Abstract
Introduction
Diabetes management in primary care remains suboptimal in China, despite its inclusion in the essential public health service (EPHS). We aimed to evaluate the effectiveness of a mobile health (mHealth) based and three-tiered diabetes management system in diverse Chinese contexts.
Methods and analysis
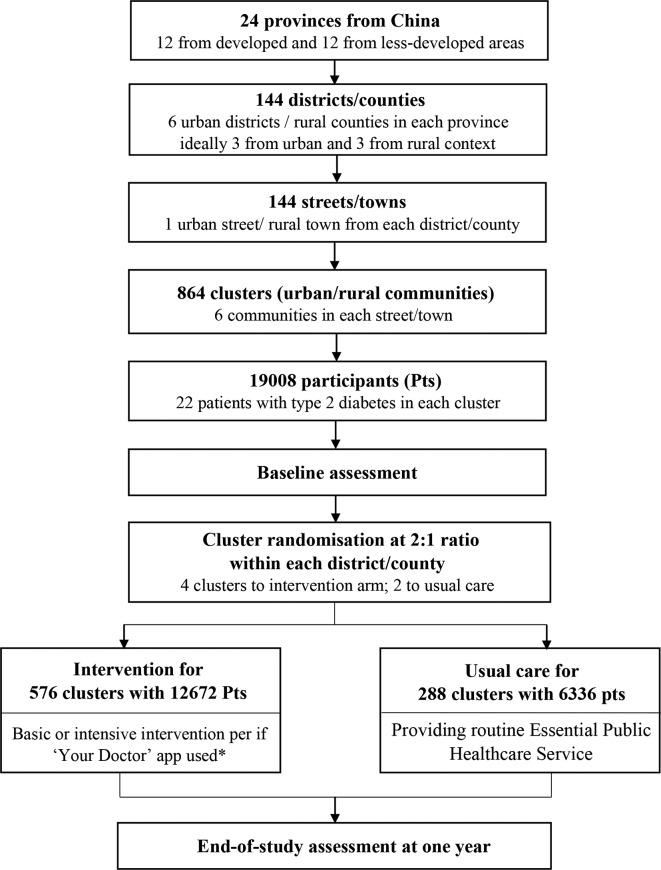
This is a cluster randomised controlled trial, named road to hierarchical diabetes management at primary care (ROADMAP). 19 008 patients with type 2 diabetes (T2D) were recruited from primary care clinics in 864 communities across 144 counties/districts of 24 provinces. Eligible participants were adult patients diagnosed with T2D and registered for diabetes management in communities. Patients within the same communities (clusters) were randomly allocated into the intervention or control arm for 1 year in a 2:1 ratio. The control arm patients received usual care as EPHS packaged: at least four blood glucose (BG) and blood pressure (BP) tests, and lifestyle and medication instruction, yearly, from primary care providers. The intervention arm patients received at least two BG and one BP tests, monthly, and lifestyle and treatment instruction from a three-tiered contracted team. A mHealth platform, Graded ROADMAP, enabled test results uploading and sharing, and patient referral within the team. The intervention participants will be further divided into basic or intensive intervention group according to whether they were actively using the Your Doctor App. The primary outcome is the BG control rate with glycated haemoglobin (HbA1c)<7.0%. Secondary outcomes include control rates and changes of ABC (HbA1c, BP and low-density lipoprotein cholesterol) and fasting BG, hypoglycaemia episodes and health-related quality of life (EuroQol (EQ-5D)).
Ethics and dissemination
The trial has been approved by the Institutional Review Board at Shanghai Sixth People's Hospital. Findings on the intervention effectiveness will be disseminated through peer-reviewed journals, conference presentations and other relevant mechanisms.
Trial registration number
ChiCTR-IOC-17011325.
Keywords: type 2 diabetes, management, primary care, cluster trial, mobile health
Strengths and limitations of this study.
This is a large-scale cluster clinical trial being implemented in diverse primary care settings of most provinces in China. The sample size allows for a formative evaluation of a complex service intervention overall, and in subgroups of developed and less-developed, urban and rural regions.
A standardised 4-in-1 comprehensive management package is designed to empower the capabilities of primary care to improve the overall diabetes management in real-world settings beyond this study.
The intervention delivery is supported by two designated mobile-based information system (Graded ROADMAP, Your Doctor), recording the condition of participants, receipt of services and health education and communications, to ensure the continuum of care with secure access.
A centrally distributed, portable instrument was applied for measuring the primary outcome, glycated haemoglobin (HbA1c), playing a role as a centralised laboratory, thus ensuring the comparability of HbA1c level.
We suggest caution in generalising any intervention benefits to the broader diabetes population, since the recruitment is limited to people with diagnosed type 2 diabetes registered for receiving services under the essential public health service package in China.
Introduction
Type 2 diabetes (T2D) imposes major morbidity, mortality and financial burden across all health systems.1–3 Globally, there are an estimated 425 million people with T2D and one fourth of them reside in China where enormous challenges of diabetes management exist given the large population across diverse settings.1 4–6 Although an essential public health services (EPHS) package, with annual increases in governmental subsides7 was introduced to provide universal access to services for patients with chronic diseases in primary care in China in 2009,8 considerable gaps in care remain.
The EPHS packaged services are delivered by primary care providers through community healthcare service (CHS) centres (sub-district level) and stations (community level) in urban areas, and township hospitals and village clinics in rural areas. Management of those with T2D is an explicit focus of the EPHS package.4 9 By 2017, there were over 9100 CHS centres, 25 500 CHS stations, 36 500 township hospitals and 632 000 village clinics in operation nationwide.10 (Further structural details of the primary care service delivery in China is available in online supplementary appendix 1.) Patients registered for T2D management of EPHS are entitled to at least four free blood glucose (BG) tests, and consultations for treatment and lifestyle advice each year.7 Despite an increasing number of patients receiving T2D management services, from 18.5 million in 2011 to 31.2 million in 2017,11 fewer than 40% of patients had adequate BG control (glycated haemoglobin (HbA1c)<7.0%),12 with only 6% achieving optimal control of combined ABC (HbA1c, blood pressure (BP) and low-density lipoprotein cholesterol (LDL-C)) targets.13
bmjopen-2019-032734supp001.pdf (86.2KB, pdf)
Achieving effective T2D management is heavily dependent on an organised and responsive primary care system.14 15 Inadequate capacity of primary healthcare providers, inefficient resource utilisation and, most importantly, fragmented delivery of care have been identified as major challenges in primary care that have potentially impeded the improvement in diabetes control.4 16–21 It is reported that over 25% of doctors at CHS centres and 45% at township hospitals have not reached the educational requirement for a licensed assistant doctor. Twelve percent of village clinic doctors were below the required education level for their position and one-third of primary healthcare providers do not receive annual training, a requirement of the authorities.4 A skills shortage as a result of inadequate education and training contributes to poorer quality care, partially explaining why patients tend to bypass primary care facilities and present to hospitals.22 Also, the fragmentation of the service delivery system and a lack of interoperable information systems have hindered the integration of the primary care and specialty care in secondary and tertiary hospitals, obstructing the coordination and continuum in care.4
In 2015, national guidelines promoting a graded diagnosis and treatment system were introduced23 in China, in line with the Healthy China 2030 policy24 to establish a cooperative, hierarchical health service system. While evidence on the effectiveness of mobile health (mHealth)-based strategies that involve service delivery design to improve diabetes management is demonstrated,25–31 its adaptability in primary care facilities varies across different economic contexts and regions.32 33 We therefore outline the protocol for a study with the aim of evaluating the effectiveness of a mHealth-based, service-delivery intervention in a cluster randomised controlled trial called road to hierarchical diabetes management at primary care (ROADMAP). The intervention follows the recommendations from the Chinese Diabetes Society (CDS) guideline34 to empower primary care providers in a collaborative tiered care system with mHealth-based health information and referral management system to deliver standardised services for patients with T2D in China.
Methods and analysis
Trial design and study contexts
ROADMAP is a community-based, cluster randomised controlled trial, comparing the effectiveness between the proposed intervention and the usual care on diabetes management in diverse primary care settings (figure 1). Within the intervention arm, participants will be further divided into basic and intensive intervention subgroups, based on whether an optional health education smartphone application is used. The trial will be conducted in over 800 communities in more than 20 provinces of China. To better integrate clinical services and primary care, the implementation of the trial involves three tiers of healthcare institutions: regional medical centres (tier Ⅲ: hospitals at urban district/rural county level), primary care centres (tier Ⅱ: CHS centres at urban sub-district/township hospitals at rural town level) and their subordinate primary care clinics (tier ⅼ: urban CHS stations and rural village clinics at level of community (also refer to village in rural area hereinafter)).
Figure 1.
Flow chart of the ROADMAP study. (1) Provinces in the upper half of provincial gross domestic product per capita in fiscal year of 2017 are classified into developed areas, and those at lower half are less-developed areas; urban or rural areas are classified as per national administrative area category in 2017. (2) Your Doctor app is available for those participants who possess a smartphone and capable of using applications, enabling health education and real-time communication with doctors. Patients who have used ‘Your Doctor’ app will be regarded as receiving intensive intervention.
Study sites selection and participants
Table 1 details the inclusion/exclusion criteria for study sites selection at multiple levels, including provincial, district and county level, sub-district and town level, and community level. 24 provinces will be selected nationally. In general, 6 counties, and 6 of its subordinate communities from each county will be selected in each province. In each community (cluster), an average of 22 participants will be selected at random via a purpose-built website from a full list of T2D patients, normally with over 50 registrants, from local EPHS recipient registry in each community.
Table 1.
Eligibility criteria for study sites in ROADMAP study
| Study site at different levels | Eligibility criteria description |
| Province |
|
| District/county |
|
| Sub-district/town |
|
| Community |
|
mHealth, mobile health; ROADMAP, road to hierarchical diabetes management at primary care; T2D, type 2 diabetes.
Participants will be patients with diagnosed T2D and registered for receiving EPHS in the participating communities. Individuals are eligible for enrolment if they meet following inclusion criteria: aged 18–75 years; residing in the community for the last 6 months with no plan of relocating; voluntary participation with informed consent. Patients will be excluded if: they had severe physical or psychological problems; were unable to attend the site visit; unable to consciously answer questions; were women in the process of, or planning for, pregnancy or breast feeding; and those who have participated in any other clinical trials within the last 6 months.
Randomisation
Randomisation will be performed centrally via a password-protected, encrypted smartphone application interface, stratified by provincial ranking of gross domestic product (GDP) per capita in fiscal year of 2017,35 with upper and lower half categorised as developed and less-developed, respectively, and locality including urban and rural areas as per national administrative area category in 2017. Following baseline data collection, these six communities (ie, clusters) will be randomised to either receive the intervention or continue with usual care in a 2:1 ratio (ie, 4 clusters to intervention, 2 to control).
Interventions
The basic intervention consists of four elements: (1) capacity building for service providers at primary care facilities; (2) team-based contracted standardised services; (3) mHealth-based information support; and (4) reimbursement for service delivery. The basic intervention elements are elaborated in the next paragraph. There is an additional intensive component available to participants with smartphones willing to use Your Doctor. Your Doctor is a smartphone application supporting health education (examples are available in the online supplementary appendix 2) and treatment instruction through real-time within-app interaction between the patients and their contacted doctors. Active users are defined as those with a login to Your Doctor at least four times throughout the 1-year study period. At the end of study, participants in the intervention arm will be divided into two groups (basic or intensive), based on their level of activity on Your Doctor.
bmjopen-2019-032734supp002.pdf (19.2KB, pdf)
Capacity building
Two compulsory structured training sessions will be held at the provincial and county level. The initial provincial-level training session is for doctors from participating county hospitals. This will be followed by training at the district/county level, where the qualified trainers provide training for the sub-district/township and community doctors. The training materials were developed by the working group based on current diabetes guidelines, with the purpose of upskilling service providers by addressing theoretical and operational barriers to T2D management and treatment in primary care settings. The contents include: (1) diabetes epidemiology and economic burden; (2) classification and diagnosis of diabetes; (3) hierarchical diagnosis and treatment of diabetes; (4) diabetes lifestyle intervention; (5) diabetes medication; (6) BG monitoring; (7) diabetic retinopathy; (8) diabetic nephropathy; (9) diabetic peripheral neuropathy; and (10) diabetic lower limb vascular diseases. The trainings are standardised to ensure the service would be delivered in the same manner. A package of training materials, including a set of Powerpoint slides and videos, will be sent to all doctors in the intervention arm for periodic review. Investigators in the control arm will only attend trainings for subject recruitment and data collection procedures for baseline and end-of-study assessments.
Team-based contracted services
A three-tiered care team will be assembled for each participating community. The team members comprise of three doctors, respectively, from the primary care clinic, primary care centre and regional medical centre. The primary care doctors will play a key role in routine contacting, monitoring and evaluation, service delivery and lifestyle instructions to the patients. Doctors in the regional medical centres will provide further consultation or treatment if referred to. A service contract will be signed between the care team doctors and participants to acknowledge the engagement and inform stakeholders’ responsibilities. (A full list of contracted services are available in the online supplementary appendix 3.) The planned services are listed in table 2 with comparison to those in EPHS as usual care.
Table 2.
Diabetes management related training, technical support and health services provided for intervention and control arms
| Items | Control arm (usual care per EPHS) |
Intervention arm (Strengthened care in addition to EPHS) |
| Capacity building for primary care providers | Provided by local health bureau, aims to implement EPHS, no national standard training material. | Trained by qualified trainers using national standard training materials, addressing major gaps in knowledge and skills in diabetes management, including diabetic peripheral neuropathy screening. |
| Technical support | Equipped with BG meter, BP monitor and body weight/height scale. Mostly equipped with electronic medical record system but unable to communicate with local medical centres. | Equipped with (1) a portable electronic BG meter that enables the test result uploaded to an electronic information platform in real time; (2) Graded ROADMAP, the platform, developed by the working group, acts as an electronic medical record system with features of communication with electronic BG monitors and patient referral among doctors in the same care team; and (3) a set of 128 Hz tuning forks and 10 g nylon monofilaments used to screen peripheral neuropathy. |
| Basic BG monitoring | At least four times of fasting BG test per year | Monthly or more frequently, ideally one fasting and one postprandial BG each time, emphasised as compulsory, with the hypothesis that the increased BG monitoring can improve behaviour change and medication activities. |
| Basic BP monitoring | At least four times per year | Monthly or more frequently, emphasised as compulsory. |
| Diabetic peripheral neuropathy screening | Not required | At least once per year with the hypotheses that (early) knowledge of diabetes complications can improve the adherence to diabetes control. This was suggested to start at the beginning of intervention. |
| Diet, physical exercise and medication instruction | Each time during face to face visit | Face to face, together with remote (online) communication through ‘Your Doctor’, an App supporting health education and treatment instruction through interactive real-time communication between the contacted doctors and patients (intensive intervention subgroup). |
| Patient referral | Major indications: (1) BG remains uncontrolled for two consecutive visits; (2) adverse drug reactions do not improve after two consecutive visits; or (3) new or aggravated complications. Pathway: no designated pathway; patients can seek service from any doctor in any hospital according to their wishes. |
Indications: similar to those in control arm. Pathway: The referral is designed to be processed (initialed/accpeted or rejected) through the Graded ROADMAP app, hypothesizing that the mHealth-based referral within the contracted team would improve the referral and diabetes control. This app has different end-users. A primary care doctor can make the appointment for the patient by selecting a referral doctor (usually the doctor in the same team) and date based on the availability of upstream doctors and wishes of patients. The medical record, including the trend of BG and medications, could be accessed by all the authorised doctors. |
BG, blood glucose; BP, blood pressure; EPHS, essential public health service.
bmjopen-2019-032734supp003.pdf (23.7KB, pdf)
mHealth-based information support
Most intervention activities will be carried out by or through Graded ROADMAP App (some user interfaces are displayed in the online supplementary appendix 4), including medical information recording, BG/BP monitoring, processing of referral requests and responses (referral indications are available in the online supplementary appendix 5) and performance reviews. The user ends vary with the services provided by different users. Patient data are only accessible within the contracted care team to ensure the continuum in care. For intensive group patients, Your Doctor App will be used to share their BG/BP results and interact with their doctors for better diabetes control.
bmjopen-2019-032734supp004.pdf (130.5KB, pdf)
bmjopen-2019-032734supp005.pdf (68.9KB, pdf)
Reimbursement for service delivery
Non-mandatory seasonal payments, RMB 55 per participant averagely, are suggested every 3 months to compensate care providers’ extra work hours for additional service delivery and also serve as a ‘fee for performance’ incentive for protocol compliance. The performance of the service is appraised by the aggregated data from an algorithm incorporating BG/BP measurements and control, the number of screening for any complication of T2D and necessary referrals. The amount of the reimbursement is capped at RMB 220 Yuan for each patient per year. It is estimated to be equivalent to one-tenth of per capita public input for EPHS, which is acceptable by the government if the intervention is effective.
To sum up, with support of Graded ROADMAP, the key and fundamental intervention in our study is to offer the patients with access to more frequent BG and BP monitoring services, and followed by corresponding instructions on lifestyle modification and medication treatment.
Usual care
Participants in the control arm will continue receiving usual care provided by primary care facilities, as per EPHS regulations. For community patients with T2D, the key services provided by primary care facilities were presented in table 2. Several other related services in EPHS include developing personal health records, updating health records after follow-ups, population-based health education, health management for the elderly with annual services including lifestyle and health assessment, physical examination, and health guidance for the elderly over 65 years of age, and hypertension management.7 Theoretically, all services provided to usual care were also delivered to the intervention arm.
Outcomes
The primary outcome is the change of BG control rate with HbA1c<7.0% between baseline and 1-year follow-up. Secondary outcomes include levels and control rates of ABC (HbA1c<7.0%, BP <140/80 mm Hg and LDL-C<2.6 mmol/L) targets, and fasting BG<7.0 mmol/L, episodes of hypoglycaemia (BG<3.9 mmol/L) and mean changes in health-related quality of life on the EQ-5D.
Data collection and management
Table 3 outlines the procedures for collecting baseline and end-of-study data through a secure password protected mobile electronic data capture (mEDC) app. The data collecting investigators who are unaware of the allocation are trained and not involved in intervention implementation. The primary outcome will be obtained from a centrally distributed HbA1c analyser (A1c EZ 2.0) for point-of-care testing.36 Anthropometric measurements are taken with the patient barefoot in light clothing. Standard laboratory tests of blood and urine samples, including fasting glucose, lipid profile, creatinine, and kidney function, will be performed by qualified laboratories at regional medical centres. Two extra blood samples (blood biochemistry analysis and HbA1c) and one urine sample from each village will be audited for accuracy. The mEDC has embedded features to allow logic checks and photography of source documents to support real-time data collection process overseen.
Table 3.
Data collection outline of ROADMAP study
| Assessment description | Patient screening |
Baseline assessment |
End-of-study assessment |
| Informed consent | X | ||
| Eligibility | X | X | |
| Reasons for non-participation | X | X | |
| Demographics, socio-economic status | X | ||
| Medical history, diabetes-related complications screenings | X | X | |
| Anthropometric measurements, physical examination, vital signs | X | X | |
| Diabetes self-management | X | X | |
| Costs of healthcare use | X | X | |
| Medications and treatment adherence | X | X | |
| Laboratory results | X | X | |
| Quality of life questionnaire | X | X | |
| Loss-to-follow-up/drop-out questionnaire | X |
Data collection, storage and reporting conforms to China’s privacy laws. Individual participants are encrypted and de-identified. Feedback and queries raised on data integrity, authenticity and accuracy, as well as schedule management, are achieved using unique identifier reporting. Findings raised from this study will be reported without individual participant identification.
Project management
A trial monitoring website presents aggregated regional routinely collected data on community/township/county/provincial levels of intervention clusters to allow researchers, investigators and doctors in the intervention group to monitor the intervention fidelity and study progress. Central and on-site monitoring of routinely collected data is undertaken by a project management team. All required qualification assessments for institutions/personnel involved in the study, including their training and investigative procedures, are recorded and photographed for reference. During each site visit, local investigators and trial staff assist research monitoring in verifying patient eligibility, data authenticity and implementation consistency, schedule compliance, and in providing all relevant source documents.
Sample size estimation
This study aims to recruit 19 008 patients with T2D from 864 communities in 24 provinces in mainland China, which equates to 22 patients from each community. Accounting for potential loss to follow-up of 14% in patients, a sample size of 16 416 participants (10 944 in intervention and 5472 in control groups, with 2:1 ratio) at 1 year will provide a power of 89% (2-sided α 0.05) to detect a ≥5% absolute increase in the primary outcome in the intervention group. The sample size calculation assumes that 40% of participants will have well-controlled HbA1c (<7%) at the end of the study in the control group,13 with an intra-class correlation coefficient of 0.15 based on our previous Observational Registry for Basal Insulin Treatment (ORBIT) study.37 Furthermore, assuming that 50% (5472) of participants in the intervention group will become the active users of the Your Doctor App at their discretion, thus forming an intensive intervention subpopulation (ie, a smaller cluster size of 9 participants), which will provide 86% and 99% power to detect absolute increases of 5% and 10% of HbA1c control, respectively, compared with the control group.
Outcome analysis
All analyses will be conducted at the participant level following the intention-to-treat principle. The primary endpoint, adequate control of HbA1c at 1 year, will be compared between all intervention groups and all control groups. The primary analysis of the intervention effect will be conducted by using a log-binomial regression with generalised estimating equations to account for clustering within communities with adjustment of baseline HbA1c as a continuous covariate. Secondary analyses will include (1) covariate-adjusted analyses, on the primary outcome, (2) comparison of the intensive versus basic intervention groups by exploring if there is an additional effect from intensive intervention and (3) subgroup analyses. A detailed statistical analysis plan is anticipated to be published prior to database lock or attached to the main paper.
Process evaluation
Given the widespread geographical coverage of participating sites, the staffing model and implementation of the ROADMAP intervention may differ across different regions. A process evaluation will be conducted during implementation to assess the compliance of each intervention component and identify the implementation barriers and facilitators, as well as the acceptability to improve the implementation quality and intervention fidelity. A mixed-methods approach will be adopted using routinely collected data (eg, BG/BP monitoring data) and stakeholder interviews. The lessons from different regions with different staffing models will be helpful to guide the future intervention diffusion to different primary care settings.
Economic evaluation
The economic evaluation will assess cost-effectiveness/utility from a health sector perspective, with a trial-based component and beyond-trial modelled evaluation of long-term costs and benefits, assessed using an incremental cost-effectiveness ratio. The within-trial cost will include intervention costs on trainings of staff, BG testing device and consumables, information system development and maintenance and service reimbursement, as well as healthcare use during the trial period. The effectiveness/utility will be according to the change on HbA1c within 1 year, and modelled on health-related quality of life based on the literature for the relationship of HbA1c reduction and prevention of T2D complications and improved health-related quality of life. Sensitivity analyses will be carried out to examine different scale-up scenarios in different strata.
Governance
Execution of the study is managed by a working group under the supervision of a steering committee, chaired by the leading principal investigators (PI) and representatives of the CDS and central government. The working group comprises delegates of China representative office of The George Institute for Global Health, CDS, Bethune Charity Foundation and provincial investigators.
Trial status
After the launch of the pilot phase in March 2017, the first provincial site for the main study was initiated on 2 June 2017. Up to December 2018, 19 149 participants had been validly recruited from 864 communities in 144 districts/counties in 25 participating provinces. One more province was recruited due to the difficulty in finding sufficient eligible district/county hospitals as planned in 24 provinces. Baseline assessments are complete and the intervention has commenced in 576 communities from 25 provinces. The final end-of-study assessment is due in October 2019 and database lock is anticipated for December 2019.
Patient and public involvement
Regional investigators and doctors from primary care facilities have had input into the study design, the development of the intervention tools, pilot testing phase and implementation of the intervention through roundtable and periodical national/regional review meetings. Participating doctors will be informed of study progress through monthly newsletters and progress reports. Patients with T2D in different areas have been interviewed for needs analysis at the preparatory and pilot phases, and will be interviewed again about implementation barriers and facilitators and the burden of their participation as part of a process evaluation at the end of the study. To encourage active engagement, participants receive their results from baseline and end-of-study assessments. The main results of the study will be disseminated to doctors and participants to boost community involvement in T2D management beyond the study.
Ethics and dissemination
Written approval from each participating site was granted by the local hospital research ethics committee and other relevant regional regulatory bodies. Signed informed consent is obtained from all trial participating doctors and patients prior to participant recruitment. Findings from this study will be widely disseminated through peer-reviewed journals, conference presentations, social media and other mechanisms.
Discussion
We outline the design for a large cluster clinical trial to evaluate the effectiveness of an innovative 4-in-1 T2D management model of care in China, to generate evidence for future scale up. Given the disparities in care under different contexts, the study areas are randomised according to stratification of developed or less-developed, urban or rural areas. The large sample size will enable us to appraise the effectiveness of the intervention overall and across each strata. Meanwhile, information collected on the barriers and facilitators of the intervention will better inform post-evaluation implementation and future scale up.
ROADMAP is complex in the intervention design per se and its implementation. We prepared for almost 2 years to develop and pilot the intervention as well as the project management and data collection system with the involvement of local doctors, patients and project managers. To make the 1-year intervention implemented successfully, we did not launch the project in 25 provinces (the plan was 24 provinces) in parallel, but launched one by one within a whole year, allowing lessons learnt to be transferred sequentially. Due to the limited research implementation experiences of most primary care investigators, it causes great challenges to ensure the quality of research implementation at the grassroots level. The use of two mobile phone-based project management and data collection systems (mEDC) helped to facilitate the implementation of the study with standard procedures and quality.
Intervention fidelity is another major challenge, especially considering the complexity of the ROADMAP, such as the number of study sites, and the shortage in qualified primary care workforce. mHealth technology-mediated strategies have therefore been developed and applied to prevent and address inconsistencies occurring throughout the implementation. Besides, a governance system has been built up which includes provincial primary investigators and endorsed by the CDS.
Reimbursement, or pay for performance, may affect the service providers’ motivation and quality of care. It might be argued that if the reimbursement is only given to the intervention group, the effectiveness between the two arms would be incomparable. The study working group set a cap to the payment amount. On one hand, the reimbursement intends to serve as an additional workload compensation for the staff in the intervention groups. On the other hand, since it would be included as intervention-based cost, its cost-effectiveness may inform further policy adoption. During project implementation, local medical centres will determine the provision of reimbursements. The actual amount of this payment will be recorded in the project management system for health economics analysis.
To address the inconvenience and huge cost of centralised laboratory tests, we adopted a unified, portable, proven accurate instrument for measuring HbA1c, thus avoiding measurement error arising from the use of discrepant devices/systems. However, all other laboratory tests were performed by local county hospitals. The machines, methods and laboratory skills are different among hospitals although all of the routine sample (blood and urine) tests are under supervision and authorised by the government. We also collected the information of machines and methods for biochemical testing from all the participating hospitals.
China’s health reform is still ongoing. Policy around the services delivery and financing of primary healthcare may encounter regional adjustment during the intervention period. We will record relevant policy changes but it still could potentially influence implementation and outcomes.
As all participants have been randomly recruited from the lists of those registered T2D in the communities, they are likely to be broadly representative of those with the condition in the real-world and thus enhance the generalisability of the results. We recognise, however, that our findings may not be extrapolated to those with undiagnosed or unregistered T2D.
We anticipate that ROADMAP would be implemented successfully, and the evaluation processes conducted with high quality. Most importantly, we hope this real-world trial could successfully contribute to the improvement of the management of T2D in China.
Supplementary Material
Acknowledgments
The authors acknowledge personnel who engaged in helping us accomplish all trial procedure. Thanks for the support from trial steering committee and efforts made by road to hierarchical diabetes management at primary care working group; all participating clinical research associates; investigators; doctors and patients, as well as those who helped to facilitate trial preparation; execution and evaluation. We thank Professor Craig Anderson for providing constructive guidance in writing this manuscript. We also thank Thomas Lung for proofreading the manuscript.
Footnotes
Contributors: WJ and PZ conceived the project, designed the study, equally. WJ, PZ, ND, DZ, HL, YB and XL contributed to the design of the intervention and the evaluation. ND and PZ wrote the first draft of the manuscript. YL led the development of the electronic systems involved in road to hierarchical diabetes management at primary care intervention and trial management. XL was the statistician of the study. All authors contributed to the refinement of the study protocol and approved the final manuscript.
Funding: This study receives its principle funding from following organisations: (1) Bethune Charity Foundation provides blood glucose (BG) monitoring and supporting decision-making system, BG monitoring equipment (smart BG meters) and consumables and project implementation fund required in the study (path-through cost for county hospitals to support the intervention, data collection and performance incentives) as scheduled in accordance with the provisions of this agreement. (2) George Institute for Global Health provides financial and personnel support for, including but not limited to, training, institutional review board, project and data management, qualitative analysis, statistics and result publication.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. International Diabetes Federation IDF diabetes atlas. 8th edn Brussels, Belgium: International Diabetes Federation, 2017. http://www.diabetesatlas.org [Google Scholar]
- 2. Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration Cardiovascular disease, chronic kidney disease, and diabetes mortality burden of cardiometabolic risk factors from 1980 to 2010: a comparative risk assessment. Lancet Diabetes Endocrinol 2014;2:634–47. 10.1016/S2213-8587(14)70102-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Seuring T, Archangelidi O, Suhrcke M. The economic costs of type 2 diabetes: a global systematic review. Pharmacoeconomics 2015;33:811–31. 10.1007/s40273-015-0268-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Li X, Lu J, Hu S, et al. . The primary health-care system in China. The Lancet 2017;390:2584–94. 10.1016/S0140-6736(17)33109-4 [DOI] [PubMed] [Google Scholar]
- 5. Huo L, Shaw JE. Type 2 diabetes: challenges facing GPs. Fam Med Community Health 2018;6:26–31. 10.15212/FMCH.2018.0107 [DOI] [Google Scholar]
- 6. Jin Y, Zhu W, Yuan B, et al. . Impact of health workforce availability on health care seeking behavior of patients with diabetes mellitus in China. Int J Equity Health 2017;16 10.1186/s12939-017-0576-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ministry of finance, PRC (2019) report on the execution of the central and local budgets for 2018 and on the draft central and local budgets for, 2019. Available: http://www.xinhuanet.com/english/2019-03/17/c_137901687.htm [Accessed 25 Jun 2019].
- 8. Ministry of Health, PRC Opinions on promoting the essential public health services gradually equalization, 2009. Available: http://www.nhc.gov.cn/wjw/gfxwj/201304/6cf4917e8af44fe28ac655f215f8e4ed.shtml [Accessed 25 Jun 2019].
- 9. People's Republic of China health system review. Manila : WHO Regional Office for the Western Pacific; 2015. (pg.20-21:139–42.
- 10. National Health and Family Planning Commission of the People’s Republic of China China health and family planning statistical yearbook 2017. Beijing: Peking Union Medical College Publishing House, 2018. [Google Scholar]
- 11. 2016 health system reform progress monitoring report, 2017. Available: http://www.nhc.gov.cn/tigs/ygjb/201707/72dbee11426a48cfbe66325c20099c5f.shtml?from=singlemessage&isappinstalled=0#10006-weixin-1-52626-6b3bffd01fdde4900130bc5a2751b6d1. [Accessed 20 Sep 2019].
- 12. Xu Y, et al. Prevalence and control of diabetes in Chinese adults. JAMA 2013;310:948–59. 10.1001/jama.2013.168118 [DOI] [PubMed] [Google Scholar]
- 13. Ji L, Hu D, Pan C, et al. . Primacy of the 3B approach to control risk factors for cardiovascular disease in type 2 diabetes patients. Am J Med 2013;126:925.e11–925.e22. 10.1016/j.amjmed.2013.02.035 [DOI] [PubMed] [Google Scholar]
- 14. Davidson JA. The increasing role of primary care physicians in caring for patients with type 2 diabetes mellitus. Mayo Clinic Proceedings 2010;85:S3–4. 10.4065/mcp.2010.0466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. International diabetes Federation. recommendations for managing type 2 diabetes in primary care, 2017. Available: www.idf.org/managing-type2-diabetes [Accessed 25 Jun 2019].
- 16. Meng Q, Mills A, Wang L, et al. . What can we learn from China’s health system reform? BMJ 2019;l. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yuan B, Balabanova D, Gao J, et al. . Strengthening public health services to achieve universal health coverage in China. BMJ 2019;33 10.1136/bmj.l2358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Yue J, Mao X, Xu K, et al. . Prevalence, awareness, treatment and control of diabetes mellitus in a Chinese population. PLoS One 2016;11:e0153791 10.1371/journal.pone.0153791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ahmad NS, Islahudin F, Paraidathathu T. Factors associated with good glycemic control among patients with type 2 diabetes mellitus. J Diabetes Investig 2014;5:563–9. 10.1111/jdi.12175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lou Q, Wu L, Dai X, et al. . Diabetes education in mainland China—A systematic review of the literature. Patient Educ Couns 2011;85:336–47. 10.1016/j.pec.2011.01.006 [DOI] [PubMed] [Google Scholar]
- 21. Choi TST, Davidson ZE, Walker KZ, et al. . Diabetes education for Chinese adults with type 2 diabetes: a systematic review and meta-analysis of the effect on glycemic control. Diabetes Res Clin Pract 2016;116:218–29. 10.1016/j.diabres.2016.04.001 [DOI] [PubMed] [Google Scholar]
- 22. Liu Y, Zhong L, Yuan S, et al. . Why patients prefer high-level healthcare facilities: a qualitative study using focus groups in rural and urban China. BMJ Global Health 2018;3:e000854 10.1136/bmjgh-2018-000854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. State Council, PRC Guiding opinions of the general office of the state Council on Propelling building of grading diagnosis and treatment system, 2015. Available: http://www.gov.cn/zhengce/content/2015-09/11/content_10158.htm [Accessed 25 Jun 2019].
- 24. CPC Central Committee, State Council. The plan for “Healthy China 2030”, 2016. Available: http://www.gov.cn/xinwen/2016-10/25/content_5124174.htm [Accessed 25 Jun 2019].
- 25. Johnston L, Zemanek J, Reeve MJ, et al. . The evidence for using mHealth technologies for diabetes management in low- and middle-income countries. J Hosp Manag Health Policy 2018;2 10.21037/jhmhp.2018.07.01 [DOI] [Google Scholar]
- 26. Reynolds R, Dennis S, Hasan I, et al. . A systematic review of chronic disease management interventions in primary care. BMC Fam Pract 2018;19 10.1186/s12875-017-0692-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mitchell GK, Burridge L, Zhang J, et al. . Systematic review of integrated models of health care delivered at the primary-secondary interface: how effective is it and what determines effectiveness? Aust J Prim Health 2015;21:391 10.1071/PY14172 [DOI] [PubMed] [Google Scholar]
- 28. Morrison F, Shubina M, Turchin A. Encounter frequency and serum glucose level, blood pressure, and cholesterol level control in patients with diabetes mellitus. Arch Intern Med 2011;171:1542 10.1001/archinternmed.2011.400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Coupe N, Peters S, Rhodes S, et al. . The effect of commitment-making on weight loss and behaviour change in adults with obesity/overweight; a systematic review. BMC Public Health 2019;19 10.1186/s12889-019-7185-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ralston JD, Rutter CM, Carrell D, et al. . Patient use of secure electronic messaging within a shared medical record: a cross-sectional study. J Gen Intern Med 2009;24:349–55. 10.1007/s11606-008-0899-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bredfeldt CE, Compton-Phillips AL, Snyder MH. Effects of between visit physician-patient communication on diabetes recognition program scores. Int J Qual Health Care 2011;23:664–73. 10.1093/intqhc/mzr061 [DOI] [PubMed] [Google Scholar]
- 32. Song S, Yuan B, Zhang L, et al. . Increased inequalities in health resource and access to health care in rural China. Int J Environ Res Public Health 2018;16:49 10.3390/ijerph16010049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Zhang T, Xu Y, Ren J, et al. . Inequality in the distribution of health resources and health services in China: hospitals versus primary care institutions. Int J Equity Health 2017;16 10.1186/s12939-017-0543-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chinese Diabetes Society National Office for Primary Diabetes Care. National guidelines for the prevention and control of diabetes in primary care(2018). Zhonghua Nei Ke Za Zhi 2018;57:885–93. [DOI] [PubMed] [Google Scholar]
- 35. National Bureau of statistics of China. China statistical Yearbook 2017, 2018. Available: http://www.stats.gov.cn/tjsj/ndsj/2017/indexeh.htm [Accessed 25 Jun 2019].
- 36. Zhou R, Wang W, Song Z-X, et al. . Evaluation of a new hemoglobin A1c analyzer for point-of-care testing. J Clin Lab Anal 2018;32:e22172 10.1002/jcla.22172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ji L, Zhang P, Weng J, et al. . Observational registry of basal insulin treatment (orbit) in patients with type 2 diabetes uncontrolled by oral hypoglycemic agents in China—Study design and baseline characteristics. Diabetes Technol Ther 2015;17:735–44. 10.1089/dia.2015.0054 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2019-032734supp001.pdf (86.2KB, pdf)
bmjopen-2019-032734supp002.pdf (19.2KB, pdf)
bmjopen-2019-032734supp003.pdf (23.7KB, pdf)
bmjopen-2019-032734supp004.pdf (130.5KB, pdf)
bmjopen-2019-032734supp005.pdf (68.9KB, pdf)