Abstract
Gossypiboma is a retained surgical sponge and represents a rare complication with an uncertain incidence probably due to medical–legal implications. It is an iatrogenic condition solely due to human factors. While the medical literature has previously described cases of this entity after orthopedic, abdominal, otorhinolaryngology, and plastic surgery procedures, gossypibomas in oral and maxillofacial region are uncommon. It can mimic neoplasms or other injuries, which may promote a delayed diagnosis; thus, the differential diagnosis should be based on clinical history in each particular case. Although there are no pathognomonic features of gossypiboma in oral and maxillofacial region, the most common symptoms suggestive of persistent inflammation include pain, fever, swelling, surgical wounds that do not heal, and purulent drainage. The aim of this study was to report a maxillofacial gossypiboma misdiagnosed as third molar surgery-related odontogenic infection and a diagnosis algorithm.
Keywords: Foreign bodies, Gossypibomas, Retained surgical sponge, Third molar
Introduction
Gossypiboma is a term used for a retained surgical sponge, and it represents a rare complication [1–3] with an uncertain incidence probably due to medical–legal implications [2, 4]. The word is derived from the combination of the Latin word ‘gossypium’ for ‘cotton’ and the Swahili word ‘boma’ for ‘place of concealment’ [2–5]. It can be defined as a mass within the body composed of cotton matrix, which usually refers to a forgotten wound dressing surrounded by a foreign body reaction [4, 5]. While the medical literature has previously described cases of this entity after surgery procedures, gossypibomas in oral and maxillofacial region are rare [2].
Postoperative complications of forgotten surgical gauzes may occur at any time in the postoperative period [3], and clinically this situation may be associated with persistent bleeding and infection discharge [4, 6]. In some cases, the missed surgical gauze can be accidentally found before the onset of signs and symptoms. Although there are no pathognomonic features of a foreign body reaction in oral and maxillofacial region, the most common symptoms suggestive of persistent inflammation include pain, fever, swelling, surgical wounds that do not heal, and purulent drainage [4, 5].
The aim of this study was to report a maxillofacial gossypiboma misdiagnosed as third molar surgery-related odontogenic infection and to propose a diagnosis algorithm.
Case Report
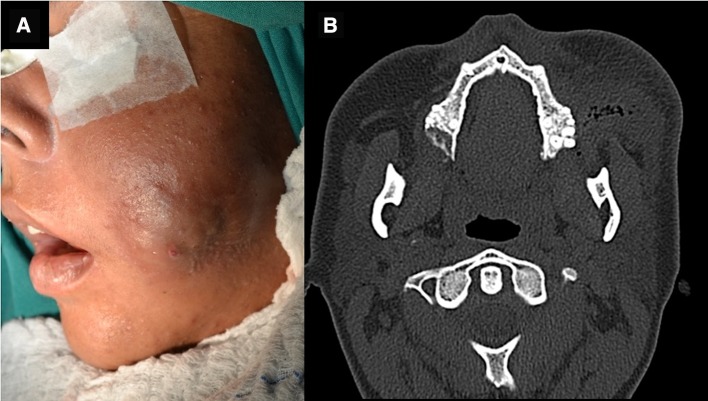
A 26-year-old female patient was attended complaining of a painful maxillary swelling. Her symptoms started 7 days after she had undergone extraction of tooth #28. In her last dental visit before the present consultation, amoxicillin (500 mg/thrice a day for 7 days) and ibuprofen (600 mg/thrice a day for 3 days) were prescribed. On extraoral examination, there was a tender swelling showing center in her left maxillary region. Clinically, limited mouth opening, poor oral hygiene, and intraoral purulent discharge were observed. Panoramic radiograph showed the absence of tooth #28 and left maxillary sinus opacification. Initially, an abscess drainage was performed via an intraoral incision and amoxicillin–clavulanate (875 mg/thrice a day for 7 days) and nimesulide (100 mg/thrice a day for 3 days) were prescribed. The patient returned 48 h later with increased pain, swelling, and purulent discharge. Then, the patient was hospitalized in order to request blood tests and imaging examinations and to prescribe an intravenous antibiotic therapy (ampicillin/sulbactam 3 mg in 6-hour intervals). Computed tomography analysis revealed cellulitis of left masseter and medial pterygoid muscles containing gas bubbles and presenting a spongiform appearance (Fig. 1a). The patient underwent surgical exploration under general anesthesia, to drain the facial abscess (Fig. 1b). During surgical manipulation, a foreign body consistent with surgical gauze in the buccal space region was retrieved. The patient remained hospitalized with an intravenous antibiotic regimen of ampicillin/sulbactam (3 mg in 6-hour intervals) associated with ciprofloxacin (500 mg in 8-hour intervals) for 5 days. The patient is still under periodic follow-up appointments, and no alterations have been observed.
Fig. 1.
a Clinical aspect of infection. b Axial, sagittal, coronal windows and 3D reconstruction with red point intersection of the three planes
Discussion
To date, only 15 cases of gossypibomas in oral and maxillomandibular region have been described. Details in the literature are presented in Table 1.
Table 1.
| Study (year) | Sex | Age (years) | Site | Retention time | Previous surgery | Image examination modality |
|---|---|---|---|---|---|---|
| Al-Ruhaimi et al. [6] | F | 19 | Right mandibular ramus | NI | Orthognathic surgery | Panoramic radiograph |
| Catterlin et al. [7] | M | 19 | Right mandibular angle | NI | Third molar surgery | Panoramic radiograph |
| Amr [1] | M | 27 | Right submandibular region | 8 years | Submandibular gland excision | CT |
| Song et al. [3] | F | 27 | Left mandibular angle | 27 days | Mandibular contouring surgery | CT |
| F | 45 | Right mandibular angle | 23 days | Mandibular contouring surgery | CT | |
| F | 27 | Mandibular angle | 15 days | Mandibular contouring and zygomatic surgeries | None | |
| Sigron et al. [2] | F | 42 | Right posterior mandible | 7 years | Implant placement + third molar surgery | Panoramic radiograph |
| Mohanavalli et al. [10] | M | 56 | Right posterior maxilla | 6 months | Cyst removal | Panoramic radiograph + CT |
| Jamjoom et al. [4] | F | 37 | Anterior mandibular region | 2 years | Implant placement | Panoramic radiograph + CT + Magnetic resonance |
| Alves-de-Oliveira et al. [5] | F | 42 | Left maxillary sinus | 2 years | Multiple tooth surgery | Panoramic radiograph |
| Park et al. [8] | F | 20 | Left Eustachian tube | 8 months | Orthognathic surgery | Magnetic Resonance |
| Park et al. [9] | F | 28 | Left infratemporal fossa | 3 years | Orthognathic surgery | CT + Magnetic resonance |
| Present study | F | 26 | Left maxillary region | 7 days | Third molar surgery | Panoramic radiograph + CT |
F female, M male, NI not informed, CT computed tomography
Forgotten surgical gauze may be found incidentally before the warning signs and symptoms appear [6]. Clinical symptoms may include persistent pain, fever, swelling, unhealed surgical wounds, and purulent drainage. In addition, some patients report subjective symptoms such as foreign body sensation [2], cacosmia [3], and unilateral otitis media with effusion [8].
Early diagnosis of gossypibomas is beneficial, avoiding the establishment of a severe infectious process, delayed recovery, and legal/ethical issues [3]. Its unspecific symptoms usually confuse the surgeon with a normal healing process, leading to a delayed diagnosis and worsening of problems [3], as observed in the present case.
Imaginologic pattern of gossypibomas depends on the local tissue reaction to the foreign body, their anatomical location, the gauze composition, the presence/absence of a radiopaque marker, and the retention time [5]. Surgical gauze containing radiopaque marker is an important tool in the early recognition of imaginologic pattern of gossypibomas, as observed in the present case.
The management of gossypibomas in oral maxillofacial region consists of surgical removal and thorough debridement of the surgical site associated with antibiotic regimen in infected areas [4], as performed in the present case. However, the best approach for gossypiboma remains in its prevention [6].
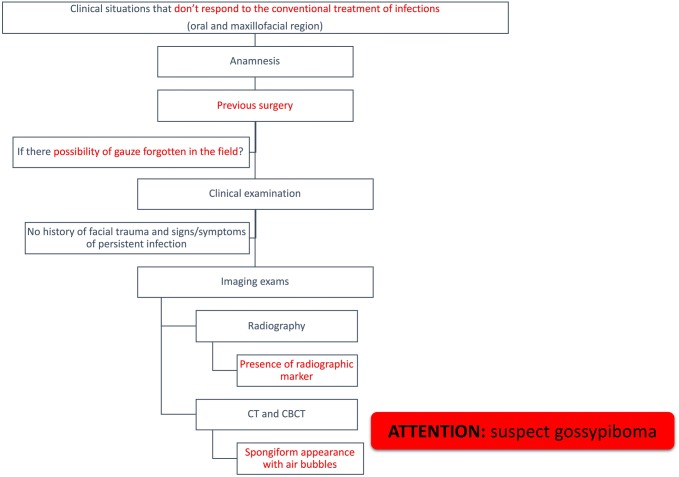
Initially, patients presenting with infectious pictures related to the maxillofacial region should be carefully evaluated, especially in those cases that did not obtain clinical improvement after a certain therapy was instituted. During the anamnesis, a previous history of any surgical procedure should be investigated because of the possibility of forgetting gauze in the operative field. In addition, it is necessary to establish a differential diagnosis that includes other conditions possibly associated with infectious signs and symptoms, such as fractures involving the region of facial bones. Then, imaging tests should be ordered for a more accurate evaluation of the case, which may be conventional or tomographic examinations. In particular, fan beam (CT) or conical computed tomography (CBCT) has a better detail and appearance of gossypiboma when air bubbles appear.
The surgeon can detect spongiform aspect or air bubbles in computed tomographies; however, these aspects should not be considered pathognomonic for maxillofacial gossypibomas. Thus, we highlight the importance of diagnosis algorithm (Fig. 2).
Fig. 2.
Diagnosis algorithm
According to the literature review, many cases of gossypiboma were observed in patients with a provisional diagnosis of infection affecting the maxillofacial region [1–10]. When analyzing the cases, it was possible to observe that most of the patients had undergone some surgical procedure in the maxillofacial region, such as third molar surgery [2, 7], orthognathic surgery [6, 8, 9], implant placement [2, 4], or mandibular contouring surgery [3], among other examples. Due to the report of gossypibomas in other regions of the body, which were suspected after a previous history of surgical procedure [11], such condition is also plausible due to orofacial surgical procedures [1–10]. In this context, due to the rarity of gossypibomas, the dental surgeon should direct the clinical examination to rule out other conditions that may be associated with infectious processes and that are more common than gossypibomas, such as fractures in the maxillomandibular complex (insert fracture article with infection in the maxilla). To complement the diagnostic process, the evaluation of clinical signs and symptoms should be combined with imaging analysis. In this aspect, gossypibomas can be observed in conventional radiographs as panoramic radiograph [2, 4–7, 10], whereas in tomographic examinations [1, 3, 4, 9, 10] such conditions present a predominant aspect of air bubbles. Taken together, these aspects may support the diagnostic process of maxillofacial gossypibomas.
Author’s Contribution
All authors have read, approved, made substantive contribution to this manuscript and/or work, and reviewed the final version of this paper prior to its submission.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Informed Consent
Informed consent was obtained from participant included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Amr AE. A submandibular gossypiboma mimicking a salivary fistula: a case report. Cases J. 2009;2:6413. doi: 10.4076/1757-1626-2-6413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sigron GR, Locher MC. A gossypiboma (foreign body granuloma) mimicking a residual odontogenic cyst in the mandible: a case report. J Med Case R. 2011;5:211. doi: 10.1186/1752-1947-5-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Song SY, Hong JW, Yoo WM, Tark KC. Gossypiboma after mandibular contouring surgery. J Craniofac Surg. 2009;20(5):1607–1610. doi: 10.1097/SCS.0b013e3181b14761. [DOI] [PubMed] [Google Scholar]
- 4.Jamjoom FZ, Kallukaran F. Gossypiboma following mandible surgery: a case report and review of the literature. Oral Surg. 2013;6:94–97. doi: 10.1111/ors.12018. [DOI] [Google Scholar]
- 5.Alves-de-Oliveira CN, Pimenta-do-Amaral TM, Ribeiro-Souto G, Alves-Mesquita R. Gossypiboma in the oral region: case report and literature review. J Clin Exp Dent. 2014;6(4):e444–e447. doi: 10.4317/jced.51553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.al-Ruhaimi KA, Nwoku AL. An unusual radiopaque image through an orthopantomogram film. Int J Oral Maxillofac Surg. 1991;20(2):96–97. doi: 10.1016/S0901-5027(05)80716-7. [DOI] [PubMed] [Google Scholar]
- 7.Catterlin RK, Throndson RR. Iodoform gauze with a radiopaque filament. Oral Surg Oral Med Oral Pathol. 1993;76(2):257. doi: 10.1016/0030-4220(93)90215-P. [DOI] [PubMed] [Google Scholar]
- 8.Park CM, Choi KY, Heo SJ, Kim JS. Unilateral otitis media with effusion caused by retained surgical gauze as an unintended iatrogenic complication of orthognathic surgery: case report. Br J Oral Maxillofac Surg. 2014;52(7):e39–e40. doi: 10.1016/j.bjoms.2014.04.014. [DOI] [PubMed] [Google Scholar]
- 9.do Park Y, Choo OS, Hong SY, Kim HJ. Infratemporal fossa cellulitis caused by a remnant iatrogenic foreign body after a bimaxillary operation. J Craniofac Surg. 2015;26(3):e196–e197. doi: 10.1097/SCS.0000000000001289. [DOI] [PubMed] [Google Scholar]
- 10.Mohanavalli S, David JJ, Gnanam A. Rare foreign bodies in oro-facial regions. Indian J Dent Res. 2011;22(5):713–715. doi: 10.4103/0970-9290.93462. [DOI] [PubMed] [Google Scholar]
- 11.Hariharan D, Lobo DN. Retained surgical sponges, needles and instruments. Ann R Coll Surg Engl. 2013;95(2):87–92. doi: 10.1308/003588413X13511609957218. [DOI] [PMC free article] [PubMed] [Google Scholar]