Abstract
Background
Two major determinants of cardiovascular disease (CVD) are a sedentary lifestyle and stress. Qigong involves physical exercise, mind regulation and breathing control to restore the flow of Qi (a pivotal life energy). As it is thought to help reduce stress and involves exercise, qigong may be an effective strategy for the primary prevention of CVD.
Objectives
To determine the effectiveness of qigong for the primary prevention of CVD.
Search methods
We searched the following electronic databases: the Cochrane Central Register of Controlled Trials (CENTRAL) (November 2014, Issue 10 of 12); MEDLINE (Ovid) (1946 to 2014 October week 4); EMBASE Classic + EMBASE (Ovid) (1947 to 2014 November 4); Web of Science Core Collection (1970 to 31 October 2014); Database of Abstracts of Reviews of Effects (DARE), Health Technology Assessment Database and Health Economics Evaluations Database (November 2014, Issue 4 of 4). We searched several Asian databases (inception to July 2013) and the Allied and Complementary Medicine Database (AMED) (inception to December 2013), as well as trial registers and reference lists of reviews and articles; we also approached experts in the field and applied no language restrictions in our search.
Selection criteria
Randomised controlled trials lasting at least three months involving healthy adults or those at high risk of CVD. Trials examined any type of qigong, and comparison groups provided no intervention or minimal intervention. Outcomes of interest included clinical CVD events and major CVD risk factors. We did not include trials that involved multi‐factorial lifestyle interventions or weight loss.
Data collection and analysis
Two review authors independently selected trials for inclusion. Two review authors extracted data from included studies and assessed the risk of bias.
Main results
We identified 11 completed trials (1369 participants) and one ongoing trial. Trials were heterogeneous in participants recruited, qigong duration and length of follow‐up periods. We were unable to ascertain the risk of bias in nine trials published in Chinese, as insufficient methodological details were reported and we were unable to contact the study authors to clarify this.
We performed no meta‐analyses, as trials were small and were at significant risk of bias. Clinical events were detailed in subsequent reports of two trials when statistically significant effects of qigong were seen for all‐cause mortality, stroke mortality and stroke incidence at 20 to 30 years after completion of the trials. However, these trials were designed to examine outcomes in the short term, and it is not clear whether qigong was practised during extended periods of follow‐up; therefore effects cannot be attributed to the intervention. None of the included studies reported other non‐fatal CVD events.
Six trials provided data that could be used to examine the effects of qigong on blood pressure. Reductions in systolic blood pressure (SBP) and diastolic blood pressure (DBP) were seen in three and two trials, respectively. Three trials examined the effects of qigong on blood lipids when favourable effects were seen in one trial for total cholesterol, low‐density lipoprotein (LDL) cholesterol and triglycerides, and two trials showed favourable effects on high‐density lipoprotein (HDL) cholesterol. The only trial considered at low risk of selection and detection bias did not demonstrate statistically significant effects on CVD risk factors with qigong, but this study was small and was underpowered. None of the included studies reported incidence of type 2 diabetes (T2D), adverse events, quality of life or costs.
Authors' conclusions
Currently, very limited evidence is available on the effectiveness of qigong for the primary prevention of CVD. Most of the trials included in this review are likely to be at high risk of bias, so we have very low confidence in the validity of the results. Publication of the ongoing trial will add to the limited evidence base, but further trials of high methodological quality with sufficient sample size and follow‐up are needed to be incorporated in an update of this review before the effectiveness of qigong for CVD prevention can be established.
Plain language summary
Qigong to prevent cardiovascular disease
Review question
This review assessed the effectiveness of qigong interventions for reducing cardiovascular events and cardiovascular risk factors among healthy adults and those at high risk of cardiovascular disease.
Background
Cardiovascular disease is a global health burden. However, by changing several modifiable behaviours, such as by increasing exercise levels and by promoting relaxation to reduce stress, it is thought that cardiovascular risk can be reduced. Qigong originated in China and involves physical exercise, mind regulation and breathing control to restore Qi (the life energy force that flows around the body). Qigong might reduce stress and increase exercise levels.
Study characteristics
The evidence is current to November 2014. We included trials with interventions lasting at least three months.
Results and conclusion
We found 11 completed trials (1369 participants). These trials showed variation in participants recruited, duration of qigong and follow‐up of the interventions. For two trials that were followed up for many years after trial completion, results showed that qigong had a beneficial effect on all‐cause mortality, stroke mortality and stroke incidence, but it is not clear whether this effect can be attributed to qigong, as it is uncertain whether qigong was practised during the years after the trials ended. Some beneficial effects of qigong on blood pressure and blood lipid levels were observed, but these results were based on only a small number of studies with small sample size that were at significant risk of bias. Therefore, additional large, high‐quality, long‐term trials are needed before we will be able to determine whether qigong is beneficial for the prevention of cardiovascular disease.
Background
Description of the condition
Cardiovascular disease (CVD) consists of a variety of conditions that affect the heart and blood vessels. These conditions are the number one cause of death and disability worldwide and were responsible for 17.3 million global deaths in 2008; in 2010, CVD accounted for 35% of total deaths in the USA and the UK, 38% in China (WHO 2011a).
Development of strategies to prevent CVD has become a public health priority, especially because the prevalence and burden of CVD are increasing worldwide (WHO 2011a). Such strategies focus on modifiable lifestyle factors such as diet, smoking habits, exercise and stress. Clinical treatments are effective in preventing and treating CVD, but other strategies involving a healthy lifestyle and stress management have also been shown to be beneficial (Frishman 2005). One potentially beneficial strategy that involves both stress management and exercise is qigong.
Description of the intervention
Qigong was developed in China several thousand years ago and is a meditative practice used in health promotion. The three main components of qigong are mind regulation, body regulation and breath regulation (Chow 2012); qigong uses gentle, focused exercises for the body and mind to increase and restore the flow of Qi (a pivotal life energy), with the aim of encouraging and accelerating the body's ability to heal itself (Lee 2009). This flow of Qi is thought to be vital for optimal vitality and physical and emotional health (Chow 2012). Many styles of qigong are known. These include Baduanjin, which is a low‐level aerobic exercise characterised by eight fine delicate movements, stretching and controlled breathing (Chyu 2011); Guolin, which is a slow walking exercise with slight twisting waist movements and arm movements (Jones 2001); and Dantian, which is characterised by a focus on breathing exercises, slow controlled movements and meditation (von Trott 2009). The therapeutic effects of qigong vary according to style (Chow 2012). Furthermore, each style of qigong falls under one of two distinct forms: internal or external qigong. Internal qigong is self directed and is performed without the aid of a teacher or therapist. It involves meditation, breathing, focused attention and movement to achieve optimal health (Ernst 2008; Lee 2007). External qigong, on the other hand, involves qigong practitioners who will direct their Qi energy into the patient to cure disease or alleviate symptoms (Ernst 2008; Lee 2007).
Interest in complementary therapies, such as qigong, for prevention of disease and maintenance of health is growing (Kraft 2009). Moreover, complementary therapies that involve exercise are increasingly popular in the elderly, and therefore may be an important strategy for the primary and secondary prevention of CVD. Qigong is practiced by 60 million people each day in China (Chow 2012) and is one of the most often recommended exercises for patients with coronary artery disease (Davis 2009). Various studies have shown qigong to be effective for reducing blood pressure (Davis 2009; Nahas 2008), triglyceride levels and fasting cholesterol (Innes 2008; Lee 2004) and to have a beneficial effect on type 2 diabetes (Xin 2007). Data also suggest that qigong may be beneficial in decreasing levels of perceived stress (Lee 2003a; Skoglund 2007), which are a determinant of CVD (WHO 2011b). Qigong has been shown to reduce catecholamine and cortisol levels in response to stressors compared with placebo (Guo 1996).
How the intervention might work
As with tai chi and yoga, qigong incorporates exercise and stress reduction, both of which are important in the prevention of CVD. An abundance of research suggests that exercise is important in preventing diabetes and CVD (Bassuk 2005; Mittal 2008; Press 2003). The exact mechanisms for this are unknown; however, potential mechanisms include enhancing insulin sensitivity and fibrinolytic and endothelial function, improving glycaemic control, reducing hypertension, regulating body weight, decreasing insulin resistance and reducing atherogenic dyslipidaemia and inflammation (Bassuk 2005).
Qigong provides an additional benefit in that it has been found to help reduce stress (Bronas 2009), which is also a determinant of CVD. Again, the exact mechanisms by which qigong does this are unknown, but some suggest that qigong reduces sympathetic stimulation, which lowers levels of catecholamines and stress hormones circulating in the body (Bronas 2009; Guo 1996).
Why it is important to do this review
To date, few randomised controlled trials (RCTs) have investigated the effectiveness of qigong for CVD prevention, and fewer systematic reviews have explored this topic. One systematic review of interest looked at the effectiveness of qigong for hypertension, and found that regular qigong practise helped to lower blood pressure in those with hypertension (Lee 2007). This was similar to the findings of Guo 2008, which indicated that internal qigong was effective in decreasing blood pressure among those with essential hypertension when compared with no‐treatment controls, but was not as effective as drug controls or conventional exercise controls. One other systematic review examined the effectiveness of qigong for type 2 diabetes; however, review authors found that information was insufficient to show whether qigong was effective for this population (Lee 2009).
None of the above systematic reviews directly focus on CVD prevention and CVD risk factors (Guo 2008; Lee 2007; Lee 2009). Therefore, a comprehensive systematic review is needed to thoroughly examine interventions involving qigong in healthy adults or those at increased risk of CVD to determine the effectiveness of qigong for the primary prevention of CVD.
Objectives
To determine the effectiveness of qigong for the primary prevention of CVD.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials.
Types of participants
Healthy adults aged 18 years and older from the general population and those at high risk for CVD. We excluded those who had experienced previous myocardial infarction (MI), stroke or a revascularisation procedure (coronary artery bypass grafting (CABG) or percutaneous transluminal coronary angioplasty (PTCA)); those with angina; and those with angiographically defined coronary heart disease (CHD), as the review focused on the primary prevention of CVD.
Types of interventions
Trials investigated any style of qigong (internal or external).
We did not include multi‐factorial lifestyle intervention trials in this review to avoid confounding. Furthermore, we focused on follow‐up periods of three months or longer, as these are the most relevant for public health interventions.
Trials were considered only when the comparison group was given no intervention or minimal intervention (e.g. leaflets promoting physical activity, other more general forms of health promotion, but no face‐to‐face interaction).
Types of outcome measures
Primary outcomes
Cardiovascular mortality.
All‐cause mortality.
Non‐fatal endpoints such as MI, CABG, PTCA, angina, angiographically defined CHD, stroke, carotid endarterectomy or peripheral arterial disease (PAD).
Secondary outcomes
Changes in blood pressure (systolic and diastolic blood pressure) and blood lipids (total cholesterol, high‐density lipid (HDL) cholesterol, low‐density lipid (LDL) cholesterol, triglycerides).
Occurrence of type 2 diabetes as a major CVD risk factor.
Health‐related quality of life.
Adverse effects.
Costs.
Search methods for identification of studies
Electronic searches
We searched the following electronic databases.
Cochrane Central Register of Controlled Trials (CENTRAL) (November 2014, Issue 10 of 12).
MEDLINE (Ovid) (1946 to 2014 November week 4).
EMBASE Classic + EMBASE (Ovid) (1947 to 4 November 2014).
Web of Science Core Collection (Thomson Reuters) (1970 to 31 October 2014).
Database of Abstracts of Reviews of Effects (DARE), Health Technology Assessment Database and Health Economics Evaluations Database (November 2014, Issue 4 of 4).
Allied and Complementary Medicine Database (AMED) (inception to 3 December 2013).
We used medical subject headings (MeSH) or equivalent text word terms. We designed searches in accordance with Cochrane Heart Group methods and guidance and tailored them to individual databases. The search strategies are shown in Appendix 1. We applied a search filter for RCTs to the MEDLINE search and adapted it for use in EMBASE and the Web of Science (Higgins 2011).
We applied no language restrictions.
Searching other resources
In addition, we checked the reference lists of reviews and retrieved articles to look for additional studies.
We searched the metaRegister of controlled trials (mRCT) (www.controlled‐trials.com/mrct), Clinicaltrials.gov (www.clinicaltrials.gov) and the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (http://apps.who.int/trialsearch/) for ongoing trials (search date: 5 December 2014). We also searched OpenGrey for grey literature (http://www.opengrey.eu/) and the following Asian Databases ‐ China National Knowledge Infrastructure (CNKI) ( www.cnki.net/), Wangfang (http://www.wanfangdata.com/) and VIP (http://lib.cqvip.com/) ‐ from their inception to July 2013.
We contacted experts in the field to ask about unpublished and ongoing trials, and we communicated with study authors when necessary to request additional information.
Data collection and analysis
Selection of studies
Two review authors (LH, NF or KR) reviewed the title and abstract of each paper and retrieved potentially relevant references. We then obtained the full text of potentially relevant studies, and two review authors (from LH, NF, DT, MSL or KR) independently selected studies to be included in the review by using predetermined inclusion criteria. In all cases, we resolved disagreements about study inclusion by consensus.
Data extraction and management
One review author (MSL) independently extracted data using a pre‐standardised data extraction form for studies written in Chinese, which was checked by a second review author (JSWK). Two review authors (LH, KR) extracted data from English language papers. We contacted chief investigators to request additional relevant information if necessary. We extracted from each included study details of study design, participant characteristics, study setting, intervention and outcome data (including details of outcome assessment, adverse effects and methodological quality (randomisation, blinding and attrition)).
Assessment of risk of bias in included studies
We assessed risk of bias by examining random sequence generation and allocation concealment, descriptions of drop‐outs and withdrawals (including analysis by intention‐to‐treat), blinding (participants, personnel and outcome assessment) and selective outcome reporting in each trial, as per the guidance provided in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We rated each domain as having low risk of bias, high risk of bias or unclear risk of bias.
Measures of treatment effect
We processed data in accordance with recommendations of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We expressed dichotomous outcomes as risk ratios (RRs) with 95% confidence intervals (CIs) calculated for each study. For continuous outcomes, we compared net changes (i.e. intervention group minus control group differences) and calculated a weighted mean difference (WMD) and 95% CIs for each study.
Assessment of heterogeneity
For each outcome, we conducted tests of heterogeneity (using the Chi2 test of heterogeneity and the I2 statistic). When no heterogeneity was noted, we performed a fixed‐effect meta‐analysis. If substantial heterogeneity (I2 > 50%) was detected, review authors looked for possible explanations for this (e.g. participants, intervention). If heterogeneity could not be explained, review authors considered the following options: providing a narrative overview without aggregating the studies at all, or using a random‐effects model with appropriate cautious interpretation.
Subgroup analysis and investigation of heterogeneity
It was our intention to stratify results according to baseline risk, age and gender, type of qigong and time and duration of qigong, but trials provided insufficient data for performance of these analyses.
Sensitivity analysis
We intended to carry out sensitivity analysis by excluding studies with high risk of bias. Similarly, we planned to examine the effects of publication bias by using funnel plots and tests of asymmetry (Egger 1997). However, identified studies that met the inclusion criteria were too few for us to perform these analyses.
Results
Description of studies
Results of the search
The electronic searches generated 662 hits after de‐duplication. Screening of titles and abstracts revealed 89 papers that could go forward for formal inclusion and exclusion. Of these, 12 RCTs met the inclusion criteria ‐ 11 completed trials and one ongoing trial. The study flow diagram is presented in Figure 1.
1.
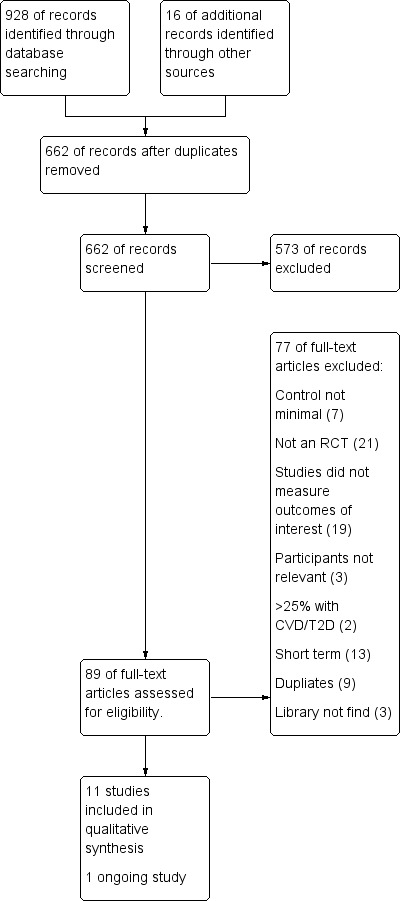
Study flow diagram.
Included studies
We have provided details of the included studies in the Characteristics of included studies table: 11 completed trials with 1369 participants randomly assigned and one ongoing trial met the inclusion criteria. Four trials recruited only male participants (Kuang 1979; Kuang 1987a; Wang 1989; Wang 1991), and five studies recruited male and female participants (Chow 2012; Li 1989; Li 1993; Li 2014; Miao 2009). The remaining two studies did not state the gender of participants (Kuang 1986; Kuang 1987). The health status of participants also varied between studies: Two studies recruited healthy participants (Chow 2012; Li 2014), one study recruited elderly people with high blood lipids (Miao 2009) and eight studies recruited hypertensive patients (Kuang 1979; Kuang 1987a; Wang 1991; Kuang 1986; Kuang 1987; Li 1989; Li 1993; Wang 1989). All 11 trials were conducted in China.
Follow‐up periods also differed among included studies ‐ from 12 weeks (Chow 2012) to 16 weeks (Li 2014) to 18 weeks (Miao 2009) to six months (Li 1993) to one year (Kuang 1987a; Wang 1989) to two years (Li 1989) to four years (Kuang 1979). Three studies reported very long‐term follow‐up (20 to 30 years), but trials were originally designed for and reported on follow‐up between six and 12 months (Kuang 1986; Kuang 1987; Wang 1991).
Duration and type of qigong varied among the 11 included studies. In four studies, qigong was practised for 20 to 30 minutes once or twice per day (Kuang 1987a; Li 1989; Wang 1989; Wang 1991); in another study, qigong was practised for 40 minutes once or twice per day (Kuang 1979). In three studies, qigong was practised for up to one hour once per week (Li 1993), at least three times per week (Li 2014) or five to seven times per week (Miao 2009). In the remaining three studies, the duration of qigong was not stated (Chow 2012; Kuang 1986; Kuang 1987). Nine of the 11 included studies did not state which type of qigong was used; in two studies, Baduanjin qigong was used (Li 2014; Miao 2009).
We identified one ongoing trial (Zheng 2014) through the search (see Characteristics of ongoing studies). This trial is recruiting community elders (aged 50 to 70 years) at high risk of ischaemic stroke and will randomly allocate to Baduanjin exercise for 12 weeks or usual physical activity. Follow‐up will be provided at 13 weeks and at 25 weeks, and outcomes of interest to the current review include cerebrovascular outcomes and lipid levels.
Excluded studies
We have provided in the Characteristics of excluded studies table details and reasons for exclusion of studies that most closely missed the inclusion criteria. Reasons for exclusion for most of the studies included no relevant outcomes reported, control that was not minimal, no intervention and lack of randomised controlled trial design. Some studies were short term and provided less than three months' follow‐up (see Figure 1).
Risk of bias in included studies
We have presented details for each of the 11 completed included trials in the risk of bias tables in the Characteristics of included studies table, and we have presented summaries in Figure 2 and Figure 3. In only two trials were we able to establish risk of bias. Nine trials reported in Chinese provided no information on most risk of bias domains, and we were unable to contact the original authors to verify these details.
2.
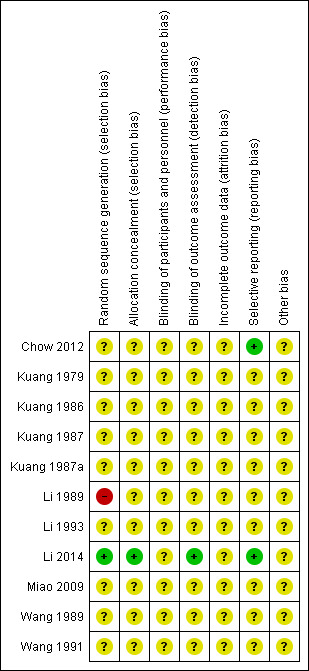
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
3.
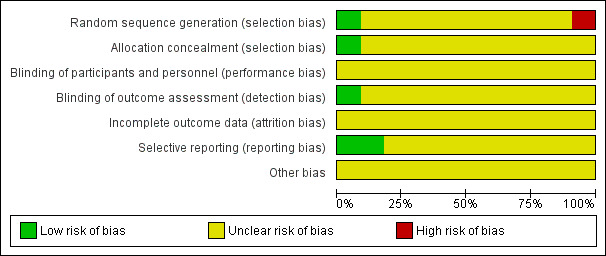
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
Methods of random sequence generation were unclear in nine of the 11 completed included studies. In one study, methods of random sequence generation were stated and were judged to be at high risk of bias, as randomisation was conducted by order of admission to the study (Li 1989), and in another these methods were deemed to be at low risk of bias (Li 2014). Methods of allocation concealment were unclear in ten of the 11 completed included studies. In the remaining study, allocation was conducted by a research assistant who was not involved in recruitment to ensure allocation concealment; this was regarded as having low risk of bias (Li 2014).
Blinding
Blinding of participants and personnel was unclear in all 11 completed included studies. However, it is difficult if not impossible to blind participants and personnel to behavioural interventions. Blinding of outcome assessors was also unclear in ten of the 11 included studies. In one study, the research assistant who collected and entered study data remained blinded to group allocation throughout the study, and this was regarded as low risk of bias (Li 2014).
Incomplete outcome data
In all 11 completed included studies, reporting of incomplete outcome data was judged as unclear, as insufficient information was provided on which a judgement could be based.
Selective reporting
Selective reporting was judged as unclear in nine of the 11 completed included studies, as available information was insufficient for a judgement to be made. The remaining two studies were considered at low risk of bias, as all outcomes listed were reported (Chow 2012; Li 2014).
Other potential sources of bias
For all included studies, information was insufficient for review authors to judge risk of bias from other potential sources.
Effects of interventions
Clinical events
Mortality
Two of the 11 completed included studies examined all‐cause mortality and mortality from stroke after 20 to 30 years of follow‐up (Kuang 1986; Wang 1991), but these trials were originally designed to look for outcomes at six months to one year, and it is unclear whether qigong was continued as practised during the 20‐ to 30‐year period, or if randomisation was preserved. Furthermore, these trials could not be assessed for risk of bias; therefore pooled estimates of treatment effect are not provided, as any pooled estimate would be at high risk of being spurious. In both trials, qigong significantly lowered all‐cause mortality (Analysis 1.1) (risk ratio (RR) 0.54, 95% confidence interval (CI) 0.33 to 0.90, 204 participants (Kuang 1986); RR 0.56, 95% CI 0.39 to 0.79, 306 participants (Wang 1991)) and stroke mortality (Analysis 1.2) (RR 0.50, 95% CI 0.26 to 0.95, 204 participants (Kuang 1986); RR 0.49, 95% CI 0.31 to 0.78, 306 participants (Wang 1991)). Results from individual trials should be treated with extreme caution for the reasons outlined above.
1.1. Analysis.
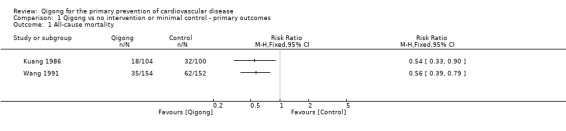
Comparison 1 Qigong vs no intervention or minimal control ‐ primary outcomes, Outcome 1 All‐cause mortality.
1.2. Analysis.
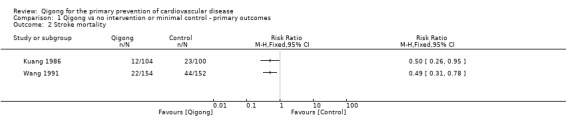
Comparison 1 Qigong vs no intervention or minimal control ‐ primary outcomes, Outcome 2 Stroke mortality.
Stroke incidence
One of the 11 completed included studies examined stroke incidence (Wang 1991). In this study (306 participants), qigong was found to significantly reduce the incidence of stroke (RR 0.56, 95% CI 0.38 to 0.83) after 25 to 30 years of follow‐up. However, as noted above, this result may not be attributable to the intervention and should be treated with extreme caution; the trial was designed to look only at outcomes at one year, and it is unclear whether qigong continued as practised during this length of follow‐up, or if randomisation was preserved.
None of the 11 completed included trials reported other non‐fatal cardiovascular events such as MI, CABG, PTCA, angina, angiographically defined CHD, carotid endarterectomy or PAD.
Cardiovascular risk factors
Blood pressure
Nine of the 11 completed included studies measured blood pressure (Chow 2012; Kuang 1979; Kuang 1986; Kuang 1987; Kuang 1987a; Li 1989; Li 1993; Li 2014; Wang 1991). Useable data were not available for three studies (Kuang 1986; Li 1989; Wang 1991). For the remaining studies, we did not perform a meta‐analysis, as risk of bias could not be rigourously assessed in four of the six trials, trials were subject to small study bias (Sterne 2000) and heterogeneity between trials was significant (I2 > 50%).
For systolic blood pressure (SBP), effect sizes for individual trials are shown in Analysis 2.1. Three of five trials showed extremely large effects and statistically significant reductions in SBP with qigong. The only study that was regarded as having low risk of both selection and detection bias showed the smallest effect, which did not reach statistical significance (mean difference ‐ 2.6 mmHg, 95% CI ‐0.58 to 3.38); however, this study was designed as a pilot study and was likely underpowered (36 participants randomly assigned) (Li 2014).
2.1. Analysis.
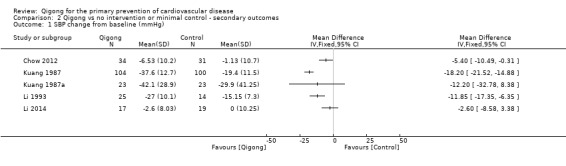
Comparison 2 Qigong vs no intervention or minimal control ‐ secondary outcomes, Outcome 1 SBP change from baseline (mmHg).
For diastolic blood pressure (DBP), effect sizes for individual trials are shown in Analysis 2.2. Two of five trials showed statistically significant reductions in DBP with qigong. The only study that was regarded as having low risk of selection and detection bias showed a reduction in DBP with qigong, but this finding did not reach formal statistical significance (mean difference ‐ 4.45 mmHg, 95% CI ‐ 9.64 to 0.74); as noted above, this was a pilot trial (Li 2014).
2.2. Analysis.
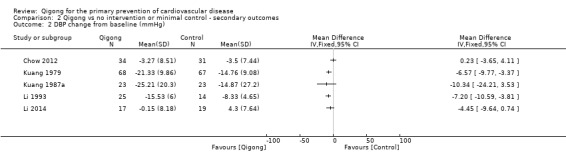
Comparison 2 Qigong vs no intervention or minimal control ‐ secondary outcomes, Outcome 2 DBP change from baseline (mmHg).
Lipid levels
Three trials reported data on lipid levels (Li 2014; Miao 2009; Wang 1989). As outlined above, we did not perform meta‐analyses, as for two of the three trials, we were unable to assess risk of bias, trials were subject to small study effects and heterogeneity was significant.
For total cholesterol, effect sizes for individual trials are shown in Analysis 2.3. One trial showed a statistically significant reduction in total cholesterol with qigong (Miao 2009), and the remaining two showed non‐statistically significant reductions with qigong (Li 2014; Wang 1989). A similar pattern was seen for LDL cholesterol and triglycerides (Analysis 2.4; Analysis 2.6). HDL cholesterol was significantly increased with qigong in two trials (Miao 2009; Wang 1989), but no evidence showed effects of the intervention in the remaining trial (Li 2014) (Analysis 2.5). As above for the blood pressure analyses, only one trial was regarded as having low risk of selection and detection bias, and no statistically significant effects were seen for this study, although it was designed as a pilot study, so numbers were small and analyses were likely underpowered (Li 2014).
2.3. Analysis.
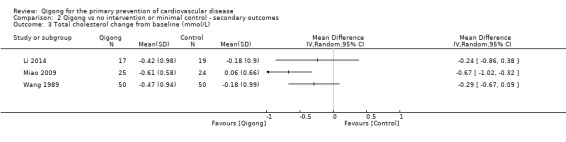
Comparison 2 Qigong vs no intervention or minimal control ‐ secondary outcomes, Outcome 3 Total cholesterol change from baseline (mmol/L).
2.4. Analysis.
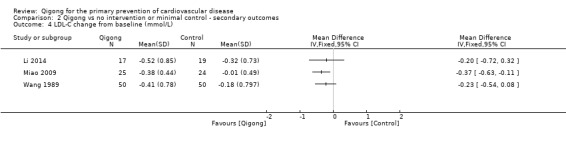
Comparison 2 Qigong vs no intervention or minimal control ‐ secondary outcomes, Outcome 4 LDL‐C change from baseline (mmol/L).
2.6. Analysis.
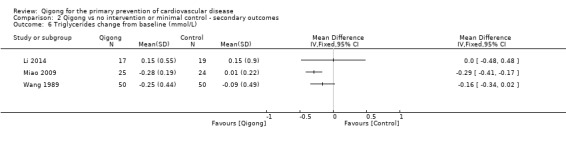
Comparison 2 Qigong vs no intervention or minimal control ‐ secondary outcomes, Outcome 6 Triglycerides change from baseline (mmol/L).
2.5. Analysis.
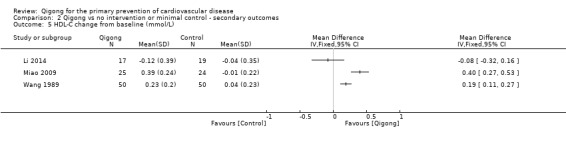
Comparison 2 Qigong vs no intervention or minimal control ‐ secondary outcomes, Outcome 5 HDL‐C change from baseline (mmol/L).
Incidence of type 2 diabetes (T2D)
None of the included trials reported the incidence of T2D.
Adverse events
None of the included studies provided information on adverse events.
Quality of life
None of the included studies reported quality of life outcomes.
Costs
None of the included studies provided data on costs.
Discussion
Summary of main results
Eleven completed trials (1369 participants randomly assigned) of at least three months' duration and one ongoing trial met the inclusion criteria for this review.
Trials were heterogeneous in terms of participants recruited, types of qigong, duration of the intervention and length of follow‐up. We were unable to ascertain risk of bias in most of the trials published in Chinese, as this was not reported in the source papers, and we were unable to contact study authors to clarify methodological details. Trials were small and were at risk of small study bias, leading to overestimation of treatment effects (Sterne 2000). Results for all outcomes therefore were not pooled statistically, and results from individual trials should be interpreted extremely cautiously for trials likely to be at high risk of bias.
Clinical events were reported in subsequent reports of two trials in which statistically significant effects of qigong were seen for all‐cause mortality, stroke mortality and stroke incidence at 20 to 30 years after completion of the trials. However, these trials were designed to examine outcomes in the short term, and it is not clear whether qigong was practised during extended periods of follow‐up, or if randomisation was preserved; therefore effects cannot be attributed to the intervention. None of the included studies reported other non‐fatal cardiovascular disease (CVD) events.
Six trials provided data that could be used to examine the effects of qigong on blood pressure. Reductions in systolic blood pressure (SBP) and diastolic blood pressure (DBP) were seen in three and two trials, respectively. Implausible large reductions in SBP were reported in three trials (‐11.85 mmHg, ‐12.20 mmHg, ‐18.20 mmHg) ‐ much higher than those observed for combined pharmacological therapy for blood pressure control. We were unable to ascertain risk of bias for these studies, and the large effects are likely due to poor methodological rigour and the fact that studies were relatively small, and small studies have been associated with exaggerated effects (Sterne 2000). Three trials examined the effects of qigong on blood lipids; favourable effects were seen in one trial for total cholesterol, low‐density lipoprotein (LDL) cholesterol and triglycerides, and two trials showed favourable effects on high‐density lipoprotein (HDL) cholesterol. The only trial considered at low risk of selection and detection bias did not demonstrate statistically significant effects on CVD risk factors with qigong, but this study was small and was underpowered. None of the included studies reported incidence of type 2 diabetes (T2D), adverse events, quality of life or costs.
Overall completeness and applicability of evidence
This review included male and female adults who were at varying levels of CVD risk. Most studies recruited participants with hypertension. All trials were conducted in China, so the effectiveness of qigong in other cultures and populations has not been studied to date.
We were unable to assess risk of bias in most included studies because of poor reporting, and we were unable to contact study authors to clarify details. Methodological limitations of the included studies prevented us from determining the effects of qigong on clinical events or on CVD risk factors.
We intended to explore reported heterogeneity in the interventions if sufficient numbers of studies of sufficient methodological quality were identified.
Quality of the evidence
Overall, the trials included in this review were at significant risk of bias; therefore the results of individual trials should be treated with extreme caution.
We were unable to ascertain risk of bias for most domains in nine trials, despite attempts to contact study authors to clarify methodological details. One of the nine trials was at high risk of bias for random sequence generation, as study authors used admission sequence (Li 1989), remaining domains were unclear and all domains in the remaining eight trials were unclear.
Two trials provided some details for assessment of methodological quality (Chow 2012; Li 2014). Both were at low risk of bias for reporting, as all outcomes listed were reported. Only one trial was at low risk of bias for selection and detection bias (Li 2014). This trial was limited by sample size, as it was designed as a pilot study (Li 2014).
We were unable to examine the effects of publication bias in funnel plots because the review included only a limited number of trials. Most of the included trials were relatively small, and small trials are often carried out less rigourously, are more likely to be carried out in selected populations and have been found to have larger beneficial effects compared with larger trials (Nüesch 2010; Sterne 2000; Sterne 2001). This should also be taken into account when the results are interpreted.
Potential biases in the review process
We conducted a comprehensive search across major databases, including those from Asia, for interventions involving qigong. We also screened the reference lists of systematic reviews and contacted study authors when necessary. In addition, two review authors independently screened trials and conducted inclusion and exclusion processes. Two people independently extracted data from trials written in English, and one review author extracted data from trials written in Chinese; data were checked by another native speaker.
The decision to restrict this review only to interventions involving qigong avoided the potential confounding effects of other behavioural interventions on outcomes examined and limited the number of trials eligible for inclusion. Moreover, the small number of trials included in this review, limitations in methodological rigour and unclear risk of bias in most trials mean that the findings of this current review are very limited.
Agreements and disagreements with other studies or reviews
As the current review reports limited findings, it is difficult to compare it with other similar studies at this time.
Two systematic reviews have focused on the effects of qigong on blood pressure: One looked at the effects of qigong on hypertension (Lee 2007) and provided evidence to suggest that regular qigong practise lowered blood pressure. This finding is consistent with the systematic review conducted by Guo et al (Guo 2008), which indicated that internal qigong was effective in decreasing blood pressure among hypertensive patients.
In another systematic review, insufficient information was found to allow review authors to determine whether qigong was effective for type 2 diabetes (Lee 2009).
A more recent systematic review examined the effects of qigong on blood lipid levels (Mei 2012). This review found that Baduanjin exercise reduced total cholesterol, LDL cholesterol and triglycerides, and increased HDL cholesterol, but when compared with other exercise interventions, these effects were attenuated (Mei 2012).
Authors' conclusions
Implications for practice.
At present, limited trial evidence is available on qigong for the primary prevention of CVD. The trials included in this review were few for relevant outcomes and small in sample size and were at significant risk of bias; therefore we have very low confidence in the validity of the results. The clinical event data provided by two trials many years after completion of the trials as originally designed may not be attributable to the intervention, and so no firm conclusions can be drawn on the basis of their findings. Similarly, changes in CVD risk factors may be a consequence of poor trial conduct, so again, no firm conclusions can be drawn.
To establish whether qigong is an effective lifestyle intervention for prevention of CVD, additional trial evidence from methodologically rigourous, adequately powered, long‐term trials is needed; at this stage, no recommendations can be made about practice.
Implications for research.
Currently, very few RCTs have examined solely the effectiveness of qigong for the primary prevention of CVD. In particular, large, rigourously conducted RCTs with long follow‐up periods that investigated the effectiveness of qigong for prevention of major CVD events and CVD risk factors are insufficient. Evidence of the effectiveness of qigong in populations outside China is lacking, and no information is available on T2D incidence, quality of life, possible adverse effects and costs of the intervention.
Acknowledgements
We are grateful to Nicole Martin and Myeong Soo Lee for conducting the searches for this review.
Appendices
Appendix 1. Search strategies 2012
CENTRAL
#1 MeSH descriptor: [Cardiovascular Diseases] explode all trees #2 cardio* #3 cardia* #4 heart* #5 coronary* #6 angina* #7 ventric* #8 myocard* #9 pericard* #10 isch?em* #11 emboli* #12 arrhythmi* #13 thrombo* #14 atrial next fibrillat* #15 tachycardi* #16 endocardi* #17 (sick next sinus) #18 MeSH descriptor: [Stroke] explode all trees #19 (stroke or stokes) #20 cerebrovasc* #21 cerebral next vascular #22 apoplexy #23 (brain near/2 accident*) #24 ((brain* or cerebral or lacunar) near/2 infarct*) #25 MeSH descriptor: [Hypertension] explode all trees #26 hypertensi* #27 (peripheral next arter* next disease*) #28 ((high or increased or elevated) near/2 blood pressure) #29 MeSH descriptor: [Hyperlipidemias] explode all trees #30 hyperlipid* #31 hyperlip?emia* #32 hypercholesterol* #33 hypercholester?emia* #34 hyperlipoprotein?emia* #35 hypertriglycerid?emia* #36 MeSH descriptor: [Arteriosclerosis] explode all trees #37 MeSH descriptor: [Cholesterol] explode all trees #38 cholesterol #39 "coronary risk factor*" #40 MeSH descriptor: [Blood Pressure] this term only #41 "blood pressure" #42 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 or #31 or #32 or #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40 or #41 #43 MeSH descriptor: [Breathing Exercises] this term only #44 Qigong #45 Qi‐gong #46 qi next gong #47 Chi next chung #48 Chi next gong #49 Chi next Kung #50 Qi next Kung #51 Jhi next gong #52 Chi next gung #53 Qi next chung #54 ch?i next kung #55 kung next ch?i #56 #43 or #44 or #45 or #46 or #47 or #48 or #49 or #50 or #51 or #52 or #53 or #54 or #55 #57 #42 and #56
MEDLINE Ovid
1. exp Cardiovascular Diseases/ 2. cardio*.tw. 3. cardia*.tw. 4. heart*.tw. 5. coronary*.tw. 6. angina*.tw. 7. ventric*.tw. 8. myocard*.tw. 9. pericard*.tw. 10. isch?em*.tw. 11. emboli*.tw. 12. arrhythmi*.tw. 13. thrombo*.tw. 14. atrial fibrillat*.tw. 15. tachycardi*.tw. 16. endocardi*.tw. 17. (sick adj sinus).tw. 18. exp Stroke/ 19. (stroke or stokes).tw. 20. cerebrovasc*.tw. 21. cerebral vascular.tw. 22. apoplexy.tw. 23. (brain adj2 accident*).tw. 24. ((brain* or cerebral or lacunar) adj2 infarct*).tw. 25. exp Hypertension/ 26. hypertensi*.tw. 27. peripheral arter* disease*.tw. 28. ((high or increased or elevated) adj2 blood pressure).tw. 29. exp Hyperlipidemias/ 30. hyperlipid*.tw. 31. hyperlip?emia*.tw. 32. hypercholesterol*.tw. 33. hypercholester?emia*.tw. 34. hyperlipoprotein?emia*.tw. 35. hypertriglycerid?emia*.tw. 36. exp Arteriosclerosis/ 37. exp Cholesterol/ 38. cholesterol.tw. 39. "coronary risk factor* ".tw. 40. Blood Pressure/ 41. blood pressure.tw. 42. or/1‐41 43. Breathing Exercises/ 44. Qigong.tw. 45. (Qi‐gong or qi gong).tw. 46. (Chi chung or Chi gong or Chi Kung).tw. 47. (Qi Kung or Jhi gong or Chi gung or Qi chung).tw. 48. (ch'i kung or kung ch'i).tw. 49. or/43‐48 50. randomized controlled trial.pt. 51. controlled clinical trial.pt. 52. randomized.ab. 53. placebo.ab. 54. drug therapy.fs. 55. randomly.ab. 56. trial.ab. 57. groups.ab. 58. 50 or 51 or 52 or 53 or 54 or 55 or 56 or 57 59. exp animals/ not humans.sh. 60. 58 not 59 61. 42 and 49 and 60
EMBASE Ovid
1. exp cardiovascular disease/ 2. cardio*.tw. 3. cardia*.tw. 4. heart*.tw. 5. coronary*.tw. 6. angina*.tw. 7. ventric*.tw. 8. myocard*.tw. 9. pericard*.tw. 10. isch?em*.tw. 11. emboli*.tw. 12. arrhythmi*.tw. 13. thrombo*.tw. 14. atrial fibrillat*.tw. 15. tachycardi*.tw. 16. endocardi*.tw. 17. (sick adj sinus).tw. 18. exp cerebrovascular disease/ 19. (stroke or stokes).tw. 20. cerebrovasc*.tw. 21. cerebral vascular.tw. 22. apoplexy.tw. 23. (brain adj2 accident*).tw. 24. ((brain* or cerebral or lacunar) adj2 infarct*).tw. 25. exp hypertension/ 26. hypertensi*.tw. 27. peripheral arter* disease*.tw. 28. ((high or increased or elevated) adj2 blood pressure).tw. 29. exp hyperlipidemia/ 30. hyperlipid*.tw. 31. hyperlip?emia*.tw. 32. hypercholesterol*.tw. 33. hypercholester?emia*.tw. 34. hyperlipoprotein?emia*.tw. 35. hypertriglycerid?emia*.tw. 36. exp Arteriosclerosis/ 37. exp Cholesterol/ 38. cholesterol.tw. 39. "coronary risk factor*".tw. 40. Blood Pressure/ 41. blood pressure.tw. 42. or/1‐41 43. breathing exercise/ 44. Qigong.tw. 45. qi gong.tw. 46. Qi‐gong.tw. 47. Qi Kung.tw. 48. Jhi gong.tw. 49. Chi gung.tw. 50. Qi chung.tw. 51. ch'i kung.tw. 52. kung ch'i.tw. 53. or/43‐52 54. 42 and 53 55. random$.tw. 56. factorial$.tw. 57. crossover$.tw. 58. cross over$.tw. 59. cross‐over$.tw. 60. placebo$.tw. 61. (doubl$ adj blind$).tw. 62. (singl$ adj blind$).tw. 63. assign$.tw. 64. allocat$.tw. 65. volunteer$.tw. 66. crossover procedure/ 67. double blind procedure/ 68. randomized controlled trial/ 69. single blind procedure/ 70. 55 or 56 or 57 or 58 or 59 or 60 or 61 or 62 or 63 or 64 or 65 or 66 or 67 or 68 or 69 71. (animal/ or nonhuman/) not human/ 72. 70 not 71 73. 54 and 72 74. limit 73 to embase
Web of Science
#17 #16 AND #15 #16 TS=((random* or blind* or allocat* or assign* or trial* or placebo* or crossover* or cross‐over*)) #15 #14 AND #9 #14 #13 OR #12 OR #11 OR #10 #13 TS=("Jhi gong" or "Chi gung" or "Qi chung" or "ch?i kung" or "kung ch?i") #12 TS=("Chi chung" or "Chi gong" or "Chi Kung" or "Qi Kung") #11 TS=(Qigong or Qi‐gong or "qi gong") #10 TS=(breath* NEAR/2 exercis*) #9 #8 OR #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1 #8 TS=(arteriosclerosis or cholesterol or "coronary risk factor*" or "blood pressure") #7 TS=(hyperlipid* or hyperlip?emia* or hypercholesterol* or hypercholester?emia* or hyperlipoprotein?emia* or hypertriglycerid?emia*) #6 TS=(high near/2 "blood pressure" or increased near/2 "blood pressure" or elevated near/2 "blood pressure") #5 TS=(brain* near/2 infarct or cerebral near/2 infarct or lacunar near/2 infarct* or hypertensi* or "peripheral arter* disease*") #4 TS=("cerebral vascular" or apoplexy or brain near/2 accident*) #3 TS=("atrial fibrillat*" or tachycardi* or endocardi* or "sick sinus" or stroke or stokes or cerebrovasc*) #2 TS=(myocard* or pericard* or isch?em* or emboli* or arrhythmi* or thrombo*) #1 TS=(cardio* or cardia* or heart* or coronary* or angina* or ventric*)
CNKI
1. 气功 2. qigong 3. qi gong 4. 1 OR 2 OR 3 5. 心血管疾病 6. 冠心病 7. 高血压 8. 高血脂 9. 心绞痛 10. 心肌梗死 11. 心律失常 12. 心力衰竭 13. 心肌缺血 14. 动脉粥样硬化 15. 冠状动脉疾病 16. 中风 17. 脑卒中 18. 脑梗死 19. Cardiovascular Diseases 20. Coronary 21. Hypertension 22. High blood pressure 23. Hyperlipidemia 24. Angina 25. Myocardial infarction 26. Arrhythmia 27. Heart failure 28. Cardiac failure 29. Myocardial ischemia 30. Atherosclerosis 31. Coronary artery disease 32. Stroke 33. Apoplexy 34. Cerebral stroke 35. Cerebral infarction 36. OR/5‐33 37. 随机 38. 对照 39. random 40. 37 and 38 or 39 41. 4 and 36 and 40
Wangfang
1. 气功 2. qigong 3. qi gong 4. 1 OR 2 OR 3 5. 心血管疾病 6. 冠心病 7. 高血压 8. 高血脂 9. 心绞痛 10. 心肌梗死 11. 心律失常 12. 心力衰竭 13. 心肌缺血 14. 动脉粥样硬化 15. 冠状动脉疾病 16. 中风 17. 脑卒中 18. 脑梗死 19. Cardiovascular Diseases 20. Coronary 21. Hypertension 22. High blood pressure 23. Hyperlipidemia 24. Angina 25. Myocardial infarction 26. Arrhythmia 27. Heart failure 28. Cardiac failure 29. Myocardial ischemia 30. Atherosclerosis 31. Coronary artery disease 32. Stroke 33. Apoplexy 34. Cerebral stroke 35. Cerebral infarction 36. OR/5‐33 37. 随机 38. 对照 39. random 40. 37 and 38 or 39 41. 4 and 36 and 40
VIP
1. 气功 2. qigong 3. qi gong 4. 1 OR 2 OR 3 5. 心血管疾病 6. 冠心病 7. 高血压 8. 高血脂 9. 心绞痛 10. 心肌梗死 11. 心律失常 12. 心力衰竭 13. 心肌缺血 14. 动脉粥样硬化 15. 冠状动脉疾病 16. 中风 17. 脑卒中 18. 脑梗死 19. Cardiovascular Diseases 20. Coronary 21. Hypertension 22. High blood pressure 23. Hyperlipidemia 24. Angina 25. Myocardial infarction 26. Arrhythmia 27. Heart failure 28. Cardiac failure 29. Myocardial ischemia 30. Atherosclerosis 31. Coronary artery disease 32. Stroke 33. Apoplexy 34. Cerebral stroke 35. Cerebral infarction 36. OR/5‐33 37. 随机 38. 对照 39. random 40. 37 and 38 or 39 41. 4 and 36 and 40
Clinicaltrials.gov
1. Cardio* 2. qigong 3. qi gong
WHO ICTRP
1. Cardio* 2. qigong 3. qi gong
ISRCTN Register
1. Cardio* 2. qigong 3. qi gong
AMED
1. cardio*.tw. 2. cardia*.tw. 3. heart*.tw. 4. coronary*.tw. 5. angina*.tw. 6. ventric*.tw. 7. myocard*.tw. 8. pericard*.tw. 9. isch?em*.tw. 10. emboli*.tw. 11. arrhythmi*.tw. 12. thrombo*.tw. 13. atrial fibrillat*.tw. 14. tachycardi*.tw. 15. endocardi*.tw. 16. (sick adj sinus).tw. 17. exp Stroke/ 18. (stroke or stokes).tw. 19. cerebrovasc*.tw. 20. cerebral vascular.tw. 21. apoplexy.tw. 22. (brain adj2 accident*).tw. 23. ((brain* or cerebral or lacunar) adj2 infarct*).tw. 24. exp Hypertension/ 25. hypertensi*.tw. 26. peripheral arter* disease*.tw. 27. ((high or increased or elevated) adj2 blood pressure).tw. 28. exp Hyperlipidemias/ 29. hyperlipid*.tw. 30. hyperlip?emia*.tw. 31. hypercholesterol*.tw. 32. hypercholester?emia*.tw. 33. hyperlipoprotein?emia*.tw. 34. hypertriglycerid?emia*.tw. 35. exp Arteriosclerosis/ 36. exp Cholesterol/ 37. cholesterol.tw. 38. "coronary risk factor* ".tw. 39. Blood Pressure/ 40. blood pressure.tw. 41. or/1‐40 42. Breathing Exercises/ 43. Qigong.tw. 44. (Qi‐gong or qi gong).tw. 45. (Chi chung or Chi gong or Chi Kung).tw. 46. (Qi Kung or Jhi gong or Chi gung or Qi chung).tw. 47. (ch'i kung or kung ch'i).tw. 48. or/42‐47 49. randomized controlled trial.pt. 50. controlled clinical trial.pt. 51. randomized.ab. 52. placebo.ab. 53. randomly.ab. 54. trial.ab. 55. groups.ab. 56. 50 or 51 or 52 or 53 or 54 or 55 or 56 57. exp animals/ not humans.sh. 58. 56 not 57 59. 41 and 48 and 59
Data and analyses
Comparison 1. Qigong vs no intervention or minimal control ‐ primary outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 All‐cause mortality | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Stroke mortality | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Stroke Incidence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
1.3. Analysis.
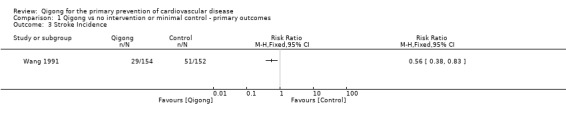
Comparison 1 Qigong vs no intervention or minimal control ‐ primary outcomes, Outcome 3 Stroke Incidence.
Comparison 2. Qigong vs no intervention or minimal control ‐ secondary outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 SBP change from baseline (mmHg) | 5 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 DBP change from baseline (mmHg) | 5 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Total cholesterol change from baseline (mmol/L) | 3 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4 LDL‐C change from baseline (mmol/L) | 3 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5 HDL‐C change from baseline (mmol/L) | 3 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6 Triglycerides change from baseline (mmol/L) | 3 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Chow 2012.
| Methods | RCT | |
| Participants | Healthy middle‐aged adults recruited by posters, leaflets and emails in April 2009 in Hong Kong. Inclusion criteria: 18 years or older, non‐smokers, physically healthy (i.e. not taking medication for chronic disease), able to partake in medium‐intensity exercise and demonstrating at least a mild degree of mood disturbance on the Depression Anxiety Stress Scales (DASS). Exclusion criteria: used psychiatric drugs within the previous 6 months, pregnant, chronic illness, have learned any type of mindful exercise (e.g. yoga, qigong) and have practised it regularly throughout the last year, regularly participate in other sports (e.g. swimming) 68 participants (45 women, 23 men) with a mean age of 44.2 years (standard deviation (SD) 11.03, range 21 to 64) were randomly assigned |
|
| Interventions | Intervention: The elementary syllabus of chan mi gong was restructured to integrate warm‐up and cool‐down elements. This approach was evaluated by a 7‐member expert panel. The intervention group learnt and practised the qigong protocol once a week for 8 weeks under supervision of the instructor, and then continued with 4 weeks of home practise. The intervention period was 12 weeks, and measurements were taken at baseline and at 12 weeks Control: wait list control. Participants were offered the intervention after 12 weeks |
|
| Outcomes | Blood pressure | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants first were matched by age and gender, and the pairs were randomly allocated to intervention or control. Method of randomisation was not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Per‐protocol analysis but small loss to follow‐up (4 of 68) |
| Selective reporting (reporting bias) | Low risk | All outcomes listed were reported |
| Other bias | Unclear risk | Information was insufficient for judgement |
Kuang 1979.
| Methods | RCT | |
| Participants | Patients aged 40 to 50 years with male essential hypertension patients were recruited from a hospital room. 135 participants were randomly assigned to 1 of 2 arms ‐ qigong and antihypertensive drugs or antihypertensive drugs only. 68 participants were randomly assigned to qigong, and 67 were randomly assigned to control or antihypertensive drugs only | |
| Interventions | Qigong group: Qigong was seen as a quiet mind, a relaxed body and smooth breathing. Exercises were done in a sitting position and occasionally while standing, with qigong practised for about 40 minutes once or twice a day. Participants were also given antihypertensive drugs (reserpine 0.125 mg, hydralazine 12.5 mg, hydrochlorothiazide 12.5 mg) Control group: antihypertensive drugs only (reserpine 0.125 mg, hydralazine 12.5 mg, hydrochlorothiazide 12.5 mg) (Changes in medication use during the trial ‐ if DBP was > 100, medication was doubled; if DBP was < 70, the dosage was reduced or suspended) Follow‐up: 4 years |
|
| Outcomes | Blood pressure | |
| Notes | Article was translated by MSL and was checked by JSWK | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Information was insufficient for judgement |
| Selective reporting (reporting bias) | Unclear risk | Information was insufficient for judgement |
| Other bias | Unclear risk | Information was insufficient for judgement |
Kuang 1986.
| Methods | RCT | |
| Participants | 204 participants with hypertension were randomly assigned to 1 of 2 arms ‐ qigong and antihypertensives or control with antihypertensive drugs only. 104 participants were randomly assigned to qigong plus antihypertensive drugs, and 100 were randomly assigned to control This study was published in China |
|
| Interventions | Qigong group: described as calming the mind and keeping the body loose and in static and dynamic combination. Participants were also given a small dose of an antihypertensive Control group: given a small dose of antihypertensives Follow‐up was originally 6 months but occurred again at 20 years |
|
| Outcomes | Blood pressure, CVD death and all‐cause mortality | |
| Notes | Article was translated by MSL and was checked by JSWK | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Information was insufficient for judgement |
| Selective reporting (reporting bias) | Unclear risk | Information was insufficient for judgement |
| Other bias | Unclear risk | Information was insufficient for judgement |
Kuang 1987.
| Methods | RCT | |
| Participants | Hypertensive patients were recruited, and 204 participants were randomly assigned to 1 of 2 arms ‐ qigong with antihypertensive drugs or antihypertensive drugs alone. 104 participants were randomly assigned to qigong, and 100 participants to control The country of publication was China |
|
| Interventions | Qigong group: practised qigong and received antihypertensive medication Control group: received antihypertensive medication only Follow‐up originally at one year but occurred again at 20 years |
|
| Outcomes | Blood pressure | |
| Notes | Article was translated by MSL and was checked by JSWK In the intervention group, 17% of participants were lost to follow‐up at 20 years; in the control group, 32% of participants were lost to follow‐up at 20 years |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Information was insufficient for judgement |
| Selective reporting (reporting bias) | Unclear risk | Information was insufficient for judgement |
| Other bias | Unclear risk | Information was insufficient for judgement |
Kuang 1987a.
| Methods | RCT | |
| Participants | 46 male essential hypertensives aged 40 to 60 years were randomly assigned to 1 of 2 arms ‐ qigong or control Inclusion criteria: DBP 100 to 120 mmHg 23 participants were randomly assigned to qigong, and 23 to control The country of publication was China |
|
| Interventions | Qigong group: developed by institute of researchers on principles of a quiet mind, a relaxed body and smooth breathing. Exercises were done in a sitting position and occasionally while standing for 20 to 30 minutes twice a day. Also given antihypertensive drugs on a regular basis Control group: given only antihypertensive drugs on a regular basis Follow‐up: 1 year |
|
| Outcomes | Blood pressure | |
| Notes | Article was translated by MSL and was checked by JSWK | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Information was insufficient for judgement |
| Selective reporting (reporting bias) | Unclear risk | Information was insufficient for judgement |
| Other bias | Unclear risk | Information was insufficient for judgement |
Li 1989.
| Methods | RCT | |
| Participants | 107 male and female patients with hypertension (mean age: qigong and antihypertension medication 57.65 ± 8.81, control 55.06 ± 10.79) were recruited from a hospital; participants were randomly assigned to 1 of 3 arms ‐ qigong, qigong plus antihypertension medication or antihypertension medication only. 42 participants were randomly assigned to qigong plus antihypertension medication, and 33 to control The country of publication was China |
|
| Interventions | Qigong plus antihypertension medication group: relaxation of the body, mind meditation and use of qigong breathing habits and principles. Qigong was practised for 30 minutes twice a day for 8 weeks. Participants also received antihypertension tablets (hydrochlorothiazide 12.5 mg to be taken twice per day and propranolol 5 mg to be taken 3 times per day) Control group: antihypertension medication only (hydrochlorothiazide 12.5 mg to be taken twice per day and propranolol 5 mg to be taken 3 times per day) Follow‐up: 2 years |
|
| Outcomes | Blood pressure | |
| Notes | Article was translated by MSL and was checked by JSWK | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Participants were randomly assigned by order of admission to the study |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Information was insufficient for judgement |
| Selective reporting (reporting bias) | Unclear risk | Information was insufficient for judgement |
| Other bias | Unclear risk | Information was insufficient for judgement |
Li 1993.
| Methods | RCT | |
| Participants | Male and female patients with hypertension (mean age: qigong 59.12 ± 6.77, control 58.21 ± 8.51) were recruited from a hospital room. 39 participants were randomly assigned to 1 of 2 arms ‐ qigong or control Inclusion criteria: patients with hypertension, with no lung, liver or thyroid disease, no diabetes and no primary renal disease 25 participants were randomly assigned to the qigong group, and 14 to the control group The country of publication was China |
|
| Interventions | Qigong group: calm relaxing movement with hypertension basic stance. Qigong was practised for 1 hour every Wednesday morning for 6 months. Participants were also given a compound of antihypertension tablets. 1 or 2 of these were to be taken 3 times a day for 6 months Control group: given a compound of antihypertension drugs with 1 or 2 tablets taken 3 times a day for 6 months Follow‐up: 6 months |
|
| Outcomes | Blood pressure | |
| Notes | Article was translated by MSL and was checked by JSWK | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Information was insufficient for judgement |
| Selective reporting (reporting bias) | Unclear risk | Information was insufficient for judgement |
| Other bias | Unclear risk | Information was insufficient for judgement |
Li 2014.
| Methods | RCT | |
| Participants | Between October 2012 and February 2013, local residents aged 20 to 59 years were recruited from the area around Wuhan Sports University, China. Participants were physically healthy with no CVD or glucose abnormalities or other acute or chronic disease that would affect physical activity. Participants did not currently partake in moderate‐intensity physical activity. 110 participants were randomly assigned (36 men and 74 women with a mean age of 34.2 years (SD 14.6)) | |
| Interventions | Intervention: Participants in the intervention group undertook learning of the Baduanjin exercise 2 weeks before the intervention period under the guidance of a professional coach. These participants practised Baduanjin exercise 3 or more times each week for 30 to 60 minutes. They were required to complete the programme together at the intervention site, and personnel recorded attendance and provided guidance The whole set of Baduanjin exercises consists of 9 postures: (1) ready position, (2) holding hands high with palms up to regulate the internal organs, (3) posing like an archer shooting on left and right sides, (4) holding 1 arm aloft to regulate functions of the spleen and stomach, (5) looking backwards to prevent sickness and strain, (6) swinging the head and lowering the body to relieve stress, (7) moving the hands down the back and legs and touching the feet to strengthen the kidneys, (8) thrusting the fists and making the eyes glare to enhance strength and (9) raising and lowering the heels to cure disease Control: Participants in the control group were asked to not take part in exercise classes or regular physical activity during the study period and were told to maintain their original lifestyle. After the 16‐week intervention period, all participants in the control group received 2 weeks of Baduanjin exercise training under the guidance of a professional coach |
|
| Outcomes | Blood pressure and lipid levels | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was performed by computer‐generated random allocation sequence with simple randomisation |
| Allocation concealment (selection bias) | Low risk | Randomisation was undertaken by a research assistant who was not involved in recruitment to ensure allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Research assistant who collected and entered study data remained blinded to group allocation throughout the study |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 84% completion rate in the intervention group, 100% in the control group |
| Selective reporting (reporting bias) | Low risk | All outcomes listed were reported |
| Other bias | Unclear risk | Information was insufficient for judgement |
Miao 2009.
| Methods | RCT | |
| Participants | Elderly men and women with high blood lipids were recruited. 50 participants were randomly assigned to 1 of 2 arms ‐ qigong or no treatment Inclusion criteria: no clinical diagnosis of endocrine disease and family history, did not participate in regular exercise and were not taking lipid‐lowering drugs. 25 participants were randomly assigned to qigong, and 25 to control of no treatment The study was published in China |
|
| Interventions | Qigong group: 50 to 60 minutes of Baduanjin qigong 5 to 7 times per week for 18 months Control group: no treatment Follow‐up: 18 weeks |
|
| Outcomes | Lipid levels | |
| Notes | Article was translated by MSL and was checked by JSWK | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Information was insufficient for judgement |
| Selective reporting (reporting bias) | Unclear risk | Information was insufficient for judgement |
| Other bias | Unclear risk | Information was insufficient for judgement |
Wang 1989.
| Methods | RCT | |
| Participants | Male patients with essential hypertension were recruited from a hospital, and 100 participants were randomly assigned to 1 of 2 arms ‐ qigong or antihypertensive drugs only Inclusion criteria: no adverse reactions to food 50 participants were randomly assigned to qigong, and 50 to control This study was published in China |
|
| Interventions | Qigong group: calm relaxing movements with hypertension basic stance. Qigong was practised for 20 to 30 minutes once or twice a day for 1 year. Participants were also given antihypertensive medication Control group: given antihypertensive medication with no qigong therapy Follow‐up: 1 year |
|
| Outcomes | Lipid levels | |
| Notes | Article was translated by MSL and was checked by JSWK | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Information was insufficient for judgement |
| Selective reporting (reporting bias) | Unclear risk | Information was insufficient for judgement |
| Other bias | Unclear risk | Information was insufficient for judgement |
Wang 1991.
| Methods | RCT | |
| Participants | Male patients with essential hypertension (mean age: qigong 47.57 ± 5.60, control 47.31 ± 6.01) were recruited from a hospital. 306 participants were randomly assigned to 1 of 2 arms ‐ qigong or control. 154 participants were randomly assigned to qigong and 152 to control Ths study was published in China |
|
| Interventions | Qigong group: described as calming the mind and keeping the body loose. Also static and dynamic combination of hypertension method in sitting position. Qigong was practised for 20 to 30 minutes once or twice a day. These participants were also given antihypertensive medication Control group: were given antihypertensive medication only Follow‐up: 25 to 30 years |
|
| Outcomes | Blood pressure, stroke incidence, all‐cause mortality and stroke death | |
| Notes | Article was translated by MSL and was checked by JSWK | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Information was insufficient for judgement |
| Selective reporting (reporting bias) | Unclear risk | Information was insufficient for judgement |
| Other bias | Unclear risk | Information was insufficient for judgement |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Du 1992 | Study did not measure outcomes of interest |
| Lee 2003 | Short term (2 days) |
| Liu 2006 | Control was not minimal |
| Liu 2010 | Not an RCT |
| Oh 2008 | Study did not measure outcomes of interest |
| Park 2014 | Short term (8 weeks) |
| Ritter 2001 | Control was not minimal |
| Stenlund 2009 | Study did not measure outcomes of interest |
| Wei 1996 | Short term (8 weeks) |
Characteristics of ongoing studies [ordered by study ID]
Zheng 2014.
| Trial name or title | Primary prevention for risk factors of ischaemic stroke with Baduanjin exercise intervention in a community elder population |
| Methods | Randomised controlled trial |
| Participants | Community elders (aged 50 to 70 years) at increased risk of ischaemic stroke (to demonstrate 2 of the following: hypertension, taking antihypertensives, atrial fibrillation, smokers, dyslipidaemia, type 2 diabetes or history of transient ischaemic attacks (TIAs)) who have not conducted regular physical activity for at least 1 year (defined as 30 minutes 3 to 4 times per week for at least 3 months). Target recruitment 170; 85 randomly assigned to the intervention, 85 to control |
| Interventions | 12 weeks of Baduanjin exercise, 5 days a week, 40 minutes per day in groups of 25 to 30 at a community centre facilitated by physical education coaches. The training scheme of Baduanjin exercise originated from a standard set of 10 postures Control group will be requested to maintain usual habits of physical activity and will receive no specific exercise training Follow‐up at the end of the intervention, at 13 weeks and at 25 weeks |
| Outcomes | Primary: cerebrovascular function, cardiopulmonary function Secondary: motor function, physical parameters, blood lipids, fasting plasma glucose, inflammation factors, quality of sleep, quality of life, happiness, emotion and mood, self confidence and self esteem |
| Starting date | Recruitment started whilst manuscript was being completed |
| Contact information | Correspondence: lidianchen87@163.com
Fujian University of Traditional Chinese Medicine, Fuzhou 350122, China zhgh_1969@aliyun.com |
| Notes | Chinese clinical trial registry ‐ ChiCTR‐TRC‐13003588; http://www.chictr.org/cn/proj/show.aspx?proj=5229 Some participants with TIA, atrial fibrillation, type 2 diabetes ‐ need to check < 25% when results are available, as this is the criterion used for primary prevention |
Differences between protocol and review
It was our intention to perform stratified analysis to examine the effects of baseline risk, duration of qigong and type of qigong, but the number of trials included in the review was insufficient for performance of this analysis. We also intended to prepare funnel plots to assess publication bias, but again the review included an insufficient number of trials for this. These methods will be addressed in future updates of this review, when more evidence is available.
Contributions of authors
All review authors contributed to protocol development. Trial search co‐ordinators for the CHG ran the searches, and MS conducted searches in the Asian databases. LH, NF and KR screened the titles and abstracts, and LH, NF, KR and DT assessed studies for formal inclusion and exclusion. MS assessed methodological rigour and extracted data from studies written in Chinese, which were checked by JSWK. LH and KR extracted data and assessed risk of bias among studies reported in English, conducted the analyses and wrote the first draft of the review. All review authors contributed to later drafts.
Sources of support
Internal sources
Warwick Medical School, University of Warwick, UK.
Peninsula Medical School, Exeter, UK.
Korea Institute of Oriental Medicine (K13400), Korea, South.
External sources
NIHR Cochrane Programme Grant, UK.
National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care, West Midlands at University Hospitals Birmingham NHS Foundation Trust. Support to Karen Rees, UK.
Declarations of interest
None known.
New
References
References to studies included in this review
Chow 2012 {published data only}
- Chow YWY, Dorcas A, Siu AMH. The effects of qigong on reducing stress and anxiety and enhancing body‐mind well‐being. Mindfulness 2012;3:51‐9. [Google Scholar]
Kuang 1979 {published data only}
- Kuang AK. Treatment of hypertensive patients with Chi‐kung and regular antihypertensive therapy ‐ a comparative study of 4‐year treatment results of 135 cases. Chung‐Hua Nei Ko Tsa Chih Chinese Journal of Internal Medicine 1979;18(3):187‐91. [PubMed] [Google Scholar]
Kuang 1986 {published data only}
- Kuang AK, Wang CX, Xu DH, Zhao GS, Qian YS, Jiang MD, et al. Comparative study on the clinical effects and prognosis of 204 hypertensive patients treated with qigong on a 20 year follow‐up and its mechanism. Journal of Integrated Traditional Chinese and Western Medicine 1986;6(1):9‐12. [PubMed] [Google Scholar]
Kuang 1987 {published data only}
- Kuang A, Chongxing W. Research on "anti‐aging" effect of qigong. Chinese Journal of Integrated Traditional and Western Medicine 1987;7(8):455‐8. [PubMed] [Google Scholar]
Kuang 1987a {published data only}
- Kuang AK, Wang CX, Li G, Xu DH, Qian YS, Huang ML. Effect of qigong therapy in plasma 18‐OH‐DOC level in hypertensives. Journal of Traditional Chinese Medicine 1987;7(3):169‐70. [PubMed] [Google Scholar]
Li 1989 {published data only}
- Li W, Pi DR, Xing ZH, Huang YT, Wu YQ, Li YG, et al. Observation of curative effect of qigong treatment of liver yang hyperactivity and hyperactivity of yang due to yin deficiency type hypertension. Chinese Journal of Sports Medicine 1989;9(1):34‐5. [Google Scholar]
Li 1993 {published data only}
- Li JP. Qigong for hypertension patient plasma noradrenaline and 5‐HT. Chinese Journal of Sports Medicine 1993;12(3):152‐6. [Google Scholar]
Li 2014 {published data only}
- Li R, Jin L, Hong P, He ZH, Huang CY, Zhao JX, et al. The effect of Baduanjin on promoting the physical fitness and health of adults. Evidence‐based Complementary and Alternative Medicine 2014;Article ID 784059:http://dx.doi.org/10.1155/2014/784059. [DOI] [PMC free article] [PubMed] [Google Scholar]
Miao 2009 {published data only}
- Maio FS, Liu XY, Li Y, Wang XC. Health qigong eight sections brocade the influence of blood lipid and lipoprotein metabolism in patients with hyperlipidemia. Journal of Shandong Institute of Physical Education and Sports 2009;25(10):46‐8. [Google Scholar]
Wang 1989 {published data only}
- Wang CX, Xu DH, Qian YS, Zhao GS, Kuang AK. The influence of qi‐gong therapy upon serum HDL‐C of hypertensive patients. Journal of Integrated Traditional Chinese and Western Medicine 1989;9(9):543‐4. [PubMed] [Google Scholar]
Wang 1991 {published data only}
- Wang CX, Xu DH, Qian YS, Dong SQ, Kang AK. Comparative observation on the long term effect of Qigong cure hypertension ‐ 306 patients with 25 to 30 years of follow‐up. Actauniversitatismedicinalissecondae Shanghai 1991;11(3):93‐6. [Google Scholar]
References to studies excluded from this review
Du 1992 {published data only}
- Du ZY, Zhang JZL. Cardiovascular effect of different 'QiGong'. Chinese Journal of Sports Medicine 1992;11:32‐5. [Google Scholar]
Lee 2003 {published data only}
- Lee MS, Jang JW, Jang HS, Moon SR. Effects of Qi‐therapy on blood pressure, pain and psychological symptoms in the elderly: a randomized controlled pilot trial. Complementary Therapies in Medicine 2003;11(3):159‐64. [DOI] [PubMed] [Google Scholar]
Liu 2006 {published data only}
- Liu JR, Jiang XW, Xia XW, Zang ZH, Guo YS. The experimental study on fitness qigong "eight peices of brocade" regulation of lipid metabolism in the elderly. Chinese Journal of Gerontology 2006;26(3):317‐9. [Google Scholar]
Liu 2010 {published data only}
- Liu X, Miller YD, Burton NW, Brown WJ. A preliminary study of the effects of Tai Chi and Qigong medical exercise on indicators of metabolic syndrome, glycaemic control, health‐related quality of life, and psychological health in adults with elevated blood glucose. British Journal of Sports Medicine 2010;44(10):704‐9. [DOI] [PubMed] [Google Scholar]
Oh 2008 {published data only}
- Oh B, Butow P, Mullan B, Clarke S. Medical Qigong for cancer patients: pilot study of impact on quality of life, side effects of treatment and inflammation. American Journal of Chinese Medicine 2008;36(3):459‐72. [DOI] [PubMed] [Google Scholar]
Park 2014 {published data only}
- Park JE, Hong S, Lee M, Park T, Kang K, Jung H, et al. Randomized controlled trial of qigong for treatment of prehypertension and mild essential hypertension. Alternative Therapies in Health and Medicine 2014;20:21‐30. [PubMed] [Google Scholar]
Ritter 2001 {published data only}
- Ritter C, Aldridge D. Qigong Yangsheng as a therapeutic approach for the treatment of essential hypertension in comparison with a western muscle relaxation therapy: a randomised, controlled pilot study. Chinesische Medizin 2001;16(2):48‐63. [Google Scholar]
Stenlund 2009 {published data only}
- Stenlund T, Birgander LS, Lindahl B, Nilsson L, Ahlgren C. Effects of Qigong in patients with burnout: a randomized controlled trial. Journal of Rehabilitation Medicine 2009;41(9):761‐7. [DOI] [PubMed] [Google Scholar]
Wei 1996 {published data only}
- Wei L, Zhihua X, Deren P, Youshan W. The efficacy of Qigong training in patients with various TCM types of hypertension. Bulletin of Hunan Medical University 1996;21(2):123‐6. [Google Scholar]
References to ongoing studies
Zheng 2014 {published data only}
- Zheng G, Chen B, Fang Q, Yi H, Lin Q, Chen L, et al. Primary prevention for risk factors of ischemic stroke with Baduanjin exercise intervention in the community elder population: study protocol for a randomized controlled trial. Trials 2014;15:113. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Bassuk 2005
- Bassuk S, Manson J. Epidemiological evidence for the role of physical activity in reducing risk of type two diabetes and cardiovascular disease. Journal of Applied Physiology 2005;99(3):1193‐204. [DOI] [PubMed] [Google Scholar]
Bronas 2009
- Bronas U, Treat‐Jacobson D, Painter P. Alternative forms of exercise training as complementary therapy in the prevention and managment of type two diabetes. Diabetes Spectrum 2009;22(4):220‐5. [Google Scholar]
Chow 2012
- Chow Y, Dorcas A, Siu A. The effects of qigong on reducing stress and anxiety and enhancing body‐mind well‐being. Mindfulness 2012;3:51‐9. [Google Scholar]
Chyu 2011
- Chyu MC, Bergen V, Brismee JM, Zhang Y, Yeh J, Shen CI. Complementary and alternative exercises for management of osteoarthritis. Arthritis 2011;2011:1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Davis 2009
- Davies CM. Complementary Therapies in Rehabilitation: Evidence for Efficacy in Therapy, Prevention and Wellness. 3rd Edition. Thorofare, NJ: Slack Incorporated, 2009. [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple graphical test. BMJ 1997;315:629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ernst 2008
- Ernst E, Pittler MH, Wider B, Boddy K. Oxford Handbook of Complementary Medicine. Oxford: Oxford University Press, 2008. [Google Scholar]
Frishman 2005
- Fishman WH, Weintraub MI, Micozzi MS. Complementary and Integrative Therapies for Cardiovascular Disease. St Louis, MO: Elsevier/Mosby, 2005. [Google Scholar]
Guo 1996
- Guo YJ, Cimei T, Feng L. Urine catecholamine and cortisol levels in qigong practitioners under stress conditions. Proceedings of the third National Academic Conference on Qigong Science, Beijing. 1996:8, 90.
Guo 2008
- Guo X, Zhou B, Nishimura T, Teramukai S, Fukushima M. Clinical effect of qigong practice on essential hypertension: a meta‐analysis of randomized controlled trials. Journal of Alternative and Complimentary Medicine 2008;14(1):27‐37. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. www.cochrane‐handbook.org.
Innes 2008
- Innes KE, Selfe TK, Taylor AG. Menopause, the metabolic syndrome, and mind‐body therapies. Menopause 2008;15(5):1005‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jones 2001
- Jones B. Changes in cytokine production in healthy subjects practicing Guolin qigong: a pilot study. BMC Complementary and Alternative Medicine 2001;1(8):1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kraft 2009
- Kraft K. Complementary and alternative medicine in the context of prevention of disease and maintenance of health. Preventive Medicine 2009;49(2‐5):88‐92. [DOI] [PubMed] [Google Scholar]
Lee 2003a
- Lee MS, Kim HJ, Moon SR. Qigong reduced blood pressure and catecholamine levels of patients with essential hypertension. International Journal of Neuroscience 2003;113:1691‐701. [DOI] [PubMed] [Google Scholar]
Lee 2004
- Lee MS, Kim HJ, Choi ES. Effects of qigong on blood pressure, high‐density lipoprotein cholesterol and other lipid levels in essential hypertension. International Journal of Neuroscience 2004;114:777‐86. [DOI] [PubMed] [Google Scholar]
Lee 2007
- Lee MS, Pittler MH, Guo RL, Ernst E. Qigong for hypertension: a systematic review of randomized clinical trials. Journal of Hypertension 2007;25(8):1525‐32. [DOI] [PubMed] [Google Scholar]
Lee 2009
- Lee MS, Pittler MH, Ernst E. Internal qigong for pain conditions: a systematic review. Journal of Pain 2009;10(11):1121‐7. [DOI] [PubMed] [Google Scholar]
Mei 2012
- Mei L, Chen Q, Ge L, Zheng G, Chen J. Systematic review of Chinese traditional exercise Baduanjin modulating the blood lipid metabolism. Evidence‐Based Complementary and Alternative Medicine 2012;Article ID 282131:doi:10.1155/2012/282131. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mittal 2008
- Mittal S. The Metabolic Syndrome in Clinical Practice. London: Springer, 2008. [Google Scholar]
Nahas 2008
- Nahas R. Complementary and alternative medicine approaches to blood pressure reduction: a evidence based review. Canadian Family Physician 2008;54(11):1529‐33. [PMC free article] [PubMed] [Google Scholar]
Nüesch 2010
- Nüesch E, Trelle S, Reichenbach S, Rutjes AW, Tschannen B, Altman DG, et al. Small study effects in meta‐analyses of osteoarthritis trials: meta‐epidemiological study. BMJ 2010;341:c3515. [DOI] [PMC free article] [PubMed] [Google Scholar]
Press 2003
- Press V, Freestone I, George CF. Physical activity: the evidence of benefit in the prevention of coronary heart disease. QJM 2003;96(4):245‐51. [DOI] [PubMed] [Google Scholar]
Skoglund 2007
- Skoglund L, Jansson E. Qigong reduces stress in computer operators. Complementary Therapies in Clinical Practice 2007;13:78‐84. [DOI] [PubMed] [Google Scholar]
Sterne 2000
- Sterne JA, Gavaghan D, Egger M. Publication and related bias in meta‐analysis: power of statistical tests and prevalence in the literature. Journal of Clinical Epidemiology 2000;53:1119‐29. [DOI] [PubMed] [Google Scholar]
Sterne 2001
- Sterne JA, Egger M, Smith GD. Systematic reviews in health care:investigating and dealing with publication and other biases in meta analysis. BMJ 2001;323:101‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
von Trott 2009
- Trott P, Wiedemann AM, Ludtke R, Reibhauer A, Willich SN, Witt M. Qigong and Exercise Therapy for Elderly Patients with Chronic Neck Pain (QIBANE): a randomized controlled study. The Journal of Pain 2009;10(5):501‐8. [DOI] [PubMed] [Google Scholar]
WHO 2011a
- World Health Organization. Media Centre: Cardiovascular Diseases (CVDs). http://www.who.int/mediacentre/factsheets/fs317/en/index.html (accessed 11 July 2012).
WHO 2011b
- World Health Organization. Noncommunicable Diseases and Mental Health. http;//www.who.int/nmh/countries/en/index.html (accessed 11 July 2012).
Xin 2007
- Xin L, Miller YD, Brown WJ. A qualitative review of the role of qigong in the management of diabetes. Journal of Alternative and Complementary Medicine 2007;13:427‐33. [DOI] [PubMed] [Google Scholar]


