatment use/care and clinical outcomes or endpoints.7
While generally measured at the individual level, health literacy reflects not only individual-level skills but also how well health systems provide services to vulnerable populations.5,8 It can also be conceptualized as a community-level characteristic, capturing the average health literacy of individuals living within a specified geographic area, and may provide an alternative solution for conceptualizing and estimating health literacy. Health behaviors and other health-related decisions do not occur in isolation, but are often influenced by community factors and input. Thus, one’s community health literacy level may also influence whether and how a patient obtains, interprets and applies health information, as well as how healthcare is accessed and used.
Recently, a method of estimating the community-level health literacy of US census block groups was developed and validated by our research team.9 The estimates of community-level health literacy have been mapped throughout the US.10 However, few, if any, studies have examined the role of community-level health literacy on patient health behaviors and outcomes. Such a study may help provide insights on the use of community-level health literacy as a more cost-effective mechanism for identifying communities or neighborhoods of individuals who may be at increased risk for complications related to diabetes, which could help promote and target public health efforts. Therefore, using this novel measurement approach, this study aimed to investigate the associations between community-level health literacy estimates and the initiation of oral antihyperglycemic agents and the use of standard preventive care in a national cohort of older adults with hypertension and newly diagnosed diabetes.
Materials and Methods
Data Sources and Study Cohort
The primary data sources used for this study were Center for Medicare and Medicaid (CMS) Chronic Conditions Warehouse (CCW) research files from 2007 to 2011, which included all Medicare patients that met chronic conditions criteria for type 2 diabetes for the first time in 2008 and were previously diagnosed with hypertension. The final analytical cohort included patients who met the following inclusion criteria: 1) had type 2 diabetes diagnosis in 2008 (first type 2 diabetes diagnosis was considered index diagnosis); 2) lived in the United States with a valid residential ZIP code; 3) were 66 years of age at the time of index diagnosis; 4) lived at least 1 day after type 2 diabetes diagnosis date; and in the 12-month baseline period had: 5) no type 2 diabetes diagnosis; 6) no fills for anti-diabetic medications; 7) no end-stage renal disease (ESRD); and 8) a diagnosis of hypertension. Figure A1 shows the details of the cohort selection process.
Community-Level Health Literacy
Community-level health literacy was estimated at the US census block group level using an approach developed by our team.9,11 Our model was based upon work by Martin et al, who used linear regression and data from the 2003 National Assessment of Adult Literacy (NAAL) and 2000 US Census to predict the mean health literacy score of individuals living in a US census tract.11 The predictor variables are the same between the original model and our model but we modified the model to predict health literacy at the census block group level for greater precision. Specifically, the model uses the following predictor variables: gender, age, race/ethnicity, language spoken at home, income, education, marital status, time in the US, and metropolitan statistical area. We used the 2010 US Census Summary File 1 to create the gender, age, race/ethnicity variables at census block group level and the 5-year (2006–2010) American Community Survey (ACS) Summary File to create the variables of language spoken at home, income, education and marital status at census block group level. Time in the USA was entered as a census tract level variable from the ACS Summary File, as no aggregated statistics at block group level were available for this variable. More detailed information on both the NAAL and the Martin et al predictive model has been published elsewhere.8,11
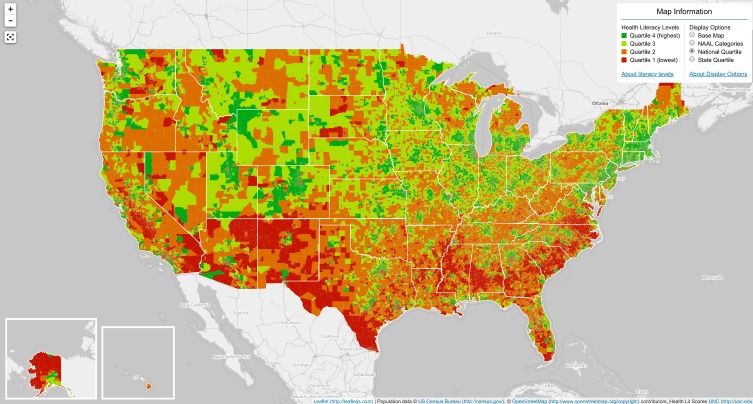
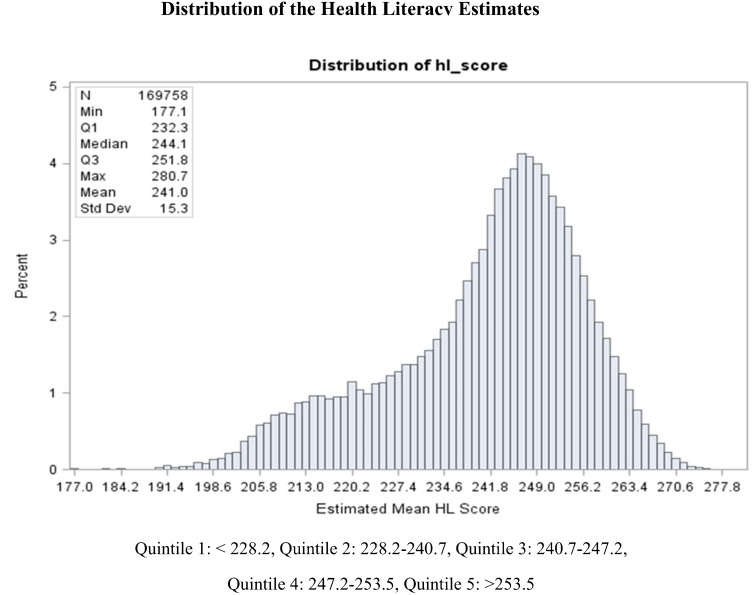
Figure 1 presents the map of the estimated community-level health literacy in the US.10 The interactive map can be accessed from http://healthliteracymap.unc.edu/. Patients were geo-coded using their residential ZIP code from the Medicare beneficiary summary file to a specific US census block group and then linked to the corresponding community-level health literacy estimate. A Census block group is generally defined to contain between 600 and 3000 people.12 The predictive model generates health literacy estimates that are consistent with scores used by the 2003 NAAL.8 Patients with the NAAL health literacy score ≤225 are described as having “basic or below” health literacy level, indicating that they have difficulty obtaining, processing, and understanding basic health information and services.8 Thus, the community health literacy estimates were categorized according to the 2003 NAAL criteria of “above basic” (score >225) and “basic/below basic” (score ≤225). We also used the quintiles of the distribution of estimates to categorize community-level health literacy, with the lowest referencing the lowest community-level health literacy estimates. The distribution of community-level health literacy estimates for our cohort and the description of the cut-off points for the quintiles are shown in Figure 2.
Figure 1.
Map of estimated community-level health literacy in the US.
Note: Reproduced from Health Literacy Data Map. US Health Literacy Data Map. Chapel Hill: University of North Carolina at Chapel Hill, 2019. Available from: http://healthliteracymap.unc.edu/.10
Figure 2.
Distribution of mean community health literacy estimates in a cohort of hypertensive Medicare patients, newly diagnosed with diabetes.
Patient Characteristics and Covariates
Patient age, race/ethnicity, and sex were identified using the 2008 CCW beneficiary summary file. The status of being in Medicare Part D prescription benefit gap (doughnut hole) prior to incident type 2 diabetes diagnosis was created using Part D claims files. Patient baseline characteristics and clinical conditions were assessed from the CMS medical service claims files during the period of 12 months prior to index type 2 diabetes diagnosis. We included comorbidity levels as measured by the Charlson comorbidity index13 and other medical conditions described previously in the literature.14 Diabetic complications noted during the index type 2 diabetes diagnosis, such as renal, ophthalmic, neurological, peripheral circulatory, ketoacidosis, hyperosmolarity, coma, and other unspecified manifestations, were also measured.
Outcomes
The first outcome of interest was length of time between the date of new type 2 diabetes diagnosis and the initiation of any oral antihyperglycemic agent (OHA). Initiation of OHA was defined as the date of the first OHA prescription fill and was measured from Medicare Part D event files. The second outcome was the use of the following standard preventive care services within 12 months post type 2 diabetes diagnosis: flu shots, eye exams, hemoglobin A1c (HbA1c) tests and lipid tests.3 We used Medicare Part B institutional and non-institutional claims to identify preventive care use based on published algorithms.15
Statistical Analyses
We compared patient characteristics by the dichotomized community-level health literacy categories of “above basic” and “basic/below basic” and by quintiles of the community-level health literacy estimates. We used the method of absolute standardized difference (ASD) to evaluate the extent of the difference in the prevalence of patient characteristics between patients living in the neighborhoods with the lowest quintile of community-level health literacy and patients living in those with the highest quintile.16 A value of ASD greater than 10 approximates alpha <0.05 and suggests a significant difference between the comparison groups.
To assess the association between community-level health literacy and time to initiation of OHA, we applied a proportional hazard regression model with death as a competing risk.17 The model estimated both the unadjusted associations (hazard risk) between community-level health literacy and the outcomes, and the adjusted associations by controlling for patients’ demographic and clinical characteristics. The follow-up period for the time to initiation of OHA outcome began on date of the index type 2 diabetes diagnosis and was censored administratively at the end of study period (Dec 31, 2011) or on the first day of the month when the patient was no longer enrolled in Medicare Part D program, whichever occurred first. To account for clustering of patients within census block group, we used a robust sandwich estimate approach to estimate robust standard errors.18 We also compared the cumulative incidence curves by quintiles of the community-level health literacy estimates and also used the Gray test to evaluate the differences in cumulative incidence between groups.19 We calculated the cumulative incidence of OHA initiation at 1 year after the index new type 2 diabetes diagnosis.
To assess the association between community-level health literacy estimates and the use of preventive care services, we used a sub-cohort of patients who survived at least 12 months post index diabetes diagnosis. We applied a modified Poisson regression model with robust error variance to estimate risk ratios (relative risk) to model the probability of receiving each of the preventive care services within 12 months post index diagnosis.20 We chose this modified Poisson model, rather than survival analysis, to analyze these outcomes as we sought to relate community-level health literacy to patients’ behavior to seek preventive care in general, instead of by timing, which could be affected by having received these services in the not too distant past. Additionally, clinical guidelines do not specify precisely how soon patients should receive these services post diagnosis, but rather how often (i.e., fasting lipid profile to be measured annually).3
In sensitivity analyses, we assessed whether controlling for primary care physician shortage in local areas affected the association between estimated community-level health literacy and the investigated outcomes. Primary care physician shortage in local areas was measured by two county-level variables from the Area Resource File (2009–2010 Release): one indicating if the whole county was designated as a shortage area; the other, indicating if parts of the county were designated as shortage areas.21 We used SAS version 9.4 for all analyses. The study was approved by the University of North Carolina at Chapel Hill Institutional Review Board.
Results
Of 340,563 hypertensive Medicare patients newly diagnosed with diabetes in 2008, 169,758 met our eligibility criteria. Of these, 149,555 (88.1%) survived at least 12 months post index type 2 diabetes diagnosis. The mean community-level health literacy estimate for this cohort was 241 (range of 177–281 with a standard deviation of 15). The mean community-level health literacy estimate for patients living in neighborhoods with the lowest community-level health literacy quintile (Q1) was 216, while the mean for the patients living in the neighborhoods with highest community-level health literacy quintile (Q5) was 259. The distribution of the community-level health literacy estimate is presented in Figure 2. Table 1 shows demographic and baseline clinical characteristics of our study cohort. Patients living in the neighborhoods with the highest community-level health literacy estimates were more likely to have fewer comorbidities, lower rates of chronic obstructive pulmonary disease and angina pectoris, and higher rates of atrial fibrillation, hyperlipidemia and hypothyroidism.
Table 1.
Patient Characteristics Stratified by Levels of Community Health Literacy Estimates
| Characteristics (N = 169,758) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Community Health Literacy Level (Census Block group) | Basic/Belowa | Above Basica | Q1 | Q2 | Q3 | Q4 | Q5 | ASD |
| Mean Community Health Literacy Score | 214.3 | 246.3 | 216.3 | 235.3 | 244.1 | 250.2 | 259.0 | – |
| Socio-Demographics, % | ||||||||
| Age (years) | ||||||||
| 66–74 | 43.6 | 42.1 | 43.2 | 42.1 | 43.5 | 42.5 | 40.6 | 5.3 |
| 75–84 | 37.6 | 38.1 | 37.8 | 38.3 | 37.4 | 37.9 | 38.5 | 1.4 |
| 85+ | 18.8 | 19.8 | 19.0 | 19.6 | 19.1 | 19.6 | 20.9 | 4.9 |
| Sex | ||||||||
| Male | 33.8 | 34.9 | 33.7 | 33.4 | 34.1 | 35.7 | 37.0 | 6.8 |
| Female | 66.2 | 65.1 | 66.3 | 66.6 | 65.9 | 64.3 | 63.0 | 6.8 |
| Race | ||||||||
| White | 41.3 | 87.0 | 44.5 | 77.7 | 89.9 | 92.1 | 92.5 | 120.6 |
| Black | 33.3 | 6.2 | 31.3 | 11.6 | 4.8 | 3.1 | 3.0 | 81.2 |
| Asian | 8.0 | 3.9 | 8.2 | 6.1 | 2.9 | 2.8 | 2.9 | 23.5 |
| Hispanic | 16.1 | 1.8 | 14.6 | 3.1 | 1.3 | 1.0 | 0.8 | 53.6 |
| Other | 1.2 | 1.1 | 1.3 | 1.5 | 1.1 | 0.9 | 0.9 | 4.6 |
| Prescription Part D benefit gap (Donut Hole) | 10.6 | 9.8 | 10.7 | 10.5 | 9.5 | 9.4 | 9.7 | 3.2 |
| Diabetic Complications at Index Diagnosis | ||||||||
| Polyneuropathy | 0.3 | 0.4 | 0.3 | 0.4 | 0.4 | 0.4 | 0.3 | 0.2 |
| Background diabetic retinopathy | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.6 |
| Proliferative diabetic retinopathy | 0.1 | 0.0 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.9 |
| Mild non-proliferative diabetic retinopathy | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 1.5 |
| Diabetic macular edema | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 1.3 |
| Baseline Comorbidities | ||||||||
| Charlson Comorbidity Index | ||||||||
| 0 | 34.8 | 38.2 | 34.8 | 36.0 | 37.9 | 39.3 | 40.1 | 11.1 |
| 1–2 | 39.5 | 38.4 | 39.7 | 39.6 | 38.5 | 38.1 | 37.0 | 5.4 |
| 3–5 | 20.6 | 19.1 | 20.5 | 20.0 | 19.3 | 18.5 | 18.6 | 4.9 |
| 6–8 | 3.6 | 3.0 | 3.6 | 3.1 | 3.0 | 2.8 | 3.1 | 2.9 |
| 9+ | 1.4 | 1.3 | 1.5 | 1.3 | 1.3 | 1.4 | 1.2 | 2.4 |
| Acute myocardial infarction | 1.8 | 2.0 | 1.8 | 1.9 | 2.0 | 2.0 | 1.9 | 1.3 |
| Cancer | 10.8 | 12.8 | 11.0 | 12.2 | 12.3 | 12.8 | 14.0 | 9.2 |
| Cerebrovascular disease | 17.7 | 16.6 | 17.8 | 17.5 | 16.4 | 15.9 | 16.4 | 3.8 |
| Congestive heart failure | 21.9 | 20.1 | 21.7 | 21.5 | 20.9 | 19.7 | 18.3 | 8.5 |
| Chronic obstructive pulmonary disease | 27.3 | 24.9 | 27.2 | 26.7 | 26.4 | 24.4 | 21.9 | 12.4 |
| Dementia | 11.0 | 8.8 | 11.0 | 9.3 | 8.4 | 8.0 | 9.0 | 6.5 |
| AIDS/HIV | 0.2 | 0.0 | 0.2 | 0.1 | 0.0 | 0.0 | 0.0 | 4.5 |
| Metastatic carcinoma | 1.6 | 1.6 | 1.6 | 1.6 | 1.6 | 1.7 | 1.7 | 0.1 |
| Mild liver disease | 3.1 | 2.1 | 3.0 | 2.5 | 2.1 | 1.8 | 2.0 | 6.7 |
| Moderate or severe liver disease | 0.3 | 0.2 | 0.3 | 0.2 | 0.2 | 0.2 | 0.2 | 2.2 |
| Paraplegia or hemiplegia | 2.7 | 1.9 | 2.7 | 2.2 | 1.8 | 1.8 | 1.8 | 5.5 |
| Peptic ulcer disease | 2.9 | 1.9 | 2.8 | 2.4 | 1.9 | 1.7 | 1.6 | 8.5 |
| Peripheral vascular disease | 20.6 | 18.1 | 20.5 | 18.8 | 17.9 | 17.5 | 18.0 | 6.4 |
| Renal disease | 10.9 | 9.8 | 10.8 | 10.3 | 9.9 | 9.7 | 9.2 | 5.4 |
| Rheumatic disease | 4.5 | 4.2 | 4.4 | 4.2 | 4.3 | 4.1 | 4.3 | 0.5 |
| Atrial fibrillation | 9.2 | 14.1 | 9.5 | 12.7 | 13.8 | 14.8 | 15.4 | 18.0 |
| Angioedema | 0.1 | 0.1 | 0.1 | 0.2 | 0.1 | 0.1 | 0.1 | 0.5 |
| Angina pectoris | 5.3 | 3.7 | 5.2 | 4.5 | 4.0 | 3.5 | 2.8 | 12.0 |
| Asthma | 9.2 | 7.1 | 9.0 | 7.7 | 7.0 | 6.9 | 6.5 | 9.2 |
| Coronary artery bypass grafting | 0.7 | 1.1 | 0.8 | 0.9 | 1.0 | 1.1 | 1.2 | 4.5 |
| Hypercalcemia | 0.6 | 0.6 | 0.6 | 0.6 | 0.7 | 0.6 | 0.7 | 0.4 |
| Hyperkalemia | 2.5 | 2.4 | 2.5 | 2.4 | 2.4 | 2.4 | 2.4 | 0.7 |
| Hyperlipidemia | 54.6 | 60.0 | 54.9 | 58.8 | 59.8 | 60.6 | 61.3 | 13.0 |
| Hypotension | 3.9 | 4.2 | 3.9 | 4.2 | 4.1 | 4.0 | 4.5 | 2.7 |
| Hypothyroidism | 14.4 | 18.3 | 14.8 | 18.0 | 18.5 | 18.2 | 18.9 | 10.9 |
| Ischemic heart disease | 34.6 | 33.3 | 34.5 | 34.5 | 33.7 | 33.1 | 31.9 | 5.6 |
| Baseline osteoporosis | 13.3 | 11.2 | 13.2 | 11.7 | 10.8 | 10.8 | 11.3 | 5.7 |
| Percutaneous transluminal coronary angioplasty/Stent | 1.3 | 1.7 | 1.3 | 1.6 | 1.9 | 1.7 | 1.8 | 3.5 |
| Rhabdomyolysis/myopathy | 7.3 | 7.5 | 7.3 | 7.8 | 7.5 | 7.4 | 7.4 | 0.4 |
| Sinus bradycardia/Heart block | 10.0 | 10.2 | 10.0 | 10.1 | 10.1 | 10.3 | 10.4 | 1.1 |
| Stroke | 10.3 | 9.1 | 10.3 | 9.7 | 9.1 | 8.4 | 8.9 | 4.8 |
| Unstable angina | 1.3 | 1.2 | 1.2 | 1.2 | 1.3 | 1.2 | 1.2 | 0.6 |
| Stage 1 chronic kidney disease | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 1.8 |
| Stage 2 chronic kidney disease | 0.5 | 0.4 | 0.5 | 0.4 | 0.4 | 0.4 | 0.3 | 2.3 |
| Stage 3 chronic kidney disease | 2.5 | 2.6 | 2.5 | 2.6 | 2.7 | 2.6 | 2.5 | 0.4 |
| Stage 4 chronic kidney disease | 1.3 | 1.2 | 1.3 | 1.3 | 1.2 | 1.3 | 1.1 | 2.1 |
| Stage 5 chronic kidney disease | 0.3 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 0.2 | 1.4 |
| Chronic kidney disease unspecified | 5.0 | 4.4 | 5.0 | 4.8 | 4.4 | 4.2 | 4.2 | 3.8 |
| Hypertensive chronic kidney disease | 5.2 | 4.6 | 5.2 | 4.9 | 4.4 | 4.4 | 4.4 | 3.5 |
Notes: Q: quintiles: first quintile is the lowest and fifth quintile is the highest health literacy level. aBased on the 2003 National Assessment of Adult Literacy (NAAL) categorization of health literacy proficiencies (8) into two categories: “above basic” (score >225) vs. “basic/below basic” (score ≤ 225). ASD = Absolute standardized difference comparing quintile 1 to quintile 5, a value ≥10 approximates α < 0.05 suggesting significant difference.
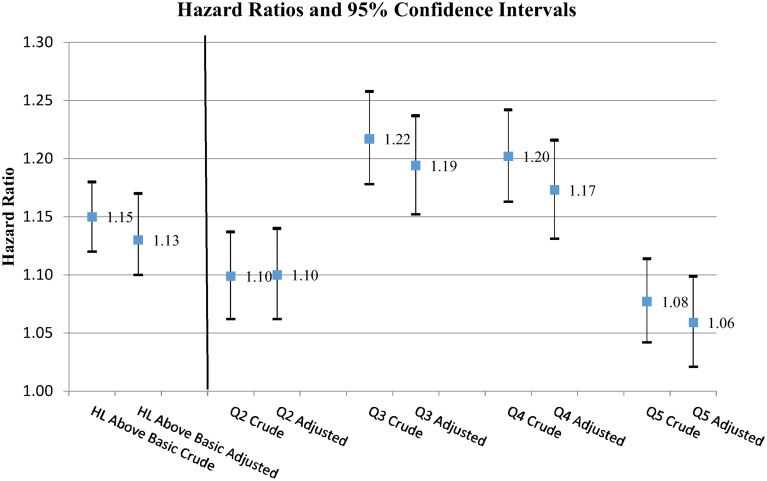
The effects of the community-level health literacy estimates on OHA initiation are presented in Table 2 and Figure 3. Compared to patients living in neighborhoods with low community-level health literacy (basic/below basic or first quintile), patients living in neighborhoods with higher community-level health literacy (above basic or second quintile through fifth quintile, respectively) had higher rates of OHA initiation after index type 2 diabetes diagnosis (Table 2). The overall rate of OHA initiation at 1 year was 17.2%. The OHA initiation rate ranged from 15.5% for patients living in neighborhoods with the lowest community-level health literacy (first quintile) to 18.6% in the third quintile. Figures A2 and A3 show the observed cumulative incidence of initiation of OHA across different levels of estimated community health literacy. Figure 2 displays the estimated associations (hazard ratios) between community-level health literacy categories and time to initiation of OHA. Patients in neighborhoods with above basic community-level health literacy were 15% (unadjusted, 95% CI of 1.12–1.18) and 13% (adjusted, 95% CI 1.10–1.17) more likely to have initiated OHA. In both unadjusted and adjusted analyses, higher levels (second quintile thru fifth quintile) of community-level health literacy were associated with increases in rates of OHA initiation as compared to the lowest community-level health literacy (first quintile). However, there was not a linear dose–response relation and the increase plateaued at the third and fourth quintiles. The adjusted hazard ratios for other quintiles compared to the first quintile were as follows: second quintile (1.10, 95% CI 1.06–1.14), third quintile (1.19, CI 1.15–1.24), fourth quintile (1.17, CI 1.13–1.22), fifth quintile (1.06, CI 1.02–1.10).
Table 2.
OHA Initiation and Preventive Care Services by Community-Level Health Literacy
| Outcomes | Medication, N (%)a | Preventive Care Services, N (%) | |||
|---|---|---|---|---|---|
| OHA Initiation | Flu Vaccination | Eye Exam | HbA1c Test | Lipid Test | |
| All Patients | 25,531 (17.2) | 80,500 (53.8) | 70,423 (47.1) | 45,232 (30.2) | 71,669 (47.9) |
| By community health literacy levels | |||||
| Basic/belowb | 3796 (15.4) | 9821 (39.5) | 10,834 (43.6) | 6552 (26.3) | 11,101 (44.6) |
| Above basicb | 21,735 (17.6) | 70,679 (56.7) | 59,589 (47.8) | 38,680 (31.0) | 60,568 (48.6) |
| Quintile 1 (lowest) | 4585 (15.5) | 12,181 (41.0) | 13,072 (44.0) | 7924 (26.7) | 13,337 (44.9) |
| Quintile 2 | 5126 (17.3) | 15,605 (52.4) | 13,829 (46.4) | 8743 (29.4) | 14,063 (47.2) |
| Quintile 3 | 5524 (18.6) | 16,503 (55.2) | 13,756 (46.0) | 9394 (31.4) | 14,720 (49.2) |
| Quintile 4 | 5429 (18.2) | 17,736 (59.1) | 14,438 (48.1) | 9780 (32.6) | 14,800 (49.3) |
| Quintile 5 (highest) | 4867 (16.3) | 18,475 (61.3) | 15,328 (50.9) | 9391 (31.2) | 14,749 (49.0) |
Notes: aNumber of patients initiating oral hyperglycemic agents per 100 patients at risk. bBased on the 2003 National Assessment of Adult Literacy (NAAL) categorization of health literacy proficiencies (8) into two categories: “above basic” (score >225) vs. “basic/below basic” (score ≤225).
Figure 3.
Associations between community health literacy levels and initiation of oral antihyperglycemic agents after new type 2 diabetes diagnosis.
Notes: Reference groups: Community health literacy at basic/below level; Q1 (lowest) level of community health literacy in quintiles. Based on the 2003 National Assessment of Adult Literacy (NAAL) categorization of health literacy proficiencies (8) into two categories: “above basic” (score >225) vs. “basic/below basic” (score ≤225). Abbreviations: HL, health literacy; Q, quintile.
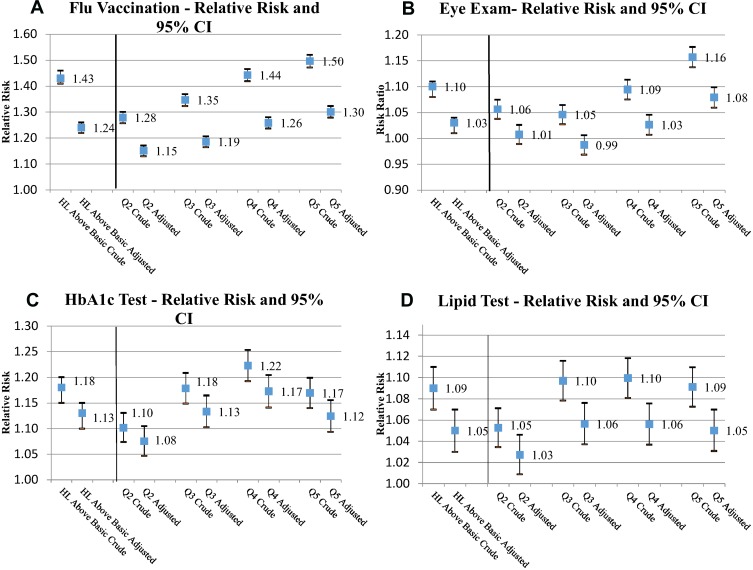
The effects of estimated community-level health literacy on preventive care service use are presented in Table 2 and Figure 4. Compared to patients living in neighborhoods with low community-level health literacy, patients living in neighborhoods with higher community-level health literacy had higher rates of standard preventive care services within 12 months post new type 2 diabetes diagnosis. Figure 4A–D shows the estimated risk ratios (relative risks) that quantify the associations between different levels of estimated community health literacy and preventive care services received within the 12 months post diagnosis period. Patients from neighborhoods with above basic community-level health literacy were more likely to receive standard care diabetes services than were patients from neighborhoods with basic or below basic community-level health literacy. In the analyses by community-level health literacy quintiles, the increases in likelihood range from 9% (unadjusted, 95% CI 1.07–1.11) and 5% (adjusted, 95% CI 1.03–1.07) for lipid test to 43% (unadjusted, 95% CI 1.41–1.46) and 24% (adjusted, 95% CI 1.22–1.26) for flu vaccination. There was a strong dose–response association between community-level health literacy and flu vaccination and a general trend of dose–response association for an eye exam and lipid tests. Further, patients living in neighborhoods with high community-level health literacy had statistically higher chances of receiving HbA1c tests, although this increase plateaued by the fourth quintile.
Figure 4.
(A–D) Associations between community health literacy levels and preventive care services within 12 months post new type 2 diabetes diagnosis.
To address the concern that lower community-level health literacy is simply a proxy for disadvantaged or underserved areas, we conducted sensitivity analyses that included two physician shortage area covariates (i.e. whole or part of residential county designated as a primary care shortage area). Results showed that the effects of community-level health literacy on outcomes were not affected by the inclusion of these variables (Tables A1 and A2). The two physician shortage variables, however, were statistically significantly associated with the initiation of OHA and flu vaccination, suggesting that physician shortage areas and community-level health literacy are capturing two distinct characteristics of the community.
Discussion
We examined whether a measure of community-level health literacy was associated with initiation of OHA and other standard preventive care services for diabetes. In our nationally representative study cohort of 169,758 older adults with hypertension and newly diagnosed diabetes, 14.5% of the study cohort lived in communities with basic/below basic health literacy.8 Patients living in neighborhoods with lower community-level health literacy had more comorbidities and chronic conditions. Compared to the basic/below basic or first (lowest) quintile of the community-level health literacy estimates, higher community-level health literacy was associated with higher rates of OHA initiation and receipt of standard preventive care services.
The association between estimated community-level health literacy and the initiation of OHA is multifaceted, as the association across quintiles is not linear, but convex. Two different mechanisms may explain this pattern. First, patients living in neighborhoods with lower community-level health literacy may be less likely to receive timely and appropriate care, reflecting disparities in care. This may explain why our analysis showed increasingly higher rates of OHA initiation from the first quintile of community-level health literacy to the third quintile. Also, we speculate that this may be a reason that patients living in areas with lower community-level health literacy had low reported rates of hyperlipidemia, atrial fibrillation and hypothyroidism. They may have less screening or access to care for these diagnoses rather than an actual lower prevalence of these medical conditions. Second, it is important to note that when newly diagnosed with diabetes, patients are first encouraged to start life-style and diet changes for glycemic control before any initiation of OHA. Patients living in areas with higher community-level health literacy may not only be able to perform better self-care and to achieve a healthier diet and lifestyle due to their own health literacy, but such changes in self-care and lifestyle may be reinforced and supported by those in the broader community, such as nearby friends, family and neighbors, who also understand the importance of such changes. Thus, those living in communities with high health literacy may have better glycemic control and consequently a reduced need to initiate OHA earlier. This may explain why the OHA initiation rate plateaued at the third and fourth quintiles of community-level health literacy, followed by a markedly lower rate at the fifth quintile. Future studies will be needed to identify and understand how to overcome community-level health literacy barriers.
There was also a dose–response association between community-level health literacy and a range of standard preventive care services evaluated in this study. However, the effect size and impact of community-level health literacy estimates on the respective standard preventive care services varied. Flu vaccination was the most affected by community-level health literacy, followed by HbA1c tests, eye exams, and lipid tests. Public health campaigns promoting flu vaccination are widespread, including messages around its importance and where to get one. Given the extensive literature linking individual-level health literacy to preventive care outcomes, it is reasonable to assume that more individuals in communities with higher average health literacy understand the importance of the flu vaccine, and not only received one, but encourage others in their community to do the same. Messaging around more diabetes-specific preventive care services may not be as pervasive in the community, which would result in less community-level knowledge and patient support to obtain these services. More research is needed to confirm this hypothesis and to test whether community-level health literacy may be a stronger predictor of more population-based health outcomes and the relative importance of community-level to individual-level health literacy for more specified clinical outcomes.
Other factors such as availability of health-care providers in an area may also influence treatment and standard preventive care use. In our sensitivity analysis, it was shown that area primary care physician shortage was associated with both the initiation of OHA and uptake of flu vaccination, but did not affect the association between estimated community health literacy and the studied outcomes. In this study, the strength of the associations between community-level health literacy eatimates and studied outcomes was attenuated after adjusting for patient baseline clinical characteristics. However, it may be reasonable to consider the baseline patient clinical characteristics as intermediaries rather than confounders. Since community-level health literacy was estimated cross-sectionally, and patients living in neighborhoods with low community-level health literacy had more comorbidities and chronic conditions at baseline, lower community-level health literacy could be seen as an important contributor to the development of chronic conditions at baseline.
These findings have important implications for research and practice. First, results suggest that community-level health literacy may be an important factor to consider in patient education efforts. Given that it is not feasible to comprehensively assess the health literacy of patients or a community on a broad scale, community-level health literacy estimates may provide a simpler and more cost-effective approach to identifying populations, or areas, that may benefit from additional support or education. Our team has provided community-level estimates of health literacy for almost all census block groups across the United States. This data is publically available, free of charge, on a university-hosted website.10 Community partners and other organizations may use this information to better target public health efforts. Secondly, community-level health literacy has other unique strengths from a research perspective. Specifically, estimates can be linked to large health-care utilization databases, providing sufficient statistical power to assess the association between health literacy and various treatment and care services use, as well as endpoint health outcomes. Studies that utilize this methodology may also be able to help address important questions about the relationship between health literacy and population health and health policy issues, which otherwise will not be possible to investigate in smaller-scale research studies that rely upon the individual-level measurement of health literacy.9,11,22,23
Despite the strengths of our approach, there are limitations that should be noted. The community-level health literacy variable is constructed as a mean health literacy estimate for all residents in a US census block group and is therefore unable to differentiate individual literacy skills within a community. Variation in outcomes contributed by between-individual variation within a community may be poorly explained by variation in the community health literacy estimates. Nonetheless, our previous study shows a good agreement between the community-level health literacy estimates and results from individual literacy assessments.9 Additionally, individual patient health beliefs may affect treatment use and care access. Our study did not have measures for individual patient beliefs.
Conclusion
In summary, this study showed notable associations between estimated community-level health literacy and the initiation of OHA and the use of standard preventive care services in a national cohort of older adults with hypertension and newly diagnosed diabetes. This suggests that community health literacy may help to inform targeted diabetes education and support.
Funding Statement
National Institute of Aging R01AG046267 (PIs: Bailey/Fang) supported this work. The findings and conclusions in this paper do not represent the official views or opinions of the National Institute of Aging. The funder was not involved in the design, analysis of interpretation of study findings.
Disclosure
MSW has predoctoral student fellowships funded through Abbvie and Amgen. He has also received grant support from Merck, Sharp & and Dohme, Eli Lilly, UnitedHealthcare, Amgen and AbbVie. MSW has also served as a consultant or advisory board member to Luto UK, Vivus, AbbVie, Abbott Labs, Merck, Pfizer, CVS/Caremark, AB Imbev Foundation, Deborah Adler and OptumHealth. SCB has served as a consultant for Merck, Sharp and Dohme, Pfizer, and Luto UK and has received grant funding via her institution from Eli Lilly and Merck, Sharp and Dohme. SCB has also received personal fees from Northwestern University/Gordon and Betty Moore Foundation. MKP-O has served as a consultant for Communicate Health, Engineered Care, Nous, and Merck. He has also received grant support from OptumHealth. MAB has received grant support from Amgen and AstraZeneca and served as a scientific advisor for RxAnte, Pfizer, Merck, and Amgen. KBF consults with QuiO, a technology adherence company and receives hourly compensation. All other authors have no conflicts of interest to report.
References
- 1.International Diabetes Federation. Diabetes Atlas: The Global Burden. Brussels, Belgium: International Diabetes Federation; 2011. [Google Scholar]
- 2.Centers for Disease Control and Prevention. 2014. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, 2014. Atlanta, GA: US Department of Health and Human Services. [Google Scholar]
- 3.American Diabetes Association. Standards of Medical Care in Diabetes-2016: summary of Revisions. Diabetes Care. 2016;39(S1):S4–S5. doi: 10.2337/dc16-S003 [DOI] [PubMed] [Google Scholar]
- 4.American Diabetes Association. 10. Older adults. Diabetes Care. 2016;39(S1):S81–S85. doi: 10.2337/dc16-S013 [DOI] [PubMed] [Google Scholar]
- 5.Institute of Medicine. Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press; 2014. [Google Scholar]
- 6.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155(2):97–107. doi: 10.7326/0003-4819-155-2-201107190-00005 [DOI] [PubMed] [Google Scholar]
- 7.Bailey SC, Brega AG, Crutchfield TM, et al. Update on health literacy and diabetes. Diabetes Educ. 2014;40(5):581–604. doi: 10.1177/0145721714540220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kutner MA. United States. Department of Education., National Center for Education Statistics. The Health Literacy of America’s Adults: Results from the 2003 National Assessment of Adult Literacy. Washington, DC: United States Department of Education; National Center for Education Statistics; 2006. [Google Scholar]
- 9.Bailey SC, Fang G, Annis IE, O’Conor R, Paasche-Orlow MK, Wolf MS. Health literacy and 30-day hospital readmission after acute myocardial infarction. Br Med Jl Open. 2015;5:e006975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Health Literacy Data Map. US Health Literacy Data Map. Chapel Hill: University of North Carolina at Chapel Hill, 2019. [Google Scholar]
- 11.Martin LT, Ruder T, Escarce JJ, et al. Developing Predictive Models of Health Literacy. J Gen Intern Med. 2014;24(11):1211. doi: 10.1007/s11606-009-1105-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The U.S. Census Bureau. Geographic Terms and Concepts - Block Groups. Census Redistricting Data (Public Law 94–171) Summary File. The U.S. Census Bureau; 2010. Available from: https://www2.census.gov/geo/pdfs/reference/GTC_10.pdf. Accessed December 5, 2019.
- 13.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8 [DOI] [PubMed] [Google Scholar]
- 14.Jensen PN, Johnson K, Floyd J, Heckbert SR, Carnahan R, Dublin S. A systematic review of validated methods for identifying atrial fibrillation using administrative data. Pharmacoepidemiol Drug Saf. 2012;21:141–147. doi: 10.1002/pds.2317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Virnig BA, Shippee ND, O’Donnell B, Zeglin J, Parashuram S. Use of and access to health care by Medicare beneficiaries with diabetes: impact of diabetes type and insulin use, 2007–2011; 2014. [PubMed]
- 16.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083–3107. doi: 10.1002/sim.3697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496–509. doi: 10.1080/01621459.1999.10474144 [DOI] [Google Scholar]
- 18.Lin DY, Wei LJ. The robust inference for the cox proportional hazards model. J Am Stat Assoc. 1989;84(408):1074–1078. doi: 10.1080/01621459.1989.10478874 [DOI] [Google Scholar]
- 19.Gray RJ. A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat. 1988;16(3):1141–1154. doi: 10.1214/aos/1176350951 [DOI] [Google Scholar]
- 20.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090 [DOI] [PubMed] [Google Scholar]
- 21.Area Health Resources Files (AHRF). Health Resources and Services Administration, U.S. Department of Health and Human Services. [Google Scholar]
- 22.Martin LT, Parker RM. Insurance expansion and health literacy. J Am Med Assoc. 2011;306(8):874–875. doi: 10.1001/jama.2011.1212 [DOI] [PubMed] [Google Scholar]
- 23.Lurie N, Martin LT, Ruder T, et al. Estimating and Mapping Health Literacy in the State of Missouri Rand Health. Santa Monica, CA: RAND Corporation; 2010. Available from: https://www.rand.org/pubs/working_papers/WR735.html. [Google Scholar]