Abstract
Objective
The current study aimed to describe the impact of parental migraine on adolescent children (aged 11–17) living at home with a parent with migraine.
Background
Emerging evidence suggests that migraine impacts the family members of people with migraine. However, there has been little research to evaluate the perspective of the child of a parent with migraine.
Methods
This cross-sectional observational study included parents who met ICHD criteria for migraine and their 11-17 year old children currently living with the parent with migraine recruited from neurologist offices and online. Parents completed measures of demographics, a diagnostic migraine criteria screener, parental illness impact (Parental Illness Impact Survey – Revised; subscales = Burden of Daily Help, Emotional Impact, Social Impact, Communication and Understanding, Impact on Personal Future, Friends Reactions, Parent/Child Relationship, and Global Well-Being), migraine-related disability (MIDAS), headache attack frequency, and headache attack pain intensity. Children completed measures of demographics, parental illness impact, and a migraine diagnostic screener if applicable.
Results
Children (n = 40) reported the greatest impact of their parent’s migraine on the Global Well-Being (M = 3.3, SD = 0.9) and Parent/Child Relationship (M = 3.5, SD = 0.6) subscales. There were no significant differences between the average child and parent rating of parental migraine impact on children. Correlations between parent and child ratings of parental migraine impact were strongest for the Social Impact subscale (ρ = .55, p < .001), and non-significant for the Parent/Child Relationship (ρ = .13, p = .416) and Friends Reactions (ρ = .18, p = .257) subscales. Higher attack frequency and endorsing severe disability on the MIDAS were associated with higher child-rated impact (e.g., lower scores) on Global Well-Being (frequency ρ = −.35, p = .028; MIDAS t(38) = 2.74, p = .009) and Impact on Personal Future (frequency ρ = −.41, p = .009; MIDAS t(35.7) = 2.49, p = .017) subscales. Higher attack pain intensity was associated with higher child-rated impact (e.g., lower scores) on Burden of Daily Help (r = −.34, p = .031) and Emotional Impact (r = −.40, p = 0.010). Over half of children (23/40, 57.5%) reported some kind of service or intervention to help them manage the impact of their parent’s migraine on their lives would be helpful.
Conclusions
Parental migraine impacts children aged 11-17 living in the home, particularly in the domains of global well-being and the parent/child relationship. Parent and child reports are not strongly correlated across all domains of parental impact.
Keywords: Migraine, Family, Children, Burden, Impact
Migraine is associated with considerable individual burden (1–5) and societal expense (6, 7). Emerging research suggests migraine also impacts the family of people with migraine (8–13). The impact of migraine on the family is particularly important in this disease because the prevalence of migraine peaks between early and middle adulthood and then subsequently declines; this period is likely to correspond with family-related major life events such as marriage and having children. Parenting in particular could be impacted by the unpredictable and disabling nature of migraine attacks. Understanding the impact of migraine on children of a parent with migraine would shed further light on the burden of migraine on the family unit.
The majority of research evaluating the impact of migraine on children has assessed the perspective of the person with migraine, and occasionally his/her spouse, but rarely his/her child. In a 1998 telephone survey, 350 people with migraine reported migraine impacted activities with children and spouses (62.0-69.0%), including ceasing to care for younger children during a migraine attack (61.0%), cancelling outings with children (56%), and requiring other child care arrangements needed (42.0%) (11). The parent with migraine reported younger children (aged <12) usually reacted positively (66%), but reported some were confused (25.0%), hostile (17.0%), or afraid (12.0%), whereas parents with migraine reported older children (aged 12-17) were more understanding (87.0%), although some were also hostile (12.0%) (11). In a 2003 telephone survey, 1,142 people with migraine and their household partners reported a negative impact of migraine on the relationship between the parent with migraine and his/her children (9); 43.0% of people with migraine thought they would be better parents if they did not have migraine. People with migraine also reported migraine attacks had caused their children to miss school (9.5%), or arrive late/leave school early (10.8%). A 2004 online survey of 866 people with migraine and 162 family members without migraine found that almost half of family members reported that living with or being related to a person with migraine had a moderate or great impact on home/family life (49.0%) (8).
Recently, an analysis of data from adolescent respondents to the Chronic Migraine Epidemiology and Outcomes (CaMEO) Study (13) reported types and rates of impact of parental migraine on adolescent children (n = 1,411; aged 13-21) living with the parent with migraine and evaluated differences reported between adolescents of parents with chronic (15 or more days/month) or episodic migraine (14 or fewer days/month) using a survey designed specifically to evaluate the family impact of migraine. Adolescents reported that migraine impacted parental support, their emotional experiences, school, and group activities; for example, 50.0% of adolescents of parents with chronic migraine, and 27.0% of adolescents of parents with episodic migraine reported they could not get help when they needed it from their parent with migraine at least once per month. Further, 46.5% of adolescents of parents with chronic migraine and 22.6% of adolescents of parents with episodic migraine reported their parent with migraine missed a family outing at least once in the past month due to migraine.
These CaMEO Study results demonstrate that adolescents (aged 13-21) perceive a negative impact of their parent’s migraine on their lives and that the impact increases with headache/migraine attack frequency. Because CaMEO used migraine-specific questions, it is difficult to compare the impact of parental migraine on children to the impact of other illnesses. Further, it has not been reported yet whether estimates of parental migraine impact on children differ between parent and child perspectives. This is important because parent report is often relied on to assess impact on children, and is necessary to understand the impact of parental migraine on young children. Systemic differences in responding between parents with migraine and their children could lead to erroneous estimates of the burden of migraine on children when assessed from only the parental perspective.
The current study aimed to describe the impact of parental migraine on adolescent children (aged 11-17) living at home with a parent with migraine. We aimed to evaluate differences in child and parent perception of the impact of parental migraine on children. We also aimed to explore the associations between headache attack frequency (days per month), headache attack pain intensity, and migraine-related disability with parental migraine impact on children. Finally, we aimed to describe the resources children reported would be beneficial to help ease the impact of their parent’s migraine on their lives.
Methods
Participants
The Family Burden of Migraine study was a cross-sectional observational study of people with migraine and their adolescent children (aged 11-17) living in the same home conducted through online surveys. This paper describes the primary outcomes of the study. Parents with migraine were recruited from the New York City metro area at neurologists’ offices and headache centers and through online recruitment from September, 2016 – February, 2017. Paper flyers were displayed in exam rooms and waiting rooms, and recruiting physicians verbally told their patients about the study in order to gauge potential interest and eligibility. Online recruitment efforts included a landing page with a description of the study and social media advertising.
Inclusion criteria for parents with migraine included: a) 18-65 years old, b) able to speak and read English fluently, c) met International Classification of Headache Disorders-3 (ICHD-3) diagnostic criteria for migraine at the time of assessment, d) has either has a physician diagnosis of migraine, or reports physician-diagnosed migraine, e) has a child between the ages of 11-17 who lives at home with the parent who has migraine. Inclusion criteria for the children included: a) 11-17 years old, b) able to speak and read English fluently, c) lives at home with a parent who has migraine, d) has an active email account. The age range of 11-17 was selected because this is the age range for which the parental illness impact measure described below is validated; further, 11 is the youngest age at which children typically can complete surveys independent of parental assistance. If multiple children within a family met the inclusion criteria, the parent decided which child would participate in the study.
Procedures
Interested individuals were phone-screened for inclusion criteria. Eligible parents with migraine were sent a link to a Qualtrics survey, a secure and HIPAA-compliant web-based data capture application. Informed consent for the participation of both the parent and the child was obtained from the parent with migraine online. The parent with migraine provided a separate email address for the child. Parents then completed surveys approximately 30 minutes in length (Duration M = 29.6 minutes, SD = 14.9 minutes) assessing demographic characteristics, headache characteristics, parent perception of child burden of parental migraine, and psychosocial factors. Upon parental completion of the survey, a second link was sent to the child’s email address. Each child provided online informed assent (ages 11-12) or informed consent (ages 13-17) and completed a survey approximately 15 minutes in length (Duration M = 14.4 minutes, SD = 10.0 minutes) assessing demographic characteristics, headache characteristics if appropriate, and child perception of the burden of parental migraine. Both the parent and child received a $10 gift card code for completing the surveys. All surveys required completion of each question, resulting in no missing data. The protocol was approved by the Einstein IRB (2015-5785).
Measures
Demographic Questionnaire.
Parents with migraine reported age (reported continuously), gender (male vs. female), race and ethnicity (reported as “White/Non-Hispanic” and “All Else”), marital status (reported as “married” and “single, separated, or divorced”), level of education (“some high school,” “high school graduate/GED,” “some college,” “college graduate,” “some graduate school,” and “graduate degree”) and employment for self and partner (“full-time,” “part-time,” “not currently working”), combined household income (“less than $25,000,” “$25,000-$50,000,” “$50,000-$74,999,” “$75,000-$99,999,” “$100,000-$199,999,” “$200,000 and above”) and breadwinner status (respondent, partner, or both). Children of parents with migraine reported age (reported continuously), gender (male vs. female), race and ethnicity (reported as “White/Non-Hispanic” and “All Else”), and household composition (two-parent or single-parent household).
The Parental Illness Impact Scale-Revised (PIIS-R).
The PIIS-R is two-part scale designed to evaluate 1) parental illness impact and 2) a needs assessment to mitigate the impact of parental illness on children (14). It was originally developed and validated to be used with children of parents with Parkinson’s disease (15); the revised version has been used to assess the impact of various neurological parental illnesses, including Parkinson’s disease and multiple sclerosis, on children (14, 16).
The first part of the PIIS-R consists of 37 items designed to assess the impact of parental illness on children (14). These items comprise 8 subscales: 1) Burden of Daily Help (household chores, parent depends on child, have to help care for parent, increased responsibility), 2) Emotional Impact (sad, worried, affected schoolwork, angry), 3) Social Impact (reduced time with friends, social activities, less independence), 4) Communication and Understanding (parent has difficulty talking about illness, understand unwell parent less than other parent, parent’s illness affects life of whole family), 5) Impact on Personal Future (uncertain about future, independence affected in future), 6) Friends Reactions (difficulty explaining parent’s illness to friends, difficulty coping with friends lack of understanding, embarrassed talking to friends), 7) Parent/Child Relationship (parent and child understand each other, parental illness brought closer together, embarrassed by parent’s illness) and 8) Global Well-Being (physical health, sleep, emotional health). Response options are on a Likert-type scale ranging from 1 to 5, with higher scores indicating lower levels of illness impact. Subscale scores were standardized such that 1 = the highest level of parental illness impact, and 5 = the lowest level of parental illness impact. In development studies, the PIIS-R has demonstrated strong psychometric properties for use in populations in which a parent has a neurologic condition; high internal consistency (α =.92) and test-retest reliability (r =.59-.74) (14, 15). In the current study, the PIIS-R was administered to both parents (α = .92) and children (α = .93).
The second part of the PIIS-R consists of a 14-item needs assessment designed to evaluate the resources that would be helpful to mitigate the impact of parental illness on children (14). Response options are on a binary scale (“Yes,” “No”).
American Migraine Study / American Migraine Prevalence and Prevention Study Migraine Diagnostic Module.
The American Migraine Study/American Migraine Prevalence and Prevention Study (AMS/AMPP) migraine diagnostic screener (17) was administered to potential participants who either had a physician diagnosis of migraine or reported physician-diagnosed migraine to assess currently meeting migraine criteria. The screener is based on lifetime recall of symptoms associated with the respondent’s “most severe” type of headache and captures the International Classification of Headache Disorders-3rd edition (ICHD-3) criteria for migraine including headache pain characteristics (unilateral location, pulsating/throbbing quality, moderate to severe intensity); exacerbation by routine activity; and associated symptoms (nausea, phonophobia, and photophobia) with the exception of Criterion A (a lifetime history of ≥ 5 migraine attacks). The screener was validated using the ICHD-2 criteria; however, the criteria used for migraine are the same as outlined in ICHD-3. The screener has sensitivity of 100% and specificity of 82% for migraine (18). All parents with migraine completed this screener. Only children who endorsed headache completed this screener.
Migraine Disability Assessment (MIDAS).
The MIDAS is a self-report instrument that was administered to the parents in order to measure migraine-related disability, headache pain intensity, and headache attack frequency (19). The five-item MIDAS score targets domains of activity and asks individuals about lost days over a three month period related to school or paid work, household work, and family, social or leisurely activities due to headache attacks. MIDAS score was analyzed as a dichotomous variable: low to moderate levels of disability (MIDAS scores = 0-20) and severe levels of disability (MIDAS score ≥ 21). The MIDAS also includes two questions querying attack frequency and average headache pain intensity (on a scale of 0-10); both questions were analyzed continuously. In development studies, the MIDAS has demonstrated good internal consistency (α =.76 in the US and .73 in the UK) and construct validity, and high test-rest reliability (19).
Analysis
This is the primary analysis of these data. All analyses were planned a priori. These data have not been used in prior publications. All variables were evaluated for distribution. Descriptive statistics (mean and standard deviation for normally distributed variables, median and interquartile range for non-normally distributed continuous variables, and n and % for categorical variables) described participant characteristics for both parents with migraine and children. Descriptive statistics also were used to describe the PIIS-R subscale scores for both children and parents, and resource items endorsed by children. Paired-sample t-tests and correlations evaluated differences in levels of burden reported by children and parents. The study aimed to recruit 45 parent-child dyads to obtain a power of .95 to detect a medium (d = 0.50) sized difference between parent and child reports of burden using paired-sample t-tests (G*Power 3.1.7). Bivariate tests explored relationships between migraine attack frequency (Spearman correlation), migraine attack intensity (Pearson correlation) and MIDAS category (t-test) with child ratings on the PIIS-R. All inferential testing was two-tailed with alpha set at .05. SPSS version 22 was used to conduct analyses.
Results
Participant Characteristics
Two-hundred forty-five parents were contacted and assessed for eligibility (Figure 1). Of these, 130 were excluded as they did not meet inclusion criteria (n=99), declined to participate (n=6), or did not respond to contact attempts (n=25). The remaining 115 eligible parents were emailed the link to the study. Seven parents did not provide an email address for a child and were excluded. Fifty parents completed the survey. Ten of these parents’ children did not complete the survey and so their data was excluded. Thus, the final sample for analysis included 40 parent-child dyads (19 from neurology offices and 21 from online recruitment; Figure 1).
Figure 1.
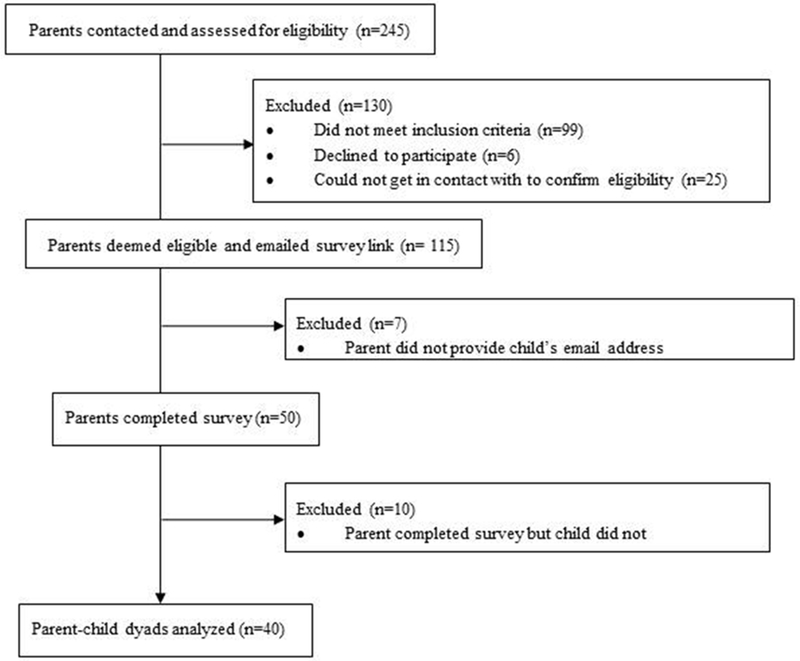
Participant Flow Diagram
Parents were predominantly women (97.5%), who were White/Non-Hispanic (87.5%), married (77.5%), and highly educated (65.0% had a college degree or higher) with an average age of 43.5 (SD = 6.3). The sample was divided among participants working full-time (37.5%), part-time (35.0%), and not working currently (27.5%). The majority of parents with a partner (n = 32) reported their partner worked full-time (93.8%). Approximately half of participants reported their partner was the primary breadwinner (55.0%), with 27.5% reporting the respondent was the breadwinner, and 17.5% reporting that both partners were breadwinners. Parents reported a median headache attack frequency of 6.8 attacks/month [IQR = 4.0–15.0] with an average headache pain intensity of 6.8/10 (SD = 1.7). Almost two-thirds of participants reported severe migraine-related disability on the MIDAS (62.5%).
Children were equally divided by gender with an average age of 13.6 (SD = 1.8) and were predominantly White/Non-Hispanic (92.7%). The majority currently lived primarily in a two-parent household (83.5%). Sixty percent of children reported headache and were screened for ICHD-3 criteria; approximately half (52.5%) met criteria for migraine.
Parental Illness Impact
Higher scores on the PIIS-R subscales indicate lower parental illness impact, with a score of 5 indicating the lowest possible parental illness impact, and a score of 1 indicating the highest possible parental illness impact. Children reported the greatest impact of their parent’s migraine on their Global Well-Being (M = 3.3, SD = 0.9) and the Parent/Child Relationship (M = 3.5, SD = 0.6) subscales (Table 3; Figure 2). Children reported the least impact of their parent’s migraine on the Friends Reactions (M = 4.6, SD = 0.7), Impact on Personal Future (M = 4.4, SD = 0.7) and Social Impact (M = 4.3, SD = 0.7) subscales.
Table 3.
Parent and Child Ratings on the Parent Illness Impact Scale – Revised Subscales
| Paired-Sample Correlation | Paired-Sample T-Test | |||||
|---|---|---|---|---|---|---|
| PIIS-R Subscale | Child M(SD) | Parent M(SD) | ρ | p | t | p |
| Burden of Daily Help | 3.8 (0.7) | 3.8 (0.7) | .40 | .011 | −0.18 | .857 |
| Emotional Impact | 3.8 (0.9) | 3.7 (0.8) | .38 | .016 | 0.43 | .667 |
| Social Impact | 4.3 (0.7) | 4.1 (0.7) | .55 | < .001 | 2.02 | .051 |
| Communication & Understanding | 3.9 (0.8) | 3.7 (0.6) | .37 | .018 | 1.64 | .110 |
| Impact on Personal Future | 4.4 (0.7) | 4.4 (0.7) | .42 | .006 | −.07 | .945 |
| Friends Reactions | 4.6 (0.7) | 4.5 (0.7) | .18 | .257 | .75 | .460 |
| Parent/Child Relationship | 3.5 (0.6) | 3.3 (0.6) | .13 | .416 | 1.25 | .217 |
| Global Well-Being | 3.3 (0.9) | 3.5 (0.9) | .40 | .011 | −1.84 | .073 |
Note. N = 40. PIIS-R = Parental Illness Impact Survey-Revised.
Figure 2.
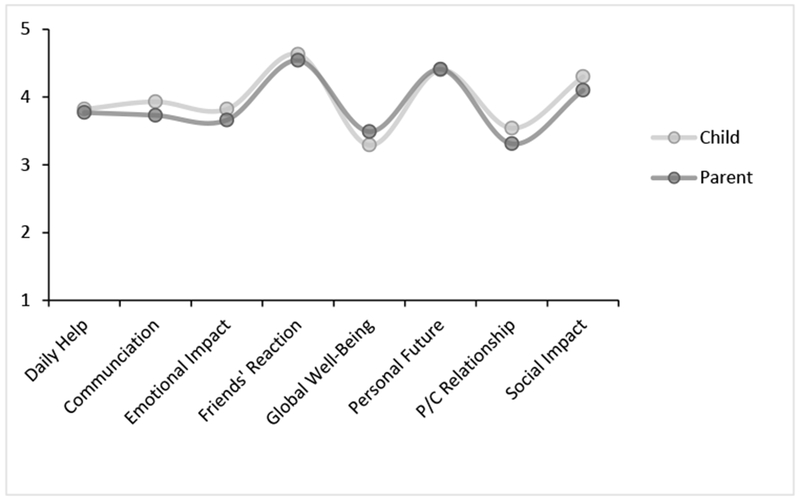
Parental Migraine Illness Impact by Child and Parent Report
Between groups (children vs. parents) there were no significant differences between average ratings of parental migraine impact on children; however, when evaluated within participant dyads (each parent matched with their own child) child and parent ratings of parental migraine impact were not strongly associated (Table 3). The strongest correlation between parent and child ratings of parental migraine impact was in the domain of Social Impact (ρ = .55, p < .001), which is considered a moderate correlation. Correlations between parent and child ratings of the Parent/Child Relationship (ρ = .13, p = .416) and Friends Reactions (ρ = .18, p = .257) subscales were very small and not significant.
Higher attack frequency was associated with higher child-rated impact (e.g., lower scores) on Global Well-Being (ρ = −.35, p = .028) and Impact on Personal Future (ρ = −.41, p = .009) subscales. Higher attack pain intensity was associated with higher child-rated impact (e.g., lower scores) on Burden of Daily Help (r = −.34, p = .031) and Emotional Impact (r = −.40, p = 0.010). Endorsing severe disability on the MIDAS was associated with higher child-rated impact (e.g., lower scores) on Global Well-Being [Severe MIDAS M = 2.99, SD = 0.81; Low-Moderate MIDAS M = 3.71, SD = 0.82; t(38) = 2.74, p = .009] and Impact on Personal Future [Severe MIDAS M = 4.20, SD = 0.76; Low-Moderate MIDAS M = 4.73, SD = 0.58; t(35.7) = 2.49, p = .017]. Children who also reported symptoms consistent with migraine (n = 21) reported greater impact of parental migraine on Global Well-Being [Child Endorsed Migraine M = 3.0, SD = 0.7; Child Did not Endorse Migraine M = 3.5, SD = 1.0; t(38) = 2.04, p = .048)].
Resources
The majority of children reported their only source of information about migraine was their parent (82.5%); however, 30.0% of children with migraine reported their parent did not speak to them about their disease (Table 4). Three-quarters of children broadly felt they had sufficient information about migraine (72.5%), and the vast majority felt they had support from friends and family (90.0%) and could talk to somebody about migraine if they wanted to (92.5%). Over half of children (57.5%) reported some kind of service or intervention to help them manage the impact of their parent’s migraine on their lives would be helpful. Approximately half of children reported it would be useful to have training for how to care for their parent with migraine (45.0%), with fewer interested in individual counseling (27.5%) and family counseling (20.0%) to help reduce the impact of migraine on the child (Table 4).
Table 4.
Child Ratings on the Parent Illness Impact Scale – Revised Resource Items
| Resource Item | N(%) of Children Endorsed |
|---|---|
| Do you have all the information you need about migraine? | 29 (72.5%) |
| Do you feel you know enough about what will happen in the future to your parent with migraine? | 25 (62.5%) |
| Do you rely on just your parent(s) for information about migraine? | 33 (82.5%) |
| Do you feel that there is somebody you can talk to about migraine if you want to? | 37 (92.5%) |
| Do you feel you have all the support you need from friends and family? | 36 (90.0%) |
| Do you have ways to cope with any anger you may feel? | 36 (90.0%) |
| Does your parent with migraine talk to you about their illness? | 28 (70.0%) |
| Would it help you to have contact with people in a similar situation? | 11 (27.5%) |
| Would it help you to have training in how to care for your parent with migraine? | 18 (45.0%) |
| Do you think it would be helpful if you had the opportunity to speak to someone professionally (i.e., a counselor)? | 11 (27.5%) |
| Do you think it would help you to have counseling as a family? | 8 (20.0%) |
| Is help available in caring for your parent with migraine? | 19 (47.5%) |
| Do you think more help should be provided to help care for your parent with migraine? | 6 (15.0%) |
| Do you feel it would help you if you were able to talk to local services about any help provided (i.e., social services)? | 3 (7.5%) |
Discussion
In this observational study, children aged 11–17 living with a parent with migraine reported moderate levels of parental migraine impact on their lives. Children and parents reported the greatest impact of migraine on children’s global well-being (physical and emotional health and sleep), parent/child relationships (difficulty understanding each other, embarrassed by parent’s migraine) , burden of daily help (e.g., taking on additional chores and responsibilities at home, including caring for the parent), and emotional impact (e.g., negative and anxious emotions, and impact on schoolwork).
The magnitude of parental migraine impact on children’s burden of daily help, parent/child relationship, emotional impact, and social impact (e.g., spending less time with friends and at social activities, having less independence, migraine impacting the child’s routine) was similar to the parental illness impact reported in previous studies by adolescent (n = 51) and adult children (n = 118) of parents with three other neurological conditions: Parkinson’s disease, multiple sclerosis, and stroke (16). This is consistent with literature directly evaluating differences in individual-level patient burden across neurological conditions. For example, a European study found people with migraine (n = 80) reported equivalent or higher levels psychosocial burden when compared to 80 patients with epilepsy, stroke, multiple sclerosis or Parkinson’s disease (20). This study adds to the literature which confirms that migraine can account for substantial burden in the lives of each individual person with migraine (and his/her children), at least on par with other neurological diseases which have higher mortality rates. In other words, the global burden of migraine is not solely accounted for by a high prevalence; individual people with migraine and their families experience clinically significant burden at least on par with other neurological diseases widely considered to be burdensome. On the other hand, children and parents reported relatively low levels of child impact of parental migraine on personal future. Compared to other neurological diseases studied, such as Parkinson’s disease and multiple sclerosis (16), the natural course of migraine is typically associated with fewer symptoms and more independence in later life; this could account for the low levels of impact children anticipated their parent’s migraine would have on their personal futures. Future studies should evaluate parental illness impact using the same inclusion criteria, recruitment strategy, and measure in multiple chronic illnesses to be able to more directly compare the differential impact of parental chronic illness on children.
On average, children and parents agreed about the level of migraine impact on children’s lives across various domains. However, within child-parent dyads, the story was more complicated. Parents and children had only moderate amounts of agreement on the impact of parental migraine on the child across most domains assessed. Further, child-parent dyads did not agree significantly on the impact of the parent’s migraine on the parent-child relationship, or on the child’s friends’ reactions. Perhaps the social impact domain is external to the child and easier to observe and quantify as a parent, but it may be more difficult for parents to perceive and accurately estimate these more subtle, internal and subjective constructs. This lack of agreement is particularly problematic when considering identifying families who most need an intervention to mitigate the impact of a parent’s migraine on the relationships within the family unit. These results are consistent with the pediatric psychiatric psychometric literature which has found somewhat stronger agreement between parent and child reports of the child’s externalizing symptoms compared to the child’s internalizing symptoms, particularly in older children (22). This finding highlights the importance of asking children how their parent’s migraine impacts their lives, rather than relying solely on parent report to elucidate the impact of parental migraine on children.
Higher severity of parental migraine characteristics, including attack frequency, attack pain intensity, and migraine-related disability, were all associated with greater impact of parental migraine on children. Higher headache attack frequency/days per month and severe MIDAS score (a measure of migraine-related disability in multiple important life domains) were associated with greater impact on children’s global well-being and personal future. This is consistent with the CaMEO study, which found that chronic migraine (vs. episodic migraine) was associated with greater impact of parental migraine on all domains assessed in that study, which included loss of parental support, emotional impact, interference with school, and missed activities and events (13). Together, these studies suggest that chronic and higher frequency episodic migraine may be a particularly important patient population in which to evaluate family migraine burden and offer interventions to mitigate the burden of migraine on children. This study further found that higher migraine attack pain intensity was associated with greater impact on burden of daily help and emotional health. These results suggest parents with more severe migraine attacks in terms of both pain intensity and associated symptoms may require greater assistance, be less available to assist with schoolwork, and children may end up taking on more household responsibility, while feeling more sad and anxious about their parent’s migraine. Thus, people with high migraine attack pain intensity and associated symptoms may also be a patient population in which researchers and providers should evaluate the burden of migraine on children and consider making interventions available, including family education, counseling, and/or social services.
Most children reported their parent was their only source of information about migraine. The impact of parental migraine on the parent-child relationship, along with the internalized migraine stigma experienced by people with migraine (21), suggests relying on one’s parent with migraine as the sole source of information about migraine is not ideal. These results highlight the responsibility of the headache clinical and research community to provide public access to high-quality information about migraine, as well as living with a parent with migraine.
More than half of the children interviewed reported that some kind of intervention or assistance in managing the impact of their parent’s migraine on their lives would be useful. These resources are not widely used or commonly available in the majority of headache treatment settings, nor do headache clinics typically have relevant referral resources. Clinical educators and researchers should consider several possible avenues for future research, including: 1) educational interventions that provide accurate age-appropriate information about migraine to children of parents with migraine, which could be integrated into typical clinic flow in headache treatment settings, 2) family counseling interventions, which could be integrated in typical clinic flow in multidisciplinary headache treatment settings and may require referral to family counseling in other settings, and 3) provision of social services and accommodations to ease the burden of parenting with migraine, which would require integration of social work into clinic flow.
More than half of children who responded to the surveys in this study met criteria for migraine. This is far greater than the 10.1% estimated population prevalence of pediatric migraine (23). Although children with and without migraine reported broadly similar impact of parental migraine, children with migraine reported greater impact on global well-being. Therefore, this group might be a particularly fruitful target for intervention development. Further, children with migraine are likely to have a parent with migraine (24, 25); therefore, a pediatric headache treatment clinic could be an advantageous setting in which to develop these intervention strategies.
Limitations
Although both in-clinic and online recruitment methods were utilized, the sample was highly intrinsically motivated to participate and remained predominantly female, White/Non-Hispanic, highly educated, and married. We could reasonably expect parental migraine impact on children to differ based on these characteristics. The study sample was also relatively small. Future studies should specifically sample fathers with migraine and a larger, more ethnically and educationally diverse sample of people with migraine to evaluate the impact of parental migraine on children in these groups. Not all children of parents who consented on their behalf completed the study, and parents of multiple children were able to select which child would participate in the study. For these reasons, results may not generalize to children who are less interested in, or engaged with, their parent’s migraine, whom parents were unlikely to select for survey participation for any reason, or who chose not to participate for a range of other reasons. In particular, children who also have migraine, or who perceive greater burden because of their parent’s migraine, may have had greater intrinsic motivation to participate in the study. Although using a validated measure of parental illness impact has several advantages, including being able to compare this sample to previous studies in different neurologic conditions, it is also likely we failed to capture potentially important domains of the impact of parental migraine on children. Future studies should consider using both the PIIS-R (14) and the Impact of Migraine on Partners and Adolescent Children Scale (IMPACS) (26) and to more fully capture the impact of parental migraine on children. Finally, this study relied on survey methodology, which allowed us to evaluate the impact of parental migraine on children quantitatively. However, this restricted our sample to children aged 11-17, as children younger than age 11 typically cannot complete surveys without adult assistance. Future studies should consider qualitatively evaluating the impact of parental migraine on children younger than 11 through both child and parent report. Future studies should also consider evaluating the role of migraine in the family, including whether one or both parents have migraine, whether other family members also have migraine, and whether the parent with migraine is the primary caregiver. Future work could also evaluate the presence of psychiatric symptoms or other comorbid conditions as moderators of the child’s perception of parental migraine burden, impact and disability.
Table 1.
Parent Demographics and Clinical Characteristics
| Variable | M (SD) or N (%) |
|---|---|
| Demographics | |
| Age | 43.5 (6.3) |
| Gender | |
| Female | 39 (97.5%) |
| Male | 1 (2.5%) |
| Race and Ethnicity | |
| White/Non-Hispanic | 35 (87.5%) |
| All Else | 5 (12.5%) |
| Marital Status | |
| Married | 31 (77.5%) |
| Single, Separated or Divorced | 9 (22.5%) |
| Education | |
| Some High School - High school Graduate/GED | 5 (12.5%) |
| Some College | 9 (22.5%) |
| College Graduate | 13 (32.5%) |
| Some Graduate School | 4 (10.0%) |
| Graduate Degree | 9 (22.5%) |
| Employment Information | |
| Employment – Self | |
| Full-Time | 15 (37.5%) |
| Part-Time | 14 (35.0%) |
| Not Currently Working | 11 (27.5%) |
| Employment – Partner (n = 32) | |
| Full-Time | 30 (93.8%) |
| Not Currently Working | 2 (3.1%) |
| Household Income (n = 34) | |
| Less than $25,000 | 5 (14.7%) |
| $25,000-$49,999 | 8 (23.5%) |
| $50,000-$74,999 | 6 (15.0%) |
| $75,000-$99,999 | 6 (15.0%) |
| $100,000-$199,999 | 5 (12.5%) |
| $200,000+ | 4 (10.0%) |
| Breadwinner Status | |
| Respondent is the breadwinner | 11 (27.5%) |
| Partner is the breadwinner | 22 (55.0%) |
| Both partners are breadwinners | 7 (17.5%) |
| Clinical Characteristics | |
| Headache Attack Frequency/Month | 6.8 [4.0-15.0] |
| Average Headache Attack Pain Intensity | 6.8 (1.7) |
| MIDAS Disability | |
| Low to Moderate | 15 (37.5%) |
| Severe | 25 (62.5%) |
N = 40 unless otherwise noted. MIDAS = Migraine Disability Assessment.
Table 2.
Child Demographics and Clinical Characteristics
| Variable | M (SD) or N (%) |
|---|---|
| Age | 13.6 (1.8) |
| Gender | |
| Female | 20 (50.0%) |
| Male | 20 (50.0%) |
| Race and Ethnicity | |
| White, Non-Hispanic | 38 (92.7%) |
| All Else | 3 (7.3%) |
| Household Composition | |
| Two-parent household | 33 (82.5%) |
| Single-parent household | 7 (17.5%) |
| Endorsed Migraine Criteria | |
| Yes | 21 (52.5%) |
| No | 19 (47.5%) |
Note. N = 40.
Acknowledgements:
The authors would like to acknowledge the contributions of the staff Northwell Health and TrialSpark for their contributions to the recruitment effort, and to all of the patients and their children who participated in this study.
Financial Support: This work was supported by institutional funds from Yeshiva University and the National Institute of Neurological Diseases and Stroke (K23 NS096107 PI: Seng).
Conflict of Interest Statements: Elizabeth Seng, Ph.D., in the past 12 months, has received funding from the National Institute of Neurological Diseases and Stroke (K23 NS096101 PI: Seng) and served as a consultant for GlaxoSmithKline and Eli Lilly. Emily D. Mauser, M.A., Maya Marzouk, B.S., and Zarine S. Patel, M.A. have no conflicts to report. Noah Rosen, M.D., has received honoraria from Allergan, Amgen, Avanir, Eli Lilly, Promius and Teva and is on the editorial board of Current Pain and Headache Reports and the Journal of Headache and Pain. Dawn C. Buse, Ph.D., in the past 12 months, has received grant support and honoraria from Allergan, Amgen, Avanir, Biohaven, Eli Lilly, Promeius and Teva. She is on the editorial board of Current Pain and Headache Reports, the Journal of Headache and Pain, Pain Medicine News, and Pain Pathways magazine.
Abbreviations:
- CaMEO
Chronic Migraine Epidemiology and Outcomes
- ICHD-3
International Classification of Headache Disorders-3
- PIIS-R
Parental Illness Impact Scale-Revised
- MIDAS
Migraine Disability Assessment
References
- 1.Blumenfeld AM, Varon SF, Wilcox TK, Buse DC, Kawata AK, Manack A, et al. Disability, HRQoL and resource use among chronic and episodic migraineurs: results from the International Burden of Migraine Study (IBMS). Cephalalgia. 2011;31(3):301–15. [DOI] [PubMed] [Google Scholar]
- 2.GBD 2015 NDCG. Global, regional, and national burden of neurological disorders during 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Neurol. 2015;16:877–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Burch RC, Loder S, Loder E, Smitherman TA. The prevalence and burden of migraine and severe headache in the United States: updated statistics from government health surveillance studies. Headache. 2015;55(1):21–34. [DOI] [PubMed] [Google Scholar]
- 4.Burch R, Rizzoli P, Loder E. The Prevalence and Impact of Migraine and Severe Headache in the United States: Figures and Trends From Government Health Studies. Headache. 2018;58(4):496–505. [DOI] [PubMed] [Google Scholar]
- 5.Buse D, Manack A, Serrano D, Reed M, Varon S, Turkel C, et al. Headache impact of chronic and episodic migraine: results from the American Migraine Prevalence and Prevention study. Headache. 2012;52(1):3–17. [DOI] [PubMed] [Google Scholar]
- 6.Stewart WF, Wood GC, Manack A, Varon SF, Buse DC, Lipton RB. Employment and work impact of chronic migraine and episodic migraine. J Occup Environ Med. 2010;52(1):8–14. [DOI] [PubMed] [Google Scholar]
- 7.Stewart WF, Bruce C, Manack A, Buse DC, Varon SF, Lipton RB. A case study for calculating employer costs for lost productive time in episodic migraine and chronic migraine: results of the American Migraine Prevalence and Prevention Study. J Occup Environ Med. 2011;53(10):1161–71. [DOI] [PubMed] [Google Scholar]
- 8.MacGregor EA, Brandes J, Eikermann A, Giammarco R. Impact of migraine on patients and their families: the Migraine And Zolmitriptan Evaluation (MAZE) survey--Phase III. Curr Med Res Opin. 2004;20(7):1143–50. [DOI] [PubMed] [Google Scholar]
- 9.Lipton RB, Bigal ME, Kolodner K, Stewart WF, Liberman JN, Steiner TJ. The family impact of migraine: population-based studies in the USA and UK. Cephalalgia. 2003;23(6):429–40. [DOI] [PubMed] [Google Scholar]
- 10.Dueland A, Leira R, Burke T, Hillyer E, S. B. The impact of migraine on work, family, and leisure among young women: a multinational study. Curr Med Res Opin. 2004;20(10):1595–604. [DOI] [PubMed] [Google Scholar]
- 11.Smith R Impact of Migraine on the Family. Headache. 1998;38(6):423–6. [DOI] [PubMed] [Google Scholar]
- 12.Buse DC, Scher AI, Dodick DW, Reed ML, Fanning KM, Manack Adams A, et al. Impact of Migraine on the Family: Perspectives of People With Migraine and Their Spouse/Domestic Partner in the CaMEO Study. Mayo Clin Proc. 2016. [DOI] [PubMed] [Google Scholar]
- 13.Buse DC, Powers SW, Gelfand AA, VanderPluym JH, Fanning KM, Reed ML, et al. Adolescent Perspectives on the Burden of a Parent’s Migraine: Results from the CaMEO Study. Headache. 2018;58(4):512–24. [DOI] [PubMed] [Google Scholar]
- 14.Morley D, Selai C, Schrag A, Thompson AJ, Jahanshahi M. Refinement and validation of the Parental Illness Impact Scale. Parkinsonism Relat Disord. 2010;16(3):181–5. [DOI] [PubMed] [Google Scholar]
- 15.Schrag A, Morley D, Quinn N, Jahanshahi M. Development of a measure of the impact of chronic parental illness on adolescent and adult children. The parental illness impact scale (Parkinson’s disease). Parkinsonism Relat Disord. 2004;10(7):399–405. [DOI] [PubMed] [Google Scholar]
- 16.Morley D, Selai C, Schrag A, Jahanshahi M, Thompson A. Adolescent and adult children of parents with Parkinson’s disease: incorporating their needs in clinical guidelines. Parkinson Dis. 2011;2011:951874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lipton RB, Diamond S, Reed M, Diamond ML, Stewart WF. Migraine diagnosis and treatment: results from the American Migraine Study II. Headache. 2001;41(7):638–45. [DOI] [PubMed] [Google Scholar]
- 18.Lipton R, Diamond S, Reed M, Diamond M, Stewart W. Migraine diagnosis and treatment: Results from the American Migraine Study II. Headache. 2001;41:638–45. [DOI] [PubMed] [Google Scholar]
- 19.Stewart WF, Lipton RB, Dowson AJ, Sawyer J. Development and testing of the Migraine Disability Assessment (MIDAS) Questionnaire to assess headache-related disability. Neurology. 2001;56(6,Suppl1):S20–S8. [DOI] [PubMed] [Google Scholar]
- 20.Leonardi M Higher burden of migraine compared to other neurological conditions: results from a cross-sectional study. Neurol Sci. 2014;35 Suppl 1:149–52. [DOI] [PubMed] [Google Scholar]
- 21.Young WB, Park JE, Tian IX, Kempner J. The stigma of migraine. PloS one. 2013;8(1):e54074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van der Ende J, Verhulst FC, Tiemeier H. Agreement of informants on emotional and behavioral problems from childhood to adulthood. Psychol Assess. 2012;24(2):293: 300. [DOI] [PubMed] [Google Scholar]
- 23.Merikangas KR. Contributions of epidemiology to our understanding of migraine. Headache. 2013;53(2):230–46. [DOI] [PubMed] [Google Scholar]
- 24.Eidlitz-Markus T, Haimi-Cohen Y, Zeharia A. Association of age at onset of migraine with family history of migraine in children attending a pediatric headahe clinic: a retrospective cohort study. Cephalaltia. 2015; 35(8): 722–727. [DOI] [PubMed] [Google Scholar]
- 25.Jeong YJ, Lee YT, Lee IG, Han JY. Primary headaches in children and adolescents – experiences at a single headache center in Korea. BMC Neurology. 2018; 18(1): 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lipton RB, Buse DC, Adams AM, Varon SF, Fanning KM, Reed ML. Family Impact of Migraine: Development of the Impact of Migraine on Partners and Adolescent Children (IMPAC) Scale. Headache. 2017;57(4):570–85. [DOI] [PMC free article] [PubMed] [Google Scholar]


