Abstract
Background.
There exists little literature on the outcomes of the medical management of men with erectile dysfunction (ED) with no overt organic etiology.
Aim.
This study was conducted to assess the outcomes of men with non-organic ED treated medically.
Methods.
All patients had normal hormone profiles and vascular assessment. All were given a trial of a PDE5 inhibitor. If no improvement was experienced, intracavernosal injection therapy (ICI) was administered. All patients were encouraged to seek a consultation with a mental health professional.
Outcomes.
Patient demographics, medical comorbidities, hormone and hemodynamics assessment, and change in International Index of Erectile Function (IIEF) scores of patients were recorded.
Results.
116 men with a mean age or 38±19 (range 16–57) years were studied. 21% had mild ED, 47% moderate and 32% severe. 21% had seen a psychiatrist. 81% of patients responded to PDE5i with a penetration hardness erection on follow-up (mean duration of 7±3 months postcommencement of PDE5i). However, only 68% of these were capable of a consistently good response. The mean EF domain score on PDE5i for the entire group improved from 18±11 to 22±6 (p=0.01) and for PDE5i responders, it was 27±4 (p<0.001). 28% of men (22 PDE5i failures and 10 with a mixed response to PDE5i) attempted ICI, all obtaining consistently functional erections. At a mean time point of 11±5 months, 83% of those responding to PDE5i had ceased using PDE5i due to a lack of need. 11% of those using ICI continued to use them 6 months after starting ICI; the remainder had been transitioned back to PDE5i. Of the 29 patients in the latter sub-group, 66% were no longer using PDE5i consistently due to a lack of need.
Clinical Implications.
Not all men with non-organic ED respond to PDE5i initially and many of those who respond, do so only intermittently; such patients are potentially curable, using erectogenic pharmacotherapy for erectile confidence restoration most men are capable of being weaned from drug therapy.
Strengths & Limitations.
The strengths of the study are the large number of patients and the use of serial validated instruments to assess erectile function outcomes. As a weakness, despite normal hormone and vascular assessments, the diagnosis of non-organic ED is still a presumptive one.
Conclusions.
Medical management of non-organic ED utilizing the process of care model results in cure in a large proportion of such patients. The transient use of ICI in some patients permits successful PDE5i rechallenge.
Keywords: Non-organic erectile dysfunction, erectile dysfunction, PDE5 inhibitor, intracavernosal injections
INTRODUCTION
Erectile dysfunction (ED) is the persistent inability to achieve or maintain an erection satisfactory for sexual performance. The absence of overt risk factors for organic ED and the presence of normal hormone and vascular assessments suggest adrenaline-mediated ED, also termed non-organic ED[1]. Despite numerous studies on psychological treatment for men with non-organic ED, there are few series within the literature assessing the outcomes of men with such ED treated via medical management.[2] Most patients with ED, regardless of the etiology, suffer from fear, anxiety, worry, depression, and distress because of their erectile impairment.[3]
While non-organic ED frequently occurs in association with psychiatric disorders[4–6], specifically anxiety and depression, clinical experience demonstrates that the majority of men with this condition do not have a specific psychiatric disorder but rather suffer from situational (performance) anxiety) at the time of sexual relations. The incidence of patients with non-organic ED is variable (10–25%) in studies looking at all-cause ED. [7, 8] Psychological approaches for such ED have included anxiety reduction and desensitization procedures, cognitivebehavioral interventions, guided sexual stimulation techniques, and couples’ or relationship counseling. [9]
PDE5 inhibitors (PDE5i) are recognized as first-line therapy according to the process of care model [10]. With the tolerability, ease-of-use, and effectiveness of PDE5i, medical therapy with or without psychological intervention, has become the mainstay of therapy for men with non-organic ED at our center. [11, 12]. This study aimed to communicate our experience in the management of men with non-organic ED using erectogenic pharmacotherapy without the use of psychological interventions.
METHODS
Study Population:
Men presenting with ED with no risk factors for organic ED who had normal androgen profiles and a normal vascular study constituted the study population. The clinical features of this population included: absence of a history of penile/perineal trauma, sudden onset ED, situational ED, excellent nocturnal erections and intermittency of function. The data presented are based upon a review of a prospectively constructed sexual medicine database of all subjects presenting with ED to a sexual medicine clinic. With Institutional Review Board approval, we retrospectively analyzed this database for males who presented for the evaluation of ED. The review included demographic characteristics, medical comorbidity data, as well as ED risk factors, vascular and hormonal analyses, and any prior therapies. A history of any psychiatric disorder (depression, psychosis, anxiety and/or personality disorders, etc.) were considered exclusions for this analysis.
Patient Evaluation:
Men presenting with ED underwent early morning (before 10 am) testing for serum total testosterone and gonadotropins as well as vascular assessment using duplex Doppler penile ultrasound (DUS) to exclude organic causes of ED. Patients had normal total testosterone levels (>300ng/dl). DUS was conducted using a vasoactive agent-redosing schedule (papaverine 30mg/ml, phentolamine 1mg/ml, PGE1 10 mcg/ml). On DUS, the achievement of an erection equivalent to the best erection achievable at home without the use of erectogenic medication was required for inclusion. The criteria for normalcy on DUS included a peak systolic velocity (PSV) >30cms/s and an end-diastolic velocity (EDV) <5 cms/s [13]. Arteriogenic ED was deemed to be present when PSV was abnormal with a normal EDV; venogenic ED (corporo-veno-occlusive dysfunction, venous leak) was deemed present when the EDV was abnormal with a normal PSV; mixed vascular insufficiency was diagnosed when both PSV and EDV values were abnormal
Clinical Care Pathway:
All patients diagnosed with non-organic ED were initially treated with a PDE5 inhibitor (PDE5i). Maximum dose was prescribed, and careful instructions for use were given. The patient was encouraged to try the first two attempts without a partner to minimize anxiety and to establish confidence in the medication. They were also urged to try the medication on at least four attempts and to titrate down for side effects or when an excellent erection was achieved with maximum dose. All patients were encouraged to seek mental health support and were followed up serially, initially 3 months after diagnosis and then every 6 months. If the PDE5i failed or gave an inconsistent response, patients were encouraged to try intracavernosal injection (ICI) therapy. If they chose to pursue this, two in-office training sessions were conducted. Patients were commenced on trimix and the dose was titrated by a nurse practitioner by phone in response to rigidity and duration achieved. Those using ICI were re-challenged with PDE5i after 3–6 months of ICI. Weaning was performed in the following fashion: if patients were on injections, they were transitioned to oral therapy starting at maximum dose. On the first occasion that they tried the medication they were encouraged to try this on their own before integrating it into a sexual encounter. If patients were using maximum dose PDE5i, they were instructed to use half maximum dose and then in a step-wise fashion titrate down to quarter maximum dose. The first attempt at each new dose, they were encouraged to try on their own.
Erectile Function Assessment:
Patients were administered the International Index of Erectile Function (IIEF) pre-PDE5i treatment and serially at each follow-up visit. The IIEF instrument is a validated inventory that has been used extensively in the evaluation of erectile function, particularly in response to pharmacotherapy. The questionnaire has 15 questions. Questions 1–5 and 15 are organized into an erectile function domain, which is scored 6–30. The questions ask about sexual function in frequency terms, and each is scored on a 5-point Likert scale, 5 indicating ‘always or almost always’ and 1 ‘never or almost never.’ A score ≥26 indicates the absence of ED and a score ≤10 defines severe ED.
Statistics:
All statistical analyses were performed using SPSS for Windows, 10.1 (SPSS inc., Chicago, IL, USA). Pre-treatment and post-treatment IIEF domain scores were evaluated with paired t-tests. P-values less than 0.05 were deemed significant.
RESULTS
Study Population:
116 men are included in this analysis. Mean age was 38±19 (range 16–57) years. 31% were partnered with a mean relationship duration of 8±13 months. With regard to vascular risk factors (diabetes, hypertension, dyslipidemia, coronary artery disease, obesity, cigarette smoking), 14% of the cohort had a single vascular comorbidity (10% dyslipidemia, 4% hypertension), 2% had two vascular risk factors (dyslipidemia plus hypertension) but 84% had none. Despite being encouraged to seek mental health support, only 21% actually saw a psychologist. Of the 24 men who saw our psychologist, all except 3 saw him for a single visit.
Patient Evaluation:
To obtain a diagnosis of non-organic ED, all vascular and hormone studies were required to be normal. On DUS, mean PSV=48±12 cm/s, EDV=1.1±1, RI=0.97±0.06. Mean total testosterone level was 472±148 ng/dl and LH 3.6±2.8 IU/ml.
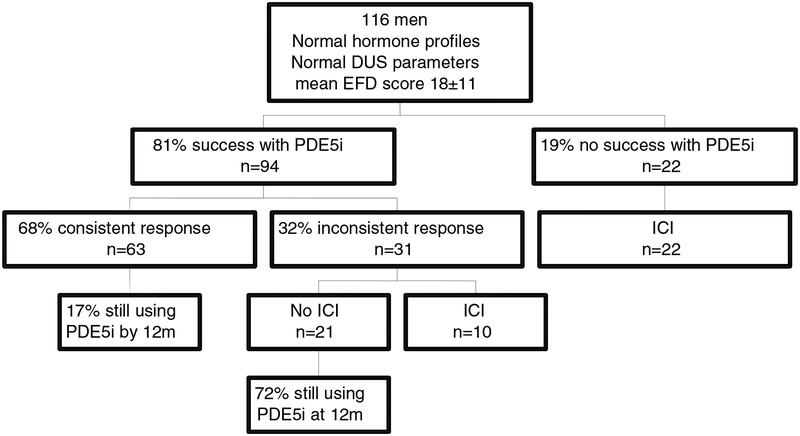
Erectile Function Outcomes (Figure 1):
Figure 1:
Erectile Function Outcomes
PDE5i use was: sildenafil 86%, tadalafil 10%, vardenafil 4%. Eighty-one percent of patients had responded to PDE5i with a penetration hardness erection at last follow-up (mean duration of 7±3 months post PDE5i commencement), however only 68% of these (55% of the entire cohort) were capable of a consistently good response. 28% of men (n=32) including the 22 PDE5i failures and 10 of those failing to get a consistently good response using PDE5i attempted ICI. 100% of those using ICI obtained consistently functional erections. At a mean time point of 11±5 months after the date of the DUS, 83% of those responding consistently to PDE5i had ceased using PDE5i because of the consistent ability to function without a pill. 11% of those using ICI continued to use them 6 months after starting; the remainder were transitioned to PDE5i. Of the 29 patients in the latter sub-group, 66% were no longer using PDE5i consistently at last follow-up because of the consistent ability to function without a pill.
IIEF-EF domain score at baseline was 18±11, 21% had mild ED, 47% moderate, and 32% severe. The scores for the remaining domains were: libido 4±3, orgasm 7±1, intercourse satisfaction 9±2 and overall satisfaction 5±2 (Table 1). The mean EF domain score on PDE5i for the entire group was 22±6 (p=0.01 vs. baseline) but for those responding consistently to PDE5i it was 27±4 (p<0.001). For medication responders, the scores for the remaining domains were: libido 7±3 (p<0.01), orgasm 8±3 (p=NS), intercourse satisfaction 12±4 (p<0.05) and overall satisfaction 7±4 (p=NS). The number seeing the psychologist for more than a single visit was too low to assess the effect of such consultation on outcomes.
Table 1:
IIEF Data
| Erectile Function (30) | 18±11 | 27±4 | <0.001 |
| Libido (10) | 4 ±3 | 7±3 | <0.01 |
| Orgasm (10) | 7±1 | 8±3 | 0.27 |
| Intercourse satisfaction (15) | 9±2 | 12±4 | <0.05 |
| Overall Satisfaction (10) | 5±2 | 7±4 | 0.38 |
DISCUSSION
Historically, ED has been classified into non-organic (psychogenic), organic (neurologic, vascular or hormonal causes) or mixed, although some effort has been made to move away from this nosology. Non-organic ED has historically been a diagnosis of exclusion whereby the clinicians make sure there are no overt underlying organic etiologies. Although primary organic etiology accounts for about 80% of cases, psychological factors are also important contributing factors [11, 14]. Epidemiologic studies looking at the prevalence of a psychosocial factor in men with ED have found it present up to 40% [15, 16]. In the Massachusetts Male Aging Study, ED was associated with self-reported depressive symptoms (OR=2.88), negative outlook on life (OR=2.3) or pessimistic attitudes (OR=3.89). [6] Depressed mood was found to be a significant predictor of ED, even after controlling for potential confounding factors. [5]
The diagnosis of non-organic ED should only be made after taking a thorough history, performing a physical examination and performing appropriate testing [11]. The basic adjunctive testing includes laboratory testing and to be definitive a well-conducted vascular assessment, most often performed using penile duplex Doppler ultrasonography, is an important aid to this diagnosis. In our study, all patients had normal hormone and vascular evaluations. When a diagnosis of non-organic ED is entertained, the presence of specific psychological stressors should be sought. For the practicing urologist, this is often difficult to determine in the limited office time available and the lack of mental health training during urology training.
PDE5i have been shown to be efficacious and well tolerated in multiple trials and for various etiologies of ED including diabetes, radical prostatectomy, hypertension, spinal cord injuries, cardiovascular disease, and depression. [17–22] In a study of two pivotal, randomized, double-blind, placebo-controlled clinical trials enrolling 1,385 men from the ED population randomized to placebo, Vardenafil 5mg, 10mg or 20mg during a 3 month period, IIEF-EF domain scores and the proportion of ‘yes’ responses to the Sexual Encounter Profile improved with medication for all etiologies of ED. 13–16% of patients were classified as having non-organic ED (termed psychogenic ED in this trial). These patients were noted to have the highest IIEF scores and SEP ‘yes’ rates after 12 weeks of treatment. On Vardenafil 10mg, 92% of the non-organic ED cohort indicated that the treatment had improved their erections on the global assessment question. [23] These results have been replicated for other PDE5i medications. In a study of 141 men with ED, looking at the efficacy of sildenafil and success of treatment among varied etiologies, 23% were classified as non-organic ED. [2] Of this group, 87% benefited from the treatment.
In a study of 136 patients with ED and clinically diagnosed depression, sildenafil was compared to placebo [4]. Mean scores for IIEF questions concerning the ability to achieve (question #3) and maintain (question #4) erections were significantly higher in men receiving sildenafil than in men receiving placebo (p<0.001). In response to the global assessment question (GAQ), 91% of the men receiving Sildenafil reported that treatment had improved their erections compared with 11% of men receiving a placebo. Moreover, improvement in ED was highly correlated with change in depressive symptoms.
The success of PDE5I was not replicated in all studies of patients with non-organic ED. In 266 combat-exposed war veterans with ED, all of whom had clinically diagnosed post-traumatic stress disorder; a double-blind, randomized, placebo-controlled study was performed to elucidate the efficacy and safety of sildenafil in this population. Patients were evaluated over 16 doses of either placebo or sildenafil 100mg doses via IIEF, SEP, Erectile Dysfunction Inventory of Treatment Satisfaction questionnaire and a GAQ. Sildenafil did not produce greater improvement over placebo in any of the outcome measures (p=0.08). A normal EF domain score (≥ 26) at end-of-treatment was reported by 10% and 8% of patients on the sildenafil and placebo regimens, respectively (p=0.09).
Men with non-organic ED may have such adrenaline discharge during sexual relations that oral agents may not lead to a functional erection. This is supported by our data, where 19% of men failed to respond to a PDE5i initially, and one-third of the responders did so only intermittently. There does not exist any literature on the use of ICI in men in this population. Furthermore, there is no data on the ability to wean men from pharmacotherapy, as outlined in our analysis.
PDE5i has been shown to have an excellent safety profile with a low incidence of severe adverse events. [23, 24] These agents were well tolerated in our population. Furthermore, while ICI is associated with the development of priapism especially in men with normal veno-occlusive function (as was the case in our entire study population), not a single patient in our population experienced priapism. The clinical implications of this study are obvious: (i) not all men with non-organic ED respond to PDE5i initially and many of those who respond, do so only intermittently (ii) such patients are potentially curable and using erectogenic pharmacotherapy for erectile confidence restoration most men are capable of being weaned from drug therapy (iii) very few such men are comfortable utilizing mental health professional support despite our strong recommendation and the presence of such a person in our practice.
The strengths of the study are the large number of patients and the use of serial validated instruments to assess erectile function outcomes. As a weakness, despite normal hormone and vascular assessments, the diagnosis of non-organic ED is still a presumptive one. Furthermore, the follow-up may be considered short-term. Indeed, it would be interesting to know what happens to such men years after their diagnosis, especially during the commencement of a new sexual relationship. Also, none of the patients had psychological input, so the exact psychological status of the patients is unknown.
CONCLUSIONS
Medical management of non-organic ED utilizing the clinical care pathway outlined results in the ability of many such patients to cease requiring ED medication assistance. The use of PDE5i and the temporary use of ICI in PDE5i failure patients can restore confidence such that a successful PDE5i rechallenge is likely and furthermore many men can wean completely from erectogenic pharmacotherapy.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- [1].Lizza EF, Rosen RC. Definition and classification of erectile dysfunction: report of the Nomenclature Committee of the International Society of Impotence Research. Int J Impot Res. 1999;11: 141–3. [DOI] [PubMed] [Google Scholar]
- [2].Basar M, Tekdogan UY, Yilmaz E, et al. The efficacy of sildenafil in different etiologies of erectile dysfunction. Int Urol Nephrol. 2001;32: 403–7. [DOI] [PubMed] [Google Scholar]
- [3].Jannini EA, McCabe MP, Salonia A, Montorsi F, Sachs BD. Organic vs. psychogenic? The Manichean diagnosis in sexual medicine. J Sex Med. 2010;7: 1726–33. [DOI] [PubMed] [Google Scholar]
- [4].Seidman SN, Roose SP, Menza MA, Shabsigh R, Rosen RC. Treatment of erectile dysfunction in men with depressive symptoms: results of a placebo-controlled trial with sildenafil citrate. Am J Psychiatry. 2001;158: 1623–30. [DOI] [PubMed] [Google Scholar]
- [5].Araujo AB, Durante R, Feldman HA, Goldstein I, McKinlay JB. The relationship between depressive symptoms and male erectile dysfunction: cross-sectional results from the Massachusetts Male Aging Study. Psychosom Med. 1998;60: 458–65. [DOI] [PubMed] [Google Scholar]
- [6].Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB. Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. The Journal of urology. 1994;151: 54–61. [DOI] [PubMed] [Google Scholar]
- [7].Melnik T, Abdo CH. Psychogenic erectile dysfunction: comparative study of three therapeutic approaches. J Sex Marital Ther. 2005;31: 243–55. [DOI] [PubMed] [Google Scholar]
- [8].Deveci S, O’Brien K, Ahmed A, et al. Can the International Index of Erectile Function distinguish between organic and psychogenic erectile function? BJU international. 2008;102: 354–6. [DOI] [PubMed] [Google Scholar]
- [9].Rosen RC. Psychogenic erectile dysfunction. Classification and management. Urol Clin North Am. 2001;28: 269–78. [DOI] [PubMed] [Google Scholar]
- [10].Rosen RC. The process of care model for evaluation and treatment of erectile dysfunction. International journal of impotence research. 1999;11: 59. [DOI] [PubMed] [Google Scholar]
- [11].Levine LA. Diagnosis and treatment of erectile dysfunction. Am J Med. 2000;109 Suppl 9A: 3S-12S; discussion 29S-30S. [DOI] [PubMed] [Google Scholar]
- [12].Aubin S, Heiman JR, Berger RE, Murallo AV, Yung-Wen L. Comparing Sildenafil alone vs. Sildenafil plus brief couple sex therapy on erectile dysfunction and couples’ sexual and marital quality of life: a pilot study. J Sex Marital Ther. 2009;35: 122–43. [DOI] [PubMed] [Google Scholar]
- [13].Aversa A, Bruzziches R, Spera G. Diagnosing erectile dysfunction: the penile dynamic colour duplex ultrasound revisited. International journal of andrology. 2005;28 Suppl 2: 61–3. [DOI] [PubMed] [Google Scholar]
- [14].DeWire DM. Evaluation and treatment of erectile dysfunction. Am Fam Physician. 1996;53: 2101–8. [PubMed] [Google Scholar]
- [15].Melman A, Tiefer L, Pedersen R. Evaluation of first 406 patients in urology department based Center for Male Sexual Dysfunction. Urology. 1988;32: 6–10. [DOI] [PubMed] [Google Scholar]
- [16].Aydin S, Unal D, Erol H, et al. Multicentral clinical evaluation of the aetiology of erectile dysfunction: a survey report. Int Urol Nephrol. 2001;32: 699–703. [DOI] [PubMed] [Google Scholar]
- [17].Rendell MS, Rajfer J, Wicker PA, Smith MD. Sildenafil for treatment of erectile dysfunction in men with diabetes: a randomized controlled trial. Sildenafil Diabetes Study Group. JAMA: the journal of the American Medical Association. 1999;281: 421–6. [DOI] [PubMed] [Google Scholar]
- [18].Zagaja GP, Mhoon DA, Aikens JE, Brendler CB. Sildenafil in the treatment of erectile dysfunction after radical prostatectomy. Urology. 2000;56: 631–4. [DOI] [PubMed] [Google Scholar]
- [19].Kloner RA, Brown M, Prisant LM, Collins M. Effect of sildenafil in patients with erectile dysfunction taking antihypertensive therapy. Sildenafil Study Group. Am J Hypertens. 2001;14: 70–3. [DOI] [PubMed] [Google Scholar]
- [20].Hultling C, Giuliano F, Quirk F, et al. Quality of life in patients with spinal cord injury receiving Viagra (sildenafil citrate) for the treatment of erectile dysfunction. Spinal Cord. 2000;38: 363–70. [DOI] [PubMed] [Google Scholar]
- [21].Olsson AM, Persson CA. Efficacy and safety of sildenafil citrate for the treatment of erectile dysfunction in men with cardiovascular disease. Int J Clin Pract. 2001;55: 171–6. [PubMed] [Google Scholar]
- [22].Nurnberg HG, Gelenberg A, Hargreave TB, et al. Efficacy of sildenafil citrate for the treatment of erectile dysfunction in men taking serotonin reuptake inhibitors. Am J Psychiatry. 2001;158: 1926–8. [DOI] [PubMed] [Google Scholar]
- [23].Donatucci C, Eardley I, Buvat J, et al. Vardenafil improves erectile function in men with erectile dysfunction irrespective of disease severity and disease classification. J Sex Med. 2004;1: 301–9. [DOI] [PubMed] [Google Scholar]
- [24].Safarinejad MR, Kolahi AA, Ghaedi G. Safety and efficacy of sildenafil citrate in treating erectile dysfunction in patients with combat-related post-traumatic stress disorder: a double-blind, randomized and placebo-controlled study. BJU Int. 2009;104: 376–83. [DOI] [PubMed] [Google Scholar]