Abstract
Introduction:
Retinoblastoma (RB) is a prototype of heritable cancers. It is more common in the lower socioeconomic strata. Delayed presentation significantly reduces the overall outcome. We have analyzed the epidemiological and clinical data of children who were diagnosed with RB between the years 2009 and 2014.
Aim:
RB being a disease of the poor, delayed presentation is common due to lack of awareness. We have analyzed the epidemiological profile of our patients and tried to establish the link between delayed presentation and the presence of high-risk features. High-risk features are associated with higher chance of metastasis and poor rates of vision salvage in RB.
Methodology:
Data were collected in a retrospective manner from the patient case files retrieved from the Medical Records Department, Kidwai cancer Institute. The data were analyzed using Excel and SPSS software (IBM Corp. released 2016, IBM SPSS statistics software for Mac OS, version 24, IBM Corp., Armonk, NY).
Results:
A total of 53 patients were diagnosed with RB in the years 2009–2014. There was a male predominance with 1.2:1 incidence. Bilateral RB was present in 21 cases. The mean age of children with bilateral RB was 2.1 years, against 1.5 years in unilateral cases. High-risk features such as optic nerve invasion, choroidal invasion, intracranial extension, and orbital involvement were found in 12, 6, 5, and 5 eyes, respectively. Bone marrow involvement was detected in 5% and lung metastasis in 2%. Intracranial involvement was found in 10.4% and cerebrospinal fluid positivity in 15%. Children with high-risk features had a significant delay in presentation in comparison to those without high-risk features (P = 0.035).
Conclusion:
Incidence of metastatic disease and delayed presentation is still high in developing countries. Routine eye examination during vaccination visits can ensure early diagnosis and appropriate referral in many of these children.
Keywords: Delayed presentation, high-risk features, metastasis
Introduction
Retinoblastoma (RB) is a prototype of inheritable cancers. It is the most common primary intraocular tumor in the pediatric age group.[1] It has been found to affect the lower socioeconomic strata more frequently, which also appears to have an implication on the stage at presentation of the disease. According to various studies, RB could metastasize within 6 months of onset of symptoms, if left untreated.[2] Therefore, delay in diagnosis may result in poorer outcome. We have analyzed the clinicopathological profile of children diagnosed with RB in our institute, primarily to understand the epidemiology and also to study the relationship between advanced disease and delayed presentation. The early detection would improve patient outcomes significantly and in familial cases may help detection in the contralateral eye earlier, aiding vision salvage. We thereby wish to propose a screening strategy for all children, during routine pediatrician visits.
Methodology
All the patients who were registered in the Pediatric Oncology Department, Kidwai Cancer Institute with the diagnosis of RB, between the years 2009 and 2014, were included in the study retrospectively. Diagnosis of RB was confirmed clinically and by imaging. Computed tomography (CT) scan or magnetic resonance imaging (MRI) was performed based on availability. A routine bone marrow examination and cerebrospinal fluid (CSF) analysis were performed in all these children. Chest X-ray and bone scan were also done as a part of metastatic workup.
Results
A total of 53 patients (with 21 bilateral cases, 73 eyes in total) were diagnosed with RB between 2009 and 2014. There was a male predominance (1.2:1) in the study group [Figure 1]. Bilateral RB was detected in 21 cases. The most common presenting symptom was a white reflex, seen in 43 eyes (58%). Proptosis with orbital mass was seen in 10 eyes (13.5%). Paralytic squint was seen in 7 eyes (9.5%). Two of our children presented with features of raised intracranial pressure and one of them succumbed to status epilepticus. Hemocoria with hyphema was seen in one patient. There was no family history of intraocular malignancy in any of our children; however, consanguineous marriage was found in 10/53 families. Sixteen percent (n = 12) of our children had been delivered at home, but none of them had a history of perinatal complications or oxygen requirement. All the patients were referred to us from ophthalmologists, and the diagnosis at referral was RB. Although there had been delay in presentation to a medical facility in several cases, all of the patients were diagnosed initially to have RB. The mean duration from onset of symptoms to presentation was 3 months (range 1–5 months). High-risk features such as optic nerve invasion, choroidal invasion, intracranial extension, and orbital involvement were found in 12, 6, 5, and 5 eyes, respectively [Figure 2]. Although MRI is the investigation of choice to detect the high-risk features, CT scan was more feasible and accessible at our center. Optic nerve involvement was picked up in CT scan in 7/12 patients (58.3%). Pathological review of surgical specimens however showed the involvement of the cut end in 2 children, in whom CT scan had missed the optic nerve invasion. In 3 children in whom MRI could be performed, imaging provided additional information regarding optic nerve involvement and choroidal breech, which was not evident on an initial CT of the orbit. Bone scan, bone marrow examination, CSF analysis, and chest X-ray were done as a part of metastatic workup. Bone marrow involvement was detected in 3/53 (5%) and lung metastasis in 1/53 (2%). Intracranial involvement was found in 5/53 (10.4%), and CSF showed malignant cells in 8/53 (15%). Eighteen patients were referred postsurgery, and 11 were started on neoadjuvant chemotherapy at another center followed by enucleation. Most of the children presented with advanced disease. We identified that those children with high-risk features (28/53) had a significant delay in presentation in comparison to those without high-risk features, as represented in Table 1 (P = 0.035). Out of the patients that took treatment in our institute, only 39.6% completed the scheduled therapy. Therefore, outcome analysis could not be performed. Twenty-four patients refused treatment following diagnosis and prognostication based on severity of disease. Twenty-nine patients agreed for chemotherapy, of which 8 had irregular follow-up and did not complete therapy.
Figure 1.
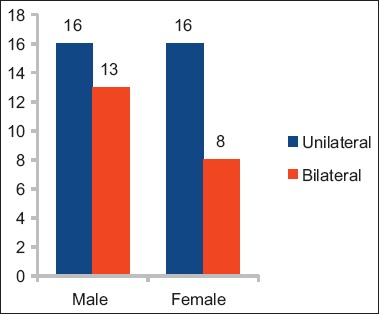
Gender and laterality
Figure 2.
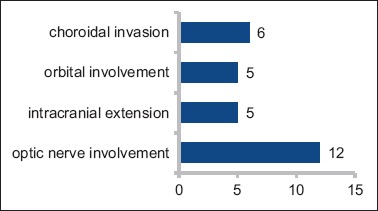
High-risk features in retinoblastoma
Table 1.
Delayed presentation versus advanced disease
| High risk feature | No. of cases | Mean duration of illness (months) |
|---|---|---|
| Yes | 23 | 1.8 P=0.035 |
| No | 30 | 2.53 |
Discussion
RB is a prototype of heritable cancers and is the most common intraocular tumor in the pediatric age group. Most of these tumors are sporadic and unilateral in up to 60% of the cases. The remaining 40% are inherited, with bilateral presentation seen in 25% of the cases.[3] The median age at diagnosis is 18 months, an average of 12 months for children with bilateral disease and 24 months for children with unilateral disease.[4] Approximately 95% of children with RB present before the age of five.[4] Our group had a male predominance with a male: female ratio of 1.2:1. Bilateral disease was found in 39%. Although it is well known that bilateral tumors tend to present early, in our group, there was a difference.[5] The mean age of children with bilateral RB was 25 months, against 18 months in unilateral cases. The median duration of illness was 3 months (range 1–5 months). The two-hit hypothesis comes to play in RB with an autosomal-dominant inheritance pattern.[1] While it is ideal to detect RB early, it is unfortunate that a significant proportion of patients present with advanced disease. As RB is commonly seen in the lower socioeconomic strata in our country, lack of awareness is one of the main reasons why parents do not seek medical assistance early. Unsatisfactory visual prognostication and therapy-related complications lead to refusal of treatment. In our group of patients, only 54.7% agreed for treatment and only 39.6% completed the scheduled therapy. The most common presenting features was leukocoria, followed by mass protruding from the eye and strabismus. Vision loss was observed in 46.2%. This is in concurrence with the other major study from AIIMS, India.[6] The tumor was intraocular in 41.6% and extraocular in 58.4% cases. Most common site of metastasis in our group was to the central nervous system. This is in contrast to most studies that indicate bone to be the most common site of metastasis in RB. However, central nervous system was the most common site of metastasis in the above mentioned study from India, which is in concurrence with our data as well.6 The average age of children with metastasis was 32 months. This was much higher than the average age in unilateral cases, indicating delayed presentation probably resulted in metastatic disease in these children. Any child presenting with new-onset strabismus should be evaluated for possibility of an underlying RB.[7] Several viruses have also been implicated in the etiopathogenesis such as human papillomavirus, simian virus, and adenovirus. A study from our own institute had shown positive correlation between HPV infection in the mother and development of RB in the child.[8]
Several prognostic factors have been defined in RB. Choroidal invasion, optic nerve involvement, orbital extension, and intracranial extension are well-known risk factors. Choroidal invasion alone has not shown any significant decrease in outcome, but when combined with the rest, it significantly lowers the survival in patients with RB.[9] In our children, 54.7% had presented with the above risk features. This is slightly higher than some case series that quote an incidence of high-risk features in RB to be 40%–50%.[10] In 15% of the children, more than one risk feature were observed. These high-risk features are a concern mainly because they are associated with high incidence of extraocular relapse and low chances of recovering vision. Multimodality treatment with chemotherapy, surgery, and radiotherapy are needed for adequate disease control. Chemotherapy if administered alone has inadequate central nervous system penetration and therefore can result in extraocular relapse.[10]
We would like to emphasize that children with a white reflex must be screened at the earliest for underlying RB. Considering that it is the most common symptom and is likely to be picked up even in a photograph, it is important to sensitize the general pediatricians to routinely screen the children during vaccination visits. Early detection can aid better survival and improve visual prognosis in these children. Twelve out of the 53 children's parents had noticed a white reflex in photographs several months before presentation. However, due to lack of awareness, this was not given medical attention despite the fact that these children had regular vaccination visits to their local health facility.
Conclusion
RB is curable in 90% cases in the developed countries, while the cure rate continues to be far lesser in developing countries. The prevalence of metastatic disease with delayed presentation is still high in lower middle-income countries like ours, which remains the main culprit for poorer outcome in RB.[11] With mobile phone cameras being widely accessible, creating awareness about the white reflex and routine basic eye examination during the vaccination visits are essential for identifying disease at an early stage. Aggressive multimodality treatment can aid adequate disease control and vision salvage.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Pandey AN. Retinoblastoma: An overview. Saudi J Ophthalmol. 2014;28:310–5. doi: 10.1016/j.sjopt.2013.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang P, Li YJ, Zhang SB, Cheng QL, Zhang Q, He LS. Metastatic retinoblastoma of the parotid and submandibular glands: A rare case report. BMC Ophthalmol. 2017;17:229. doi: 10.1186/s12886-017-0627-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Naik AS, Jyothi S, Shah PK. Retinoblastoma: A comprehensive review. Kerala J Ophthalmol. 2016;28:164–70. [Google Scholar]
- 4.Shifa JZ, Gezmu AM. Presenting signs of retinoblastoma at a tertiary level teaching hospital in Ethiopia. Pan Afr Med J. 2017;28:66. doi: 10.11604/pamj.2017.28.66.11199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saiju R, Duwal S. Bilateral retinoblastoma in early infancy. Nepal J Ophthalmol. 2013;5:124–8. doi: 10.3126/nepjoph.v5i1.7840. [DOI] [PubMed] [Google Scholar]
- 6.Chawla B, Hasan F, Azad R, Seth R, Upadhyay AD, Pathy S, et al. Clinical presentation and survival of retinoblastoma in Indian children. Br J Ophthalmol. 2016;100:172–8. doi: 10.1136/bjophthalmol-2015-306672. [DOI] [PubMed] [Google Scholar]
- 7.Goddard AG, Kingston JE, Hungerford JL. Delay in diagnosis of retinoblastoma: Risk factors and treatment outcome. Br J Ophthalmol. 1999;83:1320–3. doi: 10.1136/bjo.83.12.1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bhuvaneswari A, Pallavi VR, Jayshree RS, Kumar RV. Maternal transmission of human papillomavirus in retinoblastoma: A possible route of transfer. Indian J Med Paediatr Oncol. 2012;33:210–5. doi: 10.4103/0971-5851.107080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shields CL, Shields JA, Baez KA, Cater J, De Potter PV. Choroidal invasion of retinoblastoma: Metastatic potential and clinical risk factors. Br J Ophthalmol. 1993;77:544–8. doi: 10.1136/bjo.77.9.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Seema R, Parul S, Nita K, Kamlesh High-risk histomorphological features in retinoblastoma and their association with p53 expression: An Indian experience. Indian J Ophthalmol. 2014;62:1069–71. doi: 10.4103/0301-4738.146747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Faranoush M, Hedayati Asl AA, Mehrvar A, Mehrvar N, Zangooei R, Abadi E, et al. Consequences of delayed diagnosis in treatment of retinoblastoma. Iran J Pediatr. 2014;24:381–6. [PMC free article] [PubMed] [Google Scholar]


