Abstract
Introduction
Pectoralis myocutaneous flap remains the workhorse for the reconstruction of large defects in the head and neck region despite free flaps gaining popularity; because of its drawbacks such as long operating hours, high cost and special skill techniques, it is not used in most of the institutions. Even in our institution, free tissue transfers are carried out on a regular basis, but there is a definite scope and role for PMMC flap in reconstruction. We present our experience with pectoralis major myocutaneous flap in terms of postoperative complications, donor site morbidity, flap survival and long-term healing of the flap.
Materials and methods
In this study, 150 patients who underwent pectoralis myocutaneous flap reconstruction from 2008 to 2016 were analysed for postoperative complications like donor site morbidity, flap survival and long-term healing of the flap.
Results
On analysis of our data, it was found that the most common complication was wound dehiscence, which was seen in 25 patients(16%), followed by orocutaneous fistula in 15 (10%), wound infection and partial skin margin necrosis, which was seen in a maximum of 12 each(8%), hematoma in 5 (3%), and donor site wound dehiscence in 5 (3%), and there was no case of total flap failure or carotid blowout.
Discussion
We conclude that PMMC flap along with its modifications is the most cost-effective and associated with least complications.
Keywords: PMMC flap, Reconstruction of oral cavity, Complications of PMMC flap, Cancer, Pectoralis major myocutaneous flap
Introduction
Oral cavity plays an important role in an individual’s life as it forms an integral part during the speech, deglutition, respiration and cosmesis. Malignancy of head and neck region is a threat that is increasing day by day because of tobacco and alcohol abuse. Majority of patients present with an advance disease stage because of which aggressive resection is used leading to large postablative defects that result in significant functional and aesthetic problems [1, 2]. Reconstruction of these defects should aim to restore near normal form and function in individuals.
Composite defects of the head and neck region after aggressive resection require reconstruction of several layers, including the intraoral lining, osseous reconstruction of the mandible or maxilla and soft tissue/skin coverage. Free flaps are now considered as “gold standard” for reconstruction of post-resection defects [3]. The utility of pectoralis major myocutaneous flap (PMMC) still exists in advanced diseases with systemic co-morbidities and compromised vessel calibre which prevents use of free flaps.
Before the introduction of free vascularized flap, the pectoralis major myocutaneous flap (PMMC) was the flap of choice for reconstruction of head and neck defects. It was introduced by Ariyan in 1980 and described as “Workhorse Flap.” It offers head and neck reconstructive surgeons a single-stage reconstruction technique with minimal donor site morbidities, satisfactory cosmetic results and well-vascularized tissue bulk that can fill up the maxillofacial post-surgical defects with the added advantage of covering the vital structure of the neck. Due to its robust vascularity and easy learning curve for surgeons, it is still a workhorse at centres with limited resources and heavy patient load [4].
The PMMC flap is classified as type 5 flap based on the classification system given by Mathes and Nahai which has a sole principal pedicle and accessory segmental vascular pedicles. The vascularity of the pectoralis major flap is usually consistent with the pedicle positioned between clearly defined tissue planes and supplied by numerous perforators for skin.
Although the medical literature has got plenty of publications associated with PMMC flap, only few of them have covered the complications related to the flap. With the present study, we have done the critical analysis of all the flap-related complications and also we present our experience with PMMC flap.
Materials and Methods
Clinical records of 160 patients who underwent the pectoralis major myocutaneous flap reconstruction between the year 2008–2016 at SDM craniofacial surgery and research centre were screened. The study was cleared for publication from institutional review board. Inclusion criteria for the study were patients operated for malignancy of the oral cavity whose 1-year follow-up data were available. Out of these, 10 patients were excluded from the study because of lack of medical records and patient follow-up and only 150 patients were included in the study. The age of patients in this series ranged between 30 to 60 years.
Parameters included in our study were post-operative complications in terms of (1) flap necrosis immediate post-operative, (2) wound infection during hospital stay, (3) wound dehiscence in immediate post-operative period and (4) status of PMMC flap after 1 year.
Technique of Flap Harvesting
The flap design and the skin island were dependent on the site, size and shape of the defects with the skin island being usually below and medial to the nipple about the level of the 6th rib. The vascular axis marking was done on chest; a line from shoulder tip to xiphoid process was drawn.
The vascular pedicle was situated along this line coming at right angle from mid clavicle and meeting xiphoid acromial line. The paddle of skin was marked over this pedicle. The flap elevation was started from a distal to a proximal direction. The perfusion of the sources of the flap is the pectoral branch of the acromiothoracic artery and the lateral thoracic artery which was identified between major and minor muscles. During the flap elevation, the pectoral fascia and the muscle were secured to the skin to protect the perforator vessels and the muscle was exposed over the length and the breadth of the pedicle and lignocaine without the preservative was sprayed for vasodilatation of the pedicle during manipulation. The pectoral nerve was sacrificed. The skin and muscle were elevated from the chest wall exposing the ribs and the intercostals muscles. The flap was elevated up as far as the coracoid process where the pedicle was narrowed. The lateral pectoral vessels were left intact or divided depending on the volume of the flap required and the tension produced if the vessels were left intact (Fig. 1). To increase the arc of rotation and reach of the flap, deltoid muscle fibres overlying the pedicle was debulked.
Fig. 1.
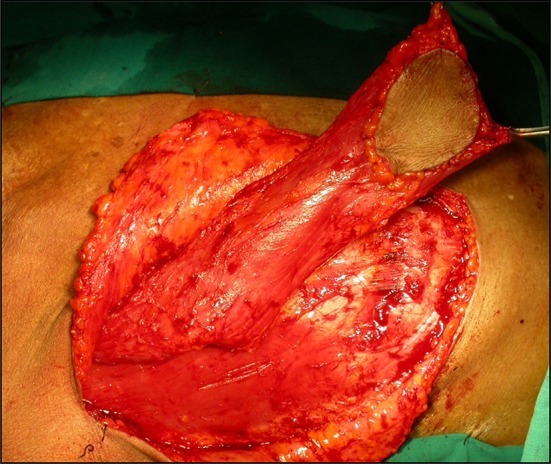
Flap raised intraoperatively
Results
On assessment of the collected data, it was found that amongst 150 patients 103 were males and 47 females, between age group of 30–60 years with mean age of patients at the time of surgery as 52.5 years. Main complaint of patients in our study was painful ulcer in 54% cases followed by trismus in 26% cases and pain with swelling in 20% cases. All patients had biopsy proven malignancy of oral cavity, and resection of primary lesion was performed along with reconstruction with PMMC flap. Majority of cases showed squamous cell carcinoma involving gingivobuccal complex (51%) (Fig. 2) followed by malignancy of the retromolar region (18%), floor of mouth (15%) and tongue (9%). History of tobacco consumption in smokeless form with and without smoking was present in 95% of cases.
Fig. 2.

Preoperative intraoral view involving gingivobuccal sulcus
Most of the patients were having advanced disease that is 54.6% and 45.3% in stage 3 and stage 4, respectively. Out of 150 patients, 96 patients underwent hemimandibulectomy, 27 underwent bite excision (hemimandibulectomy plus ipsilateral maxillary segmental resection), 15 underwent marginal mandibulectomy, and 12 underwent segmental resection in which the mandibular continuity was maintained with reconstruction plate and soft tissue defect was closed with PMMC flap. Lymph nodes were palpable clinically in 68% cases out of which 39% had N2b status, 16% had N2a, and 13% had N1 status. In our study, 96% (144 cases) of patients with cervical nodes were managed with modified radical neck dissection with preservation of spinal accessory nerve and internal jugular vein, while remaining patients underwent RND. Ten per cent (15 patients) were managed with bilateral neck dissection with MRND on ipsilateral side and SOHND on contralateral side. Average number of hospital stay in our study was 12 days (Table 1).
Table 1.
Gender distribution, primary site, type of resection, type of neck dissection, complications in study
| Number | Percentage | |
|---|---|---|
| Gender distribution | ||
| Male | 103 | 68.6 |
| Female | 47 | 31.3 |
| Site | ||
| Gingivobuccal complex | 76 | 51 |
| Retromolar region | 28 | 18.8 |
| Floor of mouth | 27 | 18 |
| Tongue | 19 | 12.6 |
| Type of resection | ||
| Hemimandibulectomy | 96 | 64 |
| Bite excision | 27 | 18 |
| Marginal mandibulectomy | 15 | 10 |
| Segmental resection | 12 | 8 |
| Type of neck dissection | ||
| Modified radical neck dissection | 144 | 96 |
| Radical neck dissection | 6 | 4 |
| Bilateral neck dissection—SOHND | 15 | 10 |
We also noted that amongst 150 patients there were 11 patients who underwent free flaps as preliminary procedure for reconstruction, but due to complete flap necrosis, PMMC flap was used as salvage procedure.
On analysis of our data, we found the most common post-operative complication to be wound dehiscence which was seen in 25 patients (16%), orocutaneous fistula in 15 (10%) followed by wound infection and partial skin margin necrosis which was seen in maximum of 12 each (8%), haematoma in 5 (3%), donor site wound dehiscence in 5 (3%). There was no case of total flap failure in present case series.
Out of 150 patients, 128 patients underwent radiotherapy two to three weeks post-operatively as per the indications and remaining 22 patients refused to undergo radiotherapy because of financial constraints. A total of 128 patients tolerated radiotherapy with minimal toxicity, and there was no evidence of flap necrosis in the neck, nor any case of carotid blow out.
Discussion
Pectoralis major myocutaneous flap is one of the most versatile flaps available and workhorse for reconstruction of head and neck defects. This flap has now replaced other large regional cutaneous flaps because of its inherent properties. Different authors have given different complication rates in relation to PMMC flap, but due to factors like small number of sample size, lack of detailed analysis of result exact status of this flap is still not available; our study has included all complications we have encountered and possible reasons causing them.
Free flaps have distinctive advantages over pedicled flap like better cosmetic results, less bulk of the flap and better rehabilitation although one important finding that we noted in present study is the ability of the PMMC flap to be used as salvage procedure after failure of free flaps. In present study, there were 7.33% patients (11 patients) who underwent salvage procedure after failure of free flaps; these findings suggested that PMMC flap forms an important tool in cases where use of vascularised flaps is not possible or in patients with vessels abnormalities, extremes of ages, patients with medical co-morbidities (Fig. 3). Also PMMC flap as stated above is final backup plan in cases of free flaps failure because it is more cost-effective in patients with poor socio-economic status who are common in developing countries. Same results were reflected by Schneider et al. [5] who stated PMMC flap was used as salvage procedure in 38% of their case series and another study done by Saito et al. [6] stated that 75% of cases operated for PMMC flaps were only used as salvage procedure supporting our findings.
Fig. 3.

Postoperative intraoral view of flap
Wound Dehiscence (Fig. 4)
Fig. 4.

Wound dehiscence in postoperative period
In our study, we noted total complication rate of 49% with wound dehiscence as the most common complication (16%) for which no other secondary surgical procedure was required and it healed with secondary healing. El-Marakby [7] concluded that the high incidence of dehiscence and orocutaneous fistulas was due to the fact that their case series included defects of oral cavity and pharyngeal oesophageal junction, but in our study all the patients had primarily oral defects and no conclusion could be drawn due to lack of comparison like in above-mentioned study.
Although on detailed analysis of our results we can state that the incidence of wound dehiscence was noted in patients with Schobinger incision when compared to MacFee incision as trifurcation area in Schobinger is a weak zone with the placement of bulk of PMMC flap. Wound dehiscence can also be prevented by avoiding over tight closure of wound that can lead to reduced blood supply of skin margins, and subsequently, dehiscence also post-operative regular dressing of sutured margins is pivotal in preventing as well as managing wound dehiscence at neck region. We also noted that amongst the 25 patients presenting with wound dehiscence 11 patients had undergone segmental resection, indicating that continuity defect predisposes the flap to wound breakdown in between 5th to 7th post-operative day although this correlation needs to be further investigated before any final conclusion could be drawn.
Re Exploration for Haematoma
Second surgical procedure in our study was done in 3% (5 patients) of cases for re exploration of operated site for evacuation of haematoma from the neck in 4 patients and 1 in chest. Most of these haematoma collection occurred between 12 to 36 h after surgery in majority of these patients. Although there was no definite bleeder in the neck upon exploration, in the chest one of the patients developed bleeding from intercostal perforator. Hence, it is advisable to ligate the 3–4 intercostal perforators which are encountered during the harvesting of the flap rather than cauterising bleeder. It was noted that number of hospital stay increased to about 14 days when second surgical procedure was done. A retrospective study done by Shah et al. [8] in which complications of 211 patients were presented further concluded that there were total of 63% flap-related complications including infection, dehiscence, haematoma, orocutaneous fistulas, flap necrosis. They stated that in their case series 6 patients required second surgical procedure for evacuation of haematoma.
Flap Failure
In a study done by Sharma et al. [2], total complication rates of 63% were noted out of which dehiscence was noted in 27% cases, infection in 23% cases, partial flap necrosis in 3% cases. In the present study, no case of total flap necrosis was noted, but a study done by El-Marakby [7] reported 8% cases of total flap necrosis amongst 25 patients. Also another study done by Baek et al. [9] in 1982 reported incidence of total flap necrosis in their 1.5% cases. This contrasting difference between other studies and present study can be attributed by careful handling of pedicle, use of vasodilator, avoiding kinking of vascular pedicle and avoiding closure of the flap under tension by prior planning for proper reconstruction.
Infections (Fig. 5)
Fig. 5.

Stich abscess around the suture line
In present study, 8% (12 patients) had wound infection presenting either with stitch abscess or pus discharge from wound dehiscence as compared to a study by El-Marakby [7]; 20% (5 patients) had wound infection. In our scenario, out of 12 patients who presented with wound infection 7 patients had diabetes mellitus, which could be a contributing factor for wound infection; these cases were managed conservatively with regular dressing and by controlling blood sugar levels within normal range post-operatively. No additional surgical procedure was required.
Donor Site Wound Dehiscence
One of the rare complications reported about PMMC flap is costal osteomyelitis [10] which was later managed by vertical rectus abdominis myocutaneous flap. In the present study, no such rare major complications were seen related to donor sites except few cases of minor dehiscence (5 in number) which were managed conservatively without any surgical intervention.
One of the most important advantages of PMMC flap is its ability to be used for reconstruction of through-and-through defect, while avoiding intricacy of free flaps, this is possible with use of bilobed flap by dividing the skin in two parts for extraoral and intraoral lining both.
In a study done by Bhola et al. [11] where after resection of oral cancer, 62 cases of through-and-through defects of the oral cavity were reconstructed using bilobed PMMC flap. They concluded with results that all the flaps survived, and no patient developed a major complication. The most common complication in the current series was wound dehiscence. The bilobed/bipaddled PMMC flap is a straightforward and reliable flap that provides an effective mechanism to reconstruct full-thickness cheek defects [12]. Another modification of PMMC flap was given by Chaturvedi and Joshi [13] in which partial bipaddling of the flap leaving an island of intact skin to form lip commissure was done. They concluded that this technique reduces oral incompetence without compromising on the adequacy of mouth opening.
We have also noted on 1-year follow-up of all patients that skin surface of PMMC flap used to reconstruct oral cavity exhibited desquamative changes indicating mucosalization of flap, although these changes were patchy rather than continuous. These changes on the surface of flap suggested adaptive changes of skin according to the oral environment. A study done by Wei et al. [14] in which histological examination was done in 112 patients who were operated for malignancy of oral cavity and reconstructed with PMMC flap, reported changes of skin in oral cavity especially in areas exposed to increased friction like floor of mouth.
One disadvantage of the PMMC flap that we encountered in our study was bulky nature of the flap that gave the patient oedematous appearance affecting the patient’s satisfaction in the early post-operative period, but it was observed in our study that during 3–6-month follow-up period there was gross reduction/shrinkage of muscle bulk due to sacrifice of pectoral nerve while harvesting flap and other reason being radiotherapy.
As already mentioned above in present study after radiotherapy, there was no evidence of carotid blow out; the reason is bulk of PMMC flap which acts as protective barrier for major vessels of neck during and after radiotherapy. The incidence of carotid blow out as per different authors ranges from 2.6% to 25% in head and neck irradiated region [15, 16]. In a comparative study done by Sabra et al. [17] to assess the effectiveness of pectoralis major muscle flap in prevention of fistula formation and protection against catastrophic vascular blowouts concluded that when closure of defect was done by PMMC flap there was no case of carotid blow out as compared to 25% incidence of carotid blow out in cases where primary closure was achieved.
One major disadvantage of this flap as described in literature is unaesthetic results in women due to distortion and asymmetry following reconstruction; in our study none of the patients male/female complained about this post-operative scar over the chest as all the patients were counselled about the need to treat the disease aggressively and importance of disease-free survival.
There are many advantages of PMMC flap relating to its versatility and viability due to abundant blood supply. The larger skin defects can be closed along with the primary closure of the donor site. Pectoralis major myocutaneous flap with all its advantages like versatility, local availability, ease of harvesting, excellent blood supply with reliable pedicle, with very good reach to all the corners of oral cavity and with minimal morbidity forms still remains workhorse for reconstruction of oral cavity defects.
Conclusion
We conclude that PMMC flap along with its modifications is the most cost-effective and reliable method of reconstruction in head and neck surgery.
There are many advantages of PMMC flap relating to its versatility and viability due to abundant blood supply.
Pectoralis major myocutaneous flap with all its advantages like versatility, local availability, ease of harvesting, excellent blood supply with reliable pedicle, with very good reach to all the corners of oral cavity and with minimal morbidity forms still remains workhorse for reconstruction of oral cavity defects.
Acknowledgement
Authors would like to thanks Dr. Srinath Thakur, Principal, SDM college of dental sciences Dharwad and Dr. Niranjan Kumar, Medical Director, SDM craniofacial research centre Dharwad for the encouragement and facilities provided.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Compliance with Ethical Standards
Conflict of interest
Authors would like to declare there is no funding from institution or commercial company with regard to this study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Venkatesh Anehosur, Email: venkyrao12@yahoo.co.in.
Punit S. Dikhit, Email: dikhit.punit@gmail.com
References
- 1.Ariyan S. Further experiences with the pectoralis major myocutaneous flap for the immediate repair of defects from excisions of head and neck cancers. Plast Reconstr Surg. 1979;64(5):605–612. doi: 10.1097/00006534-197911000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Sharma S, Murty P, Hazarika P, Nayak D, Sharma S. The indications and complications of pectoralis major myocutaneous flap reconstruction in head and neck surgery-our experience. Indian J Otolaryngol Head Neck Surg. 1998;50(4):362–367. doi: 10.1007/bf03000688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pinto F, Malena C, Vanni C, Capelli F, Matos L, Kanda J. Pectoralis major myocutaneous flaps for head and neck reconstruction: factors influencing occurrences of complications and the final outcome. Sao Paulo Med J. 2010;128(6):336–341. doi: 10.1590/s1516-31802010000600005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tripathi M, Parshad S, Karwasra R, Singh V. Pectoralis major myocutaneous flap in head and neck reconstruction: an experience in 100 consecutive cases. Natl J Maxillofac Surg. 2015;6(1):37. doi: 10.4103/0975-5950.168225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schneider D, Wu V, Wax M. Indications for pedicled pectoralis major flap in a free tissue transfer practice. Head Neck. 2011;34(8):1106–1110. doi: 10.1002/hed.21868. [DOI] [PubMed] [Google Scholar]
- 6.Saito A, Minakawa H, Saito N, Nagahashi T. Indications and outcomes for pedicled pectoralis major myocutaneous flaps at a primary microvascular head and neck reconstructive center. Mod Plast Surg. 2012;02(04):103–107. doi: 10.4236/mps.2012.24025. [DOI] [Google Scholar]
- 7.El Marakby H. The reliability of pectoralis major myocutaneous flap in head and neck reconstruction. J Egypt Natl Canc Inst. 2006;18(1):41–50. [PubMed] [Google Scholar]
- 8.Shah J, Haribhakti V, Loree T, Sutaria P. Complications of pectoralis major myocutaneous flap in head and neck reconstruction. Am J Surg. 1990;160:352–355. doi: 10.1016/s0002-9610(05)80541-0. [DOI] [PubMed] [Google Scholar]
- 9.Baek S, Lawson W, Biller H. An analysis of 133 pectoralis major myocutaneous flaps. Plast Reconstr Surg. 1982;69(3):460–467. doi: 10.1097/00006534-198203000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Nagarjuna M, Patil B, Nagraj N, Gopalkrishnan K. Use of superiorly based vertical rectus abdominis myocutaneous flap for the correction of costal osteomyelitis at the pectoralis major myocutaneous flap donor site. J Oral Maxillofac Surg. 2013;71(2):e132–e136. doi: 10.1016/j.joms.2012.10.011. [DOI] [PubMed] [Google Scholar]
- 11.Bhola N, Jadhav A, Borle R, Khemka G, Kumar S, Shrivastava H. Is there still a role for bilobed/bipaddled pectoralis major myocutaneous flap for single- stage immediate reconstruction of post ablative oncologic full-thickness defects of the cheek? Oral Maxillofac Surg. 2014;19(2):125–131. doi: 10.1007/s10006-014-0458-1. [DOI] [PubMed] [Google Scholar]
- 12.Deo S, Purkayastha J, Diganta DL, Kar M, Srinivas G, Asthana S, Shridhar D, Shukla NK. Reconstruction of complex oral defects using bi-paddle pectoralis major flap-technical modifications and outcome in 54 cancer patients. Indian J Otolaryngol Head Neck Surg. 2003;55(1):5–9. doi: 10.1007/bf02968744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chaturvedi P, Joshi P. Partial Bipaddling of PMMC flap in full thickness cheek defects involving lip commissure: a novel technique. Int J Head Neck Surg. 2013;4:113–114. doi: 10.5005/jp-journals-10001-1155. [DOI] [Google Scholar]
- 14.Wei W, Lam K, Lau W. Fate of skin element of pectoralis major flap in intraoral reconstruction. Arch Otolaryngol Head Neck Surg. 1989;115(3):360–363. doi: 10.1001/archotol.1989.01860270102022. [DOI] [PubMed] [Google Scholar]
- 15.Chen Y, Wang C, Wang C, Jiang R, Lin J, Liu S. Carotid blowout in patients with head and neck cancer: associated factors and treatment outcomes. Head Neck. 2014;37(2):265–272. doi: 10.1002/hed.23590. [DOI] [PubMed] [Google Scholar]
- 16.McDonald M, Moore M, Johnstone P. Risk of carotid blowout after reirradiation of the head and neck: a systematic review. Int J Radiat Oncol Biol Phys. 2012;82(3):1083–1089. doi: 10.1016/j.ijrobp.2010.08.029. [DOI] [PubMed] [Google Scholar]
- 17.Sabra R, Taha M, Hamdy T, Rabie H, Riad M. Pectoralis major flap reconstruction in the prevention of wound breakdown and fistula formation after salvage laryngectomy: a controlled study. Egypt J Otolaryngol. 2016;32(1):32. doi: 10.4103/1012-5574.175803. [DOI] [Google Scholar]


