Abstract
Introduction
Identification of detailed anatomy of mandibular canal (MC) with its contents including the position, course, and morphology is extremely important for the management of various surgical procedures including dental implant placement, third molar surgery, dental anesthesia, mandibular osteotomy, bone-harvesting procedure from the ramus and body of mandible, bone plating in angle and body region of mandible, or any other surgical procedure involving the mandible.
Methods
This prospective randomized study was carried out in the Department of Oral and Maxillofacial Surgery, Saraswati Dental College, Lucknow, on 100 randomly selected cone-beam computed tomography (CBCT) mandibular views displaying the entire mandible.
Results
Various parameters of the canal were studied in detail and subjected to statistical analysis using SPSS 20 software. For all the observations, paired t test was applied to compare right and left sides and independent t test for the comparison of gender.
Conclusion
For centuries MC has been a paramount topic of discussion, and with the contraption of CBCT, we can finally decipher the canal in great detail. CBCT acts as a guide to prevent damage to the neurovascular bundle as the canal traverses its course and sometimes with certain variations.
Keywords: Mandibular canal, Inferior alveolar neurovascular bundle, CBCT, Variations
Introduction
The mandibular canal (MC) is an imperative anatomical structure which has been studied in detail since ages with respect to its location and path as well as the possible variations in normal anatomy since it can have diverse configurations. The anatomy of MC comprises an extension from the mandibular foramen to the mental foramen bilaterally, carrying the inferior alveolar nerve, artery, and vein. Certain variations in the anatomy of mandibular canal and its course are not uncommon [1]. Acquaintance with the morphology and topography of the inferior alveolar neurovascular bundle is essential for various surgical procedures including dental implant placement, third molar surgery, dental anesthesia, mandibular osteotomy, bone-harvesting procedure from the ramus and body of mandible, bone plating in angle and body region of mandible, or any other surgical procedure involving the mandible [2, 3].
The presence of bifid/trifid canals, anterior loop of mental nerve, and its anterior extensions lack explicit definitions. So, a radiographic examination with superior image quality becomes essential. In oral and maxillofacial surgery, routinely IOPAs, OPG, MRI, and CT form the mainstream of diagnostic tools. CBCT machine which produces superior image quality with 1:1 measurement and 3D display has added further dimension to the diagnosis and treatment planning. If proper preoperative evaluation is not carried out, there can be failure in anesthetic techniques, and patients can also suffer from hemorrhagic complications and paresthesia [4]. Lack of clear definitions in the literature, wider availability of three-dimensional imaging, and increased demand of implant surgeries indicate that features of mandibular canal should be revisited. This holistic study focuses on diverse parameters in respect to the mandibular canal in different regions done exclusively in Indian population using CBCT. Review of the literature suggests that such studies have been not carried out earlier with this wide spectrum especially in Indian inhabitants.
Materials and Method
This prospective randomized study was carried out in the Department of Oral and Maxillofacial Surgery, Saraswati Dental College, Lucknow, on 100 randomly selected CBCT mandibular views displaying the entire mandible. i-CAT CBCT machine using i-CAT CB 500 (GENDEX) cone-beam 3D imaging system with high resolution (0.125/0.2 mm voxel), standard pulsed exposure with acquisition time of 23 s (exposure time 8–10 s) and 12.6 s (exposure time 8–9 s), tube voltage (270 kV and 10–15 mA), field of view (14 × 6 cm and 8.5 × 6 cm) and (0.125 × 0.125 × 0.125 mm3) spherical imaging volume was used in the study, and parameters were recorded in millimeters.
Following parameters were assessed on CBCT:
Diameter of the MC
Length of the MC
-
Location of the MC
Horizontal plane—(distance of the outer margin of the canal)-
(i)from buccal cortical plate
-
(ii)from lingual cortical plate
Vertical plane—(distance of the outer margin of the canal)-
(i)from crestal bone level
-
(ii)from base of mandible
-
(i)
- Relationship of mandibular roots to the MC
-
(i)distance
-
(ii)position
-
(i)
Length of the anterior loop of the mental nerve
Bifid/trifid canals
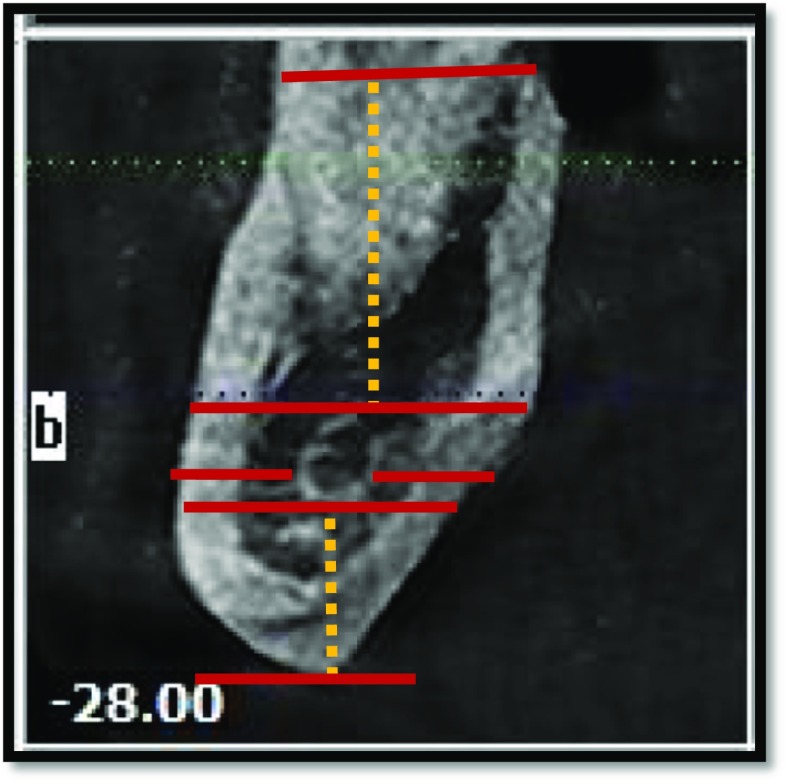
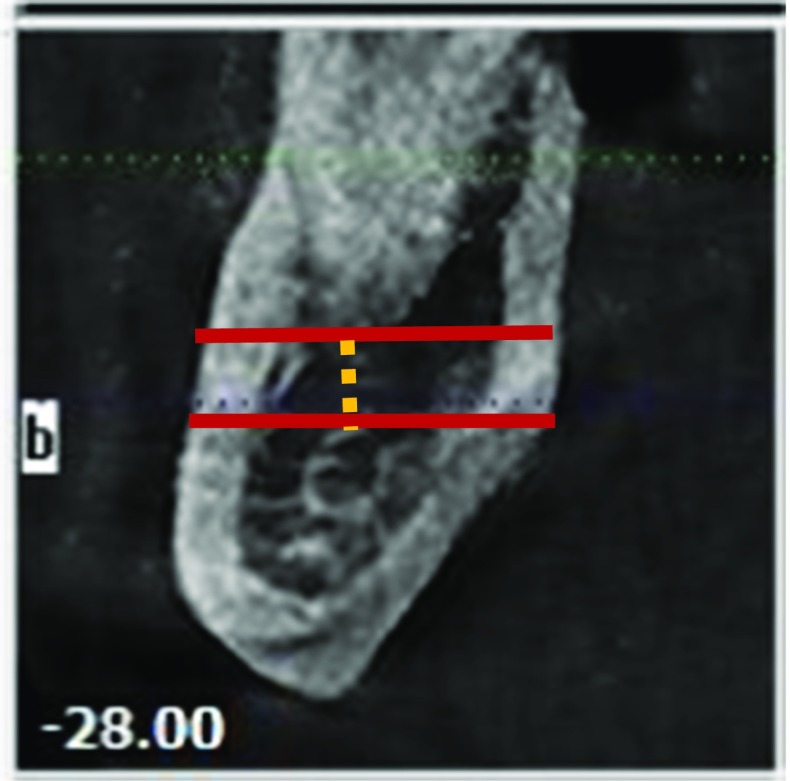
Diameter of the MC
The inner maximum vertical and horizontal diameters were measured in coronal plane (cross section in each tooth region). In multi-rooted tooth, the diameter was measured in relation to each root, and the final value was the mean of the measurements taken (Fig. 1).
Fig. 1.
Measurement of maximum vertical and horizontal diameters
Length of the MC
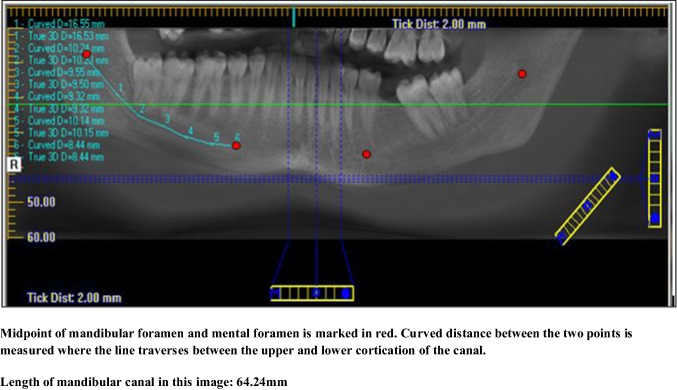
The length of the MC was assessed in the panoramic view after locating a midpoint in the mandibular and mental foramen region and measured along the line traversing between the two points in the midline between upper and lower cortication of the canal (Fig. 2).
Fig. 2.
Measurement of length of mandibular canal
Location of the MC
The distance from the outermost margin of the MC to the buccal cortical plate, lingual cortical plate, crestal bone level, and inferior border of mandible was measured (Fig. 3).
Fig. 3.
Measurement of the distance of mandibular canal from the crestal bone level, inferior border of mandible, buccal, and lingual cortical plate
Relationship of the Roots to the MC
The distance of the roots from the upper margin of the MC was measured in the cross section. In multi-rooted tooth, the distance was measured in relation to each root, and the final value was the mean of the measurements taken (Fig. 4).
Fig. 4.
Measurement of the distance between the root tip and upper border of the mandibular canal
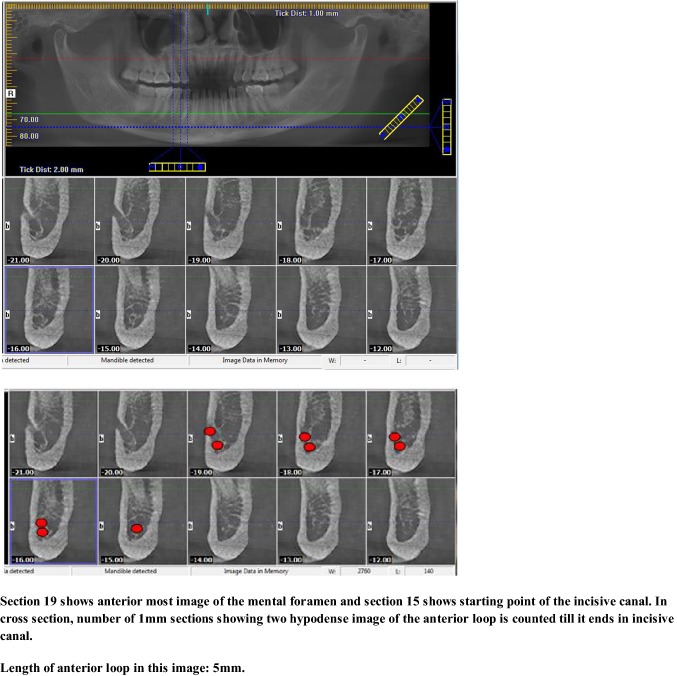
Anterior Loop of the Mental Nerve
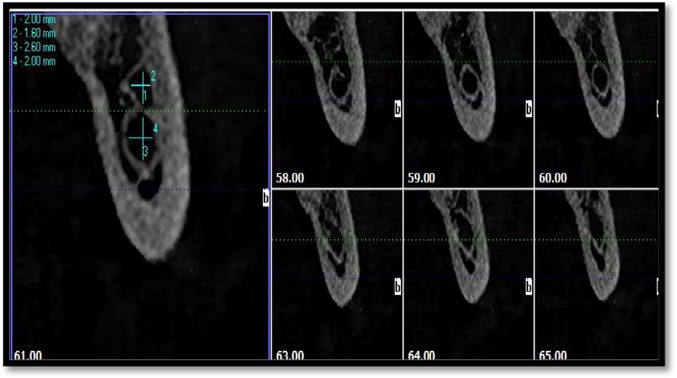
For the cross sections, the anterior loop was determined by counting the number of sequential 1-mm slices displaying two round hypodense images (corresponding to the upper and lower segments of the MC, typically ending in an “8-like” shape anteriorly), from the anterior-most image of the mental foramen and starting point of the incisive canal (Fig. 5).
Fig. 5.
Measurement of the anterior loop
Bifid/trifid Canal
Axial, coronal, sagittal, cross sections, and volume rendering were viewed to assess bifid MC (Fig. 6).
Fig. 6.
Assessment of bifid canal
The results were subjected to statistical analysis using SPSS 20 software. For all the observations, paired t test was applied to compare right and left sides, and independent t test was used for the comparison of the gender.
Results
A total of 100 patients comprising 47 female patients with the mean age of 41.85 ± 14.363 and 53 male patients with the mean age of 40.96 ± 14.771 were included in the study. Comparing the mean age between two genders (independent t test), no statistical significance was found with a p value of 0.762, the level of significance being p value < 0.05.
The inner vertical diameter of the MC on right and left side was found to be maximum in third molar region which gradually decreased till first premolar region. The inner vertical diameter in each tooth region was found to be more than the inner horizontal diameter, suggestive of oval to round shape of the MC (Table 1).
Table 1.
Inner diameter of the mandibular canal in different regions (in mm)
| Third molar | Second molar | First molar | Second premolar | First premolar | |
|---|---|---|---|---|---|
| Right vertical (RV) | 2.5927 | 2.4877 | 2.4362 | 2.2189 | 1.931 |
| Right horizontal (RH) | 2.259 | 2.2435 | 2.3204 | 2.0875 | 1.7462 |
| Left vertical (LV) | 2.7167 | 2.5269 | 2.3718 | 2.1369 | 1.746 |
| Left horizontal (LH) | 2.304 | 2.2622 | 2.2972 | 2.065 | 1.675 |
The length of the MC on right side was in the range of (50.63–78.55 mm) with mean value being 65.175 ± 5.578 mm, while on left side it was in the range of (49.84–78.73 mm) with mean value being 66.039 ± 5.753 mm (Table 2).
Table 2.
Length of the mandibular canal (in mm)
| Mean | SD | Maximum | Minimum | |
|---|---|---|---|---|
| Length right (R) | 65.7155 | 5.5783 | 78.5500 | 50.6300 |
| Length left (L) | 66.0395 | 5.7536 | 78.7300 | 49.8400 |
The location of the MC was found to be close to lingual cortical plate in third molar, second molar, and first molar region, while it was close to the buccal cortical plate in second premolar and first premolar region, suggesting S-shaped topography of the canal in horizontal plane. Also, the distance of the MC from the crestal bone level and inferior border of mandible in various regions was suggestive of catenary course of the canal meaning “curled as hanging between two points” as mentioned by Ozturk et al. [5] (Table 3).
Table 3.
Location of the mandibular canal (in mm)
| Third molar | Second molar | First molar | Second premolar | First premolar | |
|---|---|---|---|---|---|
| Right horizontal distance from buccal cortical plate (RHB) | 4.2514 | 5.0238 | 4.5526 | 2.0954 | 1.8846 |
| Right horizontal distance from lingual cortical plate (RHL) | 1.8277 | 1.8314 | 2.1834 | 4.6632 | 4.7769 |
| Right vertical distance from crestal bone level (RVC) | 13.9243 | 14.3786 | 14.5946 | 14.3166 | 14.3092 |
| Right vertical distance from inferior border of mandible (RVIB) | 6.793 | 6.3579 | 6.0643 | 7.0266 | 8.0077 |
| Left horizontal distance from buccal cortical plate (LHB) | 4.4112 | 5.3317 | 4.6192 | 2.1262 | 2.523 |
| Left horizontal distance from lingual cortical plate (LHL) | 1.8118 | 1.798 | 2.1064 | 4.7722 | 4.7063 |
| Left vertical distance from crestal bone level (LVC) | 13.9955 | 14.1443 | 14.6273 | 14.1852 | 15.0812 |
| Left vertical distance from inferior border of mandible (LVIB) | 7.0688 | 6.1974 | 6.1331 | 7.7139 | 8.3625 |
The roots of the mandibular third molar on right and left side was found in closest relationship to the MC, while the distance gradually increased till first molar region where it was found to be maximum on both sides (Table 4).
Table 4.
Relationship of roots to the mandibular canal (in mm)
| Third molar | Second molar | First molar | Second premolar | First premolar | |
|---|---|---|---|---|---|
| Relationship of roots to canal R | 1.7449 | 3.4568 | 4.2354 | 2.7691 | 2.422 |
| Relationship of roots to canal L | 1.5173 | 3.0274 | 3.7115 | 2.762 | 2.8693 |
Anterior loop was found in 20% of the cases on both sides. A total of 18 cases (18%) of bilateral anterior loop and four cases (4%) (2 each on right and left side) of unilateral anterior loop were found (Tables 5, 6).
Table 5.
Anterior loop of mandibular canal—right side (in mm)
| Length of the anterior loop | Number of cases | Valid percent |
|---|---|---|
| 2 | 4 | 20 |
| 3 | 6 | 30 |
| 4 | 5 | 25 |
| 5 | 3 | 15 |
| 6 | 1 | 5 |
| 9 | 1 | 5 |
| Total | 20 | 100 |
Table 6.
Anterior loop of mandibular canal—left side (in mm)
| Length of the anterior loop | Number of cases | Valid percent |
|---|---|---|
| 2 | 6 | 30 |
| 3 | 4 | 20 |
| 4 | 8 | 40 |
| 5 | 2 | 10 |
| Total | 20 | 100 |
Out of 100 CBCT, one case (1%) of bilateral bifid canal was found which was type 2 bifid (bifid within body of mandible) according to Langlais’ classification of bifid MC [21]. The canal divided supero-inferiorly in the first molar region bilaterally and rejoined in the first premolar region, terminating at single mental foramen.
Discussion
Diameter of the MC
In our study, the mean vertical and horizontal diameter of the MC was found to be 2.326 mm and 2.131 mm, respectively, on right side and 2.289 mm and 2.120 mm, respectively, on left side. The difference in the dimensions between two sides was not statistically significant. Our findings co-relate with that of other authors as well [6–9].
Length of the MC
On comparison of the mean values of length on both sides, the mean value on left side was higher with a difference of 0.324 mm which was statistically not significant with a p value of 0.223.
Location of the MC
The anatomic features of the ascent of the canal as well as its buccolingual relationships have been studied extensively [10, 11]. It has been reported by various authors that MC might have different anatomic configurations in the horizontal plane also. Buccolingual orientation is an important parameter which should be analyzed prior to surgical procedures. In our study, the location of the MC was found to be close to lingual cortical plate in third molar, second molar, first molar region, while it was close to the buccal cortical plate in second premolar and first premolar region. Usually, the MC crosses from the lingual to the buccal side of the mandible, and in most cases, midway between the buccal and lingual cortical plates of bone is in the region of first molar [12–14]. Also, the canal was found to be at a mean distance of 4.331 mm from the lateral aspect of the buccal cortical plate and 1.819 mm from medial aspect of the lingual cortical plate in the third molar region. Our findings co-relate with other authors as well [7, 15, 16]. The clinical implication of the location of the MC is that the orientation of the neurovascular bundle should be ascertained pre-operatively in order to avoid inadvertent injury to the neurovascular bundle in case of anatomical variation buccolingually.
Relationship of the Roots to the MC
In our study, the MC was found to be in closest relationship with the roots of third molar followed by second premolar, second molar, and first molar with a mean distance of 1.630 mm, 2.765 mm, 3.241 mm, and 3.973 mm, respectively. Similar findings were observed by other authors [17].
Anterior Loop
In our study, the anterior loop was found in 20% (20 of 100) cases with length ranging between 2 and 9 mm and mean value of 3.55 mm. Similar findings have been reported by other authors [18–20].
A safe guideline of 4 mm, from the most anterior point of the MF, is recommended for implant treatment planning based upon the anatomical findings. There is a wide variation in the incidence and length of the anterior loop, and these studies indicate that sufficient data are not available to draw a definitive conclusion. Studies on larger sample size in diverse population need to be done to characterize this parameter.
Bifid Canal
There can be variation in the number of canals as well. In our study, the canal divided in the first molar region bilaterally and rejoined in the first premolar region, terminating at the mental foramen. The incidence (1%) correlates with findings of other authors as well [21–23]. The clinical significance of this lies in the fact that diagnostic errors in interpreting a bifid MC on OPG may be attributed to superimposition of structures, inadequate positioning of the patient, and bone condensation produced by the mylohyoid muscle in the floor of the mouth. It is interesting to emphasize that MC bifurcates in the infero-superior or medio-lateral plane in about 1% of patients.
The mechanism of development of bifid/trifid MC has been hypothesized by the explanation that during embryonic development a rapid prenatal growth and remodeling in the ramus region lead to intramembranous ossification that forms MC. The occurrence of bifid/trifid MC is thought to be secondary to the incomplete fusion of these three nerves. Once the multiple canals are identified, the local anesthetic injection technique and surgical procedures can be modified to prevent pain, discomfort, or even numbness during treatment.
Our study collectively incorporates various parameters pertaining to the morphology and dimensions of the mandibular canal using CBCT as compared to previous studies on diverse population which focuses on single or few related parameters using conventional techniques. Earlier studies on the course of the canal were mainly restricted to the third molar region, whereas we have traced the canal throughout its course. Also, the length of the canal has been measured which was not taken into consideration in previous studies. Significant limitations have been found in earlier studies describing the intra-bony anatomy of MC. For example, dry skull reports may have variable diseases and lack relevant data such as age, gender, or include edentulous mandibles, or use inconsistent and anatomically irrelevant landmarks. Differences in the value may be related to morphological, geographical, ethnical differences, and variable methodology and landmarks used in different studies. Studies on larger sample size in diverse population needs to be done to draw a definite conclusion.
Conclusions
From our study, following conclusions can be drawn:
Inferior alveolar neurovascular bundle exists in different locations and presents many variations. Individual deviation, gender, age, race, and assessing technique used largely influence these variations.
The inner vertical diameter in each tooth region on the right and left side was found to be more than the inner horizontal diameter, suggestive of oval to round shape of the MC.
The length of the MC should be ascertained prior to the neurectomy procedure in cases of trigeminal neuralgia.
In order to plan a proper dental implant insertion method and select the implants of a relevant type, it is important to be aware of the position of the MC in connection with the cortical plates and crest of alveolar ridge. Osteotomies in BSSO procedure should not be performed in the posterior mandible until the position of the MC is established. Also, the parameters obtained acts as guide in bone-harvesting procedures from the ramus and body of mandible and bone plating in angle and body region of mandible.
The distance of the MC from the crestal bone level and inferior border of mandible in various regions was suggestive of catenary course of the canal. These criteria should be considered in surgeries involving posterior mandible especially in third molar region.
CBCT provides a clear dimension of the anterior loop. Based upon the anatomical findings, a safe guideline of 4 mm from the most anterior point of the MF is recommended for implant treatment planning.
The bifid MC is of rare occurrence. The detection of these anatomical variations is important because of its clinical implications such as the ineffective mandibular block or numbness, injury to the nerve causing paresthesia, or injury to vessels resulting in inadvertent bleeding in surgeries involving the lower jaw.
It is clear that with the advances in technology and the improvement in images as diagnostic tools, the number of anatomical variations of the MC is likely to increase considerably. So, to comment on anatomic variations, there is a requirement for a large multicentric study with defined anatomical landmarks to quantify and precisely predict these parameters and confirm the trends observed.
Compliance with Ethical Standards
Conflict of interest
Authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Juodzbalys G, Wang H, Sabalys G. Anatomy of mandibular vital structures. Part I: MC and inferior alveorlar neurovascular bundle in relation with dental implantology. J Oral Maxillofac Res. 2010;1:e2. doi: 10.5037/jomr.2010.1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lindh C, Petersson A, Klinge B. Measurement of distances related to the MC in radiographs. Clin Oral Implants Res. 1995;6(2):96–103. doi: 10.1034/j.1600-0501.1995.060205.x. [DOI] [PubMed] [Google Scholar]
- 3.Xie Q, Wolf J, Soikkonen K, Ainamo A. Height of mandibular basal bone in dentate and edentulous subjects. Acta Odontol Scand. 1996;54(6):379–383. doi: 10.3109/00016359609003555. [DOI] [PubMed] [Google Scholar]
- 4.Oliveira-Santos CD, et al. Assessment of variations of the MC through cone beam computed tomography. Clin Oral Invest. 2012;16:387–393. doi: 10.1007/s00784-011-0544-9. [DOI] [PubMed] [Google Scholar]
- 5.Ozturk A, Potluri A, Vieira AR. Position and course of the mandibular canal in skulls. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113(4):453–458. doi: 10.1016/j.tripleo.2011.03.038. [DOI] [PubMed] [Google Scholar]
- 6.Sato I, Ueno R, Kawai T, Yosue T. Rare courses of the MC in the molar regions of the human mandible: a cadaveric study. Okajimas Folia Anat Jpn. 2005;82(3):95–101. doi: 10.2535/ofaj.82.95. [DOI] [PubMed] [Google Scholar]
- 7.Rajchel J, Ellis E, Fonseca RJ. The anatomical location of the MC: its relationship to the sagittal ramus osteotomy. Int J Adult Orthod Orthognath Surg. 1998;1(1):37–47. [PubMed] [Google Scholar]
- 8.Obradovic O, Todorovic L, Pesic V, Pejkovic B, Vitanovic V. Morphometric analysis of MC: clinical aspects. Bull Group Int Rech Sci Stomatol Odontol. 1993;36(3–4):109–113. [PubMed] [Google Scholar]
- 9.Ikeda K, Ho KC, Nowicki BH, Haughton VM. Multiplanar MR and anatomic study of the MC. AJNR Am J Neuroradiol. 1996;17(3):579–584. [PMC free article] [PubMed] [Google Scholar]
- 10.Tamás F. Position of the MC. Int J Oral Maxillofac Surg. 1987;16(1):65–69. doi: 10.1016/S0901-5027(87)80032-2. [DOI] [PubMed] [Google Scholar]
- 11.Anderson LC, Kosinski TF, Mentag PJ. A review of the intraosseous course of the nerves of the mandible. J Oral Implantol. 1991;17(4):394–403. [PubMed] [Google Scholar]
- 12.Miller CS, Nummikoski PV, Barnett DA, Langlais RP. Cross-sectional tomography. A diagnostic technique for determining the buccolingual relationship of impacted mandibular third molars and the inferior alveolar neurovascular bundle. Oral Surg Oral Med Oral Pathol. 1990;70(6):791–797. doi: 10.1016/0030-4220(90)90023-L. [DOI] [PubMed] [Google Scholar]
- 13.Obradović O, Todorovic L, Vitanovic V. Anatomical considerations relevant to implant procedures in the mandible. Bull Group Int Rech Sci Stomatol Odontol. 1995;38(1–2):39–44. [PubMed] [Google Scholar]
- 14.Davis H. Advanced osseointegration surgery: application in the maxillofacial region. Chicago: Quintessence Publishing Co.; 2000. Mobilization of the alveolar nerve to allow placement of osseointegratible fixtures; pp. 129–141. [Google Scholar]
- 15.Levine MH, Goddard AL, Dodson TB. Inferior alveolar nerve canal position: a clinical and radiographic study. J Oral Maxillofac Surg. 2007;65(3):470–474. doi: 10.1016/j.joms.2006.05.056. [DOI] [PubMed] [Google Scholar]
- 16.Denio D, Torabinejad M, Bakland LK. Anatomical relationship of the MC to its surrounding structures in mature mandibles. J Endod. 1992;18(4):161–165. doi: 10.1016/S0099-2399(06)81411-1. [DOI] [PubMed] [Google Scholar]
- 17.Jacobs R, Mraiwa N, Van Steenberghe D, Sanderink G, Quirynen M. Appearance of the mandibular incisive canal on panoramic radiographs. Surg Radiol Anat. 2004;26(4):329–333. doi: 10.1007/s00276-004-0242-2. [DOI] [PubMed] [Google Scholar]
- 18.Rosenquist B. Is there an anterior loop of the inferior alveolar nerve? Int J Periodontics Restor Dent. 1996;16(1):40–45. [PubMed] [Google Scholar]
- 19.Yosue T, Brooks SL. The appearance of mental foramina on panoramic radiographs. I. Evaluation of patients. Oral Surg Oral Med Oral Pathol. 1989;68(3):360–364. doi: 10.1016/0030-4220(89)90224-7. [DOI] [PubMed] [Google Scholar]
- 20.Misch CE, Crawford EA. Predictable mandibular nerve location—a clinical zone of safety. Int J Oral Implantol. 1990;7(1):37–40. [PubMed] [Google Scholar]
- 21.Langlais RP, Broadus R, Glass BJ. Bifid MCs in panoramic radiographs. J Am Dent Assoc. 1985;110(6):923–926. doi: 10.14219/jada.archive.1985.0033. [DOI] [PubMed] [Google Scholar]
- 22.Claeys V, Wackens G. Bifid MC: literature review and case report. Dentomaxillofac Radiol. 2005;34(1):55–58. doi: 10.1259/dmfr/23146121. [DOI] [PubMed] [Google Scholar]
- 23.Grover PS, Lorton L. Bifid mandibular nerve as a possible cause of inadequate anesthesia in the mandible. J Oral Maxillofac Surg. 1983;41(3):177–179. doi: 10.1016/0278-2391(83)90076-9. [DOI] [PubMed] [Google Scholar]