Abstract
Background:
Environmental health (EH) professionals, one of the largest segments of the public health workforce, are responsible for delivery of essential environmental public health services. The challenges facing these professionals and research needs to improve EH practice are not fully understood, but 26% of EH professionals working in health departments of the United States plan to retire in 5 y, while only 6% of public health students are currently pursuing EH concentrations.
Objectives:
A groundbreaking initiative was recently launched to understand EH practice in health departments of the United States. This commentary article aims to identify priority EH practice challenges and related research needs for health departments.
Methods:
A horizon scanning approach was conducted in which challenges facing EH professionals were provided by 1,736 respondents working at health departments who responded to a web-based survey fielded in November 2017. Thematic analyses of the responses and determining the frequency at which respondents reported specific issues and opportunities identified primary EH topic areas. These topic areas and related issues informed focus group discussions at an in-person workshop held in Anaheim, California. The purpose of the in-person workshop was to engage each of the topic areas and issues, through facilitated focus groups, leading to the formation of four to five related problem statements for each EH topic.
Discussion:
EH professionals are strategically positioned to diagnose, intervene, and prevent public health threats. Focus group engagement resulted in 29 priority problem statements partitioned among 6 EH topic areas: a) drinking water quality, b) wastewater management, c) healthy homes, d) food safety, e) vectors and public health pests, and f) emerging issues. This commentary article identifies priority challenges and related research needs to catalyze effective delivery of essential environmental public health services for common EH program areas in health departments. An unprecedented initiative to revitalize EH practice with timely and strategic recommendations for student and professional training, nontraditional partnerships, and basic and translational research activities is recommended. https://doi.org/10.1289/EHP5161
Introduction
Flint, PFAS (per-and polyfluoroalkyl substances), Zika. Hurricanes Harvey, Irma, Maria, and Michael. Environment and health issues that capture the public’s attention can often result in significant economic impacts and render decidedly adverse health outcomes, particularly when interventions are not effectively and efficiently delivered. Globally, influences of environmental pollution on health are palpable, where disease burdens are routinely pronounced in lower- to middle-income countries with especially vulnerable populations (Landrigan et al. 2018). Such observations are also routinely realized in developed countries, as illustrated recently by PFAS- and lead-contaminated drinking water and devastation caused by hurricanes on the Gulf Coast, Puerto Rico, and the U.S. Virgin Islands.
In the United States, environmental health (EH) professionals working at health departments have the responsibility to address environment-related threats and determinants of health. These professionals are specifically charged with protecting local communities through delivery of the 10 Essential Environmental Public Health Services (CDC 2016), which are structured within the core functions of public health (assessment, policy development, and assurance). System management connects directly to each essential service and is informed by research innovation. Thus, EH professionals form a critical component of the public health delivery system, routinely providing services to prevent adverse health outcomes and preparing for, responding to, and recovering from disease outbreaks and natural or anthropogenic disasters. EH professionals are strategically positioned to identify and intervene to help prevent public health threats affecting local communities. While various assessment efforts have described aspects of the EH workforce (ASTHO 2016; NACCHO 2016; Halverson 2019), a comprehensive understanding of the demographics, current challenges, and opportunities facing this profession in the United States has remained elusive (Gerding et al. 2017).
Prioritization activities are beneficial for professions with identified strategic research needs. For example, grand challenge exercises in the United States for environmental engineering and health and medicine have yielded major science and engineering themes for future research that aim to further transform scientific discoveries, which then ultimately translate to practice. Yet socially relevant transformative science is achievable when efforts are based on credible science, salient policy, and aligned with societal significance (Rudd et al. 2014). Towards this goal, research prioritization efforts using a key research question have identified priority science and policy research needs in conservation biology (Sutherland et al. 2009) and agriculture (Pretty et al. 2010), as well as for specific classes of chemical contaminants (Boxall et al. 2012; Rudd et al. 2014) and global ocean systems (Rudd 2014). Horizon scanning employs a systematic methodology for collecting information and examining current and emerging issues or conditions to support decision-making and strategic approaches for effectively responding to a changing environment (Sutherland and Woodroof 2009). More recently, the Global Horizon Scanning project, which identifies priority research needs to achieve more sustainable environmental quality, is transparently engaging multiple science and engineering disciplines from the academic, government, and business sectors around the world (Furley et al. 2018; Van den Brink et al. 2018; Fairbrother et al. 2019; Gaw et al. 2019). Collectively, these global horizon scanning activities are already making an impact in which specific research needs have been selected for strategic funding in several countries.
Although EH professionals represent one of the largest segments of the public health workforce, making up approximately 10% of the local and 7% of the state health department workforce (NACCHO 2016; ASTHO 2016), an understanding of the challenges they face now and research needed to advance their practice in the future is decidedly lacking. In fact, the last national study of Sanitarians, a title historically associated with a segment of EH professionals, was performed more than a half century ago by the U.S. Department of Health, Education, and Welfare (Pennell et al. 1963). Such an exercise appears timely and important for public health because 26% of EH professionals working in U.S. health departments plan to retire within 5 y (Gerding et al. 2019), but only 6% of students pursuing public health degrees are focusing their studies in EH (Leider et al. 2018).
Here we begin to address this critical gap through an unprecedented initiative entitled Understanding Needs, Challenges, Opportunities, Vision and Emerging Roles in Environmental Health (UNCOVER-EH), which was recently launched by the Centers for Disease Control and Prevention (CDC), National Environmental Health Association (NEHA), and Baylor University (Gerding et al. 2017). We expanded our previous experience with horizon scanning (Boxall et al. 2012; Rudd et al. 2014; Furley et al. 2018; Van den Brink et al. 2018; Fairbrother et al. 2019; Gaw et al. 2019) to directly engage EH professionals working in state, tribal, local, and territorial health departments in the United States.
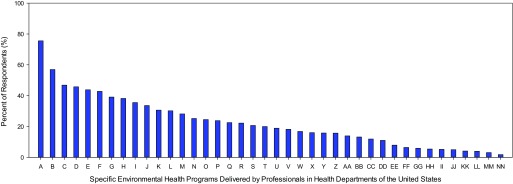
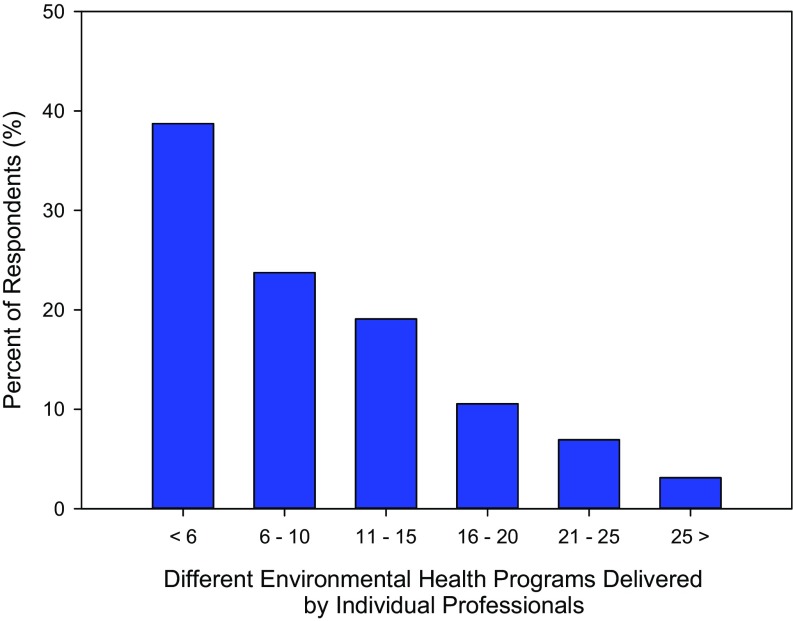
This initial UNCOVER-EH phase consisted of two primary components, a web-based survey and in-person workshops. Through the web-based survey, we received information from 1,736 EH professionals from 48 states, which included professionals working in health departments at the state, local, and tribal levels, along with two Pacific Island territories. In addition to providing demographic data (Gerding et al. 2019) and identifying the primary programs in which they deliver services (Figures 1 and 2), survey respondents were specifically asked to relay information on challenges and opportunities facing their existing programs and issues they anticipate increasingly engaging in the near future (5–10 y). EH professionals are delivering essential health services in diverse programs, ranging from food safety, emergency response, drinking water, and wastewater to vector control, recreational waters, and hazardous materials (Figure 1). Impressively, these professionals must be systems thinkers, problem solvers, risk communicators, and generalists, routinely called on to deliver essential health services for a number of programs as part of their routine work (Figure 2). Thematic analysis of open-ended, text survey responses and the frequency at which respondents reported specific issues and opportunities identified primary EH topic areas for further consideration. These topic areas and related issues thus informed focus group discussions at an in-person workshop held in Anaheim, California during the NEHA 2018 Annual Educational Conference and Exhibition.
Figure 1.
Percentage of environmental health professionals delivering specific programs in health departments of the United States. The web-based survey allowed environmental health professionals multiple responses to indicate the various programs in which they worked. Note: A, food safety and protection; B, public swimming pools; C, emergency preparedness and response; D, schools; E, onsite wastewater (e.g., septic systems); F, private or onsite drinking water; G, hotels/motels; H, vector control; I, body art (e.g., tattoo); J, day care/early childhood development facilities; K, special events/mass gatherings; L, campgrounds and RVs; M, public drinking water systems; N, lead prevention; O, solid waste; P, smoke-free ordinances; Q, children’s camps; R, indoor air quality; S, other recreational water (e.g., beaches); T, healthy homes; U, other; V, mobile homes; W, radon control; X, animal control; Y, land-use planning; Z, hazardous waste disposal; AA, pollution prevention; BB, health-related facilities; CC, outdoor air quality; DD, hazmat response; EE, tobacco retailers; FF, noise pollution; GG, cosmetology businesses; HH, collection of unused pharmaceuticals; II, radiation control; JJ, injury prevention; KK, toxicology; LL, occupational health; MM, milk processing; and NN, poison control () (adapted from Gerding et al. 2019).
Figure 2.
Number of different environmental health programs delivered by percent of respondent professionals working in health departments of the United States ().
At the workshop, the authors, which include EH professionals working in different capacities (field staff, managers, and directors) at state and local health departments, participated in or facilitated two of six different 90-min focus groups (each focus group consisted of three to four participants). After examining submissions received from the UNCOVER-EH survey, we specifically developed four to five priority problem statements associated with each of the six preidentified EH topics (drinking water quality, wastewater management, healthy homes, food safety, vectors and public health pests, and emerging issues). The authors then finalized, through consensus, 29 priority problem statements, following examination of challenges and needs submitted with these six topic areas. We therefore consider all the problem statements as timely and important priorities for environmental public health practice. Thus, we individually examine these problem statements (in italics) by each topic area below, and subsequently provide recommendations to advance public health for the benefit of local communities.
Discussion of Problem Statements
Drinking Water Quality
Drinking water supplies are not consistently being monitored and evaluated for contaminants of historical (e.g., Escherichia coli, arsenic, lead, and nitrate/nitrite) and emerging (e.g., per-and polyfluoroalkyl substances, noroviruses, legionella, and algal toxins) concern.
Monitoring and surveillance represent essential environmental public health services (NCEH 2014). Unfortunately, potable water quality remains under examined, particularly in rural areas and private wells where exposures to contaminants of emerging concern (e.g., PFAS, endocrine disruptors, antibiotics), and even historically recognized threats, are unknown. Some efforts, including the Unregulated Contaminant Monitoring Rule (UCMR), which was developed in the United States to examine suspected contaminants in drinking water that lack health-based standards, focus on rural drinking water (EPA 2018a). However, these activities are inherently limited in spatial scope and for which contaminants are evaluated (Oxenford and Barrett 2016). For example, cyanotoxins represent an increasingly important public health threat (Brooks et al. 2016), but only a few were recently included in UCMR activities, and they are commonly not evaluated in source waters. Similarly, diverse PFAS compounds exist with limited toxicology information (Patlewicz et al. 2019), yet these emerging threats are not routinely monitored in drinking water supplies. Drinking water quality from private wells across the United States remains largely unknown.
Although aging drinking water infrastructure is recognized as an environmental public health threat for larger utilities, risk-based interventions in smaller communities and rural settings, including on private property, are limited.
As highlighted by recent lead contamination (Pieper et al. 2018) and Legionnaires’ disease (Schwake et al. 2016) events in Flint, Michigan, differential management effectiveness and aging drinking water infrastructure continue to present risks to public health. Population growth, urbanization, and climate change are further stressing existing systems. However, addressing such infrastructure deficiencies while advancing innovation in urban water systems promises to increase urban water security and resiliency (Zodrow et al. 2017). Although drinking water infrastructure in urban areas has received increased attention, private water supplies (e.g., wells) and small and rural systems have received less study than larger municipal utilities (Allaire et al. 2018). The extent of public health risks from compromised drinking water infrastructure in these smaller systems and in rural areas requires future assessment.
Private drinking water supplies do not receive adequate environmental health services (i.e., inform but not enforce, cannot retest unless asked) due to inconsistent policies (i.e., no jurisdiction) and public perceptions (i.e., lack of trust).
Drinking water quality of private wells and small and rural systems can be impaired by diverse biological and chemical agents (Allaire et al. 2018). Herein, impoverished and minority communities are often affected, which highlights diverse environmental justice challenges for addressing rural health disparities (Balazs et al. 2011; Stillo and MacDonald Gibson 2017). Our analysis indicates that private water supplies (e.g., wells) and points of personal uses (e.g., inside personal residences) remain difficult to sample due to jurisdictional barriers, and when drinking water quality is examined in these settings, EH professionals routinely inform community members of findings but often cannot enforce and implement corrective measures or drinking water standards compliance. Further, if drinking water exceedances are observed in private wells, which are not regulated by the U.S. Environmental Protection Agency (EPA), then we identify that EH professionals cannot retest water quality unless asked by the property owner. These collective challenges may result in decreased public trust in health departments, which further challenges effective delivery of EH services. Systems research is needed to improve delivery of essential services and address this issue.
Source water quantity (e.g., groundwater, surface water), which is stressed by population growth, overexploitation (e.g., unregulated pumping), and droughts, is not consistently managed (i.e., by private and public).
Drought and mismanagement of source waters directly threaten drinking water quantity and then intersect with potable water quality concerns. In some drought-prone regions, excessive aquifer withdrawals, which are not consistently governed across the United States, are resulting in brackish conditions that impair drinking water quality and compromise conventional treatment technologies (Konikow 2013), but these brackish groundwaters can augment drinking water resources if desalination occurs (Ahdab et al. 2018). When groundwater is excessively contaminated with arsenic from natural or anthropogenic sources, diverse chronic health risks, including cancers, emerge from inorganic arsenic, particularly in drought-susceptible rural areas (Gong et al. 2011, 2015). Innovative approaches, such as the National Aeronautics and Space Administration (NASA)'s Gravity Recovery and Climate Experiment (GRACE) mission, are providing novel technologies to assess groundwater deficits and derive groundwater drought indices that can support monitoring, surveillance, and forecasting efforts (Thomas et al. 2017). Clearly, leveraging such technologies to identify regions where stressed source water quality elevates public health risks, particularly in small and rural systems and private wells, represents a pressing EH research opportunity.
Wastewater Management
Lack of collaboration during onsite wastewater management policy development (delegation without consideration) results in gaps in programmatic capacity.
In the United States, at least 20% of the population is served by decentralized (or onsite) wastewater treatment technologies (e.g., septic and advanced aerobic) (EPA 2002, 2005). These decentralized systems are not directly regulated by the EPA, which focuses on centralized municipal and industrial wastewater treatment plants and thus transfers responsibilities for onsite sewage management to tribes and states (EPA 2018b). Regulatory responsibility is then routinely passed on to the local level of government, which performs site assessments and permits construction of decentralized systems (EPA 2018b). Onsite wastewater management activities, training, and workforce capacity differ among and within states. Although such differences in local policies and practices exist, the extent to which this fractured management system presents risks to public health and the environment is often not directly studied until surface water quality impairments are observed and regulatory actions proceed (e.g., through development of total maximum daily loads).
Onsite wastewater management is differentially implemented (e.g., design parameters), administered, and assessed.
New decentralized technologies are routinely evaluated to meet several general water quality parameters. For example, these technologies are tested independently and certified for conformance to standards prior to installation [e.g., standard 40 from the National Sanitation Foundation International/American National Standards Institute (NSFI 2018)]. However, when onsite systems are improperly installed or not functioning, use impairments for drinking water, fisheries, and recreation result (Bremer and Harter 2012; Withers et al. 2014; Scott et al. 2016, 2019). Such degradation of surface water and groundwater quality directly occurs from bacteria, anthropogenic chemicals, and nutrients (Schaider et al. 2017), which can stimulate development of harmful algal blooms (Brooks et al. 2016). Delivery of implementation, assessment, and enforcement activities for onsite systems varies among and within states, resulting in diverse risks to public health and the environment. Spatial magnitude, frequency, and duration of these public health risks remain poorly understood.
There is a lack of data to support transitions from prescriptive to performance-based standards for onsite systems.
Installation of new onsite wastewater treatment systems includes site assessments using a prescriptive approach, in which locations with characteristics (e.g., soil types and location to wells) suitable for a given technology (e.g., septic) and use scenario (e.g., sewage volume per day) are determined (NOWRA 2006). Watershed heterogeneity inherently challenges consistent implementation of this paradigm. Performance-based standards are ideally risk based and include specific measures of parameters that, if not exceeded, are expected to protect public health and the environment (NOWRA 2006). Such performance-based codes for decentralized systems promise to more closely resemble compliance to water quality goals of centralized systems. For example, a model code framework has been developed to advance performance-based practice (NOWRA 2006), particularly as onsite technologies continue to advance to address diverse and emerging water quality challenges (Garcia et al. 2013; Du et al. 2014). However, strategic EH research is needed to provide appropriate data to support identification and implementation of robust performance-based efforts across the United States.
Adverse health outcomes are presented from aging wastewater infrastructure associated with and because of increasing rural to urban demographic transitions and urbanization.
It has been estimated that over $1 trillion is needed over the next two decades to address aging water and wastewater infrastructure in the United States (Selvakumar et al. 2015). Degradation of centralized sewage treatment is now recognized as a major need; however, infrastructure challenges for decentralized systems has received limited attention, similar to the rural and small drinking water systems described above. Revitalizing improperly functioning decentralized infrastructure appears critically important because diverse adverse health outcomes and surface water quality impairments (e.g., recreational use due to enteric bacterial contamination) are associated with failing septic tanks when these systems are decades old or were not installed properly (Borchardt et al. 2003; Tollestrup et al. 2014). For example, hookworm is reemerging in socioeconomically challenged rural areas of the southeastern United States due to exposure from onsite wastewater (McKenna et al. 2017). Although these decentralized systems are often considered a rural issue, periurban and urban water quality issues have been reported, particularly when higher-density housing with onsite systems is developed in vulnerable watersheds of urbanizing unincorporated areas (Forbis-Stokes et al. 2016; Scott et al. 2016, 2019). Research is needed to identify high-risk regions across the rural–periurban–urban gradient. This information will support prioritization of areas requiring public health interventions.
New onsite technologies lack sustainable onsite wastewater implementation and performance data, including during droughts and flooding, to address emerging threats.
Onsite technologies continue to advance to address nutrient pollution and other stresses to water quality. Although these systems must undergo standard testing as described above, empirical performance data in response to extreme weather events are lacking in the refereed literature. This information is necessary because the global magnitude, frequency, and duration of environmental disasters are increasing (IPCC 2012; Field et al. 2012). As evidenced during the 2017 hurricane season, some regions, such as the Houston–Galveston region with over 300,000 onsite systems (www.h-gac.com), are particularly vulnerable. For example, based on sampling after Hurricane Harvey, widespread presence of antibiotic resistance bacteria were reported in surface waters of the Houston area (Yu et al. 2018). Such observations require further attention because over 80% of surface waters in this region were previously identified as impaired, including 47% of waterways exceeding water quality standards for indicator bacteria (E. coli) (Clean Rivers Program 2015). Here again, research is needed to identify watersheds for interventions, develop more robust treatment systems, and ensure new onsite technologies are resilient when disasters occur.
Healthy Homes
Environmental health professionals have limited regulatory authority to assess housing and recommend/implement corrective actions.
Healthy housing programs include diverse topics that are routinely engaged by EH professionals in the United States (CDC and HUD 2006). For example, a number of drinking water, wastewater, and vectors problem statements are associated with common healthy homes topics and are discussed elsewhere in this paper. Similarly, recreational pools and spas represent an important healthy housing program commonly delivered by EH professionals. Evaluation of spas and swimming pools routinely focus on bacterial exposures, although recent studies identified exposure to carcinogens (i.e., disinfection byproducts) in spas, which requires additional attention (Daiber et al. 2016). Similar to challenges associated with private wells and point-of-use drinking water surveillance identified above, EH programs for healthy homes efforts routinely are challenged by restricted access to private property. Although lead exposure from drinking water in Flint, Michigan has rightly received attention, identifying the extent of degraded potable water and wastewater infrastructure is inherently challenged by limited access to perform point-of-use sampling. However, instead of retrospective action following identification of problems, inspector-generated housing inspections present opportunities to prioritize locations for interventions (Korfmacher and Holt 2018).
Another problem statement was directly related to the necessity of more prospective interventions in healthy housing: Officials are only reacting to hoarding and filthy housing situations once they have become a public health and safety problem. Here again, EH professionals are often responsible for engaging domestic health and safety issues associated with unsanitary conditions after exposures occur. It thus appears clear that, in the absence of national scale changes in consistent regulatory responsibilities to protect public health from such threats in residences, additional research is needed to develop and implement technologies (e.g., sensors) and communication channels (e.g., through smartphone apps) that could be voluntarily adopted by the public. These advances could provide near-real-time information on conditions of individual residences or those approaching unsanitary conditions in their community to EH professionals.
Lack of public awareness regarding health and safety implications of mold, insects, and other indoor asthma/allergen triggers challenges effective delivery of essential services.
Asthma, particularly in children, is directly triggered by diverse environmental factors (e.g., mold, dust mites, particulates) and can be exacerbated by poor indoor air quality (Ege et al. 2011), including exposures to diverse organic chemicals (Bornehag et al. 2005; Salthammer et al. 2018). Unfortunately, such observations can be pronounced in some regions (Lowe 2018), particularly when outdoor air quality is degraded. It appears that public awareness of the diverse factors influencing asthma is limited, which presents translational research opportunities for collaboration with and among EH professionals and community health education specialists.
There remains continued focus on secondary prevention of childhood lead poisoning instead of focusing on primary prevention of removing lead hazards in the environment before children are exposed.
Despite an understanding of linkages between lead exposure and impacts on children for centuries (Needleman 2009), some children continue to experience blood lead levels that exceed CDC guidelines in communities across the United States (Benson et al. 2017). Recently, a high-profile example of lead exposure was observed in Flint, Michigan (Ruckart et al. 2019). However, despite this important event, lead from contaminated drinking water may represent a relatively lower age-dependent point of exposure for children, especially in infants possibly consuming formula prepared with tap water, compared with lead from paint and dust in many areas of the United States (Dixon et al. 2009; Zartarian et al. 2017). Elevated blood lead levels observations in children are routinely associated with pre-1978 housing, which may have used lead-based paint prior to the ban in residential use, and industrial sources, especially when local interventions are ineffective (Dixon et al. 2009). Further, elevated blood lead levels are often associated with socioeconomically depressed areas in which higher proportions of minority populations reside (Schultz et al. 2017). Blood lead testing results provide an important safety net for children who have been exposed to lead. However, primary prevention of lead exposure, before children are poisoned, should be advanced to prevent effects on childhood development in the United States.
Abdication of responsibility by rental property owners is affecting public health in situations where tenants are underserved populations.
Health equity intersections with challenges delivering environmental public health services remain palpable in some regions of the United States (Morello-Frosch and Shenassa 2006). Such social determinants of health are often highlighted by housing conditions and corresponding health inequities experienced by underserved populations (Jacobs et al. 2009), including immigrant populations. If rental property owners abdicate their responsibilities to ensure healthy housing for tenants, then adverse health outcomes can result. Unfortunately, much like the EH delivery system, consistent implementation of building codes and health homes goals for rental housing appears fractured within and among states. Research is needed to define the extent to which unacceptable conditions are being experienced by tenants and which interventions are necessary in local communities.
Food Safety
Environmental health programs lack capacity to identify and regulate illegal food vendors and home kitchens.
Ensuring food safety through regulation and inspection is a primary service of most local and state health departments (NACCHO 2016; ASTHO 2016). Reductions in local health department capacity and budgets have resulted in negative impacts to EH services, including food safety programs (Li and Elligers 2014). The food safety landscape continually evolves with the introduction of new food types and alternative food service settings (e.g., food trucks and home kitchens). The observation of critical food safety risk factors among food trucks is not uncommon; however, difficulties in locating trucks can create regulatory challenges (Faw and Tuttle 2014). These conditions are also applicable in the case of home kitchens. Identification and effective regulation of these food service anomalies, which are becoming more and more common, requires increased EH program capacity.
Environmental health professionals cannot consistently regulate and/or monitor cottage foods and food additives.
Cottage foods are those prepared in a home kitchen and sold to the public at a variety of venues such as farmers’ markets. Acknowledging the challenges associated with regulating cottage foods, the Association of Food and Drug Officials published a guidance document on best practices for regulating cottage foods (AFDO 2012). Jurisdictional laws on cottage food regulation vary across the United States, creating challenges for regulating these facility types. Conducting inspections is a necessary regulatory function, yet home kitchens are not easily identified, especially in the absence of permitting requirements (AFDO 2012). The Food and Drug Administration (FDA) approves the use of certain food additives and offers a decision tree for determining the regulatory status of additives (FDA 2018). While certain food additives may be assigned a regulatory classification, challenges remain in determining whether unsafe, unregulated additives are added to foods.
Food service workers lack the ability to apply their food safety training to their food safety systems at an operational level.
Food safety training is recognized as a primary intervention for ensuring food service workers follow safe food handling practices. Certification, commonly preceded by training, has shown to result in increased food service worker knowledge (Brown et al. 2014). Additionally, research shows that training may improve knowledge and influence behaviors associated with proper hand hygiene (Soon et al. 2012). While training occurs and benefits to being trained are noted, food service workers may not consistently apply their food safety knowledge in the kitchen or operational settings.
Sick workers are working while sick.
The FDA Food Code requires that workers exhibiting certain symptoms of illness (e.g., diarrhea) be excluded from work (FDA 2017). However, high percentages of food service employees work while sick. This may be associated with factors such as restaurant policies not addressing sick workers, concerns about leaving the restaurant short-staffed, and the threat of job loss for not coming to work (Carpenter et al. 2013; Norton et al. 2015). Charles and Radke (2017) explained that federal laws like the Health Insurance Portability and Accountability Act and Americans with Disabilities Act do not prevent managers from speaking with employees about illness. Managers may consider promoting a culture of open communication, encouraging staff to discuss illness-related symptoms with management. Policies encouraging staff to talk with managers when ill may also lead to fewer workers working while ill (Sumner et al. 2011).
Governing bodies of environmental health programs do not always have an understanding of the value of interventions and may have competing interests other than public health.
Rapid changes and developments in the food safety arena require increased programmatic capacity and a robust workforce. This, in turn, necessitates governing body support for enhancing food safety programs. Government decision-makers and leaders face challenges when determining priority programs or areas to receive, in most cases, already limited available resources. Communicating the value of related interventions, such as training for food service workers and performing regulatory services, is important for ensuring awareness of the value of food safety interventions and increasing support and resources for strengthening food safety programs.
Vectors and Public Health Pests
There is indication that vectors are spreading to new areas, but there is a lack of surveillance and understanding.
Emerging vector-borne diseases and the spread of vectors to new geographic areas (e.g., Zika virus and Aedes aegypti and Aedes albopictus mosquitoes), particularly with changing climate, reinforces the need for increased resources and enhancement of surveillance, educational, and policy-related interventions (Imperato 2016). While mosquito vectors are spreading to new areas, local and state health department arboviral surveillance capacity has decreased (Hadler et al. 2015). In general, the emergence of vector-borne pathogens and disease, along with significant increases in tick-borne disease rates, require strengthened vector and vector-borne disease surveillance (Rosenberg et al. 2018) and research to identify and manage such threats as climatic and habitat changes occur.
Pest management policies restrict control methods and programs cannot expand their approaches.
Limitations in existing pest management policies may restrict jurisdictional use of new approaches and strategies for controlling vectors and public health pests. Factors such as pesticide resistance require new vector control methods. The methods include, for example, biocontrol strategies such as use of biological organisms or releasing sterile mosquitoes to impact vector populations and control vectors (Benelli et al. 2016). Technological advances and development of alternative control methods may require evaluation of existing pest management policies and ensuring the ability to employ new vector control strategies.
The authority to address bed bug complaints is not clearly defined.
Bed bugs, which are not known to transmit disease but are recognized as pests of public health significance, can be a source of public concern (Goddard and deShazo 2009; Kaylor et al. 2015). Addressing bed bug infestations, especially in multifamily housing units, is challenging and requires an integrated pest management approach consisting of a range of strategies (Bennett et al. 2016). Bed bugs present significant public health challenges and concerns (Lai et al. 2016), yet agency policies are not consistent among and within states and do not always clearly specify the authority to respond or enforce requirements to address bed bugs infestations.
Public education and awareness of vector prevention and control is limited.
The Interim CDC Recommendations for Zika Vector Control in the Continental United States highlighted communication and educating the public about controlling A. aegypti and A. albopictus mosquitoes as an essential element for preparing to control Zika virus vectors and the potential for disease transmission (CDC 2019). Additionally, educating the community about EH issues is one of the 10 essential environmental public health services (CDC 2016). However, much like indoor air and allergen challenges discussed above, there remain limitations in the public’s awareness of vector prevention and control strategies. Here again, this area presents an opportunity for collaboration with community health educators.
Lack of coordination and communication in community design and construction can lead to the creation of vector habitat opportunities.
Anthropogenic changes or alterations to the environment, specifically landscapes, can create conditions (i.e., safe harborage spaces) conducive to vector presence and potential vector-borne disease transmission (Reisen 2010). Establishing relationships between governmental partners, planners, contractors, and others involved in community design or construction is essential for addressing environmental factors in the community that may create vector habitats or be conducive to the presence of vectors and pests. Efforts to encourage increased coordination among stakeholders could prevent the creation of vector habitats as they may result from community design and construction projects.
Emerging Issues
Expectations are to increase involvement and activities in nontraditional areas, such as regulating new facility types, substances, and community events without opportunities to incorporate science and best practices.
The expansion of EH regulatory responsibilities in nontraditional areas and facility types (e.g., body art, cannabis-infused products, or large-scale community events of varying themes and attractions) requires the incorporation of science and best practices into regulatory functions. However, delegation and requirements to fulfill such responsibilities are commonly accompanied with an urgent need to respond. This urgency limits opportunities to establish regulatory approaches based on current knowledge and science. Research is needed to advance proactive, rather than reactive, response systems to ensure the timely development of best practice–based guidelines.
Regulations and guidelines are outdated, not existent, or behind industry advances and standards for new facility types and events (e.g., body art and swimming pools).
The availability of up-to-date standards for EH professionals is crucial for effectively regulating traditional and new facility types. Responses to the need for such standards include the CDC’s release of the Model Aquatic Health Code (2018) and NEHA’s release of a Body Art Model Code and subsequent updates (Hlavsa et al. 2015; Armstrong and Fell 2000; NEHA 2018). While current standards may exist, jurisdictions sometimes face legislative challenges with adopting new standards and regulatory guidelines. Research is needed to examine best practices, modify existing standards where necessary, and develop new standards to address outdated practices.
Environmental health professionals are expected to respond to a wide range of emergencies or disasters without inclusion in planning efforts.
Recognizing the emergence of public health threats and the need for rapid response to and recovery from emergencies and disasters, there has been a call to action for ensuring an equipped and ready EH workforce (National Environmental Health Partnership Council 2017). EH professionals fulfill a critical role in emergency response and recovery; however, they are commonly left out of community emergency response preparedness (e.g., planning, exercises, and training) efforts in the United States. Collaboration among EH, emergency responders, and other community stakeholders can establish a high level of community-based emergency preparedness (Eldridge and Tenkate 2006; Gamboa-Maldonado et al. 2012), particularly given increased recognition of noncommunicable diseases following disasters (Ryan et al. 2018). Future research is needed to comparatively examine the structure of emergency response systems to optimize preparedness and disaster risk reduction efforts.
Environmental health has limited involvement in population health and health equity initiatives.
Public health departments are engaging in population health and health equity initiatives to address health disparities in communities without EH involvement. However, involvement from multiple public health disciplines is essential to addressing community health disparities (Richardson 2016). Health departments are seeking accreditation through the Public Health Accreditation Board, which exemplifies engagement in an initiative leading to improved population health and addressing health equity (Yeager et al. 2016; Wooten et al. 2018). EH plays an important role in the accreditation process (Gerding et al. 2013), which likely extends to other initiatives aimed at improving population health and addressing health equity. Future research efforts are clearly needed in this space.
Environmental health’s role in sustainability and community planning is not clearly defined.
Sustainability and community planning are topics receiving much attention from local and state governments, and EH has an undefined role to play. In terms of community planning, the built environment and community design are areas that can benefit from EH expertise. For example, EH professionals may be able to contribute to transportation planning efforts to address related community health impacts or inform a parks and recreation program’s approach to protecting sensitive environments and increasing green space to promote physical activity (Whitfield and Wendel 2015; Merriam 2016). Urban sprawl is another phenomenon with sustainability and environmental implications for air pollution, land use, and water quality and quantity (Frumkin 2002). EH professionals have a vested interest in and can make substantial contributions to sustainability and community planning, yet a defined role is lacking in most jurisdictions.
Conclusions
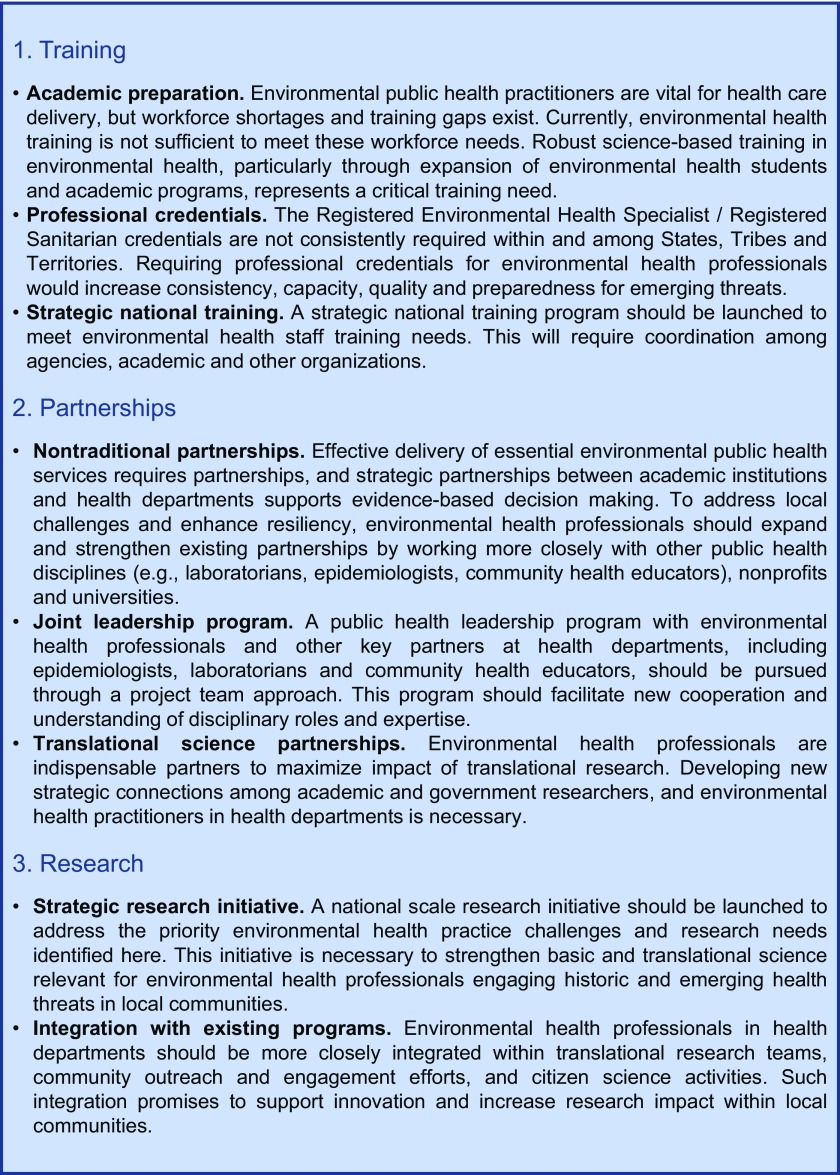
EH is a foundational area of public health (Leider et al. 2015), providing core public health science formation during undergraduate and graduate training programs. EH professionals are critical to the public health delivery system as they consistently engage multiple program areas (Figure 2), routinely respond to disasters and other emergencies (Figure 1), and are strategically positioned to diagnose, intervene, and prevent historic and emerging threats (NEHA 2017). Here, we report an initial effort to identify challenges and research opportunities for common EH programs of health departments in the United States. After receiving information from over 1,700 EH professionals from health departments, we developed 29 priority problem statements that identify key challenges and represent important delivery and research needs in this field. We further provide recommendations to strategically engage these timely problem statements through training, partnership, and research activities (Figure 3).
Figure 3.
Environmental health practice recommendations.
As noted above, Gerding et al. (2019) recently identified that 26% of EH professionals in health departments plan to retire in the next 5 y. Although these and other important workforce issues are facing the EH profession (Gerding et al. 2019), academic training at the undergraduate and graduate levels is not currently meeting such trajectories. For example, only 6% (in 2015) of students in public health degree programs are pursuing EH concentrations (Leider et al. 2018), but EH training provides scientific rigor necessary to engage historic and emerging threats to public health. Further, this percentage has decreased by 5% over the past two decades (from 11% in 1996), which contributes to EH practitioners sometimes perceived as an “invisible” or a “silent” profession (Blake 2007; Whiley et al. 2018). Such trends are decidedly problematic because the environmental determinants of health will continue to present leading threats to public health. Thus, expanding the number of students enrolled in EH undergraduate and graduate programs, including master of public health concentrations in EH, represents a critically important national health care necessity (Figure 3). Similarly, once professionals enter the workforce, the registered environmental health specialist (REHS)/registered sanitarian (RS) credentials support professional preparedness through initial competency examination and continuing education. However, REHS/RS credentialing are not consistently required within and among states, tribes, and territories, but formally requiring these credentials would improve consistency in EH workforce training and health service delivery. Based on our assessment of UNCOVER-EH information submitted by EH professionals, it thus appears necessary to launch a strategic training effort at the national scale to meet these timely EH training needs (Figure 3).
EH professionals are clearly not alone in engaging challenges associated with the problem statements in common program areas identified here. Effective delivery of the essential services inherently requires partnerships within local communities, among sectors, and across professions. For example, strategic partnerships between institutions of higher learning and health departments can support evidence-based decision-making in local health departments (Erwin et al. 2019). To address local health challenges and enhance resiliency when emerging threats present and disasters occur, we recommend that EH professionals should pursue nontraditional partnerships and strengthen existing partnerships, particularly by working more closely with other public health disciplines (e.g., laboratorians, epidemiologists, and community health educators) within and among health departments and other government agencies, and with nonprofits and universities. We also see utility of implementing a project team-based public health leadership program, which would couple EH professionals with laboratorians, epidemiologists, and community health educators (Figure 3). Further, we submit that EH professionals working in health departments are ideal partners for translational science researchers from government agencies and academic institutions, but partnerships are not consistently occurring within and among geographic regions. Simply stated, we identify this space to represent a reciprocally beneficial opportunity for EH professionals and translational researchers (Figure 3).
Addressing the problem statements reported here will not be trivial, but doing so is decidedly necessary to protect public health of local communities. It therefore seems appropriate to launch a new national-scale science–practice research initiative. For example, the National Nanoscience Initiative has significantly advanced research, through individual investigator grants, center grants, and training grants, on the environmental implications of nanotechnologies, but it required coordination of academic and government research with multiple federal agencies (www.nano.gov). A similar initiative appears warranted to advance toward addressing EH science–practice priorities. Although timely environmental quality research questions for North America were recently identified (Fairbrother et al. 2019), and many of those questions examined environment and health interfaces, coordinating environmental quality research among research scientists and engineers with EH professionals in health departments is underdeveloped but promises transformational benefits for public health and innovation. We recommend that EH professionals should also more significantly engage in translational research teams through community outreach and engagement cores and citizen science programs (Figure 3).
Because we specifically targeted EH professionals in health departments for the current study, future phases of UNCOVER-EH could perform similar studies with professionals in other governmental agencies, private settings, and other professions engaging EH. Similarly, formally ranking these priority problem statements by EH professionals could provide more geographically detailed information to tailor regionally specific basic and translational research and practice activities. We expect information from the current study will be useful for EH research and practice efforts in other countries. Engaging the problem statements identified here will require commitment but doing so will catalyze future science–practice research program trajectories in EH, which aim to improve the delivery of the essential services and protect the health of local communities.
Acknowledgments
Support for this study was provided by the CDC. We thank the EH professionals for taking time to participate in this study.
The findings and conclusions in this manuscript are those of the author(s) and do not necessarily represent the official position of the CDC.
Footnotes
The authors declare they have no actual or potential competing financial interests.
Note to readers with disabilities: EHP strives to ensure that all journal content is accessible to all readers. However, some figures and Supplemental Material published in EHP articles may not conform to 508 standards due to the complexity of the information being presented. If you need assistance accessing journal content, please contact ehponline@niehs.nih.gov. Our staff will work with you to assess and meet your accessibility needs within 3 working days.
References
- Ahdab YD, Thiel GP, Böhlke JK, Stanton J, Lienhard JH. 2018. Minimum energy requirements for desalination of brackish groundwater in the United States with comparison to international datasets. Water Res 141:387–404, PMID: 29857319, 10.1016/j.watres.2018.04.015. [DOI] [PubMed] [Google Scholar]
- Allaire M, Wu H, Lall U. 2018. National trends in drinking water quality violations. Proc Natl Acad Sci USA 115(9):2078–2083, PMID: 29440421, 10.1073/pnas.1719805115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong ML, Fell PR. 2000. Body art: regulatory issues and the NEHA body art model code. J Environ Health 62:25–30. [Google Scholar]
- AFDO (Association of Food and Drug Officials). 2012. Regulatory guidance for best practices: cottage foods. http://www.afdo.org/resources/temp/Cottage_Foods_013.pdf [accessed 25 September 2019].
- ASTHO (Association of State and Territorial Health Officials). 2016. Profile of State and Territorial Public Health. Vol. 4 Arlington, VA: ASHTO. [Google Scholar]
- Balazs C, Morello-Frosch R, Hubbard A, Ray I. 2011. Social disparities in nitrate contaminated drinking water in California’s San Joaquin Valley. Environ Health Perspect 119(9):1272–1278, PMID: 21642046, 10.1289/ehp.1002878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benelli G, Jeffries C, Walker T. 2016. Biological control of mosquito vectors: past, present, and future. Insects 7(4):52, PMID: 27706105, 10.3390/insects7040052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett GW, Gondhalekar AD, Wang C, Buczkowski G, Gibb TJ. 2016. Using research and education to implement practical bed bug control programs in multifamily housing. Pest Manag Sci 72(1):8–14, PMID: 26251256, 10.1002/ps.4084. [DOI] [PubMed] [Google Scholar]
- Benson SM, Talbott EO, Brink LL, Wu C, Sharma RV, Marsh GM. 2017. Environmental lead and childhood blood lead levels in US children: NHANES, 1999–2006. Arch Environ Occup Health 72(2):70–78, PMID: 26942652, 10.1080/19338244.2016.1157454. [DOI] [PubMed] [Google Scholar]
- Blake R. 2007. President’s message: environmental health—the invisible profession, part I. J Environ Health 70(1):4–11. [PubMed] [Google Scholar]
- Borchardt MA, Chyou PH, Devries EO, Belongia EA. 2003. Septic system density and infectious diarrhea in a defined population of children. Environ Health Perspect 111(5):742–748, PMID: 12727604, 10.1289/ehp.5914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornehag CG, Lundgren B, Weschler CJ, Sigsgaard T, Hagerhed-Engman L, Sundell J. 2005. Phthalates in indoor dust and their association with building characteristics. Environ Health Perspect 113(10):1399–1404, PMID: 16203254, 10.1289/ehp.7809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boxall AB, Rudd MA, Brooks BW, Caldwell DJ, Choi K, Hickmann S, et al. 2012. Pharmaceuticals and personal care products in the environment: what are the big questions? Environ Health Perspect 120(9):1221–1229, PMID: 22647657, 10.1289/ehp.1104477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bremer JE, Harter T. 2012. Domestic wells have high probability of pumping septic tank leachate. Hydrol Earth Syst Sci 16(8):2453–2467, 10.5194/hess-16-2453-2012. [DOI] [Google Scholar]
- Brooks BW, Lazorchak JM, Howard MD, Johnson MV, Morton SL, Perkins DA, et al. 2016. Are harmful algal blooms becoming the greatest inland water quality threat to public health and aquatic ecosystems? Environ Toxicol Chem 35(1):6–13, PMID: 26771345, 10.1002/etc.3220. [DOI] [PubMed] [Google Scholar]
- Brown LG, Le B, Wong MR, Reimann D, Nicholas D, Faw B. 2014. Restaurant manager and worker food safety certification and knowledge. Foodborne Pathog Dis 11(11):835–843, PMID: 25361386, 10.1089/fpd.2014.1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter LR, Green AL, Norton DM, Frick R, Tobin-D’Angelo M, Reimann DW. 2013. Food worker experiences with and beliefs about working while ill. J Food Prot 76(12):2146–2154, PMID: 24290694, 10.4315/0362-028X.JFP-13-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC (Centers for Disease Control and Prevention). 2016. 10 Essential environmental public health services. www.cdc.gov/nceh/ehs/10-essential-services/index.html [accessed 25 September 2019].
- CDC. 2018. Model aquatic health code. www.cdc.gov/mahc/ [accessed 28 September 2019].
- CDC. 2019. Interim CDC recommendations for Zika vector control in the continental United States. https://www.cdc.gov/zika/public-health-partners/vector-control-us.html [accessed 25 September 2019].
- CDC, HUD (U.S. Department of Housing and Urban Development). 2006. Healthy Housing Reference Manual. Atlanta, GA: U.S. Department of Health and Human Services. [Google Scholar]
- Charles J, Radke T. 2017. Discussing symptoms with sick food service employees. J Environ Health 80:24–26. [Google Scholar]
- Clean Rivers Program. 2015. How’s the Water? Houston-Galveston Area Council Basin Highlights Report. Houston, TX: Houston-Galveston Area Council. [Google Scholar]
- Daiber EJ, DeMarini DM, Ravuri SA, Liberatore HK, Cuthbertson AA, Thompson-Klemish A, et al. 2016. Progressive increase in disinfection byproducts and mutagenicity from source to tap to swimming pool and spa water: impact of human inputs. Environ Sci Technol 50(13):6652–6662, PMID: 27124361, 10.1021/acs.est.6b00808. [DOI] [PubMed] [Google Scholar]
- Dixon SL, Gaitens JM, Jacobs DE, Strauss W, Nagaraja J, Pivetz T, et al. 2009. Exposure of U.S. children to residential dust lead, 1999–2004: II. The contribution of lead-contaminated dust to children’s blood lead levels. Environ Health Perspect 117(3):468–474, PMID: 19337524, 10.1289/ehp.11918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du B, Price AE, Scott WC, Kristofco LA, Ramirez AJ, Chambliss CK, et al. 2014. Comparison of contaminants of emerging concern removal, discharge, and water quality hazards among centralized and on-site wastewater treatment system effluents receiving common wastewater influent. Sci Total Environ 466–467:976–984, PMID: 23988745, 10.1016/j.scitotenv.2013.07.126. [DOI] [PubMed] [Google Scholar]
- Ege MJ, Mayer M, Normand A, Genuneit J, Cookson WOCM, Braun-Fahrländer C, et al. 2011. Exposure to environmental microorganisms and childhood asthma. N Engl J Med 364:701–709, PMID: 21345099, 10.1056/NEJMoa1007302. [DOI] [PubMed] [Google Scholar]
- Eldridge D, Tenkate TD. 2006. The role of environmental health in disaster management: an overview and review of barriers and facilitators for action. Rev Environ Health 21(4):281–294, PMID: 17243351, 10.1515/REVEH.2006.21.4.281. [DOI] [PubMed] [Google Scholar]
- EPA (U.S. Environmental Protection Agency). 2002. Onsite Wastewater Treatment Systems Manual. EPA/625/R-00/008. Washington, DC: Office of Water, Office of Research and Development, EPA. [Google Scholar]
- EPA. 2005. Handbook for Managing Onsite and Clustered (Decentralized) Wastewater Treatment Systems: An Introduction to Management Tools and Information for Implementing EPA’s Management Guidelines. EPA No. 832-B-05-001. Washington, DC: Office of Water, Office of Research and Development, EPA. [Google Scholar]
- EPA. 2018a. Monitoring the occurrence of unregulated drinking water contaminants. https://www.epa.gov/dwucmr [accessed 11 August 2018].
- EPA. 2018b. Septic systems (onsite/decentralized systems). https://www.epa.gov/septic [accessed 19 August 2018].
- Erwin PC, Parks RG, Mazzucca S, Allen P, Baker EA, Hu H, et al. 2019. Evidence-based public health provided through local health departments: importance of academic-practice partnerships. Am J Public Health 109(5):739–747, PMID: 30896995, 10.2105/AJPH.2019.304958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairbrother A, Muir D, Solomon KR, Ankley GT, Rudd MA, Boxall ABA, et al. 2019. Toward sustainable environmental quality: priority research questions for North America. Environ Toxicol Chem 38(8):1606–1624, PMID: 31361364, 10.1002/etc.4502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faw BV, Tuttle JL. 2014. Mobile food trucks: California EHS-Net study on risk factors and inspection challenges. J Environ Health 76(8):36–37, PMID: 24749225. [PubMed] [Google Scholar]
- FDA (Food and Drug Administration). 2017. Food Code. College Park, MD: FDA, U.S. Department of Health and Human Services. [Google Scholar]
- FDA. 2018. Determining the regulatory status of a food ingredient. https://www.fda.gov/food/ingredientspackaginglabeling/foodadditivesingredients/ucm228269.htm [accessed 28 October 2019].
- Field CB, Barros V, Stocker TF, Qin D, Dokken DJ, Ebi KL, et al. 2012. Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation. A Special Report of Working Groups I and II of the Intergovernmental Panel on Climate Change. Cambridge, UK: Cambridge University Press. [Google Scholar]
- Forbis-Stokes A, Munster C, Karthikeyan R, Mohanty BP, Boulanger B. 2016. Modeling onsite wastewater treatment systems in a coastal Texas watershed. Water Air Soil Pollut 227(12):430, 10.1007/s11270-016-3120-8. [DOI] [Google Scholar]
- Frumkin H. 2002. Urban sprawl and public health. Public Health Rep 117(3):201–217, PMID: 12432132, 10.1093/phr/117.3.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furley TH, Brodeur JC, Silva de Assis HC, Carriquiriborde P, Chagas KR, Corrales J, et al. 2018. Towards sustainable environmental quality: identifying priority research questions for Latin America. Integr Environ Assess Manag 14(3):344–357, PMID: 29469193, 10.1002/ieam.2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamboa-Maldonado T, Marshak HH, Sinclair R, Montgomery S, Dyjack DT. 2012. Building capacity for community disaster preparedness: a call for collaboration between public environmental health and emergency preparedness and response programs. J Environ Health 75(2):24–29, PMID: 22984732. [PMC free article] [PubMed] [Google Scholar]
- Garcia SN, Clubbs RL, Stanley JK, Scheffe B, Yelderman JC Jr, Brooks BW. 2013. Comparative analysis of effluent water quality from a municipal treatment plant and two on-site wastewater treatment systems. Chemosphere 92(1):38–44, PMID: 23557723, 10.1016/j.chemosphere.2013.03.007. [DOI] [PubMed] [Google Scholar]
- Gaw S, Harford A, Pettigrove V, Sevicke-Jones G, Manning T, Ataria J, et al. 2019. Towards sustainable environmental quality: priority research questions for the Australasia region of Oceania. Integr Environ Assess Manag 15(6):917–935, PMID: 31273905, 10.1002/ieam.4180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerding J, Carlson VP, Wilcox R. 2013. Public health department accreditation and environmental public health: sustaining the collaboration. J Environ Health 76(1):56–57, PMID: 23947290. [PubMed] [Google Scholar]
- Gerding J, Landeen E, Brooks BW. 2017. Understanding the needs, challenges, opportunities, vision and emerging roles in environmental health (UNCOVER-EH). J Environ Health 80:36–37. [Google Scholar]
- Gerding J, Landeen E, Kelly K, Whitehead S, Dyjack D, Sarisky J, et al. 2019. Uncovering environmental health: an initial assessment of the profession's health department workforce and practice. J Environ Health 81:24–33. [PMC free article] [PubMed] [Google Scholar]
- Goddard J, deShazo R. 2009. Bed bugs (Cimex lectularius) and clinical consequences of their bites. JAMA 301(13):1358–1366, PMID: 19336711, 10.1001/jama.2009.405. [DOI] [PubMed] [Google Scholar]
- Gong G, Basom J, Mattevada S, Onger F. 2015. Association of hypothyroidism with low-level arsenic exposure in rural West Texas. Environ Res 138:154–160, PMID: 25721242, 10.1016/j.envres.2015.02.001. [DOI] [PubMed] [Google Scholar]
- Gong G, Hargrave KA, Hobson V, Spallholz J, Boylan M, Lefforge D, et al. 2011. Low-level groundwater arsenic exposure impacts cognition: a project FRONTIER study. J Environ Health 74(2):16–22, PMID: 21949980. [PubMed] [Google Scholar]
- Hadler JL, Patel D, Nasci RS, Petersen LR, Hughes JM, Bradley K, et al. 2015. Assessment of arbovirus surveillance 13 years after introduction of West Nile Virus, United States. Emerg Infect Dis 21(7):1159–1166, PMID: 26079471, 10.3201/eid2107.140858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halverson PK. 2019. Ensuring a strong public health workforce in the 21st century: reflections on PH WINS 2017. J Public Health Manag Pract 25(suppl 2):S1–S3, PMID: 30720609, 10.1097/PHH.0000000000000967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hlavsa MC, Kunz JM, Beach MJ. 2015. It’s all about the return on investment: the model aquatic health code. J Environ Health 77(9):34–35, PMID: 25985536. [PubMed] [Google Scholar]
- Imperato PJ. 2016. The convergence of a virus, mosquitoes, and human travel in globalizing the Zika epidemic. J Community Health 41(3):674–679, PMID: 26969497, 10.1007/s10900-016-0177-7. [DOI] [PubMed] [Google Scholar]
- IPCC (Intergovernmental Panel on Climate Change). 2012. Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation. A Special Report of Working Groups I and II of the Intergovernmental Panel on Climate Change. Field CB, Barros V, Stocker TF, Qin D, Dokken DJ, Ebi KL, Mastrandrea MD, Mach KJ, Plattner GK, Allen SK, Tignor M, Midgley PM, eds. Cambridge University Press, Cambridge, UK. [Google Scholar]
- Jacobs DE, Wilson J, Dixon SL, Smith J, Evens A. 2009. The relationship of housing and population health: a 30-year retrospective analysis. Environ Health Perspect 117(4):597–604, PMID: 19440499, 10.1289/ehp.0800086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaylor MB, Wenning P, Eddy C. 2015. Prevalence, knowledge, and concern about bed bugs. J Environ Health 78(1):20–24, PMID: 26427264. [PubMed] [Google Scholar]
- Konikow LF. 2013. Groundwater Depletion in the United States (1900–2008). U.S. Geological Survey Scientific Investigations Report 2013–5079 Reston, VA: U.S. Geological Survey, 63. [Google Scholar]
- Korfmacher KS, Holt KD. 2018. The potential for proactive housing inspections to inform public health interventions. J Public Health Manag Pract 24(5):444–447, PMID: 29474210, 10.1097/PHH.0000000000000757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai O, Ho D, Glick S, Jagdeo J. 2016. Bed bugs and possible transmission of human pathogens: a systematic review. Arch Dermatol Res 308(8):531–538, PMID: 27295087, 10.1007/s00403-016-1661-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landrigan PJ, Fuller R, Acosta NJR, Adeyi O, Arnold R, Basu NN, et al. 2018. The Lancet Commission on pollution and health. Lancet 391(10119):462– 512, PMID: 29056410, 10.1016/S0140-6736(17)32345-0. [DOI] [PubMed] [Google Scholar]
- Leider JP, Juliano C, Castrucci BC, Beitsch LM, Dilley A, Nelson R, et al. 2015. Practitioner perspectives on foundational capabilities. J Public Health Manag Pract 21(4):25–335, PMID: 25486134, 10.1097/PHH.0000000000000189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leider JP, Plepys CM, Castrucci BC, Burke EM, Blakely CH. 2018. Trends in the conferral of graduate public health degrees: a triangulated approach. Public Health Rep 133(6):729–737, PMID: 30227771, 10.1177/0033354918791542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J, Elligers A. 2014. Impact of budget cuts to environmental health services at local health departments: key findings. J Environ Health 76(10):38–40, PMID: 24988663. [PubMed] [Google Scholar]
- Lowe M. 2018. Embedding health considerations in urban planning. Plann Theor Pract 19(4):623–627, 10.1080/14649357.2018.1496979. [DOI] [Google Scholar]
- Mckenna ML, Mcatee S, Hotez PJ, Bryan PE, Jeun R, Bottazzi ME, et al. 2017. Human intestinal parasite burden and poor sanitation in rural Alabama. Am J Trop Med Hyg 97(5):1623–1628, PMID: 29016326, 10.4269/ajtmh.17-0396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merriam D. 2016. Parks: an opportunity to leverage environmental health. J Environ Health 78(6):112–114, PMID: 26867300. [PubMed] [Google Scholar]
- Morello-Frosch R, Shenassa ED. 2006. The environmental “riskscape” and social inequality: implications for explaining maternal and child health disparities. Environ Health Perspect 114(8):1150–1153, PMID: 16882517, 10.1289/ehp.8930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NACCHO (National Association of County and City Health Officials). 2016. National Profile of Local Health Departments. Washington, DC: NACCHO. [Google Scholar]
- National Environmental Health Partnership Council. 2017. Environmental Health Playbook: Investing in a Robust Environmental Health System. Washington, DC: National Environmental Health Partnership Council. [Google Scholar]
- NCEH (National Center for Environmental Health). 2014. Improving Environmental Public Health Service: Performance to Meet Community Needs. Washington, DC: Centers for Disease Control and Prevention. [Google Scholar]
- Needleman H. 2009. Low level lead exposure: history and discovery. Ann Epidemiol 19(4):235–238, PMID: 19344860, 10.1016/j.annepidem.2009.01.022. [DOI] [PubMed] [Google Scholar]
- NEHA (National Environmental Health Association). 2018. Body art. https://www.neha.org/eh-topics/body-art [accessed 25 September 2019].
- Norton DM, Brown LG, Frick R, Carpenter LR, Green AL, Tobin-D’Angelo M, et al. 2015. Managerial practices regarding workers working while ill. J Food Prot 78(1):187–195, PMID: 25581195, 10.4315/0362-028X.JFP-14-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NOWRA (National Onsite Wastewater Recycling Association). 2006. Model code framework. http://www.nowra.org/content.asp?pl=25&contentid=36 [accessed 27 August 2018].
- NSFI (National Sanitation Foundation International). 2018. NSF/ANSI 40: residential onsite systems. http://www.nsf.org/services/by-industry/water-wastewater/onsite-wastewater/residential-wastewater-treatment-systems [accessed 27 August 2018].
- Oxenford JL, Barrett JM. 2016. Understanding small water system violations and deficiencies. J Am Water Works Assoc 108:31–37, 10.5942/jawwa.2016.108.0040. [DOI] [Google Scholar]
- Patlewicz G, Richard AM, Williams AJ, Grulke CM, Sams R, Lambert J, et al. 2019. A chemical category-based prioritization approach for selecting 75 per-and polyfluoroalkyl substances (PFAS) for tiered toxicity and toxicokinetic testing. Environ Health Perspect 127(1):014501, PMID: 30632786, 10.1289/EHP4555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pennell MY, Light I, Taylor DW. 1963. Sanitarians. In: Health Manpower Sourcebook. Washington DC: U.S. Department of Health, Education, and Welfare, Public Health Service, Division of Public Health Methods and Office of Resource Development. [Google Scholar]
- Pieper KJ, Martin R, Tang M, Walters L, Parks J, Roy S, et al. 2018. Evaluating water lead levels during the Flint water crisis. Environ Sci Technol 52(15):8124–8132, PMID: 29932326, 10.1021/acs.est.8b00791. [DOI] [PubMed] [Google Scholar]
- Pretty J, Sutherland WJ, Ashby J, Auburn J, Baulcombe D, Bell M, et al. 2010. The top 100 questions of importance to the future of global agriculture. Int J Agr Sustain 8(4):219–236, 10.3763/ijas.2010.0534. [DOI] [Google Scholar]
- Reisen WK. 2010. Landscape epidemiology of vector-borne diseases. Annu Rev Entomol 55:461–483, PMID: 19737082, 10.1146/annurev-ento-112408-085419. [DOI] [PubMed] [Google Scholar]
- Richardson LD. 2016. Integrating health equity into practice and policy. J Public Health Manag Pract 22:S107–S109, PMID: 26599023, 10.1097/PHH.0000000000000372. [DOI] [PubMed] [Google Scholar]
- Rosenberg R, Lindsey NP, Fischer M, Gregory CJ, Hinckley AF, Mead PS, et al. 2018. Vital signs: trends in reported vectorborne disease cases—United States and Territories, 2004–2016. MMWR Morb Mortal Wkly Rep 67(17):496–501, PMID: 29723166, 10.15585/mmwr.mm6717e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruckart PZ, Ettinger AS, Hanna-Attisha M, Jones N, Davis SI, Breysse PN. 2019. The Flint water crisis: a coordinated public health emergency response and recovery initiative. J Public Health Manag Pract 25(suppl 1):S84–S90, PMID: 30507775, 10.1097/PHH.0000000000000871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd MA. 2014. Scientists’ perspectives on global ocean research priorities. Front Mar Sci 1, 10.3389/fmars.2014.00036. [DOI] [Google Scholar]
- Rudd MA, Ankley GT, Boxall ABA, Brooks BW. 2014. International scientists’ research priorities for pharmaceuticals and personal care products in the environment. Integr Environ Assess Manag 10(4):576–587, PMID: 24954797, 10.1002/ieam.1551. [DOI] [PubMed] [Google Scholar]
- Ryan BJ, Franklin RC, Burkle FM, Smith EC, Aitken P, Watt K, et al. 2018. Ranking and prioritizing strategies for reducing mortality and morbidity from noncommunicable disease post disaster: An Australian perspective. Int J Disaster Risk Reduct 27:223–238, 10.1016/j.ijdrr.2017.10.009. [DOI] [Google Scholar]
- Salthammer T, Zhang Y, Mo J, Koch HM, Weschler CJ. 2018. Assessing human exposure to organic pollutants in the indoor environment. Angew Chem Int Ed Engl 57(38):12228–12263, PMID: 29537125, 10.1002/anie.201711023. [DOI] [PubMed] [Google Scholar]
- Schaider LA, Rodgers KM, Rudel RA. 2017. Review of organic wastewater compound concentrations and removal in onsite wastewater treatment systems. Environ Sci Technol 51(13):7304–7317, PMID: 28617596, 10.1021/acs.est.6b04778. [DOI] [PubMed] [Google Scholar]
- Schultz BD, Morara M, Buxton BE, Weintraub M. 2017. Predicting blood-lead levels among U.S. children at the census tract level. Environ Justice 10(5):129–136, 10.1089/env.2017.0005. [DOI] [Google Scholar]
- Schwake DO, Garner E, Strom OR, Pruden A, Edwards MA. 2016. Legionella DNA markers in tap water coincident with a spike in Legionnaires’ disease in Flint, MI. Environ Sci Technol Lett 3(9):311–315, 10.1021/acs.estlett.6b00192. [DOI] [Google Scholar]
- Scott WC, Breed CS, Haddad SP, Burket SR, Saari GN, Pearce PJ, et al. 2019. Spatial and temporal influence of onsite wastewater treatment systems, centralized effluent discharge, and tides on aquatic hazards of nutrients, indicator bacteria, and pharmaceuticals in a coastal bayou. Sci Total Environ 650(Pt 1):354–364, PMID: 30199681, 10.1016/j.scitotenv.2018.09.029. [DOI] [PubMed] [Google Scholar]
- Scott WC, Du B, Haddad SP, Breed CS, Saari GN, Kelly M, et al. 2016. Predicted and observed therapeutic dose exceedances of ionizable pharmaceuticals in fish plasma from urban coastal systems. Environ Toxicol Chem 35(4):983–995, PMID: 27003720, 10.1002/etc.3236. [DOI] [PubMed] [Google Scholar]
- Selvakumar A, Matthews JC, Condit W, Sterling R. 2015. Innovative research program on the renewal of aging water infrastructure systems. Journal Water Supply Res T 64(2):117–129, 10.2166/aqua.2014.103. [DOI] [Google Scholar]
- Soon JM, Baines R, Seaman P. 2012. Meta-analysis of food safety training on hand hygiene knowledge and attitudes among food handlers. J Food Prot 75(4):793–804, PMID: 22488073, 10.4315/0362-028X.JFP-11-502. [DOI] [PubMed] [Google Scholar]
- Stillo F, MacDonald Gibson J. 2017. Exposure to contaminated drinking water and health disparities in North Carolina. Am J Public Health 107(1):180–185, PMID: 27854523, 10.2105/AJPH.2016.303482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sumner S, Brown LG, Frick R, Stone C, Carpenter LR, Bushnell L, et al. 2011. Factors associated with food workers working while experiencing vomiting or diarrhea. J Food Prot 74(2):215–220, PMID: 21333140, 10.4315/0362-028X.JFP-10-108. [DOI] [PubMed] [Google Scholar]
- Sutherland WJ, Adam WM, Aronson RB, Aveling R, Blackburn TM, Broad S, et al. 2009. One hundred questions of importance to the conservation of global biological diversity. Conserv Biol 23(3):557–567, PMID: 19438873, 10.1111/j.1523-1739.2009.01212.x. [DOI] [PubMed] [Google Scholar]
- Sutherland WJ, Woodroof HJ. 2009. The need for environmental horizon scanning. Trends Ecol Evol (Amst) 24(10):523–527, PMID: 19660827, 10.1016/j.tree.2009.04.008. [DOI] [PubMed] [Google Scholar]
- Thomas BF, Famiglietti JS, Landerer FW, Wiese DN, Molotch NP, Argus DF. 2017. GRACE groundwater drought index: evaluation of California ventral valley groundwater drought. Remote Sens Environ 198:384–392, 10.1016/j.rse.2017.06.026. [DOI] [Google Scholar]
- Tollestrup K, Frost FJ, Kunde TR, Yates MV, Jackson S. 2014. Cryptosporidium infection, onsite wastewater systems and private wells in the arid Southwest. J Water Health 12(1):161–172, PMID: 24642442, 10.2166/wh.2013.049. [DOI] [PubMed] [Google Scholar]
- Van den Brink PJ, Boxall ABA, Maltby L, Brooks BW, Rudd MA, Backhaus T, et al. 2018. Towards sustainable environmental quality: priority research questions for Europe. Environ Toxicol Chem 37(9):2281–2295, PMID: 30027629, 10.1002/etc.4205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiley H, Willis E, Smith J, Ross K. 2018. Environmental health in Australia: overlooked and underrated. J Public Health (Oxf) 41(3):470–475, PMID: 30289461, 10.1093/pubmed/fdy156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitfield GP, Wendel AM. 2015. Modeling health impacts of the transportation built environment: challenges and opportunities. J Environ Health 77(7):36–37, PMID: 25796702. [PMC free article] [PubMed] [Google Scholar]
- Withers PJ, Jordan P, May L, Jarvie HP, Deal NE. 2014. Do septic tank systems pose a hidden threat to water quality? Front Ecol Environ 12(2):123–130, 10.1890/130131. [DOI] [Google Scholar]
- Wooten WJ, Julien J, Werth J. 2018. How public health accreditation helped one local health department integrate and promote health equity. J Public Health Manag Pract 24:S60–S65, PMID: 29595602, 10.1097/PHH.0000000000000777. [DOI] [PubMed] [Google Scholar]
- Yeager VA, Ye J, Kronstadt J, Robin N, Leep CJ, Beitsch LM. 2016. National voluntary public health accreditation. J Public Health Manag Pract 22(2):149–156, PMID: 25851799, 10.1097/PHH.0000000000000242. [DOI] [PubMed] [Google Scholar]
- Yu P, Zaleski A, Li Q, He Y, Mapili K, Pruden A, et al. 2018. Elevated levels of pathogenic indicator bacteria and antibiotic resistance genes after Hurricane Harvey’s flooding in Houston. Environ Sci Technol Lett 5(8):481–486, 10.1021/acs.estlett.8b00329. [DOI] [Google Scholar]
- Zartarian V, Xue J, Tornero-Velez R, Brown J. 2017. Children’s lead exposure: a multimedia modeling analysis to guide public health decision-making. Environ Health Perspect 125(9):097009, PMID: 28934096, 10.1289/EHP1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zodrow KR, Li Q, Buono RM, Chen W, Daigger G, Dueñas-Osorio L, et al. 2017. Advanced materials, technologies, and complex systems analysis: emerging opportunities to enhance urban water security. Environ Sci Technol 51(18):10274–10281, PMID: 28742338, 10.1021/acs.est.7b01679. [DOI] [PubMed] [Google Scholar]