Abstract
Introduction:
Oral cancer is now a major public health problem in India. It does not only affect the patient, but also has a deep psychosocial impact on the family caregivers who are deeply involved with the cancer patient for nursing, timely medication, and consulting the doctor. Studies have found that the caregivers often suffer from depression, anxiety, and fear of losing their near and dear ones. This study aims to capture the psychosocial impact of oral cancer on the family caregivers.
Materials and Methods:
This was a cross-sectional study carried out in a tertiary care hospital with the primary caregivers of those oral cancer patients who completed their treatment and came for follow-up after 2–3 months of treatment completion. The study participants were recruited till a sample size of 100 was reached. This was adequate to report proportions with an error of 10%. We have used “The Caregiver Quality of Life Index – Cancer” scale to capture the psychosocial impact of oral cancer on primary caregiver of the patient. The study was initiated after obtaining approval from the Institutional Ethics Committee. Informed written consents were obtained from all the study participants before beginning the interviews.
Results:
Caregivers played an important role in the recovery of the patients. However, the strain of caregiving resulted in increased emotional stress among them. We found 56% of the family caregivers were female and 41% were male. Majority of the caregivers who accompanied the patients to hospital were the spouses. For the caregivers, the mean score for burden of the disease was found to be 60.0 (±20.2), that for disruption was 50.4 (±21.7), and for positive adaptation was 61.4 (±20.7).
Conclusion:
Caregivers, who are usually invisible to the health-care team, should be recognized and their mental and physical well-being should also be given attention.
Keywords: Family caregiver, oral cancer, psychosocial impact, the Caregiver Quality of Life Index – Cancer questionnaire
Introduction
Oral cancer, which is mostly related to chewing oral tobacco, is very much prevalent in our country. The age-adjusted rate of oral cancer in India is high, that is, 20 per 100,000 population and accounts for 30% of all cancers in the country.[1,2] As per the Global burden of Cancer study 2013,[3] Oral cancer ranks second as the number of incident cases among both sexes in India after breast cancer and ranks eighth as per the number of deaths occurring as a result of the disease in both sexes. The burdens imposed by cancer vary greatly between regions within India.[3,4,5] As per the population-based cancer registry, Wardha, Maharashtra, India, oral cancer ranks first among the males in the Wardha district [Figure 1]. In Wardha district, 24.87% cancer in males and 11.55% cancer among females consists of oral cancer and the crude incidence rate of oral cancer per 100,000 population in Wardha is 12.8 and 6.9 for males and females, respectively.[6]
Figure 1.
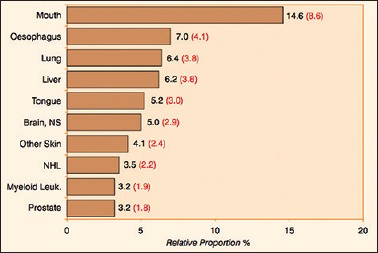
Leading sites of cancer occurrences among males in Wardha district (2012–2014) with their age-adjusted rates in brackets(6). [NS= Nervous System ,NHL= Non Hodgkin's Leukemia]
Oral cancer and its treatment have a profound effect on not only the patients, but also the family caregivers. There is a complex emotional mixup, when the family members get to know that their near and dear ones are suffering from such a deadly disease. All the family members – spouses, siblings, children and parents – each play a specific role in taking care of the patient, starting from the diagnosis till the treatment gets completed. Blanchard et al.[7] studied the psychosocial impact of cancer on family caregivers. According to the author, families are important in providing the environment for adjustment for the cancer patient. It is not only the patient, but also the family members have to directly confront with the impact of cancer. Northouse and Peters-Golden[8] found that, 22.7% of caregivers suffer from depression and 2.7% have severe depression. Anxiety was often associated with depression, noted in 79.3% of caregivers and led to intake of anxiolytics among 10% of them. It was linked to the fear of losing their close ones in 57.3% of cases.[7,8]
Each of the family caregivers face a different degree of impact as a result of the disease per se, but the one who is directly involved in nursing the patient at home, giving timely medication and taking him/her to the treatment center is considered as a primary caregiver in our study. There are very less studies on the psychosocial impact of oral cancer on caregivers in Indian scenario, as a result of which we planned to carry out this very study to capture the psychosocial impact of the disease on family caregivers.
Materials and Methods
This is a cross-sectional study. It was conducted in a tertiary care center of Wardha, Maharashtra, India. The study was continued from September 2015 to August 2017. The study population included the primary caregivers accompanying the patients diagnosed histopathologically with squamous cell cancer of lip, tongue, buccal mucosa, alveolus and gallbladder mucosa who came to the radiotherapy unit of the hospital for follow-up after 2–3 months of completion of their treatment.
The study participants were recruited till a sample size of 100 was reached. This was adequate to report proportions with an error of 10%.
The one who is directly involved in nursing the patient at home, giving timely medication and taking him/her to the treatment center, is considered as a primary caregiver in our study. The patient's family was contacted previously over phone, in order to inform the primary caregiver to come to the hospital on the scheduled visit for the interview. Informed written consents were obtained from all the study participants. The caregivers were explained regarding the objective of this study and interview was taken in private, in absence of the patient of oral cancer, where they could speak openly and talk about the different experiences faced by him/her throughout the tenure of the cancer treatment, starting from the time of diagnosis of illness till the interview was taken.
We have used “The Caregiver Quality of Life Index – Cancer (CQOLC)” scale[9] to capture the psychosocial impact of the oral cancer on the primary caregiver of the patient. The CQOLC was a self-reported questionnaire that was translated into the local language (Marathi) before using it. It captured the psychosocial impact of the disease on the caregiver by identifying the burden of the disease on the caregiver, how it caused disruption in family, the positive adaptation of the caregiver, and lastly the financial concern of the family for carrying out the treatment.
Pilot testing of the tool was done in the same setup, with ten primary caregivers of oral cancer patients, before we started the study, which was not included for the analysis.
The CQOLC scales used Likert scale, which we converted into a score from 0 to 100 using the following method that was already mentioned in the manual of EORTC questionnaires:
Step 1: Calculation of the Raw Score (RS): In practical terms, if items II, I2., In are included in a scale, then RS was calculated as RS = (II + I2 +……In)/n
Step 2: A linear transformation method was used to standardize the RS so that the scores range from 0 to 100.
In practical terms, if items II, I2., In are included in a scale, the procedure is as follows:
The RS (Raw Score) was calculated as RS = (II + I2+……In)/n
The linear transformation was applied to 0–100 to obtain score S,
S = (RS – [Minimum score in the Likert scale]/Range*) × 100
*Range is the difference between the maximum and minimum possible values of RS. This technique has been designed so that all items in any scale take the same range of values (0–100). Therefore, the range of RS equals the range of the item values.
The data were entered into EPI INFO software version 7[10] and analysis was done using R software.[11]
We also took in-depth interview (IDI) of purposively chosen family caregivers (n = 20) on the same topic to know in detail the impact of the disease. The interviewer was trained in qualitative methods and the interviews were taken in the language the patient could understand. All the interviews were audio recorded after taking due permission from the study participants. A field guide was prepared previously that included open-ended questions and we have also included certain probes to further go in-depth to have a better understanding of their experience as family caregivers. The IDI was conducted on a separate day, when those study participants could give us time on their following visit to hospital. The study was initiated after obtaining approval from the institutional Ethics Committee.
The study participants who were found to be in need of counseling were counseled after the interview session by the interviewer himself and, wherever specialist care was needed, they were referred to the specialists for additional counseling sessions. All data were dealt confidentially and the identification details of the study participants were anonymized in the report and other communication.
Results
Caregivers played an important role in the recovery of the oral cancer patients. We have included the caregivers who were accompanying the patients included in our study to the hospital for follow-up. We found that there were four patients included in our study were not accompanied by the primary caregiver when they came to the hospital for follow-up and two of the caregivers refused to sign consent form for the interview. Hence, we have included 94 caregivers in our study for final analysis. Characteristics of the caregivers included in our study are described in Table 1.
Table 1.
Characteristics of family caregivers (n=94)
| n (%) | |
|---|---|
| Sex | |
| Male | 41 (44) |
| Female | 53 (56) |
| Relationship with patient | |
| Spouse | 53 (56) |
| Children | 34 (36) |
| Others | 7 (8) |
| Occupation | |
| Farmer | 20 (21) |
| Daily wage labor | 22 (23) |
| Homemaker | 28 (30) |
| Service | 13 (14) |
| Others | 11 (12) |
Among the caregivers, 56% of them were female and 41% were male. Moreover, majority of the caregivers who accompanied the patients to the hospital were the spouses and 34% were the children. We found that 44% of the caregivers were farmers or daily wage laborers; 30% were homemakers; 14% were in salaried job; and 12% were either retired or had their own small or large business.
To understand the burden of the disease among the family caregivers, it becomes essential to have a basic understanding of the sociodemographic profile of the oral cancer patients, as is narrated in Table 2. Here, we found, out of 100 oral cancer patients which included cancer of lip, tongue, buccal mucosa, gingivo-buccal mucosa and alveolus, the mean age was 48.7 years (range, 30–72 years), with majority of the patients being male (81%). Nearly 83% of the patients stayed with their spouse and 48% of them stayed in nuclear families. We have noted the years of schooling of the study participants and it was found that 19% of them never went to school, while 15% of them studied till class VI. Majority of the participants studied for 7–12 years and only 6% of them attended college. Approximately, three-fifth of the study participants (60%) were from other backward classes. As per modified B J Prasad classification, 13%, 21%, 33%, 32% and 1% of the families were from Class I (upper), Class II (upper middle), Class III (Lower middle), Class IV (upper lower), and Class V (lower), respectively.
Table 2.
Sociodemographic charactersitics of oral cancer patients (n=100)
| n (%) | |
|---|---|
| Age (years) | |
| <40 | 22 (22) |
| 40-60 | 59 (59) |
| >60 | 19 (19) |
| Sex | |
| Male | 81 (81) |
| Female | 19 (19) |
| Years of schooling/education | |
| 0 | 19 (19) |
| 1-6 | 15 (15) |
| 7-12 | 60 (60) |
| >12 | 6 (6) |
| Category | |
| SC | 23 (23) |
| ST | 11 (11) |
| OBC | 43 (43) |
| Open | 17 (17) |
| Others | 6 (6) |
| Marital status | |
| With spouse | 83 (83) |
| Without spouse | 17 (17) |
| Socioeconomic status | |
| Class I (upper) | 13 (13) |
| Class II (upper middle) | 21 (21) |
| Class III (lower middle) | 33 (33) |
| Class IV (upper lower) | 32 (32) |
| Class V (lower) | 1 (1) |
| Family | |
| Nuclear | 48 (48) |
| Joint | 52 (52) |
| Occupation | |
| Service (government/private) | 30 (30) |
| Business (small) | 7 (7) |
| Daily labor/farmer | 29 (29) |
| Retired (pensioner) | 2 (2) |
| Homemaker/staying at home | 32 (32) |
OBC=Other backward class
Table 3 shows the relationship of the caregiver with the sex of the patients included in our study. We found that for the male oral cancer patients attending the hospital, 63% of the caregivers were their wives, but for the female patients, 62% were their sons and 28% were their husbands. Around 66% of the female patients whose caregiver were their sons were widowed.
Table 3.
Relationship of sex of patient with caregiver relation of caregiver with patient
| Relation of caregiver with patient | |||||
|---|---|---|---|---|---|
| Husband | Wife | Son | Daughter | Others | |
| Sex of patient | |||||
| Male (%) | NA | 48 (63) | 20 (26) | 2 (3) | 6 (8) |
| Female (%) | 5 (28) | NA | 11 (62) | 1 (5) | 1 (5) |
NA=Not available
We have used “CQOLC” scale to capture the psychosocial impact of the oral cancer on the primary caregiver of the patient. The questionnaire captured the psychosocial impact of the disease on the caregiver by identifying the burden of the disease on the caregiver, how it caused disruption in family, the positive adaptation of the caregiver, and lastly the financial concern of the family for carrying out the treatment, the distribution of which is shown in Table 4. We found the mean score for burden of the disease to be 60.0 ± 20.2. The mean score for disruption was 50.4 ± 21.7 and that for positive adaptation was 61.4 ± 20.7. The mean for the financial concern score was found to be the highest (78.4 ± 21.5). The similar findings are further illustrated in the box plot in Figure 2. Table 5 shows the correlation between the scores of the burden of disease, disruption in family, the positive adaptation of the caregiver, and lastly the financial concern of the family.
Table 4.
Calculated scores of Caregiver Quality of Life Index - Cancer for caregivers of the oral cancer patients (n=94)
| Scales | Mean±SD | Median (IQR) | Range |
|---|---|---|---|
| Burden score | 60.0±20.2 | 57.1 (44.62-75.0) | 14.3-100.0 |
| Disruption score | 50.4±21.7 | 50.0 (33.3-58.3) | 0.0-100.0 |
| Positive adaptation score | 61.4±20.7 | 62.5 (50.0-75.0) | 0.0-100.0 |
| Financial concern score | 78.4±21.5 | 87.5 (68.7-100.0) | 12.5-100.0 |
SD=Standard deviation, IQR=Interquartile range
Figure 2.
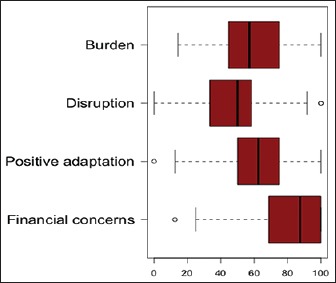
Boxplot showing the Caregiver Quality of Life Index – Cancer questionnaire scores
Table 5.
Correlation between the different caregivers scores (Caregiver Quality of Life Index - Cancer)
| CAPD | CADD | CASS | CAFC | |
|---|---|---|---|---|
| CAPD | 1.00 | |||
| CADD | 0.60 | 1.00 | ||
| CASS | 0.26 | 1.00 | ||
| CAFC | 0.26 | 0.26 | 0.06 | 1.00 |
CAPD=Caregivers’ psychological distress score, CAFC=Caregivers’ financial concern score, CASS=Caregivers’ social support score, CADD=Caregivers’ disruption on daily basis score
The caregiver's score was calculated from the scores for burden of the disease on caregiver, disruption in family, positive adaptation of caregiver, and lastly financial concern. To see the relationship between different characteristics of the caregivers and caregiver scores, we developed a model of multiple linear regressions, where we have included sex of caregiver, occupation, relationship with the patient, socioeconomic status, time since diagnosis, time since completion of treatment, stage of disease, presence of cut down of important expenses for carrying out cancer treatment, type of family, stage of oral cancer, and treatment given to the patients as independent variables. The final model of the multiple linear regression is shown in Table 6, which shows cut down of important family expenses was included in the model and was significantly related (P < 0.05) to the caregiver's score.
Table 6.
Multivariate analysis for caregivers’ score
| β | SE | t | P | |
|---|---|---|---|---|
| Intercept | 55.2 | 1.8 | 26.7 | <2e-16*** |
| Cut down of family expenses | 7.1 | 3.1 | 2.3 | 0.02* |
β=Unstandardized regression coefficient, SE=Standard error, Residual SE=12.0, SE=Standard error, Multiple R2=0.07, Adjusted R2=0.06, F statistics=−5.1, P < 0.05, *=Statistically significant, ***=Statistically highly significant
The duration of illness since the time of diagnosis of oral cancer was on an average 15 months till the interview was taken. But on IDIs, it was found that majority of the patients had a number of symptoms related to oral cancer for near about a year, prior to their histopathological diagnosis. And during the time being, they went on consulting one physician to another and many of them has also reported to have undergone indigenous treatment.
Discussion
In our study on psychosocial impact of oral cancer on caregivers of patients suffering with oral cancer, we found that caregivers were predominantly females and were the spouses of patients. Similar findings were also found in Brazilian study conducted by Rigoni et al.,[12] where 76.7% of the caregivers were women. This finding might influence the study results says Röing et al.[13] who felt that wives’ affective relationship make patients more susceptible to emotional adjustment. Pinquart and Sörensen[14] in their meta-analysis on the correlates of physical health of informal caregivers found that females or wives were more often socialized to be caregivers and more prepared than the males for the role of caregiving, making them less viable to the negative impacts of caregiving. While in another meta-analysis, Pinquart and Sörensen[14] found that spouses reported to have worse physical health and were more prone to physical decline due to age factor as compared to the grown-up children as caregivers. However, Ross et al.[15] claim that the caregiver's gender was not associated significantly with psychosocial well-being of the caregiver.
In this study, we found that caregivers of the oral cancer patients suffer from a high burden of caretaking with an equally increased score for disruption of family as a result of taking care of the ill family member. Still, they adapted to the change of their daily routine and lifestyle with a positive adaptation. Rigoni et al.[12] found that a significant number of caregivers suffer from mental stress, agony, anxiety, and depression than the general population. From the IDIs, we could find similar observations in our study. Apart from all these, financial instability was found to be another reason for increased psychosocial impact on the family while trying to meet the expenses for treating oral cancer.
At present, the National Program for Prevention and Control of Cancer, Diabetes, CVD and Stroke[16] has a component on cancer prevention and management, but it is solely concerned on the patients alone and no program is yet launched which incorporates the caregivers as well.
Conclusion
Caregivers are usually invisible to the health-care team. It is the high time that their contribution in cancer management should be recognized and their mental and physical well-being should also be given due attention.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Fauci A, Kasper D, Braunwald E, Hauser S, Longo D, Jameson J, et al. Harrison's principles of internal medicine. J Chem Inf Modeling. 2008;19:1–2958. [Google Scholar]
- 2.American Cancer Society. Global Cancer Facts & Figures. American Cancer Society. American Cancer Society. 2015. [Last assessed on 2017 Dec 20]. pp. 1–57. Available from: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/global-cancer-facts-and-figures/global-cancer-facts-and-figures-3rd-edition.pdf .
- 3.Fitzmaurice C, Dicker D, Pain A, Hamavid H, Moradi-Lakeh M, et al. Global Burden of Disease Cancer Collaboration. The global burden of cancer 2013. JAMA Oncol. 2015;1:505–27. doi: 10.1001/jamaoncol.2015.0735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park K. Park's Textbook of Preventive and Social Medicine. 23rd ed. Jabalpur: Bhanot Publications; 2015. pp. 381–90. [Google Scholar]
- 5.National Cancer Registry Program. Three Year Report of Population Based Cancer Registries: 2012-2014. Bangalore: National Cancer Registry Program; 2014. [Google Scholar]
- 6.Gangane N. Sewagram, Wardha: MGIMS; 2011. [Last accessed on 2017 Dec 07]. Population Based Cancer Registry 2010-2011. Available from: http://www.ncrpindia.org/ALL_NCRP_REPORTS/PBCR_REPORT_2009_2011/ALL_CONTENT/ALL_PDF/Wardha.pdf . [Google Scholar]
- 7.Blanchard CG, Albrecht TL, Ruckdeschel JC. The crisis of cancer: Psychological impact on family caregivers. Oncology (Williston Park) 1997;11:189–94. [PubMed] [Google Scholar]
- 8.Northouse LL, Peters-Golden H. Cancer and the family: Strategies to assist spouses. Semin Oncol Nurs. 1993;9:74–82. doi: 10.1016/s0749-2081(05)80102-0. [DOI] [PubMed] [Google Scholar]
- 9.Weitzner MA, Jacobsen PB, Wagner H, Jr, Friedland J, Cox C. The caregiver quality of life index-cancer (CQOLC) scale: Development and validation of an instrument to measure quality of life of the family caregiver of patients with cancer. Qual Life Res. 1999;8:55–63. doi: 10.1023/a:1026407010614. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. [Last accessed on 2017 Nov 12];Epi Info. 2016 6:1–11. Available from: https://www.cdc.gov/epiinfo/index.html . [Google Scholar]
- 11.Team RC. AVienna, Austria: 2013. [Last accesed on 2017 Dec 23]. The R Project for Statistical Computing; pp. 1–12. Available from: http://www.r-project.org/ [Google Scholar]
- 12.Rigoni L, Bruhn RF, De Cicco R, Kanda JL, Matos LL. Quality of life impairment in patients with head and neck cancer and their caregivers: A comparative study. Braz J Otorhinolaryngol. 2016;82:680–6. doi: 10.1016/j.bjorl.2015.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Röing M, Hirsch JM, Holmström I. Living in a state of suspension – A phenomenological approach to the spouse's experience of oral cancer. Scand J Caring Sci. 2008;22:40–7. doi: 10.1111/j.1471-6712.2007.00525.x. [DOI] [PubMed] [Google Scholar]
- 14.Pinquart M, Sörensen S. Correlates of physical health of informal caregivers: A meta-analysis. J Gerontol B Psychol Sci Soc Sci. 2007;62:P126–37. doi: 10.1093/geronb/62.2.p126. [DOI] [PubMed] [Google Scholar]
- 15.Ross S, Mosher CE, Ronis-Tobin V, Hermele S, Ostroff JS. Psychosocial adjustment of family caregivers of head and neck cancer survivors. Support Care Cancer. 2010;18:171–8. doi: 10.1007/s00520-009-0641-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Directorate General of Health Services, Ministry of Health and Family Welfare. Government of India. National Program for Prevention and Control of Cancer, Diabetes, CVD and Stroke. [Last accessed on 2018 Jan 05]. Available from: http://www.dghs.gov.in/content/1363_3_NationalProgrammePreventionControl.aspx .


