Abstract
Background
Self-harm in adolescents is common and repetition frequent. Evidence for effective interventions to reduce self-harm is limited. Long term follow-up of existing studies is rare.
Methods
Extended follow up, from 18 to at least 36-months, of the SHIFT trial: a pragmatic, multi-centre, individually-randomised, controlled trial involving young people (11–17) who had self-harmed at least twice and presented to Child & Adolescent Mental Health Services (CAMHS). SHIFT evaluated manualised family therapy (FT) versus treatment as usual (TAU) in reducing repetition of self-harm leading to hospital attendance 18 months post-randomisation.
We obtained ONS mortality data, adult mental health data, and further details of hospital attendance from routine Hospital Episode Statistics (HES) data plus researcher follow-up. We assessed longer-term differences in outcome using multivariable Cox Proportional Hazards regression analysis, and assessed all-cause mortality and morbidity relating to hospital attendances for reasons other than self-harm.
Study registration
ISRCTN 59793150
Outcomes
The original sample of 832 were randomised between April 2010 and December 2013. Extended follow-up continued until February 2017 for a median 55·4 months (range 0–82·5 months), providing post 18-month data for 804 (96·6%) participants, of whom 785 (94·4%) had a minimum of 36-months follow-up.
There was no evidence of a between-group difference in the primary outcome during the extended follow-up period (Hazard Ratio (HR) 1·03; 95% CI: 0·83, 1·28; p-value=0·78), consistent with our findings in the original trial with 18 months follow-up (HR 1·14, 95% CI 0·87, 1·49; p-value 0·33). There was a reduced rate of self-harm in older participants aged 15–17 (HR 0·7, 95% CI 0·56, 0·88), as compared with those aged 11–14; and significantly increased rates of self-harm in participants whose index episode combined self-injury and poisoning (HR 1·8, 95% CI 1·2, 2·7). Two deaths were reported during the extended follow up period.
Interpretation
For adolescents referred to CAMHS after self-harm, having self-harmed at least once before, trial FT confers no benefits over TAU in reducing subsequent hospitalisation for self-harm over 18 months or 36 months.
Funding
NIHR HTA Reference: 07/33/01
Keywords: Self-harm, Family therapy, Long term follow up, RCT
Research in Context.
Evidence before this study
We searched electronic databases from the first available year to 31 March 2007 for randomised controlled trials of interventions to address self-harm in people under the age of 18, where the primary outcome was reduction in self-harm. We identified one trial of a token allowing re-admission, which found no effect and one trial of group therapy for adolescents but no other studies in the appropriate age group with reduction in repetition of self-harm as the primary outcome (subsequent replication of the group therapy study did not find a positive impact of group therapy). We identified two studies of family interventions related to self-harm; a depression study reporting suicidal ideation as a secondary outcome; and a study of a home-based intervention designed to improve family communication, powered to detect between-group differences in suicidal ideation, not repeat self-harm.
Added value of this study
We found no evidence that for adolescents referred to CAMHS after self-harm, having self-harmed at least once before, the trial's manualised systemic family therapy conferred any benefits over TAU in reducing subsequent hospitalisation for self-harm at 36 months post-randomisation nor throughout the extended follow-up period. Self-harm continued from 18–36 months at much the same rate as from 0 −18 months. Younger girls, those with multiple past self-harm events, and those who combine self-poisoning with self-injury are at greater risk of further self-harm. Further attendances at hospital for any reason are an indicator of risk.
Implications of all the available evidence
SHIFT family therapy confers no additional benefits over TAU in reducing subsequent hospitalisation for self-harm. Young people who self-harm form a heterogeneous group with self-harm likely to be the final common pathway for a wide range of predicaments. Further research is needed to develop a more personalised approach and to identify which interventions are most helpful for which young people. This study suggests that lack of repetition by 18 months is not an indication of no further risk of repetition and points to a number of factors that predict further self-harm and risk.
Alt-text: Unlabelled box
1. Introduction
Self-harm in adolescents is a global public health problem, with perhaps 11% of adolescents self-reporting self-harm within the last year in England [1,2] and suicide the second commonest cause of death in 10 to 24-year olds, after road traffic accidents [3]. A single effective intervention has not been identified [4,5], and our recent, large randomised controlled trial showed no specific benefit for a manualised form of family therapy (FT) when compared with treatment as usual (TAU) over an 18 month follow up period, whilst providing suggestions that some sub-groups might do better (or worse) with FT [6].
Trials of interventions for children's mental health are often criticised for short follow-up duration. Studies in the most recent systematic review of interventions for adolescent self-harm [5] reported a mean of 10.1 months follow up (range 2–24 months), with only three studies reporting follow up beyond 12 months.
2. Methods
This paper presents the results of an extended follow up (to at least 36 months post-randomisation) of the primary outcome and other hospital related outcomes in the Self-Harm Intervention: Family Therapy (SHIFT) trial. Detailed trial methods and results at 18 months, have already been reported [6,7]. We present a brief summary of methods from the original trial, followed by a detailed description of methods for the extended follow-up.
2.1. Brief summary of original trial methods
2.1.1. Design
A UK pragmatic, multi-centre individually-randomised, controlled trial of FT compared with TAU.
2.1.2. Participants
Eligible adolescents 11–17, living with a primary caregiver, had self-harmed at least twice and were referred to CAMHS following self-harm (index episode). In common with UK, European and Australasian practice, we defined self-harm as any form of intentional non-fatal self-poisoning or self-injury (including cutting, taking excess medication, hanging, self-strangulation, jumping from height, running into traffic), regardless of suicidal intent; this includes US definitions of non-suicidal self-injury (NSSI) and suicidal behaviour.
2.1.3. Setting
Within 40 English National Health Service (NHS) CAMHS in 15 NHS Trusts across Greater Manchester, London and Yorkshire, young people were screened by a CAMHS clinician following the index self-harm episode. Those eligible and consenting to researcher contact were visited at home by a researcher who discussed the trial, obtained written consent for participation and conducted baseline assessments.
2.1.4. Ethical approval
Approved by the UK NHS National Research Ethics Service in April 2009 (Reference: 09/H1307/20).
2.1.5. Randomisation and masking
Following consent and baseline assessment, 832 participants were randomised sequentially to receive FT or TAU (1:1), via a computer-generated minimisation programme incorporating a random element, stratified by CAMHS, gender, age (11–14 and 15–17 based on evidence that under 14 s might have lower intent and lower rates of longer-term suicide [8]), living arrangements, previous self-harm episodes, and index episode type. Family therapists working across multiple services were also randomly allocated to FT participants. Participants and therapists were aware of treatment allocation, researchers were blinded.
2.1.6. Interventions
6-8 sessions of manualised and supervised FT [9] delivered by experienced, qualified family therapists or for TAU, the care offered to young people by local CAMHS teams. This was unrestricted and expected to be diverse. Further information about SHIFT FT, TAU, adherence and fidelity is reported elsewhere [6,10].
2.1.7. Outcomes
Primary outcome: Repetition of self-harm leading to hospital attendance within 18 months post-randomisation. Secondary outcomes included a range of clinical and economic outcomes at 12 and 18 months.
2.1.8. Assessment and data collection
Researcher administered and self-reported young person and caregiver questionnaires at baseline, 12 and 18 months post-randomisation; data from treating CAMHS clinicians, family therapists, and local Research Networks. Hospital attendance data (primary outcome) were obtained from Accident and Emergency (A&E) and in-patient Hospital Episode Statistics (HES) datasets from NHS Digital (https://digital.nhs.uk) up to January 2015, augmented by directed hospital record searches, undertaken by blinded researchers until the end of the 18-month follow-up period in June 2015 [11].
Link to published protocol for main trial: http://www.trialsjournal.com/content/16/1/501
Trial registration: 26 January 2009. http://www.controlled-trials.com/ISRCTN59793150
2.2. Extended follow-up methods
2.2.1. Design
Additional data supplemented 18 month follow up. Extended follow up to a minimum 36 months post-randomisation, of SHIFT participants.
2.2.2. Participants
Those in the original study unless consent for further data collection had been withdrawn.
2.2.3. Ethical approval
In addition to the original approval, all participants who had not already withdrawn were contacted via a newsletter and given an option to withdraw from further follow up.
2.2.4. Outcomes
Repetition of self-harm leading to hospital attendance (original primary outcome); characteristics of further episodes of self-harm leading to hospital attendance; all-cause morbidity and mortality; all measured over the extended follow-up period.
Health economic methods and results will be published separately.
2.2.5. Assessment and data collection
Three years after the last participant was recruited to the trial, identifiers were sent to NHS Digital (https://digital.nhs.uk) for linkage to A&E and in-patient HES datasets, providing follow-up data to February 2017. ONS mortality data and adult mental health data were also obtained, however, at the time of data collection an England wide CAMHS data reporting system had not been agreed, and so data on attendances to child and adolescent facilities were not available. Identifiers were not sent for participants with original or subsequent withdrawal from further clinical data collection, lack of original consent for linkage, or where the newsletter alerting participants of long-term follow-up could not be delivered to a current address (address unknown or returned to sender). Where it was not possible to obtain further HES data, participants’ post-18-month HES data received within the original trial (to January 2015) were included.
As with the original trial, HES episode data were processed to derive complete hospital attendances and classified as self-harm related, possibly self-harm related, and not self-harm related [11]. Minor changes to the classification algorithm followed the original trial (Supplementary Table 1). To maximise the chance of identifying self-harm attendances given limited research resources and time, unclassified attendances were prioritised, identifying those probably self-harm related (Supplementary Table 2).
Directed hospital record searches of unclassified attendances (including low priority attendances where time constraints allowed) were undertaken by blinded researchers between July 2017 January 2018 [11]. to supplement routine HES data downloaded from NHS Digital. Limited resources restricted our search and so we obtained approval for researcher follow up in the 34 hospital providers identified where participants were most likely to attend (based on original trial data and proximity to recruitment site). These researchers were not involved in the original study, and had no knowledge of treatment allocation.
2.3. Statistical analysis
Analyses were conducted using SAS version 9.4, in the intention-to-treat population and all statistical testing used two-sided 5% significance levels.
We used Cox's Proportional Hazards Model accounting for covariates (minimisation factors sex, age (11-14 vs 15-17), two vs three or more previous self-harm episodes, and index episode type; and NHS Trust) to test for differences in longer-term repetition rates. Hazard ratios; 95% confidence intervals (CIs) and Kaplan–Meier curves showing time to self-harm for each group and estimates of repetition rate are presented. Participants without an event were censored at the time last known to be event free. A sensitivity analysis examined the impact of unclassified hospital attendances. Moderators of treatment effect, caregiver-reported affective involvement and young person-reported unemotional traits, detected in the original 18 month analysis [6], were re-assessed via interaction effects in the primary endpoint analysis.
To analyse all hospital attendances due to self-harm, we conducted a recurrent events analysis using the Andersen-Gill counting process model [12] with robust sandwich variance estimator, and stratified models for restricted gap-time and total time proposed by Prentice et al. [13]. Each model provides common regression coefficient(s) across recurrent events resulting in the marginal means model.
We present between-group differences in all-cause morbidity and mortality, with morbidity measured through hospital attendances for reasons other than self-harm (including unclassified attendances). We explored the association between hospital attendances for reasons other than self-harm, and for reasons related to self-harm, using the Cochran-Mantel-Haenszel statistics [14] to estimate the common odds ratio across treatment arm. Hospital admissions are investigated through ICD-10 diagnosis codes (International Classification of Diseases 10 [15]), and adversity-related admissions identified and reported according to the methods of Herbert et al. [16,17].
2.3.1. Sample size
The original trial sample size of 832 (416 per group) provided 90% power to detect a 35% relative reduction in 18-month repetition rates between TAU (29%) and FT (18·8%), using a 5% significance level log-rank test for equality of survival curves, assuming 10% loss to follow-up by 18 months for the primary outcome (repetition of self-harm resulting in hospital attendance). The trial recruited to target; only 21 (2·5%) withdrew from the primary outcome follow-up at 18 months.
3. Results
3.1. Follow-up
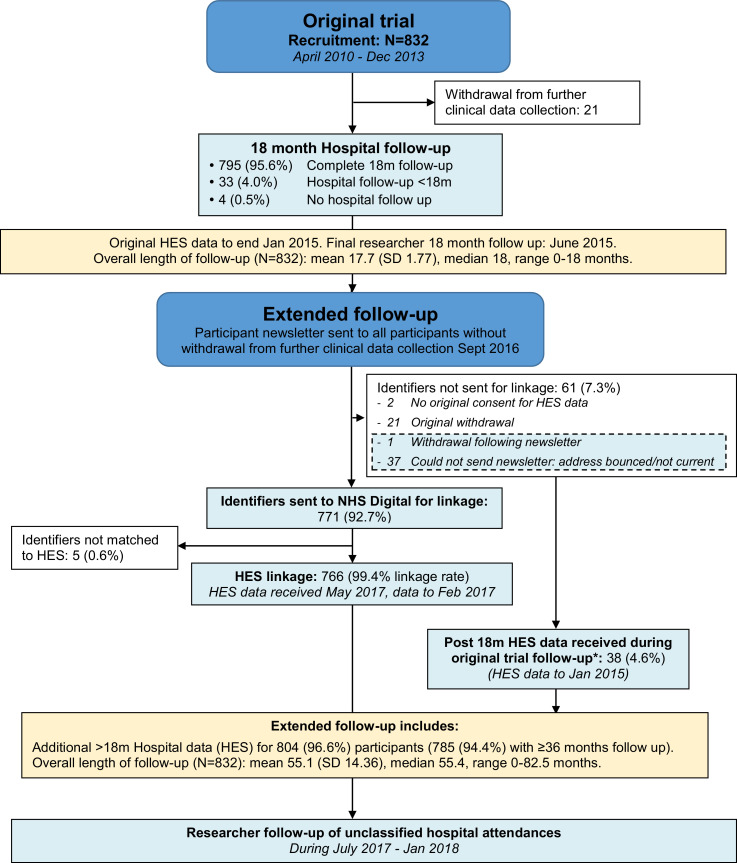
Additional data supplemented 18 month follow up for 804 (96·6%) participants; 785 (94·4%) participants were followed up to a minimum 36 months. Median overall length of follow up was 55·4 months (range 0 - 82·5, IQR 46·7-66·7, n = 832) (Fig. 1, Supplementary Figure 1). Follow up duration remained similar across trial arms, and according to whether a primary outcome event was reported or not (Supplementary Table 3).
Fig. 1.
Flow diagram and timing of participants’ original and extended follow-up.
*Note post 18 m HES data was included for these participants based on post 18 m HES data obtained during the original trial follow-up period. This data was not included in the original 18-month analysis.
3.2. Reported attendances
A total of 4359 previously unreported HES episodes were retrieved and linked resulting in 3479 unique complete hospital attendances (seven previously reported via researcher only). Of these, 333 (9·6%) were classified as self-harm, 1600 (46·0%) non self-harm, and 1546 (44·4%) were unclassified (Supplementary Figure 2).
Including 89 unclassified attendances remaining from the original 18-month follow-up, a total of 1635 unclassified attendances required targeted researcher follow up; 408 (25·0%) high and 1227 (75·0%) low priority. Unclassified attendances were reported across 103 different providers, of which 1284 (78·5%) took place in 34 providers with approval for researcher follow up. Of these 1284 attendances, 976 were followed up by the researcher, who contacted 271/318 (85·2%) high priority, and 705/966 (73·0%) low priority attendances. Of those followed up 99/271 (36·5%) high priority and 91/705 (12·9%) low priority were found to be self-harm related.
Over the entire follow-up period (including original 18-month follow up), 4985 attendances were reported, compared to 1513 in the original 18-month follow-up: 927 (18·6%) vs 404 (26·7%) due to self-harm, 3383 (67·9%) vs 1011 (66·8%) not due to self-harm, and 675 (13·5%) vs 98 (6·5%) unclassified respectively.
3.3. Repetition of self-harm leading to hospital attendance (original primary outcome)
Over the entire follow-up period, a total 916 hospital attendances (excluding 11 minor injury or walk-in centre attendances) following self-harm were reported in 334 (40·1%) of 832 young people; 427 events in 168 (40·5%) of 415 in the FT group and 489 events in 166 (39·8%) of 417 in the TAU group (Table 1).
Table 1.
Details of self-harm events.
| Family therapy N | Treatment as usual N | Total N | |
|---|---|---|---|
| Number of participants | 415 | 417 | 832 |
| N participants with one or more self-harm event | 168 (40.5%) | 166 (39.8%) | 334 (40.1%) |
| Estimated self-harm repetition rate (Kaplan Meier estimate, 95% CI) | |||
| 18 months | 28.9% (24.5%, 33.3%) | 25.2% (21.0%, 29.4%) | 27.1% (24.0%, 30.1%) |
| 36 months | 36.5% (31.8%, 41.2%) | 35.4% (30.8%, 40.1%) | 36.0% (32.7%, 39.3%) |
| N events per participant | |||
| Mean (SD) | 1.0 (2.19) | 1.2 (3.22) | 1.1 (2.76) |
| Median (range) | 0.0 (0, 22) | 0.0 (0, 39) | 0.0 (0, 39) |
| IQR | (0, 1) | (0, 1) | (0, 1) |
| N events per participant | |||
| 0 | 247 (59.5%) | 251 (60.2%) | 498 (59.9%) |
| 1 | 75 (18.1%) | 75 (18.0%) | 150 (18.0%) |
| 2-3 | 66 (15.9%) | 53 (12.7%) | 119 (14.3%) |
| 4-5 | 14 (3.4%) | 23 (5.5%) | 37 (4.4%) |
| 6+ | 13 (3.1%) | 15 (3.6%) | 28 (3.4%) |
| Type of self-harm per participanta(not mutually exclusive) | |||
| Self-injury | 72 (17.3%) | 75 (18.0%) | 147 (17.7%) |
| Self-poisoning | 122 (29.4%) | 124 (29.7%) | 246 (29.6%) |
| Self-injury and poisoning | 18 (4.3%) | 22 (5.3%) | 40 (4.8%) |
| Other (Threats/Thoughts/Risk) | 30 (7.2%) | 28 (6.7%) | 58 (7.0%) |
| Missing | 13 (3.1%) | 15 (3.6%) | 28 (3.4%) |
| No self-harm event | 247 (59.5%) | 251 (60.2%) | 498 (59.9%) |
| Total number of events | 427 | 489 | 916 |
| Type of self-harm | |||
| Self-injury | 128 (30.0%) | 160 (32.7%) | 288 (31.4%) |
| Self-poisoning | 216 (50.6%) | 238 (48.7%) | 454 (49.6%) |
| Self-injury and poisoning | 20 (4.7%) | 27 (5.5%) | 47 (5.1%) |
| Other (Threats/Thoughts/Risk) | 42 (9.8%) | 44 (9.0%) | 86 (9.4%) |
| Missing | 21 (4.9%) | 20 (4.1%) | 41 (4.5%) |
| Outcome of self-harm eventsb | |||
| Discharged from A&E | 174 (40.7%) | 216 (44.2%) | 390 (42.6%) |
| Admitted to hospital ward | 253 (59.3%) | 273 (55.8%) | 526 (57.4%) |
| Admission involves a psychiatric inpatient stay? | |||
| Yesc | 16 (6.3%) | 23 (8.4%) | 39 (7.4%) |
| No | 237 (93.7%) | 250 (91.6%) | 487 (92.6%) |
| Total Admissions | 253 (100%) | 273 (100%) | 526 (100%) |
Of 184 participants with more than one self-harm event, 98 (53.3%) used multiple methods, 86 (46.7%) used a single method (excluding threats as an alternative method).
The 390 events discharged from A&E and the 526 admission events were in 187 (22.5%) and 249 (29.9%) participants respectively.
The 39 psychiatric admissions were in 23 (2.8%) participants.
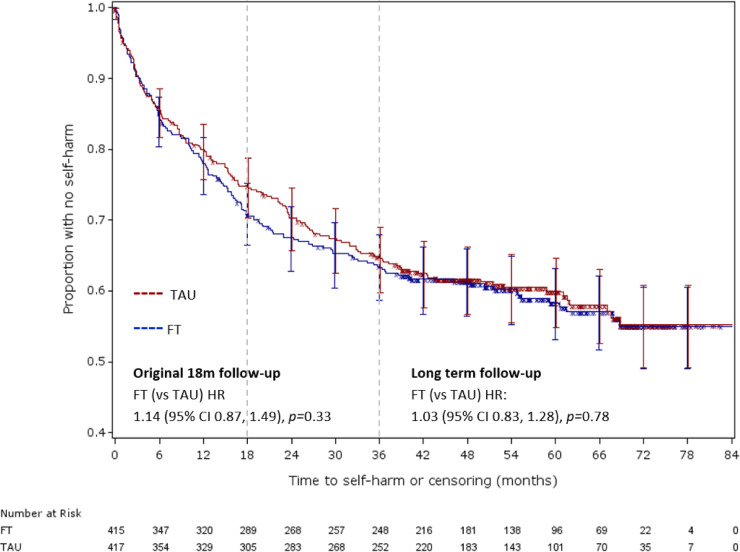
Self-harm repetition can be seen to continue at a similar rate beyond the original 18-month follow-up period (Fig. 2), with Kaplan Meier estimated self-harm rates (Table 1) of 27·1% (95% CI: 24·0%, 30·1%) at 18 months, increasing to 36·0% (95% CI: 32·7%, 39·3%) at 36 months post-randomisation. The Kaplan Meier curves for FT and TAU can be seen to be at their most divergent around 18 months post-randomisation, the timing of original primary analysis, before converging from 36 months.
Fig. 2.
Kaplan-Meier plot of time to self-harm by Randomised Treatment group with 95% CIs.
Consistent with the original 18-month follow-up, whilst the estimated HR (1·03, 95% CI: 0·83, 1·28, p-value=0·78) represents a marginally increased rate of self-harm in FT compared to TAU, there is no evidence to suggest a statistically or clinically significant difference in self-harm repetition rates between treatment groups over the duration of the extended follow-up (Table 2).
Table 2.
Cox Proportional Hazards Model (adjusted for covariates) for time to first event.
| Full long-term follow-up |
||||||
|---|---|---|---|---|---|---|
| Original 18-month follow-up |
Primary analysis |
Exploratory analysis – Gender* Age interaction |
||||
| Hazard Ratio (95% CI) | p-value | Hazard Ratio (95% CI) | p-value | Hazard Ratio (95% CI) | p-value | |
| Treatment: FT (vs. TAU) | 1.14 (0.87, 1.49) | 0.33 | 1.03 (0.83, 1.28) | 0.78 | 1.03 (0.83, 1.28) | 0.77 |
| Gender: female (vs. male) | 1.60 (0.98, 2.61) | 0.059 | 1.22 (0.86, 1.73) | 0.25 | 0.028 | |
| 11-14 years | 1.76 (1.06, 2.91) | |||||
| 15-17 years | 0.78 (0.48, 1.27) | |||||
| Age group: 15–17 (vs. 11–14) | 0.70 (0.53, 0.92) | 0.011 | 0.7 (0.56, 0.88) | 0.0019 | 0.28 | |
| Females | 0.64 (0.50, 0.81) | |||||
| Males | 1.44 [0.74, 2.77) | |||||
| Gender*Age: Female*15-17 | 0.022 | |||||
| Previous self-harm episodes: ≥ 3 (vs. 2) | 1.22 (0.78, 1.92) | 0.39 | 1.16 (0.81, 1.66) | 0.42 | 1.13 (0.79, 1.63) | 0.495 |
| Type of index episode: | 0.033 | 0.015 | 0.015 | |||
| Combined (vs. Injury) | 1.83 (1.14, 2.96) | 1.80 (1.20, 2.70) | 1.81 (1.21, 2.71) | |||
| Poisoning (vs. Injury) | 1.03 (0.69, 1.54) | 1.11 (0.79, 1.54) | 1.13 (0.81, 1.59) | |||
| Referred via hospital: yes (vs. no) | 1.31 (0.93, 1.86) | 0.12 | 1.03 (0.77, 1.37) | 0.86 | 1.00 (0.75, 1.34) | 0.9975 |
| NHS Trust | 0.094 | 0.0078 | 0.0095 | |||
Repeated self-harm was less common in participants who were 15 years or older and more common in participants with an index episode combining self-injury and poisoning. A significant effect on the risk of self-harm, irrespective of treatment arm, was detected for the NHS Trust where the patient was located (p = 0·0078). Whilst weak evidence of an increased rate of self-harm in females was detected in the original 18-month follow-up, this effect was reduced within the extended follow up. Further investigation detected a significant interaction between age and gender, with younger females more likely to repeat self-harm (p = 0·022, Supplementary Figure 3). Sensitivity analyses yielded similar results (Supplementary text and Supplementary Figure 4) (i.e. using an alternative modelling strategy for centre investigating the impact of remaining unclassified attendances).
3.4. Moderation
Our extended follow-up found a similar trend for the moderating effect of caregiver-reported affective involvement, and for young person-reported unemotional traits on treatment effect, as detected at 18 months. Affective involvement problems increased the risk of self-harm to a greater degree in TAU (HR 1·5, 95% CI 1·10–2·03) than in FT (HR 1.06, 95% CI 0·75–1·49). As difficulty in talking about feelings increased, the risk of self-harm decreased in TAU (HR 0·93, 95% CI 0·88–0·99) and increased in FT (HR 1·05, 95% CI I 0·98–1·12). However there was no longer evidence of a statistically significant treatment interaction for either moderator (p = 0.1361, p = 0.2731).
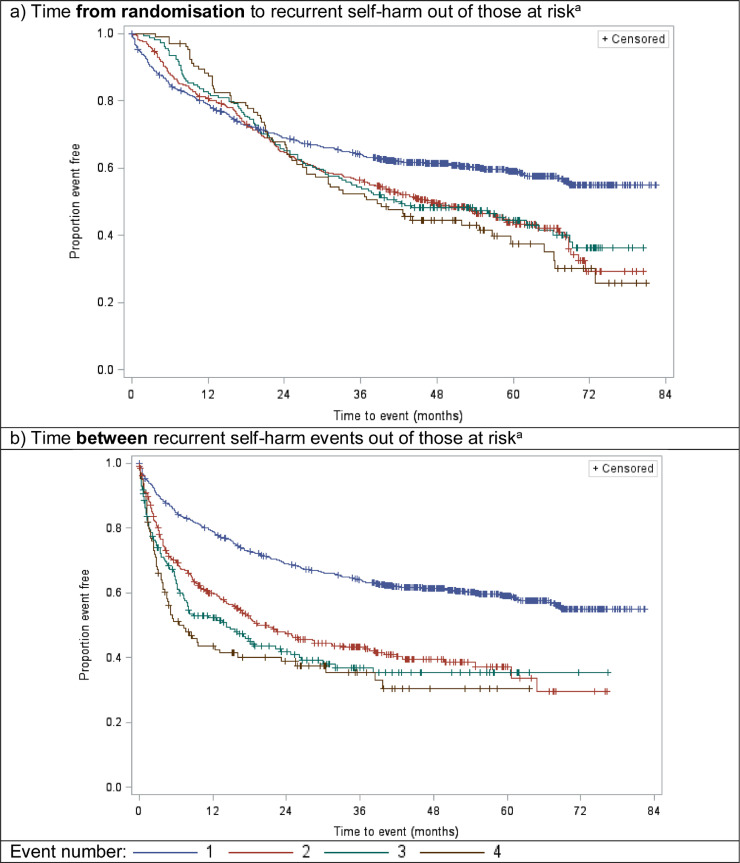
3.5. Characteristics of further episodes of self-harm leading to hospital attendance
Time to recurrent self-harm events (up to the fourth event per participant) is shown in Kaplan-Meier plots in Fig. 3, from (a) randomisation, and (b) the previous self-harm event. The at-risk population comprises all participants for the first event, and participants with a preceding event for subsequent events, i.e. only those with a first event are at risk of a second event. Having a first event substantially increased the risk of having a second, with subsequent events of a similar risk (Fig. 3a). Time to subsequent events decreased with each event (Fig. 3b). Similar findings were observed across trial arms (not presented).
Fig. 3.
Kaplan–Meier plot of time to recurrent self-harm events (up to 4 events) (a) from randomisation, and (b) between self-harm events.
Recurrent event analysis (Supplementary Table 4) over the extended follow up of the participants found no evidence to suggest a statistically significant difference in the rate of recurrent events between the arms (HR 0·86, 95% CI: 0·63, 1.19, p-value=0·3746). In contrast to the analysis of the first event in the extended follow-up, the number of previous self-harm episodes was highly significant with an increased rate of recurrent self-harm in those with three or more self-harm episodes at baseline (HR 2·05, 95% CI: 1·35, 3·12, p-value=0·0008) and there was a higher rate of self-harm in those referred via hospital (HR 1·64, 95% CI 1·04, 2·61, p-value=0·0348).
3.6. All cause morbidity and mortality
Over the extended follow-up period, two participants were reported to have died, between three and four years post randomisation. Both participants were allocated to FT; neither death was related to self-harm.
A total of 4058 hospital attendances for reasons other than self-harm (including unclassified attendances), were reported over the extended follow-up period, for 333 (80·2%) participants in the FT arm and 343 (82·3%) in TAU; with a median of three attendances per participant in both arms, and a mean of 4·9 (SD 6·58). A&E attendances resulting in discharge were more common than admissions: 627 (75·4%) participants attended A&E and were discharged. 416 (50%) participants had a hospital admission, with a mean of 3·2 A&E attendances and 1·6 admissions per participant (Supplementary Table 5).
Exploratory analysis found that participants with a primary outcome self-harm event during follow-up were more likely to attend hospital for other non-self-harm reasons (Odds Ratio: 2·32, 95% CI 1·57-3·44, p-value < 0·001) and more often than those without a primary outcome event. This was consistent for both A&E attendances and hospital admissions, and across trial arms, with no evidence of a statistically significant difference between trial arms.
3.7. Non-self-harm hospital admissions
Similar admission rates according to ICD-10 diagnosis classification were observed across trial arms (Supplementary Tables 6 and 7).
Rates of admission were higher across almost all ICD-10 classifications in participants with a primary outcome self-harm hospital attendance; in particular for mental and behavioural disorders (ICD-10 F01-F99), and symptoms, signs, abnormal clinical & lab findings (ICD-10 R00-R99). Considering all mental health related ICD-10 codes, diagnosis codes for A&E attendances leading to admission, and researcher-reported details, 486 (35·9%) admissions in 239 (28·7%) participants contained a mental health related diagnosis. In participants with a primary outcome event this included 335 (48%) admissions in 143 (42·8%) participants; compared to 151 (23%) admissions in 96 (19·3%) participants without a primary outcome event. Excluding psychoactive substance use, 337 (24·9%) admissions in 172 (20·7%) participants received a mental health related diagnosis (Table 3).
Table 3.
Non self-harm hospital admissions for mental health related reasons (excluding self-harm events) by trial arm and primary outcome event status during overall follow-up.
| Family therapy |
Treatment as usual |
Total |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Primary outcome self-harm event? | Primary outcome self-harm event? | Primary outcome self-harm event? | |||||||
| Mental Health related admission* | Yes | No | Total | Yes | No | Total | Yes | No | Total |
| N participants | 168 | 247 | 415 | 166 | 251 | 417 | 334 | 498 | 832 |
| Yes (Including substance use F10-F19⁎⁎) | 77 (45.8%) | 40 (16.2%) | 117 (28.2%) | 66 (39.8%) | 56 (22.3%) | 122 (29.3%) | 143 (42.8%) | 96 (19.3%) | 239 (28.7%) |
| Yes (Excluding substance use F10-F19) | 64 (38.1%) | 24 (9.7%) | 88 (21.2%) | 53 (31.9%) | 31 (12.4%) | 84 (20.1%) | 117 (35.0%) | 55 (11.0%) | 172 (20.7%) |
| N admissions | 382 | 283 | 665 | 316 | 374 | 690 | 698 | 657 | 1355 |
| Yes (Including substance use F10-F19) | 164 (42.9%) | 70 (24.7%) | 234 (35.2%) | 171 (54.1%) | 81 (21.7%) | 252 (36.5%) | 335 (48.0%) | 151 (23.0%) | 486 (35.9%) |
| Yes (Excluding substance use F10-F19) | 114 (29.8%) | 39 (13.8%) | 153 (23.0%) | 135 (42.7%) | 49 (13.1%) | 184 (26.7%) | 249 (35.7%) | 88 (13.4%) | 337 (24.9%) |
Excludes admissions for self-harm (primary outcome events).
F10-F19 refer to the disease classification codes in ICD-10 [15].
3.8. Adversity related hospital admissions
Approximately 260 (31·3%) participants had one or more emergency admission for adversity related injury for self-harm, violence, drug or alcohol abuse (girls 28·9%, boys 31·9%), accounting for 88% of all emergency admissions for injury (girls 89·5%, boys 76·2%), and 28·3% of all admissions (girls 27·6%, boys 37·5%) (Supplementary Table 8). This compares to approximately 4·3% (n = 141,248) of adolescents in the general population (n = 3,254,046) with one or more emergency admissions for adversity related injury (girls 4·6%, boys 4·1%), accounting for 50% of all emergency admissions for injury in girls and 29·1% in boys [16,17].
4. Discussion
This trial tested the impact of a specifically adapted and manualised family therapy intervention for self-harming adolescents. In young people who had self-harmed more than once and had done so recently, at 36 months follow up, and throughout the complete extended follow-up period we found no clinical benefits for FT over TAU in reducing hospital attendance due to subsequent repetition of self-harm. At 18 months, repetition curves were diverging but our extended follow up shows that from month 24 repetition rates begin to converge again, with no difference from month 42.
However, a number of important clinical implications arise from the findings. Firstly, rates of self-harm continued from 18 to 36 months, at much the same rate as they did from 0 to 18 months, although the risk of repetition is probably highest in the first 12 months. Lack of repetition at 18 months should not be seen as an indication of no further risk of repetition.
Secondly, across the whole trial cohort we found a reduced rate of repeated self-harm in older participants aged 15-17 compared to those aged 11 – 14, suggesting a reduction in self-harm repetition as adolescence proceeds. This is consistent with other findings, with similar results in the ASSIST trial [18].
Thirdly we found two important indicators of repetition risk with a significantly increased rate of self-harm in participants whose index episode combined self-injury and poisoning compared to those with self-injury only, and a significant interaction between age and gender, with younger females more likely to repeat self-harm – as has been shown in other studies [2,19].
Fourthly, analysis of all self-harm episodes leading to hospital attendance showed that having a second self-harm event (bearing in mind this group had already self-harmed at least twice prior to randomisation) substantially increased the risk of having a third, and the time to subsequent events decreased with each event. In contrast to the 18-month primary analysis of the first event, there was a higher rate of recurrent self-harm in those with three or more self-harm episodes at baseline compared to those with two.
There was a significant difference in the rate of repeat self-harm across study centres, with participants recruited from some centres significantly less likely to repeat self-harm and more likely in others. This finding was irrespective of treatment arm and could have been be due to a variety of reasons – random variation, differences in population, differences in type and quality of therapy offered, however, with the data available it is not possible to draw firm conclusions.
Finally, participants with a primary outcome self-harm event during follow up were more likely to attend hospital for reasons other than self-harm and more often than those without a primary outcome event and were more likely to have a mental and behavioural disorder diagnostic code linked with their admission. Herbert et al. [17] reported that the risk of death from suicide or from drug or alcohol related causes was significantly higher in young people who had an emergency hospital admission following adversity related injury. In the present study, a far higher proportion of participants were admitted following adversity related injury than in the national cohort of Herbert et al., suggesting an even higher risk of death from suicide or from a drug or alcohol related cause.
This is the largest trial of a self-harm intervention and one of the largest ever conducted in CAMHS for any condition. The use of hospital episode statistics and ONS mortality data demonstrates their feasibility and potential as objective outcome measures in studies of this type and led to very high ascertainment (additional primary outcome data after 18 months on 804/832 [96·6%] participants; linkage rate of 766/771 [99·4%] participants further submitted to NHS Digital). Follow-up extending up to 82·5 months post-randomisation (median of 55·4 months) and a similar duration of follow-up across both trial arms are further strengths.
We have previously reported that the trial sample presented with levels of difficulty at least as severe as the average UK CAMHS referral and that TAU was broadly comparable to CAMHS practice in the UK [6].
Although the routine data we collected indicated that only 20·7% of participants (excluding those with a psychoactive substance use diagnosis) received a mental health related diagnosis, this may reflect the use of data which is derived from the involvement of non-psychiatric staff in acute hospitals who may be reluctant to commit to formal diagnoses. It should be noted that at baseline our sample had relatively high rates of emotional and behavioural problems generally (66% scored high or very high on the Strengths and Difficulties Questionnaire) and for depression in particular (66% scored moderately depressed or above on the Children's Depression Rating Scale) [6].
Limitations, in addition to those cited at 18 month follow up [6], include the differential lengths of follow-up for participants for whom the acquisition of further HES data was not possible, remaining unclassified attendances, and the resource and length of time required to achieve approval and to conduct researcher follow-up of unclassified attendances. A further limitation may have been an inadequate ‘dose’ of SHIFT FT. Treatment length was informed by the typical length of treatment offered in UK CAMH services so as to ensure broadly equal amounts of contact in this pragmatic trial. This issue is addressed in more detail in the original trial publication [6].
Although conclusions about the primary outcome with respect to treatment differences are unchanged, this extended follow-up confirmed a number of factors that predict repetition in this at-risk clinical group. Clinicians should exercise more caution with younger girls, those with multiple past self-harm events, and those who combine self-poisoning with self-injury. In a young person who has self-harmed, attendance at hospital for any reason may be an indicator of risk but those who re-present with an adversity-related injury may be at particular risk.
The Multicentre Study of Self-harm in England investigated mortality following self-harm [20] collected data on all patients aged 18 years and under who presented with self-harm to general hospital emergency departments in Oxford (one), Manchester (three) and Derby (two) for the 8-year period 1 January 2000 to 31 December 2007. As in the present study, self-harm was defined as intentional self-poisoning or self-injury, irrespective of type of motivation including degree of suicidal intent. No data are available about interventions offered to this cohort, although it is unlikely that all were offered treatment. Follow up until 31 December 2010 for 5133 of the 5205 (98·6%), using national mortality registers (median follow-up period, 6 years), showed that overall, 51 (1%) had died by the end of the follow-up period, nearly half by suicide or probable suicide (undetermined cause) (N = 25, 49·0%), a quarter (25·5%) with an accidental verdict, and a quarter (25·5%) due to other causes. In our study, over a similar follow up period (median 55 months), but with a more at-risk group (as all SHIFT participants had self-harmed at least twice before randomisation), two (0·2%) deaths were reported. Numbers are too small to draw firm conclusions, but this finding raises the possibility that treatment of any sort may reduce subsequent mortality.
We continue to argue that future research related to adolescent self-harm needs to explore the characteristics of specific sub-groups within the self-harming population. As it is still not clear yet what works for whom in this population, the adoption of newer methods such as micro- trials may help in the optimisation of treatments offered [21] although such methods may not be able to deal with the heterogeneity in the target population. Additional options such as the modelling of large datasets that include therapy data might also be considered. The findings of this study also make the case that intervention trials in child and adolescent mental health need longer follow-up periods to inform evidence-based services.
Data sharing statement
Individual participant data (with any relevant supporting material, e.g. data dictionary, protocol, statistical analysis plan) for all trial participants (excluding any trial-specific participant opt-outs) will be made available for secondary research purposes according to a controlled access approach. Data will only be made available in such a way that data recipients cannot identify individuals by any reasonably likely means, and we will only share data for projects that are clearly in the public interest and compatible with the original purpose of the data processing. No data will be released before an appropriate agreement is in place setting out the conditions of release.
The primary outcome was derived using data supplied by NHS Digital (DARS-NIC-325074-F0J3D). The data sharing agreement between University of Leeds and NHS Digital permits use of data for the specific purpose of this project and use of any other purpose will require approval from NHS Digital.
The study protocol is in the public domain and referenced in this manuscript. Requests to access trial data should be made to CTRU-DataAccess@leeds.ac.uk in the first instance.
Contributors
The SHIFT trial was conceived by the trial team in response to a call by the NIHR HTA programme for a study investigating the clinical and cost-effectiveness of family therapy for adolescents who self-harm (HTA 07/33). This long term follow up was designed by DC, IE, SF, AH, DO, MS, JG, AF and AWH. DC, IE, and JG led the research teams in Yorkshire, London and Greater Manchester, respectively. MK contributed to the design of the original trial for which this was a follow up. AW-H provided statistical input into the trial design, implementation, Statistical Analysis Plan, and undertook the statistical analysis under the supervision of AF. VM led the implementation of the extended follow-up, acquisition of trial data, trial monitoring, GCP and reporting requirements. ST designed the health economics analysis and had oversight of the economic evaluation.
All authors (excepting MK, deceased) contributed to the writing of the report and had the opportunity to revise prior to submission.
Declaration of Competing Interest
All authors received funding from NIHR HTA to conduct this study
DC is Co-chair of the NIHR Advanced Fellowship Panel and a co-author of the SHIFT Manual
AF was a member of the NIHR HTA Clinical Evaluation & Trials Board and the HTA Commissioning Strategy Group until December 2018
JG is an NIHR Senior Investigator
AH is a member of the NIHR Advanced Fellowships Panel and a sub-panel member for NIHR Programmes for Applied Health Research
IE was a co-author of the SHIFT Manual
ST is a member of the NIHR Programmes for Applied Health Research
MS has received personal fees as co-author of the book Cutting Down: a CBT Workbook for Treating Young People Who Self-harm
Acknowledgments
Acknowledgements
This research was funded by the National Institute for Health Research Health Technology Assessment programme (project number: 07/33). The views expressed in this publication are those of the authors and do not necessarily reflect those of the HTA programme, NIHR, NHS, or the Department of Health. The authors would like to thank the trial researchers, staff from the Clinical Research Networks, and other staff from the Leeds Clinical Trials Research Unit for their commitment to SHIFT. The authors would also like to thank all those authors on the original trial publication who made significant contributions to the original study but were not directly involved with this long term follow up. We thank the members of the SHIFT TSC and DMEC.
In particular, we wish to express our thanks to the young people and their families who agreed to participate in the study.
Role of the Funding Source
The funder commissioned the original trial of family therapy following self-harm in adolescents and subsequently funded an extended follow-up, but had no role in study design, data collection, analysis, interpretation, or writing of this paper. The corresponding author had full access to all data in the study and had final responsibility for the decision to submit for publication.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2019.100246.
Appendix. Supplementary materials
References
- 1.Evans E., Hawton K., Rodham K., Psychol C., Deeks J. The prevalence of suicidal phenomena in adolescents: a systematic review of population‐based studies. Suicide Life Threat Behav. 2005;35(3):239–250. doi: 10.1521/suli.2005.35.3.239. [DOI] [PubMed] [Google Scholar]
- 2.Geulayov G., Casey D., McDonald K.C. Incidence of suicide, hospital-presenting non-fatal self-harm, and community-occurring non-fatal self-harm in adolescents in England (the iceberg model of self-harm): a retrospective study. Lancet Psychiatry. 2018;5(2):167–174. doi: 10.1016/S2215-0366(17)30478-9. [DOI] [PubMed] [Google Scholar]
- 3.Hawton K., Saunders K.E., O'Connor R.C. Self-harm and suicide in adolescents. Lancet North Am Ed. 2012;379(9834):2373–2382. doi: 10.1016/S0140-6736(12)60322-5. [DOI] [PubMed] [Google Scholar]
- 4.Hawton K., Witt K.G., Taylor-Salisbury T.L. Interventions for self-harm in children and adolescents. Cochrane Database Syst Rev. 2015;(12) doi: 10.1002/14651858.CD012013. Art. No.: CD012013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ougrin D., Tranah T., Stahl D., Moran P., Asarnow J.R. Therapeutic interventions for suicide attempts and self-harm in adolescents: systematic review and meta-analysis. J Am Acad Child dolesc Psychiatry. 2015;54(2):97–107. doi: 10.1016/j.jaac.2014.10.009. . e2. [DOI] [PubMed] [Google Scholar]
- 6.Cottrell D.J., Wright-Hughes A., Collinson M. Effectiveness of systemic family therapy versus treatment as usual for young people after self-harm: a pragmatic, phase 3, multicentre, randomised controlled trial. Lancet Psychiatry. 2018;5(3):203–216. doi: 10.1016/S2215-0366(18)30058-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wright-Hughes A, Graham E, Farrin A. Self-Harm Intervention: family Therapy (SHIFT), a study protocol for a randomised controlled trial of family therapy versus treatment as usual for young people seen after a second or subsequent episode of self-harm. Trials. 2015;16(1):1. doi: 10.1186/s13063-015-1007-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hawton K, Harriss L. Deliberate self-harm by under-15-year-olds: characteristics, trends and outcome. J Child Psychol Psychiatry. 2008;49(4):441–448. doi: 10.1111/j.1469-7610.2007.01852.x. [DOI] [PubMed] [Google Scholar]
- 9.Boston P., Eisler I., Cottrell D. University of Leeds; Leeds: 2009. Systemic family therapy manual for adolescent self-harm. [Google Scholar]
- 10.Masterson C., Barker C., Jackson D., Boston P. Constructing a SHIFT adherence measure (SAM): the development of a family therapy integrity measure for the SHIFT trial. J Family Therapy. 2016;38:274–290. [Google Scholar]
- 11.Wright-Hughes A., Graham E., Cottrell D., Farrin A. Routine hospital data – is it good enough for trials? An example using England's Hospital Episode Statistics in the SHIFT trial of Family Therapy vs. Treatment as Usual in adolescents following self-harm. Clin Trials. 2017;15(2):197–206. doi: 10.1177/1740774517751381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andersen P.K., Gill R.D. Cox's regression model for counting processes: a large sample study. TAnn Stat. 1982:1100–1120. [Google Scholar]
- 13.Prentice R.L., Williams B.J., Peterson A.V. On the regression analysis of multivariate failure time data. Biometrika. 1981;68(2):373–379. [Google Scholar]
- 14.Landis J, Heyman E, Koch G. Average Partial association in three-way contingency tables: a review and discussion of alternative tests. Int Stat Rev. 1978;46:237–254. [Google Scholar]
- 15.World Health O . 2nd ed. World Health Organization; Geneva: 2004. ICD-10: international statistical classification of diseases and related health problems: tenth revision. ed. [Google Scholar]
- 16.Herbert A., Gilbert R., González-Izquierdo A., Li L. Violence, self-harm and drug or alcohol misuse in adolescents admitted to hospitals in England for injury: a retrospective cohort study. BMJ Open. 2015;5(2) doi: 10.1136/bmjopen-2014-006079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Herbert A., Gilbert R., Cottrell D., Li L. Causes of death up to 10 years after admissions to hospitals for self-inflicted, drug-related or alcohol-related, or violent injury during adolescence: a retrospective, nationwide, cohort study. Lancet North Am Ed. 2017;390(10094):577–587. doi: 10.1016/S0140-6736(17)31045-0. [DOI] [PubMed] [Google Scholar]
- 18.Green J., Wood A., Kerfoot M. Group therapy for adolescents with repeated self harm: randomised controlled trial with economic evaluation. BMJ. 2011;342:d682. doi: 10.1136/bmj.d682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Diggins E., Kelley R., Cottrell D., House A., Owens D. Age-related differences in self-harm presentations and subsequent management of adolescents and young adults at the emergency department. J Affect Disord. 2017;208:399–405. doi: 10.1016/j.jad.2016.10.014. [DOI] [PubMed] [Google Scholar]
- 20.Hawton K., Bergen H., Kapur N. Repetition of self‐harm and suicide following self‐harm in children and adolescents: findings from the Multicentre Study of Self‐harm in England. J Child PsycholPsychiatry. 2012;53(12):1212–1219. doi: 10.1111/j.1469-7610.2012.02559.x. [DOI] [PubMed] [Google Scholar]
- 21.Klasnja P, Hekler EB, Shiffman S. Microrandomized trials: an experimental design for developing just-in-time adaptive interventions. Health Psychol. 2015;34S(0):1220–1228. doi: 10.1037/hea0000305. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.