Abstract
Neuropsychiatric disorders stem from gene-environment interaction and their development can be, at least in some cases, prevented by the adoption of healthy and protective lifestyles. Once full blown, neuropsychiatric disorders are prevalent conditions that patients live with a great burden of disability. Indeed, the determinants that increase the affliction of neuropsychiatric disorders are various, with unhealthy lifestyles providing a significant contribution in the interplay between genetic, epigenetic, and environmental factors that ultimately represent the pathophysiological basis of these impairing conditions. On one hand, the adoption of Healthy Eating education, Physical Activity programs, and Sleep hygiene promotion (HEPAS) has the potential to become one of the most suitable interventions to reduce the risk to develop neuropsychiatric disorders, while, on the other hand, its integration with pharmacological and psychological therapies seems to be essential in the overall management of neuropsychiatric disorders in order to reduce the disability and improve the quality of life of affected patients. We present an overview of the current evidence in relation to HEPAS components in the prevention and management of neuropsychiatric disorders and provide suggestions for clinical practice.
Keywords: neuropsychiatry, diet, motor activity, sleep, quality of health care
Introduction
Neurological and psychiatric disorders are among the non-communicable diseases that are associated the most with several years lived with disability, and are currently, and will likely become progressively, part of a pervasive illness affecting physical and mental fitness.1 Indeed, these conditions continue to show a large prevalence in the general population and, in the last 10 years, a further increase in all-age years lived with disabilities has been observed for both neurological (mean increase in counts of 17.8%) and mental (mean increase in counts of 13.5%) disorders.2 These conditions encompass a wide range of illnesses that affect brain anatomy and function, such as schizophrenia spectrum disorders, mood and anxiety disorders, cognitive disorders with collateral alterations of attention, mood, emotion, and memory. Diagnosis and management is often arduous because symptoms may derive from neurological, psychological, or iatrogenic causes and can easily lead to poor course and outcome. The overlap of etiopathogenetic phenomena led to the existence of multifaceted spectra and multiple specifiers, such as the “with anxious distress” in major depressive episodes, the schizo-obsessive3 phenotype, or the tic-related obsessive-compulsive disorder,4 thus stressing the need for a holistic approach in neuropsychiatric disorders now more than ever. Although the current psychotropic drug- and psychotherapy-centered approaches are deemed effective for many patients, some show pharmacological refractoriness or are unable to tolerate side effects, and physical treatments have been largely implemented.5 Despite the fact that determinants increasing the burden of neuropsychiatric diseases are various, the behavioral factors still provide the highest contribution over metabolic and environmental/occupational risks. According to the Institute for Health Metrics and Evaluation (IHME) classification, the behavioral risks mainly comprise bad dietary habits, smoking, malnutrition, alcohol use, and low physical activity.2 A consistent body of literature identifies eating patterns and physical activity as crucial determinants for physical and mental fitness, the latter being associated to a good sleep. In fact, the brain governs basic sleep/wake cycle, behavioral states and shapes cognitive functions, and sleep disturbances are often associated to a stressed body and mind. Sleep changes are often the earliest signs of several neuropsychiatric disorders, but have also been considered as state markers for mental illnesses, partly as our genetic makeup.6
For the purpose of the present overview, data from Google Scholar, PubMed, and Scopus databases were searched and reviewed, focusing on publications regarding diet, physical fitness, and sleeping patterns in the prevention and overall management of neuropsychiatric disorders, mainly encompassing schizophrenia spectrum disorders, mood disorders, anxiety disorders, and neurocognitive disorders. The search considered relevant studies to introduce the rationale for each section and discuss retrospective and prospective clinical trials, systematic and non-systematic reviews, meta-analyses, guidelines and expert opinions. Our ultimate aim was to deliver practical suggestions for neuropsychiatrists and clinical psychologists that can support the application of a program covering Healthy Eating education, Physical Activity planning, and Sleep hygiene (HEPAS).
Healthy Eating in Neuropsychiatry
Eating is essential to life, as well as breathing, sleeping, and evacuating. We eat for hunger, for pleasure, for boredom, and for addiction.7 Most people eat three meals plus snacks daily, which is an unusual eating pattern from an evolutionary perspective,8 as we have been purely hunters and gatherers for thousands of years. Food had always influenced our mental abilities: the ability to harness fire and cook food allowed the brain of the Homo erectus to grow over 1.8 million years ago,9 with the progressive hypotrophy of masseter and pterygoid muscles allowing cranial development since the consumption of raw and fibrous meat was abandoned. Brain activity is constant, with activity peaks that depend on what the mind is involved in. This activity requires relentless supply of fuel that is mainly glucose, but may also be of non-carbohydrate origin, with a variety of crucial vitamins, minerals, and trace elements integrating core processes. Mechanisms through which diet influences brain functions are likely to be numerous and composite. They mainly comprise the modulation of neuronal energy metabolism and the epigenetic regulation of synaptic plasticity.10 As such, foods can affect brain function according to the content or lack of nutrients.11,12 Food components have a role in brain development since the early orchestration of morphogenic signaling13 towards late fetal and early postnatal life,14 till the modulation of adult neurogenesis. Foods routinely affect brain even if not consumed with the involvement of rewarding mechanisms.15 Substantial improvements have been achieved in the field of nutraceuticals, with antioxidant properties, immune system modulation, and neurotrophic activity16 being just some of the effects attributed to food substances that are concentrated and sold as dietary supplements.16–18 However, while nutrients are thoughtfully absorbed by the body, non-nutritive compounds less easily cross physiological barriers and targeted drug delivery system would be needed to properly enhance their bioavailability.19
Hunters and gatherers no longer exist, but food availability is almost excessively guaranteed with a wealth of ready-to-eat, high-calorie, tasty products, as if there was the threat of food famine. Most people have forgotten that food is medicine.20 In the following paragraphs, we describe and discuss: I) the reciprocal relationship between diet and neuropsychiatric disorders, II) existing methods to assess eating habits, III) practical suggestions to promote healthy eating.
The Reciprocal Relationship Between Diet and Neuropsychiatric Disorders
The existence during early stages of life span of a bidirectional relationship between healthy diet and superior mental health has been shown by many epidemiologic studies.21 Single food components are considered as significant exposure variables that concur to cause various neuropsychiatric conditions. For instance, even if neurons primarily rely on glucose to function, a high intake of sugars may be noxious and may increase the risk for depression22 and neurocognitive impairment.23,24 Indeed, the importance of the dietary pattern as a modifiable risk factor for mental illness gave birth to the nutritional psychiatry field.25,26 Unfortunately, poor dietary choices are made by patients suffering from schizophrenia,27 tics, obsessions, and compulsions,28–31 thus further exposing patients to nutritional deficiencies that are associated with worse mental health issues.32 Moreover, unhealthy diet was reported for bipolar patients33 and patients with depressive and anxiety disorders.34 Drug therapy can easily predispose to worse physical health, being some psychotropics obesogenic in nature.35 As soon as an individual adopts an unhealthy dietary pattern, his mental functions could be exposed to negative anatomical variations in critical brain areas, such as the hippocampus.36,37 Vascular impairments, because of glycemic alterations, may have a role in the development of dementia38 and psychiatric conditions.22 Cognitive deficits were found in individuals consuming sugar-sweetened beverages.39 A new frontier in nutritional psychiatry is stemming from research targeting the modulation of the gut microbiota. In fact, diet is a direct modulator of gut microbiota, whose role has been extensively studied not only in association with neuropsychiatric diseases, but also with subclinical emotional states,40 possibly evoked by the production of specific neurotransmitters.12 Besides having a role in food and drug metabolism, gut microbiota composition seems to either influence or be influenced by numerous neuropsychiatric conditions, through the induction of dysbiosis and alteration of gut permeability, which can, in turn, release pro-inflammatory mediators, activate the immune system and induce a state of low-grade inflammation.41 All these mechanisms can alter brain functioning at various levels, with repercussions on mental health.
Existing Methods to Assess Eating Habits
Diet quality, quantity, meal timing, and environment are four features characterizing eating patterns. Past dietetic habits may be meticulously analyzed through dietetic history questionnaires (eg, those developed by the National Cancer Institute can be found here https://epi.grants.cancer.gov/dhq3/), whereas more recent eating behaviors can be derived from a seven-day food diary that can be either paper-based or web-based.42 Dietetic history questionnaires are certainly more time-consuming, consisting of 135 food and beverage items and 26 dietary supplement questions. Objective evaluations of eating behaviors are quite difficult to acquire, and subjective questionnaires are widely used. Seven-day food diary is the most suitable method for an objective analysis, but also body weight changes may indeed objectively reflect all the four features of eating patterns. Dietary habits of neuropsychiatric patients might be investigated through less time-consuming tests that evaluate how similar patient’s diet is to the Mediterranean dietary pattern, which is the one recognized as the healthiest. In fact, this diet has been implemented worldwide from European to American populations.43 It is mainly characterized by appropriate intakes of vegetables, fruits, whole grains, dairy products, seafood, lean meats and poultry, eggs, legumes, nuts, olive oil, and alcohol. Calories from added sugars and saturated fats should be limited and sodium intake should be reduced. Healthy eating is inexpensive, and low-income individuals can afford it.44 Higher adherence to these dietary guidelines is associated with reduced total, cardiovascular, and cancer mortality risks45 and better general physical health.46 Average intakes of different food groups are far from recommended amounts: about 75% of the Americans has an eating pattern that is low in vegetables, fruits, dairy, and oils, and most of subjects exceed the recommendations for added sugars, saturated fats, and sodium,47 with important differences during the transition from adolescence to young adulthood.48 In younger patients, the test of Serra-Majem and colleagues can be used for non-quantitatively evaluate the adherence to the Mediterranean diet.49 The score, which was validated in healthy Spanish children and youths, consists of 16 questions with either positive (+1) or negative (−1) connotation, with the sum identifying the Mediterranean quality among three levels (ie, low, improvements needed, optimal). For adults, the literature-based adherence score to the Mediterranean diet of Sofi and colleagues might be particularly convenient.50 The score, who was estimated from data coming from over 4 million subjects, ranges from 0 (lowest Mediterranean diet adherence) to 18 points (highest Mediterranean diet adherence), and comprises 9 quantity-based questions to be answered with the assignment of 0, 1, or 2 points each according to the higher Mediterranean connotation. Both suggested indexes can be easily used in clinical practice and they take about 5 mins each to be completed.
Practical Suggestions to Promote Healthy Eating
An adjunctive-personalized dietary advice and a nutritional counselling support, focusing on healthy eating recommendations, were found to be effective in reducing symptoms in patients with unipolar depression.51 Even small changes may be sufficient to achieve greater advantages: the addition of a specific food category, such as nuts,52 to an individual’s eating habit may be effective in the integrated treatment of depression. Moreover, the supplementation with omega-3 fatty acids, zinc, B vitamins have been often studied in neuropsychiatric populations, with debated results.53,54 Targeted probiotic supplementations could be also considered an encouraging integrative approach.55 In clinical practice, patients should be first educated to pursue an optimal quality of the diet. In some psychiatric patients, it is important to avoid restrictive and/or selective eating patterns.29 Because people have different preferences for specific foods, it is important to understand whether quantity, quality, or timing is the most beneficial intervention for them. Patients should be informed that quality and timing are surely more important than quantity, at least for weight management.56 A nutritional counseling may be more pragmatic as part of dietetic sessions to be taken with the support of written information, meal ideas, recipe examples, shopping lists, label reading instructions, and food security information.30,57 The tailored dietetic plan should eventually be designed to be easy to follow, sustainable, palatable, and satiating,51 with the eventual meal assistance support to convey motivational eating. The general aim should be to instruct patients to follow a balanced diet that contains suitable options for carbohydrates, proteins, lipids, vegetables, and fruits. Impulsive eating may be circumvented through the consumption of snacks in-between meals. Early identification of low baseline adherence to a specific diet, learned helplessness (ie, perceived absence of control to achieve any success) for previous attempts to lose body weight, fear or gain in body weight because of pharmacological therapy, or displeasure of body image should be investigated.29 Moreover, family environment affecting food habits should be always explored, especially for younger patients.28 Pathological behaviors might vitiate food habits, therefore a thoughtful assessment should be always considered.29 Neuropsychiatric patients may use dietary supplements without informing their doctor, as they may consider the use of supplements not worth of note or feel uncomfortable in admitting their choice of complementary remedies. Patients can present misperceptions about the efficacy of certain supplements, and a more scientific education should be provided for these cases.12 Dietetic sessions should include information about conditional recommendations to avoid foods or beverages known to interfere with drug pharmacokinetic/pharmacodynamic profile.29,58
Physical Activity in Neuropsychiatry
As hunters and gatherers, our ancestors trekked miles every day and had the highest activity levels59 compared both to the present day and to our past apelike existence. In fact, our ancestors initially transitioned from a sedentary simian lifestyle to a more physically demanding hunter-gatherer one, when they started carrying out foraging tasks. This evolutionary process is believed to have promoted brain development because of the combination of aerobic activity with control of motor systems, spatial navigation, memory, executive functions including decision making and planning, and control of sensory and attentional systems.60 “Until recently, all of us were athletes”.61 It is worth of note that not only the lowest level of physical activity, but also the extensively and uninterrupted sedentary behavior are risk factors for non-communicable diseases. Keeping active improves cardiopulmonary and musculoskeletal systems, which in turn ameliorate the mechanical potential of the body. The more the physical activity, the more the branching of blood capillaries and pruning of neuronal cells.62,63 Physical activity affects levels of neurotransmitters, endorphins, and neurotrophic factors, such as the brain-derived neurotrophic factor, which are implicated in body and mental functioning.64 An active lifestyle increases the antioxidant capacity and boosts the immune system (eg, myokines), thus rendering the body less vulnerable to both disease and cognitive decline. Common cellular pathways important for neurogenesis and plasticity may be synergistically promoted by physical exercise and food components.65
Nowadays, we are provided with excessive labor-saving innovations, such as cars, elevators, and escalators, which prevent us from significantly increasing our heart rate or breaking a sweat for days. “Few jobs require physical activity and most of us have little inclination to exercise in our spare time … Let’s help each other exercise more. In fact, it’s what we evolved to do”.61 Exercise is medicine.66 In the following paragraphs, we discuss and describe: I) the reciprocal relationship between physical fitness and neuropsychiatric disorders, II) existing methods to assess physical activity levels, III) practical suggestions to promote physical activity.
The Reciprocal Relationship Between Physical Fitness and Neuropsychiatric Disorders
The less a subject moves, the more he appears to be exposed to a higher risk of anxiety and depressive disorders,67,68 cognitive decline and dementia.69 Other than low physical activity, also sedentary behaviors should be reasonably avoided. Of note, different types of sedentary behaviors, such as television viewing and reading, may have a different impact on cognitive development,70 thus suggesting that a hierarchy exists among sedentary activities, with some having to be preferred over others. In terms of physical commitment, reading and watching television are comparable activities, but most likely require different degrees of cognitive and emotional commitment as was showed by previous results comparing television viewing and regular computer use.71 Indeed, screen sedentary behavior are associated, among other routinely behaviors, with greater distress.72 Normally, maintaining an active outdoor lifestyle promotes mental health and mentally active subjects are those who exercise the most,73 but this is not always true: professional athletes may suffer from brain disorders, with important performance affections, and these conditions gave birth, similarly to the nutritional psychiatry field, to sport psychiatry.74 To this extent, the positive effects of an increased physical activity on mental distress cannot be always explained by physiological factors associated with ameliorated hormonal responses or endorphin production. The bi-directional relationship between a healthy brain and physical fitness is not a new concept75,76 and many cross-sectional studies showed that people suffering from severe mental illness, such as schizophrenia, bipolar disorder, and major depressive disorder, have very low levels of physical activity in relation with longer illness duration and drug use.77 Not only the lowest physical activity levels, but even much time spent being sedentary are behavioral features of those subjects with severe neuropsychiatric disorders.78,79 Individuals who exercise the most may have a larger total brain volume, with the incremental physical activity having different effects on multiple brain regions.80 As previously mentioned, the amelioration of hemodynamic responses may be at the basis of brain modifications upon physical exercise, extraordinarily mirroring cardiovascular improvements and the acquisition of a general physical and psychological health.
Existing Methods to Assess Physical Activity Levels
What does “move enough” mean? Quality, quantity, timing, and environment are important specifiers of physical activity programs. The quality of physical activity comprises the intensity (ie, effort level) and type, which vary between people according to demographic and health status. Endurance, muscle-strengthening, stretching, and balance activities are the main type categories, and they are all dependent on the environment (eg, outdoor, indoor, at school, watersports, mountain sports). Quantity comprises the duration (length of training) and frequency (times per week), while the timing means the moment of the day. Objective assessment of the usual body activity, in terms of energy consumed, may derive from actigraphy, which is a non-invasive method for monitoring rest/activity cycles.81 To record physical activity, actigraphy devices (eg, single or multiple axis accelerometers) are usually worn on the wrist to record movements that can be used to estimate wavering parameters with the support of computerized algorithms. Subjective questionnaires may also be useful in order to obtain a different perceptive information, but they show more variability in properties of methodological effectiveness than objective measures,82 such as accelerometer/activity monitor, as the latter allows examining the motion in free-living environments.83 Reliable questionnaires are available for physical activity surveillance at the population level to collect data at work, for travelling to and from places, and for recreational activities (https://www.who.int/ncds/surveillance/steps/GPAQ/en/), but they seem to be outdated by last generation smartphones with built-in accelerometry.84 Diverse physical activity guidelines are available online (https://health.gov/paguidelines/second-edition/) with infographics that can be more suitable for the public population. To achieve at least 150 mins of moderate to vigorous physical activity a week plus muscle-strengthening activities at least 2 days a week is recommended by the physical activity guidelines for Americans,85 with similar advices from those of the World Health Organization and specific key objectives are available for preschool-aged children, adolescents, adults and older adults. However, more than 80% of adolescents is not active enough, together with 1 in 4 adults,86 and the overall picture could be worse for people suffering from mental illnesses. In clinical practice, all different neuropsychiatric patient groups can be daily monitored with wrist-mounted motion sensors, which are very useful for measuring total energy expenditure,87 thus observing the adherence to exercise programs. An actigraphy device worn on the non-dominant wrist for 2 weeks is able to give not only motor activity, but also sleep duration data in patients, with associations being reported between motor activity and mood.88 Collected data from daily monitoring are then downloaded to a computer for display and analysis of activity/inactivity that, in turn, can be further analyzed to estimate the rest-activity circadian rhythms.89
Practical Suggestions to Promote Physical Activity
Rather different physical exercise interventions had all positive clinical effects in patients with schizophrenia, unipolar depression, Alzheimer’s disease, Huntington’s disease, Parkinson’s disease, and multiple sclerosis.90 Many professionals state that the prescription of physical activity interventions should be placed on a par with drug prescription, but this implies that neuropsychiatrists “know how to prescribe, monitor, and evaluate the effectiveness of the exercise prescribed”.91 However, this is not often the case and this obstacle must be overcome by the multidisciplinary approach with the support of the exercise trainer. It is important to note that while dietary guidelines are very precise in terms of “what to eat” and “how much”, physical activity guidelines are still much generalized. Various efforts and sport type combinations may have different mental health outcomes. While there are only limited ways of healthy eating (ie, the Mediterranean pattern), for physical activity it can be assumed that no matter what you do, just do something that you are allowed and enjoy. However, patients with low compliance may be more prone to poor adherence to general advices and a tailored exercise training program might be more effective than those unsupervised, as was shown in patients suffering from obsessive-compulsive disorder92 and depression.93 Hospitalized patients are certainly more manageable, and optimal results may be achieved in a short time, as was shown after 4-month prescriptions in schizophrenic patients.94 To the extent that people have preferences for specific exercises, it is important to understand whether different combinations of specifiers could be equally beneficial for the patients, who should conceivably be able to choose their favorite sport, or whether it would be better to focus on certain forms of exercise to avoid. In fact, despite various benefits of sport participation may be attained, such as the opportunity to overcome challenges or to fulfill basic psychological needs, there is a dark side of sport, ranging from injuries to addictions.95,96 Patients with displeasure of body image or fear of gain in body weight should be carefully accompanied through mild exercise interventions, as compensatory behaviors may be present.29 As stated by the guidelines, when subjects suffering from specific conditions are not able to meet the key recommendations of guidelines, they should still be engaged in regular physical activity according to their abilities, avoiding sedentary behaviors. Contrarily to the Mediterranean pattern,44 to increase structured physical activity levels in the gym may be not affordable for high costs, but routine tips to make more movement are available (https://www.choosemyplate.gov/physical-activity-tips). To keep a daily active lifestyle, patients should make tricks to increase physical activity at home, at work, at school, in the community (eg, park the car away from the workplace, get off public transport a few stations before). Generally, little structured physical activity is much better than too much and unfocused, and sports with teammates are always preferable to individual sports.
Sleep in Neuropsychiatry
Sleeping is a neurobiological state that occupies about 30–35% of our entire lifespan (7–8 hrs/night), being an essential behavioral factor for human life that is affected by environment, technology, and our 24/7 society.97 Post-industrialized sleep hygiene is different from sleep of hominin ancestors, primarily attributed to changed sleep environment (ie, sleep site) that includes photoperiod, thermal stress, noise, sociality, and familiarity of surroundings.98 However, sleep states are conserved across diverse animal species, possibly because of their brainstem-dependence (highly conserved among vertebrates), in turn suggesting that sleep drives a common benefit to animal survival, which seems to be also related to the clearance of brain metabolites.99 As we mentioned earlier, brain activity is constant and it primarily depends on the level of arousal, with a totally different pattern around day and night cycle. During the night, sleep cycles between two distinct states: the Rapid Eye Movement (REM) sleep, which occurs with vivid dreams, and the non-REM sleep, which occurs after sleep onset, both stages being distinguished through electroencephalogram or electromyogram. An imbalance between the two sleep states represents an early symptom of various neuropsychiatric disorders, suggesting that both sleep states have important roles.100
We mention that healthy eating and physical activity are worth promoting in patients affected by neuropsychiatric conditions, but we argue sleep hygiene is the third player of this triad to be promoted in terms of good quality and quantity. The compromising neurobehavioral performance resulting from poor sleep might indeed induce neuropsychiatric symptoms in healthy subjects and worsen the condition of affected subjects, therefore deeming necessary to consider also this aspect in clinical practice. In the following paragraphs, we discuss and describe: I) the reciprocal relationship between sleep and neuropsychiatric disorders, II) existing methods to assess sleep, III) practical suggestions to promote sleep hygiene.
The Reciprocal Relationship Between Sleep and Neuropsychiatric Disorders
Sleep acts as a mediator of cognition, mood, and emotional memory101 and, therefore, poor sleep hygiene is associated with worse mental health in both adolescents and adults. In healthy youths, short weekday sleep duration was associated with increased odds of mood, anxiety, substance use, and behavioral disorders.102 Both poor sleep quantity and quality (ie, insomnia) are associated with worse mental health. For instance, short sleep durations are known to be a significant predictor of developing depression during adulthood103 and subjects with insomnia are almost 10 or 17 times more likely to develop a depressive disorder or an anxiety disorder than good sleepers.104 Sleep disorders have been intertwined with concomitant neuropsychiatric conditions105 and different sleep structures can differentiate the clinical phenotypes, for instance between bipolar disorder and attention-deficit hyperactivity disorder.106 Indeed, laboratory-based studies have demonstrated that sleep abnormalities are commonly present in affective disorders since years.107,108 However, sleep disturbances still represent a growing public health concern, affecting youths and older adults suffering from neuropsychiatric diseases. About 88% of children with anxiety disorders exhibits sleep disturbances109 and main complaints in adults suffering from Alzheimer’s disease include fragmentation of nocturnal sleep, prolonged awakenings, REM sleep abnormalities, and daytime sleepiness with frequent napping.110 Sleep may be disturbed in some patients with obsessive thoughts that prevent them from falling asleep.29 Sleep disturbances are also present in patients with bipolar disorder111 and even non-treated schizophrenic patients,112 clearly demonstrating that sleep is directly affected by the disease rather than drugs themselves. Interestingly, the clinical response to a specific drug therapy may be predicted by the cellular circadian rhythms in some patients.113 Indeed, circadian rhythm disturbances may be one of the key etiological factors for neuropsychiatric disease onset, as they are frequently present in children diagnosed with attentional or hyperactive symptoms114 and in older adults suffering from dementing disorders.115
Existing Methods to Assess Sleep
Sleep quality, quantity, timing (fractal or condensed), and environment are four features that characterize sleep hygiene. As happens for eating patterns, quality appears to be the most important, because of its comprehensive annexation with efficiency (ie, time in bed spent sleeping), latency to fall asleep, and time in bed spent awake at night (we assume to have diurnal behaviors) after first falling asleep. Sleep behavior can be studied through several objective methods, such as polysomnography and actigraphy, or subjective methods, such as the more practical sleep diaries. Polysomnography refers to the continuous monitoring of multiple neurophysiological and cardiorespiratory variables over the night course116 and specifically provides information about physiological changes occurring in relation to sleep stages and wakefulness.117 The reference for the evaluation (https://aasm.org/clinical-resources/scoring-manual/) comprehensively provides rules for scoring sleep stages, arousals, respiratory events during sleep, movements during sleep and cardiac events, but it may be of limited use for clinical routine. Of note, existing recommendations for a good sleep hygiene focus on the sole quantity factor. The hours of sleep per night should be at least eight and seven for healthy adolescents118 and adults,119 respectively. Failing to meet these recommendations is associated with poorer physical health in youths120 and adults.121 Overall, almost one third of adults in the US sleep less than 7 hrs in a 24 hr period.122 Furthermore, sleep quality seems to be far from being optimal with insomnia being one of the most prevalent health problems related to sleep. Insomnia is a chronic condition with difficulties in initiating and maintaining sleep that occurs in approximately 9–15% of the world population with daytime consequences.123,124 Dietary supplements to alleviate insomnia symptoms are used in about 15% of cases,72 potentially exposing to drug–food interactions.58,125 Despite not being the gold standard method for sleep monitoring, actigraphy can certainly represent a useful alternative and many scientific studies have been conducted with this objective method in different settings.126,127 Actigraphy devices worn on the wrist record movements that can be used to estimate total sleep time and wakes after sleep onset.128 Since decades, the American Academy of Sleep Medicine highlighted actigraphy as a valid and cost-effective method for diagnosing insomnia, circadian rhythm disorders, or excessive sleepiness.129 Other practical tools are sleep diaries and questionnaires, which quantitatively summarize the individual’s perception of sleep, and can easily be used to monitor the behavioral treatment of sleep disorders.130 Sleep questionnaires are filled in once, while sleep diaries are filled in over a period of time, thus underscoring the greater amount of information recorded by the latter. Similar to dietary or physical activity questionnaires, sleep questionnaires are influenced by different sources of bias and inaccuracy, but their subjectivity does not necessarily provide inaccurate results. Since many sleep questionnaires, scales, and diaries have been validated and proposed130 and since their primary outcome can be extremely different (eg, sleep quality or daytime sleepiness), the selection of a questionnaire should be based on the purpose of each specific study or clinical question. A recent study by Ibanez and colleagues81 created and provided a public repository where all sleep diaries and questionnaires can be downloaded (http://users.dsic.upv.es/~jsilva/Sleep/).
Practical Suggestions to Promote Sleep Hygiene
A cognitive-behavioral sleep intervention was able to ameliorate self-reported indices of sleep, daytime sleepiness, anxiety, and depression in adolescents with higher levels of anxiety and depressive symptoms.131 The treatment of sleep-wake alterations in older adults with dementing disorders may provide immediate benefits on neuropsychiatric symptoms.132 Light, as the main environmental modulator of the biological clock, is able to resynchronize the circadian system and bright-light therapy is currently proposed for the treatment of seasonal affective disorder, and in cases of non-seasonal depression, and bipolar depression.133 In clinical practice, actigraphy represents the more practical method to detect activity-rest circadian rhythms disorders in patient’s natural sleep environment.134 Nevertheless, sleep diaries and questionnaires should be always used to complement the objective evaluations. As mentioned for the dietetic sessions, sleep hygiene education may be more concrete with the support of written information. Generally, behaviors that augment physiological or mental arousal, or which delay the circadian phase, should be avoided. For instance, the consumption of methylxanthine-containing beverages, such as coffee, tea, and guarana should be avoided close to bedtime. Also, smoking should be avoided because of its insomnia-like sleep impairments,135 but also alcohol.29 Indeed, sleep may be indirectly favored by the abovementioned dietary and physical activity interventions, but patients may take prescribed or over-the-counter sleeping aids, such as melatonin.136 Neuropsychiatric patients should be educated to ensure that their sleep environment is relaxing (eg, no light or noise, comfortable bed), by also limiting the use of mobile phones and television during bedtime. Concomitantly, patients should keep an active lifestyle (regular moderate-intensity aerobic exercise),137 avoid heavy food close to bedtime,138 avoid sugar-sweetened or energy beverages,139–141 and possibly follow a tailored sleep plan or even use actionable resources, such as apps that promote sleep self-monitoring.142
Conclusion
The medical-surgical world is increasingly oriented towards drug- or surgeon-centered treatments. Obesity is treated with anti-obesity medications or bariatric surgery,143,144 insomnia with transcranial magnetic stimulation,145 and treatment-resistant conditions with neurosurgical implants.146 It seems that multiple benefits deriving from healthy diet, physical activity, and restful sleep have been progressively forgotten. The impending global pandemics of obesity and sleep disturbances are not effectively controlled by lifestyle interventions because the integration in clinical practice has never been systematic. Neuropsychiatric patients were often reported to have unhealthy dietary habits,27,34,147,148 sedentary behaviors,77–79 and poor sleep hygiene.109–112 Even if some neuropsychiatric conditions can directly or indirectly affect eating behaviors,29 in terms of direction of causality, a poor diet has remarkably been shown to precede the onset of mental illnesses,149 with similar time dependence for both sedentary lifestyles and poor sleep.150,151 Our suggestions, proposed in Table 1, may be applied to the general neuropsychiatric population, with no regard for age, gender, or ethnicity. Public and private clinics, university hospitals, and research facilities are encouraged to integrate HEPAS, in order to pursue better course and outcome compared to related standard of care.
Table 1.
Considerations for Clinical Practice Regarding Single Determinants of Healthy Eating, Physical Activity, and Sleep Hygiene (HEPAS) in Patients at Risk for or with Neuropsychiatric Disorders
| Healthy eating in neuropsychiatry practice |
|
|
|
|
|
|
|
|
|
|
|
| Physical activity in neuropsychiatry practice |
|
|
|
|
|
|
| Sleep hygiene in neuropsychiatry practice |
|
|
|
|
|
|
|
Disadvantages, Barriers, Advantages
In Neuropsychiatry, routine screening of eating behaviors, physical activity levels, and sleep patterns are not always accurate, mostly due to packed schedules or growing caseloads that prevent proper multidisciplinary interactions between neuropsychiatrists, nutritionists, and exercise trainers. HEPAS applicability may also be limited according to patient’s severity/stage of disease and resource availability (eg, financial burden, lack of specialized personnel). Moreover, all three factors are quite onerous to monitor (weak point = low compliance) and patients are not often informed enough, hyperinformed (which may be probably worse), uneducated, and socially unengaged.152,153 However, HEPAS epitomizes the novel approach that accounts for modifiable factors not only to ameliorate the grueling years lived with disability after diagnosis through tertiary preventive interventions, but also to avoid complications of clinical spectrum or to reduce disease onset through primary preventive interventions. HEPAS may certainly account for other non-communicable disease associated with the longest years lived with disability, such as musculoskeletal disorders (ie, osteosarcopenia in older adults with mild cognitive impairment), diabetes, kidney and cardiovascular diseases that are often comorbid with neuropsychiatric disorders.154,155 Single HEPAS components were reported to provide various advantages also in neuropsychiatric populations, but no study ever investigated all of the three components.
Past Evidences
HEPAS determinants are exceedingly intertwined, so that one cannot be dissociated from another. The combination of healthy eating and right amount of physical activity was observed to have multiplicative effects on mortality risk reduction.156 The worse a subject eat the less active he is, and that was confirmed for both children and adults.157,158 Moreover, youths who sleep little may be more prone to fast food consumption and vegetable or fruit avoidance,140 with late sleep timing being associated with increased consumption of energy drinks, sugar-sweetened beverages, and breakfast skipping.139 These associations may be due to changes in appetite regulatory hormones that subsequently contribute to overeating and obesity.159,160 Conversely, eating habits can influence sleep through gut microbiota modulation.161 Staying active is clearly better because it ameliorates sleep quality162 and mood163 not only in youths, but also in adults and elderly in turn providing a more resting sleep.164 Regular physical activity has also positive effects on sleep quantity,165 and the amelioration of sleep habits is in turn associated with a general risk reduction for obesity, heart diseases, and diabetes,166 which are conditions often being counted among the long-term metabolic side effects of neuropsychiatric drugs. Previously, some authors already acknowledged this concept of reciprocity among apparently disconnected domains, and advocated interventions targeting multiple factors simultaneously rather than focusing on single components. Similarly to HEPAS, a past multidomain lifestyle-based intervention provided ample evidence about of the importance of coupling nutritional advices, exercise, and mental training for cognitive decline prevention.167 In the same field, other trials targeted disease onset reduction through support in chronic disease management, smoking cessation, and health coaching.168
Future Directions
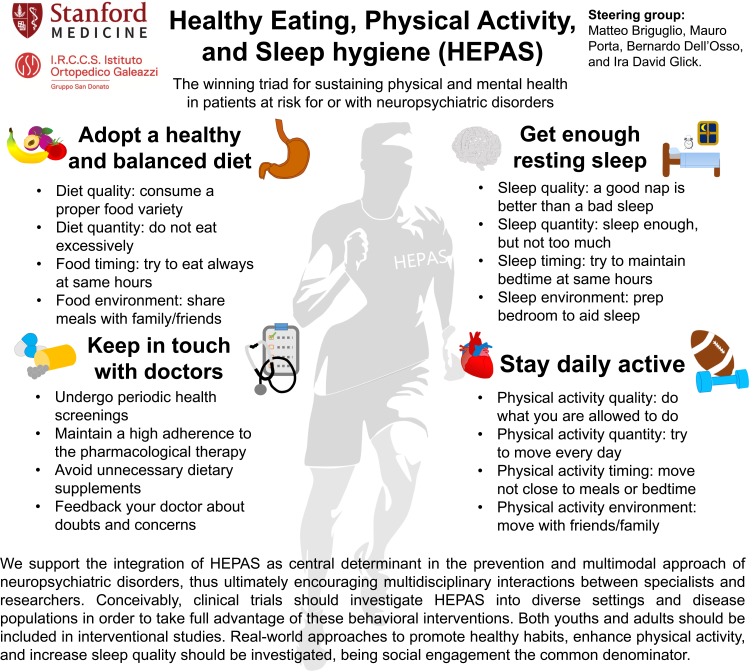
We support the integration of HEPAS as central determinant in the prevention and multimodal approach of neuropsychiatric disorders, thus ultimately encouraging multidisciplinary interactions between specialists and researchers. Conceivably, high quality and adequately powered clinical trials should investigate HEPAS into diverse settings and disease populations in order to take full advantage of these behavioral interventions. In particular, there is the need of prospective experimental studies with an appropriate research methodology to legitimately support the beneficial effects of dietary,169 exercise,170 and sleep programs as primary or secondary prevention initiatives. Both youths and adults should be included in interventional studies, being the research on adolescent populations even more important because of the negative trend towards adulthood for healthy eating,171 physical activity,172 and sleep.173 Real-world approaches to promote healthy habits, increase sleep time, and enhance physical activity should be investigated, being social engagement the common denominator. Patients should be ultimately confident, motivated, and enabled to sustain long-term health outcomes. Infographic of Figure 1 comprehensively summarizes our considerations for clinical practice, also comprising advices on a proper therapeutic alliance. Importantly, caregivers and family members should always be involved in this multimodal approach to practically and psychologically support the individual. If necessary, psychotherapists and life coaches may be involved to enhance compliance and community-based engagement.152 We know all positive effects of abovementioned HEPAS interventions, but for instance, how does an individual eat better, sleep better, and do exercise? Since each component can provide various advantages per se, the possibility of combined use of all three interventions unlocks numerous potential avenues, facilitating a comprehensive management of neuropsychiatric disorders in affected patients.
Figure 1.
Scholarly infographic depicting the Healthy Eating, Physical Activity, and Sleep hygiene (HEPAS) in patients at risk for or with neuropsychiatric disorders.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
Professor Ira Glick reports research support from Alkermes, speaker's bureau from Sunovion, consultant from Neurocrine, equity fromJohnson & Johnson, outside the submitted work.This study was part of the Italian project “Ricerca Corrente del Ministero Della Salute”. The authors report no other conflicts of interest in this work.
References
- 1.Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry. 2016;3(2):171–178. doi: 10.1016/S2215-0366(15)00505-2 [DOI] [PubMed] [Google Scholar]
- 2.Disease GBD, Injury I, Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392(10159):1789–1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Poyurovsky M, Zohar J, Glick I, et al. Obsessive-compulsive symptoms in schizophrenia: implications for future psychiatric classifications. Compr Psychiatry. 2012;53(5):480–483. doi: 10.1016/j.comppsych.2011.08.009 [DOI] [PubMed] [Google Scholar]
- 4.Dell’Osso B, Marazziti D, Albert U, et al. Parsing the phenotype of obsessive-compulsive tic disorder (OCTD): a multidisciplinary consensus. Int J Psychiatry Clin Pract. 2017;21:1–4. [DOI] [PubMed] [Google Scholar]
- 5.Malhi GS, Loo C, Cahill CM, Lagopoulos J, Mitchell P, Sachdev P. “Getting physical”: the management of neuropsychiatric disorders using novel physical treatments. Neuropsychiatr Dis Treat. 2006;2(2):165–179. doi: 10.2147/nedt.2006.2.issue-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rusterholz T, Hamann C, Markovic A, Schmidt SJ, Achermann P, Tarokh L. Nature and nurture: brain region-specific inheritance of sleep neurophysiology in adolescence. J Neurosci. 2018;38(43):9275–9285. doi: 10.1523/JNEUROSCI.0945-18.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ruddock HK, Dickson JM, Field M, Hardman CA. Eating to live or living to eat? Exploring the causal attributions of self-perceived food addiction. Appetite. 2015;95:262–268. doi: 10.1016/j.appet.2015.07.018 [DOI] [PubMed] [Google Scholar]
- 8.Mattson MP, Allison DB, Fontana L, et al. Meal frequency and timing in health and disease. Proc Natl Acad Sci U S A. 2014;111(47):16647–16653. doi: 10.1073/pnas.1413965111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bradt S Invention of cooking drove evolution of the human species, new book argues. 2009. Available from: https://news.harvard.edu/gazette/story/2009/06/invention-of-cooking-drove-evolution-of-the-human-species-new-book-argues/. Accessed December12, 2019.
- 10.Gomez-Pinilla F, Tyagi E. Diet and cognition: interplay between cell metabolism and neuronal plasticity. Curr Opin Clin Nutr Metab Care. 2013;16(6):726–733. doi: 10.1097/MCO.0b013e328365aae3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harrison NL, Skelly MJ, Grosserode EK, et al. Effects of acute alcohol on excitability in the CNS. Neuropharmacology. 2017;122:36–45. doi: 10.1016/j.neuropharm.2017.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Briguglio M, Dell’Osso B, Panzica G, et al. Dietary neurotransmitters: a narrative review on current knowledge. Nutrients. 2018;10(5):591. doi: 10.3390/nu10050591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Knobloch M, Jessberger S. Metabolism and neurogenesis. Curr Opin Neurobiol. 2017;42:45–52. doi: 10.1016/j.conb.2016.11.006 [DOI] [PubMed] [Google Scholar]
- 14.Cusick SE, Georgieff MK. The role of nutrition in brain development: the golden opportunity of the “first 1000 days”. J Pediatr. 2016;175:16–21. doi: 10.1016/j.jpeds.2016.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spence C, Okajima K, Cheok AD, Petit O, Michel C. Eating with our eyes: from visual hunger to digital satiation. Brain Cogn. 2016;110:53–63. doi: 10.1016/j.bandc.2015.08.006 [DOI] [PubMed] [Google Scholar]
- 16.Carito V, Ceccanti M, Tarani L, Ferraguti G, Chaldakov GN, Fiore M. Neurotrophins’ modulation by olive polyphenols. Curr Med Chem. 2016;23(28):3189–3197. doi: 10.2174/0929867323666160627104022 [DOI] [PubMed] [Google Scholar]
- 17.Neshatdoust S, Saunders C, Castle SM, et al. High-flavonoid intake induces cognitive improvements linked to changes in serum brain-derived neurotrophic factor: two randomised, controlled trials. Nutr Healthy Aging. 2016;4(1):81–93. doi: 10.3233/NHA-1615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gomez-Pinilla F. Brain foods: the effects of nutrients on brain function. Nat Rev Neurosci. 2008;9(7):568–578. doi: 10.1038/nrn2421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Enteshari Najafabadi R, Kazemipour N, Esmaeili A, Beheshti S, Nazifi S. Using superparamagnetic iron oxide nanoparticles to enhance bioavailability of quercetin in the intact rat brain. BMC Pharmacol Toxicol. 2018;19(1):59. doi: 10.1186/s40360-018-0249-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mozaffarian D, Mande J, Micha R. Food is medicine-the promise and challenges of integrating food and nutrition into health care. JAMA Intern Med. 2019;179(6):793–795. doi: 10.1001/jamainternmed.2019.0184 [DOI] [PubMed] [Google Scholar]
- 21.O’Neil A, Quirk SE, Housden S, et al. Relationship between diet and mental health in children and adolescents: a systematic review. Am J Public Health. 2014;104(10):e31–e42. doi: 10.2105/AJPH.2014.302110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Salari-Moghaddam A, Saneei P, Larijani B, Esmaillzadeh A. Glycemic index, glycemic load, and depression: a systematic review and meta-analysis. Eur J Clin Nutr. 2019;73(3):356–365. doi: 10.1038/s41430-018-0258-z [DOI] [PubMed] [Google Scholar]
- 23.Pistollato F, Iglesias RC, Ruiz R, et al. Nutritional patterns associated with the maintenance of neurocognitive functions and the risk of dementia and alzheimer’s disease: a focus on human studies. Pharmacol Res. 2018;131:32–43. doi: 10.1016/j.phrs.2018.03.012 [DOI] [PubMed] [Google Scholar]
- 24.Psaltopoulou T, Sergentanis TN, Panagiotakos DB, Sergentanis IN, Kosti R, Scarmeas N. Mediterranean diet, stroke, cognitive impairment, and depression: a meta-analysis. Ann Neurol. 2013;74(4):580–591. doi: 10.1002/ana.v74.4 [DOI] [PubMed] [Google Scholar]
- 25.Sarris J, Logan AC, Akbaraly TN, et al. Nutritional medicine as mainstream in psychiatry. Lancet Psychiatry. 2015;2(3):271–274. doi: 10.1016/S2215-0366(14)00051-0 [DOI] [PubMed] [Google Scholar]
- 26.Marx W, Moseley G, Berk M, Jacka F. Nutritional psychiatry: the present state of the evidence. Proc Nutr Soc. 2017;76(4):427–436. doi: 10.1017/S0029665117002026 [DOI] [PubMed] [Google Scholar]
- 27.McCreadie RG; Scottish Schizophrenia Lifestyle G. Diet, smoking and cardiovascular risk in people with schizophrenia: descriptive study. Br J Psychiatry. 2003;183:534–539. doi: 10.1192/bjp.183.6.534 [DOI] [PubMed] [Google Scholar]
- 28.Briguglio M, Zanaboni Dina C, Servello D, Porta M Tourette syndrome and nutritional implications. 9° meeting of european society for the study of tourette syndrome. COST International Conference for Tourette Syndrome; 2016; Warsaw. [Google Scholar]
- 29.Briguglio M, Dell’Osso B, Galentino R, Zanaboni Dina C, Banfi G, Porta M. Tics and obsessive-compulsive disorder in relation to diet: two case reports. Encephale. 2018. Nov ;44(5):479–481. doi: 10.1016/j.encep.2017.06.004. [DOI] [PubMed] [Google Scholar]
- 30.Briguglio M, Dell’Osso B, Galentino R, Banfi G, Porta M. Higher adherence to the mediterranean diet is associated with reduced tics and obsessive-compulsive symptoms: a series of nine boys with obsessive-compulsive tic disorder. Nutr Clin Metab. 2019;33(3):227–230. doi: 10.1016/j.nupar.2019.04.004 [DOI] [Google Scholar]
- 31.Vitale JA, Briguglio M, Galentino R, et al. Exploring circannual rhythms and chronotype effect in patients with Obsessive-Compulsive Tic Disorder (OCTD): a pilot study. J Affect Disord. 2020. Feb 1;262:286–292. doi: 10.1016/j.jad.2019.11.040. [DOI] [PubMed] [Google Scholar]
- 32.Jacka FN, Pasco JA, Mykletun A, et al. Association of Western and traditional diets with depression and anxiety in women. Am J Psychiatry. 2010;167(3):305–311. doi: 10.1176/appi.ajp.2009.09060881 [DOI] [PubMed] [Google Scholar]
- 33.Lojko D, Stelmach-Mardas M, Suwalska A. Diet quality and eating patterns in euthymic bipolar patients. Eur Rev Med Pharmacol Sci. 2019;23(3):1221–1238. doi: 10.26355/eurrev_201902_17016 [DOI] [PubMed] [Google Scholar]
- 34.Gibson-Smith D, Bot M, Brouwer IA, Visser M, Penninx B. Diet quality in persons with and without depressive and anxiety disorders. J Psychiatr Res. 2018;106:1–7. doi: 10.1016/j.jpsychires.2018.09.006 [DOI] [PubMed] [Google Scholar]
- 35.Domecq JP, Prutsky G, Leppin A, et al. Clinical review: drugs commonly associated with weight change: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2015;100(2):363–370. doi: 10.1210/jc.2014-3421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Akbaraly T, Sexton C, Zsoldos E, et al. Association of long-term diet quality with hippocampal volume: longitudinal cohort study. Am J Med. 2018;131(11):1372–1381 e1374. doi: 10.1016/j.amjmed.2018.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jacka FN, Cherbuin N, Anstey KJ, Sachdev P, Butterworth P. Western diet is associated with a smaller hippocampus: a longitudinal investigation. BMC Med. 2015;13:215. doi: 10.1186/s12916-015-0461-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pardeshi R, Bolshette N, Gadhave K, et al. Insulin signaling: an opportunistic target to minify the risk of alzheimer’s disease. Psychoneuroendocrinology. 2017;83:159–171. doi: 10.1016/j.psyneuen.2017.05.004 [DOI] [PubMed] [Google Scholar]
- 39.Munoz-Garcia MI, Martinez-Gonzalez MA, Martin-Moreno JM, et al. Sugar-sweetened and artificially-sweetened beverages and changes in cognitive function in the SUN project. Nutr Neurosci. 2019. 1–9. doi: 10.1080/1028415X.2019.1580919 [DOI] [PubMed] [Google Scholar]
- 40.Taylor AM, Thompson SV, Edwards CG, Musaad SMA, Khan NA, Holscher HD. Associations among diet, the gastrointestinal microbiota, and negative emotional states in adults. Nutr Neurosci. 2019;1–10. doi: 10.1080/1028415X.2019.1582578 [DOI] [PubMed] [Google Scholar]
- 41.Valles-Colomer M, Falony G, Darzi Y, et al. The neuroactive potential of the human gut microbiota in quality of life and depression. Nat Microbiol. 2019;4:623–632. doi: 10.1038/s41564-018-0337-x [DOI] [PubMed] [Google Scholar]
- 42.Fuller NR, Fong M, Gerofi J, et al. Comparison of an electronic versus traditional food diary for assessing dietary intake-A validation study. Obes Res Clin Pract. 2017;11(6):647–654. doi: 10.1016/j.orcp.2017.04.001 [DOI] [PubMed] [Google Scholar]
- 43.DeSalvo KB, Olson R, Casavale KO. Dietary guidelines for Americans. JAMA. 2016;315(5):457–458. doi: 10.1001/jama.2015.18396 [DOI] [PubMed] [Google Scholar]
- 44.Jetter KM, Adkins J, Cortez S, Hopper GK Jr, Shively V, Styne DM. Yes we can: eating healthy on a limited budget. J Nutr Educ Behav. 2019;51(3):268–276. doi: 10.1016/j.jneb.2018.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fresan U, Sabate J, Martinez-Gonzalez MA, Segovia-Siapco G, de la Fuente-arrillaga C, Bes-Rastrollo M. Adherence to the 2015 Dietary guidelines for Americans and mortality risk in a mediterranean cohort: the SUN project. Prev Med. 2019;118:317–324. doi: 10.1016/j.ypmed.2018.11.015 [DOI] [PubMed] [Google Scholar]
- 46.Jessri M, Lou WY, L’Abbe MR. The 2015 dietary guidelines for Americans is associated with a more nutrient-dense diet and a lower risk of obesity. Am J Clin Nutr. 2016;104(5):1378–1392. doi: 10.3945/ajcn.116.132647 [DOI] [PubMed] [Google Scholar]
- 47.US Department of Health and Human Services and US Department of Agriculture. Shifts needed to align with healthy eating patterns - a closer look at current intakes and recommended shifts. 2015. Available from: https://health.gov/dietaryguidelines/2015/guidelines/chapter-2/a-closer-look-at-current-intakes-and-recommended-shifts/#a-closer-look-at-current-intakes-and-recommended-shifts, https://health.gov/dietaryguidelines/2015/guidelines/chapter-2/current-eating-patterns-in-the-united-states/.
- 48.Christoph MJ, Larson NI, Winkler MR, Wall MM, Neumark-Sztainer D. Longitudinal trajectories and prevalence of meeting dietary guidelines during the transition from adolescence to young adulthood. Am J Clin Nutr. 2019;109(3):656–664. doi: 10.1093/ajcn/nqy333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Serra-Majem L, Ribas L, Ngo J, et al. Food, youth and the mediterranean diet in Spain. Development of KIDMED, mediterranean diet quality index in children and adolescents. Public Health Nutr. 2004;7(7):931–935. doi: 10.1079/PHN2004556 [DOI] [PubMed] [Google Scholar]
- 50.Sofi F, Macchi C, Abbate R, Gensini GF, Casini A. Mediterranean diet and health status: an updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr. 2014;17(12):2769–2782. doi: 10.1017/S1368980013003169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jacka FN, O’Neil A, Opie R, et al. A randomised controlled trial of dietary improvement for adults with major depression (the ‘SMILES’ trial). BMC Med. 2017;15(1):23. doi: 10.1186/s12916-017-0791-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sanchez-Villegas A, Martinez-Gonzalez MA, Estruch R, et al. Mediterranean dietary pattern and depression: the PREDIMED randomized trial. BMC Med. 2013;11:208. doi: 10.1186/1741-7015-11-208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Deacon G, Kettle C, Hayes D, Dennis C, Tucci J. Omega 3 polyunsaturated fatty acids and the treatment of depression. Crit Rev Food Sci Nutr. 2017;57(1):212–223. doi: 10.1080/10408398.2013.876959 [DOI] [PubMed] [Google Scholar]
- 54.Yatham LN, Kennedy SH, Parikh SV, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) 2018 guidelines for the management of patients with bipolar disorder. Bipolar Disord. 2018;20(2):97–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Slykerman RF, Hood F, Wickens K, et al. Effect of lactobacillus rhamnosus HN001 in pregnancy on postpartum symptoms of depression and anxiety: a randomised double-blind placebo-controlled trial. EBioMedicine. 2017;24:159–165. doi: 10.1016/j.ebiom.2017.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gardner CD, Trepanowski JF, Del Gobbo LC, et al. Effect of low-fat vs low-carbohydrate diet on 12-month weight loss in overweight adults and the association with genotype pattern or insulin secretion: the DIETFITS randomized clinical trial. JAMA. 2018;319(7):667–679. doi: 10.1001/jama.2018.0245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.O’Neil A, Berk M, Itsiopoulos C, et al. A randomised, controlled trial of a dietary intervention for adults with major depression (the “SMILES” trial): study protocol. BMC Psychiatry. 2013;13:114. doi: 10.1186/1471-244X-13-114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Briguglio M, Hrelia S, Malaguti M, et al. Food bioactive compounds and their interference in drug pharmacokinetic/pharmacodynamic profiles. Pharmaceutics. 2018;10(4):277. doi: 10.3390/pharmaceutics10040277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pontzer H, Wood BM, Raichlen DA. Hunter-gatherers as models in public health. Obes Rev. 2018;19(Suppl 1):24–35. doi: 10.1111/obr.v19.S1 [DOI] [PubMed] [Google Scholar]
- 60.Raichlen DA, Alexander GE. Adaptive capacity: an evolutionary neuroscience model linking exercise, cognition, and brain health. Trends Neurosci. 2017;40(7):408–421. doi: 10.1016/j.tins.2017.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lieberman D, Baggish A Exercise: it’s what we evolved to do. 2013. Available from: https://edition.cnn.com/2013/11/01/health/evolution-exercise/index.html. Accessed December12, 2019.
- 62.Vecchio F, Babiloni C, Lizio R, et al. Resting state cortical EEG rhythms in alzheimer’s disease: toward EEG markers for clinical applications: a review. Suppl Clin Neurophysiol. 2013;62:223–236. [DOI] [PubMed] [Google Scholar]
- 63.Hillman CH, Buck SM, Themanson JR, Pontifex MB, Castelli DM. Aerobic fitness and cognitive development: event-related brain potential and task performance indices of executive control in preadolescent children. Dev Psychol. 2009;45(1):114–129. doi: 10.1037/a0014437 [DOI] [PubMed] [Google Scholar]
- 64.Lin TW, Kuo YM. Exercise benefits brain function: the monoamine connection. Brain Sci. 2013;3(1):39–53. doi: 10.3390/brainsci3010039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.van Praag H. Exercise and the brain: something to chew on. Trends Neurosci. 2009;32(5):283–290. doi: 10.1016/j.tins.2008.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.American College of Sports Medicine (ACSM). Exercise is medicine. Exercise is medicine®: a global health initiative. 2019. Available from: https://www.exerciseismedicine.org/. Accessed December12, 2019.
- 67.Schuch FB, Stubbs B, Meyer J, et al. Physical activity protects from incident anxiety: a meta-analysis of prospective cohort studies. Depress Anxiety. 2019. doi: 10.1002/da.22915 [DOI] [PubMed] [Google Scholar]
- 68.Schuch FB, Vancampfort D, Firth J, et al. Physical activity and incident depression: a meta-analysis of prospective cohort studies. Am J Psychiatry. 2018;175(7):631–648. doi: 10.1176/appi.ajp.2018.17111194 [DOI] [PubMed] [Google Scholar]
- 69.Blondell SJ, Hammersley-Mather R, Veerman JL. Does physical activity prevent cognitive decline and dementia?: A systematic review and meta-analysis of longitudinal studies. BMC Public Health. 2014;14:510. doi: 10.1186/1471-2458-14-510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Carson V, Kuzik N, Hunter S, et al. Systematic review of sedentary behavior and cognitive development in early childhood. Prev Med. 2015;78:115–122. doi: 10.1016/j.ypmed.2015.07.016 [DOI] [PubMed] [Google Scholar]
- 71.Kesse-Guyot E, Charreire H, Andreeva VA, et al. Cross-sectional and longitudinal associations of different sedentary behaviors with cognitive performance in older adults. PLoS One. 2012;7(10):e47831. doi: 10.1371/journal.pone.0047831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Morin CM, LeBlanc M, Daley M, Gregoire JP, Merette C. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med. 2006;7(2):123–130. doi: 10.1016/j.sleep.2005.08.008 [DOI] [PubMed] [Google Scholar]
- 73.Elbe AM, Lyhne SN, Madsen EE, Krustrup P. Is regular physical activity a key to mental health? Commentary on “association between physical exercise and mental health in 1.2 million individuals in the USA between 2011 and 2015: A cross-sectional study”, by Chekroud et al., published in lancet psychiatry. J Sport Health Sci. 2019;8(1):6–7. doi: 10.1016/j.jshs.2018.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Glick ID, Castaldelli-Maia JM. Sport psychiatry 2016: brain, mind, and medical-psychiatric care. Int Rev Psychiatry. 2016;28(6):545–546. doi: 10.1080/09540261.2016.1218148 [DOI] [PubMed] [Google Scholar]
- 75.Loprinzi PD, Herod SM, Cardinal BJ, Noakes TD. Physical activity and the brain: a review of this dynamic, bi-directional relationship. Brain Res. 2013;1539:95–104. doi: 10.1016/j.brainres.2013.10.004 [DOI] [PubMed] [Google Scholar]
- 76.Steinmo S, Hagger-Johnson G, Shahab L. Bidirectional association between mental health and physical activity in older adults: whitehall II prospective cohort study. Prev Med. 2014;66:74–79. doi: 10.1016/j.ypmed.2014.06.005 [DOI] [PubMed] [Google Scholar]
- 77.Vancampfort D, Firth J, Schuch FB, et al. Sedentary behavior and physical activity levels in people with schizophrenia, bipolar disorder and major depressive disorder: a global systematic review and meta-analysis. World Psychiatry. 2017;16(3):308–315. doi: 10.1002/wps.v16.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Stubbs B, Williams J, Gaughran F, Craig T. How sedentary are people with psychosis? A systematic review and meta-analysis. Schizophr Res. 2016;171(1–3):103–109. doi: 10.1016/j.schres.2016.01.034 [DOI] [PubMed] [Google Scholar]
- 79.Scheewe TW, Jorg F, Takken T, et al. Low physical activity and cardiorespiratory fitness in people with schizophrenia: a comparison with matched healthy controls and associations with mental and physical health. Front Psychiatry. 2019;10:87. doi: 10.3389/fpsyt.2019.00087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Spartano NL, Davis-Plourde KL, Himali JJ, et al. Association of accelerometer-measured light-intensity physical activity with brain volume: the framingham heart study. JAMA Netw Open. 2019;2(4):e192745. doi: 10.1001/jamanetworkopen.2019.2745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ibanez V, Silva J, Cauli O. A survey on sleep assessment methods. PeerJ. 2018;6:e4849. doi: 10.7717/peerj.4849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Prince SA, Adamo KB, Hamel ME, Hardt J, Connor Gorber S, Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Act. 2008;5:56. doi: 10.1186/1479-5868-5-56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Dowd KP, Szeklicki R, Minetto MA, et al. A systematic literature review of reviews on techniques for physical activity measurement in adults: a DEDIPAC study. Int J Behav Nutr Phys Act. 2018;15(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Althoff T, Sosic R, Hicks JL, King AC, Delp SL, Leskovec J. Large-scale physical activity data reveal worldwide activity inequality. Nature. 2017;547(7663):336–339. doi: 10.1038/nature23018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Services UDoHaH. Physical Activity Guidelines for Americans. 2nd Washington, DC; 2018. [Google Scholar]
- 86.(WHO) WHO. Key facts: physical activity. 23 February 2018. Accessed 1August, 2019.
- 87.Kinnunen H, Hakkinen K, Schumann M, Karavirta L, Westerterp KR, Kyrolainen H. Training-induced changes in daily energy expenditure: methodological evaluation using wrist-worn accelerometer, heart rate monitor, and doubly labeled water technique. PLoS One. 2019;14(7):e0219563. doi: 10.1371/journal.pone.0219563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Merikangas KR, Swendsen J, Hickie IB, et al. Real-time mobile monitoring of the dynamic associations among motor activity, energy, mood, and sleep in adults with bipolar disorder. JAMA Psychiatry. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ancoli-Israel S, Cole R, Alessi C, Chambers M, Moorcroft W, Pollak CP. The role of actigraphy in the study of sleep and circadian rhythms. Sleep. 2003;26(3):342–392. doi: 10.1093/sleep/26.3.342 [DOI] [PubMed] [Google Scholar]
- 90.Dauwan M, Begemann MJH, Slot MIE, Lee EHM, Scheltens P, Sommer IEC. Physical exercise improves quality of life, depressive symptoms, and cognition across chronic brain disorders: a transdiagnostic systematic review and meta-analysis of randomized controlled trials. J Neurol. 2019. doi: 10.1007/s00415-019-09493-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.de Souto Barreto P. Prescription of physical activity. Lancet. 2013;381(9878):1623. doi: 10.1016/S0140-6736(13)61019-3 [DOI] [PubMed] [Google Scholar]
- 92.Abrantes AM, Farris SG, Brown RA, et al. Acute effects of aerobic exercise on negative affect and obsessions and compulsions in individuals with obsessive-compulsive disorder. J Affect Disord. 2019;245:991–997. doi: 10.1016/j.jad.2018.11.074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hallgren M, Kraepelien M, Ojehagen A, et al. Physical exercise and internet-based cognitive-behavioural therapy in the treatment of depression: randomised controlled trial. Br J Psychiatry. 2015;207(3):227–234. doi: 10.1192/bjp.bp.114.160101 [DOI] [PubMed] [Google Scholar]
- 94.Curcic D, Stojmenovic T, Djukic-Dejanovic S, et al. Positive impact of prescribed physical activity on symptoms of schizophrenia: randomized clinical trial. Psychiatr Danub. 2017;29(4):459–465. doi: 10.24869/psyd.2017.459 [DOI] [PubMed] [Google Scholar]
- 95.Immonen T, Brymer E, Davids K, Liukkonen J, Jaakkola T. An ecological conceptualization of extreme sports. Front Psychol. 2018;9:1274. doi: 10.3389/fpsyg.2018.01274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Di Lodovico L, Poulnais S, Gorwood P. Which sports are more at risk of physical exercise addiction: a systematic review. Addict Behav. 2019;93:257–262. doi: 10.1016/j.addbeh.2018.12.030 [DOI] [PubMed] [Google Scholar]
- 97.Grandner MA. Sleep, health, and society. Sleep Med Clin. 2017;12(1):1–22. doi: 10.1016/j.jsmc.2016.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Samson DR, Crittenden AN, Mabulla IA, Mabulla AZP. The evolution of human sleep: technological and cultural innovation associated with sleep-wake regulation among hadza hunter-gatherers. J Hum Evol. 2017;113:91–102. doi: 10.1016/j.jhevol.2017.08.005 [DOI] [PubMed] [Google Scholar]
- 99.Sun BL, Wang LH, Yang T, et al. Lymphatic drainage system of the brain: a novel target for intervention of neurological diseases. Prog Neurobiol. 2018;163–164:118–143. doi: 10.1016/j.pneurobio.2017.08.007 [DOI] [PubMed] [Google Scholar]
- 100.Miyazaki S, Liu CY, Hayashi Y. Sleep in vertebrate and invertebrate animals, and insights into the function and evolution of sleep. Neurosci Res. 2017;118:3–12. doi: 10.1016/j.neures.2017.04.017 [DOI] [PubMed] [Google Scholar]
- 101.Navarro-Sanchis C, Brock O, Winsky-Sommerer R, Thuret S. Modulation of adult hippocampal neurogenesis by sleep: impact on mental health. Front Neural Circuits. 2017;11:74. doi: 10.3389/fncir.2017.00074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Zhang J, Paksarian D, Lamers F, Hickie IB, He J, Merikangas KR. Sleep patterns and mental health correlates in US adolescents. J Pediatr. 2017;182:137–143. doi: 10.1016/j.jpeds.2016.11.007 [DOI] [PubMed] [Google Scholar]
- 103.Zhai L, Zhang H, Zhang D. Sleep duration and depression among adults: a meta-analysis of prospective studies. Depress Anxiety. 2015;32(9):664–670. doi: 10.1002/da.2015.32.issue-9 [DOI] [PubMed] [Google Scholar]
- 104.Taylor DJ, Lichstein KL, Durrence HH, Reidel BW, Bush AJ. Epidemiology of insomnia, depression, and anxiety. Sleep. 2005;28(11):1457–1464. doi: 10.1093/sleep/28.11.1457 [DOI] [PubMed] [Google Scholar]
- 105.Winokur A. The relationship between sleep disturbances and psychiatric disorders: introduction and overview. Psychiatr Clin North Am. 2015;38(4):603–614. doi: 10.1016/j.psc.2015.07.001 [DOI] [PubMed] [Google Scholar]
- 106.Estrada-Prat X, Alvarez-Guerrico I, Batlle-Vila S, et al. Sleep alterations in pediatric bipolar disorder versus attention deficit disorder. Psychiatry Res. 2019;275:39–45. doi: 10.1016/j.psychres.2019.01.108 [DOI] [PubMed] [Google Scholar]
- 107.Reynolds CF 3rd, Kupfer DJ. Sleep research in affective illness: state of the art circa 1987. Sleep. 1987;10(3):199–215. doi: 10.1093/sleep/10.3.199 [DOI] [PubMed] [Google Scholar]
- 108.Emslie GJ, Armitage R, Weinberg WA, Rush AJ, Mayes TL, Hoffmann RF. Sleep polysomnography as a predictor of recurrence in children and adolescents with major depressive disorder. Int J Neuropsychopharmacol. 2001;4(2):159–168. doi: 10.1017/S1461145701002383 [DOI] [PubMed] [Google Scholar]
- 109.Steinsbekk S, Berg-Nielsen TS, Wichstrom L. Sleep disorders in preschoolers: prevalence and comorbidity with psychiatric symptoms. J Dev Behav Pediatr. 2013;34(9):633–641. doi: 10.1097/01.DBP.0000437636.33306.49 [DOI] [PubMed] [Google Scholar]
- 110.McCurry SM, Reynolds CF, Ancoli-Israel S, Teri L, Vitiello MV. Treatment of sleep disturbance in alzheimer’s disease. Sleep Med Rev. 2000;4(6):603–628. doi: 10.1053/smrv.2000.0127 [DOI] [PubMed] [Google Scholar]
- 111.Harvey AG, Talbot LS, Gershon A. Sleep disturbance in bipolar disorder across the lifespan. Clin Psychol (New York). 2009;16(2):256–277. doi: 10.1111/j.1468-2850.2009.01164.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Monti JM, Monti D. Sleep disturbance in schizophrenia. Int Rev Psychiatry. 2005;17(4):247–253. doi: 10.1080/09540260500104516 [DOI] [PubMed] [Google Scholar]
- 113.McCarthy MJ, Wei H, Nievergelt CM, et al. Chronotype and cellular circadian rhythms predict the clinical response to lithium maintenance treatment in patients with bipolar disorder. Neuropsychopharmacology. 2019;44(3):620–628. doi: 10.1038/s41386-018-0273-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Silvestri R, Gagliano A, Arico I, et al. Sleep disorders in children with Attention-Deficit/Hyperactivity Disorder (ADHD) recorded overnight by video-polysomnography. Sleep Med. 2009;10(10):1132–1138. doi: 10.1016/j.sleep.2009.04.003 [DOI] [PubMed] [Google Scholar]
- 115.Vitiello MV, Borson S. Sleep disturbances in patients with alzheimer’s disease: epidemiology, pathophysiology and treatment. CNS Drugs. 2001;15(10):777–796. doi: 10.2165/00023210-200115100-00004 [DOI] [PubMed] [Google Scholar]
- 116.Jafari B, Mohsenin V. Polysomnography. Clin Chest Med. 2010;31(2):287–297. doi: 10.1016/j.ccm.2010.02.005 [DOI] [PubMed] [Google Scholar]
- 117.Bloch KE. Polysomnography: a systematic review. Technol Health Care. 1997;5(4):285–305. doi: 10.3233/THC-1997-5403 [DOI] [PubMed] [Google Scholar]
- 118.Paruthi S, Brooks LJ, D’Ambrosio C, et al. Recommended amount of sleep for pediatric populations: a consensus statement of the American s. J Clin Sleep Med. 2016;12(6):785–786. doi: 10.5664/jcsm.5866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Consensus Conference P, Watson NF, Badr MS, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American academy of sleep medicine and sleep research society. J Clin Sleep Med. 2015;11(6):591–592. doi: 10.5664/jcsm.4758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Sluggett L, Wagner SL, Harris RL. Sleep duration and obesity in children and adolescents. Can J Diabetes. 2019;43(2):146–152. doi: 10.1016/j.jcjd.2018.06.006 [DOI] [PubMed] [Google Scholar]
- 121.Grandner MA. Sleep and obesity risk in adults: possible mechanisms; contextual factors; and implications for research, intervention, and policy. Sleep Health. 2017;3(5):393–400. doi: 10.1016/j.sleh.2017.07.014 [DOI] [PubMed] [Google Scholar]
- 122.Liu Y, Wheaton AG, Chapman DP, Cunningham TJ, Lu H, Croft JB. Prevalence of healthy sleep duration among adults–United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65(6):137–141. doi: 10.15585/mmwr.mm6506a1 [DOI] [PubMed] [Google Scholar]
- 123.Ancoli-Israel S, Roth T. Characteristics of insomnia in the United States: results of the 1991 national sleep foundation survey. I. Sleep. 1999;22(Suppl 2):S347–S353. [PubMed] [Google Scholar]
- 124.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6(2):97–111. doi: 10.1053/smrv.2002.0186 [DOI] [PubMed] [Google Scholar]
- 125.Briguglio M, Gianturco L, Stella D, et al. Correction of hypovitaminosis D improved global longitudinal strain earlier than left ventricular ejection fraction in cardiovascular older adults after orthopaedic surgery. J Geriatr Cardiol. 2018;15(8):519–522. doi: 10.11909/j.issn.1671-5411.2018.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Vitale JA, Banfi G, La Torre A, Bonato M. Effect of a habitual late-evening physical task on sleep quality in neither-type soccer players. Front Physiol. 2018;9:1582. doi: 10.3389/fphys.2018.01582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Roveda E, Vitale JA, Bruno E, et al. Protective effect of aerobic physical activity on sleep behavior in breast cancer survivors. Integr Cancer Ther. 2017;16(1):21–31. doi: 10.1177/1534735416651719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Sadeh A, Acebo C. The role of actigraphy in sleep medicine. Sleep Med Rev. 2002;6(2):113–124. doi: 10.1053/smrv.2001.0182 [DOI] [PubMed] [Google Scholar]
- 129.Sadeh A, Hauri PJ, Kripke DF, Lavie P. The role of actigraphy in the evaluation of sleep disorders. Sleep. 1995;18(4):288–302. doi: 10.1093/sleep/18.4.288 [DOI] [PubMed] [Google Scholar]
- 130.Lomeli HA, Perez-Olmos I, Talero-Gutierrez C, et al. Sleep evaluation scales and questionaries: a review. Actas Esp Psiquiatr. 2008;36(1):50–59. [PubMed] [Google Scholar]
- 131.Blake MJ, Blake LM, Schwartz O, et al. Who benefits from adolescent sleep interventions? Moderators of treatment efficacy in a randomized controlled trial of a cognitive-behavioral and mindfulness-based group sleep intervention for at-risk adolescents. J Child Psychol Psychiatry. 2018;59(6):637–649. doi: 10.1111/jcpp.2018.59.issue-6 [DOI] [PubMed] [Google Scholar]
- 132.Tanev KS, Winokur A, Pitman RK. Sleep patterns and neuropsychiatric symptoms in hospitalized patients with dementia. J Neuropsychiatry Clin Neurosci. 2017;29(3):248–253. doi: 10.1176/appi.neuropsych.16090166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Maruani J, Geoffroy PA. Bright Light as a personalized precision treatment of mood disorders. Front Psychiatry. 2019;10:85. doi: 10.3389/fpsyt.2019.00085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Martin JL, Hakim AD. Wrist actigraphy. Chest. 2011;139(6):1514–1527. doi: 10.1378/chest.10-1872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Jaehne A, Unbehaun T, Feige B, Lutz UC, Batra A, Riemann D. How smoking affects sleep: a polysomnographical analysis. Sleep Med. 2012;13(10):1286–1292. doi: 10.1016/j.sleep.2012.06.026 [DOI] [PubMed] [Google Scholar]
- 136.Geoffroy PA, Micoulaud Franchi JA, Lopez R, Schroder CM; membres du consensus Melatonine S. The use of melatonin in adult psychiatric disorders: expert recommendations by the French institute of medical research on sleep (SFRMS). Encephale. 2019. doi: 10.1016/j.encep.2019.04.068 [DOI] [PubMed] [Google Scholar]
- 137.Chennaoui M, Arnal PJ, Sauvet F, Leger D. Sleep and exercise: a reciprocal issue? Sleep Med Rev. 2015;20:59–72. doi: 10.1016/j.smrv.2014.06.008 [DOI] [PubMed] [Google Scholar]
- 138.Hyun MK, Baek Y, Lee S. Association between digestive symptoms and sleep disturbance: a cross-sectional community-based study. BMC Gastroenterol. 2019;19(1):34. doi: 10.1186/s12876-019-0945-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Ogilvie RP, Lutsey PL, Widome R, Laska MN, Larson N, Neumark-Sztainer D. Sleep indices and eating behaviours in young adults: findings from project EAT. Public Health Nutr. 2018;21(4):689–701. doi: 10.1017/S1368980017003536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Kruger AK, Reither EN, Peppard PE, Krueger PM, Hale L. Do sleep-deprived adolescents make less-healthy food choices? Br J Nutr. 2014;111(10):1898–1904. doi: 10.1017/S0007114514000130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Katagiri R, Asakura K, Kobayashi S, Suga H, Sasaki S. Low intake of vegetables, high intake of confectionary, and unhealthy eating habits are associated with poor sleep quality among middle-aged female Japanese workers. J Occup Health. 2014;56(5):359–368. doi: 10.1539/joh.14-0051-OA [DOI] [PubMed] [Google Scholar]
- 142.Quante M, Khandpur N, Kontos EZ, Bakker JP, Owens JA, Redline S. “Let’s talk about sleep”: a qualitative examination of levers for promoting healthy sleep among sleep-deprived vulnerable adolescents. Sleep Med. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Bhat SP, Sharma A. Current drug targets in obesity pharmacotherapy - a review. Curr Drug Targets. 2017;18(8):983–993. doi: 10.2174/1389450118666170227153940 [DOI] [PubMed] [Google Scholar]
- 144.Wolfe BM, Kvach E, Eckel RH. Treatment of obesity: weight loss and bariatric surgery. Circ Res. 2016;118(11):1844–1855. doi: 10.1161/CIRCRESAHA.116.307591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Riemann D, Nissen C, Palagini L, Otte A, Perlis ML, Spiegelhalder K. The neurobiology, investigation, and treatment of chronic insomnia. Lancet Neurol. 2015;14(5):547–558. doi: 10.1016/S1474-4422(15)00021-6 [DOI] [PubMed] [Google Scholar]
- 146.Porta M, Servello D, Zanaboni C, et al. Deep brain stimulation for treatment of refractory tourette syndrome: long-term follow-up. Acta Neurochir (Wien). 2012;154(11):2029–2041. doi: 10.1007/s00701-012-1497-8 [DOI] [PubMed] [Google Scholar]
- 147.Lojko D, Stelmach-Mardas M, Suwalska A. Is diet important in bipolar disorder? Psychiatr Pol. 2018;52(5):783–795. doi: 10.12740/PP/OnlineFirst/78703 [DOI] [PubMed] [Google Scholar]
- 148.Aucoin M, LaChance L, Cooley K, Kidd S. Diet and psychosis: a scoping review. Neuropsychobiology. 2018;1–23. doi: 10.1159/000493399 [DOI] [PubMed] [Google Scholar]
- 149.Owen L, Corfe B. The role of diet and nutrition on mental health and wellbeing. Proc Nutr Soc. 2017;76(4):425–426. doi: 10.1017/S0029665117001057 [DOI] [PubMed] [Google Scholar]
- 150.Sanchez-Villegas A, Ara I, Guillen-Grima F, Bes-Rastrollo M, Varo-Cenarruzabeitia JJ, Martinez-Gonzalez MA. Physical activity, sedentary index, and mental disorders in the SUN cohort study. Med Sci Sports Exerc. 2008;40(5):827–834. doi: 10.1249/MSS.0b013e31816348b9 [DOI] [PubMed] [Google Scholar]
- 151.Anderson KN, Bradley AJ. Sleep disturbance in mental health problems and neurodegenerative disease. Nat Sci Sleep. 2013;5:61–75. doi: 10.2147/NSS.S34842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Zanaboni Dina C, Porta M. Understanding Tourette Syndrome. A Guide to Symptoms, Management and Treatment. Oxon: Routledge; 2020. [Google Scholar]
- 153.Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7(7):e1000316. doi: 10.1371/journal.pmed.1000316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Briguglio M, Gianola S, Aguirre MFI, et al. Nutritional support for enhanced recovery programs in orthopedics: future perspectives for implementing clinical practice. Nutr Clin Metab. 2019;33(3):190–198. doi: 10.1016/j.nupar.2019.04.002 [DOI] [Google Scholar]
- 155.Dell’Osso B, Benatti B, Hollander E, et al. Socio-demographic and clinical characterization of patients with Obsessive-Compulsive Tic-related Disorder (OCTD): an Italian multicenter study. J Psychopathol. 2018;24:148–153. [Google Scholar]
- 156.Alvarez-Alvarez I, Zazpe I, Perez de Rojas J, et al. Mediterranean diet, physical activity and their combined effect on all-cause mortality: the Seguimiento Universidad de Navarra (SUN) cohort. Prev Med. 2018;106:45–52. doi: 10.1016/j.ypmed.2017.09.021 [DOI] [PubMed] [Google Scholar]
- 157.Leech RM, McNaughton SA, Timperio A. The clustering of diet, physical activity and sedentary behavior in children and adolescents: a review. Int J Behav Nutr Phys Act. 2014;11:4. doi: 10.1186/1479-5868-11-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Jezewska-Zychowicz M, Gebski J, Guzek D, et al. The associations between dietary patterns and sedentary behaviors in polish adults (lifestyle study). Nutrients. 2018;10(8). doi: 10.3390/nu10081004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Tasali E, Chapotot F, Wroblewski K, Schoeller D. The effects of extended bedtimes on sleep duration and food desire in overweight young adults: a home-based intervention. Appetite. 2014;80:220–224. doi: 10.1016/j.appet.2014.05.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.St-Onge MP, O’Keeffe M, Roberts AL, RoyChoudhury A, Laferrere B. Short sleep duration, glucose dysregulation and hormonal regulation of appetite in men and women. Sleep. 2012;35(11):1503–1510. doi: 10.5665/sleep.2198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.St-Onge MP, Zuraikat FM. Reciprocal roles of sleep and diet in cardiovascular health: a review of recent evidence and a potential mechanism. Curr Atheroscler Rep. 2019;21(3):11. doi: 10.1007/s11883-019-0772-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Lang C, Brand S, Feldmeth AK, Holsboer-Trachsler E, Puhse U, Gerber M. Increased self-reported and objectively assessed physical activity predict sleep quality among adolescents. Physiol Behav. 2013;120:46–53. doi: 10.1016/j.physbeh.2013.07.001 [DOI] [PubMed] [Google Scholar]
- 163.Kalak N, Gerber M, Kirov R, et al. Daily morning running for 3 weeks improved sleep and psychological functioning in healthy adolescents compared with controls. J Adolesc Health. 2012;51(6):615–622. doi: 10.1016/j.jadohealth.2012.02.020 [DOI] [PubMed] [Google Scholar]
- 164.Yang PY, Ho KH, Chen HC, Chien MY. Exercise training improves sleep quality in middle-aged and older adults with sleep problems: a systematic review. J Physiother. 2012;58(3):157–163. doi: 10.1016/S1836-9553(12)70106-6 [DOI] [PubMed] [Google Scholar]
- 165.de Castro Toledo Guimaraes LH, de Carvalho LB, Yanaguibashi G, Do Prado GF. Physically active elderly women sleep more and better than sedentary women. Sleep Med. 2008;9(5):488–493. doi: 10.1016/j.sleep.2007.06.009 [DOI] [PubMed] [Google Scholar]
- 166.Pizinger TM, Aggarwal B, St-Onge M-P. Sleep extension in short sleepers: an evaluation of feasibility and effectiveness for weight management and cardiometabolic disease prevention. Front Endocrinol (Lausanne). 2018;9:392. doi: 10.3389/fendo.2018.00392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Ngandu T, Lehtisalo J, Solomon A, et al. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): a randomised controlled trial. Lancet. 2015;385(9984):2255–2263. doi: 10.1016/S0140-6736(15)60461-5 [DOI] [PubMed] [Google Scholar]
- 168.Bott NT, Hall A, Madero EN, et al. Face-to-face and digital multidomain lifestyle interventions to enhance cognitive reserve and reduce risk of alzheimer’s disease and related dementias: a review of completed and prospective studies. Nutrients. 2019;11(9):2258. doi: 10.3390/nu11092258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Adan RAH, van der Beek EM, Buitelaar JK, et al. Nutritional psychiatry: towards improving mental health by what you eat. Eur Neuropsychopharmacol. 2019. doi: 10.1016/j.euroneuro.2019.10.011 [DOI] [PubMed] [Google Scholar]
- 170.Firth J, Siddiqi N, Koyanagi A, et al. The lancet psychiatry commission: a blueprint for protecting physical health in people with mental illness. Lancet Psychiatry. 2019;6(8):675–712. doi: 10.1016/S2215-0366(19)30132-4 [DOI] [PubMed] [Google Scholar]
- 171.Winpenny EM, van Sluijs EMF, White M, Klepp KI, Wold B, Lien N. Changes in diet through adolescence and early adulthood: longitudinal trajectories and association with key life transitions. Int J Behav Nutr Phys Act. 2018;15(1):86. doi: 10.1186/s12966-018-0719-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Corder K, Winpenny E, Love R, Brown HE, White M, Sluijs EV. Change in physical activity from adolescence to early adulthood: a systematic review and meta-analysis of longitudinal cohort studies. Br J Sports Med. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Lund HG, Reider BD, Whiting AB, Prichard JR. Sleep patterns and predictors of disturbed sleep in a large population of college students. J Adolesc Health. 2010;46(2):124–132. doi: 10.1016/j.jadohealth.2009.06.016 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Bradt S Invention of cooking drove evolution of the human species, new book argues. 2009. Available from: https://news.harvard.edu/gazette/story/2009/06/invention-of-cooking-drove-evolution-of-the-human-species-new-book-argues/. Accessed December12, 2019.