Abstract
Objectives
We aimed at exploring the underlying mechanisms and contextual conditions by which leadership may influence ‘public service motivation’ of health providers in Moroccan hospitals.
Design
We used the realist evaluation (RE) approach in the following steps: eliciting the initial programme theory, designing the study, carrying out the data collection, doing the data analysis and synthesis. In practice, we adopted a multiple embedded case study design.
Settings
We used purposive sampling to select hospitals representing extreme cases displaying contrasting leadership practices and organisational performance scores using data from the Ministry of Health quality assurance programmes from 2011 to 2016.
Participants
We carried out, on average, 17 individual in-depth interviews in 4 hospitals as well as 7 focus group discussions and 8 group discussions with different cadres (administrators, nurses and doctors). We collected relevant documents (eg, performance audit, human resource availability) and carried out observations.
Results
Comparing the Intervention-Context-Actor-Mechanism-Outcome configurations across the hospitals allowed us to confirm and refine our following programme theory: “Complex leaders, applying an appropriate mix of transactional, transformational and distributed leadership styles that fit organisational and individuals characteristics [I] can increase public service motivation, organisational commitment and extra role behaviours [O] by increasing perceived supervisor support and perceived organizational support and satisfying staff basic psychological needs [M], if the organisational culture is conducive and in the absence of perceived organisational politics [C]”.
Conclusions
In hospitals, the archetype of complex professional bureaucracies, leaders need to be able to balance between different leadership styles according to the staff’s profile, the nature of tasks and the organisational culture if they want to enhance public service motivation, intrinsic motivation and organisational commitment.
Keywords: human resource management, leadership, public service motivation, complex leadership, basic psychological needs, health workers
Strengths and limitations of this study.
Realist evaluation (RE) is useful in explaining how, why and under which conditions an intervention or a social phenomenon (leadership in our study) generates a particular outcome (in casu public service motivation).
Continuous refinement of programme theories through RE cycles allows for a cumulative process of knowledge creation by constant shuttling across cases from theory to empirical data and back.
The time and resource constraints of the PhD research project, of which this study is a part, precludes testing and validating existing measurement scales of concepts such as public service motivation, perceived organisational support and organisational commitment.
Introduction
Health workers’ performance has received increased attention from policy makers, scholars and global health organisations,1–3 and is recognised as an essential driver for the achievement of the sustainable development goals,4 the implementation and the scale up of effective public health sectors reforms .5–9
Motivation in the public sector
In low-income and middle-income countries (LMICs), poor performance of health workers is a critical barrier to quality of care and to the implementation of health policies in general.5 10 This often stems from a lack of motivation and to negative attitudes of health workers in the provision of care.11–15
The motivation of health workers is recognised as a critical determinant of the performance of health workers in public performance.2 5 6 16 While staff availability, knowledge and skills are essential in health service delivery, they are not sufficient to ensure good health worker performance. This critically depends on staff motivation, and in public services specifically on their willingness to pursue public service values and work in line with the best interest of patients.16–19
This notion is encompassed by the concept of public service motivation (PSM), understood as the altruistic desire of health workers to serve the common interest and to help patients and their families regardless of financial or external rewards. PSM has been shown to be key to the performance of public servants in public administration20 21 and in the health sector.22 23
Since 1990, public management scholars have been developing the concept of ‘public service motivation’ (PSM), defined as “an individual’s predisposition to respond to motives grounded primarily or uniquely in public institutions and organizations”.24 PSM involves a set of “beliefs, values and attitudes that go beyond self-interest and organizational interest, that concern the interest of a larger political entity, and that motivate individuals to act accordingly whenever appropriate”.25 From this perspective, health workers can be driven by an altruistic desire to serve the public interest and the population.26–30 Research in public sector settings and in healthcare produced evidence on the positive effect of PSM on job satisfaction, reduced turnover and individual performance.28 29 31–34 Within the field of PSM, research has focused on how managers and leaders can enhance PSM among public servants.35–39
This perspective on the motivation offers an alternative perspective to the recent trends in health system performance management reforms inspired from new public management, including pay for performance and contracting out, which focuses on extrinsic motivation of health providers, and risks to crowd out intrinsic motivation.30 Such strategies may also generate negative self-interested behaviours, goal displacement and mistrust.30 40–44
Leadership in the health sector
In Morocco, research evidence points to how a lack of motivation and poor leadership of health managers may have hampered the performance of health workers, the quality of care and the scaling up of proven effective health policies45–52 and quality assurance programmes.53 54
In LMIC, health managers often display poor leadership practices either by avoiding getting involved, delaying decisions (laissez-faire leadership) or by overemphasising top-down controlling behaviours perceived as inefficient in the motivation of health workers.55–59
‘Traditional’ leadership theories emphasise the importance of individual leadership and leader–employee exchange relationships. They comprise transactional leadership (where leaders focus on top down contingent rewards and sanctions) and transformational leadership (where leaders focus on inspiring staff, infusing jobs with meaning and acting as a role model).60 Recent leadership theories emphasise the need for more complex approaches that allow for better adaptation to the complex social nature of healthcare organisations.61–63 Complex leadership scholars highlight the multilayered nature of effective leadership, which includes information sharing, distributed leadership and support for lower level cadres. They define complex leadership as the ability of leaders in complex unpredictable situations to balance between transactional, transformational and distributed leadership so as to fit the nature of task, type of staff and organisational characteristics.61 62 64–66
The relationship between leadership and PSM
Complex processes underlie the effect of leadership on PSM, and they are conditioned by contextual factors (professionalism, religion and family education)67–73 and organisational factors (organisational culture74 75 and job characteristics28 29).
Most PSM research in the field of public administration relies on quantitative measures of the effect of leadership on PSM. Little attention has been paid to the mechanisms underlying this relationship in healthcare and public service settings,16 31 33 35 37 39 76–78 and the existing studies often display methodologies challenges.79 80 Understanding these mechanisms is valuable in the sense that it can guide health managers in developing appropriate leadership and managerial practices that reinforce organisational value systems, and foster health workers’ PSM and intrinsic motivation, and consequently their performance.59 81–83
In response, we set out to explore the causal processes through which leadership, context and organisational attributes influence public service motivation of health workers in Moroccan hospitals. The research questions we address are as follows: (1) How does leadership influence public service motivation of health workers? and (2) Which organisational or contextual conditions underlie the effect of leadership on PSM? This study is part of a larger study on the nature and effects of leadership practices on health workers in four Moroccan hospitals.
Methods
We adopted the RE approach.84 RE aims at identifying causal mechanisms that explain how, why and under which conditions an intervention or a social phenomenon (leadership in our study) generates a particular outcome (in casu PSM).84 Realists posit that causal mechanisms are generative in nature and embedded in a stratified social reality; they reside in the interplay between individuals, institutional and structural factors.85 86
We applied the steps of the realist research cycle85 87 to structure our study: (1) eliciting the initial programme theory, (2) designing the study, (3) carrying out the data collection, (4) analysing the data and (5) synthesis. We refer to our paper reporting on a case study of leadership for more details on the realist approach.88
Step 1: eliciting the initial programme theory
Our scoping review of complex leadership62 allowed us to elicit an initial programme theory (PT) on the relationship between leadership and motivation. It was further developed through a first exploratory case study (coded NHMH) (see Belrhiti et al 88), and this led to the initial PT that is the starting point of this study:
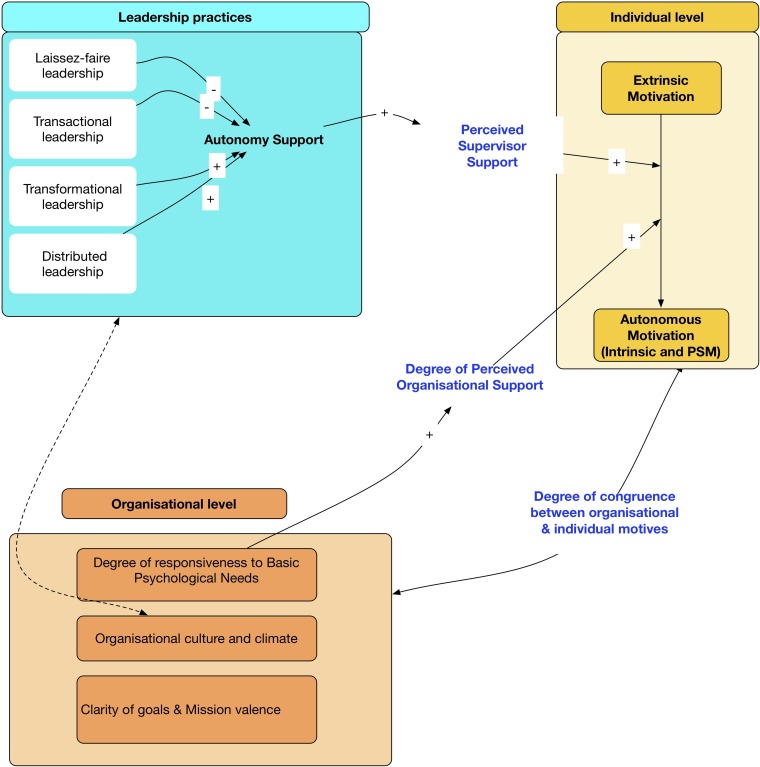
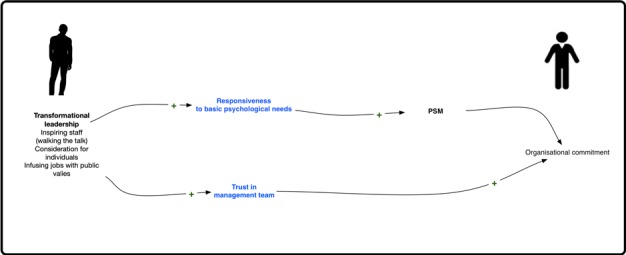
Complex leaders adopt an appropriate mix of transactional, transformational and distributed leadership styles that fit the mission, goals, organisational culture, nature of the tasks of the organisation and the individual characteristics of the personnel. This adaptation of leadership style enhances staff perceived supervisor support and perceived organizational support, and contributes to the satisfaction of basic psychological needs of the staff (figure 1).
Figure 1.
Programme theories. PSM, public service motivation.
As we described before,88 the underlying theories used to build our above-mentioned programme theory rely on two mechanisms that have shown to be important in explaining the complex relationship between leadership and motivation89–91: (1) the satisfaction of basic psychological needs, based on self-determination theory92 (see box 1), and (2) perceived supervisor support and perceived organisational support89 90 93 (see box 2).
Box 1. Definition of basic psychological needs.
According to self-determination theory, every individual thrive to satisfy three basic psychological needs (autonomy, competence, relatedness). Autonomy corresponds to the sense of volition and willingness ones feel when undertaking specific behaviours. This allow staff to self-endorse their actions. Competence needs means the feeling self efficacy when experiencing work opportunities that allow individuals to express and use their abilities and skills. Relatedness means that staff need to feel mutual respect, consideration from others, connectedness and a sense of belonging to a social group.
Box 2. Perceived organisational and supervisor support.
Perceived organisational support (POS) is understood as the beliefs of health workers about the extent to which the organisation (eg, top management teams) values their efforts and their psychological well-being.
Perceived supervisor support (PSS) is identical to the former but focuses on the relationship between staff and their supervisor.
In this study, we adopted a dynamic perspective of leadership which we considered as a multilevel process embedded in a multilayered social and organisational context.62 64 94–98 From this perspective, leadership is shaped by the organisational culture and by how staff interpret their organisational context (organisational climate).99–101
We mean by the organisational culture “the shared values, underlying assumptions and expectations that characterise organisational membership”.102 Different types of organisational culture are presented in box 3.103 The visible aspect of the organisational culture is represented by the organisational climate (‘the tip of the iceberg’) and is “the visible behaviour of group members”.99
Box 3. Types of organisational culture according to Cameron and Quinn.
Hierarchical culture: strong emphasis on stability, predictability and efficiency. Formalisation, procedures and rules govern individual behaviour.
Clan culture: emphasis on cohesion, teamwork, high levels of employee morale, employee involvement and commitment within an autonomy supportive environment.
Market culture: emphasis on employee productivity, results and profit orientation, individualism and competitiveness, in an environment that is considered as hostile.
Adhocratic culture: emphasis on creativity, innovation, individuality, experimentation, risk taking and adaptability. Power is decentralised to task teams.
We adopt the definition of organisational climate of Bock e t al: the “contextual situation at a point in time and its link to the thoughts, feelings, and behaviours of organizational members. Thus, it is temporal, subjective, and often subject to direct manipulation by people with power and influence”.104 It is a multidimensional concept that includes role conflict and ambiguity, professional and organisational esprit, job challenges, workgroup cooperation and mutual trust.105
Figure 1 shows our programme theory (PT) and the complex relationship between leadership, individual motivation and organisational characteristics (organisational culture and climate, mission and goals, and degree of responsiveness to basic psychological needs).88 The quality and type of staff motivation (extrinsic vs autonomous motivation, including PSM and intrinsic motivation) depends on the degree of autonomy support by leaders, and consequently their perceived supervisor support (which in itself is increased by transformational and distributed leadership and reduced by laissez-faire and transactional leadership). Autonomous motivation is enhanced when staff have positive levels of perceived organisational support, which depends on the degree of responsiveness of top management teams to staff’s basic psychological needs and the congruence between the organisational culture and the individual values.
More specifically, we identified four causal configurations (figure 1):
Configuration 1
Laissez-faire leadership decreases the levels of perceived organisational support and staff motivation by being less responsive to their basic psychological needs of autonomy, competence and relatedness. Lack of vision and goal setting contributes to a climate of ambiguity and role conflict. The inadequate enforcement of the hierarchical structure and high job pressure can contribute to mistrust between administration and staff.
Configuration 2
Transactional leaders can improve extrinsic motivation of staff if they offer the necessary support and ensure adequate working conditions. By improving the latter, transactional leaders reduce job pressure, and by implementing a clear hierarchical line, they reduce role conflicts.
Configuration 3
By showing individual consideration and communicating clearly about mission valence, transformational leaders enhance self-esteem of staff, perceived supervisor support and satisfaction of their autonomy needs. This in turn contributes to staff commitment, mutual trust and respect between the management team and staff.
Configuration 4
Distributed leadership can contribute to improved communication and interaction between staff from different units, to problem solving and a reinforced clan culture. Distributing leadership roles and embedding them throughout the organisation, combined with engaging staff in decision making, contributes to staff’s perceived autonomy and organisational commitment, which in turn leads to extra role activities.
In this study, we zoom in on the role of public service motivation. We assume that leaders who stimulate staff’s awareness of the value of their work to society and its contribution to the public good may enhance PSM and intrinsic motivation. Leaders who are responsive to the basic psychological needs of their staff are likely to stimulate the internalisation of public values and may shift the locus of individual motivation from extrinsic to more autonomous forms of motivation.106 This requires a conducive organisational culture and absence of conflicts between individual and organisational values. We hypothesise that the specific attributes of the Moroccan health system, and specifically its hierarchical organisational culture, may impede the emergence of PSM.
Step 2: study design—a multiple embedded case study design
We adopted a multiple case study design107 because it fits the exploration of multifaceted complex phenomena, such as PSM, in real-world settings (in our case in four hospitals). We defined the case as the relationship between leadership and ‘public service motivation’. We took a hospital as the unit of analysis. Purposive sampling allowed us to select hospitals that would allow us to test the PT. We selected hospitals representing extreme cases, displaying contrasting organisational performance and leadership practices.108 109 To select hospitals, we used data from the Ministry of Health’s quality assurance programme called ‘concours qualité’ from 2011 to 2016.110 111 More specifically, we used the leadership scores and the overall organisational quality performance scores (table 1). We refer to Sahel et al 54 for a discussion of the ‘concours qualité’.
Table 1.
List of high-performing and low-performing hospitals (Ministère de la santé du Maroc, 2011 and 2016 report)
| Hospital | Size (No. of beds) | Performance scores, % | Leadership score (2016) | |
| 2011 | 2016 | |||
| NHMH | <120 | 65 | 80.33 | 75.76 |
| EJMH | >240 | 46 | 65.98 | 57.61 |
| SMBA | >240 | 44 | 20.01 | 14.54 |
| RKMH | <120 | 44 | 18.91 | 6.97 |
We purposefully selected two well-performing hospitals with high leadership scores (NHMH and EJMH) and two poor-performing hospitals with low leadership scores (RKMH and SMBA) (table 1). This selection was informed by independence of cases, variation in hospital size (seeking to have one large and one small sized hospital in each category), variation in location (urban, periurban, rural) and accessibility to the first author.
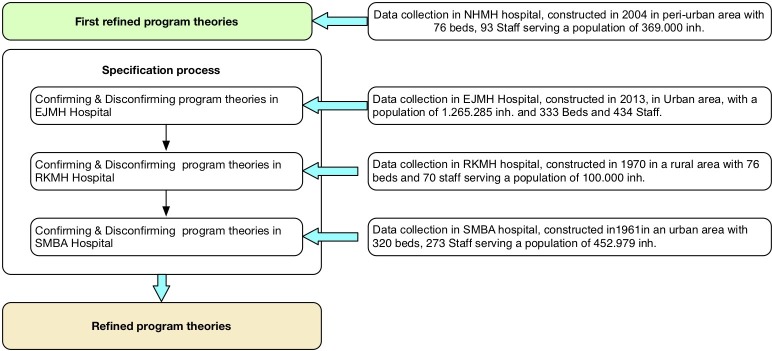
RE seeks to refine PTs through a process of specification: the PT is gradually refined by testing it in different settings or in different cases. For this study, we started the data collection in NHMH and developed a first refined PT. This was then tested in EJMH and the poor-performing hospitals RKMH and SMBA. The analysis of each site led to successive refinement, confirmation or disconfirmation of the elements of the initial PT.
Step 3: data collection
We based the choice of the data collection methods on our PT (figure 1) to ensure that data would allow us to test the initial PT. We used interviews, focus group discussions and document review (see figure 2). We collected data during the period January–June 2018.
Figure 2.
Case studies and data collection, Morocco, January–June 2018.
Interviews
In each hospital, we interviewed health professionals, and senior, middle and operational managers. We explored the antecedents of PSM, its expression and the relationship with leadership and management practices, organisational structure and cultural context. We used open-ended interview guides tailored to each category of respondents (online supplementary file 1). We collected data until saturation was attained. In the first site (NHMH), we carried out 18 individual in-depth interviews (IDIs). Subsequently, we carried out 17, 16 and 17 IDIs in EJMH, RKMH and SMBA, respectively. Each respondent was anonymised and given a unique identifier. Sociodemographic characteristics of the respondents are summarised in table 2.
Table 2.
Respondent characteristics
| NHMH | EJMH | RKMH | SMBA | |
| Managerial function | ||||
| Senior managers | 4 | 4 | 3 | 4 |
| Middle managers | 3 | 7 | 2 | 5 |
| Line managers | 5 | 2 | 4 | 3 |
| Operational staff | 20 | 30 | 17 | 33 |
| Total | 32 | 43 | 26 | 45 |
| Professional profile | ||||
| Doctors | 13 | 14 | 4 | 14 |
| Pharmacist | 1 | 3 | 1 | 1 |
| Nurses | 14 | 15 | 14 | 20 |
| Administrators | 4 | 11 | 7 | 10 |
| Total | 32 | 43 | 26 | 45 |
| Age category | ||||
| 20–30 | 6 | 3 | 5 | 3 |
| 31–40 | 11 | 11 | 6 | 17 |
| 41–50 | 9 | 10 | 9 | 11 |
| 51–63 | 6 | 19 | 6 | 14 |
| Total | 32 | 43 | 26 | 45 |
| Gender | ||||
| Female | 20 | 25 | 10 | 24 |
| Male | 12 | 18 | 15 | 21 |
| Total | 32 | 43 | 26 | 45 |
bmjopen-2019-033010supp001.pdf (50.1KB, pdf)
Focus group discussions
To further explore the key constructs used by interviewees in relation to ‘public service motivation’, we carried out seven focus group discussions and eight group discussions with different cadres (administrators, nurses and doctors). Group discussions were carried out whenever the number of participants did not reach the appropriate size (six to eight) to carry out focus group discussions (FGDs). This was encountered in practice in low staffed hospitals (RKMH and NHMH) particularly for doctors and administrative staff.
This allowed us to deepen the analysis across the different categories of health workers (managers, service providers). The first author led the FGD. Probes, follow-up questions and summarised key themes were used and verification from participants was sought at the end of each FGD.112 113 The FGD facilitator guide is presented in online supplementary file 2.
bmjopen-2019-033010supp002.pdf (63.8KB, pdf)
Respondents for the IDIs and the FGDs were identified through qualitative purposive sampling.108 All FGD and IDI were audio recorded with the exception of one interview. In this specific case, we took notes and transcribed the unrecorded interview using memory recall.114 Following guidance provided by Miles and Huberman115 and Krueger and Casey,112 we wrote a brief contact summary at the end of any contact with research participants. It included major themes and ideas arising after each interaction. All recordings were transcribed verbatim. Two researchers (ZB and BM) checked the transcripts for accuracy.
Document review
We collected documents at the study sites (760 pages) and at the Ministry of Health (460 pages). We focused on human resources availability and skill mix, the strategic plans of the hospitals, audit documents and quality assurance reports.
Observations
The first author carried out opportunistic observations (between appointments with interviewee), following the guidance described by Spradley.116 Close attention was paid to the interaction between supervisors and staff. We recorded our observations about feelings and goals expressed during informal interaction with hospital staff and external actors and the physical spaces.
Step 4: analysis
We carried out the data analysis following the ‘traditional’ analytical phases of compiling data, interpreting, discussion and drawing conclusions.109 Guided but not restricted by the initial PT, we coded all data sources (transcripts, contact summaries and field notes) using different coding techniques (concept, hypothesis and ‘in vivo’ coding)117 (see online supplementary file 3). We used the ICAMO (Intervention-Context-Actor-Mechanism-Outcome) heuristic to identify causal configurations. We revisited the data to test conjectural ICAMO configurations.118 We adopted a retroductive approach119 to contrast patterns of leadership effectiveness between different types of actors (doctors, nurses and administrators). We compared these patterns with the chronology of the Chief Executive Officer (CEO) succession periods. Guided by our research question, we focused on leadership effects on ‘public service motivation’ that emerged as a natural motivational driver of Moroccan public health workers.120
bmjopen-2019-033010supp003.pdf (58.1KB, pdf)
NVivo V.10 software121 was used to manage the data. Milestones in the coding process were discussed during research team meetings.
Step 5: synthesis
When the data from all sites were analysed, we compared the ICAMO configurations with the initial PT and modified it accordingly. We followed the RAMESES II reporting standards in writing the research report and this paper.87
Ethical considerations
We informed all interviewees before the start of data collection about the study objectives, topics, type of questions and their right to refuse being interviewed and to interrupt the interview at any time. This information was also provided in an information sheet and reiterated before the start of interview when the written consent procedure was explained. The respondents were asked to sign the informed consent form if they agreed to participate in the study. The forms were cosigned by the researcher and a copy was given to research participants.
Patient and public involvement statement
There was no direct patient involvement in this study.
Results
In this section, we first present for each hospital the main leadership and management practices, the perspective of staff, their views on public service motivation and a summary. Then we present a summary of the cross case analysis and the resulting refined programme theory.
EJM Hospital
Main leadership and management practices
In EJMH, there were two successive leadership periods. Between 2012 and 2015, CEO 1 had a transactional leadership style, relying on administrative procedures, assertion of power and compliance with rules and procedures. He was perceived by his staff as being distant and not responsive to their needs for professional autonomy. Conflicts and tensions with unions and doctors were high. He left in 2015.
CEO 1 was too strict in the application of the new hospital procedures. We could not discuss the rules with him. The hospital cannot be managed by strictly following the rules. For instance, in compliance with the new procedures, CEO 1 decided to implement night shifts for administrative staff and stopped the night shifts of nursing supervisors. The administrators did not accept to carry out this task because the new procedures did not mention who should do this and how this ‘overtime’ job would be reimbursed. (EJMH 3 administrator)
In mid-2015, CEO 1 was replaced by CEO 2. He was upto then the chief medical officer of the hospital and had quite some management experience. For instance, he was the director of EJMH between 2002 and 2006. In 2016, EJMH won the first price at the quality contest. CEO 2 had an explicit vision on leadership:
I had the chance to manage the hospital in 2002. This allowed me to really know the personal and vice versa. Now, we work as a team in that sense that staff are involved in decision making. This is very important. In a real world setting, participative decision making is very important, because you avoid many problems. When you involve them, you avoid resistance. If staff is involved from the beginning, they will adopt the solution and will not feel that it was imposed on them. This will be totally different if the solution was imposed on the staff. (…) When you involve staff in decision making, you build trust relationships. Trust relationships are very important in our context, where the hospital director has little power over his staff. [….] When we explain to staff well defined objectives. They know which organisational objectives to pursue. Achieving these goals at the operational level bring legitimacy to the hospital direction. It is important that health workers know that you are thriving to achieve these objectives. This is what I call credibility. (EJMH 7, CEO 2)
The perspective of staff
Leadership style
Our analysis shows that the staff found that the transactional leadership style of CEO 1 was incongruent with their professional values and their need for autonomy. This contributed to mistrust in the management team, low organisational commitment and a high level of tension with unions.
CEO 1, with whom I worked, was authoritative. This was not congruent with my values. I value participative decision making. I try to share with others, I need to be treated the same way by my superior. CEO 1 was just commanding: ‘Do this, give this to this person’. I would have accepted and engaged with him if he would have involved me in participative decision making with other members of the hospital committee, if he would have used polite inquiries, like “Would it be possible to do this?, rather than giving orders without listening to team members or involving them in decision making. (EJMH 25, pharmacist)
The participative decision-making style of CEO 2 and his consideration for individuals restored trust in the management team and reduced the tensions with the unions.
Now everything works smoothly. He does things that are right. He reacts to wrong doings. He is sympathetic with all staff. CEO 2 has a long experience. He knows everyone, he knows their personal characters, motivation and personal needs…. He is very successful in doing that! He knows how to reduce tensions between his close collaborators. He takes decisions smoothly. As a physician, he is able to reduce tensions between medical union representatives and internal coalitions within the medical departments. His door is open to everyone. He listens to staff. He does not rush decisions. He maintains a low level of tension within the hospital. He does not complicate things. The former CEO took rapid decisions and was facing much resistance […]. CEO 2 involves his close collaborators and chiefs of departments in decision making. This way, they adhere to his decisions. He listened to them. He has a participative leadership. (EJMH 25, pharmacist)
Public service motivation
Frontline providers said that compassion and self-sacrifice are important components of their public service motivation.
While recording electrocardiographs on patients, I was constantly communicating with them. Sometimes, women shared with me their feelings, their worries about their siblings, their fear of death, their personal life and stories about their deceased or ill husbands. They were often crying. I feel their sufferings as if I were living with them. (EJMH 17, nurse)
We found that the intrinsic motivation of health providers is sustained by their feelings of competence and their ability to adequately apply their professional skills and competencies.
I love my job. I chose deliberately to work at the emergency unit. I love working at the emergency unit. I am totally engaged. Handling serious medical emergencies is a motivation in itself. (EJMH 38, doctor)
Participative decision-making was perceived by staff as congruent with their professional identity and their public service values. It enhanced their self-esteem and satisfied their needs for autonomy and relatedness and increased their public service motivation. It also increased their perceived autonomy support.
Leaders needs to be fair, listen to our needs and resolve our organizational issues. Most importantly, they need to understand my professional needs, take into consideration my suggestions and contributions to work. This make me feel satisfied. In contrast, with the former leader, I was not feeling secured. He was exerting excessive control. I suffered the martyr!. I was constantly under constant threats. I even sent an administrative correspondence to the ministry of health against the injust treatment. I was just trying to do my job correctly!. (EJMH 17, nurse)
Summary
Our analysis showed that the transactional leadership of CEO 1 did not address the basic psychological needs of the staff and specifically the need for autonomy. This not only contributed to low organisational commitment and reduced public service motivation but also to tensions with the unions.
In contrast, CEO 2 had a transformational leadership style: he effectively understood how people are motivated, listened to them and clearly communicated his vision and objectives to the health workers. He showed genuine concern for the needs of his staff, effectively resolving problems through a constructive dialogue with informal leaders and union representatives. He also involved his close collaborators and heads of department in decision-making.
CEO 2 also stimulated the emergence of distributed leadership to lower levels of the organisation, which increased trust between the staff and the CEO, and reduced resistance to change. This was considered by mid-level managers as crucial in maintaining the ‘public service motivation’ of staff, in particular given the perceived limited decision spaces they have over their personal work. We saw that not only senior managers but also mid-level managers engaged in distributing leadership. For the latter, participating in decision-making increased their perceived leader support and satisfaction of their autonomy needs. This has enhanced their autonomous motivation (intrinsic and public service motivation).
RKM Hospital
Main leadership and management practices
This hospital has known two leadership periods since 2010. From 2010 to 2012, CEO 1 displayed transactional leadership: he assiduously monitored staff attendance, planned their shifts and dealt with his staff through administrative correspondence. He was confronted with staff resistance.
Because of shortage of intensive care anaesthetists, nurse anaesthetists often take over their tasks, like sedating patients in the operating theatre without medical supervision. When they were confronted with excessive control by the director, they stopped carrying out this ‘medical’ task. This has negatively impacted the continuity of surgical activities. In this case, nurses used their professional expertise as a source for discretionary power (eg, ability to intubate and sedate patients in the operating theatre).
(CEO 1) was suspicious and was strictly applying the regulations to correct the staff absenteeism. When the cat’s away, the mice will play. There were many conflicts, especially with nurse anesthesists who did not comply with the control of attendance. As a result, they stopped sedating patients and argued that they are not allowed to sedate patients without an intensive medical care anaesthetist. (RKMH8, close collaborator)
CEO 2 managed the hospital between 2012 and 2018. He favoured a distant laissez-faire leadership approach and was often absent. He would then be replaced by the chief nursing officer who adopted the same leadership style. The latter seemed overwhelmed by day-to-day operational management responsibilities. During our field work, we noted that the management of the hospital was poor. No organisational action plans were available, and there were no meetings. Strikingly, our FGD with nurses was the only meeting they attended in 3 years. We observed high level of absenteeism among hospital staff.
The perspective of staff
Leadership style
Our analysis shows that the close collaborators, administrators and technical staff appreciated the leadership of CEO 1 because he reduced role ambiguity and job pressure. However, nurses and doctors were unhappy with his overcontrolling behaviour and engaged in resistance. Also CEO 2 was appreciated by his close collaborators, now because of his gentle wording and good interpersonal management. However, doctors and nurses perceived his laissez-faire leadership as non-responsive to their needs in terms of resources and working conditions. This had led to reduce their public service motivation by reducing their willingness to improve service delivery and to work for the common good. Some have expressed that laissez-faire leadership has catalysed their intention to quit the public sector for good.
Nowadays the strength and pace of my motivation to improve the service quality has decreased. This is essentially due to the lack of responsiveness of the hierarchy to my needs. There is no response. Even though we are engaged to improve our working conditions and the panel of services, the lack of feed back from the management teams has stopped our willingness to improve health service delivery. I found myself complaining alone. This has reduced my attraction to improve public service. This has negatively impacted my psychological well being. In all cases, I get my salary at the end of the month, however, from my personal point of view, I could not contend my self to work without thriving to improve the quality of public service at the pediatric unit. My husband is telling me that improving service delivery in the public sector is not my mission and that I am not a sort of social reformer!!. I am always told that these poor working conditions are common in the public sector and I need to stop trying to work for the common good. My motivation has decreased for while now. But I hope later to try again with the new chief provincial hospital that has recently been appointed. Maybe, he will be more responsive to our needs than the former. If in the coming three years this does not change, I will quit the public sector and start my own private practice. (RKMH 16 paediatrician)
Respondents complained management engaging in clientelism and nepotism, which they found to conflict with their public service values.
The chief of the admission office is carrying out tasks that are not his. He manages the personnel! Staff who come from the town of CEO2 are privileged compared with others. Decisions are guided by his close interpersonal relationship with them. (RKMH 11, nurse)
For instance, when I take necessary administrative measures to correct staff absenteeism, the provincial district officer takes no actions to sanction these deviant behaviours. My authority is weakened. Either you accept staff’s deviant behaviours and thus participate in this “crime”, or you are intransigent and staff will build an alliance against you and you will be demonised. As you may know, unions and political parties are corrupt, they seek only the interest of their members and not the general interest. (RKMH 15, administrator)
Staff perceived that they were unable to treat adequately patients because of lack of material and resources (eg, laboratory tests, mobile radiology) and the inadequate organisational support to their supply needs. They did not feel self-efficacious. Some felt that they were doing more harm than good for patients. This reduced their PSM and negatively impacted their psychological well-being.
We suffer because we transfer patients for simple technical procedures that we could have handled locally. (RKMH 10, nurse)
We often ask relatives to help us carry patients with a fractured femur to the fixed X Ray table. By doing this, we may worsen the fracture. I feel sorry when I had to ask sick patients to go themselves to the fixed X-Ray table. No organisational support is given, despite our relentless asking the administration to provide us with a mobile X Ray system. (RKMH 14, radiology technician)
Poor management and bad working conditions led to low levels of perceived organisational support among nurses. Staff felt inadequately supported by their supervisors and were left to face problems in the execution of their daily tasks. This created a stressful job pressure they were unable to deal with.
During the transfer (of a patient to the referral hospital), we do not focus on what care to give to the patient, but we are stressed by the poor conditions of the ambulance. It is not an ambulance, it is a wreck! (RKMH 12, nurse anaesthesiologist)
Reluctance of the managers to start up legal procedures against patients or families who assaulted nurses or doctors further reduced the latter’s trust in the management.
Many times, staff were assaulted. The management just forgave the assaulter, because the CEO knows him. Leaders should support staff, … support them in a sense that if someone of us is assaulted one day, I mean a nurse staff in his shift or a doctor, staff should be protected. This assault should not be considered as an assault on an individual person, it is an assault on all of us, on all health care providers cadres in general. (RKMH 24, nurse, ED)
Public service motivation
In this hospital, we found that front-line providers value the importance of adequately serving patients and improving health outcomes. They derive satisfaction from relieving suffering and saving lives, or at least preventing them from developing complications. Health workers mentioned that compassion, self-sacrifice, serving the underprivileged and caring for the poor are crucial drivers of their public service motivation.
We often sacrifice our own time for the sake of patients and for the sake of God to avoid unnecessary delays and prevent parturients from getting complications, for exemple, severe neurological and cardiac complications of post partum haemorrhage. We even help patient’s families to pay for ambulance fees in order to avoid delays. (RKMH 14, midwife)
Here, I work a lot with vulnerable citizens. It is a reward in itself to serve poor patients. It is my source of motivation. (RKMH 3, doctor)
We noted that the laissez-faire and transactional leadership had a negative effect on staff with high levels of public service motivation. It led to psychological distress, low organisational commitment and self-interested behaviour. This was compounded by the perceived organisational politics (see clientelism and nepotism).
Summary
Our analysis showed that the laissez-faire and transactional leadership in this hospital did not respond to the basic psychological needs of health workers. This led to reduced public service motivation with negative consequences on their psychological well-being because of the lack of opportunities of experiencing valued patient outcomes (eg, saving lives).
The leadership styles also contributed to low perceived organisational support, which in a context of perceived organisational politics, in turn lowered organisational commitment, and increased self-interested behaviour and mistrust between administration and staff.
SMBA Hospital
Main leadership and management practices
In SMBA Hospital, one of the low-performing hospitals, there were three leadership periods. CEO 1 (2007–2010) displayed strong transactional leadership, emphasising conformity with rules and procedures and insisting on top-down hierarchical management. He carried out many performance audits and clinical supervisions, and organised training to staff. He showed high moral standards and was both respected and feared by staff. He was replaced in 2010 by CEO 2, who retired in 2013. He had some experience in management, displayed transactional leadership and stressed the conformity with rules similar to his predecessor. In 2014, CEO 2 was replaced by CEO 3, who adopted a laissez-faire leadership. The hierarchical line was no longer respected. He managed the hospital poorly: no organisational action plans were available, and he did not carry any audit nor supervision. No inter-unit meetings were held and the departmentalisation process was halted. During our field work, we observed a strike of the clerical officers in charge of hospital admission and of the private company in charge of security in reaction to bad working conditions and perceived low responsiveness of management to their needs.
The perspective of staff
Leadership style
CEO 1 and 2 were highly appreciated by the administrators and their close collaborators. The health professionals (nurses and doctors) pointed to reduced perceived organisational support and to lack of participative decision-making. Under the leadership of CEO 3, staff felt less supported by their supervisors. They said they were left to deal with problems alone. Lack of clarity of goals led health workers to perceive role ambiguity and job pressure.
Poor management and low responsiveness of leaders to staff needs in terms of improving working conditions decreased their public service motivation.
Leaders do not play a role in our motivation. […]. We came to work despite constraints and poor working conditions. If we were only motivated by working conditions, we wouldn’t come to work. The management team was even unable to timely replace a broken window of our reception desk counter! (SMBA 29, reception desk officer)
Our respondents also mentioned the clientelism and nepotism of CEO 3, who privileged some staff and patients over others. This led to perceived organisational politics and mistrust, and contributed to low organisational commitment, demotivation and crowding out of public service motivation.
In this hospital, there are some external actors who pretend to do social work, and pretend to act as benefactors. These external actors, often members of associations, intervene illegimitely in hospital activities. They are like parasites. They definitely impact on our productivity. They are like stockbrokers. They do not care about citizens. They frequently mediate between citizens and services providers. The CEO responds quickly to patients needs when these actors are involved. This what I call clientelism. This is not fair! All citizens are equal. (SMBA 21, support staff, reception desk)
Public service motivation
Physicians and nurses perceived compassion with patients’ conditions and self-sacrifice as major components of their public service motivation.
Patients are important for me because I got sick myself. So, I sense what the patients are feeling. My family members, my daughter and my grandmother got sick. I feel the pain patients are suffering from. I can feel their suffering. (SMBA 35, nurse)
Public service motivation is also driven by religious cultural beliefs including elements of fear of God and divine rewards.
We work because of our sense of humanity, our own consciousness and our fear of God. One day, we will be asked about the quality of work we have done in the past. We feel sorry for patients. (SMBA 29, reception desk officer)
Staff said they were suffering from psychological distress due to poor working conditions, and experienced feelings of guilt because of their inability to perform their job adequately and to ease their patients’ suffering. Lack of opportunities to experience positive patients outcomes reduced their public service motivation.
When you do not have necessary material you are in trouble! It is not only a constraint but a source of suffering. Instead of relieving patients’ distress, it is us who get stressed. (SMBA 45, doctor)
Here, ressources are limited compared to the teaching hospital where we were trained. Real world practices are really different. When we first were assigned to this hospital we could not change things around. This is really depressing. We have the ability to provide specialised care but we do not have the necessary ressources to do it! (SMBA 42, doctor)
This impacted negatively on their perceived organisational support. This led to crowding out of their public service motivation and lowered their organisational commitment and their well-being.
It is really depressing. I do not want to work anymore because I do not have the necessary ressources.[…] I often cry when I watch newborns suffering from intramuscular injections because nurses are not skilled to administrater intraveineus infusions to newborns and often use instead intramuscular injection for 10 days. I am not only frustrated, I hate entering neonatology service!!!. I only grudgingly go see my patients whereas in the past I loved providing neonatology care. I cannot stand seeing newborn almost dying of hypoglycaemia 0.3 g/L because they are not adequately fed. This is due to the acute shortage of nurses (one nurse per shift) who are unable to reconciliate between administering antibiotics and treating infections and baby feeding. I am not anymore motivated to cure newborns ‘infections but I am terribly stressed avoiding newborns to die from hypoglycaemia. If babies are left alone with the feeding bottles they may die by suffocation. How can we come motivated to work in the next morning? of course not!!! (SMBA 42, paediatrician)
Shortage of material reduced their ability to properly care for patients, which reduced their PSM and contributed to a reduced sense of competency, self-efficacy and autonomy.
During my pediatric residency, I practiced neonatology and neonatal reanimation for two years, I developped many skills that I am not using now because I do not have the necessary equipments. I have only few neonatal rescuscitation tables and two sources of oxygen for 21 patients. I do not have a respirator. During my training I learned to intubate and manage cardiorespiratory distress. Now, in neonatology service instead of using unavailable syringe pumps,we manage pediatric diabetes by intraveinous perfusion. I never been thaught to do this!!. (SMBA 42, paediatrician)
I am very proud to serve my population, however I am truly unsatisfied. We have strong faith and we work eagerly to serve people. But our faith is not sufficiant. We need more ressources. For exemple, I am often called for patients with cranial trauma. We do what is possible depending on available ressources. Cerebral trauma patients need an emergency cerebral CT-scan and the golden hour must be respected. When they arrive at the hospital, often with a delay, the CT Scan is unavailable. It is often out of order. What could we do? In this case, We help teams transfer the patient to the nearby hospital in Marrakech. We often collect money to pay ambulance fuel and to avoid extradelays. I feel that my contribution to patient health is useless, despite being present for about 5 or 6 six hours at night. I feel that our contribution is hampered by organisational problems that are beyond our control. (SMBA 43, intensive care anaesthetist)
Summary
In this hospital, we found that leaders (like CEO 1) who are perceived as showing a high sense of moral and ethical standards, and who stimulate the awareness of staff of public service values and their contribution to society, were positively considered by some cadres. For the administrative staff, the transactional leadership displayed by CEO 1 led to higher clarity of goals, reduced job pressure and increased extrinsic motivation. However, it was negatively perceived by frontline workers because they felt it did not respond to their needs for autonomy.
Laissez-faire leadership crowded out public service motivation by reducing frontline healthworkers’ opportunities to help. Such management did not respond to the basic psychological needs of staff and led to low organisational commitment.
In table 3, we present a summary of the perspectives of staff on the leadership and management practices. We present in the first column the key summary data derived from the initial exploratory case study (NHMH Hospital) and detailed in Belrhiti et al. 88
Table 3.
The perspectives of staff on the leadership and management practices
| NHMH | EJMH | RKMH | SMBA |
|
CEO 1 (2007–
2013) Transactional leadership Conformity to rules and procedures, role model. Improved staff working conditions. Staff perspective Strong perceived leader support, which catalysed the quality culture. CEO 2 (2014– 2016) Transformational leadership Clear communication of his vision. Genuine concern for staff needs. Enhanced staff mission valence. Distributed leadership Stimulated network formation, ‘kind heart actions’ Staff perspective Responsiveness to their basic psychological needs Reinforced existing clan culture. Positive organisational climate (mutual trust and team work). This led to increased organisational commitment and extra role performance. In 2016, the hospital won the second price in the national quality contest). CEO 3 (July 2016–Sep 2017): Laissez-faire leadership Passive attitude. Reliance on administrative correspondence. Poor communication with staff. Hierchical line not enforced. Staff perspective Role ambiguity, high job stressors. Unresponsiveness to staff needs. Deteriorating working conditions. Perceived organisational politics. Demotivation, conflicts and tensions with unions. CEO 4 (Oct 2017–March 2018) Transactional leadership Reinforcing the hierarchical line. Building alliance with informal leaders. Staff perspective Distant leader. Reduced perceived autonomy support. Improved working conditions. Clarifying goals reduced role ambiguity and job pressures for admin. staff. Reduced interaction between health units. |
CEO 1 (2012–
2015)
Transactional leadership Power-assertive attitude. Overemphasis on compliance with rules and procedures. Staff perspective Perceived distant leader. Low perceived autonomy support. Decreased organisational commitment. Mistrust, conflicts and tensions with unions. CEO 2 (2015– 2018) Transformational leadership Good communication of vision and objectives. Genuine concern for the needs of staff. Distributed leadership Constructive dialogue to resolve professional issues. Catalysing role of mid-level managers. Participative decision-making. In 2016, the hospital won the first price of the quality contest. Staff perspective High perceived autonomy support. Good congruence with professional and public service motives. Trust relationship between staff and management team. Reduced tensions with unions. |
CEO 1 (2010–
2012) Transactional leadership Strict application of administrative procedures. Staff perspective Appreciated by administrators and close collaborators. Increased extrinsic motivation of staff. Nurses and doctors resisting to his overcontrolling behaviour engaging in conflicts and strikes. CEO2 (2012– 2018) Laissez-faire leadership Often absent. Chief nursing officer overwhelmed by day-to-day operational management duties. Staff perspective Appreciated by administrators and close collaborators. Nurses and doctors unhappy about lack of responsiveness to their needs and the poor working conditions. Conflictual organisational climate, characterised by high job pressure and role ambiguity. Perceived organisational politics (nepotism and clientelism), contributing to perceived unfairness. |
CEO 1 (2007–
2010)
Transactional leadership Enforcement of hierarchy. Emphasis on conformity with rules and procedures. Audit and clinical supervision. High moral standards. Staff perspective Highly appreciated by close collaborators and administrative staff. Nurses and doctors perceived a lack of participative decision-making and reduced perceived autonomy support. CEO 2 (2010– 2013) Transactional leadership Enforcing conformity with rules and regulations. Close supervision, administrative sanctions. Staff perspective Well appreciated by administrators and close collaborators. Perceived unresponsiveness to nurses’ needs. CEO 3 (2014– 2018) Laissez-faire leadership Hierarchical line not respected. No meetings, no clinical supervision. No inter-unit interaction. Staff perspective Decreased organisational commitment Inadequate working conditions and supply of consumables. Low perceive organisational support. High role ambiguity and job pressure. High level of perceived organisational politics. |
Cross case analysis and refined causal configurations
Comparing the initial PT with the results of the analysis of the data from the hospitals EJMH, RKMH and SMBA allowed us to refine it (table 4). We used the ICAMO configuration to structure the analysis.118 We confirmed or refuted the four causal configurations presented above.
Table 4.
Testing the initial configurations in the study sites
| Programme theories based on literature review and the study of NHMH Hospital | EJMH Hospital | RKMH Hospital | SMBA Hospital |
| Laissez-faire leadership decreases the levels of perceived organisational support and staff motivation by being less responsive to their basic psychological needs of autonomy, competence and relatedness. Lack of vision and goal setting contributes to a climate of ambiguity and role conflict. The inadequate enforcement of the hierarchical structure and high job pressure can contribute to mistrust between administration and staff. | Not confirmed not refuted. | Confirmed and refined: Laissez-faire leadership decreases the levels of (…) contributes to general malaise, mistrust between administration and staff and decreases public service motivation and psychological well being. This mechanism is triggered by the lack of opportunities for experiencing positive patient outcomes and the perceived organisational politics. | Confirmed. |
| Transactional leaders can improve extrinsic motivation of staff if they offer the necessary support and ensure adequate working conditions. By improving the latter, transactional leaders reduce job pressure and by implementing a clear hierarchical line they reduce role conflicts. | Confirmed and refined. Transactional leaders are effective on staff extrinsic motivation … leading in turn to reduced motivation and low organisational commitment and tension with unions. | Confirmed | Confirmed |
| By showing individual consideration and communicating clearly about mission valence, transformational leaders enhance self-esteem of staff, perceived supervisor support, and satisfaction of their autonomy needs. This, in turn, contributes to staff commitment, mutual trust and respect between the management team and staff. | Confirmed | Not confirmed nor refuted, because no transformational leadership was enacted in this hospital. | Not confirmed nor refuted because no transformational leadership was enacted in this hospital |
| Distributed leadership can contribute to improved communication and interaction between staff from different units, to problem solving and a reinforced clan culture. Distributing leadership roles and embedding them throughout the organisation, combined with engaging staff in decision-making, contributes to staff’s perceived autonomy and organisational commitment, which, in turn, leads to extra role activities. | Confirmed | Not confirmed nor refuted, because no distributed leadership was enacted in RKMH. | Not confirmed nor refuted because no distributed leadership was enacted in SMBA. |
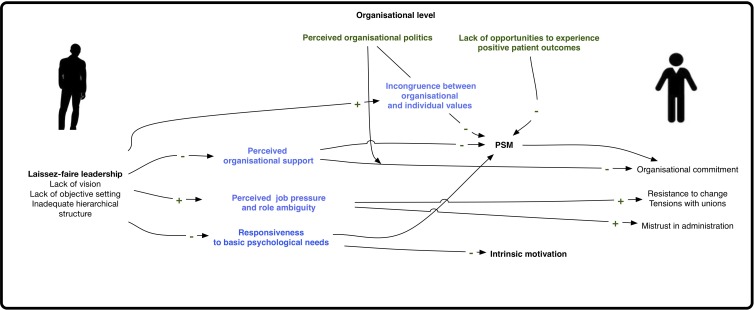
ICAMO configuration 1: Laissez-faire leadership and PSM
This configuration was confirmed in the RKMH (CEO 1) and SMBA (CEO 3) hospitals (see table 4 and figure 3).
Figure 3.
Laissez-faire leadership and PSM (ICAMO 1).
Laissez-faire leadership [I] decreases intrinsic motivation and public service motivation [O] of health providers [A] by being less responsive to the basic psychological needs of autonomy, competence and relatedness [M] and by reducing perceived organisational support [M] in situations of reduced opportunities to experience positive patient outcomes [C].
Laisser-faire leadership [I] contributes to mistrust between administration and staff, resistance to change and tensions with unions [O] by inducing perceived job pressure and role ambiguity [M] for health providers [A].
Laissez-faire leadership [I] reduces public service motivation [O] in a context of perceived organisational politics (clientelism and nepotism) [C] by being incongruent with individual public service values [M] of all cadres [A].
ICAMO configuration 2: transactional leadership and PSM
This configuration is confirmed by empirical data from the three hospitals (EJMH (CEO 1), RKMH (CEO 1), SMBA (CEO 1 and 2)). As a result, we retain ICAMO 2 as follows (see figure 4):
Figure 4.
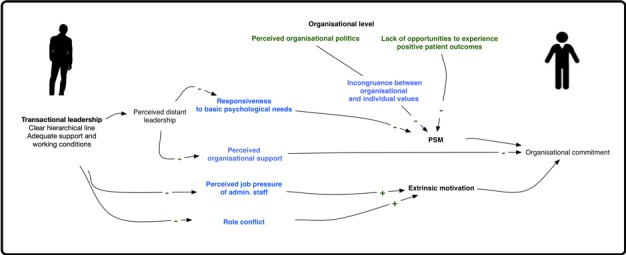
Transactional leadership-PSM (ICAMO 2).
If transactional leadership ensures adequate support and working conditions of administrative staff [I] or if enforces a clear hierarchical line [I], it can reduce job pressure [M] and reduce role conflict [M] and thus increase the extrinsic motivation of administrative staff [O] and the level of organisational commitment [O]. If transactional leaders [I] are felt by health professionals [A] to be distant, this can reduce perceived autonomy support and reduce the satisfaction of the need for mutual respect (relatedness) [M], leading in turn to reduced motivation [O] and low organisational commitment [O].
ICAMO configuration 3: transformational leadership and PSM
Configuration 3 is confirmed only in EJMH Hospital (CEO 2) (figure 5, table 4).
Figure 5.
Transformational leadership and PSM (ICAMO 3).
Transformational leadership understood as inspiring staff (walking the talk), infusing jobs with public service values and showing individual consideration to staff [I] increases public service motivation [O] by responding to basic psychological needs of autonomy and relatedness [M] of all staff [A] and contributes to higher organisational commitment and expressed mutual trust between staff with administration [O].
ICAMO configuration 4: distributed leadership and PSM
Distributed leadership was observed only in the high performing hospitals EJMH and NHMH (see figure 6).
Figure 6.
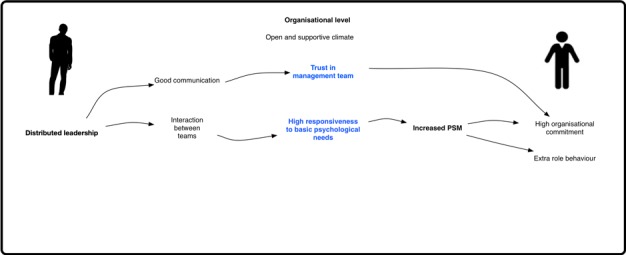
Distributed leadership and PSM (ICAMO4).
Distributed leadership in the sense of creating a supportive and open climate and good relations between staff [I] increased staff public service motivation [O] and organisational commitment [O] and led to extra role behaviours by satisfying staff basic psychological needs [M] and increasing trust in management teams [M]
As described in tables 3 and 4, we noticed that only CEO 2 in NHMH and CEO 2 in EJMH displayed complex leadership understood as the balancing between transactional, transformational and distributed leadership that fits best the diversity of professional profiles, the nature of the tasks and the organisational culture. Transactional leadership fits the administrators who value role clarity and reduced job ambiguity, whereas transformational and distributed leadership addresses the basic psychological needs of health providers. The other CEOs either adopted a transactional leadership style or laissez-faire leadership, which was not well received by a majority of staff.
The four ICAMOs presented above allowed us to refine our initial programme theory:
Complex leaders, applying an appropriate mix of transactional, transformational and distributed leadership styles that fit organisational and individual’s characteristics [I] can increase public service motivation, organisational commitment and extra role behaviours [O] by increasing perceived supervisor support and perceived organisational support and satisfying staff basic psychological needs [M], if the organisational culture is conducive and in the absence of perceived organisational politics [C].
Discussion
In this study, we explored mechanisms and contextual conditions by and in which leadership influences ‘public service motivation’ of health workers.
Our study shows, in line with leadership literature,122 123 that laissez-faire leadership decreases intrinsic motivation and public service motivation of all cadres by being less responsive to the basic psychological needs of autonomy, competence and relatedness of staff and by reducing perceived organisational support.1 5 92
Our findings suggest that transactional leadership, when it ensures adequate managerial support and improvement of working conditions, can enhance the extrinsic motivation of staff by reducing role ambiguity and job pressure, and by increasing perceived organisational support. This is supported by other studies.124–127 However, we also found indications that transactional leadership can crowd out intrinsic motivation and public service motivation of health workers by reducing the satisfaction of their needs for autonomy. This is supported by other studies in LMICs.40 41 128–130
We found transformational leaders who clearly communicate their vision and walk the talk, infuse jobs with public services meaning, and show individual consideration can enhance PSM by responding to their need for relatedness. This is supported by recent studies.29 37 56 75 78 131–133 Transactional leadership can lead to higher organisational commitment and extra role behaviours.134 135
Distributed leadership facilitated teamwork, information flows and team cohesion. It nurtured feelings of connectedness, enhancing the perception of autonomy support and perceived organisational support. This led to creative problem solving, collective learning and better performance at the quality assurance contest, in ways similar to other study findings.11–15 136
Our study supports the hypothesis that the effect of leadership on PSM depends on the degree of responsiveness to basic psychological needs (autonomy, competency and relatedness). This points to the relevance of self-determination theory92 106 as a middle range theory that may frame how individual psychological mechanisms underlie the effects of leadership on staff motivation (extrinsic motivation, intrinsic motivation and PSM). It also supports the hypothesis that the effect of leadership on PSM is conditioned by the existence of a conducive organisational culture (a clan culture and absence of perceived organisational politics). This is explained by value congruence, understood as the degree of congruence between individual and organisational values, which represents a major mechanism in the integration of public service values in individual behaviours.70 75 137 138
In summary, in healthcare organisations, leaders able to adapt their leadership practices to the nature of individuals and organisational characteristics (complex leaders) are likely to be more effective. They foster networking and connections between staff by distributing leadership responsibilities and reinforcing the role of middle managers, infusing jobs with meaning and creating constructive dialogues with professional health workers.12 61 62 64 139 140
Study contributions, validity and limitations
This study contributed to fill the gap in leadership studies in general83 141 142 and in healthcare specifically62 143 by unravelling the underlying mechanisms of leadership effects on health workers’ motivation. It contributes to the study of leadership in North African Muslim countries, a neglected field of research.144
This study contributes to the case that RE can contribute to building a better understanding of complex phenomena in health systems.85 RE proved an appropriate approach to unravel the relationship between leadership and PSM, and thus responded to calls of PSM scholars for robust research methodologies.33 35 37 76 77
The RE proved to be a suitable approach for capturing the multilevel dynamic nature that evolved over time and across contexts. RE facilitated the unveiling of causal mechanisms (value congruence and satisfaction of basic psychological needs) and the contingent effect of contextual factors (organisational culture, climate and perceived organisational politics) and the individual reasoning of different social actors (eg, perceived supervisor and organisational support).85 145 146
By using ICAMO configurational analysis, we were able to provide evidence on the contextual nature and social construction of leadership. Adopting a situational approach on leadership help overcome the inconsistency of findings when studying leadership effectiveness in organisations.147–149
In addition, the qualitative multiple embedded case study design proved appropriate in providing qualitative design rich, dynamic, contextual data with a focus on mechanisms rather than variables.150 Qualitative approaches are complex sensitive and allow for more research flexibility in unveiling the mechanisms and conditions underlying complex social phenomena in general and more specifically leadership effectiveness in health.98 150–153
The validity of our study findings is derived from theoretical guidance in study design, sampling and analysis, and cross-validation154–156 and theoretical replication across cases.119 Theoretical replication allows for a retroductive process of knowledge creation119 by constantly shuttling from theory to empirical data and by continuously refining our programme theories across negative and positive cases.
There are limitations to our study. The causal configurations developed here are the most plausible explanation for the outcomes observed in our study, but may likely not be the unique explanation. Further empirical testing in a larger set of cases would enable to further refine the PTs. A second limitation is that we did not quantitatively measure public service motivation, organisational commitment, perceived organisational support and other variables. The time and resource limits of the PhD study, of which the study presented here is part, precluded testing and validating existing scales for these constructs.
Implications for practice
In Morocco, similar to other LMICs,56 the hierarchical culture within the Ministry of Health favours transactional leadership styles49 157 and this may impede the emergence of PSM.158–160 We raise some concerns in relation to the actual health reforms carried out in Morocco, which are inspired by new public management (eg, performance-based management, contracting out and public–private partnerships) and which may have negative consequences on health workers’ performance by facilitating the practice of transactional leadership, focusing on extrinsic rewards (and sanctions) and crowding out the expression of PSM and self-altruistic behaviours of frontline health workers. Policy makers should stimulate the development of complex leadership competencies (eg, fostering network building, generative sense making, see also Belrhiti et al 62 in their capacity building programme.
Conclusion
In the context of healthcare organisations, the motivation of health workers relies on individual, organisational and contextual antecedents. The effectiveness of leaders depends on the degree of responsiveness to the basic psychological needs of health workers and on value congruence between organisational and individual values. Leaders should learn how to adapt their leadership practices to the organisational characteristics (nature of task, mission valence) and to type of motivation of health workers (extrinsic vs intrinsic and PSM). Further research is needed to explore the role of value congruence and to understand how the social institutions (ie, religion, family education, professionalism) may shape the expression of public service motivation of health workers in LMICs.
Supplementary Material
Footnotes
Twitter: @drbelrhiti
Contributors: All the four authors (ZB, BM, WVD, AB) contributed to the original design and analysis and writing of the manuscript. ZB carried out the data collection. BM cross checked the transcripts. Initial coding was done by ZB and discussed between the research team members (BM, WVD, AB). ZB edited the final draft. All authors read and approved the final manuscript.
Funding: This work was funded through a PhD framework agreement between the Belgian Directorate-General for Development Cooperation and the Institute of Tropical Medicine, Antwerp. The sponsors had no role in the study or in the writing of the paper.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: The research protocol was approved by the Moroccan Institutional Review Board (No. 90/16) of the Faculty of Medicine of Pharmacy, Rabat and the Institutional Review Board of the Institute of Tropical Medicine, Antwerp (No. 1204/17). All participants have been informed prior to the conduct of the research and written consent forms were signed by the respondents and countersigned by the researcher. A signed copy was given to each respondents.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data sharing not applicable as no datasets generated and/or analysed for this study.
References
- 1. George A, Scott K, Govender V. A health policy and systems research reader on human resources for health. Geneva: World Health Organisation, 2017. [Google Scholar]
- 2. Dieleman M, Gerretsen B, van der Wilt GJ. Human resource management interventions to improve health workers' performance in low and middle income countries: a realist review. Health Res Policy Syst 2009;7 10.1186/1478-4505-7-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. WHO The world health report 2006: working together for health. Geneva: World Health Organization, 2006. [Google Scholar]
- 4. WHO Health workforce requirements for universal health coverage and the sustainable development goals. (human resources for health observer, 17, report no: 9241511400). Geneva: World Health Organization, 2016. [Google Scholar]
- 5. Rowe AK, de Savigny D, Lanata CF, et al. How can we achieve and maintain high-quality performance of health workers in low-resource settings? The Lancet 2005;366:1026–35. 10.1016/S0140-6736(05)67028-6 [DOI] [PubMed] [Google Scholar]
- 6. Haines A, Kuruvilla S, Borchert M. Bridging the implementation gap between knowledge and action for health. Bull World Health Organ 2004;82:724–31. [PMC free article] [PubMed] [Google Scholar]
- 7. Topp SM. Health worker performance, practice and improvement : A health policy and systems research reader on human resources for health. Geneva: World Health Organisation, 2017:73. [Google Scholar]
- 8. Chopra M, Munro S, Lavis JN, et al. Effects of policy options for human resources for health: an analysis of systematic reviews. The Lancet 2008;371:668–74. 10.1016/S0140-6736(08)60305-0 [DOI] [PubMed] [Google Scholar]
- 9. Siddiqi K, Newell J, Robinson M. Getting evidence into practice: what works in developing countries? Int J Qual Health Care 2005;17:447–54. 10.1093/intqhc/mzi051 [DOI] [PubMed] [Google Scholar]
- 10. WHO The world health report 2000: health systems: improving performance. World Health Organization, 2000. [Google Scholar]
- 11. Fitzgerald L, Ferlie E, McGivern G, et al. Distributed leadership patterns and service improvement: evidence and argument from English healthcare. Leadersh Q 2013;24:227–39. 10.1016/j.leaqua.2012.10.012 [DOI] [Google Scholar]
- 12. Uhl-Bien M, Marion R, McKelvey B. Complexity leadership theory: shifting leadership from the industrial age to the knowledge era. Leadersh Q 2007;18:298–318. 10.1016/j.leaqua.2007.04.002 [DOI] [Google Scholar]
- 13. Baker GR, Denis J-L. Medical leadership in health care systems: from professional authority to organizational leadership. Public Money & Management 2011;31:355–62. 10.1080/09540962.2011.598349 [DOI] [Google Scholar]
- 14. Denis JL, Lamothe L, Langley A. The dynamics of collective leadership and strategic change in Pluralistic organisations. The Academy of Management Journal 2001;44:809–37. [Google Scholar]
- 15. Hooijberg R, Choi J. The impact of organizational characteristics on leadership effectiveness models: an examination of leadership in a private and a public sector organization. Administration & Society 2001;33:403–31. [Google Scholar]
- 16. Franco LM, Bennett S, Kanfer R. Health sector reform and public sector health worker motivation: a conceptual framework. Soc Sci Med 2002;54:1255–66. 10.1016/S0277-9536(01)00094-6 [DOI] [PubMed] [Google Scholar]
- 17. Ofori-Adjei D, Arhinful DK. Effect of training on the clinical management of malaria by medical assistants in Ghana. Soc Sci Med 1996;42:1169–76. 10.1016/0277-9536(95)00389-4 [DOI] [PubMed] [Google Scholar]
- 18. Ross-Degnan D, Laing R, Santoso B, et al. Improving pharmaceutical use in primary care in developing countries: a critical review of experience and lack of experience. Chiang Mai, Thailand: International Conference on Improving Use of Medicines, 1997. [Google Scholar]
- 19. Paredes P, de la Peña M, Flores-Guerra E, et al. Factors influencing physicians' prescribing behaviour in the treatment of childhood diarrhoea: knowledge may not be the clue. Soc Sci Med 1996;42:1141–53. 10.1016/0277-9536(95)00387-8 [DOI] [PubMed] [Google Scholar]
- 20. Brewer GA, Selden SC. Why elephants Gallop: assessing and predicting organizational performance in federal agencies. Journal of Public Administration Research and Theory 2000;10:685–712. 10.1093/oxfordjournals.jpart.a024287 [DOI] [Google Scholar]
- 21. Rainey HG, Steinbauer P. Galloping elephants: developing elements of a theory of effective government organizations. Journal of Public Administration Research and Theory 1999;9:1–32. 10.1093/oxfordjournals.jpart.a024401 [DOI] [Google Scholar]
- 22. Belrhiti Z, Damme WV, Belalia A, et al. Does public service motivation matter in Moroccan public hospitals? a multiple embedded case study submitted at the International Journal of equity in health (article in press). International Journal of Equity in Health 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. van Loon NM, Vandenabeele W, Leisink P. Clarifying the relationship between public service motivation and In-Role and Extra-Role behaviors: the relative contributions of Person-Job and Person-Organization fit. The American Review of Public Administration, 2015. [Google Scholar]
- 24. Perry JL, Wise LR. The motivational bases of public service. Public Adm Rev 1990;50:367–73. 10.2307/976618 [DOI] [Google Scholar]
- 25. Vandenabeele W. Toward a public administration theory of public service motivation. Public Management Review 2007;9:545–56. 10.1080/14719030701726697 [DOI] [Google Scholar]
- 26. Andersen LB. What determines the behaviour and performance of health professionals? public service motivation, professional norms and/or economic incentives. International Review of Administrative Sciences 2009;75:79–97. 10.1177/0020852308099507 [DOI] [Google Scholar]
- 27. van Loon NM, Leisink P, Vandenabeele W. Talking the talk of public service motivation: how public organization logics matter for employees' expressions of PSM. International Journal of Public Administration 2013;36:1007–19. 10.1080/01900692.2013.798811 [DOI] [Google Scholar]
- 28. Bellé N. Leading to make a difference: a field experiment on the performance effects of transformational leadership, perceived social impact, and public service motivation. Journal of Public Administration Research and Theory 2014;24:109–36. 10.1093/jopart/mut033 [DOI] [Google Scholar]
- 29. Bellé N. Experimental evidence on the relationship between public service motivation and job performance. Public Adm Rev 2013;73:143–53. 10.1111/j.1540-6210.2012.02621.x [DOI] [Google Scholar]
- 30. Bellé N, Cantarelli P. Monetary incentives, motivation, and job effort in the public sector. Rev Public Pers Adm 2015;35:99–123. 10.1177/0734371X13520460 [DOI] [Google Scholar]
- 31. Ritz A, Brewer GA, Neumann O. Public service motivation: a systematic literature review and outlook. Public Adm Rev 2016;76:414–26. 10.1111/puar.12505 [DOI] [Google Scholar]
- 32. Homberg F, McCarthy D, Tabvuma V. A meta-analysis of the relationship between public service motivation and job satisfaction. Public Adm Rev 2015;75:711–22. 10.1111/puar.12423 [DOI] [Google Scholar]
- 33. Petrovsky N, Ritz A. Public service motivation and performance: a critical perspective. Evidence-based HRM: a Global Forum for Empirical Scholarship 2014;2:57–79. 10.1108/EBHRM-07-2013-0020 [DOI] [Google Scholar]
- 34. Warren DC, L-t C. The relationship between Public Service Motivation and Performance : Rincquist E, Meta-Analysis for public management and policy. San Francisco, USA: John Wiley & Sons, 2013. [Google Scholar]
- 35. Park SM, Rainey HG. Leadership and public service motivation in U.S. federal agencies. International Public Management Journal 2008;11:109–42. 10.1080/10967490801887954 [DOI] [Google Scholar]
- 36. Paarlberg LE, Lavigna B. Transformational leadership and public service motivation: driving individual and organizational performance. Public Adm Rev 2010;70:710–8. 10.1111/j.1540-6210.2010.02199.x [DOI] [Google Scholar]
- 37. Wright BE, Moynihan DP, Pandey SK. Pulling the levers: transformational leadership, public service motivation, and mission valence. Public Adm Rev 2012;72:206–15. 10.1111/j.1540-6210.2011.02496.x [DOI] [Google Scholar]
- 38. Vandenabeele W. Explaining public service motivation: the role of leadership and basic needs satisfaction. Review of Public Personnel Administration 2014;34:153–73. [Google Scholar]
- 39. Anderson LB, Bjornholt B, Bro LL, et al. Leadership and motivation:a qualitative study of transformational leadership and public service motivation. International review of Administrative Sciences 2016;0:1–17. [Google Scholar]
- 40. Mathauer I, Imhoff I. Health worker motivation in Africa: the role of non-financial incentives and human resource management tools. Hum Resour Health 2006;4:24 10.1186/1478-4491-4-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Willis-Shattuck M, Bidwell P, Thomas S, et al. Motivation and retention of health workers in developing countries: a systematic review. BMC Health Serv Res 2008;8:247 10.1186/1472-6963-8-247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Deci EL, Koestner R, Ryan RM. A meta-analytic review of experiments examining the effects of extrinsic rewards on intrinsic motivation. Psychol Bull 1999;125:627–68. 10.1037/0033-2909.125.6.627 [DOI] [PubMed] [Google Scholar]
- 43. Frey BS, Jegen R, Joes J. Motivation crowding theory. J Econ Surv 2001;15:589–611. 10.1111/1467-6419.00150 [DOI] [Google Scholar]
- 44. Frey BS, Homberg F, Osterloh M. Organizational control systems and pay-for-performance in the public service. Organization Studies 2013;34:949–72. 10.1177/0170840613483655 [DOI] [Google Scholar]
- 45. Ministère de la Santé Evaluation de l’impact de la politique de gratuité de l’accouchement et de la césarienne au niveau de six provinces au Maroc. Rabat: Ecole Nationale de Santé Publique, Rabat/ FemHealth/Seventh Framework Program, 2014. [Google Scholar]
- 46. Gruenais ME. une approche qualitative de la question de la motivation des personnels de santé. Le point de Vue des acteurs de la région sanitaire Du grand Casablanca. Rabat, Maroc: Institut National d’Administration Sanitaire Observatoire régional de la Santé, Institut de Recherche Developpement, 2008. [Google Scholar]
- 47. Boffin N, Brouwere D. Expériences de renforcement des capacités de pilotage Du Système de santé; étude comparative des résultats des études dans six pays, 2003. [Google Scholar]
- 48. Bossert TJ, Beauvais JC. Decentralization of health systems in Ghana, Zambia, Uganda and the Philippines: a comparative analysis of decision space. Health Policy Plan 2002;17:14–31. 10.1093/heapol/17.1.14 [DOI] [PubMed] [Google Scholar]
- 49. Akhnif E, Macq J, Meessen B. The place of learning in a universal health coverage health policy process: the case of the RAMED policy in Morocco. Health Res Policy Sys 2019;17 10.1186/s12961-019-0421-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Blaise P, Sahel A, Afilal R, et al. Ten years of quality projects and their effect on the organisational culture of the Morrocan health care system. quality in services: higher education, health care, local government. Toulon, France: 7th" Toulon-Verona" Conference, 2004. [Google Scholar]
- 51. Blaise PJ, Dujardin B, Kegels G. Culture qualité et organisation bureaucratique, Le défi Du changement dans les systèmes publics de santé: une évaluation réaliste de projets de qualité en Afrique, 2004. [Google Scholar]
- 52. Blaise P, Kegels G. A realistic approach to the evaluation of the quality management movement in health care systems: a comparison between European and African contexts based on Mintzberg's organizational models. Int J Health Plann Manage 2004;19:337–64. 10.1002/hpm.769 [DOI] [PubMed] [Google Scholar]
- 53. Sahel A, Alaoui Belghiti A, DeBrouwere V, et al. A systemic approach to quality improvement in public health services : The Moroccan “quality contest”. Leadersh Health Serv 2015;28:8–23. [DOI] [PubMed] [Google Scholar]
- 54. Sahel A, DeBrouwere V, Dujardin B, et al. Implementing a nationwide quality improvement approach in health services. Leadersh Health Serv 2015;28:24–34. 10.1108/LHS-04-2014-0042 [DOI] [PubMed] [Google Scholar]
- 55. Gilson L. Everyday politics and the leadership of health policy implementation. Health Syst Reform 2016;2:187–93. 10.1080/23288604.2016.1217367 [DOI] [PubMed] [Google Scholar]
- 56. Okello DRO, Gilson L. Exploring the influence of trust relationships on motivation in the health sector: a systematic review. Hum Resour Health 2015;13:16 10.1186/s12960-015-0007-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Kwamie A, Dijk Hvan, Agyepong IA. Advancing the application of systems thinking in health: realist evaluation of the leadership development programme for district manager decision-making in Ghana. Health Res Policy Sys 2014;12 10.1186/1478-4505-12-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Kwamie A. Balancing Management and Leadership in Complex Health Systems Comment on "Management Matters: A Leverage Point for Health Systems Strengthening in Global Health". Int J Health Policy Manag 2015;4:849–51. 10.15171/ijhpm.2015.152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Kwamie ABA, Lehmann U. Leadership, management and organizational cultures : G A, S K, G V, Health policy and systems research reader on human resources for health. Geneva: WHO, 2017. [Google Scholar]
- 60. Bass BM, Riggio RE. Transformational leadership. 2nd edn, 2006. [Google Scholar]
- 61. Ford R. Complex leadership competency in health care: towards framing a theory of practice. Health Serv Manage Res 2009;22:101–14. 10.1258/hsmr.2008.008016 [DOI] [PubMed] [Google Scholar]
- 62. Belrhiti Z, Nebot Giralt A, Marchal B. Complex leadership in healthcare: a scoping review. Int J Health Policy Manag 2018;7:1073–84. 10.15171/ijhpm.2018.75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Plsek PE, Wilson T. Complexity science: complexity, leadership, and management in healthcare organisations. BMJ 2001;323:746–9. 10.1136/bmj.323.7315.746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Uhl-Bien M, Marion R. Complexity leadership in bureaucratic forms of organizing: a meso model. Leadersh Q 2009;20:631–50. 10.1016/j.leaqua.2009.04.007 [DOI] [Google Scholar]
- 65. Weberg D. Complexity leadership: a healthcare imperative. Nurs Forum 2012;47:268–77. 10.1111/j.1744-6198.2012.00276.x [DOI] [PubMed] [Google Scholar]
- 66. Zimmerman B, Lindberg C, Plsek P. Edgeware: lessons from complexity science for health care leaders. 2nd edv Irving, Tex, USA: VHA, 1998. [Google Scholar]
- 67. Ritz A, Brewer GA. Does societal culture affect public service motivation? evidence of Sub-national differences in Switzerland. International Public Management Journal 2013;16:224–51. 10.1080/10967494.2013.817249 [DOI] [Google Scholar]
- 68. Rockstuhl T, Dulebohn JH, Ang S, et al. Leader-member exchange (LMX) and culture: a meta-analysis of correlates of LMX across 23 countries. J Appl Psychol 2012;97:1097–130. 10.1037/a0029978 [DOI] [PubMed] [Google Scholar]
- 69. Perry JL. Antecedents of public service motivation. Journal of Public Administration Research and Theory 1997;7:181–97. 10.1093/oxfordjournals.jpart.a024345 [DOI] [Google Scholar]
- 70. Pandey SK, Stazyk ECJ. Antecedents and correlates of public service motivation. motivation in public management: the call of public service. Oxford: Oxford University Press, 2008: 101. [Google Scholar]
- 71. Bøgh Andersen L, Holm Pedersen L. Public service motivation and professionalism. International Journal of Public Administration 2012;35:46–57. 10.1080/01900692.2011.635278 [DOI] [Google Scholar]
- 72. Vandenabeele W. Who wants to deliver public service? do institutional antecedents of public service motivation provide an answer? Rev Public Pers Adm 2011;31:87–107. 10.1177/0734371X10394403 [DOI] [Google Scholar]
- 73. Camilleri E. Antecedents affecting public service motivation. Personnel Review 2007;36:356–77. 10.1108/00483480710731329 [DOI] [Google Scholar]
- 74. Wise LR. Bureaucratic posture: on the need for a composite theory of bureaucratic behavior. Public Adm Rev 2004;64:669–80. 10.1111/j.1540-6210.2004.00414.x [DOI] [Google Scholar]
- 75. Moynihan DP, Pandey SK. The role of organizations in fostering public service motivation. Public Adm Rev 2007;67:40–53. 10.1111/j.1540-6210.2006.00695.x [DOI] [Google Scholar]
- 76. Chapman C, Getha-Taylor H, Holmes MH, et al. How public service leadership is studied: an examination of a quarter century of scholarship. Public Adm 2016;94:111–28. 10.1111/padm.12199 [DOI] [Google Scholar]
- 77. Perry JL, Hondeghem A. Motivation in public management: the call of public service. New York: Oxford University Press, 2008. [Google Scholar]
- 78. Moynihan DP, Pandey SK, Wright BE. Transformational Leadership in the Public Sector: Empricial Evidence of Its effects : Dwivedi YK, Shareef MA, Pandey SK, Public administration reformation. Market Demand from Public Organizations Routeledge/ Taylor and Francis, 2014: 87–104. [Google Scholar]
- 79. McVeigh J, MacLachlan M, Gilmore B, et al. Promoting good policy for leadership and governance of health related rehabilitation: a realist synthesis. Global Health 2016;12:49 10.1186/s12992-016-0182-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Brand SL, Thompson Coon J, Fleming LE, et al. Whole-system approaches to improving the health and wellbeing of healthcare workers: a systematic review. PLoS One 2017;12:e0188418 10.1371/journal.pone.0188418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Paarlberg LE, Perry JL. Values management: aligning employee values and organization goals. The American Review of Public Administration 2007;37:387–408. [Google Scholar]
- 82. Paarlberg LE, Perry JL, Hondeghem A. From theory to practice: strategies for applying public service motivation. Motivation in public management: The call of public service, 2008: 268–93. [Google Scholar]
- 83. Perry JL, Hondeghem A. Directions for future theory and research : Press OU, Motivation in public management: the call of public service. Oxford, 2008: 294–313. [Google Scholar]
- 84. Pawson R, Tilley N, Tilley N. Realistic evaluation. Sage, 1997. [Google Scholar]
- 85. Marchal B, van Belle S, van Olmen J, et al. Is realist evaluation keeping its promise? A review of published empirical studies in the field of health systems research. Evaluation 2012;18:192–212. 10.1177/1356389012442444 [DOI] [Google Scholar]
- 86. Astbury B, Leeuw FL. Unpacking black boxes: mechanisms and theory building in evaluation. Am J Eval 2010;31:363–81. 10.1177/1098214010371972 [DOI] [Google Scholar]
- 87. Wong G, Westhorp G, Manzano A, et al. RAMESES II reporting standards for realist evaluations. BMC Med 2016;14:96 10.1186/s12916-016-0643-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Belrhiti Z, Van Damme W, Belalia A, et al. Unravelling the role of leadership in motivation and performance of health workers in a Moroccan public Hospital: a realist evaluation in press. BMJ Open 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Eisenberger R, Stinglhamber F, Vandenberghe C, et al. Perceived supervisor support: contributions to perceived organizational support and employee retention. J Appl Psychol 2002;87:565–73. 10.1037/0021-9010.87.3.565 [DOI] [PubMed] [Google Scholar]
- 90. Eisenberger R, Fasolo P, Davis-LaMastro V. Perceived organizational support and employee diligence, commitment, and innovation. J Appl Psychol 1990;75:51–9. 10.1037/0021-9010.75.1.51 [DOI] [Google Scholar]
- 91. Rhoades L, Eisenberger R, Armeli S. Affective commitment to the organization: the contribution of perceived organizational support. J Appl Psychol 2001;86:825–36. 10.1037/0021-9010.86.5.825 [DOI] [PubMed] [Google Scholar]
- 92. Ryan R, Deci E. Psychological Needs. Varied Concepts and a Preliminary Description of SDT’s Approach : Press TG, Self-determination theory: basic psychological needs in motivation, development, and wellness. New York London, 2017: 80–101. [Google Scholar]
- 93. Kottke JL, Sharafinski CE. Measuring perceived Supervisory and organizational support. Educ Psychol Meas 1988;48:1075–9. 10.1177/0013164488484024 [DOI] [Google Scholar]
- 94. Dinh JE, Lord RG, Gardner WL, et al. Leadership theory and research in the new millennium: current theoretical trends and changing perspectives. Leadersh Q 2014;25:36–62. 10.1016/j.leaqua.2013.11.005 [DOI] [Google Scholar]
- 95. Marion R, Rumsey MG. Organizational leadership and complexity mechanisms. Oxford Handbook of Leadership, 2012. [Google Scholar]
- 96. Uhl-Bien M, Marion R, McKelvey B. Complexity leadership theory: shifting leadership from the industrial age to the knowledge era (CH 8). Leadership, Gender, and, 2011. [Google Scholar]
- 97. Uhl-Bien M. Complexity leadership :part 1. Unites States of America: Information aged publishing, 2008. [Google Scholar]
- 98. Viitala R. Leadership in transformation: a longitudinal study in a nursing organization. J Health Organ Manag 2014;28:602–18. 10.1108/JHOM-02-2014-0032 [DOI] [PubMed] [Google Scholar]
- 99. Schein EH. Organizational culture and leadership. John Wiley & Sons, 2004. [Google Scholar]
- 100. Casida JJ, Pinto-Zipp G. Leadership-organizational culture relationship in nursing units of acute care hospitals. Nursing Economics 2008;26. [PubMed] [Google Scholar]
- 101. Tsai Y. Relationship between organizational culture, leadership behavior and job satisfaction. BMC Health Serv Res 2011;11:98 10.1186/1472-6963-11-98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Cameron KS, Quinn RE. Diagnosing and changing organizational culture: based on the competing values framework. John Wiley & Sons, 2011. [Google Scholar]
- 103. Cameron KS, Quinn RE. Diagnosing and changing organizational culture: based on the competing values framework. John Wiley & Sons, 2005. [Google Scholar]
- 104. Bock G-W, Zmud RW, Kim Y-G, et al. Behavioral intention formation in knowledge sharing: examining the roles of extrinsic motivators, social-psychological forces, and organizational climate. MIS Quarterly 2005;29:87–111. 10.2307/25148669 [DOI] [Google Scholar]
- 105. Jones AP, James LR. Psychological climate: dimensions and relationships of individual and aggregated work environment perceptions. Organ Behav Hum Perform 1979;23:201–50. 10.1016/0030-5073(79)90056-4 [DOI] [Google Scholar]
- 106. Deci EL, Ryan RM. Self-determination theory: a macrotheory of human motivation, development, and health. Canadian Psychology/Psychologie canadienne 2008;49:182–5. 10.1037/a0012801 [DOI] [Google Scholar]
- 107. Yin RK. Case study research: design and methods, applied social research methods series. Thousand Oaks, CA: Sage Publications, Inc, 2008. [Google Scholar]
- 108. Patton MQ. Qualitative Research & Evaluation Methods. Thousand Oaks, London, New Delhi: Sage Publications, 2001. [Google Scholar]
- 109. Yin RK. Qualitative research from start to Finish. New York, London: The Guilford Press, 2016. [Google Scholar]
- 110. Ministère de la Santé du Maroc Concours Qualité. 4th edn Rabat: Direction des Hopitaux et Soins Ambulatoires, 2011. [Google Scholar]
- 111. Ministère de la Santé du Maroc Concours Qualité. 6th edn Rabat: Direction des Hopitaux et Soins Ambulatoires, 2016. [Google Scholar]
- 112. Krueger RA, Casey MA. Focus groups: a practical guide for applied research. Los Angeles, London, New Delhi, Singapore, Washington DC: Sage publications, 2014. [Google Scholar]
- 113. Morgan DL, Krueger RA. Analyzing and reporting focus group results. Sage, 1998. [Google Scholar]
- 114. Rubin HJ, Rubin IS. Qualitative interviewing: the art of hearing data. Sage, 2011. [Google Scholar]
- 115. Miles MB, Huberman AM, Saldana J. Qualitative data analysis. 3 ed Los Angeles, London, New Delhi, Singapore, Washington DC: Sage, 2016. [Google Scholar]
- 116. Spradley JP. Participant observation. Waveland Press, 2016. [Google Scholar]
- 117. Saldaña J. The coding manual for qualitative researchers. Los Angeles, London, New Delhi, Singapore, Washington DC: Sage, 2015. [Google Scholar]
- 118. Marchal B, Kegels G, Belle SV. Theory and realist methods : Emmel N, Greenhalgh J, Manzano A, et al., Doing realist research. Los Angeles, London, New Delhi: SAGE, 2018. [Google Scholar]
- 119. Bhaskar R. A realist theory of science. London and New York: Routledge, 2013. [Google Scholar]
- 120. Belrhiti Z, Van Damme W, Belalia A, et al. Does public service motivation matter in Moroccan public hospitals? a multiple embedded case study. Int J Equity Health 2019;18 10.1186/s12939-019-1053-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. QSR International Pty Ltd NVivo qualitative data analysis software. 11.4 ed, 2014. [Google Scholar]
- 122. Hinkin TR, Schriesheim CA. An examination of "nonleadership": from laissez-faire leadership to leader reward omission and punishment omission. J Appl Psychol 2008;93:1234–48. 10.1037/a0012875 [DOI] [PubMed] [Google Scholar]
- 123. Judge TA, Piccolo RF. Transformational and transactional leadership: a meta-analytic test of their relative validity. J Appl Psychol 2004;89:755–68. 10.1037/0021-9010.89.5.755 [DOI] [PubMed] [Google Scholar]
- 124. Lee RT, Ashforth BE. A meta-analytic examination of the correlates of the three dimensions of job burnout. J Appl Psychol 1996;81:123–33. 10.1037/0021-9010.81.2.123 [DOI] [PubMed] [Google Scholar]
- 125. Moyle P. Longitudinal influences of managerial support on employee well-being. Work Stress 1998;12:29–49. 10.1080/02678379808256847 [DOI] [Google Scholar]
- 126. van Dierendonck D, Haynes C, Borrill C, et al. Leadership behavior and subordinate well-being. J Occup Health Psychol 2004;9:165–75. 10.1037/1076-8998.9.2.165 [DOI] [PubMed] [Google Scholar]
- 127. Rooney JA, Gottlieb BH. Development and initial validation of a measure of supportive and unsupportive managerial behaviors. J Vocat Behav 2007;71:186–203. 10.1016/j.jvb.2007.03.006 [DOI] [Google Scholar]
- 128. Fritzen SA. Strategic management of the health workforce in developing countries: what have we learned? Hum Resour Health 2007;5:4 10.1186/1478-4491-5-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Musinguzi C, Namale L, Rutebemberwa E, et al. The relationship between leadership style and health worker motivation, job satisfaction and teamwork in Uganda. J Healthc Leadersh 2018;10:21–32. 10.2147/JHL.S147885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Zakumumpa H, Taiwo MO, Muganzi A, et al. Human resources for health strategies adopted by providers in resource-limited settings to sustain long-term delivery of art: a mixed-methods study from Uganda. Hum Resour Health 2016;14:63 10.1186/s12960-016-0160-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Caillier JG. Toward a better understanding of the relationship between transformational leadership, public service motivation, mission valence, and employee performance. Public Pers Manage 2014;43:218–39. 10.1177/0091026014528478 [DOI] [Google Scholar]
- 132. Caillier JG, Leadership T. And Whistle-Blowing attitudes: is this relationship mediated by organizational commitment and public service motivation? The American Review of Public Administration 2013;45:458–75. [Google Scholar]
- 133. Gould-Williams J. The importance of HR practices and workplace trust in achieving superior performance: a study of public-sector organizations. The International Journal of Human Resource Management 2003;14:28–54. 10.1080/09585190210158501 [DOI] [Google Scholar]
- 134. Alimo-Metcalfe B, Alban-Metcalfe J. Engaging leadership: creating organisations that maximise the potential of their people. CIPD, 2008. [Google Scholar]
- 135. Baumeister RF, Leary MR. The need to belong: desire for interpersonal attachments as a fundamental human motivation. Psychol Bull 1995;117:497–529. 10.1037/0033-2909.117.3.497 [DOI] [PubMed] [Google Scholar]
- 136. Quinn RE. Beyond rational management: mastering the paradoxes and competing demands of high performance. San Francisco, CA, US: Jossey-Bass, 1988. [Google Scholar]
- 137. Krogsgaard JA, Thomsen P, Andersen LB. Only if we agree? how value conflicts moderate the relationship between transformational leadership and public service motivation. International Journal of Public Administration 2014;37:895–907. 10.1080/01900692.2014.928315 [DOI] [Google Scholar]
- 138. McKee MC, Driscoll C, Kelloway EK, et al. Exploring linkages among transformational leadership, workplace spirituality and well-being in health care workers. Journal of Management, Spirituality & Religion 2011;8:233–55. 10.1080/14766086.2011.599147 [DOI] [Google Scholar]
- 139. Plsek PE, Greenhalgh T. The challenge of complexity in health care. BMJ 2001;323:625–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Hazy J. Measuring leadership effectiveness in complex socio-technical systems. E:co 2006;8:58–77. [Google Scholar]
- 141. Kark R, Dijk DV, Lead Mto. Motivation to follow: the role of the self-regulatory focus in leadership processes. Academy of Management 2007;32:500–28. [Google Scholar]
- 142. Avolio BJ, Walumbwa FO, Weber TJ. Leadership: current theories, research, and future directions. Annu Rev Psychol 2009;60:421–49. 10.1146/annurev.psych.60.110707.163621 [DOI] [PubMed] [Google Scholar]
- 143. Brady Germain P, Cummings GG. The influence of nursing leadership on nurse performance: a systematic literature review. J Nurs Manag 2010;18:425–39. 10.1111/j.1365-2834.2010.01100.x [DOI] [PubMed] [Google Scholar]
- 144. Avolio BJ, Reichard RJ, Hannah ST, et al. A meta-analytic review of leadership impact research: experimental and quasi-experimental studies. Leadersh Q 2009;20:764–84. 10.1016/j.leaqua.2009.06.006 [DOI] [Google Scholar]
- 145. Marchal B, Kegels G, Belle SV. Theory and realist methods : Emmel N, Greenhalgh J, Manzano A, Doing realist research. Los Angeles, London, New Delhi: SAGE, 2018: 79–90. [Google Scholar]
- 146. Greenhalgh T, Humphrey C, Hughes J, et al. How do you Modernize a health service? A realist evaluation of Whole-Scale transformation in London. Milbank Quarterly 2009;87:391–416. 10.1111/j.1468-0009.2009.00562.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Anderson RA, Crabtree BF, Steele DJ, et al. Case study research: the view from complexity science. Qual Health Res 2005;15:669–85. 10.1177/1049732305275208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Marion R. Complexity theory for organizations and organizational leadership : Bien MU, Marion R, Complexity leadership, part 1. Charlotte North Carolina: Information Age Publishing, 2008. [Google Scholar]
- 149. Yukl G. Contingency theories of effective leadership : Bryman A, Collinson D, Grint K, The SAGE Handbook of leadership. USA: Sage Publications, 2011: 286–98. [Google Scholar]
- 150. Yin RK. Case study research and applications: design and methods. Thousand Oaks, California, USA: Sage publications, 2018. [Google Scholar]
- 151. Weberg DR. Complexity leadership theory and innovation: a new framework for innovation leadership, 2013. [Google Scholar]
- 152. Forbes-Thompson S, Leiker T, Bleich MR. High-performing and low-performing nursing homes: a view from complexity science. Health Care Manage Rev 2007;32:341–51. 10.1097/01.HMR.0000296789.39128.f6 [DOI] [PubMed] [Google Scholar]
- 153. Plowman DA, Solansky S, Beck TE, et al. The role of leadership in emergent, self-organization. Leadersh Q 2007;18:341–56. 10.1016/j.leaqua.2007.04.004 [DOI] [Google Scholar]
- 154. Cassell C, Symon G. Essential guide to qualitative methods in organizational research. Sage, 2004. [Google Scholar]
- 155. Ferlie E. Organisational studies. studying the organisation and delivery of health services. Routledge, 2004: 36–51. [Google Scholar]
- 156. Murphy E. Micro-level qualitative research. studying the organisation and delivery of health services. Routledge, 2004: 52–67. [Google Scholar]
- 157. Belghiti AA, Boffin N, Brouwere D. L’espace de décision de la gestion des ressources humaines sanitaires au Maroc. Rabat: Royaume du Maroc, Ministère de la santé, 2004. [Google Scholar]
- 158. Cox JB, Estrada SD, Lynham SA, et al. Defining human resource development in Morocco: an exploratory inquiry. Human Resource Development International 2005;8:435–47. 10.1080/13678860500356135 [DOI] [Google Scholar]
- 159. Benson PG, Al Arkoubi K. Human resource management in Morocco. Managing human resources in the Middle East 2006;29:273–90. [Google Scholar]
- 160. Al-Arkoubi K, McCourt W. The politics of HRM: waiting for Godot in the Moroccan civil service. The International Journal of Human Resource Management 2004;15:978–95. 10.1080/09585190410001677278 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2019-033010supp001.pdf (50.1KB, pdf)
bmjopen-2019-033010supp002.pdf (63.8KB, pdf)
bmjopen-2019-033010supp003.pdf (58.1KB, pdf)