Abstract
Given the public health importance of depression, the identification of prevention programs with long-term effects on reducing the rate of depression is of critical importance, as is the examination of factors that may moderate the magnitude of such prevention effects. This study examines the impact of the Family Check-Up, delivered in public secondary schools beginning in sixth grade, on the development of major depression in adulthood (aged 28 – 30). The multilevel intervention program included (a) a universal classroom-based intervention focused on problem solving and peer relationship skills, (b) the Family Check-Up (selected), a brief assessment-based intervention designed to motivate parents to improve aspects of family functioning when warranted, and (c) family management treatment (indicated), focused on improving parenting skills. Demographic (gender and ethnicity) and baseline risk factors (family conflict, academic problems, antisocial behavior, and peer deviance) were examined as possible moderators in logistic regression analyses. Intervention effects on depression were moderated by baseline family conflict and academic performance, with stronger intervention effects for youth with low grade point averages and from low-conflict families at baseline. Such findings extend the emerging literature on prevention programs with long-term effects on depression, and highlight directions for future research to enhance such effects.
Keywords: Family intervention, prevention, depression, moderators
Introduction
Depression in adolescence is highly prevalent, significantly impairing, and associated with heightened risk for recurrent depressive episodes and suicidality in early adulthood (e.g., Fombonne, Wostear, Cooper, Harrington, & Rutter, 2001; Lewinsohn, Rohde, Seeley, Klein, & Gotlib, 2003). Thus, efforts to improve our understanding of effective prevention and intervention strategies for adolescent depression are critical. Indeed, a sizeable literature has examined psychosocial prevention and intervention efforts for depressed youth, most of which have focused on individual or group therapy provided to adolescents, based upon cognitive behavioral therapy (CBT; see Horowitz & Garber, 2006) or interpersonal therapy principles (IPT-A; Mufson, et al., 2011). While such interventions are beneficial for many youth, effect sizes are generally small-to-moderate (Sandler, Wolchick, Cruden, Mahrer, Ahn, Brincks, & Brown, 2014), substantial relapse rates are often observed (e.g., Birmaher et al., 2000), and few studies have examined longer-term durability beyond the first year (Beardslee et al., 2013). Clearly, additional research into improving intervention models for depressed youth is needed.
One opportunity to enhance intervention effectiveness is to expand the focus to improving family functioning. Many studies have documented the association between youth depression and problems in family functioning, including high levels of parental criticism and negative affect, parental psychopathology, and family conflict, as well as low parental support (see Sheeber, Hops, & Davis, 2001). Further, several studies have found that poorer responses to child-focused intervention is related to problems in family functioning, including maternal depression, parent-child conflict, low parental support, and high parental criticism (e.g., Asarnow, Goldstein, Thompson & Guthri, 1993; Brent et al, 1998; Birmaher et al., 2000; Feeny et al., 2009; Lewinsohn & Clarke, 1984). However, in the few studies of depression-focused programs that included at least some parent or family sessions, difficulty engaging parents into youth-focused treatments has emerged as a common challenge (Stark et al., 2012). For instance, Schochet and colleagues (2001) offered 3 sessions of parent-training in addition to an 11-session teen-focused prevention program, and found that only 10% of families took part in all 3 sessions. Not surprisingly, such studies have yielded limited evidence of the incremental benefits to youth of such adjunctive parenting components.
Thus, the development of alternative prevention and intervention approaches that might promote increased family engagement with treatment is an important goal. Of note, family interventions are much better established for other youth disorders, such as conduct problems. Many family risk processes are common across conduct problems and depression, including high levels of family stress and conflict, low parental warmth and support, and hostile and coercive parenting (Dishion & Patterson, 2006). Similarly, the dual-failure model (Patterson & Stoolmiller, 1991) highlights that conduct problems predict increased peer rejection and academic difficulties, which predict subsequent depression. Thus, the extensive literature on parent-focused interventions for youth conduct problems may have implications for augmenting depression-focused prevention efforts. Indeed, several prevention programs for conduct problems have been found to predict reductions in depression and internalizing symptoms (e.g., Mason et al., 2007; Perrino, Pantin, Prado, Huang, Brincks, Howe, … & Brown, 2014; Trudeau et al., 2007, 3015). Indeed, parenting programs have been found to yield larger effect sizes for reducing internalizing than externalizing problems (Kaminski, Valle, Filene, & Boyle, 2008).
The current study examines the Family Check-Up prevention program, which was developed as a family-focused model to reduce conduct problems and substance use in adolescence via improved parenting and family relationships (see Dishion & Kavanagh, 2003; Dishion & Stormshak, 2007). The program follows an adaptive intervention framework, in which intervention targets and doses are tailored to the individual needs of families, promoting increased family engagement and more efficient use of resources (Collins, Murphy, & Bierman, 2004). At the core of the intervention model is the Family Check Up assessment, a brief intervention based on motivational interviewing techniques designed to enhance family engagement and trigger the behavior change process (Miller & Rollnick, 1991). The outcome of the Family Check Up assessment is the identification of specific targets for subsequent family-based intervention, tailored to the individual goals of the family. Further intervention then focuses upon these agreed-upon targets.
The Family Check Up has produced reductions in conduct problems, substance use and family conflict, as well as improvements in academic functioning across from early through late adolescence in several school-based prevention trials (e.g., Connell et al., 2007; Dishion, Nelson & Kavanagh, 2003; Stormshak, Connell, & Dishion, 2009; Stormshak, et al., 2011; Van Ryzin, Stormshak, & Dishion, 2012). Of note, the Family Check Up has been shown to predict reductions in symptoms of depression across three randomized controlled trials, one in early childhood (Connell et al., 2008), and two in early adolescence (Connell & Dishion, 2008; Connell et al., in press). The evidence regarding the effectiveness across the adolescent trials has varied somewhat, with one trial producing a main effect of treatment for reducing depressive symptoms in high-risk youth across grades 6 through 8 (Connell & Dishion, 2008), while the subsequent trial found reduced depressive symptoms only for youth following an “adolescent onset” symptom trajectory (Connell et al, in press).
The current study examines the long-term effects of the Family Check Up on depression, from a school-based prevention trial of youth followed-from grades 6 (approximately age 11 – 12 years) through early adulthood (age 28 – 30). This work extends prior results for this sample by examining depression diagnoses, rather than self-reported symptoms, by examining the persistence of effects into adulthood, and by examining possible moderators of intervention effects. Of note, the examination of moderators of intervention effects can provide important insights into subgroups of youth who respond more or less strongly to intervention efforts, thereby providing information that can guide future efforts to better reach such youth.
Moderation of intervention effects
Several risk and demographic variables were examined as possible moderators of prevention effects on long-term depression outcomes in the current trial, including family conflict, antisocial behavior, peer deviance, and academic functioning, all measured at baseline, prior to initiation of the prevention program. Given the relatively consistent evidence that problematic family functioning predicts decreased intervention effects on youth depression (e.g., Asarnow, Goldstein, Thompson & Guthri, 1993; Brent et al, 1998; Birmaher et al., 2000; Feeny et al., 2009; Lewinsohn & Clarke, 1984), we hypothesized that elevated family conflict would predict decreased intervention effects. A competing hypothesis was that family conflict might predict improved intervention effects, as we have found that family conflict predicts increased engagement with the Family Check Up (see Connell et al., 2007), which might enhance intervention effects. In line with this competing hypothesis, Pantin and colleagures (2014) recently reported stronger effects on internalizing symptoms among families with poorer parent-child communication at baseline in several school-based trials of a prevention program targeting behavior problems in early adolescence.
Antisocial behavior, academic functioning, and peer deviance were all of potential importance because they are at the heart of the dual-failure model of the co-occurrence of depression and conduct problems in adolescence (Patterson & Stoolmiller, 1991). The current trial was designed to disrupt the development of behavior problems, and so the cumulative failure model might help to explain the “cross-over effects” of the program on depression. We hypothesized that youth higher in these problem-domains may, therefore, show stronger improvements in depression in response to the prevention program, as they would be at greatest risk for developing depression, and therefore most likely to benefit from the prevention program. There have been relatively few direct tests of such moderation hypotheses in the depression literature, however. Of note, Pantin and colleagues (2014) found that baseline antisocial behavior did not moderate the effects of a school-based prevention trial for behavior problems on adolescent internalizing symptoms. We are not aware of depression treatment or prevention studies that have directly examined academic functioning or peer deviance as moderators, although Brier, Rohde, Shaw, & Stice (2014) reported that peer support did not moderate effects of two cognitive behavioral depression prevention programs in adolescence.
Demographic factors of interest as potential moderators including youth gender and ethnicity. Gender has been examined as a moderator in several prevention and intervention trials for depression, and results have been quite mixed across primary studies. Nevertheless, two meta-analytic reviews suggest that prevention programs may be somewhat more effective for girls, compared to boys, perhaps because of the higher rate of depression in girls versus boys (Horowitz & Garber, 2006; Stice, Shaw, Bohon, & Marti, 2009). Of note, however, Horowitz and Garber (2006) found that the gender difference was eliminated when they excluded two studies of college students, suggesting a lack of gender differences among prevention programs for children and adolescence. Ethnicity has rarely been directly examined as a moderator, although a meta-analytic review by Stice and colleagues (2009) suggested that effects of prevention programs may be more effective for ethnic minority youth, which may be related to the higher rates of depression in ethnic minority populations, which might prompt greater engagement with prevention efforts.
Current study
The current study examines the long-term effects of the Family Check Up prevention program, initiated in early adolescence, on the likelihood of being diagnosed with depression in adulthood, at age 28 – 30. We also examined baseline risk factors (family conflict, conduct problems, peer deviance, and academic functioning), as well as demographic factors (youth gender and ethnicity) as potential moderators of intervention effects. In line with the results of several prevention and intervention studies for adolescent depression, we predicted that attenuated effects of the Family Check Up and adult depression would be observed in highly conflictual families, and speculated that stronger effects might be observed in youth higher in behavior problems, peer deviance, and poor academic functioning at baseline. Predictions regarding the effects of gender and ethnicity were more tenuous as the existing results for gender as a moderator of depression outcome in past studies are mixed, while the literature examining ethnicity as moderator is relatively sparse.
Methods
Participants
Participants included 998 adolescents and their families, recruited in sixth grade from three middle schools within an ethnically diverse metropolitan community in the northwestern United States. Parents of all sixth grade students in two cohorts were approached, and 90% consented to participate (see Figure 1). The sample included 526 males (52.7%) and 472 females (47.3%), including 423 Caucasians (42.3%), 291 African Americans (29.1%), 68 Latinos (6.8%), 52 Asian American families (5.2%), and 164 (16.4%) youth of other ethnicities (including biracial). Biological fathers were present in 585 families (58.6%). Youth were randomly assigned at the individual level to either control (498 youth) or intervention classrooms (500 youth) in the spring of sixth grade. Approximately 80% of youth were retained to the end of high-school, while diagnostic interviews at age 28-30 were not available for 244 youth (24.4%). Preliminary analyses suggested that attrition was consistent with Missing at Random assumptions.
Figure 1:
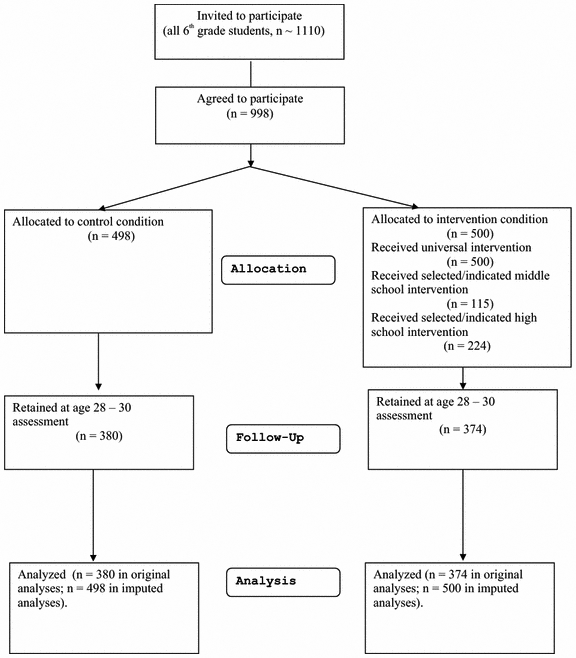
Flow of participants through study.
Intervention Protocol
The Family Check Up is part of a multilevel intervention program (see Dishion & Kavanagh, 2003; Dishion et al., 2003). The universal intervention was designed to support positive parenting practices and engage parents of high-risk youth for the selected intervention. This level included the establishment of a Family Resource Center (FRC) in each middle school, offering brief parent consultations, feedback to parents on their student’s behavior at school, and access to videotapes and books. In addition, the FRC parent consultant conducted six in-class lessons with students, modeled after the Life Skills Training (LST) program (Botvin, Baker et al, 1990), and focused on academic success, decision making, positive peer relationships, and coping/anger management, and problem-solving.
The selected intervention is the Family Check Up assessment, a brief, three-session intervention based on motivational interviewing (Miller & Rollnick, 2002). While all families could receive the Family Check Up, families of high-risk youth, determined by teacher ratings, were specifically offered the Family Check Up in 7th and 8th grades. The three sessions include an initial interview, where the therapist explores parent concerns and stage of change, and motivates involvement in the family assessment. The second session involves family participation in assessment tasks, including in-home videotaped parent–child interaction. In the third feedback session, the therapist summarizes the results of the assessment using motivational interviewing strategies, and explores potential intervention services that support family management practices.
The Family Check Up feedback leads to a collaborative decision with parents on indicated services appropriate for their family, including a parent group intervention and individually based behavior family therapy, based on the Everyday Parenting curriculum (EPC; Dishion et al., 2011), and focused on building positive parenting skills (e.g., positive reinforcement, limit-setting, problem-solving, and communication skills). Students who moved schools were offered services if they remained in the county. All services were delivered by Parent Consultants, including two Master’s-level therapists and one with a Bachelor of Science. Parent consultant ethnicity closely matched that of the participating families. Parent consultants were trained using a combination of strategies, including didactic instruction, role-playing, and videotaped supervision throughout the two years of intervention activity, and followed a written manual.
In the intervention condition, 115 families (23%) received the Family Check Up in grades 7 - 9, and 88 families received further intervention services after the Family Check Up. For Cohort 1, 46% of Family Check Ups were completed following the seventh grade family assessment, 53% following the eighth grade assessment, and 1% following the ninth grade assessment. For Cohort 2, 93% of Family Check Ups were completed following the seventh grade family assessment, and 7% following the eighth grade family assessment. These families had an average of 8.9 hours of direct contact with intervention staff over the study (SD = 9.42 hours). Family Check Ups were also offered in high school (in Grades 10–11) for families remaining in the school district, and 170 families (34%) received the Family Check Up, 109 of whom had not received it during middle school. Therefore, 224 families (45%) received the Family Check Up across the study. Additionally, youth were offered the Teen Check-Up (TCU) at age 16–17, that included the same three sessions as the Family Check Up (initial interview, assessment, and feedback). In the intervention group, 174 youths (35%) received the TCU, including 58 whose families had not received the Family Check Up.
Assessment Procedures
From grades 6 through 9, student surveys were conducted in schools in the spring semester, using an instrument developed by Metzler, Biglan, Rusby, and Sprague (2001). Students moving out of their original schools were followed at their new location. Youth were paid $20 for completing each assessment. Diagnostic interviews were administered when youth were aged 28-30 years of age. Interviews were primarily face-to-face except for participants living more than 100 miles from the study center, which were administered over the telephone. Evidence suggests good reliability between telephone and face-to-face diagnostic interviews for major depression (Rohde, Lewinsohn et al, 2014).
Measures
DSM-IV diagnoses.
Diagnostic interviews were administered at age 28 - 30, using the Composite International Diagnostic Interview (CIDI; World Health Organization, 1997), administered by trained research staff, unaware of the participant’s intervention status. Current analyses examined diagnoses according the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV), focused on past-year and lifetime Major Depressive Disorder (MDD) diagnoses. Overall, 65 (8.6% of individuals completing the interview) reported past year major depressive disorder diagnoses, and 124 (16.4% of individuals completing the interview) reported lifetime major depressive disorder diagnoses.
Adolescent problem behavior.
Youth reports of problem behavior were measured with 6 items reflecting past month engagement in the following behaviors: (a) lying to parents, (b) skipping school, (c) staying out all night without permission, (d) stealing, (e) panhandling, and (f) carrying a weapon. Responses were given on a 6-point scale, ranging from 1 (never) to 6 (more than 20 times). Good internal reliability was found for this scale across assessments (alpha reliability = .74).
Child gender.
Child gender was coded as 0 = “male,” and 1 = “female.”
Child ethnicity.
Youth ethnicity was coded as 0 = “Caucasian,” and 1 = “ethnic minority.”
Teacher report of sixth grade risk behavior.
Teachers used a 16-item questionnaire to rate their roster of sixth grade students on a variety of risk behaviors. Items included aggression, oppositionality, peer relationship problems, disliking school, and moodiness. The frequency with which youth engaged in these behaviors was reported using a 5-point scale ranging from 1 (never/almost never) to 5 (always/almost always). The sample mean =1.85 (SD = .85). High internal consistency reliability was found for this scale (alpha reliability = .95).
Deviant peer involvement.
Youth reports of deviant peer involvement were measured with 4 items that assessed the number of times in the past week they had spent time with peers who (a) get into trouble, (b) fight a lot, (c) take things that don’t belong to them, and (d) smoke cigarettes or chew tobacco. Responses ranged from 0 (never) to 7 (more than seven times). The sample mean = .76 (SD = 1.11). Good internal reliability was found for this scale (alpha reliability = .79).
Family conflict.
Youth reports of family conflict in sixth grade were measured averaging across 5 items reflecting the frequency with which family members engaged in a variety of conflict behaviors (e.g., “got angry with each other,” “argued at the dinner table”). Responses ranged from 0 (never) to 7 (more than seven times). The sample mean = .91 (SD = 1.03). Good internal reliability was found for this scale (alpha reliability = .81).
Intervention Status.
Random assignment was coded as 0 = “control,” and 1 = “intervention.”
Analytic Plan
Binary logistic regression analyses examined the effect of intervention on depression diagnoses in adulthood, as well as interactions between intervention status and baseline moderators (family conflict, grade point average, antisocial behavior, peer deviance, gender, ethnicity). Follow-up analyses for significant interactions were conducted by stratifying the sample by median split on the moderator, and examining intervention effects within the subsamples. In order to account for missing data, analyses also used Mulitple Imputation procedures in SPSS 23. These analyses used 10 imputations, with the imputation model including all main effect and interaction terms used in the original analyses.
Results
Descriptive Analyses
Descriptive statistics and correlations are presented in Table 1. Past year and lifetime depression diagnoses were unrelated to ethnicity, but were related to gender. Females were significantly more likely than males to report past year depression (11.1% of females who completed diagnostic interviews, and 5.8% of males; χ2 [df = 1] = 6.68, p < .05) and lifetime depression (20% of females, 12.5% of males; χ2 [df = 1] = 7.67, p < .05). Average age of first major depressive episode was 16.19 years (SD = 5.63, range = 4 – 28 years). Age of first episode was unrelated to any baseline covariates.
Table 1.
Descriptive statistics and correlations among study variables
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | ||
|---|---|---|---|---|---|---|---|---|---|
| 1. | Female gender | -- | |||||||
| 2. | Ethnic minority | .02 | -- | ||||||
| 3. | Family conflict (baseline) | .01 | .16* | -- | |||||
| 4. | Deviant peer association (baseline) | −.10* | .15* | .46* | -- | ||||
| 5. | Antisocial behavior (baseline) | −.12* | .18* | .41* | .57* | -- | |||
| 6. | GPA (baseline) | .19* | −.32* | −.24* | −.30* | −.35* | -- | ||
| 7. | Past year MDD (age 28 – 30) | .09* | .01 | .01 | −.01 | .00 | .02 | -- | |
| 8. | Lifetime MDD (age 28 – 30) | .10* | −.02 | .04 | .00 | .02 | .05 | .69* | -- |
| Mean: | .47 | .58 | 91 | .76 | 1.35 | 2.69 | .09 | .16 | |
| SD: | (.50) | (.49) | (.76) | (1.11) | (.56) | (.89) | (.28) | (.37) |
Note:
p < .05
Intervention Effects
Past-year depression.
Sixty-five youth were diagnosed with past-year major depressive disorder diagnoses, including 38 in the control condition, and 27 in the intervention condition. We first conducted an analysis including only main effects of intervention and baseline covariates. Intervention status was not significantly related to past year depression diagnoses (beta = −.36, SE = .26, p = .17). Next, we examined a model that included main and interaction effects, as shown in Table 2. With interaction terms included in the model, the main effect of intervention was at the level of a statistical trend (p = .06). Trend-level main effects for intervention status, gender, and family conflict were observed, along with a significant two-way interaction between intervention status and family conflict, and a trend-level two-way interaction between intervention status and grade point average (p = .06). Follow-up analyses for the intervention x family conflict interaction were conducted by stratifying the sample at the median for family conflict (median family conflict = .79). In the low-conflict group, 31 youth were diagnosed with past-year depression, including 22 (71%) in the control condition, and 9 (29%), a significant difference (χ2 [df = 1] = 5.24, p < .05; Odds ratio = 2.48). In the high family conflict group, 34 participants were diagnosed with MDD in the past year, of whom 47.1% (n = 16) were in the control condition, and 52.9% (n = 18) were in the intervention condition, a non-significant difference (χ2 [df = 1] = .08, n.s).
Table 2.
Binary logistic regression predicting past year MDD diagnoses.
| Past Year MDD | Lifetime MDD | |||
|---|---|---|---|---|
| Predictor | B (SE) | Odds Ratio | B (SE) | Odds Ratio |
| Intervention | −2.73 (1.64) + | .07 | −2.04 (1.18) + | .13 |
| Female Gender | .86 (.47) + | 2.36 | .45 (.31) | |
| Ethnic Minority | .08 (.24) | −.01 (.32) | ||
| Family Conflict (6th grade) | −.46 (.24) * | .63 | −.43(.17) * | .65 |
| Peer Deviance (6th grade) | .03 (.25) | .05 (.17) | ||
| Antisocial Behavior (6th grade) | −.01 (.52) | −.18 (.35) | ||
| GPA (6th grade) | −.49 (.32) | −.44 (.22) * | .65 | |
| Intervention x gender | −.31 (.60) | .18 (.43) | ||
| Intervention x ethnic minority | −.14 (.58) | −.24 (.44) | ||
| Intervention x Family conflict | .80 (.34) * | 2.83 | .61 (.25) * | 1.85 |
| Intervention x peer deviance | .10 (.33) | .07 (.24) | ||
| Intervention x antisocial behavior | −.32 (.66) | −.18 (.48) | ||
| Intervention x GPA | .74 (.39) + | 2.10 | .55 (.28) * | 1.74 |
Note:
p < .05
p < .10
Follow-up analyses examined the intervention x grade point average interaction by stratifying the sample at the median for grade point average (median grade point average = 2.77). In the low grade point average group, 28 youth were diagnosed with major depressive disorder in the past year, including 20 (71.4%) in the control condition, and 8 (28.6 %) in the intervention condition, a significant difference (χ2 [df = 1] = 4.69, p < .05; Odds ratio = 2.49). In the high grade point average group, 37 participants were diagnosed with major depressive disorder in the past year, of whom 48.6 % (n = 18) were in the control condition, and 50.9 % (n = 19) were in the intervention condition, a non-significant difference (χ2 [df = 1] = .03, n.s).
Lifetime Major Depressive Disorder.
Of 124 youth with lifetime depression diagnoses, 64 were in the control condition, while 60 were in the intervention condition. We first conducted an analysis including only main effects of intervention and baseline covariates. Intervention status was not significantly related to lifetime major depression diagnoses (beta = −.10, SE = .20, p = .62). Next, we examined a model that included main and interaction effects, as shown in table 3. A trend-level main effect was found for intervention status, while effects of family conflict and grade point average measured at age 11 were statistically reliable. Further, a significant two-way interaction between intervention status and family conflict was observed, as was the two-way interaction between intervention status and grade point average.
Follow-up analyses for the intervention x family conflict interaction were conducted by stratifying the sample at the median for family conflict. In the low-conflict group, 60 youth endorsed lifetime depression diagnoses, including 38 (63.3 %) in the control condition, and 22 (36.7 %) in the intervention condition, a significant difference (χ2 [df = 1] = 4.13, p < .05; Odds ratio = 1.79). In the high family conflict group, 64 participants with lifetime depression diagnoses, of whom 40.6 % (n = 26) were in the control condition, and 59.4 % (n = 38) were in the intervention condition, a non-significant difference (χ2 [df = 1] = 2.43, n.s).
Follow-up analyses were also conducted for the intervention x grade point average interaction by stratifying the sample at the median for academic performance. In the low grade point average group, 53 youth endorsed lifetime depression diagnoses, including 32 (60.4%) in the control condition, and 21 (39.6 %) in the intervention condition. Although the interaction term was statistically significant, this difference did not achieve statistical significance (χ2 [df = 1] = 1.84, n.s.; Odds ratio = .66). In the high grade point average group, 71 participants were diagnosed with depression, including 32 (45.1 %) in the control condition, and 39 (54.9 %) in the intervention condition, a non-significant difference (χ2 [df = 1] = .56, n.s).
Sensitivity Analyses
In order to examine the potential impact of missing data on analytic results, we replicated the analyses using multiple imputation procedures in SPSS 23. These analyses used 10 imputations, with the imputation model including all main effect and interaction terms used in the original analyses. The pooled results for the logistic regression analyses across the 10 imputations were nearly identical to the original results for both past-year and lifetime depression diagnoses. The formerly trend-level interaction between intervention status and grade point averages predicting past-year depression became statistically significant, most likely due to the increase in statistical power gained by including all participants, but there were no other substantial differences in results for either past-year or lifetime depression diagnoses using multiple imputation procedures.
Discussion
Although a number of depression prevention and intervention approaches have received empirical support in the literature, effects sizes are typically modest, evidence of long-term effectiveness is sparse, and programs incorporating families are relatively rare (see Sandler et al., 2014). Thus, there is substantial need for continued research on depression prevention programs, including efforts to better incorporate aspects of family functioning into intervention efforts. The current article examined long-term effects of the Family Check Up program, initiated in early adolescence, on reductions in depression diagnoses in adulthood, between the ages of 28 to 30 years. Additionally, we examined potential moderators of intervention effects, including family conflict, antisocial behavior, peer deviance, and academic performance, as these factors have been associated with risk for both antisocial behavior and depression in prior research (e.g., Connell & Dishion, 2008; Connell et al., 2007; Stormshak, et al., 2011; Van Ryzin, Stormshak, & Dishion, 2012), and were targets of the Family Check Up program. The examination of moderators of prevention effects may point to opportunities to enhance the program in future work.
In models including only main effects of intervention and baseline predictors, intervention was not significantly associated with the likelihood of either past-year or lifetime depression diagnoses at age 28 – 30. In the full analyses that included interaction terms, however, trend-level main effects of intervention on both past-year and lifetime depression diagnoses were observed. Importantly, however, the effects of intervention were moderated by baseline family conflict and academic performance. Stronger effects of intervention on adult depression diagnoses were observed for families low in conflict, and for youth with low grade point averages at baseline. We discuss each of these sets of results in turn
Family Conflict
For family conflict, moderation analyses indicated that the effects of intervention on depression diagnoses in adulthood were limited to youth from families low in conflict at baseline. Among low-conflict families, youth in the control group were approximately 2.5 times more likely to develop a depression diagnosis by adulthood, relative to youth in the intervention condition. However, for families high in conflict at baseline, the Family Check Up intervention did not predict long-term reductions in the likelihood of developing depression. These results are generally consistent with the broader literature on family dysfunction as a moderator of depression-focused prevention and intervention programs documenting reduced intervention effects on adolescent depression in the face of elevated family conflict (e.g., Asarnow, Goldstein, Thompson & Guthri, 1993; Brent et al, 1998; Birmaher et al., 2000; Feeny et al., 2009; Lewinsohn & Clarke, 1984).
It appears that elevated family conflict interferes with adolescent responsiveness to intervention and prevention efforts for depression across treatment modalities (youth-focused CBT and family-focused interventions). The mechanisms for such interference, however, remain to be identified. In the current study, high-conflict families were more likely to receive the selected and indicated levels of the multilevel prevention framework (see Connell et al., 2007), and so high conflict did not simply predict diminished willingness to receive services. It may be that exposure to high family conflict interferes with youth’s uptake of skills (such as problem-solving and communication) during treatment. Additionally, youth from high conflict families in early adolescence may disengage from family relationships and become more involved in peer or dating relationships across early adolescence, and these extra familial sources of stress may become more important precipitants of depression in adulthood for such youth. Family-intervention may need to be initiated earlier (to prevent disengagement from the family), or may need to more fully address a broader range of domains of functioning (e.g., Wolchik, Sandler et al, 2013). Such explanations for reduced intervention effect on adult depression in high-conflict families are clearly speculative, and future work on the manner in which family conflict interferes with improvements in youth depression is needed, in light of the consistency of moderation findings for family conflict across studies. Nevertheless, it will be important to adapt the Family Check Up to more directly address depression-specific` aspects of family functioning in high-conflict families.
It is also worth highlighting that there are studies that have found the opposite pattern of moderation of intervention effects on depression by family conflict. Perrino and colleagues (2014) found stronger effects on internalizing symptoms among Hispanic youth, aggregating data across three prevention trials of the Familias Unidas program, a family-focused program originally designed to reduce behavior problems. Several factors might explain the different results for that study. For instance, Perrino and colleagues (2014) examined parent-reported internalizing symptoms, rather than depression diagnoses by youth report, and it is parental reports of symptoms might yield a different pattern of results. Further, the Familias Unidas samples included only Hispanic youth, while most studies (including the current one) included more ethnically diverse samples with a preponderance of European American families, and it is possible that family conflict effects might differ across ethnic groups.
Academic performance
For academic performance (measured by grade point average), results suggest that the prevention approach was most effective for the highest risk youth at baseline (those with the lowest grade point averages). Among youth with lower grade point averages, the prevention program was associated with significant reductions in past-year depression diagnoses by adulthood, relative to youth with higher grade point averages. A similar result was observed for lifetime diagnoses, although the interaction between intervention status and academic performance was only significant in analyses using multiple imputation to account for missing data, which yielded somewhat increased statistical power. Of note, lifetime diagnoses covers a broad time-frame, including pre-intervention, and so may be somewhat less sensitive to prevention effects. Broadly, however, such results may reflect the importance of early academic difficulties in motivating families to respond to intervention services through the school, as families of youth with lower grade point averages were disproportionately likely to engage with the Family Check Up across middle-school (Connell et al., 2007). Such a possibility is consistent with the dual-failure model, which suggests that academic difficulties are important predictors of the risk for depression in early adolescence, and to the extent that high-risk families engaged with the Family Check Up, that engagement may ultimately disrupt the developmental pathway towards depression.
Non-significant Moderation Results
While baseline family conflict and academic functioning were found to moderate the effects of intervention on adult depression diagnoses, results for demographic factors (gender and ethnicity) and other baseline moderators (antisocial behavior and peer deviance) were not significant. Of note, the literature on these factors as moderators is either mixed (for gender) or relatively sparse (for ethnicity, antisocial behavior, and peer deviance). Effects for gender have been somewhat mixed across studies, and indeed across metanalytic reviews of the depression prevention literature. For instance, while Stice and colleagues (2009) found significantly stronger effects for prevention programs in samples that included a larger proportion of girls when they included several studies with college-student samples, Horowitz and Garber (2006) reported non-significant effects of gender as a moderator across prevention studies when they removed studies with college students. The current results are, therefore, consistent with the bulk of prevention programs delivered in adolescence, and indicate that the effects of the Family Check Up program on adult depression diagnoses do not differ for boys and girls.
Ethnicity has been relatively rarely examined as a moderator of effects in depression prevention studies, although a large meta-analysis by Stice and Colleagues (2009) suggested that studies including a larger percentage of ethnic minority youth tend to yield larger effect sizes, which they suggested might be due to the elevated risk for depression among ethnic minority youth. Such effects were not observed in the current study, however. Given that youth in the current study were originally recruited from urban schools in lower-income communities, it is possible that there might have been fewer ethnic-group differences in exposure to stressors associated with depression, such as poverty, in the current sample relative to the broader population.
Conduct problems and peer deviance have rarely been examined as moderators of prevention effects on depression. A review by Ollendick, Jarrett, Grills-Taquechel, Hovey, & Wolff (2008), however, found that comorbid conduct problems did not appear to moderate intervention effects on internalizing problems across studies. Thus, the lack of moderation results for these variables in the current study is consistent with the broader literature, and suggests that co-occurring behavior problems (and closely related factors such as peer deviance) do not appear to moderate the impact of the Family Check-Up on adult depression diagnoses.
Limitations and Future Directions
There are several limitations to the current study that point to future research directions. First, most measures included in the current analyses were derived from youth report, and future research employing independent measurement approaches would be valuable. However, the primary outcome measure, major depressive disorder diagnoses, was collected using a well-validated diagnostic interview schedule, which enhances our confidence in the long-term effects on depression. Second, we only collected depression symptom data at baseline on a subset of participants deemed at-risk for behavior problems by teacher reports (n = 141), and measures of depression (either questionnaire or interview based) were not available for the rest of the sample at the start of the study. As such, we cannot rule out possible baseline differences in depression across intervention and control condition as a possible explanation for apparent intervention effects. Several factors mitigate this concern, however. Youth were randomly assigned to intervention and control conditions, and the large sample size suggests that substantial random differences would be unlikely. Indeed, baseline differences across groups have not been observed across any of the primary variables examined in this study in prior work (e.g., demographic factors, antisocial behavior, substance use, peer problems). Finally, high-risk youth (determined via teachers’ reports at baseline) completed a lengthier assessment battery including depressive symptoms, and no significant differences across this subset of youth were observed for such symptoms at baseline (see Connell & Dishion, 2008).
More broadly, it is worth highlighting that the current intent-to-treat analyses may mask substantial variability in the nature and intensity of intervention services received by families, in line with the multi-level nature of the Family Check Up program. In line with the randomized encouragement trial design, only a subset of youth received the Family Check Up assessment and follow-up parenting intervention services, and prior work with this sample has found stronger effects on youth functioning among these youth (e.g. Connell et al., 2007), relative to the full sample (most of whom received only the universal intervention). The current analyses, however, only examine the effects of the overall program (including universal, selected, and indicated levels of intervention), rather than permitting an examination of the specific program components.
Conclusion
This study highlights that family-focused preventive interventions delivered in adolescence can significantly reduce the likelihood of developing depression in adulthood, at least for subgroups of youth. The long-term nature of these results is noteworthy, as relatively few studies of depression-focused interventions have examined such long-term effects from adolescence through early adulthood, and highlight the importance of intervention and prevention efforts during this important developmental span for reductions in suicide risk in adulthood. The current results also add to the growing body of work suggesting improvements in depression as a function of the Family Check Up intervention across early childhood and adolescence (Connell & Dishion, 2008; Shaw et al., 2009; Connell, Stormshak, Dishion, Fosco, & Van Ryzin, in press), and underscore the need to conduct a randomized trial of the Family Check Up that specifically targets adolescent depression, in order to further enhance these effects. These results are also consistent with several other programs designed to prevent behavior problems and substance use that have found cross-over effects on depression in early adulthood (e.g., Trudeau et al., 2015; Wilcox et al., 2008), and highlight the potential importance of continued efforts to better integrate family processes into intervention programs for depression.
Acknowledgements
This project was supported by grants DA07031 and DA13773 from the National Institute on Drug Abuse, and AA12702 from the National Institute on Alcohol Abuse and Alcoholism, to Thomas Dishion. The authors gratefully acknowledge the clinical leadership of Dr. Kate Kavanagh on this project, and the contribution of the Project Alliance staff, Portland Public Schools, and the participating youth and families.
Biography
Arin Connell is an Associate Professor in the Department of Psychological Sciences at Case Western Reserve University. He received his doctorate in clinical psychology from Emory University. His major research interests include the etiology of emotional and behavior problems in childhood and adolescence, and prevention programs to ameliorate the risk of developing such problems.
Thomas Dishion is a Professor in the Department of Psychology and director of the REACH institute at Arizona State University. His research interests include the etiology of conduct problems and substance use across development, as well as the development and dissemination of prevention programs for at-risk youth. He is the developer of the Family Check Up prevention program.
Footnotes
Conflicts of Interest
The authors report no conflict of interests.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Contributor Information
Arin M. Connell, Case Western Reserve University
Thomas J. Dishion, Arizona State University, REACH Institute & Oregon Research Institute
References
- Asarnow J, Goldstein M, Tompson M, & Guthrie D (1993). One-year outcomes of depressive disorders in child psychiatric inpatients: Evaluation of the prognostic power of a brief measure of expressed emotion. Journal of Child Psychology and Psychiatry, 34, 129 – 137. [DOI] [PubMed] [Google Scholar]
- Beardslee W, Brent D, Weersing V, Clarke G, Porta G, Hollon S … Garber J (2013). Prevention of depression in at-risk adolescents. JAMA psychiatry, 70, 1161–1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Brent D, Kolko D, Baugher M, Bridge J, Holder D, & Ulloa R (2000). Clinical outcome after short-term psychotherapy for adolescents with major depressive disorder. Archives of General Psychiatry, 57, 29–36. [DOI] [PubMed] [Google Scholar]
- Botvin GJ, Baker E, Dusenbury L, Tortu S, & Botvin EM (1990). Preventing adolescent drug abuse through a multimodal cognitive–behavioral approach: Results of a 3-year study. Journal of Consulting and Clinical Psychology, 58(4), 437–446. [DOI] [PubMed] [Google Scholar]
- Brent D, Kolko D, Birmaher B, Baugher M, Bridge J, Roth C, & Holder D (1998). Predictors of treatment efficacy in a clinical trial of three psychosocial treatments for adolescent depression. Journal of the American Academy of Child Psychology, 37, 906–914. [DOI] [PubMed] [Google Scholar]
- Collins L, Murphy S, & Bierman K (2004). A Conceptual Framework for Adaptive Preventive Interventions. Prevention Science, 5, 185–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connell A, Bullock B, Dishion T, Shaw D, Wilson M, & Gardner F (2008). Family intervention effects on co-occurring early childhood behavioral and emotional problems: A latent transition analysis approach. Journal of Abnormal Child Psychology, 36, 1211–1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connell A, Dishion T, Yasui M, & Kavanagh K (2007). An ecological approach to family intervention: Linking parent compliance with treatment to long-term prevention of adolescent problem behavior. Journal of Consulting & Clinical Psychology, 75, 568 – 579. [DOI] [PubMed] [Google Scholar]
- Connell A, Stormshak E, Dishion T, Fosco G, & Van Ryzin M (in press). The Family Check-Up and adolescent depression: An examination of treatment responders and non-responders. Prevention Science. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dishion T, & Patterson G (2006). The development and ecology of antisocial behavior in children and adolescents In Developmental Psychopathology. In Cicchetti D & Cohen DJ (Eds). (Vol. 3, pp. 503 – 541). New York: Wiley. [Google Scholar]
- Dishion T, & Stormshak E (2007). Intervening in children’s lives: An ecological, family-centered approach to mental health care. Washington, DC: American Psychological Association. [Google Scholar]
- Dishion TJ, Stormshak EA, & Kavanagh KA (2011). Everyday parenting: A professional's guide to building family management skills: Champaign, IL: Research Press. [Google Scholar]
- Feeny N, Silva S, Reinecke M, McNulty S, Findling R, Rohde P, … & March J (2009). An exploratory analysis of the impact of family functioning on treatment for depression in adolescents. Journal of Clinical Child & Adolescent Psychology, 38(6), 814–825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fombonne E, Wostear G, Cooper V, Harrington R, & Rutter M (2001). The Maudsley long term follow-up of child and adolescent depression: I. Psychiatric outcomes in adulthood. British Journal of Psychiatry, 179, 210 – 217. [DOI] [PubMed] [Google Scholar]
- Horowitz J, & Garber J (2006). The prevention of depressive symptoms in children and adolescents: A meta-analytic review. Journal of Consulting & Clinical Psychology, 74, 401–415. [DOI] [PubMed] [Google Scholar]
- Kaminski J, Valle L, Filene J, & Boyle C (2008). A Meta-analytic Review of Components Associated with Parent Training Program Effectiveness. Journal of Abnormal Child Psychology, 36, 567–589. [DOI] [PubMed] [Google Scholar]
- Lewinsohn P, & Clarke G (1984). Group treatment of depressed individuals: The "coping with depression" course. Advances in Behaviour Research & Therapy, 6, 99–114. [Google Scholar]
- Lewinsohn P, Rohde P, Seeley J, Klein D, & Gotlib I (2003). Psychosocial functioning of young adults who have experienced and recovered from Major Depressive Disorder during adolescence. Journal of Abnormal Psychology, 112, 353 – 363. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, & Williams J (2004). Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research, 39, 99–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason W, Kosterman R, Hawkins J, Haggerty K, Spoth R, & Redmond C (2007). Influence of a family-focused substance use preventive intervention on growth in adolescent depressive symptoms. Journal of Research on Adolescence, 17, 541–564. [Google Scholar]
- Metzler CW, Biglan A, Rusby JC, & Sprague JR (2001). Evaluation of a comprehensive behavior management program to improve school-wide positive behavior support. Education & Treatment of Children, 24(4), 448–479. [Google Scholar]
- Miller W, & Rollnick S (2002). Motivational interviewing: Preparing people for change. New York: Guilford press. [Google Scholar]
- Mufson L, Dorta KP, Moreau D, & Weissman MM (2011). Interpersonal psychotherapy for depressed adolescents. Guilford Press. [Google Scholar]
- Muthén L, & Muthén B (2013). Mplus User’s Guide, V. 7. Los Angeles: Muthen & Muthen. [Google Scholar]
- Ollendick TH, Jarrett MA, Grills-Taquechel AE, Hovey LD, & Wolff JC (2008). Comorbidity as a predictor and moderator of treatment outcome in youth with anxiety, affective, attention deficit/hyperactivity disorder, and oppositional/conduct disorders. Clinical Psychology Review, 28(8), 1447–1471. [DOI] [PubMed] [Google Scholar]
- Patterson G, & Stoolmiller M (1991). Replications of a dual failure model for boys’ depressed mood. Journal of Consulting and Clinical Psychology, 59, 491 – 498. [DOI] [PubMed] [Google Scholar]
- Perrino T, Pantin H, Prado G, Huang S, Brincks A, Howe G, … & Brown CH (2014). Preventing internalizing symptoms among Hispanic adolescents: A synthesis across Familias Unidas trials. Prevention Science, 15(6), 917–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, & Seeley JR (2014). Comparability of telephone and face-to-face interviews in assessing axis I and II disorders. American Journal of Psychiatry. [DOI] [PubMed] [Google Scholar]
- Sandler I, Wolchik S, Cruden G, Mahrer N, Ahn S, Brincks A, & Brown C (2014). Overview of Meta-Analyses of the Prevention of Mental Health, Substance Use, and Conduct Problems. Annual review of clinical psychology, 10, 243–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schochet I, Dadds M, Holland D, Whitefield K, Harnett P, & Osgarby S (2001). The efficacy of a universal school-based program to prevent adolescent depression. Journal of Clinical Child Psychology, 30, 303 – 315. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Connell A, Dishion TJ, Wilson MN, & Gardner F (2009). Improvements in maternal depression as a mediator of intervention effects on early childhood problem behavior. Development and psychopathology, 21, 417–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheeber L, Hops H, & Davis B (2001). Family processes in adolescent depression. Clinical child and family psychology review, 4, 19–35. [DOI] [PubMed] [Google Scholar]
- Smith JD, Knoble NB, Zerr A, Dishion TJ, & Stormshak EA (2014). Multicultural competence and the Family Check-Up: Indirect effect on adolescent antisocial behavior through family conflict. Journal of Clinical Child & Adolescent Psychology, 43(3), 400–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stark K, Banneyer K, Wang L, & Arora P (2012). Child and adolescent depression in the family. Couple and Family Psychology: Research and Practice, 1, 161–184. [Google Scholar]
- Stormshak E, Connell A, & Dishion T (2009). An adaptive approach to family-centered intervention in schools. Prevention Science, 10, 221–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stormshak E, Connell A, Véronneau MH, Myers M, Dishion T, Kavanagh K, & Caruthers A (2011). An ecological approach to promoting early adolescent mental health and social adaptation. Child Development, 82, 209–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trudeau L, Spoth R, Randall GK, Mason WA, & Shin C (2012). Internalizing symptoms: Effects of a preventive intervention on developmental pathways from early adolescence to young adulthood. Journal of youth and adolescence, 41(6), 788–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trudeau L, Spoth R, Mason WA, Randall GK, Redmond C, & Schainker L (2015). Effects of adolescent universal substance misuse preventive interventions on young adult depression symptoms: mediational modeling. Journal of abnormal child psychology, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Ryzin MJ, Stormshak EA, & Dishion TJ (2012). Engaging parents in the family check-up in middle school: Longitudinal effects on family conflict and problem behavior through the high school transition. Journal of Adolescent Health, 50(6), 627–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox HC, Kellam SG, Brown CH, Poduska JM, Ialongo NS, Wang W, & Anthony JC (2008). The impact of two universal randomized first-and second-grade classroom interventions on young adult suicide ideation and attempts. Drug and Alcohol Dependence, 95, S60–S73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolchik SA, Sandler IN, Tein JY, Mahrer NE, Millsap RE, Winslow E, … & Reed A (2013). Fifteen-year follow-up of a randomized trial of a preventive intervention for divorced families: effects on mental health and substance use outcomes in young adulthood. Journal of consulting and clinical psychology, 81(4), 660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (1997). Composite International Diagnostic Interview — Version 2.1. Geneva: World Health Organization. [Google Scholar]


