Abstract
Traditional cancer treatment approaches have focused on surgery, radiation therapy, and cytotoxic chemotherapy. However, with rare exceptions, metastatic cancers were considered to be incurable by traditional therapy. Over the past 20 years a fourth modality – immunotherapy – has emerged as a potentially curative approach for patients with advanced metastatic cancer. However, in many patients cancer “finds a way” to evade the anti-tumor effects of immunotherapy. Immunotherapy resistance mechanisms can be employed by both cancer cells and the non-cancer elements of tumor microenvironment. This review focuses on the resistance mechanisms that are specifically mediated by cancer cells. In order to extend the impact of immunotherapy to more patients and across all cancer types, and to inhibit the development of acquired resistance, the underlying biology driving immune escape needs to be better understood. Elucidating mechanisms of immune escape may shed light on new therapeutic targets, and lead to successful combination therapeutic strategies.
Keywords: Immunotherapy, Resistance, Combination Therapy, Antibody
Introduction
The startling reduction in cancer mortality rates since the signing of the US National Cancer Act in 1971 is a result of reductions in smoking rates, improved early detection, effective adjuvant therapy, and the deployment of increasingly effective and acceptably toxic cancer therapies. Traditional treatment approaches have focused on surgery, radiation therapy, and cytotoxic chemotherapy. However, with rare exceptions, metastatic cancers were considered to be incurable by traditional therapy. Over the past 20 years a fourth modality – immunotherapy – has emerged as a potentially curative approach for patients with advanced metastatic cancer. Commencing with the approval in 1997 of rituximab, an anti-CD20 monoclonal antibody with remarkable anti-tumor activity in patients with B cell malignancies, the field of cancer immunotherapy has been further energized by the discovery and exploitation of immune checkpoints as therapeutic targets.
As of today, there are at least 64 FDA approved monoclonal antibodies and 11 Fc-fusion proteins [1,2]. More than half of these antibody-based molecules are currently in clinical use for cancer treatment [2], and 6 of them are immune checkpoint blockades (ICBs) that target either the PD-1/PD-L1 or the CTLA4/CD28 axes (Table 1). These antibodies act by perturbing proliferative signaling and mediating immune cell destruction via antibody dependent cell-mediated cytotoxicity [3,4]. The ICBs work by releasing effector T cells from their inhibitory signals, allowing T cells to attack their target cancer cells. Interfering with immunological checkpoints can lead to durable clinical responses with generally manageable toxicity profiles. Moreover, because PD-1, PD-L1, and/or CTLA4 blockade targets components of host immunity rather than tumor cell-intrinsic factors, their therapeutic effects are not limited to one type of malignancy but are efficacious across a broad spectrum of cancers.
Table 1.
FDA-Approved Immune Checkpoint Inhibitors
| Antibody | Target | Approved For |
|---|---|---|
| Ipilimumab | CTLA4 | Metastatic Melanoma, Renal Cell Carcinoma, Colorectal Cancer |
| Nivolumab | PD-1 | Metastatic Melanoma, Non-Small Cell Lung Cancer, Renal Cell Carcinoma, Hodgkin’s Lymphoma, Head and Neck Cancer, Urothelial Carcinoma, Colorectal Cancer, Hepatocellular Carcinoma, and Small Cell Lung Cancer |
| Pembrolizumab | PD-1 | Metastatic Melanoma, Non-Small Cell Lung Cancer, Head and Neck Cancer, Hodgkin’s Lymphoma, Urothelial Carcinoma, Gastric Cancer, Cervical Cancer, Hepatocellular Carcinoma, Merkel Cell Carcinoma, Renal Cell Carcinoma, Small Cell Lung Cancer, and Esophageal Carcinoma |
| Atezolizumab | PD-L1 | Urothelial Carcinoma, Non-Small Cell Lung Cancer, Breast Cancer, and Small Cell Lung Cancer |
| Avelumab | PD-L1 | Merkel Cell Carcinoma, Urothelial Carcinoma, and Renal Cell Carcinoma |
| Durvalumab | PD-L1 | Urothelial Carcinoma and Non-Small Cell Lung Cancer |
| Cemiplimab | PD-1 | Advanced cutaneous squamous cell carcinoma (CSCC) |
Despite the remarkable clinical efficacy of monoclonal antibody therapy and durability of responses specifically seen with immune checkpoint inhibitors, many challenges still need to be addressed. When used as monotherapy, ICBs are effective only in a fraction of patients and acquired resistance is common. In fact, pooled analysis of long-term survival data for 1,861 patients from 10 prospective and 2 retrospective clinical studies of ipilimumab in unresectable or metastatic melanoma shows that the plateau in the survival curve was 21%, beginning around year 3 and lasting 10 years or more [5]. Also, several cancer types, such as pancreatic cancer, prostate cancer, colon cancer, and most cases of breast cancer, have shown very low frequencies of clinical benefit from ICBs [6].
In addition, monoclonal antibodies such as cetuximab and trastuzumab that target growth receptors overexpressed by cancer cells are used in both first and second line treatment regimens for common malignancies [7]. Despite the reported clinical benefits of targeted monoclonal antibodies, such as trastuzumab, and continued clinical use, the majority of patients develop therapeutic resistance that remains poorly understood [8].
Effective immune cell killing is regulated by many factors. These include the quantity and quality of antigens expressed on cancer cells, the kinetics of antigen appearance and discontinuity [9], the frequency and activity of intra-tumoral T cells, and the dynamic complex interactions between malignant cells and the surrounding stroma [10]. In order to extend the impact of therapeutic antibodies to more patients and across all cancer types, and to inhibit the development of acquired resistance, the underlying biology driving immune escape needs to be better understood. This understanding may lead to new successful therapeutic strategies. This review will focus on the mechanisms of antibody-based immunotherapy resistance that are specifically mediated by cancer cells.
Malignant Cell-based Mechanisms of Resistance
The goal of antibody-based cancer immunotherapy is to establish an anti-tumor immune response or to inhibit pro-tumor signaling. While this strategy has been effective, many tumor cell-intrinsic factors contribute to antibody-based immunotherapy resistance. Malignant cell-based resistance mechanisms can be broadly placed in four main categories that include: the loss of antigenicity, immunomodulation, immunosuppression, and oncogenic signaling. The various forms of immune evasion that comprise those categories can contribute to both primary (tumors do not initially respond to therapy) and adaptive (tumors initially respond to therapy) resistance [6]. Development of new antibody-based immunotherapies and combination paradigms must address the following known tumor cell-intrinsic resistance mechanisms.
(i). Loss of Antigenicity
Tumor cells can express a variety of tumor specific antigens that are recognizable by cytotoxic T lymphocytes. The fact that tumors express immunogenic antigens that often arise due to the same mutations that drive cancer development [11] provided a strong rationale for the development of immunotherapy. Unfortunately, tumor cells can evade both natural host and therapy induced immunity by becoming poor antigen presenters [12]. Normal cells process intracellular proteins into antigens that are expressed on the cell surface in the context of major histocompatibility (MHC) class I. Mutations in genes important for antigen processing machinery, specifically β−2-microglobulin (B2M) which is a component of MHC class I, have been found in multiple cancer types [13] and correlate with host T cell responses [14] indicating that primary resistance can be due to clonal selection of tumor cells with an intrinsic capacity to reduce their antigen presentation. Defects in antigen presentation have also been demonstrated to occur as adaptive resistance to ICB [15,16]. Future development of immune checkpoint inhibitors will need to address the downregulation of MHC Class I due to loss of B2M or other associated proteins [17]. The loss of MHC Class I normally triggers an immune response by NK cells that recognize MHC class I polypeptide-related sequence A and B (MICA/B) through the activating NKG2D receptor [18]. Tumor cells have greatly reduced levels of MICA and MICB on their surfaces, and their expression levels correlate with responses to immunotherapy [19]. Tumor cell modulation of antigen and cell surface repertoires represents a powerful immune evasion mechanism that remains a challenge for immunotherapy.
Recently, tumor cells have been demonstrated to downregulate other cell surface proteins in addition to antigens as a form of adaptive resistance to targeted monoclonal antibody therapy [20]. This is not traditional antigenic modulation, and may prove to be a new mechanism of resistance to immune attack.
Even when tumor cells retain their antigenicity and cytotoxic T lymphocytes recognize and target them for destruction tumor cells employ additional mechanisms to inhibit their lysis. T lymphocyte mediated tumor destruction is classically carried out by release of perforins and granzymes and/or ligation of death receptors that induce apoptosis in the target tumor cells. Evading or resisting apoptosis is considered one of the hallmarks of human cancers and is a form of primary resistance. A major apoptosis signaling pathway consists of the death receptors from the tumor necrosis factor receptor family such as Fas and TRAIL which upon activation recruit caspase-8 to form the death induced signaling complex (DISC) [21]. Tumor cells have reduced expression of Fas and TRAIL in order to evade activation of the apoptotic pathway [22,23]. Additionally, caspase-8 is frequently downregulated or functionally impaired in many cancers [24]. Moreover, there is a class of proteins known as inhibitors of apoptosis (IAP) that can become dysregulated as adaptive resistance to immunotherapy. For example, XIAP was found to mediate resistance to targeted antibody therapy [25].
(ii). Immunomodulation
While ICB therapy has proven to be effective many patients fail to respond due to adaptive resistance [26]. The use of an antibody to an immune checkpoint can lead to compensatory upregulation of additional immune checkpoints. For example, patients who received anti-PD-1 therapy but progressed were found to have tumor cells with increased levels of galectin-9 and higher proportions of TIM-3 positive exhausted T cells [27]. Similarly, it has been demonstrated that tumors can up-regulate the ligands to the immune checkpoints TIGIT and VISTA in response to ICB [28]. Paradoxically, tumor cells can also increase their expression of Fas. Although in some cases Fas can be downregulated to avoid T cell induced apoptosis, the inverse has been found to occur. Tumor cells with upregulated Fas expression can induce apoptosis in responding T cells [29]. The discovery of molecular immune targets beyond classical immune checkpoints such as CD40, CD47, and toll-like receptors whose signaling has been shown to inhibit the antitumor immune response mediated by traditional ICB has furthered the need for additional study [30]. Upregulation of various cell surface molecules that modulate T cell function in response to therapy will likely require combination treatments to increase clinical efficacy.
(iii). Immunosuppression
Tumor cell-mediated immunosuppression via alterations of the tumor microenvironment (TME) is a cause of both primary and adaptive resistance. Tumor cells release many pro-angiogenic factors that remodel the surrounding vasculature, which in turn can prevent T cell trafficking to the TME [31]. Immune evasion via exclusion of immune cell infiltration is a well-established form of primary resistance known to occur in pancreatic cancer due to formation of dense stroma and recruitment of cancer-associated fibroblasts [32]. Tumor cells also can secrete immunosuppressive metabolites into the local TME in response to immune attack. For example, the enzyme Indoleamine-pyrrole 2,3-dioxygenase (IDO) reduces T cell proliferation and activity and is overexpressed by tumor cells [33]. Preclinical studies demonstrated that IDO production was activated upon treatment with ICB [34]. Taken together, these results indicate the use of IDO inhibitors in combination with ICB therapy. Another TME molecule, Arginase I, has been demonstrated to impair T cell function [35]. In a model of ovarian cancer, tumor cells produced extracellular vesicles that delivered arginase I to immune cells to confer primary resistance to immune attack. Tumor derived exosomes have further been implicated as mediators of adaptive resistance to immunotherapy by delivering immunosuppressive molecules to responding immune cells [36]. In addition to secreting immunosuppressive molecules, tumor cells can elaborate cytokines that recruit immunosuppressive immune cell variants to the TME. For instance, in a melanoma mouse model tumor cells inhibited ICB efficacy by expressing chemotactic factors for the recruitment of myeloid derived suppressor cells (MDSCs) [37]. Thus, tumor cell intrinsic mechanisms exist that prevent an anti-tumor response by creating and maintaining an immunosuppressive TME.
(iv). Oncogenic Signaling
Oncogenic signaling pathways also play significant and complex roles in affecting the anti-tumor immune response. Alterations in the mitogen-activated protein kinase (MAPK) pathway, PI3K signaling due to PTEN loss, WNT/β-catenin signaling, and/or interferon-gamma (IFNγ) signaling have all been demonstrated to contribute to adaptive resistance to immunotherapy [38]. Furthermore, the use of monoclonal antibodies that target growth receptors such as epidermal growth factor receptor (EGFR) and human epidermal growth factor receptor 2 (HER2) directly perturb those signaling axes. Tumor cells can modify the receptor or downstream signaling pathways in acquired resistance [39,40]. The different signaling pathways that contribute to immunotherapy resistance will be covered more in depth in the next section.
Oncogenic Signaling Contributions to Resistance to Immunotherapy
Cancer cells can escape host immune surveillance by induction of oncogenic signaling pathways (41). Pathways that contribute to resistance to be reviewed in this section include: JAK/STAT signaling, the DNA damage response pathway, stimulator of interferon genes (STING) signaling, WNT/β-catenin signaling, EGFR signaling, Epithelial to Mesenchymal transition (EMT), and transforming growth factor-beta signaling.
(i). JAK/STAT Signaling
The Janus kinase (JAK) family and the signal transducer and activator of transcription (STAT) family constitute a rapid membrane-to-nucleus signaling module that can affect every aspect of the mammalian immune system. JAK/STAT signaling has consistently found to be involved in immune resistance. In pancreatic cancer epithelial cells and Hodgkin’s Reed-Sternberg (HRS) cells, constitutive activation of JAK/STAT signaling leads to chronic inflammation via secretion of pro-inflammatory cytokines including IL-6, IL-3, and IL-21 [42,43]. JAK/STAT-mediated chronic inflammation decreases anti-PD-1 immunotherapy efficacy by impairing cytotoxic T lymphocyte (CTL) activation in pancreatic cancer. The JAK1/2 inhibitor Ruxolitinib, which inhibits the JAK/STAT signaling pathway, efficiently inhibits systemic inflammation in the tumor microenvironment. This increases CTL infiltration and activation, and thus can overcome resistance to anti-PD-1 immunotherapy in a murine preclinical model of pancreatic adenocarcinoma [43].
STAT1 is part of the JAK/STAT signaling cascade and is best known for its essential role in mediating responses to all types of interferons (IFN). STAT1 regulates a variety of cellular processes such as antimicrobial activities, cell proliferation, and cell death. It possesses important immune modulatory functions both in innate and the adaptive immune responses [44]. The IFNγ signaling pathway is essential for host cancer immune surveillance. Expression of HLA class I antigens is often dysregulated in cancers, for example as the result of downregulation by EGFR signaling pathways in head and neck cancer (HNC), and is associated with interferon signaling dysfunction [45]. Interestingly, STAT1 and IFNs are also involved in resistance to T-cell-based immunotherapy [46]. More recently, it has been demonstrated that IFNγ signaling plays duel and opposing roles in the anti-tumor immune response whereby IFNγ signaling in T cells promotes response but IFNγ signaling in the tumor cells is inhibitory [47]. STAT1-dependent HLA class I upregulation also enhances clinical responses to anti-EGFR cetuximab therapy in HNC patients. Abrogating EGFR-induced immune escape mechanisms and restoring STAT1 signaling to reverse HLA downregulation using cetuximab should be considered to be a potential strategy to enhance adaptive cellular immunity [45].
(ii). DNA Damage Response
DNA damage results from physiological conditions or genotoxic agents, triggering the DNA damage response (DDR) [48]. Briefly, upon detection of DNA breaks by sensor protein complexes, DDR is initiated by phosphoinositide 3-kinase-like serine threonine kinases such as ataxia telangiectasia mutated (ATM), DNA-dependent protein kinase catalytic subunits (DNA-PKcs), and ataxia telangiectasia and RAD3 related (ATR). These upstream DDR kinases phosphorylate downstream proteins which lead to different cellular events: 1) activation of cell cycle checkpoints to prevent cells with DNA breaks from progressing through the cell cycle, 2) DNA repair pathways to maintain genomic integrity, and 3) apoptosis to eliminate cells with un-repairable DNA damage. Checkpoint kinase 1 (Chk1) regulates the G2/M checkpoint and Checkpoint kinase 2 (Chk2)/p53 monitors the G1/S checkpoint. After cell cycle arrest, DNA repair occurs through various DNA repair pathways, such as mismatch repair (MMR), base excision repair (BER), nucleotide excision repair (NER), and double-strand break repair pathways: homologue repair (HR) and non-homologue end joining repair (NHEJ). Thus, the balance of DNA damage and repair is well maintained to protect genome integrity.
DNA repair is closely related with immunotherapy efficiency. First, in tumor cells, DNA repair decreases mutation frequency and neoantigen production and confers resistance to immunotherapy under some circumstances because normal DNA repair prevents mutations, chromosomal rearrangement, and genomic aberration [49–50]. Compared to MMR-proficient tumors, MMR-deficient tumors have high tumor mutation load, which correlates with high microsatellite instability and higher responsiveness to ICB therapy [51,52]. Second, as a consequence of decreased immunogenicity, CTL infiltration is inhibited in the tumor microenvironment which impairs ICB efficacy. Breast cancers with mutations in the BReast CAncer genes 1 and 2 (BRCA1/2) have been shown to be associated with increased lymphocytic infiltrates [53]. In a small cell lung cancer in vivo tumor model, Poly (ADP-ribose) polymerase (PARP) inhibition potentiates the anti-tumor effect of PD-L1 blockade by increasing cytotoxic CD8+ T-cell infiltration at the tumor sites [52]. Moreover, the expression of PD-L1 is negatively regulated by DNA repair, such as MMR, NER and BER [52]. MMR-deficient tumors present higher surface expression of PD-L1 [54]. PARP inhibitors also augment PD-L1 expression on the surface [52,55]. It is plausible that inhibition of the DNA repair signaling pathway would sensitize tumor cells to antibody-based immunotherapy, providing the rationale for this combination therapeutic strategy [56,57].
(iii). STING Signaling
STING senses pathogen-derived or abnormal self-DNA in the cytosol, which can be generated as a result of DNA damage [58]. STING controls the transcription of numerous host defense genes, including type I interferons and pro-inflammatory cytokines, triggering an innate immune defense against microbial infection and cancer [58]. Since the STING pathway can stimulate host anti-tumor immunity, cancer cells tend to suppress this pathway, favoring tolerogenic cell death [59]. The DNA-sensing defense response, involving the STING pathway, is the most suppressed pathway in immune-resistant Head and Neck Squamous Cell Carcinoma (HNSCC) cells [60]. STING expression is suppressed by histone H3K4 lysine demethylases Lysine Demethylase 5 (KDM5) and activated by H3K4 methyltransferase [61]. SRY (sex determining region Y)-box 2 (SOX2) inhibits STING, facilitating autophagy-dependent STING degradation to inhibit IFN type I signaling [60]. Activation of the STING pathway can reverse adaptive immune resistance and sensitize tumor cells to immunotherapy such as ICB, chimeric antigen receptor cell therapy, and cancer vaccines [62,63]. STING agonists have been shown to promote IFN signaling and extend survival in two acute myeloid leukemia mouse models [64]. Despite the encouraging pre-clinical observations, the characterization of the STING pathway is species-dependent. Thus, STING agonists have failed thus far in clinical trials. In order to develop successful STING agonistic therapies, better characterization of human STING signaling is still needed [65].
(iv). WNT/β-catenin Signaling
WNT is a family of secreted glycolipoproteins and regulates cell proliferation, cell polarity, and cell fate determination during embryonic development and tissue homeostasis. The WNT signaling pathway functions by regulating the expression of the transcriptional co-activator β-catenin which controls developmental gene expressions [66]. The WNT/β-catenin signaling cascade is initiated after binding of a lipid-modified WNT protein to the receptor complex. Briefly, lipoprotein receptor- related protein (LRP) is phosphorylated by serine/threonine kinases casein kinase 1 (CK1) and glycogen synthase kinase 3β (GSK3β). Axis inhibition protein 1 (AXIN1) is then recruited to the plasma membrane. Upon the inactivation of the kinases in the β-catenin destruction complex, β-catenin translocates to the nucleus and forms an active transcription factor complex with T- cell factor (TCF)/lymphocyte- enhancer- binding factor (LEF), initiating transcription of target genes [67].
The WNT/β-catenin pathway has been associated with resistance to ICB-based immunotherapy. β-catenin pathway activation correlates with the lack of a T-cell gene expression signature in human melanomas. Mouse melanoma models with active β-catenin show a complete absence of CD3+ T cells and are resistant to anti–CTLA4/anti–PD-L1 therapy, which is dependent on the absence of CD103+ dendritic cells-derived chemokines such as C-X-C motif chemokine ligand 9 (CXCL9) and CXCL10 [68,69]. Therefore, modulation of WNT/β-catenin pathway would be expected to overcome resistance to cancer immunotherapy.
(v). EGFR Signaling
The epidermal growth factor receptor is a transmembrane tyrosine kinase receptor involved in the proliferation and survival of cancer cells. EGFR blockade therapy by EGFR-targeted monoclonal antibodies, such as cetuximab and panitumumab have been clinically used in colorectal cancer, head and neck cancer, non-small-cell lung cancer, and kidney cancer [70]. Anti-EGFR antibodies exert anti-tumor effects by either direct cell killing or eliciting ADCC. The mechanisms of anti-EGFR resistance include: 1) Acquisition of EGFR gene mutations, such as second-site mutation T790M, third-site mutation C797S, and S468R. These mutations map to the cetuximab epitope on EGFR, preventing antibody binding [71,72]. 2) RAS gene mutation; in colorectal cancer cells, KRAS, NRAS, BRAF and amplification of ERBB2 and MET gene mutations drive primary resistance to anti-EGFR treatment [73]. Additionally, in circulating tumor DNA (ctDNA) of colorectal cancer patients with primary or acquired resistance to EGFR blockade, there are alterations in KRAS, NRAS, MET, ERBB2, EGFR, FLT3 and MAP2K1 [74]. 3) Autophagy, which induces EGFR internalization and ubiquitination [75]. 4) ATM mutation and low-E-cadherin expression [76]. 5) inflammatory cytokines including IL1A, IL1B and IL8; this module of secreted cytokines is associated with non-response to cetuximab treatment in vitro and in patient-derived xenografts [77].
(vi). Epithelial-Mesenchymal Transition
EMT is a biological process mediated by multiple biochemical changes, allowing the transition of epithelial cells to cells with a mesenchymal phenotype; characterized by increased migratory capacity, invasion, resistance to apoptosis, and enhanced induction of extracellular molecules such as Vimentin [78]. EMT has been shown to play a function in the tumorigenic progression from initiation, primary tumor growth, invasion, dissemination and metastasis to colonization as well as in resistance to therapy [79]. Mesenchymal feature acquisition decreases the susceptibility of tumor cells to immune effector cell-mediated lysis. Moreover, a cohort study of patients with metastatic urothelial cancer treated with a PD-1 inhibitor, nivolumab, demonstrated that higher EMT/stroma-related gene expression is associated with lower response rates and shorter progression-free and overall survival in patients with T-cell infiltrated tumors [80]. EMT-associated mechanisms of immunoresistance include regulation of PD-L1/PD-L2 expression, increased autophagy, decreased sensitivity to the cell death receptor pathway, immunoproteasome deficiency and initiation of defective immunological synapses [81].
In addition, the T-box transcription factor Brachyury is recognized as the driver of the acquisition of mesenchymal features, by inducing the loss of p21 and cyclin-dependent kinase inhibitor 1 (CDK1), which results in inefficient caspase-dependent apoptosis. Stabilization of CDK1 by reconstitution of p21 expression or inhibition of WEE1, a negative kinase of CDK1 increases the lysis of Brachyury-high level tumor cells mediated by antigen-specific CD8+ T cells, NK cells, and lymphokine-activated killer (LAK) cells [82,83].
(vii). Transforming Growth Factor-β (TGF-β) Signaling
The TGF-β superfamily of cytokines is comprised of secreted polypeptides regulating a multitude of cellular processes including proliferation, differentiation, and neoplastic transformation [84]. The members of this superfamily elicit their biological effects through a family of transmembrane serine/threonine kinase receptors classified as type I or type II receptors. Cell signaling is transduced either via receptors that activate intracellular mediators (Smad) or in Smad-independent signaling pathways. Impaired T cell function or proliferation is one of the mechanisms of resistance to ICB therapy [38,85]. TGF-β represses proliferation of both CD4+ and CD8+ T cells, although CD28 co-stimulation can overcome this TGF-β-mediated repression [86]. TGF-β-induced EMT promotes resistance to complement-dependent cytotoxicity (CDC) of cetuximab in lung cancer, which is mediated by up-regulation of CD59 expression on the cell surface. CD59 knockdown could re-sensitize cells undergoing EMT to cetuximab-mediated CDC [87].
Combination Strategies to Overcome Immunotherapy Resistance
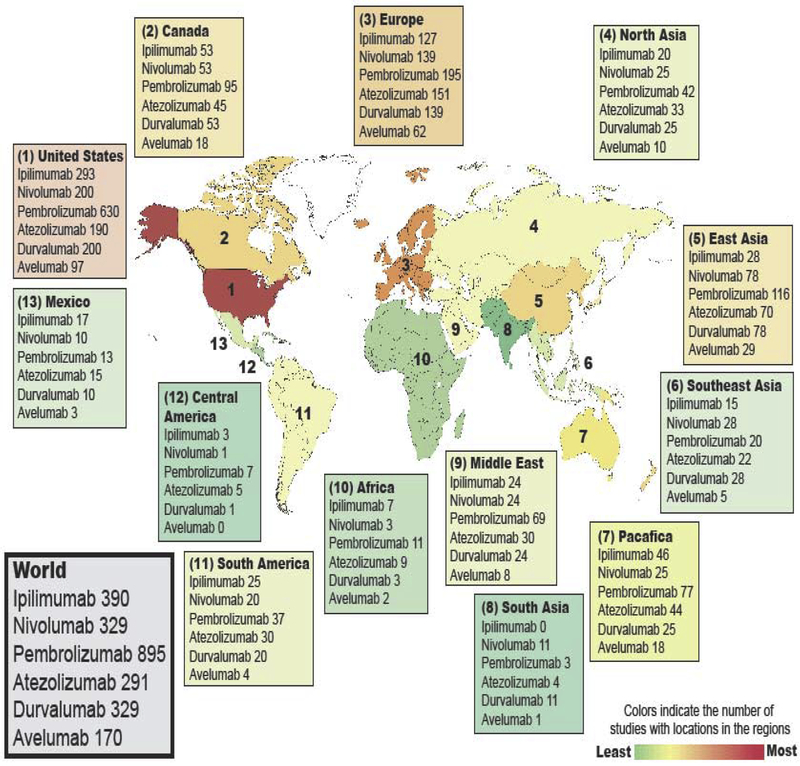
In order for cancer cells to successfully overcome the cytotoxic T cell response, they tend to induce several immune evasion mechanisms simultaneously. Therefore, with relatively rare exceptions it is unlikely that targeting a single resistance mechanism is sufficient to eradicate immunotherapy refractory tumors. Supporting evidence comes from the observation that patients and mice with high PD-L1 expression may still fail to respond to PD-1/PD-L1 inhibitors [88–89]. Also, even when the overexpression of immune checkpoints is considered the major mechanism of primary immune evasion and administration of FDA-approved ICBs results in favorable outcomes, acquired resistance is not uncommon. Driven by this knowledge, hundreds of therapeutic strategies that involve the combination of immune checkpoint inhibitory antibodies with conventional genotoxic cancer treatment, molecular targeted therapy, and/or other types of immunotherapies are currently being investigated (Figure 1). Below we provide some examples of these combination therapy strategies and describe how they are being designed to overcome the reviewed antibody-based immunotherapy resistance mechanisms.
Figure 1:
Current landscape for FDA-approved immune checkpoint inhibitor clinical trials. Using clinicaltrials.gov/, clinical trials (interventional studies) with status “Not yet recruiting”, “Recruiting”, “Enrolling by invitation” and “Active, not recruiting” were included in the figure.
(i). Combining ICB with Conventional Genotoxic Cancer Treatments
A large body of evidence indicates that conventional cancer treatments (i.e. chemotherapy and radiation therapy) have immunomodulatory effects [90,91]. They can induce immunogenic cell death, affect the expression of immune checkpoints on cancer cells, and reduce the infiltration of immunosuppressive stromal cells (such as T regulatory cells [92,93], MDSCs [94,95], dysfunctional dendritic cells (DCs) [96], tumor associated neutrophils (TANs) [97], and tumor associated macrophages (TAMs) [98]).
As mentioned earlier, reduced tumor antigenicity is a major immunotherapy resistance mechanism that typically leads to a relative paucity of intra-tumoral cytotoxic T cells. Classic examples of these immune-ignorant tumors, which are also referred to as “immunologically cold” tumors, are pancreatic cancer [99], prostate cancer [100], and glioblastoma [101]. One possible therapeutic approach to improve tumor immunogenicity is by inducing immunogenic cell death, the first and a crucial step in the initiation of T cell anti-tumor immunity.
Conventional cancer therapies promote immunogenic cell death by disrupting the genomic integrity through induction of DNA double-stranded breaks, DNA cross-links, chromosome bridges, and/or other chromosomal abnormalities during mitosis. Since cancer cells contain protein sequences that differ either in form or in level of expression than the proteins of their normal counterparts, the death of cancer cells results in the release of potentially immunogenic cancer antigens. While providing naive T cells with the antigenic peptides they can recognize is essential for their activation, induction of the pMHC-TCR signal only is insufficient in isolation to mount an effective adaptive immune response. Therefore, although cancer therapy-mediated DNA damage can increase mutational abundance, tumor antigenicity seems to have little impact on tumor immunogenicity. In fact, McGranahan et al. reported that chemotherapy-induced sub-clonal mutations that contribute to higher mutational load are enriched in some poor responders [102].
Several studies suggest that cytotoxic cancer therapy induces tumor immunogenicity by stimulating tumor adjuvanticity. As a result of cellular damage, intracellular contents (such as high mobility group box 1 (HMGB1), nucleic acids, and high concentrations of purine metabolites) are released. These endogenous molecules, which are termed damage-associated molecular patterns (DAMPs), can then be recognized by innate immune cells, including DCs, through their cognate pattern recognition receptors (PRRs). DAMPs-PRRs binding events promote the expression of a subset of cytokines and chemokine receptors, allowing DCs to migrate to T cell-rich areas of secondary lymphoid organs, such as regional draining lymph nodes. Also, PRR stimulation further enhances DCs antigen processing and presentation, and promotes DC expression of co-stimulatory molecules [103]. These co-stimulatory molecules on active DCs and the released cytokines provide the additional signals required for productive naïve T cell priming and activation. In a KP lung adenocarcinomas Kras/Trp53 mutant cancer mouse model, chemotherapies with favorable immunomodulatory properties (oxaliplatin combined with cyclophosphamide) control tumor growth by stimulating toll-like receptor 4 (TLR4) signaling, a PRR family member, and by eliciting CTL infiltration into the tumor, leading to durable responses to immune checkpoint inhibitors [104]. Notably, this particular tumor mouse model is resistant to chemotherapy or anti-PD-1 treatment when either is used as a monotherapy. Similarly, radiation therapy enhances the diversity of the TCR repertoire of intra-tumoral T cells [105], increases MHC class I expression, and improves antigen processing [106]. Interestingly, this immunogenic effect of radiation seems to be dependent on the activation of the STING pathway [107] and the subsequent stimulation of IFN signaling as a result of the release of cytosolic DNA from irradiated-cancer cells.
Driven by these findings, many clinical trials are currently underway to investigate the additional benefit of combining immune checkpoint blockades with chemotherapy [108] and/or radiation therapy [109]. Given that both immune checkpoint blockades and conventional cancer treatments are FDA approved and thus readily available, some of these combination therapeutic strategies may lead to relatively quick, meaningful clinical impacts.
Nonetheless, many questions remain to be answered in this field. For example, there are many different types of cell death (such as necroptosis, pyroptosis, ferroptosis, entotic cell death, necrotic cell death, parthanatos, lysosome-dependent cell death, autophagy-dependent cell death, alkaliptosis, and oxeiptosis) [110], and only some of these types can elicit immune responses [111]. Therefore, studying which type of cell death can be induced by each genotoxic agent is necessary. Moreover, the structural and biochemical features of chemotherapeutic agents are unlikely to predict their therapeutic efficacy when combined with immunotherapy. Hence, the clinical benefit of combining genotoxic chemotherapies with immune checkpoint inhibitors needs to be addressed experimentally. In fact, pre-clinical and/or clinical studies have demonstrated that only a few agents can induce immunogenic cell death, including doxorubicin, epirubicin, idarubicin, mitoxantrone, bleomycin, bortezomib, cyclophosphamide and oxaliplatin [90]. Similarly, the dose and schedule of radiation therapy can profoundly impact the degree of tumor immunogenicity, and thus needs to be carefully investigated. Along the same line, there is an urgent need to determine the proper timing and sequencing of combination therapy that can generate durable favorable immune and clinical responses with minimal toxicities [112].
(ii). Combining ICB with Molecularly Targeted Cancer Therapy
Many of identified molecules have the potential to generate favorable outcomes when targeted in combination with immunotherapies. These molecules either contribute to (i) aspects of the cancer cells’ intrinsic biology such as oncogenic signaling pathways, (ii) the cancer cells’ extrinsic biology (i.e. the tumor stroma comprised of immunosuppressive cytokines, chemokines, and angiogenic molecules), or (iii) the whole tumor biology, such as tumor epigenetic properties. In this review, we selectively emphasize targeting components of the DNA repair pathway in combination with FDA-approved immune checkpoint blockade as an example.
Four PARP inhibitors have received FDA approval as monotherapy for cancer. They are olaparib (Lynparza), rucaparib (Rubraca), niraparib (Zejula), and talazoparib (Talzenna). In preclinical in vivo studies, PARP inhibition remarkably potentiated the anti-tumor effect of PD-L1 blockade and increased the recruitment of cytotoxic CD8+ T cell infiltration in multiple immunocompetent in vivo tumor models [52,113]. More detailed studies revealed that PARP inhibitors trigger the accumulation of cytosolic DNA fragments due to unresolved DNA lesions. This can induce the activation of the STING pathway and the production of type I IFNs, leading to the stimulation of CXCL10 and CCL5, key chemokines to recruit T lymphocytes to the tumor site. Notably, this anti-tumor T cell immunity is independent of BRCA status. Moreover, exposure to the PARP inhibitor olaparib increases tumor sensitivity to NK cell killing and ADCC in both BRCA wild-type and BRCA mutant prostate cancer cells, independent of PD-L1 or EGFR modulation [114]. These results support the notion that inhibition of DNA damage response, including DNA repair signaling pathways, can sensitize tumor cells to antibody-based immunotherapy, providing the rationale for combination therapeutic strategies.
Very recently, a clinical trial was conducted to evaluate the safety and efficacy of niraparib in combination with pembrolizumab and led to very impressive results in 60 ovarian carcinoma patients [115]. The disease control rate was 65% (90% CI, 54%–75%), including 3 patients (5%) with confirmed complete responses, 8 patients (13%) with confirmed partial responses, and 28 patients (47%) with stable disease. The results of this study and similar ones set the stage for several ongoing clinical trials to evaluate the safety and efficacy of combining PARP inhibitors with anti-PD-1, anti-PD-L1 or anti-CTLA4 inhibitory antibodies for the treatment of ovarian cancer, triple negative breast cancer, prostate cancer, pancreatic cancer, and gastric cancer.
(iii). Combining ICB with other forms of immunotherapy
Currently, in addition to PD-1/PD-L1 and CTLA4, several other inhibitory immune checkpoints have been identified [116]. At least three of these molecules, Lag-3, Tim-3, and TIGIT, have potential to be translated to the clinic as immunotherapy targets. The biological activity, associated disorders, and therapeutic targeting of Lag-3, Tim-3, and TIGIT are nicely summarized in another review [117]. Despite the lack of deep mechanistic insight, a large amount of evidence suggests that immune checkpoints have distinct properties and exhibit non-overlapping functions, providing a preclinical rationale for combining multiple immune checkpoint inhibitors. Indeed, the objective response rates of metastatic melanoma patients treated with nivolumab plus ipilimumab are significantly higher (57.6%) than for patients treated with ipilimumab alone (19.0%) or nivolumab alone (43.7%).
In addition to co-inhibitory receptors, T cell immunity can also be regulated by co-stimulatory receptors, including CD40, CD27, glucocorticoid-induced TNFR-related protein (GITR), OX40, 4–1BB, and inducible T cell co-stimulator (ICOS) [118]. Pre-clinical and clinical studies show that targeting these co-stimulatory molecules is very promising. In this review, we discuss the antitumor activity of CD40 agonists as an example. The CD40 co-stimulator molecule is predominantly expressed by antigen presenting cells (APCs) and binds to CD40 ligand (CD40L) on the surface of T helper cells. CD40 is required for APC function. Thus, the major mechanism of CD40 agonists is to stimulate APC proliferation and activity. Interestingly, CD40 can be expressed by some malignant B cells and some cancer cells in solid tumors. Thus, CD40 agonists can also be employed to induce targeted cancer cell death.
At least four approaches have been implemented to target CD40/CD40L signaling: recombinant multimeric CD40-ligand [119], CD40L expressing chimeric antigen-receptor T cells (CAR-T cells) [120], gene therapeutic delivery of CD40L to leukemia cells [121], and agonistic monoclonal antibodies [122]. The latter approach has received the most attention with at least nine antibody-based therapies that are now being evaluated in clinical trials: APX005M, ABBV-927, ABBV-428, RO7009789, JNJ-64457107 (ADC-1013), CDX-1140, 2141 V-11, Chi Lob 7/4, and SEA-CD40. These drugs are currently investigated for the treatment of a wide range of solid tumors, including melanoma, pancreatic cancer, esophageal cancer, as well as hematological malignancies, such as lymphoma. Among the many clinical trials that reported promising therapeutic responses for CD40 agonists is NCT02482168 [123]. In this small phase Ib study, 30 previously untreated pancreatic ductal adenocarcinoma patients received therapy and 24 were dose-limiting toxicity-evaluable. These 24 patients were divided equally into 4 cohorts: (i) Gemcitabine/nab-paclitaxel/APX005M at 0.1 mg/kg, (ii) Gemcitabine/nab-paclitaxel/APX005M at 0.3 mg/kg, (iii) Gem/nab-paclitaxel/nivolumab/APX005M at 0.1 mg/kg, and (iv) Gem/nab-paclitaxel/nivolumab/APX005M at 0.3 mg/kg. Those patients demonstrated manageable safety profiles and promising anti-tumor activity. In fact, 14 (58%) patients had partial response, 8 (33%) patients had stable disease, 1 patient (4%) had progressive disease, and 1 patient (4%) had no treatment evaluation. Driven by these encouraging results, a randomized phase II study evaluating chemotherapy, APX005M 0.3 mg/kg, with and without nivolumab is currently underway.
In addition to antibody-based immunotherapy, the combination of immune checkpoint inhibitors with T cell adoptive therapy is being extensively explored in clinical trials in various settings. There are three types of T cell-based immunotherapy: (i) autologous tumor infiltrating lymphocyte (TIL) therapy, (ii) adoptive cell transfer of the patient’s peripheral T cells (ACT) with genetically-modified TCR therapy, and (iii) ACT with engineered CAR-T cell therapy. In a clinical trial, using TIL therapy in heavily pretreated patients with metastatic melanoma, 20% of patients had complete durable responses and the vast majority of them had more than 5 years of survival [124]. However, the TIL approach requires the isolation of sufficient number of anti-tumor T cells from large surgical samples, in vitro expansion, and then re-infusion into lymphocyte-depleted patients. The two ACT approaches described above have overcome some of these limitations. For example, CAR-T cell therapy, in particular, has shown remarkable efficacy in CD19 positive hematological malignancies, leading to the first FDA approval of a gene therapy. Despite these promising results, the field of adoptive T cell therapy faces several challenges. For example, the expression of immune checkpoints, such as PD-1, on adoptively transferred T cells increases after antigen stimulation, resulting in the development of acquired resistance to T cell therapy.
Additionally, the success of T cell therapy has been largely limited to hematological malignancies thus far. Among several potential mechanisms of resistance to T cell therapy in solid tumors is the expression of immune checkpoint molecules, such as PD-L1, by cancer cells and the stroma. These findings provide a rationale for combining T cell adoptive therapy with PD1/PD-L1 inhibitors. In pre-clinical studies, PD-1/PD-L1 blockade enhances the efficacy of CAR-T-cell therapy against established solid tumors. Interestingly, these studies also reported that the combination strategy of PD-1/PD-L1 inhibitors with CAR-T cell therapy can downregulate the frequency of intra-tumoral myeloid-derived suppressor cells (MDSC), and thus can further increase CAR-T cell activity [125,126]. Driven by these encouraging observations, several clinical trials of combination therapy have been conducted. Initial evidence in human clinical studies suggests that immune checkpoint inhibitors can be used safely with CAR-T cell therapy [127]. Also, this combination therapy strategy can decrease T cell exhaustion, thereby augmenting CAR-T cell function and persistence. While these early clinical results are promising, larger trials are still needed.
In addition to targeting immune checkpoints with monoclonal inhibitory antibodies, several attempts have been reported to genetically engineer CAR-T cells to either (i) lack PD-1 [128] or CTLA-4 [129] genes, (ii) to secrete anti-PD-L1 antibodies at the tumor site [130], or (iii) to convert the inhibitory signal generally transduced by the PD-1 cytoplasmic domain into an activating signal using a chimeric switch-receptor consists of the extracellular domain of PD-1 fused to the transmembrane and cytoplasmic domains of CD28 [131]. These novel CAR-T cell approaches are currently under investigation.
Conclusion
The field of cancer immune checkpoint inhibitors is expected to always face emergent challenges. In addition to the malignant cell-based mechanisms of resistance to immunotherapy, there are many other immune evasion mechanisms that can be employed by the non-cancer elements of the tumor microenvironment. The tumor stroma serves as a well-organized physical barrier and intricate biochemical system. It consists of diverse cellular types, non-cellular extracellular matrix (ECM) components, and altered microorganisms. All of these components continuously interact with each other and with cancer cells, creating a very dynamic and complex crosstalk network. Some of these factors regulate tumor immunity in synergistic or opposing manners, and thus can impact immunotherapy responses [132]. Therefore, although we have covered the relatively narrower but critically important area of how malignant cells evade immune destruction, it is important to think about such issues in the larger context of sophisticated tumor biology mechanisms.
For instance, tumors are typically very heterogeneous. Tumor heterogeneity can be exemplified by significant variations between cancers from different patients, between multiple tumors within a single patient, or even within different parts of the same tumor mass [133–135]. Tumor heterogeneity may involve variations in cancer cell intrinsic factors such as genomic and epigenomic features. It may also involve the diversity of the surrounding tumor microenvironment, including the type, frequency, and activity profiles of intra-tumoral immune cells and the expression of various immune checkpoints [136]. Therefore, every tumor may represent a unique ‘haystack’. Finding the needle (i.e. the effective therapeutic target) in each ‘haystack’ is challenging, illustrating the need for good biomarkers and personalized cancer treatments. Even if such ‘needles’ were successfully identified and resulted in initial favorable clinical outcomes, the persistence of immune selection forces may drive the continuing evolution of tumor heterogeneity and concomitant immune resistance. However, the durability of many anti-tumor immune responses suggests that in some, or perhaps many situations, the host immune system will be up to this challenge. In order to fill these current gaps in understanding, recent technological advances in molecular sciences combined with advanced data analysis and machine learning are being heavily employed to support the field of cancer immunotherapy [137–141].
Acknowledgments:
This research was supported by NCI R01 CA50633 (LMW) and National Institutes of Health (NIH)/National Cancer Institute (NCI) Grant P30-CA051008.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest
Louis M. Weiner, MD
| Name of Entity | Nature of Interest or Relationship | Expiration Date |
|---|---|---|
| Financial Interests | ||
Celldex Therapeutics,
|
Scientific Advisory Board | N/A |
CytomX Therapeutics, Inc.
|
External Advisory Board | N/A |
Jounce Therapeutics
|
Scientific Advisory Board, Co-Founder | N/A |
Targeted Diagnostic and Therapeutics, Inc.
|
Investment/Stock | N/A |
Immunome, Inc.
|
Scientific Advisory Board | N/A |
Klus Pharmaceuticals, Inc.
|
Scientific Advisory Board | N/A |
Bioxcel Therapeutics, Inc.
|
Clinical Advisory Board | N/A |
Forty-Seven, Inc.
|
Scientific Advisory Board | N/A |
Origin Commercial Ventures
|
Consultant | N/A |
Tessa Therapeutics
|
Scientific Advisory Board | N/A |
Samyang Biopharm USA Inc.
|
Scientific Advisory Board | N/A |
References
- 1.Tsumoto K, Isozaki Y, Yagami H, Tomita M. Future perspectives of therapeutic monoclonal antibodies. Immunotherapy. 2019;11(2):119–127. doi: 10.2217/imt-2018-0130 [DOI] [PubMed] [Google Scholar]
- 2.Dos Santos ML, Quintilio W, Manieri TM, Tsuruta LR, Moro AM. Advances and challenges in therapeutic monoclonal antibodies drug development. Brazilian J Pharm Sci. 2018;54(Special Issue):1–15. doi: 10.1590/s2175-97902018000001007 [DOI] [Google Scholar]
- 3.Bibeau F, Lopez-Crapez E, Fiore F Di, et al. Impact of fcγRIIa-fcγRIIIa polymorphisms and KRAS mutations on the clinical outcome of patients with metastatic colorectal cancer treated with cetuximab plus irinotecan. J Clin Oncol 2009;27(7):1122–1129. doi: 10.1200/JCO.2008.18.0463 [DOI] [PubMed] [Google Scholar]
- 4.Arnould L, Gelly M, Penault-Llorca F, et al. Trastuzumab-based treatment of HER2-positive breast cancer: An antibody-dependent cellular cytotoxicity mechanism? Br J Cancer. 2006;94(2):259–267. doi: 10.1038/sj.bjc.6602930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schadendorf D, Hodi FS, Robert C, et al. Pooled analysis of long-term survival data from phase II and phase III trials of ipilimumab in unresectable or metastatic melanoma. J Clin Oncol. 2015;33(17):1889–1894. doi: 10.1200/JCO.2014.56.2736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharma P, Hu-Lieskovan S, Wargo JA, Ribas A. Primary, Adaptive, and Acquired Resistance to Cancer Immunotherapy. Cell. 2017;168(4):707–723. doi: 10.1016/j.cell.2017.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Serna-Gallegos TR, La-Fargue CJ, Tewari KS. The Ecstacy of Gold: Patent Expirations for Trastuzumab, Bevacizumab, Rituximab, and Cetuximab. Recent Pat Biotechnol. 2018;12(2):101–112. doi: 10.2174/1872208311666171122152131 [DOI] [PubMed] [Google Scholar]
- 8.Vu T, Claret FX. Trastuzumab: Updated mechanisms of action and resistance in breast cancer. Front Oncol. 2012;2 JUN(June):1–6. doi: 10.3389/fonc.2012.00062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pradeu T, Carosella ED. On the definition of a criterion of immunogenicity. Proc Natl Acad Sci U S A. 2006;103(47):17858–17861. doi: 10.1073/pnas.0608683103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Balachandran VP, Beatty GL, Dougan SK. Broadening the Impact of Immunotherapy to Pancreatic Cancer: Challenges and Opportunities. Gastroenterology. 2019;156(7):2056–2072. doi: 10.1053/j.gastro.2018.12.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ilyas S, Yang JC. Landscape of Tumor Antigens in T Cell Immunotherapy. J Immunol. 2015. doi: 10.4049/jimmunol.1501657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cai L, Michelakos T, Yamada T, et al. Defective HLA class I antigen processing machinery in cancer. Cancer Immunol Immunother. 2018;67(6):999–1009. doi: 10.1007/s00262-018-2131-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grasso CS, Giannakis M, Wells DK, et al. Genetic mechanisms of immune evasion in colorectal cancer. Cancer Discov. 2018. doi: 10.1158/2159-8290.CD-17-1327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rooney MS, Shukla SA, Wu CJ, Getz G, Hacohen N. Molecular and genetic properties of tumors associated with local immune cytolytic activity. Cell. 2015. doi: 10.1016/j.cell.2014.12.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zaretsky JM, Garcia-Diaz A, Shin DS, et al. Mutations Associated with Acquired Resistance to PD-1 Blockade in Melanoma. N Engl J Med. 2016. doi: 10.1056/nejmoa1604958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gurjao C, Liu D, Hofree M, et al. Intrinsic Resistance to Immune Checkpoint Blockade in a Mismatch Repair Deficient Colorectal Cancer. Cancer Immunol Res. 2019;7(August):canimm.0683–2018.. doi: 10.1158/2326-6066.cir-18-0683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Šmahel M PD-1/PD-L1 blockade therapy for tumors with downregulated MHC class I expression. Int J Mol Sci. 2017;18(6):1–14. doi: 10.3390/ijms18061331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Drew PARDOLL. Does the immune system see tumors as foreign or self? Annu Rev Immunol. 2003. [DOI] [PubMed] [Google Scholar]
- 19.Chen Y, Lin W song, Zhu W feng, et al. Tumor MICA status predicts the efficacy of immunotherapy with cytokine-induced killer cells for patients with gastric cancer. Immunol Res. 2016. doi: 10.1007/s12026-015-8743-0 [DOI] [PubMed] [Google Scholar]
- 20.Aldeghaither DS, Zahavi DJ, Murray JC, et al. A Mechanism of Resistance to Antibody-Targeted Immune Attack. Cancer Immunol Res. 2019;7(2):230–243. doi: 10.1158/2326-6066.cir-18-0266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Germer M, Krammer PH, Hellbardt S, et al. Cytotoxicity-dependent APO-1 (Fas/CD95)-associated proteins form a death-inducing signaling complex (DISC) with the receptor. EMBO J. 2018;14(22):5579–5588. doi: 10.1002/j.1460-2075.1995.tb00245.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bullani RR, Wehrli P, Viard-Leveugle I, et al. Frequent downregulation of Fas (CD95) expression and function in melanoma. Melanoma Res. 2002;12(3):263–270. doi: 10.1097/00008390-200206000-00010 [DOI] [PubMed] [Google Scholar]
- 23.Nguyen T, Zhang XD, Hersey P. Relative Resistance of Fresh Isolates of Melanoma to Tumor Necrosis Factor-related Apoptosis-inducing Ligand (TRAIL)-induced Apoptosis. Cancer Res. 2001;7(March):966–974. [PubMed] [Google Scholar]
- 24.Fulda S Evasion of apoptosis as a cellular stress response in cancer. Int J Cell Biol. 2010;2010. doi: 10.1155/2010/370835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Evans MK, Sauer SJ, Nath S, Robinson TJ, Morse MA, Devi GR. X-linked inhibitor of apoptosis protein mediates tumor cell resistance to antibody-dependent cellular cytotoxicity. Cell Death Dis. 2016;7(1):e2073. doi: 10.1038/cddis.2015.412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.O’Donnell JS, Long GV., Scolyer RA, Teng MWL, Smyth MJ. Resistance to PD1/PDL1 checkpoint inhibition. Cancer Treat Rev. 2017;52:71–81. doi: 10.1016/j.ctrv.2016.11.007 [DOI] [PubMed] [Google Scholar]
- 27.Koyama S, Akbay EA, Li YY, et al. Adaptive resistance to therapeutic PD-1 blockade is associated with upregulation of alternative immune checkpoints. Nat Commun. 2016;7:1–9. doi: 10.1038/ncomms10501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Saleh R, Elkord E. Acquired resistance to cancer immunotherapy: Role of tumor-mediated immunosuppression. Semin Cancer Biol. 2019;(July):0–1. doi: 10.1016/j.semcancer.2019.07.017 [DOI] [PubMed] [Google Scholar]
- 29.Gastman BR, Johnson DE, Whiteside TL, Rabinowich H. Tumor-induced apoptosis of T lymphocytes: elucidation of intracellular apoptotic events. Blood. 2000;95(6):2015–2023. http://www.ncbi.nlm.nih.gov/pubmed/10706869. [PubMed] [Google Scholar]
- 30.Omar HA, Tolba MF. Tackling molecular targets beyond PD-1/PD-L1: Novel approaches to boost patients’ response to cancer immunotherapy. Crit Rev Oncol Hematol. 2019;135(January):21–29. doi: 10.1016/j.critrevonc.2019.01.009 [DOI] [PubMed] [Google Scholar]
- 31.Gajewski TF, Woo SR, Zha Y, et al. Cancer immunotherapy strategies based on overcoming barriers within the tumor microenvironment. Curr Opin Immunol. 2013;25(2):268–276. doi: 10.1016/j.coi.2013.02.009 [DOI] [PubMed] [Google Scholar]
- 32.Murakami T, Hiroshima Y, Matsuyama R, Homma Y, Hoffman RM, Endo I. Role of the tumor microenvironment in pancreatic cancer. Ann Gastroenterol Surg. 2019;3(2):130–137. doi: 10.1002/ags3.12225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Uyttenhove C, Pilotte L, Théate I, et al. Evidence for a tumoral immune resistance mechanism based on tryptophan degradation by indoleamine 2,3-dioxygenase. Nat Med. 2003;9(10):1269–1274. doi: 10.1038/nm934 [DOI] [PubMed] [Google Scholar]
- 34.Holmgaard RB, Zamarin D, Munn DH, Wolchok JD, Allison JP. Indoleamine 2,3-dioxygenase is a critical resistance mechanism in antitumor T cell immunotherapy targeting CTLA-4. J Exp Med. 2013;210(7):1389–1402. doi: 10.1084/jem.20130066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Correa P, Ortiz B, Delgado A, et al. Arginase I Production in the Tumor Microenvironment by Mature Myeloid Cells Inhibits T-Cell Receptor Expression and Antigen-Specific T-Cell Responses. Cancer Res. 2005;64(16):5839–5849. doi: 10.1158/0008-5472.can-04-0465 [DOI] [PubMed] [Google Scholar]
- 36.Li I, Nabet BY. Exosomes in the tumor microenvironment as mediators of cancer therapy resistance. Mol Cancer. 2019;18(1):1–10. doi: 10.1186/s12943-019-0975-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Steinberg SM, Shabaneh TB, Zhang P, et al. Myeloid Cells That Impair Immunotherapy Are Restored in Melanomas with Acquired Resistance to BRAF Inhibitors. Cancer Res. 2017;77(7):1599–1610. doi: 10.1158/0008-5472.CAN-16-1755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jenkins RW, Barbie DA, Flaherty KT. Mechanisms of resistance to immune checkpoint inhibitors. Br J Cancer. 2018;118(1):9–16. doi: 10.1038/bjc.2017.434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sforza V, Martinelli E, Ciardiello F, et al. Mechanisms of resistance to anti-epidermal growth factor receptor inhibitors in metastatic colorectal cancer. World J Gastroenterol. 2016;22(28):6345–6361. doi: 10.3748/wjg.v22.i28.6345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vernieri C, Milano M, Brambilla M, et al. Resistance mechanisms to anti-HER2 therapies in HER2-positive breast cancer: Current knowledge, new research directions and therapeutic perspectives. Crit Rev Oncol Hematol. 2019;139(December 2018):53–66. doi: 10.1016/j.critrevonc.2019.05.001 [DOI] [PubMed] [Google Scholar]
- 41.Rieth J, Subramanian S. Mechanisms of Intrinsic Tumor Resistance to Immunotherapy. Int J Mol Sci 2018;19(5):1340. doi: 10.3390/ijms19051340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ju W, Zhang M, Wilson KM, et al. Augmented efficacy of brentuximab vedotin combined with ruxolitinib and/or Navitoclax in a murine model of human Hodgkin’s lymphoma. Proc Natl Acad Sci U S A. 2016;113(6):1624–1629. doi: 10.1073/pnas.1524668113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lu C, Talukder A, Savage NM, Singh N, Liu K. JAK-STAT-mediated chronic inflammation impairs cytotoxic T lymphocyte activation to decrease anti-PD-1 immunotherapy efficacy in pancreatic cancer. Oncoimmunology. 2017;6(3):1–15. doi: 10.1080/2162402X.2017.1291106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stark GR, Darnell JE. The JAK-STAT Pathway at Twenty. Immunity. 2012;36(4):503–514. doi: 10.1016/j.immuni.2012.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Srivastava RM, Trivedi S, Concha-Benavente F, et al. Stat1-induced HLA class i upregulation enhances immunogenicity and clinical response to anti-EGFR mab cetuximab therapy in HNC patients. Cancer Immunol Res. 2015;3(8):936–945. doi: 10.1158/2326-6066.CIR-15-0053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gettinger S, Choi J, Hastings K, et al. Impaired HLA class I antigen processing and presentation as a mechanism of acquired resistance to immune checkpoint inhibitors in lung cancer. Cancer Discov. 2017;7(12):1420–1435. doi: 10.1158/2159-8290.CD-17-0593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Benci JL, Johnson LR, Choa R, et al. Opposing Functions of Interferon Coordinate Adaptive and Innate Immune Responses to Cancer Immune Checkpoint Blockade. Cell. 2019;178(4):933–948.e14. doi: 10.1016/j.cell.2019.07.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jackson SP, Bartek J. The DNA-damage response in human biology and disease. Nature. 2009;461(7267):1071–1078. doi: 10.1038/nature08467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Branzei D, Foiani M. Regulation of DNA repair throughout the cell cycle. Nat Rev Mol Cell Biol. 2008;9(4):297–308. doi: 10.1038/nrm2351 [DOI] [PubMed] [Google Scholar]
- 50.Mouw KW, Goldberg MS, Konstantinopoulos PA, D’Andrea AD. DNA damage and repair biomarkers of immunotherapy response. Cancer Discov. 2017;7(7):675–693. doi: 10.1158/2159-8290.CD-17-0226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Germano G, Lamba S, Rospo G, et al. Inactivation of DNA repair triggers neoantigen generation and impairs tumour growth. Nature. 2017;552(7683):1–5. doi: 10.1038/nature24673 [DOI] [PubMed] [Google Scholar]
- 52.Permata TBM, Hagiwara Y, Sato H, et al. Base excision repair regulates PD-L1 expression in cancer cells. Oncogene. 2019;38(23):4452–4466. doi: 10.1038/s41388-019-0733-6 [DOI] [PubMed] [Google Scholar]
- 53.Lord CJ, Ashworth A. BRCAness revisited. Nat Rev Cancer. 2016;16(2):110–120. doi: 10.1038/nrc.2015.21 [DOI] [PubMed] [Google Scholar]
- 54.Viale G, Trapani D, Curigliano G. Mismatch Repair Deficiency as a Predictive Biomarker for Immunotherapy Efficacy. Biomed Res Int. 2017;2017:1–8. doi: 10.1155/2017/4719194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jiao S, Xia W, Yamaguchi H, et al. PARP inhibitor upregulates PD-L1 expression and enhances cancer-associated immunosuppression. Clin Cancer Res. 2017;23(14):3711–3720. doi: 10.1158/1078-0432.CCR-16-3215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Brzostek-Racine S, Gordon C, Van Scoy S, Reich NC. The DNA Damage Response Induces IFN. J Immunol. 2011;187(10):5336–5345. doi: 10.4049/jimmunol.1100040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gasser S, Orsulic S, Brown EJ, Raulet DH. The DNA damage pathway regulates innate immune system ligands of the NKG2D receptor. Nature. 2005;436(7054):1186–1190. doi: 10.1038/nature03884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Barber GN. STING: Infection, inflammation and cancer. Nat Rev Immunol. 2015;15(12):760–770. doi: 10.1038/nri3921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Xia T, Konno H, Ahn J, Barber GN. Deregulation of STING Signaling in Colorectal Carcinoma Constrains DNA Damage Responses and Correlates With Tumorigenesis. Cell Rep. 2016;14(2):282–297. doi: 10.1016/j.celrep.2015.12.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tan YS, Sansanaphongpricha K, Xie Y, et al. Mitigating SOX2-potentiated Immune Escape of Head and Neck Squamous Cell Carcinoma with a STING-inducing Nanosatellite Vaccine. Clin Cancer Res. 2018;24(17):4242–4255. doi: 10.1158/1078-0432.CCR-17-2807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wu L, Cao J, Cai WL, et al. KDM5 histone demethylases repress immune response via suppression of STING. Cadwell K, ed. PLOS Biol. 2018;16(8):e2006134. doi: 10.1371/journal.pbio.2006134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dahal LN, Dou L, Hussain K, et al. STING activation reverses lymphoma-mediated resistance to antibody immunotherapy. Cancer Res. 2017;77(13):3619–3631. doi: 10.1158/0008-5472.CAN-16-2784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Moore E, Clavijo PE, Davis R, et al. Established T cell-inflamed tumors rejected after adaptive resistance was reversed by combination STING activation and PD-1 pathway blockade. Cancer Immunol Res. 2016;4(12):1061–1071. doi: 10.1158/2326-6066.CIR-16-0104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Curran E, Chen X, Corrales L, et al. STING Pathway Activation Stimulates Potent Immunity against Acute Myeloid Leukemia. Cell Rep. 2016;15(11):2357–2366. doi: 10.1016/j.celrep.2016.05.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Corrales L, Gajewski TF. Molecular Pathways: Targeting the Stimulator of Interferon Genes (STING) in the Immunotherapy of Cancer. Clin Cancer Res. 2015;21(21):4774–4779. doi: 10.1158/1078-0432.CCR-15-1362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.MacDonald BT, Tamai K, He X. Wnt/β-Catenin Signaling: Components, Mechanisms, and Diseases. Dev Cell. 2009;17(1):9–26. doi: 10.1016/j.devcel.2009.06.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Staal FJT, Luis TC, Tiemessen MM. WNT signalling in the immune system: WNT is spreading its wings. Nat Rev Immunol. 2008;8(8):581–593. doi: 10.1038/nri2360 [DOI] [PubMed] [Google Scholar]
- 68.Spranger S, Bao R, Gajewski TF. Melanoma-intrinsic β-catenin signalling prevents anti-tumour immunity. Nature. 2015;523(7559):231–235. doi: 10.1038/nature14404 [DOI] [PubMed] [Google Scholar]
- 69.Spranger S, Dai D, Horton B, Gajewski TF. Tumor-Residing Batf3 Dendritic Cells Are Required for Effector T Cell Trafficking and Adoptive T Cell Therapy. Cancer Cell. 2017;31(5):711–723.e4. doi: 10.1016/j.ccell.2017.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Martinelli E, De Palma R, Orditura M, De Vita F, Ciardiello F. Anti-epidermal growth factor receptor monoclonal antibodies in cancer therapy. Clin Exp Immunol. 2009;158(1):1–9. doi: 10.1111/j.1365-2249.2009.03992.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bagchi A, Haidar JN, Eastman SW, et al. Molecular basis for necitumumab inhibition of EGFR variants associated with acquired cetuximab resistance. Mol Cancer Ther. 2018;17(2):521–531. doi: 10.1158/1535-7163.MCT-17-0575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Mancini M, Gal H, Gaborit N, et al. An oligoclonal antibody durably overcomes resistance of lung cancer to third-generation EGFR inhibitors. EMBO Mol Med. 2018;10(2):294–308. doi: 10.15252/emmm.201708076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Misale S, Di Nicolantonio F, Sartore-Bianchi A, Siena S, Bardelli A. Resistance to Anti-EGFR therapy in colorectal cancer: From heterogeneity to convergent evolution. Cancer Discov. 2014;4(11):1269–1280. doi: 10.1158/2159-8290.CD-14-0462 [DOI] [PubMed] [Google Scholar]
- 74.Siravegna G, Mussolin B, Buscarino M, et al. Clonal evolution and resistance to EGFR blockade in the blood of colorectal cancer patients. Nat Med. 2015;21(7):795–801. doi: 10.1038/nm.3870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Koustas E, Karamouzis MV, Mihailidou C, Schizas D, Papavassiliou AG. Co-targeting of EGFR and autophagy signaling is an emerging treatment strategy in metastatic colorectal cancer. Cancer Lett. 2017;396:94–102. doi: 10.1016/j.canlet.2017.03.023 [DOI] [PubMed] [Google Scholar]
- 76.Geißler AL, Geißler M, Kottmann D, et al. ATM mutations and E-cadherin expression define sensitivity to EGFR-targeted therapy in colorectal cancer. Oncotarget. 2017;8(10):17164–17190. doi: 10.18632/oncotarget.15211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gelfo V, Rodia MT, Pucci M, et al. A module of inflammatory cytokines defines resistance of colorectal cancer to EGFR inhibitors. Oncotarget. 2016;7(44):72167–72183. doi: 10.18632/oncotarget.12354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kalluri R, Weinberg RA, Kalluri R, Weinberg RA. The basics of epithelial-mesenchymal transition Find the latest version : Review series The basics of epithelial-mesenchymal transition. J Clin Invest. 2009;119(6):1420–1428. doi: 10.1172/JCI39104.1420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Brabletz T, Kalluri R, Nieto MA, Weinberg RA. EMT in cancer. Nat Rev Cancer. 2018;18(2):128–134. doi: 10.1038/nrc.2017.118 [DOI] [PubMed] [Google Scholar]
- 80.Wang L, Saci A, Szabo PM, et al. EMT- and stroma-related gene expression and resistance to PD-1 blockade in urothelial cancer. Nat Commun. 2018;9(1). doi: 10.1038/s41467-018-05992-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Terry S, Savagner P, Ortiz-Cuaran S, et al. New insights into the role of EMT in tumor immune escape. Mol Oncol. 2017;11(7):824–846. doi: 10.1002/1878-0261.12093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hamilton DH, Huang B, Fernando RI, Tsang KY, Palena C. WEE1 inhibition alleviates resistance to immune attack of tumor cells undergoing epithelial-mesenchymal transition. Cancer Res. 2014;74(9):2510–2519. doi: 10.1158/0008-5472.CAN-13-1894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hamilton DH, McCampbell KK, Palena C. Loss of the cyclin-dependent kinase inhibitor 1 in the context of brachyury-mediated phenotypic plasticity drives tumor resistance to immune attack. Front Oncol. 2018;8(MAY):1–10. doi: 10.3389/fonc.2018.00143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kaklamani V, Pasche B. Transforming Growth Factor Beta and breast cancer. Cancer Treat Res. 2005;126:129–156. [DOI] [PubMed] [Google Scholar]
- 85.Jarnicki AG, Lysaght J, Todryk S, Mills KHG. Suppression of Antitumor Immunity by IL-10 and TGF-β-Producing T Cells Infiltrating the Growing Tumor: Influence of Tumor Environment on the Induction of CD4 + and CD8 + Regulatory T Cells. J Immunol. 2006;177(2):896–904. doi: 10.4049/jimmunol.177.2.896 [DOI] [PubMed] [Google Scholar]
- 86.Koehler H, Kofler D, Hombach A, Abken H. CD28 costimulation overcomes transforming growth factor-β-mediated repression of proliferation of redirected human CD4+ and CD8 + T cells in an antitumor cell attack. Cancer Res. 2007;67(5):2265–2273. doi: 10.1158/0008-5472.CAN-06-2098 [DOI] [PubMed] [Google Scholar]
- 87.Goswami MT, Reka AK, Kurapati H, et al. Regulation of complement-dependent cytotoxicity by TGF-β-induced epithelial-mesenchymal transition. Oncogene. 2016;35(15):1888–1898. doi: 10.1038/onc.2015.258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Reck M, Rodriguez-Abreu D, Robinson AG, et al. Pembrolizumab versus Chemotherapy for PD-L1-Positive Non-Small-Cell Lung Cancer. N Engl J Med. 2016;375(19):1823–1833. doi: 10.1056/NEJMoa1606774 [DOI] [PubMed] [Google Scholar]
- 89.Ding W, LaPlant BR, Call TG, et al. Pembrolizumab in patients with CLL and Richter transformation or with relapsed CLL. Blood. 2017;129(26):3419–3427. doi: 10.1182/blood-2017-02-765685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Brown JS, Sundar R, Lopez J. Combining DNA damaging therapeutics with immunotherapy: More haste, less speed. Br J Cancer. 2018;118(3):312–324. doi: 10.1038/bjc.2017.376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Patel SA, Minn AJ. Combination Cancer Therapy with Immune Checkpoint Blockade: Mechanisms and Strategies. Immunity. 2018;48(3):417–433. doi: 10.1016/j.immuni.2018.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ercolini AM, Ladle BH, Manning EA, et al. Recruitment of latent pools of high-avidity CD8+ T cells to the antitumor immune response. J Exp Med. 2005;201(10):1591–1602. doi: 10.1084/jem.20042167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Banissi C, Ghiringhelli F, Chen L, Carpentier AF. Treg depletion with a low-dose metronomic temozolomide regimen in a rat glioma model. Cancer Immunol Immunother. 2009;58(10):1627–1634. doi: 10.1007/s00262-009-0671-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Vincent J, Mignot G, Chalmin F, et al. 5-Fluorouracil selectively kills tumor-associated myeloid-derived suppressor cells resulting in enhanced T cell-dependent antitumor immunity. Cancer Res. 2010;70(8):3052–3061. doi: 10.1158/0008-5472.CAN-09-3690 [DOI] [PubMed] [Google Scholar]
- 95.Suzuki E, Kapoor V, Jassar AS, Kaiser LR, Albelda SM. Gemcitabine selectively eliminates splenic Gr-1+/CD11b + myeloid suppressor cells in tumor-bearing animals and enhances antitumor immune activity. Clin Cancer Res. 2005;11(18):6713–6721. doi: 10.1158/1078-0432.CCR-05-0883 [DOI] [PubMed] [Google Scholar]
- 96.Cubillos-Ruiz JR, Silberman PC, Rutkowski MR, et al. ER Stress Sensor XBP1 Controls Anti-tumor Immunity by Disrupting Dendritic Cell Homeostasis. Cell. 2015;161(7):1527–1538. doi: 10.1016/j.cell.2015.05.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Coffelt SB, Kersten K, Doornebal CW, et al. IL17-producing γδ T cells and neutrophils conspire to promote breast cancer metastasisdV performed the experiments Europe PMC Funders Group. Nature. 2015;522(7556):345–348. doi: 10.1038/nature14282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ruffell B, Chang-Strachan D, Chan V, et al. Macrophage IL-10 Blocks CD8+ T Cell-Dependent Responses to Chemotherapy by Suppressing IL-12 Expression in Intratumoral Dendritic Cells. Cancer Cell. 2014;26(5):623–637. doi: 10.1016/j.ccell.2014.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lohneis P, Sinn M, Bischoff S, et al. Cytotoxic tumour-infiltrating T lymphocytes influence outcome in resected pancreatic ductal adenocarcinoma. Eur J Cancer. 2017;83:290–301. doi: 10.1016/j.ejca.2017.06.016 [DOI] [PubMed] [Google Scholar]
- 100.Strasner A, Karin M. Immune infiltration and prostate cancer. Front Oncol. 2015;5(MAY). doi: 10.3389/fonc.2015.00128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Buerki RA, Chheda ZS, Okada H. Immunotherapy of primary brain tumors: Facts and hopes. Clin Cancer Res. 2018;24(21):5198–5205. doi: 10.1158/1078-0432.CCR-17-2769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.McGranahan N, Furness AJS, Rosenthal R, et al. Clonal neoantigens elicit T cell immunoreactivity and sensitivity to immune checkpoint blockade. Science (80-). 2016;351(6280):1463–1469. doi: 10.1126/science.aaf1490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Chen DS, Mellman I. Oncology meets immunology: The cancer-immunity cycle. Immunity. 2013;39(1):1–10. doi: 10.1016/j.immuni.2013.07.012 [DOI] [PubMed] [Google Scholar]
- 104.Pfirschke C, Engblom C, Rickelt S, et al. Immunogenic Chemotherapy Sensitizes Tumors to Checkpoint Blockade Therapy. Immunity. 2016;44(2):343–354. doi: 10.1016/j.immuni.2015.11.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Twyman-Saint Victor C, Rech AJ, Maity A, et al. Radiation and dual checkpoint blockade activate non-redundant immune mechanisms in cancer. Nature. 2015;520(7547):373–377. doi: 10.1038/nature14292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Reits EA, Hodge JW, Herberts CA, et al. Radiation modulates the peptide repertoire, enhances MHC class I expression, and induces successful antitumor immunotherapy. J Exp Med. 2006;203(5):1259–1271. doi: 10.1084/jem.20052494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wang H, Hu S, Chen X, et al. cGAS is essential for the antitumor effect of immune checkpoint blockade. Proc Natl Acad Sci U S A. 2017;114(7):1637–1642. doi: 10.1073/pnas.1621363114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Garg AD, More S, Rufo N, et al. Trial watch: Immunogenic cell death induction by anticancer chemotherapeutics. Oncoimmunology. 2017;6(12):1–18. doi: 10.1080/2162402X.2017.1386829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Shabason JE, Minn AJ. Radiation and Immune Checkpoint Blockade: From Bench to Clinic. Semin Radiat Oncol. 2017;27(3):289–298. doi: 10.1016/j.semradonc.2017.03.002 [DOI] [PubMed] [Google Scholar]
- 110.Tang D, Kang R, Berghe T Vanden, Vandenabeele P, Kroemer G. The molecular machinery of regulated cell death. Cell Res. 2019;29(5):347–364. doi: 10.1038/s41422-019-0164-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Galluzzi L, Buqué A, Kepp O, Zitvogel L, Kroemer G. Immunogenic cell death in cancer and infectious disease. Nat Rev Immunol. 2017;17(2):97–111. doi: 10.1038/nri.2016.107 [DOI] [PubMed] [Google Scholar]
- 112.Lazzari C, Karachaliou N, Bulotta A, et al. Combination of immunotherapy with chemotherapy and radiotherapy in lung cancer: is this the beginning of the end for cancer? Ther Adv Med Oncol. 2018;10(2s):175883591876209. doi: 10.1177/1758835918762094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Shen J, Zhao W, Ju Z, et al. PARPI triggers the STING-dependent immune response and enhances the therapeutic efficacy of immune checkpoint blockade independent of BRCANEss. Cancer Res. 2019;79(2):311–319. doi: 10.1158/0008-5472.CAN-18-1003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Fenerty KE, Padget M, Wolfson B, et al. Immunotherapy utilizing the combination of natural killer-and antibody dependent cellular cytotoxicity (ADCC)-mediating agents with poly (ADP-ribose) polymerase (PARP) inhibition 11 Medical and Health Sciences 1112 Oncology and Carcinogenesis 11 Medical. J Immunother Cancer. 2018;6(1):1–14. doi: 10.1186/s40425-018-0445-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Konstantinopoulos PA, Waggoner S, Vidal GA, et al. Single-Arm Phases 1 and 2 Trial of Niraparib in Combination with Pembrolizumab in Patients with Recurrent Platinum-Resistant Ovarian Carcinoma. JAMA Oncol. 2019;5(8):1141–1149. doi: 10.1001/jamaoncol.2019.1048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. 2012;12(4):252–264. doi: 10.1038/nrc3239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Anderson AC, Joller N, Kuchroo VK. Lag-3, Tim-3, and TIGIT: Co-inhibitory Receptors with Specialized Functions in Immune Regulation. Immunity. 2016;44(5):989–1004. doi: 10.1016/j.immuni.2016.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Mayes PA, Hance KW, Hoos A. The promise and challenges of immune agonist antibody development in cancer. Nat Rev Drug Discov. 2018;17(7):509–527. doi: 10.1038/nrd.2018.75 [DOI] [PubMed] [Google Scholar]
- 119.Vonderheide RH, Dutcher JP, Anderson JE, et al. Phase I study of recombinant human CD40 ligand in cancer patients. J Clin Oncol. 2001;19(13):3280–3287. doi: 10.1200/JCO.2001.19.13.3280 [DOI] [PubMed] [Google Scholar]
- 120.Kuhn NF, Purdon TJ, van Leeuwen DG, et al. CD40 Ligand-Modified Chimeric Antigen Receptor T Cells Enhance Antitumor Function by Eliciting an Endogenous Antitumor Response. Cancer Cell. 2019;35(3):473–488.e6. doi: 10.1016/j.ccell.2019.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Messmer D, Kipps TJ. CD154 gene therapy for human B-cell malignancies. Ann N Y Acad Sci. 2005;1062:51–60. doi: 10.1196/annals.1358.008 [DOI] [PubMed] [Google Scholar]
- 122.Vonderheide RH. The Immune Revolution: A Case for Priming, Not Checkpoint. Cancer Cell. 2018;33(4):563–569. doi: 10.1016/j.ccell.2018.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.O’Hara MH, O’Reilly EM, Rosemarie M, et al. A Phase Ib study of CD40 agonistic monoclonal antibody APX005M together with gemcitabine (Gem) and nab-paclitaxel (NP) with or without nivolumab (Nivo) in untreated metastatic ductal pancreatic adenocarcinoma (PDAC) patients [abstract] In: Proceedings of the American Association for Cancer Research Annual Meeting 2019; 2019 Mar 29-Apr 3; Atlanta, GA. Philadelphia (PA): AACR; Cancer Res; 2019;79(13 Suppl):Abstract nr CT004. doi: 10.1158/1538-7445.AM2019-CT004 [DOI] [Google Scholar]
- 124.Rosenberg SA, Yang JC, Sherry RM, et al. Durable Complete Responses in Heavily Pretreated Patients with Metastatic Melanoma Using T-Cell Transfer Immunotherapy. Clin Cancer Res. 2011;17(13):4550–4557. doi: 10.1158/1078-0432.CCR-11-0116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Gargett T, Yu W, Dotti G, et al. GD2-specific CAR T Cells Undergo Potent Activation and Deletion Following Antigen Encounter but can be Protected from Activation-induced Cell Death by PD-1 Blockade. Mol Ther. 2016;24(6):1135–1149. doi: 10.1038/mt.2016.63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Moon EK, Wang L-C, Dolfi DV., et al. Multifactorial T-cell Hypofunction That Is Reversible Can Limit the Efficacy of Chimeric Antigen Receptor-Transduced Human T cells in Solid Tumors. Clin Cancer Res. 2014;20(16):4262–4273. doi: 10.1158/1078-0432.CCR-13-2627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Gay F, D’Agostino M, Giaccone L, et al. Immuno-oncologic Approaches: CAR-T Cells and Checkpoint Inhibitors. Clin Lymphoma, Myeloma Leuk. 2017;17(8):471–478. doi: 10.1016/j.clml.2017.06.014 [DOI] [PubMed] [Google Scholar]
- 128.Su S, Hu B, Shao J, et al. CRISPR-Cas9 mediated efficient PD-1 disruption on human primary T cells from cancer patients. Sci Rep. 2016;6:1–13. doi: 10.1038/srep20070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Shi L, Meng T, Zhao Z, et al. CRISPR knock out CTLA-4 enhances the anti-tumor activity of cytotoxic T lymphocytes. Gene. 2017;636(August):36–41. doi: 10.1016/j.gene.2017.09.010 [DOI] [PubMed] [Google Scholar]
- 130.Suarez ER, Chang DK, Sun J, et al. Chimeric antigen receptor T cells secreting anti-PD-L1 antibodies more effectively regress renal cell carcinoma in a humanized mouse model. Oncotarget. 2016;7(23):34341–34355. doi: 10.18632/oncotarget.9114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Liu X, Ranganathan R, Jiang S, et al. A Chimeric Switch-Receptor Targeting PD1 Augments the Efficacy of Second-Generation CAR T Cells in Advanced Solid Tumors. Cancer Res. 2016;76(6):1578–1590. doi: 10.1158/0008-5472.CAN-15-2524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Binnewies M, Roberts EW, Kersten K, et al. Understanding the tumor immune microenvironment (TIME) for effective therapy. Nat Med. 2018;24(5):541–550. doi: 10.1038/s41591-018-0014-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Jamal-Hanjani M, Quezada SA, Larkin J, Swanton C. Translational Implications of Tumor Heterogeneity. Clin Cancer Res. 2015;21(6):1258–1266. doi: 10.1158/1078-0432.CCR-14-1429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Lawrence MS.; Stojanov P; Kryukov G; Cibulskis K et al. Mutational heterogeneity in cancer and search for new cancer genes. Nature. 2014;499(7457):214–218. doi: 10.1038/nature12213.Mutational [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Gerlinger M, Rowan AJ, Horswell S, et al. Intratumor heterogeneity and branched evolution revealed by multiregion sequencing. New Engl J Med. 2012;366(10):883–892. doi: 10.1056/NEJMoa1113205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Jiménez-Sánchez A, Memon D, Pourpe S, et al. Heterogeneous Tumor-Immune Microenvironments among Differentially Growing Metastases in an Ovarian Cancer Patient. Cell. 2017;170(5):927–938.e20. doi: 10.1016/j.cell.2017.07.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Kumar MP, Du J, Lagoudas G, et al. Analysis of Single-Cell RNA-Seq Identifies Cell-Cell Communication Associated with Tumor Characteristics. Cell Rep. 2018;25(6):1458–1468. doi: 10.1016/j.celrep.2018.10.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Brubaker DK, Proctor EA, Haigis KM, et al. Computational translation of genomic responses from experimental model systems to humans. PLoS Comput Biol. 2019;15(1): e1006286. doi: 10.1371/journal.pcbi.1006286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Stein-O’Brien GL, Arora R, Culhane AC, et al. Enter the Matrix: Factorization Uncovers Knowledge from Omics. Trends Genet. 2018;34(10):790–805. doi: 10.1016/j.tig.2018.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Racle J, Michaux J, Rockinger GA, et al. Robust prediction of HLA class II epitopes by deep motif deconvolution of immunopeptidomes. Nat Biotechnol. 2019;37(11):1283–1286. doi: 10.1038/s41587-019-0289-6 [DOI] [PubMed] [Google Scholar]
- 141.Goldberg MS. Improving cancer immunotherapy through nanotechnology. Nat Rev Cancer. 2019;19(10):587–602. doi: 10.1038/s41568-019-0186-9 [DOI] [PubMed] [Google Scholar]