Abstract
Food security, nutrition, and clean water are important factors for health and well-being, particularly for people living with HIV. Global gender inequalities, including women’s dependence on men for food and financial support, lack of access to control over land and resources, and responsibilities providing for children and family members likely shape the experience and impacts of food insecurity among women living with HIV. We performed a systematic review of the impact of food insecurity on sexual risk behaviors and antiretroviral therapy (ART) adherence among women living with HIV. We searched PubMed, CINAHL, PsycINFO, and Sociological Abstracts for peer-reviewed articles through February, 2016. Secondary reference searching was conducted on included studies. Studies were eligible for inclusion if they presented primary data, either qualitative or quantitative, for women living with HIV and described the associations between food insecurity and ART adherence, safer sex, or sexual risk behaviors. Data extraction was conducted in duplicate, including assessment of study rigor. Six studies met the inclusion criteria, four from sub-Saharan Africa and two from North America. Food insecurity was associated with increased sexual risk through transactional sex and lack of ability to negotiate safer sex. Findings also identified hunger and food insecurity as a barrier to ART initiation and adherence. The limited number of studies identified suggests that more research is needed on the relationship between food insecurity and key outcomes among women living with HIV. Results reinforce the need for multidimensional programming and policies that address poverty, gender inequality, food insecurity, and HIV simultaneously.
Keywords: food insecurity, HIV, ART, women, adherence, sexual risk behaviors
Introduction
HIV and food insecurity have profound implications on the health and well-being of populations across the globe. Food insecurity has been defined as existing when “the availability of nutritionally adequate and safe foods or the ability to acquire acceptable foods in socially acceptable ways is limited or uncertain.”[1] A growing body of literature suggests an association between food insecurity and HIV prevalence.[2, 3]
Among people living with HIV, food insecurity has been linked to a variety of negative health and behavioral outcomes. Food insecurity is associated with poor clinical outcomes, including lower CD4 counts,[4–6] increased opportunistic infections[7] and hospitalizations,[7, 8] and decreased bioavailability and efficacy of antiretroviral therapy (ART),[9] leading to a more rapid disease progression. In addition, food insufficiency has been associated with incomplete viral load suppression[5, 10, 11] and increased risks of mortality even on ART.[10, 12, 13] Researchers are increasingly recognizing that the link between food insecurity and HIV is bidirectional.[14–16] For example, food insecurity is associated with an increased reliance on social networks for food and monetary resources,[17] while lack of social support due to HIV stigma worsens food insecurity and increases poor health outcomes.[18] Additionally, studies have established ties between food insecurity and decreased ART adherence[19] and subsequent elevated risks of inadequate viral load suppression, drug resistance, and difficulty remaining healthy for people living with HIV.[20–22] There are side effects associated with taking ART on an empty stomach and ART may be less effective at sustaining CD4 levels among individuals who are suffering from malnutrition or food insecurity.[23] Lack of clean and safe drinking water also has implications for the health and well-being of people living with HIV who are more prone to opportunistic infections and thus need access to clean drinking water.[24–26] A systematic review published in 2015 identified substantial evidence tying food insecurity to suboptimal ART adherence in populations of both men and women.[27]
While numerous studies have examined food insecurity among people living with HIV, most do not focus on differences by gender. The impact of food insecurity on the lives of people living with HIV is likely to disproportionately affect women because of gender inequalities facing women.[24, 28] Women are more vulnerable to risks of food insecurity given their lack of access to and control over resources including land, employment, and money. Their primary role within families in preparing food and feeding families and children shape the impacts of food insecurity. In addition, women living with HIV often face particular challenges, resulting in increased vulnerability not only because of requirements related to adequate food and nutrition needed to adhere to ART, but also because pregnant and lactating women living with HIV may have additional nutritional requirements.[29] Food insecurity can have other consequences related to sexual and reproductive health for women, such as an increased risk of mother-to-child transmission of HIV among pregnant women living with HIV.[30, 31] Several studies have identified food insecurity as a motivation for HIV-negative women to engage in transactional sex to obtain food and/or resources, or to engage in sex work,[32–35] thereby increasing their risk for HIV. A large study from Botswana and Swaziland found that food insufficiency was correlated with both inconsistent condom use with a non-primary partner and intergenerational sexual relationships.[35] The correlation between food insecurity and HIV risk behaviors was also observed in a study of sexually active women in Brazil, which found food insecurity to be associated with reduced odds of consistent condom use in the past year and condom use at last sex.[34]
To inform the World Health Organization Guideline on the sexual and reproductive health and rights of women living with HIV, we conducted a systematic review of the impact of food insecurity on sexual risk behaviors and ART adherence among women living with HIV. Our goal was to review the literature on these relationships and inform strategies for creating an enabling environment that will address the sexual and reproductive health needs of women living with HIV and ensure that HIV and food security are jointly considered in the implementation of policies and programs.
Methods
We used systematic search and screening methods to identify articles examining the relationship between food insecurity and sexual risk behaviors and ART adherence among women living with HIV.
Inclusion criteria
To be included in the review, an article had to meet the following criteria:
Presented primary data, either qualitative or quantitative, collected among women living with HIV
Described the associations between food insecurity and ART adherence, safer sex, or sexual risk behaviors
Published in a peer-reviewed journal prior to the search date of February 18, 2016
No restrictions were placed based on type of population (specific sub-populations of women living with HIV) or location of the study. We excluded studies conducted among people living with HIV that did not stratify data by gender.
Search strategy
We searched the following electronic databases to identify articles for inclusion: PubMed, CINAHL (Cumulative Index to Nursing and Allied Health Literature), PsycINFO, and Sociological Abstracts. We also conducted secondary reference searching on all studies included in the review. We did not include search terms around the concepts of adherence and sexual risk behavior in order to broaden the search and avoid missing potentially relevant articles.
The following terms were used in the search for PubMed and adapted for each database: (“HIV positive” [tiab] OR “living with HIV” [tiab] OR “HIV infected” [tiab]) AND (Women’s Health [mesh] OR women [tiab] OR woman[tiab] OR female* [tiab] OR gender[tiab]) AND (“food security” [tiab] OR “food insufficiency” [tiab] OR “food insecurity” [tiab] OR hunger [tiab] OR “food scarcity” OR (“food security” AND “risk”))
Screening abstracts
Titles, abstracts, citation information, and descriptor terms of citations identified through the search strategy were screened by a member of the study staff. Full text articles were obtained of all selected abstracts and final decisions on inclusion were made by two members of the study team. All articles underwent data abstraction in duplicate with differences in interpretation between reviewers resolved through discussion. Rigor for quantitative studies was assessed using an approach designed for multiple study designs in the field of HIV research by the Evidence Project.[36, 37] Qualitative studies were not assessed for study rigor given the challenges of using checklists to assess rigor of qualitative studies, but we did consider aspects of rigor where appropriate.[38]
Results
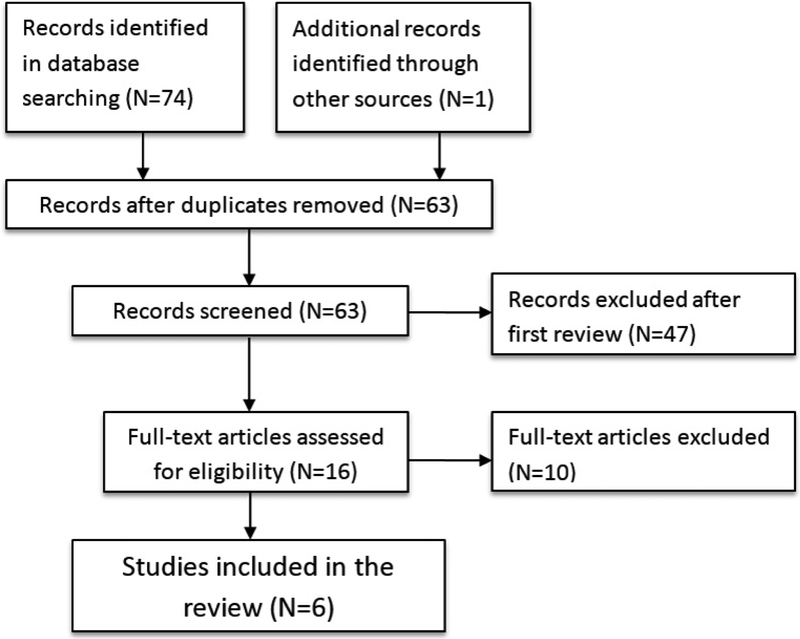
Of 63 unique articles identified through the database search, 6 articles ultimately met the inclusion criteria for the review (Figure 1). Included studies came from Canada, Swaziland, Uganda, Zambia, Democratic Republic of Congo, and the United States (Table 1). Five qualitative studies[39–43] and one prospective cohort study[44] were included. While the majority of the qualitative studies relied on in-depth interviews to uncover main themes among study populations, one study used free listing techniques and key informant interviews to elicit results.[42] In the prospective cohort study, loss to follow-up was not reported. People living with HIV who inject drugs were surveyed at baseline and every 6 months for 2 years; data were drawn from 470 participants who completed at least one follow-up survey (1310 total observations), and the analysis was adjusted for potential confounders.[44] Findings are summarized narratively by major themes below.
Figure 1.
Disposition of study citations through the search and screening process
Table 1.
Descriptions of included studies
| Author Year | Location/setting and Population | Study objective | Study design and Methods | Sample size and Food security status | Outcomes |
|---|---|---|---|---|---|
| Fielding-Miller et al., 2014 |
Location: Four sites in Swaziland: a rural border town, a peri-urban community, and two side in the urban Manzini-Mbabane corridor Population: HIV-positive female sex workers |
Self-identified female sex workers were recruited for participation in this study through purposive and snowball sampling in order to examine the relationship between food insecurity and risky sexual practices. |
Study design:
Qualitative Participant selection: Purposive Sampling Methods: Two semi-structured in-depth interviews were conducted with each participant. |
Sample size:
Total: 20 Food security status: Not specified |
Relevant Themes:
|
| Miller et al., 2011 |
Location:
Mbarara, Uganda Population: HIV-positive adults both on and off ARV treatment |
Interviews were conducted with people living with HIV attending an ARV distribution clinic in Mbarara, Uganda, in order to examine the relationship between food insecurity and risky sexual behaviors. |
Study design:
Qualitative Participant selection: Purposive Sampling Methods: Semi-structured in-depth interviews |
Sample Size:
Total: 41 Women: 25 Men: 16 Food security status: Not specified |
Relevant Themes:
|
| Murray et al., 2009 |
Location:
Urban Zambia Population: HIV-positive pregnant and breastfeeding women attending an HIV clinic |
Conducted among women involved in the Zambia Exclusive Breastfeeding Study (ZEBS), this cohort study examined mother to child transmission of HIV through breast milk to uncover barriers to ART adherence. |
Study design:
Qualitative Participant selection: Purposive Sampling Methods: Free listing and key informant interviews |
Sample size:
Total: 80 Free listing: 47 Key informant interviews: 33 Food security status: Not specified |
Relevant Themes:
|
| Musumari et al., 2014 |
Location:
Kinshasa, Democratic Republic of Congo Population: HIV-positive adults on ART, those on ART after an interruption, and those who had been off ART for 3+ consecutive months. |
Interviews were conducted with people living with HIV of different treatment profiles to identify barriers and facilitators of ART adherence in Kinshasa, DRC. |
Study design:
Qualitative Participant selection: Purposive Sampling Methods: Semi-structured in-depth interviews |
Sample Size:
Total: 38 Women: 24 Men: 14 Food security status: 42.1 % reported having irregular meals (≤1 meal/day) |
Relevant Themes:
|
| Peretti-Watel et al., 2006 |
Location: France Population: HIV-infected patients at hospital departments delivering HIV care |
A national cross-sectional study was conducted among a random stratified sample HIV patients to investigate the correlates of non-adherence to ART. |
Study design:
Cross-sectional Participant selection: Random stratified sampling |
Sample size: Total: 1809 Women: 408 Men: 1401 Food security status: 17.2% of heterosexual women living with HIV (70/408) experienced food privation in the household in the prior four weeks |
ART adherence: Among heterosexual women living with HIV who reported food privation in the household in the prior four weeks, 56% were non-adherent to ART and 44% were adherent (p=0.04); among those who did not report food privation, 43% were non-adherent to ART and 57% were adherent. (OR = 1.30, 95%CI: 0.79–2.14) |
| Shannon et al., 2011 |
Location:
Vancouver, Canada Population: HIV-positive people who inject drugs both on and not on HAART |
HIV-positive people who inject drugs in inner city Vancouver were recruited through snowball sampling and street outreach to participate in a prospective observational cohort study, also known as the AIDS Care Cohort to evaluate Exposure to Survival Services, 2005–2008 |
Study design:
Prospective Cohort Participant selection: Non-random Follow-up time: Observations taken every six months between Dec 2005 and May 2009 |
Sample size: Total: 470 Women: 183 Men: 287 Food security status: 39% of those severely food insecure were women and 38% of those not severely food insecure were women (No difference between men and women p=0.789) |
Behavioral Outcomes: Unprotected sex (vaginal and/or anal) and severe food insecurity Unadjusted OR: 2.98 (1.56–5.05) p<0.10 Adjusted OR: 2.68 (1.49–4.82) p<0.10 * Adjusted for age, sex/gender, married/cohabitating partner, binge drug use, homelessness, and HAART use Unprotected sex (vaginal and/or anal) among females Unadjusted OR: 1.54 (1.00–2.37) p<0.10 Adjusted OR: 1.5 (1.02–2.22) p<0.10 * Adjusted for age, sex/gender, married/cohabitating partner, binge drug use, homelessness, and HAART use |
| Whittle et al., 2015 |
Location:
San Francisco and Alameda County, CA, United States Population: Low-income people living with HIV |
Semi-structured in-depth interviews were conducted with participants recruited from a program providing 3 meals a day with the aim of documenting experiences with food insecurity and risky sexual practices. |
Study design: Qualitative Participant selection: Purposive Sampling Methods: Semi-structured in-depth interviews |
Sample Size:
Total: 34 Women: 6 Men: 28 Food security status: Not specified but all participants were receiving daily food assistance |
Relevant Themes:
|
Food insecurity and sex as a means of economic survival through transactional sex and sex work
Three studies found that food insecurity directly contributed to women’s decision to engage in sex in exchange for resources and food, either through transactional sex or through sex work.[39–41] A qualitative study from Uganda among women living with HIV found that many women relied on transactional sex as a survival tool to buy food, which was not considered “prostitution.”[39] Participants in the study (6 men and 26 women living with HIV) distinguished women who had sex for food from “prostitutes” who were generally viewed as women in bars and urban settings who sought out one-time customers. Women reported receiving multiple solicitations from men for sex in exchange for food or resources. Women whose husbands or primary partners had died – particularly those with children – were especially targeted by men for transactional sex. Although knowledge of a woman’s HIV status did not always deter men from offering food in exchange for sex, other women reported feeling hesitant to disclose their HIV status to a new sexual partner for fear they would be rejected and therefore unable to provide for themselves or their children.
In a qualitative study with 20 female sex workers living with HIV in Swaziland, hunger was frequently cited as both the main reason for initiating sex work and as the primary motivation to continue to sell sex.[40] Similar to the findings from Uganda, single women with children in Swaziland were especially vulnerable to food shortages and as a result, engaged in transactional sex as a means to feed and support their families. Many women described their introduction into sex work as precipitated by the death or departure of a partner. Though women originally entered sex work to cope with hunger, few women in the study identified themselves as currently food secure. Both HIV and sex work are stigmatized in Swaziland and many women worried they would lose support, including food, from family and friends if they disclosed either their HIV status or their occupation. The authors described the women’s situations as a “cycle of food insecurity, HIV risk, and social marginalization.”
A third qualitative study conducted in the San Francisco Bay area of the United States among low-income HIV positive men and women found that women and men who have sex with men resorted to transactional sex with men in times of food insecurity.[41] Women in this population described how absolute lack of food and severe hunger acted as motivators to sell sex. High rent in urban areas and homelessness was also found to be a driver of transactional sex for food and shelter. A notable difference between these transactional relationships and those found in resource-poor countries included in this review is that they were generally not long-term arrangements.
Food insecurity and lack of control in sexual relationships
Four studies found that food insecurity was related to a lack of control in sexual relationships. In the study from Uganda described above, women living with HIV with primary partners often reported a lack of control in their sexual relationships due to their reliance on their male partners for food.[39] Some women reported that their male sexual partners would deny food sources in order to control the circumstances around sex, including the timing. Many women stayed in high-risk violent or abusive relationships because of their dependence on partners for food. This was particularly true for women with children and women living far from family who could provide assistance. This lack of control prevented women from successfully negotiating condom use, with many women reporting being threatened with losing access to food or even violence if they insisted on using condoms.
In the qualitative study from Swaziland, female sex workers living with HIV also reported food insecurity as a barrier to condom use.[40] Clients were often willing to pay more for sex without a condom, which was hard to refuse in the face of hunger. Many of the women believed that they had contracted HIV through lack of condom use during sex. Similarly, the qualitative study conducted in San Francisco, United States, described how food insecurity led to a decreased ability to insist on protection during sexual encounters.[41] Women also described how their experiences with transactional sex sometimes forced them to compromise their safety by engaging with clients with whom they did not feel comfortable.
A fourth study among both men and women living with HIV who inject drugs in Vancouver, Canada found no difference in food insecurity by sex, but women had 1.5 times the odds of reporting unprotected sex compared to men.[44] Controlling for sex, people who were severely food insecure had nearly three times the odds of condom-less sex compared to those who were not severely food insecure (adjusted odds ratio (aOR): 2.68, 95% confidence interval (CI): 1.49–4.82).
Food insecurity as a barrier to ART initiation and adherence
A study in Zambia investigated factors related to the decision to initiate and adhere to ART among urban women with access to free comprehensive HIV care.[42] In this qualitative study involving a sample of 47 women living with HIV, hunger emerged as a key barrier to consistently taking medication. Participants discussed the difficulty of eating sufficient quantities of food and the associated negative side effects of treatment. Many women believed that it was better not to start ART due to fears that the drugs increased appetite and many had limited access to food. Relatedly, several women described lack of financial independence, unemployment, and dependence on a husband or partner for resources as barriers to accessing food. Hunger and lack of food also emerged as major themes for why women stopped taking their ART. Women complained that they became hungry when taking ART and needed to eat a lot or that the medication made them vomit up the little food they did have.
A qualitative study in the Democratic Republic of Congo exploring factors influencing adherence among HIV-positive adults with different treatment profiles (currently on ART, on ART re-initiation following an interruption, and lost to follow-up) found similar results.[43] Women in this sample cited lack of food as the most significant barrier to daily ART adherence and the main reason for treatment interruptions. Participants described increased side effects experienced when taking ART without food and many believed that treatment was ineffective or harmful when taken without sufficient quantities of food. These intensified side effects and beliefs impeded adherence.
Though the female sex workers living with HIV in the Swaziland study did not directly address food insecurity and ART medication adherence, many discussed the difficulty in taking ART on an empty stomach.[40] Some women feared that inability to obtain food could lead to a deterioration of their health, motivating some to continue to engage in sex work. Local clinics advised them to eat “healthy foods” to manage their HIV infection and women often talked about “healthy food” when asked how they coped with their HIV status, but had different conceptions of what that entailed.
Discussion
There is some evidence that people living with HIV who begin antiretroviral therapy without adequate nutrition have lower survival rates.[45, 46] For women living with HIV, particularly from poorer communities, treatment adherence is even more important since economic or social dependency may lead them to engage in high-risk situations such as transactional or commercial sex or staying in high-risk or abusive sexual relationships. Despite the extensive amount of literature published on HIV, we identified only six studies evaluating the relationship between food insecurity and sexual risk behaviors and ART adherence among women living with HIV. Studies included populations of pregnant and breastfeeding women, sex workers, people who inject drugs, and women both on and off ART. Study design and rigor varied across studies with five qualitative studies and one prospective cohort study. Results suggest that food insecurity remains a very real problem for many women living with HIV across diverse settings, resulting in risky coping strategies like transactional sex and sub-optimal ART adherence.
Findings from this review indicate that food insecure women living with HIV often engage in transactional sex and sex work in order to obtain resources and food for themselves and their families. Our findings among women are consistent with previous research on food insecurity and sexual risk conducted among both men and women living with HIV in high-resource settings.[41, 47, 48] The correlation between food insecurity and HIV-risk behaviors has also been extensively studied among HIV-negative populations across various settings.[32–35, 49–54] A study conducted in South Africa found that economic survival strategies, which included transactional sex with non-primary partners, were associated with a 1.5-fold increased risk of HIV infection.[32] Food insecurity has been cited as a significant motivator for women to enter sex work and as a barrier to condom use despite high rates of HIV awareness.[33, 40]
This review also found that food insecurity serves as a barrier to ART initiation and adherence. Again, our findings among women align with a larger evidence base linking food insecurity and sub-optimal adherence among both men and women living with HIV across a variety of settings.[5, 12, 55–59] In a systematic review conducted in 2015 with results not stratified by gender, nine of thirteen studies presenting an adjusted effect estimate found a statistically significant correlation between food insecurity and ART non-adherence.[27] Several plausible mechanisms for this relationship have been suggested, including fears or experiences of increased hunger on ART, fears of intensified side effects of ART if taken without adequate food, and having to choose between buying food and accessing ART (often causing people to sell or trade ART for food or resources) and other medical care, resulting in poor treatment retention.[60] People living with HIV are often advised to “eat healthy foods” by health care workers and health promotion campaigns,[61] yet some people must choose between paying for ART or paying for food.[62] Conversely, a prospective cohort study conducted among 602 treatment-naïve people in Uganda found that initiating ART was linked with reduced odds of food insecurity, perhaps due to improved mental and physical health and increased ability to work.[63] These findings, along with substantial evidence linking food insecurity with HIV risk behaviors and ART adherence, point to the bidirectionality and syndemicity of food security and risk behaviors like non-adherence and condomless sex or transactional sex.[14–16, 63] While this systematic review did not examine other aspects or consequences of food insecurity, there may also be other important health consequences that merit further research. For instance, food insecurity could be related to maternal and infant health, stress, depression, or violence against women living with HIV.
The particular risks of food insecurity and transactional sex as well as links to adherence and initiation of ART must be understood within the context of gender inequalities. Globally, women are often dependent on men for food and financial support. Women are less likely to have access to and control over land (for food production and income generation), employment, money and other economic resources (e.g. inheritance)[64, 65] In many settings, women also have primary roles in procuring/buying, preparing food, and feeding children, other family members and community members in ways that might shape the impacts of food insecurity on their ability to adhere to ART or their reasons for engaging in sexual risk behaviors. Similarly, in many settings where clean and safe drinking water is not available, it is the primary responsibility of women to travel long distances in search of clean water and to transport clean water, requiring them to carry heavy loads and walk long distances.[25, 66–68] The role of women in securing food, water, preparing meals and feeding families also places a heavy burden on their time as shown by time use surveys.[68] This “time poverty” has implications for their ability to take care of their own health and wellbeing. For women living with HIV, the stigma and discrimination related to HIV status pose additional burdens as they face the risk of being abandoned, deprived of family property, land, inheritance and housing in ways that increase their food insecurity.[64, 65]
Findings of this review must be understood in light of certain limitations. The small number of studies identified that met our criteria limits our understanding of the resulting themes. Due to the limited number of studies stratifying results regarding food insecurity by gender, we broadened our inclusion criteria to include any study that presented at least some data separately for women, presenting challenges in separating results by gender. Some of the included studies relied on observational data involving self-reporting of sexual risk behaviors and food security, potentially allowing for social desirability bias or recall bias. Additionally, the included studies were conducted in only six countries, with four in sub-Saharan Africa and two in North America. With this limited geographic variation, results may not be generalizable across settings. We focused only on outcomes related to sexual behavior and ART adherence, so did not capture the full range of effects that food insecurity may have on the lives of women living with HIV. We also did not include lack of access to clean water in our definition of food insecurity, though women often bear a disproportionate burden in obtaining water when it is scarce and lack of clean water has severe implications for the health of women living with HIV in particular due to their risk of infections.
In summary, current literature points to an association between food insecurity, lack of control within sexual relationships, and various behavioral outcomes related to HIV and STI risk, as well as HIV medication adherence, among women living with HIV. Our findings have the following implications for programs and policies that seek to address the needs of women living with HIV. The HIV response must create an enabling environment for women living with HIV by implementing programs that reduce hunger and food insecurity, especially for women. This includes efforts to provide information and education on growing, preparing and eating healthy foods. The context in which women experience food insecurity also needs to be addressed.[69] This includes investment in programs that enhance women’s legal and social rights and economically empower them, particularly those that promote/secure their property and inheritance rights in conjunction with food assistance and income generation,[70] There is also a need to identify which interventions and programs are effective in order to improve women’s legal and social rights and empower them economically (e.g. cash transfers, microfinance, vocational and skills training).[15] The paucity of studies included in our review suggests that more research is needed that specifically addresses food security, sexual risk behavior, and ART adherence among women living with HIV. Disaggregation of results by sex would allow future researchers to better understand gender dynamics of HIV and food insecurity.
Acknowledgements
The authors would like to acknowledge the members of the WHO guideline development group who provided input to this review.
Footnotes
Competing interests
The authors declare that they have no competing interests.
References
- 1.Anderson SA: Core indicators of nutritional state for difficult-to-sample populations. J Nutr 1990, 120 Suppl 11:1559–1600. [DOI] [PubMed] [Google Scholar]
- 2.Fawzi MC, Lambert W, Boehm F, Finkelstein JL, Singler JM, Leandre F, Nevil P, Bertrand D, Claude MS, Bertrand J et al. : Economic risk factors for HIV infection among women in rural Haiti: implications for HIV prevention policies and programs in resource-poor settings. J Womens Health (Larchmt) 2010, 19(5):885–892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Palar K, Laraia B, Tsai AC, Johnson MO, Weiser SD: Food insecurity is associated with HIV, sexually transmitted infections and drug use among men in the United States. AIDS 2016, 30(9):1457–1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aibibula W, Cox J, Hamelin AM, Mamiya H, Klein MB, Brassard P: Food insecurity and low CD4 count among HIV-infected people: a systematic review and meta-analysis. AIDS Care 2016:1–9. [DOI] [PubMed] [Google Scholar]
- 5.Weiser SD, Palar K, Frongillo EA, Tsai AC, Kumbakumba E, Depee S, Hunt PW, Ragland K, Martin J, Bangsberg DR: Longitudinal assessment of associations between food insecurity, antiretroviral adherence and HIV treatment outcomes in rural Uganda. AIDS 2014, 28(1):115–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weiser SD, Yuan C, Guzman D, Frongillo EA, Riley ED, Bangsberg DR, Kushel MB: Food insecurity and HIV clinical outcomes in a longitudinal study of urban homeless and marginally housed HIV-infected individuals. AIDS 2013, 27(18):2953–2958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weiser SD, Tsai AC, Gupta R, Frongillo EA, Kawuma A, Senkungu J, Hunt PW, Emenyonu NI, Mattson JE, Martin JN et al. : Food insecurity is associated with morbidity and patterns of healthcare utilization among HIV-infected individuals in a resource-poor setting. AIDS 2012, 26(1):67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weiser SD, Hatcher A, Frongillo EA, Guzman D, Riley ED, Bangsberg DR, Kushel MB: Food insecurity is associated with greater acute care utilization among HIV-infected homeless and marginally housed individuals in San Francisco. J Gen Intern Med 2013, 28(1):91–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bartelink IH, Savic RM, Mwesigwa J, Achan J, Clark T, Plenty A, Charlebois E, Kamya M, Young SL, Gandhi M et al. : Pharmacokinetics of lopinavir/ritonavir and efavirenz in food insecure HIV-infected pregnant and breastfeeding women in Tororo, Uganda. J Clin Pharmacol 2014, 54(2):121–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Feldman MB, Alexy ER, Thomas JA, Gambone GF, Irvine MK: The Association Between Food Insufficiency and HIV Treatment Outcomes in a Longitudinal Analysis of HIV-Infected Individuals in New York City. Journal of Acquired Immune Deficiency Syndromes 2015, 69(3):329–337. [DOI] [PubMed] [Google Scholar]
- 11.Koss CA, Natureeba P, Nyafwono D, Plenty A, Mwesigwa J, Nzarubara B, Clark TD, Ruel TD, Achan J, Charlebois ED et al. : Food Insufficiency is Associated with Lack of Sustained Viral Suppression among HIV-Infected Pregnant and Breastfeeding Ugandan Women. J Acquir Immune Defic Syndr 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anema A, Chan K, Chen Y, Weiser S, Montaner JS, Hogg RS: Relationship between food insecurity and mortality among HIV-positive injection drug users receiving antiretroviral therapy in British Columbia, Canada. PLoS One 2013, 8(5):e61277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weiser SD, Fernandes KA, Brandson EK, Lima VD, Anema A, Bangsberg DR, Montaner JS, Hogg RS: The association between food insecurity and mortality among HIV-infected individuals on HAART. J Acquir Immune Defic Syndr 2009, 52(3):342–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Waal A, Whiteside A: New variant famine: AIDS and food crisis in southern Africa. Lancet 2003, 362(9391):1234–1237. [DOI] [PubMed] [Google Scholar]
- 15.Himmelgreen DA, Romero-Daza N, Turkon D, Watson S, Okello-Uma I, Sellen D: Addressing the HIV/AIDS-food insecurity syndemic in sub-Saharan Africa. African Journal of AIDS Research 2009, 8(4):401–412. [DOI] [PubMed] [Google Scholar]
- 16.Weiser SD, Young SL, Cohen CR, Kushel MB, Tsai AC, Tien PC, Hatcher AM, Frongillo EA, Bangsberg DR: Conceptual framework for understanding the bidirectional links between food insecurity and HIV/AIDS. Am J Clin Nutr 2011, 94(6):1729S–1739S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kaschula S: Using people to cope with the hunger: social networks and food transfers amongst HIV/AIDS afflicted households in KwaZulu-Natal, South Africa. AIDS Behav 2011, 15(7):1490–1502. [DOI] [PubMed] [Google Scholar]
- 18.Tsai AC, Bangsberg DR, Emenyonu N, Senkungu JK, Martin JN, Weiser SD: The social context of food insecurity among persons living with HIV/AIDS in rural Uganda. Soc Sci Med 2011, 73(12):1717–1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kalofonos IA: “All I eat is ARVs”: the paradox of AIDS treatment interventions in central Mozambique. Med Anthropol Q 2010, 24(3):363–380. [DOI] [PubMed] [Google Scholar]
- 20.Mills EJ, Nachega JB, Buchan I, Orbinski J, Attaran A, Singh S, Rachlis B, Wu P, Cooper C, Thabane L et al. : Adherence to antiretroviral therapy in sub-Saharan Africa and North America: a meta-analysis. JAMA 2006, 296(6):679–690. [DOI] [PubMed] [Google Scholar]
- 21.Nachega JB, Hislop M, Dowdy DW, Chaisson RE, Regensberg L, Maartens G: Adherence to nonnucleoside reverse transcriptase inhibitor-based HIV therapy and virologic outcomes. Ann Intern Med 2007, 146(8):564–573. [DOI] [PubMed] [Google Scholar]
- 22.Sethi AK, Celentano DD, Gange SJ, Moore RD, Gallant JE: Association between adherence to antiretroviral therapy and human immunodeficiency virus drug resistance. Clin Infect Dis 2003, 37(8):1112–1118. [DOI] [PubMed] [Google Scholar]
- 23.Grobler L, Siegfried N, Visser ME, Mahlungulu S, Volmink J: Nutritional interventions for reducing morbidity and mortality in people with HIV. Cochrane Database Syst Rev 2013, 2. [DOI] [PubMed] [Google Scholar]
- 24.Amin A: Addressing gender inequalities to improve the sexual and reproductive health and wellbeing of women living with HIV. J Int AIDS Soc 2015, 18(Suppl 5):20302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.West BS, Hirsch JS, El-Sadr W: HIV and H2O: tracing the connections between gender, water and HIV. AIDS Behav 2013, 17(5):1675–1682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Levy JM, Webb AL, Sellen DW: “On our own, we can’t manage”: experiences with infant feeding recommendations among Malawian mothers living with HIV. Int Breastfeed J 2010, 5:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Singer AW, Weiser SD, McCoy SI: Does Food Insecurity Undermine Adherence to Antiretroviral Therapy? A Systematic Review. AIDS Behav 2015, 19(8):1510–1526. [DOI] [PubMed] [Google Scholar]
- 28.Ivers LC, Cullen KA: Food insecurity: special considerations for women. Am J Clin Nutr 2011, 94(6):1740S–1744S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Montgomery KS: Nutrition and HIV-Positive Pregnancy. J Perinat Educ 2003, 12(1):42–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McCoy SI, Buzdugan R, Mushavi A, Mahomva A, Cowan FM, Padian NS: Food insecurity is a barrier to prevention of mother-to-child HIV transmission services in Zimbabwe: a cross-sectional study. BMC Public Health 2015, 15:420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Villamor E, Saathoff E, Msamanga G, O’Brien ME, Manji K, Fawzi WW: Wasting during pregnancy increases the risk of mother-to-child HIV-1 transmission. J Acquir Immune Defic Syndr 2005, 38(5):622–626. [DOI] [PubMed] [Google Scholar]
- 32.Dunkle KL, Jewkes RK, Brown HC, Gray GE, McIntryre JA, Harlow SD: Transactional sex among women in Soweto, South Africa: prevalence, risk factors and association with HIV infection. Social Science & Medicine 2004, 59(8):1581–1592. [DOI] [PubMed] [Google Scholar]
- 33.Oyefara JL: Food insecurity, HIV/AIDS pandemic and sexual behaviour of female commercial sex workers in Lagos metropolis, Nigeria. SAHARA-J: Journal of Social Aspects of HIV/AIDS 2007, 4(2):626–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tsai AC, Hung KJ, Weiser SD: Is food insecurity associated with HIV risk? Cross-sectional evidence from sexually active women in Brazil. PLoS Med 2012, 9(4):e1001203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weiser SD, Leiter K, Bangsberg DR, Butler LM, Percy-de Korte F, Hlanze Z, Phaladze N, Iacopino V, Heisler M: Food Insufficiency Is Associated with High-Risk Sexual Behavior among Women in Botswana and Swaziland. PLoS Med 2007, 4(10):e260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Denison JA, O’Reilly KR, Schmid GP, Kennedy CE, Sweat MD: HIV voluntary counseling and testing and behavioral risk reduction in developing countries: a meta-analysis, 1990--2005. AIDS Behav 2008, 12(3):363–373. [DOI] [PubMed] [Google Scholar]
- 37.Medley A, Kennedy C, O’Reilly K, Sweat M: Effectiveness of peer education interventions for HIV prevention in developing countries: a systematic review and meta-analysis. AIDS Educ Prev 2009, 21(3):181–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Higgins JPTGS: Cochrane Handbook for Systematic Reviews of Interventions. In.: The Cochrane Collaboration; 2011. [Google Scholar]
- 39.Miller CL, Bangsberg DR, Tuller DM, Senkungu J, Kawuma A, Frongillo EA, Weiser SD: Food insecurity and sexual risk in an HIV endemic community in Uganda. AIDS and Behavior 2011, 15(7):1512–1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fielding-Miller R, Mnisi Z, Adams D, Baral S, Kennedy C: “There is hunger in my community”: a qualitative study of food security as a cyclical force in sex work in Swaziland. BMC public health 2014, 14:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Whittle HJ, Palar K, Napoles T, Hufstedler LL, Ching I, Hecht FM, Frongillo EA, Weiser SD: Experiences with food insecurity and risky sex among low-income people living with HIV/AIDS in a resource-rich setting. J Int AIDS Soc 2015, 18:20293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Murray LK, Semrau K, McCurley E, Thea DM, Scott N, Mwiya M, Kankasa C, Bass J, Bolton P: Barriers to acceptance and adherence of antiretroviral therapy in urban Zambian women: a qualitative study. AIDS Care 2009, 21(1):78–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Musumari PM, Feldman MD, Techasrivichien T, Wouters E, Ono-Kihara M, Kihara M: “If i have nothing to eat, i get angry and push the pills bottle away from me”: A qualitative study of patient determinants of adherence to antiretroviral therapy in the Democratic Republic of Congo. AIDS Care - Psychological and Socio-Medical Aspects of AIDS/HIV 2013, 25(10):1271–1277. [DOI] [PubMed] [Google Scholar]
- 44.Shannon K, Kerr T, Milloy MJ, Anema A, Zhang R, Montaner JS, Wood E: Severe food insecurity is associated with elevated unprotected sex among HIV-seropositive injection drug users independent of HAART use. Aids 2011, 25(16):2037–2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.de Pee S, Semba RD: Role of nutrition in HIV infection: review of evidence for more effective programming in resource-limited settings. Food Nutr Bull 2010, 31(4):S313–344. [PubMed] [Google Scholar]
- 46.Gupta A, Nadkarni G, Yang WT, Chandrasekhar A, Gupte N, Bisson GP, Hosseinipour M, Gummadi N: Early mortality in adults initiating antiretroviral therapy (ART) in low- and middle-income countries (LMIC): a systematic review and meta-analysis. PLoS One 2011, 6(12):e28691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vogenthaler NS, Hadley C, Rodriguez AE, Valverde EE, del Rio C, Metsch LR: Depressive symptoms and food insufficiency among HIV-infected crack users in Atlanta and Miami. AIDS Behav 2011, 15(7):1520–1526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vogenthaler NS, Kushel MB, Hadley C, Frongillo EA, Jr., Riley ED, Bangsberg DR, Weiser SD: Food insecurity and risky sexual behaviors among homeless and marginally housed HIV-infected individuals in San Francisco. AIDS Behav 2013, 17(5):1688–1693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Davidoff-Gore A, Luke N, Wawire S: Dimensions of poverty and inconsistent condom use among youth in urban Kenya. AIDS Care 2011, 23(10):1282–1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Eaton LA, Cain DN, Pitpitan EV, Carey KB, Carey MP, Mehlomakulu V, Simbayi LC, Mwaba K, Kalichman SC: Exploring the relationships among food insecurity, alcohol use, and sexual risk taking among men and women living in South African townships. J Prim Prev 2014, 35(4):255–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Greif MJ: Housing, medical, and food deprivation in poor urban contexts: implications for multiple sexual partnerships and transactional sex in Nairobi’s slums. Health Place 2012, 18(2):400–407. [DOI] [PubMed] [Google Scholar]
- 52.McCoy SI, Ralph LJ, Njau PF, Msolla MM, Padian NS: Food insecurity, socioeconomic status, and HIV-related risk behavior among women in farming households in Tanzania. AIDS Behav 2014, 18(7):1224–1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Raiford JL, Herbst JH, Carry M, Browne FA, Doherty I, Wechsberg WM: Low prospects and high risk: structural determinants of health associated with sexual risk among young African American women residing in resource-poor communities in the south. Am J Community Psychol 2014, 54(3–4):243–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wang EA, Zhu GA, Evans L, Carroll-Scott A, Desai R, Fiellin LE: A pilot study examining food insecurity and HIV risk behaviors among individuals recently released from prison. AIDS Educ Prev 2013, 25(2):112–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Anema A, Weiser SD, Fernandes KA, Ding E, Brandson EK, Palmer A, Montaner JS, Hogg RS: High prevalence of food insecurity among HIV-infected individuals receiving HAART in a resource-rich setting. AIDS Care 2011, 23(2):221–230. [DOI] [PubMed] [Google Scholar]
- 56.Berhe N, Tegabu D, Alemayehu M: Effect of nutritional factors on adherence to antiretroviral therapy among HIV-infected adults: a case control study in Northern Ethiopia. BMC Infect Dis 2013, 13:233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Franke MF, Murray MB, Muñoz M, Hernández-Díaz S, Sebastián JL, Atwood S, Caldas A, Bayona J, Shin SS: Food insufficiency is a risk factor for suboptimal antiretroviral therapy adherence among HIV-infected adults in urban Peru. AIDS and Behavior 2011, 15(7):1483–1489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sasaki Y, Kakimoto K, Dube C, Sikazwe I, Moyo C, Syakantu G, Komada K, Miyano S, Ishikawa N, Kita K et al. : Adherence to antiretroviral therapy (ART) during the early months of treatment in rural Zambia: influence of demographic characteristics and social surroundings of patients. Ann Clin Microbiol Antimicrob 2012, 11:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Surratt HL, O’Grady CL, Levi-Minzi MA, Kurtz SP: Medication adherence challenges among HIV positive substance abusers: the role of food and housing insecurity. AIDS Care 2015, 27(3):307–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Young S, Wheeler AC, McCoy SI, Weiser SD: A review of the role of food insecurity in adherence to care and treatment among adult and pediatric populations living with HIV and AIDS. AIDS Behav 2014, 18 Suppl 5:S505–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Makoae MG: Food meanings in HIV and AIDS caregiving trajectories: ritual, optimism and anguish among caregivers in Lesotho. Psychol Health Med 2011, 16(2):190–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jones C: “IF I TAKE MY PILLS I’ll GO HUNGRY”: THE CHOICE BETWEEN ECONOMIC SECURITY AND HIV/AIDS TREATMENT IN GRAHAMSTOWN, SOUTH AFRICA. Annals of Anthropological Practice 2011, 35(1):67–80. [Google Scholar]
- 63.Palar K, Wagner G, Ghosh-Dastidar B, Mugyenyi P: Role of antiretroviral therapy in improving food security among patients initiating HIV treatment and care. AIDS 2012, 26(18):2375–2381. [DOI] [PubMed] [Google Scholar]
- 64.Swaminathan HA K; Kes A; et al. : Women’s property rights, HIV and AIDS, and domestic violence: Research findings from two rural districts in South Africa and Uganda. In.; 2008. [Google Scholar]
- 65.Swaminathan HB N; Chakraborty S: Women’s property rights as an AIDS response: emerging efforts in South Asia. In. Washington, DC; 2007. [Google Scholar]
- 66.Ray I: Women, Water, and Development. Annual Review of Environment and Resources 2007, 32(1):421–449. [Google Scholar]
- 67.Buor D: Water needs and women’s health in the Kumasi metropolitan area, Ghana. Health Place 2004, 10(1):85–103. [DOI] [PubMed] [Google Scholar]
- 68.Nations U: The world’s women 2015: trends and statistics. In. New York: Department of Economic and Social Affairs, Statistics Division; 2015. [Google Scholar]
- 69.Aberman NL, Rawat R, Drimie S, Claros JM, Kadiyala S: Food security and nutrition interventions in response to the AIDS epidemic: assessing global action and evidence. AIDS Behav 2014, 18 Suppl 5:S554–565. [DOI] [PubMed] [Google Scholar]
- 70.Hardee K, Gay J, Croce-Galis M, Peltz A: Strengthening the enabling environment for women and girls: what is the evidence in social and structural approaches in the HIV response? J Int AIDS Soc 2014, 17:18619. [DOI] [PMC free article] [PubMed] [Google Scholar]